Abstract
Objective: Ear acupuncture might be the form of acupuncture best suited to improving acute pain management in the emergency department (ED). The primary aim of this review was to assess the analgesic efficacy of ear acupuncture in the ED. Secondary outcomes included measures of patient satisfaction, adverse effects, cost, administration techniques, and reduction of medication usage.
Methods: Seven databases and Google Scholar were searched up to April 27, 2017, using MeSH descriptors for three overarching themes (ear acupuncture, pain management, and emergency medicine). Meta-analyses were performed in 3 comparator groups: (1) ear acupuncture versus sham; (2) ear acupuncture-as-adjunct to standard care; and (3) ear acupuncture (both as sole therapy and adjuvant) versus control to calculate the standardized mean difference (SMD) and weighted mean difference (WMD) for pain scores out of 10.
Results: Six randomized controlled trials and 2 observational studies, totaling 458 patients, were retrieved after exclusions. The meta-analysis used data from 4 randomized studies representing 286 patients. The above 3 comparator groups resulted in SMDs of 1.69, 1.68, and 1.66, and WMDs of 2.47, 2.84, and 2.61 respectively, all favoring acupuncture. Battlefield (ear) acupuncture was the most commonly used technique. There were no significant adverse effects and patient satisfaction improved. Results regarding if acupuncture reduced medication use were equivocal. Significant study bias and heterogeneity were found.
Conclusions: While study numbers are limited, ear acupuncture, either as stand-alone or as-an-adjunct technique, significantly reduced pain scores and has potential benefits for use in the ED. Further studies will define acupuncture's role and if it reduces use of analgesic medications.
Keywords: : ear acupuncture, auriculotherapy, emergency medicine, pain management, systematic review, meta-analysis
Introduction
Pain is the most common presenting symptom in patients presenting in an emergency department (ED).1–4 ED pain management is often characterized by delays in analgesia as well as inadequate pain-score reduction.5,6 Furthermore, EDs continue to seek improved patient satisfaction with pain management.7 The current mainstay of pain management is medication.8 However, medications have significant side-effects in both the short- and long-term.9–11 Of particular concern is recurrent opioid use,12 which, in part, can lead to a reluctance to prescribe and administer such medications.13 Nonsteroidal anti-inflammatory drugs (NSAIDs), another mainstay of ED pain management, also have side-effects especially in the gastrointestinal system and kidneys in the elderly.14
Characteristics ideally required for any new analgesic modality are: efficacy, rapidity of administration, low side-effects, minimal post-administration monitoring, improved patient satisfaction, and low cost.9 A novel modality such as ear acupuncture might offer a solution for these issues.
In 2014, Yeh et al. performed a meta-analysis of pain score reduction, using ear acupuncture for acute and chronic pain in a variety of comparator groups and settings.15 The researchers concluded that ear acupuncture is useful as an adjunct therapy for pain management. This conclusion was based on a meta-analysis of 13 randomized controlled trials (RCTs), totaling 806 patients with a mixture of pain types. The researchers reported a standardized mean difference (SMD) in pain reduction of 1.59, indicating a large effect-size.15 Further subgroup analyses of immediate pain score reduction under 15 minutes in 4 studies with 193 patients reported an SMD of 2.84.15 For acute pain relief at 12–24 hours, there were 4 studies including 314 patients and, here, the SMD was 1.71.15 When reviewing various modalities (i.e., acupuncture versus acupressure versus electroacupuncture [EA]), the researchers found that EA was the least effective. Unfortunately, most of the studies were on perioperative and not on ED pain and, furthermore, an emergency setting RCT was missed in this review.16
Murakami et al. did a further review in 2016 on ear acupuncture for acute pain relief, particularly looking at analgesic use up to 48 hours.17 The researchers' meta-analysis of 6 studies included 303 patients and showed a statistically significant reduction in analgesia usage with an SMD of 1.08.17 Again, the studies were predominantly perioperative and not in the emergency setting.
The current authors performed a prior review that analyzed both body and ear acupuncture together in the ED setting and concluded that acupuncture was superior to sham and non-inferior to standard analgesic care (SAC) in selected conditions, with limited evidence for analgesia as-an-adjunct.18 This conclusion was based on meta-analyses of 14 RCTs involving 1210 patients.
Therefore, unlike other prior reviews, which focused on perioperative pain, the current authors identified a need for a specific systematic review that focused on the effectiveness of ear acupuncture for acute pain in the emergency setting, while asking further questions about applicability and best technique.
Objectives
The primary aim of the current systematic review and meta-analysis was to specifically evaluate the effectiveness of ear acupuncture for acute pain management in the emergency setting. Changes in acute pain scores were assessed with ear acupuncture as a stand-alone therapy or ear acupuncture-as-an-adjunct to other analgesia (AdjEA), compared with SAC. Secondarily, acupuncture-associated effects were evaluated on analgesic medication use, patient satisfaction, adverse events, and health care costs. Furthermore, the current authors aimed to describe the specific acupuncture techniques and acute pain conditions for which acupuncture was applied. See Table 1 for explanations of terms.
Table 1.
Key Terms and Study Definitions
| Term | Definition |
|---|---|
| Acute pain | “Acute pain is defined as pain of recent onset and probable limited duration. It usually has an identifiable temporal and causal relationship to injury or disease.”aAcute pain management occurs in a variety of patient-care settings (e.g., prehospital, emergency department, and perioperative environments. b In all settings, patients may suffer from acute and chronic pain simultaneously. |
| Ear acupuncture | Ear acupuncture or auriculotherapy includes: ear acupuncture with needle skin penetration, electroacupuncture stimulation, laser acupuncture, and acupressure.c Unless otherwise specified, ear acupuncture includes all forms of auriculotherapy. |
| Sham ear acupuncture | “Sham is the term used to refer to a faked operative intervention used in the same manner as a placebo to enable blinding and reduce bias.”21 In ear acupuncture, sham includes: “1. same treatment on ear acupoints that are not theoretically effective for the condition; 2. same treatment on non-acupoints on the ear; 3. placebo needles or adhesive patches without pellet/seed on the same ear acupoints as experimental group; 4. pseudo-interventions (e.g., switched-off laser acupuncture devices, electro-acupuncture devices with minimum emission, Vaccaria seeds without pressing) on the same ear acupoints as [the] experimental group.”d The current authors would also include pharmacologic placebo techniques in this pseudo-intervention group. |
| Sham ear acupuncture trial (sham) | This is a trial comparing ear acupuncture alone against sham ear acupuncture alone. |
| Standard analgesia care (SAC) trial | This is a trial that use the SAC of pain care designated by the local institution, researcher, or guidelines as the comparator against acupuncture. |
| Ear acupuncture-as-an-adjunct to other analgesia (AdjEA) trial | This is a trial in which SAC is combined with ear acupuncture versus SAC alone. |
Ready LB, Oden R, Chadwick HS, Benedetti C, Rooke GA, Caplan R, Wild LM. Development of an anesthesiology-based postoperative pain management service. Anesthesiology. 1988;68(1):100–106.
Tighe P, Buckenmaier CC 3rd, Boezaart AP, et al. Acute pain medicine in the United States: A status report. Pain Med. 2015;16(9):1806–1826.
Ref. 15.
Ref. 40.
Methods
The methodology for this study was closely aligned to that of the current authors' previous systematic review and meta-analysis of all forms of acupuncture18 and was approved as part of the first author's PhD proposal by the University of Notre Dame Fremantle, in Fremantle, Western Australia. The current systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.19 Seven databases were searched from database inception to April 27, 2017: AMED, CINAHL, EMBASE, PubMed®, Science Direct, Scopus, and the Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials (CENTRAL). Additional studies were identified by hand searches of the proceedings of key scientific meetings, the Conference Papers Index, relevant systematic reviews, and Google Scholar. Three themes were explored using a Boolean search strategy: (1) ear acupuncture; (2) pain management; and (3) emergency medicine. The search used MeSH terms and keywords relevant to: the intervention (auricular acupuncture, ear acupuncture, battlefield acupuncture, auriculoacupuncture, auriculotherapy, auricular therapy); pain management (pain, acute pain, analgesia); and the setting (emergency medical services, emergency, prehospital, retrieval medicine, emergency department, acute care, military).
Inclusion and Exclusion Criteria
All potentially eligible articles identified were screened for appropriate RCTs and uncontrolled observational studies (UOBS) independently by the first 2 authors (A.L.J., E.S.A.) for inclusion or exclusion. Any discrepancies were resolved by consensus or discussion with the other coauthors. RCTs were eligible for both the systematic review and meta-analysis, while UOBS were included in the systematic review for information on secondary outcomes. Studies on acutely painful conditions treated by ear acupuncture were included if they involved the following settings: prehospital, retrieval, ED, or other settings if the condition is frequently managed in the ED. Studies on painful conditions were excluded if they were: not assessed within the first 24 hours; not involved with ear acupuncture; chronic conditions; involving animals; or concerned with perioperative pain. No language restrictions were applied.
Data Extraction
All of the eligible studies were read by the first 2 authors (A.L.J. and E.S.A.), who extracted data from the articles according to a predefined standard template based on the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines.20 This data for each article included information regarding: condition, setting, subjects, methods for both intervention and control groups, and data for both the primary and secondary outcomes, including relevant statistical information. Any missing data were derived from within the article, other sources, or by contacting the authors.
Data Synthesis
Primary outcome
While all clinical endpoints were considered, the primary outcome measure in this review was the pain score out of 10 (PS-10) difference in 3 comparator treatment groups: (1) ear acupuncture versus sham; (2) AdjEA versus SAC; and (3) ear acupuncture (sole therapy and AdjEA) versus control presented as the SMD and WMD.
To be included in the meta-analysis, a converted PS-10 mean score change along with standard deviations (SDs) needed to be retrieved or calculated. Different pain-score modes and scales (e.g., visual analogue scale 100 or 10) were converted to a standard numerical pain-rating scale, the PS-10, as a continuous variable. Pain scores closest to 60 minutes after treatment were used. For those SDs that were not provided, they were calculated from the pre-and-post PS-10 SD, using the correlation coefficient approximated to 0.5 as outlined in the Cochrane Handbook.21 In one study, the SDs were approximated from similar studies by the same authors under similar trial circumstances.16,22,23
Secondary outcomes
Medication usage included opioids and nonopioids, the frequency of usage both during and post ED stay, and the rate of discharge analgesic dispensing and prescriptions. Patient satisfaction was measured either on a continuous scale out of a 100 or percentages chosen for specified Likert categories. Adverse effects were coded as minor (required no treatment) or significant (required treatment) for both acupuncture and control groups. Ear acupuncture techniques were described regarding: training of the acupuncturist, acupoints used, methods of point location, whether unilateral or bilateral, needle types (or acupressure alone), duration of application, EA, and needle retention times. Time-based outcomes were measured as: time taken to perform procedures (e.g., needling time in minutes) and the duration of needle insertion. The cost of acupuncture consumables was expressed in U.S. dollars per person if specified.
Risk of bias
The risk of bias was assessed, using the following criteria from the Cochrane Classification: sequence generation, allocation concealment, subject, practitioner, and assessor blinding, completeness of outcomes data (reporting dropouts and withdrawals), selective reporting, and any other potential forms of bias.21 Using the same method as the current authors' prior review on all forms of acupuncture,18 bias was categorized into low (low risk of bias in all criteria), medium (high risk of bias in patient and practitioner blinding), or high (risk of bias in multiple items). Again, any discrepancies between data abstractors were resolved by consensus or discussion with the other coauthors.
Meta-analyses
Stata software (14.1 StataCorp,™ College Station, TX, 2015) was used to perform the statistical analyses and calculate the SMD and WMD from the pooled RCT data. The magnitude of the effect-size was categorized as small (SMD of 0.2), medium (SMD of 0.5) or large (SMD of 0.8).24 A WMD for the PS-10 of >1.3 was regarded as clinically meaningful.25 Study heterogeneity (I2) was provisionally assigned as low (I2 of 25%), moderate (I2 of 50%), or high (I2 of 75%).26 Probability values (P) were considered to indicate statistical significance if P < 0.05.27
Results
Of the 149 studies found, 8 were included in the systematic review and/or meta-analysis (Fig. 1). In total, 4 RCTs were included in the meta-analysis, and a further 2 RCTs and 2 UOBS were used in the systematic review (Table 2). Two of the RCTs had inadequate data for meta-analysis.28,29 The studied conditions included mixed pain types (2 studies), migraine (2 studies), hip fractures, low-back pain, sore throats, and biliary colic. The most frequent forms of ear acupuncture were BFA (4 studies) 28,30–32 and ear acupuncture using a point finder (skin conduction and algometer; 2 studies).33,34 (Fig. 1 and Table 2)
FIG. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) chart explaining study selection and exclusions. RCTs, randomized controlled trials; UOBS, uncontrolled observational studies.
Table 2.
Included Studies Detailing Acute Pain Type, Setting & Study Design
| First author, year & ref. | Acute pain type | Study setting | Study type |
|---|---|---|---|
| Allais, 201133 | Migraine | Ward | RCT ear acupuncture vs. sham |
| Barker, 200616 | Hip fractures | Ambulance | RCT ear acupressure vs. sham |
| Goertz, 200631 | Pain not requiring medical intervention | ED | RCT AdjEA & SAC vs. SAC alone |
| Gu, 199329 | Biliary colic | ED | RCT ear acupuncture vs. SAC |
| Moss, 201532 | Sore throat | GP Military | RCT ear acupuncture & SAC vs. SAC alone |
| Fox, 201628a | Low-back pain | ED | RCT ear acupuncture & SAC vs. SAC alone |
| Burns, 201330 | All types | Retrieval | Observational study of ear acupuncture & SAC |
| Graff, 201634 | Migraines | ED | Observational study of ear acupuncture alone |
Abstract only.
RCT, randomized controlled trial; AdjEA, ear acupuncture-as-an-adjunct to other analgesia; SAC, standard analgesia care; ED, emergency department; GP, general (family) practice.
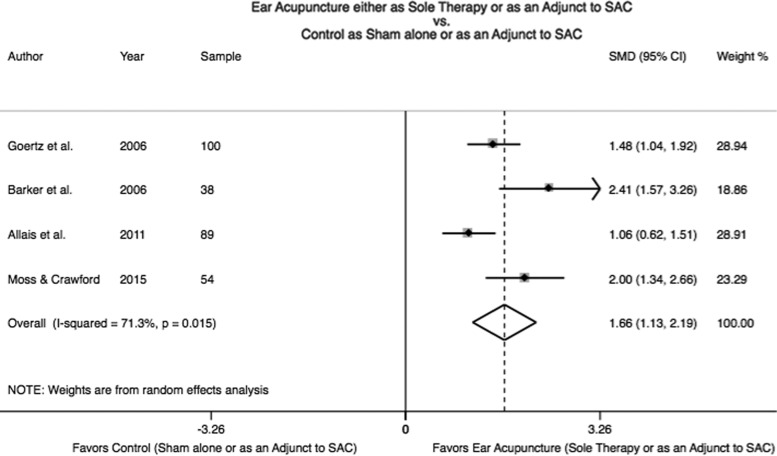
Primary Outcome
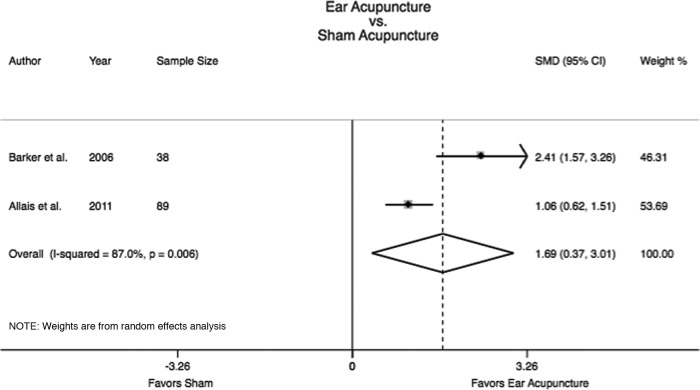
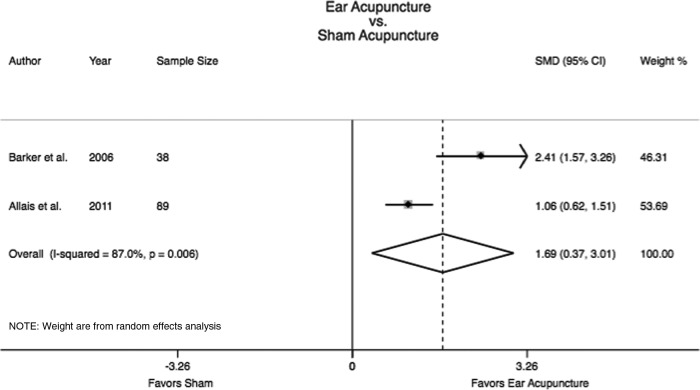
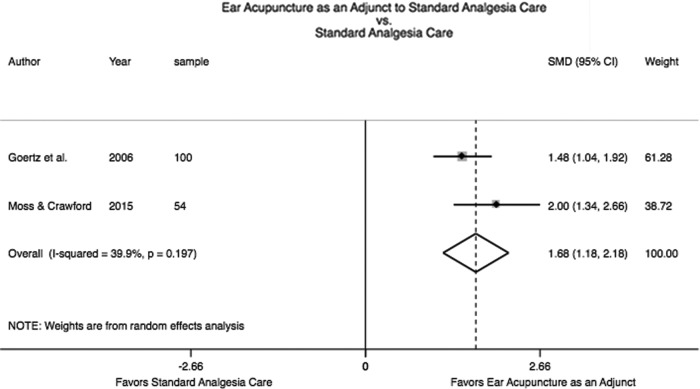
Four RCTs, representing 281 patients, were eligible for meta-analyses. Two RCTs with 127 patients compared the change in PS-10 for ear acupuncture (including 1 acupressure study) versus sham with an SMD of 1.69 (confidence interval [CI]: 0.37–3.01), I2 = 87.0%, and P < 0.01 (Fig. 2); and and a WMD of 2.47 (CI: 1.79–3.16) and P = 0.22 (Supplementary Fig. S1; Supplementary Data are available online at www.liebertpub.com/acu). Two RCTs with 154 patients compared AdjEA to SAC without sham; the SMD PS-10 was 1.68 (CI: 1.18–2.18), I2 = 39.9%; P = 0.20 (Fig. 3); and the WMD was 2.84 (CI: 1.45–4.22), P = 0.01 (Supplementary Fig. S2). When combining all 4 RCTs as ear acupuncture (both sole and adjuvant) versus control, the SMD PS-10 was 1.66 (CI: 1.13–2.19), I2 = 71.3%, and P = 0.02 (Fig. 4); and the WMD was 2.61 (CI: 2.00–3.22), P = 0.05 (Supplementary Fig. S3).
FIG. 2.
Forest plot of ear acupuncture versus sham with calculated standardized mean difference (SMD) for pain score difference on a pain score out of 10 (PS-10). CI, confidence interval.
FIG. 3.
Forest plot of ear acupuncture as an adjunct versus standard analgesia care with calculated standardized mean difference (SMD) for pain score difference on a pain score out of 10 (PS-10). CI, confidence interval.
FIG. 4.
Forest plot of ear acupuncture (both sole and adjuvant) versus control (sham or standard analgesia care) with calculated standardized mean difference (SMD) for pain score difference on a pain score out of 10 (PS-10). SAC, standard analgesia care; CI, confidence interval.
Secondary Outcomes (Tables 3–5)
Table 3.
Methodological Characteristics of Included RCT Ear Acupuncture Studies of Pain Management in the Emergency Setting
| Experimental group | Control group | ||||||
|---|---|---|---|---|---|---|---|
| First author, year & setting | Condition | Study design (acupuncture practitioner qualification) | Intervention | Length of time needles retained | Number & locations of acupuncture points | Intervention | Method/acupuncture points number & locations |
| Allais, 201133 clinic, Italy | Migraines | 2 arms, acupuncture (n = 46) & sham (n = 48) (not specified) | Acupuncture | 24 h | Several (not specified): Ear: Thalamus (bilateral) | Sham | Four: Nonsensitive sciatic point on antihelix inferior crus × 2 bilateral |
| Barker, 200616 prehospital, Austria | Hip fractures | 2 arms, acupressure (n = 18) & sham (n = 20) (paramedics inexperienced in acupuncture) | Acupressure | N/A | 3 ear: Shenmen; Hip point; & Tranquilizer point (bilateral) | Sham | 2 ear: Stomach point bilateral (concha ridge) |
| Goertz, 200631 ED, US | Mixed | 2 arms, AdjEA (n = 50) & standard care (n = 50) (medical acupuncturist) | AdjEA | 4–6 d | 4 ear: Cingulate, Thalamus (bilateral) | SAC | SAC |
| Gu, 1993,29 ED, China | Biliary colic | 2 arms AdjEA (n = 30) & standard care (n = 18) (not specified) | Acupuncture | 20 min | 2 ear: Point Zero, De Qi every 3–5 min (bilateral) | SAC | 0.5 mg atropine & 25 mg promethazine |
| Moss, 2015,32 general practice, US | Sore throat | 2 arms AdjEA (n = 27) & standard care (n = 27) (certified acupuncturist and physicians inexperienced in acupuncture) | AdjEA | 48 h | Up to 10 ear: Cingulate; Thalamus; Omega 2; Point Zero; Shenmen (bilateral) | SAC | Ibuprofen or equivalent PRN |
| Fox, 2016,28a ED, US | Low-back pain | 2 arms, AdjEA (n = 15) & standard care (n = 15) (certified acupuncturist and physicians inexperienced in acupuncture) | AdjEA | Not specified | Up to 10 ear: Cingulate; Thalamus; Omega 2; Point Zero; Shenmen (bilateral) | SAC | SAC |
Abstract only.
RCT, randomized controlled trial; h, hours; N/A, not applicable; AdjEA, ear acupuncture-as-an adjunct to other analgesia; d, days; SAC, standard analgesia care; ED, emergency department; min, minutes; PRN, pro re nata (as needed).
Table 4.
Results of Included RCT Ear Acupuncture Studies of Pain Management in the Emergency Setting
| Experimental group | Control group | ||||||
|---|---|---|---|---|---|---|---|
| First author, year, ref. & condition | Mean age yrs with SD or P-value (% female) | Adverse events from acupuncture | Mean age yrs with SD or P-value (% female) | Adverse events from control intervention | Mean pain score change difference between intervention & control | Bias | Secondary outcomes |
| Allais, 201133 migraines | 35.9; range: 15–60 yrs (100%) | Not specified | 33.2 range: 16–58 yrs (100%) | Not specified | 2.1 | Medium | Nil |
| Barker, 200616 hip fractures | 86.5 ± 4.0 yrs (83%) | Not specified | 86.0 ± 4.8 yrs (90%) | Not specified | 2.8 | Low | Anxiety 38/100 change vs. 3/100; P < 0.001; Lower HR; more satisfied than sham. |
| Goertz, 200631 mixed | 30.4 ± 9.7 yrs (42%) | Not specified | 32.8 ± 7.5 yrs (64%) | Not specified | 2.18 | Medium | No reduction in medication frequency or prescribed usage; cost: $1.52 $USD/patient |
| Gu, 199329 biliary colic | 47 ± 8.8 yrs (53.3%) | Not specified | 42 ± 6.6 yrs (42.7%) | Not specified | Not specified | High | Nil |
| Moss, 201532 sore throat | 34 yrs; P = 0.48 (74%) | Not specified | 31 yrs; P = 0.48 (56%) | Not specified | 3.6 | High | Less medication at 6, 24, 48 h; P < 0.009; no difference in time off work |
| Fox, 201628a low-back pain | Not specified | 2 events: pain at needle site | Not specified | Not specified | Post pain score: 1.7 | High | Ambulation & ROM: improved; leg pain: no significant improvement; LOS: no difference; medication usage: no difference in ED & more opioid prescriptions at discharge with BFA. |
Abstract only.
RCT, randomized controlled trial; yrs, years; SD, standard deviation; HR, heart rate; h, hours; ROM, range of movement; LOS, length of stay; ED, emergency department; BFA, Battlefield Acupuncture.
Table 5.
Methods & Results of Included Observational Ear Acupuncture Studies on Pain Management in the Emergency Setting
| First author, year, ref. & setting | Condition (sample size) | Intervention | Acupuncturist practitioner qualification | Method/acupuncture points | Length of time needles retained | Mean age years with ± SD (% female) | Adverse events from acupuncture | Mean pain score out of 10 pre–post with SD or P-value (change) | Secondary outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Burns, 2013,30 retrieval, Germany/US | Varied pain types (75) | AdjEA SAC | Nonacupuncturists: Nurse–practitioners (2) Physician (1) trained in BFA | Up to 10 Ear: Cingulate, Thalamus, Omega 2, Point Zero & Shenmen (bilateral) | Not specified | 55.4% ages 21–30 (14.9%) | Not specified | 4.07–2.17 (1.89) P < 0.0001 | Satisfaction: 62% would have treatment again; 50% mostly satisfied; 21% very satisfied |
| Graff, 2016,34 ED | Migraine (19) | Acupuncture | Physician | Up to 6 (3 in each ear): Thalamus & migraine line (bilateral) | 2 weeks or till needles fell out | 14 ± 2.9 yrs (89%) | 0 | 7.63 ± 1.2–0.55 ± 0.4 (7.08 ± 1.0) | Nil |
SD, standard deviation; AdjEA, ear acupuncture-as-an-adjunct to other analgesia; SAC, standard analgesia care; BFA, Battlefield Acupuncture; ED, emergency department; yrs, years.
Medication usage
One RCT showed a reduction in NSAID usage for sore throats, with a reduced mean number of doses at 6 hours (0.4 versus 1.1), 24 hours (1.4 versus 2.6), and 48 hours (2.2 versus 4.1), with all P < 0.05.32 Another RCT showed no difference in overall medication usage regarding frequency or obtaining of analgesics via prescription.31 One small pilot study (abstract only) showed no difference in ED opioid use but, upon discharge, fewer analgesia prescriptions were given to the control group.28 The statistical significance of these differences for this latter pilot study was not reported.28
Patient satisfaction
Two studies measured patient satisfaction. In the prehospital acupressure RCT there was a quoted improvement over sham but no quantitative data was provided.16 In the UOBS using acupuncture as-an-adjunct, 62% of respondents said that they “would have the same treatment again,” while 71% reported that they were either mostly satisfied or very satisfied.30
Adverse effects
Adverse events were only specifically measured in 2 of the 8 studies, with 1 documenting minor pain for 2 participants28 and nil in the other.34
Ear acupuncture techniques (points and training)
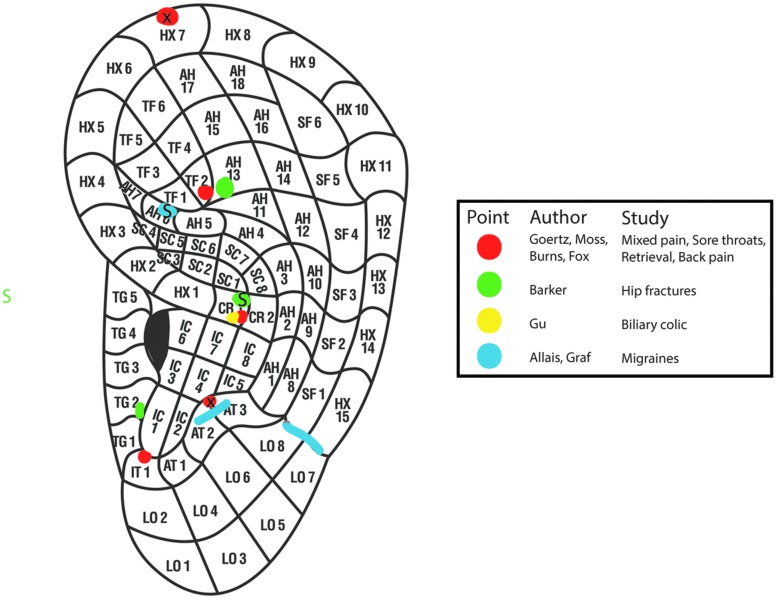
All 8 studies used set points in both ears, however 2 studies located efficacious points within or adjacent to set anatomical points, using localized tenderness (including use of an algometer), skin-resistance measurement, and the “point contact test.”33,34 The numbers of intervention ear acupuncture points ranged from 1 to 10. The points used, along with their anatomical locations, if used in more than one study were as follows: Thalamus/antitragus (6 studies), Cingulate/inter-tragic notch (4 studies), Shenmen/apex of triangular fossa (4 studies), Point Zero/concha ridge (4 studies), and Omega 2/helix adjacent to base of triangular fossa (3 studies; see Fig. 5). Only 1 study used De Qi,29 and none used EA. Four studies specified that the practitioner delivering the acupuncture utilized nonacupuncturists trained in the specific prescription alone.16,28,30,32 Five studies specified the use of semipermanent needles that were retained >24 hours.30–35 (Fig. 5).
FIG. 5.
Points used in the 8 pain studies using Oleson's ear map. S, sham; X, either internal or external; TG, tragus; HX, helix; CR, concha ridge; AH, antihelix; TF, triangular fossa; SF, scaphoid fossa; SC, scaphoid concha; TG, tragus; IT, intertragic notch; LO, lobe. This figure was used with permission.
Time-based outcomes and costs
The time required to apply ear acupuncture was specified for 6 of the 8 studies and ranged from 2 to 10 minutes.16,39,30,32–34 Three studies quoted actual costs of consumables as < $5 USD/per patient.16,31,32 and “low cost” was also mentioned by another study.30
Bias and Heterogeneity
There was significant bias regarding practitioner and patient blinding and, of note, 2 studies did not blind the assessors (Table 6). The heterogeneity measure (I2) for the three SMD Forest plots (Figs. 2–4) ranged from 39.9% to 87.0% (Tables 3–6).
Table 6.
Bias Assessment for Included RCTs Judged According to the Cochrane Assessment Tool
| First author, year & ref. | Adequate randomization | Allocation concealment | Patient blinding | Practitioner blinding | Assessor blinding | Incomplete outcome data | Selective reporting | Other sources | Summary of bias risk |
|---|---|---|---|---|---|---|---|---|---|
| Allais, 201133 | L | L | L | H | L | L | L | L | Medium |
| Barker, 200616 | U | L | L | L | L | L | L | L | Low |
| Goertz, 200631 | L | L | H | H | L | L | L | L | Medium |
| Gu, 199329 | U | U | H | H | U | U | U | U | Medium |
| Moss, 201532 | L | U | H | H | H | L | L | L | High |
| Fox, 201628a | U | U | H | H | H | L | U | L | High |
Abstract only.
RCTs, randomized controlled trials; L, low; H, high; U, unclear.
Discussion
The most important conclusion of this review is that ear acupuncture has some limited evidence of effectiveness for acute pain in the emergency setting as a stand-alone treatment and as an adjunct treatment. This is based on meta-analyses of 4 RCTs involving 281 patients from 2006 to 2015. This analysis determined that ear acupuncture has some evidence suggesting statistical significance,35 clinically meaningful analgesia,25 and improved level of satisfaction.7,36 This current review provides more information on ear acupuncture in the emergency setting, compared to prior reviews.15,17,18,37 These prior reviews provided evidence from meta-analyses that all forms of acupuncture were effective in the ED environment and that ear acupuncture is effective for acute perioperative pain, but did not address the specific role of ear acupuncture in the ED setting.
Effectiveness Across Study Groups
Ear acupuncture versus sham
In the ear acupuncture versus sham group, there was a large statistical effect-size significance favoring ear acupuncture. The clinical significance of a pain score change of 2.47 of 10 should be interpreted with caution, as the P-value for the WMD was 0.22. One study measured patient satisfaction and documented improved satisfaction, compared with sham.16 Patient satisfaction is an important aspect to quantifying analgesia effectiveness and is not necessarily captured by pain-score reduction.7,36
Some researchers argue against the use of sham in acupuncture trials, as, in these researchers' view, simply piercing the skin is likely to have a therapeutic effect and they would prefer to compare acupuncture against SAC.38,39 The analgesic effects of sham ear acupuncture needling nonactive or irrelevant acupoints (types 1 and 2; see sham ear acupuncture definition in Table 1) is perhaps more therapeutic, compared to body sham, as the ear is small and has >93 documented active acupoints,40 and, furthermore, each point has active neighboring zones.41 Thus, attempts to show efficacy of ear acupuncture above sham using supposedly inactive ear acupoints is theoretically more difficult. However, Zhang et al. in their review of sham control methods in ear acupuncture was not able to demonstrate this.40 These researchers found no difference between the needling of nonactive or irrelevant acupoints versus pseudo-interventions (type 4; see sham ear acupuncture definition in Table 1).
While the current authors chose to focus on ear acupuncture in the ED setting, the small number of sham studies and P-value >0.05 for the overall WMD indicate that further evidence from studies of other non-ED scenarios and body acupuncture is helpful. Yeh et al. in 2014 performed review15 of ear acupuncture for immediate pain relief (15 minutes) in non-ED conditions and documented 2 acupuncture versus sham studies involving the changing of burns dressings42 and chronic distal extremity pain.43 Both studies showed significant but small effect-size differences favoring ear acupuncture (SMD = 0.37 and 0.34, respectively).15 The current authors' prior meta-analysis of acupuncture versus sham included both body (6 RCTs) and ear (2 RCTs) acupuncture, and the results also favored acupuncture for a broader range of conditions, with a large effect-size and improved patient satisfaction.18 Both of these latter reviews supported the current finding that ear acupuncture is likely to be more effective than sham acupuncture.
AdjEA compared to SAC
The current meta-analysis of 2 studies revealed a large statistical effect-size (SMD) that was not statistically significant and a clinically meaningful reduction in a numeric rating scale pain score of 2.84/10 favoring AdjEA. There were no patient-satisfaction measures in this group. Again, because of the limited number of ED studies and a P-value >0.05 for the SMD, further evidence is required elsewhere to allow useful interpretation. In the perioperative setting in Yeh et al.'s meta-analysis (4 studies),15 AdjEA showed a large effect-size difference (SMD = 1.71) for pain-score change in a 12–24-hour period. These results are consistent and support the current analysis for this comparator group. Thus, the evidence for ear acupuncture in this group and in the group against sham—albeit with limited numbers of studies—suggest that ear acupuncture might be a suitable adjunct with simple analgesia such as acetaminophen or NSAIDs, or as an alternative when concerns for analgesic drug side-effects are high, contraindicated, or previously ineffective.
Ear acupuncture alone compared to SAC
There was only 1 study in this group, dating from 1993.29 The drug comparator of atropine and promethazine would no longer be considered standard therapy. In the current authors' prior review of body acupuncture, a meta-analysis of this group showed that body acupuncture was noninferior to SAC.18 No further studies on ear acupuncture could be found in the perioperative setting for this comparator group.
Ear acupuncture versus control (all groups combined)
In this group, all eligible RCTs that had adequate data were combined. There was both a large statistical effect-size difference of 1.66 and a clinically meaningful PS-10 of 2.61 (P = 0.05) above the threshold of 1.3, all favoring ear acupuncture.25,35 While this meta-analysis combined various style designs, allowing interpretation of acupuncture effects relative to the control, it still should be interpreted with some caution due to these heterogeneous trial designs. Many acupuncture systematic reviews performed this meta-analysis including 3 major reviews on ear acupuncture and pain management. These reviews by Murakami et al. (2017),17 Yeh et al. (2014)15 and Asher et al. (2010)37 all highlighted large effect-size differences favoring ear acupuncture for acute pain (both perioperative and ED pain) with SMDs of 0.96 (3 studies; 333 patients), 2.84 (4 studies; 193 patients), and 1.35 (2 studies; 111 patients), respectively. These 3 meta-analyses were consistent with the current results.
Quality of Studies and Heterogeneity
Like body acupuncture, ear acupuncture RCTs have unique challenges to overcome blinding, sham needling effects, and lack of mainstream support or funding.44 The quality of studies in this review was variable. One high-quality study overcame the challenge of practitioner blinding successfully by using acupuncture-naive paramedics,16 as opposed to another 2 studies that did not blind their assessors.28,32 Heterogeneity was moderate-to-high in the current meta-analysis.26 The issues of bias and heterogeneity both diminished positive interpretation of acupuncture in these meta-analyses.
Adverse Effects
This current systematic review was not able to extract useful data on adverse effects from the studies selected, due to the inconsistent reporting of such events. Only 2 studies were identified that measured adverse events as a secondary outcome, and no serious adverse events were found in either study
These results are consistent with the literature. A 2014 review by Tan et al. on adverse events with ear acupuncture collected data on adverse events in 18 studies (RCTs and UOBS) involving 1753 patients.45 The researchers recorded no serious adverse events but there were short-term minor events, including pain, nausea, dizziness, local bleeding, and mild inflammation.45 Xu et al., in 2013, in their review of case reports noted the more serious adverse event of perichondritis.46 A previous review from 2004 estimated the incidence of serious adverse events requiring treatment for all forms of acupuncture at 0.05 per 10,000 treatments, with perichondritis comprising ∼5% of these.47 Fainting (a vasovagal event) is a potentially more serious complication of ear acupuncture, as injuries can be sustained from falling. In 1 survey, the incidence of fainting was quoted as 0.1%, but this incidence included both ear and body acupuncture.48 Needle-stick injuries to staff from indwelling ear needles falling out are another reported and preventable complication.49
Medication Usage
One of the adjunct studies showed a reduction in medication use,32 while the other 2 did not.31,34 Therefore, no conclusions could be drawn in this current review on whether or not ear acupuncture reduced medication use in the emergency setting. However, the perioperative meta-analyses provided some indirect evidence that ear acupuncture could reduce medication usage. Murakami et al. performed a meta-analysis on medication usage in 6 RCTs with a total 303 patients.17 There, the SMD was 1.08 favoring AdjEA for medication reduction.17
Technique and Applicability to the ED Setting
There were two predominant styles of ear acupuncture in the current review. One style was developed by Marco Moroli, FISA (2 studies) and the other was developed by Richard C. Niemztow, MD, PhD, MPH (4 studies). The former style relies on more skills, with identification of ear points through a combination of: anatomical location, localized tenderness (including use of an algometer), and trial of improvement (needle-contact test) or electrical skin resistance. The latter style, BFA, uses up to 5 set points that are only anatomically located. There were inadequate studies in this review to evaluate which of these two styles was most effective for pain-score reduction.
The BFA technique is attractive—as it can be applied in a wide spectrum of conditions, using the same point prescription—and is extensively used by nonacupuncturists. BFA has already been taught to more than 2800 nonacupuncturist military providers (personal written communication with coauthor Dr. Niemtzow on September 15, 2016). In the current review, there were 4 BFA studies that utilized noncertified acupuncturists.
Application time for ear acupuncture in the current review was under 10 minutes. It is noteworthy that body acupuncture has not been shown to be more efficacious and might delay usual care for up to 30 minutes because of the need for widespread needle placement.18 Ear acupuncture, however, allows body access for observations, intravenous access, imaging (except magnetic resonance imaging), and procedures.
Future Research
The current review highlighted issues in the methodological quality of the RCTs, encouraging future researchers to address basic requirements such as assessor blinding. Adverse events were only reported sporadically, so the current authors recommend uniform reporting standards be used for minor adverse events. More studies with a comparator group of acupuncture versus SAC would allow the relative risk of adverse events to be calculated. Patient satisfaction is an important determinant of acupuncture efficacy, and more studies require this as a secondary outcome. Other painful conditions besides those to date are needed for BFA assessment to show that it is efficacious across all painful conditions. Further studies are required to assess the various techniques of ear acupuncture, ear versus body acupuncture, and utilization of certified acupuncturists versus nonacupuncturists. The acceptance of acupuncture in the ED setting is likely to be partially dependent on proving medication-usage reduction; thus, further testing using AdjEA versus SAC with medication usage as a secondary outcome is required.
Limitations
While this review and its outcomes were preapproved as part of a PhD proposal, it was not preregistered on a systematic review database. This review was limited by the numbers of patients and studies, substantial study heterogeneity, limited statistical significance within the meta-analyses, and quality issues within the RCTs. Further research is likely to have an effect on the results of this review. While grouping of the studies is advantageous because of trial design (i.e., ear acupuncture versus sham, AdjEA versus SAC, and ear acupuncture versus SAC), this is fraught with assumptions that ear acupuncture is effective across a range of conditions. Grouping all RCTs together into 1 meta-analysis variant study designs compiles together and should be interpreted with caution. Finally, a random-effects model was used, as it was assumed that the studies were not homogeneous and there might have been studies that were missed or unpublished.
Conclusions
Based on this systematic review, there is limited evidence that ear acupuncture (as stand-alone or adjunct therapy) can provide effective analgesia for some acute pain conditions in the ED. Until further research occurs, it is necessary to interpret the effectiveness of ear acupuncture—at least in part—in the light of prior reviews on perioperative studies and body acupuncture. ED clinicians may consider ear acupuncture as an adjunct to SAC or as an alternative when concerns about analgesic drug side-effects are high, contraindicated, or previously ineffective. While ear acupuncture has been shown to reduce medication usage in perioperative pain, this has not yet been established in the ED setting. However, ear acupuncture has additional potential features that make it suitable to the emergency setting. These features are: low risk, low cost, reasonable application time, improved patient satisfaction, and allowing body access for other dimensions of ED care.
Supplementary Material
Acknowledgments
Support for this research was provided by the University of Notre Dame, St. John of God Hospital Murdoch, and the Australian Government Research Training Program Scholarship.
All of the authors conceived the study and designed the search and data collection. A.L.J. and E.S.A. undertook data collection and analysis. All of the authors contributed to review and revision of this article, and all take responsibility for the final version.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Karwowski-Soulié F, Lessenot-Tcherny S, Lamarche-Vadel A, et al. Pain in an emergency department: An audit. Eur J Emerg Med. 2006;13(4):218–224 [DOI] [PubMed] [Google Scholar]
- 2.Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20(3):165–169 [DOI] [PubMed] [Google Scholar]
- 3.National Health and Medical Research Council (NHMRC). NHMRC NICS National Emergency Care Pain Management Initiative Final Report 2011. Melbourne, Australia: NHMRC; 2011:12 [Google Scholar]
- 4.Dale J, Bjørnsen LP. Assessment of pain in a Norwegian emergency department. Scand J Trauma Resusc and Emerg Med. 2015;23:86–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, Tanabe P; PEMI Study Group. Pain in the emergency department: Results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8(6):460–466 [DOI] [PubMed] [Google Scholar]
- 6.Doherty S, Knott J, Bennetts S, Jazayeri M, Huckson S. National project seeking to improve pain management in the emergency department setting: Findings from the NHMRC-NICS National Pain Management Initiative. Emerg Med Australas. 2013;25(2):120–126 [DOI] [PubMed] [Google Scholar]
- 7.Bhakta HC, Marco CA. Pain management: Association with patient satisfaction among emergency department patients. J Emerg Med. 2014;46(4):456–464 [DOI] [PubMed] [Google Scholar]
- 8.National Institute of Clinical Studies. Emergency Care Acute Pain Management Manual. Canberra: National Health and Medical Research Council; 2011 [Google Scholar]
- 9.Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J. Acute Pain Management: Scientific Evidence, 4th ed. Melbourne: ANZCA & FPM; 2015 [DOI] [PubMed] [Google Scholar]
- 10.Cameron P. Is Analgesia in the ED Helping Our Patients?—Or Killing Them? Emergency Physicians International. 2016. Online document at: www.epijournal.com/articles/270/analgesia-in-the-ed Accessed November21, 2016
- 11.Butler MM, Ancona RM, Beauchamp GA, et al. Emergency department prescription opioids as an initial exposure preceding addiction. Ann Emerg Med. 2016;68(2):202–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2015;65(5):493–499 [DOI] [PubMed] [Google Scholar]
- 13.Morgan JP. American opiophobia: Customary underutilization of opioid analgesics. Adv Alcohol Subst Abuse. 1985;5(1–2):163–173 [DOI] [PubMed] [Google Scholar]
- 14.Thomas SH. Management of Pain in the Emergency Department. ISRN Emergency Medicine. 2013;1–20. Article ID 583132. Online document at: http://dx.doi.org/10.1155/2013/583132 Accessed June16, 2017
- 15.Yeh CH, Chiang YC, Hoffman SL, et al. Efficacy of auricular therapy for pain management: A systematic review and meta-analysis. Evid Based Complement Alternat Med. 2014;2014:934670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barker R, Kober A, Hoerauf K, et al. Out-of-hospital auricular acupressure in elder patients with hip fracture: A randomized double-blinded trial. Acad Emerg Med. 2006;13(1):19–23 [DOI] [PubMed] [Google Scholar]
- 17.Murakami M, Fox L, Dijkers MP. Ear acupuncture for immediate pain relief—a systematic review and meta-analysis of randomized controlled trials. Pain Med. 2017;18(3):551–564 [DOI] [PubMed] [Google Scholar]
- 18.Jan AL, Aldridge ES, Rogers IR, Visser EJ, Bulsara MK, Niemtzow RC. Does acupuncture have a role in providing analgesia in the emergency setting? A systematic review and meta-analysis. Emerg Med Australas. 2017. [Epub ahead of print]; DOI: 10.1111/1742-6723.12832 [DOI] [PubMed]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA statement. Int J Surg. 2010;8(5):336–341 [DOI] [PubMed] [Google Scholar]
- 20.MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, Moher D; STRICTA Revision Group. Revised STandards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. J Evid Based Med. 2010;3(3):140–155 [DOI] [PubMed] [Google Scholar]
- 21.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions: The Cochrane Collaboration, version 5.1.0. 2011. Updated March 2011. Online document at: http://handbook-5-1.cochrane.org/ Accessed November11, 2016
- 22.Kober A, Scheck T, Greher M, et al. Prehospital analgesia with acupressure in victims of minor trauma: A prospective, randomized, double-blinded trial. Anesth Analg. 2002;95(3):723–727 [DOI] [PubMed] [Google Scholar]
- 23.Lang T, Hager H, Funovits V, Barker R, Steinlechner B, Hoerauf K, Kober A. Prehospital analgesia with acupressure at the Baihui and Hegu points in patients with radial fractures: A prospective, randomized, double-blind trial. Am J Emerg Med. 2007;25(8):887–893 [DOI] [PubMed] [Google Scholar]
- 24.Faraone SV. Interpreting estimates of treatment effects: Implications for managed care. P T. 2008;33(12):700–711 [PMC free article] [PubMed] [Google Scholar]
- 25.Todd KH, Funk KG, Funk JP, Bonacci R. Clinical significance of reported changes in pain severity. Ann Emerg Med. 1996;27(4):485–489 [DOI] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ried K. Interpreting and understanding meta-analysis graphs: A practical guide. Aust Fam Physician. 2006;35(8):635–638 [PubMed] [Google Scholar]
- 28.Fox L, Danesh H, Murakami M, et al. Randomized trial of acupuncture versus standard therapy to treat low back pain in the emergency department [abstr]. Ann Emerg Med. 2016;68(4[suppl):S81 [Google Scholar]
- 29.Gu X. Clinical study on analgesia for biliary colic with ear acupuncture at point Erzhong. Am J Acupunct. 1993;21(3):237–239 [Google Scholar]
- 30.Burns S, York A, Niemtzow RC, Garner BK, Steele N, Walter JAG. Moving acupuncture to the front line of military medical care: A feasibility study. Med Acupunct. 2013;25(1):48–54 [Google Scholar]
- 31.Goertz CM, Niemtzow R, Burns SM, Fritts MJ, Crawford CC, Jonas WB. Auricular acupuncture in the treatment of acute pain syndromes: A pilot study. Mil Med. 2006;171(10):1010–1014 [DOI] [PubMed] [Google Scholar]
- 32.Moss DA, Crawford P. Ear acupuncture for acute sore throat in patients unable to take non-steroidal anti-inflammatory agents (NSAIDs). J Am Board Fam Med. 2015;28(6):697–705 [DOI] [PubMed] [Google Scholar]
- 33.Allais G, Romoli M, Rolando S, et al. Ear acupuncture in the treatment of migraine attacks: A randomized trial on the efficacy of appropriate versus inappropriate acupoints. Neurol Sci. 2011;32(suppl1):S173–S175 [DOI] [PubMed] [Google Scholar]
- 34.Graff DM, McDonald MJ. Auricular acupuncture for the treatment of pediatric migraines in the emergency department. Pediatr Emerg Care. 2016;May 2;e-pub ahead of print [DOI] [PubMed]
- 35.Cohen J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillsdale: NJ: Lawrence Erlbaum Associates; 1988:48 [Google Scholar]
- 36.Kelly AM. Patient satisfaction with pain management does not correlate with initial or discharge VAS pain score, verbal pain rating at discharge, or change in VAS score in the emergency department. J Emerg Med. 2000;19(2):113–116 [DOI] [PubMed] [Google Scholar]
- 37.Asher GN, Jonas DE, Coeytaux RR, Reilly AC, Loh YL, Motsinger-Reif AA, Winham SJ. Auriculotherapy for pain management: A systematic review and meta-analysis of randomized controlled trials. J Altern Complement Med. 2010;16(10):1097–1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Witt CM, Schützler L. The gap between results from sham-controlled trials and trials using other controls in acupuncture research: The influence of context. Complement Ther Med. 2013;21(2):112–114 [DOI] [PubMed] [Google Scholar]
- 39.Dincer F, Linde K. Sham interventions in randomized clinical trials of acupuncture—a review. Complement Ther Med. 2003;11(4):235–242 [DOI] [PubMed] [Google Scholar]
- 40.Zhang CS, Yang AW, Zhang AL, May BH, Xue CC. Sham control methods used in ear-acupuncture/ear-acupressure randomized controlled trials: A systematic review. J Altern Complement Med. 2014;20(3):147–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Falk CX, Birch S, Avants SK, Tsau Y, Margolin A. Preliminary results of a new method for locating auricular acupuncture points. Acupunct Electrother Res. 2000;25(3–4):165–177 [DOI] [PubMed] [Google Scholar]
- 42.Lewis S, Clelland J, Knowles C, Jackson J, Dimick A. Effects of auricular acupuncture-like transcutaneous electric nerve stimulation on pain levels following wound care in patients with burns: A pilot study. J Burn Care Res. 1990;11(4):322–329 [DOI] [PubMed] [Google Scholar]
- 43.Longobardi AG, Clelland JA, Knowles CJ, Jackson JR. Effects of auricular transcutaneous electrical nerve stimulation on distal extremity pain: A pilot study. Phys Ther. 1989;69(1):10–17 [DOI] [PubMed] [Google Scholar]
- 44.Ernst E. Acupuncture—a critical analysis. J Intern Med. 2006;259(2):125–137 [DOI] [PubMed] [Google Scholar]
- 45.Tan JY, Molassiotis A, Wang T, Suen LK. Adverse events of auricular therapy: A systematic review. Evid Based Complement Alternat Med. 2014;2014:506758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu S, Wang L, Cooper E, et al. Adverse events of acupuncture: A systematic review of case reports. Evid Based Complement Alternat Med. 2013;2013:581203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22(3):122–133 [DOI] [PubMed] [Google Scholar]
- 48.Ernst G, Strzyz H, Hagmeister H. Incidence of adverse effects during acupuncture therapy—a multicentre survey. Complement Ther Med. 2003;11(2):93–97 [DOI] [PubMed] [Google Scholar]
- 49.Filshie J. Safety aspects of acupuncture in palliative care. Acupunct Med. 2001;19(2):117–122 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.