Abstract
Objectives
To examine whether moderate/vigorous physical activity (MVPA) measured by accelerometry is associated with incident falls, and whether associations differ by physical function or history of falls.
Design
Prospective study with baseline data collection in 2012-2014 and one year of follow-up.
Setting
Women's Health Initiative particip ants living in the U.S.
Participants
5545 ambulatory women aged 63-99
Measurements
Minutes of MVPA per day measured by Actigraph GT3X+ accelerometer; functional status measured by the Short Physical Performance Battery (SPPB); fall risk factors assessed by questionnaire; fall injuries assessed by phone interview; incident falls ascertained from fall calendars.
Results
Incident rate ratios (IRR) revealed increased fall risk among women in the lowest compared to highest quartiles of MVPA (IRR=1.26; 95% CI 1.08-1.48) adjusted for age, race/ethnicity, and fall risk factors. Fall rates were not significantly associated with MVPA among women with high SPPB (9-12) or 0-1 falls in the previous year. However, among women with low SPPB (≤8) or history of frequent falls, fall rates were increased among women with low vs. higher MVPA levels (interaction P -values <0.03 and <0.00001, respectively). Falls among women with MVPA above the median were less likely to involve injuries requiring medical treatment (9.9%), than falls among women with lower MVPA levels (13.0%; P <0.001).
Conclusion
These findings indicate that falls are not more common or injurious among older women who engage in higher levels of MVPA. These findings support encouraging women to engage in the amounts and types of MVPA that they prefer. Older women with low physical function or frequent falls who choose low MVPA represent a high risk group for whom vigilance about falls prevention is warranted.
Keywords: physical activity, falls, older adults, accelerometer, cohort study
Introduction
Twenty-nine million older Americans fell in 2014 causing 2.8 million emergency room visits, 800,000 hospitalizations, 27,000 deaths and an estimated $31.3 billion in Medicare expenditures. 1 Older women are at highest risk for both falling and being injured by falls. 1
While there is strong evidence that multicomponent exercise programs focused on balance, gait, and strength, reduce risk of falls in older adults, 2-4 evidence on the role of aerobic moderate-to-vigorous intensity physical activity (MVPA) in reducing risk of falls among older adults is conflicted. Some studies suggest a role of MVPA in fall prevention via improved muscle mass, 5 and cardiorespiratory fitness. 6 Against this hypothesis is the consensus that the improved cardiorespiratory fitness produced by MVPA is less important to fall risk than is neuromuscular fitness, specifically balance and muscle strength. 4 In the context of public health guidelines that encourage older adults to engage in 2.5 hours of MVPA per week or as much as they are able, 7 it is critical to determine whether such activity reduces risk of falls through maintaining mobility and reducing frailty, or increases fall risk through accidents or fatigue associated with behaviors requiring more rigorous effort.
The Objective Physical Activity and Cardiovascular Health Study (OPACH), nested within the Women's Health Initiative (WHI) Cohort, was designed to examine associations of accelerometer-measured MVPA with cardiovascular disease and fall incidence in older women. This report examines the following questions: (1) Is MVPA associated with incidence of falling? (2) Do associations of MVPA with fall incidence vary by level of physical function and past history of falls? (3) Is MVPA associated with falls that are injurious or require medical care?
Methods
Study Population
Details about the design, recruitment, and data collection for the OPACH study have been previously published. 8 The parent WHI program, which enrolled postmenopausal women, ages 50 to 79 years, between 1993 and 1998 has also been described. 9,10 Enrollment for OPACH occurred concurrently with the Long Life Study (2012-2013), an ancillary study that conducted in-person home visits for phlebotomy and clinical and functional assessments in a subset of older WHI participants. Ambulatory women in the Long Life Study were invited to enroll in OPACH. Informed consent for both studies occurred by mail or telephone. In total, 8618 women consented to OPACH, of whom 1361 (16%) subsequently refused participation or could not be contacted and 219 (3%) were ineligible due to death or inability to walk. An additional 468 (5%) women were excluded because they did not complete the Long Life Study home visit. The remaining 6570 women were given a 13-month falls calendar, physical activity questionnaire, sleep log, and triaxial accelerometer (ActiGraph GT3X+; Pensacola, Florida). Of these, 5545 women had sufficient accelerometer and falls calendar data to be included in this analysis (details below). The Institutional Review Board at the Fred Hutchinson Cancer Research Center approved the study protocols for the Long Life Study and OPACH.
Measures
Women were asked to wear the accelerometer on their right hip for seven days, 24 hours per day, and told to remove the device only for bathing or other water-based activities.
The accelerometer was initialized to collect raw data at 30 Hertz on three orthogonal axes. Using the manufacturer software (ActiLife Firmware v2.4), activity counts at each axis were calculated per 15-second interval (“epoch”). Vector magnitude (VM) counts were calculated by taking the square root of the sum of each axis squared. A computer-based automated algorithm was used to identify the window with the maximum amount of wear over the 7-day wear period. 11 Wear time during sleep was removed using the information provided in the sleep logs or from imputed sleep log data, when sleep logs were incomplete or missing (12%). Non-wear was defined using the Choi algorithm. 12,13 Any nonzero counts (except the allowed short intervals) were considered wear time. An adherent day was defined as 10 or more hours of wear while out of bed and only data from adherent days were analyzed. Participants with less than four adherent days were excluded from analysis. Time spent in total physical activity (PA) included all minutes with VM counts greater than 18 per 15-second epoch. Based on the OPACH Calibration Study, MVPA was defined as VM counts over 518/15s (using 1 metabolic equivalent (MET)=3 ml/kg/min, median MET value= 3.3, interquartile range (IQR) 2.7 to 4.0) and light intensity PA was defined as VM counts of 19-518/15s (median MET value=2.0, IQR 1.6, 2.4). 14 The MVPA cutpoint was equivalent to a walking speed of 2.2 miles per hour (IQR 2.0, 2.5). 14
Incident falls were captured using a 13-month falls calendar, starting with the month the accelerometer was worn. Women were instructed to report a fall if they lost balance and fell to the ground or a lower level or if they had to use a wall, rail or other object to prevent themselves from falling to the ground. Participants reporting falls were interviewed by telephone about the circumstances of the fall, whether they suffered an injury, the type of injury, where the injuries occurred on their body, and the level of medical care received. Women could be interviewed for multiple falls over the course of a year. To conserve resources while ensuring adequate representation for the most active women, after April 2013 fall interviews were conducted for all reported falls among the most physically active women (WHI PA Questionnaire 15 reported PA ≥ 21 MET-hours/week; top 20%), and 1 in 5 randomly selected falls reported by other women.
The OPACH PA questionnaire captured the number of falls in the past year, fall injuries, falls self-efficacy, 16 self-assessed walking ability, and self-reported physical activity. 15 Number of chronic conditions was calculated based on a list of ten conditions from a multi-morbidity study in WHI women. 17 Lower limb physical function, assessed by the Short Physical Performance Battery (SPPB), 18,19 and clinically-measured height and weight were collected at the Long Life Study home visit. Body mass index (BMI) was calculated by weight (kg), divided by height (M), squared.
Statistical Methods
Participants were grouped by quartiles of minutes spent in accelerometer-measured MVPA. For completeness, we also report the main findings for quartiles of accelerometer-measured total PA and light PA. Differences across MVPA quartiles in baseline characteristics were evaluated by the Chi-square tests for categorical variables or analysis of variance for continuous variables. Incident fall rates were calculated as the number of falls reported from the calendar pages divided by the number of person-months of calendar pages received. Since fall incidence is highly right-skewed, negative binomial regression models were used to examine the association of PA quartiles with the incidence rate of falling. Covariates were entered into models adjusting for accelerometer wear time, age, race/ethnicity, and education and then additionally for fall risk factors. These parametric negative-binomial regression models assumed a linear relationship between the incidence rate ratios (IRR) and covariates. These analyses were performed using SAS v9.3 (SAS Institute, Cary, NC). Hypothesis tests were conducted at alpha .05 with two-sided P -values <0.05 considered nominally significant.
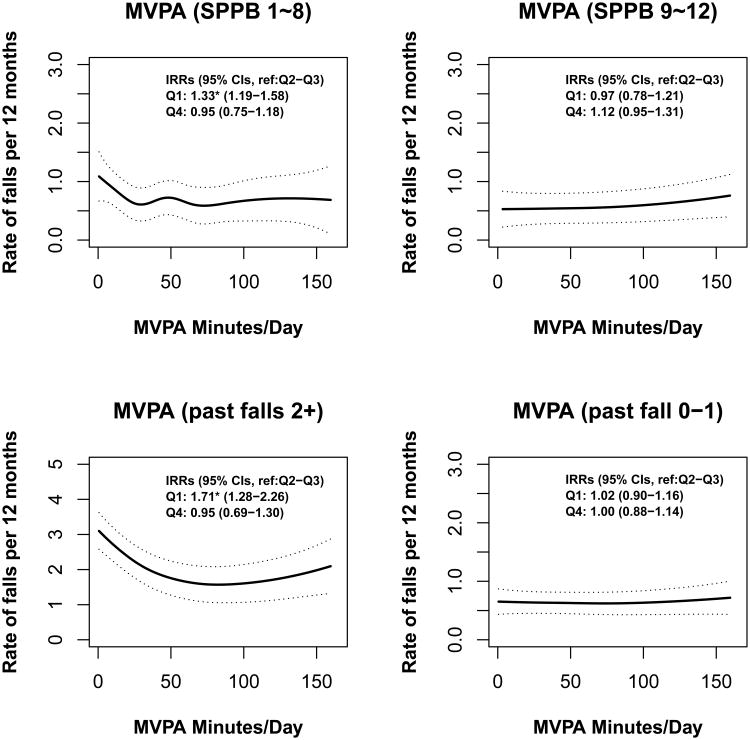
Non-parametric negative binomial generalized additive models that allow flexible modeling of nonlinear relationships without specifying the functional form were used to plot fall incidence rates (number of falls per 13 person-months) by continuous MVPA. These models investigated differences in falls incidence among women with high (SPPB 9-12) vs. low (SPPB 1-8) physical function scores and separately for women with and without history of 2 or more falls in the year before baseline. Stratum-specific P -values were calculated to test the overall association between MVPA and incident falls while accounting for potentially nonlinear effects. Then potential interactions between MVPA and SPPB or past fall history were tested using models fitted with interaction terms. These analyses were performed using the “mgcv package” in R (version 3.2.2).
Finally, associations between MVPA and falls injury events (the unit of analysis) were tested using weighted negative binomial regression with inverse probability weighting to account for sampling of fall interviews.
Ethics Approval
The study was reviewed and approved by the Fred Hutchinson Cancer Research Center Institutional Review Board (Protocol 3467-EXT), Seattle, WA, USA.
Results
Study Population and Baseline Characteristics
A total of 5545 participants with 4-7 adherent wear days of accelerometer data (wear time average=14.9 hours/day, median (IQR)=15.0 (1.7) hours/day) were included. During up to 13 months of falls follow-up (average=11.1 calendar months, median (IQR)=13 (2) calendar-months) women recorded 5464 falls. Participants had an average age of 79 years (SD=6.7, range 63-99) and were diverse by race/ethnicity (50% white, 33% African-American, 17% Hispanic). Many baseline characteristics had statistically significant linear associations by quartile of time spent in accelerometer-measured MVPA (Table 1). Older age, white race, high school education or less, use of assistive devices for walking, higher levels of multiple morbidity, and higher BMI were all strongly associated with lower amounts of time spent in MVPA (Table 1).
Table 1. Participant Characteristics by Accelerometer-measured Moderate/Vigorous Physical Activity.
| Accelerometer-measured minutes per day of MVPA | |||||
|---|---|---|---|---|---|
| Characteristic | Quartile 1(<25.1) | Quartile 2(25.1-<44.1) | Quartile 3(44.1-<69.3) | Quartile 4(≥69.3) | P -value |
| Age category, No. (%) | <0.001 | ||||
| 63 - 74 years | 182 (13.1) | 324 (23.3) | 501 (36.2) | 688 (49.6) | |
| 75 - 79 years | 196 (14.2) | 313 (22.5) | 278 (20.1) | 274 (19.8) | |
| 80 - 84 years | 461 (33.3) | 442 (31.8) | 382 (27.6) | 309 (22.3) | |
| 85 - 89 years | 401 (29.0) | 266 (19.2) | 189 (13.7) | 102 (7.4) | |
| 90+ years | 145 (10.5) | 44 (3.2) | 35 (2.5) | 13 (0.9) | |
| Race/Ethnicity, No. (%) | <0.001 | ||||
| White | 832 (60.1) | 705 (50.8) | 643 (46.4) | 617 (44.5) | |
| Black | 411 (29.7) | 495 (35.6) | 493 (35.6) | 422 (30.5) | |
| Hispanic/Latina | 142 (10.3) | 189 (13.6) | 249 (18.0) | 347 (25.0) | |
| College Graduate, No. (%) | 507 (36.9) | 550 (39.9) | 589 (42.8) | 601 (43.5) | 0.01 |
| Alcohol use in prior 3 months, No. (%) | <0.001 | ||||
| Non-drinker | 574 (46.0) | 510 (39.9) | 431 (33.8) | 393 (29.9) | |
| Less than 1 per week | 422 (33.8) | 448 (35.1) | 444 (34.9) | 427 (32.5) | |
| 1 or more drinks per week | 251 (20.1) | 320 (25.0) | 399 (31.3) | 493 (37.6) | |
| Excellent or very good vision, No. (%) | 598 (48.2) | 646 (50.8) | 662 (52.0) | 759 (58.0) | <0.001 |
| None or very mild body pain, No. (%) | 420 (33.7) | 491 (38.6) | 590 (46.2) | 702 (53.8) | <0.001 |
| Has depressive symptoms, No. (%) | 99 (8.3) | 68 (5.6) | 73 (6.0) | 66 (5.2) | 0.007 |
| Uses sleep aid ≥1 time/week, No. (%) | 233 (18.9) | 230 (18.0) | 201 (15.7) | 206 (15.8) | 0.08 |
| Number of chronic conditions, No. (%) | <0.001 | ||||
| Zero | 171 (13.1) | 199 (15.4) | 297 (22.9) | 378 (28.9) | |
| One | 408 (31.4) | 508 (39.2) | 503 (38.8) | 548 (42.0) | |
| Two | 400 (30.8) | 366 (28.3) | 343 (26.5) | 275 (21.1) | |
| Three or more | 322 (24.8) | 222 (17.1) | 152 (11.7) | 105 (8.0) | |
| Number of falls in past year, No. (%) | <0.001 | ||||
| None | 836 (63.5) | 921 (68.3) | 970 (72.1) | 964 (70.7) | |
| 1 Fall | 281 (21.3) | 283 (21.0) | 255 (19.0) | 269 (19.7) | |
| 2 or more Falls | 200 (15.2) | 144 (10.7) | 121 (9.0) | 131 (9.6) | |
| Injured from fall in past year, No. (%) a | 239 (40.7) | 192 (37.7) | 183 (40.4) | 181 (38.7) | 0.72 |
| Body mass index, mean (SD), kg/m 2 | 28.6 (6.0) | 28.9 (6.0) | 28.0 (5.5) | 26.8 (4.9) | <0.001 |
| Obese (BMI ≥30 kg/m 2), No. (%) | 486 (35.4) | 523 (37.9) | 415 (30.2) | 300 (21.8) | <0.001 |
| SPPB Score categorized, No. (%) | <0.001 | ||||
| 1 - 4 | 230 (19.0) | 98 (7.8) | 51 (4.0) | 38 (3.0) | |
| 5 - 8 | 611 (50.6) | 610 (48.3) | 491 (38.3) | 373 (29.3) | |
| 9 – 12 | 367 (30.4) | 556 (44.0) | 741 (57.8) | 864 (67.8) | |
Among those reporting a fall in the past year. Abbreviations: BMI, body mass index; MVPA, moderate/vigorous physical activity; SD, standard deviation; SPPB, Short Physical Performance Battery. MVPA cutpoint is vector magnitude counts ≥519 per 15-seconds. Percents may not sum to 100 because all variables, except age and race/ethnicity, have some missing data. A higher SPPB score indicates better physical function, scores = 0 were excluded.
PA Levels and Incident Falls
Table 2 shows results of multivariable-adjusted negative binomial regression analyses relating accelerometer-measured MVPA, light PA and total PA to fall incidence rates. Incident rate ratios by quartiles of time spent in MVPA and after adjustment for age, race/ethnicity, education and accelerometer wear time (Model 1), revealed an increased falls rate in the lowest quartile compared to the highest quartile (IRR= 1.43; 95% CI 1.24-1.65; P -value for trend<0.001). This association was decreased, but remained significantly elevated after additional adjustment for falls risk factors (IRR=1.18; 95% CI 1.01-1.38; P -value for trend=0.04). The association of total PA with fall risk was similar to that observed for MVPA after adjustment for fall risk factors (IRR= 1.20 for lowest vs. highest quartiles, 95% CI, 1.03-1.40). No significant association with fall risk was observed for light PA. (Table 2).
Table 2. Falls Incidence Rate Ratios by Minutes per day of Accelerometer-Measured Physical Activity.
| Minutes per day in accelerometer-measured physical activity (quartiles) | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | P for trend | |
| MVPA quartile ranges [mean minutes (SD) =51 (35)] | <25.1 | 25.1-<44.1 | 44.1-<69.3 | ≥ 69.3 | |
| Number of Falls | 1659 | 1375 | 1240 | 1190 | |
| Person-Months | 14443 | 15365 | 15631 | 16117 | |
| Crude falls rate per 1000 PM | 114.9 | 89.5 | 79.3 | 73.8 | |
| Model 1 a, IRR (95% CI) | 1.43 (1.24-1.65) | 1.11 (0.97-1.27) | 1.05 (0.92-1.19) | 1.0 (Ref) | <0.001 |
| Model 2 b, IRR (95% CI) | 1.18 (1.01-1.38) | 1.01 (0.87-1.16) | 0.98 (0.86-1.13) | 1.0 (Ref) | 0.04 |
| Light activity quartile ranges [mean minutes (SD) = 288 (77)] | <233.2 | 233.2-<286.2 | 286.2-<337.4 | ≥ 337.4 | |
| Number of Falls | 1535 | 1325 | 1272 | 1332 | |
| Person-Months | 14723 | 15463 | 15631 | 15739 | |
| Crude falls rate per 1000 PM | 104.3 | 85.7 | 81.4 | 84.6 | |
| Model 1 a, IRR (95% CI) | 1.12 (0.98-1.29) | 0.92 (0.80-1.04) | 0.93 (0.82-1.06) | 1.0 (Ref) | 0.12 |
| Model 2 b, IRR (95% CI) | 1.09 (0.93-1.27) | 0.99 (0.86-1.14) | 1.02 (0.89-1.17) | 1.0 (Ref) | 0.38 |
| Total activity quartile ranges [mean minutes (SD) = 339 (97)] | <270.7 | 270.7-<335.7 | 335.7-<402.0 | ≥ 402.0 | |
| Number of Falls | 1585 | 1327 | 1305 | 1247 | |
| Person-Months | 14688 | 15267 | 15581 | 16020 | |
| Crude falls rate per 1000 PM | 107.9 | 86.9 | 83.8 | 77.8 | |
| Model 1 a, IRR (95% CI) | 1.25 (1.09-1.43) | 1.02 (0.89-1.16) | 1.03 (0.91-1.18) | 1.0 (Ref) | 0.004 |
| Model 2 b, IRR (95% CI) | 1.20 (1.03-1.40) | 1.01 (0.88-1.17) | 1.10 (0.96-1.26) | 1.0 (Ref) | 0.07 |
Adjusted for age, race/ethnicity, education, and wear time.
Adjusted for age, race/ethnicity, education, wear time, vision, body pain, alcohol use, sleep aid use, body mass index, and chronic conditions. Abbreviations: CI, confidence interval; IRR, incidence rate ratio; MVPA, moderate/vigorous physical activity; PM, person-months; Q, quartile; SD, standard deviation. Cutpoint values for moderate/vigorous, light, and total physical activity are vector magnitude counts of ≥519, 19-518, and ≥19 per 15-seconds, respectively. Excludes one participant with 327 verified falls.
Consideration of Functional Status and Fall History
Stratification by high (SPPB 9-12) vs. low (SPPB ≤8) physical function levels and 0-1 falls vs. 2+ falls revealed that incidence rates of falls were not significantly associated with MVPA among women with high physical function or 0-1 falls in the previous year (Figure 1). However, among women with low physical function, incidence rates of falls were significantly increased (IRR=1.33, 95% CI 1.19-1.58) among women with low MVPA levels compared to women in the middle MVPA quartiles, whereas no increased fall risk was seen with high MVPA levels (P -interaction=0.03). Incidence rates of falls were also higher among women with low MVPA who had 2 or more falls (IRR=1.71, 95% CI 1.28-2.26) compared to similar women with MVPA in the middle quartiles, again with no increased risk seen among women with high MVPA levels (Figure 1; P -interaction<0.001).
Figure 1.
Associations of moderate/vigorous physical activity with incidence rate of falls stratified by physical functioning (top panels) and by history of past falls (bottom panels).
MVPA and Fall Injuries
Among the 2495 interviews completed in women who reported falls on monthly calendars, 763 (30.6%) falls caused some type of injury. Women with MVPA below the median were significantly more likely to sustain an injury requiring medical treatment (13.0%; 167/1280) compared to women with higher MVPA levels (9.9%; 120/1215, P <0.001) (Table 3). Fractures were re p orted for 63 falls among women with lower MVPA (4.9%) and for 45 falls among women with higher MVPA (3.7%) (Table 3).
Table 3. Descriptive Information on Falls Injuries by Accelerometer-measured Minutes per day of Moderate/Vigorous Physical Activity.
| Accelerometer-measured minutes per day in MVPA | |||||
|---|---|---|---|---|---|
| Total | Quartile 1(<25.1) | Quartile 2(25.1-<44.1) | Quartile 3(44.1-<69.3) | Quartile 4(≥69.3) | |
| Interviews Completed a, n | 2495 | 726 | 554 | 579 | 636 |
| Interview-reported injurious fall, No. (% of fall interviews) | 763 (30.6) | 192 (26.4) | 187 (33.8) | 183 (31.6) | 201 (31.6) |
| Received medical treatment after injurious fall, No. (% of fall interviews) b | 287 (11.5) | 85 (11.7) | 82 (14.8) | 63 (10.9) | 57 (9.0) |
| Type of medical treatment, No. (% medically treated) | |||||
| Hospital admission | 28 (3.7) | 11 (5.7) | 8 (4.3) | 3 (1.6) | 6 (3.0) |
| Emergency room visit | 127 (16.6) | 33 (17.2) | 41 (21.9) | 28 (15.3) | 25 (12.4) |
| Doctor's office visit | 98 (12.8) | 28 (14.6) | 28 (15.0) | 23 (12.6) | 19 (9.5) |
| Medically treated by someone other than a doctor | 34 (4.5) | 13 (6.8) | 5 (2.7) | 9 (4.9) | 7 (3.5) |
| Self treated or treated by non-medical person | 437 (57.3) | 98 (51.0) | 93 (49.7) | 116 (63.4) | 130 (64.7) |
| Was seriously injured, No. (% of injurious falls) b,c | 349 (45.7) | 98 (51.0) | 98 (53.0) | 78 (43.1) | 75 (37.3) |
| Types of injuries, No. (% of injurious falls) d | |||||
| Fracture | 108 (14.2) | 27 (14.1) | 36 (19.3) | 25 (13.7) | 20 (10.0) |
| Sprain | 122 (16.0) | 31 (16.2) | 29 (15.5) | 32 (17.5) | 30 (14.9) |
| Bruising | 528 (69.2) | 138 (71.9) | 123 (65.8) | 129 (70.5) | 138 (68.7) |
| Cut | 145 (19.0) | 45 (23.4) | 33 (17.7) | 28 (15.3) | 39 (19.4) |
| Scrape | 268 (35.1) | 65 (33.9) | 60 (32.1) | 68 (37.2) | 75 (37.3) |
| Soreness | 620 (81.3) | 162 (84.4) | 151 (80.8) | 140 (76.5) | 167 (83.1) |
Women could be interviewed multiple times.
P <0.001.
Serious injury defined as receiving medical treatment or suffering fracture or sprain.
Multiple injuries possible. Abbreviations: MVPA, moderate/vigorous physical activity.
Discussion
This prospective study shows that the rate of incident falls in older, community-dwelling, ambulatory women is higher among those with low MVPA, not higher MVPA, as measured by accelerometry. The higher risk of falls in the lowest quartile of MVPA was only apparent among women with low levels of objectively-measured physical function or a history of frequent falling in the 12 months prior to baseline and tests for interaction were statistically significant. Low levels of light PA were not associated with significantly increased risk of falling. Higher levels of MVPA also did not impact the risk of falling in these older women regardless of physical function or fall history. Injurious falls requiring medical attention were significantly more common in women with low compared with higher MVPA.
There has been concern that the higher intensity movements of MVPA, including walking, may increase risk of falling. 20 The majority of the evidence on MVPA and falls comes from supervised exercise trials, rather than naturally occurring MVPA in daily life as typically assessed in observational cohort studies. One meta-analysis reported fall prevention exercise programs were more effective if the exercise did not include walking. 21 Yet, recent randomized trials testing MVPA found no increased fall risk 22 even with a walking intervention. 23 A recent systematic review concluded there was insufficient evidence to determine how walking affects fall risk. 24,25 Most fall prevention trials tested multi-component exercise programs and many did not include MVPA as a component. 2 These trials were not designed to evaluate dose-response relationships relating MVPA to risk of falls.
Cross-sectional, nationally representative US data show an association of leisure-time PA with lower prevalence of falling two or more times in the previous year among middle-aged and older adults, but the association diminished in the participants over age 85. 26 Self-reported leisure time physical activity is poorly correlated with accelerometry measurements of MVPA 27 and may be especially inaccurate in older adults and women. 28,29 Accelerometers capture movements during daily life beyond those identified as leisure-time exercise. 27 To our knowledge, the present study is the only US prospective study of accelerometer-measured physical activity with careful falls surveillance in a large population of older women, the group at highest risk of falls and fall-related injuries. 26 The results of this observational study support no association of higher levels of MVPA with fall risk in community-dwelling ambulatory women. Consistent with the present study, the ActiFE-Ulm Study, conducted in Southern Germany among 1214 older adults, found no increased risk of falls among older men or women with higher levels of accelerometer-measured PA. 30
Low levels of MVPA were associated with increased risk of falls and this association appeared to be present only among women in the current study with low physical function or history of frequent falls. This finding is supported by two recent studies showing that fall rates were higher at low levels of walking PA among German older adults with slow walking speeds or history of falls, 30 and with low step counts measured by accelerometry among UK older men with mobility limitations. 31 The higher risk of falls at the lowest levels of MVPA in the present study could reflect a level of severe frailty that prohibits greater amounts of MVPA. Thus, low MVPA may identify a group of older women at exceptionally high risk of falls within two identifiable high risk subgroups, those with low functional status or history of frequent falls. The association may also reflect a modifiable risk factor for falls, if some of these women can be supported to increase their MVPA levels to somewhat higher levels. The similar rates of falls among OPACH women in the highest 3 quartiles of MVPA suggests both the hypothesis that women need not increase their MVPA to the highest levels to achieve a possible reduction in fall risk, and that higher MVPA among women who are capable and chose as such does not necessarily impart increased falls risk. However, an observational study cannot rule out the possibility that women self-select amounts of MVPA that are perceived as safe for them, and that for some women, going from low to medium levels of MVPA may increase fall risk. Future randomized trials should focus on determining whether MVPA can be safely increased in such women.
Use of age appropriate accelerometer cutpoints for classification of MVPA is a major and unique strength of this study. Resting metabolic rate declines with age 32 and the energy costs of activity increase with age. 33,34 These two factors define the numerator (activity energy expenditure) and denominator (resting metabolic rate) of MET intensity values. The OPACH Calibration Study 14 showed that the typically used NHANES cutpoints 35 result in substantial underestimation of MVPA in older women who represent a range of fitness levels, functional abilities and chronic disease burdens (12 vs. 51 minutes/day, respectively in the OPACH women studied here). Age-specific accelerometer intensity cutpoints are critical for accurate classification of PA in older adults.
This study has strengths beyond accelerometer measurement of physical activity, including objective measurement of physical function, a large and race/ethnicity diverse study population, prospective ascertainment of falls using monthly calendars, and the ability to adjust for numerous fall risk factors measured at or prior to baseline. The OPACH study was nested within WHI and thus, not able to include men. The generalizability of these findings to older men is supported by two European studies showing higher fall rates at low levels of accelerometer-measured PA in frail older populations that were exclusively 31 or over half 30 men. While having African-American and Hispanic women constitute half of the study population is a strength, minority women were systematically at the younger end of the age range, necessitating careful adjustment of age and race/ethnicity in all analyses. Surveillance for falls was conducted over one year of follow-up. Although nearly 5800 falls were reported during this period, it would be informative to study fall incidence rates, and their relationship with physical activity habits, over a longer follow-up period. We had insufficient resources to conduct fall interviews for all reported falls, and thus, could only ascertain injurious falls in a subgroup. Future linkage to Medicare data injury codes will be conducted to ascertain rates of injurious falls in this population.
Conclusion
Because of its many health benefits, regular aerobic MVPA is strongly recommended for all older adults. 7 Yet, there has been concern that the body movement of MVPA may increase fall risk, particularly in women with lower levels of physical function and/or history of falls. The present findings reveal that falls are not more common and do not cause more serious injuries among community dwelling women who choose higher levels of MVPA, regardless of physical function level. These findings support encouraging women to engage in the amounts and types of MVPA that they prefer.
Older women with low physical function or frequent falls who choose low MVPA represent a high risk group for participation in effective fall prevention programs. Trials are warranted to determine the benefits and risks of increasing MVPA in such women.
Acknowledgments
The authors acknowledge the following investigators in the WHI Program: Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques E. Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller
Clinical Coordinating Center: Women's Health Initiative Clinical Coordinating Center: (Public Health Sciences, Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet L. Anderson, Ross L. Prentice, Andrea Z. LaCroix, and Charles L. Kooperberg
Investigators and Academic Centers: (Brigham and Women's Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian C. Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert M. Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis H. Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally A. Shumaker
Women's Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally A. Shumaker
For a list of all the investigators who have contributed to WHI science, please visit: https://cleo.whi.org/researchers/SitePages/Write%20a%20Paper.aspx
Sponsor's Role: Decisions concerning study design, data collection and analysis, interpretation of the results, the preparation of the manuscript, and the decision to submit the manuscript for publication resided with committees comprised of WHI investigators that included NHLBI representatives. The contents of the paper are solely the responsibility of the authors.
Funding: This work was supported by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services (contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C) and National Heart, Lung and Blood Institute (grant R01HL105065).
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
Author Contributions: All authors participated in selected portions or all of the planning, design and execution of the study protocol described in this manuscript. AZL drafted this manuscript in close collaboration with all co-authors, each of whom have reviewed, edited, and approved of the final manuscript.
References
- 1.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged >/=65 Years - United States, 2014. MMWR Morb Mort Wkly Rep. 2016;65:993–998. doi: 10.15585/mmwr.mm6537a2. [DOI] [PubMed] [Google Scholar]
- 2.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9 doi: 10.1002/14651858.CD007146.pub3. CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer VA. U.S. Preventive Services Task Force. Prevention of falls in community-dwelling older adults: U.S. Preventive Services Task Force recommendation statement. Ann Int Med. 2012;157:197–204. doi: 10.7326/0003-4819-157-3-201208070-00462. [DOI] [PubMed] [Google Scholar]
- 4.Panel on Prevention of Falls in Older Persons AGS. British Geriatrics S. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 5.Mijnarends DM, Koster A, Schols JM, et al. Physical activity and incidence of sarcopenia: the population-based AGES-Reykjavik Study. Age Ageing. 2016;45:614–620. doi: 10.1093/ageing/afw090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mertz KJ, Lee DC, Sui X, Powell KE, Blair SN. Falls among adults: the association of cardiorespiratory fitness and physical activity with walking-related falls. Am J Prev Med. 2010;39:15–24. doi: 10.1016/j.amepre.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 8.LaCroix AZ, Rillamas-Sun E, Buchner DM, et al. The Objective Physical Activity and Cardiovascular Disease Health in Older Women (OPACH) Study. BMC Public Health. 2017;17:192. doi: 10.1186/s12889-017-4065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Design of the Women's Health Initiative clinical trial andobservational study. The Women's Health Initiative Study Group. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 10.Anderson GL, Manson J, Wallace R, et al. Implementation of the Women's Health Initiative study design. Ann Epidemiol. 2003;13(9 Suppl):S5–17. doi: 10.1016/s1047-2797(03)00043-7. [DOI] [PubMed] [Google Scholar]
- 11.Rillamas-Sun E, Buchner DM, Di C, Evenson KR, LaCroix AZ. Development and application of an automated algorithm to identify a window of consecutive days of accelerometer wear for large-scale studies. BMC Res Notes. 2015;8:270. doi: 10.1186/s13104-015-1229-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43:357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc. 2012;44:2009–2016. doi: 10.1249/MSS.0b013e318258cb36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evenson KR, Wen F, Herring AH, et al. Calibrating physical activity intensity for hip-worn accelerometry in women age 60 to 91 years: The Women's Health Initiative OPACH Calibration Study. Prev Med Rep. 2015;2:750–756. doi: 10.1016/j.pmedr.2015.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer AM, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the Women's Health Initiative physical activity questionnaire. Med Sci Sports Exerc. 2009;41:530–538. doi: 10.1249/MSS.0b013e31818ace55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kempen GI, Yardley L, van Haastregt JC, et al. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008;37:45–50. doi: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- 17.Rillamas-Sun E, LaCroix AZ, Bell CL, Ryckman K, Ockene JK, Wallace RB. The Impact of Multimorbidity and Coronary Disease Comorbidity on Physical Function in Women Aged 80 Years and Older: The Women's Health Initiative. J Gerontol A Biol Sci Med Sci. 2016;71(Suppl 1):S54–61. doi: 10.1093/gerona/glv059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Geronotol A Biol Sci Med Sci. 2000;55:M221–231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 19.Simonsick EM, Gardner AW, Poehlman ET. Assessment of physical function and exercise tolerance in older adults: reproducibility and comparability of five measures. Aging (Milano) 2000;12:274–280. doi: 10.1007/BF03339847. [DOI] [PubMed] [Google Scholar]
- 20.Bea JW, Thomson CA, Wallace RB, et al. Changes in physical activity, sedentary time, and risk of falling: The Women's Health Initiative Observational Study. Prev Med. 2017;95:103–109. doi: 10.1016/j.ypmed.2016.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 22.Gawler S, Skelton DA, Dinan-Young S, et al. Reducing falls among older people in general practice: The ProAct65+ exercise intervention trial. Arch Gerontol Geriatr. 2016;67:46–54. doi: 10.1016/j.archger.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 23.Voukelatos A, Merom D, Sherrington C, Rissel C, Cumming RG, Lord SR. The impact of a home-based walking programme on falls in older people: the Easy Steps randomised controlled trial. Age Ageing. 2015;44:377–383. doi: 10.1093/ageing/afu186. [DOI] [PubMed] [Google Scholar]
- 24.NICE Clinical Guideline 161. London: National Institute for Health and Care Excellence; 2013. National Institute for Health and Care Excellence. Falls: Assessment and prevention of falls in older people. guidance.nice.org.uk/CG161. [PubMed] [Google Scholar]
- 25.Swift CG, Iliffe S. Assessment and prevention of falls in older people--concise guidance. Clin Med (Lond) 2014;14:658–662. doi: 10.7861/clinmedicine.14-6-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caban-Martinez AJ, Courtney TK, Chang WR, et al. Leisure-Time Physical Activity, Falls, and Fall Injuries in Middle-Aged Adults. Am J Prev Med. 2015;49:888–901. doi: 10.1016/j.amepre.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Shiroma EJ, Cook NR, Manson JE, Buring JE, Rimm EB, Lee IM. Comparison of Self-Reported and Accelerometer-Assessed Physical Activity in Older Women. PloS One. 2015;10:e0145950. doi: 10.1371/journal.pone.0145950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bonnefoy M, Normand S, Pachiaudi C, Lacour JR, Laville M, Kostka T. Simultaneous validation of ten physical activity questionnaires in older men: a doubly labeled water study. J Am Geriatr Soc. 2001;49:28–35. doi: 10.1046/j.1532-5415.2001.49006.x. [DOI] [PubMed] [Google Scholar]
- 29.Pettee Gabriel K, McClain JJ, Lee CD, et al. Evaluation of physical activity measures used in middle-aged women. Med Sci Sports Exerc. 2009;41:1403–1412. doi: 10.1249/MSS.0b013e31819b2482. [DOI] [PubMed] [Google Scholar]
- 30.Klenk J, Kerse N, Rapp K, et al. Physical Activity and Different Concepts of Fall Risk Estimation in Older People--Results of the ActiFE-Ulm Study. PloS One. 2015;10:e0129098. doi: 10.1371/journal.pone.0129098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jefferis BJ, Merom D, Sartini C, et al. Physical Activity and Falls in Older Men: The Critical Role of Mobility Limitations. Med Sci Sports Exerc. 2015;47:2119–2128. doi: 10.1249/MSS.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruggiero C, Metter EJ, Melenovsky V, et al. High basal metabolic rate is a risk factor for mortality: the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. 2008;63:698–706. doi: 10.1093/gerona/63.7.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hall KS, Morey MC, Dutta C, et al. Activity-related energy expenditure in older adults: a call for more research. Med Sci Sports Exerc. 2014;46:2335–2340. doi: 10.1249/MSS.0000000000000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.VanSwearingen JM, Studenski SA. Aging, motor skill, and the energy cost of walking: implications for the prevention and treatment of mobility decline in older persons. J Gerontol A Biol Sci Med Sci. 2014;69:1429–1436. doi: 10.1093/gerona/glu153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]