Abstract
Objectives
Each year millions of children suffer from unintentional injuries resulting in poor emotional and physical health. This study examined selected bio-psycho-social factors (child heart rate, peri-trauma appraisals, early coping, trauma history) to elucidate their roles in promoting emotional recovery following injury. The study evaluated specific hypotheses that threat appraisals (global and trauma-specific) and coping would predict subsequent posttraumatic stress symptoms (PTSS), that coping would mediate the association between early and later PTSS, and that heart rate would predict PTSS and appraisals would mediate this association.
Method
96 children hospitalized for injury participated in assessments at T1 (within two weeks of injury), T2 (6-week follow-up), and T3 (12-week follow-up). Participants completed measures of trauma history and appraisals at T1, coping at T2, and PTSS at T1, T2, and T3. Heart rate was abstracted from medical records. Structural equation modeling was employed to evaluate study hypotheses.
Results
Heart rate was not associated with PTSS or appraisals. Models including trauma history, appraisals, coping, and PTSS were constructed to test other study hypotheses and fit the data well. T1 global and trauma-specific threat appraisals were associated with T1 PTSS; T2 avoidant coping was a significant mediator of the relation between T1 and T3 PTSS.
Conclusions
Findings confirm a role for appraisals and coping in the development of PTSS over the weeks following pediatric injury. Early appraisals and avoidant coping may be appropriate targets for early preventive interventions. Future research should further explicate the utility of a bio-psycho-social framework in predicting PTSS.
Keywords: bio-psycho-social model, appraisals, coping, injury, posttraumatic stress, children
Acute pediatric injuries are among the most common potentially traumatic experiences for children; approximately 30 million children are injured each year in the United States alone (Centers for Disease Control and Prevention, 2014). Following injury, children may experience challenges such as decreased quality of life and symptoms of depression (Kassam-Adams, Bakker, Marsac, Fein, Winston, 2015; Landolt, Vollrath, Gnehm, & Sennhauser, 2009). Further, 10–30% of children with injury have symptoms of posttraumatic stress disorder (PTSS; re-experiencing, avoidance, arousal) up to one year later (De Young, Kenardy, Cobham, & Kimble, 2012; Kassam-Adams, Marsac, Hildenbrand, & Winston, 2013). The high prevalence and impact of PTSS for children with injury necessitates research to understand the development of PTSS and inform preventive interventions.
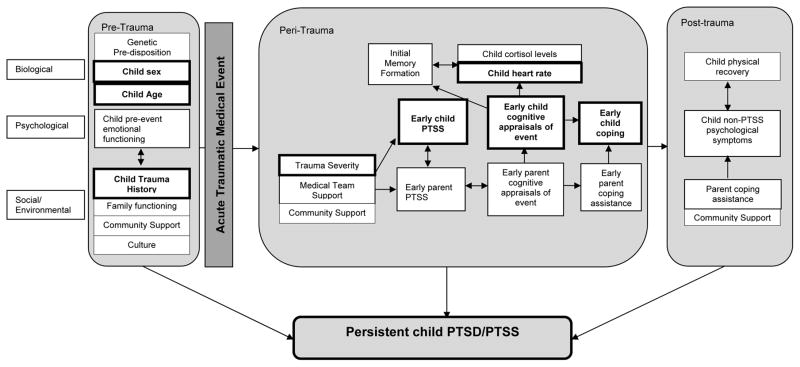
Biological, psychological, and environmental risk factors associated with the development of PTSS in children with injuries may occur pre-, peri-, or post-trauma (Kazak et al., 2007). See Figure 1 for an overview of selected bio-psycho-social factors across these time periods. Focusing on biological factors potentially associated with PTSS, Schwartz and Perry (1994) have suggested that physiological symptoms maintain hyper-arousal and influence the formation of memories. Hence, when a child encounters an acute potentially traumatic event such as an injury, his or her body systems activate the fight-or-flight response. Heart rate can serve as a proxy of this response. Heart rate within the first 24 hours of hospital admission has predicted PTSS up to six months post-injury even after controlling for age, sex, and injury severity (De Young, Kenardy, & Spence, 2007; Kassam-Adams, Garcia-España, Fein, & Winston, 2005; Nugent, Christopher, & Delahanty, 2006a,b). It may be that initial sympathetic hyperarousal in response to the trauma results in in a stronger physiological response (e.g., heart rate) when an individual appraises a situation as more stressful and that this appraisals affects memory formation (Olff, Langeland, & Gersons, 2005; Schwartz & Perry, 1994).
Figure 1.
Theoretical model for the development of child PTSD/PTSS following acute medical trauma*
*This figure is modified from the original to show the focused variables in this study. Specifically, variables included in this study are indicated in bold. The original figure can be found at the following: Marsac, M. L., Kassam-Adams, N., Delahanty, D. L., K, F. W., & Barakat, L. P. (2014). Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clinical child and family psychology review, 17(4), 399–411. doi: 10.1007/s10567-014-0174-2.
Regarding psychological variables, research and theory suggest early threat appraisals and coping behaviors serve as mechanisms in the development of PTSS in children following injury (Ehlers & Clark, 2000; Marsac, Kassam-Adams, Delahanty, Widaman, & Barakat, 2014; Marsac, et al., 2016; Meiser-Stedman, 2002). PTSS severity has been associated with children’s perception of threat during the traumatic event, global negative appraisals about vulnerability to future harm, and negative interpretation of PTSS symptoms (Ehlers, Mayou, & Bryant, 2003; Marsac, et al., 2016; Stallard & Smith, 2007). Studies to date have varied in whether they assess children’s global appraisals (i.e. general appraisals of self and the world) versus trauma-specific appraisals (Marsac, et al., 2016; Meiser-Stedman, Dalgleish, Glucksman, Yule, & Smith, 2009; Stallard & Smith, 2007), and this variation may be important in interpreting results: If global appraisals affect a child’s recovery from exposure to a trauma, universal screening during routine health care could help identify children to participate in a primary prevention program (i.e., work to re-shape global appraisals without requiring exposure to trauma) whereas if trauma-specific appraisals are the best predictors of PTSS, early secondary prevention programs post-trauma exposure may be a better resource. Assessing global and trauma-specific appraisals within the same study could help to clarify the relationship between appraisals and PTSS.
A child’s amount and type of coping post-injury also appear to be related to PTSS risk: more coping overall is consistently related to prior, concurrent, and subsequent PTSS (Landolt, Vollrath, & Ribi, 2002; Marsac, Donlon, Hildenbrand, Winston, & Kassam-Adams, 2014; Stallard, Velleman, Langsford, & Baldwin, 2001; Zehnder, Prchal, Vollrath, & Landolt, 2006). Roth and Cohen’s (1986) approach- versus avoidance-oriented coping classification system is well-validated (Aldridge & Roesch, 2007). Approach-oriented coping (e.g., cognitive restructuring, seeking social support) involves behaviors directed towards managing a stressor or its associated emotions, while avoidance-oriented strategies are those intended to distance an individual from a stressor or related emotions (Roth & Cohen, 1986). Specific to pediatric injury avoidant coping has demonstrated relationships with PTSS post-pediatric injury. Higher amounts of avoidant coping are related to more PTSS (Stallard, et al., 2001; Marsac, et al., 2014; Marsac et al., 2016). The roles of approach-oriented coping strategies (e.g., cognitive restructuring, seeking social support) are less clear (e.g., Marsac et al., 2016).
Research to date has most often examined appraisals and coping separately as potential mechanisms in child PTSS development and has most often assessed appraisals or coping concurrently with PTSS, which precludes examination of these variables together over time with PTSS. Only two studies examined the relative associations of cognitive appraisals and coping with PTSD symptoms in children with injury. Stallard and Smith (2007) found that appraisals and coping together accounted for 64% of the variance in concurrent PTSD symptoms eight months after injury. Marsac et al. (2016) assessed appraisals and coping in the peri-trauma period and PTSS six to twelve months later, finding that escape coping (a type of avoidant coping) served as a mediator in the relationship between peri-trauma negative appraisals and subsequent PTSS. However, the evidence so far is not clear how appraisals and coping strategies work together potentially contribute to or prevent PTSS over time (e.g., Do more severe PTSS result in more coping attempts or a different type of coping? Can certain coping strategies prevent PTSS? What is the relationship between appraisals and PTSS over time?). Given that cognitive-behavioral theories of PTSS development suggest that adaptive post-trauma recovery involves creative adaptive appraisals of the event and behaviors that promote safe approaches to the trauma stimuli, a better understanding of these processes may be helpful (Ehlers & Clark, 2000).
Environmental factors that have the potential to influence PTSS have been highlighted by Kazak’s (2006) application of the Pediatric Psychosocial Preventative Health Model (PPPHM) suggesting a bi-directional influence between a child’s health and their social systems (e.g., medical, school, and family systems). Two variables that reflect part of a child’s environment that have shown small predictive validity for child PTSS are trauma history and severity of trauma exposure (Alisic, et al., 2011; Trickey, et al., 2014). However, while these factors (and other environmental factors) may play a role, the child’s perception of their life events and potentially traumatic event may be of more importance. Further research is needed to better examine these relationships.
The current study sought to examine the contributions of selected pre-, peri-, and post-trauma biological (i.e., heart rate, child sex, child age), psychological (i.e., appraisals, coping), and environmental (i.e., trauma history, trauma severity) factors in predicting PTSS over time. This study had two primary objectives. The first was to examine the roles of children’s peri-trauma global and trauma-specific (injury-related) appraisals and early post-trauma coping in predicting subsequent child PTSS. We hypothesized that children’s threat appraisals during the peri-trauma period would predict subsequent child PTSS (H1), that children using cognitive restructuring and support-seeking coping would have fewer PTSS while children using avoidance coping would have more T3 PTSS (H2), and that coping would serve as a mediator between T1 PTSS and T3 PTSS (H3). The second objective was to elucidate the contribution of peri-trauma biological responses (i.e., heart rate) to peri-trauma cognitive appraisals and post-trauma PTSS. We hypothesized that heart rate (earliest available) would predict post-trauma child PTSS (H4), and that cognitive appraisals would serve as a mediator between heart rate and post-trauma child PTSS (H5). Finally, we explored the relationships of two environmental factors in predicting child PTSS: trauma history and injury severity. See Figure 1 for the overarching conceptual theoretical model, highlighting variables assessed in the current study.
Method
The current analyses are part of a larger study examining child-parent interaction and child recovery following acute injury. Procedures for this larger study included a video-recorded parent-child interaction task and a series of child and parent self-report measures. Study data was collected prospectively, over three time points, allowing us to examine how appraisals and coping may predict PTSS over time.
Participants
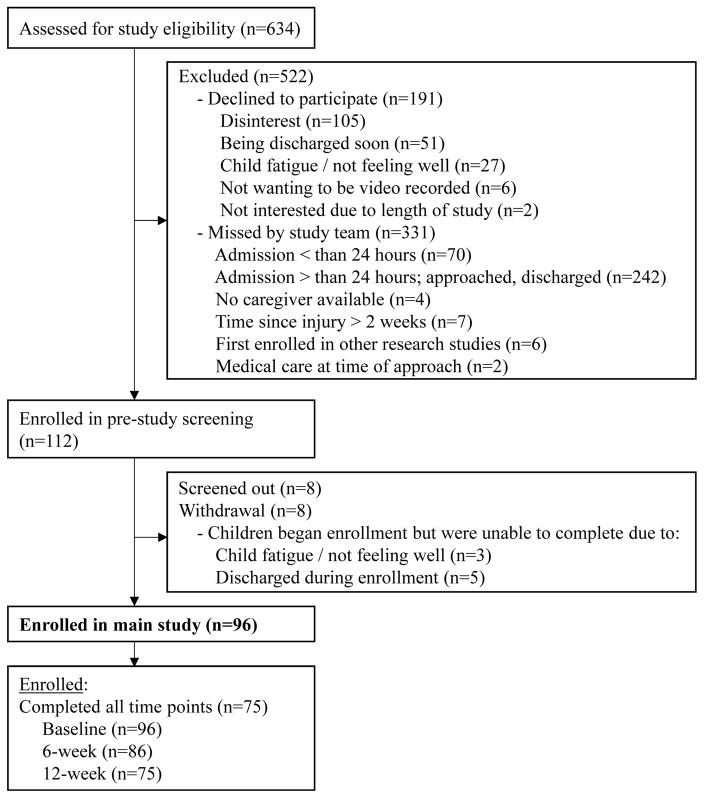
The study sample consisted of 96 children (62 male) aged 8 to 13 years (M = 10.6, SD = 1.7) who were hospitalized for treatment of an injury. Children were eligible for inclusion if they were injured within the past two weeks, had sufficient mastery of English to complete study measures, and perceived the injury event as potentially traumatic via a screener. Children were excluded from participation if their current medical condition or cognitive limitations would not allow completion of study tasks, their Glasgow Coma Score was less than 14, their injury was due to family violence or suspected child abuse, the child or parent was subject to legal proceedings related to the injury, or the child or parent was the perpetrator of violence related to the injury. See the consort diagram (Figure 2) for an overview of study recruitment and retention across time points. See Table 1 for demographic and injury characteristics of study participants.
Figure 2.
Consort Diagram
Table 1.
Demographics and event characteristics
| Variable | n = 96 |
|---|---|
| Child age in years (M (SD), range) | 10.6 (1.7), 8–13 |
| Child sex- male (N (%)) | 62 (64.5) |
| Child race (N (%)) | |
| Black/ African American | 39 (40.6) |
| White | 50 (52.1) |
| Other | 7 (7.3) |
| Child ethnicity (N (%)) | |
| Hispanic | 4 (4.2) |
| Non-Hispanic | 92 (95.8) |
| Child injury type (N (%)) | |
| Fracture(s) | 60 (62.5) |
| Other | 36 (37.5) |
| Injury circumstances (N (%)) | |
| Recreational activity (e.g. playground, bike) | 55 (57.3) |
| Sports (i.e., game or practice) | 16 (16.7) |
| Motor-vehicle crash | 15 (15.6) |
| Injured by animal | 5 (5.2) |
| Gunshot wound | 2 (2.1) |
| Kitchen incidents (i.e., burns during food preparation) | 3 (3.1) |
Procedure
Participants were recruited while admitted for treatment of an injury at a hospital (level I pediatric trauma center) in the northeastern United States. Potentially eligible participants were identified via hospital registries. Research assistants (RAs) approached the parents or guardians, explained the study, and invited participation in the screening phase of the study. After written parental consent and child assent, the child completed a validated four-item screen derived from the Acute Stress Checklist for Children (Kassam-Adams, 2006). If the child’s responses indicated that he or she perceived the injury event as potentially traumatic (by endorsing an item on the screener as described below), the child was eligible to participate in the full study. All baseline assessments occurred within two weeks of the index injury event (T1; M = 3.0 days post-injury, SD = 2.9 days post-injury). Follow-up assessments were conducted by phone approximately six weeks (T2; M = 48.9 days, SD = 10.3 days) and 12 weeks (T3; M = 94.8 days, SD = 16.3 days) later. At T1, children completed measures of trauma history, appraisals, and PTSS. At T2, children completed a coping measure and repeated the PTSS measure. At T3, children completed the PTSS measure again. RAs reviewed participants’ medical charts and abstracted type of injury and heart rate from medical records, and obtained injury severity scores (ISS) from the Trauma Registry. All study procedures were approved by the hospital’s Institutional Review Board at The Children’s Hospital of Philadelphia.
Measures
Heart rate
Heart rate is recorded in medical charts as part of routine medical care. Depending on the course of care, each child’s first available heart rate could have been when emergency medical services first arrived to the scene, when the child arrived in the emergency department, or when the child was admitted to the hospital. First available heart rate was selected because past research has identified this heart rate variable as the best predictor of PTSS (Nugent et al., 2006a,b). Because of developmental variation in normal heart rate, each child’s raw heart rate (in beats per minute) was converted to a standard deviation score (z score) based on sex and age-specific reference values obtained from an existing sample of healthy children (Kassam-Adams, et al., 2005; Wuhl et al., 2002).
Injury severity
The Injury Severity Score (ISS; Baker, O’Neill, & Haddon, 1974), a widely-used index of overall injury severity, is determined using standard ratings of the three most severely injured body regions. ISS ranges from 1 to 75, with scores higher than 16 suggesting severe injury. Average ISS in our sample was 5.82 (SD = 4.4, range = 1–22).
Trauma history
The UCLA PTSD Index includes 12 items assessing prior exposure to a range of traumatic events (e.g., natural disaster, accident, war, violence, and medical treatment) (Pynoos, Rodriguez, Steinberg, Stuber, & Frederick, 1998). The current analyses use a dichotomous variable for presence of any trauma history, i.e., children who reported one or more prior traumatic events versus those who reported none.
Trauma-specific appraisals of injury event
Each potentially eligible participant answered a validated subscale of the Acute Stress Checklist for Children (ASC-Kids) assessing subjective perceptions / appraisals of the injury event (Kassam-Adams, 2006), e.g., “It was really shocking, awful, or horrible” and “I thought I might die.” Items are rated on a 3-point scale (0=never/not true; 1=sometimes/somewhat true; 2=often/very true). We used this measure in two ways in the current study – as a screener to determine whether the injury was perceived by the child as potentially traumatic and as an assessment of appraisals specific to this injury event. The injury event was considered “potentially traumatic” (and the child eligible for study participation) only if the child rated at least one item as “often/very true” (Kassam-Adams, 2006; Kassam-Adams et al., 2016). In later analyses, the summed score for all four items was used as a measure of trauma-specific appraisals, i.e., appraisals related to the injury event. Thus, total possible scores ranged from 2 to 8 (those with scores less than 2 were not eligible for the study).
Global Appraisals
The Child Post-Traumatic Cognitions Inventory (CPTCI) is a 25-item scale adapted from the adult Post-Traumatic Cognitions Inventory (Foa, Ehlers, Clark, Tolin, & Orsillo, 1999; Meiser-Stedman et al., 2009). The CPTCI was developed and validated in a large sample of children and adolescents aged 6–18 years. Psychometric analyses indicate two subscales, labeled as “permanent/disturbing change”, and “fragile person in a scary world”, with good internal consistency, test-retest reliability, convergent validity, and discriminant validity (Meiser-Stedman, Smith, et al., 2009). Internal consistencies in the current sample were acceptable: permanent/disturbing change α = .85; fragile person in a scary world α = .75. In this study, the two subscales were used as indicators for the latent global appraisal variable.
Coping
The How I Coped Under Pressure Scale (HICUPS) is a self-report questionnaire that assesses children’s use of coping strategies with regard to a specific event (Ayers, Sandler, West, & Roosa, 1996). The HICUPS’ theoretically-derived subscales were validated via confirmatory factor analyses (Ayers, et al., 1996). The current study used three HICUPS subscales relevant to our hypotheses: cognitive restructuring subscale (e.g., “remind myself that things could be worse”), the social support subscale (e.g., “talked with someone who could help make the situation better”), and the avoidance coping subscale (e.g., “avoided it by going to my room”). Internal consistencies in the current sample were good: cognitive restructuring α = .88; social support α = .85; avoidance α = .87. In this study, the subscales were used as manifest variables.
Posttraumatic stress symptoms
The Child PTSD Symptom Scale (CPSS) is a 24-item self-report instrument that can yield an overall PTSS severity score and severity scores for three subscales corresponding to DSM-IV PTSD symptom categories of re-experiencing, avoidance, and arousal (Foa, Johnson, Feeny, & Treadwell, 2001). The CPSS has shown excellent internal consistency, test-retest reliability, and convergent validity with structured clinical interview measures of PTSD (Foa, et al., 2001). Internal consistencies for subscale scores in the current sample were acceptable across three time points: re-experiencing α = .71–.87, avoidance α = .65–.83, arousal α = .64–.79. In this study, subscale scores were used as indicators for the latent PTSS variables.
Statistical Analysis
Using bivariate analyses (i.e., chi squares, t-tests), we first examined differences in demographics characteristics (child sex, age, and race) for those who participated in the study compared to those who were missed or who elected not to participate in the study. Next, we assessed demographic differences between children who completed T1 assessments compared to subsequent assessments (T2, T3). We first examined bivariate relationships (Pearson’s or point-biserial correlations) among key study variables (heart rate, global appraisals, trauma-specific appraisals, coping strategies, and PTSS). Bivariate analyses of heart rate with PTSS and appraisals served as an initial examination of study hypotheses 4 and 5.
We then used structural equation modeling (SEM) to evaluate study hypotheses 1 to 3 and test the overall fit of several models based on the overarching conceptual model presented in Figure 1. Missing data were managed using a Full Information Maximum Likelihood approach within SEM. The application of SEM procedures allowed modeling with both latent and manifest variables. Data analyses were conducted using SPSS version 22 (for descriptive and bivariate analyses) and Mplus (for SEM analyses; Muthén & Muthén, 1998–2011).
To examine hypotheses, we first included Global appraisals (latent variable with CPTCI subscales as indicators), Trauma-specific appraisals (manifest variable using the ASC-Kids 4-item subscale score), and PTSS (latent variable with CPSS subscales as indicators). Latent variables were identified with a fixed factor loading of one for the first indicator. Correlated uniqueness was added across time points for the indictors of the PTSS latent variable. Trauma history was included in all models as a manifest (dichotomous) variable. Child age, sex, and injury severity were included in covariates for each model. Each type of coping (Cognitive restructuring coping, Social support coping, and Avoidance coping) was first examined in a separate model (as manifest variables using HICCUPS subscales), followed by a final model including all three coping types. In the combined models (i.e., those with all three types of coping) the residuals of each coping type were allowed to correlate.
Overall model fit was evaluated using three indices: the chi-square statistic, the comparative fit index (CFI), and the root mean square error of approximation (RMSEA). Values of chi-square increase with increasing misfit between a model and the empirical data. A non-significant chi-square is desirable. The CFI is a widely used relative fit index comparing the fit of an independence model (in which all variables are unrelated) to the fit of the substantive model. CFI values of .95 or greater are desirable and indicate adequate fit to the data (Hu & Bentler, 1999). The RMSEA provides a measure of absolute fit between the observed and model-implied covariance matrices. RMSEA values below .05 are desired to indicate close fit of a model to data (Hu & Bentler, 1999). Hypotheses regarding mediation were tested using bootstrapping procedures; confidence intervals of indirect effects were calculated using the bias-corrected bootstrap (Hayes, 2013; MacKinnon, 2008), as implemented in Mplus.
Results
Bivariate analyses
There were no significant differences in child sex, race, or age between those who participated in the study compared to those who were eligible but were missed by the research team. No significant differences were identified in child sex or age when comparing those children who participated in the study to those who were offered study participation and decided not to participate; however, differences in child race were detected, χ2 (1) = 9.2, p <.01, with a higher proportion of children identified in the medical record as White declining participation compared to those identified as Black/African American (71.3% vs 51.9%). For those children who completed the T1 assessment, there were no significant differences in child sex or race for those who completed T2 or T3. However, the those children who completed the T2 assessment (not T3) were slightly younger in age on average (10.5 years vs 11.6 years, t(94) = 2.2, p <.05).
Bivariate analyses suggested Trauma history was associated with Cognitive restructuring coping (r = .31, p <.01), Avoidance coping (r = .33, p <.01), and child sex (χ2 = 5.01, p < .05; with a higher proportion of boys endorsing a trauma history compared to girls, 90.3% vs 70.3%); Trauma history was thus retained in the structural models we tested. Child age was significantly related to Social support coping (r = −0.24, p < .05). Injury severity was significantly related to Global appraisals (subscale: permanent change r = −0.26, p < .05). Child sex, age, and injury severity were retained as covariates in the tested models.
Bivariate analyses suggested significant relationships between each type of appraisal and PTSS at every time point (r = .27–.60, p <.05) as well as each type of coping and PTSS at every time point (r =.25–.59, p < .05). In bivariate analyses, heart rate was not significantly related to PTSS at any time point or either type of appraisals. Thus, Hypothesis 4 (heart rate predicting PTSS) was not supported, and we were unable to examine Hypothesis 5 (mediation of heart rate to PTSS prediction via appraisals). Based on this finding, heart rate was not included in structural models. See Supplemental Table 1 for bivariate correlations among study variables.
Structural Models
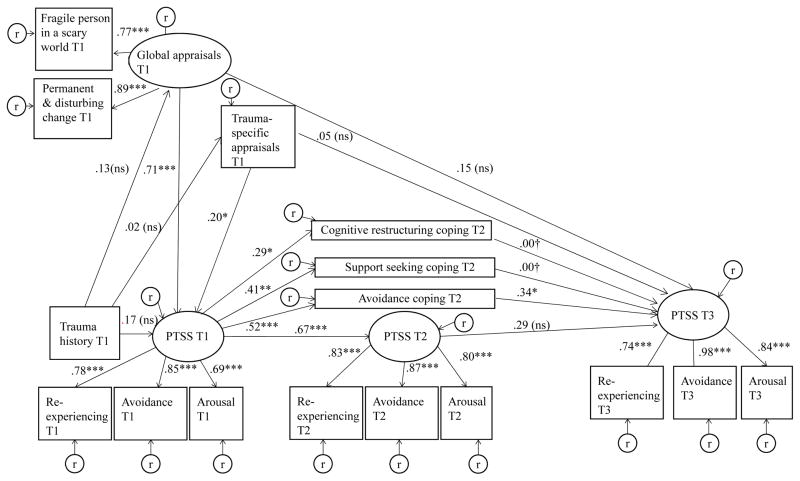
As shown in Supplemental Figure 1, we specified an autoregressive model for PTSS, in which T1 PTSS predicted T2 PTSS, which in turn predicted T3 PTSS. We included Global appraisals (T1) and Trauma-specific appraisals as concurrent predictors of T1 PTSS and as lagged predictors of T3 PTSS. Then, in Supplemental Figures 2, 3, and 4, we separately added Cognitive restructuring coping, Social support coping and Avoidance coping at T2, respectively, as potential mediators of the relation between T1 PTSS and T3 PTSS. Finally, in Figure 3, we included all three forms of coping in a combined model. Given results from the individual models and multicollinearity among coping variables in the combined model in Figure 3, we set the paths from Cognitive restructuring coping and Social support coping to T3 PTSS to zero. Next, we relaxed these paths to examine model fit and ensure we did not misspecifiy the model. Conceptually, our models tested whether appraisal and coping variables predict PTSS over time while controlling for prior levels of PTSS (hypotheses 1–2). Additionally, we tested whether coping was a mediator between T1 PTSS and T3 PTSS (hypothesis 3).
Figure 3.
Model results examining the relations of appraisals and three dimensions of coping with PTSS status over time.
Fit indices: χ2[104, N=96] = 114.43, p = .23; CFI = .99; RMSEA = .03. PTSS= Posttraumatic Stress Symptoms; T1 = < 2 weeks since injury; T2 = 6 week follow-up; T3 = 12 week follow-up, * = < .05, **, = < .01, *** = < .001. † Coefficient fixed at zero. Not pictured: covariates relationships (child age, sex, and injury severity; none had a direct effect on PTSS at any time point).
Results suggested that each of the hypothesized models provided a good fit to the data (See Figure 3 and Supplemental Figures 1–4 for model fit statistics). All factor loadings for indicators of latent variables were statistically significant (all ps < .001), with standardized estimates > .68. Standardized effects are presented in Figure 3 and Supplemental Figures 1–4. Hypothesis 1: Neither Global appraisals nor Trauma-specific appraisals significantly predicted T3 PTSS in any model but were significantly associated with T1 PTSS in every model. Hypothesis 2: Significant associations emerged between T1 PTSS and each type of T2 coping, both in individual models and combined models. Only Avoidance coping was in turn predictive of T3 PTSS in the individual models. To ensure that we did not misspecify the model in Figure 3, we relaxed the constraints, allowing for estimation of non-zero effects of Cognitive restructuring and Social support coping on T3 PTSS. The resulting model did not improve model fit significantly, Δχ2 (2) = 3.26, ns, so we retained the constrained model as shown in Figure 3. Hypothesis 3: Coping significantly mediated the effect of T1 PTSS on T3 PTSS in the avoidance coping (Supplemental Figure 4) and overall coping model (Figure 3). The bootstrapped estimate of the indirect effect was .18, p < .05, [95% CI = .04–.40 and .18, p < .05, [95% CI: .03–.40], for the avoidance coping model and for the overall model, respectively.
Discussion
The current study results contribute to our understanding of the development of PTSS in children with injuries across the pre-, peri-, and post-trauma periods. This research highlights the integration of selected variables from a bio-psycho-social framework to begin to grow a foundation and encourage future research into the utility of this approach to understanding child PTSS. Primary study findings suggest that both global and trauma-specific appraisals may play a role in initiating PTSS in children following injury. The findings also elucidate the complex relationship between coping and PTSS over time, indicating that children who display early PTSS engage in more coping strategies of various types, but that avoidant coping in particular may inadvertently maintain PTSS.
This study adds to the literature on child PTSS following acute trauma exposure by following children across multiple assessment points and assessing both appraisals and coping strategies (psychological variables), in the context of other key biological (e.g., child age, sex, physiological reactivity-heart rate) and environmental variables (e.g., trauma history, ISS). The proposed models fit the data well, highlighting the importance of examining independent and interdependent relationships of bio-psycho-social variables together over time. Solely examining bivariate relationships, especially among factors assessed concurrently, can miss important relationships among factors in the development and maintenance of PTSS in children recovering from injury.
Certain types of threat appraisals have been shown to be associated with more PTSS in children (Ehlers, et al., 2003; Marsac, et al., 2016; Meiser-Stedman, Dalgleish, et al., 2009). The current study extends past work by finding that global and trauma- specific appraisals, assessed in the early aftermath of an injury, had unique, independent relationships with PTSS development. Each type of appraisal was related to current and later PTSS in bivariate analyses. However, neither global nor trauma-specific appraisals served as a significant predictor of future PTSS when the relationship between appraisals and baseline PTSS was accounted for in the model. This latter finding differs from past research (Bryant, Salmon, Sinclair, & Davidson, 2007; Ehlers, et al., 2003; Marsac, et al., 2016). One possible explanation is that some past studies did not control for the association of PTSS and appraisals at baseline (e.g., Ehlers, et al., 2003). Another potential source of variation is a study design difference: screening procedures in the current study excluded children who did not perceive the index event as at least somewhat threatening (though only 8 children assessed became ineligible due to this screening). This may mean that the current sample did not include a set of children who would ultimately have shown more variation in the relationship of their early (low) threat appraisals to later PTSS development.
This study extends previous research on the relationship between coping and PTSS by examining PTSS at multiple time points and coping as a mediator. As suggested by Marsac and colleagues’ (2014) bio-psycho-social model, considering the interrelationships among these variables over time adds to our understanding of persistent PTSS. Consistent with prior literature, we found that children with early PTSS tended to use more coping strategies of all types in the subsequent weeks (Marsac, et al., 2014; Stallard, et al., 2001) and those who used more avoidance coping had more severe PTSS later on (Marsac, et al., 2016; Stallard, et al., 2001). This study puts these pieces together in a new way by showing that while children who are in more distress (early PTSS) make more attempts to manage their distress (i.e., via more coping), those who use avoidance coping as a strategy may inadvertently increase their persistent, future PTSS. Too much use of avoidance coping likely interferes with processes that undergird emotional recovery following a traumatic event. Cognitive-behavioral theories of PTSS development posit that adaptive post-trauma recovery involves thinking and talking about the event and having some exposure to trauma reminders under safe circumstances, so that newly developed and unrealistic threat appraisals can be unlearned and replaced with more adaptive appraisals (Ehlers & Clark, 2000). Over time, the reminders become less distressing and the individual is able to assimilate the trauma experience (Foa, 1997; Kassam-Adams, et al., 2013). Excessive use of avoidance coping to manage distressing reactions to trauma reminders may divert this adaptive process. These results confirm that one target of early preventive interventions should be to help children decrease their use of avoidance coping; however, the current results do not provide clear guidance for specific adaptive coping strategies that would reduce or prevent PTSS.
Beyond appraisals and coping, this study also considered the potential role of pre- and peri-trauma variables that represent selected biological and environmental factors (not every potentially important predictor was included). Following initial bivariate analyses, heart rate was not included in our models for parsimony, but likely deserves further attention in subsequent studies with larger samples given past research. Our finding that heart rate did not predict subsequent PTSS differs from past work (De Young, et al., 2007; Kassam-Adams, et al., 2005; Nugent, et al., 2006a.b). It is important to note this the current study included heart rate as an initial step to integrate biological factors into the study of child PTSS; however, future investigations of biological mechanisms in PTSS development may benefit from assessing genetic and epigenetic factors, memory formation related to the traumatic event, and changes in hormones (Marsac, et al., 2014; Schwartz & Perry, 1994). Our finding that child age was not significantly associated with PTSS is consistent with past work (Alisic, et al., 2011). Evidence to date has suggested child sex (female) as a potential risk factor for PTSS, but most studies (that have found this affect) have demonstrated weak associations between child sex and PTSS (Alisic, et al., 2011); thus, the finding that child sex was not a direct contributor to PTSS in this sample is not surprising but warrants further investigation with larger samples.
Regarding environmental factors, this study examined only trauma history and injury severity. Past research has shown mixed results for the role of injury severity and PTSS, with studies generally finding either small or no relationship (Alisic, et al., 2011). Study results confirmed this very consistent (if counter-intuitive) finding that physical severity of injury was not associated with PTSS severity. Much past research has indicated that children reporting a prior trauma history have greater initial PTSS (Alisic, et al., 2011; Trickey et al., 2012); the current study findings are consistent with this in the bivariate analyses but not in the context of the larger model. While we might have expected an association to operate via increased initial threat appraisals, in our models trauma history did not appear to have a meaningful association with either global or trauma-specific appraisals. This particular association merits further study, to better understand how prior experiences of potentially traumatic events can impact child recovery post-injury.
There are several limitations to the current study. The current project presented self-report data only; taking a mixed methods approach or observational approach to the assessment of study constructs (particularly appraisals and coping) may provide a more thorough understanding of these variables and is an excellent avenue for future research. Coping strategies may change over time following medical events (Stallard, et al., 2001); our inclusion of a single coping assessment at T2 allowed us to examine some but not all aspects of the interrelationship among coping strategies and PTSS over time. Avoidance coping strategies and the avoidance symptoms that are part of the PTSD construct could be seen as having conceptual or measurement overlap; however because our models include avoidant coping in the context of multiple assessments of PTSS, we are able to demonstrate a unique relationship between avoidant coping and later PTSS. Another limitation of this study is that our screening procedures required children to have perceived the index event as at least somewhat threatening: thus, the study is missing the group of children who did not experience their injury as possibly traumatic. While less than 10% of children assessed became ineligible because of this screener (n = 8), these children many have an entirely different response pattern across all study measures. Future research can build on the current study’s results by including children with the full range of threat appraisals. Because of the timing of the study (during the transition from DSM-IV to DSM-5), we used a PTSS measure based on DSM-IV rather than DSM-5 criteria. Finally, the refusal rate for the study was high (~31%) and a large number of potentially eligible participants were missed during study recruitment (~54%). While these factors may limit the generalizability of results, there were no differences in child sex or age between participating and non-participating children. More research needs to be conducted to better understand the potential role that culture or race may play in the child’s decision to participate in this type of research.
With millions of children experiencing acute medical events each year, understanding child emotional recovery from these events is essential to inform clinical care and health policy. Consistent with cognitive theories of PTSS development, the results of the models we tested paint a picture of one pathway to persistent PTSS after injury: children with early threat appraisals (global or trauma-specific) develop more severe initial PTSS, and when these children employ avoidance coping strategies to manage this distress, they become more likely to have PTSS that persist over time. There are several clinical implications of these findings. Early threat appraisals may complement direct symptom assessment as a useful way to identify children experiencing problematic early reactions to injury. Targeting these early appraisals for preventive intervention could decrease early PTSS and reduce the risk for ongoing PTSS. Results also confirm reducing the use of avoidant coping as a target for early preventive interventions in the weeks following injury. The Coping Coach intervention is one example of a preventive intervention which aims to help children (a) challenge any maladaptive trauma-specific appraisals and promote adaptive appraisals, and (b) reduce their use of avoidant coping in the face of trauma reminders (Kassam-Adams, et al., 2016; Marsac et al., 2015). Given the current state of the empirical literature, we need more prospective descriptive studies, as well as intervention trials, that explicitly examine specific pathways and mechanisms involved in the initiation, maintenance, and prevention of persistent PTSS in children after acute trauma exposure (Kassam-Adams, 2014).
Supplementary Material
Acknowledgments
This work was supported by a Mentored Career Award grant 1K23MH093618-01A1 from the National Institute of Mental Health.
Contributor Information
Meghan L. Marsac, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia, Department of Psychiatry, University of Pennsylvania, Department of Pediatrics, Kentucky Children’s Hospital, College of Medicine, University of Kentucky.
Nancy Kassam-Adams, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia; Department of Pediatrics, University of Pennsylvania.
Douglas L. Delahanty, Department of Psychology, Kent State University.
Jeffrey Ciesla, Department of Psychology, Kent State University.
Danielle Weiss, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia.
Keith F. Widaman, Graduate School of Education, University of California-Riverside.
Lamia P. Barakat, Division of Oncology, The Children’s Hospital of Philadelphia, Department of Pediatrics, University of Pennsylvania.
References
- Aldridge A, Roesch S. Coping and adjustment in children with cancer: a metaanalytic study. Journal of Behavioral Medicine. 2007;30(2):115–129. doi: 10.1007/s10865-006-9087-y. [DOI] [PubMed] [Google Scholar]
- Alisic E, Jongmans MJ, van Wesel F, Kleber RJ. Building child trauma theory from longitudinal studies: a meta-analysis. Clinical Psychology Review. 2011;31(5):736–747. doi: 10.1016/j.cpr.2011.03.001. [DOI] [PubMed] [Google Scholar]
- Ayers T, Sandler I, West S, Roosa M. A dispositional and situational assessment of children’s coping: Testing alternative models of coping. Journal of Personality. 1996;64(4):923–958. doi: 10.1111/j.1467-6494.1996.tb00949.x. [DOI] [PubMed] [Google Scholar]
- Baker S, O’Neill B, Haddon W. The injury severity score: A method for describing patients with multiple injuries and evaluation of emergency care. The Journal of Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Bryant R, Salmon K, Sinclair E, Davidson P. A prospective study of appraisals in childhood posttraumatic stress disorder. Behaviour Research and Therapy. 2007;45:2502–2507. doi: 10.1016/j.brat.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Injury prevention & control: Data & statistics (WISQARS) 2014 from http://www.cdc.gov/injury/wisqars/nonfatal.html.
- De Young A, Kenardy J, Spence SH. Elevated heart rate as a predictor of PTSD six months following accidental pediatric injury. Journal of Traumatic Stress. 2007;20(5):5. doi: 10.1002/jts.20235. [DOI] [PubMed] [Google Scholar]
- De Young A, Kenardy J, Cobham VE, Kimble R. Prevalence, comorbidity and course of trauma reactions in young burn-injured children. Journal of Child Psychology, Psychiatry, and Allied Disciplines. 2012;53(1):56–63. doi: 10.1111/j.1469-7610.2011.02431.x. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark D. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Mayou R, Bryant B. Cognitive predictors of posttraumatic stress disorder in children: results of a prospective longitudinal study. Behaviour Research and Therapy. 2003;41(1):1–10. doi: 10.1016/s0005-7967(01)00126-7. [DOI] [PubMed] [Google Scholar]
- Foa E. Psychological processes related to recovery from a trauma and an effective treatment for PTSD. In: McFarlane A, Yehuda R, editors. Psychobiology of Posttraumatic Stress Disorder. Vol. 821. New York: New York Academy of Sciences; 1997. pp. 410–424. [DOI] [PubMed] [Google Scholar]
- Foa E, Ehlers A, Clark D, Tolin D, Orsillo S. The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment. 1999;11(3):303–314. [Google Scholar]
- Foa E, Johnson K, Feeny N, Treadwell K. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press; 2013. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kassam-Adams N. The Acute Stress Checklist for Children (ASC-Kids): Development of a child self-report measure. Journal of Traumatic Stress. 2006;19(1):129–139. doi: 10.1002/jts.20090. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N. Design, delivery, and evaluation of early interventions for children exposed to acute trauma. European Journal of Psychotraumatology. 2014;5:10. doi: 10.3402/ejpt.v5.22757. 3402/ejpt.v5.22757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams N, Bakker A, Marsac ML, Fein JA, Winston FK. Traumatic stress, depression, and recovery: Child and parent responses after emergency medical care for unintentional injury. Pediatric Emergency Care. 2015;31(11):737–742. doi: 10.1097/PEC.0000000000000595. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Garcia-España J, Fein J, Winston FK. Heart rate and posttraumatic stress in injured children. Archives of General Psychiatry. 2005;62:335–340. doi: 10.1001/archpsyc.62.3.335. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Marsac ML, Hildenbrand AK, Winston FK. Posttraumatic stress following pediatric injury: Update on diagnosis, risk factors, and intervention. JAMA Pediatrics. 2013;167(12):1158–1165. doi: 10.1001/jamapediatrics.2013.2741. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Marsac ML, Kohser K, Kenardy J, March S, Winston FK. Pilot randomized controlled trial of a novel web-based intervention to prevent posttraumatic stress in children following medical events. Journal of Pediatric Psychology. 2016;41:138–148. doi: 10.1093/jpepsy/jsv057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak A. Pediatric Psychosocial Preventative Health Model (PPPHM): Research, practice, and collaboration in pediatric family systems medicine. Families, Systems, & Health. 2006;24(4):381–395. [Google Scholar]
- Kazak A, Rourke M, Alderfer M, Pai A, Reilly A, Meadows A. Assessment, intervention, and psychosocial care in pediatric oncology: Two models. Journal of Pediatric Psychology. 2007;32(9):1099–1110. doi: 10.1093/jpepsy/jsm031. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath M, Ribi K. Predictors of coping strategy selection in paediatric patients. Acta paediatr. 2002;91:945–960. doi: 10.1080/080352502760272650. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath ME, Gnehm HE, Sennhauser FH. Post-traumatic stress impacts on quality of life in children after road traffic accidents: Prospective study. Australian and New Zealand Journal of Psychiatry. 2009;43(8):746–753. doi: 10.1080/00048670903001919. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Marsac M, Kassam-Adams N, Delahanty D, Widaman FK, Barakat L. Posttraumatic Stress Following Acute Medical Trauma in Children: A Proposed Model of Bio-Psycho-Social Processes During the Peri-Trauma Period. Clinical Child and Family Psychology Review. 2014:1–13. doi: 10.1007/s10567-014-0174-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsac M, Winston F, Hildenbrand A, Kohser K, March S, Kenardy J, Kassam-Adams N. Systematic, theoretically grounded development and feasibility testing of an innovative, preventive web-based game for children exposed to acute trauma. Clinical Practice in Pediatric Psychology. 2015;3(1):12–24. doi: 10.1037/cpp0000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsac ML, Ciesla J, Barakat LP, Hildenbrand AK, Delahanty DL, Widaman KF, … Kassam-Adams N. The role of appraisals and coping in predicting posttraumatic stress following pediatric injury. Psychological Trauma: Theory, Research, Practice, and Policy. 2016 doi: 10.1037/tra0000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsac ML, Donlon K, Hildenbrand AK, Winston FK, Kassam-Adams N. Understanding recovery in children following traffic-related injuries: Exploring acute traumatic stress reactions, child coping, and coping assistance. Clinical Child Psychology and Psychiatry. 2014;19(2):233–243. doi: 10.1177/1359104513487000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman R. Towards a cognitive -behavioral model of PTSD in children and adolescents. Clinical Child and Family Psychology. 2002;5(4):217–232. doi: 10.1023/a:1020982122107. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R, Dalgleish T, Glucksman E, Yule W, Smith P. Maladaptive cognitive appraisals mediate the evolution of posttraumatic stress reactions: A 6-month follow-up of child and adolescent assault and motor vehicle accident survivors. Journal of Abnormal Psychology. 2009;118(4):9. doi: 10.1037/a0016945. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R, Smith P, Bryant R, Salmon K, Yule W, Dalgleish T, Nixon R. Development and validation of the Child Post-Traumatic Cognitions Inventory (CPTCI) Journal of Child Psychology and Psychiatry. 2009;50(4):432–440. doi: 10.1111/j.1469-7610.2008.01995.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- Nugent N, Christopher N, Delahanty D. Emergency medical service and in-hospital vital signs as predictors of subsequent PTSD symptom severity in pediatric injury patients. Journal of Child Psychology and Psychiatry. 2006a;47:919–926. doi: 10.1111/j.1469-7610.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Nugent N, Christopher N, Delahanty D. Initial physiological responses and perceived hyperarousal predicts subsequent emotional numbing in child trauma victims. Journal of Traumatic Stress. 2006b;19:349–359. doi: 10.1002/jts.20130. [DOI] [PubMed] [Google Scholar]
- Nugent N, Ostrowski S, Christopher N, Delahanty D. Parental posttraumatic stress symptoms as a moderator of child’s acute biological response and subsequent posttraumatic stress symptoms in pediatric injury patients. Journal of Pediatric Psychology. 2007;32(3):309–318. doi: 10.1093/jpepsy/jsl005. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Gersons B. The psychology of PTSD: Coping with trauma. Psychoneuroendocrinology. 2005;30:8. doi: 10.1016/j.psyneuen.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Pynoos R, Rodriguez N, Steinberg A, Stuber M, Frederick C. UCLA PTSD Index for DSM-IV. Los Angeles: Trauma Psychiatric Services; 1998. [Google Scholar]
- Roth S, Cohen LJ. Approach, avoidance, and coping with stress. American Psychologist. 1986;41(7):813–819. doi: 10.1037//0003-066x.41.7.813. [DOI] [PubMed] [Google Scholar]
- Schwartz E, Perry B. The post-traumatic response in children and adolescents. Psychiatric Clinics of North America. 1994;17(2):311–326. [PubMed] [Google Scholar]
- Stallard P, Smith E. Appraisals and cognitive coping styles associated with chronic post-traumatic symptoms in child road traffic accident survivors. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2007;48(2):194–201. doi: 10.1111/j.1469-7610.2006.01692.x. [DOI] [PubMed] [Google Scholar]
- Stallard P, Velleman R, Langsford J, Baldwin S. Coping and psychological distress in children involved in road traffic accidents. British Journal of Clinical Psychology. 2001;40:197–208. doi: 10.1348/014466501163643. [DOI] [PubMed] [Google Scholar]
- Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32:122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Wuhl E, Witte K, Soergel l, Mehls O, Schaefer F, Kirschstein M, … Rascher W. Distribution of 24-h ambulatory blood pressure in children: Normalized reference values and role of body dimensions. Journal of Hypertension. 2002;20(10):1995–2007. doi: 10.1097/00004872-200210000-00019. [DOI] [PubMed] [Google Scholar]
- Zehnder D, Prchal A, Vollrath M, Landolt M. Prospective study of the effectiveness of coping in pediatric patients. Child Psychiatry and Human Development. 2006;36:351–368. doi: 10.1007/s10578-005-0007-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.