Abstract
Ageing can occur at different rates, but what controls this variable rate is unknown. Here I have developed a hypothesis that vitamin D may act to control the rate of ageing. The basis of this hypothesis emerged from studyng the various cellular processes that control ageing. These processes such as autophagy, mitochondrial dysfunction, inflammation, oxidative stress, epigenetic changes, DNA disorders and alterations in Ca2+ and reactive oxygen species (ROS) signalling are all known to be regulated by vitamin D. The activity of these processes will be enhanced in individuals that are deficient in vitamin D. Not only will this increase the rate of ageing, but it will also increase the probability of developing age‐related diseases such as Alzheimer's disease, Parkinson's disease, multiple sclerosis and cardiovascular disease. In individual with normal vitamin D levels, these ageing‐related processes will occur at lower rates resulting in a reduced rate of ageing and enhanced protection against these age‐related diseases.
![]()
Keywords: autophagy, mitochondrial dysfunction, inflammation, oxidative stress, epigenetics, DNA disorders, calcium, reactive oxygen species (ROS), Vitamin D
Introduction
One of the interesting aspects of ageing is that it can occur at different rates (Grabowska et al. 2017). As part of the hypothesis developed here, it is proposed that those individuals that age slowly live a lot longer and have a healthy old age in that they tend not to develop age‐related diseases. On the other hand, those that age faster do not survive so long and are likley to develop the age‐related diseases such as Alzheimer's disease, Parkinson's disease and cardiovascular disease. Perhaps the best example of how the rate of ageing can vary is the increased ageing that occurs in Hutchinson–Gilford progeria syndrome (HGPS). This premature ageing disorder, which is caused by a mutation in the LMNA gene, greatly accelerates the rate of ageing such that young children become old during their teenage years and do not survive much beyond 20 years (Burtner & Kennedy, 2010; Gonzalo et al. 2017). It is of interest that vitamin D supplementation can slow the increased rate of ageing that occurs during HGPS (Kreienkamp et al. 2016).
In order to understand how ageing can occur at different rates, it is necessary to understand what controls the ageing process. There is increasing evidence that ageing is not a single process in that it seems to be driven by a number of cellular processes such as autophagy, mitochondrial dysfunction, inflammation, oxidative stress, epigenetic changes, DNA disorders, and alterations in Ca2+ and reactive oxygen species (ROS) signalling (Ding & Shen, 2008; López‐Otín et al. 2013; Aunan et al. 2016; Seals et al. 2016; Jylhävä et al. 2017). What is remarkable about all of these cellular ageing processes is that their activity is regulated by vitamin D (Fig. 1). This protective function of vitamin D in ageing is markedly enhanced by its ability to control the expression of Nrf2 (Nakai et al. 2014) and the anti‐ageing protein Klotho (Forster et al. 2011), which are also important regulators of multiple cellular signalling systems including the formation of antioxidants. Nrf2 plays a major role in protecting cells against oxidative stress (Lewis et al. 2010). Defects in the Klotho gene induces the premature‐ageing syndrome in mice (Kuro‐o, 2009).
Figure 1. The vitamin D hypothesis of ageing.
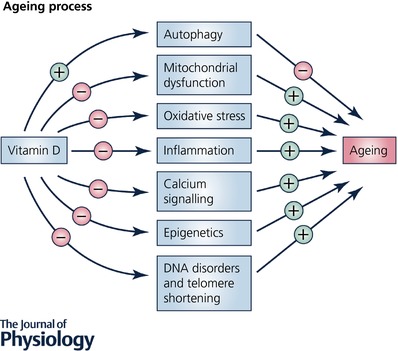
It is proposed that vitamin D acts to regulate ageing by controlling the activity of a number of the ageing processes. Vitamin D promotes the activity of autophagy, which acts to slow down the ageing processes by removing dysfunctional mitochondria. Vitamin D also acts to reduce mitochondrial dysfunction, oxidative stress, inflammation, calcium signalling, epigenetics and DNA disorders including telomere shortening, which act to drive the processes of ageing.
On the basis of this information, I shall develop a hypothesis that this vitamin D–Klotho–Nrf2 signalling network is a key regulator of the rate of ageing. When vitamin D levels are normal, these processes will operate to drive healthy ageing that occurs at a slow rate (Tuohimaa, 2009; Haussler et al. 2010). However, when vitamin D is deficient these ageing processes will be enhanced and this will result in an increase in the rate of ageing. An example of how the rate of ageing can vary is the observation that the onset of menopause in women, who have lower levels of vitamin D than men (Looker et al. 2011), is enhanced by vitamin D deficiency (Purdue‐Smithe et al. 2017), i.e., menopause occurs earlier in those women that are deficient in vitamin D. There is also considerable evidence to indicate that vitamin D deficiency is related to mortality (Schöttker et al. 2013; Gaksch et al. 2017; Ordóñez‐Mena et al. 2017). A decrease in vitamin D activity has been linked to premature ageing in mice (Keisala et al. 2009). In addition, an increase in the activity of these ageing processes during vitamin D deficiency may also set the stage for the onset of many of the age‐related disorders such as a decline in cognition, depression, osteoporosis, hypertension and cardiovascular disease, diabetes, cancer, muscle weakness, and Alzheimer's disease (Zittermann, 2003; Annweiler et al. 2010; Pittas & Dawson‐Hughes, 2010; Meehan & Penckofer, 2014; Banerjee et al. 2015; Berridge, 2015b, 2016; Costantino et al. 2016; Dawson‐Hughes, 2017; Wang et al. 2017). In the case of cancer, polymorphisms of the vitamin D receptor (VDR) have been linked to the onset of prostate cancer (Liu et al. 2017). The fact that the ability of the skin to make vitamin D declines as ageing progresses is one reason why cognition tends to decline during ageing (MacLaughlin & Holick, 1985; Kennel et al. 2010; Grady, 2012). In order to develop this hypothesis that the rate of ageing is regulated by vitamin D, I will describe the role of these different ageing processes and how vitamin D carries out its regulatory activity.
Autophagy and ageing
There is increasing evidence that autophagy plays a key role in maintaining healthy ageing (Rubinsztein et al. 2011; Madeo et al. 2015; Plaza‐Zabala et al. 2017). In those families that have extended longevity, the process of autophagy is better maintained (Raz et al. 2017). Autophagy is an essential process in that it maintains healthy cells by removing damaged proteins and malfunctioning organelles, especially the mitochondria (Hubbard et al. 2012; Fivenson et al. 2017; Palikaras et al. 2017). As mitochondria age, there is a decline in their ability to generate ATP and they begin to generate large amounts of reactive oxygen species (ROS). Such an increase in oxidative stress is one of the processes that enhances ageing (Fig. 1; Terman et al. 2007; Salminen et al. 2012; Ureshino et al. 2014). Therefore, to reduce ageing it is essential that these damaged mitochondria are removed by autophagy. It is essential, therefore, that the process of autophagy is maintained and there is evidence that it may decline when ageing is occurring at a fast rate.
The autophagy process is regulated by changes in the level of Ca2+ (Høyer‐Hansen et al. 2007; Decuypere et al. 2011b; La Rovere et al. 2016; Sun et al. 2016; Luyten et al. 2017) and by increases in the levels of ROS (Navarro‐Yepes et al. 2014). The action of Ca2+ is complicated because it exerts a dual action on autophagy. For example, an increase in the level of Ca2+, especially following the activation of inositol trisphosphate receptors (InsP3Rs), acts to inhibit autophagy (Criollo et al. 2007). On the other hand, a reduction in the level of Ca2+ also enhances autophagy. It has been proposed that the nature of the cellular state may determine how this dual action of Ca2+ occurs (Decuypere et al. 2011b).
There is now growing evidence that vitamin D plays an important role in maintaining autophagy (Fig. 1; Yuk et al. 2009; Høyer‐Hansen et al. 2010; Verway et al. 2010; Wu & Sun, 2011; Jang et al. 2014; Uberti et al. 2014; Wang et al. 2016; Chirumbolo et al. 2017; Mushegian, 2017; Tavera‐Mendoza et al. 2017; Wei et al. 2017). It is possible that vitamin D will act to promote autophagy by regulating the level of Ca2+ through its ability to promote the expression of Ca2+ pumps and Ca2+ buffers as will be described in a later section. By maintaining autophagy, vitamin D will reduce the ageing process by ensuring that the mitochondria do not generate excessive amounts of ROS, which have been implicated in ageing as described below.
Inflammation and ageing
Inflammation has been implicated in the process of ageing (Cevenini et al. 2010, 2013; Salminen et al. 2012; López‐Otín et al. 2013; Petersen & Smith, 2016; Di Benedetto et al. 2017). Damaged mitochondria may play a role in initiating this increase in inflammation (Green et al. 2011). These dysfunctional mitochondria are the result of a decline in autophagy that acts normally to remove such damaged mitochondria as described above (Salminen et al. 2012).
One of the important actions of vitamin D is to reduce inflammation (Fig. 1; Garcion et al. 1999; Hewison, 2010; Sundar & Rahman, 2011; Briones & Darwish 2012; Berk et al. 2013; Alvarez et al. 2014; Lucas et al. 2014; Wang et al. 2014). One way it does this is to reduce the expression of inflammatory cytokines (d'Hellencourt et al. 2003; Beilfuss et al. 2012; Grossmann et al. 2012; Wei & Christakos, 2015), which are such a prominent feature of how inflammatory responses alter cellular activity. One of these inflammatory cytokines is tumour necrosis factor‐α (TNF‐α), which acts to increase the expression of the InsP3Rs (Park et al. 2009) thus inducing an increase in the level of Ca2+, which accelerates ageing as described below.
Mitochondrial dysfunction and ageing
Mitochondrial dysfunction is one of the main drivers of ageing (Lin & Beal 2006; Petrosillo et al. 2008; Wang et al. 2013; Yin et al. 2016). As a result of their dysfunction, the mitochondria produce insufficient ATP but generate increased amounts of ROS that enhance oxidative stress (Terman et al. 2006, 2010; Petrosillo et al. 2008; Toman & Fiskum, 2011; Marzetti et al. 2013; Wang et al. 2013), which is one of the main drivers of ageing (Fig. 1). It is likely that this mitochondrial dysfunction is driven by a deficiency in vitamin D.
One of the main functions of vitamin D is to maintain the activity of the mitochondrial respiratory chain (Consiglio et al. 2015). Vitamin D also regulates the expression of the uncoupling protein (UCP), which is located on the inner mitochondrial membrane where it acts to control thermogenesis (Abbas, 2016). During vitamin D deficiency, mitochondrial respiration declines due to a reduction in the nuclear mRNA molecules and proteins that contribute to mitochondrial respiration (Kim et al. 2014; Scaini et al. 2016). In particular, the formation of ATP declines because there is a vitamin D‐dependent reduction in the expression of complex I of the electron transport chain. This decline in the electron transport chain also results in an increase in the formation of ROS, which induce oxidative stress, which is a feature of ageing (Brownlee, 2005; Lowell & Shulman, 2005) as described in the following section.
Members of the sirtuin family, such as sirtuin (SIRT) 1, also play an important role in maintaining normal mitochondrial function (Westphal et al. 2007). The sirtuins, which are NAD+‐dependent protein deacetylases, function as anti‐ageing proteins that reduce ageing by regulating a wide range of protein targets (Guarente, 2007; Law et al. 2009; Donmez & Guarente, 2010; Grabowska et al. 2017). The sirtuins also play an important role in reducing brain ageing (Satoh et al. 2017). SIRT1 contributes to mitochondrial biogenesis by activating PGC‐1α. These beneficial effects of SIRT1 on mitochondrial function are regulated by vitamin D, which acts by increasing the formation of SIRT1 (An et al. 2010; Polidoro et al. 2013; Chang & Kim, 2016; Marampon et al. 2016; Manna et al. 2017).
One of the main actions of vitamin D is to maintain the normal mitochondrial control of cellular bioenergetics (Calton et al. 2015). The Ca2+ buffering role of dysfunctional mitochondria is also compromised resulting in an increase in the intracellular level of Ca2+, which is a feature of ageing as described later.
Oxidative stress and ageing
Oxidative stress, which is one of the main drivers of ageing (Finkel & Holbrook, 2000; Stadtman, 2002; Brewer, 2010; Paradies et al. 2011; Ureshino et al. 2014; Petersen & Smith, 2016), is caused by the increase in ROS formation by dysregulated mitochondria as described above. Vitamin D plays a major role in regulating ROS levels through its ability to control the expression of cellular antioxidants as part of its role to maintain phenotypic stability of cell signalling pathways (Dong et al. 2012; George et al. 2012; Berridge, 2015a,b). Vitamin D also supports such redox control by maintaining normal mitochondrial function (Bouillon & Verstuyf, 2013; Ryan et al. 2016) as described earlier.
Many of the genes that are controlled by the vitamin D–Klotho–Nrf2 regulatory network function to maintain redox homeostasis. For example, vitamin D together with Klotho and Nrf2 increases cellular antioxidants to maintain the normal reducing environment within the cell thereby preventing oxidative stress by removing ROS. For example, the expression of γ‐glutamyl transpeptidase, glutamate cysteine ligase and glutathione reductase, which contribute to the synthesis of the major redox buffer glutathione (GSH), is regulated by vitamin D. Vitamin D also increases the activity of glucose‐6‐phosphate dehydrogenase to increase the formation of GSH. It down‐regulates the nitrogen oxide (NOX) that generates ROS while upregulating the superoxide dismutase that rapidly converts O2 −• to H2O2 (Berridge, 2016). Vitamin D also up‐regulates expression of the glutathione peroxidase that drives the conversion of H2O2 to water.
Ca2+ signalling and ageing
An alteration in the Ca2+ signalling pathway has also be linked to an acceleration in the process of ageing (Fig. 1; Mattson, 2007; Puzianowska‐Kuznicka & Kuznicki 2009; Ureshino et al. 2010; Decuypere et al. 2011a; Gant et al. 2014; Berridge, 2016; Veldurthy et al. 2016; Martin & Bernard, 2017). During ageing, there is an alteration in Ca2+ signalling in atrial myocytes (Herraiz‐Martínez et al. 2015) and neurons (Buchholz et al. 2007; Murchison & Griffith, 2007). The relationship between Ca2+ signalling and ageing is particularly evident in the ageing brain (Thibault et al. 2001; Foster & Kumar, 2002; Gant et al. 2006; Foster, 2007; Thibault et al. 2007; Kumar et al. 2009; Gant et al. 2014). An increase in the release of Ca2+ from internal stores by the InsP3Rs and ryanodine receptors (RYRs) contributes to this increase in neural Ca2+ levels during ageing (Banerjee & Hasan, 2005; Puzianowska‐Kuznicka & Kuznicki, 2009; Santulli & Marks 2015). The increase in Ca2+ release from the RYRs is caused by a decline in the expression of the FK506‐binding proteins 1a and 1b (FKBP1a/1b), which act normally to reduce the release of Ca2+ by the RYRs (Gant et al. 2014). Inserting an adeno‐associated viral vector bearing a transgene encoding FKBP1b was able to reduce the effects of the elevated levels of Ca2+ that function to impair cognitive functions that occur during ageing (Gant et al. 2015).
When considering the role of Ca2+ in ageing, it is important to include magnesium, which is closely linked to both vitamin D and Ca2+. One the functions of magnesium is to enhance the synthesis of vitamin D (Rude et al. 1985; Risco & Traba, 1992; Deng et al. 2013). There are now indications that low levels of magnesium are linked to a number of diseases that are also associated with vitamin D deficiency. For example, a deficieny in magnesium has been linked to ageing. Lower magnesium levels have been found in individuals with hypertension and metabolic syndrome (Rotter et al. 2015). Low blood pressure and an increased risk of stroke have also been observed in individual with low magnesium levels (Bain et al. 2015). Some of the actions of magnesium are mediated through a reduction in Ca2+ signalling processes. In the brain, extracacellular magnesium can reduce Ca2+ entry through voltage‐gated Ca2+ channels and NMDA receptors (Wilmott & Thompson 2013). An increase in magnesium in the brain reverses the decline in cognition in Alzheimer's disease (Li et al. 2014). It is clear from all this evidence that magnesium plays an important role in regulating the activity of both Ca2+ and vitamin D.
During ageing, there is a decline in the level of the Ca2+ buffer calbindin‐D28K in the cholinergic neurons in the brain (Riascos et al. 2011). In motoneurons, vitamin D acts to increase the expression of calbindin‐D28 and parvalbumin (Alexianu et al. 1998). High levels of these buffers contributes to the low levels of Ca2+. A decline in these buffers, caused by a decline in the level of vitamin D that occurs during ageing, will result in an elevation of the level of Ca2+, which is a feature of brain ageing. In the ageing brain, there also is a decrease in the expression of Bcl‐2 (Ureshino et al. 2010), which may contribute to the increase in Ca2+ release by the InsP3Rs. Bcl‐2 interacts with the InsP3Rs to reduce the release of Ca2+ (Distelhorst & Bootman 2011). One of the consequences of this increase in the levels of Ca2+ during brain ageing is a decline in cognition (Thibault et al. 2001, 2007; Foster 2007; Toescu & Verkhratsky, 2007; Toepper, 2017). This decline in cognition is particularly evident in ageing patients (Seamans et al. 2010). In addition to this decline in cognition, there also is evidence of a decline in sleep in older adults, which may contribute to the decline in cognition (Mander et al. 2017).
Vitamin D has been shown to alleviate this enhanced Ca2+ elevation in the ageing brain. By reducing the levels of Ca2+, vitamin D restores normal cognitive function (Landfield & Cadwallader‐Neal, 1998; Brewer et al. 2006; Przybelski & Binkley, 2007; Perna et al. 2014; Schlögl & Holick, 2014; Toffanello et al. 2014; Banerjee et al. 2015). Strong support for such a notion has come from the study of the decline in cognition in ageing rats that is driven by a marked increase in the amplitude of the slow after‐hyperpolarization (sAHP) that depends on a build‐up of Ca2+ that activates the SK potassium channel (Landfield, 1987). This Ca2+ signal, which depends on the opening of L‐type voltage‐dependent Ca2+ channels that provides trigger Ca2+ to activate RYRs, inhibits memory by curtailing the spiking activity necessary for LTP, whereas the increase in Ca2+ stimulates calcineurin to induce the long‐term depolarization that erases memories. The development of this sAHP during ageing depends on dysregulation of both Ca2+ and ROS signalling that can be directly attributed to vitamin D deficiency.
One of the consequences of the elevation of Ca2+ and ROS that occurs during vitamin D deficiency is an increase in the incidence of age‐related diseases. For example, the onset of Alzheimer's disease occurs in those individuals who are deficient in vitamin D (Banerjee et al. 2015) and thus have abnormally elevated levels of both Ca2+ and ROS, which may induce the formation of the pathological amyloid beta (Aβ) oligomers that then initiate the onset of Alzheimer's disease (Berridge, 2016). Such a possibility is based on the fact that elevated levels of Ca2+ act to stimulate the enzymes that form Aβ (Querfurth & Selkoe, 1994; Green & LaFerla, 2008; Itkin et al. 2011). Such an increase in Ca2+ that occurs during vitamin D deficiency may also be associated with the onset of other neurodegenerative diseases such as Parkinson's disease, Huntington's disease and amyotrophic lateral sclerosis.
Vitamin D acts to increase the expression of both Klotho and Nrf2, which also act to reduce the ageing process. Vitamin D working together with Nrf2 and Klotho plays an essential role in maintaining the phenotypic stability of many cell signalling pathways and particularly the Ca2+ and redox signalling systems (Berridge, 2015a, b). This vitamin D–Klotho–Nrf2 regulatory system can prevent the dysregulation of Ca2+ and ROS signalling through multiple mechanisms. Vitamin D suppress the expression of the L‐type Ca2+ channel (Brewer et al. 2001, 2006) that initiates the Ca2+ signal that induces the sAHP and it also maintains the expression of plasma membrane Ca2+‐ATPase (PMCA) and the Na+/Ca2+ exchanger (NCX1), which extrude Ca2+ from the cell. In dendritic cells, vitamin D reduces the level of Ca2+ by increasing the expression of the NCX1 that extrudes Ca2+ from the cell (Shumilina et al. 2010). Klotho, which is an anti‐ageing protein (Kim et al. 2015), acts to stimulate the Na+/K+‐ATPase responsible for maintaining the Na+ gradient necessary for Ca2+ extrusion by NCX1. Finally, premature ageing occurs when Nrf2 is repressed (Kubben et al. 2016). Nrf2 increases the expression of many antioxidants that ensure that ROS levels are kept low (Lewis et al. 2010; Niture et al. 2010; Sykiotis et al. 2011; Nakai et al. 2014), which will prevent the sensitization of the RYRs that are triggering the sAHP and memory erasure.
The central role of vitamin D deficiency in this neuronal dysregulation and cognitive decline can be reversed by treating neurons with vitamin D, which dramatically reduces the sAHP (Brewer et al. 2006). When tested on ageing rats, vitamin D was found to enhance hippocampal synaptic function and, more significantly, it could prevent the decline in cognition (Landfield & Cadwallader‐Neal, 1998; Latimer et al. 2014).
Epigenetics and ageing
Epigenetic changes in the genome play an important role in the ageing process (Gonzalo, 2010; Gravina & Vijg, 2010; Ford et al. 2011; Lillycrop et al. 2014; Benayoun et al. 2015; Aunan et al. 2016; Pal & Tyler, 2016; Sen et al. 2016). The main epigenetic change that influences ageing is DNA and histone methylation, which has a marked influence on expression of many of the genes that are responsible for healthy ageing. A good example of this is the fact that such epigenetic changes have been linked to oxidative stress (Hedman et al. 2016). As described earlier, such oxidative stress is enhanced by a decline in the expression of cellular antioxidants. Such a view is supported by the fact that the most important signalling pathways that are maintained by vitamin D are the Ca2+ and redox signalling pathways (Berridge, 2016).
One of the major regulators of antioxidant expression is vitamin D and there is increasing evidence that vitamin D also controls the epigenetic landscape of its multiple gene promoters (Hossein‐nezhad & Holick, 2012; Hossein‐nezhad & Holick, 2013; Fetahu et al. 2014; Xue et al. 2016). Both the acetylation and methylation states of its promotor regions are maintained by vitamin D. With regard to acetylation, the vitamin D receptor (VDR) complex recruits histone acetylases such as p300–CREB‐binding protein (CBP) and steroid receptor coactivator 1 (SRC‐1). Perhaps its most significant action is to increase the expression of a number of DNA demethylases. Control of demethylation is critical because many of the genes regulated by vitamin D are silenced by methylation of the CpG islands located in their promotor regions. Such hypermethylation can also account for a decline in the expression of Klotho that occurs during ageing (King et al. 2011). Such age‐dependent hypermethylation is also evident in many age‐related diseases (cancer, cardiovascular and neurodegenerative diseases; van Otterdijk et al. 2013). For example, hypermethylation of promotors in GABAergic neurons may contribute to the phenotypic remodelling responsible for schizophrenia and bipolar disorder (Guidotti et al. 2011). Since many of these diseases have also been linked to vitamin D deficiency, it is not surprising to find that vitamin D can modulate the epigenetic landscape. Vitamin D controls the expression of a number of key DNA demethylases such as Jumonji C domain‐containing demethylase (JMJD) 1A, JMJD3, lysine‐specific demethylase (LSD) 1 and LSD2 (Pereira et al. 2012), which contributes to its ability to maintain phenotypic stability.
DNA disorders and ageing
Two DNA disorders contribute to the ageing process: telomere shortening and DNA alterations caused by the defective repair of DNA double‐strand breaks (DSB); both cause genomic instability (Ding & Shen, 2008; Gonzalez‐Suarez et al. 2011; López‐Otín et al. 2013; Chow & Herrup, 2015; Aunan et al. 2016). It is of interest that both these defects can be reduced by vitamin D. Telomeres, which are located at the ends of chromosomes, play an important role in preventing the ends of chromosomes from fusing with neighbouring chromosomes (Campisi et al. 2001; Oeseburg et al. 2010; Prasad et al. 2017). During ageing, there is a decline in the length of these telomeres and this causes a decline in cell proliferation resulting in cell senescence, which characterizes the ageing processes (Prasad et al. 2017). There is increasing evidence that vitamin D can act to reduce the rate of telomere shortening (Hoffecker et al. 2013; Liu et al. 2013; Pusceddu et al. 2015; Beilfuss et al. 2017; Mazidi et al. 2017). SIRT6 can also play an important role in stabilizing both the genome and telomeres (Tennen & Chua, 2011).
The defective repair of DNA double‐strand breaks (DSBs) is another DNA disorder that contributes to ageing. A deficiency of p53‐binding protein 1 (53BP1), which is a key factor in DNA DSBs, is the cause of the defective DSB. It has been established that the cysteine protease cathepsin L (CTSL) is responsible for degrading 53BP1 (Gonzalez‐Suarez et al. 2011; Grotsky et al. 2013). Vitamin D acts to prevent this DNA disorder caused by DSBs by inhibiting CTSL, which leads to the stabilizatioin of 53BP1 (Gonzalez‐Suarez et al. 2011; Grotsky et al. 2013).
Conclusion
There is increasing evidence that ageing can proceed at variable rates. In this review, I have developed the hypothesis that vitamin D may play a major role in regulating the rate of ageing. The basis of this hypothesis is that a number of the processes that drive ageing (e.g. autophagy, mitochondrial dysfunction, inflammation, oxidative stress, epigenetics, DNA disorders, and alterations in Ca2+ and ROS signalling) are regulated by vitamin D. Normal levels of vitamin D are capable of maintaining these processes at their normal low rates and this slows down the ageing process and also helps to prevent the onset of a number of age‐related diseases (e.g. Alzheimer's disease, Parkinson's disease, multiple sclerosis, hypertension and cardiovascular disease).
When vitamin D is deficient, there is an increase in the activity of these ageing processes that not only accelerates the rate of ageing, but it also creates the conditions that initiate the onset of the age‐related diseases such as Alzheimer's disease. Such an increase in Ca2+ that occurs during vitamin D deficiency has also been associated with the onset of other neurodegenerative diseases such as Parkinson's disease, Huntington's disease and amyotrophic lateral sclerosis.
Additional information
Competing interests
There are no competing interests.
Biography
Michael J. Berridge is best known for his discovery of inositol trisphosphate (IP3), which plays a universal role in regulating many different cellular processes. He became a Fellow of Trinity College in 1972 and was elected a Fellow of The Royal Society in 1984. For his work on second messengers he has received numerous awards and prizes, including The King Faisal International Prize in Science, The Louis Jeantet Prize in Medicine, The Albert Lasker Medical Research Award, The Heineken Prize, the Shaw Prize, and The Wolf Foundation Prize in Medicine. In 1998 he was knighted for his service to science.
This is an Editor's Choice article from the 15 November 2017 issue.
References
- Abbas MA (2016). Physiological functions of Vitamin D in adipose tissue. J Steroid Biochem Mol Biol 165, 369–381. [DOI] [PubMed] [Google Scholar]
- Alexianu ME, Robbins E, Carswell S & Appel SH (1998). 1α,25‐Dihydroxyvitamin D3‐dependent up‐regulation of calcium‐binding proteins in motoneuron cells. J Neurosci Res 51, 58–66. [DOI] [PubMed] [Google Scholar]
- Alvarez JA, Chowdhury R, Jones DP, Martin GS, Brigham KL, Binongo JN, Ziegler TR & Tangpricha V (2014). Vitamin D status is independently associated with plasma glutathione and cysteine thiol/disulphide redox status in adults. Clin Endocrinol (Oxf) 81, 458–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An BS, Tavera‐Mendoza LE, Dimitrov V, Wang X, Calderon MR, Wang HJ & White JH (2010). Stimulation of Sirt1‐regulated FoxO protein function by the ligand‐bound vitamin D receptor. Mol Cell Biol 30, 4890–4900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annweiler C, Schott AM, Berrut G, Chauviré V, Le Gall D, Inzitari M & Beauchet O (2010). Vitamin D and ageing: neurological issues. Neuropsychobiology 62, 139–150. [DOI] [PubMed] [Google Scholar]
- Aunan JR, Watson MM, Hagland HR & Søreide K (2016). Molecular and biological hallmarks of ageing. Br J Surg 103, e29–e46. [DOI] [PubMed] [Google Scholar]
- Bain LK, Myint PK, Jennings A, Lentjes MA, Luben RN, Khaw KT, Wareham NJ & Welch AA (2015). The relationship between dietary magnesium intake, stroke and its major risk factors, blood pressure and cholesterol, in the EPIC‐Norfolk cohort. Int J Cardiol 196, 108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S & Hasan G (2005). The InsP3 receptor: its role in neuronal physiology and neurodegeneration. Bioessays 27, 1035–1047. [DOI] [PubMed] [Google Scholar]
- Banerjee A, Khemka VK, Ganguly A, Roy D, Ganguly U & Chakrabarti S (2015). Vitamin D and Alzheimer's disease: Neurocognition to therapeutics. Int J Alzheimers Dis 2015, 192747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beilfuss J, Berg V, Sneve M, Jorde R & Kamycheva E (2012). Effects of a 1‐year supplementation with cholecalciferol on interleukin‐6, tumor necrosis factor‐alpha and insulin resistance in overweight and obese subjects. Cytokine 60, 870–874. [DOI] [PubMed] [Google Scholar]
- Beilfuss J, Camargo CA Jr & Kamycheva E (2017). Serum 25‐hydroxyvitamin D has a modest positive association with leukocyte telomere length in middle‐aged US adults. J Nutr 147, 514–520. [DOI] [PubMed] [Google Scholar]
- Benayoun BA, Pollina EA & Brunet A (2015). Epigenetic regulation of ageing: linking environmental inputs to genomic stability. Nat Rev Mol Cell Biol 16, 593–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berk M, Williams LJ, Jacka FN, O'Neil A, Pasco JA, Moylan S, Allen NB, Stuart AL, Hayley AC, Byrne ML & Maes M (2013). So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 11, 200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge MJ (2015a). Vitamin D: a custodian of cell signalling stability in health and disease. Biochem Soc Trans 43, 349–358. [DOI] [PubMed] [Google Scholar]
- Berridge MJ (2015b). Vitamin D cell signalling in health and disease. Biochem Biophys Res Commun 460, 53–71. [DOI] [PubMed] [Google Scholar]
- Berridge MJ (2016). Vitamin D, reactive oxygen species and calcium signalling in ageing and disease. Philos Trans R Soc Lond B Biol Sci 371, 20150434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouillon R & Verstuyf A (2013). Vitamin D, mitochondria, and muscle. J Clin Endocrinol Metab 98, 961–963. [DOI] [PubMed] [Google Scholar]
- Brewer LD, Thibault V, Chen KC, Langub MC, Landfield PW & Porter NM (2001). Vitamin D hormone confers neuroprotection in parallel with downregulation of L‐type calcium channel expression in hippocampal neurons. J Neurosci 21, 98–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer LD, Porter NM, Kerr DS, Landfield PW & Thibault O (2006). Chronic 1α,25‐(OH)2 vitamin D3 treatment reduces Ca2+‐mediated hippocampal biomarkers of aging. Cell Calcium 40, 277–286. [DOI] [PubMed] [Google Scholar]
- Brewer GJ (2010). Epigenetic oxidative redox shift (EORS) theory of aging unifies the free radical and insulin signaling theories. Exp Gerontol 45, 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briones TL & Darwish H (2012). Vitamin D mitigates age‐related cognitive decline through the modulation of pro‐inflammatory state and decrease in amyloid burden. J Neuroinflammation 9, 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownlee M (2005). The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54, 1615–1625. [DOI] [PubMed] [Google Scholar]
- Buchholz JN, Behringer EJ, Pottorf WJ, Pearce WJ & Vanterpool CK (2007). Age‐dependent changes in Ca2+ homeostasis in peripheral neurones: implications for changes in function. Aging Cell 6, 285–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burtner CR & Kennedy BK (2010). Progeria syndromes and ageing: what is the connection? Nat Rev Mol Cell Biol 11, 567–578. [DOI] [PubMed] [Google Scholar]
- Calton EK, Keane KN & Soares MJ (2015). The potential regulatory role of vitamin D in the bioenergetics of inflammation. Curr Opin Clin Nutr Metab Care 18, 367–373. [DOI] [PubMed] [Google Scholar]
- Campisi J, Kim SH, Lim CS & Rubio M (2001). Cellular senescence, cancer and aging: the telomere connection. Exp Gerontol 36, 1619–1637. [DOI] [PubMed] [Google Scholar]
- Cevenini E, Caruso C, Candore G, Capri M, Nuzzo D, Duro G, Rizzo C, Colonna‐Romano G, Lio D, Di Carlo D, Palmas MG, Scurti M, Pini E, Franceschi C & Vasto S (2010). Age‐related inflammation: the contribution of different organs, tissues and systems. How to face it for therapeutic approaches. Curr Pharm Des 16, 609–618. [DOI] [PubMed] [Google Scholar]
- Cevenini E, Monti D & Franceschi C (2013). Inflamm‐ageing. Curr Opin Clin Nutr Metab Care 16, 14–20. [DOI] [PubMed] [Google Scholar]
- Chang E & Kim Y (2016). Vitamin D decreases adipocyte lipid storage and increases NAD‐SIRT1 pathway in 3T3‐L1 adipocytes. Nutrition 32, 702–708. [DOI] [PubMed] [Google Scholar]
- Chirumbolo S, Bjørklund G, Sboarina A & Vella A (2017). The role of Vitamin D in the immune system as a pro‐survival molecule. Clin Ther 39, 894–916. [DOI] [PubMed] [Google Scholar]
- Chow HM & Herrup K (2015). Genomic integrity and the ageing brain. Nat Rev Neurosci 16, 672–684. [DOI] [PubMed] [Google Scholar]
- Consiglio M, Viano M, Casarin S, Castagnoli C, Pescarmona G & Silvagno F (2015). Mitochondrial and lipogenic effects of vitamin D on differentiating and proliferating human keratinocytes. Exp Dermatol 24, 748–753. [DOI] [PubMed] [Google Scholar]
- Costantino S, Paneni F & Cosentino F (2016). Ageing, metabolism and cardiovascular disease. J Physiol 594, 2061–2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criollo A, Vicencio JM, Tasdemir E, Maiuri MC, Lavandero S & Kroemer G (2007). The inositol trisphosphate receptor in the control of autophagy. Autophagy 3, 350–353. [DOI] [PubMed] [Google Scholar]
- Dawson‐Hughes B (2017). Vitamin D and muscle function. J Steroid Biochem Mol Biol 173, 313–316. [DOI] [PubMed] [Google Scholar]
- Decuypere JP, Bultynck G & Parys JB (2011b). A dual role for Ca2+ in autophagy regulation. Cell Calcium 50, 242–250. [DOI] [PubMed] [Google Scholar]
- Decuypere JP, Monaco G, Missiaen L, De Smedt H, Parys JB & Bultynck G (2011a). IP3 receptors, mitochondria, and Ca2+ signaling: Implications for aging. J Aging Res 2011, 920178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng X, Song Y, Manson JE, Signorello LB, Zhang SM, Shrubsole MJ, Ness RM, Seidner DL & Dai Q (2013). Magnesium, vitamin D status and mortality: results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III. BMC Medicine 11, 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d'Hellencourt LC, Montero‐Menei CN, Bernard R & Couez D (2003). Vitamin D3 inhibits proinflammatory cytokines and nitric oxide production by the EOC13 microglial cell line. J Neurosci Res 71, 575–582. [DOI] [PubMed] [Google Scholar]
- Di Benedetto S, Müller L, Wenger E, Düzel S & Pawelec G (2017). Contribution of neuroinflammation and immunity to brain aging and the mitigating effects of physical and cognitive interventions. Neurosci Biobehav Rev 75, 114–128. [DOI] [PubMed] [Google Scholar]
- Ding SL & Shen CY (2008). Model of human aging: recent findings on Werner's and Hutchinson‐Gilford progeria syndromes. Clin Interv Aging 3, 431–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Distelhorst CW & Bootman MD (2011). Bcl‐2 interaction with the inositol 1,4,5‐trisphosphate receptor: role in Ca2+ signaling and disease. Cell Calcium 50, 234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong J, Wong SL, Lau CW, Lee HK, Ng CF, Zhang L, Yao X, Chen ZY, Vanhoutte PM & Huang Y (2012). Calcitriol protects renovascular function in hypertension by down‐regulating angiotensin II type 1 receptors and reducing oxidative stress. Eur Heart J 33, 2980–2990. [DOI] [PubMed] [Google Scholar]
- Donmez G & Guarente L (2010). Aging and disease: connections to sirtuins. Aging Cell 9, 285–290. [DOI] [PubMed] [Google Scholar]
- Fetahu IS, Höbaus J & Kállay E (2014). Vitamin D and the epigenome. Front Physiol 5, 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkel T & Holbrook NJ (2000). Oxidants, oxidative stress and the biology of ageing. Nature 408, 239–247. [DOI] [PubMed] [Google Scholar]
- Fivenson EM, Lautrup S, Sun N, Scheibye‐Knudsen M, Stevnsner T, Nilsen H, Bohr VA & Fang EF (2017). Mitophagy in neurodegeneration and aging. Neurochem Int 109, 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford D, Ions LJ, Alatawi F & Wakeling LA (2011). The potential role of epigenetic responses to diet in ageing. Proc Nutr Soc 70, 374–384. [DOI] [PubMed] [Google Scholar]
- Forster RE, Jurutka PW, Hsieh J‐C, Haussler CA, Lowmiller CL, Kaneko I, Haussler MR, Kerr Whitfield G (2011). Vitamin D receptor controls expression of the anti‐aging Klotho gene in mouse and human renal cells. Biochem Biophys Res Commun 414, 557–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster TC (2007). Calcium homeostasis and modulation of synaptic plasticity in the aged brain. Aging Cell 6, 319–325. [DOI] [PubMed] [Google Scholar]
- Foster TC & Kumar A (2002). Calcium dysregulation in the aging brain. Neuroscientist 8, 297–301. [DOI] [PubMed] [Google Scholar]
- Gaksch M, Jorde R, Grimnes G, Joakimsen R, Schirmer H, Wilsgaard T, Mathiesen EB, Njølstad I, Løchen ML, März W, Kleber ME, Tomaschitz A, Grübler M, Eiriksdottir G, Gudmundsson EF, Harris TB, Cotch MF, Aspelund T, Gudnason V, Rutters F, Beulens JW, van 't Riet E, Nijpels G, Dekker JM, Grove‐Laugesen D, Rejnmark L, Busch MA, Mensink GB, Scheidt‐Nave C, Thamm M, Swart KM, Brouwer IA, Lips P, van Schoor NM, Sempos CT, Durazo‐Arvizu RA, Škrabáková Z, Dowling KG, Cashman KD, Kiely M & Pilz S (2017). Vitamin D and mortality: Individual participant data meta‐analysis of standardized 25‐hydroxyvitamin D in 26916 individuals from a European consortium. PLoS One 12, e0170791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gant JC, Blalock EM, Chen KC, Kadish I, Porter NM, Norris CM, Thibault O & Landfield PW (2014). FK506‐binding protein 1b/12.6: a key to aging‐related hippocampal Ca2+ dysregulation? Eur J Pharmacol 739, 74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gant JC, Chen KC, Kadish I, Blalock EM, Thibault O, Porter NM & Landfield PW (2015). Reversal of aging‐related neuronal Ca2+ dysregulation and cognitive impairment by delivery of a transgene encoding FK506‐binding protein 12.6/1b to the hippocampus. J Neurosci 35, 10878–10887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gant JC, Sama MM, Landfield PW & Thibault O (2006). Early and simultaneous emergence of multiple hippocampal biomarkers of aging is mediated by Ca2+‐induced Ca2+ release. J Neurosci 26, 3482–3490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcion E, Sindji L, Leblondel G, Brachet P & Darcy F (1999). 1,25‐Dihydroxyvitamin D3 regulates the synthesis of γ‐glutamyl transpeptidase and glutathione levels in rat primary astrocytes. J Neurochem 73, 859–866. [DOI] [PubMed] [Google Scholar]
- George N, Kumar TP, Antony S, Jayanarayanan S & Paulose CS (2012). Effect of vitamin D3 in reducing metabolic and oxidative stress in the liver of streptozotocin‐induced diabetic rats. Br J Nutr 108, 1410–1418. [DOI] [PubMed] [Google Scholar]
- Gonzalez‐Suarez I, Redwood AB, Grotsky DA, Neumann MA, Cheng EH, Stewart CL, Dusso A & Gonzalo S (2011). A new pathway that regulates 53BP1 stability implicates cathepsin L and vitamin D in DNA repair. EMBO J 30, 3383–3396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalo S (2010). Epigenetic alterations in aging. J Appl Physiol 109, 586–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalo S, Kreienkamp R & Askjaer P (2017). Hutchinson‐Gilford progeria syndrome: a premature aging disease caused by LMNA gene mutations. Ageing Res Rev 33, 18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowska W, Sikora E & Bielak‐Zmijewska A (2017). Sirtuins, a promising target in slowing down the ageing process. Biogerontology 18, 447–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady C (2012). The cognitive neuroscience of ageing. Nat Rev Neurosci 13, 491–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravina S & Vijg J (2010). Epigenetic factors in aging and longevity. Pflugers Arch 459, 247–258. [DOI] [PubMed] [Google Scholar]
- Green DR, Galluzzi L & Kroemer G (2011). Mitochondria and the autophagy‐inflammation‐cell death axis in organismal aging. Science 333, 1109–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KN & LaFerla FM (2008). Linking calcium to Aβ and Alzheimer's disease. Neuron 59, 190–194. [DOI] [PubMed] [Google Scholar]
- Grossmann RE, Zughaier SM, Liu S, Lyles RH & Tangpricha V (2012). Impact of vitamin D supplementation on markers of inflammation in adults with cystic fibrosis hospitalized for a pulmonary exacerbation. Eur J Clin Nutr 66, 1072–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grotsky DA, Gonzalez‐Suarez I, Novell A, Neumann MA, Yaddanapudi SC, Croke M, Martinez‐Alonso M, Redwood AB, Ortega‐Martinez S, Feng Z, Lerma E, Ramon y Cajal T, Zhang J, Matias‐Guiu X, Dusso A & Gonzalo S (2013). BRCA1 loss activates cathepsin L‐mediated degradation of 53BP1 in breast cancer cells. J Cell Biol 200, 187–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarente L (2007). Sirtuins in aging and disease. Cold Spring Harb Symp Quant Biol 72, 483–488. [DOI] [PubMed] [Google Scholar]
- Guidotti AJ, Auta, J , Chen Y, Davis JM, Dong E, Gavin DP, Grayson DR, Matrisciano F, Pinna G, Satta R, Sharma RP, Tremolizzo L, Tueting P (2011). Epigenetic GABAergic targets in schizophrenia and bipolar disorder. Neuropharmacology 60, 1007–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haussler MR, Haussler CA, Whitfield GK, Hsieh JC, Thompson PD, Barthel TK, Bartik L, Egan JB, Wu Y, Kubicek JL, Lowmiller CL, Moffet EW, Forster RE & Jurutka PW (2010). The nuclear vitamin D receptor controls the expression of genes encoding factors which feed the “Fountain of Youth” to mediate healthful aging. J Steroid Biochem Mol Biol 121, 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman ÅK, Zilmer M, Sundström J, Lind L & Ingelsson E (2016). DNA methylation patterns associated with oxidative stress in an ageing population. BMC Med Genomics 9, 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herraiz‐Martínez A, Álvarez‐García J, Llach A, Molina CE, Fernandes J, Ferrero‐Gregori A, Rodríguez C, Vallmitjana A, Benítez R, Padró JM, Martínez‐González J, Cinca J & Hove‐Madsen L (2015). Ageing is associated with deterioration of calcium homeostasis in isolated human right atrial myocytes. Cardiovasc Res 106, 76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewison M (2010). Vitamin D and the immune system: new perspectives on an old theme. Endocrinol Metab Clin North Am 39, 365–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffecker BM, Raffield LM, Kamen DL & Nowling TK (2013). Systemic lupus erythematosus and vitamin D deficiency are associated with shorter telomere length among African Americans: A case‐control study. PLoS One 8, e63725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossein‐nezhad A & Holick MF (2012). Optimize dietary intake of vitamin D: an epigenetic perspective. Curr Opin Clin Nutr Metab Care 15, 567–579. [DOI] [PubMed] [Google Scholar]
- Hossein‐nezhad A & Holick MF (2013). Vitamin D for health: a global perspective. Mayo Clin Proc 88, 720–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Høyer‐Hansen M, Bastholm L, Szyniarowski P, Campanella M, Szabadkai G, Farkas T, Bianchi K, Fehrenbacher N, Elling F, Rizzuto R, Mathiasen IS & Jäättelä M (2007). Control of macroautophagy by calcium, calmodulin‐dependent kinase kinase‐β, and Bcl‐2. Mol Cell 25, 193–205. [DOI] [PubMed] [Google Scholar]
- Høyer‐Hansen M, Nordbrandt SP & Jäättelä M (2010). Autophagy as a basis for the health‐promoting effects of vitamin D. Trends Mol Med 16, 295–302. [DOI] [PubMed] [Google Scholar]
- Hubbard VM, Valdor R, Macian F & Cuervo AM (2012). Selective autophagy in the maintenance of cellular homeostasis in aging organisms. Biogerontology 13, 21–35. [DOI] [PubMed] [Google Scholar]
- Itkin A, Dupres V, Dufrêne YF, Bechinger B, Ruysschaert JM & Raussens V (2011). Calcium ions promote formation of amyloid β‐peptide (1–40) oligomers causally implicated in neuronal toxicity of Alzheimer's disease. PLoS One 6, e18250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang W, Kim HJ, Li H, Jo KD, Lee MK, Song SH & Yang HO (2014). 1,25‐Dyhydroxyvitamin D₃ attenuates rotenone‐induced neurotoxicity in SH‐SY5Y cells through induction of autophagy. Biochem Biophys Res Commun 451, 142–147. [DOI] [PubMed] [Google Scholar]
- Jylhävä J, Pedersen NL & Hägg S (2017). Biological age predictors. EBioMedicine 21, 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keisala T, Minasyan A, Lou YR, Zou J, Kalueff AV, Pyykkö I & Tuohimaa P (2009). Premature aging in vitamin D receptor mutant mice. J Steroid Biochem Mol Biol 115, 91–97. [DOI] [PubMed] [Google Scholar]
- Kennel KA, Drake MT & Hurley DL (2010). Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc 85, 752–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HK, Andreazza AC, Yeung PY, Isaacs‐Trepanier C & Young LT (2014). Oxidation and nitration in dopaminergic areas of the prefrontal cortex from patients with bipolar disorder and schizophrenia. J Psychiatry Neurosci 39, 276–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Hwang KH, Park KS, Kong ID & Cha SK (2015). Biological role of anti‐aging protein Klotho. J Lifestyle Med 5, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King GD, Rosene DL & Abraham CR (2011). Promoter methylation and age‐related downregulation of klotho in rhesus monkey. Age 34, 1405–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreienkamp R, Croke M, Neumann MA, Bedia‐Diaz G, Graziano S, Dusso A, Dorsett D, Carlberg C & Gonzalo S (2016). Vitamin D receptor signaling improves Hutchinson‐Gilford progeria syndrome cellular phenotypes. Oncotarget 7, 30018–30031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubben N, Zhang W, Wang L, Voss TC, Yang J, Qu J, Liu GH & Misteli T (2016). Repression of the antioxidant NRF2 pathway in premature aging. Cell 165, 1361–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A, Bodhinathan K & Foster TC (2009). Susceptibility to calcium dysregulation during brain aging. Front Aging Neurosci 1, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuro‐o M (2009). Klotho and aging. Biochim Biophys Acta 1790, 1049–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landfield PW (1987). ‘Increased calcium‐current’ hypothesis of brain aging. Neurobiol Aging 8, 346–347. [DOI] [PubMed] [Google Scholar]
- Landfield PW & Cadwallader‐Neal L (1998). Long‐term treatment with calcitriol (1,25(OH)2 vit D3 retards a biomarker of hippocampal aging in rats. Neurobiol Aging 19, 469–477. [DOI] [PubMed] [Google Scholar]
- La Rovere RM, Roest G, Bultynck G & Parys JB (2016). Intracellular Ca2+ signaling and Ca2+ microdomains in the control of cell survival, apoptosis and autophagy. Cell Calcium 60, 74–87. [DOI] [PubMed] [Google Scholar]
- Latimer CS, Brewer LD, Searcy JL, Chen KC, Popović J, Kraner SD, Thibault O, Blalock EM, Landfield PW & Porter NM (2014). Vitamin D prevents cognitive decline and enhances hippocampal synaptic function in aging rats. Proc Natl Acad Sci USA 111, E4359–E4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law IK, Liu L, Xu A, Lam KS, Vanhoutte PM, Che CM, Leung PT & Wang Y (2009). Identification and characterization of proteins interacting with SIRT1 and SIRT3: implications in the anti‐aging and metabolic effects of sirtuins. Proteomics 9, 2444–2456. [DOI] [PubMed] [Google Scholar]
- Lewis KN, Mele J, Hayes JD & Buffenstein R (2010). Nrf2, a guardian of health span and gatekeeper of species longevity. Integr Comp Biol 50, 829–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Yu J, Liu Y, Huang X, Abumaria N, Zhu Y, Huang X, Xiong W, Ren C, Liu XG, Chui D & Liu G (2014). Elevation of brain magnesium prevents synaptic loss and reverses cognitive deficits in Alzheimer's disease mouse model. Mol Brain 7, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillycrop KA, Hoile SP, Grenfell L & Burdge GC (2014). DNA methylation, ageing and the influence of early life nutrition. Proc Nutr Soc 73, 413–421. [DOI] [PubMed] [Google Scholar]
- Lin MT & Beal MF (2006). Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443, 787–795. [DOI] [PubMed] [Google Scholar]
- Liu JJ, Prescott J, Giovannucci E, Hankinson SE, Rosner B, Han J & De Vivo I (2013). Plasma vitamin D biomarkers and leukocyte telomere length. Am J Epidemiol 177, 1411–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Cai H, Cheng W, Zhang H, Pan Z & Wang D (2017). Association of VDR polymorphisms (Taq I and Bsm I) with prostate cancer: a new meta‐analysis. J Int Med Res 45, 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Looker AC, Johnson CL, Lacher DA, Pfeiffer CM, Schleicher RL & Sempos CT (2011). Vitamin D status: United States, 2001–2006. NCHS Data Brief 59, 1–8. [PubMed] [Google Scholar]
- López‐Otín C, Blasco MA, Partridge L, Serrano M & Kroemer G (2013). The hallmarks of aging. Cell 153, 1194–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowell BB & Shulman GI (2005). Mitochondrial dysfunction and type 2 diabetes. Science 307, 384–387. [DOI] [PubMed] [Google Scholar]
- Lucas RM, Gorman S, Geldenhuys S & Hart PH (2014). Vitamin D and immunity. F1000Prime Rep 6, 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyten T, Welkenhuyzen K, Roest G, Kania E, Wang L, Bittremieux M, Yule DI, Parys JB & Bultynck G (2017). Resveratrol‐induced autophagy is dependent on IP3Rs and on cytosolic Ca2+ . Biochim Biophys Acta 1864, 947–956. [DOI] [PubMed] [Google Scholar]
- MacLaughlin J & Holick MF (1985). Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest 76, 1536–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madeo F, Zimmermann A, Maiuri MC & Kroemer G (2015). Essential role for autophagy in life span extension. J Clin Investig 125, 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mander BA, Winer JR & Walker MP (2017). Sleep and human aging. Neuron 94, 19–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manna P, Achari AE & Jain SK (2017). Vitamin D supplementation inhibits oxidative stress and upregulate SIRT1/AMPK/GLUT4 cascade in high glucose‐treated 3T3L1 adipocytes and in adipose tissue of high fat diet‐fed diabetic mice. Arch Biochem Biophys 615, 22–34. [DOI] [PubMed] [Google Scholar]
- Marampon F, Gravina GL, Festuccia C, Popov VM, Colapietro EA, Sanità P, Musio D, De Felice F, Lenzi A, Jannini EA, Di Cesare E & Tombolini V (2016). Vitamin D protects endothelial cells from irradiation‐induced senescence and apoptosis by modulating MAPK/SirT1 axis. J Endocrinol Invest 39, 411–422. [DOI] [PubMed] [Google Scholar]
- Martin N & Bernard D (2017). Calcium signaling and cellular senescence. Cell Calcium (in press; https://doi.org/10.1016/j.ceca.2017.04.001). [DOI] [PubMed] [Google Scholar]
- Marzetti E, Csiszar A, Dutta D, Balagopal G, Calvani R & Leeuwenburgh C (2013). Role of mitochondrial dysfunction and altered autophagy in cardiovascular aging and disease: from mechanisms to therapeutics. Am J Physiol Heart Circ Physiol 305, H459–H476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson MP (2007). Calcium and neurodegeneration. Aging Cell 6, 337–350. [DOI] [PubMed] [Google Scholar]
- Mazidi M, Michos ED & Banach M (2017). The association of telomere length and serum 25‐hydroxyvitamin D levels in US adults: the National Health and Nutrition Examination Survey. Arch Med Sci 13, 61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehan M & Penckofer S (2014). The role of vitamin D in the aging adult. J Aging Gerontol 2, 60–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murchison D & Griffith WH (2007). Calcium buffering systems and calcium signaling in aged rat basal forebrain neurons. Aging Cell 6, 297–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mushegian AA (2017). Autophagy and vitamin D. Sci Signal 10, eaan2526. [DOI] [PubMed] [Google Scholar]
- Nakai K, Fujii H, Kono K, Goto S, Kitazawa R, Kitazawa S, Hirata M, Shinohara M, Fukagawa M & Nishi S (2014). Vitamin D activates the Nrf2‐Keap1 antioxidant pathway and ameliorates nephropathy in diabetic rats. Am J Hypertens 27, 586–595. [DOI] [PubMed] [Google Scholar]
- Navarro‐Yepes J, Burns M, Anandhan A, Khalimonchuk O, del Razo LM, Quintanilla‐Vega B, Pappa A, Panayiotidis MI & Franco R (2014). Oxidative stress, redox signaling, and autophagy: cell death versus survival. Antioxid Redox Signal 21, 66–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niture SK, Kaspar JW, Shen J & Jaiswal AK (2010). Nrf2 signaling and cell survival. Toxicol Appl Pharmacol 244, 37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oeseburg H, de Boer RA, van Gilst WH & van der Harst P (2010). Telomere biology in healthy aging and disease. Pflugers Arch 459, 592–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordóñez‐Mena JM, Maalmi H, Schöttker B, Saum KU, Holleczek B, Wang TJ, Burwinkel B & Brenner H (2017). Genetic variants in the vitamin D pathway, 25(OH)D levels, and mortality in a large population‐based cohort study. J Clin Endocrinol Metab 102, 470–474. [DOI] [PubMed] [Google Scholar]
- Pal S & Tyler JK (2016). Epigenetics and aging. Sci Adv 2, e1600584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palikaras K, Daskalaki I, Markaki M & Tavernarakis N (2017). Mitophagy and age‐related pathologies: Development of new therapeutics by targeting mitochondrial turnover. Pharmacol Ther 178, 157–174. [DOI] [PubMed] [Google Scholar]
- Paradies G, Petrosillo G, Paradies V & Ruggiero FM (2011). Mitochondrial dysfunction in brain aging: role of oxidative stress and cardiolipin. Neurochem Int 58, 447–457. [DOI] [PubMed] [Google Scholar]
- Park KM, Yule DI & Bowers WJ (2009). Tumor necrosis factor‐α‐mediated regulation of the inositol 1,4,5‐trisphosphate receptor promoter. J Biol Chem 284, 27557–27566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira F, Barbáchano A, Singh PK, Campbell MJ, Muñoz A & Larriba MJ (2012). Vitamin D has wide regulatory effects on histone demethylase genes. Cell Cycle 11, 1081–1089. [DOI] [PubMed] [Google Scholar]
- Perna L, Mons U, Kliegel M & Brenner H (2014). Serum 25‐hydroxyvitamin D and cognitive decline: a longitudinal study among non‐demented older adults. Dement Geriatr Cogn Disord 38, 254–263. [DOI] [PubMed] [Google Scholar]
- Petersen KS & Smith C (2016). Ageing‐associated oxidative stress and inflammation are alleviated by products from grapes. Oxid Med Cell Longev 2016, 6236309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosillo G, Matera M, Casanova G, Ruggiero FM & Paradies G (2008). Mitochondrial dysfunction in rat brain with aging involvement of complex I, reactive oxygen species and cardiolipin. Neurochem Int 53, 126–131. [DOI] [PubMed] [Google Scholar]
- Pittas AG & Dawson‐Hughes B (2010). Vitamin D and diabetes. J Steroid Biochem Mol Biol 121, 425–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plaza‐Zabala A, Virginia Sierra‐Torre V & Amanda Sierra A (2017). Autophagy and microglia: Novel partners in neurodegeneration and aging. Int J Mol Sci 18, 598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polidoro L, Properzi G, Marampon F, Gravina GL, Festuccia C, Di Cesare E, Scarsella L, Ciccarelli C, Zani BM & Ferri C (2013). Vitamin D protects human endothelial cells from H₂O₂ oxidant injury through the Mek/Erk‐Sirt1 axis activation. J Cardiovasc Transl Res 6, 221–231. [DOI] [PubMed] [Google Scholar]
- Prasad KN, Wu M & Bondy SC (2017). Telomere shortening during aging: Attenuation by antioxidants and anti‐inflammatory agents. Mech Ageing Dev 164, 61–66. [DOI] [PubMed] [Google Scholar]
- Przybelski RJ & Binkley NC (2007). Is vitamin D important for preserving cognition? A positive correlation of serum 25‐hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys 460, 202–205. [DOI] [PubMed] [Google Scholar]
- Purdue‐Smithe AC, Whitcomb WB, Szegda KL, Boutot ME, Manson JE, Hankinson SE, Rosner BA, Troy LM, Michels KB & Bertone‐Johnson ER (2017). Vitamin D and calcium intake and risk of early menopause. Am J Clin Nutr 105, 1493–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pusceddu I, Farrell CJ, Di Pierro AM, Jani E, Herrmann W & Herrmann M (2015). The role of telomeres and vitamin D in cellular aging and age‐related diseases. Clin Chem Lab Med 53, 1661–1678. [DOI] [PubMed] [Google Scholar]
- Puzianowska‐Kuznicka M & Kuznicki J (2009). The ER and ageing II: calcium homeostasis. Ageing Res Rev 8, 160–172. [DOI] [PubMed] [Google Scholar]
- Querfurth HK & Selkoe DJ (1994). Calcium ionophore increases amyloid beta peptide production by cultured cells. Biochemistry 33, 4550–4561. [DOI] [PubMed] [Google Scholar]
- Raz Y, Guerrero‐Ros I, Maier A, Slagboom PE, Atzmon G, Barzilai N & Macian F (2017). Activation‐Induced autophagy is preserved in CD4+ T‐Cells in familial longevity. J Gerontol A Biol Sci Med Sci 72, 1201–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riascos D, de Leon D, Baker‐Nigh A, Nicholas A, Yukhananov R, Bu J, Wu CK & Geula C (2011). Age‐related loss of calcium buffering and selective neuronal vulnerability in Alzheimer's disease. Acta Neuropathol 122, 565–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risco F & Traba ML (1992). Influence of magnesium on the in vitro synthesis of 24,25‐dihydroxyvitamin D3 and 1 alpha, 25‐dihydroxyvitamin D3. Magnes Res 5, 5–14. [PubMed] [Google Scholar]
- Rotter I, Kosik‐Bogacka D, Dołęgowska B, Safranow K, Lubkowska A & Laszczyńska M (2015). Relationship between the concentrations of heavy metals and bioelements in aging men with metabolic syndrome. Int J Environ Res Public Health 12, 3944–3961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinsztein DC, Mariño G & Kroemer G (2011). Autophagy and aging. Cell 146, 682–695. [DOI] [PubMed] [Google Scholar]
- Rude RK, Adams JS, Ryzen E, Endres DB, Niimi H, Horst RL, Haddad JG Jr & Singer FR (1985). Low serum concentrations of 1,25‐dihydroxyvitamin D in human magnesium deficiency. J Clin Endocrinol Metab 61, 933–940. [DOI] [PubMed] [Google Scholar]
- Ryan ZC, Craig TA, Folmes CD, Wang X, Lanza IR, Schaible NS, Salisbury JL & Nair KS, Terzic A, Sieck GC & Kumar R (2016). 1α,25‐Dihydroxyvitamin D3 regulates mitochondrial oxygen consumption and dynamics in human skeletal muscle cells. J Biol Chem 291, 1514–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salminen A, Kaarniranta K & Kauppinen A (2012). Inflammaging: disturbed interplay between autophagy and inflammasomes. Aging (Albany NY) 4, 166–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santulli G & Marks AR (2015). Essential roles of intracellular calcium release channels in muscle, brain, metabolism, and aging. Curr Mol Pharmacol 8, 206–222. [DOI] [PubMed] [Google Scholar]
- Satoh, A , Imai S‐I & Guarente L (2017). The brain, sirtuins, and ageing. Nat Rev Neurosci 18, 362–374. [DOI] [PubMed] [Google Scholar]
- Scaini G, Rezin GT, Carvalho AF, Streck EL, Berk M & Quevedo J (2016). Mitochondrial dysfunction in bipolar disorder: Evidence, pathophysiology and translational implications. Neurosci Biobehav Rev 68, 694–713. [DOI] [PubMed] [Google Scholar]
- Schlögl M & Holick MF (2014). Vitamin D and neurocognitive function. Clin Interv Aging 9, 559–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schöttker B, Ball D, Gellert C & Brenner H (2013). Serum 25‐hydroxyvitamin D levels and overall mortality. A systematic review and meta‐analysis of prospective cohort studies. Ageing Res Rev 12, 708–718. [DOI] [PubMed] [Google Scholar]
- Seals DR, Justice JN & LaRocca TJ (2016). Physiological geroscience: targeting function to increase healthspan and achieve optimal longevity. J Physiol 594, 2001–2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seamans KM, Hill TR, Scully L, Meunier N, Andrillo‐Sanchez M, Polito A, Hininger‐Favier I, Ciarapica D, Simpson EE, Stewart‐Knox BJ, O'Connor JM, Coudray C & Cashman KD (2010). Vitamin D status and measures of cognitive function in healthy older European adults. Eur J Clin Nutr 64, 1172–1178. [DOI] [PubMed] [Google Scholar]
- Sen P, Shah PP, Nativio R & Berger SL (2016). Epigenetic mechanisms of longevity and aging. Cell 166, 822–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shumilina E, Xuan NT, Matzner N, Bhandaru M, Zemtsova IM & Lang F (2010). Regulation of calcium signaling in dendritic cells by 1,25‐dihydroxyvitamin D3 . FASEB J 24, 1989–1996. [DOI] [PubMed] [Google Scholar]
- Stadtman ER (2002). Importance of individuality in oxidative stress and aging. Free Radic Biol Med 33, 597–604. [DOI] [PubMed] [Google Scholar]
- Sun F, Xu X, Wang X & Zhang B (2016). Regulation of autophagy by Ca2+ . Tumor Biology 37, 15467–15476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundar IK & Rahman I (2011). Vitamin D and susceptibility of chronic lung diseases: role of epigenetics. Front Pharmacol 2, 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sykiotis GP, Habeos IG, Samuelson AV & Bohmann D (2011). The role of the antioxidant and longevity‐promoting Nrf2 pathway in metabolic regulation. Curr Opin Clin Nutr Metab Care 14, 41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavera‐Mendoza LE, Westerling T, Libby E, Marusyk A, Cato L, Cassani R, Cameron LA, Ficarro SB, Marto JA, Klawitter J & Brown M (2017). Vitamin D receptor regulates autophagy in the normal mammary gland and in luminal breast cancer cells. Proc Natl Acad Sci USA 114, E2186–E2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennen RI & Chua KF (2011). Chromatin regulation and genome maintenance by mammalian SIRT6. Trends Biochem Sci 36, 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terman A, Gustafsson B & Brunk UT (2006). Mitochondrial damage and intralysosomal degradation in cellular aging. Mol Aspects Med 27, 471–482. [DOI] [PubMed] [Google Scholar]
- Terman A, Gustafsson B & Brunk UT (2007). Autophagy, organelles and ageing. J Pathol 211, 134–143. [DOI] [PubMed] [Google Scholar]
- Terman A, Kurz T, Navratil M, Arriaga EA & Brunk UT (2010). Mitochondrial turnover and aging of long‐lived postmitotic cells: the mitochondrial‐lysosomal axis theory of aging. Antioxid Redox Signal 12, 503–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thibault O, Hadley R & Landfield PW (2001). Elevated postsynaptic [Ca2+] I and L‐type calcium channel activity in aged hippocampal neurons: relationship to impaired synaptic plasticity. J Neurosci 21, 9744–9756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thibault O, Gant JC & Landfield PW (2007). Expansion of the calcium hypothesis of brain aging and Alzheimer's disease: minding the store. Aging Cell 6, 307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toepper M (2017). Dissociating normal aging from Alzheimer's disease: A view from cognitive neuroscience. J Alzheimers Dis 57, 331–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toescu EC & Verkhratsky A (2007). The importance of being subtle: small changes in calcium homeostasis control cognitive decline in normal aging. Aging Cell 6, 267–273. [DOI] [PubMed] [Google Scholar]
- Toffanello ED, Coin A, Perissinotto E, Zambon S, Sarti S, Veronese N, De Rui M, Bolzetta F, Corti MC, Crepaldi G, Manzato E & Sergi G (2014). Vitamin D deficiency predicts cognitive decline in older men and women: The Pro.V.A. Study. Neurology 83, 2292–2298. [DOI] [PubMed] [Google Scholar]
- Toman J & Fiskum G (2011). Influence of aging on membrane permeability transition in brain mitochondria. J Bioenerg Biomembr 43, 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuohimaa P (2009). Vitamin D and aging. J Steroid Biochem Mol Biol 114, 78–84. [DOI] [PubMed] [Google Scholar]
- Uberti F, Lattuada D, Morsanuto V, Nava U, Bolis G, Vacca G, Squarzanti DF, Cisari C & Molinari C (2014). Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways. J Clin Endocrinol Metab 99, 1367–1374. [DOI] [PubMed] [Google Scholar]
- Ureshino RP, Bertoncini CR, Fernandes MJ, Abdalla FM, Porto CS, Hsu YT, Lopes GS & Smaili SS (2010). Alterations in calcium signaling and a decrease in Bcl‐2 expression: possible correlation with apoptosis in aged striatum. J Neurosci Res 88, 438–447. [DOI] [PubMed] [Google Scholar]
- Ureshino RP, Rocha KK, Lopes GS, Bincoletto C & Smaili SS (2014). Calcium signaling alterations, oxidative stress, and autophagy in aging. Antioxid Redox Signal 21, 123–137. [DOI] [PubMed] [Google Scholar]
- van Otterdijk SD, Mathers JC & Strathdee G (2013). Do age‐related changes in DNA methylation play a role in the development of age‐related diseases? Biochem Soc Trans 41, 803–807. [DOI] [PubMed] [Google Scholar]
- Veldurthy V, Wei R, Oz L, Dhawan P, Jeon YH & Christakos S (2016). Vitamin D, calcium homeostasis and aging. Bone Res 4, 6041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verway M, Behr MA & White JH (2010). Vitamin D, NOD2, autophagy and Crohn's disease. Expert Rev Clin Immunol 6, 505–508. [DOI] [PubMed] [Google Scholar]
- Wang CH, Wu SB, Wu YT & Wei YH (2013). Oxidative stress response elicited by mitochondrial dysfunction: implication in the pathophysiology of aging. Exp Biol Med (Maywood) 238, 450–460. [DOI] [PubMed] [Google Scholar]
- Wang H, Chen W, Li D, Yin X, Zhang X, Olsen N & Zheng SG (2017). Vitamin D and chronic diseases. Aging Dis 8, 346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, He Y, Shen Y, Zhang Q, Chen D, Zuo C, Qin J, Wang H, Wang J & Yu Y (2014). Vitamin D inhibits COX‐2 expression and inflammatory response by targeting thioesterase superfamily member 4. J Biol Chem 289, 11681–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, He D, Ni C, Zhou H, Wu S, Xue Z & Zhou Z (2016). Vitamin D induces autophagy of pancreatic β‐cells and enhances insulin secretion. Mol Med Rep 14, 2644–2650. [DOI] [PubMed] [Google Scholar]
- Wei H, Qu H, Wang H, Ji B, Ding Y, Liu D, Duan Y, Liang H, Peng C, Xiao X & Deng H (2017). 1,25‐Dihydroxyvitamin‐D3 prevents the development of diabetic cardiomyopathy in type 1 diabetic rats by enhancing autophagy via inhibiting the β‐catenin/TCF4/GSK‐3β/mTOR pathway. J Steroid Biochem Mol Biol 168, 71–90. [DOI] [PubMed] [Google Scholar]
- Wei R & Christakos S (2015). Mechanisms underlying the regulation of innate and adaptive immunity by vitamin D. Nutrients 7, 8251–8260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal CH, Dipp MA & Guarente L (2007). A therapeutic role for sirtuins in diseases of aging? Trends Biochem Sci 32, 555–560. [DOI] [PubMed] [Google Scholar]
- Wilmott LA & Thompson LT (2013). Sex‐ and dose‐dependent effects of post‐trial calcium channel blockade by magnesium chloride on memory for inhibitory avoidance conditioning. Behav Brain Res 257, 49–53. [DOI] [PubMed] [Google Scholar]
- Wu S & Sun J (2011). Vitamin D, vitamin D receptor, and macroautophagy in inflammation and infection. Discov Med 11, 325–335. [PMC free article] [PubMed] [Google Scholar]
- Xue J, Schoenrock SA, Valdar W, Tarantino LM & Ideraabdullah FY (2016). Maternal vitamin D depletion alters DNA methylation at imprinted loci in multiple generations. Clin Epigenetics 8, 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin F, Sancheti H, Liu Z & Cadenas E (2016). Mitochondrial function in ageing: coordination with signalling and transcriptional pathways. J Physiol 594, 2025–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuk JM, Shin DM, Lee HM, Yang CS, Jin HS, Kim KK, Lee ZW, Lee SH, Kim JM & Jo EK (2009). Vitamin D3 induces autophagy in human monocytes/macrophages via cathelicidin. Cell Host Microbe 6, 231–243. [DOI] [PubMed] [Google Scholar]
- Zittermann A (2003). Vitamin D in preventive medicine: are we ignoring the evidence? Br J Nutr 89, 552–572. [DOI] [PubMed] [Google Scholar]


