Abstract
Purpose
To detect macular perfusion defects in glaucoma using projection-resolved optical coherence tomography (OCT) angiography.
Design
Prospective observation study.
Participants
30 perimetric glaucoma and 30 age-matched normal participants were included.
Methods
One eye of each participant was imaged using 6mm×6mm macular OCT angiography (OCTA) scan pattern by 70-kHz 840-nm spectral-domain OCT. Flow signal was calculated by the split-spectrum amplitude-decorrelation angiography algorithm (SSADA). A projection-resolved OCTA (PR-OCTA) algorithm was used to remove flow projection artifacts. Four en face OCTA slabs were analyzed: the superficial vascular complex (SVC), intermediate capillary plexus (ICP), deep capillary plexus (DCP) and all-plexus retina (SVC+ICP+DCP). The vessel density (VD), defined as the percentage area occupied by flow pixels, was calculated from en face OCTA. A novel algorithm was used to adjust the vessel density to compensate for local variations in OCT signal strength.
Main Outcome Measures
Macular retinal VD, ganglion cell complex (GCC) thickness, and visual field (VF) sensitivity.
Results
Focal capillary dropout could be visualized in the SVC, but not the ICP and DVP, in glaucomatous eyes. In the glaucoma group, the SVC and all-plexus retinal VD (mean±SD: 47.2%±7.1% and 73.5%±6.6%) were lower than the normal group (60.5%±4.0% and 83.2%±4.2%, both P <0.001, t test). The ICP and DCP VD were not significantly lower in the glaucoma group. Among the overall macular VD parameters, the SVC VD had the best diagnostic accuracy as measured by the area under the receiver operating characteristic curve (AROC). The accuracy was even better when the worse hemisphere (inferior or superior) was used, achieving an AROC of 0.983 and a sensitivity of 96.7% at a specificity of 95%. Among the glaucoma participants, the hemispheric SVC VD values were highly correlated with the corresponding GCC thickness and VF sensitivity (P<0.003). The reflectance compensation step in VD calculation significantly improved repeatability, normal population variation, and correlation with VF and GCC thickness.
Conclusions
Based on PR-OCTA, glaucoma preferentially affects perfusion in the SVC in the macula more than the deeper plexuses. Reflectance-compensated SVC VD measurement by PR-OCTA detected glaucoma with high accuracy and could be useful in the clinical evaluation of glaucoma.
Introduction
Glaucoma is the second leading cause of blindness worldwide, affecting over 60 million people and predicted to affect 79.6 million by 2020.1–3 Early diagnosis and close monitoring of glaucoma are important given glaucoma’s insidious onset with irreversible nerve damage associated with vision loss. While studies of glaucoma have traditionally focused on the optic nerve and peripapillary retina, there are multiple reasons to evaluate the macula in glaucoma diagnosis and monitoring.
Histologic studies have shown that glaucoma results in loss of retinal ganglion cells and over 30% of the ganglion cells in the eye reside in the macula.4, 5 Many recent OCT studies have shown that macular thinning is associated with glaucoma, and that the thinning preferentially affects the ganglion cell complex (GCC) – the inner most layers of the retina which include the retinal nerve fiber layer (NFL), the ganglion cell layer (GCL) and the inner plexiform layer (IPL).6–8 Diagnostic accuracy for glaucoma can be improved when macular OCT measurements focus particularly on the GCC.6, 9, 10 Given that a preponderance of retinal ganglion cells reside in the macula, studies have also suggested that early glaucomatous damage involves the macula.11 Recent studies have shown that early visual field (VF) loss often occurs in the central 10 degrees of vision, an area represented by the macula.12 Focal loss of the GCC on OCT appears to be an excellent predictor of progression from pre-perimetric to perimetric glaucoma.13 However, glaucomatous damage in macular retinal circulation has not been demonstrated.
OCT angiography (OCTA) with the split-spectrum amplitude-decorrelation angiography (SSADA) algorithm has provided a quick and reproducible way to qualitatively and quantitatively show areas of decreased or altered perfusion in the eye.14–19 Using OCTA, Jia et al. demonstrated significantly decreased perfusion at the optic nerve head in glaucoma14 and Liu et al. similarly showed decreased perfusion in the peripapillary retina.15 More recently, we developed a “projection-resolved” (PR) algorithm which effectively suppresses projection artifacts on both en face and cross-sectional angiograms and enhances depth resolution of vascular networks.20, 21 Using projection-resolved OCTA (PR-OCTA), we are now able to visualize the distinct vascular patterns in the 4 retinal plexuses. This study aims to compare the macular circulation in normal participants and glaucomatous participants in different retinal plexuses and to detect and characterize macular circulation defects in glaucoma using PR-OCTA.
Methods
Study Population
This prospective observation study was performed from September 16, 2014 to February 20, 2016 at the Casey Eye Institute, Oregon Health & Science University (OHSU). The research protocols were approved by the Institutional Review Board at OHSU, carried out in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from each participant.
All participants were part of the “Functional and Structural Optical Coherence Tomography for Glaucoma” study. The inclusion criteria for the perimetric glaucoma (PG) group were: (1) an optic disc rim defect (thinning or notching) or NFL defect visible on slit-lamp biomicroscopy; and (2) a consistent glaucomatous pattern, on both qualifying Humphrey SITA 24-2 VFs, meeting at least one of the following criteria: pattern standard deviation (PSD) outside normal limits (p < 0.05) or glaucoma hemifield test outside normal limits.
For the normal group, the inclusion criteria were: (1) no evidence of retinal pathology or glaucoma; (2) a normal Humphrey 24-2 visual field; (3) intraocular pressure < 21 mm Hg; (4) central corneal pachymetry > 500 microns; (5) no chronic ocular or systemic corticosteroid use; (6) an open angle on gonioscopy; (7) a normal appearing optic nerve head (ONH) and NFL; and (8) symmetric ONH between left and right eyes.
The exclusion criteria for both groups were: (1) best-corrected visual acuity less than 20/40; (2) age < 30 or >80 years; (3) refractive error of > +3.00D or < −7.00D; (4) previous intraocular surgery except for an uncomplicated cataract extraction with posterior chamber intraocular lens implantation; (5) any diseases that may cause VF loss or optic disc abnormalities; or (6) inability to perform reliably on automated VF testing. One eye from each participant was scanned and analyzed.
Visual Field Testing
VF tests were performed with the Humphrey Field Analyzer II (Carl Zeiss, Inc.) set for the 24-2 threshold test, size III white stimulus, using the SITA standard algorithm.
Optical Coherence Tomography
A 70-kHz, 840-nm wavelength spectral-domain OCT system (Avanti RTVue-XR, Optovue Inc.) was used. The AngioVue version 2014.1.0.2 software was used to acquire OCTA scans.
Image Acquisition and Processing
The macular region was scanned using a 6mm×6mm volumetric angiography scan centered on fixation. Each volume was comprised of 304 line-scan locations at which 2 consecutive B-scans were obtained. Each B-scan contains 304 A-scans. The AngioVue software uses the SSADA algorithm, which compares the consecutive B-scans at the same location to detect flow using motion contrast.22 Each scan set comprises of 2 volumetric scans: 1 vertical-priority raster and 1 horizontal-priority raster. The AngioVue software uses an orthogonal registration algorithm to register the 2 raster volumes to produce a merged 3D OCT angiogram.23 Two sets of scans were performed within one visit.
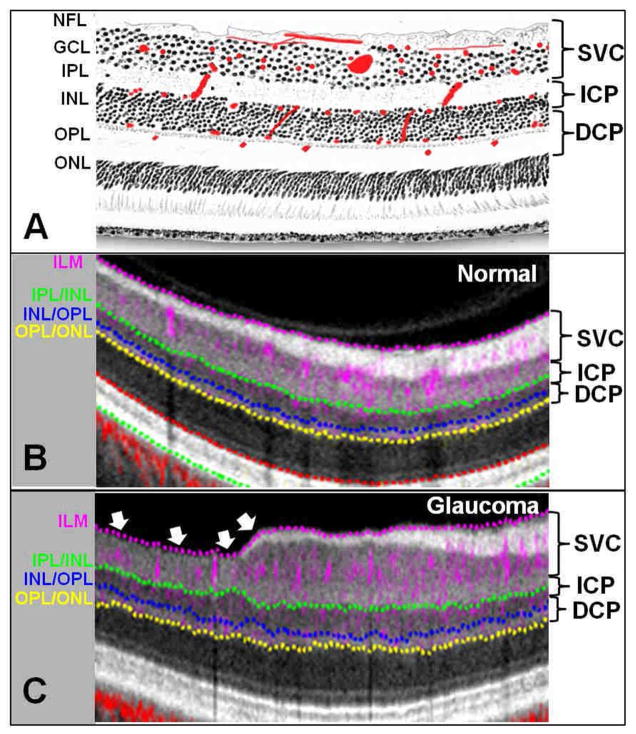
The merged volumetric angiograms were then exported for custom processing using the Center for Ophthalmic Optics & Lasers-Angiography Reading Toolkit (COOL-ART) software. COOL-ART removes flow projection artifacts and calculates reflectance-compensated vessel density (VD). These custom programs were developed at the Casey Eye Institute using the MATLAB programming language. The OCTA scans contain both volumetric flow (decorrelation) data as well as structural (reflectance) data. The projection-resolved OCT angiography (PR-OCTA) algorithm retains flow signal from real blood vessels while suppressing projected flow signal in deeper layers, which appears as downward tails on cross-sectional angiograms and duplicated vascular patterns on en face angiograms.20, 24 PR-OCTA could visualize up to four retinal plexuses: the radial peripapillary capillary plexus (RPCP), the superficial vascular plexus (SVP), the intermediate capillary plexus (ICP), and the deep capillary plexus (DCP).21, 25–28 In the temporal portion of the macula, the RPCP (residing in the NFL) is very thin and cannot be distinguished from the SVP, therefore we lump the RPCP and the SVP into the superficial vascular complex (SVC). Four en face OCTA slabs were analyzed for VD measurement: SVC, ICP, DCP and all-plexus retina (SVC+ICP+DCP) (Figure 1). Segmentation of the retinal layers was done by automated MATLAB programs that operate on the structural OCT data. An en face angiogram of each slab was obtained by maximum flow (decorrelation value) projection. The vessel density (VD), defined as the percentage area occupied by the large vessels and microvasculature, was evaluated in the entire 6mm×6mm scan area excluding of the foveal avascular zone (FAZ), which was defined as a 0.6 mm diameter circle centered at the FAZ. The GCC thickness was averaged over the same region. Superior and inferior hemispheric averages were obtained by dividing the scan area across the horizontal meridian.
Figure 1.
Relationship between the retinal vascular plexuses and anatomic layers. (A) An illustration of the retinal vascular plexuses in red (labeled on right) hand drawn on top of a histological section of the human retina showing anatomic layers (labeled on left). The SVC supplies most of the the ganglion cell complex. The ICP straddles the IPL and INL. The DCP straddles the INL and OPL. (B) Cross-sectional projection-resolved optical coherence tomography angiograms (PR-OCTA) of a normal eye. The 6-mm section is taken 750 μm superior to the fovea. Flow signals (purple for retinal and red for choroidal blood flow) were overlaid on reflectance signal (gray scale). (C) PR-OCTA cross-section from a perimetric glaucomatous eye. Focal thinning of NFL and GCL could be visualized temporally in the glaucomatous eye (arrows), corresponding with the loss of capillaries in the SVC. Abbreviations: NFL = nerve fiber layer, GCL = ganglion cell layer, IPL = inner plexiform layer, GCC(NFL+GCL+IPL)=ganglion cell complex, INL = inner nuclear layer, OPL = outer plexiform layer, ONL = outer nuclear layer, SVC = superficial vascular complex (inner 80% of the GCC), ICP = intermediate capillary plexus (outer 20% of the GCC + inner 50% of INL), DCP = deep capillary plexus (outer 50% of INL + OPL).
Because we found VD to be strongly correlated with signal strength index in previous studies, we developed a reflectance-adjustment method that corrected the artifactually lower flow signal in regions of reduced reflectance (e.g. due to media opacity or pupil vignetting).29 The method is based on statistical analysis of the relationship between the flow noise in the FAZ with reflectance in retinal tissue, in which the reflectance was manipulated by simulated media opacity (optical filters). In the extrafoveal retina, the average reflectance in the INL, OPL, and ONL layers to adjust the threshold flow signal value used to classify vessel v. static tissue on en face OCTA. Reflectance compensation is another aspect of the OCTA technique that can be used with either PR-OCTA or nonPR-OCTA. Clinical validation showed that this algorithm was able to remove the dependence of retinal VD measurements on OCT signal strength index and reduce population variation.29
Image quality was assessed for all OCTA scans. Poor quality scans with signal strength index below 50, or registered image sets with residual motion artifacts (discontinuous vessel pattern) were excluded from analysis. Two image sets, each meeting the quality criteria, were required in order to be included in the analysis.
Within-visit repeatability of the VD was calculated with two sets of scans performed within a single visit. Within-visit repeatability and population variation were assessed by the coefficient of variation (CV).
All eyes from the glaucoma and normal groups were qualitatively graded for the presence of capillary dropout on the en face OCTA of the SVC, ICP, and DCP slabs. Only the first merged OCTA from the first set of scan was used in the qualitative grading. The second set was not graded. The grader is a fellowship-trained glaucoma specialist. A training set of macular angiograms of each plexus (SVC, ICP, and DCP) were used to train the grader. The training set was obtained from five normal and five glaucomatous participants who were not included in the primary analysis. The grader was masked to the identity, clinical information, and glaucoma status of the participant.
Statistical Analysis
Pearson correlation was employed to investigate the effect of age, mean ocular perfusion pressure (MOPP), and intraocular pressure (IOP) on VD measurements. MOPP=2/3*MAP – IOP, where mean arterial pressure (MAP) = 2/3*diastolic blood pressure + 1/3*systolic blood pressure. The Student’s t test was used to compare normal and glaucoma groups. Pearson correlation was also used to determine the relationships between macular VD and the traditional glaucoma measurements of function and structure, such as the average retinal sensitivity over the corresponding VF points (central 16 points) and GCC thickness in the glaucoma group. The dB values for the retinal sensitivity points in the HFA 24-2 test were converted to a linear scale (1/Lambert unit) using the expression 10 0.1 × dB value and then averaged over hemispheres or the whole eye. The SVC VD value and GCC thickness from that worse hemisphere (superior or inferior) was used to calculate the worse-hemisphere diagnostic power. The worse hemisphere has lower fractional deviation from normal. The fractional deviation being the value from the eye under evaluation minus the average of the normal group, then divided by the normal average. Generalized linear model was employed to evaluate the effect of eye drops and other factors on the macular VD. All statistical analyses were performed with SPSS20.0 (SPSS Inc., Chicago, IL) and MedCalc 10.1.3.0 (MedCalc Software, Ostend, Belgium, www.medcalc.be). The area under the receiver operating characteristic curve (AROC), sensitivity, and specificity are used to evaluate diagnostic accuracy. McNemar test and the method of Delong et al were used to compare sensitivity and AROC of different parameters.30 The odds ratio test was performed for the qualitative grading results. The statistical significance was assumed at P<0.05. However, for multiple comparisons among the 5 parameters (SVC VD, ICP VD, DCP VD, all-plexus VD and GCC thickness) measured by OCTA, a Bonferroni correction was applied with resultant significance level set at P <0.01. All OCT and OCTA parameters had normal distributions according to the Shapiro-Wilk test.
Results
Study Population
Macular perfusion was studied in 30 normal and 33 perimetric glaucoma participants. Three glaucoma participants were not analyzed due to poor OCT angiography scan quality – leaving 30 for statistical analysis. The 30 normal participants provided age-matched comparison with the 30 glaucoma participants (Table 1). Nine glaucoma participants had mild (stage 0–1), fifteen had moderate (stage 2–3), six had advanced (stage 4–5) glaucoma, according to Glaucoma Staging System 2.31 26 participants had primary open angle glaucoma, 3 participants had low-tension glaucoma, and 1 participant had pigmentary glaucoma. There was no statistically significant difference between the normal and glaucoma groups for age, IOP, MOPP and systolic/diastolic blood pressure (Table 1).
Table 1.
Participant Characteristics
| Parameter | Normal | Glaucoma | Difference (P value) | |
|---|---|---|---|---|
| Participants, n
|
30 | 30 | ||
| Eyes, n
|
30 | 30 | ||
| Age (Years)
|
65± 9 | 65 ± 10 | ||
| Glaucoma drops, n (%)
|
0 (0%) | 28(93%) | ||
| Intraocular Pressure (mm Hg)
|
15.1 ± 3.0 | 14.9 ± 3.1 | 0.2 (0.609) | |
| Diastolic Blood Pressure (mm Hg)
|
78.2 ± 11.2 | 78.8 ± 10.8 | −0.6 (0.815) | |
| Systolic Blood Pressure (mm Hg)
|
125.3 ± 16.9 | 124.5 ± 17.0 | 0.8 (0.850) | |
| Mean Ocular Perfusion Pressure (mm Hg)
|
49.0 ± 7.6 | 47.8 ± 6.6 | 1.2 (0.782) | |
|
| ||||
| Visual Field | MD (dB) | 0.27 ± 1.10 (−3.22~1.87) | −5.32 ± 3.50 (−13.2~0.58) | 5.59 (<0.001) |
| PSD (dB) | 1.41 ± 0.22 (1.02~1.85) | 6.80± 3.70 (1.96~14.46) | −5.39 (<0.001) | |
|
|
||||
| Macular Structure | GCC Thickness(μm) | 99.8 ± 5.7 (87.0~111.3) | 80.4 ± 10.9 (58.0~99.0) | 19.4 (<0.001) |
|
|
||||
| Macular Retinal Vessel Density (% area) | SVC | 60.5 ± 4.0(51.2~68.2) | 47.2 ± 7.1(31.3~60.5) | 13.3 (<0.001) |
| ICP | 38.4 ± 5.9(29.6~48.6) | 36.3 ± 4.7(28.0~46.7) | 2.1 (0.133) | |
| DCP | 26.3 ± 5.7(17.3~38.0) | 24.2 ± 7.0(12.7~40.4) | 2.1 (0.197) | |
| All-Plexus | 83.2 ± 4.2(72.5~89.6) | 73.5 ± 6.6(53.2~84.2) | 9.7 (<0.001) | |
Numbers displayed are mean ± standard deviation (range); MD = mean deviation, PSD = pattern standard deviation, GCC= ganglion cell complex, SVC= superficial vascular complex, ICP = intermediate capillary plexus, DCP = deep capillary plexus
Qualitative Assessment of Focal Capillary Dropout
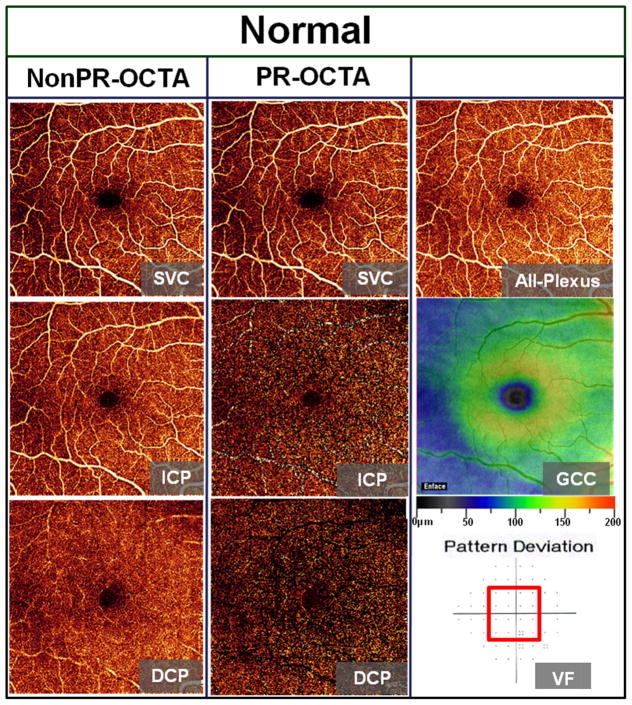
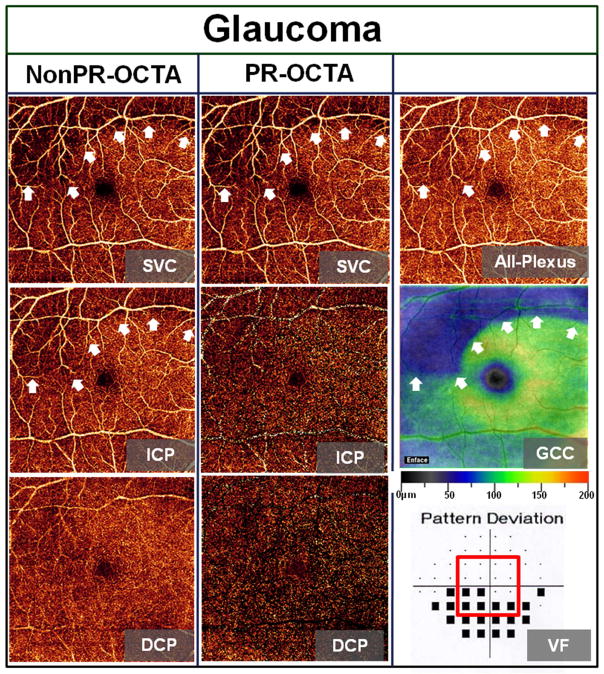
In the normal eye (Figure 2), the en face PR-OCTA of the SVC in the macula shows centripetally branching vessels, terminating in the central foveal avascular zone (FAZ). The vessel density is higher nasally, corresponding to the thicker NFL near the optic disc. The ICP and DCP are pure capillary layers of uniform vessel caliber and density, with the exception of the FAZ. The normal GCC is thickest in the parafoveal annulus, but absent in the fovea itself. The PR-OCTA and nonPR-OCTA SVC angiograms were identical as would be expected as this is the most superficial layer and thus should be devoid of projection artifacts. NonPR-OCTA angiograms showed vessel patterns in the SVC are duplicated in the ICP and DCP. The majority of artifactual duplication from the SVC were absent in PR-OCTA ICP and DCP angiograms. A perimetric glaucoma eye with a well-defined arcuate defect was chosen to demonstrate the regional correspondence between VD, GCC thickness, and VF (Figure 3). Severe capillary dropout could be visualized in the SVC within the arcuate defect, while the ICP and DCP were not visibly affected in PR-OCTA angiograms. However, focal defects and vessel patterns from the SVC are clearly projected in the ICP and DCP in nonPR-OCTA angiograms. Cross-sectional OCTA of the same eye (Figure 1) also demonstrated the correspondence between GCC thinning and loss of capillaries in the SVC. The all-plexus angiogram (Figure 3), which includes the SVC, ICP, and DCP, showed only mild decrease in vessel density in the area of the arcuate defect. Thus the SVC slab provided the best contrast for visualizing focal glaucomatous defect on en face PR-OCTA. The GCC map showed thinning in the same area as the SVC capillary dropout. The VF pattern deviation map shows an inferior arcuate defect matching the location of the SVC and GCC defects.
Figure 2.
The 6mm×6mm en face angiograms of a normal eye shown were from nonPR-OCTA (first column) and PR-OCTA (second column). The central 16 points (±10° enclosed in red line) of the Humphrey 24-2 visual field (VF) pattern deviation map approximately corresponds to the area of the 6mm×6mm PR-OCTA and ganglion cell complex (GCC) thickness maps.11 The vessel pattern in the SVC is duplicated in the nonPR-OCTA ICP and DCP angiograms. The majority of the projection artifacts were absent in the PR-OCTA ICP and DCP angiograms. Abbreviations: GCC= ganglion cell complex, SVC = superficial vascular complex, ICP = intermediate capillary plexus, DCP = deep capillary plexus. PR-OCTA= projection-resolved optical coherence tomography angiography.
Figure 3.
The 6mm×6mm en face angiograms of a perimetric glaucoma eye shown were from nonPR-OCTA (first column) and PR-OCTA (second column). The glaucomatous eye has a superior arcuate defect (arrows) appearing as focal decrease of vessel density on the PR-OCTA of the SVC and all-plexus slabs, as well as focal thinning on the GCC map. They correspond to the inferior VF defect (bottom 6 black squares within the red outlined area). The focal defects in the SVC are clearly projected in the nonPR-OCTA ICP angiogram (arrows). Abbreviations: GCC= ganglion cell complex, SVC = superficial vascular, ICP = intermediate capillary plexus, DCP = deep capillary plexus. PR-OCTA= projection-resolved optical coherence tomography angiography.
A masked qualitative grading was performed on en face OCTA of the SVC, ICP, and DCP separately. In the SVC angiograms, 27 (90%) glaucomatous eyes and 4 (13%) normal eyes were identified as having areas of capillary dropout. The ratios were significantly different (P<0.001). In the ICP angiograms, 16 (53%) glaucomatous eyes and 5 (16%) normal eyes were graded as having capillary dropout. The ratios were significantly different (P=0.004). In the DCP angiograms, 5 (16%) glaucomatous eyes and 6 (20%) normal eyes were graded as having capillary dropout. The ratios were similar (P=0.52).
Correlation of OCTA and Structural OCT Parameters with Clinical Variables
After the application of the Bonferroni correction for multiple comparisons, the SVC VD, all-plexus VD and GCC thickness in the glaucoma group were significantly lower than the normal group (all P <0.001, t test). The VD of the deeper plexuses (ICP and DCP) in the glaucoma group were not significantly lower than the normal group (Table 1).
In the normal group, the all-plexus VD and ICP VD were both correlated with age (r=−0.467, P=0.009, all-plexus VD = (−0.22*age+97.6)*100%; r=−0.539, P=0.002, ICP VD= (−0.107*age+67.5)*100%).
4 classes of glaucoma drops were used in 29 eyes. Prostaglandin analogs were used in 26 eyes. Beta-blockers were used in 10 eyes. Alpha agonists were used in 6 eyes. Topical carbonic anhydrase inhibitors were used in 15 eyes. Because SVC is the most relevant slab to glaucoma damage, a generalized linear model was performed to evaluate the correlation between glaucoma drops and SVC VD. The eyes with beta-blocker use had 3.3% lower macular SVC VD (P=0.043), after adjusting for macular GCC thickness.
Repeatability and Population Variation
In both normal and glaucoma participants, the SVC/all-plexus VD and GCC thickness all had excellent within-visit repeatability (Table 2). In comparison, the repeatability of ICP and DCP VD were significantly worse (P<0.025, Wilcoxon Signed Ranks Test). The SVC VD, all-plexus VD, and GCC thickness all had tight population variation. In comparison, ICP and DCP VD had wider population variation, but the difference was not statistically significant.
Table 2.
Repeatability and Normal Population Variability of Macular Parameters
| Group | Normal | Glaucoma | |
|---|---|---|---|
| Parameter | Within-visit repeatability(CV) | Population variation (CV) | Within-visit repeatability(CV) |
| SVC VD | 1.8% | 6.6% | 3.0% |
| ICP VD | 5.6% | 15.4% | 7.4% |
| DCP VD | 8.4% | 21.7% | 10.5% |
| All-Plexus VD | 1.7% | 5.0% | 2.4% |
| GCC Thickness | 1.2% | 5.7% | 1.9% |
CV= coefficient of variation, VD=vessel density, SVC= superficial vascular complex, ICP = intermediate capillary plexus, DCP = deep capillary plexus, GCC= ganglion cell complex.
Glaucoma Diagnostic Accuracy
The overall SVC VD had the best diagnostic accuracy among the global parameters, as judged by the sensitivity and area under the receiver operating curve (AROC) for differentiating normal and glaucoma eyes (Table 3). However, it did not differ significantly with all-plexus VD and GCC thickness AROCs (P>0.109). Similarly, parameters in the worse hemisphere had even higher diagnostic accuracy than the global parameters, but again the superiority was not statistically significant when comparing the SVC, all-plexus VD and GCC thickness. The best diagnostic accuracy was obtained with the SVC VD in the worse hemisphere, which had AROC of 0.983 and sensitivity of 96.7% at a fixed specificity of 95%.
Table 3.
Diagnostic Accuracy of Macular OCT Parameters
| Parameters | AROC | Sensitivity |
|---|---|---|
| Overall SVC VD | 0.961 | 80.0% |
| Overall All-plexus VD | 0.906 | 70.0% |
| Overall GCC Thickness | 0.950 | 76.7% |
| Worse Hemisphere SVC VD | 0.983 | 96.7% |
| Worse Hemisphere GCC Thickness | 0.973 | 86.7% |
Sensitivities at 95% specificity were evaluated. AROC=area under the receiver operating characteristic curve, GCC= ganglion cell complex, SVC= superficial vascular complex, ICP = intermediate capillary plexus, DCP = deep capillary plexus
Correlation with Traditional Glaucoma Diagnostic Measurements
In the glaucoma group, the overall SVC VD had excellent correlation with the GCC thickness and good correlation with the VF sensitivity averaged within the corresponding central 16 points (Table 4). These correlations were highly significant. The overall all-plexus VD did not correlate as well with GCC and had no significant correlation with VF. When the SVC VD and GCC thickness were divided into hemisphere, they had even higher correlation with VF sensitivity in the corresponding hemisphere (Table 5). This correlation was region specific, as there was no correlation with the non-corresponding hemisphere.
Table 4.
Correlation Matrix of Macular Parameters in Glaucoma Participants
| Parameters | SVC VD | All-Plexus VD | GCC Thickness |
|---|---|---|---|
| All-Plexus VD | 0.696 (0.000) | ||
| GCC Thickness | 0.804(0.000) | 0.435(0.016) | |
| VF Retinal Sensitivity* | 0.444(0.014) | 0.186(0.326) | 0.450(0.013) |
Pearson’s r (p-value); Statistically significant correlation (p < 0.05) are bold faced.
The visual field retinal sensitivity values were converted from dB to 1/lambert.
SVC = superficial vascular complex, GCC = ganglion cell complex, VF = visual field, VD= vessel density
Table 5.
Correlation of Hemisphere Macular Parameters in Glaucoma Participants
| Parameters | Superior VF Retinal Sensitivity* | Inferior VF Retinal Sensitivity* | Superior GCC Thickness | Inferior GCC Thickness |
|---|---|---|---|---|
| Superior SVC VD | 0.063(0.739) | 0.530 (0.003) | 0.827(0.000) | 0.284(0.128) |
| Inferior SVC VD | 0.689(0.000) | 0.082(0.668) | 0.299(0.109) | 0.845(0.000) |
Pearson’s r (p-value to test |R| = 0); Statistically significant correlation (p < 0.05) are bold faced. SVC = superficial vascular complex, VD= vessel density, GCC = ganglion cell complex, VF= visual field
The visual field retinal sensitivity values were converted from dB to 1/lambert.
Correlation of VD with Stage of Glaucoma
In the glaucoma group, both SVC VD (r= −0.369, P=0.045) and GCC thickness (r= −0.410, P=0.025) were significantly correlated with glaucoma stage, as determined by the enhanced Glaucoma Staging System.31 The all-plexus VD, ICP VD and DCP VD did not have statistically significant correlation with glaucoma stages.
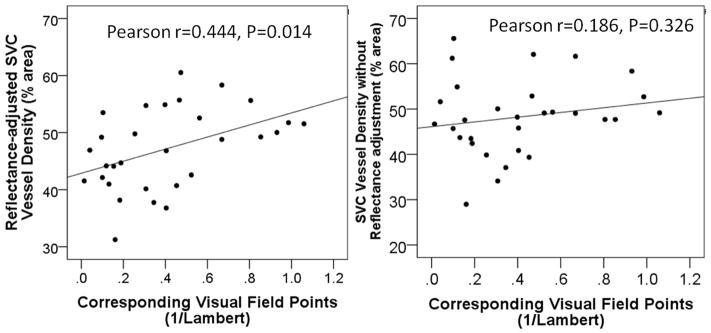
The Role of Reflectance Compensation in VD Measurements
The VD values shown above are compensated for retinal reflectance variation using a previously published method to adjust the threshold decorrelation value for distinguishing vessel from static tissue according to the local retinal reflectance value.29 To demonstrate the importance of this reflectance compensation method, we also calculated the SVC VD using a fixed threshold that does not compensate for reflectance variation. In normal participants, the population variation of the reflectance-adjusted macular SVC VD was 6.6% CV, which was smaller (P=0.013, F test) than the variation without reflectance adjustment (9.7% CV). The repeatability of the reflectance-adjusted SVC VD was 1.8% CV, which was better (0.002, Wilcoxon signed rank test) than the repeatability without reflectance adjustment (3.8% CV). The SVC VD without reflectance adjustment was correlated with signal strength index (Pearson r=0.731, P<0.001), while the reflectance-adjusted SVC VD was independent from signal strength index (Pearson r=0.107, P=0.416). The AROC was 0.961 for the reflectance-adjusted SVC VD, which was not significantly better than the AROC (0.933) for the SVC VD without reflectance adjustment. When the specificities were fixed at 95%, the sensitivities were the same (80%) for the two methods. In the glaucoma group, there was no correlation between the SVC VD without reflectance adjustment and the corresponding VF points (Pearson r=0.186, P=0.326). After the reflectance compensation, the SVC VD correlated well with the corresponding VF points (Pearson r=0.444, P=0.014) (Figure 4). The reflectance adjustment appears to reduce the spread (noise) in VD values and therefore improved the correlation with VF sensitivity. The reflectance compensation also improved the correlation between SVC VD and GCC thickness (from Pearson r 0.616 to 0.804, both P<0.001).
Figure 4.
Plots of reflectance-adjusted SVC vessel density versus corresponding visual field retinal sensitivity (left) and SVC vessel density without reflectance adjustment versus corresponding visual field retinal sensitivity (right).
Discussion
Studies using OCTA have shown that glaucoma reduces perfusion in the optic nerve head and the peripapillary retina.14–19 But the 6mm × 6mm macular region has not been studied with this new imaging technology. Since glaucoma damages retinal ganglion cells (RGC) and approximate 1/3 of RGCs resides in the macula, macular perfusion is theoretically a good place to detect glaucoma and assess disease severity.4, 5 Structural OCT studies have shown that the macular GCC thickness and other measures of RGC volume are reduced in glaucoma patients,6–8 and focal loss of macular GCC is a good predictor of VF conversion and progression.13 Measuring the macular perfusion has the potential for detecting reduced metabolic rate in dysfunctional in RGCs before they undergo apoptosis and cause the GCC to become thinner. This study aimed to evaluate whether macular VD, as measured by OCTA, is decreased in glaucomatous eyes, and if so, to characterize the regional correlation with VF and structural OCT parameters.
In order to better characterize the location of decreased perfusion in glaucomatous eyes, we used a “projection-resolved” algorithm to remove flow projection artifacts.20 This algorithm allowed us to separately analyze the retinal circulation in three layers: SVC, ICP, and DCP. We found that glaucoma affected the SVC to a much greater degree than the deep vascular complex (DVC, comprising the ICP and DCP). This was shown by both qualitative grading of focal capillary dropout as well as automated quantitative VD measurements. It is not surprising that the SVC VD was greatly reduced in glaucomatous eyes, as it supplies the NFL, GCL, and part of the IPL,25, 27, 32 the anatomic layers most affected by glaucoma.6, 8–10 The ICP also partly supplies the IPL, but its density was only slightly reduced by glaucoma in this study. And the DCP was minimally affected by glaucoma, as it supplies the middle retinal layers that do not include the retinal ganglion cells.
While the PR-OCTA algorithm aids in removing flow projection artifacts, it does not do so perfectly. The en face OCTA of the ICP and DCP still show some residual projection and shadow artifacts that are visible under large retinal vessels in the SVC. However, the repeatability of the overall VDs in all of the plexuses were all acceptable. And we were able to show that ICP and DCP are mostly preserved in glaucomatous eyes, which suggests that PR-OCTA was effective in removing most of the projection artifacts. If conventional OCTA were used, one would see a duplication of SVC vascular patterns in the deeper retinal layers, including the ICP and DCP slabs,33–37 and this would have led to an erroneous impression that ICP and DCP are also affected by glaucoma. However, for glaucoma evaluation, both PR-OCTA and nonPR-OCTA will work. Because SVC is the preferential affected layer and there’s no projection artifact in this most superficial layer.
Although the DVC was only minimally reduced in glaucoma, it is not clear a priori whether combining it with the SVC to obtain measurement of the all-plexus retinal circulation would aid or hinder the diagnosis of glaucoma. On one hand, including the DVC in VD measurement might introduce noise from tissue unaffected by glaucoma. On the other hand, segmentation of the all-plexus retinal slab is easier than segmentation of the narrower SVC slab, and might provide more robust results. Our results showed that although the all-plexus retinal VD was slightly more repeatable than SVC-VD, the diagnostic accuracy was better using the SVC-VD. Although the difference in diagnostic accuracy was not statistically significant due to the limited sample size, we were able to further demonstrate that SVC-VD was significantly better correlated with VF sensitivity in the macular test points. Thus for the purpose of glaucoma assessment, it is advantageous to assess the SVC perfusion and exclude the DVC.
Qualitative grading of SVC angiograms also showed good sensitivity (90%) and specificity (87%) for distinguishing glaucomatous and normal eyes. Thus even in the absence of automated diagnostic parameters in commercial OCTA systems, the clinician could already use the en face SVC angiogram to visualize capillary dropout and evaluate glaucoma damage. There is a need to develop automated software to identification of areas of reduced capillary perfusion, which could improve the evaluation of focal glaucoma damage.
The SVC VD in the worse hemisphere (either superior or inferior) had excellent diagnostic accuracy with an AROC of 0.983 and a sensitivity of 96.7% at 95% specificity. This compares favorably with the diagnostic accuracy in studies that used structural OCT parameters for diagnosis in comparable groups of perimetric glaucoma subjects (mostly early to moderate stage).6, 8, 38 Our sample size of 30 glaucoma and 30 normal participants would only be able to detect a statistically significant difference from an AROC of 0.983 if the comparative AROC were 0.900 or less. Thus, we are not able to detect a significant difference in diagnostic accuracy between OCTA and structural OCT parameters. A larger study with higher statistical power is needed to compare OCTA and structural OCT in the diagnosis of glaucoma.
The diagnostic accuracy of macular OCTA had been studied by Rao et al. in comparison with peripapillary and disc OCTA.39 In sharp contrast to our results, they found that macular vessel density had poor diagnostic accuracy (AROC = 0.69), significantly worse than that of the whole disc/peripapillary region (AROC = 0.90). Our higher diagnostic accuracy was most likely due to a much larger macular scan area of 6mm×6mm compared to the small scan area of 3mm×3mm used by Rao et al. The macular area that is most vulnerable to glaucoma is inferior and inferotemporal, lying mostly outside the central 3mm×3mm area.11 We further improved AROC by measuring the vessel density in the SVC and compensating for variation in OCT signal strength. The glaucoma populations in the two studies were similar in terms of the severity of visual field damage as summarized by mean deviation.
In our previous work, we noticed that OCTA flow signals were affected by the structural OCT reflectance signal strength. Vessels under vitreous opacities appeared fainter on OCTA, and eyes with lower signal strength index tended to have lower retinal VD. We developed a method to adjust for the effect of reflectance on vessel density.29 This algorithm effectively removes the dependence of VD on the signal strength index. However, it was not known a priori whether the reflectance-adjustment would aid or hinder glaucoma diagnostic accuracy. On one hand, the reflectance adjustment could provide more accurate VD measurements by removing variability due to factors that affect signal strength (media opacity, pupil vignetting, defocus). On the other hand, the glaucomatous retina might have lower tissue reflectivity and adjusting for reflectance might remove this contributory diagnostic information. Our results empirically demonstrated that reflectance-adjustment significantly improved the repeatability of the SVC VD measurements in both normal and glaucoma groups, as well as reducing the normal population variation. Reflectance adjustment also improved glaucoma diagnostic accuracy was also improved, but statistical significance could not be demonstrated due to the small sample size. The importance of using the reflectance-adjusted vessel density became clear when evaluating the association between SVC VD and visual field defects. Without the reflectance adjustment, there was no significant association between SVC VD and retinal sensitivity in the corresponding VF points. With the reflectance adjustment, there was a significant association between SVC VD and retinal sensitivity (Figure 4), indicating that it improved the measurement of disease severity. Overall, our results indicate that reflectance adjustment is helpful when using macular OCTA to evaluate glaucoma.
Currently, visual field testing remains the gold-standard for assessing glaucoma severity and progression.40 However, patients often having difficulty taking a visual field test, and often lengthy procedure, and repeatability is a problem with this subjective test.41, 42 In contrast, both SVC VD with reflectance adjustment and GCC thickness data provide quick, objective data that shows excellent correlation with VF measures and disease severity. Thus SVC VD and GCC thickness data may be well positioned to provide an objective, quantitative measure of glaucoma severity. Our results didn’t show SVC VD to be superior to GCC thickness in terms of diagnosis of glaucoma and correlation with visual field which may limit clinical utility. However, the two parameters may be complementary and further studies will be needed. The excellent reproducibility of SVC VD and GCC thickness suggests that they may offer a precise way of monitoring disease progression. Further longitudinal studies are warranted.
Hand in hand with the need for further longitudinal studies is the need for further age-adjusted normative data on OCTA paramenters.43 Our data suggests that all-plexus VD in normal participants may decline with age at a rate of approximately 0.2% per year. This number is remarkably similar to the age-related rate of GCC and NFL thinning found in a recent longitudinal study of OCT structural parameters,44 raising the intriguing possibility that the age-related decline in both retinal VD and thickness may be aspects of the same process. However, the small sample size and cross-sectional nature of our current study precludes making any definitive conclusions.
Another limitation of this study was that pre-perimetric glaucoma patients and glaucoma suspects were not included. Therefore we could not draw conclusions concerning diagnostic accuracy in the earliest stages of glaucoma.
Our study also found an association between beta-blocker eye drop use and decreased macular SVC VD. The causative explanation could be that beta blockers have a direct vasocontrictive effect that decreased vessel density, which would have implications on the use of beta blocker eye drops compared to a choice of other glaucoma medications. However, we cannot yet conclude that beta-blocker caused a reduction in blood flow because the regression analysis could be affected by selection bias. Although we have already adjusted for the effect of glaucoma severity by using GCC thickness as a covariate in the analysis, we cannot completely rule out the possibility that participants with worse glaucoma, and thus decreased SVC VD, may be more likely to be using a beta-blocker. Further prospective investigations of glaucoma drop use on ocular perfusion are needed. In any case, the beta-blocker effect is too small to account for the dramatically decreased SVC VD that we identified in glaucoma patients – that is clearly due to glaucoma damage given the high correlation with the severity and location of VF and GCC defects.
In summary, we showed that OCTA evaluation of the macula could measure VD with high repeatability and detect glaucoma damage with high sensitivity. Focusing the vessel density analysis to the SVC slab and the use of a reflectance-compensation method to reduce the effect of signal strength variation appeared to enhance glaucoma diagnostic accuracy and correlation with disease severity as measured by VF and GCC thickness. Both SVC VD and GCC thickness correlated well with VF, and may work synergistically to serve as an objective alternative for central VF assessment in glaucoma diagnosis and monitoring. Several OCT companies have introduced OCTA products that could assess perfusion in the macular and optic nerve regions. We hope the results presented here will help motivate and guide further investigations of OCTA in glaucoma evaluation.
Supplementary Material
Acknowledgments
Financial Support: NIH grants R01 EY023285, P30 EY010572, Oregon Health & Science University (OHSU) foundation, NSFC (Grant No. 61471226), and by unrestricted departmental funding from Research to Prevent Blindness (New York, NY). The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Partially presented at the American Glaucoma Society (AGS) annual meeting, March 2016 Fort Lauderdale, FL, USA, and the Association for Research in Vision and Ophthalmology (ARVO) annual meeting, May, 2016, Seattle, WA, USA.
Conflict of interest: OHSU, Yali Jia, and David Huang have financial interest in Optovue, Inc., a company that may have a commercial interest in the results of this research and technology. These potential conflicts of interest have been reviewed and managed by OHSU. Other authors do not have financial interest in the participant of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leske MC. Open-angle glaucoma -- an epidemiologic overview. Ophthalmic Epidemiol. 2007;14(4):166–72. doi: 10.1080/09286580701501931. [DOI] [PubMed] [Google Scholar]
- 3.Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003;290(15):2057–60. doi: 10.1001/jama.290.15.2057. [DOI] [PubMed] [Google Scholar]
- 4.Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107(5):453–64. doi: 10.1016/0002-9394(89)90488-1. [DOI] [PubMed] [Google Scholar]
- 5.Curcio CA, Allen KA. Topography of ganglion cells in human retina. The Journal of comparative neurology. 1990;300(1):5–25. doi: 10.1002/cne.903000103. [DOI] [PubMed] [Google Scholar]
- 6.Tan O, Chopra V, Lu AT, et al. Detection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomography. Ophthalmology. 2009;116(12):2305–14. e1–2. doi: 10.1016/j.ophtha.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan O, Li G, Lu AT, et al. Mapping of macular substructures with optical coherence tomography for glaucoma diagnosis. Ophthalmology. 2008;115(6):949–56. doi: 10.1016/j.ophtha.2007.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mwanza JC, Durbin MK, Budenz DL, et al. Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology. 2012;119(6):1151–8. doi: 10.1016/j.ophtha.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 9.Burgansky-Eliash Z, Wollstein G, Chu T, et al. Optical coherence tomography machine learning classifiers for glaucoma detection: a preliminary study. Invest Ophthalmol Vis Sci. 2005;46(11):4147–52. doi: 10.1167/iovs.05-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loewen NA, Zhang X, Tan O, et al. Combining measurements from three anatomical areas for glaucoma diagnosis using Fourier-domain optical coherence tomography. Br J Ophthalmol. 2015;99(9):1224–9. doi: 10.1136/bjophthalmol-2014-305907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hood DC, Raza AS, de Moraes CG, et al. Glaucomatous damage of the macula. Prog Retin Eye Res. 2013;32:1–21. doi: 10.1016/j.preteyeres.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Traynis I, De Moraes CG, Raza AS, et al. Prevalence and nature of early glaucomatous defects in the central 10 degrees of the visual field. JAMA ophthalmology. 2014;132(3):291–7. doi: 10.1001/jamaophthalmol.2013.7656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang X, Loewen N, Tan O, et al. Predicting Development of Glaucomatous Visual Field Conversion Using Baseline Fourier-Domain Optical Coherence Tomography. Am J Ophthalmol. 2016;163:29–37. doi: 10.1016/j.ajo.2015.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jia Y, Wei E, Wang X, et al. Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology. 2014;121(7):1322–32. doi: 10.1016/j.ophtha.2014.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu L, Jia Y, Takusagawa HL, et al. Optical Coherence Tomography Angiography of the Peripapillary Retina in Glaucoma. JAMA ophthalmology. 2015;133(9):1045–52. doi: 10.1001/jamaophthalmol.2015.2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yarmohammadi A, Zangwill LM, Diniz-Filho A, et al. Relationship between Optical Coherence Tomography Angiography Vessel Density and Severity of Visual Field Loss in Glaucoma. Ophthalmology. 2016;123(12):2498–508. doi: 10.1016/j.ophtha.2016.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suh MH, Zangwill LM, Manalastas PI, et al. Optical Coherence Tomography Angiography Vessel Density in Glaucomatous Eyes with Focal Lamina Cribrosa Defects. Ophthalmology. 2016;123(11):2309–17. doi: 10.1016/j.ophtha.2016.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hollo G. Vessel density calculated from OCT angiography in 3 peripapillary sectors in normal, ocular hypertensive, and glaucoma eyes. Eur J Ophthalmol. 2016;26(3):e42–5. doi: 10.5301/ejo.5000717. [DOI] [PubMed] [Google Scholar]
- 19.Lee EJ, Lee KM, Lee SH, Kim TW. OCT Angiography of the Peripapillary Retina in Primary Open-Angle Glaucoma. Invest Ophthalmol Vis Sci. 2016;57(14):6265–70. doi: 10.1167/iovs.16-20287. [DOI] [PubMed] [Google Scholar]
- 20.Zhang M, Hwang TS, Campbell JP, et al. Projection-resolved optical coherence tomographic angiography. Biomed Opt Express. 2016;7(3):816–28. doi: 10.1364/BOE.7.000816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yali Jia PLB, MD, Gao Simon, PhD, Huang David, MD, PhD, Wilson David J., MD Chapter 3: Cross-Sectional and En Face Visualization of Posterior Eye Circulations. 2017 in press. [Google Scholar]
- 22.Jia Y, Tan O, Tokayer J, et al. Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express. 2012;20(4):4710–25. doi: 10.1364/OE.20.004710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kraus MF, Potsaid B, Mayer MA, et al. Motion correction in optical coherence tomography volumes on a per A-scan basis using orthogonal scan patterns. Biomed Opt Express. 2012;3(6):1182–99. doi: 10.1364/BOE.3.001182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao Simon SYJ. David Huang Chapter 5: Artifacts in Optical Coherence Tomography Angiography. Optical Coherence Tomography Angiography of the Eye. 2017 in press. [Google Scholar]
- 25.Snodderly DM, Weinhaus RS, Choi JC. Neural-vascular relationships in central retina of macaque monkeys (Macaca fascicularis) The Journal of neuroscience: the official journal of the Society for Neuroscience. 1992;12(4):1169–93. doi: 10.1523/JNEUROSCI.12-04-01169.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Provis JM. Development of the primate retinal vasculature. Prog Retin Eye Res. 2001;20(6):799–821. doi: 10.1016/s1350-9462(01)00012-x. [DOI] [PubMed] [Google Scholar]
- 27.Snodderly DM, Weinhaus RS. Retinal vasculature of the fovea of the squirrel monkey, Saimiri sciureus: three-dimensional architecture, visual screening, and relationships to the neuronal layers. The Journal of comparative neurology. 1990;297(1):145–63. doi: 10.1002/cne.902970111. [DOI] [PubMed] [Google Scholar]
- 28.Campbell JP, Zhang M, Hwang TS, et al. Detailed Vascular Anatomy of the Human Retina by Projection-Resolved Optical Coherence Tomography Angiography. Sci Rep. 2017;7:42201. doi: 10.1038/srep42201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao Simon SYJ, Liu Liang, Zhang Miao, Takusagawa Hana L, Morrison John C, Huang David. Compensation for Reflectance Variation in Vessel Density Quantification by Optical Coherence Tomography Angiography. Invest Ophthalmol Vis Sci. 2016 doi: 10.1167/iovs.16-20080. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45. [PubMed] [Google Scholar]
- 31.Brusini P, Filacorda S. Enhanced Glaucoma Staging System (GSS 2) for classifying functional damage in glaucoma. J Glaucoma. 2006;15(1):40–6. doi: 10.1097/01.ijg.0000195932.48288.97. [DOI] [PubMed] [Google Scholar]
- 32.Provis JM. Development of the primate retinal vasculature. Progress in retinal and eye research. 2001;20(6):799–821. doi: 10.1016/s1350-9462(01)00012-x. [DOI] [PubMed] [Google Scholar]
- 33.Spaide RF, Fujimoto JG, Waheed NK. Image Artifacts in Optical Coherence Tomography Angiography. Retina. 2015;35(11):2163–80. doi: 10.1097/IAE.0000000000000765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferrara D. Image artifacts in optical coherence tomography angiography. Clinical & experimental ophthalmology. 2016;44(5):367–8. doi: 10.1111/ceo.12781. [DOI] [PubMed] [Google Scholar]
- 35.Zhang A, Zhang Q, Wang RK. Minimizing projection artifacts for accurate presentation of choroidal neovascularization in OCT micro-angiography. Biomedical optics express. 2015;6(10):4130–43. doi: 10.1364/BOE.6.004130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang M, Hwang TS, Campbell JP, et al. Projection-resolved optical coherence tomographic angiography. Biomedical optics express. 2016;7(3):816–28. doi: 10.1364/BOE.7.000816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.David Huang BL, Jia Yali, Waheed Nadia K. Chapter 5:Artifacts in optical Coherence Tomography Angiography. Optical Coherence Tomography Angiography of the Eye SLACK Incorporated. 2017 in press. [Google Scholar]
- 38.Mwanza JC, Oakley JD, Budenz DL, Anderson DR. Ability of cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology. 2011;118(2):241–8. e1. doi: 10.1016/j.ophtha.2010.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rao HL, Pradhan ZS, Weinreb RN, et al. Regional Comparisons of Optical Coherence Tomography Angiography Vessel Density in Primary Open-Angle Glaucoma. Am J Ophthalmol. 2016;171:75–83. doi: 10.1016/j.ajo.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 40.Sharma P, Sample PA, Zangwill LM, Schuman JS. Diagnostic tools for glaucoma detection and management. Survey of ophthalmology. 2008;53(Suppl1):S17–32. doi: 10.1016/j.survophthal.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Keltner JL, Johnson CA, Anderson DR, et al. The association between glaucomatous visual fields and optic nerve head features in the Ocular Hypertension Treatment Study. Ophthalmology. 2006;113(9):1603–12. doi: 10.1016/j.ophtha.2006.05.061. [DOI] [PubMed] [Google Scholar]
- 42.Keltner JL, Johnson CA, Levine RA, et al. Normal visual field test results following glaucomatous visual field end points in the Ocular Hypertension Treatment Study. Archives of ophthalmology. 2005;123(9):1201–6. doi: 10.1001/archopht.123.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coscas F, Sellam A, Glacet-Bernard A, et al. Normative Data for Vascular Density in Superficial and Deep Capillary Plexuses of Healthy Adults Assessed by Optical Coherence Tomography Angiography. Investigative ophthalmology & visual science. 2016;57(9):OCT211–23. doi: 10.1167/iovs.15-18793. [DOI] [PubMed] [Google Scholar]
- 44.Zhang X, Francis BA, Dastiridou A, et al. Longitudinal and Cross-Sectional Analyses of Age Effects on Retinal Nerve Fiber Layer and Ganglion Cell Complex Thickness by Fourier-Domain OCT. Translational vision science & technology. 2016;5(2):1. doi: 10.1167/tvst.5.2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.