Abstract
OBJECTIVE:
Blunt head trauma is a common injury in children, although it rarely requires surgical intervention. Cranial computed tomography (CT) is the reference standard for the diagnosis of traumatic brain injury but has been associated with increased lifetime malignancy risk. We implemented a multifaceted quality improvement initiative to decrease the use of cranial CT for children with minor head injuries.
METHODS:
We designed and implemented a quality improvement effort that included an evidence-based guideline as well as individual feedback for children aged 0 to 21 years who present to the emergency department (ED) for evaluation of minor blunt head trauma. Our primary outcome was cranial CT rate, and our balancing measure was any return to the ED within 72 hours that required hospitalization. We used statistical process control methodology to measure cranial CT rates over time.
RESULTS:
We included 6851 ED visits of which 4242 (62%) occurred in the post–guideline implementation period. From a baseline CT rate of 21%, we observed an absolute reduction of 6% in cranial CT rate (95% confidence interval 3% to 9%) after initial guideline implementation and an additional absolute reduction of 6% (95% confidence interval 4% to 8%) after initiation of individual provider feedback. No children discharged from the ED required admission within 72 hours of initial evaluation.
CONCLUSIONS:
An ED quality improvement effort that included an evidence-based guideline as well as individual provider feedback was associated with a reduction in cranial CT rates without an increase in missed significant head injuries.
Head injuries are a common reason that children present to the emergency department (ED) for evaluation. Although most injuries are minor, many children undergo cranial computed tomography (CT) as part of their diagnostic evaluation. 1 Ionizing radiation exposure from a CT scan has been associated with increased lethal malignancy risk, with the greatest risk to the youngest children. 2 – 4
Recognition of this risk has driven efforts to limit unnecessary imaging studies. The Pediatric Emergency Care Applied Research Network (PECARN) traumatic brain injury (TBI) clinical prediction rules accurately identify children at low risk of a clinically important TBI. 5 – 7 As part of the Choosing Wisely campaign, an initiative of the American Board of Internal Medicine, the American Academy of Pediatrics (AAP) suggests that the PECARN TBI rules in combination with clinical observation should be used to determine whether imaging is indicated. 8
At the study institution, ED-wide quality improvement (QI) efforts to bring evidence-based care to the bedside for both common and high-stakes pediatric conditions were ongoing. Our preliminary review demonstrated a baseline cranial CT rate of >20% for ED patients with minor blunt head trauma. Although the CT rate was lower than reported at other institutions, 9 we noted that few children had a head injury that required an acute intervention. We suspected that this CT rate could safely be decreased. Therefore, we designed and implemented a multifaceted QI effort aimed at reducing cranial CT rates for children with minor blunt head trauma consistent with the PECARN TBI age-based rules as well as the AAP Choosing Wisely campaign. Our efforts included the development and implementation of an evidence-based guideline followed by individual provider feedback. Our aim was to safely reduce cranial CT use by 10% in children with mild blunt head trauma.
Methods
Setting
Boston Children’s Hospital is an urban tertiary care academic center with pediatric trauma level I designation. The ED has an annual volume of ∼60 000 visits per year.
Study Design
We performed a multifaceted QI initiative to improve the care for children with minor blunt head trauma. We determined the impact of these initiatives on the management of children with minor blunt head trauma between January 1, 2010, and June 30, 2014. The institutional review board approved the study protocol with a waiver of informed consent.
Patients
We included ED visits for children ≤21 years with minor blunt head trauma, which we defined as ED diagnosis of minor blunt head trauma with Glasgow Coma Score (GCS) of ≥14 recorded by the triage registered nurse on arrival to the ED. We included visits with any of the following International Classification of Disease Ninth Revision Clinical Modification (ICD-9-CM) primary discharge diagnosis codes: 959.01 head injury, unspecified and 850.0–850.9 concussion with and without loss of consciousness. Children with ≥1 ED visit with a primary head trauma discharge diagnosis were included for each eligible visit. Children without GCS recorded were not included.
QI Strategy
Planning the Intervention
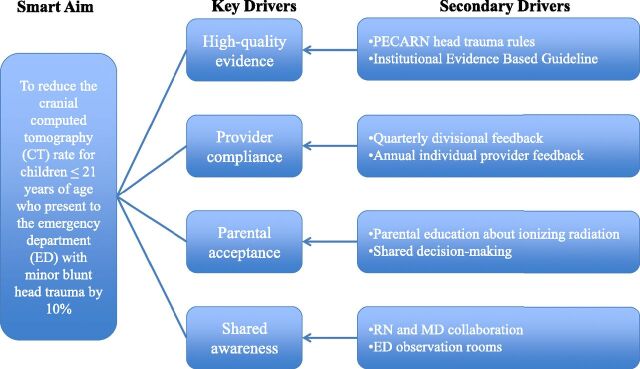
The institutional ED leadership was developing a comprehensive program for improving clinical care with a focus on translation of published evidence as well as national guidelines, when available, into local evidence-based guidelines and to both improve and standardize practice. We developed guidelines for both common and rare conditions with a significant risk for morbidity or mortality. In that context, care for children with minor head injury was identified as an opportunity for improving care, both to decrease non–value added resource utilization and to spare children from unnecessary and risky testing. The improvement team analyzed key drivers and constructed a multidisciplinary plan to reduce the CT rate by 10% for ED patients with minor blunt head trauma (Fig 1).
FIGURE 1.
Key driver diagram for reduction of cranial CT for minor blunt head trauma. PECARN, Pediatric Emergency Care Applied Research Network.
Evidence-Based Guideline
First, a pediatric emergency medicine attending and nurse developed the initial head trauma clinical guideline based on the PECARN TBI age-based clinical prediction rules (published October 2009). 5 The guideline was revised through an iterative process with input from multiple pediatric emergency medicine and neurosurgical attending physicians from the study institution.
The head trauma guideline focused on appropriate CT decision-making (Supplemental Information). Recommendations for CT use are based on PECARN TBI predictors 5 modified for local use. An immediate CT is recommended for children with either a single high-risk or ≥3 of the other PECARN TBI predictors. A period of observation before CT decision-making is recommended for children with 1 or 2 predictors, and no CT is recommended for children with no PECARN TBI predictors.
Because development of a guideline is only a single step in the process of changing care and effective translation to the bedside is imperative for success, we carried out a multifaceted implementation strategy. To optimize successful integration of the entire guideline program into care, a team was assembled and charged with reviewing implementation science literature, increasing awareness of the guidelines, and developing strategies to support adoption. This team consisted of an ED physician, a nurse educator and research expert, a QI expert, and an administrator. First, we arranged for an hour-long multidisciplinary conference where peers were encouraged to provide guideline feedback. Second, because structural support has been shown to be effective at supporting reliable change, 10 we created a head trauma electronic order set that included a link to the guideline plus supporting text to remind clinicians of the predictors of clinically significant TBI. We also created electronic discharge instructions readily accessed in the electronic health record.
A date was identified for rollout of the improvement project (October 2011). At this time, electronic communications, posted reminders in the ED, as well as changes to the electronic head trauma order set began. Additionally, every quarter after the initial guideline rollout, we used e-mail and in-person educational refreshers for all ED fellow and attending providers. Throughout, clinicians were encouraged to actively involve parents and caregivers in CT decision-making.
Individual Provider Feedback
Because individual provider feedback is a reliable way of implementing new practices, 11 we include this method in our implementation strategy to improve awareness, acceptance, adoption, and adherence to head trauma guideline recommendations. 12 The ED division chief (R.G.B.) performs an annual review for every pediatric emergency medicine attending physician that includes several clinical quality metrics. Each fall starting in 2012, every attending provider in the ED of the study institution received a confidential report of annual cranial CT rates for ED patients with minor blunt head trauma for the previous year. In addition, the division chief provided median overall division CT rate (with interquartile range) for the previous academic year. The goal of the individual feedback was to reduce variability between providers while further decreasing overall CT rate.
Data Collection
We identified eligible records using an automated search of the institutional data warehouse to identify ED visits with both an eligible discharge diagnosis code and a GCS assigned. We abstracted patient demographics including age, gender, and self-reported race as well as initial GCS. We then determined whether neuroimaging (either a cranial CT or a magnetic resonance imaging) was performed as well as ED length of stay. We also identified return visits within 72 hours of initial ED encounter that resulted in hospital admission.
Outcome Measure
Our primary outcome measure was the performance of a CT during the initial ED visit. Our primary balancing measure was a missed clinically significant TBI defined as revisit within 72 hours of index visit requiring hospitalization for management of head injury. Our secondary balancing measure was ED length of stay defined as time from ED triage to disposition (either time of discharge or of hospital admission). We selected this balancing measure because the institutional head trauma guideline recommended a period of observation in lieu of imaging for selected patients.
Statistical Analysis
We compared the characteristics of the patients from the “preperiod” QI implementation period (January 2010–October 2011) and the “postperiod” (November 2011–June 2014). We compared proportions with the χ2 test and medians with the Mann-Whitney test.
Statistical process control methods were used to monitor changes in the primary outcome (cranial CT rate) over time for children with minor blunt head trauma. Control limits were set at 3 SD from the mean rate. 13 Standard criteria were used to determine if observed changes were due to random variation (common cause variation) or a specific intervention (special cause variation). 14 We also examined trends in the primary (missed clinically significant head injuries) and secondary (ED length of stay) balancing measures.
To investigate whether any observed changes in CT rate could be explained by a temporal trend, we compared the study institution CT rate by quarter to the other 34 tertiary-care pediatric EDs that contributed reliable ED visit data to the Pediatric Hospital International System (PHIS) administrative database 15 during the study period (January 1, 2010–June 30, 2014). For this analysis, we identified children aged ≤21 years with a head trauma ED discharge code (using the same International Classification of Disease codes as noted earlier) from the PHIS database for both the study institution and the comparison hospitals. Because GCS was not available in this administrative database, we restricted this analysis to patients who were discharged from the ED to exclude children with more significant injuries. Using a linear regression model with clustered robust standard errors to adjust for study center, we compared trends over the study period in CT rate between the study institution and the other PHIS hospitals employing an interaction term for the effect of time by center.
We used ChartRunner Lean version 3.0 for the statistical process charts. 16 All other analyses were performed with Statistical Package for the Social Sciences (SPSS) version 21.0.0. 17
Results
Over the 54-month study period, we identified 7902 ED visits with a head trauma discharge diagnosis of which 7000 (89%) had an available GCS. Of these, we identified 6856 encounters with a GCS ≥14 for 6607 unique patients. For the 220 children with multiple ED visits, 201 (91%) had 2 and 19 (9%) had ≥3 ED visits for minor blunt head trauma. Of the included ED visits, 4104 (60% of overall visits) occurred in the postperiod (after the implementation of the institutional head trauma QI initiative). Patients in the pre- and postperiods were similar (Table 1).
TABLE 1.
Comparison of Eligible ED Encounters From the Pre- Versus Postintervention Periods
| Characteristics | Preperiod, n (%), N = 2752 | Postperiod, n (%), N = 4104 | P |
|---|---|---|---|
| Eligible ED encounters/mo a | 121 (107–149) | 128 (112–141) | .49 |
| Age, y a | 6.4 (1.7–13.3) | 6.8 (2.0–13.4) | .23 |
| Male gender, (%) | 1634 (59) | 2504 (61) | .18 |
| Race, (%) | .10 | ||
| White | 1486 (54) | 1962 (48) | |
| Black | 458 (17) | 678 (17) | |
| Initial GCS of 14, (%) | 94 (3) | 129 (3) | .53 |
| Admission, (%) | 204 (7) | 310 (8) | .80 |
| Clinically important TBI, (%) b | 5 (0.2) | 10 (0.2) | .59 |
Mann-Whitney test for medians.
Clinically important TBI as defined by head injury resulting in death, intubation for >24 h, neurosurgery, or ≥2 nights in the hospital for management of head injury.
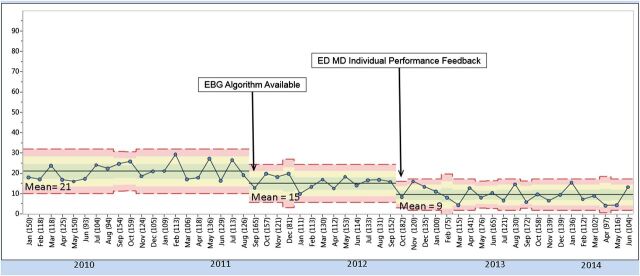
Next we examined the CT rate over time at the study institution (Fig 2). The preintervention CT rate was 21% (lower control limit [LCL] 10% and upper control limit [UCL] 31%). The CT rate dropped to 15% (LCL 6% and UCL 25%) after evidence-based guideline implementation and to 9% (LCL 2% and UCL 18%) after individual provider feedback on cranial CT rate was implemented. We identified no ED visits for minor blunt head trauma in either the pre- or postinterventional period in which the child was initially discharged and subsequently required hospitalization within 72 hours of initial ED evaluation for management of a TBI. Magnetic resonance imaging was used in only a minority of ED visits (0.6% preintervention vs 0.3% postintervention period, P = .09).
FIGURE 2.
Statistical process control chart showing CT rate over time with control limits. EBG, evidence based guideline.
ED length of stay for study patients decreased slightly from 2.9 hours (interquartile range 2.0–4.0) in the preintervention to 2.7 hours (interquartile range 1.7–3.8 hours) in the postintervention period (median difference 0.2 hours 0.1–0.4 hours), while overall ED length of stay for all patients did not change (data not shown).
Next, we examined the impact of provider feedback on cranial CT rate over time for pediatric emergency medicine attending providers who had evaluated at least 5 children with minor blunt head trauma each of the 4 years of the study (Table 2). We identified 29 eligible providers with 3658 ED visits for children with minor blunt head trauma (53% of the included ED visits during the same interval). Providers with the highest baseline CT rates had the largest observed decreases (13% pre vs 6% post; mean difference 7%, 95% confidence interval 4%–10%).
TABLE 2.
Impact of Provider Feedback on Cranial CT Rate by Baseline Quartile of Provider CT Rate (2010–2011) Compared With Postimplementation Period (2012–June 2014)
| Quartile | Mean CT rate Pre-Period, % (95% CI) | Mean CT Rate Postperiod, % (95% CI) | Mean Difference, % (95% CI) |
|---|---|---|---|
| 1 (lowest baseline), (%) | 4 (2 to 5) | 2 (1 to 4) | 2 (1 to 4) |
| 2, (%) | 6 (5 to 7) | 6 (2 to 10) | 0 (–2 to 3) |
| 3, (%) | 8 (7 to 9) | 5 (2 to 10) | 3 (1 to 5) |
| 4 (highest baseline), (%) | 13 (10 to 16) | 6 (1 to 14) | 7 (5 to 9) |
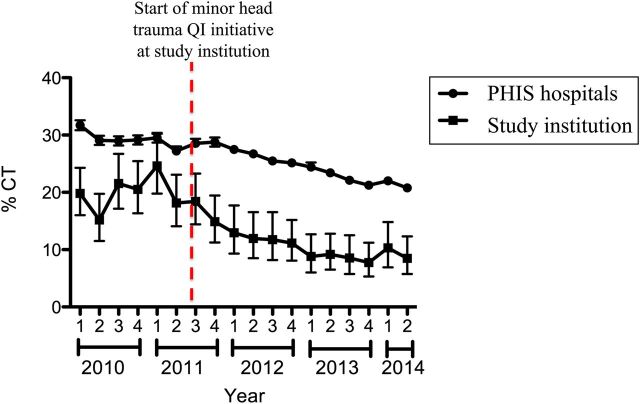
Last, we compared our institutional cranial CT rate to the other pediatric institutions that contribute ED data to the PHIS administrative database (Fig 3). The baseline CT rate at our study institution was substantially lower than the other study institutions. Although CT rates declined at all included PHIS institutions (from 32% to 20%), the rate of decrease was more substantial at the study institution (P < .001).
FIGURE 3.
Mean CT rate with 95% CI by quarter for the study institution compared with other 35 comparator hospitals contributing ED data to the PHIS administrative database.
Discussion
We designed and implemented a multifaceted QI initiative designed to reduce the cranial CT rate for ED patients with minor blunt head trauma. By applying QI methodology, we demonstrated declines in cranial CT rate associated both with the introduction of an evidence-based guideline and with individual provider feedback about cranial CT rate. No children with a head injury requiring any acute intervention were missed throughout the study period. Although CT rates also declined at the other similar academic centers, the CT rate fell more quickly at the study institution.
Our main goal for improvement was a reduction of CT use to minimize ionizing radiation exposure. At baseline, few children who had a CT performed required acute intervention, suggesting that neuroimaging might not be required in every case. The publication of the PECARN TBI age-based clinical prediction rules 5 and 2 subsequent external validation studies 6 , 7 have provided clinicians high-quality evidence to determine the risk of a clinically significant TBI. Recognizing the well-described gap between evidence generation and change in clinical practice, 18 we designed our implementation strategy to provide clinicians high-quality evidence at the point of decision-making by careful integration into existing work flow. Of note, the reduction in head CT rates has been sustained over >2 years since the improvement initiative was begun. Future QI efforts that include further integration of clinical decision support for children with minor blunt head trauma into the electronic health records might further reduce CT utilization. 19
Provider feedback is an effective vehicle of behavior change for clinicians. 20 , 21 In 1 recent QI initiative to improve the timeliness of discharge summary completion, provider feedback was an important component of the implementation strategy. 22 The impact of physician feedback has been correlated with the knowledge and credibility of the person who provides the feedback. 23 We observed a further reduction of cranial CT rates temporally related to providers receiving annual CT reports delivered by the ED division chief. The primary impact was to reduce variability in CT rates between ED providers. Clinicians with high baseline CT utilization demonstrated the greatest declines in CT rates.
Clinical observation allows selective CT use for children whose symptoms worsen or fail to improve during a period of ED observation. 24 Observation has previously been associated with a time-dependent reduction in CT rate 25 and has been suggested for the management of minor blunt head trauma in the AAP Choosing Wisely campaign. 8 We had expected ED length of stay for children with minor blunt head trauma to increase over the implementation period as more clinicians used observation rather than immediate CT. Interestingly, ED length of stay for children with minor blunt head trauma decreased slightly from the pre- to postimplementation periods, suggesting that the institutional head trauma QI initiative allowed for more efficient care delivery for children with minor blunt head trauma.
CT use has been steadily increasing over the past several decades. 26 The association between ionizing radiation and increased risk of lifetime malignancy is now well recognized. 2 – 4 Recent investigations have suggested that CT rates have started to decline, at least for children cared for in pediatric institutions. 9 , 27 To address the anticipated temporal trends in our analysis, we included a secular control group of children with minor blunt head trauma cared for in the ED of pediatric centers that contribute to the PHIS administrative database. As suspected, the cranial CT rates declined across institutions over the study period. However, the rate of decline was steeper at the study institution, suggesting the institutional head trauma QI initiative had an independent impact on cranial CT rate.
There were limitations to this project. First, our QI project was conducted at a single institution and the observed impact may not be generalizable. However, we based our management algorithm on high-quality published evidence and used well-validated methods of physician behavior change. Second, we were unable to account for severity of head injury because we did not collect standardized clinical data. However, we limited our statistical control chart analysis to those children with initial GCS of ≥14. Although GCS score is used widely, EDs that evaluate a low number of pediatric patients may have limited familiarity with the pediatric GCS, which might limit the generalizability of our approach. For the PHIS secular trend analysis, we selected discharged patients with head injuries to limit heterogeneity in injury severity because GCS was not available in this administrative data set. Although we clustered by center in the PHIS analysis, we were not able to adjust for institutional differences in injury severity. Third, we were unable to capture return visits to other health care facilities and may have underestimated the primary balancing measure, missed head injuries requiring hospitalization with 72 hours. However, previous work has suggested that most patients return to the same institution for follow-up care. 5 , 28 Last, as the provider feedback investigation was restricted to attending providers with a minimum of 5 head trauma visits for each of the study years, new providers or providers with low head trauma volume were not included. We hypothesize that the impact of the provider feedback might be greater for less-experienced or low-volume attending providers.
Conclusions
Our multifaceted QI intervention was effective at reducing the cranial CT rate at the study institution without missing significant injuries. Both the clinical guideline and individual provider feedback had an independent impact on the cranial CT rates. Importantly, the observed reductions in CT rate have been sustained for 2 years postimplementation, which supports the sustainability of the QI interventions.
Supplementary Material
Acknowledgments
We thank Michael C. Monuteaux, ScD, for his help with obtaining PHIS data and Stephanie Parver, MPH, for her help preparing the statistical process control chart.
Glossary
- AAP
American Academy of Pediatrics
- CI
95% confidence interval
- CT
computed tomography
- ED
emergency department
- GCS
Glasgow Coma Score
- LCL
lower control limit
- PECARN
Pediatric Emergency Care Applied Research Network
- PHIS
Pediatric Hospital Institutional System
- QI
quality improvement
- SPSS
Statistical Package for the Social Sciences
- TBI
traumatic brain injury
- UCL
upper control limit
Footnotes
Dr Nigrovic conceptualized and designed the study, performed and supervised the primary data abstraction and analysis, and drafted the initial manuscript; Dr Stack helped design the quality improvement [QI] initiative, provided leadership for the QI implementation, identified eligible cases, and provided critical review of the manuscript, and approved the final manuscript; Dr Mannix conducted multivariate regression analyses and provided critical review of the manuscript; Dr Lyons helped with QI implementation and provided critical review of the manuscript; Dr Samnaliev helped to plan the analysis and provided critical review of the manuscript; Dr Bachur designed and implemented the individual provider feedback and provided critical review of the manuscript; Dr Proctor conceptualized and designed the study and provided critical review of the manuscript; and all authors approved the final manuscript as submitted.
FUNDING: This project was supported by a grant from the Provider Payor Quality Initiative foundation (Boston, MA).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1. Mannix R , Bourgeois FT , Schutzman SA , Bernstein A , Lee LK . Neuroimaging for pediatric head trauma: do patient and hospital characteristics influence who gets imaged? Acad Emerg Med. 2010;17(7):694–700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brenner DJ , Hall EJ . Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284 [DOI] [PubMed] [Google Scholar]
- 3. Frush DP , Goske MJ , Hernanz-Schulman M . Computed tomography and radiation exposure. N Engl J Med. 2008;358(8):851 , author reply 852–853 [PubMed] [Google Scholar]
- 4. Pearce MS , Salotti JA , Little MP , et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kuppermann N , Holmes JF , Dayan PS , et al. Pediatric Emergency Care Applied Research Network (PECARN) . Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160–1170 [DOI] [PubMed] [Google Scholar]
- 6. Schonfeld D , Bressan S , Da Dalt L , Henien MN , Winnett JA , Nigrovic LE . Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice. Arch Dis Child. 2014;99(5):427–431 [DOI] [PubMed] [Google Scholar]
- 7. Easter JS , Bakes K , Dhaliwal J , Miller M , Caruso E , Haukoos JS . Comparison of PECARN, CATCH, and CHALICE rules for children with minor head injury: a prospective cohort study. Ann Emerg Med. 2014;64(2):145–152, e1–e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics. Choosing Wisely. Available at: http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-pediatrics/. Accessed April 23, 2013
- 9.Mannix R, Meehan WP, Monuteaux MC, Bachur RG. Computed tomography for minor head injury: variation and trends in major United States pediatric emergency departments. J Pediatr. 2012;160(1):136–139.e131 [DOI] [PMC free article] [PubMed]
- 10. Gagliardi AR , Brouwers MC , Palda VA , Lemieux-Charles L , Grimshaw JM . How can we improve guideline use? A conceptual framework of implementability. Implement Sci. 2011;6:26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. C humpitazi CE, Barrera P, Macias CG. Diagnostic accuracy and therapeutic reliability in pediatric emergency medicine: the role of evidence-based guideline. Clin Pediatr Emerg Med. 2011;12(2):113–120 [Google Scholar]
- 12. Pathman DE , Konrad TR , Freed GL , Freeman VA , Koch GG . The awareness-to-adherence model of the steps to clinical guideline compliance. The case of pediatric vaccine recommendations. Med Care. 1996;34(9):873–889 [DOI] [PubMed] [Google Scholar]
- 13. Benneyan JC , Lloyd RC , Plsek PE . Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Back SE, Book SW, Santos AB, Brady KT. Training physician-scientists: a model for integrating research into psychiatric residency. Acad Psychiatry. 2011;35(1):40–45 [DOI] [PMC free article] [PubMed]
- 15. Bourgeois FT , Monuteaux MC , Stack AM , Neuman MI . Variation in emergency department admission rates in US children’s hospitals. Pediatrics. 2014;134(3):539–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. ChartRunner Lean [computer program]. Version 3.0. Dayton, OH: PQ Systems, Inc; 2013
- 17. PASW Statistics 21 [computer program]. Version 21.0. Chicago, IL; 2012
- 18. Institute of Medicine of the National Academies; Committee on the Future of Emergency Care in the US Health System; Board on Health Care Services. Emergency Care for Children: Growing Pains. Washington, DC: National Academy Press; 2007. [Google Scholar]
- 19. Sheehan B , Nigrovic LE , Dayan PS , et al. Pediatric Emergency Care Applied Research Network (PECARN) . Informing the design of clinical decision support services for evaluation of children with minor blunt head trauma in the emergency department: a sociotechnical analysis. J Biomed Inform. 2013;46(5):905–913 [DOI] [PubMed] [Google Scholar]
- 20. Jamtvedt G , Young JM , Kristoffersen DT , O’Brien MA , Oxman AD . Does telling people what they have been doing change what they do? A systematic review of the effects of audit and feedback. Qual Saf Health Care. 2006;15(6):433–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Forrest CB , Fiks AG , Bailey LC , et al. Improving adherence to otitis media guidelines with clinical decision support and physician feedback. Pediatrics. 2013;131(4). Available at: www.pediatrics.org/cgi/content/full/131/4/e1071 [DOI] [PubMed] [Google Scholar]
- 22.Bischoff K, Goel A, Hollander H, Ranji SR, Mourad M. The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774 [DOI] [PubMed]
- 23. Ferguson J , Wakeling J , Bowie P . Factors influencing the effectiveness of multisource feedback in improving the professional practice of medical doctors: a systematic review. BMC Med Educ. 2014;14:76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nigrovic LE , Schunk JE , Foerster A , et al. Traumatic Brain Injury Group for the Pediatric Emergency Care Applied Research Network . The effect of observation on cranial computed tomography utilization for children after blunt head trauma. Pediatrics. 2011;127(6):1067–1073 [DOI] [PubMed] [Google Scholar]
- 25. Schonfeld D , Fitz BM , Nigrovic LE . Effect of the duration of emergency department observation on computed tomography use in children with minor blunt head trauma. Ann Emerg Med. 2013;62(6):597–603 [DOI] [PubMed] [Google Scholar]
- 26. Blackwell CD , Gorelick M , Holmes JF , Bandyopadhyay S , Kuppermann N . Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Ann Emerg Med. 2007;49(3):320–324 [DOI] [PubMed] [Google Scholar]
- 27. Menoch MJ , Hirsh DA , Khan NS , Simon HK , Sturm JJ . Trends in computed tomography utilization in the pediatric emergency department. Pediatrics. 2012;129(3):e690–e697 [DOI] [PubMed] [Google Scholar]
- 28. Axon RN , Williams MV . Hospital readmission as an accountability measure. JAMA. 2011;305(5):504–505 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.