Abstract
Background
Burn-related mortality has decreased significantly over the past several decades. While often attributed in part to regionalization of burn care, this has not been evaluated at the population level.
Methods
We conducted a retrospective, population-based cohort study of all patients with > 20% total burned surface area (TBSA) burn injury in Ontario, Canada. Adult (>16y) patients injured between 2003–2013 were included. Deaths in the emergency department were excluded. Logistic generalized estimating equations were used to estimate risk-adjusted 30-day mortality. Mortality trends were compared at burn and non-burn centers.
Results
772 patients were identified at 84 centers (2 burn, 82 non-burn). Patients were 74% (n=570) male, of median age 46 (IQR 35–60) years and median TBSA 35% (IQR 25–45). Mortality at 30 days was 19% (n=149). The proportion of patients treated at a burn center increased from 57% to 71% between 2003–2013 (p=0.07). Average risk-adjusted 30-day mortality rates decreased over time; there were significantly reduced odds of death in 2010–2013 compared to 2003–2006 (OR 0.39, 95% CI 0.25–0.61). Burn centers exhibited significantly reduced mortality from 2003–2006 to 2010–2013 (OR 0.36, 95% CI 0.34–0.38) compared to non-designated centers (OR 0.41, 95% CI 0.13–1.24).
Conclusions
Mortality rates have decreased over time; significant improvements have occurred at burn centers while mortality rates at non-designated centers vary widely. A high proportion of patients continue to receive care outside of burn centers. These data suggest there are further opportunities to regionalize burn care and in so doing, potentially lower burn-related mortality.
Level of Evidence
Level III epidemiological study
Keywords: burns, epidemiology, mortality, regionalization, trends
Background
Mortality following burn injury has dropped over the last twenty years such that most burn injuries are now survivable(1,2). These improvements have been attributed, in part, to a dedicated, multidisciplinary approach to the care of burn injury, prompting efforts to develop regional systems for the care of burn-injured patients(3,4). While there is evidence in other areas of surgery and medicine that regionalization or concentration of care improves outcomes, there are limited data available relevant to the patient with major burn injury(5–9).
Efforts to characterize trends in regionalization, and its effect on the outcomes of burn injured patients, have been hindered by the lack of a consensus definition for what constitutes a burn center and a lack of data regarding care at non-burn centers(4,10). The only recognized mechanism for assessing and confirming the quality of care provided in a burn center is verification by the American Burn Association (ABA)(11). However, in the US, non-verified (self-designated) burn centers outnumber verified burn centers(10), and half of all patients are treated outside of burn centers altogether(12). Additionally, outside of the US, there are only 4 ABA verified burn centers(13).
A further factor precluding efforts to study regionalization is that data regarding burn care and outcomes are largely derived from the National Burn Repository (NBR), a database maintained by the ABA. Participation in the NBR is voluntary for non-verified burn centers; as a result, the NBR only captures the 36% of burn patients who are treated at a participating center(14). While the NBR is a rich data resource for the study of outcomes among participating centers, it does not allow the study of processes of care or outcomes outside of NBR centers. A comprehensive evaluation of the benefits related to the regionalization of burn care requires data from all centers caring for burn-injured patients – both burn centers and non-burn centers, similar to the approach evaluating the benefits of trauma systems and/or trauma center care(7,15). As a result, there is limited information on the benefits of regionalization in burn care.
In this study, we aimed to evaluate temporal trends in 30-day mortality over a period characterized by increasing regionalization of burn care in Ontario, Canada’s most populous province. Our population-based approach allows the capture of burn-injured patients across all centers, overcoming the limitations of previous studies. We postulated that the concentration of burn care had increased over time and associated with this, was a significant improvement in survival.
Methods
Study Design & Setting
We conducted a population-based retrospective cohort study of patients living in Ontario, Canada who were admitted to hospital for treatment of acute major burn injury between April 1, 2003 and March 31, 2014. Ontario has a population of greater than 13 million in a geographic area of 415,598 miles(16), and is served by two adult regional burn centers, one of which is verified by the ABA. Similar to other Canadian provinces, the Ontario government administers a single-payer system that universally funds all hospital, laboratory, and physician services for eligible residents. This study was approved by the institutional review board at Sunnybrook Health Sciences Centre, Toronto, Canada.
Data Sources
Data were derived from three sources: (1) the Discharge Abstract Database (DAD) – a population-based administrative database which records all acute care hospitalizations in the province of Ontario after the year 1991; (2) the Registered Persons Database (RPDB) – an administrative database of all residents of the province of Ontario who are alive and eligible for coverage under the Ontario Health Insurance Plan (OHIP); and (3) the National Ambulatory Care Reporting System (NACRS) – a population-based administrative database which records all emergency department visits in Ontario. These data were made available through the Institute for Clinical Evaluative Sciences (ICES). ICES is a prescribed entity under the Province of Ontario’s privacy law and holds a large proportion of the administrative health data collected in Ontario. Databases held at ICES contain health and sociodemographic information on residents of Ontario. These datasets were linked using unique encoded identifiers and analyzed at ICES.
Study Population
All individuals aged 16 years or older, living in the province of Ontario, Canada, and admitted to hospital for treatment of acute burn injury involving a total body surface area (TBSA) of 20% or greater between April 1, 2003 and March 31, 2014 were included. Patients lacking a valid health card number and non-residents of Ontario were excluded. In order to focus on a cohort of patients likely to benefit from burn center care, we excluded patients who sustained other concurrent major injuries, including brain injury, major torso trauma, or long bone fractures. To limit the analysis to patients who might benefit from in hospital care, whether at a burn center or not, we excluded patients who died in the ED.
Eligible patients were identified from the DAD by the presence of an ICD-10CA diagnosis code in the range T31.20-T31.99. Patient characteristics were abstracted from the RPDB, and injury characteristics and admitting center were abstracted from the DAD. Age- and gender-stratified population estimates were derived from a database of yearly Ontario intercensal population estimates held at ICES.
Burn center care and regionalization
Our goal was to characterize trends in mortality alongside trends in regionalization, defined as the proportion of patients receiving care in a regional burn center. A regional burn center was defined in accordance with the province’s ‘Burns Center Consultation Guidelines’(17). These guidelines were developed by the Ontario Trauma Advisory committee and Critical Care Services Ontario, the entity responsible for oversight of burn care in the region, and serve to guide the transfer of patients to designated burn centers – of which there are three in Ontario (2 adult, 1 pediatric). Attribution of burn center care was determined by the location of initial burn care. If a transfer from a non-burn center to a burn center occurred beyond 3 days after admission, the care was attributed to the non-burn center, recognizing that patients transferred after 3 days were likely initially admitted with the intent of definitive, rather than preliminary care.
Outcomes
The primary outcome in this study was 30-day mortality, including both in-hospital and post-discharge deaths within 30 days of injury. Discharge disposition in the DAD was used to capture in-hospital deaths, and post-discharge deaths were identified in the RPDB.
Covariates
Baseline patient characteristics including sex, comorbidity burden, urban versus rural residence, and income quintile were considered potential confounders, and therefore included in multivariable analyses. Comorbidity burden was represented based on the Johns Hopkins Adjusted Clinical Groups case mix system(18), which assigns patients to one of six morbidity categories based on prior healthcare utilization. Income quintiles based on each patient’s postal code were used as a marker of socioeconomic status. Patient residence was classified as urban or rural on the basis of the Rurality Index of Ontario (RIO)(19); this takes into account the population density of the city/town of the patient’s residence, as well as the distance to the nearest basic and advanced referral center. A RIO >45 is considered rural(19). We also considered the following injury characteristics to be potential confounders: TBSA, burn mechanism, and inhalation injury, as defined by ICD-10 diagnoses codes in the DAD. We have previously validated the use of ICD-10CA codes for identifying and estimating burn size(20).
Statistical Analysis
A descriptive analysis of patient demographics and injury characteristics across the study period was performed. Annual age- and gender-specific incidence rates were estimated using annual Ontario population estimates, and compared across all years. Incidence rates were directly standardized for age and sex to the 2015 Canadian population(21). The Cochran-Armitage test was performed to test for temporal trends, stratified by age and gender.
Logistic generalized estimating equations were used to derive risk-adjusted odds ratios for 30-day mortality across each year of the study. Least squares means were then used to estimate risk-adjusted mortality rates for each year. A second multivariable model was used to estimate the odds of mortality in the last 4 years of the study (2010–2013) compared to the first 4 years (2003–2006). We considered that in-hospital deaths occurring within 24 hours of admission might not be modifiable by regionalization; thus, we conducted two analyses, one including deaths within 24 hours, and one excluding these deaths. Stratified analyses were used to determine whether there was any effect modification, allowing for the determination of whether the secular trends in burn mortality differed by burn center status. Given the smaller sample size at non-burn centers, only age, comorbidity, TBSA, and inhalation injury were included in the analysis of outcomes at non-burn centers for model parsimony. Model concordance was assessed by determining the area under receiver-operating curves. All statistical analyses were performed using SAS 9.4 (Cary, NC). In all analyses, p < 0.05 was considered significant.
Results
During the study period, 803 patients with acute major burn injury were identified, who received definitive care at 84 different centers (2 burn centers, and 82 non-burn centers). Of these, 31 patients died in the emergency department and were excluded from further analysis; the vast majority of these deaths (>90%) occurred in EDs at hospitals without a burn center. The proportion of patients treated at a regional burn center increased from 57% in 2003 to 71% in 2013 (p=0.07).
The overall age- and gender-standardized incidence of major burn injury across the study period was 1.15 per 100,000 person years. The highest incidence of major burn injury was observed in males aged 45–54 years (1.26/100,000). In contrast, the incidence of major burn injury in females was highest among those aged 75 years and older (1.10/100,000), while males >75 years represented the second highest incidence group (1.19/100,000). The overall rate of major burns increased from 2003 to 2006, then peaked and subsequently declined, before reaching a plateau in 2010. The age- and gender-stratified rates of major burn injury between 2003 and 2013 are presented in Figures 1 and 2. Rates were higher in males (0.85 per 100,000 person-years) than females (0.30 per 100,000 person years), yielding an incidence rate ratio of 2.83 (95% CI 2.47–3.25). No significant trends in rates were observed across age strata.
Figure 1.
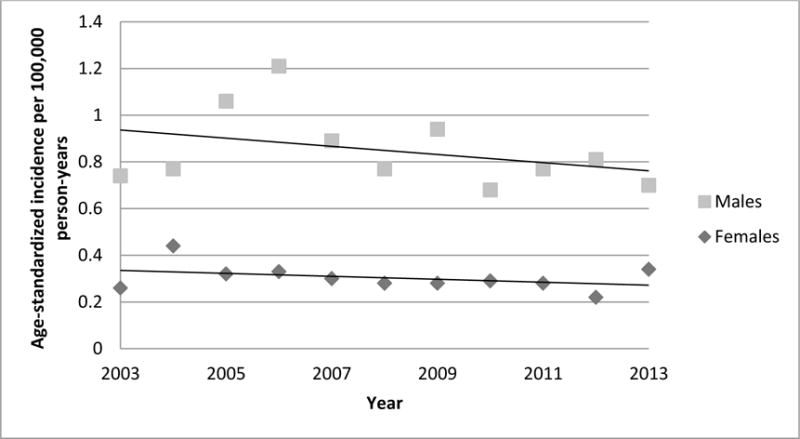
Trends in incidence by gender. Rates were directly age-standardized to the 2015 Canadian general population.
Figure 2.
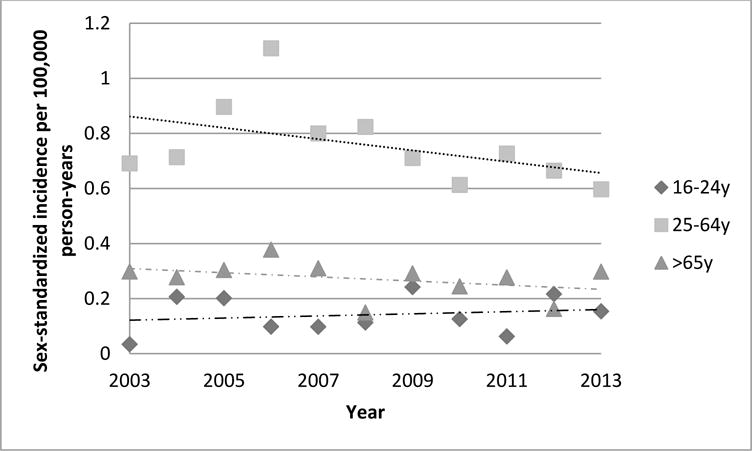
Trends in incidence by age group. Rates were directly sex-standardized to the 2015 Canadian general population.
Patient characteristics
Patients were 74% (n=570) male, with a median age of 46 years (IQR 35–60) (Table 1). The majority of patients were urban-dwelling (80%, n=620). A quarter of patients (n=202, 26%) were in the lowest income quintile and only 8% (n=58) were in the highest quintile.
Table 1.
Baseline patient and injury characteristics
| Overall N=772 |
Burn center N=490 |
Non-burn center N=282 |
P value* | |
|---|---|---|---|---|
|
Patient characteristics
| ||||
| Median age (IQRa) | 46 (35–60) | 48 (35–63) | 46 (34–58) | 0.09 |
| Male (%) | 570 (74) | 373 (76) | 197 (70) | 0.11 |
| Comorbidity (%) | 0.31 | |||
| 1 - None | 55 (7) | 32 (7) | 23 (8) | |
| 2 | 82 (11) | 55 (11) | 27 (10) | |
| 3 | 321(42) | 209 (43) | 112 (40) | |
| 4 | 164 (21) | 108 (22) | 56 (20) | |
| 5 - Highest | 148 (19) | 84 (17) | 64 (23) | |
| Income Quintile (%) | 0.31 | |||
| 1- Lowest | 202 (26) | 120 (24) | 82 (29) | |
| 2 | 174 (23) | 119 (24) | 55 (20) | |
| 3 | 134 (17) | 82 (17) | 52 (18) | |
| 4 | 137 (18) | 84 (17) | 53 (19) | |
| 5- Highest | 58 (8) | 19 (16) | 39 (14) | |
| Rural (%) | 152 (20) | 78 (16) | 74 (26) | 0.001 |
|
Injury characteristics | ||||
| Median TBSAb (IQRa) | 35 (25–45) | 35 (25–45) | 25 (25–45) | 0.05 |
| Inhalation injury (%) | 70 (9) | 56 (11) | 14 (5) | 0.003 |
| Burn Mechanism (%) | 0.10 | |||
| Flame | 510 (66) | 324 (66) | 186 (66) | |
| Contact | 238 (31) | 146 (30) | 92 (33) | |
| Electrical | 24 (3) | 20 (4) | <6 | |
|
Outcomes | ||||
| 24 hour mortality (%)c | 81 (10) | 50 (10) | 31 (11) | 0.73 |
| 30 day mortality (%)d | 149 (19) | 101 (21) | 48 (17) | 0.22 |
Interquartile range
Total body surface area
within 24 hours of admission; excluding deaths in the emergency department
including deaths within 24 hours of admission
comparing burn and non-designated centers
Counts less than 6 suppressed for confidentiality
There were few changes in patient characteristics over 2003–14. Gender, age distribution and rurality were unchanged over time. However, there were significant changes in the distribution of patients across income quintiles over the interval of study; the proportion of patients in the lowest income quintile decreased from 35% to 16%, while the proportion of patients in the middle two quintiles (2–3) increased from 29% to 55%. The proportion of patients in the highest two quintiles (4–5) did not change significantly, representing approximately 25–30% of all patients each year.
A comparison of the patient and injury characteristics between 2003–2006 and 2010–2013, stratified by burn center status, is presented in Table 2. No changes were observed in age, income quintile, or comorbidity. The proportion of female patients treated outside of burn centers increased over time, while the proportion of rural residents treated outside of burn centers decreased over time.
Table 2.
Patient and injury characteristics, by time period
| 2003–2006 | 2010–2013 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Burn Center N=193 |
Non-Burn Center N=121 |
p-value | Burn Center N=171 |
Non-Burn center N=79 |
p-value | |
|
Patient characteristics
| ||||||
| Median age (IQRa) | 45 (34–59) | 45 (35–63) | 0.39 | 47 (34–58) | 52 (34–67) | 0.13 |
|
| ||||||
| Male (%) | 143 (74) | 89 (74) | 0.92 | 135 (79) | 48 (61) | 0.006 |
|
| ||||||
| Comorbidity (%) | 0.19 | 0.83 | ||||
| 1 None | 16 (8) | 12 (10) | 13 (8) | <6 | ||
| 2 | 20 (10) | 12 (10) | 19 (11) | 6 (8) | ||
| 3 | 78 (40) | 37 (31) | 74 (44) | 39 (49) | ||
| 4 | 48 (25) | 26 (21) | 36 (21) | 15 (19) | ||
| 5 Highest | 31 (26) | 34 (28) | 25 (15) | 14 (18) | ||
|
| ||||||
| Income Quintile (%) | 0.13 | 0.74 | ||||
| 1 Lowest | 48 (25) | 40 (33) | 43 (25) | 22 (28) | ||
| 2 | 39 (20) | 19 (16) | 43 (25) | 16 (20) | ||
| 3 | 26 (13) | 20 (17) | 29 (17) | 28 (23) | ||
| 4 | 41 (21) | 29 (24) | 24 (14) | 9 (11) | ||
| 5 Highest | 38 (20) | 13 (11) | 28 (17) | 14 (18) | ||
|
| ||||||
| Rural (%) | 25 (13) | 33 (27) | 0.002 | 34 (20) | 15 (19) | 0.61 |
|
Injury Characteristics | ||||||
| Median TBSAb (IQR) | 35 (25–45) | 25 (25–45) | 0.09 | 35 (25–45) | 25 (25–35) | 0.05 |
|
| ||||||
| Inhalation injury (%) | 21 (11) | 6 (5) | 0.07 | 23 (13) | <6 | 0.05 |
|
| ||||||
| Mechanism (%) | 0.05 | 0.39 | ||||
| Flame | 130 (67) | 71 (59) | 107 (63) | 55 (70) | ||
| Electrical | 10 (5) | <6 | 8 (5) | <6 | ||
| Contact | 53 (27) | 48 (40) | 56 (33) | 23 (29) | ||
|
Outcomes | ||||||
| 24 hour mortality (%)c | 21 (11) | 11 (9) | 0.61 | 19 (11) | <6 | 0.12 |
|
| ||||||
| 30 day mortality (%)d | 47 (24) | 18 (15) | 0.04 | 31 (18) | 7 (9) | 0.06 |
Interquartile range
Total body surface area
within 24 hours of admission; excluding deaths in the emergency department
including deaths within 24 hours of admission
Counts <6 suppressed for confidentiality
Injury Characteristics
Baseline injury characteristics are presented in Table 1. The median %TBSA was 35 (IQR 25–45), and the incidence of inhalation injury was 9% (n=70). Most injuries were secondary to flame (66%, n=510), or contact (31%, n=238) burns while a small proportion (3%, n=24) were electrical in nature. Cause of burn remained relatively stable over time. No significant temporal trends were observed in either burn extent or incidence of inhalation injury.
In both 2003–2006 and 2010–2013, burn centers admitted significantly more patients with inhalation and electrical injuries compared to non-burn centers (Table 2). The proportion of patients with flame injuries treated outside of burn centers increased over time.
Resource utilization and discharge disposition
Median (IQR) hospital length of stay was 12 (18) days. The majority of patients were discharged home (58%, n=350); of these, most (33%, n=205) were discharged home with support, such as in-home nursing visits for wound care, while 145 (n=24%) patients were discharged home without support. One-third (31%, n=189) of patients were discharged to a rehabilitation or long-term care facility. The proportion of patients discharged home decreased significantly between 2003 and 2014 (68% to 46%, p <0.001); concomitantly, there was a significant increase in the proportion of patients discharged to inpatient rehabilitation facilities or long-term care (9% to 36%, p<0.001).
Mortality
The overall 30-day mortality rate was 19% (n=149); excluding deaths within 24 hours of admission, the 30-day mortality rate was 10% (n=68).
After adjustment for patient and injury characteristics, the odds of death in 2010–2013 were significantly lower than 2003–2006, both including (OR 0.39, 95% CI 0.25–0.61) and excluding (OR 0.34, 95% CI 0.20–0.58) 24-hour deaths. The area under the receiver operating curve (ROC) for these models was 0.87 (95% CI 0.81–0.92) and 0.92 (0.89–0.95), respectively. On stratified analysis including only burn centers, there was a significant reduction in mortality at burn centers between 2003–2006 and 2010–2013, both when including 24-hour deaths (OR 0.36, 95% CI 0.34–0.38) and when excluding them (RR 0.34, 95% CI 0.29–0.40) (Table 3). The ROC for these models was 0.90 (95% CI 0.85–0.96) and 0.94 (95% CI 0.91–0.97), respectively. In contrast, at non-burn centers, mortality did not change significantly when comparing 2010–2013 to 2003–2006, either including (OR 0.41, 95% CI 0.13–1.24) or excluding (OR 0.99, 95% CI 0.20–4.91) deaths within 24 hours (Table 3). The ROC for these models was 0.75 (95% CI 0.53–0.97) and 0.88 (95% CI 0.79–0.97), respectively.
Table 3.
Trends in 30-day Mortality
| OR (95% CI) 2010–2013 vs 2003–2006a |
p-value | OR (95% CI) 2010–2013 vs 2003–2006b |
p-value | |
|---|---|---|---|---|
| All centers | 0.39 (0.25–0.61) | <0.001 | 0.34 (0.20–0.58) | <0.001 |
| Burn centers | 0.36 (0.34–0.38) | <0.001 | 0.34 (0.29–0.40) | <0.001 |
| Non-burn centers | 0.41 (0.13–1.24) | 0.09 | 0.99 (0.20–4.91) | 0.35 |
Hierarchical Logistic regression models accounting for age, sex, comorbidity, %TBSA, inhalation injury burn mechanism, and correlated outcomes within centers. Non-burn center models adjusted for age, comorbidity, %TBSA, and inhalation injury. OR, odds ratio; CI, confidence interval
Including deaths within 24 hours of admission
Excluding deaths within 24 hours of admission
Trends in risk-standardized mortality rates are presented in Figure 3. Greater variation in year on year mortality was observed at non-designated centers as compared to burn centers.
Figure 3.
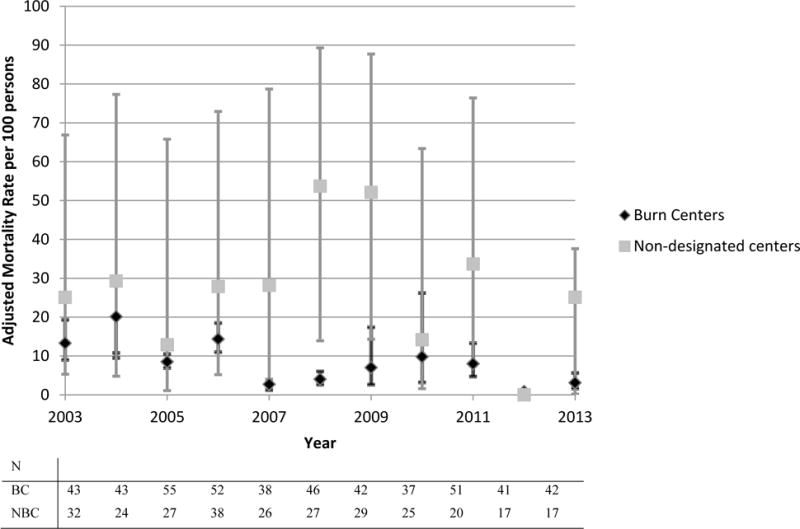
Trends in adjusted 30-day mortality by burn center status. Yearly mean adjusted rates derived from multivariable hierarchical logistic regression model adjusted for patient and injury characteristics. Error bars represent 95% confidence intervals. Annual admission volumes are reported in the table. BC, burn center; NBC, non-burn center; N, total yearly admissions.
Discussion
This population-based analysis characterizes the burden of major burn injury in the province of Ontario, providing critical epidemiologic data for future resource planning and injury prevention efforts. We characterized the concentration of care in our geographical region, and examined trends in regionalization over time. Overall, the proportion of patients treated at a burn center increased from 57% to 71%; thus, almost 30% of patients with major burn injury continue to receive care outside of regional burn centers. Our data suggest that 30-day mortality rates have improved significantly over the last ten years. While these improvements were observed at burn and non-burn centers, consistent improvements were observed at burn centers, particularly over the last three years. At non-burn centers, mortality varied greatly from year to year. The overall incidence and severity of burn injury, in terms of both burn extent and the incidence of inhalation injury, has remained stable over time.
We have identified a significant opportunity to further centralize the care of majorly burn-injured patients, and in so doing, to potentially improve their outcomes. While burn care did become increasingly concentrated over time, 30% of patients continue to receive care outside of a burn center. Few data sources exist to facilitate the study of trends in regionalization of burn care, limiting our ability to compare local trends in regionalization to other areas. Some data exist to suggest regionalization has occurred throughout the United States. Kastenmeier et al found that admissions to five regional burn centers in the United States increased by 31% over 1998 to 2006(22); given reports of stable, or decreasing incidence of burn injury overall, this increase in admissions likely reflects improved regionalization of care. Similarly, in New York, the proportion of patients receiving burn center care increased from 33% to 77% between 1985 and 2006(3). While difficult to quantify, many authors attribute recent improvements in mortality and health care utilization to the concentration of care in burn centers(23,24). Our study endorses this finding, as mortality rates decreased alongside increasing concentration of care in burn centers.
The factors that may contribute to reductions in mortality remain to be definitively characterized. The observed differences in mortality trends on the analyses stratified by burn center status suggest that the effect of time on mortality is modified by treatment in a burn center. Burn centers employ a resource-intensive, multidisciplinary approach to burn care that is patient-oriented and rooted in processes of care aimed at improving the quality and outcomes of burn care. Prior efforts to demonstrate an association between burn center care and improved outcomes have largely focused on burn center volumes, rather than burn versus non-burn center care. This work has not conclusively demonstrated better survival in high-volume burn centers(25,26). Our study compared trends in mortality at two regional burn centers to eighty-two non-burn centers, irrespective of patient volumes. The definition of a burn center in our region is largely based on available resources; one of the two burn centers is an ABA-verified center. Thus, direct comparisons with our study are limited, as this is the first study to compare burn and non-burn center outcomes using a population-based approach. The failure of previous studies to link burn center volumes and mortality might be explained in several ways. Mortality might be an insensitive marker of burn center care, due to confounding by varying illness severity, immortality time bias, or other unmeasured factors. It may be that centers have not met the volume threshold at which a mortality benefit exists, or that all centers studied have actually exceeded this critical volume. Another possibility is that the benefit of regionalized burn care is best represented by outcomes other than mortality, such as inpatient and post-acute care health resource utilization, health-related quality-of-life, and functional recovery. These outcomes have not traditionally been studied in the burn literature(27–29), though one study has demonstrated that burn center care is associated with reduced length of stay and inpatient costs(30). The next improvements in the structures of burn care will follow characterization of these outcomes, an understanding of the patients most likely to benefit from specialized care, a consistent definition of what constitutes specialized care, and further characterization of the infrastructure required to support a centralized burn care system. Furthermore, an understanding of triage practices is also necessary; that 30% of patients with major burn injury do not reach a burn center might reflect a conscious decision on the part of community surgeons who feel burn care is within their scope of practice, versus an infrastructure problem, where differences exist in access to care. A characterization of these barriers will inform future efforts to achieve fully concentrated care, with resultant improvements in outcomes following major burn injury.
Efforts to further regionalize care and improve outcomes for burn-injured patients are justified, given that the overall incidence of major burn injury in our geographical region has remained stable over the last eleven years. This finding is similar to that reported in a non-population-based Canadian study which reported stable incidence between 1995 and 2004(31). In contrast, Australian and European studies have reported a decreased incidence of overall burn admissions(32,33). These observed differences might reflect differences in inclusion criteria and study periods, as well as increased awareness of patients that can be successfully managed as outpatients, regional case mix variations, and local cultures of care and resource availability.
To date, few studies have published population-based rates of burn injury. We have estimated an overall incidence of 1.15 admissions per 100,000 person-years; this is not directly comparable to other published rates, as we have included only patients with >20% TBSA injury, and no other population-based rates exist for this specific cohort. While the overall incidence of major burn injury is relatively low compared to other causes of injury(34), these patients have significant health resource needs, with inpatient length of stay regularly approaching two weeks, and the majority requiring inpatient rehabilitation following discharge; only one-quarter of patients are discharged home without support. The incidence of major burn injury is particularly high among the elderly; among females, incidence is highest among those aged >75, and among males those aged >75 represent the second highest incidence. Resource planning efforts must acknowledge that as the population grows, particularly alongside aging of the baby boomer generation(35), the volume of patients requiring burn care may increase.
We recognize several limitations of this study. The use of administrative data precludes our ability to perform comprehensive risk adjustment. Furthermore, significant variation in burn size estimation exists among physicians(36), which may result in incorrect documentation of burn size. Overestimation of burn size may introduce misclassification bias, such that patients with <20% TBSA may be included. Ultimately, this may lead to an overestimation of the number of centers providing care to major (>20% TBSA) burns, and an underestimation of regionalization and mortality. Another limitation concerns our definition of burn centers. We considered a patient to have received burn center care if they were transferred within 3 days of their injury; this may have underestimated the number of patients who received definitive care in a burn center. However, this likely has resulted in an underestimation of the true association between burn center care and mortality. If we assume a benefit to burn center care, then attributing the outcomes of patients transferred beyond 3 days to the non-burn center likely biases our comparison towards the null. The optimal interval within which burn patients should receive definitive care has not been defined. Errors in the estimation of burn size and depth by inexperienced practitioners can result in under- or over-resuscitation, with well described negative sequelae, including compartment syndrome, acute kidney injury, and shock(37,38). Thus, patients transferred more than 3 days after their injury might not have modifiable outcomes to the same extent as those transferred in a timely manner. Our conclusions are also limited by the sample size of patients treated in non-burn centers; as a result, we are likely underpowered to detect significant trends in mortality at non-burn centers. Significant variations in mortality were observed at non-burn centers compared to burn centers, and future work should characterize whether this variation truly reflects varying processes of care. Our analysis of the health resource needs of burn survivors has not extended beyond the inpatient phase; it is likely that these patients continue to require regular contact with the healthcare system that we have not captured.
In conclusion, we have characterized the burden of major burn injury at the population level in a geographical region of more than 13 million, and have demonstrated that burn injury is a consistent source of morbidity and mortality year after year. Significant improvements in mortality have occurred following major burn injury. These improvements were most significant at burn centers, while mortality rates vary widely outside of burn centers. A considerable opportunity to further regionalize care exists. Future work should focus on identifying barriers to regionalization of burn care and delineating the outcomes most valid to patients.
Acknowledgments
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Dr Nathens is supported by the DeSouza Chair in Trauma Research. Dr Jeschke is supported by: Canadian Institutes of Health Research #123336 and CFI Leader’s Opportunity Fund Project # 25407, NIH RO1 GM087285-01. Dr Fowler’s work was supported by a personnel award from the Heart and Stroke Foundation, Ontario Provincial Office. Dr Karanicolas is supported by a CIHR New Investigator Award.
Footnotes
Disclaimer: This study was supported the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI
This work was presented as a poster presentation at the Annual Meeting of the American Burn Association, May 4, 2016, Las Vegas, NV.
Conflicts of interest: None reported
Author Contributions
Conception and design: SM, ABN, PK, RF, MGJ
Acquisition, analysis, and interpretation of the data: SM, ABN, AG, RM, JPB
Drafting manuscript: SM, ABN, RF, RM, PK, JPB
Revisions of manuscript: SM, ABN, RF, AG, PK, RM, MGJ, JPB
References
- 1.Brusselaers N, Hoste EAJ, Monstrey S, Colpaert KE, De Waele JJ, Vandewoude KH, Blot SI. Outcome and changes over time in survival following severe burns from 1985 to 2004. Intensive Care Med [Internet] 2005 Dec;31(12):1648–53. doi: 10.1007/s00134-005-2819-6. [cited 2015 Oct 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/16220315. [DOI] [PubMed] [Google Scholar]
- 2.McGwin G, Cross JM, Ford JW, Rue LW. Long-term trends in mortality according to age among adult burn patients. J Burn Care Rehabil [Internet] 2003 Jan;24(1):21–5. doi: 10.1097/00004630-200301000-00006. [cited 2015 Oct 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/12543987. [DOI] [PubMed] [Google Scholar]
- 3.Yurt RW, Bessey PQ. The development of a regional system for care of the burn-injured patients. Surg Infect (Larchmt) [Internet] 2009 Oct;10(5):441–5. doi: 10.1089/sur.2009.050. [cited 2016 Jan 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19943776. [DOI] [PubMed] [Google Scholar]
- 4.Brigham PA, Dimick AR. The evolution of burn care facilities in the United States. J Burn Care Res [Internet] 2008 Jan;29(1):248–56. doi: 10.1097/BCR.0b013e31815f366c. [cited 2016 Jan 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/18182929. [DOI] [PubMed] [Google Scholar]
- 5.Cram P, Vaughan-Sarrazin M, Wolf B, Katz J, Rosenthal GA. Comparison of Total Hip and Knee Replacement in Specialty and General Hospitals. J Bone Jt Surg [Internet] 2007;89(A 8):1675–1684. doi: 10.2106/JBJS.F.00873. [cited 2016 Feb 18] Available from: http://ovidsp.tx.ovid.com.myaccess.library.utoronto.ca/sp-3.18.0b/ovidweb.cgi?Link+Set+Ref=01253092-200909000-00003%7C00004623_2007_89_1675_cram_replacement_%257c01253092-200909000-00003%2523xpointer%2528id%2528R19-3%2529%2529%257c10%257c%257covftdb%257c00004623-200708000-0000. [DOI] [PubMed] [Google Scholar]
- 6.Holme I, Fellström BC, Jardine AG, Hartmann A, Holdaas H. Model comparisons of competing risk and recurrent events for graft failure in renal transplant recipients. Clin J Am Soc Nephrol [Internet] 2013 Feb;8(2):241–7. doi: 10.2215/CJN.03760412. [cited 2015 Nov 18] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3562856&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med [Internet] 2006 Jan;354(4):366–78. doi: 10.1056/NEJMsa052049. [cited 2016 Feb 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/16436768. [DOI] [PubMed] [Google Scholar]
- 8.Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. N Engl J Med [Internet] 2002 Apr;346(15):1128–37. doi: 10.1056/NEJMsa012337. [cited 2016 Feb 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/11948273. [DOI] [PubMed] [Google Scholar]
- 9.Edwards EB, Roberts JP, McBride MA, Schulak JA, Hunsicker LG. The effect of the volume of procedures at transplantation centers on mortality after liver transplantation. N Engl J Med [Internet] 1999 Dec;341(27):2049–53. doi: 10.1056/NEJM199912303412703. [cited 2016 Feb 18] Available from: http://www.ncbi.nlm.nih.gov/pubmed/10615076. [DOI] [PubMed] [Google Scholar]
- 10.Klein MB, Kramer CB, Nelson J, Rivara FP, Gibran NS, Concannon T. Geographic access to burn center hospitals. JAMA [Internet] 2009 Oct;302(16):1774–81. doi: 10.1001/jama.2009.1548. [cited 2016 Jan 13] Available from: http://jama.jamanetwork.com/article.aspx?articleid=184780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Burn Association. Burn Center Verification Review Program [Internet] [cited 2016 Jan 14]. Available from: http://ameriburn.org/Verification/CriterionDeficiencies.pdf.
- 12.Zonies D, Mack C, Kramer B, Rivara F, Klein M. Verified centers, nonverified centers, or other facilities: a national analysis of burn patient treatment location. J Am Coll Surg [Internet] 2010 Mar;210(3):299–305. doi: 10.1016/j.jamcollsurg.2009.11.008. [cited 2016 Jan 13] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2831802&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Burn Association Verified Centers [Internet] [cited 2016 Jan 14]. Available from: http://ameriburn.org/verification_verifiedcenters.php.
- 14.Veeravagu A, Yoon BC, Jiang B, Carvalho CM, Rincon F, Maltenfort M, Jallo J, Ratliff JK. National trends in burn and inhalation injury in burn patients: results of analysis of the nationwide inpatient sample database. J Burn Care Res [Internet] 2015 Jan;36(2):258–65. doi: 10.1097/BCR.0000000000000064. [cited 2015 Oct 23] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24918946. [DOI] [PubMed] [Google Scholar]
- 15.Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, Rivara FP. Relationship between trauma center volume and outcomes. JAMA [Internet] 2001 Mar;285(9):1164–71. doi: 10.1001/jama.285.9.1164. [cited 2016 Feb 18] Available from: http://www.ncbi.nlm.nih.gov/pubmed/11231745. [DOI] [PubMed] [Google Scholar]
- 16.Ontario Fact Sheet July 2016 [Internet] Available from: http://www.fin.gov.on.ca/en/economy/ecupdates/factsheet.html.
- 17.Burns Centre Consultation Guidelines [Internet] [cited 2016 Feb 18]. Available from: http://www.oninjuryresources.ca/downloads/news/CCSO_BurnsCentreGuidelines_11×14-EN.PDF.
- 18.Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care [Internet] 1991 May;29(5):452–72. doi: 10.1097/00005650-199105000-00006. [cited 2015 Nov 23] Available from: http://www.ncbi.nlm.nih.gov/pubmed/1902278. [DOI] [PubMed] [Google Scholar]
- 19.Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Ont Med Rev. 2000;67(9):33–52. [Google Scholar]
- 20.Mason SA, Nathens AB, Byrne JP, Fowler R, Gonzalez A, Karanicolas PJ, Moineddin R, Jeschke M. The accuracy of burn diagnosis codes in health administrative data: A validation study. Burns. 2017 Jan; doi: 10.1016/j.burns.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Population by sex and age group [Internet] 2015 [cited 2016 Feb 18]. Available from: http://statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo10a-eng.htm.
- 22.Kastenmeier A, Faraklas I, Cochran A, Pham TN, Young SR, Gibran NS, Gamelli R, Halerz M, Light TD, Kealey GP, et al. The evolution of resource utilization in regional burn centers. J Burn Care Res [Internet] 2010 Jan;31(1):130–6. doi: 10.1097/BCR.0b013e3181cb8ca2. [cited 2015 Oct 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20061848. [DOI] [PubMed] [Google Scholar]
- 23.Sheridan RL. Burn care: results of technical and organizational progress. JAMA [Internet] 2003 Aug;290(6):719–22. doi: 10.1001/jama.290.6.719. [cited 2016 Feb 16] Available from: http://jama.jamanetwork.com/article.aspx?articleid=197051. [DOI] [PubMed] [Google Scholar]
- 24.Gibran NS, Klein MB, Engrav LH, Heimbach DM. UW Burn Center: A model for regional delivery of burn care. Burns [Internet] 2005;31(1):S36–S39. doi: 10.1016/j.burns.2004.10.003. [cited 2016 Feb 17] Available from: http://resolver.scholarsportal.info/resolve/03054179/v31i0001_s/s36_ubc.xml. [DOI] [PubMed] [Google Scholar]
- 25.Light TD, Latenser BA, Kealey GP, Wibbenmeyer LA, Rosenthal GE, Sarrazin MV. The effect of burn center and burn center volume on the mortality of burned adults–an analysis of the data in the National Burn Repository. J Burn Care Res [Internet] 2009 Jan;30(5):776–82. doi: 10.1097/BCR.0b013e3181b47ed2. [cited 2015 Sep 14] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19692917. [DOI] [PubMed] [Google Scholar]
- 26.Hranjec T, Turrentine FE, Stukenborg G, Young JS, Sawyer RG, Calland JF. Burn-center quality improvement: are burn outcomes dependent on admitting facilities and is there a volume-outcome “sweet-spot”? Am Surg [Internet] 2012 May;78(5):559–66. [cited 2015 Oct 26] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3374848&tool=pmcentrez&rendertype=abstract. [PMC free article] [PubMed] [Google Scholar]
- 27.Pereira C, Murphy K, Herndon D. Outcome measures in burn care. Is mortality dead? Burns. 2004;30:761–771. doi: 10.1016/j.burns.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Palmieri TL, Przkora R, Meyer WJ, Carrougher GJ. Measuring burn injury outcomes. Surg Clin North Am [Internet] 2014 Aug;94(4):909–16. doi: 10.1016/j.suc.2014.05.010. [cited 2015 Oct 15] Available from: http://www.ncbi.nlm.nih.gov/pubmed/25085096. [DOI] [PubMed] [Google Scholar]
- 29.van Baar ME, Essink-Bot ML, Oen IMMH, Dokter J, Boxma H, van Beeck EF. Functional outcome after burns: A review. Burns [Internet] 2006;32(1):1–9. doi: 10.1016/j.burns.2005.08.007. Available from: http://www.sciencedirect.com/science/article/pii/S030541790500238X. [DOI] [PubMed] [Google Scholar]
- 30.Sheridan R, Weber J, Prelack K, Petras L, Lydon M, Tompkins R. Early burn center transfer shortens the length of hospitalization and reduces complications in children with serious burn injuries. J Burn Care Rehabil [Internet] 1999 Jan;20(5):347–50. doi: 10.1097/00004630-199909000-00002. [cited 2016 Jan 13] Available from: http://www.ncbi.nlm.nih.gov/pubmed/10501318. [DOI] [PubMed] [Google Scholar]
- 31.Burton KR, Sharma VK, Harrop R, Lindsay R. A population-based study of the epidemiology of acute adult burn injuries in the Calgary Health Region and factors associated with mortality and hospital length of stay from 1995 to 2004. Burns [Internet] 2009;35(4):572–579. Available from: http://www.sciencedirect.com/science/article/pii/S0305417908003355. [Google Scholar]
- 32.Duke J, Wood F, Semmens J, Spilsbury K, Edgar DW, Hendrie D, Rea S. A 26-year population-based study of burn injury hospital admissions in Western Australia. J Burn Care Res [Internet] 2011 Jan;32(3):379–86. doi: 10.1097/BCR.0b013e318219d16c. [cited 2015 Jul 11] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21448072. [DOI] [PubMed] [Google Scholar]
- 33.Brusselaers N, Monstrey SF, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14 doi: 10.1186/cc9300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Macpherson A, Schull M, Manuel D, Cernat G, Redelmeier D, Laupacis A. Injuries in Ontario: ICES Atlas. Toronto: 2005. [Google Scholar]
- 35.Government of Canada SDCSM and R. Canadians in Context - Aging Population/Indicators of Well-being in Canada. 2006 Sep; [cited 2016 Jan 14. ] Available from: http://well-being.esdc.gc.ca/misme-iowb/.3ndic.1t.4r@-eng.jsp?iid=33.
- 36.Parvizi D, Kamolz LP, Giretzlehner M, Haller HL, Trop M, Selig H, Nagele P, Lumenta DB, Burns The potential impact of wrong TBSA estimations on fluid resuscitation in patients suffering from burns: things to keep in mind. Burns. 2014;40:241–245. doi: 10.1016/j.burns.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 37.Dulhunty JM, Boots RJ, Rudd MJ, Muller MJ, Lipman J. Increased fluid resuscitation can lead to adverse outcomes in major-burn injured patients, but low mortality is achievable. Burns [Internet] 2008 Dec;34(8):1090–7. doi: 10.1016/j.burns.2008.01.011. [cited 2015 Jul 3] Available from: http://www.sciencedirect.com/science/article/pii/S0305417908000363. [DOI] [PubMed] [Google Scholar]
- 38.Klein MB, Hayden D, Elson C, Nathens AB, Gamelli RL, Gibran NS, Herndon DN, Arnoldo B, Silver G, Schoenfeld D, et al. The association between fluid administration and outcome following major burn: a multicenter study. Ann Surg [Internet] 2007;245(4):622–628. doi: 10.1097/01.sla.0000252572.50684.49. Available from: http://bf4dv7zn3u.search.serialssolutions.com.myaccess.library.utoronto.ca/?url_ver=Z39.88-2004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&rfr_id=info:sid/Ovid:medc&rft.genre=article&rft_id=info:doi/&rft_id=info:pmid/17414612&rft.issn=0003-4932&rft.volume=2. [DOI] [PMC free article] [PubMed] [Google Scholar]


