Abstract
The “silent epidemic” of traumatic brain injury (TBI) has been placed in the spotlight following investigations and popular press coverage of athletes and returning soldiers with single and repetitive injuries; however, treatments to improve the outcome for patients with TBI across the spectrum from mild to severe TBI are lacking. Neuroinflammation may cause acute secondary injury after TBI, and it has been linked to chronic neurodegenerative diseases. Despite these findings, anti-inflammatory agents have failed to improve outcomes in clinical trials. We therefore propose in this review a new framework for future exploration of targeted immunomodulation after TBI that incorporates factors such as the time from injury, mechanism of injury, and secondary insults in considering potential treatment options. Structured around the dynamics of the immune response to TBI – from initial triggers to chronic neuroinflammation – the ability of soluble and cellular inflammatory mediators to promote repair and regeneration versus secondary injury and neurodegeneration is highlighted, with knowledge from human studies explicitly defined throughout this review. Recent advances in neuroimmunology and TBI-responsive neuroinflammation are incorporated, including inflammasomes, mechanisms of microglial polarization, and glymphatic clearance. In addition, we identify throughout this review where these findings may offer novel therapeutic targets for translational and clinical research, incorporate evidence from other brain injury models, and identify outstanding questions in the field.
Keywords: traumatic brain injury, inflammation, secondary brain injury, repair, neurodegeneration, microglial activation
I. INTRODUCTION AND OVERVIEW
The Centers for Disease Control estimates 1.7 million people suffer traumatic brain injury (TBI) in the United States each year and 5.3 million are living with TBI-related disability.1 This may grossly underestimate the scope of the epidemic, particularly for mild TBI (mTBI)2, and globally the incidence of TBI appears to be increasing.1 TBI and mTBI are “signature injuries” of the wars in Iraq and Afghanistan, primarily due to blast exposure from conventional and improvised explosive devices, and can similarly represent consequences of civilian terrorist attacks. In addition, TBI has now been linked to post-traumatic stress disorder, memory deficits, chronic traumatic encephalopathy (CTE), and chronic neuroinflammation.3
The inflammatory reaction to TBI was thought to occur solely through peripheral immune mediators entering via a disturbed blood brain barrier (BBB); it is now recognized as a robust and complex interaction between central and peripheral cellular and soluble components influenced by patient age, sex, mechanism of injury (focal, diffuse, blast), degree of injury (mild, repetitive mild, severe), secondary insults (hypoxemia, hypotension), therapeutic interventions, and genetic variability. TBI leads to early resident microglial activation and peripheral neutrophil recruitment, followed later by infiltration of lymphocytes and monocyte-derived macrophages.4 Simultaneously, pro- and anti-inflammatory cytokines vie to promote and terminate the post-traumatic neuroinflammatory response, and chemokine signaling results in the activation and recruitment of immune cells towards the lesion.5–9
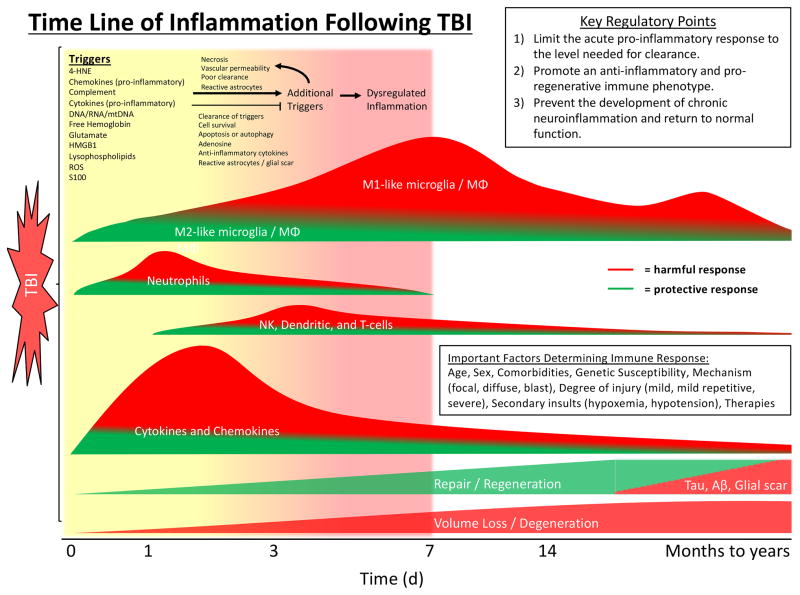
This post-traumatic inflammation may be beneficial, by promoting clearance of debris and regeneration, and/or harmful, mediating neuronal death and progressive neurodegeneration (Figure 1). Several multicenter clinical trials have been conducted with therapies shown in pre-clinical and single center trials to have beneficial anti-inflammatory effects. Unfortunately, each trial failed to show benefit; several therapies were deleterious.10–17 We therefore propose in this review a new framework to guide future preclinical and clinical trials to optimize the immune response to TBI:
Figure 1. Overview of Neuroinflammation after TBI.
Primary mechanical injury to the CNS may cause cell membrane disruption, vascular rupture, and BBB damage followed by secondary reactions involving ionic imbalance, release of excitatory amino acids, calcium overload, and mitochondrial dysfunction - ultimately culminating in cell death pathways. Primary and secondary injury lead to release of DAMPs, cytokines, chemokines, activation of microglia and astrocytes, and recruitment of circulating immune cells. These immune responses largely overlap temporally. The inflammatory response is crucial to clearance of debris, repair, and regeneration after TBI. However, dysregulated inflammation can lead to additional acute and chronic brain injury.
Abbreviations: CNS, central nervous system; BBB, blood brain barrier; DAMP, damage-associated molecular pattern; TBI, traumatic brain injury
Limit the acute pro-inflammatory response to the level needed for clearance of debris and danger signals.
Promote an anti-inflammatory and pro-regenerative immune phenotype.
Prevent the development of chronic neuroinflammation and return to normal function.
Using this framework, we review the dynamics of the immune response to TBI, progressing from initiation of acute inflammation by danger signals and early inflammatory mediators, to subacute inflammation occurring days to weeks after injury, and lastly to chronically activated elements of the immune system which may remain active for months to years and have been linked to the development of traumatic encephalopathies. Mechanisms that balance pro-inflammatory and pro-reparative immune activation are discussed, as well as potential for therapies to promote beneficial aspects of inflammation. We discuss recent discoveries in immunology and our current understanding of the role these processes and systems may play in the immune response to TBI. Acknowledging the limitations of TBI models18,19, we incorporate a comprehensive review of what is known from human studies over the past two decades of TBI research; though, notably, limited human data are available of mTBI. Lastly, considering the current knowledge of post-traumatic neuroinflammation we propose new areas for advancing translational and clinical research.
II. ACUTE AND SUBACUTE NEUROINFLAMMATION
A. Triggers–DAMPs, Mitochondrial stress, Excitotoxicity, Vascular Injury
Cellular membrane disruption as a result of primary mechanical insult or secondary injury causes release of damage associated molecular patterns (DAMPs) capable of triggering and amplifying neuroinflammation (Table 1). Examples include DNA and RNA, high mobility group box 1 (HMGB1), S-100 proteins, adenosine triphosphate, uric acid, lysophospholipids, and lipid peroxidation-derived carbonyl adducts of proteins, among others.4,20,21 In response, tumor necrosis factor (TNF)α, interleukin (IL)-6 and IL-1β are up-regulated rapidly by local glial cells and infiltrating immune cells22 and represent early effectors that drive post-traumatic neuroinflammation (Table 2).
Table 1.
Human Studies of Neuroinflammation after TBI: Triggers / Brakes
| Inflammatory mediator | Tissue / Fluid | Time Course | Association with clinical outcome(s) | Other | Ref |
|---|---|---|---|---|---|
| Triggers / Brakes | |||||
| Adenosine | CSF ECF |
Increased within hours of injury Rapidly decline over 12–24h |
Pediatric: No association with outcome after severe TBI Adult: Higher level in patients that died after severe TBI |
A1AR gene variants associated with post-traumatic epilepsy Increased CSF adenosine associated with jugular vein desaturation |
222–224 |
| Complement | CSF | Peak day 1 post-injury, decline day 2–7 | Adult: Increased MAC level associated with BBB dysfunction in severe TBI | C3 and Factor B increased relative to controls | 58,225 |
| Tissue | Increased in tissue resected 2–82h post-injury | Unknown | C3-mRNA also detected in penumbra, suggesting a contribution of local synthesis | 57 | |
| Glutamate | CSF ECF |
Multiple courses described Most common peak day 1, decline day 2–3 |
Pediatric: Higher level associated with poor 6mo-GOS in severe TBI Adult: Increase in ECF glutamate associated with poor outcomes |
Increased glutamate associated with age < 4 and child abuse Hourly levels not affected by transient hemodynamic or ICP change |
41,226–228 |
| HMGB1 | CSF | No change over time | Pediatric: Higher level associated with unfavorable 6 month GOS in severe TBI Adults: Increased level associated with high ICP |
Not associated with age or mechanism of injury | 27,28 |
| Tissue | Translocated to cytoplasm of cells in contused area at 30min – 1d Localized to cytoplasm of phagocytic microglia at 2–20d |
Unknown | HMGB1 receptor, RAGE, expression also increased in contused area in phagocytic microglia | 229 | |
| NLRP1 | CSF | Unknown | Adult: Higher level in patients with unfavorable 5 month GOS in moderate to severe TBI | Adaptor protein ASC also increased in CSF of TBI patients | 230 |
| Caspase-1 | CSF | Unknown | Adult: Higher level in patients with unfavorable 5mo-GOS in moderate to severe TBI | Identified by p20 subunit suggests activated form of enzyme | 230 |
| Tissue | Pro-caspase-1 is cleaved to active form on day 1 | Unknown | 231 | ||
| mtDNA | CSF | Peak day 1, declined on day 3, though still above control | Pediatric: Higher levels associated with unfavorable 6mo- GOS in severe TBI | Positively correlated with HMGB1 level | 52 |
Abbreviations: TBI – traumatic brain injury; CSF – Cerebrospinal fluid; ECF – Extracellular fluid; A1AR – adenosine receptor A1; MAC – membrane attack complex; ICP – intracranial pressure; HMGB1 – high mobility group box 1; RAGE – receptor for advanced glycation endproducts; NLRP1 – NACHT, LRR and PYD domains-containing protein 1; GOS – Glasgow Outcome Scale; mtDNA – mitochondria DNA; BBB – blood brain barrier; GCS – Glasgow Coma Scale
Table 2.
Human Studies of Neuroinflammation after TBI: Cytokines / Chemokines
| Inflammatory mediator | Tissue / Fluid | Time Course | Association with clinical outcome(s) | Other | Ref |
|---|---|---|---|---|---|
| Cytokines / Chemokines | |||||
| TNFα | CSF ECF |
Peaks early on day 1 Prolonged elevation in patients with hypoxia |
Mixed results Most studies show no association with outcome Higher 6h level may be associated with ICP and outcome |
Soluble TNF receptor levels peak later (day 4–9) TNF allele variants associated with clinical outcome |
5,7,136,189,232–237 |
| Tissue | Increased above control within 17min of injury | Unknown | 4-fold increase in mRNA within 17 min | 6 | |
| IFN-γ | Tissue | Increased above control within 17min of injury | Unknown | Behind IL-6, was second highest cytokine concentration measured | 6 |
| IL-1β | CSF ECF |
Peak day 1–2, decrease day 2–4 IL-1ra consistently much higher than IL-1β |
Pediatric: Mixed results – no correlation with outcome vs. worse outcome Adults: Mixed results – no correlation with outcome vs. worse outcome and elevated ICP Adults: High ECF IL-1ra and IL-1ra/IL-1β ratio associated with good outcome |
IL-1RN (IL-1ra gene) polymorphisms associated with cerebral hemorrhage after TBI Principle component analysis of microdialysis data shows close covariance with TNFα |
136,237–244 |
| Tissue | Increased above control 6–122h after injury | Unknown | 5-fold increase in mRNA at 6–122h | 6 | |
| IL-6 | CSF ECF |
Marked increase after TBI Peak day 1, decline day 2–3 |
Pediatric: Mixed results – no correlation with outcome vs. worse outcome Adults: Higher CSF or ECF level associated with favorable GOS |
Pediatric: 2-fold greater in children with intermittent vs. continuous CSF drainage Adults: Associated with NGF level. CSF added to astrocyte culture induced NGF production, blocked by anti-IL6 antibody |
237–239,243,245–251 |
| Tissue | Increased above control within 17min of injury | No relationship to ICP, brain oxygenation, edema | 20-fold increase in mRNA levels at 6–122h | 6,243 | |
| IL-10 | CSF ECF |
Peak day 1, decline day 2–3 May have second or third peak of lower magnitude Later peak in ECF, day 4–6 |
Pediatric: Higher level associated with mortality in severe TBI Adults: Mixed results – no correlation with outcome vs. worse outcome |
Higher level associated with age < 4y No change relative to control in contused tissue |
5,6,136,237,242,243,245,248,252 |
| IL-12p70 | CSF ECF |
Increased day 2–3 Peak day 3–5 |
Pediatric: No association with outcome | 35-fold greater in ECF than plasma | 237,238 |
| GM-CSF | Tissue | Increased above control 6–122h after injury | Unknown | Expression in CSF prolonged by hypoxia | 6,253 |
| TGF-β | CSF | Peak day 1, gradually decrease over 21 days | Adult: No associated with outcome | Associated with BBB permeability | 254 |
| CCL2 (MCP-1) | CSF ECF |
Peak day 1, decrease and plateau by day 4 but remains elevated relative to controls through day 10 | Unknown | 10-fold higher in ECF relative to plasma | 237,255,256 |
| Tissue | mRNA detected 3h – 15d after injury | Unknown | Chemokine most consistently and strongly expressed mRNA in evacuated contusion | 256 | |
| CCL3 (MIP1α) | CSF ECF |
Increased day 1–3, no clear peak | Pediatric: Not associated with outcome | No association with age, gender, GCS | 237,238 |
| Tissue | mRNA detected 3h – 15d after injury | Unknown | Intermediate levels of mRNA detected | 256 | |
| CXCL8 (IL-8) | CSF ECF |
Peak day 1. Marked decline day 2–3. Above control up to 108h after injury | Pediatric: Higher level strongly associated with mortality Adult: Higher level associated with BBB permeability, but not mortality |
No association with age, gender, or GCS 10 to 20-fold higher in CSF and ECF relative to plasma |
237,238,248,257 |
| Tissue | mRNA detected 3h-15d after injury | Unknown | 139-fold increase in mRNA at 6–122h | 6,256 | |
Abbreviations: TBI – traumatic brain injury; CSF – Cerebrospinal fluid; ECF – Extracellular fluid; TNF – tumor necrosis factor; IFN – interferon; IL – interleukin; NGF – nerve growth factor; GOS – Glasgow Outcome Scale; TGF – transforming growth factor; BBB – blood brain barrier; CCL – C-C motif chemokine ligand; CXCL – C-X-C motif ligand; GCS – Glasgow Coma Scale
The dual nature of inflammation was demonstrated in experimental models investigating the role of TNFα and inducible nitric oxide synthase (iNOS) after TBI. TNFα is linked to brain edema, BBB disruption, and recruitment of leukocytes.9 However, TNFα−/− mice had impaired motor function and larger lesions at 4 weeks after injury, despite showing early neuroprotection.23 Similarly, although TBI increased iNOS expression in the brain with multiple pro-inflammatory and neurotoxic effects, genetic or chemical iNOS blockade resulted in significantly worsened spatial memory 2–3 weeks after injury.24
Cell death via programmed necrosis, such as necroptosis through TNFα mediated RIP kinase activation,25,26 may lead to a vicious cycle of necrosis→membrane disruption→ DAMP release→necrosis and amplification of inflammation. The prototypical DAMP, HMGB1, is increased in cerebrospinal fluid (CSF) of patients after severe TBI and is associated with elevated intracranial pressure (ICP) in adults and poor outcome in children.27,28 HMGB1 is a structural DNA-binding protein that regulates transcription by stabilizing nucleosomes under normal conditions.28 It can be released from cells by membrane disruption or actively secreted by monocytes/macrophages and signals through receptor for advanced glycation end products and toll like receptor 2 (TLR2)/TLR4 receptors to increase production and release of cytokines.25
One mechanism of cytokine production triggered by DAMPs is via activation of the inflammasome complex. Binding to intracellular pattern recognition receptors such as the NOD-like receptor containing an N-terminal pyrin domain (NLRP) family or absent in melanoma (AIM) leads to auto-activation of caspase-1 and processing of pro-IL-1β and pro-IL-18 to their active forms.29,30 Relatively few inflammasome complexes are expressed in the brain: NLRP1 and AIM2 in neurons,31–33 NLRP3 in astrocytes33 and microglia are present in both mice and humans.34–36 In patients, NLRP1 and caspase-1 are increased in the CSF after severe TBI and are associated with unfavorable outcomes.33 In mice, neutralization of the NLRP1 and NLRP3 inflammasomes attenuated IL-1β processing and reduced lesion volume.31,32 Inflammasome-dependent cytokine production also contributes to disease progression in mouse models of multiple sclerosis, Alzheimer’s disease, and amyotrophic lateral sclerosis.34,37,38 However, it remains unclear which inflammasome complexes are the primary producers of IL-1β and IL-18 after TBI, and whether neurons, microglia or astrocytes are the key cellular mediators of inflammasome-mediated tissue damage.
Concurrent with the release of DAMPs, a massive increase in extracellular glutamate (and other excitatory amino acids)39–41 may occur and lead to excitotoxic neuronal injury via activation of neuronal glutamate receptors, such as N-methyl-D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, followed by Ca++-dependent degeneration.42 Elegant interactions between inflammatory mediators and glutamate signaling have been demonstrated in mice, including: 1) TNFα and IL-1β mediated changes in cell surface expression, distribution, and function of NMDA and AMPA receptors, 2) NMDA receptor induction of inflammatory gene expression, and 3) TNFα and IL-1β mediated reduction in astrocytic glutamate transporters resulting in impaired glutamate clearance from the synaptic cleft.43 NMDA receptor blockade is therefore an attractive therapeutic strategy, however, antagonists have failed in clinical TBI trials due in part to a limited therapeutic window, off-target neurotoxicity, and as a result of inhibiting normal synaptic function and plasticity.44 In response to TBI and glutamate toxicity, high levels of the endogenous neuroprotectant adenosine is produced from breakdown of adenosine triphosphate and mRNA.45 Activation of the adenosine A1 receptor after TBI has anti-excitotoxic46 and anti-inflammatory effects in mice,47 however systemic administration of adenosine to patients may result in bradycardia and hypotension. A variety of adenosine related strategies are being actively investigated to mitigate excitoxicity and various facets of acute and chronic neuroinflammation.48
Mitochondrial dysfunction and reactive oxygen species (ROS) generation, caused by direct and indirect injury after TBI, has also been identified as a trigger of neuroinflammation.49 Translocation of the phospholipid cardiolipin from the inner to outer mitochondrial membrane, shown to occur after experimental TBI, tags damaged mitochondria for mitophagy but may also be a final pathway for inflammasome activation.50,51 Failure of mitophagy and resultant cell death can lead to release of mitochondrial DAMPs as reported for mitochondrial DNA after TBI in children.52 These mitochondrial danger signals produce local and systemic responses by the interaction with receptors on immune cells: mitochondrial DNA by TLR9 on dendritic cells and N-formyl peptides by formyl peptide receptor-1 on neutrophils.53 Membranes with mitochondrial cardiolipins on their surface are engulfed via cluster of differentiation 36 (CD36)-dependent phagocytosis.54 There is a paucity of data regarding CD36-mediated inflammatory response after TBI, however, CD36 plays a beneficial role in neurological outcome in patients with intracranial hemorrhage.55
In addition to inflammatory triggers released from neurons and glia, trauma to the vasculature can lead to leakage of blood components into the cerebral parenchyma, including complement and the potent neurotoxin and immune modulator cell-free hemoglobin (fHb).56 Complement factors have been detected in brain tissue57 and CSF58 of patients within hours of severe TBI, and have been found to correlate with BBB permeability. Although required for normal wound healing, evidence from murine models59–61 suggests acute dysregulation of complement may cause secondary injury after TBI (for review:62). Inhibition of alternative complement pathway63 or the membrane attack complex64,65 in a weight-drop model of TBI in mice reduced neurodegeneration and axonal loss, and improved neurologic outcomes. Also released into contused areas of brain, fHb-haptoglobin complexes are cleared by CD163 receptors on microglia and macrophages with resultant differentiation to an anti-inflammatory phenotype.66 If the haptoglobin-CD163 pathway is dysfunctional or is outcompeted by the amount of fHb present, fHb and its breakdown products heme and iron can induce direct neuronal toxicity by generating ROS and scavenging nitric oxide (NO).67 This pathway is implicated in the development of post-traumatic epilepsy in rodents.68 CSF levels of soluble CD163 and the iron-binding protein ferritin are increased after TBI in children and correlate with injury severity and unfavorable outcome.69 Thus, inflammation triggered by fHb and its degradation products could be therapeutic targets after TBI.
Several of the biochemical and molecular mechanisms of secondary injury listed above have been reported in blast-induced mTBI. Characterized by axonal, periventricular, and hippocampal neuronal injury, blast-induced mTBI is associated with cytokine and chemokine release, adenosine production (likely from mRNA breakdown), and activation of microglia.70,71 Promising neuroprotective effects were demonstrated with the anti-inflammatory drug minocycline in this model.72
B. Cellular mechanisms regulating acute neuroinflammation following TBI
i. Dynamics of cellular response to TBI
The first circulating immune cells to infiltrate the CNS after trauma are neutrophils, which typically peak in mice within 24–48 hours before rapidly declining.73,74 Diapedesis between endothelial cells is dependent on binding of integrins to vascular adhesion molecules, and within 4 hours of experimental TBI the expression of neutrophilic vascular adhesion molecules endothelial (E)-selectin (CD62E) and intracellular adhesion molecule-1 (CD54) is increased on endothelium of the injured hemisphere.75 Administration to mice of antibody to the CD11d/CD18 integrin, located on cell surface of neutrophils and monocytes, reduced leukocyte infiltration to the CNS as well as the systemic inflammatory response to TBI (Box 1).76,77 Chemokine gradients are established (e.g. C-C motif chemokine ligand 2 [CCL2]) that attract monocytes from the circulation to injured brain where they differentiate into macrophage subpopulations distinguished by relative cell-surface expression of the chemokine receptors, C-C motif chemokine receptor 2 (CCR2) and CX3CR1 (inflammatory monocytes: CD11b+CD45hiCCR2+Ly6Chi | patrolling monocytes: CD11b+CD45hiCX3CR1+)78. Chemokines and their receptors play several crucial roles in response to TBI, and the reader is referred to several excellent reviews on this topic: 8,9. Studies of monocyte infiltration in mice have demonstrated accumulation within the lesion through 3 days post-injury.79,80 Dendritic cells (DCs), T lymphocytes and natural killer cells are similarly recruited during this period,81 but at lower numbers.
Box 1. Systemic Inflammatory Response Syndrome and the Compensatory Anti-Inflammatory Response.
In this review we focus primarily on the neuroinflammatory response to TBI. A systemic inflammatory response syndrome (SIRS) and compensatory anti-inflammatory response have also been described after isolated TBI that may increase risk of nosocomial infection or multiple organ dysfunction. Via the sympathetic and parasympathetic nervous system, glymphatic and lymphatic clearance, hypothalamic-pituitary-adrenal axis, and disrupted blood-brain-barrier, there are several pathways for CNS injury to affect the peripheral immune response. In addition, therapeutic agents routinely used in neurocritical care such as sedatives, antiepileptics, and hyperosmolar agents may affect peripheral immune function. Age appears to be an important factor, for example early neutrophilia in adults is associated with significantly greater oxidative burst activity219 whereas neutrophils in children with TBI have significantly reduced ROS generation.220 Perhaps the most important factor influencing the characteristics of the systemic inflammatory response to TBI is time from injury. Although few studies have carefully studied the time course of peripheral immune function, there appears to be a marked immunosuppressed state at ~ 1 week out from TBI that corresponds to the time of peak nosocomial infection rate. For excellent review and future directions, the reader is referred to: 221.
Concurrently within the CNS, astrocytes, a vital regulator of CNS inflammation, undergo reactive astrogliosis characterized by morphological and functional adaptations including up-regulation of GFAP and production of cytokines and chemokines that further recruit and activate immune cells (for review: 82,83). YKL-40, a marker of reactive astrocytes, is significantly elevated in the CSF of adults with severe TBI on day 2 and peaked on day 4 post-injury (Table 3). Microglia undergo a similar transformation in morphology and function with an initial peak approximately 7 days post-injury.66,84,85
Table 3.
Human Studies of Neuroinflammation after TBI: Cellular Mediators
| Inflammatory mediator | Tissue / Fluid | Time Course | Association with clinical outcome(s) | Other | Ref |
|---|---|---|---|---|---|
| Cellular mediators | |||||
| Microglia | Tissue (path) | Proliferating microglia observed after 72h Peak 3mo Extensive amoeboid CR3/43 and CD68 immunoreactive cells seen in ~25% of cases surviving >2wk and up to years after TBI, particularly with DAI |
Unknown | Associated with ongoing white matter degeneration. May be influenced by IL-1 genotype |
6,183,184,187,258 |
| Tissue (image) | Increased [11C]DPA -713 binding to TPSO 24–42yr since NFL play Increased [11C](ROPK11195 binding to TPSO in thalami, putamen, occipital cortex, and internal capsule years after moderate to severe TBI |
Adults: Higher PK binding associated with more severe cognitive impairment | Observed atrophy of hippocampus | 185,188 | |
| Astrocytes | CSF | YKL-40 (reactive astrocytes) elevated day 1, peak day 4 | Adults: Trend to association with outcome | Associated with CSF IL-1β, TNFα, and CRP | 259 |
| Tissue | Increased GFAP in ipsilateral and contralateral cortex at 6–122h | Unknown | Anti-GFAP antibodies detectable in serum | 6,260 | |
Abbreviations: TBI – traumatic brain injury; CD – cluster of differentiation; DAI – diffuse axonal injury; IL – interleukin; TPSO – translocator protein; NFL – National Football League; CSF – Cerebrospinal fluid; TNF – tumor necrosis factor; CRP – C-reactive protein; GFAP – glial fibrillary acidic protein
ii. Pro and anti-inflammatory roles of microglia
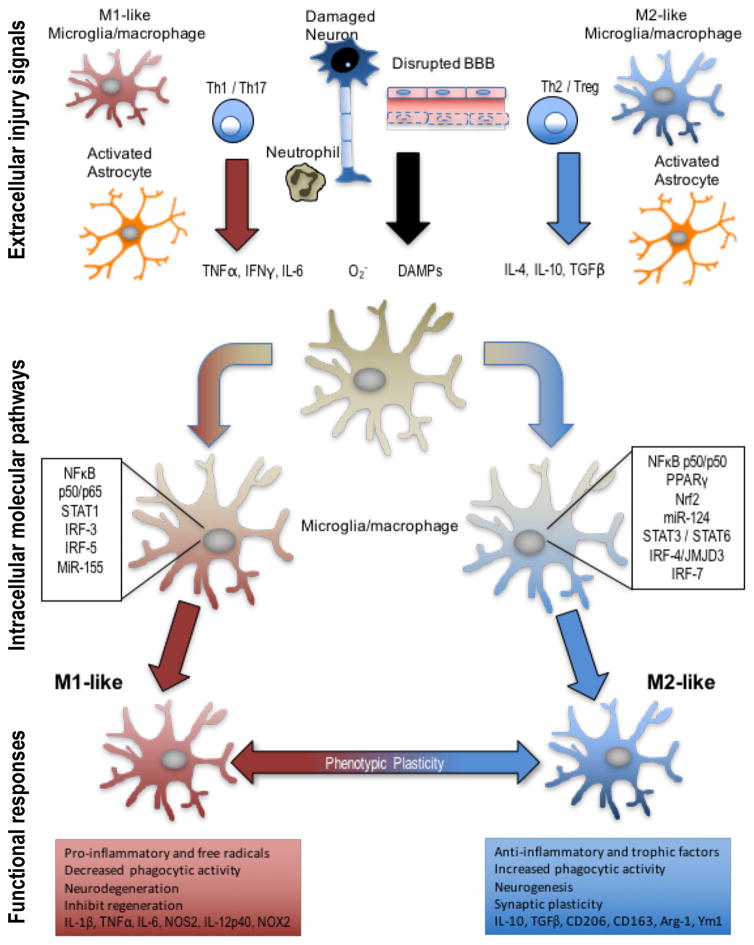
The concept of post-traumatic neuroinflammation as a “double-edged sword”86, with both beneficial and injurious effects, has recently been expanded to include the function of microglia.87,88 Similar to peripheral macrophages, microglia respond to changes in their microenvironment to become polarized along an activation spectrum ranging from classical M1-like to alternative M2-like (Figure 2).89 This concept has evolved from the canonical M1/M2 subset classification to reflect mixed-phenotypes and the functional plasticity of tissue macrophages / microglia to changes in the microenvironment. Stimulation by DAMPs, free radicals, or pro-inflammatory cytokines such as interferon-(IFN)γ induce a M1-like phenotype characterized by production of pro-inflammatory cytokines (e.g. IL-1β, TNFα), chemokines (e.g. CCL2, CXCL9), ROS generation, and reduced phagocytic activity.89–91 Although M1-like ‘pro-inflammatory’ cells are often presumed to be harmful, a well-regulated M1-like response may be neuroprotective after TBI. An exaggerated or prolonged M1-like response, however, can lead to secondary brain injury and drive a self-propagating hyperinflammatory state.92,93 The M2a-like ‘alternative’ phenotype89–91, in response to IL-4 and IL-13 stimulation, is associated with production of anti-inflammatory cytokines and increased phagocytic activity.90,91 The M2c-like ‘deactivated’ phenotype occurs in response to IL-10, glucocorticoids, or uptake of apoptotic cells regulates tissue repair and remodeling.90,91 Lastly, the M2b-like ‘intermediate’ phenotype is stimulated by immune complex exposure or TLR ligands89–91 and has both pro- (IL-1, IL-6, TNFα) and anti-inflammatory (IL-10) effects.90,91 The degree to which microglia assume a particular phenotype (or multiple phenotypes) is dependent upon these and other changes in the lesion microenvironment driving complex intracellular signaling pathways, influenced by genetic and epigenetic factors, that may offer additional opportunities for therapeutic intervetion.91,94
Figure 2. Extracellular injury signals and intracellular molecular pathways control polarization of microglia and macrophages following TBI.
Molecular signals from injured tissue can drive phenotypic and functional responses in microglia/macrophages after TBI. DAMPs released by injured neurons, pro-inflammatory or oxidative mediators released by infiltrating immune cells including TNFα, IFNγ, IL-6, and O2− can polarize cells towards an M1-like phenotype. M1-like populations are characterized by expression of proteins such as IL-1β, TNFα, IL-6, NOS2, IL-12p40, and NOX2. Molecular pathways that regulate the M1-phenotype include STAT1, IRF-3/5, NFκB p50/p65 and miR-155, among others. M1-like microglia and macrophages release pro-inflammatory factors and free radicals that promote chronic neuroinflammation, oxidative stress and neurodegeneration, and inhibit regeneration. In response to anti-inflammatory and neurotrophic signals microglia and macrophages can be polarized towards an M2-like phenotype, characterized by expression of proteins such as CD206, CD163, Arginase 1, FCγR, Ym1, IL-10, and TGFβ. Molecular pathways that regulate M2-like phenotypic transitions include STAT6/3, IRF-4/7, NF-κB p50/p50, Nrf2 and miR-124, among others. M2-like microglia and macrophages release anti-inflammatory and trophic factors that resolve inflammation. They also have increased phagocytic activity, and improve brain repair by modulating neurogenesis, axonal regeneration, synaptic plasticity, and angiogenesis. Microglia and macrophages demonstrate significant plasticity and can switch between M1- and M2-like phenotypes. Moreover, it is recognized that following TBI they present mixed phenotypes during the acute phase post-injury, and transitions to an M1-like dominant phenotype in the chronic phase after TBI.
Abbreviations: TBI, traumatic brain injury; DAMP, damage-associated molecular pattern; TNF, tumor necrosis factor; IFN, interferon; IL, interleukin; NOS, nitric oxide synthase; NOX, nicotinamide adenine dinucleotide phosphate oxidase; STAT, signal transducer and activator of transcription; IRF, interferon regulatory factor; CD, cluster of differentiation; TGF, transforming growth factor; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells
Microglial polarization has been shown to vary over time and between different TBI models. In mice, activated microglia demonstrate a bimodal increase after focal contusion with an initial M2-like peak at 7 days followed by an M1-like peak at 21–28 days; though, the bulk of activated microglia have mixed M1-/M2-like activation markers.81,84,93 In diffuse brain injury, M1-/M2-like polarization dynamics are strikingly different, likely due to altered cellular immune responses that include reduced neutrophil infiltration and restricted macrophage/microglial accumulation to white matter regions that incurred greatest damage. Diffuse brain injury results in transient increases in IL-1β, TNFα, and CD14 expression in the cortex and hippocampus of mice as early as 4 hours post-injury that return to baseline by 72 hours.95 In addition, iNOS+/Arginase1+ microglia/macrophages are also increased at 24 hours post-injury,96 indicating that diffuse injury also up-regulates mixed M1- and M2-like activation markers. However, the functional role of M1-/M2-like phenotypes in axonal injury and repair following diffuse brain injury remains to be elucidated.
iii. Links to adaptive immune response
The adaptive immune response mediated by T cells and B cells can strongly influence microglia phenotype and function, but the role of the adaptive immune system after TBI remains rather unclear. T cells infiltrate injured tissues after CNS injury and sequestration of lymphocytes in lymph nodes by FTY720 administration results in reduced inflammation and better recovery in rodents with spinal cord injury.97–99 However, FTY720 also acts directly on CNS cells complicating data interpretation. On the other hand, mice deficient in T cells (due to deficiency of RAG or MHCII genes) have worse outcomes in CNS injury models,100,101 suggesting a dominant neuroprotective effect of T cells.
Somewhat counter-intuitively, activation of autoimmune T cells in mice that provoke myelin- targeted encephalitis provides protection from secondary neurodegeneration in CNS injury, coined ‘protective autoimmunity’.101–104 One mechanism for this protection may be T cell production of neurotrophic factors that act on neurons and astrocytes to promote survival and repair.105,106 T cells are required for normal CNS development, as mice deficient in T cells show cognitive and behavioral developmental abnormalities, suggesting that T cells also contribute to the development and perhaps maintenance of the healthy brain.107 As well as regulating the M1/M2-like balance, T cell-produced IL-4 protects neurons through potentiation of neurotrophin signaling.100 Unusually, IL-4-mediated T cell protection of injured CNS tissue does not appear to require antigen-specific receptor activation of T cells, and neurons directly induce IL-4.100 The IL-1 family alarmin IL-33 is released from damaged cells, and is also neuroprotective after CNS injury in mice.108 IL-33 is known to act on Th2 cells that produce IL-4;109 hence IL-33 may provide a link between CNS injury and activation of IL-4 production. An IL-33-responsive population of tissue-resident regulatory T cells has been identified in muscle110,111 and gut of mice,112 and contributes to resolution of inflammation and wound repair in those tissues. It is intriguing to speculate that a similar IL-33-Treg axis could operate in human brain after TBI.
Specific mechanisms of T cell mediated protection versus damage need to be precisely targeted to produce benefit. The methods used to invoke a CNS injury-protective autoimmune response are also used to induce the rodent model of multiple sclerosis, experimental autoimmune encephalomyelitis (EAE). Th17 cells, named because of their production of IL-17 along with other pro-inflammatory cytokines, are thought to drive inflammatory demyelination of the spinal cord in EAE.113 Th17 cells and other ‘type 17’ T cells have been associated with myriad autoimmune and inflammatory conditions114 but have not yet been investigated in TBI. Type-17 responses are promoted by cytokines known to be released after TBI in humans, particularly IL-1β, and induce CXCL8 and neutrophil recruitment. In ischemic stroke, harmful IL-17 is largely produced by ‘type-17’ γδT cells that rapidly infiltrate the injured brain.115 These cells are strongly influenced by the remote gut environment, as antibiotic-induced dysbiosis of gut microbial flora resulted in protection from stroke that could be linked to reduced frequencies of IL-17+ γδT cells.116 The profound impact of the gut microbiome on peripheral tissue immune responses, including the CNS, is a recurring theme in immunology.117–119 CNS-gut communication may also influence cognition, mood and anxiety.120,121 It is thus possible that antibiotic administration or changes in diet associated with intensive care unit hospitalization after severe TBI could inadvertently alter this gut microbiome-brain-inflammation axis.
Lymphatic drainage of body tissues regulates interstitial fluid and removal of waste products. The lymphatics also support immune surveillance by carrying macromolecules and activated dendritic cells bearing foreign antigens to local lymph nodes where they can be presented to activate the adaptive immune response. This may represent a critical step, since naïve T and B cells typically circulate through lymph nodes via blood and efferent lymphatics but do not enter non-lymphoid tissues until primed. Until recently, the brain was considered an immune privileged site with lack of lymphatic drainage supporting the blinding of the peripheral immune system to ongoing events in that tissue. However, adaptive immune responses are primed and recruited following CNS injury, and waste products must be rapidly cleared from this highly metabolic organ. Technological advances in imaging that allowed for interrogation of brain drainage in closed skull systems have resolved these paradoxes. Two most likely intercepting systems that drain brain tissue have been delineated in mice. The ‘glymphatic system’, describes the astrocyte-regulated convective bulk flow of CSF from the paravascular space through interstitial fluid in an arterial-venous direction.122,123 This flow allows for rapid entry of small molecules, and perhaps more importantly for fluid drainage and clearance of metabolites, soluble proteins and waste products including beta amyloid from the brain interstitial space.122,124,125 Glymphatic flow is greatly increased during sleep, associated with increased brain interstitial space volume; this can be partly attributed to mechanical mechanisms as lateral posture in awake mice replicated the increased flow compared to upright posture.126,127 The second CNS clearance system consists of lymphatics that line the dural sinuses and meningeal arteries.128,129 These vessels have classical lymphatic architecture and drain to the deep cervical lymph nodes—providing a direct conduit between the brain and the peripheral immune system. They also contain immune cells and macromolecules, mimicking peripheral lymphatics. Brain lymphatics include populations of T cells and B cells,129 which have presumably migrated through and surveyed the brain tissue.
TBI impairs the glymphatic system drainage in rodent models,130 resulting in accumulation of damage and waste products such as Tau,124 and providing a potential link between injury-induced disruption of glymphatic drainage and development of CTE. Inflammatory astrocyte activation may amplify the effects of mechanical damage on glymphatic flow after TBI. Effects of TBI on brain lymphatic drainage to deep cervical lymph nodes have not yet been investigated, but one could envision that TBI would readily alter the associated lymph vessels. Accumulation of waste products due to impaired lymphatic drainage might trigger neuroinflammation by activating pattern recognition receptors on microglia. The interaction between altered lymphatic drainage and neuroinflammation and ensuing long-term consequences therefore warrants further investigation.
C. The impact of secondary insults on the acute inflammatory response to TBI
A critical determinant of outcome after TBI, particularly in severe TBI, is the presence of a concurrent secondary insult such as polytrauma, hypotension, and/or hypoxemia. With severe TBI, secondary insults occur in as many as two-thirds of victims.131 These insults are frequently hemorrhagic in nature, compromising perfusion and oxygen delivery to the injured brain.132 Analysis of >2000 patients with severe TBI revealed a mortality rate of 72% for combined injury vs. 46% for TBI alone.133
Despite the importance of polytrauma and secondary insults in TBI, there has been little study of their impact on the cerebral or systemic inflammatory responses in both pre-clinical and clinical investigations. Although one might anticipate that polytrauma and/or secondary insults, by superimposing tissue hypoxemia and/or ischemia onto the traumatic insult, would amplify the local inflammatory response in brain, surprisingly that has not been observed. Instead, both pre-clinical and clinical studies have revealed that second insults shift the cytokine response to a more anti-inflammatory phenotype, amplifying the IL-10 response. Shein et al.134 studied the impact of a brief period of severe hemorrhagic shock (HS) after controlled cortical impact TBI in mice. The combination of TBI plus HS led to nearly 100-fold and 30-fold increases in serum IL-10 levels vs. TBI or HS alone. Also, six pro-inflammatory cytokines and chemokines, namely IP-10, TNFα, CXCL1, CCL2, CCL3, and CCL11 were all increased in serum after TBI alone but not after TBI plus HS. In addition, animals with combined TBI and HS had lower serum IL-6 vs. TBI alone. However, despite worsening of both long term behavioral and histological outcomes by HS after TBI,135 the local cytokine and chemokine responses in brain were not appreciably altered.
Clinical data, in general, parallel these pre-clinical findings. Relative to patients with TBI alone, patients with TBI plus polytrauma have increased serum concentration of the anti-inflammatory agents IL-10, IL-1ra, an sTNFr-I and no change in pro-inflammatory cytokines IL-1β and TNFα.136 Kumar et al.137 carried out a trajectory analysis of cytokines and adhesion molecules in serum and CSF after severe TBI in 114 adults. Again, serum IL-10 levels were higher among individuals with TBI plus polytrauma versus isolated TBI. It remains unclear, however, if all types of secondary insults produce a similar shift to an anti-inflammatory phenotype, or whether HS confers a unique effect.
Indeed, several forms of peripheral injury such as skeletal fracture or hepatic contusion may increase the circulation of pro-inflammatory cytokines in patients. To address the effect of peripheral injuries on TBI outcomes, combined models that incorporate long-bone fracture have increased in use.138,139 Shultz et al.140 reported findings on a mouse model of tibia fracture plus diffuse brain injury in which mice with combined injury exhibited increased anxiety-related behavior and brain atrophy. Associated with these outcomes, the combined injury group had evidence of increased astrogliosis, neutrophil infiltration, and brain tissue IL-1β relative to mice with isolated fracture or TBI. Similarly, the systemic administration of pro-inflammatory mediators IL-1β141 and lipopolysaccharide142 in rodent models of diffuse TBI exacerbate the neuroinflammatory response, result in larger contusion volume, and worsen behavioral outcomes. Whether this was mediated directly via binding to receptors on microglia and astrocytes, or through effects such as hypotension or hyperthermia may confound the results of these studies.
Finally, there has been limited study of the impact of secondary insults in mTBI. Titus et al.143 reported that a brief period of imposed hyperthermia to 39°C beginning 15 min before and continued for 4 hours after mild fluid percussion injury (FPI) in rats, produced cognitive deficits despite the use of an injury level that was otherwise devoid of cognitive deficits. Cooling back to normothermia at 15 min after TBI prevented development of the deficits. Amplification of neuroinflammation by hyperthermia was implicated. Given the prevalence of concussions during the summer months in training camps for sports such as football, this observation if translated to humans could be important.
D. Inflammation-mediated neurogenesis, gliogenesis, and angiogenesis
Neuronal death after TBI may be mitigated by an increase in neuronal progenitor cell (NPC) proliferation, migration to injured brain regions, differentiation to neurons, and integration into neural networks.144 Similar to the dual effects of inflammation on secondary brain injury, experimental evidence suggests that inflammatory mediators are a key component of neurogenesis and may support or hinder NPCs at multiple steps. For example, microglia stimulated to an M1-like phenotype with LPS reduce adult hippocampal neurogenesis in the mouse,145 an effect similarly seen with pro-inflammatory cytokines TNFα, IL-1β, and IL-6.146 This was reversed by treatment with minocycline145 or indomethacin.147 In contrast, M2-like microglia, stimulated by IL-4 or low-dose IFN-γ, release neurotrophins such as insulin-like growth factor-1 (IGF-1) and induce neurogenesis.148 This effect was seen in mice with addition of a running wheel to the cage after TBI, simulating clinical rehabilitation, which reduced M1-like microglial activation and was associated with increased production of IGF-1 (as well as IL-10 and brain-derived neurotrophic factor) to increase neurogenesis and improve cognitive outcomes.149 NPCs also express chemokine receptors, such as CCR2 and CXCR4, and chemokines may direct their migration to the area of injury.150
Brain atrophy increases over time after TBI,151–157 and yet most survivors of TBI will show a temporally linked degree of functional recovery.158 This recovery represents brain plasticity and reorganization, in addition to recovery of function of existing neuronal pathways. Although data from TBI models are limited, experiments modeling other forms of brain injury suggest neural-immune interactions may be critical to forming and strengthening new synaptic connections.159–161 The degree of activation and the local inflammatory milieu likely define whether any particular cytokine or inflammatory cell type benefits or disrupts brain plasticity. For example, in a GFAP-IL-6 transgenic mouse model, over-expression of IL-6 caused a significant reduction in long-term potentiation (LTP) in the hippocampus.159 However, when anti-IL-6 is used to block basal levels of IL-6 signaling, there is a significant prolongation of LTP and improved long-term memory.162 Elevated IL-1β also impairs LTP but surprisingly promotes neurite outgrowth and is synergistic with neurotrophin-3.163 In rats subjected to repetitive mTBI, activation of microglia was associated with inability to induce LTP, attenuated NMDA-mediated signal, and impaired memory–these effects were not seen after single mTBI.164
Microglial polarization and the local inflammatory milieu may also influence repair through activation of angiogenesis and gliogenesis. Although evidence from TBI models is scant, experimental autoimmune and hypoxic/ischemic brain injury suggest M1-like microglia impair oligodendrogensis, oligodendrocyte maturation and viability by a TNFα-dependent mechanism.94,165 In contrast, M2-like microglia or conditioned media from M2-like microglial culture promote oligodendrogenesis and remyelination in these models. M2-like microglia may also, via production of pro-angiogenic cytokines (e.g. TGFβ) and growth factors, induce angiogenesis and vascular repair. Whether these findings translate to recovery from TBI in humans is unknown, however treatment with pro-angiogenic growth factors released by M2-like microglia is neuroprotective in mice and promotes neurogenesis and angiogenesis in experimental TBI.166
E. Clinical experience of agents impacting acute neuroinflammation
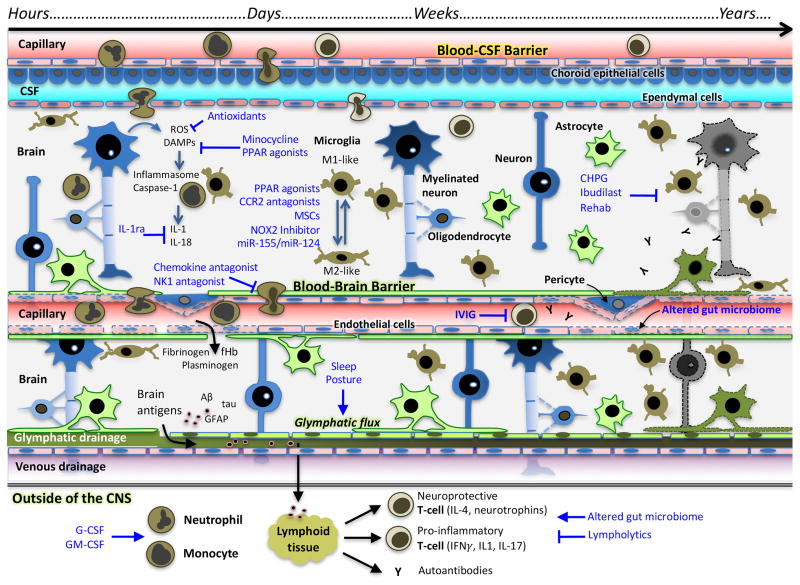
A key question arises, is TBI-responsive neuroinflammation a clinically relevant therapeutic target (Figure 3)? As described above, numerous pre-clinical studies suggest this is the case. However, few clinical trials of therapies primarily targeting inflammation have been reported. Corticosteroids, surprisingly, have been the least successful anti-inflammatory class of drugs in TBI (Table 3). Despite the potent effects on suppressing inflammation, high dose methylprednisolone (5 mg/kg/day),167 “megadose” dexamethasone (100 mg),168 “ultrahigh dose” dexamethasone (2.3 g),169 the aminosteroid tirilazad,170 and a trial of hydrocortisone and fludrocortisone (primary outcome hospital acquired pneumonia)171 all failed to demonstrate benefits on neurological outcome. Off-target effects with systemic administration of corticosteroids likely impact outcomes, and in the case of tirilazad, limited brain exposure may have been a confounder.172
Figure 3. Novel therapies for TBI targeting inflammation at different time points from injury.
Therapies targeting TBI-responsive inflammation may be effective at different time points depending on the therapeutic target(s). Similarly, design of pre-clinical and clinical trials of anti-inflammatory agents should note that inflammation causing secondary injury at one time-point may be protective at others. Initially, inflammation triggered by release of DAMPs and ROS generation can be blocked through the use of antioxidants, minocycline, and PPAR agonists, among others. Inflammasome activation will cause release of IL-1β, the action of which can be inhibited at IL-1 receptors with IL-1ra (Anakinra). Over the next several hours-days, invasion of CNS by circulating immune cells will contribute to neuroinflammation, and this process can be inhibited by therapies such as NK1 antagonism and chemokine antagonists. Microglial polarization to M2-like phenotype has been shown to be neuroprotective. M1-like phenotype, which peaks ~7 days from injury, is proinflammatory and associated with secondary injury. The M2-like phenotype can be promoted by MSC, PPAR agonists, and CCR2 antagonists, among other possibilities. The adaptive immune response peaks days after injury. T-cells must be primed to enter CNS – this may be inhibited by therapies such as IVIG. Additionally, alterations in gut microbiome may affect the relative number of pro- and anti-inflammatory T-lymphocytes. Glymphatic clearance may be impaired after TBI, which may lead to impaired clearance of pro-inflammatory mediators. Investigations are ongoing to determine ways to improve glymphatic flow, however it has been shown to be maximized during sleep. Chronic microglial activation may develop and lead to chronic neurodegeneration, encephalopathy, and dementia. Activation of the mGluR5 on microglia, such as with CHPG, attenuates M1-like microglial activation. Rehabilitation and exercise have also been shown to reduce M1-like microglial activation.
Abbreviations: TBI, traumatic brain injury; CSF, cerebrospinal fluid; ROS, reactive oxygen species; DAMP, damage-associated molecular pattern; BBB, blood brain barrier; PPAR, peroxisome proliferator-activated receptor; IL, interleukin; MSC, mesenchymal stem cell; CHPG, (RS)-2-Chloro-5-hydroxyphenylglycine; IVIG, intravenous immunoglobulin; IFN, interferon; fHb, free hemoglobin; GFAP, glial fibrillary acidic protein
Other anti-inflammatory strategies have been evaluated in humans including testing of the bradykinin B2 receptor antagonist Anatibant, which produced a trend toward worse outcome in 228 patients enrolled.173 A provocative randomized controlled trial (RCT) used recombinant human granulocyte colony stimulating factor (G-CSF) to enhance the cellular inflammatory response.174 Although the primary outcome in this study was the incidence of nosocomial infection, and the number of patients was low, no differences in mortality or hospital length of stay were detected between G-CSF treated and placebo groups, nor was there a difference in primary outcome. Minocycline has shown promise in a phase II trial in patients with spinal cord injury;175 however, it has not been reported in human TBI and pre-clinical data are equivocal.176 Of note, all of the studies targeting inflammation after TBI have been performed in adult patients. Given studies showing an association between heightened inflammation and younger age in children with severe TBI, anti-neuroinflammatory strategies may be more impactful in the developing brain.69,177
Inferences can also be made extrapolating from clinical trials using multi-faceted therapies with anti-inflammatory consequences. The anti-inflammatory effects of hypothermia were touted as one of its main modes of efficacy.178 Disappointingly, despite single center studies in adults with severe TBI showing reduction of IL-1β in CSF,179 multicenter RCTs of therapeutic hypothermia after TBI have failed to show benefit in adults180,181 or children.11,12 Progesterone, which blunted the neuroinflammatory response to trauma in mice, was evaluated in two large multicenter RCTs13,14 of adults with moderate-severe TBI and failed to show benefit in 6-month GOS or mortality.
These clinical studies suggest that non-selective attenuation of the inflammatory response early after severe TBI is not beneficial, or possibly detrimental. The existing literature lacks studies using targeted, single pathway anti-inflammatory strategies in humans, and more personalized approaches that individualize treatments to genotype, inflammatory biomarkers, timing and duration of therapy, patient age and sex. Identification of specific patient subsets, for example the study by Diamond et al.182 that identified an IL-1β gene variant associated with risk of post-traumatic epilepsy, to target enrollment criteria for clinical studies may favorably influence their success.
Furthermore, it is unclear whether inhibiting inflammation after mild or repetitive mild TBI acutely may prevent chronic sequelae such as CTE. Raising the key questions, does a single exposure, or multiple exposures, to TBI prime the brain for chronic neuroinflammation, and accordingly would impacting the inflammatory response early after mTBI, or targeting the immune response late, represent clinically relevant approaches? Finally, from a therapeutic perspective, given the aforementioned benefit of strategies mimicking rehabilitation on neuroinflammation neurogenesis and cognitive outcome, it is possible that optimal enhancement of beneficial aspects of neuroinflammation, rather than inhibiting detrimental effects, could represent a more successful avenue for future clinical investigation.
III. CHRONIC NEUROINFLAMMATION
A. Chronic neuroinflammation after TBI: innocent bystander or driver of pathology?
As discussed, after TBI an acute inflammatory response is elicited that one might expect would resolve to a resting state, prepared for the next inflammatory trigger. However, in a subset of patients, chronic neuroinflammation may develop and last for years after injury.183–186 The proportion of patients in whom chronic inflammation will develop, the dominant triggers and intracellular pathways propagating inflammation, and genetic susceptibilities to chronic inflammation are under active investigation.
An examination of autopsy specimens from patients surviving >1 year after TBI, and in cases up to 18 years, revealed a significant increase in amoeboid microglia in subcortical white matter tracts versus control tissue.184,187 Activated microglia were observed in 28% of the autopsies and was associated with thinning of the corpus callosum.184,187 These findings are supported by positron emission tomography (PET) imaging studies using translocator protein (TSPO) ligands, which likely bind activated microglia, to examine chronic neuroinflammation in TBI survivors.185,188 In one study, diffuse [11C]R-PK11195 (TSPO ligand) binding was found in adults with moderate to severe injury up to 17 years later in areas remote to the trauma including thalamus, putamen, and the occipital cortex.185 Inflammation in the thalamus was associated with more severe cognitive impairments.185 The 2nd generation TPSO ligand [11C]DPA-713 was used to study retired National Football League (NFL) players with self-reported history of career concussions. The supramarginal gyrus and right amygdala exhibited ligand binding to levels greater than seen in age matched controls.188 Serum cytokines may also demonstrate a chronic immune activation state after TBI. For example, a prospective TBI biomarker study reported chronically elevated expression of TNFα in serum after TBI and association of increased TNFα with unfavorable long-term neuropsychiatric outcomes.189
Experimental studies substantiate the clinical evidence of a chronic inflammatory state after TBI, and indicate underlying molecular mechanisms and potential therapeutic strategies.164,190–194 Chronic microglial activation with cell surface markers MHC II, CD68, and NADPH oxidase (NOX2) is seen one year after moderate to severe contusion.92 These markers would indicate M1-like phenotype, with pro-inflammatory cytokine production and reduced phagocytic activity that would be less effective at protective functions such as Aβ clearance. Over the course of the year, mice demonstrate progressive neurodegeneration with enlarging lesion volume, persistent oxidative stress, demyelination, and cognitive impairments. Chronic neuroinflammation is also observed in several repetitive mTBI models. Like the acute inflammatory response to mild repetitive injury, microglia are characteristically localized to white matter tracts and may be seen in those regions bordering degenerating axons with associated neurobehavioral changes 12–18 months after injury.164,191,195–198
There is interest, therefore, in the development of pharmacologic and non-pharmacologic approaches to reduce chronic neuroinflammation after TBI as a therapeutic strategy, greatly expanding the window for targeted interventions. This concept has been examined in pre-clinical studies, for example, with the selective metabotropic glutamate receptor 5 agonist (RS)-2-chloro-5-hydroxyphenylglycine (CHPG), previously shown to reduce microglial activation199 and improve functional recovery200 when given acutely after trauma. Mice given CHPG at 1 month after focal brain injury had improved neurological recovery, decreased neuroinflammation, arrested lesion expansion, sparing of white matter, and reduced neurodegeneration at 4 months.201 Similarly, although with a more generalized anti-inflammatory approach, administration of the phosphodiesterase inhibitor ibudilast on days 30–34 after FPI in rats reduced anxiety-like behavior and gliosis at 6 months.202 Exercise regimens that simulate physical rehabilitation may modulate neuroinflammation and promote release of neurotrophic factors after TBI. Piao et al.149 found that a 4-week treatment with voluntary exercise attenuated IL-1β gene expression and chronic microglial activation, increased production of IL-10 and neurotrophic factors, improved behavioral outcomes, and reduced lesion volume.149 Importantly, the authors compared two start dates for the exercise regimen which was only effective if delayed to 5 weeks after injury and was potentially pro-inflammatory when initiated at 1 week post-injury. Thus, accumulating pre-clinical research indicates that chronic neuroinflammation and related neurodegeneration can be treated weeks after TBI, which suggests exciting potential for clinical translation of delayed anti-inflammatory therapies.
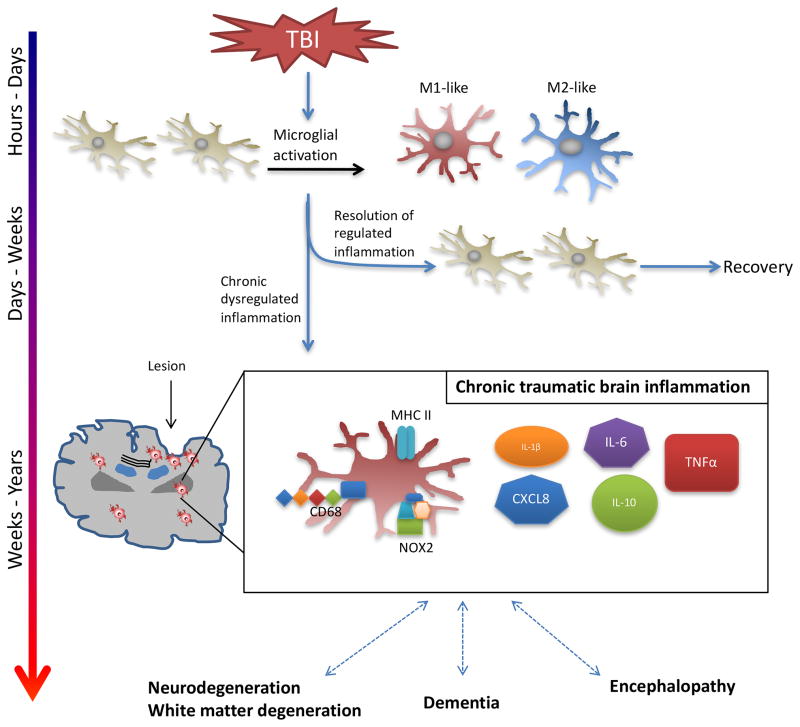
B. Progressive neurodegeneration following single and repetitive brain trauma
Accelerated neurodegeneration and CTE may occur following single or repetitive TBI, as has been reported in cases of athletes203 and military personnel3 with high incidence of head trauma and concussion.204 TBI increases the risk of developing dementia in some patients, specifically non-Alzheimer’s dementia, years after the initial injury.205–209 Recently, the role of chronic inflammation in the pathophysiology of neurodegenerative disorders has attracted considerable attention210,211 and led investigators to speculate about the role of post-traumatic neuroinflammation in mediating neurodegeneration, non-Alzheimer’s dementias, and CTE. Cases of CTE associated with repetitive mTBI have also shown activated microglia in perivascular regions of subcortical white matter and throughout the brain as the disease progresses.3,212,213 To date, however, comprehensive studies of neuroinflammation in patients with CTE have yet to be reported. Webster et al.214 investigated an early intervention with progesterone to prevent neurodegeneration after repetitive mTBI in rodents. Animals were administered three mild diffuse injuries, each separated by 5 days, and randomized to vehicle or progesterone for 15 days after the first injury. At 12-weeks post-treatment, a chronic time point in rodent TBI models, progesterone-treated rats exhibited improved neurocognitive outcomes, reduced brain atrophy, and attenuated neuroinflammation compared to repetitive mTBI plus vehicle. Based on these promising data, additional preclinical studies are warranted.
It remains unclear whether persistent inflammation initiates the characteristic neuropathology – formation of neurofibrillary tangles, phosphorylated TAR DNA-binding protein 43 (TDP-43) accumulation, and Aβ deposition – and should be targeted. Or, if accumulation of these abnormal proteins triggers the inflammatory response, though perhaps one ill-suited to restore normal function. Further research is required to advance our understanding of critical mechanisms underlying the chronic pathologies of TBI, including chronic neuroinflammation, and their relationship to development of neurodegenerative disease (Figure 4). Advances in clinical TBI neuroimaging, including use of selective PET ligands for amyloid,215,216 tau,217,218 and neuroinflammation,185,188 may clarify the mechanisms driving chronic neurodegeneration after TBI, and provide opportunities to develop targeted therapies for the long-term sequelae.
Figure 4. Chronic neuroinflammation contributes to chronic neurodegeneration, dementias, and encephalopathy after TBI.
Neuroinflammation and microglial activation are key mediators of repair and recovery from TBI. However, recent clinical and laboratory data have shown that TBI can cause persistent neuroinflammation and microglial activation, in some cases lasting many years, and lead to chronic neurodegeneration, dementia, and encephalopathy. Prospective studies of TBI biomarkers in adults with severe TBI have shown that serum levels of IL-1β, IL-6, CXCL8, IL-10, and TNFα are chronically increased. Experiments in animal models have demonstrated persistently increased numbers of microglia expressing MHC II, CD68, and NOX2 at the margins of the lesion and in the thalamus at 1-year post-injury associated with oxidative stress and white matter disruption. These inflammatory findings have been correlated with chronic neurodegeneration, the development of dementia, and encephalopathies – which may subsequently cause additional inflammation in a self-perpetuating deleterious feedback mechanism.
Abbreviations: TBI, traumatic brain injury; IL, interleukin; CD, cluster of differentiation; TNF, tumor necrosis factor
IV. CONCLUDING REMARKS
Advances in our understanding of TBI-responsive neuroinflammation have led to exciting new questions (Box 2), identified new therapeutic targets and expanded the time frame in which to consider treating. Clinical trials with therapies modulating inflammation after TBI are in their infancy – even in severe TBI – and therapies targeting neuroinflammation after mTBI in patients are completely unexplored. Nevertheless, thus far it appears that treating all patients with TBI using a broad-acting anti-inflammatory agent has not shown benefit in RCTs. Clearly, there is a need to define inflammatory phenotypes of our patients based on injury characteristics such as patient age, sex, genetic predisposition, presence or absence of secondary insults, and serum / CSF / imaging biomarkers. Such an approach will allow us to answer questions posited in our initial framework, including: how to target inflammation for clearance of debris, who will benefit from therapies to promote reparative aspects of inflammation, and when should therapies targeting chronic inflammation be initiated. This approach should be combined with enhanced pre-clinical trials, which 1) incorporate multiple injury models, injury severities, and secondary insults 2) define clinically-relevant therapeutic window(s) and treatment durations 3) expand outcomes to examine both harmful and protective aspects of inflammation and include acute- and chronic endpoints. Coupled with important new trials design strategies such as adaptive design, the result of this approach will be clinical trials targeting specific patients with personalized immunomodulatory treatments that we hope will reduce secondary injury, enhance repair, and improve patient outcomes.
Box 2. Outstanding Research Questions / Unmet Needs.
What is the level of acute inflammation needed for clearance of debris? How can it be determined?
Does the M1-/M2-like paradigm translate to human brain injury? Are there injury severity or regional differences in phenotype?
Can autoreactive adaptive immune responses be harnessed for benefit in TBI? Do Th17/IL-17 adaptive responses contribute to neurodegeneration in TBI?
Does the extent of damage to the CNS lymphatic drainage systems following TBI play a role in defining the magnitude of long-term neuroinflammation?
What mechanisms prime reactivity of glia acutely after TBI and sustain their immune activation for weeks, months and years? Will delayed interventions that modulate chronic microglial activation be effective for treatment?
How can we determine that the reparative processes are no longer beneficial and how should we facilitate return of the inflammatory process to a normal state?
Can therapeutic trials be targeted to inflammatory phenotypes or biomarkers?
Imaging biomarkers: There is an urgent need to identify new stable and selective PET ligands or MRI based methods to image neuroinflammation.
Table 4.
Human Studies of Neuroinflammation after TBI: Selected Clinical Trials
| Clinical Trials | ||||||||
|---|---|---|---|---|---|---|---|---|
| Therapy | Effects on Inflammation | Study / Design | N | Dose | Primary Outcome | Secondary Outcomes | Comments | Refs |
| Anatibant | Block bradykinin signaling, prevent BBB disruption | “Brain Trial” Multicenter RCT | 228 adults with GCS ≤ 12 | Low (10mg load, 5mg/d), Mid (20mg load, 10mg/d), High (30mg load, 15mg/d) vs. placebo | No difference in incidence of serious adverse events | Trend towards harm in discharge GCS, DRS, and HIREOS | Recruitment paused due to DSMB concerns Terminated due to withdrawal of funding |
173 |
| Cyclosporin A | Reduces T-cell counts and activation | Single center RCT | 38 adults with GCS ≤ 8 | 5mg/kg over 24h vs. 10mg/kg over 48h vs. placebo | No difference in T-cell counts in blood | No difference in incidence of infection | Reduced lymphocyte count on admission associated with worse outcome and increased respiratory infections | 261 |
| Dexanabinol | Inhibitor of TNFα NMDA antagonism |
Multicenter RCT | 861 adults with ICP monitoring, GCS motor 2–5 | Single 150mg dose vs. placebo, within 6h of injury | No difference in GOS-E at 6mo | No difference in adverse events | 262 | |
| Erythropoietin | Decreases production of pro-inflammatory cytokines and chemokines IL-1 and TNF block EPO production |
“EPO-TBI” Multicenter RCT | 606 adults with moderate and severe groups - GCS 9–12 and GCS ≤ 8 | 40,000IU weekly x 3wk vs. placebo | No difference in GOS-E at 6mo | No difference in mortality or DVT | Mortality reduced in patients without mass lesions, no increase in good outcome Many patients did not receive full course |
16 |
| Multicenter RCT | 200 adults with TBI, unable to follow commands | 500IU/kg q24h x 3 doses or 500IU/kg x 1 dose then weekly x 2wk vs. placebo | No difference in GOS-E at 6mo | No difference in mortality, ARDS, or infection | Original dosing regimen (daily x 3 doses) stopped by FDA due to safety concern (higher mortality in stroke trial) | 15 | ||
| G-CSF | Stimulate stem cells to produce granulocytes | Multicenter RCT | 61 adults GCS ≤ 8 expected to require mechanical ventilation > 3d | 75μg/d vs. 300μg/d x 10d vs. placebo | Dose-dependent increase in neutrophil count | No difference in mortality, LOS, or nosocomial infection Significant decrease in bacteremia incidence |
Adverse events similar between groups Included patients with cerebral hemorrhage as well as TBI |
174 |
| Hypertonic saline | Improve T-cell function Reduced TNF-α and IL-10 |
Multicenter RCT | 1331 adults with severe TBI | 250mL bolus of 7.5% saline / 6% dextran 70 vs. 7.5% saline vs. 0.9% saline initiated pre-hospital | No difference in GOS-E at 6mo | No difference in survival at 28d | Terminated early for futility | 263 |
| Hypothermia | Humoral and cellular immune response is temperature dependent Decreased neutrophil accumulation in CNS Decreased IL-1β, possibly by reduction in temperature-dependent Caspase-1 activity |
“Cool Kids” Multicenter RCT | 77 children with GCS ≤ 8 | 32–33°C vs. 36.5–37.5°C for 48–72h | No difference in mortality at 3mo | No adverse events | Terminated early for futility | 264 |
| Multicenter RCT | 225 children with GCS ≤ 8 | 32.5°C vs. 37°C for 24h | No difference in 6mo PCPC score | No difference in mortality | Trend to increased mortality and significantly higher incidence of hypotension and vasoactive agent use during rewarming (+0.5°C q2h) | 11 | ||
| “NABIS: H II” Multicenter RCT | 97 adults with GCS 4–8 Enrolled within 2.5h of injury |
32–34°C vs. 35.5 – 37°C for 72h | No difference in 6mo outcome | No difference in mortality | Terminated early for futility Improved outcomes in patients with evacuated hematoma treated with hypothermia |
181 | ||
| Eurotherm3235 Multicenter RCT | 387 adults with severe TBI and ICP > 20mmHg despite stage 1 treatments | Cooled to 32–35°C followed by stage 2 if ICP remained high vs. stage 2 treatments alone | Lower GOS-E in hypothermia group | Stage 3 treatments (coma, craniectomy) were required in more patients of the control group | Terminated early for safety concerns | 180 | ||
| Anakinra | Block IL-1 signal transduction | Single Center RCT | 20 adults with GCS ≤ 8 | 100mg S.Q. q24h x 5 doses | Increased IL-1ra in CNS ECF within 6h | PCA of 42 cytokine multiplex demonstrated separation between treatment and placebo groups | Subsequent study showed patients receiving rIL-1ra had cytokines biasing to M1-like microglial phenotype Control patients were relatively biased to M2-like phenotype |
265,266 |
| Probiotics | Modify lymphocyte polarization prior to CNS infiltration | Single Center RCT | 52 adults with GCS 5–8 | 109 bacteria for 21d vs. placebo | No difference in 28d mortality | On day 21, treatment group had higher IFNγ and lower IL-10 and IL-4 | Trend to decrease late VAP Unclear what effects might be in CNS |
267 |
| Statins | Inhibit expression of vascular adhesion molecules and chemokines to reduce leukocyte infiltration of CNS Associated with reductions in pro-inflammatory cytokines |
Single Center RCT | 21 adults with GCS 9–13 | Rosuvastatin 20mg/d x 10d vs placebo | Modest decrease in amnesia and disorientation time | No difference in disability at 3mo | Subsequent study showed reduction in plasma TNFα at 72h | 268,269 |
| Steroids | Inhibit leukocyte activation and infiltration Modulate cytokine release Progesterone decreased upregulation of IL-1β, TNFα, and complement factors 3 and 5 Reduce M1-like microglial activation |
“CRASH” Multicenter RCT | 10,008 adults with GCS ≤ 14 |
Methylprednisolone Load: 2g over 1h Maintenance: 0.4g/h x 48h vs placebo |
Higher risk of mortality at 2wk in steroid group | Higher risk of mortality at 6mo in steroid group | Terminated early for safety concerns | 167 |
| Multicenter RCT | 161 adults with TBI and coma | Dexamethasone 100mg vs placebo | No difference in survival | No difference in 6mo outcome | 168 | |||
| Multicenter RCT | 163 adults with GCS 9–12 and 957 adults with GCS 4–8 |
Tirilazad 10mg/kg within 4h of injury and q6 x 5d vs placebo |
No difference in 6mo GOS | No difference in mortality | Significant differences in pretreatment hypotension and hypoxia related to inter-center variation | 170 | ||
| “Corti-TC” Multicenter RCT | 336 adults with GCS ≤ 8 |
Hydrocortisone (200mg/day, tapered) + Fludrocortisone (50μg/day) x 10d vs. placebo |
No difference in incidence of hospital acquired pneumonia | No change when analyzed according to presence or absence of adrenal insufficiency | Study may have been underpowered due to lower than expected incidence of hospital-acquired pneumonia | 171 | ||
| “ProTECT III” Multicenter RCT | 882 adults with GCS 4–12 |
Progesterone Infusion started within 4h of injury, duration 96h |
No difference in 6mo-GOS | No difference in mortality | Terminated for futility | 14 | ||
| “SyNAPSe” Multicenter RCT | 1195 adults with GCS ≤ 8 |
Progesterone 0.71mg/kg load then 0.5mg/kg/h infusion for 119h |
No difference in 6mo-GOS | No difference in mortality | 13 | |||
Abbreviations: TBI – traumatic brain injury; BBB – blood brain barrier; RCT – randomized controlled trial; GCS – Glasgow coma scale; DRS – Disability Rating Scale; HIREOS – head injury related early outcomes score; DSMB – data safety monitoring board; TNF – tumor necrosis factor; NMDA – N-methyl-D-aspartate; ICP – intracranial pressure; IL – interleukin; EPO – erythropoietin; DVT – deep venous thrombosis; ARDS – acute respiratory distress syndrome; LOS – length of stay; PCPC – pediatric cerebral performance category; CNS – central nervous system; ECF – extracellular fluid; PCA – principal components analysis; GABA – gamma-aminobutyric acid; IFN – interferon; VAP – ventilator associated pneumonia
Review Criteria.
For review of human data on TBI neuroinflammation, we searched PubMed for articles published in English from January 1950 to March 2016 using the following query: “traumatic brain injury” or “closed head injury” or “closed-head injury” or “head trauma” AND ( ( Case Reports[ptyp] OR Clinical Study[ptyp] OR Clinical Trial[ptyp] OR Clinical Trial, Phase I[ptyp] OR Clinical Trial, Phase II[ptyp] OR Clinical Trial, Phase III[ptyp] OR Clinical Trial, Phase IV[ptyp] OR Controlled Clinical Trial[ptyp] OR Comparative Study[ptyp] OR Meta-Analysis[ptyp] OR Multicenter Study[ptyp] OR Randomized Controlled Trial[ptyp] ) AND Humans[Mesh]). We selected articles reporting clinical findings of neuroinflammation in human traumatic brain injury. Reference lists were used, as well as these authors’ expertise, for inclusion of additional relevant studies.
Key Points.
Traumatic brain injury is a significant public health issue that is increasing in global incidence and recognition in popular press, particularly for mild, repetitive, and blast injuries.
Neuroinflammation, triggered by release of endogenous danger signals and innate immune activation, is crucial to recovery after traumatic brain injury; however, a dysregulated immune response may lead to secondary injury.
The activity of microglia and infiltrating macrophages and adaptive immune cells is driven by extracellular injury signals and intracellular molecular pathways that may represent novel therapeutic targets.
Design of preclinical and clinical trials studying immunomodulatory interventions should account for changes in neuroinflammation that occur over time, between injury type / severity / secondary injury, and across patient characteristics such as age, sex, and genetic variability.
Chronic neuroinflammation, which may develop and last for years after traumatic brain injury, is being investigated as a link to accelerated neurodegeneration and chronic traumatic encephalopathy.
Acknowledgments
Support: T32 HD40686 (DS), R01 NS087978 (PK), R01 AI110822-01 (MM), R01NS082308 (DL), DoD Grants W81XWH-10-1-0623 (PK) and W81XWH-14-2-0018; NS061817 (HB), NS076511 (HB), NIA Claude D. Pepper Older Americans Independence Center P30-AG028747 (DL), and Children’s Hospital of Pittsburgh - Children’s Trust (DS)
Biographies
Dennis W. Simon
Department of Critical Care Medicine, University of Pittsburgh School of Medicine, 4401 Penn Avenue, Pittsburgh, PA 15224, USA.
Dennis Simon is an Assistant Professor of Critical Care Medicine and Pediatrics at the University of Pittsburgh School of Medicine and a Scientist at the Safar Center for Resuscitation Research in Pittsburgh, PA, USA. He is a member of the Neurointensive Care Service at the Children’s Hospital of Pittsburgh of UPMC. Dr. Simon trained in Pediatrics and at Boston Children’s Hospital, Critical Care Medicine at Children’s Hospital of Pittsburgh of UPMC, and Pediatric Neurocritical Care and Resuscitation Research under Dr. Kochanek. Dr. Simon’s basic and translational research is thematically centered around neuroinflammation in critical illness.
Mandy McGeachy
Department of Medicine, University of Pittsburgh School of Medicine, 3500 Terrace Street, BST South, S719, Pittsburgh, PA 15261, USA.
Mandy McGeachy is an Assistant Professor of Medicine at the University of Pittsburgh School of Medicine, Pittsburgh, PA, USA. Dr. McGeachy received her PhD from the University of Edinburgh, Scotland, UK and performed post-doctoral work at Schering-Plough Biopharma/DNAX before becoming a Senior Scientist at Merck Research Labs. Dr. McGeachy has since moved to the University of Pittsburgh, where her lab aims to understand the mechanisms that regulate autoimmune inflammation in the CNS and other target organs, with a particular focus on the roles and regulation of Th17 cells.
Hülya Bayır
Department of Critical Care Medicine, University of Pittsburgh School of Medicine, 4401 Penn Avenue, Pittsburgh, PA, 15224, USA.
Hülya Bayır is a Professor of Critical Care Medicine and Environmental and Occupational Health at the University of Pittsburgh School of Medicine, Pittsburgh, PA, USA. She is Associate Director of the Safar Center for Resuscitation Research, Associate Director of Center for Free Radical and Environmental Health, and Associate Chief of Pediatric Critical Care Medicine at the Children’s Hospital of Pittsburgh of UPMC. Dr. Bayır received her medical degree from Hacettepe University, Ankara, Türkiye, and completed pediatrics and pediatric critical care training at State University of New York at Stony Brook and Children’s Hospital of Pittsburgh of UPMC respectively. Dr. Bayır’s research interests include mitochondrial injury and development of novel approaches to treatment of mitochondrial dysfunction by redox therapy.
Robert S. B. Clark
Department of Critical Care Medicine, University of Pittsburgh School of Medicine, 4401 Penn Avenue, Pittsburgh, PA, 15224, USA.
Robert Clark is the Children’s Hospital of Pittsburgh Endowed Chair in Pediatric Critical Care Medicine and Division Chief. He is Professor of Critical Care Medicine, Pediatrics, and Clinical and Translational Science at the University of Pittsburgh School of Medicine. He is Associate Director of the Safar Center for Resuscitation Research and Director of the Brain Care Institute at the Children’s Hospital of Pittsburgh of UPMC. Dr. Clark received his medical degree from the Medical College of Wisconsin, Milwaukee, WI. He completed residency in Pediatrics at the University of Utah, Salt Lake City, UT and fellowship in Critical Care Medicine at the Children’s Hospital of Pittsburgh. His current research interests include mechanisms of cell death and neurologic dysfunction after traumatic and ischemic brain injury, particularly in the developing brain.
David J. Loane
Department of Anesthesiology, University of Maryland School of Medicine, 655 W. Baltimore Street, BRB, 6-011, Baltimore, MD, 21201, USA.
David Loane is an Associate Professor at the Shock, Trauma, and Anesthesiology Research (STAR) at the University of Maryland School of Medicine, Baltimore, MD, USA. Dr. Loane conducted his graduate studies at the Department of Pharmacology and MRC Center for Synaptic Plasticity, University of Bristol, England. He pursued postdoctoral training at Trinity College Institute of Neuroscience, Trinity College Dublin, Ireland and the Department of Neuroscience, Georgetown University Medical Center, Washington D.C. Dr. Loane leads a multi-disciplinary team dedicated to studying the complexities of TBI, neuroinflammation, and tissue repair.
Patrick M. Kochanek
Safar Center for Resuscitation Research, University of Pittsburgh School of Medicine, 3434 Fifth Avenue, Pittsburgh, PA, 15260, USA.
Patrick Kochanek is the Ake Grenvik Professor of Critical Care Medicine, and Professor of Anesthesiology, Pediatrics, Bioengineering, and Clinical and Translational Science at the University of Pittsburgh School of Medicine, Pittsburgh, PA, UA. Dr. Kochanek is Vice Chairman of the Department of Critical Care Medicine, Director of the Safar Center for Resuscitation Research, at the University of Pittsburgh and Editor-in-Chief of the journal Pediatric Critical Care Medicine. He received his MD from the University of Chicago. After a residency in Pediatrics at the University of California, San Diego he did a Pediatric Critical Care Fellowship at the Children’s National Medical Center in Washington, D.C. During his fellowship he trained in the area of experimental brain ischemia at the Naval Medical Research Institute in Bethesda, Maryland. Dr. Kochanek’s research addresses studies in experimental and clinical traumatic brain injury and cardiac arrest.
Footnotes
DECLARATION OF INTERESTS
The authors declare no competing interests
References
- 1.Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nature reviews. Neurology. 2013;9:231–236. doi: 10.1038/nrneurol.2013.22. [DOI] [PubMed] [Google Scholar]
- 2.Feigin VL, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet neurology. 2013;12:53–64. doi: 10.1016/s1474-4422(12)70262-4. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein LE, et al. Chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model. Science translational medicine. 2012;4:134ra160. doi: 10.1126/scitranslmed.3003716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corps KN, Roth TL, McGavern DB. Inflammation and neuroprotection in traumatic brain injury. JAMA neurology. 2015;72:355–362. doi: 10.1001/jamaneurol.2014.3558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Csuka E, et al. IL-10 levels in cerebrospinal fluid and serum of patients with severe traumatic brain injury: relationship to IL-6, TNF-alpha, TGF-beta1 and blood-brain barrier function. Journal of neuroimmunology. 1999;101:211–221. doi: 10.1016/s0165-5728(99)00148-4. [DOI] [PubMed] [Google Scholar]
- 6.Frugier T, Morganti-Kossmann MC, O’Reilly D, McLean CA. In situ detection of inflammatory mediators in post mortem human brain tissue after traumatic injury. Journal of neurotrauma. 2010;27:497–507. doi: 10.1089/neu.2009.1120. [DOI] [PubMed] [Google Scholar]
- 7.Kossmann T, et al. Interleukin-8 released into the cerebrospinal fluid after brain injury is associated with blood-brain barrier dysfunction and nerve growth factor production. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 1997;17:280–289. doi: 10.1097/00004647-199703000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Semple BD, Kossmann T, Morganti-Kossmann MC. Role of chemokines in CNS health and pathology: a focus on the CCL2/CCR2 and CXCL8/CXCR2 networks. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2010;30:459–473. doi: 10.1038/jcbfm.2009.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ziebell JM, Morganti-Kossmann MC. Involvement of pro- and anti-inflammatory cytokines and chemokines in the pathophysiology of traumatic brain injury. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2010;7:22–30. doi: 10.1016/j.nurt.2009.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts I, et al. Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004;364:1321–1328. doi: 10.1016/s0140-6736(04)17188-2. [DOI] [PubMed] [Google Scholar]
- 11.Hutchison JS, et al. Hypothermia therapy after traumatic brain injury in children. The New England journal of medicine. 2008;358:2447–2456. doi: 10.1056/NEJMoa0706930. [DOI] [PubMed] [Google Scholar]
- 12.Adelson PD, et al. Comparison of hypothermia and normothermia after severe traumatic brain injury in children (Cool Kids): a phase 3, randomised controlled trial. Lancet neurology. 2013;12:546–553. doi: 10.1016/s1474-4422(13)70077-2. [DOI] [PubMed] [Google Scholar]
- 13.Skolnick BE, et al. A clinical trial of progesterone for severe traumatic brain injury. The New England journal of medicine. 2014;371:2467–2476. doi: 10.1056/NEJMoa1411090. [DOI] [PubMed] [Google Scholar]
- 14.Wright DW, et al. Very early administration of progesterone for acute traumatic brain injury. The New England journal of medicine. 2014;371:2457–2466. doi: 10.1056/NEJMoa1404304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robertson CS, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA : the journal of the American Medical Association. 2014;312:36–47. doi: 10.1001/jama.2014.6490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nichol A, et al. Erythropoietin in traumatic brain injury (EPO-TBI): a double-blind randomised controlled trial. Lancet. 2015;386:2499–2506. doi: 10.1016/s0140-6736(15)00386-4. [DOI] [PubMed] [Google Scholar]
- 17.Saxena M, Andrews PJ, Cheng A, Deol K, Hammond N. Modest cooling therapies (35 masculineC to 37.5 masculineC) for traumatic brain injury. The Cochrane database of systematic reviews. 2014;8:Cd006811. doi: 10.1002/14651858.CD006811.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiong Y, Mahmood A, Chopp M. Animal models of traumatic brain injury. Nature reviews. Neuroscience. 2013;14:128–142. doi: 10.1038/nrn3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marklund N, Hillered L. Animal modelling of traumatic brain injury in preclinical drug development: where do we go from here? British journal of pharmacology. 2011;164:1207–1229. doi: 10.1111/j.1476-5381.2010.01163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheikh AM, et al. Lysophosphatidylcholine induces glial cell activation: role of rho kinase. Glia. 2009;57:898–907. doi: 10.1002/glia.20815. [DOI] [PubMed] [Google Scholar]
- 21.Uchida K. Redox-derived damage-associated molecular patterns: Ligand function of lipid peroxidation adducts. Redox biology. 2013;1:94–96. doi: 10.1016/j.redox.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ransohoff RM, Brown MA. Innate immunity in the central nervous system. The Journal of clinical investigation. 2012;122:1164–1171. doi: 10.1172/jci58644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scherbel U, et al. Differential acute and chronic responses of tumor necrosis factor-deficient mice to experimental brain injury. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:8721–8726. doi: 10.1073/pnas.96.15.8721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sinz EH, et al. Inducible nitric oxide synthase is an endogenous neuroprotectant after traumatic brain injury in rats and mice. The Journal of clinical investigation. 1999;104:647–656. doi: 10.1172/jci6670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frank MG, Weber MD, Watkins LR, Maier SF. Stress sounds the alarmin: The role of the danger-associated molecular pattern HMGB1 in stress-induced neuroinflammatory priming. Brain, behavior, and immunity. 2015;48:1–7. doi: 10.1016/j.bbi.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.You Z, et al. Necrostatin-1 reduces histopathology and improves functional outcome after controlled cortical impact in mice. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2008;28:1564–1573. doi: 10.1038/jcbfm.2008.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laird MD, et al. High mobility group box protein-1 promotes cerebral edema after traumatic brain injury via activation of toll-like receptor 4. Glia. 2014;62:26–38. doi: 10.1002/glia.22581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Au AK, et al. Cerebrospinal fluid levels of high-mobility group box 1 and cytochrome C predict outcome after pediatric traumatic brain injury. Journal of neurotrauma. 2012;29:2013–2021. doi: 10.1089/neu.2011.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Latz E, Xiao TS, Stutz A. Activation and regulation of the inflammasomes. Nature reviews. Immunology. 2013;13:397–411. doi: 10.1038/nri3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Molecular cell. 2002;10:417–426. doi: 10.1016/s1097-2765(02)00599-3. [DOI] [PubMed] [Google Scholar]
- 31.de Rivero Vaccari JP, et al. Therapeutic neutralization of the NLRP1 inflammasome reduces the innate immune response and improves histopathology after traumatic brain injury. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2009;29:1251–1261. doi: 10.1038/jcbfm.2009.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Rivero Vaccari JP, Lotocki G, Marcillo AE, Dietrich WD, Keane RW. A molecular platform in neurons regulates inflammation after spinal cord injury. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2008;28:3404–3414. doi: 10.1523/jneurosci.0157-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adamczak SE, et al. Pyroptotic neuronal cell death mediated by the AIM2 inflammasome. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2014;34:621–629. doi: 10.1038/jcbfm.2013.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Halle A, et al. The NALP3 inflammasome is involved in the innate immune response to amyloid-beta. Nature immunology. 2008;9:857–865. doi: 10.1038/ni.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanamsagar R, Torres V, Kielian T. Inflammasome activation and IL-1beta/IL-18 processing are influenced by distinct pathways in microglia. Journal of neurochemistry. 2011;119:736–748. doi: 10.1111/j.1471-4159.2011.07481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu HD, et al. Expression of the NLRP3 inflammasome in cerebral cortex after traumatic brain injury in a rat model. Neurochemical research. 2013;38:2072–2083. doi: 10.1007/s11064-013-1115-z. [DOI] [PubMed] [Google Scholar]
- 37.Lukens JR, Barr MJ, Chaplin DD, Chi H, Kanneganti TD. Inflammasome-derived IL-1beta regulates the production of GM-CSF by CD4(+) T cells and gammadelta T cells. Journal of immunology (Baltimore, Md : 1950) 2012;188:3107–3115. doi: 10.4049/jimmunol.1103308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meissner F, Molawi K, Zychlinsky A. Mutant superoxide dismutase 1-induced IL-1beta accelerates ALS pathogenesis. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:13046–13050. doi: 10.1073/pnas.1002396107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palmer AM, Marion DW, Botscheller ML, Bowen DM, DeKosky ST. Increased transmitter amino acid concentration in human ventricular CSF after brain trauma. Neuroreport. 1994;6:153–156. doi: 10.1097/00001756-199412300-00039. [DOI] [PubMed] [Google Scholar]
- 40.Brown JI, Baker AJ, Konasiewicz SJ, Moulton RJ. Clinical significance of CSF glutamate concentrations following severe traumatic brain injury in humans. Journal of neurotrauma. 1998;15:253–263. doi: 10.1089/neu.1998.15.253. [DOI] [PubMed] [Google Scholar]
- 41.Ruppel RA, et al. Excitatory amino acid concentrations in ventricular cerebrospinal fluid after severe traumatic brain injury in infants and children: the role of child abuse. J Pediatr. 2001;138:18–25. doi: 10.1067/mpd.2001.110979. [DOI] [PubMed] [Google Scholar]
- 42.Kochanek PM, et al. Biochemical, cellular, and molecular mechanisms in the evolution of secondary damage after severe traumatic brain injury in infants and children: Lessons learned from the bedside. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2000;1:4–19. doi: 10.1097/00130478-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Viviani B, Boraso M, Marchetti N, Marinovich M. Perspectives on neuroinflammation and excitotoxicity: a neurotoxic conspiracy? Neurotoxicology. 2014;43:10–20. doi: 10.1016/j.neuro.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 44.Ikonomidou C, Turski L. Why did NMDA receptor antagonists fail clinical trials for stroke and traumatic brain injury? Lancet neurology. 2002;1:383–386. doi: 10.1016/s1474-4422(02)00164-3. [DOI] [PubMed] [Google Scholar]
- 45.Verrier JD, et al. Expression of the 2′,3′-cAMP-adenosine pathway in astrocytes and microglia. Journal of neurochemistry. 2011;118:979–987. doi: 10.1111/j.1471-4159.2011.07392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kochanek PM, et al. Adenosine A1 receptor knockout mice develop lethal status epilepticus after experimental traumatic brain injury. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2006;26:565–575. doi: 10.1038/sj.jcbfm.9600218. [DOI] [PubMed] [Google Scholar]
- 47.Haselkorn ML, et al. Adenosine A1 receptor activation as a brake on the microglial response after experimental traumatic brain injury in mice. Journal of neurotrauma. 2010;27:901–910. doi: 10.1089/neu.2009.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jackson EK, Boison D, Schwarzschild MA, Kochanek PM. Purines: forgotten mediators in traumatic brain injury. Journal of neurochemistry. 2016;137:142–153. doi: 10.1111/jnc.13551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suliman HB, Piantadosi CA. Mitochondrial Quality Control as a Therapeutic Target. Pharmacological reviews. 2016;68:20–48. doi: 10.1124/pr.115.011502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chu CT, Ji J, Dagda RK. Cardiolipin externalization to the outer mitochondrial membrane acts as an elimination signal for mitophagy in neuronal cells. 2013;15:1197–1205. doi: 10.1038/ncb2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Iyer SS, et al. Mitochondrial cardiolipin is required for Nlrp3 inflammasome activation. Immunity. 2013;39:311–323. doi: 10.1016/j.immuni.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Walko TD, 3rd, et al. Cerebrospinal fluid mitochondrial DNA: a novel DAMP in pediatric traumatic brain injury. Shock. 2014;41:499–503. doi: 10.1097/shk.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galluzzi L, Kepp O, Kroemer G. Mitochondria: master regulators of danger signalling. Nature reviews. Molecular cell biology. 2012;13:780–788. doi: 10.1038/nrm3479. [DOI] [PubMed] [Google Scholar]
- 54.Balasubramanian K, et al. Dichotomous roles for externalized cardiolipin in extracellular signaling: Promotion of phagocytosis and attenuation of innate immunity. Science signaling. 2015;8:ra95. doi: 10.1126/scisignal.aaa6179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fang H, et al. CD36-mediated hematoma absorption following intracerebral hemorrhage: negative regulation by TLR4 signaling. Journal of immunology (Baltimore, Md : 1950) 2014;192:5984–5992. doi: 10.4049/jimmunol.1400054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wagner KR, Sharp FR, Ardizzone TD, Lu A, Clark JF. Heme and iron metabolism: role in cerebral hemorrhage. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2003;23:629–652. doi: 10.1097/01.wcb.0000073905.87928.6d. [DOI] [PubMed] [Google Scholar]
- 57.Bellander BM, Singhrao SK, Ohlsson M, Mattsson P, Svensson M. Complement activation in the human brain after traumatic head injury. Journal of neurotrauma. 2001;18:1295–1311. doi: 10.1089/08977150152725605. [DOI] [PubMed] [Google Scholar]
- 58.Stahel PF, et al. Intrathecal levels of complement-derived soluble membrane attack complex (sC5b-9) correlate with blood-brain barrier dysfunction in patients with traumatic brain injury. Journal of neurotrauma. 2001;18:773–781. doi: 10.1089/089771501316919139. [DOI] [PubMed] [Google Scholar]
- 59.Stahel PF, et al. Absence of the complement regulatory molecule CD59a leads to exacerbated neuropathology after traumatic brain injury in mice. Journal of neuroinflammation. 2009;6:2. doi: 10.1186/1742-2094-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rancan M, et al. Central nervous system-targeted complement inhibition mediates neuroprotection after closed head injury in transgenic mice. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2003;23:1070–1074. doi: 10.1097/01.wcb.0000084250.20114.2c. [DOI] [PubMed] [Google Scholar]
- 61.Kaczorowski SL, Schiding JK, Toth CA, Kochanek PM. Effect of soluble complement receptor-1 on neutrophil accumulation after traumatic brain injury in rats. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 1995;15:860–864. doi: 10.1038/jcbfm.1995.108. [DOI] [PubMed] [Google Scholar]
- 62.Brennan FH, Anderson AJ, Taylor SM, Woodruff TM, Ruitenberg MJ. Complement activation in the injured central nervous system: another dual-edged sword? Journal of neuroinflammation. 2012;9:137. doi: 10.1186/1742-2094-9-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rich MC, et al. Site-targeted complement inhibition by a complement receptor 2-conjugated inhibitor (mTT30) ameliorates post-injury neuropathology in mouse brains. Neuroscience letters. 2016;617:188–194. doi: 10.1016/j.neulet.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 64.Fluiter K, Opperhuizen AL, Morgan BP, Baas F, Ramaglia V. Inhibition of the membrane attack complex of the complement system reduces secondary neuroaxonal loss and promotes neurologic recovery after traumatic brain injury in mice. Journal of immunology (Baltimore, Md : 1950) 2014;192:2339–2348. doi: 10.4049/jimmunol.1302793. [DOI] [PubMed] [Google Scholar]
- 65.Ruseva MM, Ramaglia V, Morgan BP, Harris CL. An anticomplement agent that homes to the damaged brain and promotes recovery after traumatic brain injury in mice. Proceedings of the National Academy of Sciences of the United States of America. 2015;112:14319–14324. doi: 10.1073/pnas.1513698112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang Z, Zhang ZY, Wu Y, Schluesener HJ. Lesional accumulation of CD163+ macrophages/microglia in rat traumatic brain injury. Brain research. 2012;1461:102–110. doi: 10.1016/j.brainres.2012.04.038. [DOI] [PubMed] [Google Scholar]
- 67.Wang X, Mori T, Sumii T, Lo EH. Hemoglobin-induced cytotoxicity in rat cerebral cortical neurons: caspase activation and oxidative stress. Stroke; a journal of cerebral circulation. 2002;33:1882–1888. doi: 10.1161/01.str.0000020121.41527.5d. [DOI] [PubMed] [Google Scholar]
- 68.Willmore LJ, Ueda Y. Posttraumatic epilepsy: hemorrhage, free radicals and the molecular regulation of glutamate. Neurochemical research. 2009;34:688–697. doi: 10.1007/s11064-008-9841-3. [DOI] [PubMed] [Google Scholar]
- 69.Newell E, et al. Cerebrospinal Fluid Markers of Macrophage and Lymphocyte Activation After Traumatic Brain Injury in Children. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2015;16:549–557. doi: 10.1097/pcc.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kochanek PM, et al. Screening of biochemical and molecular mechanisms of secondary injury and repair in the brain after experimental blast-induced traumatic brain injury in rats. Journal of neurotrauma. 2013;30:920–937. doi: 10.1089/neu.2013.2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bandak FA, Ling G, Bandak A, De Lanerolle NC. Injury biomechanics, neuropathology, and simplified physics of explosive blast and impact mild traumatic brain injury. Handbook of clinical neurology. 2015;127:89–104. doi: 10.1016/b978-0-444-52892-6.00006-4. [DOI] [PubMed] [Google Scholar]
- 72.Kovesdi E, et al. Acute minocycline treatment mitigates the symptoms of mild blast-induced traumatic brain injury. Frontiers in neurology. 2012;3:111. doi: 10.3389/fneur.2012.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Clark RS, Schiding JK, Kaczorowski SL, Marion DW, Kochanek PM. Neutrophil accumulation after traumatic brain injury in rats: comparison of weight drop and controlled cortical impact models. Journal of neurotrauma. 1994;11:499–506. doi: 10.1089/neu.1994.11.499. [DOI] [PubMed] [Google Scholar]
- 74.Soares HD, Hicks RR, Smith D, McIntosh TK. Inflammatory leukocytic recruitment and diffuse neuronal degeneration are separate pathological processes resulting from traumatic brain injury. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1995;15:8223–8233. doi: 10.1523/JNEUROSCI.15-12-08223.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carlos TM, Clark RS, Franicola-Higgins D, Schiding JK, Kochanek PM. Expression of endothelial adhesion molecules and recruitment of neutrophils after traumatic brain injury in rats. Journal of leukocyte biology. 1997;61:279–285. doi: 10.1002/jlb.61.3.279. [DOI] [PubMed] [Google Scholar]
- 76.Bao F, et al. A CD11d monoclonal antibody treatment reduces tissue injury and improves neurological outcome after fluid percussion brain injury in rats. Journal of neurotrauma. 2012;29:2375–2392. doi: 10.1089/neu.2012.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Weaver LC, et al. CD11d integrin blockade reduces the systemic inflammatory response syndrome after traumatic brain injury in rats. Experimental neurology. 2015;271:409–422. doi: 10.1016/j.expneurol.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Auffray C, et al. Monitoring of blood vessels and tissues by a population of monocytes with patrolling behavior. Science (New York, NY) 2007;317:666–670. doi: 10.1126/science.1142883. [DOI] [PubMed] [Google Scholar]
- 79.Hsieh CL, et al. Traumatic brain injury induces macrophage subsets in the brain. European journal of immunology. 2013;43:2010–2022. doi: 10.1002/eji.201243084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Morganti JM, et al. CCR2 antagonism alters brain macrophage polarization and ameliorates cognitive dysfunction induced by traumatic brain injury. 2015;35:748–760. doi: 10.1523/jneurosci.2405-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jin X, Ishii H, Bai Z, Itokazu T, Yamashita T. Temporal changes in cell marker expression and cellular infiltration in a controlled cortical impact model in adult male C57BL/6 mice. PloS one. 2012;7:e41892. doi: 10.1371/journal.pone.0041892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.de Lanerolle NC, Lee TS, Spencer DD. Astrocytes and epilepsy. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2010;7:424–438. doi: 10.1016/j.nurt.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Burda JE, Bernstein AM, Sofroniew MV. Astrocyte roles in traumatic brain injury. Experimental neurology. 2016;275(Pt 3):305–315. doi: 10.1016/j.expneurol.2015.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Turtzo LC, et al. Macrophagic and microglial responses after focal traumatic brain injury in the female rat. Journal of neuroinflammation. 2014;11:82. doi: 10.1186/1742-2094-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Loane DJ, Byrnes KR. Role of microglia in neurotrauma. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2010;7:366–377. doi: 10.1016/j.nurt.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Morganti-Kossmann MC, Rancan M, Stahel PF, Kossmann T. Inflammatory response in acute traumatic brain injury: a double-edged sword. Current opinion in critical care. 2002;8:101–105. doi: 10.1097/00075198-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 87.David S, Kroner A. Repertoire of microglial and macrophage responses after spinal cord injury. Nature reviews. Neuroscience. 2011;12:388–399. doi: 10.1038/nrn3053. [DOI] [PubMed] [Google Scholar]
- 88.Kumar A, Loane DJ. Neuroinflammation after traumatic brain injury: opportunities for therapeutic intervention. Brain, behavior, and immunity. 2012;26:1191–1201. doi: 10.1016/j.bbi.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 89.Colton CA. Heterogeneity of microglial activation in the innate immune response in the brain. Journal of neuroimmune pharmacology : the official journal of the Society on NeuroImmune Pharmacology. 2009;4:399–418. doi: 10.1007/s11481-009-9164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gordon S. Alternative activation of macrophages. Nature reviews. Immunology. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 91.Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. The Journal of clinical investigation. 2012;122:787–795. doi: 10.1172/jci59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Loane DJ, Kumar A, Stoica BA, Cabatbat R, Faden AI. Progressive neurodegeneration after experimental brain trauma: association with chronic microglial activation. Journal of neuropathology and experimental neurology. 2014;73:14–29. doi: 10.1097/nen.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang G, et al. Microglia/macrophage polarization dynamics in white matter after traumatic brain injury. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2013;33:1864–1874. doi: 10.1038/jcbfm.2013.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Loane DJ, Kumar A. Microglia in the TBI brain: The good, the bad, and the dysregulated. Experimental neurology. 2016;275(Pt 3):316–327. doi: 10.1016/j.expneurol.2015.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fenn AM, et al. Immune activation promotes depression 1 month after diffuse brain injury: a role for primed microglia. Biological psychiatry. 2014;76:575–584. doi: 10.1016/j.biopsych.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fenn AM, et al. Methylene blue attenuates traumatic brain injury-associated neuroinflammation and acute depressive-like behavior in mice. Journal of neurotrauma. 2015;32:127–138. doi: 10.1089/neu.2014.3514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee KD, et al. FTY720 reduces inflammation and promotes functional recovery after spinal cord injury. Journal of neurotrauma. 2009;26:2335–2344. doi: 10.1089/neu.2008.0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang J, Zhang A, Sun Y, Cao X, Zhang N. Treatment with immunosuppressants FTY720 and tacrolimus promotes functional recovery after spinal cord injury in rats. The Tohoku journal of experimental medicine. 2009;219:295–302. doi: 10.1620/tjem.219.295. [DOI] [PubMed] [Google Scholar]
- 99.Norimatsu Y, et al. FTY720 improves functional recovery after spinal cord injury by primarily nonimmunomodulatory mechanisms. The American journal of pathology. 2012;180:1625–1635. doi: 10.1016/j.ajpath.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 100.Walsh JT, et al. MHCII-independent CD4+ T cells protect injured CNS neurons via IL-4. The Journal of clinical investigation. 2015;125:699–714. doi: 10.1172/jci76210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kipnis J, et al. Neuroprotective autoimmunity: naturally occurring CD4+CD25+ regulatory T cells suppress the ability to withstand injury to the central nervous system. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:15620–15625. doi: 10.1073/pnas.232565399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yoles E, et al. Protective autoimmunity is a physiological response to CNS trauma. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2001;21:3740–3748. doi: 10.1523/JNEUROSCI.21-11-03740.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moalem G, et al. Autoimmune T cells retard the loss of function in injured rat optic nerves. Journal of neuroimmunology. 2000;106:189–197. doi: 10.1016/s0165-5728(00)00240-x. [DOI] [PubMed] [Google Scholar]
- 104.Hauben E, et al. Autoimmune T cells as potential neuroprotective therapy for spinal cord injury. Lancet. 2000;355:286–287. doi: 10.1016/s0140-6736(99)05140-5. [DOI] [PubMed] [Google Scholar]
- 105.Hammarberg H, et al. Neuroprotection by encephalomyelitis: rescue of mechanically injured neurons and neurotrophin production by CNS-infiltrating T and natural killer cells. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2000;20:5283–5291. doi: 10.1523/JNEUROSCI.20-14-05283.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Linker R, Gold R, Luhder F. Function of neurotrophic factors beyond the nervous system: inflammation and autoimmune demyelination. Critical reviews in immunology. 2009;29:43–68. doi: 10.1615/critrevimmunol.v29.i1.20. [DOI] [PubMed] [Google Scholar]
- 107.Filiano AJ, Gadani SP, Kipnis J. Interactions of innate and adaptive immunity in brain development and function. Brain research. 2015;1617:18–27. doi: 10.1016/j.brainres.2014.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gadani SP, Walsh JT, Smirnov I, Zheng J, Kipnis J. The glia-derived alarmin IL-33 orchestrates the immune response and promotes recovery following CNS injury. Neuron. 2015;85:703–709. doi: 10.1016/j.neuron.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 109.Lohning M, et al. T1/ST2 is preferentially expressed on murine Th2 cells, independent of interleukin 4, interleukin 5, and interleukin 10, and important for Th2 effector function. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:6930–6935. doi: 10.1073/pnas.95.12.6930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Burzyn D, et al. A special population of regulatory T cells potentiates muscle repair. Cell. 2013;155:1282–1295. doi: 10.1016/j.cell.2013.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kuswanto W, et al. Poor Repair of Skeletal Muscle in Aging Mice Reflects a Defect in Local, Interleukin-33-Dependent Accumulation of Regulatory T Cells. Immunity. 2016;44:355–367. doi: 10.1016/j.immuni.2016.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Schiering C, et al. The alarmin IL-33 promotes regulatory T-cell function in the intestine. Nature. 2014;513:564–568. doi: 10.1038/nature13577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fletcher JM, Lalor SJ, Sweeney CM, Tubridy N, Mills KH. T cells in multiple sclerosis and experimental autoimmune encephalomyelitis. Clinical and experimental immunology. 2010;162:1–11. doi: 10.1111/j.1365-2249.2010.04143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Patel DD, Kuchroo VK. Th17 Cell Pathway in Human Immunity: Lessons from Genetics and Therapeutic Interventions. Immunity. 2015;43:1040–1051. doi: 10.1016/j.immuni.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 115.Shichita T, et al. Pivotal role of cerebral interleukin-17-producing gammadeltaT cells in the delayed phase of ischemic brain injury. Nature medicine. 2009;15:946–950. doi: 10.1038/nm.1999. [DOI] [PubMed] [Google Scholar]
- 116.Benakis C, et al. Commensal microbiota affects ischemic stroke outcome by regulating intestinal gammadelta T cells. Nature medicine. 2016;22:516–523. doi: 10.1038/nm.4068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014;157:121–141. doi: 10.1016/j.cell.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kasper LH. The evolving role of the gut microbiome in human disease. FEBS letters. 2014;588:4101. doi: 10.1016/j.febslet.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 119.Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain, behavior, and immunity. 2014;38:1–12. doi: 10.1016/j.bbi.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nature reviews. Neuroscience. 2012;13:701–712. doi: 10.1038/nrn3346. [DOI] [PubMed] [Google Scholar]
- 121.Kelly JR, et al. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Frontiers in cellular neuroscience. 2015;9:392. doi: 10.3389/fncel.2015.00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Iliff JJ, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Science translational medicine. 2012;4:147ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The Glymphatic System: A Beginner’s Guide. Neurochemical research. 2015;40:2583–2599. doi: 10.1007/s11064-015-1581-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Iliff JJ, Chen MJ, Plog BA, Zeppenfeld DM, Soltero M. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. 2014;34:16180–16193. doi: 10.1523/jneurosci.3020-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Peng W, et al. Suppression of glymphatic fluid transport in a mouse model of Alzheimer’s disease. Neurobiology of disease. 2016 doi: 10.1016/j.nbd.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lee H, et al. The Effect of Body Posture on Brain Glymphatic Transport. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2015;35:11034–11044. doi: 10.1523/jneurosci.1625-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Xie L, et al. Sleep drives metabolite clearance from the adult brain. Science (New York, NY) 2013;342:373–377. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Aspelund A, et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. The Journal of experimental medicine. 2015;212:991–999. doi: 10.1084/jem.20142290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Louveau A, et al. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015;523:337–341. doi: 10.1038/nature14432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Plog BA, et al. Biomarkers of traumatic injury are transported from brain to blood via the glymphatic system. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2015;35:518–526. doi: 10.1523/jneurosci.3742-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tortella FC, Leung LY. Traumatic Brain Injury and Polytrauma in Theaters of Combat: The Case for Neurotrauma Resuscitation? Shock. 2015;44(Suppl 1):17–26. doi: 10.1097/shk.0000000000000380. [DOI] [PubMed] [Google Scholar]
- 132.Chesnut RM, et al. The role of secondary brain injury in determining outcome from severe head injury. The Journal of trauma. 1993;34:216–222. doi: 10.1097/00005373-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 133.Tisherman SA, et al. Detailed description of all deaths in both the shock and traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium. Annals of surgery. 2015;261:586–590. doi: 10.1097/sla.0000000000000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shein S, et al. Hemorrhagic shock shifts the serum cytokine profile from pro-to anti-inflammatory after experimental traumatic brain injury in mice. Journal of neurotrauma. 2014 doi: 10.1089/neu.2013.2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hemerka JN, et al. Severe brief pressure-controlled hemorrhagic shock after traumatic brain injury exacerbates functional deficits and long-term neuropathological damage in mice. Journal of neurotrauma. 2012;29:2192–2208. doi: 10.1089/neu.2011.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Shiozaki T, et al. Cerebrospinal fluid concentrations of anti-inflammatory mediators in early-phase severe traumatic brain injury. Shock. 2005;23:406–410. doi: 10.1097/01.shk.0000161385.62758.24. [DOI] [PubMed] [Google Scholar]
- 137.Kumar RG, et al. Acute CSF interleukin-6 trajectories after TBI: associations with neuroinflammation, polytrauma, and outcome. Brain, behavior, and immunity. 2015;45:253–262. doi: 10.1016/j.bbi.2014.12.021. [DOI] [PubMed] [Google Scholar]
- 138.Simon DW, Vagni VM, Kochanek PM, Clark RS. Combined Neurotrauma Models: Experimental Models Combining Traumatic Brain Injury and Secondary Insults. Methods in molecular biology (Clifton, NJ) 2016;1462:393–411. doi: 10.1007/978-1-4939-3816-2_22. [DOI] [PubMed] [Google Scholar]
- 139.McDonald SJ, Sun M, Agoston DV, Shultz SR. The effect of concomitant peripheral injury on traumatic brain injury pathobiology and outcome. Journal of neuroinflammation. 2016;13:90. doi: 10.1186/s12974-016-0555-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Shultz SR, et al. Tibial fracture exacerbates traumatic brain injury outcomes and neuroinflammation in a novel mouse model of multitrauma. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2015;35:1339–1347. doi: 10.1038/jcbfm.2015.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Utagawa A, Truettner JS, Dietrich WD, Bramlett HM. Systemic inflammation exacerbates behavioral and histopathological consequences of isolated traumatic brain injury in rats. Experimental neurology. 2008;211:283–291. doi: 10.1016/j.expneurol.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hang CH, et al. Effect of systemic LPS injection on cortical NF-kappaB activity and inflammatory response following traumatic brain injury in rats. Brain research. 2004;1026:23–32. doi: 10.1016/j.brainres.2004.07.090. [DOI] [PubMed] [Google Scholar]
- 143.Titus DJ, Furones C, Atkins CM, Dietrich WD. Emergence of cognitive deficits after mild traumatic brain injury due to hyperthermia. Experimental neurology. 2015;263:254–262. doi: 10.1016/j.expneurol.2014.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Richardson RM, Sun D, Bullock MR. Neurogenesis after traumatic brain injury. Neurosurgery clinics of North America. 2007;18:169–181. xi. doi: 10.1016/j.nec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 145.Ekdahl CT, Claasen JH, Bonde S, Kokaia Z, Lindvall O. Inflammation is detrimental for neurogenesis in adult brain. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:13632–13637. doi: 10.1073/pnas.2234031100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Whitney NP, Eidem TM, Peng H, Huang Y, Zheng JC. Inflammation mediates varying effects in neurogenesis: relevance to the pathogenesis of brain injury and neurodegenerative disorders. Journal of neurochemistry. 2009;108:1343–1359. doi: 10.1111/j.1471-4159.2009.05886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Monje ML, Toda H, Palmer TD. Inflammatory blockade restores adult hippocampal neurogenesis. Science (New York, NY) 2003;302:1760–1765. doi: 10.1126/science.1088417. [DOI] [PubMed] [Google Scholar]
- 148.Butovsky O, et al. Microglia activated by IL-4 or IFN-gamma differentially induce neurogenesis and oligodendrogenesis from adult stem/progenitor cells. Molecular and cellular neurosciences. 2006;31:149–160. doi: 10.1016/j.mcn.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 149.Piao CS, et al. Late exercise reduces neuroinflammation and cognitive dysfunction after traumatic brain injury. Neurobiology of disease. 2013;54:252–263. doi: 10.1016/j.nbd.2012.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wang B, Jin K. Current perspectives on the link between neuroinflammation and neurogenesis. Metabolic brain disease. 2015;30:355–365. doi: 10.1007/s11011-014-9523-6. [DOI] [PubMed] [Google Scholar]
- 151.Bendlin BB, et al. Longitudinal changes in patients with traumatic brain injury assessed with diffusion-tensor and volumetric imaging. NeuroImage. 2008;42:503–514. doi: 10.1016/j.neuroimage.2008.04.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Farbota KD, et al. Longitudinal volumetric changes following traumatic brain injury: a tensor-based morphometry study. Journal of the International Neuropsychological Society : JINS. 2012;18:1006–1018. doi: 10.1017/s1355617712000835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kumar R, et al. Serial changes in the white matter diffusion tensor imaging metrics in moderate traumatic brain injury and correlation with neuro-cognitive function. Journal of neurotrauma. 2009;26:481–495. doi: 10.1089/neu.2008.0461. [DOI] [PubMed] [Google Scholar]
- 154.Ng K, et al. Magnetic resonance imaging evidence of progression of subacute brain atrophy in moderate to severe traumatic brain injury. Archives of physical medicine and rehabilitation. 2008;89:S35–44. doi: 10.1016/j.apmr.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 155.Sidaros A, et al. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Brain : a journal of neurology. 2008;131:559–572. doi: 10.1093/brain/awm294. [DOI] [PubMed] [Google Scholar]
- 156.Sidaros A, et al. Long-term global and regional brain volume changes following severe traumatic brain injury: a longitudinal study with clinical correlates. NeuroImage. 2009;44:1–8. doi: 10.1016/j.neuroimage.2008.08.030. [DOI] [PubMed] [Google Scholar]
- 157.Trivedi MA, et al. Longitudinal changes in global brain volume between 79 and 409 days after traumatic brain injury: relationship with duration of coma. Journal of neurotrauma. 2007;24:766–771. doi: 10.1089/neu.2006.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Shaklai S, Peretz R, Spasser R, Simantov M, Groswasser Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain injury : [BI] 2014;28:915–921. doi: 10.3109/02699052.2013.862739. [DOI] [PubMed] [Google Scholar]
- 159.Bellinger FP, Madamba SG, Campbell IL, Siggins GR. Reduced long-term potentiation in the dentate gyrus of transgenic mice with cerebral overexpression of interleukin-6. Neuroscience letters. 1995;198:95–98. doi: 10.1016/0304-3940(95)11976-4. [DOI] [PubMed] [Google Scholar]
- 160.Rogers JT, et al. CX3CR1 deficiency leads to impairment of hippocampal cognitive function and synaptic plasticity. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:16241–16250. doi: 10.1523/jneurosci.3667-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ziebell JM, Adelson PD, Lifshitz J. Microglia: dismantling and rebuilding circuits after acute neurological injury. Metabolic brain disease. 2015;30:393–400. doi: 10.1007/s11011-014-9539-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Balschun D, et al. Interleukin-6: a cytokine to forget. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2004;18:1788–1790. doi: 10.1096/fj.04-1625fje. [DOI] [PubMed] [Google Scholar]
- 163.Boato F, et al. Interleukin-1 beta and neurotrophin-3 synergistically promote neurite growth in vitro. Journal of neuroinflammation. 2011;8:1–10. doi: 10.1186/1742-2094-8-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Aungst SL, Kabadi SV, Thompson SM, Stoica BA, Faden AI. Repeated mild traumatic brain injury causes chronic neuroinflammation, changes in hippocampal synaptic plasticity, and associated cognitive deficits. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2014;34:1223–1232. doi: 10.1038/jcbfm.2014.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Miron VE, et al. M2 microglia and macrophages drive oligodendrocyte differentiation during CNS remyelination. Nature neuroscience. 2013;16:1211–1218. doi: 10.1038/nn.3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Thau-Zuchman O, Shohami E, Alexandrovich AG, Leker RR. Combination of vascular endothelial and fibroblast growth factor 2 for induction of neurogenesis and angiogenesis after traumatic brain injury. Journal of molecular neuroscience : MN. 2012;47:166–172. doi: 10.1007/s12031-012-9706-8. [DOI] [PubMed] [Google Scholar]
- 167.Saul TG, Ducker TB, Salcman M, Carro E. Steroids in severe head injury: A prospective randomized clinical trial. Journal of neurosurgery. 1981;54:596–600. doi: 10.3171/jns.1981.54.5.0596. [DOI] [PubMed] [Google Scholar]
- 168.Braakman R, Schouten HJ, Blaauw-van Dishoeck M, Minderhoud JM. Megadose steroids in severe head injury. Results of a prospective double-blind clinical trial. Journal of neurosurgery. 1983;58:326–330. doi: 10.3171/jns.1983.58.3.0326. [DOI] [PubMed] [Google Scholar]
- 169.Gaab MR, et al. “Ultrahigh” dexamethasone in acute brain injury. Results from a prospective randomized double-blind multicenter trial (GUDHIS). German Ultrahigh Dexamethasone Head Injury Study Group. Zentralblatt fur Neurochirurgie. 1994;55:135–143. [PubMed] [Google Scholar]
- 170.Marshall LF, et al. A multicenter trial on the efficacy of using tirilazad mesylate in cases of head injury. Journal of neurosurgery. 1998;89:519–525. doi: 10.3171/jns.1998.89.4.0519. [DOI] [PubMed] [Google Scholar]
- 171.Asehnoune K, et al. Hydrocortisone and fludrocortisone for prevention of hospital-acquired pneumonia in patients with severe traumatic brain injury (Corti-TC): a double-blind, multicentre phase 3, randomised placebo-controlled trial. The Lancet. Respiratory medicine. 2014;2:706–716. doi: 10.1016/s2213-2600(14)70144-4. [DOI] [PubMed] [Google Scholar]
- 172.Raub TJ, et al. Use of a biophysical-kinetic model to understand the roles of protein binding and membrane partitioning on passive diffusion of highly lipophilic molecules across cellular barriers. Journal of drug targeting. 1993;1:269–286. doi: 10.3109/10611869308996085. [DOI] [PubMed] [Google Scholar]
- 173.Shakur H, et al. The BRAIN TRIAL: a randomised, placebo controlled trial of a Bradykinin B2 receptor antagonist (Anatibant) in patients with traumatic brain injury. Trials. 2009;10:109. doi: 10.1186/1745-6215-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Heard SO, et al. Effect of prophylactic administration of recombinant human granulocyte colony-stimulating factor (filgrastim) on the frequency of nosocomial infections in patients with acute traumatic brain injury or cerebral hemorrhage. The Filgrastim Study Group. Crit Care Med. 1998;26:748–754. doi: 10.1097/00003246-199804000-00027. [DOI] [PubMed] [Google Scholar]
- 175.Casha S, et al. Results of a phase II placebo-controlled randomized trial of minocycline in acute spinal cord injury. Brain : a journal of neurology. 2012;135:1224–1236. doi: 10.1093/brain/aws072. [DOI] [PubMed] [Google Scholar]
- 176.Hanlon LA, Huh JW, Raghupathi R. Minocycline Transiently Reduces Microglia/Macrophage Activation but Exacerbates Cognitive Deficits Following Repetitive Traumatic Brain Injury in the Neonatal Rat. Journal of neuropathology and experimental neurology. 2016;75:214–226. doi: 10.1093/jnen/nlv021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Satchell MA, et al. Cytochrome c, a biomarker of apoptosis, is increased in cerebrospinal fluid from infants with inflicted brain injury from child abuse. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2005;25:919–927. doi: 10.1038/sj.jcbfm.9600088. [DOI] [PubMed] [Google Scholar]
- 178.Rosomoff HL. Protective effects of hypothermia against pathological processes of the nervous system. Annals of the New York Academy of Sciences. 1959;80:475–486. doi: 10.1111/j.1749-6632.1959.tb49225.x. [DOI] [PubMed] [Google Scholar]
- 179.Marion DW, et al. Treatment of traumatic brain injury with moderate hypothermia. The New England journal of medicine. 1997;336:540–546. doi: 10.1056/nejm199702203360803. [DOI] [PubMed] [Google Scholar]
- 180.Andrews PJ, et al. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. The New England journal of medicine. 2015;373:2403–2412. doi: 10.1056/NEJMoa1507581. [DOI] [PubMed] [Google Scholar]
- 181.Clifton GL, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet neurology. 2011;10:131–139. doi: 10.1016/s1474-4422(10)70300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Diamond ML, et al. IL-1beta associations with posttraumatic epilepsy development: A genetics and biomarker cohort study. Epilepsia. 2015;56:991–1001. doi: 10.1111/epi.13100. [DOI] [PubMed] [Google Scholar]
- 183.Gentleman SM, et al. Long-term intracerebral inflammatory response after traumatic brain injury. Forensic science international. 2004;146:97–104. doi: 10.1016/j.forsciint.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 184.Johnson VE, et al. Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain : a journal of neurology. 2013;136:28–42. doi: 10.1093/brain/aws322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Ramlackhansingh AF, et al. Inflammation after trauma: microglial activation and traumatic brain injury. Annals of neurology. 2011;70:374–383. doi: 10.1002/ana.22455. [DOI] [PubMed] [Google Scholar]
- 186.Smith DH, Johnson VE, Stewart W. Chronic neuropathologies of single and repetitive TBI: substrates of dementia? Nature reviews. Neurology. 2013;9:211–221. doi: 10.1038/nrneurol.2013.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Smith C, et al. The neuroinflammatory response in humans after traumatic brain injury. Neuropathology and applied neurobiology. 2013;39:654–666. doi: 10.1111/nan.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Coughlin JM, et al. Neuroinflammation and brain atrophy in former NFL players: An in vivo multimodal imaging pilot study. Neurobiology of disease. 2015;74:58–65. doi: 10.1016/j.nbd.2014.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Juengst SB, Kumar RG, Arenth PM, Wagner AK. Exploratory associations with tumor necrosis factor-alpha, disinhibition and suicidal endorsement after traumatic brain injury. Brain, behavior, and immunity. 2014;41:134–143. doi: 10.1016/j.bbi.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 190.Nagamoto-Combs K, McNeal DW, Morecraft RJ, Combs CK. Prolonged microgliosis in the rhesus monkey central nervous system after traumatic brain injury. Journal of neurotrauma. 2007;24:1719–1742. doi: 10.1089/neu.2007.0377. [DOI] [PubMed] [Google Scholar]
- 191.Mouzon BC, et al. Chronic neuropathological and neurobehavioral changes in a repetitive mild traumatic brain injury model. Annals of neurology. 2014;75:241–254. doi: 10.1002/ana.24064. [DOI] [PubMed] [Google Scholar]
- 192.Loane DJ, et al. Novel mGluR5 positive allosteric modulator improves functional recovery, attenuates neurodegeneration, and alters microglial polarization after experimental traumatic brain injury. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2014;11:857–869. doi: 10.1007/s13311-014-0298-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Holmin S, Mathiesen T. Long-term intracerebral inflammatory response after experimental focal brain injury in rat. Neuroreport. 1999;10:1889–1891. doi: 10.1097/00001756-199906230-00017. [DOI] [PubMed] [Google Scholar]
- 194.Acosta SA, et al. Long-term upregulation of inflammation and suppression of cell proliferation in the brain of adult rats exposed to traumatic brain injury using the controlled cortical impact model. PloS one. 2013;8:e53376. doi: 10.1371/journal.pone.0053376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Shitaka Y, et al. Repetitive closed-skull traumatic brain injury in mice causes persistent multifocal axonal injury and microglial reactivity. Journal of neuropathology and experimental neurology. 2011;70:551–567. doi: 10.1097/NEN.0b013e31821f891f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Petraglia AL, et al. The spectrum of neurobehavioral sequelae after repetitive mild traumatic brain injury: a novel mouse model of chronic traumatic encephalopathy. Journal of neurotrauma. 2014;31:1211–1224. doi: 10.1089/neu.2013.3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Petraglia AL, et al. The pathophysiology underlying repetitive mild traumatic brain injury in a novel mouse model of chronic traumatic encephalopathy. Surgical neurology international. 2014;5:184. doi: 10.4103/2152-7806.147566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Winston CN, et al. Dendritic Spine Loss and Chronic White Matter Inflammation in a Mouse Model of Highly Repetitive Head Trauma. The American journal of pathology. 2016;186:552–567. doi: 10.1016/j.ajpath.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Byrnes KR, et al. Metabotropic glutamate receptor 5 activation inhibits microglial associated inflammation and neurotoxicity. Glia. 2009;57:550–560. doi: 10.1002/glia.20783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Loane DJ, Stoica BA, Byrnes KR, Jeong W, Faden AI. Activation of mGluR5 and inhibition of NADPH oxidase improves functional recovery after traumatic brain injury. Journal of neurotrauma. 2013;30:403–412. doi: 10.1089/neu.2012.2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Byrnes KR, Loane DJ, Stoica BA, Zhang J, Faden AI. Delayed mGluR5 activation limits neuroinflammation and neurodegeneration after traumatic brain injury. Journal of neuroinflammation. 2012;9:43. doi: 10.1186/1742-2094-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Rodgers KM, et al. Reversal of established traumatic brain injury-induced, anxiety-like behavior in rats after delayed, post-injury neuroimmune suppression. Journal of neurotrauma. 2014;31:487–497. doi: 10.1089/neu.2013.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.McKee AC, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. Journal of neuropathology and experimental neurology. 2009;68:709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.McKee AC, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain : a journal of neurology. 2013;136:43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Gardner RC, et al. Dementia risk after traumatic brain injury vs nonbrain trauma: the role of age and severity. JAMA neurology. 2014;71:1490–1497. doi: 10.1001/jamaneurol.2014.2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Barnes DE, et al. Traumatic brain injury and risk of dementia in older veterans. Neurology. 2014;83:312–319. doi: 10.1212/wnl.0000000000000616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lee YK, et al. Increased risk of dementia in patients with mild traumatic brain injury: a nationwide cohort study. PloS one. 2013;8:e62422. doi: 10.1371/journal.pone.0062422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Nordstrom P, Michaelsson K, Gustafson Y, Nordstrom A. Traumatic brain injury and young onset dementia: a nationwide cohort study. Annals of neurology. 2014;75:374–381. doi: 10.1002/ana.24101. [DOI] [PubMed] [Google Scholar]
- 209.Wang HK, et al. Population based study on patients with traumatic brain injury suggests increased risk of dementia. Journal of neurology, neurosurgery, and psychiatry. 2012;83:1080–1085. doi: 10.1136/jnnp-2012-302633. [DOI] [PubMed] [Google Scholar]
- 210.Heneka MT, et al. Neuroinflammation in Alzheimer’s disease. Lancet neurology. 2015;14:388–405. doi: 10.1016/s1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Perry VH, Nicoll JA, Holmes C. Microglia in neurodegenerative disease. Nature reviews. Neurology. 2010;6:193–201. doi: 10.1038/nrneurol.2010.17. [DOI] [PubMed] [Google Scholar]
- 212.McKee AC, et al. TDP-43 proteinopathy and motor neuron disease in chronic traumatic encephalopathy. Journal of neuropathology and experimental neurology. 2010;69:918–929. doi: 10.1097/NEN.0b013e3181ee7d85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Saing T, et al. Frontal cortex neuropathology in dementia pugilistica. Journal of neurotrauma. 2012;29:1054–1070. doi: 10.1089/neu.2011.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Webster KM, et al. Progesterone treatment reduces neuroinflammation, oxidative stress and brain damage and improves long-term outcomes in a rat model of repeated mild traumatic brain injury. Journal of neuroinflammation. 2015;12:238. doi: 10.1186/s12974-015-0457-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Hong YT, et al. Amyloid imaging with carbon 11-labeled Pittsburgh compound B for traumatic brain injury. JAMA neurology. 2014;71:23–31. doi: 10.1001/jamaneurol.2013.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Scott G, et al. Amyloid pathology and axonal injury after brain trauma. Neurology. 2016;86:821–828. doi: 10.1212/wnl.0000000000002413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Barrio JR, et al. In vivo characterization of chronic traumatic encephalopathy using [F-18]FDDNP PET brain imaging. Proceedings of the National Academy of Sciences of the United States of America. 2015;112:E2039–2047. doi: 10.1073/pnas.1409952112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Mitsis EM, et al. Tauopathy PET and amyloid PET in the diagnosis of chronic traumatic encephalopathies: studies of a retired NFL player and of a man with FTD and a severe head injury. Translational psychiatry. 2014;4:e441. doi: 10.1038/tp.2014.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Junger WG, et al. Prehospital hypertonic saline resuscitation attenuates the activation and promotes apoptosis of neutrophils in patients with severe traumatic brain injury. Shock. 2013;40:366–374. doi: 10.1097/shk.0000000000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Pagowska-Klimek I, Lewkowicz P, Banasik M, Krajewski W, Tchorzewski H. Isolated head injury in children affects the neutrophil function and lymphocyte count. The Journal of trauma. 2007;63:179–186. doi: 10.1097/TA.0b013e3180340dc9. [DOI] [PubMed] [Google Scholar]
- 221.Hazeldine J, Lord JM, Belli A. Traumatic Brain Injury and Peripheral Immune Suppression: Primer and Prospectus. Frontiers in neurology. 2015;6:235. doi: 10.3389/fneur.2015.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Wagner AK, et al. Adenosine A1 receptor gene variants associated with post-traumatic seizures after severe TBI. Epilepsy research. 2010;90:259–272. doi: 10.1016/j.eplepsyres.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Clark RS, et al. Cerebrospinal fluid adenosine concentration and uncoupling of cerebral blood flow and oxidative metabolism after severe head injury in humans. Neurosurgery. 1997;41:1284–1292. doi: 10.1097/00006123-199712000-00010. discussion 1292–1283. [DOI] [PubMed] [Google Scholar]
- 224.Bell MJ, Kochanek PM, Jackson EK. Interstitial Adenosine, Inosine, and Hypoxanthine Are Increased after Experimental Traumatic Brain Injury in the Rat. Journal of neurotrauma. 1998;15:163–170. doi: 10.1089/neu.1998.15.163. [DOI] [PubMed] [Google Scholar]
- 225.Kossmann T, Stahel PF, Morganti-Kossmann MC, Jones JL, Barnum SR. Elevated levels of the complement components C3 and factor B in ventricular cerebrospinal fluid of patients with traumatic brain injury. Journal of neuroimmunology. 1997;73:63–69. doi: 10.1016/s0165-5728(96)00164-6. [DOI] [PubMed] [Google Scholar]
- 226.Baker AJ, Moulton RJ, MacMillan VH, Shedden PM. Excitatory amino acids in cerebrospinal fluid following traumatic brain injury in humans. Journal of neurosurgery. 1993;79:369–372. doi: 10.3171/jns.1993.79.3.0369. [DOI] [PubMed] [Google Scholar]
- 227.Bullock R, et al. Factors affecting excitatory amino acid release following severe human head injury. Journal of neurosurgery. 1998;89:507–518. doi: 10.3171/jns.1998.89.4.0507. [DOI] [PubMed] [Google Scholar]
- 228.Chamoun R, Suki D, Gopinath SP, Goodman JC, Robertson C. Role of extracellular glutamate measured by cerebral microdialysis in severe traumatic brain injury. Journal of neurosurgery. 2010;113:564–570. doi: 10.3171/2009.12.jns09689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gao TL, et al. Expression of HMGB1 and RAGE in rat and human brains after traumatic brain injury. The journal of trauma and acute care surgery. 2012;72:643–649. doi: 10.1097/TA.0b013e31823c54a6. [DOI] [PubMed] [Google Scholar]
- 230.Adamczak S, et al. Inflammasome proteins in cerebrospinal fluid of brain-injured patients as biomarkers of functional outcome: clinical article. Journal of neurosurgery. 2012;117:1119–1125. doi: 10.3171/2012.9.jns12815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Clark RS, et al. Increases in Bcl-2 and cleavage of caspase-1 and caspase-3 in human brain after head injury. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 1999;13:813–821. doi: 10.1096/fasebj.13.8.813. [DOI] [PubMed] [Google Scholar]
- 232.Hayakata T, et al. Changes in CSF S100B and cytokine concentrations in early-phase severe traumatic brain injury. Shock. 2004;22:102–107. doi: 10.1097/01.shk.0000131193.80038.f1. [DOI] [PubMed] [Google Scholar]
- 233.Maier B, et al. Delayed elevation of soluble tumor necrosis factor receptors p75 and p55 in cerebrospinal fluid and plasma after traumatic brain injury. Shock. 2006;26:122–127. doi: 10.1097/01.shk.0000223127.41641.f4. [DOI] [PubMed] [Google Scholar]
- 234.Ross SA, Halliday MI, Campbell GC, Byrnes DP, Rowlands BJ. The presence of tumour necrosis factor in CSF and plasma after severe head injury. British journal of neurosurgery. 1994;8:419–425. doi: 10.3109/02688699408995109. [DOI] [PubMed] [Google Scholar]
- 235.Yan EB, et al. Post-traumatic hypoxia is associated with prolonged cerebral cytokine production, higher serum biomarker levels, and poor outcome in patients with severe traumatic brain injury. Journal of neurotrauma. 2014;31:618–629. doi: 10.1089/neu.2013.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Waters RJ, et al. Cytokine gene polymorphisms and outcome after traumatic brain injury. Journal of neurotrauma. 2013;30:1710–1716. doi: 10.1089/neu.2012.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Helmy A, Carpenter KL, Menon DK, Pickard JD, Hutchinson PJ. The cytokine response to human traumatic brain injury: temporal profiles and evidence for cerebral parenchymal production. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2011;31:658–670. doi: 10.1038/jcbfm.2010.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Buttram SD, et al. Multiplex assessment of cytokine and chemokine levels in cerebrospinal fluid following severe pediatric traumatic brain injury: effects of moderate hypothermia. Journal of neurotrauma. 2007;24:1707–1717. doi: 10.1089/neu.2007.0349. [DOI] [PubMed] [Google Scholar]
- 239.Chiaretti A, et al. Interleukin 1beta and interleukin 6 relationship with paediatric head trauma severity and outcome. Child’s nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2005;21:185–193. doi: 10.1007/s00381-004-1032-1. discussion 194. [DOI] [PubMed] [Google Scholar]
- 240.Hadjigeorgiou GM, et al. IL-1RN and IL-1B gene polymorphisms and cerebral hemorrhagic events after traumatic brain injury. Neurology. 2005;65:1077–1082. doi: 10.1212/01.wnl.0000178890.93795.0e. [DOI] [PubMed] [Google Scholar]
- 241.Helmy A, Antoniades CA, Guilfoyle MR, Carpenter KL, Hutchinson PJ. Principal component analysis of the cytokine and chemokine response to human traumatic brain injury. PloS one. 2012;7:e39677. doi: 10.1371/journal.pone.0039677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Mellergard P, Aneman O, Sjogren F, Saberg C, Hillman J. Differences in cerebral extracellular response of interleukin-1beta, interleukin-6, and interleukin-10 after subarachnoid hemorrhage or severe head trauma in humans. Neurosurgery. 2011;68:12–19. doi: 10.1227/NEU.0b013e3181ef2a40. discussion 19. [DOI] [PubMed] [Google Scholar]
- 243.Perez-Barcena J, et al. Lack of correlation among intracerebral cytokines, intracranial pressure, and brain tissue oxygenation in patients with traumatic brain injury and diffuse lesions. Crit Care Med. 2011;39:533–540. doi: 10.1097/CCM.0b013e318205c7a4. [DOI] [PubMed] [Google Scholar]
- 244.Hutchinson PJ, et al. Inflammation in human brain injury: intracerebral concentrations of IL-1alpha, IL-1beta, and their endogenous inhibitor IL-1ra. Journal of neurotrauma. 2007;24:1545–1557. doi: 10.1089/neu.2007.0295. [DOI] [PubMed] [Google Scholar]
- 245.Bell MJ, et al. Interleukin-6 and interleukin-10 in cerebrospinal fluid after severe traumatic brain injury in children. Journal of neurotrauma. 1997;14:451–457. doi: 10.1089/neu.1997.14.451. [DOI] [PubMed] [Google Scholar]
- 246.Kossmann T, Hans V, Imhof HG, Trentz O, Morganti-Kossmann MC. Interleukin-6 released in human cerebrospinal fluid following traumatic brain injury may trigger nerve growth factor production in astrocytes. Brain research. 1996;713:143–152. doi: 10.1016/0006-8993(95)01501-9. [DOI] [PubMed] [Google Scholar]
- 247.Kossmann T, et al. Intrathecal and serum interleukin-6 and the acute-phase response in patients with severe traumatic brain injuries. Shock. 1995;4:311–317. doi: 10.1097/00024382-199511000-00001. [DOI] [PubMed] [Google Scholar]
- 248.Maier B, et al. Differential release of interleukines 6, 8, and 10 in cerebrospinal fluid and plasma after traumatic brain injury. Shock. 2001;15:421–426. doi: 10.1097/00024382-200115060-00002. [DOI] [PubMed] [Google Scholar]
- 249.Shore PM, et al. Continuous versus intermittent cerebrospinal fluid drainage after severe traumatic brain injury in children: effect on biochemical markers. Journal of neurotrauma. 2004;21:1113–1122. doi: 10.1089/neu.2004.21.1113. [DOI] [PubMed] [Google Scholar]
- 250.Singhal A, et al. Association between cerebrospinal fluid interleukin-6 concentrations and outcome after severe human traumatic brain injury. Journal of neurotrauma. 2002;19:929–937. doi: 10.1089/089771502320317087. [DOI] [PubMed] [Google Scholar]
- 251.Winter CD, Pringle AK, Clough GF, Church MK. Raised parenchymal interleukin-6 levels correlate with improved outcome after traumatic brain injury. Brain : a journal of neurology. 2004;127:315–320. doi: 10.1093/brain/awh039. [DOI] [PubMed] [Google Scholar]
- 252.Kirchhoff C, et al. Cerebrospinal IL-10 concentration is elevated in non-survivors as compared to survivors after severe traumatic brain injury. European journal of medical research. 2008;13:464–468. [PubMed] [Google Scholar]
- 253.Yan EB, Hellewell SC, Bellander BM, Agyapomaa DA, Morganti-Kossmann MC. Post-traumatic hypoxia exacerbates neurological deficit, neuroinflammation and cerebral metabolism in rats with diffuse traumatic brain injury. Journal of neuroinflammation. 2011;8:147. doi: 10.1186/1742-2094-8-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Morganti-Kossmann MC, et al. TGF-beta is elevated in the CSF of patients with severe traumatic brain injuries and parallels blood-brain barrier function. Journal of neurotrauma. 1999;16:617–628. doi: 10.1089/neu.1999.16.617. [DOI] [PubMed] [Google Scholar]
- 255.Semple BD, Bye N, Rancan M, Ziebell JM, Morganti-Kossmann MC. Role of CCL2 (MCP-1) in traumatic brain injury (TBI): evidence from severe TBI patients and CCL2−/− mice. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2010;30:769–782. doi: 10.1038/jcbfm.2009.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Stefini R, et al. Chemokine detection in the cerebral tissue of patients with posttraumatic brain contusions. Journal of neurosurgery. 2008;108:958–962. doi: 10.3171/jns/2008/108/5/0958. [DOI] [PubMed] [Google Scholar]
- 257.Whalen MJ, et al. Interleukin-8 is increased in cerebrospinal fluid of children with severe head injury. Crit Care Med. 2000;28:929–934. doi: 10.1097/00003246-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 258.Engel S, et al. Dynamics of microglial activation after human traumatic brain injury are revealed by delayed expression of macrophage-related proteins MRP8 and MRP14. Acta neuropathologica. 2000;100:313–322. doi: 10.1007/s004019900172. [DOI] [PubMed] [Google Scholar]
- 259.Bonneh-Barkay D, et al. YKL-40 expression in traumatic brain injury: an initial analysis. Journal of neurotrauma. 2010;27:1215–1223. doi: 10.1089/neu.2010.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Zhang Z, et al. Human traumatic brain injury induces autoantibody response against glial fibrillary acidic protein and its breakdown products. PloS one. 2014;9:e92698. doi: 10.1371/journal.pone.0092698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Mazzeo AT, et al. Severe human traumatic brain injury, but not cyclosporin a treatment, depresses activated T lymphocytes early after injury. Journal of neurotrauma. 2006;23:962–975. doi: 10.1089/neu.2006.23.962. [DOI] [PubMed] [Google Scholar]
- 262.Maas AI, et al. Efficacy and safety of dexanabinol in severe traumatic brain injury: results of a phase III randomised, placebo-controlled, clinical trial. Lancet neurology. 2006;5:38–45. doi: 10.1016/s1474-4422(05)70253-2. [DOI] [PubMed] [Google Scholar]
- 263.Bulger EM, et al. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA : the journal of the American Medical Association. 2010;304:1455–1464. doi: 10.1001/jama.2010.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Adelson PD, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 11. Use of hyperosmolar therapy in the management of severe pediatric traumatic brain injury. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2003;4:S40–44. [PubMed] [Google Scholar]
- 265.Helmy A, et al. Recombinant human interleukin-1 receptor antagonist in severe traumatic brain injury: a phase II randomized control trial. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2014;34:845–851. doi: 10.1038/jcbfm.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Helmy A, et al. Recombinant human interleukin-1 receptor antagonist promotes M1 microglia biased cytokines and chemokines following human traumatic brain injury. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2015 doi: 10.1177/0271678x15620204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Tan M, Zhu JC, Du J, Zhang LM, Yin HH. Effects of probiotics on serum levels of Th1/Th2 cytokine and clinical outcomes in severe traumatic brain-injured patients: a prospective randomized pilot study. Critical care (London, England) 2011;15:R290. doi: 10.1186/cc10579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Tapia-Perez J, et al. Effect of rosuvastatin on amnesia and disorientation after traumatic brain injury (NCT003229758) Journal of neurotrauma. 2008;25:1011–1017. doi: 10.1089/neu.2008.0554. [DOI] [PubMed] [Google Scholar]
- 269.Sanchez-Aguilar M, et al. Effect of rosuvastatin on cytokines after traumatic head injury. Journal of neurosurgery. 2013;118:669–675. doi: 10.3171/2012.12.jns121084. [DOI] [PubMed] [Google Scholar]