Abstract
Mullerian anomalies cause a significant impact on the reproductive outcomes. A bicornuate uterus is a type of lateral fusion defect, which constitutes 26% of all uterine anomalies. Strassmann’s metroplasty is a unification procedure performed to correct the two smaller uterine cavities into a more spacious single cavity. Improved reproductive performance was reported after unification metroplasty. Laparoscopic route can be adopted for this procedure with all the advantages of minimally invasive surgery. Here, we report a success story of a woman who suffered with six miscarriages and secondary infertility who underwent laparoscopic Strassmann’s metroplasty in a tertiary care center and later delivered a baby by caesarean section.
KEYWORDS: Bicornuate uterus, laparoscopy, minimally invasive surgery, Strassmann’s, metroplasty, uterus unification
INTRODUCTION
A bicornuate uterus is a type of lateral fusion defect constituting approximately 26% of all uterine anomalies.[1] In bicornuate uteri, the mean abortion, preterm delivery, term delivery, and live birth rates were 36, 23, 40.6, and 55.2%, respectively.[1] Strassmann’s abdominal metroplasty is a unification procedure, correcting the underlying defect of two uterine cornua in a bicornuate uterus, making it a single uterine cavity.[2] Postoperative fetal salvage rate up to 100% after the corrective surgery was reported.[3] Laparoscopic route is a feasible and better alternative to abdominal metroplasty. The laparoscopic route provides better magnification, lower tissue drying, reduced infections, lesser adhesions, shorter hospital stay, and quicker recovery. Here, we report a successful reproductive outcome after laparoscopic Strassmann’s metroplasty from a tertiary care center.
CASE HISTORY
A 25-year-old female presented to the outpatient department of obstetrics and gynecology in a tertiary care center with a history of six spontaneous first trimester abortions (2–2½ months) and inability to conceive since 1 year. She had regular cycles and her BMI was 22 kg/m2. Her TSH and prolactin levels were in normal limits. Acquired thrombophilia workup was negative. Hysterosalpingogram was suggestive of a septate uterus with bilateral peritoneal spill.
Diagnostic laparohysteroscopy was performed in anticipation of septate uterus but intraoperatively a bicornuate uterus with recto-vesical (RV) band of peritoneum was diagnosed. Later, she was posted for laparoscopic Strassmann’s metroplasty.
The patient was placed in Lloyd-Davies position after general anesthesia with endotracheal intubation. A central 12 mm umbilical trocar was inserted after pneumoperitoneum with Veress needle. Two left lateral (surgeon) and one right lateral (assistant) trocars were inserted. Pelvic anatomy revealed a partial bicornuate uterus with RV band of peritoneum between hemi corpora [Figure 1] with normal fallopian tubes and ovaries. The band was cut using harmonic shears. The bladder and rectal integrity was checked. The uterine horns were manipulated and stabilized vaginally using Hegar’s dilators one for each horn. The uterovesical fold of peritoneum was opened and the bladder pushed down. Dilute vasopressin solution (20 units in 100 ml dilution) was injected into the medial side of both the uterine horns, with end point being the pale white colour of the uterine horns. Using harmonic hook blade, a full thickness, serosa to endometrium, incision is given on the medial aspect of both the horns, extended caudally till the base of the horn and cranially 2 cm short of the fallopian tube insertion. By 1-0 V-LOC barbed suture, the closure of opposing myometrial edges was performed in two-layer continuous fashion excluding the endometrium and avoiding dead space in myometrium. Uterine serosa was closed with continuous 2-0 vicryl suture. The uterovesical fold of peritoneum was closed by continuous 2-0 vicryl. Hemostasis was ensured. Blood loss was approximately 50 ml and operating time 150 min. A 14French foley catheter was inserted into uterine cavity and kept for 72 h postoperatively.
Figure 1.
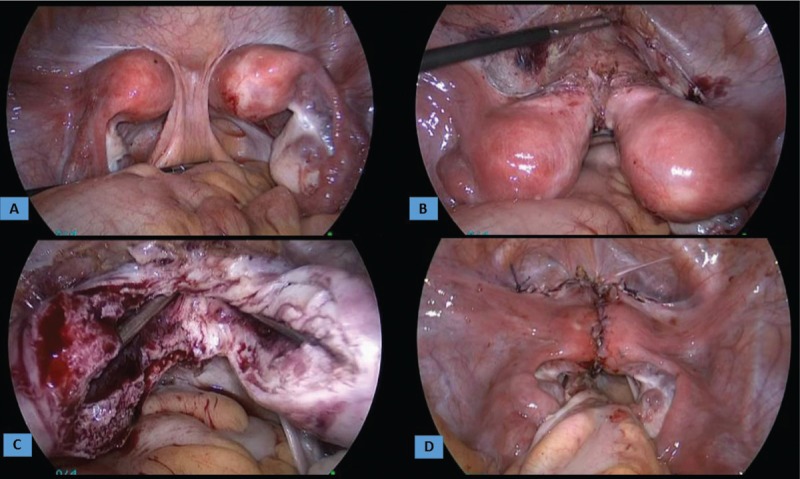
Laparoscopic view during Strassmann’s metroplasty: (A) Bicornuate uterus with recto-vesical (RV) band; (B) dissected RV band and uterovesical fold; (C) incised medial side of cornua by harmonic scalpel and cornua supported with Hegar’s dilators; (D) end result of unification after suturing with V-LOC and vicryl
She was advised to avoid conception for 6 months. Then, she tried for spontaneous conception for 6 months but it did not result in pregnancy. Later, 50 mg clomiphene citrate was given and she conceived in that very first cycle of ovulation induction.
She was under regular antenatal follow-up with micronized progesterone tablet twice daily and folic acid. Her NT-NB scan was normal, and dual marker screen was low risk. McDonald’s cervical cerclage was applied prophylactically at 14+1 gestation when her cervical length was 2.5 cm and internal os was opened 1 cm. Weekly 250 mg 17-alpha hydroxyl progesterone caproate was started which was continued till her delivery. Regular antenatal visits were continued and the antenatal investigations were within normal limits. At 32 weeks, she was admitted for antenatal steroid coverage and for the workup of morbidly adherent placenta.
Her MRI was suggestive of a right anterolateral placenta with predominantly fundal uterine contour bulge with focal areas of myometrial thinning, and on ultrasound Doppler, there was gap of retroplacental blood flow with loss of clear space. There was no heterogeneity or intraplacental bleed. The possibility of focal invasion of myometrium at scar site was noted.
In view of the above findings and patient’s choice, at 35 completed weeks’ gestation, elective caesarean section [Figure 2] was planned with written consent regarding the need and risks of caesarean hysterectomy. The abdomen was opened by a vertical midline infraumbilical incision. The uterine external contour was well maintained with no focal thinning or placental invasion. Adhesions were present between rectosigmoid and posterior uterine wall. The fetus in transverse lie delivered by breech extraction through a lower segment transverse incision. A healthy male baby weighing 2162 g was born with APGAR of 7/8/10. The previous scar line inside the uterus was reinforced with 1-0 vicryl. The uterine incision was closed with 1-0 vicryl in two layers. The routine procedure of abdominal closure was performed and cerclage removed vaginally. The patient was discharged on the 5th postoperative day. At 1-month follow-up, both mother and her baby were fine.
Figure 2.
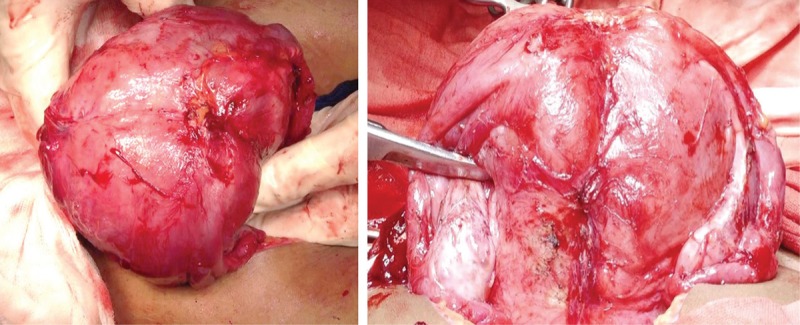
View during caesarean section after delivery of fetus: Left (superior view); right (posterior view)
DISCUSSION
The uterine malformations occur due to disturbances in the formation, development, interaction, fusion, or absorption of the mullerian ducts. A systematic review comprising 94 observational studies (89,861 women) has shown a prevalence of uterine anomalies as 5.5% [95% confidence interval (CI), 3.5–8.5] in the unselected population, 8.0% (95% CI, 5.3–12) in infertile women, 13.3% (95% CI, 8.9–20.0) in those with a history of miscarriage, and 24.5% (95% CI, 18.3–32.8) in those with a miscarriage and infertility. The arcuate uterus was most common in the unselected population (3.9%; 95% CI, 2.1–7.1) and the septate uterus was most common in women with miscarriage and infertility (15.4%; 95% CI, 12.5–19).[4]
Strassmann metroplasty for bicornuate uteri shows a good evidence of improvement in live birth rates from 3.7 to 80–100%.[3,5] In 2005, Lolis et al. achieved 88% pregnancies and 100% take-home baby rate, concluding that reproductive capacity of women with bicornuate uterus was very good postsurgery and the procedure was reserved for selected women who had history of recurrent abortion or preterm birth.[6]
In 2006, metroplasty performed by laparoscopic route was reported to be a safe and successful surgical option.[7] Following this, a series of other case reports had shown a good restoration of uterine anatomy, uniform cavity creation with good scar integrity, minimal adhesions, less blood loss, and shorter hospital stay.[8,9] An observational study, largest of its kind, that included women with double uterine cavities (bicornuate or didelphys) with a history of recurrent pregnancy loss evaluated the feasibility of laparoscopic metroplasty. Of 14 patients, 12 had conception, nine going till full term ending in caesarean section with normal pregnancy outcomes. None had rupture uterus. So laparoscopic metroplasty can be a substitute for laparotomy.[9]
To evaluate the existence of RV peritoneal band in women with a didelphic or bicornuate uterus, diagnostic laparoscopy or laparotomy to visualize the pelvic cavity had shown the existence of the band in 60% of women with bicornuate uteri.[10] The structure, due to its relation to uterine malformations, may have some share in early development of urogenital system. Similarly, in our case, we have observed RV band in a partial bicornuate uterus.
Full thickness incision over the uterus including the endometrium increases the chances of postoperative intrauterine adhesions potentially impairing fertility. After conception, these women are at an increased risk of placenta previa, morbidly adherent placenta, antenatal uterine rupture, and may land up in hysterectomy. Regular antenatal care, good obstetric ultrasound, and MRI may be needed for the evaluation of adherent placenta which was anticipated in our case.
With inherent advantages of minimally invasive surgery, laparoscopic Strassmann metroplasty is a feasible alternative to laparotomy, but the procedure requires an advanced laparoscopic surgeon with proper anatomical knowledge and good suturing skills.
CONCLUSION
The birth of a healthy baby is the ultimate goal of any fertility enhancing surgery. Recurrent miscarriages have a significant impact on the psychological, physical, and financial aspects of a couple. Strassmann’s metroplasty by laparoscopic route is a safe and effective approach in women with a bicornuate uterus suffering with recurrent miscarriages.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank the patient and her husband for consenting to publish this case report.
REFERENCES
- 1.Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001;7:161–74. doi: 10.1093/humupd/7.2.161. [DOI] [PubMed] [Google Scholar]
- 2.Strassmann EO. Fertility and unification of double uterus. Fertil Steril. 1966;17:165–76. doi: 10.1016/s0015-0282(16)35882-4. [DOI] [PubMed] [Google Scholar]
- 3.Capraro VJ, Chuang JT, Randall CL. Improved fetal salvage after metroplasty. Obstet Gynecol. 1968;31:97–103. doi: 10.1097/00006250-196801000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: A systematic review. Hum Reprod Update. 2011;17:761–71. doi: 10.1093/humupd/dmr028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rock JA, Jones HW. The clinical management of the double uterus. Fertil Steril. 1977;28:798–806. [PubMed] [Google Scholar]
- 6.Lolis DE, Paschopoulos M, Makrydimas G, Zikopoulos K, Sotiriadis A, Paraskevaidis E. Reproductive outcome after Strassmann metroplasty in women with a bicornuate uterus. J Reprod Med. 2005;50:297–301. [PubMed] [Google Scholar]
- 7.Sinha R, Mahajan C, Hedge A, Shukla A. Laparoscopic metroplasty for bicornuate uterus. J Minim Invasive Gynecol. 2006;13:70–3. doi: 10.1016/j.jmig.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Pisat S, Tas B, van Herendael B. Laparoscopic Strassmann’s metroplasty for bicornuate uterus. Gynecol Surg. 2009;6:153–8. [Google Scholar]
- 9.Alborzi S, Asefjah H, Amini M, Vafaei H, Madadi G, Chubak N, et al. Laparoscopic metroplasty in bicornuate and dideplhic uteri: Feasibility and outcome. Arch Gynecol Obstet. 2015;291:1167–71. doi: 10.1007/s00404-014-3520-1. [DOI] [PubMed] [Google Scholar]
- 10.Heinonen PK. Rectovesical ligament and fusion defect of the uterus with or without obstructed hemivagina and ipsilateral renal agenesis. Eur J Obstet Gynecol Reprod Biol. 2013;168:83–6. doi: 10.1016/j.ejogrb.2012.12.034. [DOI] [PubMed] [Google Scholar]


