Abstract
Introduction:
Recent increases in drug overdose deaths, both in New York City and nationally, highlight the need for timely data on psychoactive drug-related morbidity. We developed drug syndrome definitions for syndromic surveillance to monitor drug-related emergency department (ED) visits in real time.
Materials and Methods:
We used 2012 archived syndromic surveillance data from New York City hospitals to develop definitions for psychoactive drug-related syndromes. The dataset contained ED visit-level information that included patients’ chief complaints, dates of visits, ZIP codes of residence, discharge diagnoses, and dispositions. After manually reviewing chief complaints, we developed a classification scheme comprising 3 categories (overdose, drug mention, and drug abuse/misuse), which we used to define 25 psychoactive drug syndromes. From July 2013 through December 2015, the New York City Department of Health and Mental Hygiene performed daily syndromic surveillance of psychoactive drug-related ED visits using the 25 syndrome definitions.
Results:
Syndromic surveillance triggered 4 public health investigations, supported 8 other public health investigations that had been triggered by other mechanisms, and resulted in the identification of 5 psychoactive drug-related outbreaks. Syndromic surveillance also identified a substantial increase in synthetic cannabinoid-related visits (from an average of 3 per week in January 2014 to >300 per week in July 2015) and an increase in heroin overdose visits (from 80 to 171 in the first 3 quarters of 2012 and 2014, respectively) in a single neighborhood.
Practice Implications:
Syndromic surveillance using these novel definitions enabled monitoring of trends in psychoactive drug-related morbidity, initiation and support of public health investigations, and targeting of interventions. Health departments can refine these definitions for their jurisdictions using the described methods and integrate them into existing syndromic surveillance systems.
Keywords: syndromic surveillance, drugs, interventions
Since the terrorist attacks on September 11, 2001, many state and local health departments have developed syndromic surveillance systems to monitor emergency department (ED) visits in real time.1,2 These systems rely on information collected routinely as part of an ED visit, including the patient’s chief complaint, age, sex, and residence location. EDs transmit these data to health departments, which aggregate and analyze the data. Health departments can create “syndrome” definitions by grouping specific keywords or terms found in chief complaints. Using these syndrome definitions, health departments can more quickly query datasets and identify trends in ED visits. Although syndromic surveillance systems were initially developed to identify instances of bioterrorism, many health departments have developed syndrome definitions to monitor ED visits related to other acute health conditions of public health concern, such as heat-related illness, influenza-like illness, food poisoning, and rabies.1,3–5
For the past 10 years, the New York City Department of Health and Mental Hygiene (DOHMH) has been conducting surveillance on morbidity related to psychoactive drugs using 2 traditional administrative data systems: the Drug Abuse Warning Network (DAWN) and the Statewide Planning and Research Cooperative System (SPARCS).6,7 DAWN data were used to formulate estimates of drug-related ED visits in metropolitan areas in New York City, as well as in 37 US states; however, DAWN was discontinued after 2011. SPARCS contains patient-level data on demographic characteristics, diagnoses, treatments, services, levels of care, and charges for hospital admissions and ED visits in New York State. However, SPARCS is not particularly well-suited for surveillance of morbidity from psychoactive drugs. The data lag by ≥1 year, making it difficult to obtain real-time information from this system. In addition, SPARCS relies on the use of International Classification of Diseases, Clinical Modification (ICD-CM) codes instead of free text in its chief complaint fields. However, because no distinct ICD-CM codes exist for certain psychoactive drugs (eg, synthetic cannabinoids and methylenedioxymethamphetamine [MDMA]), visits related to these drugs cannot be uniquely identified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) or International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes.
Syndromic surveillance is an alternative approach that allows public health departments to quickly detect and intervene on new public health problems, and it has proven to be useful from a public health perspective in identifying and addressing many acute illnesses.3–5 Compared with the use of traditional administrative data for surveillance, syndromic surveillance offers several advantages, including more timely data production, more analytic flexibility, and easier integration into routine public health work. Because syndromic surveillance data usually include a free-text chief complaint field, health departments can modify syndrome definitions easily and quickly to conduct event- or situation-based surveillance. In addition, departments can standardize and automate the analysis of incoming syndromic surveillance data, allowing for smoother integration into their existing workflow.
Consequently, syndromic surveillance represents an opportunity for better surveillance of drug-related morbidity, and some public health jurisdictions have already started using it to monitor opioid overdoses or ED visits related to emerging psychoactive drugs.8,9 However, to our knowledge, no other jurisdiction has initiated comprehensive monitoring of drug-related morbidity, incorporating a wide range of psychoactive drugs, using syndromic surveillance data. Our objective was to develop a comprehensive set of syndrome definitions that could be used as part of syndromic surveillance to accurately monitor and identify trends in drug-related morbidity in real time and that would allow rapid assessment of the impact of subsequent public health interventions.
Methods
Initial Data Source
In 2013, we obtained an archived syndromic surveillance dataset from the New York City DOHMH Bureau of Communicable Diseases, consisting of information from 97% of the ED visits made to New York City hospitals during 2012. The dataset contained patient-level ED visit data concerning date and time of visit; chief complaint (free text); patient age, sex, and ZIP code of residence; discharge diagnoses (ICD-9-CM codes); and patient disposition.
Development of Syndrome Definitions
Although discharge diagnosis data containing ICD-9-CM codes were available, we decided against including them in our syndrome definitions, in an effort to maintain the ability to compare morbidity trends before and after the transition to ICD-10-CM. This transition was initially slated to occur on October 1, 2013, but it actually occurred on October 1, 2015. We anticipated that around the time of the transition, an increasing number of hospitals would begin sending the new codes to administrative databases, making comparisons of pre- and post-transition Health Level 7-compliant syndromic surveillance data challenging.
To begin building our syndrome definitions, we manually reviewed approximately 10 000 ED visit chief complaints, doing so until we stopped seeing variations in drug types, spellings, and drug-related street terminology. During this process, we identified and recorded all chief complaints related to psychoactive drugs. In reviewing these chief complaints, we found that they fell into 1 or more of 3 conceptual categories—overdose, drug mention, and drug abuse/misuse. We reasoned that these 3 conceptual categories would help us formulate syndrome definitions based on ED visit chief complaints, which would ultimately facilitate the capture of drug-related ED visits from datasets. We then began to assign the chief complaints to syndromes, applying a one-to-many approach in which the same chief complaint could be assigned to >1 syndrome. Using this process, we eventually developed a list of 25 syndromes within the 3 conceptual categories (Table).
Table.
Psychoactive drug-related conceptual categories and syndromes based on chief complaints extracted from emergency department syndromic surveillance data, New York City, 2012-2014
| Conceptual Category | Syndrome |
|---|---|
| Drug overdose | Overdose |
| Drug mention | Alcohol Amphetamines Benzodiazepine Buprenorphine Cocaine Drug (unspecified) Flakka gamma-Hydroxybutyric acid (GHB) Heroin Ketamine Kratom Marijuana Methadone Methamphetamine Methylenedioxymethamphetamine (MDMA) Naloxone Opioid Opioid analgesics Phencyclidine (PCP) Synthetic cannabinoids Synthetic cathinone (“bath salts”) |
| Drug abuse/misuse | Detoxification Drug abuse Withdrawal |
Making use of the archived dataset, we constructed the 25 syndrome definitions in the following manner: (1) We reviewed chief complaints to generate a preliminary list of drug search terms; (2) we queried drug-related words (eg, smoked, drug, overdose) to identify additional search terms to include in the individual syndrome definitions; (3) we identified possibly related misspellings by searching for fragments of words of interest (eg, searching for “uana” identified the misspelling “marijauana” for marijuana); and (4) we reviewed drug-related discharge diagnosis codes to identify additional search terms.
Once we finalized the search terms to be used for each syndrome, we manually reviewed the chief complaints again to identify exclusion terms that would be used to avoid capturing unrelated chief complaints. For example, the cocaine syndrome definition identified ED visits in which the chief complaint contained the word “crack”; however, we modified the definition so that ED visits with chief complaints containing both “crack” and “tooth” were excluded. We then tested all exclusion terms (such as “tooth”) in the archived dataset for all 25 syndromes to confirm that ED visits of interest were not inadvertently excluded.
Among the 25 syndromes, 1 was in the overdose conceptual category, 21 were in the drug mention category, and 3 were in the drug abuse/misuse category. The definition for the 1 syndrome in the drug overdose category included the search term “overdose,” as well as search terms involving related misspellings and abbreviations of “OD.” The definitions for the 21 syndromes within the drug mention conceptual category included search terms to identify particular drugs or classes of drugs. These syndromes pertained to alcohol, amphetamines, benzodiazepines, buprenorphine, cocaine, drug (unspecified), flakka, gamma-hydroxybutyric acid, heroin, kratom, ketamine, marijuana, methadone, methamphetamine, MDMA, naloxone, opioid, opioid analgesics, PCP (phencyclidine), synthetic cathinone (“bath salts”), and synthetic cannabinoids (Table). Finally, the definitions for the 3 syndromes in the drug abuse/misuse conceptual category contained search terms to identify ED visits related to detoxification, withdrawal, and substance abuse.
We coded these drug-related syndromes using SAS version 9.2 and used Perl regular expression to extract information.10 Using Perl regular expression allowed for complex pattern matching, identification of common misspellings of drugs, and exclusions of strings likely to result in misclassification. A regular expression is a character string that defines a search pattern. Perl regular expression can be used to identify specific misspellings; for example, searching for “mar[ia]juana” identifies both “marajuna” and “marijuana.” It can also be used to identify a substring for exclusion; for example, searching for “[A-Z]OD” identifies the string “xOD,” where x is any letter from A to Z. Without the “[A-Z]OD” exclusion term, a syndrome definition that searched for “OD” would classify a chief complaint containing “OD” (eg, “food”) as an overdose-related ED visit.
Analysis of Drug-Related ED Visits Identified by Syndromic Surveillance
After creating the 25 syndrome definitions and applying them to the archived 2012 dataset, we subsequently automated analysis of all of the syndromes to run daily from July 1, 2013, through December 31, 2015. For all syndromes, we calculated ED visit risk ratios by dividing the observed number of visits by the expected number of visits, with the latter value based on the daily mean number of visits determined using the 2012 archived dataset. We assumed that ED visits followed a Poisson distribution, with daily means calculated from the 2012 baseline data, and we programmed the system to send an email alert if the daily counts were significantly different than those expected daily mean values. We considered P ≤ .05 to be significant.
We generated daily maps for syndromes, showing geographic clustering and aggregated daily count data over time, to identify both city-level and neighborhood-level trends in drug-related morbidity. As part of our daily monitoring, we also reviewed data concerning drug mention syndromes, which captured information on drug specificity, in conjunction with data from related overdose or drug abuse/misuse syndromes. For example, we reviewed the status of heroin-involved overdoses by identifying chief complaint field entries meeting both the heroin drug mention and the overdose syndrome definitions.
Given the public health interest in possible overdose clusters, we also performed daily spatial analyses using 4 geographic units: hospital, neighborhood of hospital, neighborhood of patient’s residence, and ZIP code of patient’s residence. To identify possible geographic clusters with high rates of overdose-related ED visits, we used SaTScan version 9.1.1 to perform space-time analyses fitted to Poisson regression models.11 This analytic method allowed us to identify overdose clusters during varying periods of time. Because of the potential for false positives associated with multiple comparisons, we examined all alerts produced by SaTScan that had P < .001.
Using all of these syndromic data, we regularly analyzed the magnitudes of the upward changes in drug-related morbidity and the quantities of excess morbidity over time. As part of this analysis, we also considered information from other data sources, including drug poisoning mortality data from the New York City Office of the Chief Medical Examiner and DOHMH Office of Vital Statistics, as well as individual reports from medical providers. These additional data provided context and helped DOHMH decide whether to initiate drug-related investigations, which would usually include reviews of medical records and qualitative interviews with patients and medical providers.
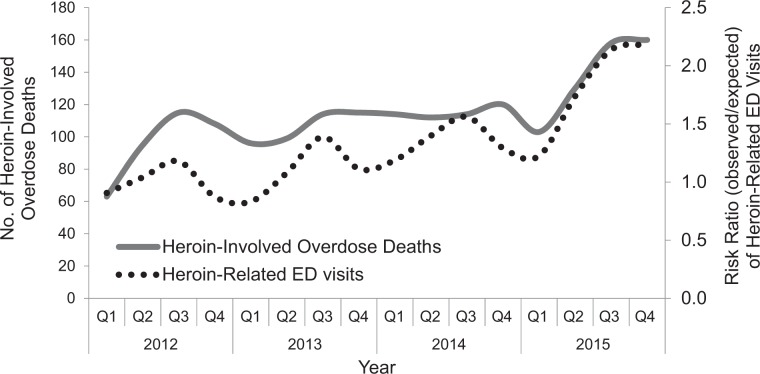
Finally, focusing only on adverse health events related to heroin, we measured the correlation between heroin-related syndromic surveillance data and heroin-involved mortality data (from the Office of the Chief Medical Examiner) to determine if changes in heroin-related morbidity were associated with changes in heroin-involved mortality. We calculated the Pearson r coefficient to determine the level of correlation between heroin-related ED visits and heroin-involved overdose deaths. We performed statistical testing using the t test and considered P ≤ .05 to be significant.
This study was considered exempt by the New York City DOHMH Institutional Review Board.
Results
From July 1, 2013, through December 31, 2015, syndromic surveillance results led directly to the initiation of 4 public health investigations, supported 8 other public health investigations that had been triggered by other mechanisms, and resulted in the identification of 5 psychoactive drug-related outbreaks. Two of the outbreaks would not have been identified without syndromic surveillance; 1 was identified without syndromic surveillance, but syndromic surveillance provided additional data that defined the scope of the outbreak; for another outbreak, syndromic surveillance provided earlier warning than did other mechanisms (eg, provider report); and 1 outbreak was identified simultaneously in syndromic surveillance and through provider reports, but syndromic surveillance provided a more accurate understanding of the affected patient population, the magnitude of the increase, and the geographic areas affected.
We describe, in detail, 3 representative psychoactive drug-related public health investigations that were triggered by syndromic surveillance and helped with decisions about whether to pursue public health interventions. In some cases, the impact of interventions was then rapidly assessed by repeating syndromic surveillance. These 3 investigations centered on an increase in synthetic cannabinoid-related morbidity, an increase in heroin-related overdoses, and a potential increase in the presence of fentanyl in New York City.
Synthetic Cannabinoids
During the 3-day period from July 24 to July 26, 2014, syndromic surveillance detected an unusual increase in synthetic cannabinoid-related ED visits in New York City, identifying a total of 10 of these visits, half of which occurred among residents of 2 New York City neighborhoods. Review of the chief complaint fields in the 10 records suggested that residents of shelters and other facilities were particularly affected.12 In comparison, during the entire month of January 2014, syndromic surveillance had detected an average of only 3 synthetic cannabinoid-related ED visits per week across all of New York City, and from January 1 to July 26, 2014, syndromic surveillance had detected 188 synthetic cannabinoid-related ED visits in the city. During this latter period, syndromic surveillance data identified a relatively consistent demographic profile across time, with a median patient age of 34.5 years and 84% (157/188) of cannabinoid-related ED visits occurring among men.
This acute increase in the number of synthetic cannabinoid-related ED visits detected by syndromic surveillance prompted DOHMH to initiate a public health investigation, which included medical chart reviews and qualitative interviews with medical providers and patients with a recent synthetic cannabinoid-related ED visit.12 After this investigation, DOHMH continued to monitor trends in synthetic cannabinoid-related ED visits, and additional increases in the number of these visits eventually prompted DOHMH to issue health advisories on 3 separate occasions between July 2014 and September 2015.13–15
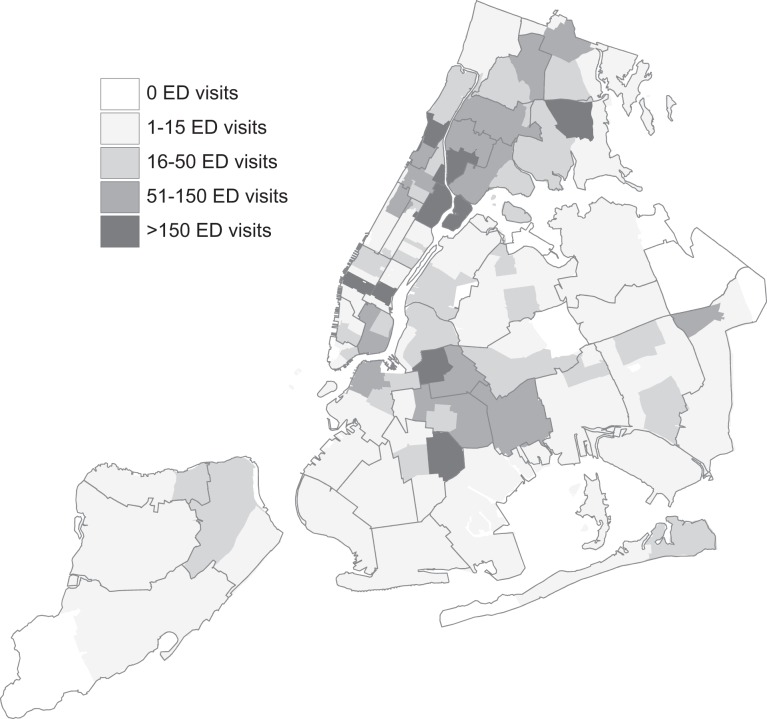
Data from syndromic surveillance, combined with the results of the public health investigation, informed DOHMH efforts to intervene. An organized program was initiated to reduce the availability of synthetic cannabinoid products throughout New York City. These efforts included removing products that were sold either openly or covertly from stores and seizing both raw materials and finished products from New York City distributors. As part of this effort, DOHMH used aggregate data from syndromic surveillance to prioritize which neighborhoods should be the focus of the synthetic cannabinoid product reduction program (Figure 1). Following these citywide efforts to reduce cannabinoid availability, which began in July 2015, DOHMH then used syndromic surveillance data again, this time to measure the impact of the product reduction intervention on synthetic cannabinoid-related ED visits. The number of synthetic cannabinoid-related ED visits decreased 73% between July 2015 (1215 ED visits) and December 2015 (334 ED visits). In this case, early detection of an at-risk population and of geographic clustering was key to initiating the formulation of a public health response to rising synthetic cannabinoid-related morbidity in New York City. In addition, the application of syndrome surveillance after initiating the intervention illustrated the impact of that intervention.
Figure 1.
Geographic spatial distribution of synthetic cannabinoid-related emergency department (ED) visits, by ZIP code of patient residence, based on data from New York City Department of Health and Mental Hygiene, Bureau of Alcohol, Drug Use Prevention, Care, and Treatment, New York City, January 1-December 31, 2015. Not all EDs reported the name of the drug involved in the ED visit. Data are incomplete and should be interpreted with caution.
Heroin
In 2014, heroin syndrome surveillance identified a single New York City neighborhood experiencing an increase in heroin-related ED visits. During the first 3 quarters of 2014, syndromic surveillance detected 171 heroin-related ED visits compared with the 80 heroin-related ED visits that were expected based on 2012 mean data, representing a significant increase (P < .001). This neighborhood was subsequently also found to have an increase in fatal drug overdoses during the same time period, in which 16 fatal heroin-involved overdoses among neighborhood residents occurred compared with the 7 fatal heroin-involved overdoses that were expected based on 2012 mean data (P = .01). DOHMH also compared those data with heroin-related mortality data to determine whether trends in heroin-related ED visits correlated with changes in the number of heroin-involved overdose deaths. Indeed, the number of heroin-related ED visits was highly correlated (r = .88, P < .001) with the number of heroin-involved overdose deaths (Figure 2).
Figure 2.
Heroin-involved overdose deaths and heroin-related emergency department (ED) visits, by quarter, based on data from New York City Department of Health and Mental Hygiene, Bureau of Alcohol, Drug Use Prevention, Care, and Treatment; New York City Office of the Chief Medical Examiner; and New York City Department of Health and Mental Hygiene, Bureau of Vital Statistics; New York City, 2012-2015. Using Pearson correlation coefficient (r = .88, P < .001, based on t test, null hypothesis: r = 0). Analysis of data performed by Bureau of Alcohol, Drug Use Prevention, Care, and Treatment. Heroin-related ED visit risk ratios calculated by dividing observed visits by expected visits, with the latter value based on the mean number of visits determined using archived syndromic surveillance dataset from the New York City Department of Health and Mental Hygiene, Bureau of Communicable Diseases, consisting of information from 97% of the ED visits made to New York City hospitals during 2012. Abbreviation: Q, quarter.
As a result, DOHMH conducted a public health investigation to confirm the cases, identify the most affected populations, and guide neighborhood-level interventions. DOHMH intervened by working with the affected neighborhoods to disseminate information about the increase in overdoses and to engage and mobilize stakeholders. Additional overdose prevention trainings—where participants learned to recognize an opioid overdose, respond by calling 9-1-1, perform rescue breathing, and administer naloxone—were also held in the neighborhood, and participants who completed the training received an overdose prevention kit, which included 2 doses of naloxone.
In addition, because syndromic surveillance data identified a single hospital that was treating most of the patients with heroin-related ED visits, DOHMH presented these findings, as well as relevant mortality data, to ED staff members at this hospital. DOHMH also instructed ED staff members in how to provide overdose prevention training and naloxone kits to those at risk for an opioid-involved overdose, particularly to those who had come to the ED because of an opioid overdose. In this case, overdose prevention trainings and distribution of naloxone were not expected to reduce the number of heroin-related ED visits but, rather, to prevent overdoses from becoming fatal. And, because overdose is a relatively rare event and this particular intervention involved only a single neighborhood, we made no attempt to measure the impact of this small-scale prevention and naloxone distribution program.
Fentanyl
In 2014, DOHMH also used overdose, opioid, and heroin syndrome surveillance to monitor trends in overdose-related ED visits during a time period in which several mid-Atlantic and Northeastern US jurisdictions had reported local heroin supplies being contaminated with fentanyl, as well as increases in overdoses involving fentanyl.16 Fentanyl is an opioid analgesic with a potency 50 to 100 times that of morphine, and so it may increase the overdose risk among people who are unaware that it may be present in illicit drugs.
We did not create a fentanyl-specific syndrome definition because we found no reason to suspect that patients with fentanyl-involved overdoses would have records mentioning fentanyl in the chief complaint field. Specifying fentanyl in the chief complaint field for overdose-related ED visits would have required patients to self-report fentanyl use (unlikely because, even now, most drug users in New York City are not aware of the potential for fentanyl contamination of the heroin supply) or an ED triage/intake nurse to suspect fentanyl use (also unlikely). Consequently, syndromic surveillance for fentanyl focused on identifying dramatic increases in heroin, opioid, or overdose syndromes rather than identifying fentanyl in the chief complaint field.
Because of the lack of drug specificity for fentanyl in the chief complaint field, DOHMH reviewed syndromic surveillance data for changes in the number of ED visits detected by the overdose, heroin, and opioid syndrome definition, with the goal of identifying trends that might suggest the presence of fentanyl in the New York City heroin supply. As part of the investigation, DOHMH also reviewed New York City Poison Control Center data, law enforcement illicit drug seizure data, and deaths reported to the New York City Office of the Chief Medical Examiner during January 2014.
The number of ED visits detected by the overdose, heroin, or opioid syndrome definitions did not increase. In addition, none of the data from other sources (New York City Poison Control Center, law enforcement seizure data, Office of the Chief Medical Examiner) suggested any increase in the presence of fentanyl in New York City. Using all of this information, in January 2014, DOHMH ultimately determined there was no increase in fentanyl-related morbidity or mortality in New York City. However, despite this reassurance, DOHMH did still issue a health advisory alerting medical and harm-reduction providers in New York City to the increase in overdoses related to fentanyl in areas surrounding New York City, although not within the city itself.16
Discussion
Public health investigations have historically focused on infectious disease outbreaks. However, the recent increase in psychoactive drug-related morbidity in the United States has renewed interest in public health investigations focusing on drug-related adverse health events. In addition, the benefits of increased public access to naloxone to reverse opioid overdoses have rekindled interest in implementing strategies to reduce drug-related morbidity and mortality. Syndromic surveillance is well suited to playing a key role in monitoring drug-related morbidity given the timeliness of the data it provides, the analytic flexibility it allows, and its ease of integration into routine public health work.
We have demonstrated how syndromic surveillance can be used to provide real-time information about local trends in drug-related ED visits. We have also given examples of how data from syndromic surveillance can be used to develop and implement timely public health interventions. As well, we have shown how syndromic surveillance can be repeated to determine whether these interventions have been successful. In New York City, syndromic surveillance of drug-related ED visits is a critical component of drug-related surveillance and helps inform core public health functions. The New York City DOHMH uses real-time drug syndromic surveillance data to determine when to initiate or assist with outbreak investigations, when to issue health advisories, and when to allocate additional resources to neighborhoods experiencing increases in drug-related morbidity.
Many health departments in the United States operate ED syndromic surveillance systems. The 25 drug syndromes described in this article can easily be integrated into those existing surveillance systems. By using these syndrome definitions and automating syndromic surveillance analyses, daily analytic workload can be reduced. The real value of such integrated surveillance, however, may be that it can serve as an early warning system for health departments, allowing them to more promptly and accurately target investigations and interventions that have the potential to reduce drug-related morbidity and mortality. An important component of initiating a drug-related syndromic surveillance process such as this one is the provision of adequate resources and staffing, not only to conduct investigations triggered by surveillance data but also to develop and implement interventions based on the findings of these public health investigations. Such resources for response and intervention are critically important for syndromic surveillance to help achieve the goal of improving public health.
Limitations
This study had several limitations. First, we used data from 51 EDs in New York City, which allowed us to analyze chief complaints from a large number and wide variety of hospitals in building our syndrome definitions. However, other jurisdictions may draw their data from hospitals with different ways of describing chief complaints. In addition, our syndrome definitions, initially formulated in 2013, may not contain a few novel uncommon misspellings, drug terms, and colloquial drug terminology that have emerged since that time or are specific to other areas of the country. Consequently, before other health departments implement surveillance with these syndrome definitions, they should consider using the previously described methods to refine these syndrome definitions at the local level. Second, because of time and resource constraints, we did not measure the sensitivity or positive predictive values of the syndrome definitions we developed. However, given that our primary interest was in trend identification, only moderate sensitivity was needed.17 Indeed, we found that trends identified in heroin-related ED visits were strongly correlated with trends in heroin overdose mortality (r = .88), and DOHMH was able to use this trend information to initiate early public health investigations and interventions. Furthermore, we favored conceptualizing the sensitivity of a surveillance system as its ability to identify an outbreak, and use of the syndrome definitions we developed led to 4 public health investigations, supported 8 other public health investigations, and resulted in identifying 5 psychoactive drug-related outbreaks. Nevertheless, we acknowledge that there may be some value in knowing the positive predictive value of each syndrome definition; as such, a manual review of the free-text chief complaint fields to calculate these positive predictive values is planned in the future.
Practice Implications
We created 25 psychoactive drug-related syndrome definitions to use in syndromic surveillance for the early identification of trends and outbreaks and for informing public health responses. When used by New York City DOHMH, syndromic surveillance with these definitions identified clustered increases in drug-related morbidity for synthetic cannabinoids and heroin, and it supported outbreak investigations of these events. Moreover, syndromic surveillance provided additional information, which we used to support public health investigations and implement interventions, than would otherwise have been available using traditional surveillance mechanisms. Syndromic surveillance was also used to provide reassurance that New York City, unlike surrounding jurisdictions, was not experiencing an acute increase in fentanyl-related overdoses. DOHMH now relies heavily on syndromic surveillance with these definitions as part of its comprehensive drug surveillance program in New York City. These syndrome definitions can be implemented by other health departments that desire an early warning system for temporal and geographical changes in psychoactive drug-related morbidity, potentially offering the opportunity to formulate more rapid public health responses.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Heffernan R, Mostashari F, Das D, Karpati A, Kulldorff M, Weiss D. Syndromic surveillance in public health practice, New York City. Emerg Infect Dis. 2004;10(5):858–864. [DOI] [PubMed] [Google Scholar]
- 2. Steiner-Sichel L, Greenko J, Heffernan R, Layton M, Weiss D. Field investigations of emergency department syndromic surveillance signals—New York City. MMWR Morb Mortal Wkly Rep. 2004;53(suppl):184–189. [PubMed] [Google Scholar]
- 3. Westheimer E, Paladini M, Balter S, Weiss D, Fine A, Nguyen TQ. Evaluating the New York City emergency department syndromic surveillance for monitoring influenza activity during the 2009-10 influenza season. PLoS Curr. 2012;4:e500563f3ea181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marx MA, Rodriguez CV, Greenko J, et al. Diarrheal illness detected through syndromic surveillance after a massive power outage: New York City, August 2003. Am J Public Health. 2006;96(3):547–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bregman B, Slavinski S. Using emergency department data to conduct dog and animal bite surveillance in New York City, 2003-2006. Public Health Rep. 2012;127(2):195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nolan M, Tuazon E, Mantha S, Yim B, Paone D. Cocaine use in New York City: morbidity and mortality. N Y City Dep Health Mental Hygiene Epi Data Brief. 2015;54:1–2. [Google Scholar]
- 7. Bradley O’Brien D, Paone D, Shah S, Heller D. Drugs in New York City: misuse, morbidity, and mortality update. NY City Dep Health Mental Hygiene Epi Data Brief. 2011;10:1–2. [Google Scholar]
- 8. Ising A, Proescholdbell S, Harmon KJ, Sachdeva N, Marshall SW, Waller AE. Use of syndromic surveillance data to monitor poisonings and drug overdoses in state and local public health agencies. Inj Prev. 2016;22(suppl 1):i43–i49. [DOI] [PubMed] [Google Scholar]
- 9. Yun LW, Beum R, Askenazi M, et al. Using emergency department data for detection of a synthetic marijuana outbreak. Online J Public Health Inform. 2015;7(1):e178. [Google Scholar]
- 10. SAS Institute Inc. SAS: Version 9.2. Cary, NC: SAS Institute Inc; 2012. [Google Scholar]
- 11. Kulldorff M. SaTScan: Version 9.1.1. Rockville, MD: Information Management Services Inc; 2011. [Google Scholar]
- 12. Nolan ML, Allen B, Kunins HV, Paone D. A public health approach to increased synthetic cannabinoid-related morbidity among New York City residents, 2014-2015. Int J Drug Policy. 2016;34:101–103. [DOI] [PubMed] [Google Scholar]
- 13. New York City Department of Health and Mental Hygiene. 2014 advisory #18: increase in synthetic cannabinoid-related adverse events and emergency department visits, New York City; 2014. https://www1.nyc.gov/assets/doh/downloads/pdf/ah/Synthetic%20cannabinoids-HAN-advisory-7%2027%2014%2011 AM.pdf. Accessed November 1, 2016. [Google Scholar]
- 14. New York City Department of Health and Mental Hygiene. 2015 advisory #6: increase in synthetic cannabinoid (marijuana)-related adverse events and emergency department visits, New York City. 2015. https://www1.nyc.gov/assets/doh/downloads/pdf/ah/marijuana-alert.pdf. Accessed November 1, 2016.
- 15. New York City Department of Health and Mental Hygiene. 2015 advisory #36: increase in synthetic cannabinoid (K2)-related adverse events and emergency department visits, New York City. 2015. https://www1.nyc.gov/assets/doh/downloads/pdf/ah/Synthetic%20cannabinoids-HAN-advisory_Summer%202015%20-penultimate8.pdf. Accessed November 1, 2016.
- 16. New York City Department of Health and Mental Hygiene. 2014 advisory #3: cases of fentanyl-associated overdoses in mid-Atlantic and Northeast United States. 2014. https://a816-health30ssl.nyc.gov/sites/nychan/lists/alertupdateadvisorydocuments/fentanyl-advisory-feb2014-han-feb6-final.pdf. Accessed November 1, 2016.
- 17. German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA, Waller MN; Guidelines Working Group, Centers for Disease Control and Prevention. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Morb Mortal Wkly Rep. 2001;50(RR-13):1–35. [PubMed] [Google Scholar]