Abstract
Background:
Mindfulness in Motion is an 8-week mindfulness-based intervention that uses yoga movement, mindfulness meditation, and relaxing music. This study examined the feasibility of using Mindfulness in Motion in people with multiple sclerosis (MS) and the effect of this program on stress, anxiety, depression, fatigue, and quality of life in people with MS.
Methods:
Twenty-two people with MS completed the 8-week mindfulness program as well as assessments 1 week before and after the intervention.
Results:
Pre/post comparison of four self-reported questionnaires—the Mental Health Inventory, 36-item Short Form Health Status Survey, Modified Fatigue Impact Scale, and Five Facet Mindfulness Questionnaire—showed significant improvement in physical functioning, vitality, and mental health. Specifically, improvements were seen in anxiety, depression, and positive affect; cognitive, psychosocial, and overall functioning regarding fatigue; and mindfulness in the areas of observing, acting with awareness, nonjudgment, and nonreactivity.
Conclusions:
Due to the uncertainty in disease progression associated with MS, and the multiplicity of mental and physical symptoms associated with it, programming that addresses anxiety, depression, and fatigue is a key area of future research in MS disease management. Mindfulness in Motion proved to be a feasible program yielding positive results, supporting the need for research to determine the extent to which the program can improve quality-of-life outcomes for people with MS.
Multiple sclerosis (MS) is a neurologic disorder that can have a major effect on quality of life (QOL) because it can negatively affect physical function, cognitive ability, and emotional health.1–5 This disorder affects 400,000 people in the United States and more than 2 million worldwide.6 There is no known cause or cure for this condition, and symptoms may include cognitive impairment; compromised mobility; chronic pain; sensory disturbance; bladder, bowel, and sexual dysfunction; and many others. Along with the physical impairments that can arise for those afflicted by MS, emotional distress takes a huge toll.3,4,7–15
A diagnosis of MS comes with a plethora of uncertainties relating to disease progression and spontaneous symptoms that can greatly decrease QOL. Coping with a diagnosis of any kind can be accompanied by depression; however, with an MS diagnosis, depression rates are three times higher than in the general population, with a lifetime depression rate of just more than 50% in people with MS.2,7,9,10 The implication of this statistic is far-reaching because depression is often regarded by people with MS as a significant determinant of QOL.5,7,11,14,15 This rate may be so high due to a combination of factors that may promote depressive symptoms, including the possible demyelination of nerves transmitting mood signals.9 Recent studies have found a complex relationship between depression and fatigue, another common symptom of MS.9,12 The results of a recent study suggest that changes in mood due to treatment for depression are associated with reduced severity of fatigue symptoms based on self-report from people with MS.12 Fatigue related to MS is unique and prevalent, occurring in 80% of people with MS. Fatigue can range from mild to severe and can have a drastic negative effect on ability to function in various roles at work and at home.13 Fatigue is frequently a disabling symptom for people with MS and is often ranked highest as the most distressing and disruptive symptom.15 Because of the toll on QOL, depression and fatigue are important areas of symptom management.5,7,8,11,12,14
Lifestyle choices incorporating mind-body therapies such as yoga and meditation hold a promise of hope for ameliorating these symptoms.4,5,8,16 Mind-body modalities are not each distinctly separate categories, and many cross over, as is the case with yoga and meditation.4 Yoga techniques may be useful in decreasing the emotional distress of disease diagnosis and health-related changes.4,17 Although a variety of studies have shown yoga to be safe and effective for improving physical function and mood states, only a handful of studies to date have been specific to MS and yoga, and only a few others to mindfulness meditation and MS.4,5,8,18–29 In addition, because MS is thought to be exacerbated by stress,1 interventions such as yoga and mindfulness-based interventions can help break patterns of excessive worry, rumination, and stress that are linked to depression and anxiety.4,16,17,30–32 Indeed, in a recent survey of 1110 people with MS, 32% of those who had used mind-body therapies found them to be beneficial.4
According to the National Center for Complementary and Integrative Health, “mind and body practices focus on the interactions between the mind and body, and how their relationship affects health and wellbeing.”33(p 8) Recent neuroscientific research has shown an association between meditation and neuroplasticity of the brain.34 Studies of long-term meditators have found increased cortical thickness35 and increased gray matter density in the brainstem (associated with cardiorespiratory control),36 hippocampus, and frontal areas (associated with emotional regulation and response control).37 Additional research on participants new to meditation has shown increases in areas of the hippocampus (associated with learning and memory)38 and increases in white matter (which is strongly involved in interconnecting brain areas).39 These findings are important because MS causes demyelination and axonal loss of the central nervous system.2 Despite these research findings, there are limited published studies using meditation or mindfulness training for people with MS.8,18,27,28 Studies using mindfulness practices or yoga for people with MS have found statistically significant improvements in QOL,5,8,19,20 reduced depression,8,21,22 reduced anxiety,8,22,23 reduced fatigue,8,18,22,24,25 increased selective attention performance,26 improved coping skills, reduced perceived stress, and increased resilience,20,27 improvements in physical mobility and balance,22,28 pain reduction,18,29 and improved overall physical and mental health.18,19
Because the unpredictable nature of MS is associated with high levels of anxiety, depression, and fatigue, mind-body therapies such as yoga and meditation may be helpful in promoting health by reducing psychological stress.4 One such program, Mindfulness in Motion, which combines yoga, mindfulness meditation, and relaxing music, has been shown to be an effective low-cost stress-reduction intervention to improve quality of sleep and perceived stress in healthy adults.40,41 Mindfulness in Motion has also effectively decreased biologic markers of sympathetic nervous system activation for health-care professionals working on a surgical intensive care unit,42 lowered elevated levels of inflammation (C-reactive protein levels) in nonobese people at risk for cardiovascular disease compared with randomized controls,43 and showed changes in brain function in older adults compared with randomized controls.44 The study reported herein tested the feasibility of Mindfulness in Motion for people with MS to determine whether they could perform the minimal yogic movement integral to the intervention and to assess QOL measures for this population to design suitable outcome measures for a future trial using the program for people with MS. To our knowledge, Mindfulness in Motion has not previously been used with this population.
Methods
Sample Population
On approval from the institutional review board of the University of Minnesota (Minneapolis), a convenience sample of 25 adults (aged ≥18 years) diagnosed as having any type of MS were recruited to participate in the Mindfulness in Motion program offered at a local community agency. Participants were recruited via fliers in the neurology department of a local medical center (Essentia Health, Duluth, MN), the Multiple Sclerosis Achievement Center at Benedictine Health Center (Duluth, MN), and local support groups. In addition, recruitment telephone calls were made to individuals who were on the contact list for the Multiple Sclerosis Achievement Center. Participants registered for the program for one of two weekly offerings and completed an approved informed consent form and liability waiver 1 week before the intervention.
Mindfulness in Motion Intervention
Mindfulness in Motion is an 8-week program that meets once per week for 1 hour. During this group hour, relaxing piano music is played as background, a mindfulness theme of the week is introduced via an educational PowerPoint presentation by the trained instructor, participants have a short group discussion relating to the theme, and the hour program concludes with 20 minutes of gentle stretching, mindfulness meditation, and chair yoga relaxation. In addition to the weekly group sessions, participants are expected to individually pursue a 20-minute daily mindfulness practice using CDs or MP3s.40
Study Design
Mindfulness in Motion is an evidence-based mindfulness intervention. This study was designed to determine 1) the feasibility of using Mindfulness in Motion for adults with MS and 2) the effect of the program on anxiety, depression, fatigue, and QOL in people with MS to design suitable outcome measures for a future trial.45 Because this study was a feasibility study, attempting to explore the power needed to see an effect, a power analysis was not conducted before the feasibility study. Quantitative surveys were given 1 week before and 1 week after the 8-week intervention. The assessments were completed with little or no intervention from the interviewer. Some participants with visual or upper-extremity disability were given these assesments in an interview format. The principal investigator of the study trained staff from the day service program as volunteers to help administer the surveys. The instruments took 45 minutes to complete and were used to assess the program's influence on mindfulness, QOL, anxiety, depression, and fatigue. Surveys included a demographic questionnaire, the Mental Health Inventory (MHI),15 the 36-item Short Form Health Status Survey (SF-36),15 the Modified Fatigue Impact Scale (MFIS),15 and the Five Facet Mindfulness Questionnaire (FFMQ).46 Attendance at weekly group meetings was recorded by the Mindfulness in Motion instructor, and mindfulness home practice was self-reported; these data were used to assess the feasibility of study adherence.
The MHI
The full-length MHI included 18 questions in four subscales (anxiety, depression, behavior control, and positive affect) and a total score. The possible range of mean scores is 1 to 6, and the possible range of the total scores is 0 to 100, with a higher score indicating better mental health. Reports from the National Multiple Sclerosis Society show that the full version has a Cronbach α value of 0.93. It takes 5 to 10 minutes to complete this 6-point Likert scale assessment.15
The SF-36
The SF-36 contains 36 items divided into eight subscales (physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health). Higher scores indicate better health. Cronbach α values for these subscales range from 0.67 to 0.94. It takes approximately 10 minutes to complete this 5-point Likert scale assessment.15
The MFIS
The full-length version of the MFIS contains 21 items that measure how fatigue affects a person diagnosed as having MS. The MFIS provides an assessment of fatigue effects in terms of physical, cognitive, and psychosocial functioning. A higher score indicates a greater impact of fatigue on a person's activities. This assessment has a Cronbach α value of 0.81. It takes 5 to 10 minutes to complete this 5-point Likert scale assessment.15 The MHI, SF-36, and MFIS have been shown to be reliable and valid in MS populations.15
The FFMQ
The FFMQ contains 39 items in a 5-point Likert scale that assesses overall mindfulness through five facets: observing, describing, acting with awareness, accepting without judgment, and nonreactivity.46,47 The FFMQ has internal consistency scores that range from 0.76 to 0.91 for the mindfulness subscales. Higher scores indicate greater levels of trait mindfulness.5,46,47 This instrument has been found to have adequate to good construct validity.47 The FFMQ has been used, or recommended, in a few studies of people with MS.5,20,48,49
Statistical Analysis
A statistical software program (IBM SPSS Statistics for Windows, version 20.0; IBM Corp, Armonk, NY) was used to analyze quantitative data. Analyses included outcome differences between sex, age, and length of time with MS; any previous experience with mindfulness training or yoga practice; and previous participation in the day service program or other MS outreach programs. Repeated measures analysis of variance was performed for within-subject (pretest and posttest) effects with each instrument (MHI, SF-36, MFIS, and FFMQ) to determine whether there was a relationship between the independent variable (Mindfulness in Motion program) and the dependent variables (QOL outcomes).
Results
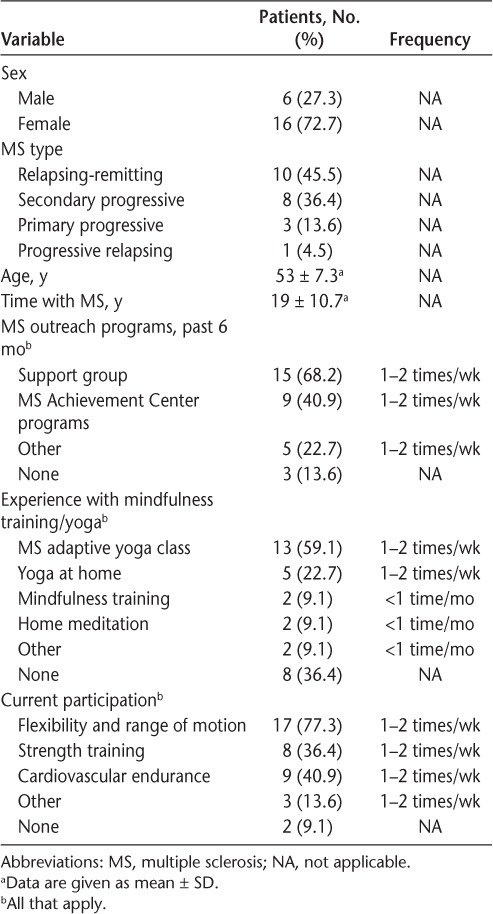
Demographic information is displayed in Table 1. Three participants were excluded from data analysis due to missing pretest or posttest survey information. Twenty-two participants were included in the data analysis. All types of MS were represented in this study. Most of the participants had little to no previous experience with meditation; only two had any formal mindfulness training. However, many patients (n = 13) had participated in an MS adaptive yoga class one to two times per week. In addition, 15 patients had participated in a support group in the previous 6 months.
Table 1.
Characteristics, MS history, and practice participation of the 22 study patients
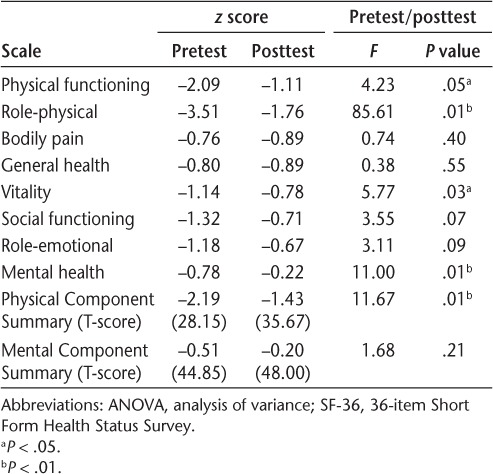
As shown in Table 2, Mindfulness in Motion participants demonstrated statistically significant changes on several of the SF-36 variables, specifically, physical functioning, role-physical, vitality, and mental health. The results of two summary scales were also analyzed, and the scoring of both summary scales involved three steps: 1) standardization of the eight SF-36 subscales, 2) weighting and aggregation of the eight subscales, and 3) transformation of the aggregate scale score to a T-score. The Physical Component Summary scale T-score increase was statistically significant after the program, but the increase in the Mental Component Summary scale T-score was not statistically significant.
Table 2.
Repeated measures ANOVA (pretest and posttest): SF-36
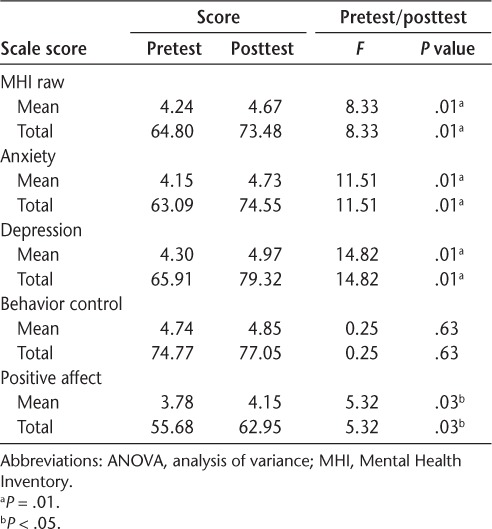
As shown in Table 3, the analysis of variance results of the MHI revealed statistically significant improvements after the 8-week program in the MHI total scores and in the subscales of anxiety, depression, and positive affect; in contrast, the increase in behavioral control was not statistically significant.
Table 3.
Repeated measures ANOVA (pretest and posttest): MHI
The MFIS has three subscales—physical, cognitive, and psychosocial—that are combined to formulate the total MFIS score.15 Postprogram assessments showed statistically significant improvements in the cognitive and psychosocial subscales and the total MFIS score; in contrast, improvement in the physical subscale was not statistically significant (Table 4).
Table 4.
Repeated measures ANOVA (pretest and posttest): MFIS and FFMQ
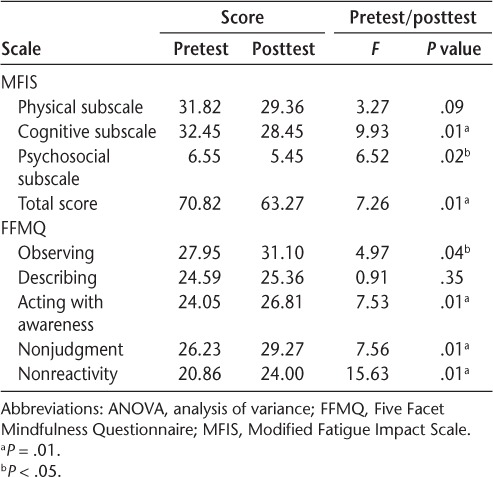
Results of the FFMQ indicated statistically significant improvement in the categories of observing, acting with awareness, nonjudgment, and nonreactivity. The increase in the describing factor was not statistically significant (Table 4).
Study participants were able to perform the gentle yoga movement included in Mindfulness in Motion. Half of the participants (n = 11) attended at least five of the eight sessions (62.5%) and completed at least 4 of 7 days (57.1%) each week of the home practice logs. These participants had greater improvements, specifically in MHI total scores including anxiety, depression, behavior control, and positive affect, compared with the other half of participants who attended four or fewer sessions and did fewer than 4 days a week of home practice logs. However, the differences were not statistically significant. Day of the week was also a nonsignificant moderator on any scale because the protocol and trained instructor were the same in all sessions.
Discussion
People with MS were able to fully participate in the Mindfulness in Motion program, attended the 8-week program at an overall rate of 75%, did the daily mindfulness practice on their own, and, on program conclusion, showed changes in symptoms of MS. Outcome measures were appropriate for the population and indicated that the program lessened bothersome symptoms for people with MS.
Participants demonstrated statistically significant changes on several of the SF-36 variables, specifically, physical functioning, role-physical, vitality, and mental health. These positive results are important given that declines in physical function and mental health are hallmark symptoms of MS.2–4,6–15 Study results also showed a significant improvement in cognitive, psychosocial, and overall functioning regarding fatigue. This is important due to fatigue's prevalence, intensity, and effect on QOL for people with MS.13–15 These results align with those of a recent pilot study of patients who had either MS or peripheral neuropathy and completed an 8-week mindfulness training compared with those who received standard care. In that study, the SF-36 and MFIS showed significant improvements in overall physical and mental health components, improvements in vitality and role-physical, and improvements in cognitive and psychosocial areas of fatigue.18 The significant improvement in vitality in this study and others is important because the vitality score can be used as an independent measure of fatigue.15 This finding supports the work of Oken et al.,24 who studied the effects of a weekly 90-minute Iyengar yoga session or an exercise class with stationary bicycles for people with MS. This 6-month study found that both exercise and yoga statistically significantly improved vitality scores and reduced fatigue. However, the effect on mood was not statistically significant.24
Using Mindfulness in Motion, we found that mental health did improve, specifically, in anxiety, depression, and positive affect. Improvements in mood are noteworthy because MS is associated with mental health conditions that decrease QOL.5,7,9–12 The possible cognitive impairments associated with MS can greatly impact day-to-day living experiences and can “lead to depression, low-self-esteem, and impaired social functioning.”3(p 1258) The present results corroborate those of the study by Grossman et al.,8 which found statistically significant improvements in QOL and reduced depression, anxiety, and fatigue with an 8-week mindfulness-based stress reduction program (n = 74) compared with usual care (n = 74) in people with MS. Because a central piece of Mindfulness in Motion is the yoga movement, it is important to note that other interventions using yoga as the primary intervention have also found improvements in mental and physical health for people with MS.21,22,24–29
Mindfulness in Motion uniquely combines yoga and mindfulness, attempting to glean the benefits of both of these mind-body approaches.40 In the present study, improvements in mindfulness were demonstrated specifically in the areas of observing, acting with awareness, nonjudgment, and nonreactivity. These findings were congruent with a study of healthy males that found that mindfulness, specifically, nonreactivity to inner experience, reduces vulnerability to depression by buffering against rumination and negativity bias and by reducing automatic emotional response.16 Several other studies have used self-reported questionnaires to study mindfulness and potential benefits for people with MS. The FFMQ can be used to assess overall mindfulness or trait mindfulness, which is “a personality characteristic associated with psychological well-being.”5,20(p 104),46,47 The most recent study found higher levels of trait mindfulness to be associated with higher QOL, effective coping skills, reduced psychological stress, and increased resilience in people with MS (n = 119).5,20 Another study found that higher levels of trait mindfulness were associated with higher levels of positive affect and relationship satisfaction and lower levels of anxiety symptoms for couples coping with MS.23 The present study's finding of improved positive affect and reduced anxiety may also be related to improvements in mindfulness. Taken together, the positive findings from the SF-36, MFIS, MHI, and FFMQ support various improvements to QOL.15 This is important because QOL can be affected by physical, cognitive, and emotional symptoms associated with MS.1,4,5,11,14
Mindfulness in Motion uses music and more yoga stretches than traditional mindfulness-based stress reduction, was created for working adults with limited time, and was hypothesized to be effective for people with MS.40 Our hypothesis was confirmed in this feasibility study, which yielded significant improvements in both physical and mental health for people with MS compared with studies using mindfulness interventions that were much more time-intensive.
This study has several limitations. Recruitment was based on self-selection into the study, affecting study success because participants may have had an affinity for a mindfulness-based program. There was no active control group because this was a feasibility study to determine the appropriateness of Mindfulness in Motion for people with MS. Without a control group, improvements cannot be deemed to be the result of the intervention. The trained instructor was also a researcher on this study; therefore, participant responses may reflect a desire to please the researcher. Participants were not screened for psychological or pharmacologic treatment for depression at the onset or during the study. Common and unpredictable symptoms associated with MS, such as fatigue, can make a commitment to attend the intervention a challenge. Because some participants had difficulty attending the didactic sessions but still had positive results from participating in the home practice, more research is needed to determine which components of the program are most effective and can be adapted to meet the varying needs of individuals. The level of MS-related disability of the participants was unknown; therefore, the most effective time for interventions such as Mindfulness in Motion to be introduced to people with MS to provide the greatest benefit is unknown. Last, stress reduction is hypothesized to be an important mediator of the effects of mindfulness, yet stress was not assessed and needs to be assessed in future studies of the program in people with MS. Future studies need to include a control group, assessor blinding, people with the level of disability associated with MS, power size for adequate sample size, and long-term follow-up.4,48 In addition, because MS extends beyond the person diagnosed as having MS, by adding to financial concerns for the family unit and adding possible caretaking responsibilities, the support individuals for people with MS could be included in future Mindfuless in Motion interventions.23,48
To our knowledge, this study is the first empirical research examining the feasibility of the Mindfulness in Motion program for people with MS, exploring its potential effect on common symptoms of MS, specifically, anxiety, depression, fatigue, and QOL. This study adds to the growing body of research supporting the benefit of mindfulness and yoga in helping people with MS cope with physical, cognitive, and emotional symptoms.4,5,8,17–29 Combining the benefits of yoga and mindfulness, Mindfulness in Motion was found to be a feasible program for people with MS, and this study indicated the appropriateness of the measures used and showed positive improvements in symptoms associated with MS.
PracticePoints
Stress is considered a possible trigger for exacerbating MS. Therefore, learning techniques that promote stress reduction is important in dealing with an MS diagnosis and managing the prevalent mental health conditions of anxiety and depression.
Another prevalent, distressing, and disruptive symptom of MS is haphazard and intense levels of fatigue. Depression and fatigue have a negative effect on quality of life for people with MS.
Mindfulness in Motion yielded positive results in this feasibility study, indicating that the pragmatic resiliency skills of mindfulness training may be beneficial in helping to mitigate unpleasant and unpredictable mental and physical symptoms that are associated with an MS diagnosis.
Financial Disclosures
The authors have no conflicts of interest to disclose.
Funding/Support
The Miller-Dwan Foundation's Van Gorden New Initiative Fund provided this project with funding to purchase participant workbooks, CD/DVD sets, study materials, and participant incentives.
References
- 1. Mohr DC, Hart SL, Julian L, Cox D, Pelletier D.. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004; 328: 731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Holland NJ, Murray TJ, Reingold SC.. Multiple Sclerosis: A Guide for the Newly Diagnosed. 3rd ed. New York, NY: Demos Medical Publishing; 2007. [Google Scholar]
- 3. Prakash RS, Snook EM, Lewis JM, Motl RW, Kramer AF.. Cognitive impairments in relapsing-remitting multiple sclerosis: a meta-analysis. Mult Scler. 2008; 14: 1250– 1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Senders A, Wahbeh H, Spain R, Shinto L.. Mind-body medicine for multiple sclerosis: a systematic review. Autoimmune Dis. 2012; 2012: 567324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schirda B, Nicholas JA, Prakash RS.. Examining trait mindfulness, emotion dysregulation, and quality of life in multiple sclerosis. Health Psychol. 2015; 34: 1107– 1115. [DOI] [PubMed] [Google Scholar]
- 6. National Multiple Sclerosis Society. . Multiple sclerosis: just the facts. http://www.nationalmssociety.org/nationalmssociety/media/msnationalfiles/brochures/brochure-just-the-facts.pdf. Accessed December 14, 2015.
- 7. Feinstein A. Multiple sclerosis and depression. Mult Scler J. 2011; 17: 1276– 1281. [DOI] [PubMed] [Google Scholar]
- 8. Grossman P, Kappos L, Gensicke H, . et al. MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology. 2010; 75: 1141– 1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Siegert RJ, Abernethy DA.. Depression in multiple sclerosis: a review. J Neurol Neurosurg Psychiatry. 2005; 76: 469– 475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sadovnik AD, Remick RA, Allen J, . et al. Depression and multiple sclerosis. Neurology. 1996; 46: 628– 632. [DOI] [PubMed] [Google Scholar]
- 11. D'Alisa S, Miscio G, Baudo S, Simone A, Tesio L, Mauro A.. Depression is the main determinant of quality of life in multiple sclerosis: a classification-regression (CART) study. Disabil Rehabil. 2006; 28: 307– 314. [DOI] [PubMed] [Google Scholar]
- 12. Mohr DC, Hart SL, Goldberg A.. Effects of treatment for depression on fatigue in multiple sclerosis. Psychosom Med. 2003; 65: 542– 547. [DOI] [PubMed] [Google Scholar]
- 13. National Multiple Sclerosis Society. . Fatigue. http://www.nationalms-society.org/Symptoms-Diagnosis/MS-Symptoms/Fatigue#section-0. Accessed February 22, 2016.
- 14. Janardhan V, Bakshi R.. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002; 205: 51– 58. [DOI] [PubMed] [Google Scholar]
- 15. Ritvo P, Fischer JS, Miller DM, . et al. Multiple Sclerosis Quality of Life Inventory: A User's Manual. New York, NY: National Multiple Sclerosis Society; 1997. [Google Scholar]
- 16. Paul NA, Stanton SJ, Greeson JM, Smoski MJ, Wang L.. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Soc Cogn Affect Neurosci. 2013; 8: 56– 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McCall T. Yoga as Medicine: The Yogic Prescription for Health and Healing. New York, NY: Bantam Books; 2007. [Google Scholar]
- 18. Tavee J, Rensel M, Planchon SM, Butler RS, Stone L.. Effects of meditation on pain and quality of life in multiple sclerosis and peripheral neuropathy: a feasibility study. Int J MS Care. 2011; 13: 163– 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Levin AB, Hadgkiss EJ, Weildand TJ, . et al. Can meditation influence quality of life, depression, and disease outcome in multiple sclerosis? findings from a large international web-based study. Behav Neurol. 2014; 2014: 916519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Senders A, Bourdette D, Hanes D, Yadav V, Shinto L.. Perceived stress in multiple sclerosis: the potential role of mindfulness in health and well-being. J Evid Based Complementary Altern Med. 2014; 19: 104– 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rahnama N, Namazizadeh M, Etemadifar M, Bambaeichi E, Arbabzadeh S, Sadeghipour HR.. Effects of yoga on depression in women with multiple sclerosis. J Isfahan Med School. 2011; 29: 483– 490. [Google Scholar]
- 22. Ahmadi A, Arastoo AA, Nikbakht M, Zahednejad S, Rajabpour M.. Comparison of the effect of 8 weeks aerobic and yoga training on ambulatory function, fatigue and mood status in MS patients. Iran Red Cresc Med J. 2013; 15: 449– 454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pakenham K, Samios C.. Couples coping with multiple sclerosis: a dyadic perspective on the roles of mindfulness and acceptance. J Behav Med. 2013; 36: 389– 400. [DOI] [PubMed] [Google Scholar]
- 24. Oken BS, Kishiyama S, Zajdel D, . et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004; 62: 2058– 2064. [DOI] [PubMed] [Google Scholar]
- 25. Garrett M, Hogan N, Larkin A, Saunders J, Jakeman P, Coote S.. Exercise in the community for people with minimal gait impairment due to MS: an assessor-blind randomized controlled trial. Mult Scler J. 2013; 19: 782– 789. [DOI] [PubMed] [Google Scholar]
- 26. Velikonja O, Čurić K, Ožura A, Jazbec SŠ.. Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin Neurol Neurosurg. 2010; 112: 597– 601. [DOI] [PubMed] [Google Scholar]
- 27. Pritchard M, Elison-Bowers P, Birdsall B.. Impact of integrative restoration (iRest) meditation on perceived stress levels in multiple sclerosis and cancer outpatients. Stress Health. 2010; 26: 233– 237. [Google Scholar]
- 28. Mills N, Allen J.. Mindfulness of movement as a coping strategy in multiple sclerosis: a feasibility study. Gen Hosp Psychiatry. 2000; 22: 425– 431. [DOI] [PubMed] [Google Scholar]
- 29. Doulatabad SN, Nooreyan K, Doulatabad AN, Noubandegani ZM.. The effects of pranayama, hatha and raja yoga on physical pain and the quality of life of women with multiple sclerosis. Afr J Tradit Complement Altern Med. 2012; 10: 49– 52. [PMC free article] [PubMed] [Google Scholar]
- 30. Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. 15th ed. New York, NY: Bantam Dell; 2009. [Google Scholar]
- 31. Desrosiers A, Vine V, Curtiss J, Klemanski DH.. Observing nonreactively: a conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. J Affect Disord. 2014; 165: 31– 37. [DOI] [PubMed] [Google Scholar]
- 32. Hazlett-Stevens H. Mindfulness-based stress reduction for comorbid anxiety and depression: case report and clinical considerations. J Nerv Ment Dis. 2012; 200: 999– 1003. [DOI] [PubMed] [Google Scholar]
- 33. Gordon JS, Hart P, Delagran L.. Overview of mind/body therapies and practices [online module]. Center for Spirituality & Healing web-site. http://www.cshmodules.umn.edu/Integrativehealingpractices/over_rlo__sq_splash.html. Accessed July 21, 2017.
- 34. Davidson RJ, Lutz A.. Buddha's brain: neuroplasticity and meditation. IEEE Signal Process Mag. 2008; 25: 176– 174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lazar SW, Kerr CE, Wasserman RH, . et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005; 16: 1893– 1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vestergaard-Poulsen P, van Beek M, Skewes J, . et al. Long-term meditation is associated with increased gray matter density in the brain stem. Neuroreport. 2009; 20: 170– 174. [DOI] [PubMed] [Google Scholar]
- 37. Luders E, Toga AW, Lepore N, Gaser C.. The underlying anatomical correlates of long-term meditation: larger hippocampal and frontal volumes of gray matter. Neuroimage. 2009; 45: 672– 678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hölzel BK, Carmody J, Vangel M, . et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011; 191: 36– 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tang Y-Y, Lu Q, Fan M, Yang Y, Posner MI.. Mechanisms of white matter changes induced by meditation. Proc Natl Acad Sci U S A. 2012; 109: 10570– 10574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Klatt M, Steinberg B, Duchemin AM.. Mindfulness in Motion (MIM): an onsite mindfulness based intervention (MBI) for chronically high stress work environments to increase resiliency and work engagement. J Vis Exp. 2015; 101: e52359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Klatt MD, Buckworth J, Malarkey WB.. Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Educ Behav. 2009; 36: 601– 614. [DOI] [PubMed] [Google Scholar]
- 42. Duchemin A, Steinberg BA, Marks DR, Vanover K, Klatt M.. A small randomized feasibility study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary α-amylase levels. J Occup Environ Med. 2015; 57: 393– 399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Malarkey WB, Jarjoura D, Klatt M.. Workplace based mindfulness practice and inflammation: a randomized trial. Brain Behav Immun. 2013; 27: 145– 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Prakash RS, De Leon AA, Klatt M, Malarkey W, Patterson B.. Mindfulness disposition and default-mode network connectivity in older adults. Soc Cogn Affect Neurosci. 2012; 8: 112– 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Arain M, Campbell MJ, Cooper CL, Lancaster GA.. What is a pilot or feasibility study? a review of current practice and editorial policy. BMC Med Res Methodol. 2010; 10: 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Baer RA, Smith GT, Hopkins J, Kreitemeyer J, Toney L.. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006; 13: 27– 45. [DOI] [PubMed] [Google Scholar]
- 47. Baer RA, Smithy GT, Lykins E, . et al. Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment. 2008; 15: 329– 342. [DOI] [PubMed] [Google Scholar]
- 48. Carletto S, Borghi M, Francone D, . et al. The efficacy of a mindfulness based intervention for depressive symptoms in patients with multiple sclerosis and their caregivers: study protocol for a randomized controlled clinical trial. BMC Neurol. 2016; 16: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hocaloski S, Elliot S, Brotto LA, Breckon E, McBride K.. A mindfulness psychoeducational group intervention targeting sexual adjustment for women with multiple sclerosis and spinal cord injury: a pilot study. Sex Disabil. 2016; 34: 183– 198. [Google Scholar]


