Abstract
As increasing attention is paid to possible genetic influences on susceptibility to obesity, recent studies have examined how genetic attributions can impact laypeople’s weight-related attitudes and eating behavior. Little consideration, however, has been devoted to understanding the potential effects of learning that one does not have a genetic predisposition to obesity. The present study investigated the possibility that such feedback might bring about negative consequences by making people feel invulnerable to weight gain, which is termed a genetic invincibility effect. After conducting a saliva test disguised as genetic screening, participants were randomly assigned to be told that there was either a very high or very low chance that they carried genes known to increase one’s risk of developing obesity. Participants who were told that they were not genetically predisposed to obesity judged the efficacy of healthy diet and exercise habits to be significantly lower than did those who were told that they were genetically predisposed and those who did not receive any genetic feedback. When prompted to select a meal from a menu of options, participants who were told that they were not genetically predisposed to obesity were also more likely than others to select unhealthy foods. These findings demonstrate the existence of a genetic invincibility effect, suggesting that personalized feedback indicating the absence of a genetic liability could have negative psychological consequences with substantial health-related implications.
1. Introduction
The world is in the midst of a global pandemic of obesity that has intensified in recent decades, affecting men, women, children, and adolescents in both developed and developing countries, causing millions of deaths, and contributing significantly to the global burden of disease, disability, and early mortality (Ng et al., 2014). In light of these alarming developments, there has been a surge of research on psychological factors that determine people’s food intake.
In particular, recent studies have examined how laypeople’s beliefs and attitudes about the causes of obesity may affect food consumption. For instance, laypeople who attribute obesity to a lack of exercise are more likely to actually be overweight than those who attribute obesity to a poor diet, because the former tend to consume more food (McFerran & Mukhopadhyay, 2013). Although laypeople tend to view lack of willpower, the food environment, and lack of exercise as the most likely causes of obesity, the general public is also becoming more and more aware of the role of genes in obesity’s etiology (e.g., Dar-Nimrod, Cheung, Ruby, & Heine, 2014; Singer, Corning, & Lamias, 1998). The current study examines how information about one’s genetic predisposition to obesity affects attitudes and behaviors related to diet and exercise, which can in turn affect actual eating behaviors.
Past studies found that more than 40% of respondents attributed obesity to genetic or hereditary factors (e.g., Beeken & Wardle, 2013; Oliver & Lee, 2005). This number is likely to grow as obesity is increasingly explained in terms of genetics (e.g., Albuquerque, Stice, Rodríguez-Lopez, Manco, & Nóbrega, 2015; Locke et al., 2015; Yang, Kelly, & He, 2007). Personalized genotyping has been proposed as a means of someday identifying individuals at risk for severe obesity, who could then be monitored using biotechnology in an effort to reduce the incidence of negative health outcomes associated with obesity (Walley, Blakemore, & Froguel, 2006). Genetic tests that purportedly provide personalized information about a person’s genetic susceptibility to obesity are already becoming available (Meisel, Walker, & Wardle, 2012; Segal, 2017). One company even claims that its genetic test “provides physicians with a genetically-matched diet allowing them to make specific recommendations to their patients to help them achieve or maintain a healthy weight” (Pathway Genomics, n.d.).
Recent studies have investigated the effect of construing obesity in terms of genetic etiology. While genetic accounts of obesity can reduce the extent to which people with obesity are blamed for their weight status (Pearl & Lebowitz, 2014), genetic explanations can also have negative consequences. Laypeople tend to hold inaccurate beliefs about genetics, endorsing genetic essentialism, which refers to the belief that genes represent the immutable essences of a person’s traits (Dar-Nimrod & Heine, 2011; Ehrlinger, Burnette, Park, Harrold, & Orvidas, 2017). Thus, the increasing emphasis on understanding the genetic bases of health and illness, including obesity, could increase fatalism about health outcomes (Dar-Nimrod & Heine, 2011). Indeed, the more overweight Americans attribute their weight status to biological causes such as genes, the more unchangeable they believe their body weight is (Pearl & Lebowitz, 2014). Genetic explanations have also been shown to decrease self-efficacy and intentions to exercise (Beauchamp, Rhodes, Kreutzer, & Rupert, 2011). Relatedly, Hoyt, Burnette, and Auster-Gussman (2014) found that when people with obesity learned about the American Medical Association’s 2013 decision to formally recognize obesity as a disease, they became less concerned about their weight (compared to people who read different information about obesity), which led to them making less healthy food choices. Other research has shown that merely being exposed to genetic explanations for obesity can increase consumption of unhealthy food (Dar-Nimrod et al., 2014). Indeed, the proportion of Americans with overweight and obesity who are trying to lose weight has declined significantly over recent decades (Snook et al., 2017), and increasing genetic attributions could be one possible reason for this trend.
Previous studies of the effects of genetic information on obesity, however, have not specifically examined how learning that one is not genetically predisposed to obesity would affect people’s attitudes towards eating and exercise or their choice of foods. Learning that one is not genetically susceptible to an illness or unhealthy condition is good news, which may explain why existing research has generally not focused on possible negative effects of such feedback. However, if people see DNA as the essence of a condition, they may view it not only as sufficient to cause the trait on its own—making them pessimistic about their control over the condition in question—but also as necessary to bring it about. Consequently, people may also hold the misconception that if they do not carry a particular genetic predisposition to obesity, they are likely to be immune to the negative effects of obesogenic dietary habits or inactivity—a misconception that we refer to as a genetic invincibility effect.
Similar phenomena, known as licensing effects or risk compensation, have been documented in other domains. For instance, people who took pills described to them as multi-vitamins—which in fact were placebo pills—showed greater desire to engage in unhealthy behaviors, such as casual sex, excessive drinking, and smoking (Chiou, Yang, & Wan, 2011). Drivers of vehicles with anti-lock brakes actually drive faster (Sagberg, Fosser, & Sætermo, 1997), and increased helmet use is positively associated with increased bicycle-related fatalities (Rodgers, 1988).
Only a few recent studies have examined the impact of learning that one does not possess a particular genetic liability, and no single clear pattern of effects has emerged. Among individuals who learned that they carried a CDKN2A/p16 mutation (which increases susceptibility to melanoma), adherence to total body skin examinations (TBSE) increased, whereas among non-carriers, it dropped (Aspinwall, Taber, Leaf, Kohlmann, & Leachman, 2013). However, these participants were from families with a history of melanoma, and the decrease among non-carriers may have reflected a reversion to general-population norms (Lakhani, Saraiya, Thompson, King, & Guy, 2014) rather than a true genetic invincibility effect. Furthermore, non-carriers’ appraisals of the effectiveness of photoprotection remained as high as carriers’ after both groups learned of their carrier status (Aspinwall et al., 2015), potentially suggesting the absence of genetic invincibility effects.
The aforementioned studies, while groundbreaking in their focus on elucidating the effect of learning that one is a non-carrier, are limited in several ways. First, no studies to our knowledge have systematically examined whether learning that one does not have genetic predisposition to obesity would cause them to feel more invincible (i.e., to assume that they will not become obese regardless of their diet or exercise habits). Second, the findings from the aforementioned studies may be difficult to generalize to a larger population because these studies focused on individuals from families with known histories of a disorder. For instance, non-carriers who are aware of such a family history may be less likely than members of the general population to show genetic invincibility effects, as individuals who know that a certain condition runs in their families may be resistant to the assumption that they are invulnerable to it (Aspinwall, Taber, Kohlmann, Leaf, & Leachman, 2014).
The current study offers the first experimental investigation of the genetic invincibility effect in the general population, using obesity as the target condition. We examine whether telling people that they are not genetically predisposed to obesity would cause them to discount the importance of healthy diet and exercise habits, and to select more unhealthy foods. In this study, participants carried out a saliva test disguised as revealing their genetic susceptibility to obesity, and we randomly determined which participants were told that they were not genetically predisposed to obesity. If genetic invincibility effects were to occur, participants told that they lacked a genetic predisposition to obesity would be expected to discount the significance and efficacy of diet and exercise relative to individuals who had not been told anything about their genetic predisposition to obesity.
In addition, the present study also included a randomly selected group of participants who were told that they were genetically predisposed to obesity. These participants might also be expected to discount the significance and efficacy of diet and exercise, if genetic essentialism plays a role, as they might expect the effects of their genes to be deterministic. Alternatively, these participants could have interpreted the genetic feedback non-deterministically because it is well known that diet and exercise affect body weight (e.g., McFerran & Mukhopadhyay, 2013), and these participants might appreciate the benefits of diet and exercise even more, as a means of overcoming their supposed genetic predisposition (Aspinwall et al., 2015).
2. Methods
2.1. Rationale for experimental methods and protection of human subjects
The current study experimentally manipulates the type of genetic feedback participants received through a saliva test disguised as a test for genetic predisposition to obesity. This experimental method has several advantages over correlational studies because it allows for participants to receive different feedback after the saliva test depending upon the condition to which they were randomly assigned.
First, had we examined those who had valid knowledge of their genetic status in relation to obesity, it would have been impossible to discern whether their exercise- and diet-related attitudes and behaviors might have been due to actual genetic differences rather than the genetic feedback itself. For instance, those who are genetically susceptible to obesity may have experienced exercise or healthy diet to be ineffective in controlling their weight, so if they were to discount the significance and efficacy of exercise and healthy diet, it would be difficult to determine whether this resulted from their knowledge about their genetic predispositions or from their actual genetic makeup.
Second, the effects of genetic feedback related to obesity may interact with other factors, such as childhood history, family weight history, personality traits, intelligence, dietary restrictions, education, income, mental health, physical fitness, etc. In the present research, such factors were unlikely to be confounding factors in explaining differences among conditions because a large sample of participants was assigned to conditions at random, making any systematic differences among conditions improbable.
In short, by eliminating not only actual genetic differences but also other background factors as alternative explanations of our findings, the experimental manipulation and random assignment of participants allow us to draw causal conclusions about the relationship between our independent and dependent variables. Given these advantages, the deception involved in the current methods was necessary.
Because the procedures of the current experiment involve deception, this section also details the methods used to protect human subjects from being harmed as a result. The work described has been carried out in accordance with the Code of Ethics of the World Medical Association. The procedures were developed through careful assessment of risks and burdens to the participants, and were approved by the Institutional Review Board. Previous studies (Lebowitz & Ahn, in press a, in press b) using methods similar to the current approach yielded no reports of adverse effects from participants, with near-perfect completion rates (greater than 95%).
The informed consent form for the present study noted that participants “may experience discomfort or distress in answering questions or receiving information as part of the study.” It explained their rights to withdraw from the study without losing their compensation and noted that “Exit Study” links would be present throughout the study as they proceeded through onscreen procedures. In bold font, it was explained, “If you choose to discontinue the study without completing all of the procedures, it is important that you click this “Exit Study” link instead of simply closing the browser window” because clicking the Exit Study link would present the debriefing information (which explained the deceptive nature of the saliva test; see Supplemental Materials) and instructions for compensation. It was not possible to state in the informed consent form that the study procedures would involve genetic testing because an informed consent form cannot state false information. However, the Exit Study link was provided on every page of the study, including the instruction page that introduced the saliva test procedure, which was described as genetic testing, and thus, participants could withdraw at that point without losing any compensation. (See Supplemental Materials for details of the debriefing procedure.)
2.2. Participants
Participants were U.S. adults recruited through Amazon.com’s Mechanical Turk (mTurk) platform in exchange for compensation. To recruit participants, we first posted on mTurk an opportunity for U.S. adults to submit their mailing addresses for a study in which they were told they would receive experimental materials by mail. Participants were told that they would receive $1 for submitting their addresses and additional $10 for completing the main study. We sent the experimental materials (described below) to 517 mailing addresses obtained in this manner. Of these, two participants selected the EXIT link described earlier, and 414 completed the main part of the study. Eight of these participants’ data were excluded for not following the instructions or due to equipment failure (see below for details). At the end of the study, we measured participants’ perceptions of the credibility of the saliva test as genetic testing (explained below) that they underwent as part of the experiment. For this credibility measure, participants rated their agreement with the following statement: “The test I underwent as part of today’s study gave accurate and reliable information about my genetic makeup.” Response options were “Strongly Disagree,” “Disagree,” “Neither Agree nor Disagree,” “Agree,” and “Strongly Agree.” Out of 406 participants, a majority (N = 226; 55.67%) selected “Agree” or “Strongly Agree.” Credibility ratings did not differ by condition, F(2, 403) 1.69, p = 0.19. Because participants knew that they were taking part in a psychology experiment, and these participants may have participated in many psychology experiments in the past given their use of mTurk, it is not surprising that some participants were suspicious of the test result’s credibility. In total, 122 participants (30.00%) selected “Neither Agree nor Disagree,” while 58 participants (14.29%) selected “Disagree” or “Strongly Disagree.” We report results only from the 226 participants who selected “Agree” or “Strongly Agree,” indicating that they considered the test results to be credible. See Table 1 for demographic information.
Table 1.
Demographic characteristics of participants included in analyses (N = 226).
| Sex | Female: 60.2% Male: 39.4% No sex indicated: 0.4% |
| Ethinicity | Hispanic or Latino: 5.8% Not Hispanic or Latino: 93.4% No ethnicity indicated: 0.9% |
| Race (it was possible to select multiple responses) | American Indian or Alaska Native: 2.2% Asian: 8.4% Black if African-American: 5.3% Native Hawaiian or Pacific Islander: 0.4% More than one race: 2.2% White: 86.3% |
| Age (Median = 32 years) | 18–29 years: 37% 30–39 years: 39% 40–49 years: 12% 50–59 years: 8% 60–68 years: 4% |
| Self-reported weight status | Underweight: 1.8% Normal weight: 45.6% Overweight: 38.9% Obese: 13.7% |
2.3. Materials, design, and procedure
The experimental materials mailed to potential participants were enclosed in a plastic container disguised as a saliva testing kit, which contained mouthwash—into which a small amount of glucose had been dissolved—and a glucose test strip (a white strip with a small blue square on one end, which would change to brownish-green upon contact with the glucose-containing mouthwash). The plastic container was labeled “Saliva self-testing kit for 5-Hydroxyindoleacetic acid.” The kit was mailed to the participants along with printed instructions, which guided participants to the URL to access the study procedures, which was programmed using Qualtrics (Qualtrics Lab, 2005), and they were told not to open the kit until they were instructed to do so.
After providing informed consent, participants were randomly assigned to one of three conditions: genes-present, genes-absent, or genes-absent/pretest-posttest (see Fig. 1 for a summary of the procedures for each of the three conditions). We first explain the procedure for the genes-present and genes-absent conditions, in which participants began with the saliva test and received the genetic feedback and then completed dependent measures. We then describe the procedure for the genes-absent/pretest-posttest condition, which began with the dependent measures, followed by the saliva test, genetic feedback, and a repeated measure of the dependent variables.
Fig. 1.
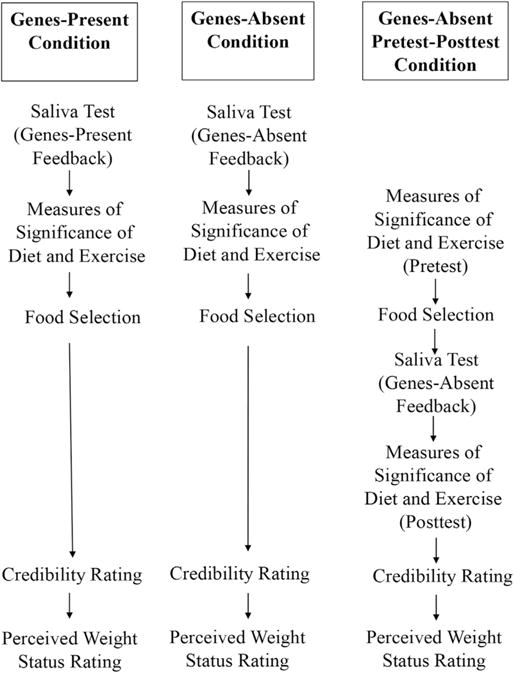
Summary of procedures for the genes-present, genes-absent, and genes-absent/pretest-posttest conditions.
Participants in the genes-present and genes-absent conditions first carried out the saliva test. They were told that they would undergo a test to determine whether they carried genes that play a role in causing obesity. Participants were not told that the mouthwash contained glucose or that the test strip in the kit was sensitive to glucose. Instead, they were told that the testing kit would reveal their salivary levels of the chemical 5-Hydroxyindoleacetic acid. In reality, this chemical is a metabolite of the neurotransmitter serotonin, but participants were not told this and were instead told that its concentration in saliva can indicate a person’s genetic susceptibility to obesity. Following onscreen instructions, participants rinsed their mouths with mouthwash provided in their testing kit, inserted the test strip into their mouths, and then selected the color to which the blue square on the test strip had changed. Although the color should have changed to brownish-green for all participants, participants were asked choose from three options (“Brown or Green,” “Red or Pink,” and “White”) in order to suggest that there were other possible outcomes to the saliva test. We excluded data from 8 participants who did not choose “Brown or Green,” as their responses suggested inattention to or failure to follow the instructions, or equipment malfunction.
Next, participants were given feedback which was disguised as the results of their saliva test, depending on the condition to which they had been randomly assigned. Those in the genes-present condition were told that the results of the saliva test indicated that “there is a very high chance that you carry genes that are known to increase a person’s risk of developing obesity.” Those in the genes-absent condition were told that there was a very low chance that this was the case. Then, all participants were provided with the following information about the genetics of obesity, adapted from Wikipedia (“Genetics of Obesity,” n.d.):
Certain forms of various genes controlling appetite and metabolism can predispose people to obesity if they eat certain kinds of diets. The percentage of obesity that can be attributed to genetics varies widely, depending on the population examined, from 6% to 85%. As of 2006, more than 41 parts of the human genome have been linked to the development of obesity under certain conditions. The involvement of genetic factors in the development of obesity is estimated to be 40–70%. Some of these genes involved in obesity may influence obese individuals’ response to weight loss or weight management.
After the saliva test and the feedback, participants in the genes-absent and genes-present conditions answered six questions developed to measure the effect of genetic feedback. These questions are shown in Table 2.
Table 2.
Items measuring perceived significance of diet and exercise.
| Item number | Questions |
|---|---|
| 1 | Imagine that in the future, you adopt a diet that is unhealthier than your current diet. How much would this increase your own personal chances of becoming obese (or remaining obese)? |
| 2 | Imagine that in the future, you become physically less active than you currently are. How much would this increase your own personal chances of becoming obese (or remaining obese)? |
| 3 | On the following scale, please rate how important you believe healthy diet is. |
| 4 | On the following scale, please rate how important you believe regular exercise is. |
| 5 | To what extent would the kind and the amount of foods you eat influence your body weight? |
| 6 | To what extent would the amount of physical exercise you get influence your body weight? |
All 6 items were answered on a 7-point scale. For items 1, 2, 5 and 6, the scale points were labeled with “not at all” for 1 and “very much” for 7; for items 3 and 4 they were labeled with “not important” for 1 and “extremely important” for 7.
Then, the participants in the genes-absent and genes-present conditions received the second dependent measure, which involved simulated food selection (e.g., Lee & Thompson, 2016). To develop this measure, we first generated three lunch items that would be considered to be healthy (chicken Caesar salad wrap, salad with grilled chicken, and roasted turkey and avocado sandwich) and three items that would be considered to be unhealthy (cheeseburger, meatloaf with mashed potato, and baked ziti with three cheeses). In selecting these items, we avoided calorie labels and terms that would make calorie content or nutritional value salient (e.g., non-fat, light), to reduce demand characteristics. A pretest from a separate group of 101 participants recruited via mTurk rated on a 7-point scale (1 = extremely unhealthy, 7 = extremely healthy) that the three options selected to be healthy were significantly healthier (M = 5.52) than the three selected to be unhealthy (M = 2.55), t(100) = 26.17, p < 0.001. All three healthy options received significantly higher mean ratings than the scale mid-point of 4 (all ps < 0.001), while all three unhealthy options received average ratings significantly lower than 4 (all ps < 0.001). In the main experiment, participants were presented with all six food options at once (as opposed to pairwise selections as used, e.g., by Masic, Christiansen, & Boyland, 2017) to simulate a food choice from a menu. Participants were told to pretend they were pre-ordering their lunch for a daylong meeting and were asked to select one of these six meal options.
After completing all dependent measures, all participants received the question about the credibility of the saliva test (as explained in the Participants section above). Then, they were asked which option best described their current weight status: underweight, normal weight, overweight, and obese. After answering optional demographic questions, participants were extensively debriefed as detailed in Supplemental Materials.
In addition to the genes-present and the genes-absent conditions, there was a third condition, the genes-absent/pretest-posttest condition, which was included to measure the effect of genetic feedback within the same participants. These participants started out with the six questions measuring their perceptions of the significance of diet and exercise, followed by the task of selecting a lunch option, before completing the saliva test. These baseline measures were taken before genetic testing for obesity was ever mentioned, because Dar-Nimrod et al. (2014) showed that merely reading about obesity genes could affect eating behavior. After the baseline measures, these participants were also presented with filler questions measuring their attitudes and feelings towards obese people in order to increase the interval between the pretest and the posttest. These were not the focus of the current study, and responses are not reported here. Then, participants in this condition performed the saliva test as described earlier, and received the same interpretation of their results as participants in the genes-absent condition. Then they were re-presented with the six questions measuring their perception of the significance of diet and exercise. By utilizing within-subject pretest-posttest comparisons, we could eliminate all potential confounding variables involving individual differences, because any unmeasured background factors were the same at pretest and posttest. After all dependent measures were taken, participants in this condition answered other questions described earlier (i.e., credibility of the saliva test, weight status, and demographic information) before receiving the debriefing.
2.3.1. Statistical analyses
Because one’s weight status might be expected to interact with the genetic invincibility effect in obesity, we created a weight status variable in which we coded participants who selected underweight or normal weight with a 0 and those who selected overweight or obese with a 1. Including this weight-status variable in our analyses allowed us to examine whether or not any observed genetic invincibility effects were independent of participants’ weight status. Controlling for weight status in this way also addressed the possible concern that limiting our sample to participants who rated the saliva test as credible could have introduced a confound (e.g., if credibility ratings were confounded with weight status such that participants who described themselves as overweight or obese were more likely to find the genes-present feedback credible). We used this variable in the subsequent analyses as explained below.
For the six ratings gauging participants’ perceptions of the significance of diet and exercise, we first computed the reliability of the items. Across conditions, responses to these six questions were highly consistent with one another, yielding a Cronbach alpha of 0.78. Thus, for our analyses these six ratings were averaged to compute a diet/exercise significance score for each participant. These average scores were used as the dependent variable for an ANOVA testing the effect of our between-subject experimental manipulations (i.e., by comparing the means of genes-absent condition, the genes-present condition, and pre-test from the genes-absent/pretest-posttest condition), with the weight status variable as an additional independent variable. We planned to follow up this ANOVA with pairwise comparisons using Tukey’s honestly significant difference (HSD) tests, if the omnibus effect of condition was significant. To examine whether the diet/exercise significance scores of participants in the genes-absent/pretest-posttest condition changed from pretest to posttest, we used a paired-samples t-test. In the Supplemental Materials, we also report both sets of analyses with each of the six individual items examined separately.
To examine the food selection choices across the three conditions, we used a binary logistic regression analysis. This allowed us to examine, as in the ANOVA reported above, both the main effects of condition and weight status as well as their interaction. In this analysis, participants’ lunch choices were coded as 1 if they selected one of the three unhealthy meal options and 0 if they selected one of the three healthy meal options. We also created a dummy code for the genes-absent feedback (for which participants in the genes-absent condition received a 1 and all others received a 0) and a dummy code for the genes-present feedback (for which participants in the genes-present condition received a 1 and all others received a 0). (Participants in the genes-absent/pretest-posttest condition were asked to select a lunch option before the saliva test, so they had received neither type of genetic feedback when they selected a lunch option and thus received a 0 for both dummy codes.) In the binary logistic regression, choice of an unhealthy (vs. healthy) lunch option was the dependent variable, and the model included the following five independent variables: the two dummy codes for genetic feedback, the aforementioned dummy code for self-reported weight-status, and two product terms representing the interactions of self-reported weight status with each type of genetic feedback.
In reporting our results, we present data in the format M ± SD.
3. Results
3.1. Significance of diet and exercise
First, we compared the diet/exercise significance scores from the genes-absent condition (N = 73), the genes-present condition (N = 70), and the pretest (baseline) from the genes-absent/pretest-posttest condition (N = 83). There was a significant main effect of condition, F(2,220) = 14.95, p < 0.001 (see Fig. 2 for a summary of results and below for more details). There was also a significant main effect of weight status, F(1,220) = 5.26, p = 0.023, because those who self-reported being overweight or obese gave higher diet/exercise significance scores (M = 6.08 ± 0.75) than those who self-reported as being normal or underweight (M = 5.82 ± 91). Importantly, the main effect of condition did not depend on self-reported weight status, as there was no significant interaction effect, F(2, 220) = 1.38, p = 0.253.
Fig. 2.
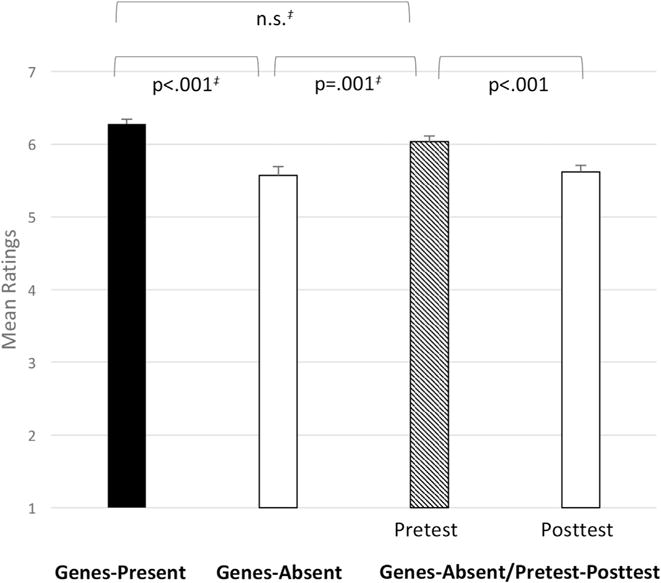
Mean ratings of the significance of diet and exercise broken down by the three conditions and by the pretest and posttest ratings in the genes-absent/pretest-posttest condition. Error bars indicate 1 standard error. P-values marked ‡ are results from Tukey HSD tests. White bars indicate ratings made by participants who had been told that they lacked a genetic predisposition to obesity.
Pairwise comparisons revealed that diet/exercise significance scores from participants in the genes-absent condition (M = 5.57 ± 1.04) were significantly lower than those from participants in the genes-present condition (M = 6.28 ± 0.57, p < 0.001) and those from the pretest of the genes-absent/pretest-posttest condition (M = 6.03 ± 0.77, p = 0.001). The difference in diet/exercise significance scores from participants in the genes-present condition and those from the pretest of the genes-absent/pretest-posttest condition was not significant in this analysis (p = 0.11).
Second, we examined the within-subjects effect of receiving the genes-absent feedback, by comparing the pretest and protest scores of participants in the genes-absent/pretest-posttest condition. Their diet/exercise significance scores were significantly lowered after they received the genes-absent feedback (M = 5.62 ± 0.81), t(82) = 6.10, p < 0.001.
In the Supplemental Materials, we report the results obtained when analyzing each of the six items separately. To summarize, there was no systematic difference between items concerning diet and items concerning exercise. Although the reliability analysis reported above suggests that the six items were generally consistent with one another, in the Supplemental Materials we report that items 3 and 4 consistently failed to show the genetic invincibility effect when analyzed in isolation. We offer a potential explanation for this in the Discussion section below and in the Supplemental Materials.
3.2. Lunch choices
The pretest baseline measure from the genes-absent/pretest-posttest condition showed that only 10.8% selected an unhealthy lunch option. Similarly, only 15.7% in the genes-present condition did so. In the genes-absent condition, however, 28.8% of participants selected an unhealthy lunch option. The only independent variable that emerged as significant in the binary logistic regression was the one representing the genes-absent feedback, B = 1.61, p = 0.012. This indicates that the genes-absent feedback significantly increased participants’ likelihood of selecting an unhealthy lunch option and that this effect was independent of, and not moderated by, self-reported weight status.
4. Discussion
The current study demonstrated the existence of a genetic invincibility effect in relation to obesity. After being told that they were not genetically predisposed to obesity, participants judged adherence to a healthy diet and physical exercise to be less effective as ways of controlling their weight. This finding was obtained within-subjects, comparing the same participants’ responses before and after receiving the genetic feedback, and also between-subjects, comparing responses of participants who were told they lacked a genetic predisposition to the baseline ratings of others who had not yet received any genetic feedback. In addition, compared to participants who had not yet received any genetic feedback, those who had been told they were not genetically susceptible to obesity were significantly more likely to select unhealthy food options. These findings are consistent with licensing effects demonstrated in other domains (e.g., Chiou et al., 2011). That is, participants who believed they lacked a genetic predisposition toward obesity felt more licensed to discount the efficacy of healthy diet and exercise habits and to eat unhealthy food.
These findings have important public health implications, as genetic invincibility effects that lead people to discount the importance of non-genetic factors like diet and exercise could actually harm people’s health by leading them to neglect health-promoting behaviors. Indeed, our results suggest that learning they are not genetically predisposed to obesity could ironically encourage people to adopt eating behaviors or a lifestyle that could place them at greater risk of obesity than they would face if they had never received the genetic information. In light of obesity’s significant contribution to the global burden of poor health, as discussed in the introduction, such a consequence could cause serious harm. Genetic testing is highly likely to become an increasingly prevalent component of healthcare in the future, and a majority of people who received personalized information about their genetic susceptibility to obesity will likely learn that they lack any particular genetic predisposition to it. Thus, it is crucial to understand that such feedback can have unintended negative consequences for beliefs and behavior related to exercise and food intake.
The current results also suggest a need for future research examining how to mitigate negative consequences even when informing people that they lack a genetic predisposition to a particular health problem. Studies to date have only investigated approaches to minimizing the potential harms that may emerge when people believe they do possess genetic a predisposition to a particular disorder (Lebowitz, Ahn, & Nolen-Hoeksema, 2013; Lebowitz & Ahn, 2015). One possible strategy to counteract genetic invincibility effects like the one observed here might be to alert people about the risk of these effects and remind them that there are other non-genetic causes of obesity (or other conditions). Whether such reminders can effectively counteract genetic invincibility effects is an empirical question.
The current study also examined the effects of learning that one is genetically susceptible to obesity. If people believe that genes determine their fate (i.e., endorse genetic essentialism), they would be expected to rate exercise and adherence to a healthy diet as significantly less effective. Dar-Nimrod et al. (2014), for instance, found that genetic attributions for obesity were negatively associated with the perception of weight as controllable (see also Pearl & Lebowitz, 2014). In contrast, Harvey-Berino, Gold, West, and Shuldiner (2001) found that giving people truthful feedback about their genetic risk for obesity increased feelings of control over weight loss. In the current study, we found that mean diet/exercise significance ratings in the genes-present condition did not differ significantly from the baseline measure. The variability of these results may reflect the existence of a variety of possible responses to genes-present feedback, which could have canceled each other out in the current study. For instance, even if some participants interpreted the genes-present feedback fatalistically, others might have responded defensively by weighting the importance of diet and exercise more heavily in order to diminish the importance of their genetic susceptibility (Dar-Nimrod et al., 2014). In the present study, we may have facilitated this type of defensive response by noting that the susceptibility genes have their effects only “under certain conditions.”
Another result from the present study that appears to diverge from previous findings is that the genes-present feedback did not make participants significantly more likely to select unhealthy lunch items, whereas Dar-Nimrod et al. (2014) found that merely being primed with information about the genetic basis of obesity caused participants eat more cookies. As discussed above, this could have occurred because (at least some) participants in the genes-present condition responded defensively to their supposed genetic predisposition by more heavily weighting the importance of diet and exercise. In addition, many of the participants who Dar-Nimrod et al. (2014) primed with information about the genetic basis of obesity could have simply assumed that they personally were not genetically predisposed to obesity. Thus, they may actually have eaten more cookies after exposure to the genetic prime as a result of assuming that obesity is caused by genes that they did not possess (perhaps like participants in our genes-absent condition).
There are several potential limitations of the study. While the inclusion of a within-subject design and random assignment of participants to conditions largely eliminated confounding variables as threats to the validity of our experiment, there is of course no guarantee that unmeasured background factors did not interact with any of the results reported here. With even larger samples, future research could measure a wider range of individual difference variables and statistically examine whether they interact with genetic invincibility effects. For instance, in the Supplementary Materials we report preliminary results suggesting that the genetic invincibility effect was less pronounced among overweight and obese participants for at least one of the items, and further research could elucidate even subtler ways in which weight status might moderate the effects of genetic feedback.
The current study utilized self-reported weight status rather than actual weight status, and we discuss two potential limitations arising from this. First, participants’ self-reported weight statuses could have been affected by the genetic feedback. For instance, the genes-absent feedback might have caused participants to report their weight as lower than they would have if they had received the genes-present feedback. It should be noted that this issue is irrelevant to the genetic invincibility effect because the effect was demonstrated by comparing the genes-absent condition and the genes-absent/pretest-posttest condition’s pretest measure, so all participants in this analysis had received genes-absent feedback by the time they self-reported their weight status. Still, we cannot rule out the possibility that weight status might have moderated the differences that emerged between the genes-present condition and the genes-absent conditions if we had objectively measured participants’ actual weight statuses. Second, self-reported weight status may not be accurate in general. Self-reported weight status, however, have been shown to be more psychologically important than objectively measured body mass index (e.g., with self-perceived weight status predicting the extent of experiencing threat from obesity stigma even after controlling for actual weight; Major, Hunger, Bunyan, & Miller, 2014). Nonetheless, it is an open question whether actual weight status interacts with the genetic invincibility effect. For example, people who are lean may be more susceptible to genetic invincibility effects related to the health effects of poor diet and exercise habits, especially if they have past experience of adhering to unhealthy diet and exercise regimens without gaining weight as a result. This, in turn, could have important negative health implications, as poor metabolic and cardiovascular fitness can lead to disease and mortality even among lean individuals (Lavie, De Schutter, & Milani, 2015).
Additionally, there might have been limitations involving the food-selection task. First, a minority of participants chose unhealthy food items overall, potentially because of demand characteristics motivating them to select healthy food items. Effectively preventing demand characteristics (e.g., by disguising the study as consumer market research, Roberto, Larsen, Agnew, Baik, & Brownell, 2010) was not feasible in the present study given that the task immediately followed the saliva test described as measuring genetic susceptibility to obesity. It is reasonable to assume, however, that the demand to select healthy food is also present in real life to some extent, and the genetic invincibility effect might have occurred partly because the genes-absent feedback reduced social desirability or pressure to select healthy food. Thus, reduced demand characteristics or social desirability could have been one of the mechanisms underlying the genetic invincibility effect rather than being a confound.
Other possible limitations involving the food-selection task include use of simulated food choices rather than actual food choices and eating behaviors, and use of verbal labels for food options rather than pictures or actual foods. There may be an elevated risk of social desirability effects when merely asking participants to choose a food from a hypothetical menu, as there is no cost to merely selecting the most socially desirable (i.e., healthiest) option because the participants will never have to actually consume the food. By contrast, social desirability effects might be less likely to be observed when presenting participants with an actual opportunity to consume unhealthy food (e.g., Ehrlinger et al., 2017; Schvey, Puhl, & Brownell, 2011), as any social desirability effects would have to be strong enough to overcome the temptation to consume unhealthy foods that are likely more palatable than healthier options. Notably, in the present study, we found that the genes-absent feedback made participants more likely to select unhealthy foods in spite of any social desirability effects, and it is unclear whether our findings might have been different if we had measured actual food consumption. As mentioned above, messages about a lack of genetic susceptibility might cause people to feel less pressure to choose healthy foods, and thus potentially less of a need to self-regulate when faced with an opportunity to consume unhealthy foods. If this is the case, they might be less resistant to the temptation to do so (which would likely be particularly strong if the food options were actually present), facilitating in the genetic invincibility effect.
We note that in the Results section above, we report the results obtained when we averaged together the six diet/exercise significance items to compute a single score for each participant. However, as detailed in the Supplemental Materials, when we separately analyzed items 3 and 4 (in which participants rated how important they believe healthy diet or regular exercise to be), a significant genetic invincibility effect did not emerge. These items might have been ambiguous in that they merely asked about the extent to which healthy diet and exercise were seen as important but did not specify in what ways (i.e., obesity was not mentioned in the questions). For instance, healthy diet and exercise can be important for social life or mental health, and thus the effect of our experimental manipulations, which were hypothesized to affect beliefs involving obesity, might have been diluted.
Finally, future research should examine whether genetic invincibility effects would extend to other health conditions besides obesity. For example, Dar-Nimrod, Zuckerman, and Duberstein (2013) found that participants who were told they did not have a genetic predisposition to alcoholism, compared to participants who were told that they did, rated themselves as having more control over their drinking but as less likely to enroll in a responsible drinking workshop. The fact that these findings resulted from comparing participants who were given genes-absent feedback to participants who were given genes-present feedback, rather than comparing each of these groups to participants who were given no genetic feedback, creates something of a challenge in interpretation. For example, the lower level of willingness to enroll in the responsible drinking workshop among participants who were led to believe they lacked the genetic predisposition could suggest the presence of a genetic invincibility effect. Yet, it could also reflect defensive increased weighting of the importance of non-genetic factors (e.g., the workshop) among participants who were led to believe they did have the genetic predisposition. Indeed, both processes could be at play, as discussed above. The present results suggest that learning that one has a health-related genetic predisposition and learning that one does not have such a genetic predisposition can both have potentially meaningful effects. Thus, future studies examining the effects of health-related genetic feedback should include a baseline condition in which no genetic feedback is provided, to allow for analysis of the unique effects of specific kinds of genetic feedback.
In conclusion, laypeople’s food intake and physical activity can be shaped by causal theories they have about obesity. Obesity is increasingly explained in terms of genetics, and given the growing prevalence of personalized genetic testing, the current study examined the effects of learning whether or not one is genetically predisposed to obesity. The present research raises the possibility that personalized feedback indicating the absence of such a genetic predisposition could ironically have negative psychological consequences by making people feel invulnerable to weight gain and less vigilant about maintaining healthy diet and exercise regimens.
Supplementary Material
Acknowledgments
This work was supported by NIH grants R01-HG007653 and P50-HG007257. We thank Sunnie Kim, Lily Sands, and Beth West-gate for assistance preparing study materials.
Footnotes
Conflicts of interest
None.
References
- Albuquerque D, Stice E, Rodríguez-López R, Manco L, Nóbrega C. Current review of genetics of human obesity: From molecular mechanisms to an evolutionary perspective. Molecular Genetics and Genomics. 2015;290(4):1191–1221. doi: 10.1007/s00438-015-1015-9. [DOI] [PubMed] [Google Scholar]
- Aspinwall LG, Stump TK, Taber JM, Kohlmann W, Leaf SL, Leachman SA. Impact of melanoma genetic test reporting on perceived control over melanoma prevention. Journal of Behavioral Medicine. 2015;38:754–765. doi: 10.1007/s10865-015-9631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspinwall LG, Taber JM, Kohlmann W, Leaf SL, Leachman SA. Perceived risk following melanoma genetic testing: A 2-year prospective study distinguishing subjective estimates from recall. Journal of Genetic Counseling. 2014;23(3):421–437. doi: 10.1007/s10897-013-9676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspinwall LG, Taber JM, Leaf SL, Kohlmann W, Leachman SA. Melanoma genetic counseling and test reporting improve screening adherence among unaffected carriers 2 years later. Cancer Epidemiology and Prevention Biomarkers. 2013;22(10):1687–1697. doi: 10.1158/1055-9965.EPI-13-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchamp MR, Rhodes RE, Kreutzer C, Rupert JL. Experiential versus genetic accounts of inactivity: Implications for inactive individuals’ self-efficacy beliefs and intentions to exercise. Behavioral Medicine. 2011;37(1):8–14. doi: 10.1080/08964289.2010.540263. [DOI] [PubMed] [Google Scholar]
- Beeken RJ, Wardle J. Public beliefs about the causes of obesity and attitudes towards policy initiatives in Great Britain. Public Health Nutrition. 2013;16(12):2132–2137. doi: 10.1017/S1368980013001821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiou WB, Yang CC, Wan CS. Ironic effects of dietary supplementation illusory invulnerability created by taking dietary supplements licenses health-risk behaviors. Psychological Science. 2011;22(8):1081–1086. doi: 10.1177/0956797611416253. [DOI] [PubMed] [Google Scholar]
- Dar-Nimrod I, Cheung BY, Ruby MB, Heine SJ. Can merely learning about obesity genes affect eating behavior? Appetite. 2014;81:269–276. doi: 10.1016/j.appet.2014.06.109. [DOI] [PubMed] [Google Scholar]
- Dar-Nimrod I, Heine SJ. Genetic essentialism: On the deceptive determinism of DNA. Psychological Bulletin. 2011;137(5):800. doi: 10.1037/a0021860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dar-Nimrod I, Zuckerman M, Duberstein PR. The effects of learning about one’s own genetic susceptibility to alcoholism: A randomized experiment (vol. 15, pg 132, 2012) Genetics in Medicine. 2013;15(5):412. doi: 10.1038/gim.2012.111. 412. [DOI] [PubMed] [Google Scholar]
- Ehrlinger J, Burnette JL, Park J, Harrold ML, Orvidas K. Incremental theories of weight and healthy eating behavior. Journal of Applied Social Psychology. 2017;47(6):320–330. [Google Scholar]
- Genetics of Obesity (n.d.) Wikipedia. Retrieved June 15, 2016 from https://en.wikipedia.org/wiki/Genetics_of_obesity.
- Harvey-Berino J, Gold EC, West DS, Shuldiner AR. Does genetic testing for obesity influence confidence in the ability to lose weight? A pilot investigation. Journal of the Academy of Nutrition and Dietetics. 2001;101(11):1351. doi: 10.1016/S0002-8223(01)00323-6. [DOI] [PubMed] [Google Scholar]
- Hoyt CL, Burnette JL, Auster-Gussman L. “Obesity is a disease” examining the self-regulatory impact of this public-health message. Psychological Science. 2014;25(4):997–1002. doi: 10.1177/0956797613516981. [DOI] [PubMed] [Google Scholar]
- Lakhani NA, Saraiya M, Thompson TD, King SC, Guy GP. Total body skin examination for skin cancer screening among US adults from 2000 to 2010. Preventive Medicine. 2014;61:75–80. doi: 10.1016/j.ypmed.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavie CJ, De Schutter A, Milani RV. Healthy obese versus unhealthy lean: The obesity paradox. Nature Reviews Endocrinology. 2015;11(1):55–62. doi: 10.1038/nrendo.2014.165. [DOI] [PubMed] [Google Scholar]
- Lebowitz MS, Ahn WK. Emphasizing malleability in the biology of depression: Durable effects on perceived agency and prognostic pessimism. Behaviour Research and Therapy. 2015;71:125–130. doi: 10.1016/j.brat.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz MS, Ahn W. Testing positive for a genetic predisposition to depression magnifies retrospective memory for depressive symptoms. Journal of Consulting and Clinical Psychology. doi: 10.1037/ccp0000254. in press a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz MS, Ahn W. Blue genes? Understanding and mitigating negative consequences of personalized information about genetic risk for depression. Journal of Genetic Counseling. doi: 10.1007/s10897-017-0140-5. in press b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz MS, Ahn WK, Nolen-Hoeksema S. Fixable or fate? Perceptions of the biology of depression. Journal of Consulting and Clinical Psychology. 2013;81(3):518–527. doi: 10.1037/a0031730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MS, Thompson JK. Exploring enhanced menu labels’ influence on fast food selections and exercise-related attitudes, perceptions, and intentions. Appetite. 2016;105:416–422. doi: 10.1016/j.appet.2016.06.007. [DOI] [PubMed] [Google Scholar]
- Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, Croteau-Chonka DC. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major B, Hunger JM, Bunyan DP, Miller CT. The ironic effects of weight stigma. Journal of Experimental Social Psychology. 2014;51:74–80. [Google Scholar]
- Masic U, Christiansen P, Boyland EJ. The influence of calorie and physical activity labelling on snack and beverage choices. Appetite. 2017;112:52–58. doi: 10.1016/j.appet.2017.01.007. [DOI] [PubMed] [Google Scholar]
- McFerran B, Mukhopadhyay A. Lay theories of obesity predict actual body mass. Psychological Science. 2013;24(8):1428–1436. doi: 10.1177/0956797612473121. [DOI] [PubMed] [Google Scholar]
- Meisel SF, Walker C, Wardle J. Psychological responses to genetic testing for weight gain: A vignette study. Obesity. 2012;20(3):540–546. doi: 10.1038/oby.2011.324. [DOI] [PubMed] [Google Scholar]
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Abraham JP. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. The Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver JE, Lee T. Public opinion and the politics of obesity in America. Journal of Health Politics, Policy and Law. 2005;30(5):923–954. doi: 10.1215/03616878-30-5-923. [DOI] [PubMed] [Google Scholar]
- Pathway Genomics. Healthy Weight DNA Insight. n.d. Retrieved August, 2017 from https://www.pathway.com/healthy-weight-dna-insight/
- Pearl RL, Lebowitz MS. Beyond personal responsibility: Effects of causal attributions for overweight and obesity on weight-related beliefs, stigma, and policy support. Psychology & Health. 2014;29(10):1176–1191. doi: 10.1080/08870446.2014.916807. [DOI] [PubMed] [Google Scholar]
- Qualtrics Labs, Inc. Qualtrics labs, Inc (Version 39660) [Computer software] Provo, UT: 2005. [Google Scholar]
- Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. American Journal of Public Health. 2010;100(2):312–318. doi: 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers GB. Reducing bicycle accidents: A reevaluation of the impacts of the CPSC bicycle standard and helmet use. Journal of Product Liability. 1988;11(4):307–317. [Google Scholar]
- Sagberg F, Fosser S, Sætermo IAF. An investigation of behavioural adaptation to airbags and antilock brakes among taxi drivers. Accident Analysis & Prevention. 1997;29(3):293–302. doi: 10.1016/s0001-4575(96)00083-8. [DOI] [PubMed] [Google Scholar]
- Schvey NA, Puhl RM, Brownell KD. The impact of weight stigma on caloric consumption. Obesity. 2011;19(10):1957–1962. doi: 10.1038/oby.2011.204. [DOI] [PubMed] [Google Scholar]
- Segal M. Genetic testing for Obesity: Implications and challenges. Current Obesity Reports. 2017;6(1):93–100. doi: 10.1007/s13679-017-0245-z. [DOI] [PubMed] [Google Scholar]
- Singer E, Corning A, Lamias M. Trends: Genetic testing, engineering, and therapy: Awareness and attitudes. The Public Opinion Quarterly. 1998;62(4):633–664. [Google Scholar]
- Snook KR, Hansen AR, Duke CH, Finch KC, Hackney AA, Zhang J. Change in percentages of adults with overweight or obesity trying to lose weight, 1988–2014. Jama. 2017;317(9):971–973. doi: 10.1001/jama.2016.20036. [DOI] [PubMed] [Google Scholar]
- Walley AJ, Blakemore AI, Froguel P. Genetics of obesity and the prediction of risk for health. Human Molecular Genetics. 2006;15(suppl_2):R124–R130. doi: 10.1093/hmg/ddl215. [DOI] [PubMed] [Google Scholar]
- Yang W, Kelly T, He J. Genetic epidemiology of obesity. Epidemiologic Reviews. 2007;29(1):49–61. doi: 10.1093/epirev/mxm004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


