Abstract
In 2013, the United States Preventive Services Task Force recommended routine intimate partner violence (IPV) screening for reproductive-age women. Given the increased attention paid to IPV on a national scale, and broader recognition of its social and physical implications, we sought to characterize the discussions resulting from routine IPV screening—specifically regarding provider response and patient perceptions. In a cross-sectional analysis, we implemented a survey to examine outcomes of IPV screening, including use of guideline-concordant discussion topics and interventions, as well as patient perception of the encounters. Women aged 18–65 with lifetime history of IPV and a past-year healthcare appointment were recruited from clinics and women's shelters in Pennsylvania. Data collection took place from May 2014–January 2015. Of 253 women, 39% were screened for IPV at a healthcare visit in the year prior to survey administration. Of women who were screened, guideline-concordant discussion topics were employed in 70% of encounters and guideline-concordant interventions were offered in 72% of encounters. 58% of women reported being “extremely” or “very satisfied,” and 53% reported being “extremely” or “very comfortable” with IPV-related discussions. The low rate of screening in this population reiterates the importance of focusing efforts on educating providers on the importance of screening, promoting the availability of community resources, and developing systems-based practices that foster IPV screening, discussion, and referral following disclosure.
Keywords: Intimate partner violence, Domestic violence, Screening
Highlights
-
•
Despite recommendations for universal IPV screening, low screening rates persist.
-
•
Guideline-concordant discussion topics were used in 70% of encounters.
-
•
Guideline-concordant interventions were employed in 72% of encounters.
-
•
Most women reported being comfortable/satisfied with IPV discussions with providers.
1. Introduction
Intimate partner violence (IPV) is psychological, physical, or sexual abuse occurring in an intimate relationship (Flitcraft et al., 2009). Centers for Disease Control (CDC) estimates from 2011 suggest that IPV is highly prevalent within US society, with 19% of women experiencing rape within their lifetimes, and 44% of women experiencing other sexual violence (Breiding et al., 2014). IPV has been identified as an etiological risk factor in the development of numerous physical and psychological comorbidities (Campbell and Lewandowski, 1997), and accounts for significant healthcare expenditure annually (Rivara et al., 2007). Thus, healthcare providers are poised to be powerful resources for women by addressing safety concerns and connecting women to resources, with the aim of preventing future violence and reducing morbidity and mortality.
While numerous organizations have issued recommendations for IPV screening, such recommendations, until recently, have not been codified at the federal level. Recognizing the substantial impact of IPV on health, the Institute of Medicine (IOM) determined in 2011 that a substantial preventive service deficit exists in the detection of and intervention in IPV-related morbidity and mortality. Accordingly, the IOM recommended that all women should be screened and counseled for IPV in the healthcare setting, stating “screening for risk of abuse is central to women's safety” (Institutes of Medicine, 2011). In 2013, the United States Preventive Services Task Force (USPSTF) recommended that healthcare providers screen all women of reproductive age (18–46) for lifetime exposure to IPV, and provide appropriate follow-up (Moyer, 2013).
Numerous organizations, including Futures Without Violence, the American Medical Association (AMA), and the American College of Obstetricians and Gynecologists (ACOG), have proposed best-practice guidelines for IPV screening, as well as recommendations for counseling following disclosure. These recommendations address the context and content of screening and provide suggestions for navigating follow-up discussions if a woman discloses abuse (Flitcraft et al., 2009, Anon., 2002, ACOG, 2012).
Evidence-based guidelines regarding the context of IPV screening focus on periodic screening that addresses recent and past IPV exposure. Research shows that women who were previously exposed to IPV are more likely to be re-exposed in the future, and thus comprise a high-risk population (McCall-Hosenfeld et al., 2013). Additionally, women should be screened in private in order to maximize disclosure, and more importantly, decrease the risk of retaliation should their partner become aware of the disclosure (Flitcraft et al., 2009, Anon., 2002, ACOG, 2012).
Guidelines regarding the content of IPV screening and counseling discussions include both discussion topics and provider interventions (Anon., 2013). Given the sensitive nature of IPV-related discussions, the healthcare provider's initial response has potential to influence further discussion as well as the patient's course of action once she leaves the office (Overstreet and Quinn, 2013, Liebschutz et al., 2008). Disclosure of IPV warrants an immediate in-depth conversation. The provider's initial response should focus on validation of the patient's experience, thus establishing a sense of solidarity against IPV (Anon., 2013). Further discussion should consist of assessing the safety of the patient and other household members, the pattern and severity of abuse, and should include development of a safety plan if abusive behavior escalates (Flitcraft et al., 2009, ACOG, 2012, Anon., 2013). Likewise, the provider should assess the impact IPV is having on the woman's physical health, mental health, and interpersonal relationships to determine how best to approach further discussion and intervention (Flitcraft et al., 2009, Anon., 2002, ACOG, 2012).
To date, relatively little research has addressed the nature of the discussions that take place following screening or patient perceptions of these encounters; however, women who discuss IPV with their healthcare providers are more likely to pursue other safety measures, such as contacting community-based domestic violence services (Bair-Merritt et al., 2014, Coker et al., 2002). Barriers to discussing IPV with patients commonly cited by healthcare providers include time constraints, provider discomfort with IPV screening questions, and lack of provider knowledge of referral resources (McCall-Hosenfeld et al., 2014). Sutherland et al., in 2014 found that, of clinicians who screened patients for IPV, 13% did not document any follow-up discussion, and the vast majority (81.5%) did not offer an action-oriented response, such as offering a follow-up appointment or making a referral to domestic violence services (Sutherland et al., 2014).
Similarly, providers historically have expressed concern that screening for IPV may harm the patient-provider relationship; however, these concerns have been largely unfounded in analysis of real-world screening programs (Renker and Tonkin, 2006). Patients who have been exposed to IPV tend to view counseling discussions with their healthcare providers as a strategic response (Swailes et al., 2016). Indeed, patients who receive preventive services such as IPV screening are more likely to report being satisfied with the encounter (Weingarten et al., 1995).
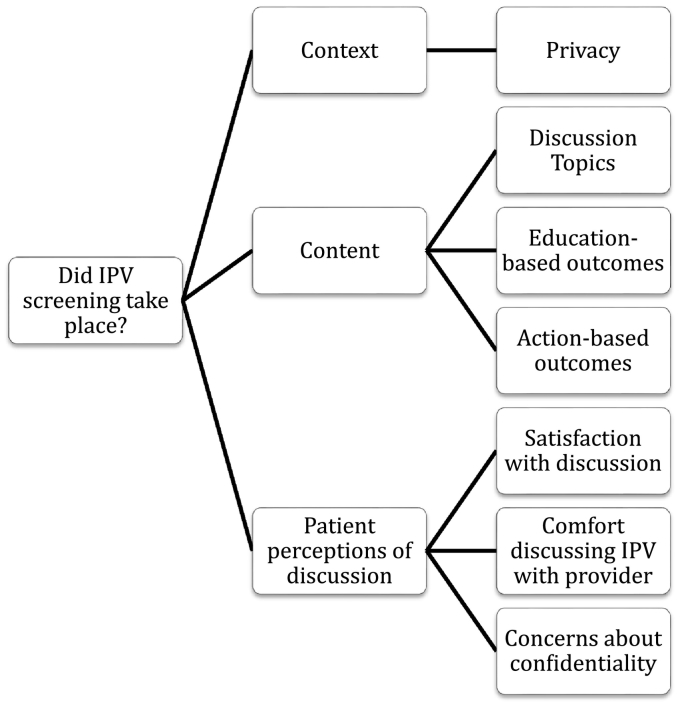
While many previous studies have addressed screening rates, very little data exists regarding the content of discussions that follow screening. Likewise, little data exists regarding the acceptability of IPV-related discussions from the patient's perspective—especially those previously exposed to IPV—as most studies focus on provider-perceived barriers to screening. This study seeks to examine screening rates following the 2013 USPSTF recommendation for universal IPV screening, as well as to add insight into the context and content of the discussion that takes place surrounding IPV screening. Finally, we seek to provide a more robust idea of the opinions of women regarding IPV-related discussions. In accordance with guidelines proposed by Futures Without Violence, as well as recommendations by AMA and ACOG, we developed a survey to examine the context and content of IPV-related discussions in the healthcare setting, and to characterize patients' comfort and satisfaction with the encounter. The conceptual framework of the study is included in Fig. 1. We underscore the importance of characterizing these clinical encounters, so as to better understand the areas for improvement in healthcare provider-based preventive screening, counseling, and intervention for IPV-exposed women.
Fig. 1.
Conceptual framework for IPV discussions in clinical setting. Data collected May 2014–January 2015, Central PA.
2. Methods
Surveys were administered as part of a longitudinal study of women's health issues in a population with lifetime exposure to IPV. Inclusion criteria included: 1) female gender, 2) age 18–64, 3) a healthcare appointment in the preceding year, and 4) history of lifetime IPV, measured by a modified HARK screening instrument (Sohal et al., 2007) (The original language of the HARK instrument asks women “Within the last year, have you [been exposed to “X”]?” We modified this to form a two-level question in which participants were asked “Within your lifetime, have you [been exposed to “X”].” If the response was affirmative, they were then asked about exposure in the preceding year). Consent to participate in this research study was obtained from all participants. Study documents and protocols were reviewed and approved by the Institutional Review Board of the Pennsylvania State University. A Certificate of Confidentiality was obtained from the National Institutes of Mental Health (CC-MH-12-204) prior to the conduct of this research.
The primary source for recruitment was the Penn State Ambulatory Research Network (PSARN), a group of outpatient primary care clinics in Central Pennsylvania affiliated with the Penn State Health Milton S. Hershey Medical Center. PSARN-associated clinics are comprised of approximately 125 providers, and encompass the specialties of Family Medicine, Internal Medicine, and Pediatrics. The mission of PSARN is to provide a platform from which to conduct primary care research.
From 24,338 eligible women with an appointment at a PSARN facility in the 12 months prior to recruitment, a randomized, rurality-stratified subsample of 2500 women was constructed. Stratification based on rurality was performed to over-sample rural residents, as the parent study was designed to examine strategies and mental health outcomes in rural women exposed to IPV. These women were sent screening questionnaires with a $2 incentive. Participants had the option of completing screening questionnaires online, by phone, or by mail. Participants were considered to screen positive for IPV exposure if they reported any lifetime exposure to emotional, physical, or sexual abuse on the modified HARK instrument. 1191 women responded to the screening questionnaire, of whom 500 reported IPV exposure. These women were invited to complete a baseline survey via mail, phone, or online survey. These women received a $25 gift card as compensation. 271 women from PSARN completed the baseline survey.
This sample was augmented by recruitment from 26 Pennsylvania women's shelters, which were non-profit organizations with the mission of assisting women with housing as well as providing crisis and counseling services for women exposed to IPV. Flyers posted in these shelters advertised the opportunity to participate in this study. Screening questionnaires were returned by 73 women, of whom 60 reported lifetime IPV exposure. 39 women completed the baseline survey. In total, 310 women completed the baseline survey. Recruitment, screening, and completion of baseline surveys took place from May 2013–January 2014.
Participants were again contacted one year later to complete a follow-up survey. Of the 310 individuals who completed the baseline survey, 266 completed follow-up surveys. 250 women reported having a healthcare visit in the year since baseline survey completion. These women comprised our analytic subsample. 222 were recruited from PSARN and 28 were recruited from women's shelters. Data collection for the current analysis took place from May 2014–January 2015.
2.1. Measures
Demographic information including age and race was obtained from questions adapted from standardized surveys already used in this population, such as the Central Pennsylvania Women's Health Study (CePAWHS) (Weisman et al., 2006).
To the authors' knowledge, there are no validated survey instruments regarding patient-reported content and context of IPV-related discussions. To evaluate the context and content of IPV screening and counseling discussions, we developed and pretested a set of questions using evidence-based guidelines from the USPSTF, the American Medical Association, Futures Without Violence, and the American College of Obstetricians and Gynecologists, and informed by prior research (Anon., 2002, McCloskey et al., 2005, Usta et al., 2012, Bair-Merritt et al., 2008, Campbell et al., 2009, HCAHPS, n.d). Pretesting was conducted by administering the survey to 10 individuals of reproductive age, who offered feedback regarding the readability of the questions, the adequacy of the answer options, and the length of the survey. Feedback was incorporated into new survey drafts.
The context of the screening encounter was determined to be the presence of other individuals in the room at the time of IPV screening. Content questions consisted of selecting discussion topics, education-based outcomes, and action-based outcomes from a list generated from guidelines published by Futures Without Violence, ACOG, and the AMA. The checklist of potential responses can be seen in the original survey document (Appendix). Participants had an option to add free-text responses, which were reviewed by investigators and recoded either as a listed option or added as a separate intervention in the descriptive statistics.
Patient perceptions centered on privacy concerns, unshared information, and satisfaction and comfort levels. Satisfaction and comfort were determined on a 5-point, Likert-type scale, with language modified from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Satisfaction Survey (HCAHPS, n.d.). Participants were subsequently asked if there was anything they wanted to discuss with their provider but were not able to. If they responded affirmatively, they were asked what they would have liked to discuss and why they felt they were unable to do so. Free-text responses were recorded. If women reported that they did not have an IPV-related discussion with their provider, a follow-up question was asked: “would you have liked to talk to a healthcare provider about domestic violence or whether you feel safe at home?”
2.2. Statistical analysis
Frequencies for demographics, screening rates, and guideline-concordant discussion topics and interventions were developed for the full population. Analyses of questions regarding context, content, and patient perceptions were limited to women who reported that screening or IPV disclosure had occurred in a healthcare visit within the past year. As the purpose of this analysis was largely to obtain descriptive measures, we did not control for potential covariates, interactions, or missing data.
Study data were collected and managed using REDCap electronic data capture tools hosted at Pennsylvania State University. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies (Harris et al., 2009).
The data analysis for this paper was generated using SAS software, Version 9.3 of the SAS System (SAS, 2002). All analyses were performed from October 2014–March 2015.
3. Results
3.1. Demographics
As shown in Table 1, of 253 IPV-exposed women, mean age was 43.4 years (± 12.4). 54.2% of the population was of reproductive age (18–46). 91% of the sample was White, non-Hispanic, with 3% Black, 1% Asian, and 1% other. 88% were recruited from clinic sites, and 11% from women's shelters. 52% were exposed to IPV within the past year.
Table 1.
Demographic information. Data collected May 2014–January 2015, Central PA.
| Mean age | 43.5 ± 12.4 |
|
|---|---|---|
| N | % | |
| Age | ||
| Reproductive age (18–46) | 137 | 54.2% |
| Greater than reproductive age (> 46) | 113 | 44.7% |
| Race | ||
| White, non-Hispanic | 229 | 91% |
| Black | 7 | 2.8% |
| Asian | 2 | 0.8% |
| Other | 24 | 9% |
| Recruitment site | ||
| PSARN | 222 | 88% |
| Women's shelter | 29 | 11% |
| Screening status | ||
| Screened | 98 | 39% |
| Not screened | 155 | 61% |
| IPV exposure | ||
| Past-year | 52 | 21% |
| Lifetime | 201 | 79% |
3.2. Screening rates
Of 253 women, 39% (N = 98) reported discussing IPV with their healthcare providers. Eight percent of women who discussed IPV with their provider reported initiating the discussion without being asked.
3.3. Screening context
As shown in Table 2, during IPV-related discussions with their healthcare providers, 10% reported that someone else was in the room. None of the other individuals in the room were spouses or partners.
Table 2.
Screening context, content, and patient perceptions. Data collected May 2014–January 2015, Central PA.
| Domain | N (%) | |
|---|---|---|
| Screening context | Other individual in room | |
| Yes | 10 (10) | |
| No | 88 (90) | |
| Screening content | Currently concerned with IPV | 7 (7) |
| Discussion topics | ||
| Patient's concern about situation | 32 (33) | |
| Patient's emotional health | 20 (20) | |
| Patient's physical health | 11 (11) | |
| Safety assessment | 19 (19) | |
| Nature of abuse | 16 (16) | |
| Partner's substance abuse | 9 (9) | |
| Effects on relationships with friends/family | 9 (9) | |
| Effects on children | 5 (5) | |
| Number of guideline-concordant discussion topics used | ||
| None | 29 (30) | |
| One | 42 (42) | |
| Multiple | 27 (28) | |
| Outcomes | ||
| Provided information about resources | 22 (22) | |
| Validated patient's experience | 18 (18) | |
| Developed/discussed a safety plan | 14 (14) | |
| Prescribed medication | 14 (14) | |
| Scheduled follow-up | 14 (14) | |
| Scheduled mental health appointment | 5 (5) | |
| Provided information about IPV | 3 (3) | |
| Provided information for social or community services | 2 (2) | |
| Contacted law enforcement | 1 (1) | |
| Number of guideline-concordant responses offered | ||
| None | 27 (28) | |
| One | 58 (59) | |
| Multiple | 13 (13) | |
| Patient perceptions | Satisfaction in discussing IPV with provider | |
| Extremely satisfied | 28 (29) | |
| Very satisfied | 27 (28) | |
| Somewhat satisfied | 12 (12) | |
| Somewhat dissatisfied | 1 (1) | |
| Very dissatisfied | 0 (0) | |
| Comfort in discussing IPV with provider | ||
| Extremely comfortable | 24 (25) | |
| Very comfortable | 26 (27) | |
| Somewhat comfortable | 9 (9) | |
| Somewhat uncomfortable | 5 (5) | |
| Very uncomfortable | 2 (2) | |
| Did not discuss IPV with provider (N = 155), but would have liked to | 10 (4) |
3.4. Screening content
As shown in Table 2, of the 98 women who discussed IPV with their healthcare provider in the past year, 7% told their healthcare provider that they were currently concerned about domestic violence. Guideline-concordant discussion topics included: patient's concern about situation (33%), patient's emotional (20%) or physical (11%) health, safety assessment (19%), nature of abuse (16%), partner's substance abuse (9%), effects on friends/family (9%), and children (5%). Composite analyses of these conversations showed that 30% of women did not have a discussion composed of any guideline-concordant topics, 42% of women had a discussion encompassing one guideline-concordant topic, and 28% of women had a discussion including more than one guideline-concordant topic.
Guideline-concordant outcomes of these discussions included providing information about available resources (22%), validation of the patient's experience (18%), development of a safety plan (14%), providing prescription medication (14%), scheduling a follow-up appointment (14%), scheduling a mental health appointment (5%), providing information regarding IPV (3%), providing contact information for social or domestic violence services (2%), and contacting law enforcement (1%). Composite analyses of these interactions showed that 28% of IPV-related discussions did not result in a guideline-concordant intervention, 58% resulted in one guideline-concordant intervention, and 14% resulted in multiple guideline-concordant interventions.
3.5. Patient perceptions
Of all women screened for IPV, 28.5% reported being “extremely satisfied” with their discussion with their healthcare provider, 27.5% “very satisfied,” 12% “somewhat satisfied”, and 1% “somewhat dissatisfied.” The non-response rate for this question was 31%. Likewise, 25% reported being “extremely comfortable” discussing IPV with their healthcare provider, 27% “very comfortable,” 9% “somewhat comfortable,” 5% “somewhat uncomfortable,” and 2% “very uncomfortable.” The non-response rate for this question was 33%. Of women who did not discuss IPV with their healthcare provider (N = 155), 4% would have liked to have talked about IPV with their providers, but did not feel they had the chance. Two participants offered free-text responses for why they felt they were unable to discuss their exposure to IPV with their healthcare provider. One participant related that she felt there was not adequate time, and the other stated, “I couldn't talk to her and get her to understand what was really going on.” No women reported having concerns about confidentiality associated with these clinical encounters. Two women had concerns they felt were not addressed in the conversation with their provider.
4. Discussion
This study adds essential knowledge to the current literature regarding universal IPV screening by 1) quantifying screening rates subsequent to the 2013 USPSTF recommendation, 2) exploring content of IPV-related discussions, and 3) investigating the acceptability of IPV screening in a subset of women previously exposed to IPV.
4.1. Screening rates post-2013 USPSTF recommendation
One of the primary aims of this study was to examine the rates of IPV screening subsequent to the 2013 USPSTF recommendation for universal screening of reproductive-aged women. Despite evidence that women who have experienced IPV in the past are more likely to experience it again (McCall-Hosenfeld et al., 2013), IPV screening in our sample remained low at 39%.
Previous studies have examined the rationale behind low rates of screening from providers' perspectives, with cited barriers including lack of time (Colarossi et al., 2010), lack of knowledge regarding community resources, feelings of powerlessness (Colarossi et al., 2010, Elliott et al., 2002), underestimation of the effects of IPV (Elliott et al., 2002), and fear of damaging rapport with patients (Elliott et al., 2002). Our data show that despite national efforts in the US supporting universal IPV screening (Moyer, 2013, Anon., 2013, de Boinville, 2013), rates of screening remain unacceptably low.
Previous research shows that educating providers about the prevalence of IPV and providing validated methods of screening increases screening rates (Waalen et al., 2000). Beyond provider education, system-wide support for IPV screening—including collaboration between physicians, nurses, staff, and social workers—has been shown to improve attitudes toward screening (Campbell et al., 2001). Thus, system-wide supports should be implemented to ensure that healthcare providers have the resources necessary to address these sensitive issues as they arise.
4.2. Screening context and content
Another primary aim of this study was to develop further insight into the context and content of IPV screening and counseling discussions. We found that the vast majority of respondents were screened in private, and those who were not alone at the time of screening were accompanied by a nurse or family member other than a partner or spouse (a young child, for example). Therefore, providers who did perform screening appeared to do so with privacy considerations in mind.
Regarding the content of IPV-related discussions, little research has explored the outcomes (particularly non-tangible outcomes) of IPV-related discussions in the healthcare setting. In their 2015 Cochrane review, O'Doherty et al. reveal that universal screening, while resulting in increased IPV detection, resulted inconsistently in increased referral to services (O'Doherty et al., 2015). Our data reflect that guideline-concordant discussion topics were employed in nearly 70% of patient encounters where screening occurred, and guideline-concordant interventions were employed in 72% of encounters. These data suggest that even though screening rates may not have changed appreciably, physicians who do screen frequently respond with guideline-concordant topics/interventions.
These data must be approached cautiously. While it is heartening that providers who screen pursue appropriate discussion topics and interventions, it is of paramount importance to remember that only 39% of providers performed IPV screening. Greater efforts must be made to remove provider-perceived barriers to screening.
The CDC's National Intimate Partner and Sexual Violence Survey addresses the outstanding need for integration of domestic violence services into the healthcare response to IPV disclosure, stating “the health care system's response must be strengthened and better coordinated for […] survivors to help navigate the health care system and access needed services and resources in the short and long term” (Black et al., 2011).
4.3. Patient perceptions of IPV screening and counseling discussions
The third aim of this study was to examine patient perceptions of IPV screening. Despite low screening rates, we found that the majority of women who participated in IPV-related discussions felt comfortable discussing IPV with their providers, and that, among women who did not have the opportunity to discuss IPV, some would have liked to have had this discussion.
Patient acceptance of IPV screening in the healthcare setting has been reported in the international literature, with studies in Germany, New Zealand, and Ireland reporting acceptability rates > 90% (Stöckl et al., 2013, Koziol-McLain et al., 2008, McDonnell et al., 2006). Likewise, US studies have shown similar figures when addressing IPV screening among pregnant women (Renker and Tonkin, 2006). To the authors' knowledge, however, this is the first study addressing the acceptability of IPV screening in women exposed to IPV. While further investigation into factors influencing the acceptability of IPV-related discussions in IPV-exposed women is warranted, our data should encourage providers who may be reluctant to discuss IPV in the clinical setting (Chuang et al., 2012).
4.4. Limitations and strengths
Limitations of this study include the fact that data obtained regarding clinical encounters rely on recollection of information that may be as distant as one year in the past. Likewise, while much of our survey instrument was based on well-validated instruments (CePAWHS, HARK, HCAHPS, etc.) (Sohal et al., 2007, Weisman et al., 2006, HCAHPS, n.d), additional questions were formulated specifically for the purposes of obtaining information regarding the context and content of IPV screening and counseling. The language of these sections of the survey has no prior validation. Additionally, as our sample was comprised of women who had attended a healthcare appointment in the past year, some of whom were using services of a local women's shelter, this group may display greater help-seeking behavior than other women who have experienced IPV, possibly influencing disclosure rates and attitudes toward medical professionals. Also, our sample was comprised of over 90% white, non-Hispanic participants. While this distribution is representative of central Pennsylvania and the catchment area of our outpatient primary clinics, it is not generalizable to other locales. Finally, our study was geographically limited. Screening practices of providers may be influenced by local context, such as the availability of referral resources, the perceived support for screening and counseling in healthcare practices, and regional culture. Thus, the experiences of the patients in our sample may not be representative of patients who are screened in a different region or practice setting.
Strengths of this study include contributing to a relatively small repository of data regarding IPV screening rates subsequent to the 2013 USPSTF recommendation. Additionally, this study is the first, to our knowledge, to measure the context and content of IPV screening and counseling encounters in accordance with best practice guidelines, and to examine acceptability of IPV screening in a high-risk population of women previously exposed to IPV.
5. Conclusions
Our data suggest that further efforts are necessary to ensure that screening and counseling discussions comprise a meaningful part of women's healthcare. Focus should remain on keeping providers abreast of resources within their communities for women who have been exposed to IPV, while systems- and community-based support must be in place in the event of a disclosure, as IPV screening that does not result in meaningful follow-up discussion and intervention does little to improve the lives of women exposed to IPV.
Transparency document
Transparency document.
Acknowledgments
Acknowledgments
The authors would like to thank Fern Gilkerson and Denise Scotland of the Doris Duke Foundation and Amanda Perry.
Funding
This work was supported by Grant 2012064 from the Doris Duke Charitable Foundation. The funders had no role in the collection, analysis or interpretation of the data. Study data were collected and managed using REDCap™ electronic data capture tools hosted at Penn State (Pennsylvania State University CTSI, NIH/NCATS grant number UL1 TR000127).
Conflicts of interest
The authors declare that there are no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2017.10.017.
Appendix A. Survey
Supplementary material
References
- ACOG Committee Opinion No. 518: Intimate partner violence. Obstet. Gynecol. 2012;119(2 Pt 1):412–417. doi: 10.1097/AOG.0b013e318249ff74. [DOI] [PubMed] [Google Scholar]
- Anon. In: National Consensus Guidelines on Identifying and Responding to Domestic Violence Victimization in Health Care Settings. TFVP Fund., editor. 2002. (San Francisco, CA) [Google Scholar]
- Anon. 2013. National Conference on Health and Domestic Violence: Futures Without Violence Guidelines. [Google Scholar]
- Bair-Merritt M.H., Jennings J.M., Eaker K., Tuman J.L., Park S.M., Cheng T.L. Screening for domestic violence and childhood exposure in families seeking care at an urban pediatric clinic. J. Pediatr. 2008;152(5) doi: 10.1016/j.jpeds.2008.01.035. (734–736, 736.e731) [DOI] [PubMed] [Google Scholar]
- Bair-Merritt M.H., Lewis-O'Connor A., Goel S. Primary care-based interventions for intimate partner violence: a systematic review. Am. J. Prev. Med. 2014;46(2):188–194. doi: 10.1016/j.amepre.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Black M.C., Basile K.C., Breiding M.J. In: The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. CfDCa Prevention., editor. National Center for Injury Prevention and Control; Atlanta, GA: 2011. [Google Scholar]
- de Boinville M. Screening for domestic violence in health care settings. In: OoHSP, editor. Health and Human Services. vol. 2014. APSE Policy Brief; 2013. [Google Scholar]
- Breiding M.J., Smith S.G., Basile K.C., Walters M.L., Chen J., Merrick M.T. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill. Summ. 2014;63(8):1–18. [PMC free article] [PubMed] [Google Scholar]
- Campbell J.C., Lewandowski L.A. Mental and physical health effects of intimate partner violence on women and children. Psychiatr. Clin. North Am. 1997;20(2):353–374. doi: 10.1016/s0193-953x(05)70317-8. [DOI] [PubMed] [Google Scholar]
- Campbell J.C., Coben J.H., McLoughlin E. An evaluation of a system-change training model to improve emergency department response to battered women. Acad. Emerg. Med. 2001;8(2):131–138. doi: 10.1111/j.1553-2712.2001.tb01277.x. [DOI] [PubMed] [Google Scholar]
- Campbell J.C., Webster D.W., Glass N. The danger assessment: validation of a lethality risk assessment instrument for intimate partner femicide. J. Interpers. Violence. 2009;24(4):653–674. doi: 10.1177/0886260508317180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang C.H., Cattoi A.L., McCall-Hosenfeld J.S., Camacho F., Dyer A.M., Weisman C.S. Longitudinal association of intimate partner violence and depressive symptoms. Ment Health Fam Med. 2012;9(2):107–114. [PMC free article] [PubMed] [Google Scholar]
- Coker A.L., Bethea L., Smith P.H., Fadden M.K., Brandt H.M. Missed opportunities: intimate partner violence in family practice settings. Prev. Med. 2002;34(4):445–454. doi: 10.1006/pmed.2001.1005. [DOI] [PubMed] [Google Scholar]
- Colarossi L., Breitbart V., Betancourt G. Barriers to screening for intimate partner violence: a mixed-methods study of providers in family planning clinics. Perspect. Sex. Reprod. Health. 2010;42(4):236–243. doi: 10.1363/4223610. [DOI] [PubMed] [Google Scholar]
- Elliott L., Nerney M., Jones T., Friedmann P.D. Barriers to screening for domestic violence. J. Gen. Intern. Med. 2002;17(2):112–116. doi: 10.1046/j.1525-1497.2002.10233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flitcraft A., Hadley S., Hendricks-Matthews M., McLeer S., Warshaw C. Archives of Family Medicine. 2009. American Medical Association diagnostic and treatment guidelines on domestic violence. [DOI] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HCAHPS Satisfaction Survey. In. https://www.hcahpsonline.org: Centers for Medicare and Medicaid Services, Baltimore, MD n.d.
- Institutes of Medicine . The National Academies Press; Washington, DC: 2011. Clinical Preventive Services for Women: Closing the Gaps. [Google Scholar]
- Koziol-McLain J., Giddings L., Rameka M., Fyfe E. Intimate partner violence screening and brief intervention: experiences of women in two New Zealand Health Care Settings. J. Midwifery Womens Health. 2008;53(6):504–510. doi: 10.1016/j.jmwh.2008.06.002. [DOI] [PubMed] [Google Scholar]
- Liebschutz J., Battaglia T., Finley E., Averbuch T. Disclosing intimate partner violence to health care clinicians - what a difference the setting makes: a qualitative study. BMC Public Health. 2008;8:229. doi: 10.1186/1471-2458-8-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall-Hosenfeld J.S., Chuang C.H., Weisman C.S. Prospective association of intimate partner violence with receipt of clinical preventive services in women of reproductive age. Womens Health Issues. 2013;23(2):e109–116. doi: 10.1016/j.whi.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall-Hosenfeld J.S., Weisman C.S., Perry A.N., Hillemeier M.M., Chuang C.H. “I just keep my antennae out”: how rural primary care physicians respond to intimate partner violence. J. Interpers. Violence. 2014;29(14):2670–2694. doi: 10.1177/0886260513517299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey L.A., Lichter E., Ganz M.L. Intimate partner violence and patient screening across medical specialties. Acad. Emerg. Med. 2005;12(8):712–722. doi: 10.1197/j.aem.2005.03.529. [DOI] [PubMed] [Google Scholar]
- McDonnell E., Holohan M., Reilly M.O., Warde L., Collins C., Geary M. Acceptability of routine enquiry regarding domestic violence in the antenatal clinic. Ir. Med. J. 2006;99(4):123–124. [PubMed] [Google Scholar]
- Moyer V.A. Screening for intimate partner violence and abuse of elderly and vulnerable adults: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2013;158(6):478–486. doi: 10.7326/0003-4819-158-6-201303190-00588. [DOI] [PubMed] [Google Scholar]
- O'Doherty L., Hegarty K., Ramsay J., Davidson L.L., Feder G., Taft A. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst. Rev. 2015;7:CD007007. doi: 10.1002/14651858.CD007007.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overstreet N.M., Quinn D.M. The intimate partner violence stigmatization model and barriers to help-seeking. Basic Appl. Soc. Psychol. 2013;35(1):109–122. doi: 10.1080/01973533.2012.746599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renker P.R., Tonkin P. Women's views of prenatal violence screening: acceptability and confidentiality issues. Obstet. Gynecol. 2006;107(2 Pt 1):348–354. doi: 10.1097/01.AOG.0000195356.90589.c5. [DOI] [PubMed] [Google Scholar]
- Rivara F.P., Anderson M.L., Fishman P. Healthcare utilization and costs for women with a history of intimate partner violence. Am. J. Prev. Med. 2007;32(2):89–96. doi: 10.1016/j.amepre.2006.10.001. [DOI] [PubMed] [Google Scholar]
- SAS Institute Statistical Analysis System. SAS/STAT User's Guide (Version 9.3). SAS Institute Inc., Cary, NC 2002–2012.
- Sohal H., Eldridge S., Feder G. The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Fam. Pract. 2007;8:49. doi: 10.1186/1471-2296-8-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stöckl H., Hertlein L., Himsl I. Acceptance of routine or case-based inquiry for intimate partner violence: a mixed method study. BMC Pregnancy Childbirth. 2013;13:77. doi: 10.1186/1471-2393-13-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland M.A., Fontenot H.B., Fantasia H.C. Beyond assessment: examining providers' responses to disclosures of violence. J. Am. Assoc. Nurse Pract. 2014;26(10):567–573. doi: 10.1002/2327-6924.12101. [DOI] [PubMed] [Google Scholar]
- Swailes A.L., Lehman E.B., Perry A.N., McCall-Hosenfeld J.S. Intimate partner violence screening and counseling in the health care setting: perception of provider-based discussions as a strategic response to IPV. Health Care Women Int. 2016;37(7):790–801. doi: 10.1080/07399332.2016.1140172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usta J., Antoun J., Ambuel B., Khawaja M. Involving the health care system in domestic violence: what women want. Ann. Fam. Med. 2012;10(3):213–220. doi: 10.1370/afm.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waalen J., Goodwin M.M., Spitz A.M., Petersen R., Saltzman L.E. Screening for intimate partner violence by health care providers. Barriers and interventions. Am. J. Prev. Med. 2000;19(4):230–237. doi: 10.1016/s0749-3797(00)00229-4. [DOI] [PubMed] [Google Scholar]
- Weingarten S.R., Stone E., Green A. A study of patient satisfaction and adherence to preventive care practice guidelines. Am. J. Med. 1995;99(6):590–596. doi: 10.1016/s0002-9343(99)80243-5. [DOI] [PubMed] [Google Scholar]
- Weisman C.S., Hillemeier M.M., Chase G.A. Preconceptional health: risks of adverse pregnancy outcomes by reproductive life stage in the Central Pennsylvania Women's Health Study (CePAWHS) Womens Health Issues. 2006;16(4):216–224. doi: 10.1016/j.whi.2006.01.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.
Supplementary material