Abstract
Posttraumatic stress disorder (PTSD) is associated with self-reported difficulties navigating the social and physical world and may also be associated with risk of functional limitations. The Short Physical Performance Battery (SPPB), an objective functional assessment, was administered during monitoring exams between January and December 2015 to a consecutive sample of 1,268 rescue workers, volunteers, and other responders who aided in response, recovery, and cleanup efforts at the World Trade Center (WTC) in New York after the September 11, 2011 attacks. Data were linked with diagnostic and longitudinal data from the WTC monitoring study. Multivariable analyses were used to examine predictors of functional limitations. Prevalence estimates weighted to the general responder population revealed a relatively high prevalence of functional limitations, SPPB ≤ 9; 16.0%, 95% CI [13.7, 18.4]. Current PTSD was associated with a two-fold increased risk of functional limitations after controlling for predisposing factors, trauma severity, behavioral factors, and WTC-related medical conditions, Adjusted Risk Ratio (aRR) = 2.11, 95% CI [1.48, 3.01]. Exposure to ergonomic risk factors at the WTC also increased the risk of functional impairments, aRR=1.34 95% CI [1.05, 1.70]. Longitudinal results suggest that individuals with current functional limitations experienced high baseline PTSD severity, B = 2.94, SE=1.33, and increasing PTSD symptom severity, B = 0.29, SE = 0.10, since September 11, 2001. This study identified a cross-sectional relationship between functional limitations and PTSD and a worsening of PTSD symptoms in persons who eventually demonstrate functional limitations. Results highlight the potential role of chronic PTSD in functional limitations.
Functional limitations, an early marker of disability indicated by slowed walking, difficulties getting out of a chair, and difficulties maintaining balance (Guralnik, et al., 1994), are strongly associated with morbidity and mortality as individuals age (Studenski, et al., 2011). Functional limitations may arise from the slow accumulation of exposures across the life course resulting in systemic degradation (Hayflick, 2007), are predictive of impaired mobility and age-related physical disabilities (Newman, et al., 2006), and are commonly attributed with degradation in quality of life (Freedman, et al., 2013). Furthermore, this degradation has been broadly documented across domains of physical capability (Kuh, Cooper, Hardy, Richards, & Ben Shlomo, 2014), with the result that physical capability is increasingly being used as a surrogate biomarker for systemic aging (Sanderson & Scherbov, 2014).
Functional limitations are increasingly being used in clinical settings as indicators of patient health (Afilalo, et al., 2014), and to identify at-risk populations with which to intervene (Fragala, et al., 2015; Pahor, et al., 2014). Known risk factors for physical impairments include age-related comorbidities such as diabetes (de Souza Moreira), cardiovascular disease (Newman, et al., 2006), obesity (Zutler, et al., 2012), depression (Geerlings, Beekman, Deeg, Twisk, & Van Tilburg, 2001), cognitive decline (Clouston, et al., 2013), and impaired pulmonary functioning (Choi, Son, Cho, Park, & Cho, 2012). Less is known about early life exposures and aging.
One potential risk factor for increased functional limitation is posttraumatic stress disorder (PTSD), a form of chronic intrusive stress that has the potential to result in more rapid aging and impairment. Though often thought of as a rare disease, nearly all older people have experienced at least one lifetime traumatic event (Kuwert, Pietrzak, & Glaesmer, 2013), and estimates suggest that as much as one-tenth of the general population may have clinical levels of PTSD (Kessler, et al., 2005), though many more experience less severe forms of the disease.
There is a known correlation between PTSD and increased risk of aging-related pathologies including, for example, cognitive impairment (Clouston, et al., 2016), dementia (Qureshi, et al., 2010), cardiovascular disease (Beristianos, Yaffe, Cohen, & Byers, 2016), obesity (Smith, Tyzik, Neylan, & Cohen, 2015), cellular senescence (Shalev, et al., 2013), and mortality (Lohr, et al., 2015). Prior work has found that chronic PTSD is also associated with poorer quality of life (Zatzick, et al., 1997), and increased levels of disability (Byers, Covinsky, Neylan, & Yaffe, 2014). Thus, despite no association between age and risk of PTSD (Luft, et al., 2012), it is possible that chronic PTSD might increase the risk of age-related functional limitation. However, alternative interpretations include that individuals with PTSD may overreport physical limitations and disability.
On September 11, 2001, terrorist attacks on the World Trade Center (WTC) in New York City traumatized many Americans. Rescue workers, volunteers, and other responders who aided in the initial response, recovery operations, and cleanup efforts that resulted from the building collapse experienced both acute and chronic environmental and psychological exposures (Dasaro, et al., 2015). More than one-fifth of responders developed WTC-related PTSD, half of whom had PTSD 13 years later (Bromet, Hobbs, et al., 2015). Since then, researchers have linked WTC exposures to various health problems, including increased risk of asthma (Wisnivesky, et al., 2011) and gastrointestinal issues (Li, et al., 2011), to name a few. Yet despite the high burden of cognitive impairment, lowered pulmonary functioning, and systemic inflammation in this population (Aldrich, et al., 2010; Clouston, et al., 2016; Kazeros, et al., 2015), little is known about the burden of functional limitations among WTC responders.
To date, the literature has not examined the extent to which PTSD is associated with physical functioning or functional limitations, nor is it clear when or why such associations develop. This study focused on a cohort of responders to the WTC disaster in order to examine whether longitudinally assessed PTSD was associated with objective measures of functional limitations after accounting for traumatic exposures and comorbid WTC-related medical conditions. We posited that PTSD would be associated with objective measures of physical impairment. Associations will be robust to exposures experienced at the WTC. Furthermore, associations should be evident broadly across different domains of functioning.
Method
Participants
In 2002, the Centers for Disease Control and Prevention established a monitoring and treatment program for September 11, 2001 rescue and recovery workers. To date, more than 33,000 responders have enrolled in the WTC general responder population (GRP; (Dasaro, et al., 2015). Stony Brook University (SBU) monitors more than 8,000 responders primarily residing on Long Island, NY, who are similar in terms of exposure, sex, and age to those enrolled in the GRP (Dasaro, et al., 2015). The responders monitored by SBU are mostly males (92.0%) who, on September 11, 2001, worked in law enforcement (71.5%) and whose average age was 38.9 years; they are now 50–60 years old. Continuing through to the present, most SBU responders (85.0%) return to either Nassau or Suffolk county clinics within 18 months of their prior visit.
In 2015, the SBU program began collecting objectively assessed indicators of physical functioning. The current study focused on a consecutive sample of responders (n = 1,268) who were monitored between January and April 2016 in Suffolk County clinics, and April 2015 to April 2016 in Nassau County clinics. All responders seen during those time periods were eligible to participate. Response rates to the additional measure were very high (98.8%). Of eligible responders who were not assessed but were approached, most cited time constraints (n = 7) as a main reason to decline the assessment and others (n = 5) refused due to vertigo or recent surgery. To understand the potential for confounding and describe PTSD symptom trajectories among those participants who had functional limitations, data were linked to monitoring data collected prospectively since 2002. The study was approved by the Stony Brook University Ethics Review Board; responders provided informed, written consent.
When compared with the SBU population of responders who were eligible for research but did not complete the functional assessment, those who completed the functional assessment were 0.85 years younger than those who did complete the assessment (p < .001) and were less likely to be women (p = .004), but had similar occupations on September 11, 2001 (p = .115), similar levels of current PTSD (p = .521), and similar baseline PCL scores (p = .455). Longitudinal data from the monitoring study revealed that 1,268 responders in the analytic sample had previously provided 10,904.5 person-years of information collected during 7,013 visits occurring between 2002 and 2015.
Few existing publicly available studies include normative data comparable to the WTC sample. Studies that have measured functional limitations have done so among individuals aged 65 years and older, and many samples are not large enough to match by occupation. For our comparison, we therefore used data from participants aged 65 to 69 years from the baseline wave of the National Health and Aging Trends Study (NHATS) (2011). The NHATS is a nationally representative study of 8,245 older American adults, 1,419 of whom were aged 65 to 69 years at baseline. To further ensure comparability, we excluded respondents with less than a high school diploma (n = 289), and those whose longest lifetime occupations were not common for WTC responders (e.g. protective services, maintenance, construction, utilities, trades/repair, transportation, community and social services, or military occupations; n = 938). Of those who remained, 170 respondents had completed the physical performance battery. Analyses were weighted to the U.S. population to account for sample selection.
Measures
Functional Limitations
To objectively measure functional limitations, trained healthcare providers administered the SPPB during monitoring visits (Guralnik, et al., 1994). The measure consists of three brief functional assessments that have been validated to objectively evaluate the potential for and extent of physical functioning and impairment: standing balance, five-times sit-to-stand testing, and usual walking speed over four meters. In each case, time taken to complete the test was recorded. Speed, in rises/second (chair-rise speed) or meters/second (walking speed), was calculated. To examine individual components of the SPPB, dichotomous cut-points were utilized to characterize people as being with or without functional limitations in these components. The following cut-points were used: < 0.8 m/s walking speed (Lauretani, et al., 2003), > 13 s on the chair rise times (Whitney, et al., 2005), and inability to hold all three positions in the balance test for ten seconds. The performance assessments were also scored according to the standard scoring algorithm for the SPPB, with the score ranging from 0 to 12, with 12 indicating the best functioning (Guralnik, et al., 2000). Scores ≤ 9 were used to identify functional limitations, a cutoff with good sensitivity and specificity to detect frailty in older adults (da Câmara, Alvarado, Guralnik, Guerra, & Maciel, 2013). Severe functional limitation was defined as occurring when SPPB ≤ 7.
Exposure history
Exposure severity was assessed during the first monitoring visit using a structured history. Many responders experienced overlapping exposures. First, “early arrival” indicated whether responders arrived at the WTC site on September 11, 2001 and were caught in the dust cloud that was present that day. Second, “chronic exposure” identified responders who worked at the WTC site at least seven days in September 2001, digging through the debris looking for survivors and human remains. Third, we examined whether individuals reported having been exposed, during WTC-related work activities, to “ergonomic exposures” (e.g., repetitive motions, forceful exertions [muscle efforts], awkward or static postures, manual or heavy lifting, vibrations, or impact tool usage). Finally, an overall exposure severity index, commonly used in WTC-related pulmonary research, was also used (Wisnivesky, et al., 2011).
PTSD symptoms
At each monitoring visit, which occurred approximately 1.5 years apart, PTSD symptoms were routinely assessed (Bromet, Hobbs, et al., 2015). Participants’ PTSD symptoms were assessed using the 17-item PTSD Checklist (PCL), a validated measure of DSM-IV PTSD symptomatology (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). Internal reliability of the PCL in this population was excellent (Cronbach’s α = .95), and the index was very good at identifying diagnosed PTSD (area under the receiver operating curve (AUC) = .86). To create a DSM-IV measure of current PTSD, the items were summed and a standard cutoff of 44 was used (Kroenke & Spitzer, 2002; Terhakopian, Sinaii, Engel, Schnurr, & Hoge, 2008). Longitudinal data were used to identify individuals with possible PTSD and lifetime symptom inventories were used to identify individuals with current or remitted PTSD.
Depression symptoms
Mental health specialists diagnosed WTC responders with major depression when appropriate. Diagnoses were verified by staff at the Centers for Disease Control and Prevention.
Predisposing characteristics
These included: (1) education: because 95.8% of responders in the SBU population had at least a high school degree, education was categorized into “some college or less” versus “bachelor’s degree or more”, with less education serving as the reference category; (2) occupation: this was dichotomized into law enforcement (which comprised a large proportion of the SBU population), and nontraditional responders (a group made up largely of construction and utility workers).
Health and behavioral mediators
These were assessed using five indicators: current or past smoking; hazardous drinking (≥ 8 on the Alcohol Use Disorder Identification Test; (Bohn, Babor, & Kranzler, 1995); obesity, operationalized as body mass index > 30 kg/m2 based on nurse-measured height and weight; and clinician-reported diagnoses of hypertension and diabetes.
WTC-related comorbidities
First, one-second forced expiratory volume (FEV1), a continuous measure of overall pulmonary functioning, was assessed using the EasyOneTM spirometer (Medical Technologies, Andover, MA, USA) following a standard protocol (Enright, Skloot, & Herbert, 2008). Because PTSD may have resulted from or been exacerbated by WTC-related medical comorbidities we also accounted for common WTC-related medical diagnoses including obstructive airway disease, upper respiratory disease, and gastroesophageal reflux disease. Finally, because PTSD may be exacerbated by stressful events occurring after WTC experiences, we included a dichotomous indicator noting whether individuals reported having experienced any stressful events experienced including, for example, job loss, loss of spouse/partner or friend, muggings or violence, robberies or break-ins, serious illnesses, arrests, and injuries, among others. Sensitivity analyses examined using a count of such activities.
Data Analysis
Descriptive sample statistics, including means and standard deviations, as well as percentages were provided. Probability weights were derived using temporally stable demographic indicators to estimate prevalence separately for the GRP. Estimates were used in combination with overall cohort size to estimate the number of patients in each cohort who may have functional limitations. Bivariate analyses were used to provide p values from, alternatively, t tests and tests of proportions. Tests of proportions were used to compare the risk of functional limitations with normative data. In both cases, exact p values were provided. Cohen’s d was calculated for all analyses; to maintain model parsimony, covariates with Cohen’s d < 0.3 were excluded from further analysis.
Logistic regression was used to estimate the odds ratios for functional limitations according to risk factor status. Functional limitations are not rare in this sample, resulting in overestimation of the relative risk, so results from logistic regression were used to calculate the Muller and MacLehose (2014) relative risk. Multivariable analyses provide adjusted risk ratios (aRR).
Longitudinal multilevel modeling was used to examine mental health trajectories since enrollment in the program and to examine associations between trajectories and current functional limitations (Gibbons, Hedeker, Waternaux, & Davis, 1988). Models are an application of multilevel modeling approaches (Rabe-Hesketh & Skrondal, 2008), which are commonly utilized in aging literature to model change over time (Gale, Allerhand, Sayer, Cooper, & Deary, 2014). Models integrated individual-level random intercepts to account for unobserved heterogeneity in baseline symptomatology. Random slopes estimate individual-specific growth and account for heteroskedasticity common in growth models. Using an unstructured covariance matrix further accounts for associations between baseline capability and change over time. To facilitate comprehension, graphical trajectories were provided that compared responders with and without functional limitations. In all analyses, two-tailed p values were used; an alpha of .05 was used to determine statistical significance. Missing data were uncommon, and were dealt with through listwise deletion. Analyses were implemented in Stata 14.1/IC. The SBU ethics review board (Stony Brook, New York) reviewed this study. Responders provided informed written consent.
Prior work has noted the sizable loss in power resulting from categorizing continuous data (Cohen, 1983; MacCallum, Zhang, Preacher, & Rucker, 2002). Sensitivity analyses therefore employed a generalized linear modeling approach in order to examine the benefit of using the continuous SPPB measure in multivariable analyses, and when examining correlates of physical functioning subdomains. In the first case, models employed a Poisson distribution and a log link function to account for underlying distributional differences, whereas in the latter case a normal distribution and identity link function was employed.
Results
The mean age of participants was 53.8 (SD=8.4) years. Overall, one-fifth of participants had a history of probable PTSD following the WTC disaster, more than half of whom had current PTSD. Estimated prevalence, weighted to the GRP, for functional limitations was 16.0%, 95% CI [13.7, 18.4], and for severe functional limitations was 4.4%, 95% CI [3.1, 5.7].
Whereas the majority of responders had physical functioning in the normal range, 22.1% showed signs of limitations in at least one measured domain of functioning and 3.5% had limitations in at least two measured domains. Overall, slow chair rise had the highest prevalence of the three measured domains. Using established cutoffs for each specific domain revealed the prevalence to be: 17.1%, 95% CI [14.6, 19.7] for slow chair-rise speed (speeds < 0.39 rises/s, equivalent to times ≥ 13 s); 6.9%, 95% CI [5.2, 8.5] for slow walking speed (< 0.8 m/s); and 5.4%, 95% CI [4.0, 6.8] for any balance difficulties.
Compared with responders with no functional limitations, those with functional limitations were older, less likely to work or have worked in law enforcement, had lower educational attainment, reported ergonomic exposures at the WTC, and were more likely to have current PTSD (Table 1). They were also more likely to have major depression, obstructive airway disease, upper respiratory disease, and gastroesophageal reflux disease.
Table 1.
Sample Characteristics and Unadjusted Analyses Linking Covariates to Functional Limitations, World Trade Center Aging Study, 2002–2015
| Variable | Full Sample (N = 1271) | No Functional Limitations (n = 1084) | Functional Limitations (n = 187) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Mean | SD | % | Mean | SD | Mean | SD | % | Cohen’s da | ||
| Current age, years | 53.75 | 8.32 | 53.32 | 8.11 | 56.22 | 9.06 | −.35*** | |||
|
| ||||||||||
| Enrollment year | 2007.47 | 3.22 | 2007.54 | 3.22 | 2007.05 | 3.16 | .15 | |||
|
| ||||||||||
| One-second Forced Expiratory Volume, liters | 3.31 | 0.72 | 3.34 | 0.71 | 3.14 | 0.74 | .30** | |||
|
| ||||||||||
| Female | 7.6 | 7.6 | 8.0 | .10 | ||||||
| Educational attainment | ||||||||||
| High school or less | 21.6 | 19.8 | 31.6 | .35** | ||||||
| Some college | 47.6 | 48.9 | 40.1 | |||||||
| University degree | 30.8 | 31.3 | 28.3 | |||||||
| Law enforcement | 72.9 | 74.9 | 61.5 | .68** | ||||||
| Early arrival to WTC siteb | 42.6 | 43.5 | 37.4 | .25 | ||||||
| Chronic exposure | 9.6 | 10.0 | 7.5 | .28 | ||||||
| Ergonomic exposures | 72.3 | 71.2 | 78.0 | .33 | ||||||
| Exposure Severity Index | ||||||||||
| Low | 18.2 | 18.2 | 18.0 | .29 | ||||||
| Medium | 57.4 | 56.4 | 63.4 | |||||||
| High | 21.8 | 22.7 | 16.8 | |||||||
| Severe | 2.6 | 2.7 | 1.9 | |||||||
| WTC-PTS | ||||||||||
| Current | 12.4 | 9.8 | 27.3 | 1.57*** | ||||||
| Remitted | 10.7 | 10.1 | 14.4 | |||||||
| None | 76.9 | 80.2 | 58.3 | |||||||
| Major depression | 14.1 | 12.4 | 24.1 | .96*** | ||||||
| Obese | 53.0 | 53.0 | 52.9 | .00 | ||||||
| Smoking status | ||||||||||
| Current smoker | 6.3 | 6.5 | 4.8 | .29 | ||||||
| Former smoker | 30.9 | 30.1 | 35.8 | |||||||
| Never smoked | 62.8 | 63.4 | 59.4 | |||||||
| Hazardous drinker | 3.0 | 2.7 | 4.8 | .72 | ||||||
| Hypertensive | 27.8 | 26.7 | 34.2 | .38 | ||||||
| Diabetic | 7.0 | 6.1 | 12.3 | .93** | ||||||
| Upper respiratory disease | 41.1 | 37.9 | 59.9 | .67*** | ||||||
| Lower respiratory disease | 62.6 | 60.3 | 75.9 | .93*** | ||||||
| Gastroesophageal Reflux Disease | 49.5 | 46.6 | 66.3 | .80*** | ||||||
Note. Moderate functional limitations were defined as scores on the Short Physical Performance Battery (SPPB) ≤ 9. Bivariate associations were derived from two-tailed t tests and chi-square tests. WTC = World Trade Center; PTS = posttraumatic stress.
Although significance was defined as alpha of .05 for interpretation, Cohen’s d < 0.3 was used as a cutoff to retain potentially important confounders for multivariable analyses.
Early arrival constitutes arriving on September 11 2001 and being caught in the dust cloud.
p < .05.
p < .01.
p < .001
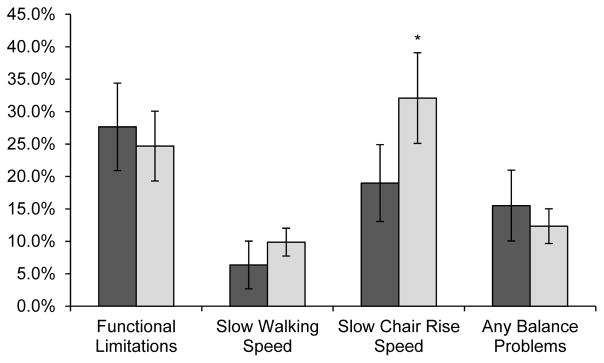
Results from normative data analyses (Figure 1) revealed that among individuals aged 65 to 69 years, WTC responders had much slower chair-rise speed than did normal comparisons from the NHATS study. On average, WTC responders had increased risk (RR=1.69, 95% CI [1.08, 2.64], p = .022) of having slow chair-rise speed when compared with normative data. However, there were no overall differences in balance or walking speed, the result of which was no overall difference in functional limitations.
Figure 1.
Comparing the risk of low physical functioning and functional limitations among responders to the September 11, 2001 World Trade Center (WTC) attacks and those of The National Health and Aging Trends Study (NHATS) respondents aged 65 to 69 years. Data were for 170 NHATS respondents (dark gray) and 81 WTC responders (light gray). 95% confidence intervals provided as error bars.
*p = .003.
Table 2 revealed that law enforcement personnel had fewer functional limitations. Older age, low education, and diagnoses of WTC-related conditions were associated with worse functioning. After adjustment, responders with current PTSD had a higher risk of functional limitations. Because associations between functional limitations and current, but not remitted, PTSD suggest that symptoms may get progressively worse, the following describes temporal trends in PTSD symptoms in the years prior to functional assessments.
Table 2.
Adjusted Risk Ratios (aRR) and 95% Confidence Intervals (CI) Examining the Association Between PTSD and Risk of Functional Limitations, World Trade Center Aging Study, 2002–2015
| Variable Name | Category | aRRa | 95% CI |
|---|---|---|---|
| Posttraumatic stress | Remitted vs. None | 1.28 | [0.77, 2.14] |
| Current vs. None | 2.02*** | [1.42, 2.87] | |
| Age in years | 1.02* | [1.00, 1.04] | |
| Enrollment year | 0.90 | [0.48, 1.67] | |
| Forced expiratory volume (1 s) | 0.80 | [0.61, 1.04] | |
| Education | Some college vs. High school | 0.50** | [0.32, 0.80] |
| University degree vs. High school | 0.58* | [0.34, 0.97] | |
| Law enforcement | 1.04 | [0.71, 1.51] | |
| Ergonomic exposures | 1.35* | [1.07, 1.72] | |
| Any post-WTC stressful events | 1.18 | [0.90, 1.54] | |
| Major depression | 0.73 | [0.45, 1.19] | |
| Hazardous drinker | 1.13 | [0.77, 1.64] | |
| Hypertensive | 0.80 | [0.56, 1.16] | |
| Diabetic | 1.51* | [1.03, 2.21] | |
| Lower respiratory disease | 1.31* | [1.05, 1.68] | |
| Upper respiratory disease | 1.24 | [0.98, 1.56] | |
| Gastroesophageal reflux disease | 1.28* | [1.03, 1.59] |
Note. p values are derived from two-tailed t tests. WTC = World Trade Center.
aRRs compare risk of possible functional limitation.
p < .05.
p < .01.
p < .001.
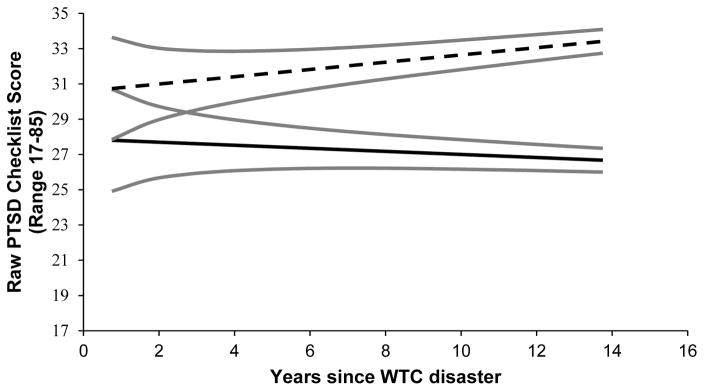
Longitudinal trajectories mapping PTSD symptom change in the years prior to measurement of functional limitations (Figure 2; full results in Table S1) revealed associations between baseline PTSD symptomatology and functional limitations. However, after accounting for these associations, responders with functional limitations experienced increasing PTSD symptomatology in the years preceding functional assessments.
Figure 2.
Longitudinal trajectories of change in posttraumatic stress disorder symptom severity by functional limitation status among responders to the September 11, 2001 World Trade Center (WTC) attacks (full results available in Table S1). Dashed black lines (- -) indicate those with functional limitations in 2015 and solid black lines (—) indicate those without functional limitations. 95% Confidence intervals (gray solid lines) were also provided. PTSD = posttraumatic stress disorder; WTC = World Trade Center.
Sensitivity analyses examining determinants of SPPB scores revealed results similar to those found for functional limitations. Analyses of functional subdomains revealed strong adjusted associations between current PTSD and having walking speed slower than 0.8 m/s (aRR = 3.72, 95% CI [1.94, 7.12]), as well as associations with chair-rise speed slower than 0.39 rises/s (aRR = 2.46, 95% CI [1.48, 4.11]) and any balance problems (aRR = 2.51, 95% CI [1.22, 5.18]). Results did not reveal any significant association with ergonomic exposures at the subdomain level. Sensitivity analyses using continuous metrics revealed similar results to those presented above.
Regarding the severity of functional limitations, the estimated prevalence of functional limitations weighted to the GRP (N ~ 33,000) was 16.0%, 95% CI [13.8, 18.4]. This prevalence translated into approximately 4,550 to 6,100 responders with functional limitations, of whom 460 to 1,130 might have had severe functional limitations.
Discussion
This study examined the possibility that PTSD might be associated with increased risk of functional limitations and found that in a clinic-based monitoring study approximately one-sixth of WTC responders (16.1%, 95% CI [13.8, 18.4]) had functional limitations. Multivariable results suggested that PTSD was associated with functional limitations (aRR = 2.11, 95% CI [1.48, 3.01]) after adjusting for sociodemographic factors, depression, and other WTC-related conditions. We found that WTC responders aged 65 to 69 years had an increased risk of slow chair-rise speed when compared with normative data (RR = 1.69, 95% CI [1.08, 2.64] p = .022). Finally, we identified a small but significant association between WTC ergonomic exposures and the risk of functional limitations (aRR = 1.34, 95% CI [1.04, 1.70]).
World Trade Center responders appear to be experiencing physical aging at a greater rate than is otherwise expected. Substantial literature highlights the role of WTC experiences in causing elevated and chronic PTSD (Bromet, Clouston, et al., 2015), and concomitant medical comorbidities (Neria, DiGrande, & Adams, 2011). This study supports earlier work noting that individuals with PTSD are at greater risk of reporting difficulties navigating their social and physical world, but extends results to objective indicators of functioning.
Although we were surprised by the extent of functional limitations in this sample, especially earlier in life, there was no data with which to compare prevalence estimates among individuals less than 65 years of age. In this paper, we were able to use national data from the NHATS to compare functional a small number of WTC responders with non-responders, and found that WTC responders had higher rates of difficulty rising from a chair. This preliminary analysis was only powered to detect large differences in risk, making these results conservative. Nevertheless, chair rise speed is a common measure of aging, and is usually discussed in the context of lower body mobility and strength (Bohannon, 2006). Chair speed is also a correlated with risk of neurological disorders including Parkinson’s (Inkster, Eng, MacIntyre, & Stoessl, 2003) and Alzheimer’s disease (de Souto Barreto, et al., 2016), indicating the potential for neurological etiology. It is, nevertheless, also worth noting that individuals aged 65 to 69 years at the time of the study were 50 to 55 years on September 11, 2001 and thus may be exceptionally healthy workers even when compared with other, younger, WTC responders and thus comparisons may be increasingly biased at older ages. Future analyses should seek to identify a more appropriate control population to replicate these findings.
The reasons for PTSD symptom growth over time are unclear. One possibility is that the experience of increasing impairments are simply frustrating and emotionally charged for WTC responders, who may increasingly attribute their limitations to WTC exposures, evident as PTSD. A second possibility is that PTSD may result in increased neurodegeneration. Prior work has detailed similar increases in PTSD symptoms among people with cognitive impairments (Clouston, et al., 2016). Of particular concern, a shared pattern of physical and cognitive impairment co-occurring with increases in emotionality may signal the potential for an increased risk of neurodegenerative diseases in general and may, specifically, highlight an elevated potential for behavioral frontotemporal dementia (FTD), a neurodegenerative disease that can include behavioral and emotional changes alongside physical impairments (Mackenzie, 2007). Future research should examine whether cognitive and physical impairment co-occurr with personality changes and should also examine whether neurodegeneration is common among those with physical limitations.
Results also support prior work highlighting the utility of understanding the role of trauma as a possible risk factor for poorer health (Ferrucci & Guralnik, 2013). Results might also support the view that functional aging may be, in traumatized populations, a long-term consequence of chronic PTSD. Further research is needed to replicate and examine mechanisms for these associations. Future research is also warranted that examines the potential for nontraumatic but chronic or intrusive stress to influence functional aging.
As the responders age, it is increasingly important that we understand how WTC exposures and experiences may impact their long-term health and aging. This study suggests that physical and psychological exposures received on-site, as well as PTSD resulting from the September 11, 2001 attacks and aftermath may have increased the risk of functional limitations. However, we did not specifically examine other mechanisms linking PTSD to functional performance. A number of possible mediators exist, including, for example, changing levels of physical activity (Vancampfort, et al., 2016), pain and comorbid anxiety disorders including PTSD (Asmundson, Coons, Taylor, & Katz, 2002; Asmundson & Katz, 2009), or increased fatigue or fatigability that may co-occur with PTSD (Keller-Ross, Schlinder-Delap, Doyel, Larson, & Hunter, 2014), potentially signifying targets for intervention.
This study used a relatively young sample. Indeed, it is the first study to examine functional limitations among those aged ≤ 55 years. This relative youth may help to contribute to our understanding of aging-related processes, as late life studies of aging are subject to different types of biases including: (a) reverse causality, when aging results in other physical or mental changes as was seen here and elsewhere (Singh-Manoux, et al., 2011); (b) mortality and survivor bias, as those experiencing the most rapid aging die and are excluded from further analysis (Studenski, et al., 2011); and (c) temporal lag, which results when exposures in early life predate both the variable of interest and confounders. Although these forces were present here, only a small fraction of responders have already died to date, and those who have may have been older or had more comorbidity, making results from this study potentially conservative.
Results from this study may not be generalizable. First, responders reside in Long Island, NY and are predominantly highly educated and employed males who were predominantly law enforcement officers at the time of the disaster. Moreover, officers passed comprehensive physical and psychological assessments prior to being hired and thus this study reflects very healthy, but severely traumatized, individuals. Yet, PTSD from different exposures does not clearly appear to have unique presentation or sequelae, making this cohort an ideal cohort with which to study long-term implications of trauma.
A second problem that is impossible to examine here is that there is at least a possibility that those who were among the older responders on September 11, 2001 were a particularly healthy subset of the overall population of potential responders. Those who were older on September 11, 2001, likely include only those who were still able to respond, despite being older and having similar overall working conditions. If true, then comparisons between responders and healthy controls from secondary data may underestimate the size of the WTC exposure effects.
This was the first assessment of physical functioning collected in this population, which occurred over a decade after the disaster. However, the vast majority of WTC responders were relatively young and working in physically demanding jobs during the disaster, suggesting that functional limitations are more likely to have developed following WTC responder experiences. Nevertheless, there is the potential for WTC experiences to have generated increasingly worsening physical functioning since September 11, 2001, thus potentially resulting in increasing levels of PTSD concurrent with increasing levels of physical disability. Future work should collect prospective data to disentangle potential effects.
Enrollment in the clinic is voluntary and ongoing although extensive outreach efforts have continued throughout the program’s lifetime. Such enrollment may result in bias if later-enrollees differ in physical capability or PTSD symptomatology from earlier enrollees. However, no association was found between enrollment year and functional limitations, or trajectories of PTSD symptomatology suggesting that such biases may be of limited importance to this study.
In the event that these results are generalizable to the WTC clinical population and are replicable in other populations, clinicians should be aware of the large, unrecognized burden of functional limitations among middle-aged and older individuals with PTSD. Functional limitations exacerbate the course of disease, as those with limitations may be less capable of interacting with the everyday world. As such, functional limitations may increase the risk for other aging-related diseases, such as cardiovascular disease or obesity. To date, however, few studies have found clinical treatments that work to improve functional limitations. One promising opportunity is through the use of structured interventions to increase moderate-intensity physical activities, which has been shown to improve functional performance and reduce the incidence of mobility disability over a period of three years (Pahor, et al., 2014). Nevertheless, further research is needed that seeks to examine the effectiveness of physical activity interventions among individuals with PTSD.
Supplementary Material
Acknowledgments
Funding for this article was provided by the National Institutes of Health (R01 AG049953), and by the Centers for Disease Control and Prevention’s National Institute of Occupational Safety and Health to administer the monitoring survey and diagnose and treat World Trade Center (WTC)-related diseases (CDC-200-2011-39361). The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. The funders played no role in data collection, analysis, interpretation, reporting, or the decision to submit for publication.
References
- Afilalo J, Alexander KP, Mack MJ, Maurer MS, Green P, Allen LA, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. 2014;63(8):747–762. doi: 10.1016/j.jacc.2013.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldrich TK, Gustave J, Hall CB, Cohen HW, Webber MP, Zeig-Owens R, et al. Lung Function in Rescue Workers at the World Trade Center after 7 Years. New England Journal of Medicine. 2010;362(14):1263–1272. doi: 10.1056/NEJMoa0910087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47(10):930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. 2009;26(10):888–901. doi: 10.1002/da.20600. [DOI] [PubMed] [Google Scholar]
- Beristianos MH, Yaffe K, Cohen B, Byers AL. PTSD and Risk of Incident Cardiovascular Disease in Aging Veterans. Am J Geriatr Psychiatry. 2016;24(3):192–200. doi: 10.1016/j.jagp.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bohannon RW. Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Percept Mot Skills. 2006;103(1):215–222. doi: 10.2466/pms.103.1.215-222. [DOI] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR. The Alcohol-Use Disorders Identification Test (Audit) - Validation of a Screening Instrument for Use in Medical Settings. Journal of Studies on Alcohol. 1995;56(4):423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- Bromet E, Clouston S, Hobbs M, Kotov R, Gonzalez A, Luft BJ. Burden of PTSD in Stony Brook WTC-HP Rescue/Recovery Workers. Paper presented at the WTC Primary Investigators Meeting; 26 Federal Plaza, NYC. 2015. [Google Scholar]
- Bromet E, Hobbs M, Clouston S, Gonzalez A, Kotov R, Luft BJ. DSM-IV PTSD among World Trade Center responders 11–13 Years after 9/11. Psychological Medicine. 2015;46(4):771–783. doi: 10.1017/S0033291715002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL, Covinsky KE, Neylan TC, Yaffe K. Chronicity of posttraumatic stress disorder and risk of disability in older persons. JAMA Psychiatry. 2014;71(5):540–546. doi: 10.1001/jamapsychiatry.2014.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi HC, Son KY, Cho B, Park SM, Cho SI. An implication of the short physical performance battery (SPPB) as a predictor of abnormal pulmonary function in aging people. Archives of Gerontology and Geriatrics. 2012;54(3):448–452. doi: 10.1016/j.archger.2011.03.010. [DOI] [PubMed] [Google Scholar]
- Clouston S, Brewster P, Kuh D, Richards M, Cooper R, Hardy R, et al. The dynamic relationship between physical function and cognition in longitudinal aging cohorts. Epidemiologic Reviews. 2013;35(1):33–50. doi: 10.1093/epirev/mxs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston S, Kotov R, Pietrzak RH, Luft BJ, Gonzalez A, Richards M, et al. Cognitive impairment among World Trade Center responders: Long-term implications of re-experiencing the 9/11 terrorist attacks. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring. 2016;4(2016):67–75. doi: 10.1016/j.dadm.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. The Cost of Dichotomization. Applied Psychological Measurement. 1983;7(3):249–253. doi: 10.1177/014662168300700301. [DOI] [Google Scholar]
- da Câmara SMA, Alvarado BE, Guralnik JM, Guerra RO, Maciel ÁCC. Using the Short Physical Performance Battery to screen for frailty in young-old adults with distinct socioeconomic conditions. Geriatrics & gerontology international. 2013;13(2):421–428. doi: 10.1111/j.1447-0594.2012.00920.x. [DOI] [PubMed] [Google Scholar]
- Dasaro CR, Holden WL, Berman KD, Crane MA, Kaplan JR, Lucchini RG, et al. Cohort Profile: World Trade Center Health Program General Responder Cohort. Int J Epidemiol. 2015:dyv099. doi: 10.1093/ije/dyv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Souto Barreto P, Cesari M, Rolland Y, Salabert AS, Payoux P, Andrieu S, et al. Cross-Sectional and Prospective Associations Between β-Amyloid in the Brain and Chair Rise Performance in Nondementia Older Adults With Spontaneous Memory Complaints. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2016 doi: 10.1093/gerona/glw195. [DOI] [PubMed] [Google Scholar]
- de Souza Moreira B. The Relationship between Diabetes Mellitus, Geriatric Syndromes, Physical Function, and Gait: A Review of the Literature. Current Diabetes Reviews. :11. doi: 10.2174/1573399811666150615142746. [DOI] [PubMed]
- Ferrucci L, Guralnik JM. Mobility in Human Aging A Multidisciplinary Life Span Conceptual Framework. Annual Review of Gerontology and Geriatrics. 2013;33(1):171–192. doi: 10.1891/0198-8794.33.171. [DOI] [Google Scholar]
- Fragala MS, Dam TTL, Barber V, Judge JO, Studenski SA, Cawthon PM, et al. Strength and Function Response to Clinical Interventions of Older Women Categorized by Weakness and Low Lean Mass Using Classifications From the Foundation for the National Institute of Health Sarcopenia Project. Journals of Gerontology Series a-Biological Sciences and Medical Sciences. 2015;70(2):202–209. doi: 10.1093/gerona/glu110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Spillman BC, Andreski PM, Cornman JC, Crimmins EM, Kramarow E, et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50(2):661–671. doi: 10.1007/s13524-012-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale CR, Allerhand M, Sayer AA, Cooper C, Deary IJ. The dynamic relationship between cognitive function and walking speed: the English Longitudinal Study of Ageing. Age (Dordr) 2014;36(4):9682. doi: 10.1007/s11357-014-9682-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings SW, Beekman AT, Deeg DJ, Twisk JW, Van Tilburg W. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. Psychol Med. 2001;31(8):1361–1371. doi: 10.1017/S0033291701004639. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker D, Waternaux C, Davis JM. Random regression models: a comprehensive approach to the analysis of longitudinal psychiatric data. Psychopharmacol Bull. 1988;24(3):438–443. [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–231. doi: 10.1093/gerona/55.4.M221. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.M85. [DOI] [PubMed] [Google Scholar]
- Hayflick L. Biological aging is no longer an unsolved problem. Ann N Y Acad Sci. 2007;1100(1):1–13. doi: 10.1196/annals.1395.001. [DOI] [PubMed] [Google Scholar]
- Inkster LM, Eng JJ, MacIntyre DL, Stoessl AJ. Leg muscle strength is reduced in Parkinson’s disease and relates to the ability to rise from a chair. Movement Disorders. 2003;18(2):157–162. doi: 10.1002/mds.10299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazeros A, Zhang E, Cheng X, Shao Y, Liu M, Qian M, et al. Systemic Inflammation Associated With World Trade Center Dust Exposures and Airway Abnormalities in the Local Community. J Occup Environ Med. 2015;57(6):610–616. doi: 10.1097/JOM.0000000000000458. [DOI] [PubMed] [Google Scholar]
- Keller-Ross ML, Schlinder-Delap B, Doyel R, Larson G, Hunter SK. Muscle fatigability and control of force in men with posttraumatic stress disorder. Med Sci Sports Exerc. 2014;46(7):1302–1313. doi: 10.1249/MSS.0000000000000244. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Kuh D, Cooper R, Hardy R, Richards M, Ben Shlomo Y, editors. A life course approach to healthy ageing. London: Oxford University Press; 2014. [Google Scholar]
- Kuwert P, Pietrzak RH, Glaesmer H. Trauma and posttraumatic stress disorder in older adults. CMAJ. 2013;185(8):685. doi: 10.1503/cmaj.120866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol (1985) 2003;95(5):1851–1860. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- Li J, Brackbill RM, Stellman SD, Farfel MR, Miller-Archie SA, Friedman S, et al. Gastroesophageal reflux symptoms and comorbid asthma and posttraumatic stress disorder following the 9/11 terrorist attacks on World Trade Center in New York City. Am J Gastroenterol. 2011;106(11):1933–1941. doi: 10.1038/ajg.2011.300. [DOI] [PubMed] [Google Scholar]
- Lohr JB, Palmer BW, Eidt CA, Aailaboyina S, Mausbach BT, Wolkowitz OM, et al. Is Post-Traumatic Stress Disorder Associated with Premature Senescence? A Review of the Literature. Am J Geriatr Psychiatry. 2015;23(7):709–725. doi: 10.1016/j.jagp.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luft BJ, Schechter C, Kotov R, Broihier J, Reissman D, Guerrera K, et al. Exposure, probable PTSD and lower respiratory illness among World Trade Center rescue, recovery and clean-up workers. Psychological Medicine. 2012;42(5):1069–1079. doi: 10.1017/S003329171100256x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychol Methods. 2002;7(1):19–40. doi: 10.1037/1082-989X.7.1.19. [DOI] [PubMed] [Google Scholar]
- Mackenzie IR. The neuropathology of FTD associated With ALS. Alzheimer Dis Assoc Disord. 2007;21(4):S44–49. doi: 10.1097/WAD.0b013e31815c3486. [DOI] [PubMed] [Google Scholar]
- Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962–970. doi: 10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health and Aging Trends Study (NHATS); NIo Aging, editor. NHATS Public Use Data. Johns Hopkins Bloomberg School of Public Health; 2011. [Google Scholar]
- Neria Y, DiGrande L, Adams BG. Posttraumatic Stress Disorder Following the September 11, 2001, Terrorist Attacks A Review of the Literature Among Highly Exposed Populations. American Psychologist. 2011;66(6):429–446. doi: 10.1037/0024791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295(17):2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi SU, Kimbrell T, Pyne JM, Magruder KM, Hudson TJ, Petersen NJ, et al. Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. J Am Geriatr Soc. 2010;58(9):1627–1633. doi: 10.1111/j.1532-5415.2010.02977.x. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata. STATA press; 2008. [Google Scholar]
- Sanderson WC, Scherbov S. Measuring the speed of aging across population subgroups. PLoS One. 2014;9(5):e96289. doi: 10.1371/journal.pone.0096289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalev I, Entringer S, Wadhwa PD, Wolkowitz OM, Puterman E, Lin J, et al. Stress and telomere biology: a lifespan perspective. Psychoneuroendocrinology. 2013;38(9):1835–1842. doi: 10.1016/j.psyneuen.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A, Dugravot A, Kauffmann F, Elbaz A, Ankri J, Nabi H, et al. Association of lung function with physical, mental and cognitive function in early old age. Age (Dordr) 2011;33(3):385–392. doi: 10.1007/s11357-010-9189-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BN, Tyzik AL, Neylan TC, Cohen BE. PTSD and obesity in younger and older veterans: Results from the mind your heart study. Psychiatry Res. 2015;229(3):895–900. doi: 10.1016/j.psychres.2015.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terhakopian A, Sinaii N, Engel CC, Schnurr PP, Hoge CW. Estimating population prevalence of posttraumatic stress disorder: an example using the PTSD checklist. J Trauma Stress. 2008;21(3):290–300. doi: 10.1002/jts.20341. [DOI] [PubMed] [Google Scholar]
- Vancampfort D, Richards J, Stubbs B, Akello G, Gbiri CA, Ward PB, et al. Physical Activity in People With PTSD: A Systematic Review of Correlates. Journal of physical activity & health. 2016 doi: 10.1123/jpah.2015-0436. [DOI] [PubMed] [Google Scholar]
- Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test. Phys Ther. 2005;85(10):1034–1045. [PubMed] [Google Scholar]
- Wisnivesky JP, Teitelbaum SL, Todd AC, Boffetta P, Crane M, Crowley L, et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet. 2011;378(9794):888–897. doi: 10.1016/S0140-6736(11)61180-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, et al. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1997;154(12):1690–1695. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]
- Zutler M, Singer JP, Omachi TA, Eisner M, Iribarren C, Katz P, et al. Relationship of obesity with respiratory symptoms and decreased functional capacity in adults without established COPD. Primary Care Respiratory Journal. 2012;21(2):194–201. doi: 10.4104/pcrj.2012.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.