Summary
Objective
This review and meta‐analysis aim at updating a previous meta‐analysis carried out by Waters et al. on the efficacy of interventions aimed at preventing childhood obesity and at identifying predictors of outcome.
Methods
Using an ad‐hoc search string, PubMed database was searched for studies assessing body mass index reduction associated with programmes lasting ≥12 weeks in overweight and obese children aged 2–18 years. Studies designed for children with eating disorders or relevant comorbidities were excluded. Studies meeting inclusion criteria were classified according to patient age (<6, 6–12 and 13–18 years), and intervention type (physical activity, diet or both), setting (educational, family or both) and duration (≤1 or >1 year). The search was also extended to other databases. Hand‐searching techniques were also applied. The Cochrane ‘risk of bias’ was applied for quality assessment.
Results
Seventy‐two studies were meta‐analysed. Overall, the best results were achieved by programmes combining diet and physical activity (n = 39). With regard to the setting, programmes involving both school and family and lasting ≤1 year were the most efficacious for 6‐ to 12‐year‐old children (n = 26); family‐based‐only interventions were also effective in children <6 years old (n = 2), although results have to be interpreted cautiously because of the small number of patients enrolled and the high study heterogeneity. In 13‐ to 18‐year‐old patients, interventions delivered at school (n = 8) were substantially unsuccessful.
Conclusions
Interventions for childhood obesity prevention should include both diet and physical activity, be preferentially targeted towards school age children and involve both the school and family setting. However, because of the important methodological limitations associated with currently available literature, additional studies are needed to draw definite conclusions.
Keywords: Childhood obesity, diet, educational programmes, physical activity
Introduction
In the last decades, overweight and obesity have exponentially grown worldwide, in both genders and across all ethnicities, reaching epidemic proportions in adults 1 but also in adolescents and children 2, 3, 4, 5. Approximately 24% and 13% of the paediatric population is currently over the body mass index (BMI) standards for age and sex in developed and developing countries, respectively 1. Alarming increasing trends have been observed in developing countries, while rates tend to gradually decrease or be stable in Europe, USA and Australia 1.
Childhood obesity predisposes to adult obesity 6, 7, 8 but also early‐onset and late‐onset cardiovascular and metabolic diseases (i.e. hypertension, atherogenic dyslipidemia and type 2 diabetes 9, 10, 11, 12, 13); pulmonary 14, hepatic 15, renal 16 and musculoskeletal complications 17, 18; and premature death 19. Finally, it has been associated with poor health‐related quality of life because of social stigmatization 20, 21 and negative emotional states (i.e. diminished perception of health and self‐esteem).
Once established, childhood obesity is very difficult to be reversed because of the poor long‐term compliance to lifestyle interventions. Moreover, a very limited number of efficacious drugs are available, and surgery is invasive and presents important side effects 22, 23.
Based on these evidences, the governments of several countries have implemented strategies to prevent childhood obesity through the promotion of healthy lifestyles in schools and primary care settings 24, 25, 26, 27, 28.
Waters et al. 24 recently revised and meta‐analysed data on the effectiveness of the various educational and lifestyle interventions aimed at preventing child obesity. After stratifying studies for programme context and duration and patient age, authors concluded about the overall effectiveness of the proposed interventions in reducing BMI, particularly of those targeting school‐aged children (6 to 12 years).
Study objective
The aims of the present study are (i) to update the results of a previous meta‐analysis by Waters et al. 24, including both RCTs and non‐randomized trials published up to June 2015; (ii) to confirm and define the effectiveness of specific interventions stratifying by patient age, and intervention setting and duration; and (iii) to conduct subgroup analyses to explore the effects of specific interventions in each age group.
Materials and methods
The definition of ‘overweight’ and ‘obesity’, based on BMI cut‐offs, has changed over time 29, 30, 31, 32. In this study, following Barlow et al. classification 30, ‘overweight’ was defined as a BMI between the 85th and 94th percentile for age and sex and ‘obesity’ as a BMI >95th percentile.
The standardized BMI (body mass index Z‐score or body mass index standard deviation score [BMI‐SDS]) was identified as the most appropriate outcome measure for the purpose of our analyses 24.
Literature search strategy was performed according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines 33 using a specific protocol.
A PICO(S) question based on the following components was developed:
P (population): obese and overweight children and adolescents;
I (intervention) and C (comparison): educational, lifestyle and health promotion; psychological and motivational interventions, directed to children/adolescents and/or their families, focusing on diet and/or physical activity;
O (outcome): obesity reduction, measured as reduction in standardized BMI score; and
(S) (study type): randomized and non‐randomized intervention studies.
After the proper identification of the major elements of the PICO question, natural language terms were translated to subject descriptors, Medical Subject Heading terms or descriptors. Terms in each field were selected by two readers (D. G. and F. G.). Any discrepancy in the selection of terms was addressed through discussion.
Literature search was performed using an ad‐hoc search string (Table S1) that expanded the one used by Waters et al. 24. PubMed database (http://www.ncbi.nlm.nih.gov/pubmed) was initially searched (last update 31 June 2015) to identify articles written in English comparing interventions to prevent paediatric obesity. The search was also extended to the Embase database (https://www.elsevier.com/solutions/embase‐biomedical‐research) and the Cochrane Library (http://www.cochranelibrary.com).
Two of the authors (D. G. and F. G.) independently identified relevant articles by abstract reading. To find additional studies of interest, the reference list of each paper retrieved was hand searched using the methods described by Greenhalg et al. 34
The inclusion and exclusion criteria and the algorithm followed for study retrieval and selection are reported in Figure 1. Briefly, interventions lasting ≥12 weeks, performed in overweight and obese children aged 2–18 years, were included. Studies designed for children with eating disorders or had relevant comorbidities were excluded.
Figure 1.
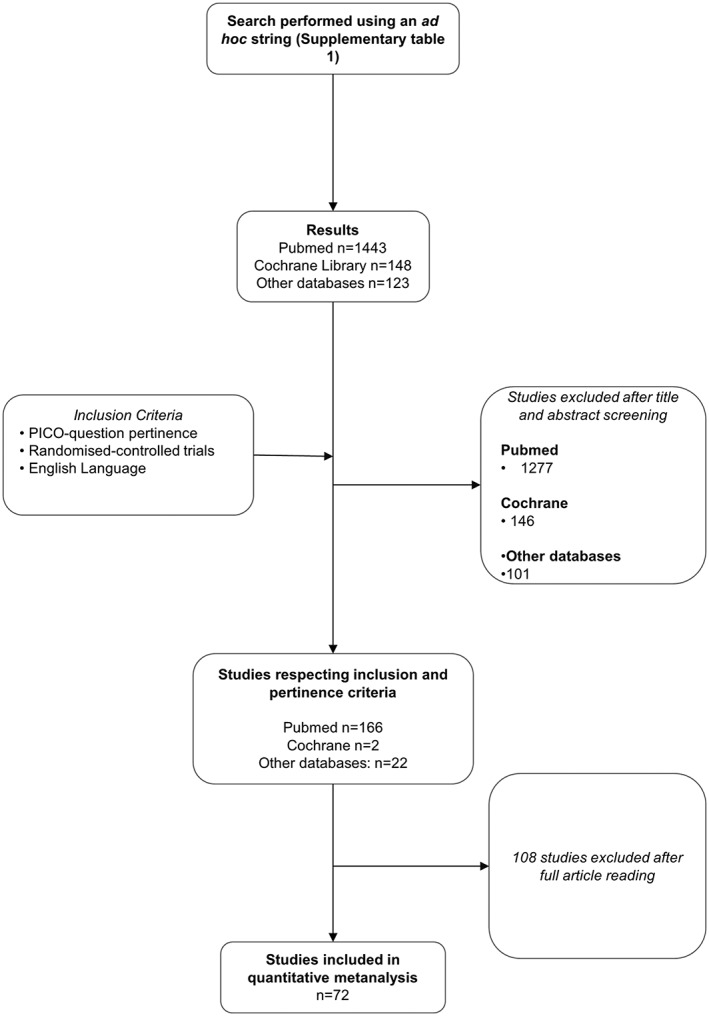
Flowchart showing the process of article selection.
Data extraction and selection
For each article that met inclusion criteria, two of the investigators (G. M. and S. C.) independently extracted: first author, year, country, sample size, description of the intervention, age group (<6, 6–12 and 13–18 years old), type of intervention (physical activity, diet or both), setting (educational, family or both), duration of the intervention (≤1 or >1 year) and change in BMI.
Statistical analysis
The meta‐analyses reported in this paper evaluated the effect of each type of intervention on BMI‐SDS reduction using revman version 5.2.11 (http://tech.cochrane.org/revman). Data entered in revman included pre‐change/post‐change in BMI‐SDS for the intervention and the control groups, the number of participants for each treatment group in the trial and standard deviations (SDs). In case of missing SD, the SD was estimated by imputing SDs of other studies using the same outcome measures.
First, the 37 studies included in Waters' meta‐analysis 24 were compared with the 35 of the studies published after February 2010. Then, data from all studies (n = 72) were analysed after stratifying by
patient age (<6, 6–12 and >12 years old);
intervention setting (educational setting, family or both);
type of intervention (physical activity, diet and combined); and
intervention duration (≤1 or >1 year).
These variables were selected among other possible modifiers of outcome, because they were considered of major interest for informing health professionals on preventive activities and health policymakers in planning preventive strategies.
A fixed‐effect model was initially used for the meta‐analyses. χ 2‐test was used to test mean subgroup differences in BMI‐SDS, and Z‐test was used to test the overall effect of interventions in specific subgroups. Heterogeneity was measured using I 2‐test. If significant heterogeneity was present (p < 0.05 from the χ 2‐test), a random‐effect model was used 35. The random effect model was also used when heterogeneity was not significant, but the number of studies was ≤5, as the test for heterogeneity is known to have low power when the number of studies is small. Forest plots were used to illustrate results from meta‐analyses 36. An I 2 between 50% and 90% was assumed as ‘substantial’ 37.
Study quality
The ‘risk of bias’ tool, developed by the Cochrane Collaboration 38, was applied to each study to identify potential biases of selection, performance, attrition, detection and reporting that could undermine study validity. The assessment was performed by two authors (G. M. and S. C.); disagreement was resolved by discussion. Additional meta‐analyses, including only high‐quality studies – defined using the risk of bias tool 41 – and comparing them to low‐quality studies, were lastly carried out.
Results
A total of 1,723 articles of potential interest were initially identified. Based on the pertinence of the abstract, 1,524 of them were excluded; the remaining 190 were read in extenso. Thirty‐five of them 22, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72 were considered pertinent (1 non‐randomized trial and 34 randomized controlled trial [RCT]) and were thus included in the meta‐analyses, together with the 37 studies (31 RCT and 6 non‐randomized trial) already included in Waters et al. meta‐analysis 24.
The main features of the studies included in the meta‐analyses are reported in Table S1. Eight studies included a dietary intervention (8 RCT), 22 an intervention based on physical activity (20 RCT and 2 non‐randomized clinical trial) and 42 both (37 RCT and 5 non‐randomized clinical trial). These interventions were compared with standard care, consisting of BMI assessment at specific time points and general recommendations on healthy lifestyles.
The dietary intervention, in the majority of the studies, consisted of a prescribed daily diet of 1,500 to 1,800 calories intake, with a balance of nutrients and calories across the day (i.e. breakfast, lunch, dinner and snacks). The most common way of monitoring diet adherence was carried out through a detailed nutrition diary, with feedback provided by the study dietician or the operator involved. In the majority of the studies, the nutritional interventions were carried out following recognized guidelines and with specifically trained operators. As far as physical activity interventions, most of the studies implemented programmes of 20/30 min medium‐intensity to high‐intensity physical activity, 5 to 7 times a week, mostly adopted in the school context or through information and recommendations to families.
When studies included in Waters' meta‐analysis 24 were compared with those published later, the more recent studies, although associated with a significant BMI reduction, proved to be significantly less effective than the older ones and more heterogeneous (−0.07 [−0.09, −0.05] vs. −0.14 [−0.18, −0.09]; χ 2 = 6.92, p < 0.001; Figure 2a,b).
Figure 2.
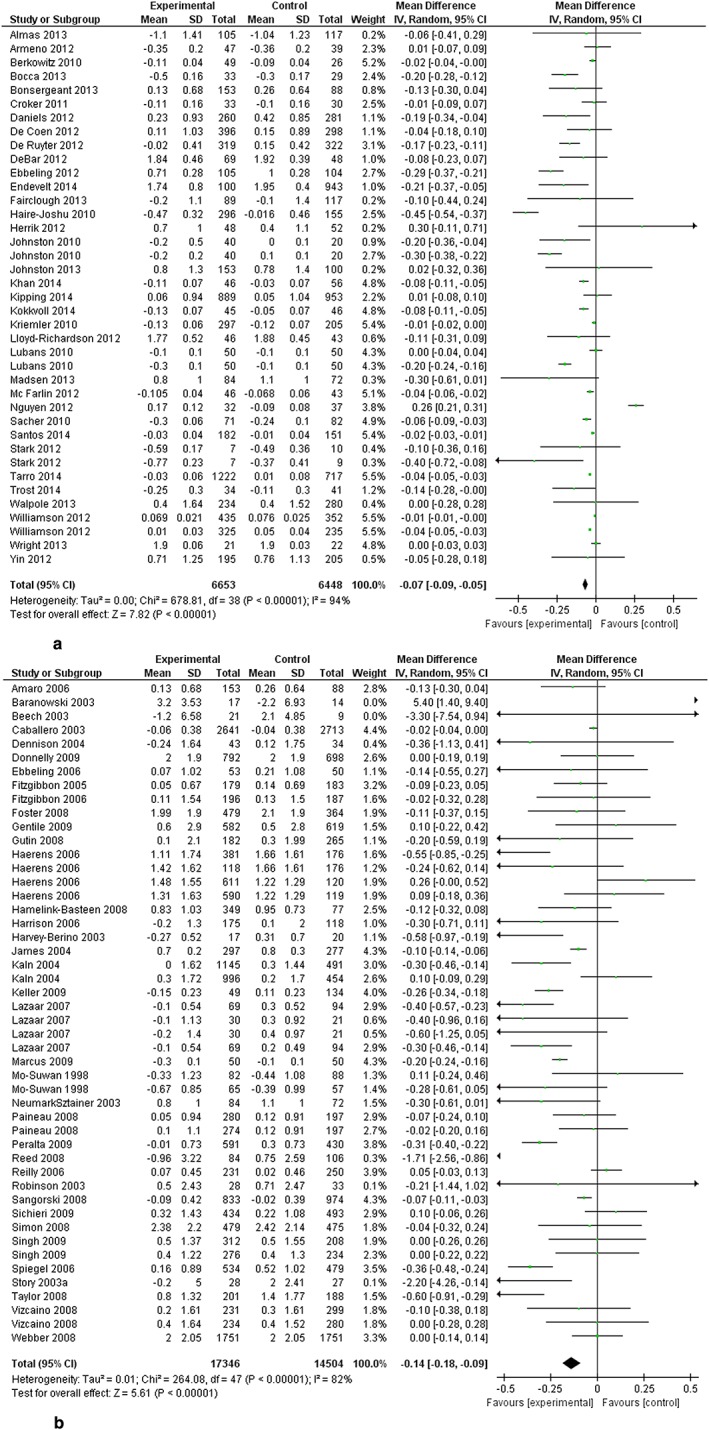
(a) Subgroup analysis of new studies included; (b) subgroup analysis of older studies already included in other meta‐analyses.
The meta‐analysis by age group revealed the strongest effect in children 6–12 years old (mean BMI reduction: −0.28 [−0.36, −0.20]). Weaker, although significant, effects were found in the groups aged 2–5 and 13–18 years old (−0.24 [−0.42, −0.06] and −0.26, [−0.41, −0.11], respectively). A moderate mean BMI‐SDS reduction was found for interventions based on physical activity or diet alone (−0.22 [−0.34, −0.11] and −0.17 [−0.30, −0.04], respectively), and a higher reduction was achieved by combined programmes (−0.29 [−0.38, −0.19]). Because the presence of a behavioural component was considered to play an important role in the determination of the efficacy of the intervention, an exploratory sensitivity subgroup analyses comparing interventions including and non‐including a behavioural component was performed. However, no significant differences between groups was identified (p = 0.66, I 2 = 0%) (Figure S2). Stratification by intervention setting pointed out the highest effectiveness of programmes delivered both at children's family and educational setting (i.e. schools or kindergartens) (mean BMI‐SDS reduction: −0.48 [−0.70, −0.26]), followed by interventions delivered only at family setting (−0.30 [−0.48, −0.11] and, lastly, at educational setting −0.22 [−0.34, −0.11]).
The intervention duration had also a strong impact on outcome: the mean BMI reduction associated with interventions lasting ≤1 year was almost twice higher than those lasting >1 year (−0.32 [−0.41, −0.24] vs. −0.17 [−0.30, −0.05]; χ 2 = 3.49, p < 0.01).
Subgroup analyses were conducted to explore the effects of specific interventions in each age group (Table 1). In children aged 2–5 years old, only four RCTs out of 10 studies reported the effectiveness of combined interventions. Family setting appeared more suitable than educational setting (Figure 3a,b) for this type of intervention (mean BMI‐SDS reduction: −0.36 [−0.65, −0.07], I 2 = 59% vs. −0.085 [−0.21, 0.0], I 2 = 0%, χ 2 = 3.0, p = 0.08, I 2 = 67%).
Table 1.
Summary of the main findings for the subgroup analysis
| Setting | Type of intervention | Age | |||||
|---|---|---|---|---|---|---|---|
| Preschool | School | Adolescents | |||||
| n | Significance | n | Significance | n | Significance | ||
| Family | Combined | 2 | * | 7 | NS | ||
| Diet | 2 | NS | |||||
| Physical activity | |||||||
| School | Combined | 2 | NS | 12 | * | 8 | NS |
| Diet | 3 | NS | |||||
| Physical activity | 14 | * | |||||
| Combined | Combined | 6 | * | 2 | NS | ||
| Diet | |||||||
| Physical activity | |||||||
Significant results found in the meta‐analysis.
n, number of studies; NS, no significant results found in the meta‐analysis.
Figure 3.
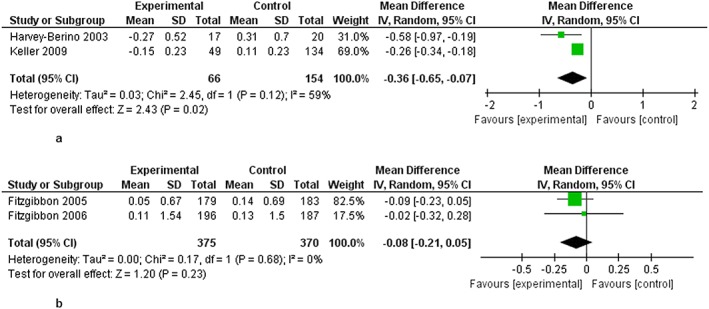
(a) Subgroup analysis of combined interventions in family setting in children <6 years; (b) subgroup analysis of combined interventions in educational setting in children <6 years.
In the age group 6–12 years, comprising 47 studies (65.3%) (41 RCT and 6 non‐randomized trials), diet alone was insufficient to significantly reduce BMI, regardless of the intervention setting. Physical activity was extremely effective when introduced in the educational setting, either alone (mean BMI‐SDS reduction: −0.13 [−0.19, −0.06], I 2 = 79%) or in association with diet (−0.11 [−0.16, −0.06], I 2 = 91%) (Figure 4a,b), but not in the family setting (−0.09 [−0.21, 0.03], I 2 = 83%). The best results were achieved by combined (diet + physical activity) interventions delivered in the family and educational settings (−0.15 [−0.22, −0.07], I 2 = 94%) (Figure 5).
Figure 4.
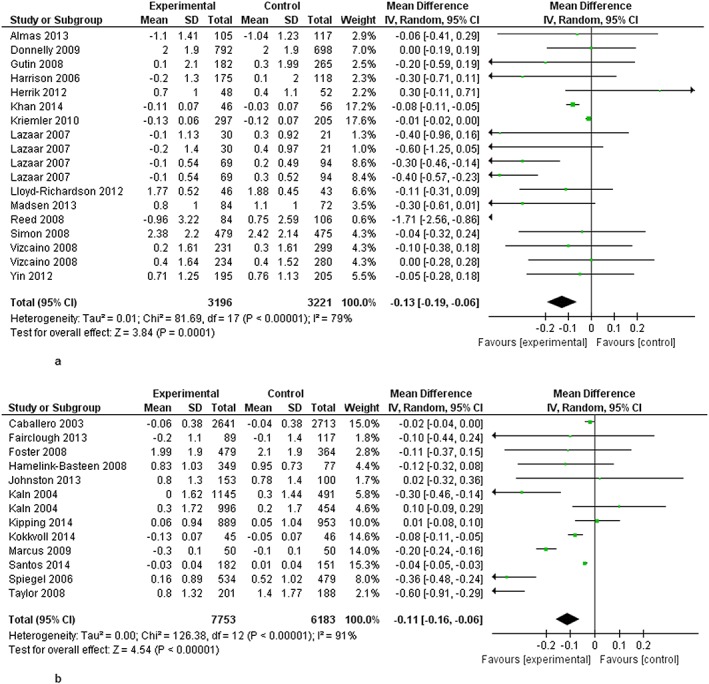
(a) Subgroup analysis of physical activity interventions in educational setting in children 6–12 years; (b) subgroup analysis of combined interventions in educational setting in children 6–12 years.
Figure 5.
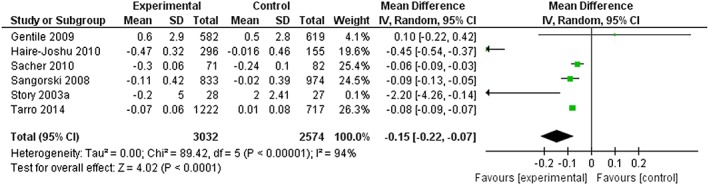
Subgroup analysis of combined interventions in combined settings in children 6–12 years.
In adolescents (age 13–18 years), combination interventions (diet + physical activity) delivered at educational or educational + family setting did not reduce the BMI significantly (Figure 6a,b).
Figure 6.
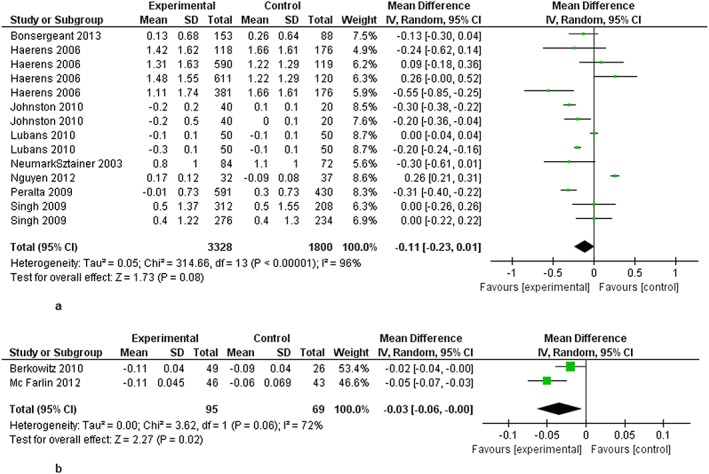
(a) Subgroup analysis of combined interventions in educational setting in adolescent >6–12 years; (b) subgroup analysis of combined interventions in combined settings in adolescent >6–12 years.
Lastly, stratification by study quality showed that, after excluding 31 studies with unknown risk of bias, a significant BMI‐SDS reduction was achieved only in the 29 studies with low risk (−0.10 [−0.12, −0.08]; Z = 9.44; p < 0.0001) and not in the 12 studies with high risk of bias (−0.07 [−0.17, 0.03]; Z = 1.41, p = 0.16) (Figure 7). No significant differences between subgroups were identified (p = 0.66, I 2 = 0%) (Figure S1).
Figure 7.
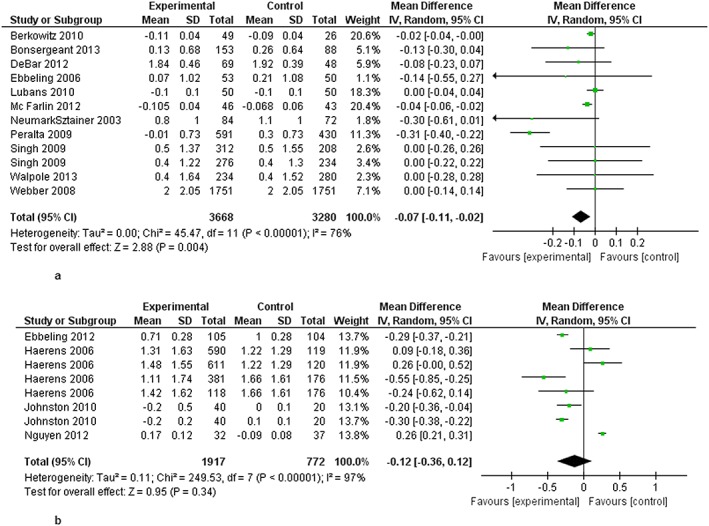
(a) Subgroup analysis of intervention duration less than 1 year in adolescent >12 years; (b) subgroup analysis of intervention duration longer than 1 year in adolescent >12 years.
Discussion
The present study extended Waters et al. meta‐analysis 24 to randomized and non‐randomized trials published between 2010 and 2015. Overall, 72 trials analysing the effectiveness of preventive interventions for paediatric obesity were identified, involving a total of 49,166 children aged 2–18 years.
The first important finding is that more recent studies, although associated with a significant BMI reduction, were less effective than the less recent ones. A possible interpretation of this result is that recent studies were very heterogeneous (I 2 = 94% vs. I 2 = 82%), and the majority were conducted on small samples (19/35 [54%] in recent studies vs. 12/37 [32%] in older studies had a sample size <100). In addition, low risk of bias was identified in a higher number of recent studies (17/35, 49%) as compared with older ones (12/37, 32%) (Figure S3).
As to pre‐school children, the present study provides new evidence on the effectiveness of the combination of diet and physical activity for interventions carried out in the family context. This result confirms that parental involvement is a predictor of intervention success, in line with evidence suggesting the prominent parental role in the prevention of unhealthy dietary habits 73, 74 and promotion of physical activity 75 in young children. However, the lack of studies exploring the effects of diet alone or physical activity in this age group prevents from drawing definite conclusions about the best intervention strategy.
As to the age group 6–12 years, the current meta‐analyses by subgroups of interventions and setting emphasized that the most effective interventions proved to be those combining diet with physical activity, delivered in the family and the school setting, and confirmed that school‐age children are the best target group for these interventions. This result is consistent with the previous literature reviews 76, 77, 78, 79, 80 and meta‐analyses 81, 82 and was the basis for the recommendations issued by the American Academy of Pediatrics 27 and the Endocrine Society 83 for childhood obesity prevention. As Katz et al. 77, 78 emphasized, in school age children, the six daily hours children spend in school more than half the year constitute a substantive allocation of their time and their lives, so it is important that the school responsibility to educate includes also education on healthy lifestyles. However, it may be both unrealistic and unreasonable to expect that school‐based interventions in isolation will appreciably influence the health, or weight, of children. In fact, children, like adults, are exposed to a large number of obesogenic factors on a daily basis (from ubiquitous access to highly palatable, energy‐dense foods to an ever proliferating array of labour sparing technologies) out of the school time, and this points to the need to involve families and school in the intervention programme.
As to adolescents, evidence available from eight studies using combination interventions showed no effects on BMI reductions, confirming Waters' results based on six studies. Previous research studies have demonstrated that there are many challenges in achieving adolescents' adherence to preventive programmes that are intrinsic to their developmental stage and demands for peer normalcy 84. Trapp et al. 85, 86 argued that successful interventions for teens tend to be those that reduce the cognitive and emotional barriers associated with a proper acceptance of their physical aspect, and encourage a supportive environment at home, at school and with peers, aimed at consolidating patients' adherence to the suggested programme and motivate behaviour changes.
Recent evidence highlights the association between low socioeconomic status and higher BMI in children aged 8–9 years in Italy 87 and 6–12 years in other countries 88. Strategies for the reduction of overweight and obesity rate, starting from childhood, could therefore contribute to reduce health inequalities 88. Because of the expected significant reduction of short‐term and long‐term healthcare costs associated with preventive interventions for obese children 89, the identification of effective interventions targeted to specific age groups and settings is fundamental and urgent for a more appropriate funding allocation, in times of budget constraints and financial crisis. Future research should focus on a more detailed description of the factors and determinants of the ‘obesogenic environment’ to which children are exposed, in order to assess feasibility and sustainability of the suggested programmes.
Finally, the potential increase of risky eating behaviours associated with programmes aimed at reducing obesity has to be considered. Indeed, only few RCTs (carried out in school age children) looked at whether programmes were harmful 24. Results from these studies suggest that obesity prevention strategies do not increase the frequency of adverse effects such as underweight, unhealthy eating practices, teasing, stigmatization, body image perceptions, satisfaction and self‐worth.
Some important study strengths can be identified. First, it was performed according to the authoritative Cochrane guidelines and method for systematic reviews and meta‐analysis. To allow a direct comparison with a previous work by Waters et al. 24, we initially applied the same inclusion criteria during the selection of studies published in the subsequent years to be included in the analysis. Then, we analysed non‐RCT to provide results from the most comprehensive possible analysis of available literature. Further subgroup analyses, based on patients' and study's features, were performed to identify predictors of study outcome. Finally, we assessed the risk of bias for the various studies.
On the other hand, the results of our analyses should be interpreted in light of some limitations. The first one is data heterogeneity. The inclusion of the most recent literature and the subgroup analyses confirmed, in fact, the high study heterogeneity for both children and intervention characteristics (i.e. amount, distribution and quality of daily caloric intake; duration and type of physical activity; time and type of educational programmes; and categories of professionals involved). The behavioural component did not contribute to determine the heterogeneity of our study, as shown by the exploratory sensitivity analysis (Figure S2).
The presence of non‐randomized trials and unadjusted data for some studies may have significantly contributed to the increase of heterogeneity in the meta‐analyses. For instance, in three out of seven non‐randomized studies, a selection bias was introduced by selecting children with a BMI >75th percentile for inclusion in the intervention group 39, 90, 91. Still, most of the studies addressed attrition bias; some tried to analyse the potential impact of missing data on their results and provided information about the characteristics of participants who did not complete post‐intervention evaluations. No differences were identified by the sensitivity subgroup analysis (Figure S1), and the quality of the included RCTs, assessed using Cochrane's tool, was good (low risk of bias) in 29 (40.2%) studies. The second limitation is the use of BMI as the only anthropometric measure used as outcome. Among the various suggested anthropometric measures, BMI is the most commonly used to assess overweight and improvement associated with study intervention, but it does not allow to assess body composition (i.e. adipose vs. muscle tissue) 92.
Third, there is a large imbalance in the number of studies carried out in each age group. Two‐thirds of them were, in fact, conducted in children aged 6–12 years, and the limited number of studies in the age groups 2–5 and 13–18 years increases the risk of overestimating or underestimating the effects of the interventions. As a result, conclusions about the most appropriate and advantageous interventions in terms of cost‐effectiveness and feasibility for pre‐school children or adolescents should be interpreted cautiously 93.
Finally, we must take into account that in order to translate and address obesogenic factors at individual, family and environmental level, an effective prevention strategy must combine complementary strengths: population approaches such as health promotion campaigns, taxes and subsidies, or government regulation such as regulation of food pricing, marketing and advertising or implementation of food quality, with individual approaches such as counselling by family doctors, to change people's perception about the norm in healthy behaviour 89, 94. Feasibility and sustainability of interventions might take advantage of new ways of ensuring that research findings benefit all children by embedding and integrating all the successful and effective programmes' activities into everyday practice, either for the different settings (homes and schools) and in the healthcare system and more generally in the community.
Conclusions
Evidence from the present study suggests that the resources available to counteract childhood obesity with preventive interventions should be preferentially targeted towards school age children, using multicomponent interventions involving schools and families, confirming the results achieved by the previous meta‐analysis that this review updates. The additional stratified analysis by age group showed no significant effects achieved in the adolescent group. In the small pre‐school children group, the study provides new evidence for the combination of diet and physical activity interventions carried out in the family setting. In the school age group, this study demonstrates the effectiveness of physical activity interventions carried out in the school context and of interventions combining diet and physical activity carried out both in the school setting only and in a setting that involves school and families.
Conflict of Interest Statement
No conflict of interest was declared.
Supporting information
Figure 1: Subgroup sensitivity analysis assessing study risk of bias performed using the Cochrane Risk of Bias Tool. Forest plot of individual and pooled weighted mean differences measured as BMI‐SDS reduction. Studies are divided into two groups, ‘LOW’ and ‘HIGH’ according to their risk of bias. A negative mean difference favors the intervention group. Data were pooled using a random effects model. SD, standard deviation; IV, inverse variance method; CI, confidence interval.
Figure 2: Subgroup sensitivity analysis comparing studies that included (above) and did not include (below) behavioural changes in the program. Forest plot of individual and pooled weighted mean differences measured in terms of BMI‐SDS reduction. A negative mean difference favors the intervention groups. Random effects model was used to pool data. SD, standard deviation; IV, inverse variance method; CI, confidence interval.
Figure 3: Subgroup sensitivity analysis comparing studies included in a previous meta‐analysis by Waters et al. [24] (below) and subsequent studies (published after 14th February 2010; above). Forest plot of individual and pooled weighted mean differences measured in terms of BMI‐SDS reduction. A negative mean difference favors the intervention groups. Random effects model was used to pool data. SD, standard deviation; IV, inverse variance method; CI, confidence interval.
Gori, D. , Guaraldi, F. , Cinocca, S. , Moser, G. , Rucci, P. , and Fantini, M. P. (2017) Effectiveness of educational and lifestyle interventions to prevent paediatric obesity: systematic review and meta‐analyses of randomized and non‐randomized controlled trials. Obesity Science & Practice, 3: 235–248. doi: 10.1002/osp4.111.
References
- 1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev 2004; 5: 4–85. https://www.ncbi.nlm.nih.gov/pubmed/?term=15096099. [DOI] [PubMed] [Google Scholar]
- 3. Popkin BM, Gordon‐Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord 2004; 28: S2–S9. https://www.ncbi.nlm.nih.gov/pubmed/?term=15543214. [DOI] [PubMed] [Google Scholar]
- 4. Wang Y. Cross‐national comparison of childhood obesity: the epidemic and the relationship between obesity and socioeconomic status. Int J Epidemiol 2001; 30: 1129–1136. https://www.ncbi.nlm.nih.gov/pubmed/?term=11689534. [DOI] [PubMed] [Google Scholar]
- 5. Wang S, Moss JR, Hiller JE. Applicability and transferability of interventions in evidence‐based public health. Health Promot Int 2006; 21: 76–83. https://www.ncbi.nlm.nih.gov/pubmed/?term=16249192. [DOI] [PubMed] [Google Scholar]
- 6. Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med (Baltim) 1999; 29: 563–570. https://www.ncbi.nlm.nih.gov/pubmed/?term=10600438. [DOI] [PubMed] [Google Scholar]
- 7. Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008; 9: 474–488. https://www.ncbi.nlm.nih.gov/pubmed/?term=18331423. [DOI] [PubMed] [Google Scholar]
- 8. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997; 337: 869–873. https://www.ncbi.nlm.nih.gov/pubmed/?term=9302300. [DOI] [PubMed] [Google Scholar]
- 9. Amed S. The future of treating youth‐onset type 2 diabetes: focusing upstream and extending our influence into community environments. Curr Diab Rep 2015; 15 https://www.ncbi.nlm.nih.gov/pubmed/?term=25644815. [DOI] [PubMed] [Google Scholar]
- 10. Ayer J, Charakida M, Deanfield JE, Celermajer DS. Lifetime risk: childhood obesity and cardiovascular risk. Eur Heart J 2015; 36: 1059–1061. https://www.ncbi.nlm.nih.gov/pubmed/?term=25810456. [DOI] [PubMed] [Google Scholar]
- 11. Cote AT, Harris KC, Panagiotopoulos C, Sandor GGS, Devlin AM. Childhood obesity and cardiovascular dysfunction. J Am Coll Cardiol 2013; 62: 1309–1319. https://www.ncbi.nlm.nih.gov/pubmed/?term=23954339. [DOI] [PubMed] [Google Scholar]
- 12. D'Adamo E, Guardamagna O, Chiarelli F, Bartuli A, Liccardo D, et al. Atherogenic dyslipidemia and cardiovascular risk factors in obese children. Int J Endocrinol 2015; 2015 https://www.ncbi.nlm.nih.gov/pubmed/?term=25663838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gupta N, Goel K, Shah P, Misra A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr Rev 2012; 33: 48–70. https://www.ncbi.nlm.nih.gov/pubmed/?term=22240243. [DOI] [PubMed] [Google Scholar]
- 14. Mahfouz RA, Dewedar A, Abdelmoneim A, Hossien EM. Aortic and pulmonary artery stiffness and cardiac function in children at risk for obesity. Echocardiography 2012; 29: 984–990. https://www.ncbi.nlm.nih.gov/pubmed/?term=22694671. [DOI] [PubMed] [Google Scholar]
- 15. Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr 2000; 136: 727–733. https://www.ncbi.nlm.nih.gov/pubmed/?term=10839867. [PubMed] [Google Scholar]
- 16. Adelman RD, Restaino IG, Alon US, Blowey DL. Proteinuria and focal segmental glomerulosclerosis in severely obese adolescents. J Pediatr 2001; 138: 481–485. https://www.ncbi.nlm.nih.gov/pubmed/?term=11295709. [DOI] [PubMed] [Google Scholar]
- 17. Chan G, Chen CT. Musculoskeletal effects of obesity. Curr Opin Pediatr 2009; 21: 65–70. https://www.ncbi.nlm.nih.gov/pubmed/?term=19242242. [DOI] [PubMed] [Google Scholar]
- 18. Thivel D, Ring‐Dimitriou S, Weghuber D, Frelut M‐L, O'Malley G. Muscle strength and fitness in pediatric obesity: a systematic review from the European childhood obesity group. Obes Facts 2016; 9: 52–63. https://www.ncbi.nlm.nih.gov/pubmed/?term=26901423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public‐health crisis, common sense cure. Lancet 2002; 360: 473–482. https://www.ncbi.nlm.nih.gov/pubmed/?term=12241736. [DOI] [PubMed] [Google Scholar]
- 20. Latzer Y, Stein D. A review of the psychological and familial perspectives of childhood obesity. J Eat Disord 2013; 1: 7 https://www.ncbi.nlm.nih.gov/pubmed/?term=24999389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tsiros MD, Olds T, Buckley JD, Grimshaw P, Brennan L, et al. Health‐related quality of life in obese children and adolescents. Int J Obes 2009; 33: 387–400. https://www.ncbi.nlm.nih.gov/pubmed/?term=19255583. [DOI] [PubMed] [Google Scholar]
- 22. Coles N, Birken C, Hamilton J. Emerging treatments for severe obesity in children and adolescents. BMJ. 2016. Sep 29; 354: i4116 https://www.ncbi.nlm.nih.gov/pubmed/27686795. [DOI] [PubMed] [Google Scholar]
- 23. Sabin MA, Kiess W. Childhood obesity: current and novel approaches. Best Pract Res Clin Endocrinol Metab 2015; 29: 327–338. https://www.ncbi.nlm.nih.gov/pubmed/?term=26051294. [DOI] [PubMed] [Google Scholar]
- 24. Waters E, de Silva‐Sanigorski A, Hall BJ, Brown T, Campbell KJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011: CD001871 https://www.ncbi.nlm.nih.gov/pubmed/?term=22161367. [DOI] [PubMed] [Google Scholar]
- 25. Spear BA, Barlow SE, Ervin C, Ludwig DS, Saelens BE, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007; 120: S254–S288. https://www.ncbi.nlm.nih.gov/pubmed/?term=18055654. [DOI] [PubMed] [Google Scholar]
- 26. Tanas R, Marcolongo R, Pedretti S, Gilli G. A family‐based education program for obesity: a three‐year study. BMC Pediatr 2007; 7: 33 https://www.ncbi.nlm.nih.gov/pubmed/?term=17953755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Barlow SE, the Expert Committee . Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007; 120: S164–S192. https://www.ncbi.nlm.nih.gov/pubmed/?term=18055651. [DOI] [PubMed] [Google Scholar]
- 28. Davoli AM, Broccoli S, Bonvicini L, et al. Pediatrician‐led motivational interviewing to treat overweight children: an RCT. Pediatrics 2013; 132: e1236–e1246. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 29. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Obesity worldwide: international survey. BMJ 2000; 320: 1–6. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 2007; 335: 194 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EAMJ. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull 2004; 25: S15–S26. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 32. de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr 2007; 137: 144–148. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 33. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Greenhalgh T. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. Bmj 2005; 331: 1064–1065. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Higgins JPT. In: Green S. (ed.). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (March 2011), 2011. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [Google Scholar]
- 36. Hardy RJ, Thompson SG. Detecting and describing heterogeneity in meta‐analysis. Stat Med 1998; 17: 841–856. https://www.ncbi.nlm.nih.gov/pubmed/?term=9595615 [DOI] [PubMed] [Google Scholar]
- 37. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003. Sep 6; 327: 557–560. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Higgins JPT Green S. Cochrane Handbook for Systematic Reviews. available at: http://community‐archive.cochrane.org/sites/default/files/Handbook510pdf_Ch08_RiskOfBias.pdf https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830 [Google Scholar]
- 39. Almas A, Islam M, Jafar TH. School‐based physical activity programme in preadolescent girls (9–11 years): a feasibility trial in Karachi, Pakistan. Arch Dis Child 2013; 98: 515–519. https://www.ncbi.nlm.nih.gov/pubmed/?term=23661575. [DOI] [PubMed] [Google Scholar]
- 40. Armeno ML, Krochik AGMC. Evaluation of two dietary treatments in obese hyperinsulinemic adolescents. J Pediatr Endocrinol Metab 2011; 24: 715–722. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 41. Berkowitz R, Tokuyama Y, Ingram SL, Woodward JL, Bethea CL. NIH Public Access. 2011; 235: 649–657. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [Google Scholar]
- 42. Bocca G, Corpeleijn E, Stolk RP, Sauer PJJ. Results of a multidisciplinary treatment program in 3‐year‐old to 5‐year‐old overweight or obese children: a randomized controlled clinical trial. Arch Pediatr Adolesc Med 2012; 166: 1109–1115. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 43. Bonsergent E, Agrinier N, Thilly N, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med 2013; 44: 30–39. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 44. Croker H, Viner R, Nicholls D. Family‐based behavioural treatment of childhood obesity in a UK National Health Service setting: randomised controlled trial. J Obes 2011; 36: 1–19. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Daniels LA, Mallan KM, Battistutta D, Nicholson JM, Perry R, Magarey A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of two intervention modules. Int J Obes 2012; 36: 1292–1298. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 46. De Coen V, De Bourdeaudhuij I, Vereecken C, et al. Effects of a 2‐year healthy eating and physical activity intervention for 3–6‐year‐olds in communities of high and low socio‐economic status: the POP (prevention of overweight among pre‐school and school children) project. Public Health Nutr 2012; 15: 1737–1745. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 47. de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar‐free or sugar‐sweetened beverages and body weight in children. N Engl J Med 2012; 367: 1397–1406. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 48. DeBar LL, Stevens VJ, Perrin N, et al. A primary care‐based, multicomponent lifestyle intervention for overweight adolescent females. Pediatrics 2012; 129: e611–e620. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Endevelt R, Elkayam O, Cohen R, et al. An intensive family intervention clinic for reducing childhood obesity. J Am Board Fam Med 2014; 27: 321–328. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 50. Fairclough SJ, Hackett AF, Davies IG, et al. Promoting healthy weight in primary school children through physical activity and nutrition education: a pragmatic evaluation of the CHANGE! randomised intervention study. BMC Public Health 2013; 13: 626 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Haire‐Joshu D, Nanney MS, Elliott M, et al. The use of mentoring programs to improve energy balance behaviors in high‐risk children. Obes (Silver Spring) 2010; 18: S75–S83. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Herrick H, Thompson H, Kinder J, Madsen KA. Use of SPARK to promote after‐school physical activity. J Sch Health 2012; 82: 457–461. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Johnston CA, Moreno JP, El‐Mubasher A, Gallagher M, Tyler C, Woehler D. Impact of a school‐based pediatric obesity prevention program facilitated by health professionals. J Sch Health 2013; 83: 171–181. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 54. Johnston CA, Tyler C, Fullerton G, et al. Corrigendum: effects of a school‐based weight maintenance program for Mexican‐American children: results at 2 years. Obesity 2010; 18: 647 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 55. Khan ANA, Raine LB. Impact of the FITKids physical activity intervention on adiposity in prepubertal children. Pediatrics 2014;133:875–883. https://www.ncbi.nlm.nih.gov/pubmed/?term=24685956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kipping RR, Howe LD, Jago R, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014; 348: g3256 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kokkvoll A, Grimsgaard S, Ødegaard R, Flægstad T, Njølstad I. Single versus multiple‐family intervention in childhood overweight – Finnmark Activity School: a randomised trial. Arch Dis Child 2014; 99: 225–231. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ 2010; 340: c785 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lloyd‐Richardson EE, Jelalian E, Sato AF, Hart CN, Mehlenbeck R, Wing RR. Two‐year follow‐up of an adolescent behavioral weight control intervention. Pediatrics 2012; 130: e281–e288. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lubans DR, Morgan PJ, Aguiar EJ, Callister R. Randomized controlled trial of the Physical Activity Leaders (PALs) program for adolescent boys from disadvantaged secondary schools. Prev Med (Baltim) 2011; 52: 239–246. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 61. Madsen K, Thompson H, Adkins A, Crawford Y. School‐community partnerships: a cluster‐randomized trial of an after‐school soccer program. JAMA Pediatr 2013; 167: 321–326. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mcfarlin BK, Johnston CJ, Carpenter KC, et al. A one‐year school‐based diet/exercise intervention improves non‐traditional disease biomarkers in Mexican‐American children. Matern Child Nutr 2013; 9: 524–532. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nguyen B, Shrewsbury VA, O'Connor J, et al. Two‐year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight‐loss maintenance: the Loozit randomized controlled trial. Int J Obes 2012: 468–472. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 64. Sacher PM, Kolotourou M, Chadwick PM, et al. Randomized controlled trial of the MEND Program: a family‐based community intervention for childhood obesity. Obesity 2010; 18: S62–S68. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 65. Santos RG, Durksen A, Rabbanni R, et al. Effectiveness of peer‐based healthy living lesson plans on anthropometric measures and physical activity in elementary school students: a cluster randomized trial. JAMA Pediatr 2014; 168: 330–337. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 66. Stark LJ, Spear S, Boles R, et al. A pilot randomized controlled trial of a clinic and home‐based behavioral intervention to decrease obesity in preschoolers. Obesity (Silver Spring) 2011; 19: 134–141. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Giralt M, Albaladejo R, Tarro L, Moriña D, Arija V, Solà R. A primary‐school‐based study to reduce prevalence of childhood obesity in Catalunya (Spain) – EDAL‐Educació en alimentació: study protocol for a randomised controlled trial. Trials 2011; 12: 54 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Trost SG, Sundal D, Foster GD, Lent MR, Vojta D. Effects of a pediatric weight management program with and without active video games a randomized trial. JAMA Pediatr 2014; 168: 407 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 69. Walpole B, Dettmer E, Morrongiello BA, Mccrindle BW, Hamilton J. Motivational interviewing to enhance self‐efficacy and promote weight loss in overweight and obese adolescents: a randomized controlled trial. J Pediatr Psychol 2013;38:944–953. https://www.ncbi.nlm.nih.gov/pubmed/?term=23671058 [DOI] [PubMed] [Google Scholar]
- 70. Williamson DA, Champagne CM, Harsha DW, et al. Effect of an environmental school‐based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity (Silver Spring) 2012; 20: 1–9. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wright JA, Phillips BD, Watson BL, Newby PK, Norman GJ, Adams WG. Randomized trial of a family‐based, automated, conversational obesity treatment program for underserved populations. Obesity 2013; 21: 1–19. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Yin Z, Moore JB, Johnson MH, Vernon MM, Gutin B. The impact of a 3‐year after‐school obesity prevention program in elementary school children. Child Obes 2012; 8: 60–70. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Variyam JN. Overweight children: is parental nutrition knowledge a factor? Food Rev 2001; 24: 18–22. [Google Scholar]
- 74. Collins WA, Maccoby EE, Steinberg L, Hetherington EM, Bornstein MH. Contemporary research on parenting. The case for nature and nurture. Am Psychol 2000; 55: 218–232. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [PubMed] [Google Scholar]
- 75. Hart B, Risley TR. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore: P.H. Brookes, 1995. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [Google Scholar]
- 76. Brown T, Summerbell C. Systematic review of school‐based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev 2009; 10: 110–141. Epub 2008/08/05. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 77. Katz DL. School‐based interventions for health promotion and weight control: not just waiting on the world to change. Annu Rev Public Health 2009; 30: 253–272. Epub 2009/08/26. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 78. Katz DL, O'Connell M, Njike VY, Yeh MC, Nawaz H. Strategies for the prevention and control of obesity in the school setting: systematic review and metaanalysis. Int J Obes 2008; 32: 1780–1789. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 79. Sharma M. School‐based interventions for childhood and adolescent obesity. Obesity Rev 2006; 7: 261–269. Epub 2006/07/27. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 80. Epstein LH, Coleman KJ, Myers MD. Exercise in treating obesity in children and adolescents. Med Sci Sport Exer 1996; 28: 428–435. Epub 1996/04/01. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 81. Lavelle HV, Mackay DF, Pell JP. Systematic review and meta‐analysis of school‐based interventions to reduce body mass index. J Public Health (Oxf) 2012; 34: 360–9. https://doi.org/10.1093/pubmed/fdr116. Epub 2012 Jan 20. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 82. Snethen JA, Broome ME, Cashin SE. Effective weight loss for overweight children: a meta‐analysis of intervention studies. Pediatr Nurs 2006; 21: 45–56. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 83. August GP, Caprio S, Fennoy I, et al. Pediatric obesity – assessment, treatment and prevention: an Endocrine Society Clinical Practice Guideline. Journal of Clinical Endocrinology & Metabolism 2008; 93: 4576–4599 URL https://endo.confex.com/endo/2016endo/webprogram/Session7466.html. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010. Aug; 22: 405–411. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Trapp S. Motivation, mindfulness, and metabolic factors predicting adolescent adherence and attrition in a multidisciplinary weight management program. Virginia Commonwealth University, 2015, 372–447 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830
- 86. Nogueira TSD, Porto Zambon M. Reasons for non‐adherence to obesity treatment in children and adolescents. Rev Paul Pediatr 2013; 31: 338–343. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Lazzeri G, Pammolli A, Pilato V, Giacchi MV. Relationship between 8/9‐yr‐old school children BMI, parents' BMI and educational level: a cross sectional survey. Nutr J 2011; 10: 76 https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Wang Y, Lim H, Program N. The global childhood obesity epidemic and the association between socio‐economic status and childhood obesity. Int Rev Psychiatry 2015; 24: 176–188. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Sassi M, Cecchini SF. Preventing obesity in the USA: impact on health service utilization and costs. Pharmacoeconomics 2015; 33: 765–776. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 90. Neumark‐Sztainer D, Story M, Hannan PJ, Rex J. New moves: a school‐based obesity prevention program for adolescent girls. Preventive Medicine 2003; 37: 41–51. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 91. Sanigorski A, Bell A, Kremer P, Cuttler R, Swinburn B. Reducing unhealthy weight gain in children through community capacity‐building: results of a quasiexperimental intervention program, Be Active Eat Well. International Journal of Obesity (Lond) 2008; 32: 1060–1067. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 92. Nooyens ACJ, Koppes LLJ, Visscher TLS, et al. Adolescent skinfold thickness is a better predictor of high body fatness in adults than is body mass index: the Amsterdam growth and health longitudinal study. Am J Clin Nutr 2007; 85: 1533–1539. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [DOI] [PubMed] [Google Scholar]
- 93. Faggiano F, Concina D, Molinar R, Allara E. Primary prevention of cancer and cardiovascular diseases: an overview of scientific literature. La Prev primaria di tumori e Mal Cardiovasc una Overv della Lett Sci 2014; 38: 19–22. https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830. [PubMed] [Google Scholar]
- 94. Sassi F. Obesity and the Economics of Prevention: Fit not Fat Published on September 23, 2010, available at https://www.oecd.org/els/health‐systems/46044572.pdf https://www.ncbi.nlm.nih.gov/pubmed/?term=24880830
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure 1: Subgroup sensitivity analysis assessing study risk of bias performed using the Cochrane Risk of Bias Tool. Forest plot of individual and pooled weighted mean differences measured as BMI‐SDS reduction. Studies are divided into two groups, ‘LOW’ and ‘HIGH’ according to their risk of bias. A negative mean difference favors the intervention group. Data were pooled using a random effects model. SD, standard deviation; IV, inverse variance method; CI, confidence interval.
Figure 2: Subgroup sensitivity analysis comparing studies that included (above) and did not include (below) behavioural changes in the program. Forest plot of individual and pooled weighted mean differences measured in terms of BMI‐SDS reduction. A negative mean difference favors the intervention groups. Random effects model was used to pool data. SD, standard deviation; IV, inverse variance method; CI, confidence interval.
Figure 3: Subgroup sensitivity analysis comparing studies included in a previous meta‐analysis by Waters et al. [24] (below) and subsequent studies (published after 14th February 2010; above). Forest plot of individual and pooled weighted mean differences measured in terms of BMI‐SDS reduction. A negative mean difference favors the intervention groups. Random effects model was used to pool data. SD, standard deviation; IV, inverse variance method; CI, confidence interval.


