Abstract
Integrating physical activity (PA) counseling in routine clinical practice remains a challenge. The purpose of this study was to evaluate the implementation and effectiveness of a pragmatic strategy aimed to improve physician PA counseling and patient PA. An effectiveness-implementation type-2 hybrid design was used to evaluate a 3-h training (i.e., implementation strategy-IS) to increase physician use of the 5-As (assess, advise, agree, assist, arrange) for PA counseling (i.e., clinical intervention-CI) and to determine if the CI improved patient PA. Patients of trained and untrained physicians reported on PA and quality of life pre-post intervention. Medical charts (N = 1700) were examined to assess the proportion of trained physicians that used the 5-As. The RE-AIM framework informed our evaluation. 305/322 of eligible physicians participated in the IS (M age = 40 years, 52% women) and 683/730 of eligible patients in the CI (M age = 49 years, 77% women). The IS was adopted by all state regions and cost ~ $20 Mexican pesos (US$1) per provider trained. Physician adoption of any of the 5-As improved from pre- to post-training (43 vs. 52%, p < .01), with significant increases in the use of assessment (43 vs. 52%), advising (25 vs. 39%), and assisting with barrier resolution (7 vs. 15%), but not in collaborative goal setting (13 vs. 17%) or arranging for follow-up (1 vs. 1%). Patient PA and quality of life did not improve. The IS intervention was delivered with high fidelity at a low cost, but appears to be insufficient to lead to broad adoption of the CI.
Electronic supplementary material
The online version of this article (10.1007/s13142-017-0524-y) contains supplementary material, which is available to authorized users.
Keywords: Translation research, Lifestyle medicine, RE-AIM, Behavior change
INTRODUCTION
Physical inactivity is the fourth leading cause of death worldwide [1] and accounts for 6–10% of major non-communicable diseases globally [2]. In Mexico, physical inactivity estimates range from 17 to 38% [3, 4], and cardiovascular disease and diabetes represent the main causes of premature death [5]. To address the physical inactivity pandemic, effective, sustainable interventions that can be implemented at scale, regularly assessed, and embedded within existing systems are needed [6].
Physician-based physical activity promotion strategies are promising, population-wide approaches that can be implemented at a scale within existing healthcare systems [7]. Physician PA counseling, prescription, and referrals to community resources have been shown to be effective strategies [8–10], although integrating these into routine clinical practice remains a challenge. To help integrate PA counseling in primary care, it is recommended that the 5-As model [11] be applied to assess PA behavior, advise on appropriate levels of PA to achieve personally-relevant health benefits, agree on PA goals, assist with barrier identification and resolution, and arrange for follow-up and feedback on goals [12]. Yet, Mexican physicians seldom address the principles encompassed by the 5-As, mainly because they lack time and knowledge to counsel about PA [13].
Strategies to promote the implementation of evidence-based approaches, such as the 5-As, in routine clinical practice include training healthcare professionals [14] and using behavior change theories to influence physician behavior [15, 16]. Physician training implemented in the USA, Finland, and Argentina has been found to improve physician self-efficacy for PA counseling, PA referrals and prescription rates, and patients’ cardiovascular health [17–20]. Regarding behavior change models, the theory of planned behavior [21] has been found to explain PA encouragement among Dutch physicians [22], and PA prescription among Mexican primary care physicians [13]. Thus, in collaboration with the Jalisco Secretary of Health, we designed a theory-based PA counseling training intervention for primary care physicians that was integrated within an existing training platform at the Secretary and delivered using existing recourses. The objective of this study was to assess both the effectiveness of the physician training intervention (i.e., implementation strategy) and the effectiveness of PA counseling by trained physicians (i.e., clinical intervention).
METHODS
Study design and context
With a population of 7.5 million people, Jalisco is the fourth largest state in México. Eighty seven percent of the population lives in urban areas, 51% are women and the average level of education is 9 years, which is similar to national estimates [23]. Healthcare institutions from the federal Secretary of Health provide healthcare to approximately 45% of the Mexican population [24]. In Jalisco, the Secretary of Health provides healthcare services across 13 sanitary regions, which group 125 municipalities according to geographical area. Primary care physicians in Jalisco (n = 1904) are trained in general medicine and 59% are male.
We employed an effectiveness-implementation type 2 hybrid design. This design allows the blending of a clinical effectiveness trial with implementation research elements to speed the translation of research findings into routine practice [25]. At the physician level, we aimed to determine the degree to which the Secretary of Health training (described as the “implementation strategy”) could reach a broad cross section of physicians in the region; effectively increase physician adoption and implementation of the 5-As approach in the short and long term; be adopted across sanitary regions; and be implemented consistently, at a reasonable cost. At the patient level, we aimed to determine the degree to which a 5-As counseling intervention (described as the “clinical intervention”) could reach a broad cross section of the patient population; effectively increase PA in the short and long term; be adopted across physicians in the region; be implemented with high fidelity; and be sustained within regular clinical practice.
Evaluation framework
The RE-AIM framework [26–29] informed the evaluation of the implementation strategy and the clinical intervention. The framework includes the assessment of Reach (i.e., representativeness of participants), Effectiveness (i.e., intervention impact), Adoption (i.e., representativeness of settings and delivery agents), Implementation (i.e., intervention fidelity), and Maintenance (i.e., individual and organizational level long-term impact) [26]. The Reach and Effectiveness dimensions assess individual-level outcomes, while the Adoption and Implementation dimensions measure organization-level outcomes. The Maintenance dimension measures both individual- and organization-level outcomes. The measures employed to assess each RE-AIM dimension are described below.
Implementation strategy
Physician sample selection
The coordinators of the 13 sanitary regions in Jalisco were invited to schedule a training session via phone calls made by our research staff. All coordinators agreed and identified 322 primary care physicians, who had never received previous training in PA counseling, to attend the training course scheduled in their sanitary region.
Two related samples of physicians were included in the study. First, the 322 physicians attending the training course were invited to participate in the study via announcements made on site by the trainer. Those who agreed to participate completed the informed consent form and baseline questionnaire before the training started. Second, from the pool of trained physicians, 36 geographically representative physicians (i.e., three per sanitary region) were selected by convenience and agreed to participate in another portion of the study. These physicians provided access to their patients’ medical charts and participated in the testing of the prompting strategy described below. Finally, 18 physicians matched by sex/region who did not attend a regional training course were invited and agreed to participate in the study during clinic visits by research staff. These physicians acted as a comparison group in the testing of the prompting and clinical interventions described below.
Physician training intervention
The training course (i.e., implementation strategy) was focused on addressing the lack of time and knowledge barriers Jalisco primary care physicians report [13]; specifically, they were trained to provide 3–5 min of PA counseling using the 5-As model. To promote physician behavior change, the training was informed by the theory of planned behavior [21] and by proven behavior change techniques [30]. Training materials focused on improving physicians’ attitudes, perceptions of control, normative beliefs, and intentions about PA counseling. Attitudes were targeted with materials that highlighted the importance of PA in the prevention of non-communicable chronic conditions. Normative beliefs were addressed through highlighting national and international initiatives for PA promotion. Perceptions of control were addressed through role-playing and practice to increase the likelihood that the physicians would perceive PA counseling using the 5-As as easy to deliver. Each of these areas constituted one of three learning modules within the training course.
The training was a stand-alone event and lasted 3 h. It was delivered by a Secretary of Health employee with an MD and PhD degrees and expertise in PA counseling. She was a recognized PA leader in the state and her existing role in the health care infrastructure included providing training courses similar to the one used in this study. She delivered all training sessions based on a protocol encompassing three learning modules and materials. The three learning modules reinforced the international PA guidelines [31], understanding of the FITT principle (frequency, intensity, type, and time of PA necessary to improve health), and how to use the 5-As model [12]. The training courses were held from January to March 2013. The course was delivered as part of the training opportunities provided by the Jalisco Secretary of Health and did not fulfill CME requirements.
Given that patient prompting of physicians to discuss PA has demonstrated success in improving referrals to local programs [32], an additional implementation strategy included encouraging patients to prompt physicians to provide PA counseling. To test this strategy, the 36 physicians whose medical charts were being reviewed were randomly assigned to a prompted (n = 18) or unprompted condition (n = 18). Then, their patients were approached in the clinic waiting room prior to their consultation and were invited to participate. Patients of physicians randomly assigned to the prompted condition were instructed to give their physicians a card prompting them to provide PA counseling. Patients of physicians randomly assigned to the unprompted condition did not receive a card to give to their physician.
Measures
To measure Reach of the implementation strategy, the demographic characteristics of physicians participating in the training course and of those declining to participate were assessed and compared to that of the overall primary care physician population working in the Jalisco Secretary of Health. Participation rates among physicians were also calculated.
Effectiveness of the training course was assessed by examining physician adoption and implementation of the 5-As clinical intervention (described below) and physician self-reported PA counseling practices using four items from the National Family Physician Workforce Survey of Canada [33]. These items measure the frequency with which physicians (1) ask patients about their PA, (2) offer verbal advice, (3) offer written prescription, and (4) refer patients to PA resources. Answers were anchored on a 5-point scale ranging from Never to Always. An adapted version of a validated theory of planned behavior questionnaire [34] translated into Spanish and tested among Mexican primary care physicians [13] was employed to measure physician attitudes, normative beliefs, perceptions of control, and intentions (1–7-point Likert scale). The questionnaire was completed by physicians immediately before and at the end of the training session.
To assess Adoption, we compared the number of sanitary region coordinators in Jalisco (N = 13) that were offered the physician training course against the number of regions that agreed to implement it. Training Implementation was assessed by an independent observer who recorded the duration, fidelity (ratio of learning modules delivered relative to content modified/omitted from the original implementation plan), and quality (1 to 5 rating of perceived success) of each training session. Training cost was determined by calculating cost of materials used to implement the 13 training sessions and trainer salary. Maintenance of training effects was evaluated by comparing physician counseling practices and psychosocial outcomes at baseline and 3 to 6 months after the training. Further, patients answered a telephone survey asking about the PA counseling received during their previous physician appointment. This served as an indicator of the continued implementation of counseling by trained physicians in the long term (see Table 1).
Table 1.
RE-AIM evaluation indicators and corresponding measures for the implementation strategy and clinical intervention
| Implementation strategy—physician level | Data source | Time of collection |
|---|---|---|
| Reach: physician participation rate (invited/agreed), sample characteristics and representativeness compared to eligible physician population (training baseline) | Physician (n = 305) baseline questionnaire | Pre-training |
| Effectiveness: changes in physician attitudes, normative beliefs, perceived control, and intentions towards PA counseling | Physician (n = 305) end of training questionnaire | Post-training |
| Adoption: adoption rate of training course across the 13 sanitary regions | Training session direct observation | Training delivery period |
| Implementation: degree to which the three learning modules were delivered as intended, physician rating of training quality, and time and cost of training sessions | Training session direct observation | Training delivery period |
| Maintenance: changes on physician attitudes, normative beliefs, perceived control and intentions, and self-reported counseling behavior in the longer-term | Physician (n = 186) follow-up questionnaire | Three to six months after receiving the training |
| Clinical intervention—patient levela | Data source | Time of collection |
|---|---|---|
| Reach: patient participation rate (invited/agreed), sample characteristics, and representativeness compared to eligible patient population | Patient pre-consultation questionnaire (n = 687) | Before consultation |
| Effectiveness: changes in PA and quality of life within patients and between groups | Patient pre-consultation and post-consultation questionnaire (n = 687) b | Before consultation and one month after consultation |
| Adoption: degree to which the 5-As were adopted and recorded in medical charts | Pre-post training medical chart review (n = 1700) among trained physicians (n = 36) | One month before and 1 month after physician training |
| Implementation: | ||
| 1. Degree to which the 5-As were implemented after training 2. Implementation of the 5-As intervention among prompted/unprompted physicians |
1. Post-training medical chart review (n = 849) 2. Post-consultation patient survey (n = 687) |
1. One month after training 2. Right after receiving clinical intervention |
| Maintenance: | ||
| 1. Changes on patient PA and quality of life in the long term 2. Sustained implementation of the 5-As in the long term |
Patient follow-up questionnaire (n = 687)b | Six months after receiving clinical intervention (12 months after physician training) |
aThe clinical intervention was implemented 6 months after the physician training was delivered
bIntent to treat sample (n = 687) with imputation performed for patient outcomes. Reports on PA counseling received are based on intervention participants with complete data (baseline n = 456; 6 months n = 360)
Clinical intervention
Patient sample
Patients of physicians in the prompted (n = 18), unprompted (n = 18), and control (n = 18) conditions were approached while they were in the clinic waiting room to assess their eligibility and invite them to participate in the study. Eligible patients were male and female adults (> 18 years), not pregnant, not meeting PA guidelines, not involved in other PA programs, and without impediments to engage in physical activity. A power calculation (effect size = 0.10, power = 0.80, and α = 0.05) with a design effect of 1.4 used to account for clustered data indicated that a total sample of 437 patient participants was needed. Informed by previous studies [35], we expected an attrition rate of ~ 38% and aimed to recruit 700 patients with the goal of having 437 patients at follow-up. There was no randomization at the patient level as their group assignment was based on the condition assigned to their physician. Patients were given a t-shirt as a gift to thank them for participating.
Counseling intervention
Physicians assigned to the prompted and unprompted conditions were trained to offer PA counseling to patients within their scheduled consultation as described in the implementation strategy. Physicians offered PA counseling based on the 5-As model [12], which included asking patients about their PA, advising on the benefits of increasing PA based on the patient’s current behavior and recommended guidelines, providing a written prescription, collaboratively agreeing on a PA goal, assisting patients with barrier identification and resolution, and arranging follow-up using referrals to PA resources in their clinic or community.
Measures
To measure the Reach of the clinical intervention, the demographic characteristics of patients agreeing to participate and of those declining to participate were assessed and compared. Participation rates were also calculated.
The Effectiveness of the clinical intervention was determined by assessing changes in patient PA and quality of life. Godin’s Leisure-Time Exercise Questionnaire was used to assess the frequency and duration of patients’ light, moderate, and vigorous leisure-time PA over an average week [36]. The questionnaire was translated into Spanish using the back-translation method [37]. Patient quality of life was measured using the Spanish version of the health-related quality of life scale developed by the Centers for Disease Control and Prevention [38]. We employed the Healthy Days Core Module which contains four items assessing general health from poor to excellent, the number of unhealthy physical or mental days the patient had in the past month, and the number of days poor physical or mental health kept the patient from engaging in their usual activities. Patients completed this questionnaire in the clinic before receiving their corresponding intervention and over the telephone 1 and 6 months after the intervention.
To assess Adoption, 851 patient medical charts corresponding to 1 month before physician training and 849 charts corresponding to 1 month after (~ 25 for each of the 36 physicians at each time point [N = 1700]) were randomly selected and reviewed. The Secretary of Health staff reviewed the charts and recorded information using a standard abstraction form. For each chart, they recorded the presence/absence of information related to the 5-As that would typically be included in the medical record (i.e., physician asking patients about their PA, offering verbal or written advice, and referring patients to PA resources). The proportion of charts containing information on any of the 5-As, 1 month before and 1 month after training, was compared.
Physician Implementation of the 5-As was assessed via patient medical chart review and via patient questionnaire. The 1700 medical charts mentioned above were examined to determine the degree to which each of the 5-As was implemented. Six months after physicians received the training, patients in the clinical intervention were asked if their physician asked them about their PA levels, explained the benefits of PA, helped them set PA goals, provided a verbal or written prescription, or referred them to a program or community resource (Yes = 1, No = 0). For Maintenance, patient PA and quality of life were assessed 6 months after receiving the PA counseling intervention and compared against those of patients in the comparison group (see Table 1).
Data analyses
Descriptive statistics were used to examine physician and patient demographic characteristics at baseline. Wilcoxon’s signed test for paired samples was used to assess pre-post training changes in physicians’ psychosocial outcomes (attitudes, normative beliefs, perceptions of control, and intentions) and PA counseling practices (ask, advice, and refer). To assess pre-post intervention changes in patient PA and quality of life, a mixed (time × group) ANOVA was conducted. Patient data analyses were conducted on an intent to treat basis. Missing patient data were imputed using the fully conditional specification method with values estimated using linear regressions [39]. Finally, chi-square tests were conducted to assess pre-post training changes in 5-As implementation as recorded in medical charts. Statistical significance was set at α = .05 and the Bonferroni correction method was employed when multiple comparisons were made. The analyses were conducted using the Statistical Package for Social Sciences version 22 for Windows 7.
RESULTS
Implementation strategy
Training reach and effectiveness
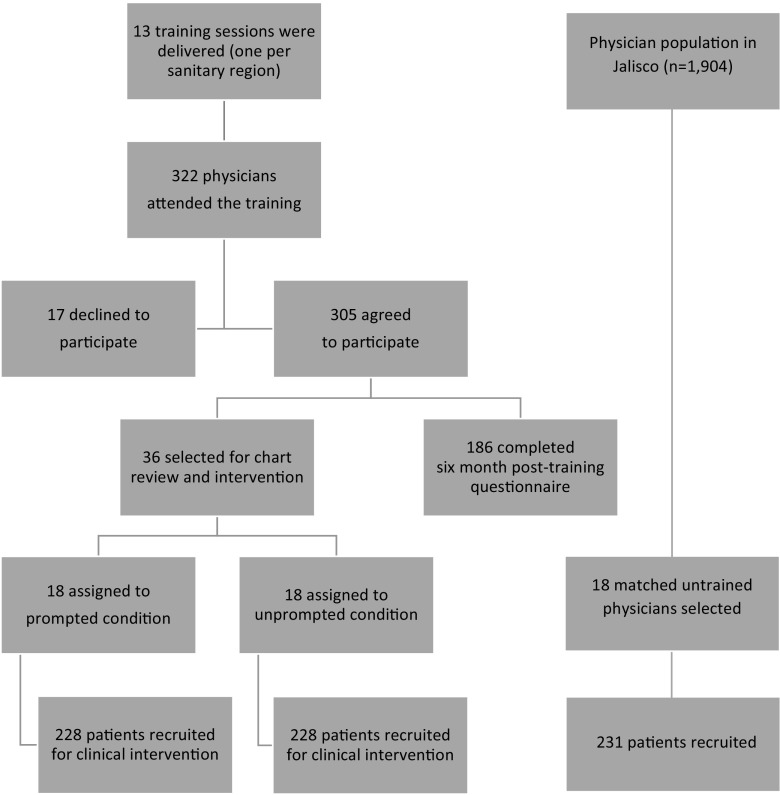
From the 322 physicians attending the training course, 305 from 119 municipalities representing the 13 sanitary regions agreed to participate in the study (Fig. 1). Most of the physicians in this study had a general medicine specialty (92%) and were located in rural clinics (54%), but female physicians (52%) were slightly overrepresented. Physicians who declined participation (n = 17) were mostly males (59%) from urban clinics (65%).
Fig. 1.
Physician and patient enrollment flow
Based on group medians and the effect size measure for Wilcoxon’s signed test (r), significant improvements in physician attitudes (r = .36, p < .05), normative beliefs (r = .46, p < .05), perceptions of control (r = .34, p < .05), and intentions (r = .26, p < .05) toward PA counseling from immediately before to immediately after the training were observed (Table 2).
Table 2.
Changes in physician outcome variables from baseline to post training and at 3–6 months after the training
| Variable | Baseline n = 305 | Post-training n = 305 | 3–6 months n = 186 | Effect size |
|---|---|---|---|---|
| Demographics | ||||
| Age (mean ± SD) | 40 ± 11 | |||
| Women | 52% | |||
| Rural | 54% | |||
| General medicine specialty | 92% | |||
| Years of practice (mean ± SD) | 13 ± 9 | |||
| Psychosociala constructs (median ± IQR) | ||||
| Attitude | 7.0 ± 0.1 | 7.0 ± 0* | 7.0 ± 0 | r = .36 |
| Normative beliefs | 6.0 ± 1.7 | 6.7 ± 1.2* | 6.3 ± 1.7 | r = .46 |
| Perceived behavioral control | 5.4 ± 1.6 | 5.8 ± 1.8* | 5.6 ± 1.6 | r = .34 |
| Intention | 6.8 ± 1.0 | 6.8 ± 0.4* | 6.8 ± 1.0 | r = .26 |
| Counselingb behavior (mean ± SD) | ||||
| Ask about PA | 4.3 ± 0.7 | 4.4 ± 0.6* | NS | |
| Provide PA verbal advice | 3.9 ± 0.9 | 4.3 ± 0.9* | d = .44 | |
| Provide PA written prescription | 2.3 ± 1.1 | Not measured | 3.0 ± 1.2* | d = .61 |
| Refer patients | 2.1 ± 1.2 | 2.8 ± 1.2* | d = .58 | |
These are data from the physician questionnaire administered before, at the end of the training, and 3–6 months after
NS not significant, PA physical activity, SD standard deviation, IQR inter quartile range, r effect size measure for Wilcoxon’s signed-rank test, d Coneh’s d effect size measure
*Significantly different from baseline at p < .001
aMeasured on a 7-point scale ranging from 1 = Low to 7 = High
bMeasured on a 5-point scale ranging from 1 = Never to 5 = Always
Training adoption and implementation
Thirteen training sessions (one per sanitary region) were delivered resulting in a 100% adoption rate by regions. Similarly, each of the three learning modules was implemented across all 13 trainings indicating a high level of adherence to the training protocol. The duration of each training session varied, ranging from 30 to 247 min (mean 170 ± 54 min). The cost per training session, excluding trainer travel/time costs and salary of the participating physicians, was $429 Mexican pesos (~ US$20), representing $150 for printed materials and $279 for 3 h of trainer salary. This translates into approximately $20 Mexican pesos (US$1) per physician trained. The quality of the training reported by the observer was good or excellent in 54 and 46% of the sessions, respectively, and 100% of the sessions were qualified as successful.
Maintenance of training effects
For the maintenance assessment, 40% of physicians were lost at follow-up because they did not receive the online/printed questionnaire or because they were no longer working at the Secretary of Health. Physicians with complete data were not different in demographic or outcome measures from physicians lost at follow-up (see supplementary material). Among physicians with complete data (N = 186, 61%), post-training improvements in psychosocial variables were not maintained 3–6 months after the training (Table 2). Paired-sample t tests showed significant improvements in all physician PA counseling practices with a medium-to-large effect size observed, except in asking patients about their PA (p < .001).
Clinical intervention
Counseling reach and effectiveness
For the clinical intervention, 730 patients were approached in the clinic waiting room and screened for eligibility (Fig. 1). Of these, 43 were not eligible because they were already physically active (n = 13), they had no telephone for contact (n = 10), they were pregnant (n = 7), they had impediments to engage in PA (n = 5), or they had another reason (n = 8). The remaining 687 eligible patients (77% female; M age = 48.5 years) agreed to participate in the study. About 55% of the patients were married; 49% had some or completed elementary school; and 41% had some or completed high school or above. Patients in the three study conditions (i.e., prompted, unprompted, control) were similar across demographic variables and outcome variables at baseline (Table 3).
Table 3.
Patient baseline characteristics and outcomes at 1 and 6 months by study group (N = 687a)
| Variable | Prompted group (n = 228) | Unprompted group (n = 228) | Control group (n = 231) |
|---|---|---|---|
| Demographics | |||
| Age (mean ± SD) | 51.6 ± 16 | 48.3 ± 16 | 45.9 ± 16 |
| Women (n (%)) | 173 (76) | 180 (79) | 176 (76) |
| Married (n (%)) | 127 (56) | 136 (60) | 115 (50) |
| Some/complete elementary school | 101 (53) | 114 (50) | 99 (43) |
| Some/complete high school or above | 82 (36) | 90 (40) | 113 (49) |
| PA score (mean ± SD)b | |||
| Baseline | 20.9 ± 15 | 21.6 ± 16 | 24.4 ± 19 |
| One month | 27.5 ± 25 | 29.4 ± 23 | 28.9 ± 24 |
| Six months | 26.9 ± 22 | 28.7 ± 22 | 28.7 ± 23 |
| Physically active (n (%))c | |||
| Baseline | 45 (20) | 32 (14) | 32 (14) |
| One month | 65 (28) | 46 (20) | 50 (22) |
| Six months | 67 (29) | 57 (25) | 58 (25) |
| Number of unhealthy days (mean ± SD) | |||
| Baseline | 15.9 ± 13 | 16.5 ± 13 | 14.7 ± 12 |
| One month | 15.9 ± 13 | 16.5 ± 13 | 14.7 ± 12 |
| Six months | 14.3 ± 12 | 14.8 ± 13 | 12.9 ± 12 |
aFrom these 687 patients, only 475 patients had complete follow-up data. Missing data were imputed to conduct analysis on an intent-to-treat basis
bThe PA score was obtained by multiplying the weekly frequencies of light, moderate, and vigorous PA by their metabolic equivalent values of 9, 5, and 3, respectively, and adding them up
c Patients were classified as physically active or inactive based on the sum of their vigorous and moderate PA scores (active ≥ 24 points or inactive ≤ 23 points)
Of the 687 patients enrolled, 475 completed all study questionnaires. Missing data were imputed and all 687 patients were included in the analyses. A t test comparing imputed outcome variables with original outcome variables (containing missing data) showed these were not different. In analyses of intervention effectiveness, we found no evidence that the clinical intervention was successful in the short (1 month) or long term (6 months). Although patients in all groups increased their PA scores and decreased the number of unhealthy days from baseline to 1 and 6 months after the intervention, these changes were not different between groups (Table 3).
Counseling adoption, implementation, and sustained delivery
In terms of adoption of the clinical intervention by trained physicians, the proportion of patient medical charts including any of the 5-As increased from 1 month pre-training to 1 month post-training (43 vs. 52%, respectively, p < .01). Likewise, the implementation of Assess (43 vs. 52%, p < .01), Advise (25 vs. 39%, p < .01), and Assist (7 vs. 15%, p < .01) improved from 1 month before to 1 month after the training. However, the implementation of the As focused on goal setting (Agree; 13 vs. 17%) and follow-up (Arrange; 1 vs. 1%) did not significantly improve (Table 4). On average, physicians completed 32% of the 5-As with patients that visited the clinic post-training.
Table 4.
Use of 5-As as recorded in medical charts of trained physicians (n = 36) 1 month before and 1 month after training
| Pre-training n = 851 | Post-training n = 849 | |
|---|---|---|
| Proportion of files containing | n (%) | n (%) |
| 0 As | 484 (57) | 405 (48) |
| 1 As | 135 (16) | 112 (13) |
| 2 As | 113 (13) | 158 (19) |
| 3 As | 78 (9) | 87 (10) |
| 4 As | 41 (5) | 84 (10) |
| 5 As | 0 | 1 (0.1) |
| Overall implementation of each A | ||
| Assess patient PA | 366 (43) | 441 (52)* |
| Advice to increase PA | 213 (25) | 331 (39)* |
| Assist to set goals | 60 (7) | 127 (15)* |
| Agree on a plan | 111 (13) | 144 (17) |
| Arrange referral and follow-up | 5 (1) | 6 (1) |
PA physical activity
*Significantly different from baseline at p < .01 in chi-square tests
When comparing intervention implementation between prompted (n = 18) and unprompted (n = 18) physicians, more prompted physicians implemented the 5-As. More patients assigned to the prompted group (n = 228) than to the unprompted group (n = 228), reported that their physician asked about their PA (93 vs. 75%, p < .001), advised about PA benefits (92 vs. 75%, p < .001), assisted them in setting goals (84 vs. 63%, p < .001), provided a prescription (75 vs. 65%, p < .001), and referred them to a PA resource (32 vs. 19%, p > .05). The proportion of patients in the control group reporting that their physician asked about their PA (63%), advised on the PA benefits (65%), assisted them in setting goals (54%), and provided a prescription (53%) was significantly lower than in the intervention groups (p < .05). The proportion of patients reporting that their physician referred them to a PA resource (21%) was not different between groups.
The proportion of prompted and unprompted physicians implementing the 5-As to counsel on PA decreased over time. Of the intervention patients completing the 6-month follow-up questionnaire (prompted n = 174, unprompted n = 186), 50% reported that their physician assessed their PA, provided advice on PA benefits, and assisted them in setting goals. Finally, 50% of patients in both intervention groups reported being referred to a community PA resource by their physician at follow up, which was higher than referral reports during the intervention period.
DISCUSSION
We aimed to determine the degree to which a PA counseling training course reached Jalisco primary care physicians, effectively changed their counseling behavior, and improved patient PA behavior through the use of the 5-As. Overall, the training course was successfully adopted and implemented across the 13 Jalisco sanitary regions, costing around $20 Mexican pesos (~ US$1) per physician trained. The training promoted physician adoption of the 5-As model and implementation of three of the As; Assess, Advise, and Assist. The use of Agree and Arrange were seldom completed. Patient PA and quality of life did not improve in response to the physician counseling intervention.
To our knowledge, this is the first effectiveness-implementation hybrid study conducted in Mexican primary care clinics. This study supports the external validity and effectiveness of a training intervention directed at primary care physicians in México. All state regions were invited to host a training course and all did so, underscoring the importance of having state level support to promote compliance. The training intervention was consistently implemented across regions, while allowing duration adaptations, and for a low cost. In line with previous findings [18, 19], this theory-based training course achieved encouraging improvements in physician perceived control and intention to counsel, and ultimately, in some counseling behaviors. Overall, our findings suggest that this training course is low-cost, feasible, and promising strategy for preparing physicians to counsel their patients about PA.
Physician training, however, did not fully translate into clinical practice changes. While the patient medical chart review showed that the 5-As were partially adopted after the training, implementation of each A remained relatively low. Similar to findings from direct observation of physician counseling [40], we found that assessing and verbally advising patients were the most commonly employed strategies, while agreeing, assisting, and arranging were seldom completed. Specifically, the use of Agree and Assist, which are critical for promoting goal setting and problem solving, were completed in less than one of five patients. Arranging for follow-up, which is critical for promoting accountability, was completed in about one of every 100 patients. This may be related to the fact that Mexican physicians are typically trained to provide information or direction, rather than to establish a collaborative relationship with patients, which may hinder the use of collaborative As. Our findings suggest that a comprehensive and sustained implementation of the 5-As in Mexican primary care settings may require additional intervention support at the physician and clinic levels to allow for the 5-As to be completed. Using a team approach that benefits from the credibility of physician prescriptions but engages other clinical staff to complete the goal setting, problem solving, and follow-up activities might improve implementation and delivery of the 5-As [12].
Our physician counseling intervention did not result in patient PA improvements, echoing conclusions that physician advice is not sufficient to promote patient behavior change [41]. Other studies have found positive effects on patient PA by employing collaborative approaches where physicians provide Advice to patients and Arrange referrals to PA experts who then deliver the collaborative As [42]. The collaborative As (Agree, Assist, and Arrange) were seldom completed in our study, suggesting patients did not receive support to set a PA goal, make plans to overcome barriers to attain their goal, nor be accountable for, or receive feedback on their behavior change. Our findings suggest that patients need more than assessment and advice from their physician to engage in health enhancing PA. Helping patients adhere to a PA prescription, improve their PA, and maintain this change long-term, remain a challenge for practitioners and researchers.
The physician training and 5-As PA counseling interventions we tested represent a first step to guide pragmatic, population-wide PA promotion efforts in Mexico. This study also highlights the need for multi-level, comprehensive strategies to affect population-wide PA change. For instance, patient-level strategies (e.g., prompting physicians) [32], physician-level strategies (e.g., audit and feedback), and clinic-level strategies (e.g., integrating PA assessment in medical records) [43] may be needed to facilitate comprehensive and continued delivery of the 5-As. Further, it may be necessary to establish referral systems where patients are referred to PA resources or experts in the community to complete the collaborative As (Assist and Arrange) [42]. Finally, creating clinic-community linkages to connect patients with PA opportunities, programs, recreational spaces, and active transportation infrastructure available in their communities must be developed or improved [44].
The present findings should be interpreted in light of the following limitations. First, the study design employed prevents us from comparing the training course with other approaches or with no training at all. Second, PA counseling practices were measured using a self-report tool, which are prone to social desirability and may result in overestimation of intervention effects. Similarly, patient PA was measured by self-report which may overestimate patient behavior. The training quality measure employed was based on a single trained observer; as such, it does not capture perceived success from the perspective of attending physicians. Our cost estimate of the training intervention is an underestimate as it excluded physician salaried time and trainer travel costs. Finally, the present findings are only representative of the physician and patient populations from the Secretary of Health in Jalisco, limiting generalizability of findings to patients/physicians in other healthcare systems in the country.
CONCLUSION
This was the first effectiveness-implementation hybrid study focused on introducing PA counseling within routine primary care practice in Mexico through an academic-government partnership. A theory-based, 3-h physician training was a low-cost, feasible, and promising strategy for preparing physicians to counsel for PA using the 5-As model. Physician counseling did not seem to have an impact on patient PA or quality of life. Because physician implementation across the 5-As remained relatively low and decreased over time, additional physician- and clinic-level strategies may be needed to fully implement physician counseling that translates into enhanced-patient PA. In light of the public health issues Mexico is facing, promoting population-wide PA is imperative and will require comprehensive strategies collaboratively implemented by providers, researchers, communities, and healthcare systems.
Electronic supplementary material
(DOCX 13.4 kb)
Acknowledgments
This study was part of the Pausa Laboral Project, a collaboration among researchers from Queen’s University, the University of Guadalajara, Arizona State University, Emory University, the University of Nebraska Medical Center, the Metropolitan Autonomous University, and the Jalisco Secretary of Health. We thank the Jalisco Secretary of Health for providing support and access to conduct this study. We also thank the physicians and patients from the Jalisco Secretary of Health who participated in this study. Finally, we thank the dietitians and physical activity experts who helped with data collection (in alphabetical order): María Bueno Rea, Claudia Brizuela Rosas, Karla Castellanos Díaz, Karen Cortez García, José de Jesús Contreras, Guillermo Cuevas Aguilar, Ricardo Echauri Baltazar, Sandra Espinolla Magallón, Silvia García González, Raúl García Robles, José Gómez Gamboa, Mara Guzmán Gómez, Dorian Lizandro Velazco, Mauricio Madrid Hernández, Carolina Márquez Muñoz, Gloria Montes López, Liliana Muñoz Moreno, Yareli Orozco Loyola, Denise Ivette Páez, Viviana Pérez Bernal, Mercedes Robles Ramos, José Luis Saavedra Gómez, Fabiola Sánchez Rodríguez, Isabel Tovar, Gibran Urbano, and Carmen Villalvazo Reina.
Funding information
This work was conducted with the financial support of a grant (CIHR GIR 127075) from the Canadian Institutes of Health Research (CIHR), Institute of Population and Public Health, the CIHR Institute of Cancer Research and the Public Health Agency of Canada–—Chronic Disease Prevention Branch.
Compliance with ethical standards
Conflict of interest
The other authors declare that they have no financial or other conflict of interests. Edtna Jauregui works for the Jalisco Secretary of Health and receives salary from that institution.
Footnotes
Implications
Practice: These findings can have an impact on researchers by providing evidence of how an effectiveness-implementation hybrid study design can be used to blend clinical effectiveness trial and implementation research elements to speed the translation of research findings into routine practice.
Policy: These findings can have an impact on practitioners by informing their physical activity promotion practices and describing an evidence-based tool they can use in their practice.
Research: These findings can have an impact on policy makers by informing current physician training strategies the Secretary of Health in Jalisco is implementing.
Electronic supplementary material
The online version of this article (10.1007/s13142-017-0524-y) contains supplementary material, which is available to authorized users.
Contributor Information
Karla I. Galaviz, Email: kgalavi@emory.edu
Paul A. Estabrooks, Email: paul.estabrooks@unmc.edu
Edtna Jauregui Ulloa, Email: edtna.jauregui@hotmail.com.
Rebecca E. Lee, Email: RELeePhD@yahoo.com
Ian Janssen, Email: ian.janssen@queensu.ca.
Juan López y Taylor, Email: taylor@cucs.udg.mx.
Luis Ortiz-Hernández, Email: lortiz@correo.xoc.uam.mx.
Lucie Lévesque, Phone: 613-533-6000, Email: levesqul@queensu.ca.
References
- 1.World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. 2009. Available at http://www.Who.Int/healthinfo/global_burden_disease/globalhealthrisks_report_full.Pdf. Accessed 9 Sept 2017.
- 2.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;280(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 4.Gutiérrez JP, Rivera-Dommarco J, Shamah-Levy T, Villalpando-Hernández S, Franco A, Cuevas-Nasu L, et al. Encuesta nacional de salud y nutrición Resultados nacionales. Cuernavaca, méxico: Instituto nacional de salud pública; 2012. [Google Scholar]
- 5.Global burden of disease collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015; 385(9963):117–71. [DOI] [PMC free article] [PubMed]
- 6.Reis RS, Salvo D, Ogilvie D, Lambert EV, Goenka S, Brownson RC. Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. Lancet. 2016;388(10051):1337–1348. doi: 10.1016/S0140-6736(16)30728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care system. Mayo Clin Proc. 2013;88(12):1446–1461. doi: 10.1016/j.mayocp.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Garrett S, Elley CR, Rose SB, O'Dea D, Lawton BA, Dowell AC. Are physical activity interventions in primary care and the community cost-effective? A systematic review of the evidence. Br J Gen Pract. 2011;61(584):e125–e133. doi: 10.3399/bjgp11X561249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orrow G, Kinmonth A-L, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012; 344:e1389–9. [DOI] [PMC free article] [PubMed]
- 10.Sanchez A, Bully P, Martinez C, Grandes G. Effectiveness of physical activity promotion interventions in primary care: a review of reviews. Prev Med. 2015;76:S56–S67. doi: 10.1016/j.ypmed.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: a evidence-based approach. Am J Prev Med. 2002;22(4):267–284. doi: 10.1016/S0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 12.Estabrooks P, Glasgow R, Dzewaltowski D. Physical activity promotion through primary care. J Am Med Assoc. 2003;289(22):2913–2916. doi: 10.1001/jama.289.22.2913. [DOI] [PubMed] [Google Scholar]
- 13.Galaviz KI, Jauregui E, Fabrigar L, Latimer-Cheung A, Lopez y Taylor J, Lévesque L. Physical activity prescription among Mexican physicians: a structural equation model testing the theory of planned behavior. Int J Clin Pract. 2015;69(3):375–383. doi: 10.1111/ijcp.12546. [DOI] [PubMed] [Google Scholar]
- 14.Scott S, Albrecht L, O'Leary K, Ball G, Hartling L, Hofmeyer A, et al. Systematic review of knowledge translation strategies in the allied health professions. Implement Sci. 2012;7(1):70. doi: 10.1186/1748-5908-7-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Godin G, Belanger-Gravel A, Eccles M, Grimshaw J. Healthcare professionals’ intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci. 2008;3(1):36. doi: 10.1186/1748-5908-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perkins MB, Jensen PS, Jaccard J, Gollwitzer P, Oettingen G, Pappadopulos E, et al. Applying theory-driven approaches to understanding and modifying clinicians’ behavior: what do we know? Psychiatr Serv. 2007;58(3):342–348. doi: 10.1176/ps.2007.58.3.342. [DOI] [PubMed] [Google Scholar]
- 17.Zilberman J, Cicco L, Woronko E, Vainstein N, Sczcygiel V, Ghigi R, et al. Cardiovascular risk factors. A multicenter uncontrolled follow-up study. Argentine J Cardiol. 2012;80(2):130–136. [Google Scholar]
- 18.Eckstrom E, Hickam D, Lessler D, Buchner D. Changing physician practice of physical activity counseling. J Gen Intern Med. 1999;14(6):376–378. doi: 10.1046/j.1525-1497.1999.00356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marcus BH, Goldstein MG, Jette A, Simkin-Silverman L, Pinto BM, Milan F, et al. Training physicians to conduct physical activity counseling. Prev Med. 1997;26(3):382–388. doi: 10.1006/pmed.1997.0158. [DOI] [PubMed] [Google Scholar]
- 20.Aittasalo M, Miilunpalo S, Ståhl T, Kukkonen-Harjula K. From innovation to practice: initiation, implementation and evaluation of a physician-based physical activity promotion programme in Finland. Health Promot Int. 2007;22(1):19–27. doi: 10.1093/heapro/dal040. [DOI] [PubMed] [Google Scholar]
- 21.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 22.Sassen B, Kok G, Vanhees L. Predictors of healthcare professionals’ intention and behaviour to encourage physical activity in patients with cardiovascular risk factors. BMC Public Health. 2011;11:246. doi: 10.1186/1471-2458-11-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Instituto Nacional de Estadística y Geografía (INEGI). Censo de poblacion y vivienda 2010. Available at http://www.beta.inegi.org.mx/proyectos/ccpv/2010/. Accessed 9 Sept 2017.
- 24.Frenk J, Gomez O, Knaul FM. The democratization of health in Mexico: financial innovations for universal coverage. Bull World Health Organ. 2009;87:542–548. doi: 10.2471/BLT.08.053199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–226. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the re-aim framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Estabrooks PA, Gyurcsik NC. Evaluating the impact of behavioral interventions that target physical activity: issues of generalizability and public health. Psychol Sport Exerc. 2003;4(1):41–55. doi: 10.1016/S1469-0292(02)00016-X. [DOI] [Google Scholar]
- 28.Antikainen I, Ellis R. A re-aim evaluation of theory-based physical activity interventions. J Sport Exerc Psychol. 2011;33(2):198–214. doi: 10.1123/jsep.33.2.198. [DOI] [PubMed] [Google Scholar]
- 29.Galaviz KI, Harden SM, Smith E, Blackman KCA, Berrey LM, Mama SK, et al. Physical activity promotion in Latin American populations: a systematic review on issues of internal and external validity. Int J Behav Nutr Phys Act. 2014; 11:77–7. [DOI] [PMC free article] [PubMed]
- 30.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization. Global recommendations on physical activity for health. 2010. Avalialbe at http://www.Who.Int/dietphysicalactivity/factsheet_recommendations/en/. Accessed 9 Sept 2017. [PubMed]
- 32.Almeida FA, Smith-Ray RL, Van Den Berg R, Schriener P, Gonzales M, Onda P, et al. Utilizing a simple stimulus control strategy to increase physician referrals for physical activity promotion. J Sport Exerc Psychol. 2005;27:505–514. doi: 10.1123/jsep.27.4.505. [DOI] [Google Scholar]
- 33.Petrella RJ, Lattanzio CN, Overend TJ. Physical activity counseling and prescription among Canadian primary care physicians. Arch Intern Med. 2007;167(16):1774–1781. doi: 10.1001/archinte.167.16.1774. [DOI] [PubMed] [Google Scholar]
- 34.Ramsay C, Thomas R, Croal B, Grimshaw J, Eccles M. Using the theory of planned behaviour as a process evaluation tool in randomised trials of knowledge translation strategies: a case study from UK primary care. Implement Sci. 2010;5(1):71. doi: 10.1186/1748-5908-5-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carroll JK, Yancey AK, Spring B, Figueroa-Moseley C, Mohr DC, Mustian KM, et al. What are successful recruitment and retention strategies for underserved populations? Examining physical activity interventions in primary care and community settings. Transl Behav Med. 2011;1(2):234–251. doi: 10.1007/s13142-011-0034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–146. [PubMed] [Google Scholar]
- 37.Brislin R. Back-translation for cross-cultural research. J Cross-Cult Psychol. 1970;1(3):185–216. doi: 10.1177/135910457000100301. [DOI] [Google Scholar]
- 38.Horner-Johnson W, Krahn G, Andresen E, Hall T, Rehabilitation R, M Training Center Expert Panel on Health Status Developing summary scores of health-related quality of life for a population-based survey. Public Health Rep. 2009;124(1):103–110. doi: 10.1177/003335490912400113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee KJ, Carlin JB. Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol. 2010;171(5):624–632. doi: 10.1093/aje/kwp425. [DOI] [PubMed] [Google Scholar]
- 40.Carroll JK, Antognoli E, Flocke SA. Evaluation of physical activity counseling in primary care using direct observation of the 5As. Ann Fam Med. 2011;9(5):416–422. doi: 10.1370/afm.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hillsdon M, Thorogood M, White I, Foster C. Advising people to take more exercise is ineffective: a randomized controlled trial of physical activity promotion in primary care. Int J Epidemiol. 2002;31(4):808–815. doi: 10.1093/ije/31.4.808. [DOI] [PubMed] [Google Scholar]
- 42.Fortier M, Hogg W, O’Sullivan T, Blanchard C, Sigal R, Reid R, et al. Impact of integrating a physical activity counsellor into the primary health care team: Physical activity and health outcomes of the physical activity counselling randomized controlled trial. Appl Physiol Nutr Metab. 2011;36(4):503–514. doi: 10.1139/h11-040. [DOI] [PubMed] [Google Scholar]
- 43.Coleman KJ, Ngor E, Reynolds K, Quinn VP, Koebnick C, Young DR, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44(11):2071–2076. doi: 10.1249/MSS.0b013e3182630ec1. [DOI] [PubMed] [Google Scholar]
- 44.Patrick K, Pratt M, Sallis RE. The healthcare sector’s role in the U.S. national physical activity plan. J Phys Act Health. 2009;6(2):S211–S219. doi: 10.1123/jpah.6.s2.s211. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 13.4 kb)