Abstract
The Chief Medical Officer recommends that all health care workers receive an influenza vaccination annually. High vaccination coverage is believed to be the best protection against the spread of influenza within a hospital, although uptake by health care workers remains low. We conducted semistructured interviews with seven medical students and nine early career doctors, to explore the factors informing their influenza vaccination decision making. Data collection and analysis took place iteratively, until theoretical saturation was achieved, and a thematic analysis was performed. Socialization was important although its effects were attenuated by participants’ previous experiences and a lack of clarity around the risks and benefits of vaccination. Many participants did not have strong intentions regarding vaccination. There was considerable disparity between an individual’s opinion of the vaccine, their intentions, and their vaccination status. The indifference demonstrated here suggests few are strongly opposed to the vaccination—there is potential to increase vaccination coverage.
Keywords: seasonal influenza vaccination, medical education, role models, socialization, medical identity construction, qualitative interviews, thematic analysis, north-west England
Background
Seasonal influenza is an acute, contagious, viral respiratory infection which causes considerable morbidity and mortality worldwide (World Health Organization, 2014). The elderly, young, and those with underlying health conditions are disproportionately affected by the disease.
Constant evolution of the influenza virus means that each year, the vaccine must be reformulated. Using information available in February, the World Health Organization predicts which strains of the virus will most likely be circulating in the northern hemisphere during the subsequent winter (Centers for Disease Control and Prevention, n.d.). Mismatched seasons occur when the predominant strain circulating in the population is not covered by the vaccine—this may happen if the virus mutates unexpectedly. A recent meta-analysis found that during mismatched seasons, the vaccine efficacy was between 56% and 60%, and that this improved to 65% to 77% during matched seasons (Tricco et al., 2013).
Each year, the Chief Medical Officer for England advises that all health care workers (HCW) receive a seasonal influenza vaccination (GOV.UK, n.d.). Increasing seasonal influenza vaccination among HCW is thought to have beneficial consequences including reductions in staff absentee days, the spread of influenza within the hospital, and elderly patient mortality (Burls et al., 2006). However, the evidence for protection of other groups of patients, conferred by HCW vaccination, is not conclusive. Views on HCW vaccination within the scientific community are often polarized; some recommend mandatory vaccination policies, believing that vaccination of HCWs benefits patients and health care institutions have an obligation to promote behavior consistent with such professional virtues and ethical principles (Helms & Polgreen, 2008; Tilburt, Mueller, Ottenberg, Poland, & Koenig, 2008), others argue that mandatory influenza immunization of all HCW is an excessive infringement on autonomy and could damage morale (Isaacs & Leask, 2008). Uptake of the vaccine by HCW in England remains at approximately 55%—well below the target of 75% (Public Health England, n.d.). Also, the recently announced national Commissioning for Quality and Innovation (CQUIN) standard will provide financial rewards for any Trust achieving 75% vaccination coverage. Given previous low vaccination uptake, Trusts will need to adjust their staff vaccination policies if they hope to achieve this (NHS England 2016/17 CQUIN, 2016).
Recent survey studies suggest that a number of factors contribute to HCW declining vaccination, including fear of adverse reactions, lack of concern, inconvenient delivery, and a lack of perception of their own risk (Hollmeyer, Hayden, Poland, & Buchholz, 2009; Smedley et al., 2007). The reasons for receiving an influenza vaccine were given as self-protection, protection of patients, convenience, and following the example set by peers (Hofmann, Ferracin, Marsh, & Dumas, 2006). However, there has been little qualitative research into these phenomena; thus, the relationship between these factors and why they arise remains unclear. Previous attempts to improve vaccine uptake have had limited success; however, studies which include a combination of interventions (focused around education, convenience, and leadership) appear slightly more effective (Rashid et al., 2016)—suggesting that some ambiguous complexities remain in current understanding.
Our study aimed to provide a deeper insight into the influenza vaccination practices of HCW. Influenza vaccination takes place within a professional and social setting occupied by medical professionals, patients, and junior staff members. When new members enter this setting, they begin to adjust to the social norms of the medical community—a formal and informal process of training and socialization. Capturing their attitudes as they are adjusting to this environment should provide an insight into vaccination culture across the hospital.
Method
We conducted a series of semistructured interviews to investigate the factors that influence seasonal influenza vaccine uptake in medical students and foundation doctors. Ethical approval was obtained from Lancaster University Research Ethics Committee prior to data collection.
Participants and Setting
Participants comprised final year medical students and foundation doctors and were recruited from a medical school and a single, large National Health Service (NHS) Trust, both in the North West of England. Foundation doctors work in a variety of settings, including hospitals, for 2 years of broad training following graduation from medical school. Final year medical students spend the majority of their time working in general practice and hospital settings.
Recruitment took place during mandatory teaching sessions, attendees were given an introduction to the study, then sent a follow-up email. Potential participants were asked to email the researcher to arrange an interview. At the time of recruitment, participants were emailed a copy of the participant information sheet (see Supplementary 1). Anyone who volunteered was interviewed, up to the point at which we believed no more information could be gained from further interviews.
Interview Protocol
Semistructured interviews were conducted by Rhiannon Edge over an 8-week period from February to April 2016, that is, between vaccination periods (October-January). Before commencement of the interview, participants were given a brief introduction to the project and signed a consent form. Interviews took between 30 minutes and an hour.
An interview schedule was used to guide discussion, although the semistructured approach allowed for flexibility and elaboration around each participant’s unique experiences (see Supplementary 2). Interviews were recorded and transcribed verbatim by Rhiannon Edge. Data collection and analysis took place in an iterative process, allowing for exploration of emerging themes.
Within the interviews, interactions were shaped by Rhiannon Edge being a similar age to the participants, and by being external to the medical professional. These factors, we feel, contributed a nonjudgmental characteristic to the interviews, as some participants reportedly shared views they had not discussed with peers. Accordingly, Rhiannon Edge did not comment on the accuracy of participants’ knowledge, but encouraged participants to elaborate on their beliefs throughout the interviews. Participants often commented that they had not previously reflected on their vaccination choices, their level of risk, and who might have been important in shaping their views. This is indicative of a decision-making process that is not necessarily a well-thought out, rational, cost-benefit analysis. It also shows that during the interviews, data were actively constructed, rather than a recording of preexisting views.
The data have been reported in participants’ own words. Due to constraints on word limit, some descriptive text has been removed and quotes were edited (e.g., by deleting repeated words). Additional context and participant’s unique identifier codes are included.
Analysis
Initial data analysis consisted of open coding line-by-line using largely descriptive labels. As the coding process evolved and consistent themes began to emerge, later transcripts were coded paragraph-by-paragraph (Braun & Clarke, 2006). Although the initial “first pass” coding was undertaken by Rhiannon Edge, the “fit” of the codes to interview excerpts, and the interpretation given to them, was the subject of detailed discussion and analysis by Rhiannon Edge and Dawn Goodwin. The coding schema was then iteratively refined following these discussions. Themes were thus developed inductively, focusing on factors which appeared most important to participants, rather than their overall prevalence (although these were highly correlated). Interviews were repeatedly reviewed, particularly if new themes emerged or in the event of a “negative case”—an example arising in which an existing theme could be re-evaluated (see discussion on professionalism). Data collection continued until theoretical saturation was observed (Morse, 2004). We deemed theoretical saturation to have occurred shortly after the point at which we felt interviews were no longer providing new insights. Participants commonly described a range of scenarios during their interviews, for example, in many cases, a single interviewee was able to discuss processes leading to vaccination and nonvaccination.
Results and Discussion
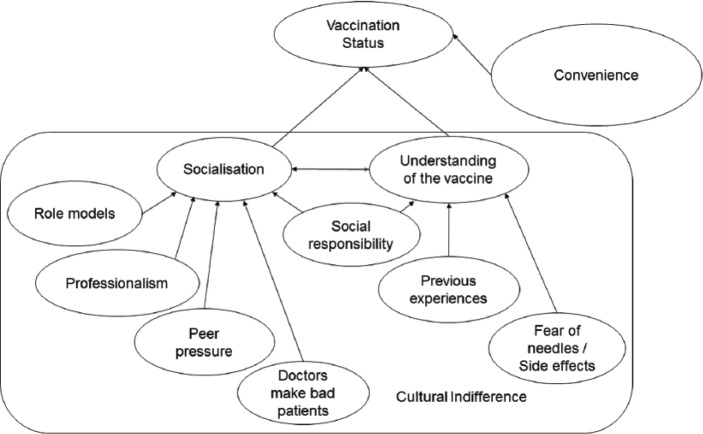
Of the nine foundation doctors and seven medical students in the sample, 10 had been vaccinated during the 2015/2016 season. However, all had been vaccinated for seasonal influenza at some point previously. We found the themes of socialization, understanding of the vaccine, and convenience to be important in whether or not the individual vaccinated (Figure 1).
Figure 1.
Schematic representation of the factors that affect medical students’ and foundation doctors’ seasonal influenza vaccination status.
Cultural Indifference
While some individuals were determined to receive or avoid vaccination, this stands in contrast to the position of most participants who did not have strong intentions relating to vaccination. We found elements of indifference toward the vaccine threaded throughout all the themes emergent in this dataset. Below, participants give examples of this (FD represents “foundation doctors” and MS represents “medical students”):
I just go and have it done and like it doesn’t, I don’t know, it’s just a bit like . . . not second nature but it doesn’t, I don’t think too much about it, I just have it done and I suppose I think other people might think, might weigh up the pros and cons a bit more, like might be a bit more scared of having the injection they might have it a bit more . . . I just kind of just have it, just roll up your sleeves stick it in and then just carry on with my day and don’t even think about it anymore . . . (MS)
I was probably a bit blasé, I think it’s important to do but I . . . yeh when I don’t see it I don’t think about it. (FD)
It’s just that I guess I don’t see the benefit in my own head I don’t see enough of a benefit to go out of my way to go and get it. (MS)
It’s just literally just I’d missed the chance to get it that day with occupational health went round and then kind of put it off and it didn’t get done. (FD)
It’s never really I can’t be bothered having it, it’s just like oh I’ve not had it that or not got round to that yet, it’s just, yeah people just don’t seem to have the time or put it high up on their priority list. (MS)
We found a lack of clear intention to vaccinate among participants. Even some who chose to vaccinate did not have clear reasons for doing so. Blank et al. found that French, German, and U.S. physicians seemed to be ambivalent toward the influenza vaccine—many did not consider the benefits of vaccinating to be worth their perceived risks (Blank, Bonnelye, Ducastel, & Szucs, 2012). This indifference suggests that the benefits and liabilities associated with vaccinating were finely balanced. Below we seek to clarify why and how the underlying tone of indifference arose, and the implications such indifference hold for vaccination uptake.
Socialization
Socialization is the
“structure, the method, and the route by which initiates move from one status to another and acquire the technical skills, knowledge, values and attitudes associated with the new position or group. Thus, one must attain a new cultural base but must also facilitate movement away from the old status.” (Leming & Dickinson, 2015).
While the socialization process is multifaceted, it is clear that senior staff are instrumental in shaping participants’ impressions of medical culture (Wright, Wong, & Newill, 1997). A vaccinated foundation doctor describes the effect of consultants on her behavior at work:
I copy what my consultants do . . . so if they don’t do it then I don’t do it. And that sounds very . . . it sounds very . . . you know that you’re just being sheep or whatever but my morning job consists of me following a consultant around and writing everything down that they say and then making a job list of what they want me to do so . . . they go very quick and just spend half my time having like no idea what’s going on and like diving after them into rooms and if they go and don’t have any protection I don’t have time to actually put on aprons, hand wash, and glove up, and everything so I literally just go straight after them and follow them like that. Otherwise, I’ll miss everything that’s going on so I kind of feel like it’s not really an option. (FD)
Junior doctors react to the behaviors to which they are exposed. Above, the participant talks about “copying” the behavior of the consultant even though she is aware she contravenes infection control procedures in doing so. Medical training emphasizes the importance of strict infection control procedures; however, she finds that these are not always practiced, and by copying the behavior of her consultant, her definition of what it means to be a professional doctor evolves. This is an example of socialization, during which early career doctors cast off their identities as lay-people and assume those of professional doctors (Toulis & Sinclair, 1997). This foundation doctor is being socialized to act in a way that conflicts with her previously held beliefs and describes the situation as stressful. Under these circumstances, the effects of socialization are particularly acute (Cruess, Cruess, & Steinert, 2001).
Socialization is a complex process involving both compliant and dissident behaviors, which are shaped by senior staff and interactions with peers. Through this process, participants learnt about their roles as doctors within the hospital. Below, an unvaccinated foundation doctor discusses her reactions to senior staff advocating vaccination:
Oh yeh, erm cos there are some consultants you should, like I said it becomes a bit of a team thing, and there were some consultants that said, “have you had your flu jab, have you had your flu jab” and you know if you haven’t had one sometimes they’ll ship you to one of the nurses and kind of stand there while you have your jab, and things like that, and we were actively you know avoiding these situations. Erm and every time we saw one of those consultants we would you know go hiding and things it’s, it’s really strange, it strange how much effort I put into avoiding these the jabs . . . erm yeah . . . (FD)
This quote demonstrates both the influence senior staff have on the development of the team’s attitude and the resistance it can sometimes provoke. This participant demonstrates a defiant attitude toward the consultants—in this comment, senior staff have facilitated a situation in which the participant, with support of her peers, rebels against their authoritative demands to vaccinate. This highlights the importance of peer support in the socialization process.
Peer Influences
Medical education is intrinsically collaborative; medical students often face challenges as a group, and interaction is an integral part of their experiences (Hafferty, 1991). Vaccination often takes place within professional, social situations and the peer group acts as an audience, regulating the vaccination performance:
When you know your friends are taking it, it feels like I will have it too, like I don’t want to be different. (FD)
As in ’cos I think like ahh, like a lot of them students have had it [the vaccination] and you haven’t had it so there’s definitely a peer pressure thing going on as well. ’Cos I think most people have had it whereas I hadn’t had it so that was another thing that made me think oh I’ve got to have it now . . . (MS)
Above, participants describe a desire to conform to social norms of their community, which leads them to vaccinate. However, as alluded to previously, both conformity and dissent are common. Below, an unvaccinated foundation doctor discusses camaraderie surrounding refusal to vaccinate:
She was one who was with me saying “yeah I think I’m going to avoid the flu jab this year,” because she also had I think a bit of a reaction to the one from the year before sooo yeah in, everybody else in the team kind of had their flu jabs and they were all talking about the jabs and how they were reacting to it, things like that. Erm me and Jenny were in our own little group saying “yeh, last year was horrific so I think I’m just going to avoid it this year,” so I think in that way there are little cliques of the yes’s and the no’s, so erm yeah that’s why . . . (FD)
This participant describes the situation in which cliques have formed based on a shared vaccination status. The two colleagues discussed side effects associated with the vaccine as part of their vaccination decision making. Clearly, the peer group helps to shape people’s understanding of the vaccine as well as influencing their actions. In this instance, we suggest that it is the defiant attitude and camaraderie, both established components of medical culture (Ives et al., 2009), rather than a fear of side effects that is important in this decision. The discussion of side effects is used to explain the resistance to the peer pressure to vaccinate, but it is the camaraderie that enables the continued resistance. Furthermore, that the two women collaborate and share in the vaccination decision making challenges the perception of vaccination as an autonomous decision. A vaccinated foundation doctor described it thus:
There are definitely more people who do it because we tend to do it in groups, there are people who get swept up into . . . who kinda don’t care either way but everyone else is doing it so . . . (FD)
This participant recognized that attitudes vary and feelings of indifference toward the vaccine exist. However, her comments suggest that peer pressure at the point of vaccine delivery overrides the indifference toward vaccination within the group.
Professionalism
As medical students and foundation doctors are socialized, being a medical professional becomes a defining feature of their identity (Monrouxe, 2010). Consequently, professionalism and social responsibility emerged as themes important in some participants’ vaccination decisions as influenza vaccination was intended to protect both HCW and their patients. This vaccinated foundation doctor describes concern for patient welfare as a key element in her vaccination decision:
We quite often feel frustrated that we’re not able to do as much for our patients as we’d like, this is something that might help almost by doing nothing if it can take a little bit of the edge off not feeling like you’re doing everything you can . . . why not? (FD)
The cost of vaccination to this individual is low, thus patient welfare was able to “tip the balance” of her decision toward vaccination. She highlights the high-pressured environment in which these decisions are taken, talking about feelings of frustration and inadequacy. For this participant, influenza vaccination is aligned with the professional value of “making the patient’s welfare your first concern” (General Medical Council, 2013). For some, this value held priority even when considering more significant costs of vaccination, such as side effects or fear of needles:
I’m getting it and then there’s one friend who I know doesn’t like needles so she never gets it and that her excuse is “I don’t like needles” . . . But I mean you do sort of think, being in the health care position you probably should because it’s about, you know, keeping your patients healthy. (MS)
The above quotes suggest that there is not only an awareness of peers’ vaccination practices but also some appraisal of their decisions. Definitions of professionalism rest on the premise of peer-review and self-regulation—both forms of social control—and thus are embedded within socialization (Cruess et al., 2001). Individuals are pragmatic; they compromise between trying to express conflicting personal thoughts and being cooperative—they may demonstrate conformist or dissenting views—but, often, the social group has some influence over the individual (Hodges & Geyer, 2006). Above, the participant is provoked by a colleague’s dissenting views which conflict with her professional values, demonstrating how one’s actions are subject to the judgment of one’s peers. Social control is facilitated by the individual’s internalization of this judgment (Aronfreed, 1968)—this is illustrated below:
It’s something you wouldn’t talk about publically and say I wouldn’t feel comfortable for example, around all my uni friends saying “okay I have not had my flu vaccination,” I wouldn’t because I know I would be judged because . . . They’d say, “well you’re a medical student your gunna be a doctor, and your gunna tell people to have it, and you haven’t had it yourself,” so that’s something that’s a bit . . . (MS)
Her perceptions of her peers’ opinions prevent discussion around the influenza vaccine. She expects that her peers would associate lack of vaccination with hypocrisy, demonstrating the link between vaccination and professionalism. The quote below is not only disapproving of nonvaccination, but positions it as illogical:
So from a sort of logical point of view I wouldn’t really understand why they are against it, because I guess we are quite derogatory with vaccinations. We always think that people that refuse them always are those hippy dippy mums that don’t want to like put their children near any sort of medications whatsoever and actually its more detrimental to them in the future . . . So I associate all people that don’t really want vaccinations in that pile, and I think that it would confuse me a little bit if I came across doctors, that are meant to be pro-healthcare, pro-medication and bit more health educated, it would confuse me about that . . . (FD)
The participant quoted above aligns vaccination with professional values; it is part of medical culture, and thus she and her peers should be pro-vaccination. The participant’s perceptions of the medical position encourage her to disparage unvaccinated individuals. However, we found that vaccination is not overtly and universally associated with professionalism. In response to a question about vaccination as an act of professionalism, one unvaccinated foundation doctor replied,
I’ve never really thought about it like that . . . but then if that is like, that would make me feel really, that would make me get it, if people were like oh its associated with professionalism, like it’s not a professional thing if you don’t get the vaccine because your putting your patients at risk, like I’ve never even thought about it that way. And if I did I think that would make me get the vaccine, but I’ve never . . . I’ve never considered that. (FD)
This foundation doctor is concerned about her image and identity as a professional, and while she understands the connection between vaccination and professionalism, concern for patient welfare had not featured as part of her rationale. Understandings of the vaccine are shaped through socialization; however, experiences of socialization are variable. This doctor had previously been placed on a surgery rotation where, as we discuss below, exposure to patients with influenza was infrequent and thus awareness of the need for vaccination was lower, which may in turn suggest heterogeneity in attitudes among different specialties within the hospital. Below is the response from an unvaccinated foundation doctor when asked if she had considered vaccinating to protect her patients:
. . . I definitely didn’t think about that, I didn’t factor that into the equation of you know, do this, if not for yourself for the safety of the patients cos I think, everybody would do it then, everybody would. You don’t want to make someone who’s sick worse, because you couldn’t be bothered to take the flu jab. I think that’s, that’s terrible ermm, we would judge you then, I think yeah even if you didn’t want to do it the entire team would judge you then saying, “do you not care for your patients, why would you not take it?” Ermm so yeah that would be a good campaign strategy actually, if you wanted to get 100% concordance with the flu jab, yeh that’s the way to go. (FD)
For the participants above, social responsibility to vaccinate, or connotations with professionalism, did not inform their decision. However, they suggest that they would vaccinate, if there was a stronger professional message—exhibited by their peers and part of their socialization—that vaccination was to be a reflection of their professionalism. Interestingly, the mention of judgment by peers, when the foundation doctor discusses the notion of vaccination as an act of professionalism, provides further evidence that perception of peers’ opinions can influence the actions of an individual within the group.
An example of a strong professional steer is given by the medical student below, who described being under institutional pressure to vaccinate (facilitated by the vaccine appearing as an activity in students’ logbooks). The logbook is used to record completed learning objectives and clinical evaluations throughout the course and thus functions as a physical representation of the student’s professionalism. Influenza vaccination appeared as an optional section in the logbook, symbolizing vaccination as a construct of professionalism, and encouraged them to actively seek it out.
In my mind this was the university telling me you have to have the flu vaccine this year, so that’s, actually, I had forgotten about that, that’s the probably the main reason why I had it done last year cos I was afraid that I wouldn’t have that signature in the log book. (MS)
Decision making, thus, cannot be isolated from professional values which are mobilized through socialization. Therefore, although participants often felt ambivalent toward the influenza vaccine, and there were variable interpretations of its association with professionalism, when the injection appeared in the medical student’s logbook, this was interpreted as a clear directive, encouraging vaccination.
Doctors Make Bad Patients
As can be identified in the data above, medical professionals feel subject to an expectation that they should conform to health care advice (BMJ Careers, 2013). A medical student describes this as a fear of judgment from her peers:
I think there is judgment, definitely, since some people would judge you: “oh so you know we should be telling patients to do this, how come you’re not doing this? That’s hypocritical" and you’ll definitely get judgment. Also I think as . . . doctors, or as health care professionals in general, not just doctors, as health care professionals I think were expected in a public setting, if were telling the public to do something were expected to do it ourselves. So it’s a bit, so I can see, you know, it’s a bit, it’s not something that I would feel comfortable talking to anyone about . . . (MS)
Although this participant reports that there is an expectation of compliance with health care advice, often participants would contradict this. During the interviews, it emerged that some participants did not vaccinate against influenza due to a wider defiant attitude toward their own health. The characterization of doctors as “the worst patients” has been previously established (Baldwin, Dodd, & Wrate, 1997; Strang, Wilks, Wells, & Marshall, 1998). For some, even a slight fear of having an injection made them less likely to vaccinate against influenza. Below, two foundation doctors describe a fear of needles leading to their refusal to vaccinate:
Er I just . . . I don’t like having any vaccinations really, I really don’t like needles. (FD)
ah I think it’s [the vaccine’s] good, erm I think it’s good to sort of get people to take it if you can just to stop people getting ill primarily. Stop people sort of taking time off work that sort of thing . . . Erm I haven’t actually had mine yet, but that’s cos I don’t like needles, but erm yeah I think it’s a good thing. (FD)
Despite a positive attitude toward the vaccine, the fear of needles “tips the balance” for these participants. However, a stronger justification for having the vaccine may outweigh their fears:
I mean the needle thing if I have to get over it I will, like I had all my shots when I was at school and stuff, and so erm it’s just the thought of doing it but when I’m there I probably would manage ok. (FD)
Some doctors believe that they will not become ill, as the patient is “the one with the disease” and they detach themselves from their own morbidity (Klitzman, 2007). Some participants did not have the influenza vaccine as they did not believe they were at a high risk from the virus. However, it appeared that this was a facet of a general “bad patient” attitude being, for example, associated with failure to complete courses of antibiotics or denial of asthma symptoms. Some examples are as follows:
As a patient, you know like I’m the worst patient I’m not compliant with anything I’m really terrible . . . like I never take my inhalers and erm . . . yeah I’m . . . I think that doctors are bad patients and I think I’m really bad I’m just not compliant at all “cut three lines of descriptive text” I’m really bad with taking medications, I think that the flu vaccine thing falls in with that. I’m not very good at like going to the GP. (FD)
I don’t think I really believe that I would catch any virus travelling either, I mean I know logically it’s possibly, but I don’t think I actually believe that I’m likely to catch anything. (FD)
Erm terrible, I am a terrible patient, yes, that’s correct, I am a terrible patient, usually on anti-biotics I don’t, whatever, I tend to be fine. If I have diarrhea for example, and erm and I’m given an antibiotic prescription, three times a day, never take them and then . . . Yeh I am a terrible patient. (MS)
Being a “bad patient” is a liberty these doctors allow themselves, despite frustration when patients demonstrate similar behavior, which falls within the heroic, infallible doctor persona (Becker, 1977; Klitzman, 2007). This behavior is normalized through the process of socialization. Nevertheless, there is an expectation that doctors will follow best health practices; thus, when they fail to do so, they have a sense of guilt. Doctors who are “bad patients” may be more likely to justify refusal of the vaccine due to side effects, inconvenience, or the lack of vaccine efficiency—possibly because of a perceived stigma attached to their attitudes. Below is an example from an unvaccinated foundation doctor:
I think, so like if there’s something you don’t like doing then you’ll find any excuse to put it off. So the fact that you know, “oh I’ve got to go down to occupational health, oh I’ve got to do this,” it adds other reasons to put it off so I think if it was something quick like a nasal spray then yeah 100% it would be a lot easier. (FD)
It also emerged that many participants did not know where the occupational health department was and did not make use of it. Baldwin et al. (1997) has previously suggested that the role of occupational health was unclear to doctors. This further highlights this group’s indifference toward their own health needs. Doctor’s courageous attitude toward work and their own health needs has been found to permit self-negligence; often doctors are found to underreport health concerns or go to work when sick (Thompson, Cupples, Sibbett, Skan, & Bradley, 2001). Within this theme there is incongruity derived from conflicting elements of an expectation to comply with health care advice and refusal to do so. This conflict suggests a broader context of ambivalence surrounding the factors involved with influenza vaccination.
Understandings of the Vaccine
Many actors are influential in the construction of our understanding of scientific knowledge. Through the processes of socialization, peers and role models informed participant’s understanding of the vaccine. Participant’s perceptions were shaped by the unique situations they were embedded within. A vaccinated foundation doctor discusses the effects of a consultant’s vaccination on her own decisions:
I know that our respiratory consultant does, and partly because he’s a respiratory consultant and should know what impact flu season has, and partly because he’s lovely—I reckon him doing it has an impact. (FD)
Here, the consultant acts as a positive role model for vaccination. His views were considered authoritative and the respondent values his seniority and the credibility of his knowledge. Cicourel (1990) noted that medical professionals determine value of information dependent on the perceived credibility of the source. There was further evidence that there were interspecialty differences in attitudes toward the influenza vaccine:
So cos I’m an F1 I’ve only been in surgery and psychiatry so far, I mean as a doctor and the, I think the surgeons, it wouldn’t be very high up on their priorities and things. The medics, maybe the acute medics are probably a bit more aware of it. Cos I did go to a medical grand round, a month or two ago and it was all about flu and how they’d had many cases in the AMU and things erm . . . (FD)
The notion, that doctors from different specialties within the hospital behave differently, is possibly a facet of slight variations in a porous process of identity construction within different specialties (Pratt, Rockmann, & Kaufmann, 2006). Therefore, the idea that influenza vaccination has greater relevance in some specialties compared with others suggests a more targeted approach to changing vaccination understanding may be appropriate to improve coverage. We also found marked differences in attitudes toward the influenza vaccine expressed by senior staff. An unvaccinated medical student gives an example of a senior member of staff opposing vaccination:
One of the GPs at the practice last year and he was telling me about how they sort of guess about what viruses come up next, and the number needed to treat was quite high, so he was very like it doesn’t really work, and you know even when it does it’s hit and miss . . . He was the one person I remember being a bit anti-flu vaccine, but I think that resonated in me. (MS)
Senior staff appear to have a greater freedom to express more diverse opinions on the influenza vaccination. It has been suggested that senior staff are above reproach; therefore, their behavior is not constrained by peer opinion, in the way our participants may have been (Bosk, 2003). Despite the difference in vaccination opinions described by participants, it is clear that senior staff acting as role models have a substantial influence on the attitudes of junior doctors.
Previous Experiences
Participants gain knowledge and experience during clinical training, and what is learnt through these experiences is shaped by socialization. As we suggest above, previous experience of influenza and its effects either seen in patients or personally experienced also informed participant’s awareness. Here, a vaccinated foundation doctor was asked about her experience of influenza patients while working on an Acute Medical Unit:
Before I started working I didn’t think that the flu could be so bad because you sort of in a in a lay-man’s sort of terms you always throw around the word flu like “oh I’ve got the flu or you’ve got man flu or something like that” . . . And its really trivialised. But this year actually working in a hospital for the first time as a doctor, and seeing what can happen. I’ve seen patients that are like my age ending up, you know looking so crap, and erm really really ill from the flu, that’s quite scared me and I think that would definitely make me want to vaccinate more . . . Because we’ve had a erm just had a huge breakout basically. (FD)
She describes a “trivialized” attitude toward influenza prior to her experiences in the hospital. Her experience is defined by empathizing with patients who are similar to herself, which has altered her understanding of the risks associated with influenza. Previously, we heard from a participant who avoided vaccination by defiantly hiding from consultants. Below, she describes her changed opinion due to experiences of illness following her refusal to vaccinate:
I think my opinion was already changed to be honest, erm by the time I had had that you know one major illness, I’d pretty much wised up to you know the advantages of flu jab, and every time we talked about it, it just kind of, validated the opinion I already had. Yeh I regretted it pretty quickly to be honest, even before the major illness, when I started to have all the minor sniffles, and just catching too many colds too quickly. I wised up to it very quickly but it was the major illness that made me really think okay that’s it, from now on I’m definitely getting all the flu jabs no questions asked. (FD)
She associates the minor illnesses with not having the influenza vaccine, in a similar way to a lay-person. Her lived experience changed her intentions regarding vaccination over time, through the intervention of multiple actors. Despite this, even following a major illness (suspected influenza), she still did not get the vaccine:
Actually began to properly worry for my health but I didn’t then act on it.
This participant was concerned for her own health, suggesting that at this point, she had clear intentions to vaccinate. When asked why she did not act, she was unable to justify failing to fulfill her plans:
I think that you have to go to occupational health or something, I don’t know where occupational health is to be honest. So yeah . . . it’s just a bit more difficult to get the jab . . .
Following her experience of illness, this participant intended to get an influenza vaccine; however, her intent did not translate into action. Discrepancies between intentions and actions are commonplace, because the relation of intent to the actual course of situated action is enormously contingent upon unforeseen events (Suchman, 1987). Rarely, when forming an intention, do we take into account all of the specific factors involved. Her intention to vaccinate was formed without consideration of the practicalities involved with vaccinating. The resultant inconvenience associated with finding occupational health then outweighed her intention to vaccinate at the specific moment in time when the decision was made.
Convenience
A disjointed understanding of the vaccine, combined with a fluid socialization process, suggests that the outcome of a vaccination decision is variable. However, it emerged that convenience appears to circumvent the complex interactions of socialization and understanding of the vaccine. This principle held despite negative perceptions of the vaccine:
“I had another flu vaccine, it made my arm hurt again, so definitely not having it next year, and then next year somebody would walk in and be like you should have a flu vaccine, I’ll do it right now, and I’d probably have it then,” so I think it’s more just a convenience thing than anything. (FD)
Although being provided with a convenient opportunity does not alter opinions of the vaccination, many will accept the vaccination without having a strong justification for it. Likewise, when participants were asked why they had not vaccinated, many did not have strongly negative views. Indeed, the act of briefly discussing their thoughts on the influenza vaccine allowed some to re-evaluate their views and found they could not justify their lack of vaccination. This is a good example of how interviews do not simply record views impartially. They are instrumental in the construction of views (Holstein & Gubrium, 2004).
Convenience is important as it manifests a common circumstance that is relevant to the vaccination decision. Some foundation doctors reported vaccinating so that they could allow colleagues to get their intramuscular injection skill signed off in their logbooks. This gave the participants a convenient incentive to vaccinate as they could practice giving the intramuscular injection:
Another thing that actually made me want to get the jab is, this really silly ok, but erm the foundations doctors need to get skills signed off, and one of them is an intramuscular injection. So actually it was perfect timing that me and alongside a whole other load of doctors, we just took it in turn, stabbing each other, so that we could get our procedure signed off as well. (FD)
This assessment of competency was a powerful enough incentive to “tip the balance” in favor of vaccination. The importance of proving one’s competency in performing the intramuscular injection is institutionally established. Combining the influenza vaccination with this is a subtly powerful social construction, which embeds vaccination within a medical task. Participants are more concerned with the procedure rather than the vaccine. The beauty of this is that peer pressure combines with convenience at the specific point of action in which the vaccination decision is made.
The convenience theme could be advantageous or detrimental to vaccination campaigns—slight inconvenience, for example, not knowing the location of occupational health, as we have seen above, would prevent participants from having the vaccine. However, improving convenience may increase vaccine uptake without the necessity for altering attitudes. Below, a vaccinated medical student discusses the importance of convenience:
Ermm for me it’s about convenience, like I probably wouldn’t go out of my way to get the flu vaccine, I wouldn’t book an appointment to the doctors cos I don’t have time really. Erm the only reason I’ve had it the past 2 years was because “cut three lines of descriptive text” it’s just easy to do it . . . (MS)
Many of the themes discussed in this study have variable and conflicting effects on the individual’s vaccination decision, which creates ambivalence toward the vaccine and leads to a finely balanced decision. Often, convenience emerged as the decisive factor which circumvents the complex interactions of socialization and understanding of the vaccine and “tipped the balance” of the vaccination decision.
Conclusion
Our research explored cognitive and social elements to the uptake of the influenza vaccine in this population of early career doctors and senior medical students. Our research innovatively takes a sociological approach to understanding the poor uptake of the seasonal influenza vaccine. Where most research on vaccination takes a psychological perspective, positioning decision making as a cognitive activity, we position vaccination as a fundamentally social activity and elucidate the processes through which vaccination does or does not occur. Results are drawn from a small but diverse sample (participants were exploring a range of clinical specialties on rotation), and the themes derived are supported by the literature. Participants’ attitudes toward the influenza vaccine were influenced by their social environment. An indifferent attitude was prevalent and thus became a tacitly accepted element of health care culture. The effects of medical socialization were attenuated by participants’ understanding of the vaccine—which was often formed from many conflicting factors: previous experiences, role models, and unclear risks and benefits of vaccination. This combination allowed convenience to be a critical element of vaccination uptake. The themes described above create an ebb and flow of factors toward and away from vaccination; this led to an overarching context of ambivalence within which vaccination decisions were made. Crucially, there often seemed to be considerable disparity between an individual’s opinion of the vaccine, their intentions, and their vaccination status.
On this basis, we suggest a number of recommendations for improving influenza vaccination uptake. Senior staff members (particularly those in acute medical specialties, for example, respiratory medicine) are ideally situated to exploit their potential influence as positive role models and should be encouraged to do so by engaging their junior colleagues around the topic of vaccination. There should be a more targeted approach to raising awareness in areas with the most vulnerable patients—in our study, many participants were unaware of the benefits of their vaccination for elderly patients, pediatric patients, and those with underlying health concerns. Policymakers could sway the feelings of vaccination indifference toward a more receptive view by associating vaccination with professionalism. Scenarios such as the vaccination appearing in the student’s logbooks and its facilitation of the intramuscular injection are indicative of successfully increasing uptake by positioning vaccination as a convenient exercise to demonstrate one’s professionalism, without having to overcome negative evaluations of the vaccine. These recommendations demonstrate the value of a sociological perspective in shifting the conceptualization of vaccination from one of individual behavior to one of professional culture.
This work has begun to fill the gap in our understanding of seasonal influenza vaccination by early career doctors, and we hope that future work in this area goes further to give a deeper insight into the influenza vaccination practices of other actors within the hospital setting. Convenience has been noted elsewhere and is likely to apply widely, not just to health care professionals. Socialization and the influence of role models is likely to be important in other health care professions although whether it results in indifference will depend on the extent to which those professions share the characteristics of medical training and practice. The study sample from which findings were drawn is small and potentially open to the criticism of a lack of geographic representativeness. However, we believe the analysis in this study demonstrates the strength of the qualitative method for showing more nuanced and novel solutions to the persistent challenge of increasing rates of HCW influenza vaccination.
Supplementary Material
Author Biographies
Rhiannon Edge was a PhD student in Statistics and Epidemiology at the time of conducting this research and is now a Senior Research Associate at Lancaster Medical School. Her research interests include multi-disciplinary approaches to understanding public health.
Dawn Goodwin is a senior lecturer in social sciences at Lancaster University. Her research interests focus on cultures of healthcare work and issues of learning, knowledge and practice. Recent journal articles include ‘The social life of the dead: the role of post-mortem examinations in medical student socialisation’ (Social Science and Medicine, 2016, 161:100–108), and ‘Decision-making and accountability: differences in distribution’ (Sociology of Health and Illness, 2014, 36 (1):44–59).
Rachel Isba is Head of Lancaster Medical School and an NHS Consultant in Paediatric Public Health Medicine.
Thomas Keegan is a Lecturer in Epidemiology at Lancaster Medical School.
Footnotes
Authors’ Note: The full datasets generated during and/or analyzed during the current study are not publicly available to protect participant’s confidentiality but are available from the corresponding author on reasonable request, and ethical approval. Each participant gave their consent for publication by signing a consent form endorsed by Lancaster University Ethics committee (see supplementary); their data have been made anonymous by using identifier codes or pseudonames (where participants talked about people not involved in the study). Ethical approval was obtained from Lancaster University Research Ethics Committee prior to data collection. Participants gave informed consent prior to data collection.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by The Colt Foundation.
Supplemental Material: The online supplemental Table 1 is available at http://qhr.sagepub.com/supplemental
References
- Aronfreed J. (1968). The concept of internalization. In Conduct and conscience (pp. 15–42). Academic Press; Retrieved from http://www.sciencedirect.com/science/article/pii/B9781483198958500066 [Google Scholar]
- Baldwin P. J., Dodd M., Wrate R. M. (1997). Young doctors’ health—II. Health and health behaviour. Social Science & Medicine, 45, 41–44. doi: 10.1016/S0277-9536(96)00307-3 [DOI] [PubMed] [Google Scholar]
- Becker H. S. (1977). Boys in White: Student culture in medical school. New Brunswick, NJ: Transaction Books. [Google Scholar]
- Blank P. R., Bonnelye G., Ducastel A., Szucs T. D. (2012). Attitudes of the general public and general practitioners in five countries towards pandemic and seasonal influenza vaccines during season 2009/2010. PLoS ONE, 7(10), e45450. doi: 10.1371/journal.pone.0045450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BMJ Careers. (2013). When doctors need treatment: An anthropological approach to why doctors make bad patients. Retrieved from http://careers.bmj.com/careers/advice/view-article.html?id=20015402
- Bosk C. L. (2003). Forgive and remember: Managing medical failure (2nd ed.). Chicago: The University of Chicago Press. [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Burls A., Jordan R., Barton P., Olowokure B., Wake B., Albon E., Hawker J. (2006). Vaccinating healthcare workers against influenza to protect the vulnerable—Is it a good use of healthcare resources? A systematic review of the evidence and an economic evaluation. Vaccine, 24, 4212–4221. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (n.d.). Selecting viruses for the seasonal influenza vaccine. Retrieved from http://www.cdc.gov/flu/about/season/vaccine-selection.htm
- Cicourel A. V. (1990). Intellectual teamwork. In Galegher J., Kraut R. E., Egido C. (Eds.). (pp. 221–242). Hillsdale, NJ: Lawrence Erlbaum; Retrieved from http://dl.acm.org/citation.cfm?id=117848.117857 [Google Scholar]
- General Medical Council. (2013). Good practice guidelines. Retrieved from http://www.gmc-uk.org/guidance/good_medical_practice/contents.asp
- GOV.UK. (n.d.). Chief medical officer and chief pharmaceutical officer: Advice on using antiviral medicines: Influenza season 2014 to 2015. Retrieved from https://www.gov.uk/government/publications/advice-on-using-antiviral-medicines/advice-on-using-antiviral-medicines-influenza-season-2014-to-2015
- Cruess R. L., Cruess S. R., Steinert Y. (Eds.). (2001). Teaching medical professionalism. Cambridge, UK: Cambridge University Press; Retrieved from http://ebooks.cambridge.org/ref/id/CBO9780511547348 [Google Scholar]
- Hafferty F. W. (1991). Into the valley: Death and the socialization of medical students. New Haven, CT: Yale University Press. [Google Scholar]
- Helms C. M., Polgreen P. M. (2008). Should influenza immunisation be mandatory for healthcare workers? Yes. British Medical Journal, 337, Article a2142. doi: 10.1136/bmj.a2142 [DOI] [PubMed] [Google Scholar]
- Hodges B. H., Geyer A. L. (2006). A nonconformist account of the Asch experiments: Values, pragmatics, and moral dilemmas. Personality and Social Psychology Review, 10, 2–19. doi: 10.1207/s15327957pspr1001_1 [DOI] [PubMed] [Google Scholar]
- Hofmann F., Ferracin C., Marsh G., Dumas R. (2006). Influenza vaccination of healthcare workers: A literature review of attitudes and beliefs. Infection, 34, 142–147. [DOI] [PubMed] [Google Scholar]
- Hollmeyer H. G., Hayden F., Poland G., Buchholz U. (2009). Influenza vaccination of health care workers in hospitals-A review of studies on attitudes and predictors. Vaccine, 27, 3935–3944. doi: 10.1016/j.vaccine.2009.03.056 [DOI] [PubMed] [Google Scholar]
- Holstein J. A., Gubrium J. F. (2004). The active interview. Qualitative Research: Theory, Method and Practice, 2, 140–161. [Google Scholar]
- Isaacs D., Leask J. (2008). Should influenza immunisation be mandatory for healthcare workers? No. British Medical Journal, 337, Article a2140. doi: 10.1136/bmj.a2140 [DOI] [PubMed] [Google Scholar]
- Ives J., Greenfield S., Parry J. M., Draper H., Gratus C., Petts J. I., . . . Wilson S. (2009). Healthcare workers’ attitudes to working during pandemic influenza: A qualitative study. BMC Public Health, 9, Article 56. doi: 10.1186/1471-2458-9-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R. (2007). When doctors become patients. Oxford, UK: Oxford University Press. [Google Scholar]
- Leming M. R., Dickenson G. E. (2015). Understanding Dying, Death, and Bereavement. Centage Learning, 147. [Google Scholar]
- Monrouxe L. V. (2010). Identity, identification and medical education: Why should we care? Medical Education, 44, 40–49. doi: 10.1111/j.1365-2923.2009.03440.x [DOI] [PubMed] [Google Scholar]
- Morse J. M. (2004). Theoretical saturation. In Lewis-Beck M., Bryman A., Liao T. (Eds.), Encyclopedia of social science research methods. Sage. Retrieved from http://sk.sagepub.com/reference/socialscience/n1011.xml
- NHS England 2016/17 CQUIN. (2016). Retrieved from https://www.england.nhs.uk/wp-content/uploads/2016/03/HWB-CQUIN-Guidance.pdf
- Pratt M. G., Rockmann K. W., Kaufmann J. B. (2006). Constructing professional identity: The role of work and identity learning cycles in the customization of identity among medical residents. Academy of Management Journal, 49, 235–262. doi: 10.5465/AMJ.2006.20786060 [DOI] [Google Scholar]
- Public Health England. (n.d.). Seasonal flu vaccine uptake in healthcare workers in England: Winter season 2015 to 2016. GOV.UK; Retrieved from https://www.gov.uk/government/statistics/seasonal-flu-vaccine-uptake-in-healthcare-workers-in-england-winter-season-2015-to-2016 [Google Scholar]
- Rashid H., Yin J. K., Ward K., King C., Seale H., Booy R. (2016). Assessing interventions to improve influenza vaccine uptake among health care workers. Health Affairs, 35, 284–292. doi: 10.1377/hlthaff.2015.1087 [DOI] [PubMed] [Google Scholar]
- Smedley J., Poole J., Waclawski E., Stevens A., Harrison J., Watson J., . . . Coggon D. (2007). Influenza immunisation: Attitudes and beliefs of UK healthcare workers. Occupational and Environmental Medicine, 64, 223–227. doi: 10.1136/oem.2005.023564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J., Wilks M., Wells B., Marshall J. (1998). Missed problems and missed opportunities for addicted doctors. British Medical Journal, 316(7129), 405–406. doi: 10.1136/bmj.316.7129.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman L. A. (1987). Plans and situated actions: The problem of human-machine communication. New York: Cambridge University Press. [Google Scholar]
- Thompson W. T., Cupples M. E., Sibbett C. H., Skan D. I., Bradley T. (2001). Challenge of culture, conscience, and contract to general practitioners’ care of their own health: Qualitative study. British Medical Journal, 323(7315), 728–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilburt J. C., Mueller P. S., Ottenberg A. L., Poland G. A., Koenig B. A. (2008). Facing the challenges of influenza in healthcare settings: The ethical rationale for mandatory seasonal influenza vaccination and its implications for future pandemics. Vaccine, 26(Suppl. 4), D27–D30. doi: 10.1016/j.vaccine.2008.07.068 [DOI] [PubMed] [Google Scholar]
- Toulis N., Sinclair S. (1997). Making doctors: An institutional apprenticeship (1st ed.). Oxford, UK: Bloomsbury Academic. [Google Scholar]
- Tricco A. C., Chit A., Soobiah C., Hallett D., Meier G., Chen M. H., . . . Loeb M. (2013). Comparing influenza vaccine efficacy against mismatched and matched strains: A systematic review and meta-analysis. BMC Medicine, 11(1), Article 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2014). Influenza: Fact sheet. Retrieved from http://www.who.int/mediacentre/factsheets/fs211/en/
- Wright S., Wong A., Newill C. (1997). The impact of role models on medical students. Journal of General Internal Medicine, 12, 53–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.