Abstract
Background
Mefloquine is one of four antimalarial agents commonly recommended for preventing malaria in travellers to malaria‐endemic areas. Despite its high efficacy, there is controversy about its psychological side effects.
Objectives
To summarize the efficacy and safety of mefloquine used as prophylaxis for malaria in travellers.
Search methods
We searched the Cochrane Infectious Diseases Group Specialized Register; the Cochrane Central Register of Controlled Trials (CENTRAL), published on the Cochrane Library; MEDLINE; Embase (OVID); TOXLINE (https://toxnet.nlm.nih.gov/newtoxnet/toxline.htm); and LILACS. We also searched the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP; http://www.who.int/ictrp/en/) and ClinicalTrials.gov (https://clinicaltrials.gov/ct2/home) for trials in progress, using 'mefloquine', 'Lariam', and 'malaria' as search terms. The search date was 22 June 2017.
Selection criteria
We included randomized controlled trials (for efficacy and safety) and non‐randomized cohort studies (for safety). We compared prophylactic mefloquine with placebo, no treatment, or an alternative recommended antimalarial agent. Our study populations included all adults and children, including pregnant women.
Data collection and analysis
Two review authors independently assessed the eligibility and risk of bias of trials, extracted and analysed data. We compared dichotomous outcomes using risk ratios (RR) with 95% confidence intervals (CI). Prespecified adverse outcomes are included in 'Summary of findings' tables, with the best available estimate of the absolute frequency of each outcome in short‐term international travellers. We assessed the certainty of the evidence using the GRADE approach.
Main results
We included 20 RCTs (11,470 participants); 35 cohort studies (198,493 participants); and four large retrospective analyses of health records (800,652 participants). Nine RCTs explicitly excluded participants with a psychiatric history, and 25 cohort studies stated that the choice of antimalarial agent was based on medical history and personal preference. Most RCTs and cohort studies collected data on self‐reported or clinician‐assessed symptoms, rather than formal medical diagnoses.
Mefloquine efficacy
Of 12 trials comparing mefloquine and placebo, none were performed in short‐term international travellers, and most populations had a degree of immunity to malaria. The percentage of people developing a malaria episode in the control arm varied from 1% to 82% (median 22%) and 0% to 13% in the mefloquine group (median 1%).
In four RCTs that directly compared mefloquine, atovaquone‐proguanil and doxycycline in non‐immune, short‐term international travellers, only one clinical case of malaria occurred (4 trials, 1822 participants).
Mefloquine safety versus atovaquone‐proguanil
Participants receiving mefloquine were more likely to discontinue their medication due to adverse effects than atovaquone‐proguanil users (RR 2.86, 95% CI 1.53 to 5.31; 3 RCTs, 1438 participants; high‐certainty evidence). There were few serious adverse effects reported with mefloquine (15/2651 travellers) and none with atovaquone‐proguanil (940 travellers).
One RCT and six cohort studies reported on our prespecified adverse effects. In the RCT with short‐term travellers, mefloquine users were more likely to report abnormal dreams (RR 2.04, 95% CI 1.37 to 3.04, moderate‐certainty evidence), insomnia (RR 4.42, 95% CI 2.56 to 7.64, moderate‐certainty evidence), anxiety (RR 6.12, 95% CI 1.82 to 20.66, moderate‐certainty evidence), and depressed mood during travel (RR 5.78, 95% CI 1.71 to 19.61, moderate‐certainty evidence). The cohort studies in longer‐term travellers were consistent with this finding but most had larger effect sizes. Mefloquine users were also more likely to report nausea (high‐certainty evidence) and dizziness (high‐certainty evidence).
Based on the available evidence, our best estimates of absolute effect sizes for mefloquine versus atovaquone‐proguanil are 6% versus 2% for discontinuation of the drug, 13% versus 3% for insomnia, 14% versus 7% for abnormal dreams, 6% versus 1% for anxiety, and 6% versus 1% for depressed mood.
Mefloquine safety versus doxycycline
No difference was found in numbers of serious adverse effects with mefloquine and doxycycline (low‐certainty evidence) or numbers of discontinuations due to adverse effects (RR 1.08, 95% CI 0.41 to 2.87; 4 RCTs, 763 participants; low‐certainty evidence).
Six cohort studies in longer‐term occupational travellers reported our prespecified adverse effects; one RCT in military personnel and one cohort study in short‐term travellers reported adverse events. Mefloquine users were more likely to report abnormal dreams (RR 10.49, 95% CI 3.79 to 29.10; 4 cohort studies, 2588 participants, very low‐certainty evidence), insomnia (RR 4.14, 95% CI 1.19 to 14.44; 4 cohort studies, 3212 participants, very low‐certainty evidence), anxiety (RR 18.04, 95% CI 9.32 to 34.93; 3 cohort studies, 2559 participants, very low‐certainty evidence), and depressed mood (RR 11.43, 95% CI 5.21 to 25.07; 2 cohort studies, 2445 participants, very low‐certainty evidence). The findings of the single cohort study reporting adverse events in short‐term international travellers were consistent with this finding but the single RCT in military personnel did not demonstrate a difference between groups in frequencies of abnormal dreams or insomnia.
Mefloquine users were less likely to report dyspepsia (RR 0.26, 95% CI 0.09 to 0.74; 5 cohort studies, 5104 participants, low certainty‐evidence), photosensitivity (RR 0.08, 95% CI 0.05 to 0.11; 2 cohort studies, 1875 participants, very low‐certainty evidence), vomiting (RR 0.18, 95% CI 0.12 to 0.27; 4 cohort studies, 5071 participants, very low‐certainty evidence), and vaginal thrush (RR 0.10, 95% CI 0.06 to 0.16; 1 cohort study, 1761 participants, very low‐certainty evidence).
Based on the available evidence, our best estimates of absolute effect for mefloquine versus doxycyline were: 2% versus 2% for discontinuation, 12% versus 3% for insomnia, 31% versus 3% for abnormal dreams, 18% versus 1% for anxiety, 11% versus 1% for depressed mood, 4% versus 14% for dyspepsia, 2% versus 19% for photosensitivity, 1% versus 5% for vomiting, and 2% versus 16% for vaginal thrush.
Additional analyses, including comparisons of mefloquine with chloroquine, added no new information. Subgroup analysis by study design, duration of travel, and military versus non‐military participants, provided no conclusive findings.
Authors' conclusions
The absolute risk of malaria during short‐term travel appears low with all three established antimalarial agents (mefloquine, doxycycline, and atovaquone‐proguanil).
The choice of antimalarial agent depends on how individual travellers assess the importance of specific adverse effects, pill burden, and cost. Some travellers will prefer mefloquine for its once‐weekly regimen, but this should be balanced against the increased frequency of abnormal dreams, anxiety, insomnia, and depressed mood.
12 April 2019
Up to date
All studies incorporated from most recent search
All eligible published studies found in the last search (22 Jun, 2017) were included
Plain language summary
Can mefloquine prevent malaria during travel to areas where the disease is widespread?
We summarized trials that evaluated the effectiveness and safety of mefloquine when used to prevent malaria in people travelling to areas where the disease is widespread. We searched for relevant studies up to 22 June 2017 and included 20 randomized trials that involved 11,470 participants, 35 cohort studies (198,493 participants) and four large retrospective analyses of health records (800,652 participants).
What are the concerns about mefloquine and what are the alternatives?
Mefloquine is often prescribed to prevent malaria during travel to areas where the disease is widespread. However, there is controversy about the safety of mefloquine, especially when prescribed for military personnel in stressful situations, and there have been reports of depression and suicide.
The only commonly‐used alternative drugs are doxycycline (which can cause skin problems and indigestion) and atovaquone‐proguanil (which is often more expensive).
What the research says
Mefloquine appears to be a highly effective drug to reduce the risk of malaria (low‐certainty evidence), however, evidence did not come from short‐term international travellers.
Mefloquine has not been shown to have more frequent serious side effects than either atovaquone‐proguanil (low‐certainty evidence) or doxycycline (very low‐certainty evidence).
People who take mefloquine are more likely to stop taking the drug due to side effects than people who take atovaquone‐proguanil (high‐certainty evidence), but may be equally as likely to stop as people who take doxycyline (low‐certainty evidence).
People taking mefloquine are more likely to have abnormal dreams, insomnia, anxiety and depressed mood during travel than people who take atovaquone‐proguanil (moderate‐certainty evidence) or doxycyline (very low‐certainty evidence). Doxycycline users are more likely to have dyspepsia, photosensitivity, vomiting, and vaginal thrush (very low‐certainty evidence).
Summary of findings
Background
Description of the condition
Malaria is a parasitic protozoal infection which is usually transmitted through the bite of female Anopheles mosquitoes (Warrell 2002). It is most common in tropical and subtropical regions. Clinical disease is caused by infection of red blood cells by one of four Plasmodium species: P. falciparum, P. vivax,P. ovale, andP. malariae (WHO 2017). Humans can also become infected by forms of malaria that usually infect animals, such asP. knowlesi (WHO 2017). Clinical presentation is nonspecific and varied; symptoms include fever, chills, headache, diarrhoea, muscle cramps, and abdominal pain (WHO 2015). Severe disease is usually caused by infection with P. falciparum, but can also occur following infection with P. vivax and P. knowlesi. Host factors determining severity include genetics, host immune status, and age (WHO 2015).
The true global incidence and prevalence of malaria is difficult to determine; the highest disease burden occurs in sub‐Saharan Africa where vital registration and disease notification systems are weak (Murray 2014). However, the latest World Health Organization (WHO) figures estimate 212 million new cases of malaria in 2015 leading to 429,000 deaths (WHO 2016). Around 125 million travellers visit malaria‐endemic areas annually, and all need to take steps to prevent infection with malaria (Croft 2005). Each year there are between 10,000 and 30,000 known cases of malaria in returned travellers, but the real figure is likely to be higher due to under‐reporting (WHO 2017).
The individual risk of acquiring malaria is determined by the host immune status, the area travelled to, the duration of travel and season, and the use of prevention measures. Pregnant women, young children and non‐immune travellers are particularly vulnerable to severe disease if they become infected (WHO 2015). In Europe, the incidence of malaria is higher in people who travel to their country of origin to visit friends and relatives than in tourists (Behrens 2015). However, mortality is higher in tourists (Behrens 2015).
The natural life cycle of malaria involves the consecutive infection of two hosts: female Anopheles mosquitoes and humans (CDC 2015a). The female mosquito acquires the disease when taking a blood meal from an infected human host. It will then become infectious over a period of 10 to 14 days depending on the region. Sporozoites are injected into the human host the next time the mosquito feeds. These travel via the blood stream to the liver and develop into schizonts which then rupture releasing merozoites. Merozoites invade erythrocytes and undergo asexual replication. Some of these develop through ring stage trophozoites into schizonts which rupture releasing further merozoites and thus perpetuate the infection. Others will develop into female and male gametocytes which are ingested by Anopheles mosquitoes during a blood meal leading to the spread of disease.
Description of the intervention
Mefloquine has been available for use in Europe since 1985 and the USA since 1990 (Schlagenhauf 1999). Alongside atovaquone‐proguanil and doxycycline, it is considered standard chemoprophylaxis by many international health guidelines (CDC 2015b; PHAC 2014; PHE 2015; WHO 2017).
Mefloquine belongs to the aryl amino acid group of antimalarial agents. Mefloquine has a long half life and is given as a weekly dose of 250 mg when used for prophylaxis in adults (Schlagenhauf 2010). Mefloquine is effective against all five strains of malaria known to affect humans. Although guidelines vary, many state that mefloquine should be taken for two to three weeks before travel and continued for four weeks following return (WHO 2017).
There are several situations in which mefloquine is potentially advantageous. All guidelines recommend that where avoidable pregnant women should not travel to areas where malaria is endemic (WHO 2017). However, where travel is essential, mefloquine is often the preferred option. Mefloquine is widely considered to be safe within the second and third trimesters of pregnancy and guidelines increasingly recommend its use in the first trimester (CDC 2015b; Schlagenhauf 2010). Mefloquine is suitable for both children who weigh more than 5 kg and breastfeeding mothers (Schlagenhauf 2010).
Doxycycline has restrictions on its use during pregnancy due to effects on skeletal development found in animal studies. The use of atovaquone‐proguanil is limited by a lack of evidence for safety (PHE 2015). Chloroquine‐proguanil is considered safe for pregnant women, but its use is limited by widespread resistance (PHAC 2014).
The main side effects of mefloquine are gastrointestinal, neurological and psychological. Psychological side effects vary from those considered to be very common (including insomnia and abnormal dreaming) to those with unknown frequency (including psychosis and suicidal ideation) (eMC 2015a). Existing drug labels suggest that these side effects are both prodromal and dose related (eMC 2015a).
How the intervention might work
Malaria chemoprophylaxis is defined as the use of antimalarial medication to prevent the clinical symptoms of malaria (Schlagenhauf 2010). This is because no drugs are able to prevent the introduction of infection by destroying the sporozoites injected by the female Anopheles mosquito. Chemoprophylaxis is one of several tools used to prevent malaria; other recommended measures include sleeping under insecticide‐treated bed nets, wearing insecticide‐treated clothing, and applying chemical repellent sprays to the skin surface (WHO 2017). None of these methods provide complete protection and a combination of approaches is advised.
Chemoprophylaxis works by blocking the development or reproduction of the malaria parasite at various stages in its life cycle:
doxycycline and mefloquine are examples of suppressive prophylactics and act in the blood stream as the schizonts invade erythrocytes. Doxycycline therefore needs to be taken for at least one month after returning from endemic areas (Shanks 2005);
atovaquone‐proguanil and primaquine have effects on the early liver stages of Plasmodium spp and prevent the progression to blood stage parasites which cause clinical illness. These agents therefore only need to be taken for one week after leaving the malaria‐endemic area (Shanks 2005).
Currently, the baseline efficacy of doxycycline, atovaquone‐proguanil and mefloquine when used as prophylaxis to prevent malaria is thought to be similar. Most guidelines therefore recommend selecting appropriate antimalarial prophylaxis based on individual choice, pre‐existing conditions, side effect profile, and drug resistance patterns in the destination country (CDC 2015b; PHE 2015; WHO 2017). Drug resistance to all antimalarial agents is a growing concern, and mefloquine resistance has been reported in some areas of north‐western Thailand (Treiber 2010; Treiber 2011).
In addition, the efficacy of all forms of malaria prevention is impeded by adherence. Nearly all cases of fatal malaria in travellers occur due to non‐adherence with prophylactic measures (Schlagenhauf 2010). However, this needs to be balanced against the tolerability and safety of chemoprophylaxis; the frequency of mild to moderate adverse drug reactions varies from 32% to 45% (Schlagenhauf 2003). Both policy makers and individual travellers need to balance carefully the risk benefit profile of contracting malaria against using chemoprophylaxis.
Why it is important to do this review
Mefloquine has long been associated with neurological and psychological side effects which range from mild headaches and dizziness to reports of suicide and psychosis. The frequency and severity of these outcomes has been debated. In 2013 the USA Food and Drug Administration (FDA) released a safety communication regarding potential long‐term and significant neurological and psychiatric side effects of mefloquine (FDA 2013). This included the addition of a boxed warning to the drug label, the most serious form of warning that can be issued. Similarly in Europe in 2014 the European Medicine Agency (EMA) Pharmacovigilance Risk Assessment Committee (PRAC) required a change to the summary of product characteristics noting that "...in a small number of patients it has been reported that neuropsychiatric reactions (for example, depression, dizziness or vertigo and loss of balance) may persist for months or longer, even after discontinuation of the drug" (EMA 2014). This has been incorporated into summaries of product characteristics throughout Europe. Most recently the UK Defence Committee has suggested mefloquine should only be used as a drug of last resort (UK Parliament 2016).
Previous reviews on this topic have limited analyses to randomized controlled trials (RCTs) (Jacquerioz 2009; Jacquerioz 2015). However, RCTs are not always the optimal study design to determine the type, prevalence or nature of adverse events and adverse effects, and many set inclusion criteria which exclude groups of people who are likely to be affected (Loke 2007). In addition, adverse effects are often the primary outcome measure of non‐randomized trials, meaning that researchers may attempt to capture and define adverse events in a more rigorous manner than when they are a tertiary measure (Loke 2011).
This Cochrane Review update broadened study inclusion criteria to include non‐randomized studies that provide useful information regarding the side effect profile of mefloquine.
This review did not address:
the efficacy or safety of alternative forms of malaria chemoprophylaxis;
the use by pregnant women of mefloquine as intermittent presumptive treatment of malaria, or;
the use by travellers of emergency standby malaria treatment.
This new edition replaces the Cochrane Review on mefloquine for preventing malaria in non‐immune adult travellers (Jacquerioz 2015). Malaria prophylaxis in children living in endemic areas, chemoprophylaxis in pregnant women, and malaria prevention in people with sickle cell disease have been assessed in other Cochrane Reviews (Meremikwu 2008; Oniyangi 2006; Radeva‐Petrova 2014).
Objectives
To summarize the efficacy and safety of mefloquine used as prophylaxis for malaria in travellers.
Methods
Criteria for considering studies for this review
Types of studies
For efficacy we included randomized and quasi‐randomized controlled trials, including cluster‐randomized trials.
For safety we also included non‐randomized controlled trials/cohort studies. We included both prospective and retrospective cohort studies, but excluded studies where recruitment was linked to the occurrence of specific adverse events.
A list of study design features for all included studies is included in Appendix 1.
Types of participants
Adults and children, including pregnant women.
Types of interventions
Intervention
Mefloquine at a prophylactic dose (for example, 250 mg once weekly in adults and equivalent dosing for children).
Control
Placebo, no intervention or an alternative malaria chemoprophylaxis agent in current use.
Types of outcome measures
Efficacy
Clinical cases of malaria.
Safety
Adverse effects of any severity: defined as "an adverse event for which the causal relation between the intervention and the event is at least a reasonable possibility" (Loke 2011);
serious adverse effects are those "leading to death, [which] are life threatening, require inpatient hospitalization or prolongation of existing hospitalization, or result in persistent or significant disability or incapacity, or is a congenital anomaly/birth defect" (ICH 1994);
adverse events of any severity: defined as “any untoward medical occurrence that may present during treatment with a pharmaceutical product but which does not necessarily have a causal relationship with this treatment” (WHO‐ART 2008);
serious adverse events are those "leading to death, [which] are life threatening, require inpatient hospitalization or prolongation of existing hospitalization, or result in persistent or significant disability or incapacity, or is a congenital anomaly/birth defect." (ICH 1994);
discontinuations of study drug due to adverse effects;
measures of adherence to the drug regimen.
Pregnancy‐related outcomes:
adverse pregnancy outcomes: spontaneous abortions, stillbirths, congenital malformations.
Study authors often use the terms 'adverse event', 'adverse effect' or 'side effect' interchangeably and loosely. Where possible, we used the definitions described above to distinguish adverse events and adverse effects. Adverse effects encompasses reporting by study authors of 'adverse effects', 'side effects', 'adverse events attributed to the study drug', 'adverse reactions', and 'symptoms related to the study drugs'.
Search methods for identification of studies
We attempted to find all relevant trials regardless of language or publication status (published, unpublished, in press, and in progress).
Electronic searches
We searched the following databases using the search terms and strategy described in Appendix 2:
Cochrane Infectious Diseases Group Specialized Register to 22 June 2017;
Central Register of Controlled Trials (CENTRAL), published on the Cochrane Library to 22 June 2017;
MEDLINE (PubMed) from 1966 to 22 June 2017;
Embase (Ovid) from 1974 to 22 June 2017; and
LILACS (Bireme) from 1982 to 22 June 2017.
We also searched the WHO International Clinical Trials Registry Platform (WHO ICTRP) and ClinicalTrials.gov (https://clinicaltrials.gov/) for trials in progress, using 'mefloquine', 'Lariam', and 'malaria' as search terms (22 June 2017).
For the safety analysis we also searched MEDLINE (PubMed) (1966 to 22 June 2017), Embase (Ovid) (1974 to 22 June 2017), and TOXLINE (1980 to 22 June 2017) (https://toxnet.nlm.nih.gov/newtoxnet/toxline.htm). The following MEDLINE terms were adapted as needed: ("Mefloquine/adverse effects"[Mesh] OR "Mefloquine/poisoning"[Mesh] OR "Mefloquine/toxicity"[Mesh] ); Mefloquine ti, ab AND (safety OR tolerability OR death*OR suicid* OR adverse OR reaction* OR “side effect*”) ti, ab.
Searching other resources
We checked the reference lists of included studies for any references not identified by our searches.
Data collection and analysis
Selection of studies
Two review authors independently screened the results of the literature search for potentially relevant trials using Covidence software (Covidence 2017), and looked for multiple publications from the same data set. Full text copies were retrieved for all trials deemed potentially relevant for inclusion.
Two review authors then independently assessed all identified trials for inclusion in the review using the prespecified inclusion criteria. Any disagreements were resolved through discussion.
Data extraction and management
Two review authors independently extracted data using a standardized and pre‐piloted data collection form. When available we extracted data on:
details of study: start and end dates, setting (country of recruitment and country of malaria exposure), study design, method of participant recruitment and selection, number of participants enrolled, number of participants for whom data was available, mean duration of exposure to malaria, antimalarial resistance pattern of mefloquine and the comparator;
study participants: inclusion and exclusion criteria, age, gender, body mass index (BMI), pregnancy status, risk factors (for malaria and for adverse outcomes), immune or non‐immune participants, military or non military;
details of the intervention: drug dose during prophylaxis, use of a loading dose, duration of drug therapy before and after travel, frequency of drug administration and use of any co‐interventions;
outcomes measured and reported including definition, method of detection, timing in relation to treatment, duration and frequency of monitoring.
We resolved any disagreements through discussion, and where necessary we consulted a third review author. If clarification was necessary, we attempted to contact the trial authors for further information.
For dichotomous data, we recorded the number of participants experiencing the event and the number analysed in each group. For continuous outcome data, we extracted arithmetic means and standard deviations for each group together with the numbers analysed in each group. We also extract medians and ranges where provided.
We extracted details of all serious adverse events and effects. For non‐serious adverse events and effects we sought information on the following specific symptoms and groups of symptoms which are frequently associated with mefloquine, doxycycline or atovaquone‐proguanil:
ear and labyrinth disorders: vertigo;
eye disorders: visual impairment;
gastrointestinal disorders: nausea, vomiting, abdominal pain, diarrhoea, dyspepsia;
nervous system disorders: dizziness and headaches;
psychiatric disorders: abnormal dreams, insomnia, anxiety, depression, psychosis; and
skin and subcutaneous tissue disorders: pruritis, photosensitivity, vaginal candida.
We also reported data on all other very common (> 1/10) and common (> 1/100 to < 1/10) adverse events and adverse effects, as defined by the electronic Medicines Compendium (eMC 2015b).
Where possible we attempted to derive absolute estimates of adverse outcomes (events or effects). For all adverse outcomes, we included only the denominator trials that actively reported the presence or absence of each specific adverse event or effect.
Most RCTs and cohort studies collected data on self‐reported or clinician‐assessed symptoms rather than formal medical diagnoses. Therefore, we reported outcomes as symptoms. For example, we reported on 'depressed mood' rather than 'depression'.
When deciding which relative effect measure to present in 'Summary of findings' tables, we considered which meta‐analysis most closely answered our PICO (population, intervention, comparator, outcome/s) question. We created a decision tree in advance to assess the directness of a group of studies in relation to: the population studied (short‐term international travellers versus other populations), outcomes measured (adverse effects versus adverse events), and study design (RCTs versus cohort studies). The intervention and comparator were fixed in each drug‐pair comparison. Other less direct meta‐analyses were used in our appraisal of the certainty of the evidence. The decision tree used is provided in Appendix 3.
Conventionally, 'Summary of findings' tables include up to seven outcomes. However, the key questions for clinical decision making relate to adverse effects, and therefore limiting the number of outcomes a priori was problematic, as we could not know in advance which adverse effects mefloquine would have. To constrain the number of outcomes in the 'Summary of findings' tables to seven would mean only reporting outcomes where effects were shown, which would lead to selective reporting.
We included 'Summary of findings' tables for comparisons of mefloquine with doxycycline and atovaquone‐proguanil. This decision was made because chloroquine is used less frequently than mefloquine, doxycyline and atovaquone‐proguanil. As reported in Results, the adverse effect profile of mefloquine in comparison to chloroquine was consistent with comparisons with doxycycline and atovaquone‐proguanil.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias of each included study. For randomized and quasi‐randomized controlled trials we used Cochrane's 'Risk of bias' tool (Higgins 2011). We followed the guidance for making judgements on the risk of bias in five domains: sequence generation; allocation concealment; blinding (of participants, personnel and outcome assessors); incomplete outcome data; selective outcome reporting and other risk of bias. We categorized these judgements as low risk of bias, high risk of bias, or unclear risk of bias.
For non‐randomized (cohort) studies we assessed the risk of bias using the Cochrane Risk of Bias Assessment Tool for Non‐Randomized Studies of Interventions (now referred to as ROBINS‐I) (ACROBAT‐NSRI tool). We followed the guidance for making judgements on the risk of bias in eight domains: confounding, selection of participants into the study, measurement of interventions, departures from intended interventions, missing data, selection of the reported result and other risk of bias. We categorized these judgements as low risk of bias, moderate risk of bias, serious risk of bias and critical risk of bias. Where no information was provided on a category, this was stated. The criteria we used to make specific judgements are provided in Table 3.
1. Risk of bias assessment methods for cohort studies.
| Bias | Authors' judgement | Support for judgement |
| Confounding | Low risk Moderate risk Serious risk Critical risk No information |
We used the following criteria: Low risk: identified confounders were measured and were balanced across groups (age, sex, destination and duration of travel) Moderate risk: identified confounders were measured and not balanced across groups, or several confounders had not been measured or not reported across groups Serious risk: a critical confounder has been measured and is not balanced across groups |
| Selection of participants into the study | Low risk Moderate risk Serious risk Critical risk No information |
We assessed whether selection into the study was unrelated to intervention or unrelated to outcome, and whether start of intervention and start of follow up coincided for most subjects. Non‐responder bias at the point of selection was considered here for cohort studies. We used the following cut offs for non‐response rate: low risk < 10%, moderate risk 10% to 20%, serious risk > 20%. |
| Measurement of interventions | Low risk Moderate risk Serious risk Critical risk No information |
We used the following criteria: Low risk: the prescription was provided by a travel clinic which also performed the study, and discontinuations were recorded and reported, or all participants were issued with their medication e.g. soldiers or participants were asked to self‐report which medication they took whilst they were taking it. Moderate risk: the prescription was provided by a travel clinic which also performed the study but no information regarding switches and discontinuations was available or patients are asked to self‐report which prophylaxis they took shortly after they finished taking it. Serious risk: Participants were asked to self‐report which prophylaxis they took a long time after they finished taking it. |
| Departures from intended interventions | Low risk Moderate risk Serious risk Critical risk No information |
We assessed whether switches between interventions of interest were available. We assessed whether discontinuations and switches between prophylactic regimens had been recorded and reported. |
| Missing data | Low risk Moderate risk Serious risk Critical risk No information |
We assessed whether outcome data was reasonably complete for most participants. We recorded missing data for included participants e.g. loss to follow up rates and treatment withdrawals. |
| Measurement of outcomes | Low risk Moderate risk Serious risk Critical risk No information |
We assessed whether the outcome measure was objective or subjective. We assessed whether participants or study personnel were blinded to the intervention received. We assessed whether the methods of outcome assessment were comparable across intervention groups. |
| Selection of the reported result | Low risk Moderate risk Serious risk Critical risk No information |
We used the following criteria: Low risk: If the questionnaire was provided in full, or it was clear what was asked within it. Moderate risk: If it is unclear which questions are asked, or information was provided on aggregate. Serious risk: If data captured within the questionnaire was clearly missing. |
| Other | Low risk Moderate risk Serious risk Critical risk No information |
We reported the study sponsor. We classified the analysis of studies sponsored by pharmaceutical companies as independent of the sponsor when it was clearly stated that the sponsor had no input to the trial analysis. |
Adapted from Higgins 2011 and ACROBAT‐NSRI tool
For adverse events and adverse effects, we assessed the risk of bias in the conduct of the study by examining whether harms were predefined using standardized or precise definitions, ascertainment methods were adequately described, monitoring was active or passive and data collection was prospective or retrospective (Table 4). For laboratory tests and other investigations we assessed whether the number and timing of the tests was adequate.
2. Adverse events and adverse effects risk of bias assessment methods.
| Criterion | Assessment | Explanation |
| On conduct | ||
| Were harms pre‐defined using standardised or precise definitions? | Adequate Inadequate Unclear |
We classified as 'adequate' if the study reported explicit definitions for adverse events and effects that allow for reproducible ascertainment e.g. what adverse events were being investigated and what constituted an “event”, what was defined as a serious or severe adverse event. |
| Was ascertainment technique adequately described? | Adequate Inadequate Unclear |
We classified as 'adequate' if the study reported methods used to ascertain complications, including who ascertained, timing, and methods used. |
| Was monitoring active or passive? | Active Passive Unclear |
We classified monitoring as 'active' when authors reviewed participants at set time points during treatment and enquired about symptoms. |
| Was data collection prospective or retrospective? | Prospective Retrospective Unclear |
We classified as ‘prospective’ if data collection occurred during treatment, or ‘retrospective’ if data collection occurred following treatment. |
| For laboratory investigations or other tests | ||
| Was the number and timing of tests adequate? | Adequate Inadequate Unclear |
We classified the number and timing of tests as 'adequate', when tests were taken at baseline and at least one time point during prophylaxis. |
Adapted from Bukiwra 2014
We resolved any disagreement through discussion, and where necessary, we consulted a third review author.
Measures of treatment effect
We analysed data using Review Manager 5 (RevMan 5) (RevMan 2014) and combined dichotomous data using risk ratios (RR). For continuous data summarized by arithmetic means and standard deviations, we combined data using mean differences (MD). We present RRs and MD with 95% confidence intervals (CI) and report medians and ranges in tables for non‐RCTs.
Unit of analysis issues
When trials included more than two comparison groups, we split the trial for analysis as individual pair‐wise comparisons. If more than one comparison group was included in a meta‐analysis, we ensured that participants were only counted once by dividing the cases and participants evenly between the comparisons.
For clinical cases of malaria, we included participants as the unit of analysis, such that each participant was counted once in the intervention or placebo arm. Where study reporting was unclear regarding the unit of analysis (that is, total clinical cases of malaria rather than clinical cases in each participant) we noted this in footnotes and performed a sensitivity analysis excluding these results.
Dealing with missing data
If data from trial reports were insufficient, unclear, or missing, we attempted to contact the trial authors for additional information.
Our primary analysis was a complete‐case analysis which excluded all participants without treatment outcomes. No imputation measures for missing data were applied.
Where studies had grouped symptoms together by body system when reporting safety outcomes, we contacted authors to obtain disaggregated data. We obtained two additional full data sets (Cunningham 2014; Korhonen 2007) and received further clarification from two study authors (Kato 2013; Sonmez 2005). The full details of subsequent analyses are provided in the characteristics of included studies tables.
Assessment of heterogeneity
We assessed heterogeneity among trials by inspecting forest plots for overlapping CIs, applying the Chi² test with a 10% level of statistical significance, and using the I² statistic with a value of 50% to denote moderate levels of heterogeneity.
Assessment of reporting biases
We were unable to assess publication bias using funnel plots because there were too few trials reporting the same outcomes.
Data synthesis
We carried out statistical analyses using RevMan 5 (RevMan 2014). We analysed randomized controlled trials (RCTs) and non‐RCTs separately, and compared interventions as individual pair‐wise comparisons.
In the absence of heterogeneity, we used a fixed‐effect model. Where we identified moderate heterogeneity, and it was appropriate to combine data, we used the random‐effects model. When it was not appropriate to combine data in a meta‐analysis, we tabulated data and reported outcomes as a narrative.
We report the term used for each adverse event in each trial. Where trials used different terminology for similar adverse events and adverse effects, we coded them using the preferred term based on Medical Dictionary for Regulatory Activities (MedDRA) terminology (for example, sleepiness, somnolence) and analysed these together (MedDRA 2016).
Subgroup analysis and investigation of heterogeneity
We explored possible sources of heterogeneity using subgroup analyses (study design, military versus non‐military participants, short‐ versus long‐duration of travel).
Sensitivity analysis
We conducted sensitivity analyses to evaluate the robustness of the results to the risk of bias components, by excluding studies at high or unclear risk of bias.
Results
Description of studies
Results of the search
Searches (conducted 22 June 2017) identified 2155 records; we screened seven additional studies after reviewing reference lists. Of these, we excluded 1953 after assessing titles and abstracts. We retrieved 209 full text publications to assess for inclusion.
Included studies
We included 20 randomized controlled trials (RCTs) (11,470 participants), 35 cohort studies (190,286 participants) and four large retrospective analyses of health records (800,652 participants).
Efficacy outcomes were reported in 14 RCTs conducted between 1977 and 2003 in Thailand (four trials), Brazil, Cambodia, Ghana, Indonesia, Ivory Coast, Malawi, Nigeria, Kenya and two studies which included travellers to various destinations (10,710 participants). Two were conducted in short‐term international travellers (Overbosch 2001; Schlagenhauf 2003); nine involved general populations living in endemic areas who are likely to have some immunity to malaria (Boudreau 1991; Bunnag 1992; Hale 2003; Nosten 1994; Pearlman 1980; Salako 1992; Sossouhounto 1995; Steketee 1996; Weiss 1995), two recruited non‐immune military personnel (Arthur 1990; Ohrt 1997), and one recruited a mixed military and civilian semi‐immune population (Santos 1993).
All 20 included RCTs and 35 cohort studies reported safety outcomes. Nine RCTs explicitly excluded participants with a psychiatric history, and 25 cohort studies stated that the choice of antimalarial agent was based on medical history and personal preference. Most RCTs and cohort studies collected data on self‐reported or clinician‐assessed 'symptoms', rather than formal medical diagnoses. Consequently, when describing these data we used non‐medical descriptions such as 'depressed mood' rather than 'depression', even where the trial authors described the symptom as depression. However, four retrospective cohort studies analysed healthcare records (Eick‐Cost 2017; Meier 2004; Schneider 2013; Wells 2006) and looked for people with formal mental health diagnoses. Where outcomes were presented grouped by organ system, we approached study authors for additional data and received full data sets for two studies (Cunningham 2014; Korhonen 2007) and additional information from another two (Kato 2013; Sonmez 2005).
Three RCTs (1827 participants) and 24 cohort studies (170,487 participants) included short‐term international travellers. Five cohort studies included long‐term occupational travellers (UK Foreign and Commonwealth Office Staff and Peace Corps volunteers) (13,211 participants); four RCTs (961 participants) and six cohort studies (6588 participants) included military personnel (including 1 study with a mixed military and civilian population). Thirteen RCTs included local residents who did not travel outside their home countries: Australia (Davis 1996), Ghana (Hale 2003), Israel (Potasman 2002), Ivory Coast (Sossouhounto 1995), Kenya (Weiss 1995), Malawi (Steketee 1996), the Netherlands (Vuurman 1996), Nigeria (Salako 1992), Switzerland (Schlagenhauf 1997) and Thailand (Boudreau 1991, Bunnag 1992, Nosten 1994, Pearlman 1980).
Seven RCTs and three cohort studies were sponsored by Roche (manufacturer of mefloquine), three RCTs and one cohort study were sponsored by GlaxoSmithKline (manufacturer of atovaquone‐proguanil), one RCT was sponsored by Pfizer (manufacturer of doxycycline), and one by Mepha Ltd (manufacturer of a film‐coated form of mefloquine). Only one RCT and one cohort study reported whether the study sponsor had any influence over collecting, analysis or interpretation of study results or the decision to publish.
Excluded studies
We excluded 141 studies after full‐text screening (Figure 1). We excluded 37 studies because they were not research studies; 29 studies reported no relevant outcomes; 23 studies were single arm cohort studies and did not meet our inclusion criteria; 17 studies compared mefloquine with a regime which is not routinely used; 11 studies were not a randomized or cohort study (for example, case report or case‐control study); in seven studies mefloquine was not used at a prophylactic dose, for example, treatment dose; seven studies were multiple publications from the same data set as included studies; four cohort studies the population was identified on the basis of having experienced adverse effects and we excluded 6 studies for other reasons. We have provided full details in the 'Characteristics of excluded studies' tables.
1.
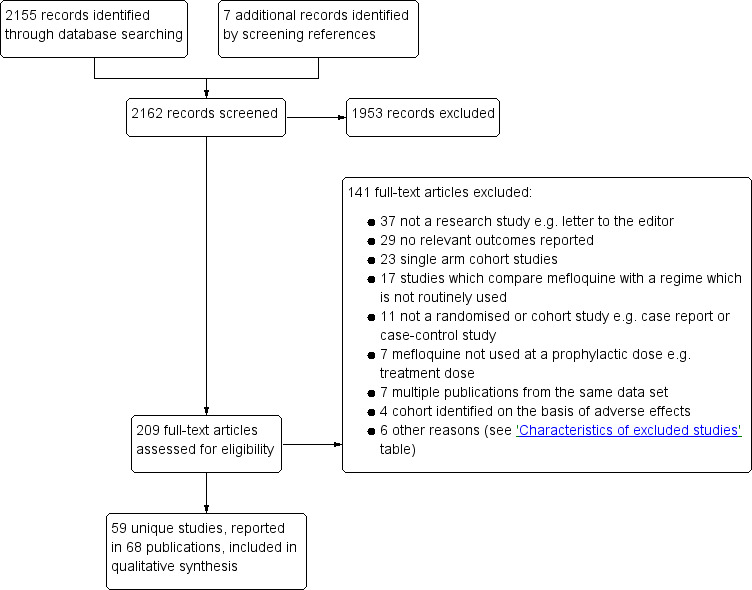
Study flow diagram.
Risk of bias in included studies
We performed 'Risk of bias' assessments for the included RCTs using the Cochrane 'Risk of bias' assessment tool. We assessed the risk of bias in the cohort studies using the ACROBAT‐NSRI tool (now referred to as ROBINS‐I). For a summary of the 'Risk of bias' assessments for RCTs see Figure 2.
2.
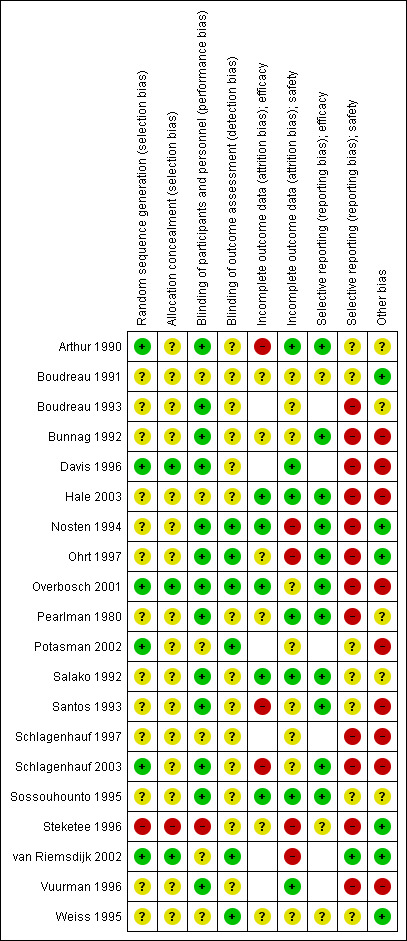
'Risk of bias' summary for RCTs: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
Three trials were at low risk of selection bias, with adequate descriptions of generation of the random sequence and allocation concealment (Davis 1996; Overbosch 2001; van Riemsdijk 2002). A further 16 trials were at unclear risk of selection bias due to providing insufficient information regarding their methodology. One trial described sequential allocation of unblinded participants (Steketee 1996).
Blinding
Seven trials adequately described blinding of study personnel, including blinding of pathology technicians when detecting malaria, and blinding of outcome assessors when assessing safety outcomes (Nosten 1994; Ohrt 1997; Overbosch 2001; Potasman 2002; Schlagenhauf 2003; van Riemsdijk 2002; Weiss 1995). The remaining 13 trials did not adequately describe how outcome assessors were blinded.
Incomplete outcome data
Six trials had low and balanced losses to follow‐up rates for efficacy outcomes (Hale 2003; Nosten 1994; Overbosch 2001; Salako 1992; Sossouhounto 1995; Weiss 1995). One trial was at high risk of bias because investigators did not follow up participants beyond the active phase of treatment for relapses (Santos 1993). Two studies did not make the method of detection of malaria, frequency or duration of follow up clear (Arthur 1990; Schlagenhauf 2003).
Seven trials had low losses to follow‐up rates for adverse outcomes (Arthur 1990; Davis 1996; Hale 2003; Pearlman 1980; Salako 1992; Sossouhounto 1995; Weiss 1995). We judged four of the trials to be at high risk of bias because investigators did not provide numbers of participants lost to follow up across groups (Nosten 1994; Steketee 1996); did not assess all participants who received the study drug in the final analysis (Ohrt 1997); and because the proportion of participants who did not complete the study due to adverse outcomes varied significantly between groups (van Riemsdijk 2002).
Selective reporting
Fourteen trials reported on efficacy outcomes, and twelve of these appropriately reported all outcomes.
However, 21 trials reported on our safety outcomes and only nine of these appropriately reported on all pre‐specified outcomes. Three of these trials only reported on statistically significant differences between groups (Boudreau 1993; Pearlman 1980; Schlagenhauf 1997), and another four did not report data from all time points (Bunnag 1992; Nosten 1994; Ohrt 1997; Overbosch 2001). Two trials reported aggregate data across multiple time points (Schlagenhauf 2003; Steketee 1996), one trial only reports symptoms which occurred in > 10% of participants in each study arm (Davis 1996). Vuurman 1996 only reported events which occurred more than once and Hale 2003 reports the total number of serious adverse events does not allocate them to a drug regimen.
Other potential sources of bias
Seven trials were sponsored by Roche (manufacturer of mefloquine) (Bunnag 1992; Davis 1996; Ohrt 1997; Santos 1993; Schlagenhauf 1997; Schlagenhauf 2003; Vuurman 1996), three were sponsored by GlaxoSmithKline (manufacturer of atovaquone‐proguanil) (Hale 2003; Overbosch 2001; Schlagenhauf 2003), one by Pfizer (manufacturer of doxycycline) (Ohrt 1997), and one by Mepha Ltd (manufacturer of a film‐coated form of mefloquine) (Potasman 2002). Only one made the role of the study sponsor clear (Ohrt 1997).
We have presented details of the risk of bias of cohort studies in the 'Effects of interventions' section.
Effects of interventions
Summary of findings for the main comparison. Mefloquine versus atovaquone‐proguanil for preventing malaria in travellers.
| Mefloquine compared with atovaquone‐proguanil for preventing malaria in travellers | ||||||
|
Population: non‐immune adults and children travelling to or living in malaria‐endemic settings Intervention: mefloquine 250 mg weekly Comparison: atovaquone‐proguanil (250 mg atovaquone and 100 mg proguanil hydrochloride) daily Outcome data collection: physicians performed blinded assessment of whether reported symptoms could be related to the study drug | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Studies contributing to effect estimate (participants) | Additional studies considered in GRADE assessment (participants) | Certainty of the evidence (GRADE) | |
| Atovoquone‐proguanil | Mefloquine | |||||
| Clinical malaria | — | — | — | 2 RCTs (1293) |
— | ⊕⊕⊝⊝ low1,2,3 |
| Serious adverse effects | 0 per 100 |
1 in 100 (0 to 12) |
RR 1.40 (0.08 to 23.22) |
4 cohort studies (3693) |
1 RCT (976) |
⊕⊕⊝⊝ low1,2,4,5 |
| Discontinuation of drug due to adverse effects | 2 per 100 |
6 per 100 (3 to 11) |
RR 2.86 (1.53 to 5.31) |
3 RCTs (1438) |
7 cohort studies (4498) |
⊕⊕⊕⊕ high1,2,4,6 |
| Abnormal dreams | 7 per 100 |
14 per 100 (10 to 21) |
RR 2.04 (1.37 to 3.04) |
1 RCT (976) |
7 cohort studies (3848) |
⊕⊕⊕⊕ high1,2,4,6 |
| Insomnia | 3 per 100 |
13 per 100 (8 to 23) |
RR 4.42 (2.56 to 7.64) |
1 RCT (976) |
8 cohort studies (3986) |
⊕⊕⊕⊕ high1,2,4,6 |
| Anxiety | 1 per 100 |
6 per 100 (2 to 21) |
RR 6.12 (1.82 to 20.66) |
1 RCT (976) |
4 cohort studies (2664) |
⊕⊕⊕⊝ moderate1,2,4,7 |
| Depressed mood | 1 per 100 |
6 per 100 (2 to 20) |
RR 5.78 (1.71 to 19.61) |
1 RCT (976) |
6 cohort studies (3624) |
⊕⊕⊕⊝ moderate1,2,4,7 |
| Abnormal thoughts or perceptions | 0 per 100 |
1 per 100 (0 to 4) |
RR 1.50 (0.30 to 7.42) |
3 cohort studies (2433) |
— | ⊕⊝⊝⊝ very low1,2,8 |
| Nausea | 3 per 100 |
8 per 100 (5 to 15) |
RR 2.72 (1.52 to 4.86) |
1 RCT (976) |
7 cohort studies (3509) |
⊕⊕⊕⊕ high1,2,4,6 |
| Vomiting | 1 per 100 |
1 per 100 (0 to 4) |
RR 1.31 (0.49 to 3.50) | 1 RCT (976) |
3 cohort studies (2180) |
⊕⊕⊕⊝ moderate1,2,4,7 |
| Abdominal pain | 5 per 100 |
5 per 100 (3 to 8) |
RR 0.90 (0.52 to 1.56) |
1 RCT (976) |
7 cohort studies (3509) |
⊕⊕⊝⊝ moderate1,2,4,8 |
| Diarrhoea | 8 per 100 |
8 per 100 (5 to 12) |
RR 0.94 (0.60 to 1.47) |
1 RCT (976) |
7 cohort studies (3509) |
⊕⊕⊕⊝ moderate1,2,4,8 |
| Headache | 4 per 100 |
7 per 100 (4 to 12) |
RR 1.72 (0.99 to 2.99) |
1 RCT (976) |
8 cohort studies (4163) |
⊕⊕⊕⊝ moderate1,2,4,8 |
| Dizziness | 2 per 100 |
8 per 100 (4 to 15) |
RR 3.99 (2.08 to 7.64) |
1 RCT (976) |
8 cohort studies (3986) |
⊕⊕⊕⊕ high1,2,4,6 |
| Pruritis | 2 per 100 |
3 per 100 (1 to 5) |
RR 1.28 (0.60 to 2.70) |
1 RCT (976) |
3 cohort studies (1824) |
⊕⊕⊕⊝ moderate1,2,4,8 |
| Visual impairment | 2 per 100 |
4 per 100 (2 to 9) |
RR 2.04 (0.88 to 4.73) |
1 RCT (976) |
2 cohort studies (1956) |
⊕⊕⊕⊝ moderate1,2,4,8 |
| Mouth ulcers | 2 per 100 |
3 per 100 (1 to 6) |
RR 1.45 (0.70 to 3.00) | 1 RCT (976) |
2 cohort studies (783) |
⊕⊕⊕⊝ moderate1,2,4,8 |
| *The assumed risk is the median control group risk across studies unless stated in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Where the control group risk was 0, we used a value of 0.5 to calculate the corresponding risk in the intervention group. Data from cohort studies were used when data from RCTs were unavailable.
Abbreviations: CI: confidence interval; RR: risk ratio 'Summary of findings' tables are usually limited to seven outcomes. For adverse effects this problematic, as there are many, and to include some and not others risks selective reporting. We have therefore included all prespecified outcomes in the table. | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
1No serious risk of bias: the RCTs were generally at low risk of bias but two of three were sponsored by the manufacturer of one of the study drugs. All cohort studies had methodological problems which could introduce confounding or bias. However, as the GRADE approach automatically downgrades certainty by two levels for non‐randomized studies, we did not downgrade further. 2No serious indirectness: the RCTs were conducted in short‐term international travellers to malaria‐endemic areas in Africa or South America for less than 28 days. The cohort studies were from a variety of populations including short‐term travellers (8 studies), longer‐term occupational travellers (3 studies) and military personnel (1 study). 3Downgraded by two levels for serious imprecision: no episodes of malaria were recorded in either trial. 4No serious inconsistency: the findings of the cohort studies were consistent with the effects seen in the RCTs. 5No serious imprecision: serious adverse effects were rare in all studies. 6No serious imprecision. The effect was statistically significant and the overall data (RCTs and cohort studies) were adequately powered to detect this effect. 7Downgraded by one level for serious imprecision: although the direction of the effect was consistent across all trials, there was substantial heterogeneity in the size of the effect. 8Downgraded by one level for serious imprecision: the 95% CI is wide and includes important effects and no effect.
Summary of findings 2. Mefloquine versus doxycycline for preventing malaria in travellers.
| Mefloquine compared with doxycycline for preventing malaria in travellers | ||||||
|
Population: Non‐immune adults and children travelling to malaria‐endemic settings Intervention: Mefloquine 250 mg weekly Comparison: Doxycycline 100 mg daily Outcome data collection: Self‐reported symptoms experienced whilst taking prophylaxis (adverse events) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Studies contributing to effect estimate (participants) | Additional studies considered in GRADE assessment (participants) | Certainty of the evidence (GRADE) | |
| Doxycycline | Mefloquine | |||||
| Clinical malaria | 1 per 100 |
1 per 100 (0 to 5) |
RR 1.35 (0.35 to 5.19) | 4 RCTs (744) |
— | ⊕⊕⊝⊝ low1,2,3,4 |
| Serious adverse effects | 6 per 10005 |
9 per 1000 (1 to 61) |
RR 1.53 (0.23 to 10.24) |
3 cohort studies (3722) |
3 RCTs, 1 cohort study (682; 3772) |
⊕⊝⊝⊝ very low2,3,6,7 |
|
Discontinuations due to adverse effects |
2 per 100 |
2 per 100 (1 to 6) |
RR 1.08 (0.41 to 2.87) |
4 RCTs (763) |
10 cohort studies (10,165) |
⊕⊕⊝⊝ low1,3,7,8 |
| Abnormal dreams | 3 per 100 |
31 per 100 (11 to 87) |
RR 10.49 (3.79 to 29.10) |
4 cohort studies (2588) |
1 RCT, 1 cohort study (123; 688) |
⊕⊝⊝⊝ very low2,6,9,10 |
| Insomnia | 3 per 100 |
12 per 100 (4 to 43) |
RR 4.14 (1.19 to 14.44) | 4 cohort studies (3212) |
1 RCT, 2 cohort studies (123; 355,627) |
⊕⊝⊝⊝ very low6,9,10,11 |
| Anxiety | 1 per 100 |
18 per 100 (9 to 35) |
RR 18.04 (9.32 to 34.93) |
3 cohort studies (2559) |
2 cohort studies (355,627) |
⊕⊝⊝⊝ very low6,9,10,11 |
| Depressed mood | 1 per 100 |
11 per 100 (5 to 25) |
RR 11.43 (5.21 to 25.07) |
2 cohort studies (2445) |
3 cohort studies (430,006) |
⊕⊝⊝⊝ very low6,9,10,11 |
| Abnormal thoughts or perceptions | 0 per 100 |
3 per 100 (0 to 24) |
RR 6.60 (0.92 to 47.20) |
2 cohort studies (2445) |
2 cohort studies (376,024) |
⊕⊝⊝⊝ very low6,9,10,11 |
| Nausea | 8 per 100 |
3 per 100 (2 to 4) |
RR 0.37 (0.30 to 0.45) |
5 cohort studies (2683) |
1 RCT, 1 cohort study (123; 668) |
⊕⊝⊝⊝ very low3,6,10,11 |
| Vomiting | 5 per 100 |
1 per 100 (1 to 1) |
RR 0.18 (0.12 to 0.27) |
4 cohort studies (5071) |
1 RCT (123) |
⊕⊝⊝⊝ very low3,6,10,11 |
| Abdominal pain | 15 per 100 |
5 per 100 (1 to 16) |
RR 0.30 (0.09 to 1.07) |
3 cohort studies (2536) |
1 RCT, 1 cohort (123; 668) |
⊕⊝⊝⊝ very low6,7,9,11 |
| Diarrhoea | 5 per 100 |
1 per 100 (1 to 4) |
RR 0.28 (0.11 to 0.73) |
5 cohort studies (5104) |
2 RCTs; 1 cohort study (376; 668) |
⊕⊝⊝⊝ very low3,6,10,11 |
| Dyspepsia | 14 per 100 |
4 per 100 (1 to 10) |
RR 0.26 (0.09 to 0.74) |
5 cohort studies (5104) |
— | ⊕⊝⊝⊝ low2,3,6,10 |
| Headache | 2 per 100 |
2 per 100 (1 to 6) |
RR 1.21 (0.50 to 2.92) |
5 cohort studies (3320) |
1 RCT, 1 cohort study (123; 688) |
⊕⊝⊝⊝ very low3,6,7,11 |
| Dizziness | 1 per 100 |
3 per 100 (1 to 14) |
RR 3.49 (0.88 to 13.75) |
5 cohort studies (2633) |
1 RCT, 2 cohort studies (123; 355,627) |
⊕⊝⊝⊝ very low3,6,7,11 |
| Visual impairment | 3 per 100 |
7 per 100 (4 to 12) |
RR 2.37 (1.41 to 3.99) |
2 cohort studies (1875) |
— | ⊕⊝⊝⊝ very low2,6,7,9 |
| Pruritis | 3 per 100 |
2 per 100 (1 to 3) |
RR 0.52 (0.30 to 0.91) |
2 cohort studies (1794) |
1 cohort study (688) |
⊕⊝⊝⊝ very low6,9,10,11 |
| Photosensitivity | 19 per 100 |
2 per 100 (1 to 2) |
RR 0.08 (0.05 to 0.11) |
2 cohort studies (1875) |
1 cohort study (688) |
⊕⊝⊝⊝ very low2,6,9,10 |
| Vaginal thrush | 16 per 100 |
2 per 100 (1 to 3) |
RR 0.10 (0.06 to 0.16) |
1 cohort study (1761) |
1 cohort study (354) |
⊕⊝⊝⊝ very low2,6,9,10 |
| *The assumed risk is the median control group risk across cohort studies unless stated in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Where the control group risk was 0, we used a value of 0.5 to calculate the corresponding risk in the intervention group. Where no RCTs including short‐term travellers reported on our prespecified adverse outcomes, we included information from cohort studies as our primary analysis. 'Summary of findings' tables are usually limited to seven outcomes. For adverse effects this problematic, as there are many, and to include some and not others risks selective reporting. We have therefore included all prespecified outcomes in the table. | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
1No serious risk of bias: none of the RCTs adequately described methods of random sequence generation or allocation concealment, However, given that so few events occurred in these trials, it is unlikely to have introduced bias. 2No serious inconsistency: the direction of the effect is consistent across study designs, or there in consistency in the finding of no effect. 3No serious indirectness: the primary analysis included studies in short‐term international travellers, longer‐term occupational travellers, and military personnel. 4Downgraded by two levels for imprecision: only seven episodes of clinical malaria occurred in the four trials, and consequently, the analysis was substantially underpowered to exclude important differences. 5For serious adverse outcomes we expressed the control group risk as the overall risk in the control group. 6No serious risk of bias: all cohort studies had methodological problems which could introduce confounding or bias. However, as the GRADE approach automatically downgrades certainty by two levels for non‐randomized studies, we did not downgrade further. 7Downgraded by one level for serious imprecision: the 95% confidence interval includes both clinically important effects and no effect. 8Downgrade by one level for serious inconsistency: although there was no substantial difference between drugs in the cohort studies, the proportion of discontinuations was higher with both drugs: 14% for mefloquine and 9% for doxycycline. 9Downgraded by one level for indirectness: the primary analysis included only cohort studies in longer‐term occupation travellers (USA Peace Corps volunteers) and military personnel. Adverse effects in shorter‐term international travellers may be lower. 10No serious imprecision: the effect was statistically significant and the overall data (RCTs and cohort studies) were adequately powered to detect this effect. 11Downgraded by one level for serious inconsistency: there was heterogeneity between trials in the direction of effect.
Comparison 1: Mefloquine versus placebo or no treatment
Description of studies
RCTs
Nine RCTs comparing prophylactic mefloquine with placebo reported efficacy (4032 participants, Table 5), and 13 reported safety outcomes (4293 participants, Table 6). The trials were conducted between 1977 and 2003, and none included participants travelling outside their home country. One trial conducted among soldiers in Indonesia described participants as non‐immune (Ohrt 1997), but immunity is likely to be low in other trials from Asia (Bunnag 1992; Nosten 1994; Pearlman 1980). The participants in four trials from Africa were described as semi‐immune (Hale 2003; Salako 1992; Sossouhounto 1995; Weiss 1995). Santos 1993 was conducted in an area of Brazil in which endemic transmission occurs.
3. Characteristics of included studies for efficacy.
| Study ID | Participants (immune status) | Number of randomised participants | Mefloquine dose | Drug comparisons of interest | Duration of exposure to malaria | Country of malaria exposure | Local drug resistance |
| Bunnag 1992 | Thai male adults (presumed semi‐immune) | 605 | 250 mg weekly for first 4 weeks, then 125 mg weekly | Placebo | 24 weeks (trial duration) | Thailand | Chloroquine, sulphadoxine‐pyrimethamine and quinine resistance |
| Nosten 1994 | Pregnant women from the Thai‐Burma border (presumed semi‐immune) | 339 | 250 mg weekly for first 4 weeks, then 125 mg weekly until delivery | Placebo | Various in endemic area (monitored until delivery) | Thai‐Burma border | Not mentioned |
| Pearlman 1980 | Thai residents aged 10 to 60 years (semi‐immune) | 990 | 180 mg tablet weekly, 360 mg tablet weekly, 360 mg every 2 weeks with appropriate adjustments for children | Placebo | 26 weeks | Thailand | Chloroquine resistant Plasmodium falciparum |
| Santos 1993 | Brazilian civilians and soldiers aged 12 to 55 years (semi‐immune) | 128 | 500 mg every 4 weeks, 250mg every 2 weeks | Placebo | 17 weeks | Brazil | P falciparum resistant to chloroquine and “high prevalence of multiresistant Plasmodium falciparum transmission” |
| Sossouhounto 1995 | Ivory Coast adult males (semi‐immune) | 500 | 250 mg weekly for first 4 weeks, then 125 mg weekly | Placebo | 20 weeks | Ivory C oast | Not mentioned |
| Ohrt 1997 | Indonesian soldiers ('largely' non‐immune) | 204 | 250 mg weekly | Placebo, doxycycline | 'approximately 13 weeks' | Indonesia | Sulfadoxine‐pyrimethamine and chloroquine resistance |
| Weiss 1995 | Kenyan children (semi‐immune) | 169 | 125 mg weekly | Placebo (multivitamin), doxycycline, primaquine | 11 weeks | Kenya | Not mentioned |
| Salako 1992 | Nigerian adult males (semi‐immune) | 567 | 250 mg weekly for first 4 weeks, then 125 mg weekly | Placebo, chloroquine | 24 weeks (trial duration) | Nigeria | "...at the time of the trial, chloroquine resistance was not a problem" |
| Hale 2003 | Ghanain adults (semi‐immune) | 530 | 250 mg weekly | Placebo | 12 weeks | Ghana | Not mentioned |
| Arthur 1990 | USA soldiers (non‐immune) | 270 | 250 mg weekly | Doxycycline | 8 weeks | Thailand | Local chloroquine resistance |
| Boudreau 1991 | Thai adult males (semi‐immune) | 501 | 500 mg fortnightly | Chloroquine | 14 weeks (trial duration) | Cambodia | Local chloroquine resistance |
| Steketee 1996 | Pregnant Malawian residents (semi‐immune) | 4220 | 250 mg weekly | Chloroquine | Various in endemic area (monitored until delivery) | Malawi | P falciparum resistant to chloroquine, documented sensitivity of P falciparum to mefloquine |
4. Mefloquine versus placebo/no treatment; characteristics of included studies for safety.
| Study ID | Participants | Number enrolled | Method of adverse event monitoring | Exclusions for psychiatric adverse effects | Trial duration | Source of funding |
| RCTs | ||||||
| Bunnag 1992 | Thai male adults | 605 | Interview with study personnel | None | 24 weeks | Roche |
| Davis 1996 | Australian adults who did not travel | 106 | Daily self‐reported diary | Past history of psychiatric conditions | 7 weeks | Roche |
| Hale 2003 | Ghanain adults | 530 | Interview with study personnel | History of neuropsychiatric illness | 12 weeks | USA Army |
| Nosten 1994 | Pregnant women, Thai‐Burma border | 339 |
Phase 1: weekly symptom questionnaire. Babies were assessed at birth and at 3, 6, 12, and 24 months. Phase 2: weekly symptom questionnaire. Babies were assessed at birth and at 2 and 9 months |
None | Various | Government funding |
| Ohrt 1997 | Indonesian soldiers | 204 | Two symptom questionnaires. Daily interview with study personnel | History of underlying illness | 13 weeks | Roche, Pfizer, USA Army |
| Pearlman 1980 | Thai residents aged 10 to 60 years | 990 | Weekly sick call by study personnel | None | 26 weeks | Not mentioned |
| Potasman 2002 | Israeli adults who did not travel | 90 | Self‐reporting diary | History of depression | 48 hours | Mepha Ltd |
| Salako 1992 | Nigerian adult males | 567 | Interview with study personnel | None | 24 weeks | Not mentioned |
| Santos 1993 | Brazilian civilians and soldiers aged 12 to 55 | 128 | Interview w ith study personnel | None | 17 weeks | Roche |
| Schlagenhauf 1997 | Swissair trainee pilots who did not travel | 23 | Interview with study personnel | Psychosis or severe depression | 4 weeks | Roche |
| Sossouhounto 1995 | Ivory C oast adult males | 500 | Access to the village health centre | None | 20 weeks | Not mentioned |
| Vuurman 1996 | Dutch adult who did not travel | 42 | Interview with study personnel | H istory of any serious psychiatric disorder; evidence of drug or alcohol abuse | 30 days | Roche |
| Weiss 1995 | Kenyan children | 169 | Interview with study personnel | None | 4 months | USA Army |
| Cohort studies | ||||||
| Participants | Number enrolled | Method of adverse event monitoring | Factors influencing drug allocation | Duration of travel | Source of funding | |
| Hoebe 1997 | Danish travellers | 300 | Telephone interview | Allocation based on guidelines and patient preference | Mean 3 weeks, range 1 to 9 weeks | Not mentioned |
| Petersen 2000 | Danish travellers | 4154 | Participant self‐reported questionnaire | Allocation based on guidelines and patient preference | Various, not specified | Not mentioned |
| Rietz 2002 | Swedish travellers | 491 | Participant self‐reported questionnaire | Allocation based on guidelines and patient preference | " Most", range 2 to 4 weeks | Not mentioned |
| van Riemsdijk 1997 | Danish travellers | 1501 | Participant self‐reported questionnaire | Allocation based on guidelines and patient preference | Mean = 23 days | Not mentioned |
| Wells 2006 | USA soldiers | 397,442 | Restrospective analysis of hospital records | No information available | Minimum 1 month | Government funding |
Seven trials used mefloquine at a dose of 250 mg weekly (or equivalent doses for children), four at 250 mg weekly for the first four weeks and then 125 mg weekly for the remainder of the study, and one trial used mefloquine doses of 500 mg every four weeks and 250 mg every two weeks (Santos 1993). Pearlman 1980 used mefloquine doses of 180 mg weekly, 360 mg weekly and 360 mg fortnightly. Trial duration varied from 48 hours to 26 weeks.
For safety, nine trials used interviews with study personnel to elicit adverse events (Bunnag 1992; Hale 2003; Nosten 1994; Ohrt 1997; Salako 1992; Santos 1993; Schlagenhauf 1997; Vuurman 1996; Weiss 1995). Of these, six trials questioned participants about symptoms at least weekly (Hale 2003; Nosten 1994; Ohrt 1997; Salako 1992; Vuurman 1996; Weiss 1995). Two trials used participant self‐reported diaries to record any adverse events (Davis 1996, Potasman 2002). Pearlman 1980 used a weekly 'sick call' by study personnel and Sossouhounto 1995 provided 'access to the village health centre'. Only two trials used explicit definitions for adverse events and effects that allow for reproducible ascertainment (Davis 1996, Vuurman 1996). For safety outcomes, nine of the 13 trials adequately described how adverse events were ascertained. Eleven trials actively sought adverse events, and all 13 collected data prospectively (Table 7).
5. Mefloquine versus placebo/no treatment; quality of adverse events reporting.
| Study ID | Description of how adverse outcomes were defined and recorded¹ | Description of ascertainment technique² | Active or passive monitoring? | Prospective or retrospective data collection? |
| Bunnag 1992 | Inadequate Comment: No definition of adverse events or effects was provided, it is unclear whether or how causality was assessed |
Adequate | Active | Prospective |
| Davis 1996 | Adequate | Adequate | Active | Prospective |
| Hale 2003 | Inadequate Comment: ‘serious’ adverse events were not defined, and methods for determining causality not described |
Adequate | Active | Prospective |
| Nosten 1994 | Inadequate Comment: It is unclear what questions were included within the questionnaire and whether and how causality was assessed. ‘Serious’ adverse effects not defined |
Adequate | Active | Prospective |
| Ohrt 1997 | Inadequate Comment: No definition of adverse events or effects provided, it was unclear whether or how causality was assessed |
Adequate | Active | Prospective |
| Pearlman 1980 | Inadequate Comment: No definition of adverse events or effects was provided, it was unclear whether or how causality was assessed |
Inadequate Comment: Weekly sick call for all villagers |
Passive | Prospective |
| Potasman 2002 | Inadequate Comment: No definition of adverse events or effects was provided, it was unclear whether or how causality was assessed |
Adequate | Active | Prospective |
| Salako 1992 | Inadequate Comment: No definition of adverse events or effects was provided, it was unclear whether or how causality was assessed |
Adequate | Active | Prospective |
| Santos 1993 | Inadequate Comment: No information given in the methods section on definition of adverse outcomes |
Inadequate Comment: No description of ascertainment method |
Active | Prospective |
| Schlagenhauf 1997 | Inadequate Comment: No definition of adverse events or effects was provided, it was unclear whether or how causality was assessed |
Adequate | Active | Prospective |
| Sossouhounto 1995 | Inadequate Comment: No definitions of adverse events or effects were provided, it was unclear whether or how causality was assessed |
Unclear | Passive | Prospective |
| Vuurman 1996 | Adequate | Unclear | Active | Prospective |
| Weiss 1995 | Inadequate Comment: No definitions of adverse events or effects were provided, it was unclear whether or how causality was assessed. |
Adequate | Active | Prospective |
| Cohort studies | ||||
| Hoebe 1997 | Adequate | Adequate | Active | Retrospective |
| Petersen 2000 | Adequate | Adequate | Active | Retrospective |
| Rietz 2002 | Adequate | Adequate | Active | Unclear 'Filled in after their return' |
| Steffen 1993 | Adequate | Adequate | Passive | Unclear Comment: information was collected during the flight home, when travellers should still have been taking their prophylactic regimen |
| van Riemsdijk 1997 | Adequate | Adequate | Active | Prospective |
| Wells 2006 | Adequate | Adequate | Passive | Retrospective |
1. Were harms pre‐defined using standardised or precise definitions?
2. Was ascertainment technique adequately described?
Eleven of thirteen which assessed safety outcomes trials did not adequately describe random sequence generation or allocation concealment, and eight did not adequately describe how outcome assessors and study personnel were blinded. We judged eight trials to be at high risk of selective outcome reporting with regard to safety outcomes. In two trials, this was because the overall number of adverse events in each study arm was reported, but not the type or severity (Bunnag 1992; Potasman 2002). Davis 1996 reported only adverse events that occurred in more than 10% of participants in both study arms; Vuurman 1996 reported only adverse events that occurred more than once; and Nosten 1994 only reported on adverse events in the second phase of the trial.
Five trials were funded by Roche (manufacturer of mefloquine) (Bunnag 1992; Davis 1996; Santos 1993; Schlagenhauf 1997; Vuurman 1996) and one by GlaxoSmithKline (manufacturer of atovaquone‐proguanil) (Hale 2003) and one by Mepha Ltd (manufacturer of a film‐coated form of mefloquine) (Potasman 2002).
Cohort studies
Five cohort studies compared mefloquine users with participants who travelled but did not take antimalarial prophylaxis at all (Hoebe 1997; Petersen 2000; Rietz 2002; van Riemsdijk 1997; Wells 2006). Four of these were conducted in travellers, and one in military personnel (Table 6).
Two cohort studies included travellers who were prescribed an antimalarial agent but did not commence using (Hoebe 1997; Petersen 2000) and two asked travellers about an extensive list of general complaints which could have occurred during their journey (Rietz 2002; van Riemsdijk 1997). Wells 2006 was a retrospective healthcare record analysis looking at hospitalizations in active‐duty USA military personnel (397, 442 participants).
Two cohort studies had non‐response rates of over 20%. Wells 2006 was at serious risk for selection of participants and measurement of outcomes because start of follow up began after participants had finished taking mefloquine, authors used surrogate measures for mefloquine exposure and there was a possibility that some participants in the reference groups took mefloquine. Four cohort studies actively sought information from participants about adverse events and only one (van Riemsdijk 1997) obtained information prospectively (see Figure 3).
3.
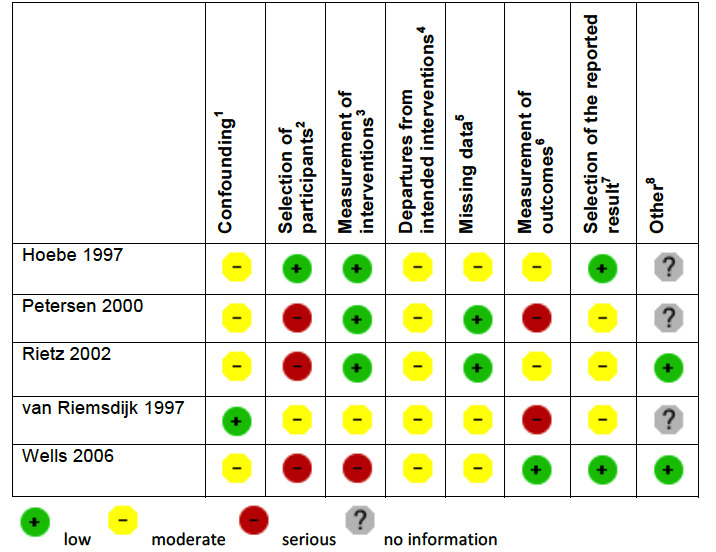
'Risk of bias' summary in cohort studies: mefloquine versus placebo/no treatment
1Assesses whether our pre‐defined confounders were measured and balanced across groups. 2Assesses the non‐response rate of prospective participants. 3Assesses the risk that participants labelled as taking mefloquine (or another antimalarial) actually took something else. 4Assesses the risk that participants whose adverse effects are attributed to mefloquine (or another antimalarial) actually took another drug as well. 5Assesses whether outcome data reasonably complete for most participants and whether intervention status reasonably complete for those in whom it was sought. 6Assesses whether the outcome measure was subjective, and whether participants and outcome assessors were blinded. 7Assesses whether it is clear that all information collected within the study has been reported. 8Assess the risk of bias due to influence by a corporate study sponsor.
Efficacy
Mefloquine is highly efficacious in reducing clinical cases of malaria compared to placebo, although there were important differences among trials, particularly regarding the dose of mefloquine used, populations studied and the risk of malaria in the control group (Analysis 1.1). The risk of malaria was highest in the trial in military personnel travelling to Indonesia, described as "largely non‐immune", where 53/65 (81%) of those in the placebo group had an episode of malaria compared to 0/67 (0%) with mefloquine (RR 0.01, 95% CI 0.00 to 0.16; Ohrt 1997, 126 participants). In the remaining trials the risk of malaria with placebo ranged from 1% to 59% (Bunnag 1992; Hale 2003; Nosten 1994; Pearlman 1980; Salako 1992; Santos 1993; Sossouhounto 1995; Weiss 1995).
1.1. Analysis.
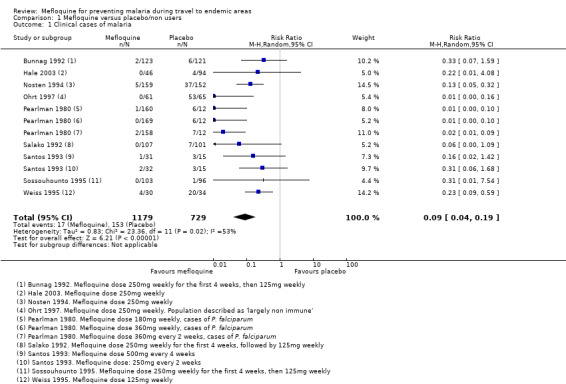
Comparison 1 Mefloquine versus placebo/non users, Outcome 1 Clinical cases of malaria.
Although quantitative heterogeneity was high, the direction of the effect was consistent across all trials. We performed a series of subgroup analyses by dose and immune status of participants, but this did not explain the heterogeneity or provide a reliable point estimate of efficacy with subgroups.
Five trials also reported the effect on parasitaemia (which was much more common than clinical malaria) (Hale 2003; Nosten 1994; Salako 1992; Sossouhounto 1995; Weiss 1995). Overall, mefloquine reduced numbers of participants who developed parasitaemia by around 80% (RR 0.18, 95% CI 0.06 to 0.55; 3 trials, 414 participants, Analysis 1.2), and substantially reduced the number of episodes of parasitaemia (RR 0.05, 95% CI 0.00 to 5.25; 2 trials, 510 participants, Analysis 1.2).
1.2. Analysis.
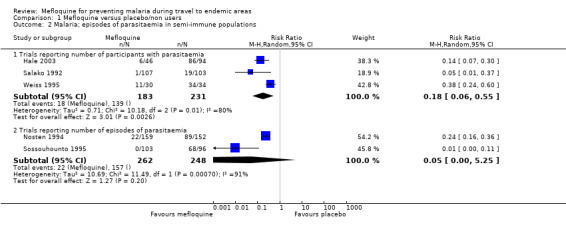
Comparison 1 Mefloquine versus placebo/non users, Outcome 2 Malaria; episodes of parasitaemia in semi‐immune populations.
Safety
Serious adverse events or effects
Only three serious adverse events were reported from six RCTs, none of which were attributed to the drug regimen (1/592 mefloquine users versus 2/629 placebo; 6 trials; 1221 participants, Analysis 1.3). The serious event in the mefloquine user was the death of a pregnant woman who received mefloquine (septic shock after an emergency caesarean section for obstructed labour) (Nosten 1994). For serious pregnancy‐related outcomes, Nosten 1994 reported four congenital malformations in the mefloquine group: limb dysplasia (1 case), ventricular septal defect (2 cases), amniotic bands (1 case) and one in the placebo group: anencephaly. All were considered unrelated to the drug regimen (Table 8).
1.3. Analysis.
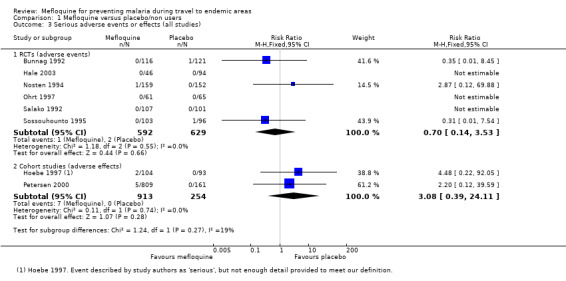
Comparison 1 Mefloquine versus placebo/non users, Outcome 3 Serious adverse events or effects (all studies).
6. Serious adverse events; mefloquine versus comparators.
| Study ID | Study design | Mefloquine users | Drug comparators | |||
| Events/ participants | Description | Drug | Events/ participants | Description | ||
| Events (not attributed by study authors or participants to the drug regimen) | ||||||
| Bunnag 1992 | RCT | 0/116 | ‐ | Placebo | 1/121 | None provided |
| Nosten 1994 | RCT | 1/159 (women) | One death
Four congenital malformations:
|
Placebo | 0/152 (women) | One congenital malformation:
|
| Sossouhounto 1995 | RCT | 0/103 | ‐ | Placebo | 1/96 | One death (not described) |
| Ohrt 1997 | RCT | 0/61 | ‐ | Placebo | 0/65 | ‐ |
| Doxycycline | 1/62 | Acute hysteria¹ | ||||
| Lobel 2001 | Cohort study | 8/3703 | 8 hospitalisations
|
Doxycycline | 0/69 | ‐ |
| Chloroquine | 0/119 | ‐ | ||||
| Overbosch 2001 | RCT | 10/483 | "...infectious illnesses in 7 subjects and breast cancer, anaphylaxis, or fractured femur in 1 subject each" | Atovaquone‐proguanil | 4/493 | "...infectious illnesses in 3 subjects and cerebral ischemia in 1 subject" |
| Studies reporting no serious events or effects | ||||||
| Salako 1992 | RCT | 0/107 | "Adverse events were all mild and there were no deaths" | Placebo Chloroquine |
0/101 0/103 |
‐ ‐ |
| Arthur 1990 | RCT | 0/134 | "No serious side effects occurred with either drug regimen" | Doxycycline | 0/119 | ‐ |
| Schlagenhauf 2003 | RCT | 0/153 | "Although a large number of adverse events were reported, none were serious" | Doxycycline Atovaquone‐proguanil |
0/153 0/164 |
‐ ‐ |
| Sonmez 2005 | Cohort study | 0/228 | "No drug induced side effects necessitating emergency care were observed" | Doxycycline | 0/506 | ‐ |
| Andersson 2008 | Cohort study | 0/491 | "No serious adverse events were recorded" | Atovaquone‐proguanil | 0/161 | ‐ |
| Napoletano 2007 | Cohort study | 0/548 | Records hospitalisations, and reports that none occurred in either group of participants | Atovaquone‐proguanil Chloroquine |
0/707 0/37 |
‐ ‐ |
| Sossouhounto 1995 | RCT | 0/103 | "All side effects were transient (and)... mild" | Chloroquine | 0/100 | ‐ |
1 This trial described a potentially serious adverse event, but did not provide enough detail to meet our definition.
By comparison in cohort studies, seven serious adverse effects (all attributed by study authors to the drug regimen) were reported among 913 mefloquine users, compared to none in 254 travellers who did not use antimalarials (RR 3.08, 95% CI 0.39 to 24.11; 2 studies, 1167 participants; Analysis 1.3; Table 9). Five of these were psychological (depression) and two were neurological adverse effects (dizziness).
7. Serious adverse effects; mefloquine versus comparators.
| Study ID | Study design | Mefloquine users | Drug comparators | |||
| Events/ participants | Description | Drug | Events/ participants | Description | ||
| Effects (attributed by study authors or participants to the drug regimen) | ||||||
| Hoebe 1997 | Cohort study | 2/104 | Two "serious acute adverse reactions"¹
|
No treatment | 0/93 | ‐ |
| Petersen 2000 | Cohort study | 5/809 | 5 hospitalisations:
|
Chloroquine | 6/1223 | 2 hospitalisations:
|
| No treatment | 0/161 | ‐ | ||||
| Korhonen 2007 | Cohort study | 15/1612 | 15 hospitalisations:
|
Doxycycline | 9/708 | 9 hospitalisations:
|
| Atovaquone‐proguanil | 0/72 | ‐ | ||||
| Chloroquine | 4/832 | 4 hospitalisations:
|
||||
| Philips 1996 | Cohortstudy | 4/285 | 3 hospitalisations with "either gastrointestinal or neurologic symptoms" and one seizure | Doxycycline | 1/383 | Severe oesophagitis |
| Steketee 1996 | RCT | 1/? | One "neuropsychiatric side effect"
|
Chloroquine | 0/? | ‐ |
| Albright 2002 | Cohort study | 1/115 | One "serious side effect"¹
|
Chloroquine | 0/22 | ‐ |
| Corominas 1997 | Cohort study | 1/609 | One hospitalisation:
|
Chloroquine | 0/137 | ‐ |
| Steffen 1993 | Cohort study | 7/52981 | 7 hospitalisations, including:
|
Chloroquine | 7/20332 | 7 hospitalisations. 'Includes':
|
| Studies reporting no serious events or effects | ||||||
| Hale 2003 | RCT | 0/46 | Nine serious adverse events in the trial (trial arm not specified) "none of which were considered by study physicians to be related to the study drug" | Placebo | 0/94 | ‐ |
| Salako 1992 | RCT | 0/107 | "Adverse events were all mild and there were no deaths" | Placebo Chloroquine |
0/101 0/103 |
‐ ‐ |
| Arthur 1990 | RCT | 0/134 | "No serious side effects occurred with either drug regimen" | Doxycycline | 0/119 | ‐ |
| Schlagenhauf 2003 | RCT | 0/153 | "Although a large number of adverse events were reported, none were serious" | Doxycycline Atovaquone‐proguanil |
0/153 0/164 |
‐ ‐ |
| Sonmez 2005 | Cohort study | 0/228 | "No drug induced side effects necessitating emergency care were observed" | Doxycycline | 0/506 | ‐ |
| Andersson 2008 | Cohort study | 0/491 | "No serious adverse events were recorded" | Atovaquone‐proguanil | 0/161 | ‐ |
| Napoletano 2007 | Cohort study | 0/548 | Records hospitalisations, and reports that none occurred in either group of participants | Atovaquone‐proguanil Chloroquine |
0/707 0/37 |
‐ ‐ |
| Sossouhounto 1995 | RCT | 0/103 | "All side effects were transient (and)... mild" | Chloroquine | 0/100 | ‐ |
¹ This trial described a potentially serious adverse effect, but did not provide enough detail to meet our strict definition.
Wells 2006 was a retrospective healthcare record analysis that reported adverse events. It compared numbers of hospitalizations in military personnel who had been prescribed mefloquine and were deployed to active duty in malarial areas, with those who had been deployed to non‐malarial areas, and with military personnel with duty zip codes for Europe or Japan, who had not been deployed to active duty. Mefloquine users were less likely to be hospitalized (after deployment) with mood disorders (RR 0.38, 95% CI 0.17 to 0.86; 241,239 participants) or for any cause (RR 0.60, 95% CI 0.51 to 0.71; 241,239 participants) than military personnel who did not receive any antimalarial agents (but who were deployed to a war zone).
Discontinuations due to adverse effects
Within RCTs the number of people who discontinued the study drug due to adverse effects was low in both groups: 6/541 (1.1%) with mefloquine versus 4/583 (0.7%) with placebo (RR 1.64, 95% CI 0.55 to 4.88; 7 trials, 1124 participants, Analysis 1.4). No comparative data were available on this outcome from cohort studies because the comparison was with no treatment.
1.4. Analysis.
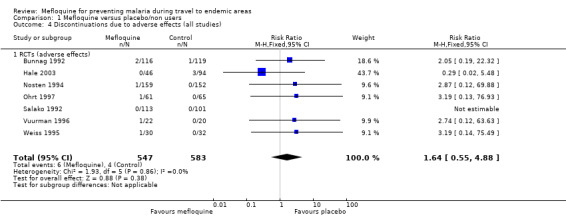
Comparison 1 Mefloquine versus placebo/non users, Outcome 4 Discontinuations due to adverse effects (all studies).
Prespecified adverse events or effects
None of the RCTs or cohort studies for this comparison reported on adverse effects (symptoms attributed by researchers or participants to the drug regimen). All comparisons were for adverse events (all symptoms that occurred while taking the study drug).
Gastrointestinal symptoms
Within RCTs, participants who received mefloquine were more likely to experience nausea than those who took placebo (RR 1.35, 95% CI 1.05 to 1.73; 2 trials, 244 participants, Analysis 1.5), but there was no difference between groups for vomiting, abdominal pain or diarrhoea (Analysis 1.6; Analysis 1.7; Analysis 1.8). The results from cohort studies were consistent with this finding, with more mefloquine users experiencing nausea (RR 1.85, 95% CI 1.42 to 2.43; 3 studies, 1901 participants, Analysis 1.5).
1.5. Analysis.
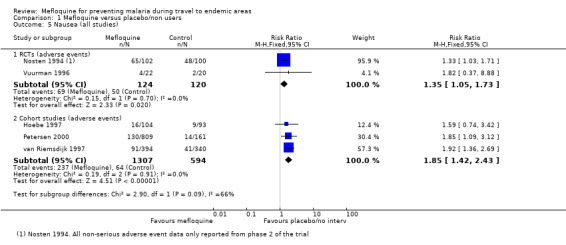
Comparison 1 Mefloquine versus placebo/non users, Outcome 5 Nausea (all studies).
1.6. Analysis.
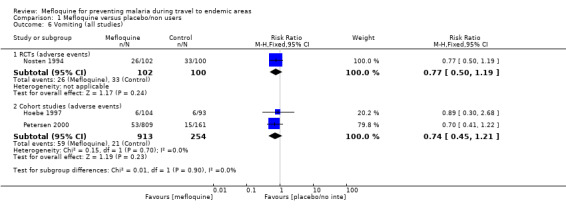
Comparison 1 Mefloquine versus placebo/non users, Outcome 6 Vomiting (all studies).
1.7. Analysis.
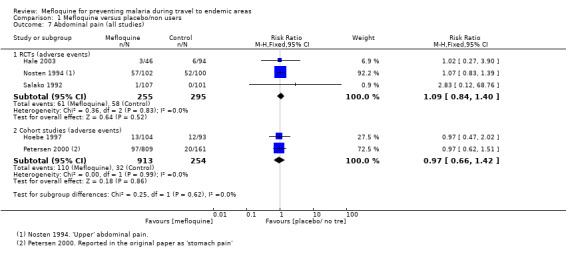
Comparison 1 Mefloquine versus placebo/non users, Outcome 7 Abdominal pain (all studies).
1.8. Analysis.
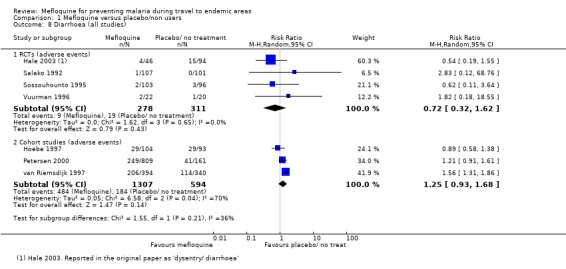
Comparison 1 Mefloquine versus placebo/non users, Outcome 8 Diarrhoea (all studies).
One RCT in pregnant women (Nosten 1994) reported on both upper and lower abdominal pain. Inclusion of both groups of results in sensitivity analyses had no impact on the results.
Neurological symptoms
Mefloquine users in RCTs were no more likely that recipients who took placebo to experience headache (RR 0.84, 95% CI 0.71 to 0.99; 5 trials, 791 participants, Analysis 1.9) or dizziness (RR 1.03, 95% CI 0.90 to 1.17; 3 trials, 452 participants, Analysis 1.10). This is in contrast to cohort studies, in which participants who took mefloquine were significantly more likely to experience dizziness than participants who travelled but took no prophylaxis (RR 1.80, 95% CI 1.29 to 2.49; 3 studies, 1901 participants, Analysis 1.10).
1.9. Analysis.
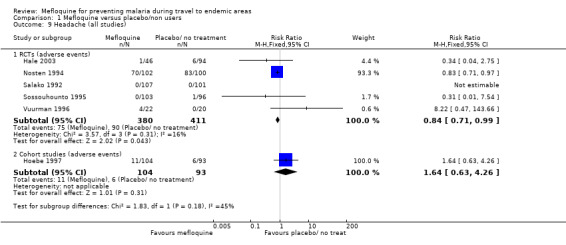
Comparison 1 Mefloquine versus placebo/non users, Outcome 9 Headache (all studies).
1.10. Analysis.
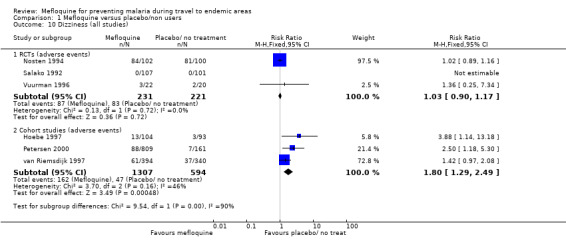
Comparison 1 Mefloquine versus placebo/non users, Outcome 10 Dizziness (all studies).
Psychological symptoms
None of the RCTs included in the analysis reported on any of our prespecified psychological symptoms. Participants in cohort studies who received mefloquine were more likely than participants who did not take prophylaxis to experience abnormal dreams (RR 2.35, 95% CI 1.15 to 4.80; 2 cohort studies, 931 participants, Analysis 1.11), and insomnia (RR 1.46, 95% CI 1.06 to 2.02; 2 cohort studies, 931 participants, Analysis 1.12). Effects on anxiety (RR 1.21, 95% CI 0.67 to 2.21; 2 cohort studies, 931 participants; I² statistic = 48%; Analysis 1.13), depressed mood (RR 2.43, 95% CI 0.65 to 9.07; 3 cohort studies, 1901 participants, I² statistic = 72%, Analysis 1.14) and abnormal thoughts or perceptions (RR 5.77, 95% CI 0.79 to 42.06; 1 cohort study, 970 participants, Analysis 1.15), were not consistent across studies, and overall, did not reach standard levels of statistical significance.
1.11. Analysis.
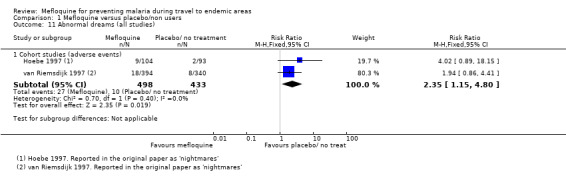
Comparison 1 Mefloquine versus placebo/non users, Outcome 11 Abnormal dreams (all studies).
1.12. Analysis.
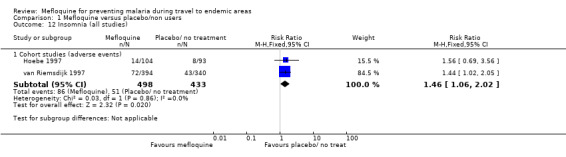
Comparison 1 Mefloquine versus placebo/non users, Outcome 12 Insomnia (all studies).
1.13. Analysis.
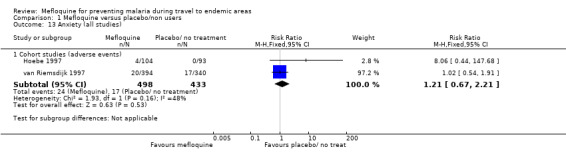
Comparison 1 Mefloquine versus placebo/non users, Outcome 13 Anxiety (all studies).
1.14. Analysis.
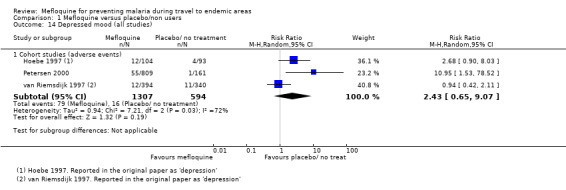
Comparison 1 Mefloquine versus placebo/non users, Outcome 14 Depressed mood (all studies).
1.15. Analysis.
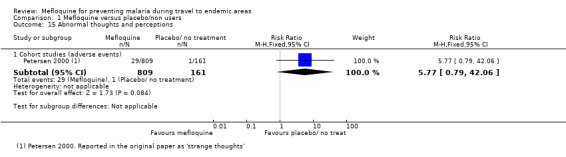
Comparison 1 Mefloquine versus placebo/non users, Outcome 15 Abnormal thoughts and perceptions.
Other symptoms
Mefloquine users in cohort studies were more likely to experience pruritis (RR 6.71, 95% CI 1.58 to 28.55; 1 cohort study, 197 participants, Analysis 1.16). However, this finding was not replicated in RCTs (RR 0.86, 95% CI 0.60 to 1.24; 3 RCTs, 609 participants, Analysis 1.16). There was no difference between groups for visual impairment and vertigo in either RCTs nor cohort studies (Analysis 1.17; Analysis 1.18).
1.16. Analysis.
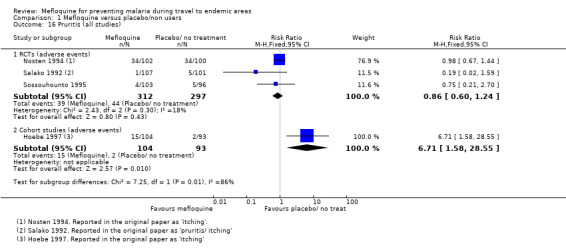
Comparison 1 Mefloquine versus placebo/non users, Outcome 16 Pruritis (all studies).
1.17. Analysis.
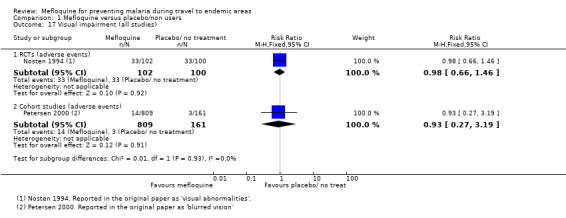
Comparison 1 Mefloquine versus placebo/non users, Outcome 17 Visual impairment (all studies).
1.18. Analysis.
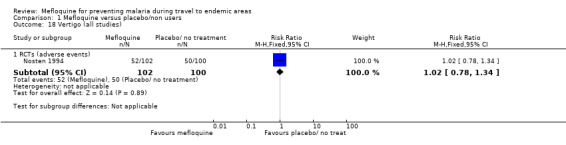
Comparison 1 Mefloquine versus placebo/non users, Outcome 18 Vertigo (all studies).
Other adverse events reported in more than 1% of study participants (in either study arm) in RCTs and cohort studies are presented in Analysis 1.19 and Analysis 1.20. Only respiratory tract infection reached statistical significance between groups; data were from a single trial with few events (RR 2.63, 95% CI 1.04 to 6.61; 1 trial, 140 participants).
1.19. Analysis.
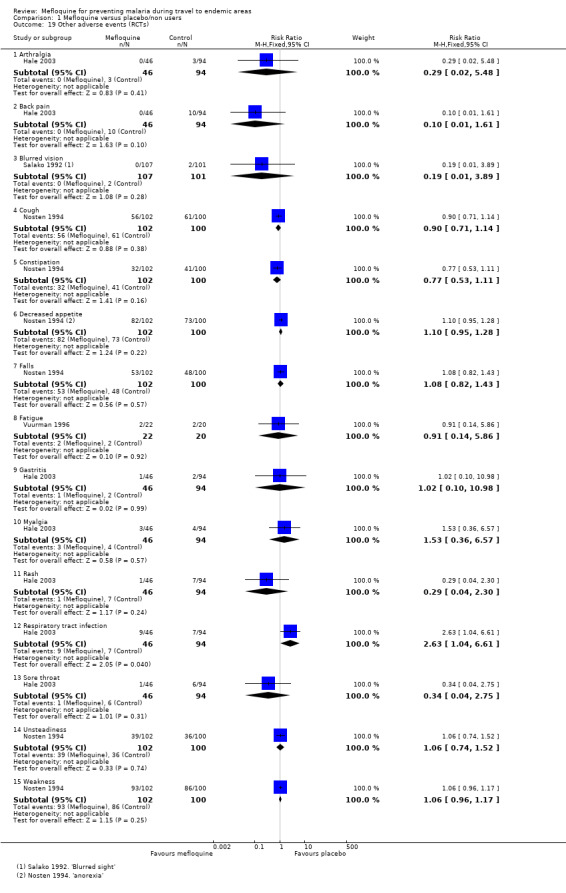
Comparison 1 Mefloquine versus placebo/non users, Outcome 19 Other adverse events (RCTs).
1.20. Analysis.
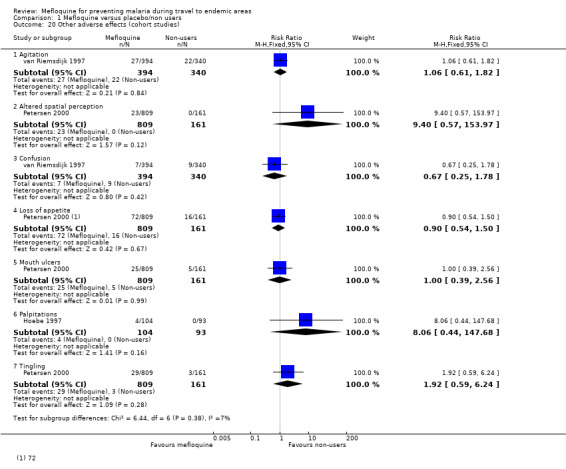
Comparison 1 Mefloquine versus placebo/non users, Outcome 20 Other adverse effects (cohort studies).
Studies reporting groups of symptoms or other outcomes which could be used as proxy markers of psychological or neurological adverse effects are reported in Appendix 4.
Pregnancy outcomes
Nosten 1994 conducted an RCT in pregnant women over 20 weeks gestation. There was no reported difference between mefloquine and placebo for spontaneous abortions (RR 0.48, 95% CI 0.04 to 5.22; 311 participants), still births (RR 2.63, 95% CI 0.86 to 8.08; 311 participants) or congenital malformations (RR 3.82, 95% CI 0.43 to 33.83; 311 pregnant women). However, the trial was significantly underpowered to evaluate these outcomes.
Adherence
In their RCT, Davis 1996 reported on any measure of adherence to the drug regimen assessed by pill count and direct questioning. Reported adherence was 100% in both arms.
Comparison 2: Mefloquine versus doxycycline
Description of studies
RCTs
Four RCTs, enrolling 1317 participants, reported on both efficacy and safety (Table 10). One was conducted in short‐term travellers (Schlagenhauf 2003), two in military personnel (Arthur 1990; Ohrt 1997) and one in Kenyan children (Weiss 1995). The populations were described as non‐immune (Arthur 1990; Schlagenhauf 2003), "largely" non‐immune (Ohrt 1997) and semi‐immune (Weiss 1995). Trial duration varied from four weeks to four months. The method for detecting malaria was unclear in two trials (Arthur 1990; Schlagenhauf 2003). Three studies conducted daily interviews with participants to monitor for adverse events (Arthur 1990; Ohrt 1997; Weiss 1995) and one used a participant self‐reporting questionnaire (Schlagenhauf 2003).
8. Mefloquine versus doxycycline; characteristics of included studies for safety.
| Study ID | Participants | Number enrolled | Method of adverse event monitoring | Significant exclusions for psychiatric adverse effects | Duration of travel | Source of funding |
| Randomized controlled trials | ||||||
| Arthur 1990 | USA soldiers | 270 | Blood tests, stool samples. Interview with study personnel | None | 5 weeks | Not mentioned |
| Ohrt 1997 | Indonesian soldiers | 204 | Interview with study personnel. Exit questionnaire | " History of underlying illness" | 13 weeks | Pfizer and Roche |
| Schlagenhauf 2003 | Non‐immune adult short‐term travellers | 674 | Participant self‐reported questionnaire | History of seizures or psychiatric disorders | 4 to 6 weeks | GlaxoSmithKline and Roche |
| Weiss 1995 | Kenyan children | 169 | Interview with study personnel | None | 4 months | Government funding |
| Non‐randomized studies | ||||||
| Participants | Number enrolled | Method of adverse event monitoring | Factors influencing drug allocation | Duration of travel | Source of funding | |
| Cunningham 2014 | UK Foreign and Commonwealth Office staff | 327 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | 0 to 36 months | Not mentioned |
| Eick‐Cost 2017 | USA s oldiers | 367,840 | Data from the Defense Medical Surveillance System, the Pharmacy Data Transaction Service and the Theater Medical Data Store | No information available | Various, not specified | Not mentioned |
| Goodyer 2011 | UK adult short‐term travellers | 185 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | < 28 days | GlaxoSmithKline |
| Korhonen 2007 | Peace Corps volunteers | 2701 | Participant self‐reported questionnaire | Allocation based on guidelines and participan t preference | ≥ 6 months | Two staff employed by Peace Corps |
| Landman 2015 | Peace Corps volunteers | 1184 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Various, not specified | Not mentioned |
| Laver 2001 | Adult short‐term travellers | 660 | Participant self‐reported questionnaire | No information available | 93% < 4 weeks | " No financial interests to disclose" |
| Lobel 2001 | Adult short‐term travellers | 5626 | Participant self‐reported questionnaire | No information available | < 5 weeks | " No financial interests to disclose" |
| Meier 2004 | UK adults enrolled in UK g eneral p ractice research database | 35,370 | Incident cases of depression, psychoses and panic attacks within the UK general practice research database | No information available | Various, not specified | Roche |
| Napoletano 2007 | Italian short‐term travellers | 1906 | Telephone interview | Allocation based on guidelines and participant preference | Mean 2 weeks, range 0 to > 35 days | Not mentioned |
| Philips 1996 | Australian short‐term travellers | 741 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Various, mean 3 weeks, maximum 3 months | Roche and Pfizer |
| Saunders 2015 | USA soldiers | 2351 | Participant self‐reported questionnaire | Primarily doxycycline, soldiers with contra‐indications received mefloquine | > 90% for 10 months or more | Not mentioned |
| Schwartz 1999 | Israeli short‐term travellers | 158 | Participant self‐reported questionnaire | "... daily doxycycline or daily primaquine... was recommended" | 14 to 20 days | Not mentioned |
| Shamiss 1996 | Israeli soldiers | 45 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | "... an average of 4 hours stay in the field over a period of 2 months" | Not mentioned |
| Sharafeldin 2010 | Dutch medical students | 180 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Mean 74 days (range 10 to 224 days) | No dedicated funding |
| Sonmez 2005 | Turkish soldiers | 1400 | Participant self‐reported questionnaire | Prior to March 2002: doxycyline After July 2002: mefloquine |
A pprox. 6 months | Not mentioned |
| Stoney 2016 | USA short‐term travellers | 370 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Median duration 13 days | Government funding |
| Tan 2017 | Peace Corps volunteers | 8931 | Participant self‐reported questionnaire | No information available | Various, not specified | No dedicated funding |
| Terrell 2015 | UK soldiers | 2032 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Median duration 13 days | "... not funded by an external body" |
| Tuck 2016 | UK soldiers | 151 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Various, not specified | No dedicated funding |
| Waner 1999 | Adult short‐term travellers | 3051 | Participant self‐reported questionnaire | No information available | A pprox. 6 weeks | Not mentioned |
None of the RCTs adequately described allocation concealment. Blinding of participants was adequately described in all but Weiss 1995; two trials did not adequately describe how outcome assessors were blinded (Arthur 1990; Schlagenhauf 2003). We also considered Ohrt 1997 and Schlagenhauf 2003 to be at high risk of selective outcome reporting because they did not report all collected data: Ohrt 1997 completed an exit questionnaire within the last month of the study, but did not report all results; Schlagenhauf 2003 collected data at baseline, twice before travel and once on return, but only presented data for participants "who completed questionnaires at recruitment and at least one of the follow up periods". All four studies collected information on adverse events actively and prospectively (Table 11). Schlagenhauf 2003 was funded by GlaxoSmithKline (manufacturer of atovaquone‐proguanil) and Roche (manufacturer of mefloquine) and Ohrt 1997 was funded by Roche and Pfizer (manufacturers of doxycycline) but specified that "neither of the pharmaceutical companies that provided support played any role in the gathering, analysing or interpreting the data".
9. Mefloquine versus doxycycline; quality of adverse event reporting.
| Study ID | Harms predefined¹ | Description of ascertainment technique² | Active or passive monitoring?³ | Prospective or retrospective data collection? |
| RCTs | ||||
| Arthur 1990 | Inadequate: No definitions provided for serious side effects |
Unclear: it is not reported who conducted the interviews | Active | Prospective |
| Ohrt 1997 | Inadequate Comment: No definitions of adverse events or effects were provided, it wa s unclear whether or how causality was assessed |
Adequate | Active | Prospective |
| Schlagenhauf 2003 | Adequate | Adequate | Active | Prospective |
| Weiss 1995 | Inadequate " Each subject was visited daily at home by an assigned field worker, who asked about symptoms of malaria or drug side effects" |
Adequate | Active | Prospective |
| Cohort studies | ||||
| Cunningham 2014 | Inadequate Comment: questionnaire included a targeted list of side effects, including " other psychological problems" . What was included within this was not defined |
Adequate | Passive | Unclear Comment: questionnaire was performed while participants were still taking chemoprophylaxis medication, although 75% were non‐compliant |
| Eick‐Cost 2017 | Adequate | Adequate | Passive | Prospective |
| Goodyer 2011 | Inadequate " Also included on the questionnaire was a single free‐text question asking travellers to describe any side effects of antimalarial medication" |
Adequate | Active | Retrospective |
| Korhonen 2007 | Adequate | Adequate | Passive | Unclear Comment: n o information wa s provided regarding the timing of the questionnaire during treatment |
| Landman 2015 | Adequate | Adequate | Passive | Unclear Comment: all participants were emailed the questionnaire at one time point, which occurred at varying points during the prophylactic regimen |
| Lobel 2001 | Inadequate "Travellers… were given a questionnaire that asked for... adverse health events attributed to those drugs" |
Adequate | Passive | Unclear Comment: information was collected at the airport, when travellers should still have been taking the prophylactic regimen |
| Meier 2004 | Adequate | Adequate | Passive | Retrospective |
| Napoletano 2007 | Unclear Comment: adverse events were categorised on a scale of one to four, but it is unclear whether and how causality was assessed |
Adequate | Active | Retrospective |
| Philips 1996 | Inadequate Comment: it wa s unclear what constituted a serious or severe event and insufficient information on the questions that travellers were asked |
Inadequate "... a mailed questionnaire approximately 2 weeks after their anticipated return home date’ ‘if a reply had not been received within 4 weeks an abbreviated questionnaire was sent out." Comment: no details provided regarding abbreviated questionnaire |
Active | Retrospective |
| Saunders 2015 | Inadequate Comment: insufficient information of the questions that travellers were asked |
Adequate | Passive | Retrospective |
| Schwartz 1999 | Inadequate "... we directly contacted all travelers for complete follow‐up and assessment of compliance. Fifty travelers taking primaquine completed a questionnaire regarding side effects" |
Inadequate Comment: see quote. Different methods of follow up for different forms of prophylaxis |
Unclear | Unclear |
| Shamiss 1996 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Inadequate " Questionnaires were distributed and collected by the flight surgeon to 45 aircrew…questionnaires were immediately evaluated and further data collection was done by telephone, if necessary" |
Passive | Unclear Comment: it wa s unclear at which time point data collection occurred |
| Sharafeldin 2010 | Inadequate Comment: n o information wa s provided on how information on adverse effects was sought |
Inadequate Comment: n o mention of how adverse events were recorded in the questionnaire |
Passive | Retrospective |
| Sonmez 2005 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Adequate | Active | Prospective |
| Stoney 2016 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Inadequate Comment: n o information is reported on how adverse events were ascertained |
Active | Prospective |
| Tan 2017 | Adequate | Adequate | Active | Retrospective |
| Terrell 2015 | Inadequate " The questionnaire approved by the MODREC included the 19 commonest adverse effects described in the manufacturers’ product documentation" Comment: Adverse events listed in the questionnaire are not reported |
Adequate | Passive | Unclear Comment: information obtained during transit through Nairobi back to the UK. It wa s unclear whether participants were still taking prophylaxis at this time point |
| Tuck 2016 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Adequate | Active | Unclear Comment: i t wa s not specified at which point during treatment the questionnaire was administered |
| Waner 1999 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Adequate | Passive | Unclear Comment: information was collected during the flight home, when travellers should still have been taking their prophylactic regimen |
1. Were harms pre‐defined using standardised or precise definitions?
2. Was ascertainment technique adequately described?
3. Monitoring classed as 'active' if it occurred at set time points during treatment.
For full description of analysis methods, see Table 4.
Cohort studies
We included 20 cohort studies that assessed and reported safety outcomes, in a total of 435,209 participants. Of these, 10 were conducted in short‐term travellers (Goodyer 2011; Laver 2001; Lobel 2001; Meier 2004; Napoletano 2007; Philips 1996; Schwartz 1999; Sharafeldin 2010; Stoney 2016; Waner 1999), four in longer‐term occupational travellers (Cunningham 2014; Korhonen 2007; Landman 2015; Tan 2017) and six in military personnel (Eick‐Cost 2017; Saunders 2015; Shamiss 1996; Sonmez 2005; Terrell 2015; Tuck 2016); none included pregnant women. Most (17 cohort studies) used participant self‐reported questionnaires to monitor adverse events.
Ten cohort studies had non‐response rates of over 20% (Cunningham 2014; Korhonen 2007; Landman 2015; Lobel 2001; Philips 1996; Sharafeldin 2010; Tan 2017; Terrell 2015; Tuck 2016; Waner 1999), (Figure 4). We judged two to be at high risk of missing data; Goodyer 2011 included pre‐ and post‐travel questionnaires, with an interim loss to follow‐up rate of 27%, and Terrell 2015 excluded participants from the analysis if they reported an adverse effect but did not record its impact on their ability to work. None of these studies blinded participants or mentioned outcome assessors being blinded to intervention status. Seven studies collected data retrospectively, and eight collected information at an unclear or variable time point during treatment (Table 11). One study (Goodyer 2011) was funded by GlaxoSmithKline (manufacturer of atovaquone‐proguanil), one (Meier 2004) by Roche (manufacturer of mefloquine), and one (Philips 1996) by Roche and Pfizer (manufacturers of doxycycline) (see Figure 4).
4.
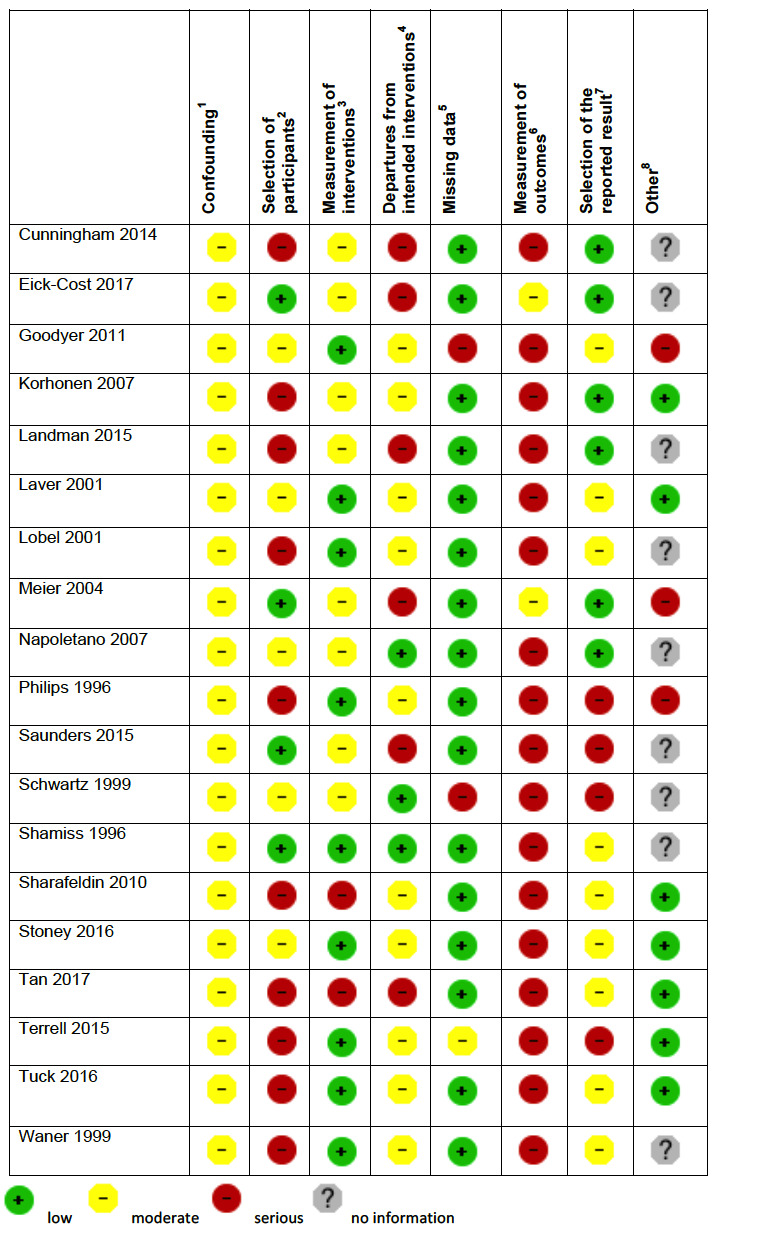
'Risk of bias' summary in cohort studies: mefloquine versus doxycycline
1Assesses whether our pre‐defined confounders are measured and balanced across groups. 2Assesses the non‐response rate of prospective participants. 3Assesses the risk that participants labelled as taking mefloquine (or another antimalarial) actually took something else. 4Assesses the risk that participants whose adverse effects are attributed to mefloquine (or another antimalarial) actually took another drug as well. 5Assesses whether outcome data reasonably complete for most participants and whether intervention status reasonably complete for those in whom it was sought. 6Assesses whether the outcome measure was subjective, and whether participants and outcome assessors were blinded. 7Assesses whether it is clear that all information collected within the study has been reported. 8Assesses the risk of bias due to influence by a corporate study sponsor.
Efficacy
Only seven episodes of malaria were reported while participants were receiving prophylaxis; similar numbers of participants were infected in both arms (4 episodes in 378 mefloquine users versus 3 episodes in 366 doxycycline users: RR 1.35, 95% CI 0.35 to 5.19; 4 trials, 744 participants, Analysis 2.1).
2.1. Analysis.
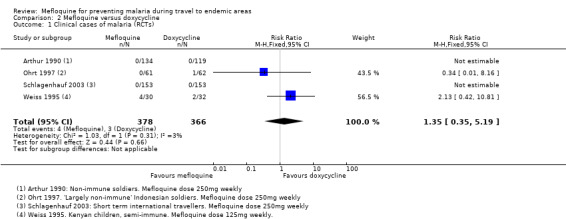
Comparison 2 Mefloquine versus doxycycline, Outcome 1 Clinical cases of malaria (RCTs).
Weiss 1995 reported on episodes of parasitaemia in the semi‐immune population. There was no clear difference between groups (RR 1.47, 95% CI 0.68 to 3.14; 62 participants).
Safety
Serious adverse events or effects
Only Ohrt 1997 described an adverse event as "serious" (acute hysteria) in a doxycycline user, but did not provide sufficient detail to meet our definition. No other serious adverse outcomes were described in RCTs including 348 mefloquine users and 334 doxycycline users (Analysis 2.2; Table 8).
2.2. Analysis.
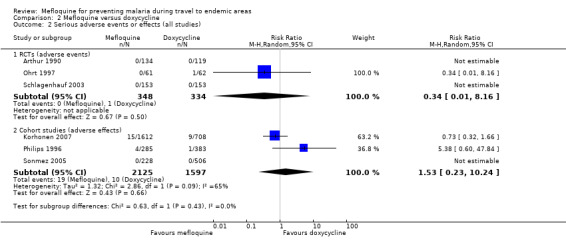
Comparison 2 Mefloquine versus doxycycline, Outcome 2 Serious adverse events or effects (all studies).
In comparison, three cohort studies reported a total of 29 serious adverse effects (attributed to the study drug by users): 19 in 2125 mefloquine users, and 10 in 1597 doxycycline users (RR 1.53, 95% CI 0.23 to 10.24; 3 cohort studies, 3722 participants; Analysis 2.2, Table 9).
Serious adverse effects in mefloquine users were psychological (4 cases) or due to dizziness (3), heart palpitations (2), limb numbness (1), abdominal pain (1), visual disturbance (1), yeast infection (1), passing out (2), seizure (1) and three hospitalizations with "either gastrointestinal or neurologic symptoms". In contrast, serious adverse effects in doxycycline users were due to gastrointestinal disturbance (6), anaemia (1), photosensitivity (1), oesophagitis (1) and cough (1).
In addition, a cohort study (Lobel 2001) reported on hospitalizations in users of mefloquine and doxycycline which were not necessarily attributed to the drug regimen (adverse events). There were eight hospitalizations in 3703 mefloquine users, and none in 69 doxycycline users, with no statistically significant difference between groups (RR 0.32, 95% CI 0.02 to 5.51; 3772 participants, Table 8).
Discontinuations due to adverse effects
There were no overall differences between groups in numbers of discontinuations due to adverse effects in the RCTs (8/391 mefloquine users, 8/382 doxycycline users, RR 1.08, 95% CI 0.41 to 2.87; 4 RCTs, 773 participants, Analysis 2.3) or cohort studies (852/6116 mefloquine users, 378/4049 doxycycline users, RR 0.92, 95% CI 0.54 to 1.55; 10 cohort studies, 10,165 participants, Analysis 2.3). However, heterogeneity among cohort studies was high (I² statistic = 85%).
2.3. Analysis.
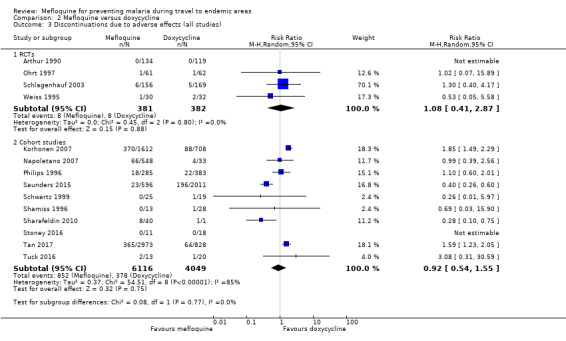
Comparison 2 Mefloquine versus doxycycline, Outcome 3 Discontinuations due to adverse effects (all studies).
Prespecified adverse outcomes
Prespecified adverse effects (attributed to the study drug) were only reported by cohort studies conducted in long‐term occupational travellers (3 studies) and military personnel (3 studies). These form our primary analysis (see Appendix 3 for decision tree).
One RCT in military personnel (Ohrt 1997) and one cohort study in short‐term international travellers (Philips 1996) reported on all symptoms experienced by participants while taking the study drug (adverse events). Two large retrospective analyses of health records in general practice (Meier 2004) and USA military personnel (Eick‐Cost 2017) databases compared rates of incident neurological or psychological diagnoses in participants who had received a prescription for mefloquine or doxycycline (adverse events).
Gastrointestinal symptoms
Across the cohort studies reporting adverse effects, mefloquine users were less likely to report nausea (RR 0.37, 95% CI 0.30 to 0.45; 5 cohort studies, 2683 participants, Analysis 2.4), vomiting (RR 0.18, 95% CI 0.12 to 0.27; 4 cohort studies, 5071 participants, Analysis 2.5), abdominal pain (RR 0.30, 95% CI 0.09 to 1.07; 4 cohort studies, 2569 participants, Analysis 2.6) and diarrhoea (RR 0.28, 95% CI 0.11 to 0.73; 5 cohort studies, 5104 participants, Analysis 2.7).
2.4. Analysis.
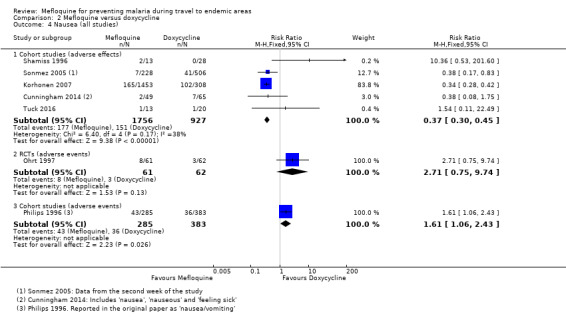
Comparison 2 Mefloquine versus doxycycline, Outcome 4 Nausea (all studies).
2.5. Analysis.
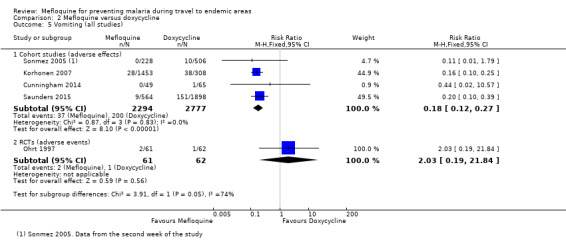
Comparison 2 Mefloquine versus doxycycline, Outcome 5 Vomiting (all studies).
2.6. Analysis.
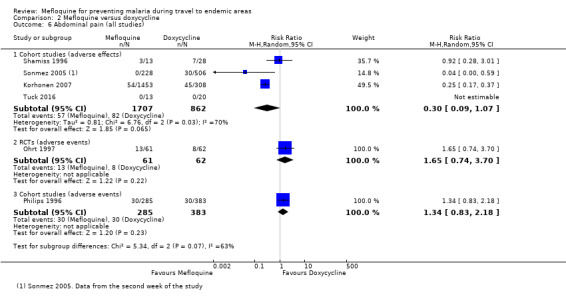
Comparison 2 Mefloquine versus doxycycline, Outcome 6 Abdominal pain (all studies).
2.7. Analysis.
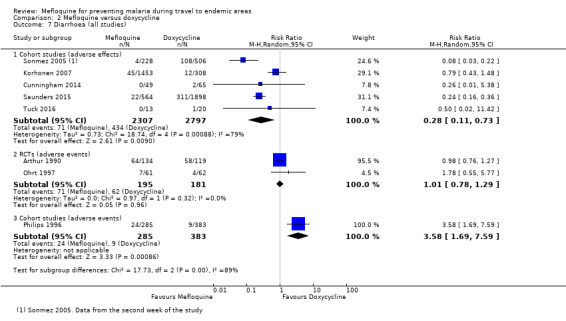
Comparison 2 Mefloquine versus doxycycline, Outcome 7 Diarrhoea (all studies).
However, this finding was not consistent across study types. In the single RCT in military personnel that reported adverse events, no differences were demonstrated for nausea, vomiting, abdominal pain or diarrhoea. In the single cohort study in short‐term international travellers reporting adverse events, mefloquine users were more likely to report nausea and diarrhoea; there was no difference between groups for abdominal pain (Analysis 2.4; Analysis 2.5; Analysis 2.6; Analysis 2.7).
Dyspepsia was consistently more common in doxycycline users but there was substantial heterogeneity in the size of this effect (RR 0.26, 95% CI 0.09 to 0.74; 5 cohort studies, 5104 participants, I² statistic = 77%, Analysis 2.8)
2.8. Analysis.
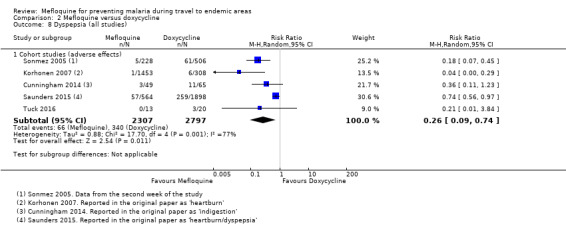
Comparison 2 Mefloquine versus doxycycline, Outcome 8 Dyspepsia (all studies).
Neurological symptoms
In the cohort studies reporting adverse effects, no difference was demonstrated for headache (RR 1.21, 95% CI 0.50 to 2.92; 5 cohort studies, 3322 participants, Analysis 2.9) or dizziness (RR 3.49, 95% CI 0.88 to 13.75; 5 cohort studies, 2633 participants, Analysis 2.10).
2.9. Analysis.
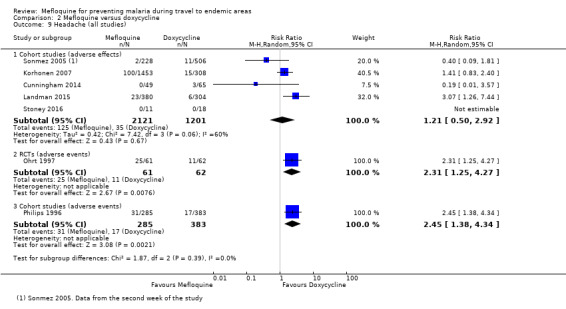
Comparison 2 Mefloquine versus doxycycline, Outcome 9 Headache (all studies).
2.10. Analysis.
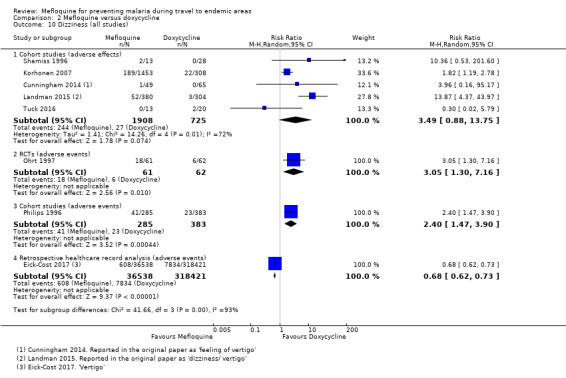
Comparison 2 Mefloquine versus doxycycline, Outcome 10 Dizziness (all studies).
In the RCT in military personnel (Ohrt 1997) and a cohort study in short‐term international travellers (Philips 1996) both headache and dizziness were more common in mefloquine users. However, a large retrospective analysis of health records in military personnel (Eick‐Cost 2017) found higher rates of dizziness in doxycycline users (Analysis 2.9; Analysis 2.10).
Psychological symptoms
In the cohort studies reporting adverse effects, mefloquine users were more likely to report abnormal dreams (RR 10.49, 95% CI 3.79 to 29.10; 4 cohort studies, 2588 participants, Analysis 2.11), insomnia (RR 4.14, 95% CI 1.19 to 14.44; 4 cohort studies, 3212 participants, Analysis 2.12), anxiety (RR 18.04, 95% CI 9.32 to 34.93; 3 cohort studies, 2559 participants, Analysis 2.13) and depressed mood (RR 11.43, 95% CI 5.21 to 25.07; 2 cohort studies, 2445 participants, Analysis 2.14). There were 15 episodes of abnormal thoughts and perceptions with mefloquine and none with doxycyline in cohort studies reporting adverse effects (RR 6.60, 95% CI 0.92 to 47.20; 2 cohort studies, 2445 participants, Analysis 2.15).
2.11. Analysis.
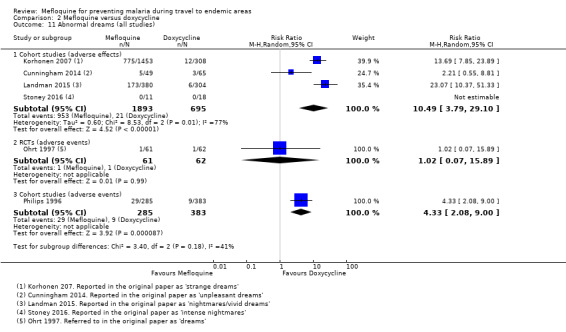
Comparison 2 Mefloquine versus doxycycline, Outcome 11 Abnormal dreams (all studies).
2.12. Analysis.
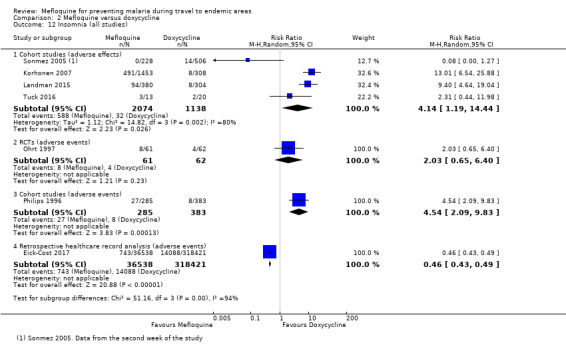
Comparison 2 Mefloquine versus doxycycline, Outcome 12 Insomnia (all studies).
2.13. Analysis.
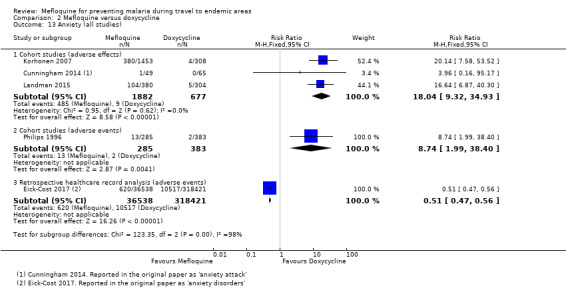
Comparison 2 Mefloquine versus doxycycline, Outcome 13 Anxiety (all studies).
2.14. Analysis.
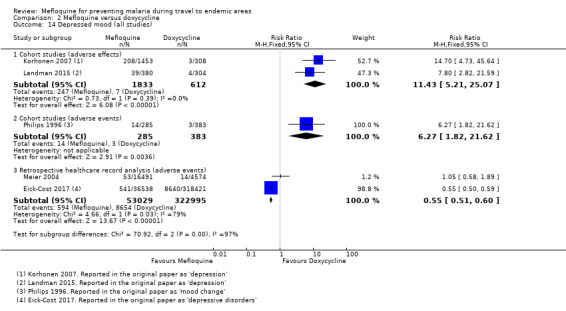
Comparison 2 Mefloquine versus doxycycline, Outcome 14 Depressed mood (all studies).
2.15. Analysis.
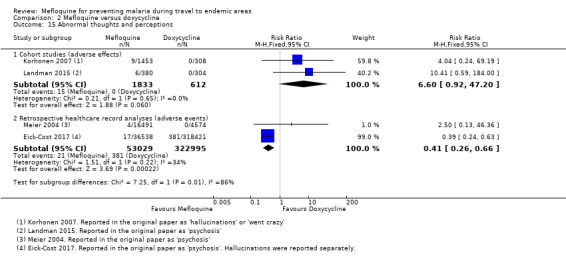
Comparison 2 Mefloquine versus doxycycline, Outcome 15 Abnormal thoughts and perceptions.
The findings of the single cohort study in short‐term international travellers reporting adverse events (Philips 1996) were consistent with this. However in the single RCT (Ohrt 1997) and the large retrospective healthcare record analyses, there were either no differences between groups, or doxycycline users were more likely to experience psychological symptoms (Analysis 2.11; Analysis 2.12; Analysis 2.13; Analysis 2.14; Analysis 2.15).
Other prespecified symptoms
Pruritis was more common in doxycycline users in cohort studies reporting adverse effects (RR 0.52, 95% CI 0.30 to 0.91; 2 cohort studies, 1794 participants, Analysis 2.16), but more common with mefloquine in the single cohort in short‐term travellers reporting adverse events (RR 2.69, 95% CI 0.93 to 7.78; 1 cohort study, 668 participants).
2.16. Analysis.
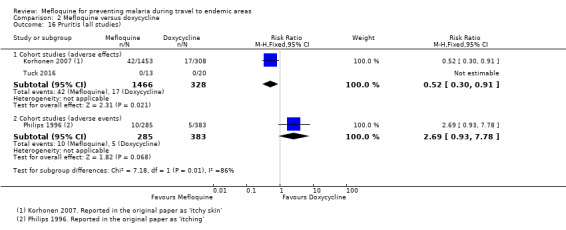
Comparison 2 Mefloquine versus doxycycline, Outcome 16 Pruritis (all studies).
In cohort studies reporting adverse effects, photosensitivity was more common in doxycycline users (RR 0.08, 95% CI 0.05 to 0.11; 2 cohort studies, 1875 participants, Analysis 2.17), as was vaginal yeast infection in female participants (RR 0.10, 95% CI 0.06 to 0.16; 1 cohort study, 1761 participants, Analysis 2.18). The findings of the single cohort study in short‐term travellers reporting adverse events were consistent with this finding (Analysis 2.17; Analysis 2.18).
2.17. Analysis.
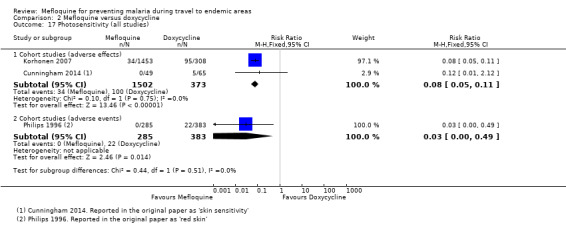
Comparison 2 Mefloquine versus doxycycline, Outcome 17 Photosensitivity (all studies).
2.18. Analysis.
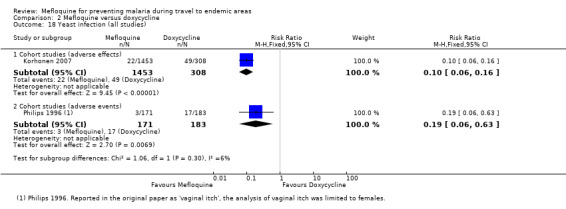
Comparison 2 Mefloquine versus doxycycline, Outcome 18 Yeast infection (all studies).
Visual impairment was more commonly reported among mefloquine users (RR 2.37, 95% CI 1.41 to 3.99; 2 cohort studies, 1875 participants; Analysis 2.19).
2.19. Analysis.
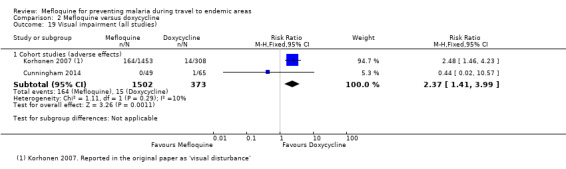
Comparison 2 Mefloquine versus doxycycline, Outcome 19 Visual impairment (all studies).
Other adverse events and effects
A range of other adverse effects were reported by the cohort studies. These included alopecia (hair loss), asthenia (physical weakness), balance disorder, decreased appetite, fatigue, hypoaesthesia (numbness), malaise, mouth ulcers, palpitations and tinnitus (Analysis 2.20). Mefloquine users were more likely to report alopecia (RR 3.44, 95% CI 1.96 to 6.03; 2 cohort studies, 1875 participants), unsteadiness (RR 2.87, 95% CI 1.48 to 5.59; 1 cohort study, 1761 participants) and limb numbness (RR 11.48, 95% CI 3.01 to 43.70; 2 cohort studies, 2445 participants), but were less likely to report malaise (RR 0.28, 95% CI 0.11 to 0.71; 1 cohort study, 734 participants).
2.20. Analysis.
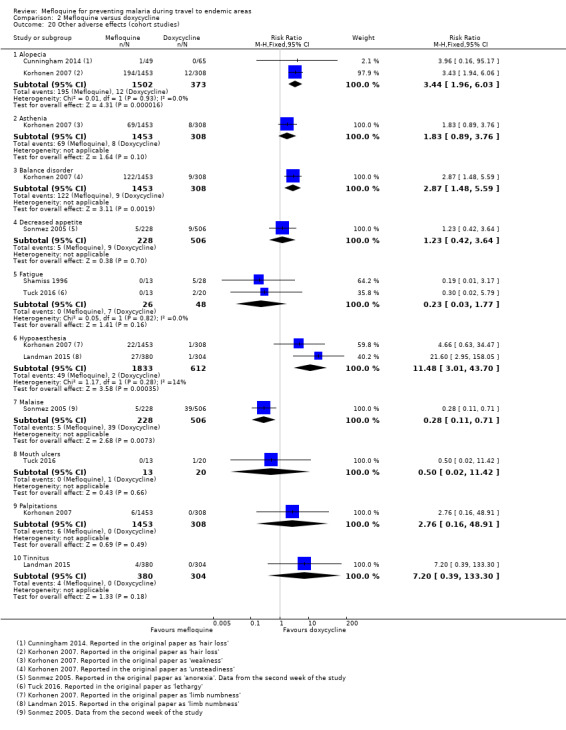
Comparison 2 Mefloquine versus doxycycline, Outcome 20 Other adverse effects (cohort studies).
Additional adverse events reported in the RCT and cohort studies are presented in Analysis 2.21 and Analysis 2.22 respectively. In Eick‐Cost 2017, a large retrospective healthcare record analysis in USA military personnel that reported adverse events, mefloquine users were less likely than doxycycline users to receive formal medical diagnoses of adjustment disorder (RR 0.43, 95% CI 0.40 to 0.45; 354,959 participants), convulsions (RR 0.58, 95% CI 0.45 to 0.75), hallucinations (RR 0.18, 95% CI 0.08 to 0.45), post‐traumatic stress disorder (PTSD) (RR 0.58, 95% CI 0.53 to 0.64), suicidal ideation (RR 0.38, 95% CI 0.31 to 0.47), and tinnitus (RR 0.65, 95% CI 0.61 to 0.71). There were no differences in overall rates of suicide in the large retrospective healthcare record analyses (4/53,029 mefloquine users and 15/322,995 doxycycline users; RR 1.21, 95% CI 0.32 to 4.56, Analysis 2.22).
2.21. Analysis.
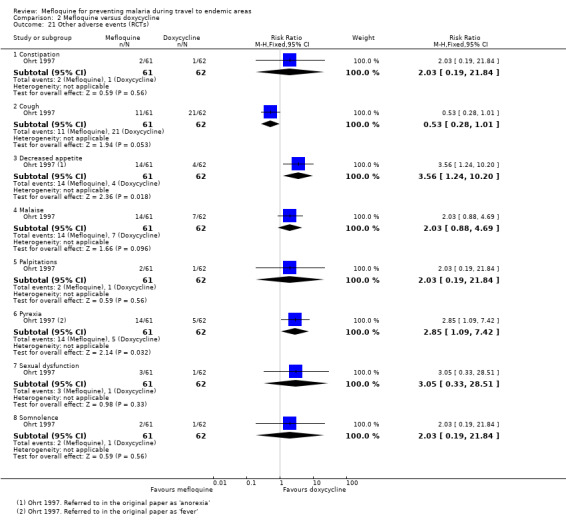
Comparison 2 Mefloquine versus doxycycline, Outcome 21 Other adverse events (RCTs).
2.22. Analysis.
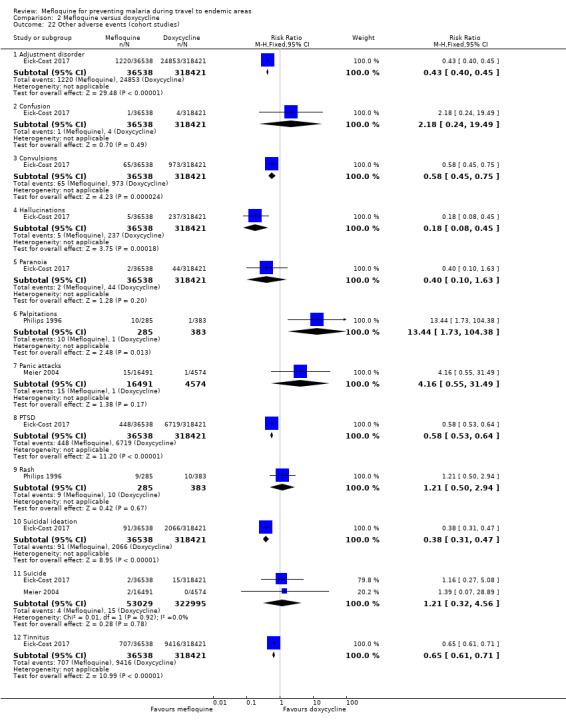
Comparison 2 Mefloquine versus doxycycline, Outcome 22 Other adverse events (cohort studies).
Studies reporting groups of symptoms or other outcomes that could be used as proxy markers of psychological or neurological adverse effects are reported in Appendix 5.
Adherence
Arthur 1990, an RCT, performed serological assays to assess adherence. Arthur 1990 reported measurable serum drug levels at the end of the trial in 87% of 119 military personnel prescribed doxycycline and 92% of 134 who were prescribed mefloquine. However, medication was administered under the supervision of each participant's squad leader.
Thirteen cohort studies compared the proportion of participants with 100% self‐reported adherence and found higher rates of adherence during travel in mefloquine users (RR 1.15, 95% CI 1.12 to 1.18; 13 cohort studies, 15,583 participants, Analysis 2.23), but no differences between groups in the post‐travel period (RR 1.08, 95% CI 0.95 to 1.22; 4 cohort studies, 840 participants, Analysis 2.23). Most (77%) mefloquine users described themselves as adherent during travel (range 24% to 100%), compared to 63% of doxycycline users (range 37% to 92%). In the post‐travel period this dropped to 55% of mefloquine users (range 50% to 87%) and 51% of doxycycline users (range 27% to 75%). There was no difference in the results when the analysis was limited to short‐term international travellers (RR 1.11, 95% CI 1.06 to 1.17; 4 cohort studies; 8390 participants).
2.23. Analysis.
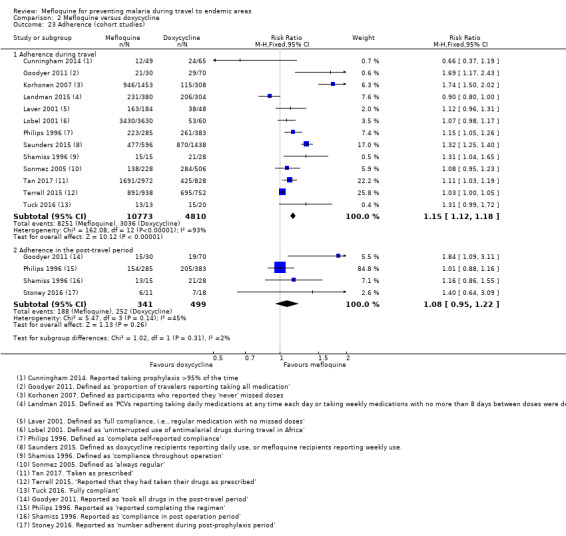
Comparison 2 Mefloquine versus doxycycline, Outcome 23 Adherence (cohort studies).
Comparison 3: Mefloquine versus atovaquone‐proguanil
Description of studies
RCTs
Two RCTs in non‐immune travellers reported efficacy, with most participants visiting sub‐Saharan Africa for fewer than three weeks (Overbosch 2001; Schlagenhauf 2003). Efficacy was assessed by testing for antibodies to a circumsporozoite protein four weeks after travel in the study by Overbosch 2001, and the method was unclear in Schlagenhauf 2003.
Three RCTs (Overbosch 2001; Schlagenhauf 2003; van Riemsdijk 2002), and 16 cohort studies (Andersson 2008; Belderok 2013; Cunningham 2014; Eick‐Cost 2017; Goodyer 2011; Kato 2013; Korhonen 2007; Kuhner 2005; Landman 2015; Laverone 2006; Napoletano 2007; Schneider 2013; Sharafeldin 2010; Stoney 2016; Tan 2017; Tuck 2016) assessed and reported safety outcomes (Table 12).
10. Mefloquine versus atovaquone‐proguanil; characteristics of included studies for safety.
| Study ID | Participants | Number enrolled | Method of adverse event monitoring | Significant exclusions for psychiatric adverse effects | Duration of travel | Source of funding |
| Randomized controlled trials | ||||||
| Overbosch 2001 | Travellers from Canada, Germany, Netherlands, South Africa, UK | 1013 | Interview with study personnel | "... history of alcoholism, seizures or psychiatric or severe neurological disorders" | Mean 2.5 weeks | GlaxoSmithKline |
| Schlagenhauf 2003 | Non‐immune adult short‐term travellers | 674 | Participant self‐reported questionnaire | " History of seizures or psychiatric disorders" | 4 to 6 weeks | GlaxoSmithKline and Roche |
| van Riemsdijk 2002 | Dutch short‐term travellers | 140 | Interview and testing with study personnel | "H istory of alcoholism, seizures, psychiatric disorders, severe neurological disorders" | Mean 19 days | Government funding |
| Non‐randomis ed studies | ||||||
| Participants | Number enrolled | Method of adverse event monitoring | Factors influencing drug allocation | Duration of travel | Source of funding | |
| Andersson 2008 | Swedish soldiers | 609 | Participant self‐reported questionnaire | Mainly mefloquine, soldiers with contra‐indications received atovaquone‐proguanil | 6 months | Not mentioned |
| Belderok 2013 | Dutch short‐term travellers | 945 | Participant self‐reported questionnaire (measured adherence) | Allocation based on guidelines and participant preference | 84% < 29 days | Government funding |
| Cunningham 2014 | UK Foreign and Commonwealth Office staff | 327 | Participant self‐reported questionnaire | Allocation based on guidelines and p articipant preference | 0‐36 months | Not mentioned |
| Eick‐Cost 2017 | USA s oldiers | 367,840 | Data from the Defense Medical Surveillance System, the Pharmacy Data Transaction Service and the Theater Medical Data Store | No information available | Various, not specified | Not mentioned |
| Goodyer 2011 | UK adult short‐term travellers | 185 | Participant self‐reported questionnaire | Allocation based on guidelines and p articipant preference | < 28 days | GlaxoSmithKline |
| Kato 2013 | Japanese short‐term travellers | 316 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Mean 20.0 ± 9.6 days in the atovaquone‐proguanil group and 59.0 ± 15.9 days in the mefloquine group | Not mentioned |
| Korhonen 2007 | Peace Corps volunteers | 2701 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | ≥ 6 months | Two staff employed by Peace Corps |
| Kuhner 2005 | German short‐term travellers | 495 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | A tovaquone‐proguanil mean 2.6 weeks, mefloquine mean 7 weeks | Not mentioned |
| Landman 2015 | Peace Corps volunteers | 1184 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Various, not specified | Not mentioned |
| Laverone 2006 | Italian short‐term travellers | 1176 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | > 90% 0 to 30 days | Not mentioned |
| Napoletano 2007 | Italian short‐term travellers | 1906 | Telephone interview | Allocation based on guidelines and participant preference | Mean 2 weeks, range 0 to > 35 days | Not mentioned |
| Schneider 2013 | UK adults enrolled in UK g eneral p ractice research database | Not available | Incident cases of a neuropsychiatric disorders during or after antimalarial drug use | No information available | Various, not specified | Roche |
| Sharafeldin 2010 | Dutch medical students | 180 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Mean duration of stay 74 days (range 10 to 224 days) | " N o dedicated funding for this project" |
| Stoney 2016 | USA short‐term travellers | 370 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Median duration 13 days | Government funding |
| Tan 2017 | Peace Corps volunteers | 8931 | Participant self‐reported questionnaire | No information available | Various, not specified | No dedicated funding |
| Tuck 2016 | UK soldiers | 151 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Various, not specified | No dedicated funding |
Two RCTs included adults and children aged ≥ 3 years (Overbosch 2001; van Riemsdijk 2002); all other studies were restricted to adults. The RCTs described participants as non‐immune travellers, and most participants visited sub‐Saharan Africa for fewer than three weeks. The cohort studies included short‐term travellers (Belderok 2013; Goodyer 2011; Kato 2013; Kuhner 2005; Laverone 2006; Napoletano 2007; Schneider 2013; Sharafeldin 2010; Stoney 2016), longer‐term occupational travellers (Cunningham 2014; Korhonen 2007; Landman 2015; Tan 2017) and military personnel (Andersson 2008; Eick‐Cost 2017; Tuck 2016).
All three RCTs that assessed and reported safety outcomes collected information on adverse events actively and prospectively, and predefined harms using standardized and precise definitions (Overbosch 2001; Schlagenhauf 2003; van Riemsdijk 2002; Table 13). Only Overbosch 2001 performed a blinded assessment of whether there was a reasonable possibility that each adverse event was caused by the study drug (adverse effects). Overbosch 2001 was funded by GlaxoSmithKline (manufacturer of atovaquone‐proguanil) and Schlagenhauf 2003 received funding from both GlaxoSmithKline and Roche (manufacturers of mefloquine).
11. Mefloquine versus atovaquone‐proguanil; quality of adverse event reporting.
| Study ID | Harms predefined¹ | Description of ascertainment technique² | Active or passive monitoring?³ | Prospective or retrospective data collection? |
| RCTs | ||||
| Overbosch 2001 | Adequate | Adequate | Active | Prospective |
| Schlagenhauf 2003 | Adequate | Adequate | Active | Prospective |
| van Riemsdijk 2002 | Adequate | Adequate | Active | Prospective |
| Cohort studies | ||||
| Andersson 2008 | Inadequate Comment: insufficient information provided on the questions which soldiers were asked |
Inadequate Comment: different ascertainment technique used for one of the three groups, which is inadequately described |
Active | Unclear Comment: d ata collection was prospective for 448/609 participants (LA04 and LA05), but retrospective for 161 participants (LA02) |
| Cunningham 2014 | Inadequate Comment: questionnaire included a targeted list of side effects, including " other psychological problems" . What was included within this was not defined |
Adequate | Passive | Unclear Comment: questionnaire was performed while participants were still taking chemoprophylaxis medication, although 75% were non‐compliant |
| Eick‐Cost 2017 | Adequate | Adequate | Passive | Prospective |
| Goodyer 2011 | Inadequate " Also included on the questionnaire was a single free‐text question asking travelers to describe any side effects of antimalarial medication" |
Adequate | Active | Retrospective |
| Kato 2013 | Adequate | Adequate | Passive | Unclear Comment: the timing of this questionnaire has not been made clear |
| Korhonen 2007 | Adequate | Adequate | Passive | Unclear Comment: n o information wa s provided regarding the timing of the questionnaire during treatment |
| Kuhner 2005 | Inadequate Comment: insufficient information provided on the questions that participants were asked |
Adequate | Active | Retrospective |
| Landman 2015 | Adequate | Adequate | Passive | Unclear Comment: all participants were emailed the questionnaire at one time point, which occurred at varying points during the prophylactic regimen |
| Laverone 2006 | Adequate | Adequate | Passive | Retrospective |
| Napoletano 2007 | Unclear Comment: adverse events were categorised on a scale of one to four, but it is unclear whether and how causality was assessed |
Adequate | Active | Retrospective |
| Schneider 2013 | Adequate | Adequate | Passive | Retrospective |
| Sharafeldin 2010 | Inadequate Comment: n o information is provided on how information on adverse effects was sought |
Inadequate Comment: n o mention of how adverse events were recorded in the questionnaire. |
Passive | Retrospective |
| Stoney 2016 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Inadequate Comment: n o information is reported on how adverse events were ascertained |
Active | Prospective |
| Tan 2017 | Adequate | Adequate | Active | Retrospective |
| Tuck 2016 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Adequate | Active | Unclear Comment: i t wa s not specified at which point during treatment the questionnaire was administered |
1. Were harms pre‐defined using standardised or precise definitions?
2. Was ascertainment technique adequately described?
3. Monitoring classed as 'active' if it occurred at set time points during treatment.
For full description of analysis methods, see Table 4.
Cohort studies
In the cohort studies, safety was assessed by self‐reported questionnaires (Andersson 2008; Belderok 2013; Cunningham 2014; Goodyer 2011; Kato 2013; Korhonen 2007; Kuhner 2005; Landman 2015; Laverone 2006; Sharafeldin 2010; Stoney 2016; Tan 2017; Tuck 2016), telephone interview (Napoletano 2007), and retrospective analysis of a healthcare records (Eick‐Cost 2017; Schneider 2013). Seven studies collected adverse event data retrospectively and six collected these data at an unclear or variable time point during treatment (Table 13). One study (Goodyer 2011) was funded by GlaxoSmithKline (manufacturer of atovaquone‐proguanil) and one (Schneider 2013) was funded by Roche (manufacturer of mefloquine) (Figure 5).
5.
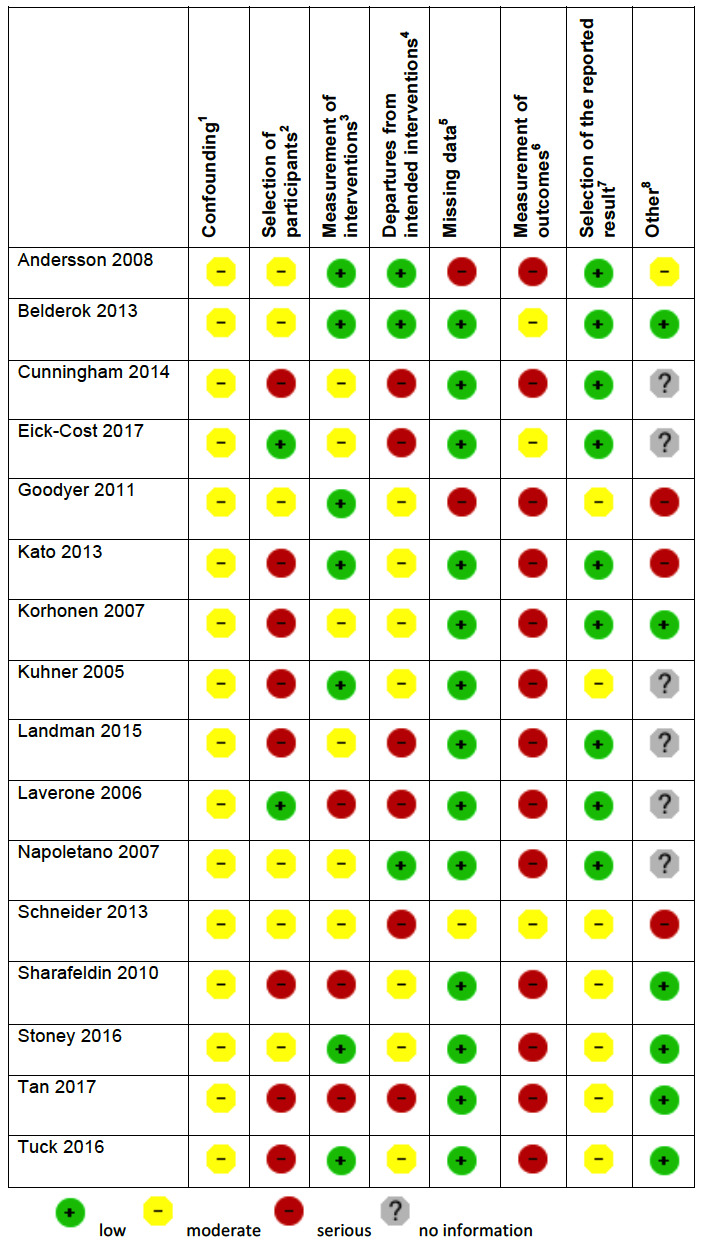
'Risk of bias' summary in cohort studies: mefloquine versus atovaquone‐proguanil
1Assesses whether our pre‐defined confounders are measured and balanced across groups. 2Assesses the non‐response rate of prospective participants. 3Assesses the risk that participants labelled as taking mefloquine (or another antimalarial) actually took something else. 4Assesses the risk that participants whose adverse effects are attributed to mefloquine (or another antimalarial) actually took another drug as well. 5Assesses whether outcome data reasonably complete for most participants and whether intervention status reasonably complete for those in whom it was sought. 6Assesses whether the outcome measure was subjective, and whether participants and outcome assessors were blinded. 7Assesses whether it is clear that all information collected within the study has been reported. 8Assesses the risk of bias due to influence by a corporate study sponsor.
Efficacy
No clinical cases of malaria were recorded (2 RCTs, 636 mefloquine users; 657 atovaquone‐proguanil users).
Safety
Serious adverse events or effects
Overbosch 2001, an RCT, reported 10 serious adverse events in 483 participants who received mefloquine and four in 493 participants who received atovaquone‐proguanil. None were considered attributable to the drug regimen (Table 8).
Three cohort studies reported a total of 15 serious adverse effects (attributed by participants to the study drug) in 2651 mefloquine users (Table 9). There were no serious adverse effects reported in participants who received atovaquone‐proguanil (940 users). The difference between groups was not statistically significant (RR 1.40, 95% CI 0.08 to 23.22; 3 cohort studies, 3591 participants, Analysis 3.2).
3.2. Analysis.
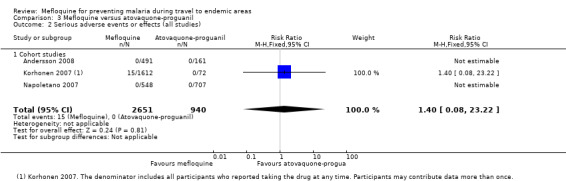
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 2 Serious adverse events or effects (all studies).
The serious adverse effects in mefloquine users were: psychological (4 cases), dizziness (3), heart palpitations (2), limb numbness (1), abdominal pain (1), visual disturbance (1), yeast infection (1), and passing out (2).
Discontinuations due to adverse effects
In the RCTs, participants who received mefloquine were more likely to discontinue their medication due to adverse effects than participants who took atovaquone‐proguanil (39/714 mefloquine versus 13/724 atovaquone‐proguanil; RR 2.86, 95% CI 1.53 to 5.31; 3 RCTs, 1438 participants, Analysis 3.3).
3.3. Analysis.
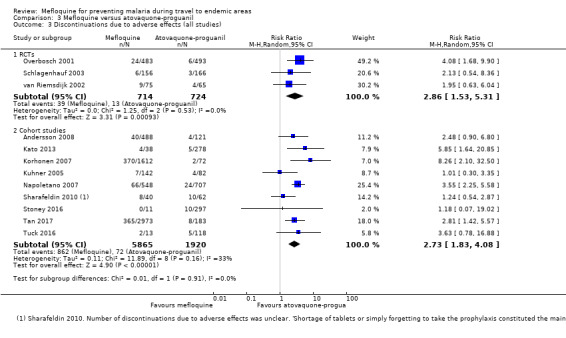
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 3 Discontinuations due to adverse effects (all studies).
The overall effect size was similar in the cohort studies (RR 2.73, 95% CI 1.83 to 4.08; 9 cohort studies, 7785 participants, Analysis 3.3).
Prespecified adverse effects
Gastrointestinal symptoms
Mefloquine users were more likely to report nausea than atovaquone‐proguanil users with similar effect sizes in the RCT (RR 2.72, 95% CI 1.52 to 4.86; 976 participants) and overall in the cohort studies (RR 2.50, 95% CI 1.54 to 4.06; 7 cohort studies, 3509 participants, Analysis 3.4). There were no consistent differences in the frequency of reported vomiting (Analysis 3.5), abdominal pain (Analysis 3.6) or diarrhoea (Analysis 3.7). Mouth ulcers were less commonly reported with mefloquine in cohort studies (RR 0.12, 95% CI 0.04 to 0.37; 2 cohort studies, 783 participants), but not in the RCT (RR 1.45, 95% CI 0.70 to 3.00; 976 participants; Analysis 3.8).
3.4. Analysis.
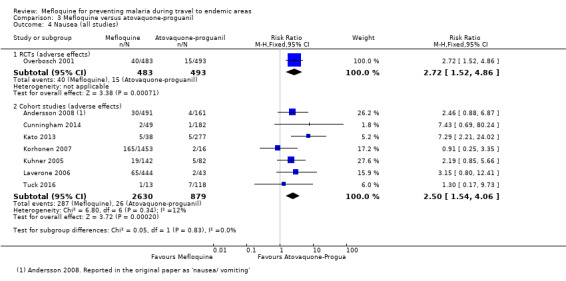
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 4 Nausea (all studies).
3.5. Analysis.
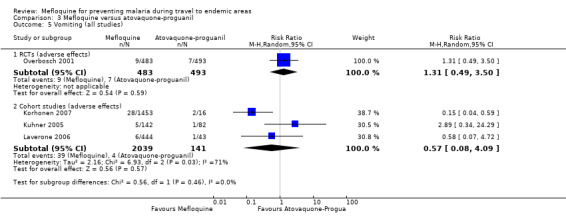
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 5 Vomiting (all studies).
3.6. Analysis.
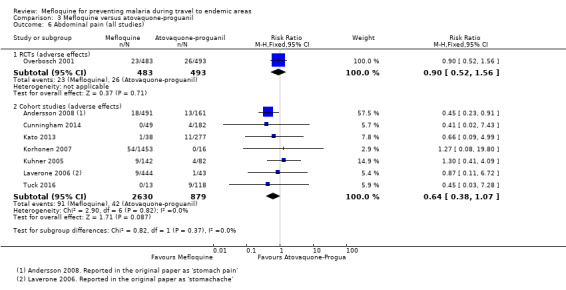
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 6 Abdominal pain (all studies).
3.7. Analysis.
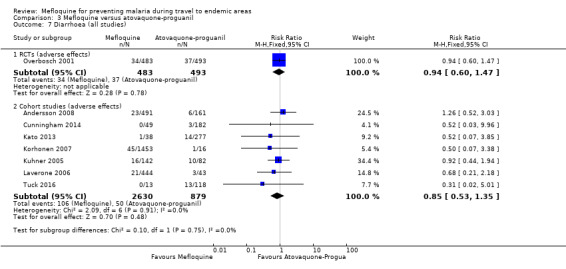
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 7 Diarrhoea (all studies).
3.8. Analysis.
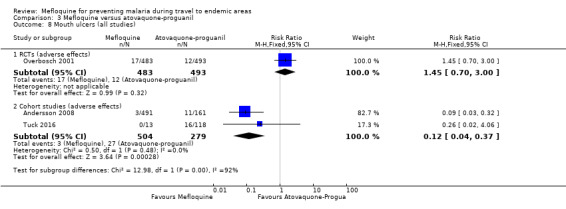
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 8 Mouth ulcers (all studies).
Neurological symptoms
Mefloquine users were more likely to report headache although this did not reach standard levels of statistical significance in the RCT (RR 1.72, 95% CI 0.99 to 2.99; 976 participants). The effect was larger and consistent across the cohort studies (RR 3.42, 95% CI 1.71 to 6.82; 8 cohort studies, 4163 participants, I² statistic = 0%, Analysis 3.9). Similarly, dizziness was more common in mefloquine users in the RCT (RR 3.99, 95% CI 2.08 to 7.64) and consistently more common in the cohort studies (RR 3.83, 95% CI 2.23 to 6.58; 8 cohort studies, 3986 participants, Analysis 3.10). The same trend was seen in the retrospective healthcare record analyses, although the effect size was smaller (RR 1.23, 95% CI 1.04 to 1.46; 49,419 participants).
3.9. Analysis.
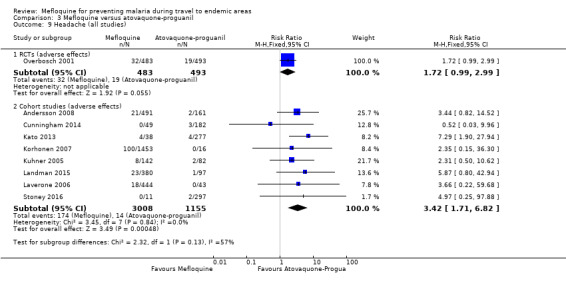
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 9 Headache (all studies).
3.10. Analysis.
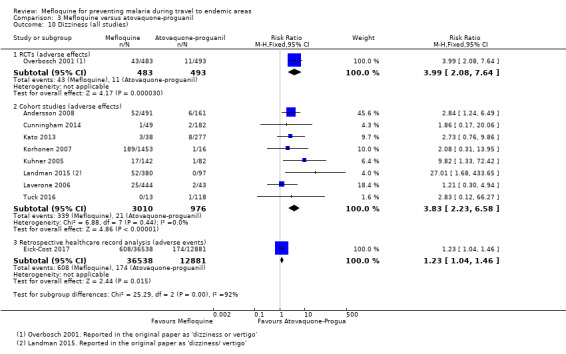
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 10 Dizziness (all studies).
Psychological symptoms
In the RCT, mefloquine users were more likely than atovaquone‐proguanil users to report abnormal dreams (RR 2.04, 95% CI 1.37 to 3.04), insomnia (RR 4.42, 95% CI 2.56 to 7.64), anxiety (RR 6.12, 95% CI 1.82 to 20.66) and depressed mood (RR 5.78, 95% CI 1.71 to 19.61; 976 participants) (Overbosch 2001). Consistent, larger effects were seen in the cohort studies: abnormal dreams (RR 6.81, 95% CI 1.65 to 28.15; 7 cohort studies, 3848 participants, Analysis 3.11), insomnia (RR 7.29, 95% CI 4.37 to 12.16; 8 cohort studies, 3986 participants, Analysis 3.12), anxiety (RR 10.10, 95% CI 3.48 to 29.32; 4 cohort studies, 2664 participants, Analysis 3.13) and depressed mood (RR 8.02, 95% CI 3.56 to 18.07; 6 cohort studies, 3624 participants, Analysis 3.14). In addition, 21 mefloquine users and no atovaquone‐proguanil users reported abnormal thoughts or perceptions, but the difference between groups was not statistically significant (RR 1.50, 95% CI 0.30 to 7.42; 3 cohort studies, 2441 participants, Analysis 3.15).
3.11. Analysis.
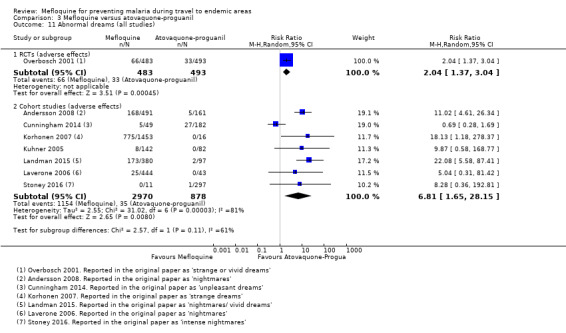
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 11 Abnormal dreams (all studies).
3.12. Analysis.
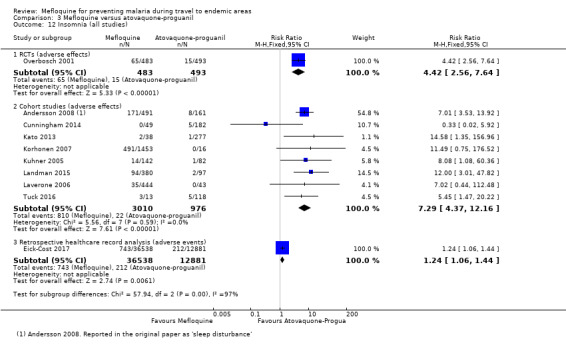
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 12 Insomnia (all studies).
3.13. Analysis.
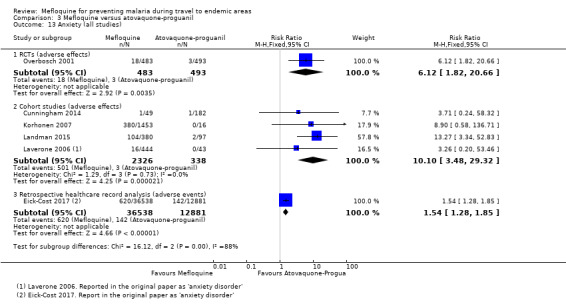
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 13 Anxiety (all studies).
3.14. Analysis.
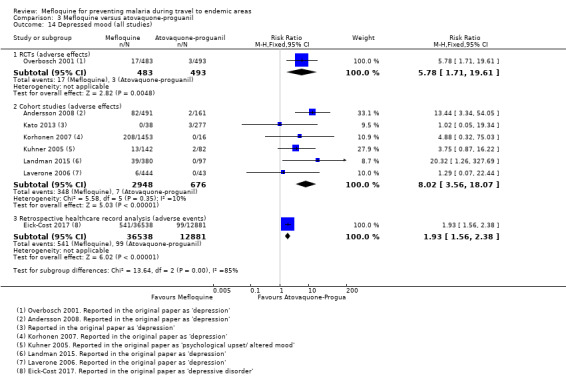
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 14 Depressed mood (all studies).
3.15. Analysis.
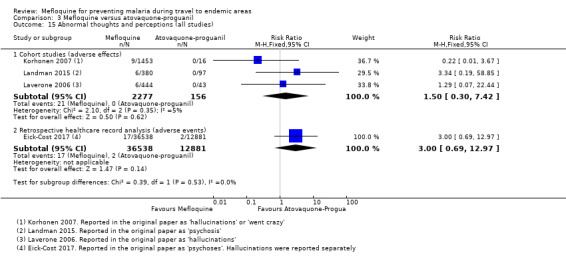
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 15 Abnormal thoughts and perceptions (all studies).
Consistent effects were seen in the retrospective healthcare record analysis (adverse events, Eick‐Cost 2017) although the effect size was smaller.
Other prespecified adverse symptoms
No differences were demonstrated for pruritis (1 RCT, 3 cohort studies; Analysis 3.16); or visual impairment (1 RCT, 2 cohort studies; Analysis 3.17).
3.16. Analysis.
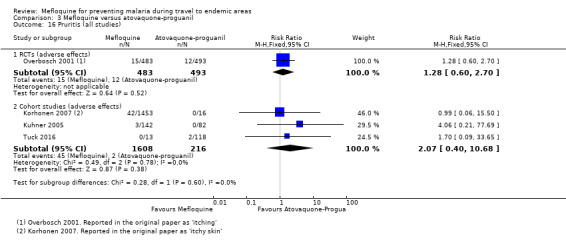
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 16 Pruritis (all studies).
3.17. Analysis.
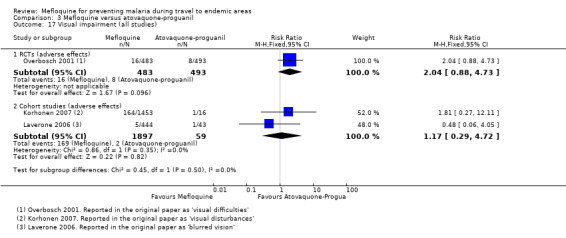
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 17 Visual impairment (all studies).
Other adverse outcomes
Other adverse effects reported in more than 1% of study participants in cohort studies (in either study arm) included: allergic reaction, alopecia (hair loss), asthenia (weakness), balance disorder, cough, disturbance in attention, dyspepsia, fatigue, hypoaesthesia, loss of appetite, muscle pain, palpitation, photosensitization, pyrexia, rash, restlessness, slight illness, somnolence, tinnitus and circulatory disorders (Analysis 3.18). Mefloquine users were more likely to report concentration difficulties (RR 4.45, 95% CI 1.84 to 10.77; 3 cohort studies, 1363 participants).
3.18. Analysis.
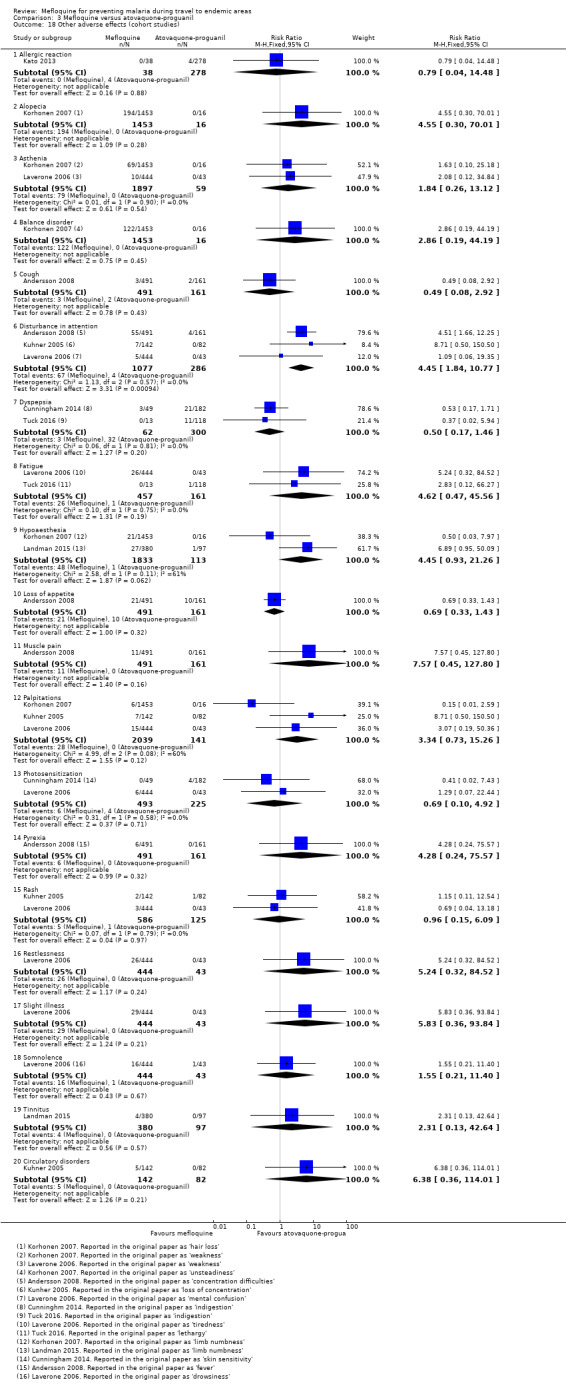
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 18 Other adverse effects (cohort studies).
In the large retrospective healthcare record analyses which reported adverse events, mefloquine users were more likely to receive formal medical diagnoses of adjustment disorder (RR 1.76, 95% CI 1.54 to 2.02; 49,419 participants, Analysis 3.19), PTSD (RR 2.51, 95% CI 1.93 to 3.26; Analysis 3.19), suicidal ideation (RR 1.69, 95% CI 1.03 to 2.77; Analysis 3.19) and tinnitus (RR 1.42, 95% CI 1.21 to 1.68; Analysis 3.19). However, users were less likely to experience hallucinations (RR 0.25, 95% CI 0.08 to 0.79; Analysis 3.19).
3.19. Analysis.
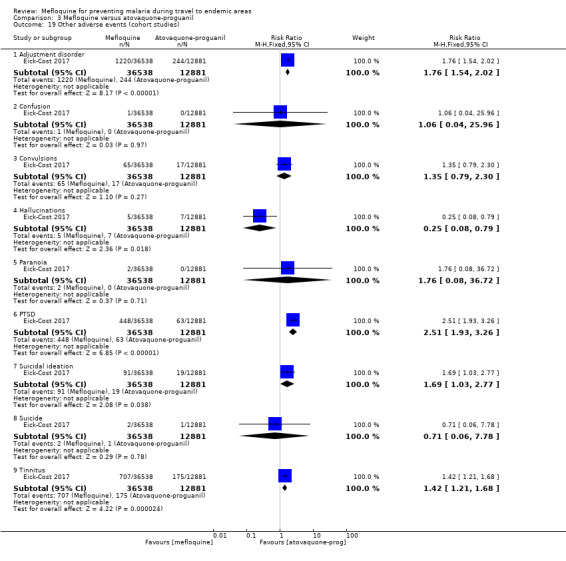
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 19 Other adverse events (cohort studies).
Studies reporting groups of symptoms, or other outcomes which could be used as proxy markers of psychological or neurological adverse effects, are reported in Appendix 6.
Adherence
van Riemsdijk 2002 monitored adherence through reference to the participants' diary cards and counts of returned study medication. It was found that 93% of mefloquine users were completely adherent, compared to 98.3% of atovaquone‐proguanil users (RR 0.95, 95% CI 0.88 to 1.02; 1 RCT, 119 participants, Analysis 3.20).
3.20. Analysis.
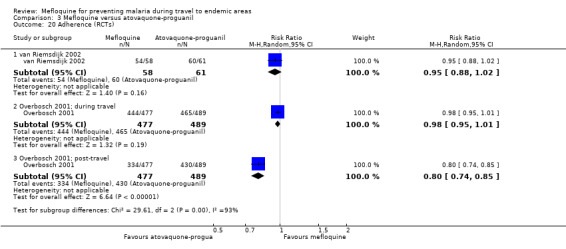
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 20 Adherence (RCTs).
Overbosch 2001 defined participants as adherent if they took at least 80% of prescribed doses. Overbosch 2001 also found no difference between the groups during travel (RR 0.98, 95% CI 0.95 to 1.01; 966 participants; Analysis 3.20). However, analysis in the post‐travel period found that mefloquine users were less likely to complete the regimen (RR 0.80, 95% CI 0.74 to 0.85; 966 participants); 93% of mefloquine users were adherent during travel, dropping to 70% in the post‐travel period, compared to 95% and 88% for atovaquone‐proguanil.
Six cohort studies compared the proportion of participants with 100% self‐reported adherence and found no difference during travel (RR 1.08, 95% CI 0.86 to 1.34; 6 cohort studies, 5577 participants, Analysis 3.21) or in the post‐travel period (RR 0.89, 95% CI 0.64 to 1.23; 2 cohort studies, 422 participants, Analysis 3.21). In these studies, 60% of mefloquine users described themselves as adherent during travel, dropping to 51% in the post‐travel period, compared to 53% and 62% respectively for people who took atovaquone‐proguanil.
3.21. Analysis.
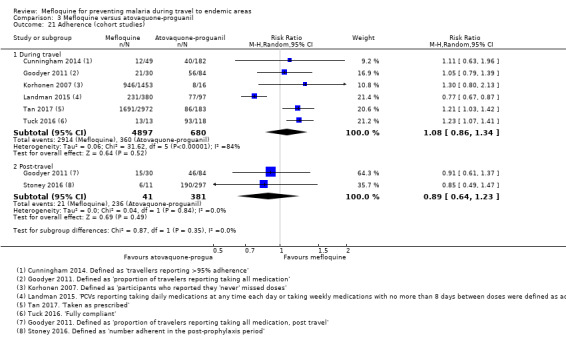
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 21 Adherence (cohort studies).
Belderok 2013 categorized travellers as adherent if they took at least 75% of prescribed doses. Belderok 2013 reported higher rates of adherence in participants who took mefloquine both during and after travel. Meta‐analysis of these results did not result in a significant difference (during travel: RR 1.04, 95% CI 0.77 to 1.40; 5 cohort studies, 2810 participants, post‐travel: RR 1.07, 95% CI 0.72 to 1.59; 3 cohort studies, 941 participants).
Pregnancy outcomes
One cohort study included respondents who were pregnant (Cunningham 2014) but did not report which prophylaxis the women took or on any outcomes related to pregnancy.
Mefloquine versus chloroquine
Description
RCTs
We included five RCTs comparing mefloquine with chloroquine that reported on efficacy and six on safety (Table 14). Trials were conducted in immune or semi‐immune adult populations in the Ivory Coast (Sossouhounto 1995), Malawi (Steketee 1996), Nigeria (Salako 1992) Thailand (Boudreau 1991; Bunnag 1992) and the USA. (Boudreau 1993). The Malawi trial by Steketee 1996 was limited to pregnant women. None included non‐immune travellers or children. All six trials used interview with study personnel to obtain information about adverse events. Boudreau 1993 excluded participants with a history of psychiatric or neurological problems.
12. Mefloquine versus chloroquine; characteristics of included studies for safety.
| Study ID | Participants | Number enrolled | Method of adverse event monitoring | Significant exclusions for psychiatric side effects | Trial duration | Source of funding |
| RCT s | ||||||
| Boudreau 1991 | Thai gem miners | 501 | Interview with study personnel | None | 14 weeks | USA Army |
| Boudreau 1993 | USA soldiers | 359 | Interview with study personnel and computerised questionnaire | "M edical history of psychiatric or neurological problems within the last 5 years" | 13 weeks | Not mentioned |
| Bunnag 1992 | Thai adult mal es | 605 | Interview with study personnel | None | 24 weeks | Roche |
| Salako 1992 | Nigerian adult males | 567 | Interview with study personnel | None | 24 weeks | Not mentioned |
| Sossouhounto 1995 | Ivory C oast adult males | 500 | " Access to the village health centre. Clinical examination with study personnel" | None | 20 weeks | Not mentioned |
| Steketee 1996 | Pregnant Malawian women | 4220 | Interview with study personnel | None | Monitored from enrolment to delivery | Government funding |
| Non‐randomised studies | ||||||
| Participants | Number enrolled | Method of adverse event monitoring | Factors influencing drug allocation | Duration of travel | Source of funding | |
| Albright 2002 | USA travelling children aged < 13 years | 177 | Interview with study personnel | Allocation based on guidelines and participant preference | Various, not specified | Not mentioned |
| Corominas 1997 | Spanish short‐term adult travellers | 1054 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Maximum 6 weeks | Not mentioned |
| Cunningham 2014 | UK Foreign and Commonwealth Office staff | 327 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | 0 to 36 months | Not mentioned |
| Hill 2000 | USA short‐term travellers | 822 | Interview with study personnel | Allocation based on guidelines and participant preference | Median 19 days, up to 90 days | Not mentioned |
| Korhonen 2007 | Peace Corps volunteers | 2701 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | ≥ 6 months | Two staff employed by Peace Corps |
| Laver 2001 | Adult short‐term travellers | 660 | Participant self‐reported questionnaire | No information available | 93% < 4 weeks | " No financial interests to disclose" |
| Laverone 2006 | Italian short‐term travellers | 1176 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | > 90% 0 to 30 days | Not mentioned |
| Lobel 2001 | Adult short‐term travellers | 5626 | Participant self‐reported questionnaire | No information available | M ost < 5 weeks | " No financial interests to disclose" |
| Napoletano 2007 | Italian short‐term travellers | 1906 | Telephone interview | Allocation based on guidelines and participant preference | Mean 2 weeks, range 0 to > 35 days | Not mentioned |
| Petersen 2000 | Danish travellers | 4154 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Various, 65% < 3 weeks | Not mentioned |
| Rietz 2002 | Swedish short‐term travellers | 491 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | " Most" 2 to 4 weeks | Not mentioned |
| Steffen 1993 | Adult short‐term travellers | 145,003 | Participant self‐reported questionnaire | No information available | 98% stayed between 1 and 4 weeks | Roche |
| Stoney 2016 | USA short‐term travellers | 370 | Participant self‐reported questionnaire | Allocation based on guidelines and participant preference | Median duration 13 days | Government funding |
| Tan 2017 | Peace Corps volunteers | 8931 | Participant self‐reported questionnaire | No information available | Various, not specified | No dedicated funding |
| Waner 1999 | Adult short‐term travellers | 3051 | Participant self‐reported questionnaire | No information available | A pprox. 6 weeks | " not funded by an external body" |
None of the trials adequately described random sequence generation or allocation concealment. Participants were adequately blinded in four trials (Boudreau 1993; Bunnag 1992; Salako 1992; Sossouhounto 1995), the trial in pregnant women did not blind participants or outcome assessors (Steketee 1996). We judged three of the trials to be at high risk of selective reporting of safety outcomes. Bunnag 1992 was funded by Roche (manufacturer of mefloquine). Five trials actively sought information on adverse events (Boudreau 1991; Boudreau 1993; Bunnag 1992; Salako 1992; Steketee 1996) and all collected information prospectively (Table 15).
13. Mefloquine versus chloroquine; quality of adverse events reporting.
| Study ID | Harms predefined¹ | Description of ascertainment technique² | Active or passive monitoring?³ | Prospective or retrospective data collection? |
| RCTs | ||||
| Boudreau 1991 | Adequate | Adequate | Active | Prospective |
| Boudreau 1993 | Adequate | Adequate | Active | Prospective |
| Bunnag 1992 | Inadequate " Adverse events were defined clinically, and starting week 14, volunteers reporting adverse events were interviewed by members of the hospital team" |
Adequate | Active | Prospective |
| Salako 1992 | Inadequate " Particular attention was paid to complaints such as fever, chills, malaise, nausea and vomiting, rashes and other symptoms and signs that could be regarded as adverse events." Comment: no clear definition of adverse events wa s provided |
Adequate | Active | Prospective |
| Sossouhounto 1995 | Inadequate " Participants had access to a village health center, where they could notify personnel of any malaise or side effects" |
Unclear " Clinical examinations and parasitologic tests were performed every 4 weeks" |
Passive | Prospective |
| Steketee 1996 | Adequate | Adequate | Active | Prospective |
| Cohort studies | ||||
| Albright 2002 | Adequate | Adequate | Passive | Retrospective |
| Corominas 1997 | Inadequate Comment: insufficient information wa s provided about the questions that travellers were asked |
Adequate | Active | Retrospective |
| Cunningham 2014 | Inadequate Comment: questionnaire included a targeted list of side effects, including " other psychological problems" . What was included within this was not defined |
Adequate | Passive | Unclear Comment: questionnaire was performed while participants were still taking chemoprophylaxis medication, although 75% were non‐compliant |
| Hill 2000 | Inadequate Comment: insufficient information wa s provided about the questions that travellers were asked |
Adequate | Active | Retrospective |
| Korhonen 2007 | Adequate | Adequate | Passive | Unclear Comment: No information wa s provided regarding the timing of the questionnaire during treatment |
| Laverone 2006 | Adequate | Adequate | Passive | Retrospective |
| Lobel 2001 | Inadequate "Travellers… were given a questionnaire that asked for... adverse health events attributed to those drugs" |
Adequate | Passive | Unclear Comment: information was collected at the airport, when travellers should still have been taking the prophylactic regimen |
| Napoletano 2007 | Unclear Comment: adverse events were categorised on a scale of one to four, but it is unclear whether and how causality was assessed |
Adequate | Active | Retrospective |
| Petersen 2000 | Inadequate Comment: i t wa s unclear whether the questionnaire implied causality to the drug regimen |
Adequate | Active | Retrospective |
| Rietz 2002 | Adequate | Adequate | Active | Retrospective |
| Steffen 1993 | Adequate | Adequate | Passive | Unclear Comment: information was collected during the flight home, when travellers should still have been taking the prophylactic regimen |
| Stoney 2016 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Inadequate Comment: n o information wa s reported on how adverse events were ascertained |
Active | Prospective |
| Tan 2017 | Adequate | Adequate | Active | Retrospective |
| Waner 1999 | Inadequate Comment: insufficient information provided on the questions that travellers were asked |
Adequate | Passive | Unclear Comment: information was collected during the flight home, when travellers should still have been taking the prophylactic regimen |
1. Were harms pre‐defined using standardised or precise definitions?
2. Was ascertainment technique adequately described?
3. Monitoring classed as 'active' if it occurred at set time points during treatment.
For full description of analysis methods, see Table 4.
Cohort studies
We included 15 cohort studies in this comparison; 12 included short‐term travellers (Albright 2002; Corominas 1997; Hill 2000; Laver 2001; Laverone 2006; Lobel 2001; Napoletano 2007; Petersen 2000; Rietz 2002; Steffen 1993; Stoney 2016; Waner 1999) and three longer‐term occupational travellers (Cunningham 2014; Korhonen 2007; Tan 2017) (Table 14). Albright 2002 included only children. Twelve studies used participant‐self reported questionnaires to collect information about adverse events; three of these, including the largest study (Steffen 1993, 145,003 participants), collected information from travellers flying back to Europe from Africa. The remaining three studies collected information through interviews with study personnel (Albright 2002; Hill 2000; Napoletano 2007)
Eight of the cohort studies had non‐response rates of over 20% (Figure 6). We judged 14 cohort studies to be at low risk of missing data, the largest study (Steffen 1993) was at moderate risk due to a 15% loss to follow‐up between the first and second questionnaire in the second phase of the study. Steffen 1993 did not report on non‐serious adverse effects from the first phase of the study (44,677 participants) and was funded by Roche (manufacturer of mefloquine). Six studies collected information about adverse events at set time points (Corominas 1997; Hill 2000; Napoletano 2007; Petersen 2000; Rietz 2002; Stoney 2016; Tan 2017), and one collected information prospectively (Stoney 2016) (Table 15; Figure 6).
6.
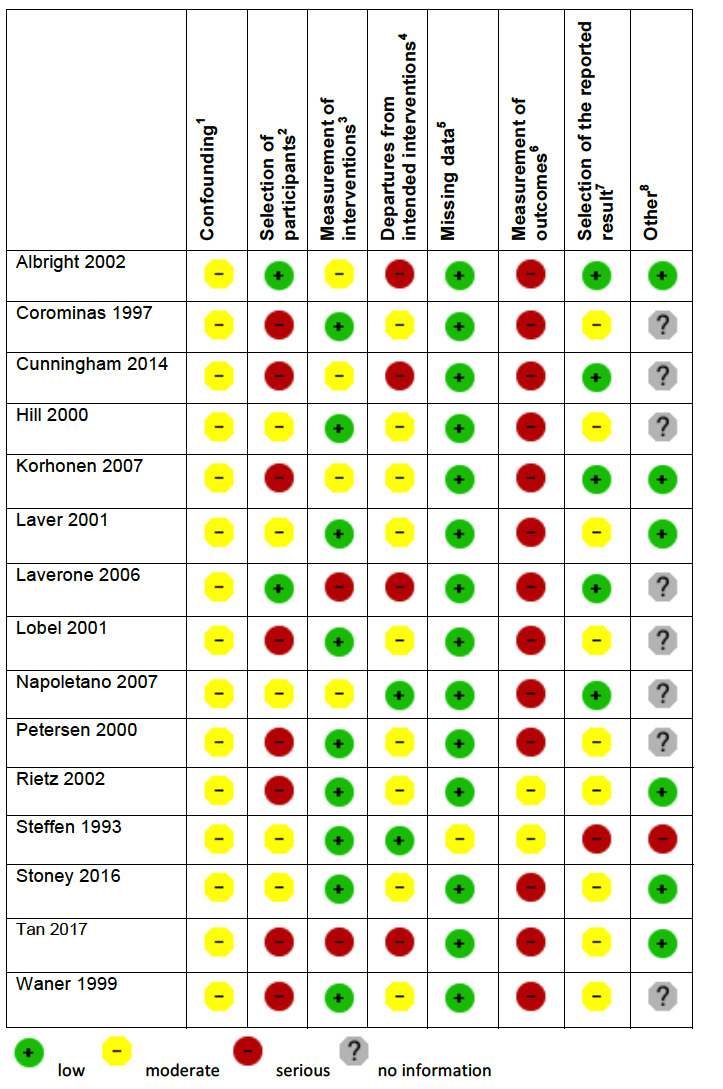
'Risk of bias' summary in cohort studies: mefloquine versus chloroquine
1Assesses whether our pre‐defined confounders are measured and balanced across groups. 2Assesses the non‐response rate of prospective participants. 3Assesses the risk that participants labelled as taking mefloquine (or another antimalarial) actually took something else. 4Assesses the risk that participants whose adverse effects are attributed to mefloquine (or another antimalarial) actually took another drug as well. 5Assesses whether outcome data reasonably complete for most participants and whether intervention status reasonably complete for those in whom it was sought. 6Assesses whether the outcome measure was subjective, and whether participants and outcome assessors were blinded. 7Assesses whether it is clear that all information collected within the study has been reported. 8Assesses the risk of bias due to influence by a corporate study sponsor.
Efficacy
Participants who took mefloquine were less likely to experience malaria than participants who took chloroquine (RR 0.38, 95% CI 0.28 to 0.52; 4 RCTs, 877 participants, Analysis 4.1). However, two RCTs were conducted in settings with known chloroquine resistance at the study sites, and the other two reported no episodes of malaria in either study arm. All RCTs included semi‐immune populations, and were conducted over 20 years ago.
4.1. Analysis.
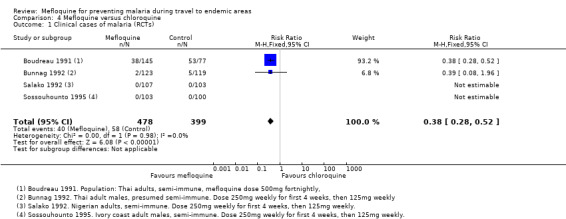
Comparison 4 Mefloquine versus chloroquine, Outcome 1 Clinical cases of malaria (RCTs).
Safety
Serious adverse events or effects
Across four RCTs, two serious adverse events were reported in 529 mefloquine users and none in 471 chloroquine users; the difference between groups was not significant (RR 2.77, 95% CI 0.32 to 23.85; 5 RCTs, 1000 participants, Analysis 4.2, Table 8). Both events were psychiatric admissions due to depression and suicidal thoughts; both study participants had previous psychiatric histories. In one case, the participant's psychiatrist did not think the event was drug‐related, and in the other "felt this individual's current depression was not drug related, unless it was aggravated by inability to sleep". Additionally, Steketee 1996 described one withdrawal due to a "neuropsychiatric side effect" (disorientation to time and place) but did not provide enough detail to meet our definition of serious adverse event or effect.
4.2. Analysis.
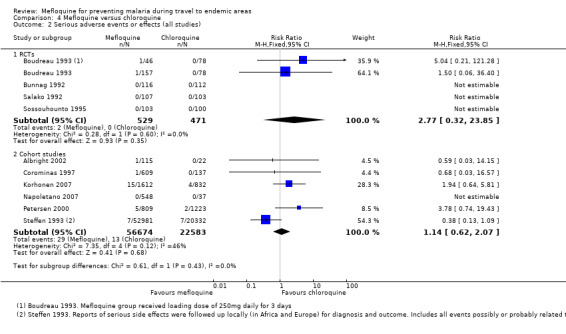
Comparison 4 Mefloquine versus chloroquine, Outcome 2 Serious adverse events or effects (all studies).
Four cohort studies reported a total of 29 serious adverse effects (attributed by users to the study drug) in 56,674 mefloquine users, and 13 serious adverse effects in 22,583 chloroquine users. The difference between groups was not statistically significant (RR 1.14, 95% CI 0.62 to 2.07; 6 cohort studies; 79,257 participants; Analysis 4.2). Serious side effects in mefloquine users were psychological (11 cases), dizziness (5), seizures (3), heart palpitations (2), abdominal pain (1), blackout (2), visual disturbance (1), limb numbness (1), yeast infection (1), and two which were not described (Table 9). Those in chloroquine users were psychological (4 cases), seizures (3), abdominal pain (1) and visual disturbance (1).
Discontinuations of the study drug due to adverse effects
There was no differences between groups in the number of discontinuations due to adverse effects in the RCTs (RR 1.60, 95% CI 0.61 to 4.18; 3 RCTs, 815 participants, Analysis 4.3) or cohort studies in short‐term international travellers (RR 0.99, 95% CI 0.78 to 1.26; 6 cohort studies, 55,397 participants, Analysis 4.3). However, in the two cohort studies in longer‐term occupational travellers, mefloquine users were significantly more likely to stop taking medication (RR 2.97, 95% CI 2.41 to 3.66; 2 cohort studies; 6085 participants; Analysis 4.3).
4.3. Analysis.
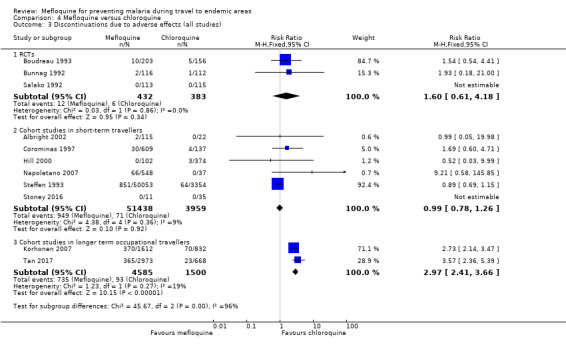
Comparison 4 Mefloquine versus chloroquine, Outcome 3 Discontinuations due to adverse effects (all studies).
Prespecified adverse effects
The RCTs only reported adverse events (all symptoms without assessing whether they might be related to the study drug). Our primary analysis was therefore taken from the six cohort studies reporting adverse effects.
Gastrointestinal symptoms
There were no consistent differences between groups for nausea (RR 1.23, 95% CI 0.89 to 1.68; I² statistic = 78%, 6 cohort studies, 58,984 participants, Analysis 4.4), vomiting (RR 1.05, 95% CI 0.78 to 1.40; 5 cohort studies, 5577 participants, Analysis 4.5) or abdominal pain (RR 0.99, 95% CI 0.80 to 1.22; 4 cohort studies, 5440 participants; Analysis 4.6). This was consistent with adverse events reported by RCTs (Analysis 4.4; Analysis 4.5; Analysis 4.6)
4.4. Analysis.
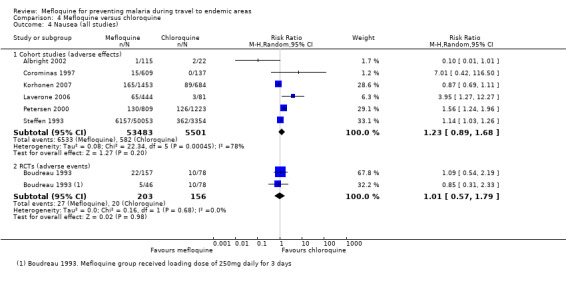
Comparison 4 Mefloquine versus chloroquine, Outcome 4 Nausea (all studies).
4.5. Analysis.
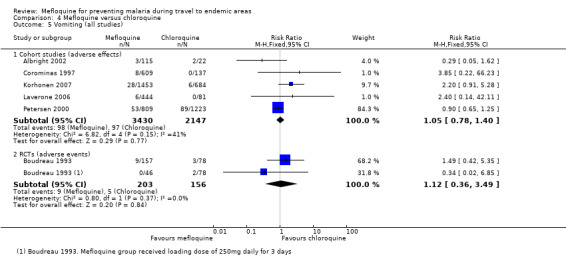
Comparison 4 Mefloquine versus chloroquine, Outcome 5 Vomiting (all studies).
4.6. Analysis.
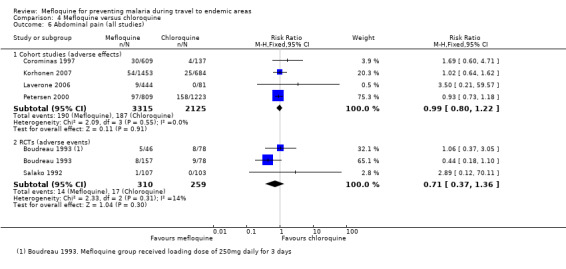
Comparison 4 Mefloquine versus chloroquine, Outcome 6 Abdominal pain (all studies).
Overall, mefloquine users were less likely to report diarrhoea but this finding was from a single cohort study with over 90% of the weight in the meta‐analysis (RR 0.84, 95% CI 0.74 to 0.95; 5 cohort studies, 5577 participants; Analysis 4.7). No difference was seen in the RCTs (Analysis 4.7).
4.7. Analysis.
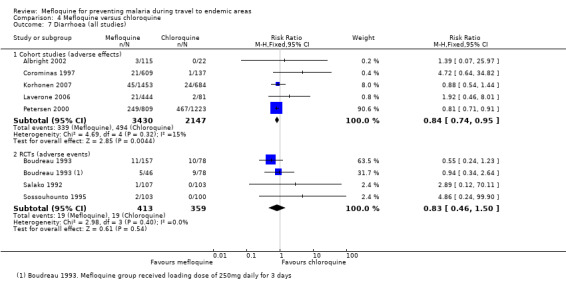
Comparison 4 Mefloquine versus chloroquine, Outcome 7 Diarrhoea (all studies).
Neurological symptoms
In the cohort studies, there was no substantial difference between groups in the proportion of participants reporting headache (RR 0.84, 95% CI 0.53 to 1.34; 6 cohort studies, 56,998 participants, Analysis 4.8), but mefloquine users reported more dizziness (RR 1.51, 95% CI 1.34 to 1.70; 5 cohort studies, 56,710 participants; Analysis 4.9). The RCTs reporting adverse events did not demonstrate a difference between groups (Analysis 4.8; Analysis 4.9).
4.8. Analysis.
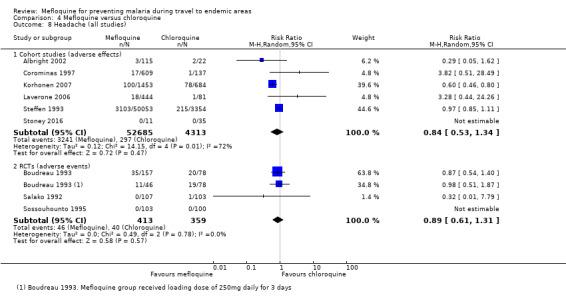
Comparison 4 Mefloquine versus chloroquine, Outcome 8 Headache (all studies).
4.9. Analysis.
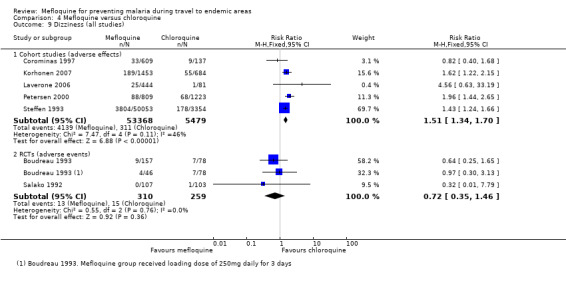
Comparison 4 Mefloquine versus chloroquine, Outcome 9 Dizziness (all studies).
Psychological symptoms
Across the cohort studies, mefloquine users were more likely to report abnormal dreams (RR 1.21, 95% CI 1.10 to 1.33; 4 cohort studies, 2845 participants, Analysis 4.10), anxiety (RR 6.30, 95% CI 4.37 to 9.09; 3 cohort studies, 3408 participants, Analysis 4.12), depressed mood (RR 3.14, 95% CI 1.15 to 8.57; I² statistic = 90%; 5 cohort studies, 58,855 participants, Analysis 4.13) and abnormal thoughts or behaviour (RR 5.49, 95% CI 2.65 to 11.35; 4 cohort studies, 4831 participants, Analysis 4.14). Of these outcomes only abnormal dreams was reported by RCTs and the result was consistent with the cohort studies (Analysis 4.10). Insomnia was reported by five cohort studies (RR 1.81, 95% CI 0.73 to 4.51; 5 cohort studies, 56952 participants) and two RCTs (RR 1.19, 95% CI 0.76 to 1.84; 2 RCTs, 359 participants), and no consistent differences were seen between groups (Analysis 4.11).
4.10. Analysis.
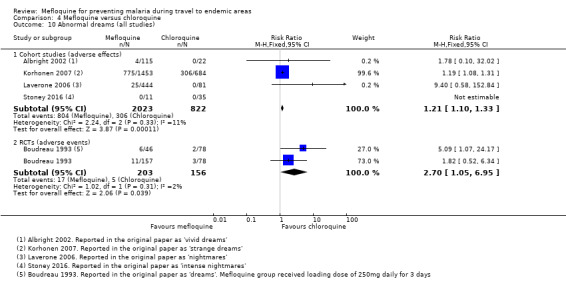
Comparison 4 Mefloquine versus chloroquine, Outcome 10 Abnormal dreams (all studies).
4.12. Analysis.
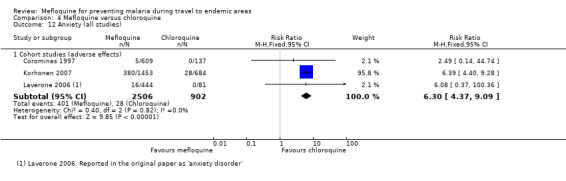
Comparison 4 Mefloquine versus chloroquine, Outcome 12 Anxiety (all studies).
4.13. Analysis.
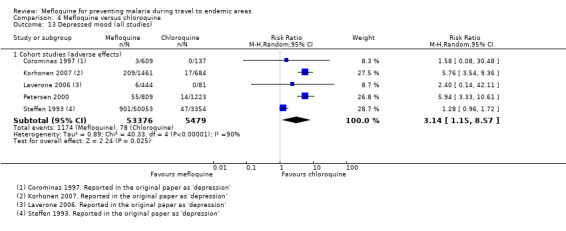
Comparison 4 Mefloquine versus chloroquine, Outcome 13 Depressed mood (all studies).
4.14. Analysis.
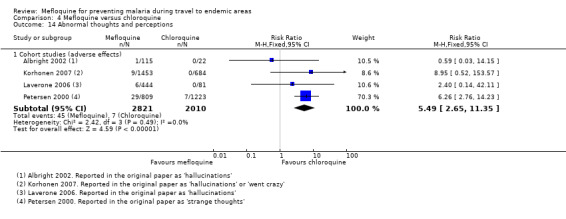
Comparison 4 Mefloquine versus chloroquine, Outcome 14 Abnormal thoughts and perceptions.
4.11. Analysis.
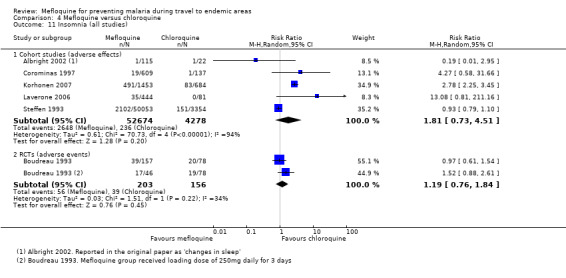
Comparison 4 Mefloquine versus chloroquine, Outcome 11 Insomnia (all studies).
Other prespecified adverse symptoms
There were no consistent differences demonstrated in reported pruritis between groups in cohort studies (RR 1.13, 95% CI 0.92 to 1.40; 2 cohort studies; 55,544 participants) or RCTs (RR 0.28, 95% CI 0.03 to 2.93; 2 RCTs, 413 participants; Analysis 4.15). There were no differences in visual impairment in cohort studies (RR 1.10, 95% CI 0.50 to 2.44; I² statistic = 90%, 5 cohort studies, 58,847 participants), or in the single RCT (RR 0.14, 95% CI 0.01 to 2.63; 210 participants, Analysis 4.16).
4.15. Analysis.
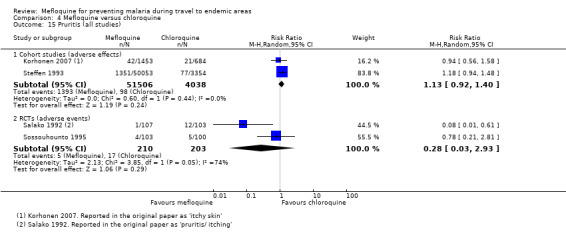
Comparison 4 Mefloquine versus chloroquine, Outcome 15 Pruritis (all studies).
4.16. Analysis.
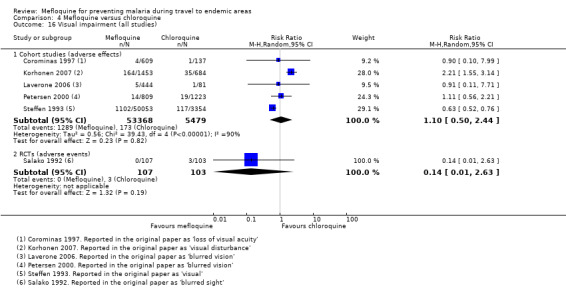
Comparison 4 Mefloquine versus chloroquine, Outcome 16 Visual impairment (all studies).
Prespecified adverse symptoms restricted to cohort studies in short‐term travellers
Analysis 4.18 presents the pre‐specified adverse symptoms restricted to the cohort studies in short‐term travellers.
4.18. Analysis.
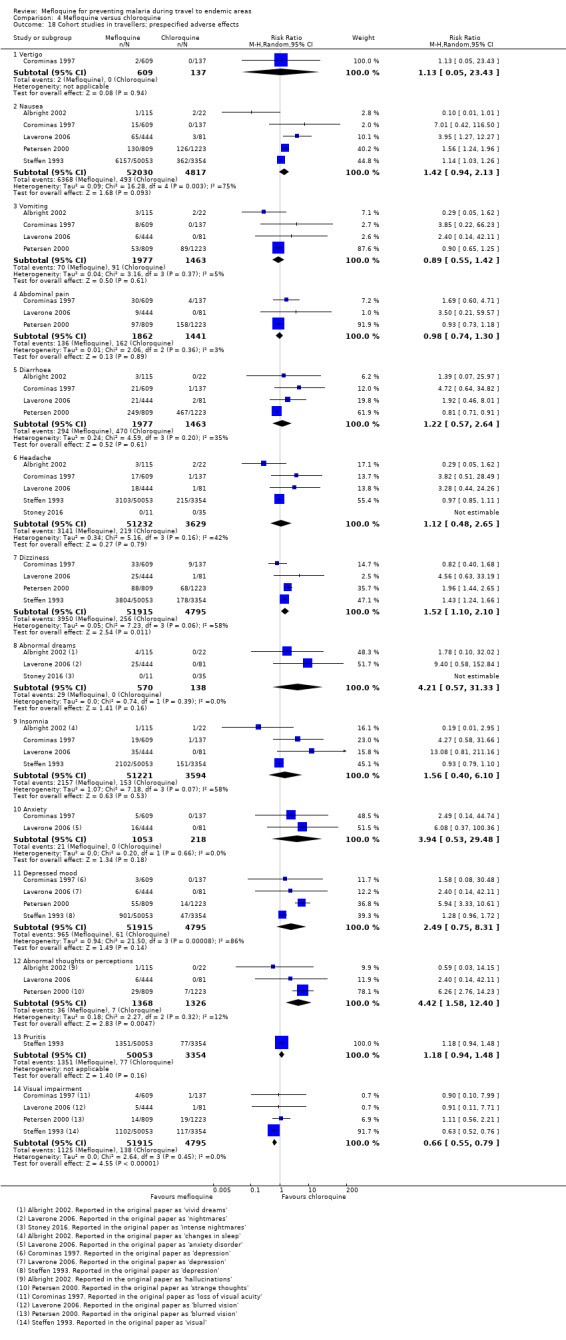
Comparison 4 Mefloquine versus chloroquine, Outcome 18 Cohort studies in travellers; prespecified adverse effects.
Other adverse outcomes
Other adverse effects reported by cohort studies were alopecia (hair loss), asthenia, altered spatial perception, balance disorder, confusion, decreased appetite, fatigue, hypoaesthesia, irritability, mouth ulcers, paraesthesia, palpitation, photosensitization, restlessness, slight illness, somnolence and yeast infection (Analysis 4.19). Of note, single cohort studies found that mefloquine users were more likely to report altered spatial perception (RR 3.16, 95% CI 1.55 to 6.45; 2032 participants), unsteadiness (RR 3.59, 95% CI 2.15 to 6.00; 2137 participants), alopecia (RR 1.69, 95% CI 1.27 to 2.25; 2137 participants), limb numbness (RR 20.26, 95% CI 1.23 to 333.93; 2137 participants) and tingling (RR 2.22, 95% CI 1.27 to 3.89; 2 cohort studies, 2778 participants).
4.19. Analysis.
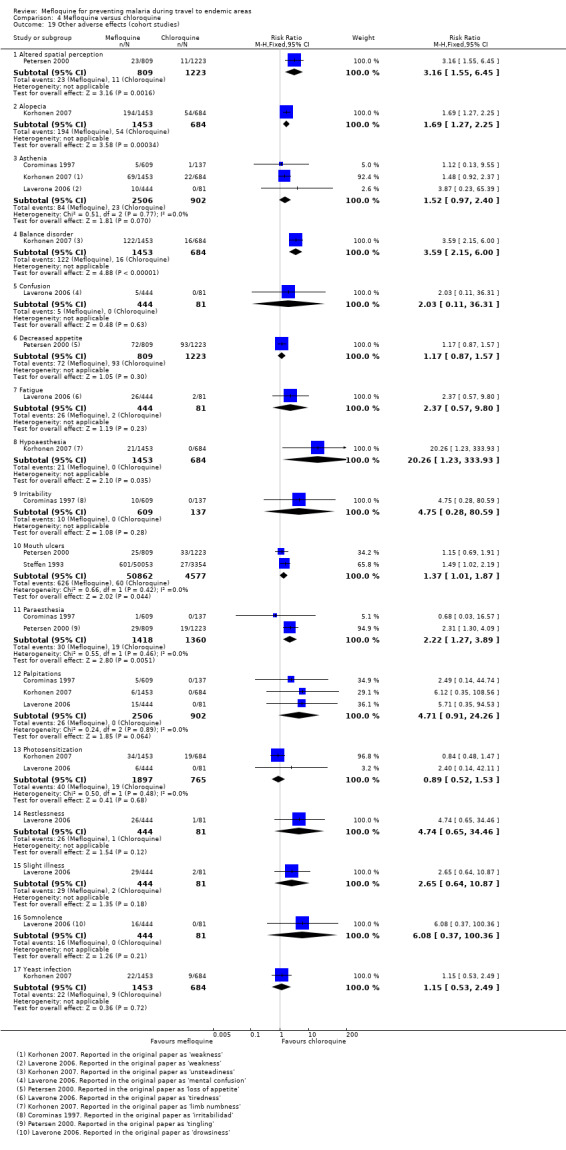
Comparison 4 Mefloquine versus chloroquine, Outcome 19 Other adverse effects (cohort studies).
Other adverse events reported by RCTs were abdominal distension, anger, disturbance in attention, irritability, loss of appetite, malaise and altered mood (Analysis 4.20). No statistically significant differences were noted.
4.20. Analysis.
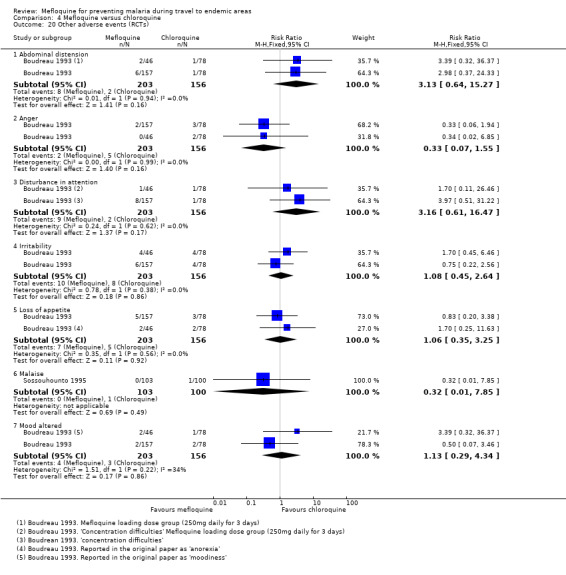
Comparison 4 Mefloquine versus chloroquine, Outcome 20 Other adverse events (RCTs).
Pregnancy‐related outcomes
One quasi‐randomized trial (Steketee 1996) was conducted in pregnant Malawian women and reported no difference between mefloquine and chloroquine for spontaneous abortions (RR 0.80, 95% CI 0.36 to 1.79; 2334 participants), still births (RR 1.01, 95% CI 0.67 to 1.52; 2334 participants) or congenital malformations (0 events in either study arm, 2334 participants, Analysis 4.21). Steketee 1996 sequentially allocated participants to each drug regimen, and did not blind participants or study personnel.
4.21. Analysis.
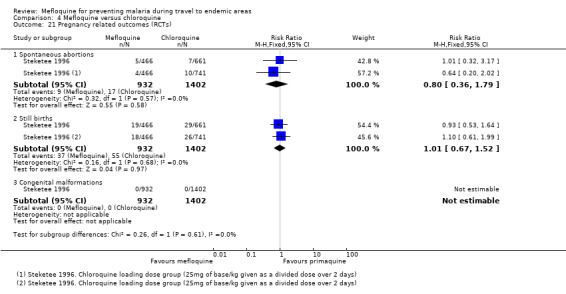
Comparison 4 Mefloquine versus chloroquine, Outcome 21 Pregnancy related outcomes (RCTs).
Adherence
Three cohort studies in short‐term travellers (Hill 2000; Laver 2001; Rietz 2002) compared the proportion of participants with 100% self‐reported adherence and found no difference overall (RR 1.00, 95% CI 0.90 to 1.13; 3 cohort studies, 852 participants, Analysis 4.22). Among participants in these studies, 84% of mefloquine users described themselves as adherent during travel (range 71% to 88%) compared to 82% of chloroquine users (range 82% to 85%). In the two studies in longer‐term occupational travellers, self‐reported adherence was higher in mefloquine users (RR 2.02, 95% CI 1.80 to 2.26; 2 cohort studies, 5777 participants).
4.22. Analysis.
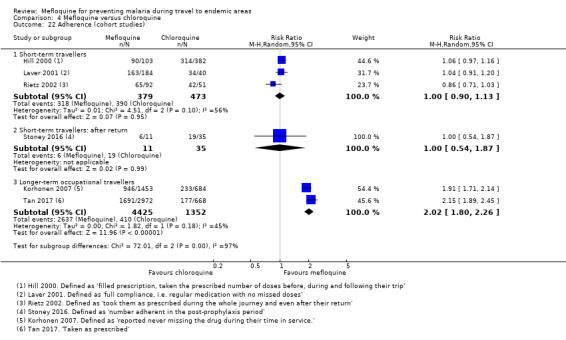
Comparison 4 Mefloquine versus chloroquine, Outcome 22 Adherence (cohort studies).
One study (Stoney 2016) measured adherence in the post‐travel period and found no difference (RR 1.00, 95% CI 0.54 to 1.87; 46 participants, Analysis 4.22). However, rates of completion were low in both groups (56% in mefloquine users and 54% in chloroquine users).
Subgroup analyses
Given the similarity in adverse effect profiles for mefloquine compared to the two main alternatives (doxycycline and atovaquone‐proguanil), we combined findings from the two comparisons and performed a series of subgroup analyses to explore the effects of study design, duration of travel, and military versus non‐military participants.
Prespecified adverse effects
Study design
Only one RCT performed a blinded assessment of whether there was a reasonable possibility that any reported symptoms could be related to the study drug (Overbosch 2001). We compared this with participants self‐reporting of adverse effects in cohort studies. The findings were largely consistent across study designs with mefloquine users experiencing higher rates of headache (Analysis 5.4), dizziness (Analysis 5.5), abnormal dreams (Analysis 5.6), insomnia (Analysis 5.7), anxiety (Analysis 5.8) and depressed mood (Analysis 5.9). Although the relative risk of psychiatric side effects was consistently slightly higher in cohort studies, in only one case was the test for subgroup differences statistically significant (abnormal dreams: RCT: RR 2.04, 95% CI 1.37 to 3.04; 976 participants, cohort studies: RR 7.30, 95% CI 2.51 to 21.18; 7 cohort studies, 4543 participants, test for subgroup differences P = 0.03).
5.4. Analysis.
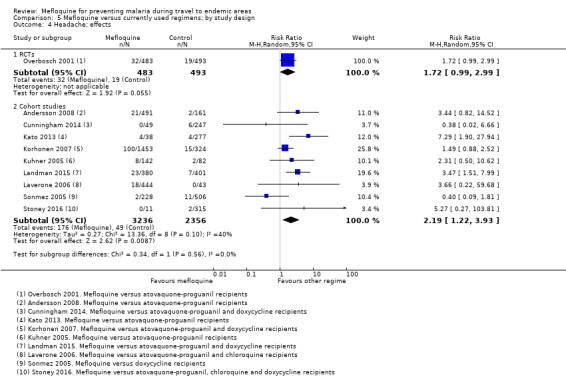
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 4 Headache; effects.
5.5. Analysis.
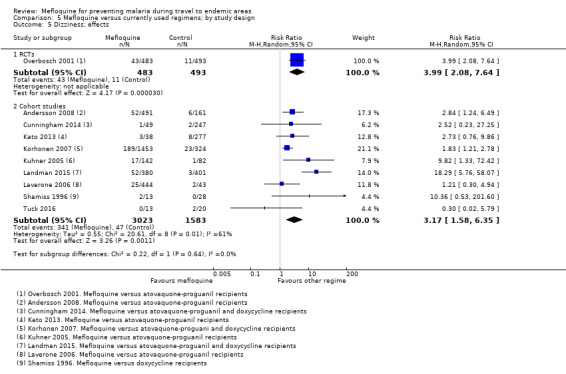
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 5 Dizziness; effects.
5.6. Analysis.
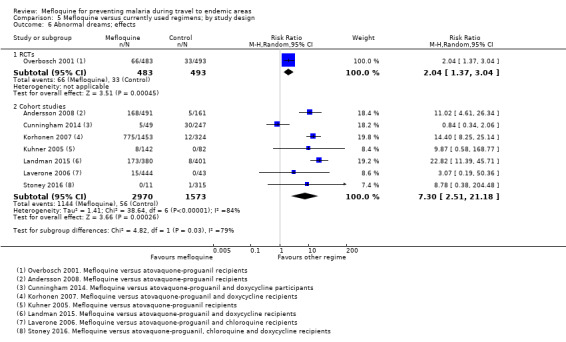
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 6 Abnormal dreams; effects.
5.7. Analysis.
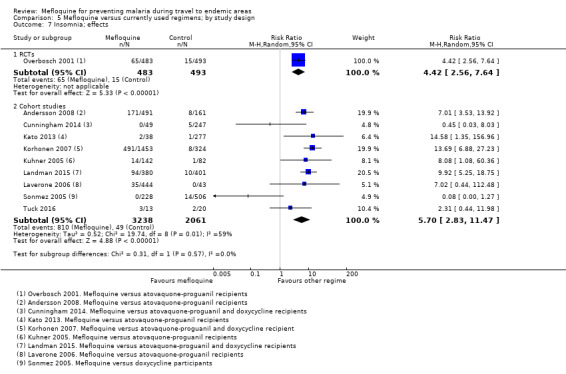
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 7 Insomnia; effects.
5.8. Analysis.
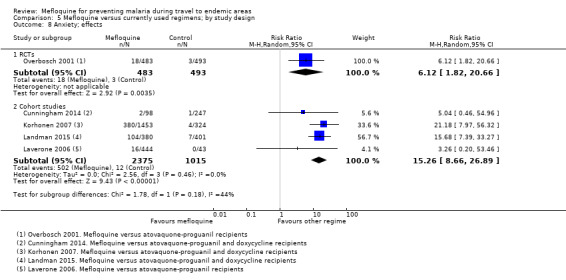
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 8 Anxiety; effects.
5.9. Analysis.
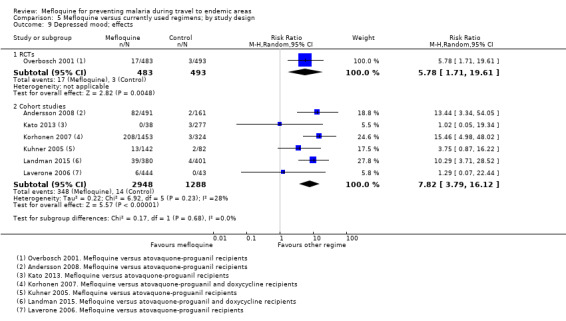
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 9 Depressed mood; effects.
Duration of travel
The relative risk of all psychological adverse effects was higher with longer‐term travel than in short‐term travel; insomnia (short‐term RR 3.09 versus longer‐term RR 8.67), anxiety (short‐term RR 3.26 versus longer‐term RR 18.05), depressed mood (short‐term RR 2.52 versus longer‐term RR 12.59) and abnormal thoughts and perceptions (short‐term RR 1.29 versus longer‐term RR 7.78) (Table 16). However, in only one case was the test for subgroup differences statistically significant (P range 0.02 to 0.40). This same effect was not observed with gastrointestinal symptoms (nausea, abdominal pain, diarrhoea) or neurological symptoms (headache, dizziness).
14. Mefloquine versus currently used regimens; by duration of travel.
| Mefloquine versus atovaquone‐proguanil and doxycycline | |||
| Outcome | Short‐ term travellers¹ | Longer‐ term travellers² | Test for subgroup differences |
| Relative effect (RR) (95% CI) Studies (participants) | Relative effect (RR) (95% CI) Studies (participants) | ||
| Serious adverse effects |
RR 5.38 (0.60 to 47.84) 3 cohort studies (2657) |
RR 0.93 (0.43 to 2.01) 3 cohort studies (3147) |
P = 0.14 |
| Discontinuations due to adverse effects (RCTs) |
RR 2.64 (1.51 to 4.62) 5 RCTs (2048) |
‐ | ‐ |
| Discontinuations due to adverse effects (cohort studies) |
RR 1.81 (0.86 to 3.80) 7 cohort studies (2907) |
RR 1.19 (0.45 to 3.17) 4 cohort studies (5711) |
P = 0.50 |
| Nausea |
RR 2.02 (0.87 to 4.68) 6 cohort studies (2469) |
RR 0.96 (0.22 to 4.18) 3 cohort studies (2725) |
P = 0.39 |
| Abdominal pain |
RR 0.66 (0.22 to 1.98) 5 cohort studies (1801) |
RR 0.30 (0.22 to 0.42) 3 cohort studies (2725) |
P = 0.18 |
| Diarrhoea |
RR 0.64 (0.15 to 2.71) 5 cohort studies (2428) |
RR 0.57 (0.22 to 1.49) 4 cohort studies (5187) |
P = 0.89 |
| Headache |
RR 2.39 (0.69 to 8.22) 5 cohort studies (2086) |
RR 2.09 (1.10 to 3.95) 4 cohort studies (3506) |
P = 0.85 |
| Dizziness |
RR 3.05 (1.15 to 8.12) 4 cohort studies (1067) |
RR 3.84 (1.34 to 11.00) 4 cohort studies (3506) |
P = 0.76 |
| Abnormal dreams |
RR 6.25 (1.16 to 33.67) 3 cohort studies (1037) |
RR 7.62 (2.06 to 28.18) 4 cohort studies (3506) |
P = 0.86 |
| Insomnia |
RR 3.09 (0.30 to 32.21) 4 cohort studies (1760) |
RR 8.67 (4.73 to 15.89) 4 cohort studies (3506) |
P = 0.40 |
| Anxiety |
RR 3.26 (0.20 to 53.46) 1 cohort study (487) |
RR 18.05 (9.75 to 33.42) 3 cohort studies (2854) |
P = 0.24 |
| Depressed mood |
RR 2.52 (0.76 to 8.29) 3 cohort studies (1026) |
RR 12.59 (6.47 to 24.49) 3 cohort studies (3210) |
P = 0.02 |
| Abnormal thoughts and behaviours |
RR 1.29 (0.07 to 22.44) 1 cohort study (487) |
RR 7.78 (1.12 to 54.06) 2 cohort studies (2558) |
P = 0.31 |
| Adherence: during travel |
RR 1.10 (1.03 to 1.18) 7 cohort studies (7241) |
RR 1.20 (0.88 to 1.62) 4 cohort studies (4890) |
P = 0.61 |
| Adherence: after return |
RR 1.04 (0.92 to 1.17) 4 cohort studies (1221) |
‐ | ‐ |
1 Short‐ term travellers: Approximately 3 weeks (range 1 day to 3 months). References: Goodyer 2011; Kato 2013; Kuhner 2005; Napoletano 2007; Laver 2001; Laverone 2006; Lobel 2001; Philips 1996; Schwartz 1999; Shamiss 1996; Sonmez 2005; Stoney 2016; Terrell 2015 2 Longer‐ term travellers: Approximately 6 months (range 0 to 36 months in Cunningham 2014 . Otherwise 3 months or longer). References Andersson 2008; Cunningham 2014; Korhonen 2007; Landman 2015; Saunders 2015; Sharafeldin 2010
Military versus non‐military participants
There were no significant differences in the relative risk of adverse effects between military and non‐military participants (Table 17). Very few cohort studies in military personnel reported on our prespecified symptoms. In one of these in which military personnel who took mefloquine for 6 months or longer (Andersson 2008), the rates of psychological side effects were significantly higher than in short‐term travellers, but not significantly different from other trials in longer‐term travellers.
15. Mefloquine versus currently used regimens; by military or non‐military participants.
| Mefloquine versus atovaquone‐proguanil and doxycycline | |||
| Outcome | Military¹ | Non‐military² | Test for subgroup differences |
| Relative effect (RR) (95% CI) Studies (participants) | Relative effect (RR) (95% CI) Studies (participants) | ||
| Serious adverse effects | 0 events in 1386 participants |
RR 1.21 (0.60 to 2.44) 4 cohort studies (4418) |
‐ |
| Discontinuations due to adverse effects (RCTs) |
RR 2.08 (0.13 to 32.73) 2 RCTs (441) |
RR 2.22 (1.17 to 4.21) 4 RCTs (1669) |
P = 0.96 |
| Discontinuations due to adverse effects (cohorts) |
RR 1.24 (0.32 to 4.88) 4 cohort studies (3408) |
RR 1.89 (1.35 to 2.64) 8 cohort studies (8938) |
P = 0.56 |
| Nausea |
RR 1.39 (0.36 to 5.36) 4 cohort studies (1578) |
RR 1.70 (0.60 to 4.81) 6 cohort studies (3767) |
P = 0.26 |
| Abdominal pain |
RR 0.43 (0.14 to 1.29) 4 cohort studies (1578) |
RR 0.56 (0.23 to 1.35) 5 cohort studies (3099) |
P = 0.72 |
| Diarrhoea |
RR 0.30 (0.09 to 0.96) 4 cohort studies (3999) |
RR 1.05 (0.54 to 2.06) 6 cohort studies (3767) |
P = 0.07 |
| Headache |
RR 1.19 (0.14 to 9.79) 2 cohort studies (1386) |
RR 2.48 (1.40 to 4.40) 7 cohort studies (4206) |
P = 0.51 |
| Dizziness |
RR 2.95 (1.37 to 6.36) 3 cohort studies (844) |
RR 3.58 (1.39 to 9.25) 6 cohort studies (3880) |
P = 0.76 |
| Abnormal dreams |
RR 11.02 (4.61 to 26.34) 1 cohort study (652) |
RR 6.59 (1.74 to 25.00) 6 cohort studies (3891) |
P = 0.53 |
| Insomnia |
RR 2.34 (0.41 to 13.35) 3 cohort studies (1537) |
RR 10.24 (6.26 to 16.76) 6 cohort studies (3880) |
P = 0.11 |
| Anxiety | ‐ |
RR 16.94 (9.36 to 30.64) 4 cohort studies (3390) |
‐ |
| Depressed mood |
RR 13.44 (3.34 to 54.05) 1 cohort study (652) |
RR 6.49 (2.66 to 15.85) 5 cohort studies (3584) |
P = 0.39 |
| Abnormal thoughts and behaviours | ‐ |
RR 5.11 (1.11 to 23.53) 3 cohort studies (3045) |
‐ |
| Adherence: during travel |
RR 1.18 (1.00 to 1.40) 5 cohort studies (4652) |
RR 1.16 (0.99 to 1.35) 8 cohort studies (10785) |
P = 0.85 |
| Adherence: after return |
RR 1.16 (0.86 to 1.55) 1 cohort study (43) |
RR 1.02 (0.89 to 1.16) 3 cohort studies (1178) |
P = 0.44 |
1 Military participants: References: RCTs: Arthur 1990; Ohrt 1997. Cohort studies: Andersson 2008, Saunders 2015; Shamiss 1996; Sonmez 2005; Terrell 2015; Tuck 2016 2 Non‐military participants: References: RCTs: Overbosch 2001; Schlagenhauf 2003; van Riemsdijk 2002; Weiss 1995. Cohort studies: Cunningham 2014; Goodyer 2011; Kato 2013; Kuhner 2005; Korhonen 2007; Landman 2015; Laver 2001; Laverone 2006; Lobel 2001; Napoletano 2007; Philips 1996; Schwartz 1999; Sharafeldin 2010; Stoney 2016
Adherence
Study design
Across cohort studies, self‐reported complete adherence was slightly higher in participants who took mefloquine than in users of other antimalarial agents (RR 1.16, 95% CI 1.03 to 1.30; 11 cohort studies, 12131 participants, Analysis 5.13). However, there was no difference in self‐reported completion of the treatment after return (RR 1.04, 95% CI 0.92 to 1.17; 4 cohort studies, 1221 participants, Analysis 5.14).
5.13. Analysis.
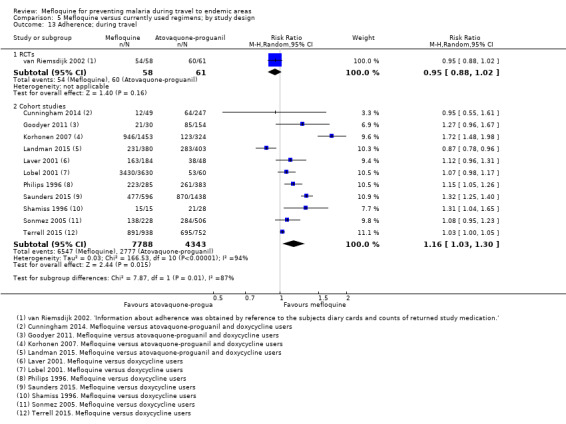
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 13 Adherence; during travel.
5.14. Analysis.
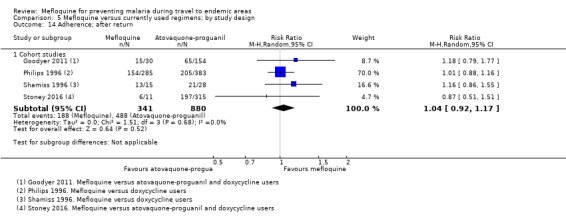
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 14 Adherence; after return.
Duration of travel
Self‐reported complete adherence was slightly higher in short‐term travellers who took mefloquine than users of other antimalarial agents (RR 1.10, 95% CI 1.03 to 1.18; 7 cohort studies, 7241 participants). However, the same effect was not seen in longer‐term travellers (RR 1.20, 95% CI 0.88 to 1.62; 4 cohort studies, 4890 participants, test for subgroup differences P = 0.61, Table 16).
There was no overall difference in rates of completing the treatment regimen after return in short‐term travellers who took mefloquine than in those who received other antimalarial agents (RR 1.04, 95% CI 0.92 to 1.17; 4 cohort studies, 1221 participants). No studies in longer‐term travellers monitored adherence after return.
Military versus non‐military participants
There were no differences in self‐reported complete adherence when comparing military versus non‐military participants, either during travel or after return (Table 17).
Discussion
Summary of main results
Mefloquine efficacy
We included 12 randomized controlled trials (RCTs) that compared mefloquine with placebo; none were performed in short‐term international travellers, and most populations had a degree of immunity to malaria. The percentage of people developing a malaria episode in the control arm varied from 1% to 82% (median 22%) and in the mefloquine group 0% to 13% (median 1%).
In four other RCTs that directly compared mefloquine, atovaquone‐proguanil and doxycycline in non‐immune, short‐term international travellers, only one clinical case of malaria occurred (low certainty evidence).
Mefloquine safety versus currently used alternatives
Serious adverse effects have been reported for mefloquine and doxycyline, but not for atovaquone‐proguanil. Serious adverse effects are uncommon, and on statistical testing, no difference was detected between mefloquine and atovaquone‐proguanil (low‐certainty evidence), or between mefloquine and doxycycline (very low‐certainty evidence).
Participants who received mefloquine were more likely to discontinue their medication due to adverse effects than participants who received atovaquone‐proguanil (high‐certainty evidence), but there was no difference in comparisons with doxycycline (low‐certainty evidence).
We included one RCT and six cohort studies that reported our prespecified adverse effects that compared mefloquine and atovaquone‐proguanil. In the RCT in short‐term travellers, mefloquine users were more likely to report abnormal dreams (moderate‐certainty evidence), insomnia (moderate‐certainty evidence), anxiety (moderate‐certainty evidence), and depressed mood during travel (moderate‐certainty evidence). The cohort studies in longer‐term travellers were consistent with these findings but most had larger effect sizes. Mefloquine users were also more likely to report nausea (high‐certainty evidence) and dizziness (high‐certainty evidence).
We included six cohort studies in longer‐term occupational travellers that compared mefloquine with doxycycline which reported our prespecified adverse effects. We also included one RCT in military personnel and one cohort in short‐term travellers that reported adverse events. Mefloquine users were more likely to report abnormal dreams (very low‐certainty evidence), insomnia (very low‐certainty evidence), anxiety (very low‐certainty evidence) and depressed mood (very low‐certainty evidence). The findings of the single cohort study reporting adverse events in short‐term international travellers were consistent with these findings but the single RCT in military personnel did not demonstrate a difference between groups in the frequency of abnormal dreams or insomnia. Doxycycline users were more likely to report dyspepsia (very low‐certainty evidence), photosensitivity (very low‐certainty evidence), vomiting (very low‐certainty evidence) and vaginal thrush (very low‐certainty evidence).
Comparisons with chloroquine showed a broadly consistent pattern with these results.
Overall completeness and applicability of evidence
Mefloquine has been licensed for prevention of malaria in travellers since the late 1980s, and as such, it is perhaps surprising how few well‐conducted RCTs were available. However, because we were mainly interested in the adverse effect profiles of different antimalarial agents, cohort studies (of which there are many) are probably the most appropriate study design despite their inherent limitations. Most RCTs excluded people with a previous history of mental health problems, precluding an analysis of whether psychological side effects are more common in this group. Conversely, many of the cohort studies explicitly stated that the choice of antimalarial agent was influenced by both past medical history and personal preference. While this undoubtedly introduces some confounding between study groups, we consider this confounding to be appropriate and directly applicable to clinical practice. Similarly, we would normally be cautious about interpreting unblinded self‐reported assessments of adverse effects and causality. In this scenario, self‐reported adverse effects provide useful and relevant information for travellers, who would also be unblinded. It should be noted that the reported adverse effects are largely self‐reported psychiatric symptoms and not formal psychiatric diagnoses.
Given the heterogeneity in trial design, mefloquine doses used, and the study population, we were unable to derive a reliable estimate for mefloquine efficacy. However, the evidence suggests that mefloquine is likely to be highly effective in reducing clinical episodes of malaria. Comparative trials found no difference in efficacy between mefloquine and atovaquone‐proguanil or doxycycline for preventing clinical malaria, but the number of malaria episodes was very low, and consequently, much larger trials would be needed to exclude clinically important differences. As a consequence, knowledge about antimalarial resistance patterns in the country of travel seems an appropriate approach to decision making rather than further RCTs.
The choice between antimalarial agents will therefore depend on how individual travellers rate the relative importance of specific adverse effects, pill burden and cost. Prophylactic mefloquine is widely acknowledged to cause abnormal dreams and psychological adverse effects and we found consistent evidence for these effects across comparisons with atovaquone‐proguanil, doxycycline and chloroquine (the most commonly used alternatives). Doxycycline does not have the same risk of psychological adverse effects, but is associated with increased risk of photosensitivity, dyspepsia, and vaginal thrush, which some travellers will undoubtedly consider important. In line with this, participants who received mefloquine were more likely to discontinue treatment due to adverse effects than participants who received atovaquone‐proguanil, but there was no difference in comparisons with doxycycline.
We found estimating the risk of serious psychological adverse effects from the studies was not straightforward. Study authors used the term 'serious' loosely, and often did not provide us with the detail required to determine whether these events met standardized definitions. Furthermore, the estimates of the absolute risk in both mefloquine and comparator arm varied considerably between trials, which may be related to data collection methods and the cut‐offs used rather than true differences among populations. Overall, we did not identify large differences in the risk of serious adverse effects among antimalarial agents; but what we did find was that the nature of these serious adverse effects corresponded with the known side effect profile of each drug.
The findings of our related systematic review which analysed deaths and parasuicides associated with mefloquine prophylaxis, and included case reports, had findings consistent with this (Tickell‐Painter 2017). This systematic review reports that there were no suicides we could reliably attribute to mefloquine prophylaxis, and one para‐suicide with a possible causal association. In the analysed reports, we identified two deaths with a probable association that appeared to be idiosyncratic drug reactions; the remaining eight deaths we categorised as “unlikely” to be related to mefloquine, or “unclassifiable”.
We believe it is important that the large retrospective healthcare record analyses did not demonstrate a clear quantitative association between mefloquine use and formal mental health disorders. This may reflect the inadequacy of the study methods to detect this outcome, but may also reflect the transient nature of the mood disturbance, with resolution once mefloquine is discontinued. We were unable to comment on the severity or duration of the reported adverse effects based on the available data.
The data on mefloquine at a prophylactic dose during pregnancy were limited (2 RCTs; no comparative cohort studies). Both RCTs included semi‐immune populations who did not travel.
Mefloquine has an advantage as the only malaria prophylaxis with a once weekly regimen. Many have cited this as a mechanism to improve adherence, which is notoriously low in all users of antimalarial prophylaxis. However, the evidence base for this assertion is weak, with almost all data originating from cohort studies which reported a variety of measures of self‐reported complete adherence.
We were unable to perform some prespecified subgroup analyses including children versus adults, female versus male travellers and pregnant versus non‐pregnant women. This meant we were unable to test whether women were more likely to experience adverse effects from mefloquine use (which has been widely reported in the literature).
We appreciate that the distinction between adverse events (all events regardless of relationship to the study drug) and adverse effects (events attributed by study authors or participants to the study drug) can seem arbitrary and cause confusion. However, we consulted extensively with methodologists who advised that both outcomes are useful to decision makers, and there is no overall gold standard. For example, reporting only the adverse effects (for example, hospitalizations, psychiatric side effects) thought to be attributed to the drug regimen can introduce selective bias by the study authors. For controversial or pharmaceutical company‐funded studies this can distort the outcomes. By comparing all events across both groups any difference in the relative risk can be compared without the potential for selective bias. However, this does have its own limitations, such as if the two groups were not comparable at baseline or if the sample size is not big enough to exclude differences due to chance. We therefore chose to include both options (events and effects) to give readers and decision makers the complete picture.
Quality of the evidence
In the 'Summary of findings' tables we present what we consider to be the best estimate of effect for each outcome, within each comparison. Where possible we chose the estimate from RCTs reporting adverse effects, but where this was not available we used estimates from cohort studies. However, when making judgements about the certainty of evidence we considered all the evidence available, as well as the consistency of the effect across different population groups and study designs.
For the comparison of mefloquine with atovaquone‐proguanil, the best estimates of effect came from a single, well‐conducted RCT in short‐term travellers, recording participant‐reported adverse effects. The findings of this study were supported by seven cohort studies in long‐term occupational travellers and military personnel. We considered the evidence of increased risk of abnormal dreams and insomnia to be high certainty because the effects were consistent across all population groups. However, we downgraded the effect estimate on anxiety and depressed mood for inconsistency to moderate certainty because there was substantial variation in the effect size across populations, with much larger effects in long‐term travellers and military personnel.
For the comparison of mefloquine with doxycycline, the only available RCT was very small, and reported adverse events rather than adverse effects. Consequently, we considered the effect estimates from cohort studies to be more reliable. Evidence from cohort studies was automatically downgraded to low based on the inherent bias in the study design. We further downgraded almost all estimates of effect for indirectness, because most data were from long‐term travellers and military personnel, and may therefore over estimate the effect in short‐term travel. The evidence is therefore considered to be very low‐certainty with little confidence in the size of the effect. It is important to note however, that the pattern of adverse effects with mefloquine in these cohort studies is entirely consistent with the pattern seen in comparisons of mefloquine with atovaquone‐proguanil and chloroquine.
Potential biases in the review process
During the course of this review we made changes to the protocol. Two changes were made to shorten the overall length of the review:
we excluded comparisons of mefloquine with primaquine and tafenoquine because these are planned for assessment in another Cochrane Review (Rodrigo 2016);
we excluded single‐arm cohort studies because there were sufficient data from comparative studies to reach reasonable conclusions. These studies have been analysed for the very rare outcomes of death or attempted suicide in another systematic review (Tickell‐Painter 2017).
We do not think these decisions biased the review.
Agreements and disagreements with other studies or reviews
Several recently published reviews regarding the safety of mefloquine have been narrative, and included little or no description of methods applied and a lack of clearly defined and prespecified outcomes (McCarthy 2015; Nevin 2015; Schlagenhauf 2010). McCarthy 2015 and Nevin 2015 discuss the policy implications of mefloquine use by the military which was beyond the scope of this Cochrane Review.
Schlagenhauf 2010 highlighted several areas in which mefloquine prophylaxis may be considered advantageous (during pregnancy and while breastfeeding, in long‐term travellers, travellers who are visiting friends and relatives and families with small children). The main disagreement with our review was in regard to safety in long‐term travellers, in whom the review authors refer to mefloquine as "a good option if well tolerated". This is based on a narrative analysis of a single cohort study which compared mefloquine users with users of chloroquine‐proguanil, which was not included in this review (Lobel 1993).
Our review added data from several additional studies evaluating longer‐term use (Andersson 2008; Cunningham 2014; Korhonen 2007; Landman 2015), and we found some observational evidence that risk of adverse effects was higher than with short‐term travel.
Our findings are broadly consistent with the previous version of this Cochrane Review, which was withdrawn (Jacquerioz 2015). Jacquerioz 2015 found higher rates of neuropsychiatric adverse events in mefloquine users compared with users of both atovaquone‐proguanil and doxycycline. We expanded on this finding by providing estimated risks for specific neurological and psychiatric symptoms, and by including additional data from cohort studies. Jacquerioz 2015 included a brief analysis of case reports of deaths associated with mefloquine in the Discussion. We excluded this analysis from this update, but this aspect has been addressed in a separate review of single‐arm cohort studies and case reports (Tickell‐Painter 2017).
Two recent reviews included evaluations of mefloquine efficacy and safety during pregnancy. González 2014 concluded there were no indications that mefloquine use during pregnancy carries an increased risk for the foetus. González 2014 included additional studies to those we included in this Cochrane Review, including mefloquine when used at treatment dose, or as intermittent presumptive treatment in pregnancy. Muanda 2015 also included mefloquine when used as intermittent presumptive treatment in pregnancy. Muanda 2015 reported findings from two trials in which the number of adverse events (Briand 2009), and number of serious adverse events (González 2014a) was higher in participants who received mefloquine as intermittent presumptive treatment in pregnancy than in those who received sulphadoxine‐pyrimethamine.
Authors' conclusions
Implications for practice.
The absolute risk of malaria during short‐term travel appears to be very low with all three established antimalarial agents (mefloquine, doxycycline and atovaquone‐proguanil).
The choice of antimalarial agent will therefore depend on how individual travellers rate the relative importance of specific adverse effects, pill burden and cost. Some will prefer mefloquine for its once‐weekly regimen, but this should be balanced against the increased frequency of abnormal dreams, anxiety, insomnia, and depressed mood during travel.
Implications for research.
Given the low absolute risk of malaria in travellers, very large trials would be necessary to exclude clinically important differences among antimalarial agents. As a consequence, knowledge about antimalarial resistance patterns in the country of travel seems an appropriate approach to decision making rather than further RCTs.
Although a large number of RCTs evaluating mefloquine prophylaxis have been performed, very few could be included in our analyses. Many RCTs chose to report proxy measures of psychiatric outcomes, such as Profile of Mood States questionnaires and Environmental Symptoms Questionnaires, which are difficult for clinicians and participants to interpret. Furthermore, many studies grouped symptoms together when reporting outcomes. 'Neuropsychiatric' or 'neuropsychologic' were commonly used terms, although the symptoms included varied from headaches to psychosis, making them of limited value in clinical decision making.
Even though we found moderate‐ and high‐certainty evidence that mefloquine use is associated with a range of psychological adverse effects, further RCTs could increase confidence in the size of the effect. The relative risk of psychological side effects was higher with long‐term use of mefloquine, although this finding was only statistically significant in one comparison. An alternative explanation is the possibility of an interaction between mefloquine and level of psychological stress given the occupation of participants surveyed (Foreign and Commonwealth Office workers, Peace Corps volunteers and military personnel). Further research should examine these potential interactions.
Furthermore, well‐designed trials could test hypotheses regarding male versus female users, whether mefloquine users with a previous history of mental health problems are more likely to experience psychological adverse effects, and the severity or duration of the reported adverse effects.
What's new
| Date | Event | Description |
|---|---|---|
| 20 October 2017 | New search has been performed | New author team appointed. Protocol rewritten. Criteria for included studies, methods, and outcomes revised. Protocol checked and agreed by two editors. Modifications included:
|
| 20 October 2017 | New citation required and conclusions have changed | The previous version of this review, 'Drugs for preventing malaria in travellers', was withdrawn. The reason for this was the editorial team detected several errors in a subsidiary analysis of case reports described in the discussion and in appendix 9 of the withdrawn review. This new edition covers only mefloquine and comparisons with alternative drugs. The case reports analysis has been removed entirely. A separate team, including the lead author of this review, carried out a new review of case reports of death and parasuicide associated with mefloquine, published in the journal, 'Travel Medicine and Infectious Disease'. |
History
Protocol first published: Issue 2, 2007 Review first published: Issue 4, 2009
| Date | Event | Description |
|---|---|---|
| 29 September 2015 | Amended | This review has been withdrawn. Please see Published notes section for explanation. |
| 16 June 2010 | Amended | In‐text links to appendices corrected. |
| 9 November 2009 | Amended | Tables moved to appendices in order to enhance readability. |
Acknowledgements
Dr Maya Tickell‐Painter, Dr Rachel Saunders, and Dr David Sinclair received support from the by the Effective Health Care Research Consortium. The Consortium and the editorial base of the Cochrane Infectious Diseases Group are funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The funding body had no role in study design, data collection and analysis, or preparation of the manuscript. The views expressed in this review do not necessarily reflect UK government policy.
Appendices
Appendix 1. List of study design features
| Feature | RCT | Q‐RCT | N‐RCT | PCS | RCS |
| Was there a comparison: | |||||
| Between two or more groups receiving the intervention? | Y | Y | Y | Y | Y |
| Within the same group of participants over time? | P | P | N | N | N |
| Were participants allocated to groups by: | |||||
| Concealed randomization? | Y | N | N | N | N |
| Quasi‐randomization? | N | Y | N | N | N |
| By other action of researchers? | N | N | Y | N | N |
| Time differences? | N | N | N | N | N |
| Location differences? | N | N | P | P | P |
| Treatment decisions? | N | N | N | P | P |
| Participants' preferences? | N | N | N | P | P |
| On the basis of outcome? | N | N | N | N | N |
| Which parts of the study were prospective: | |||||
| Identification of participants? | Y | Y | Y | Y | N |
| Assessment of baseline and allocation to intervention? | Y | Y | Y | Y | N |
| Assessment of outcomes? | Y | Y | Y | Y | P |
| Generation of hypotheses? | Y | Y | Y | Y | Y |
| On what variables was comparability between groups assessed: | |||||
| Potential confounders? | P | P | P | P | P |
| Baseline assessment of outcome variables? | P | P | P | P | P |
Footnotes
Y = Yes, N = No, P = Possibly
Abbreviations: RCT = randomized controlled trial; Q‐RCT = quasi‐randomized controlled trial; NRCT = non‐randomized controlled trial; PCS = prospective cohort study; RCS = retrospective cohort study
Adapted from Reeves 2011.
Appendix 2. Search strategies ‐ malaria chemoprophylaxis
| Search set | CIDG Specialized Register | CENTRAL | MEDLINE | Embase | LILACS |
| 1 | malaria | Malaria ti, ab, MeSH | Malaria ti, ab, MeSH | Malaria ti, ab, Emtree | malaria |
| 2 | Mefloquine OR Lariam | Antimalaria* ti, ab | Antimalaria* ti, ab | Antimalaria* ti, ab | Mefloquine OR Lariam |
| 3 | Prevent* OR prophyla* OR chemoprevent* OR chemoprophyla* | 1 or 2 | 1 or 2 | 1 or 2 | Prevent* OR prophyla* OR chemoprevent* OR chemoprophyla* |
| 4 | 1 and 2 and 3 | Mefloquine ti, ab, MeSH | Mefloquine ti, ab, MeSH | Mefloquine ti, ab, Emtree | 1 and 2 and 3 |
| 5 | — | Lariam ti, ab | Lariam ti, ab | Lariam ti, ab | — |
| 6 | — | 4 or 5 | 4 or 5 | 4 or 5 | — |
| 7 | — | Prevent* OR prophyla* OR chemoprevent* OR chemoprophyla* ti, ab | Prevent* OR prophyla* OR chemoprevent* OR chemoprophyla* ti, ab | Prevent* OR prophyla* OR chemoprevent* OR chemoprophyla* ti, ab | — |
| 8 | — | 6 and 7 | 6 and 7 | 6 and 7 | — |
Footnotes
Date of search: 22 June 2017.
Search terms for MEDLINE, Embase, and LILACS were used in combination with the search strategy for retrieving trials developed by the Cochrane Collaboration (Lefebvre 2011).
Appendix 3. Decision aid for inclusion of meta‐analyses in 'Summary of findings' tables
| Outcome reported | Study design | Population studied | Preference |
| Adverse effects | RCTs | Short term international travellers | 1 |
| Other populations | 2 | ||
| Cohort studies | Short term international travellers | 3 | |
| Other populations | 4 | ||
| Adverse events | RCTs | Short term international travellers | 5 |
| Other populations | 6 | ||
| Cohort studies | Short term international travellers | 7 | |
| Other populations | 8 |
Appendix 4. Mefloquine versus placebo: other outcomes and groups of symptoms
Groups of symptoms
RCTs
Potasman 2002 (an RCT) compared 'neuropsychiatric' outcomes between study arms, and did not show a difference (RR 2.28, 95%CI 0.70 to 7.41, 90 participants). The authors did not define what they included within 'neuropsychiatric' although they do note that it 'included sleep disturbances, strange dreams, and inability to concentrate'. Within the RCTs there was no difference in the number of participants experiencing 'any adverse event' (RR 1.04, 95% CI 0.85 to 1.27, 7 trials, 1040 participants).
Other outcomes
RCTs
Three RCTs reported other outcomes which could be used as proxy measures of psychological or neurological adverse effects. These are described in the table below.
| Study ID | Mefloquine participants | Drug comparator(s) (N) | Outcome(s) measured | Results reported |
| Davis 1996 | 46 | Placebo (49) |
|
Symbol digit modalities test and digit span backwards and forwards: no significant differences between groups ECG: "there was a statistically significant prolongation in the electrocardiographic QTc interval between the first and second assessments in the subjects who received mefloquine (P 0.007); a less pronounced and later trend was in the placebo group (P 0.03)." Hearing loss at 6k: reports no statistically significant differences between groups |
| Schlagenhauf 1997 | 23 (cross‐over) | Placebo (23, cross‐over) |
|
POMS: Reports no statistically significant differences between groups. ESQ: Reports no statistically significant differences between groups. NES: Reports no statistically significant differences between groups. Sleep assessment: "the means of participants taking the mefloquine loading dose (456 mm) and weekly dose (450 mm) were less than the corresponding means for those taking the placebo loading (491 mm) and weekly doses (484 mm) by 35 and 34 mm, respectively" ICA: Reports no statistically significant differences between groups. Body sway: "mefloquine users ha[d] a higher mean sway than placebo users but no differences were significant" |
| Vuurman 1996 | 22 | Placebo (20) |
|
Critical flicker/fusion frequency: Reports no statistically significant differences between groups. Critical instability tracking tests: Reports no statistically significant differences between groups. Body sway: Reports no statistically significant differences between groups. Tests of driving performance: "[mefloquine] significantly improved road tracking performance on Day 4" |
1Symbol digit modalities test: a test of information processing speed. 2Digit span backwards and forwards: Participants are presented a series of numbers (for example, 2, 7, 4 at a rate of one digit per second), and asked to repeat them in the same (digit span forwards) or reverse (digit span backwards) sequence. These are usually viewed as simple short‐term memory tasks. 3Profile of Mood States (POMS): a validated questionnaire designed to measure feelings in five domains: tension, depression, anger, fatigue, and vigor. Answers are graded ranging from 'not at all (0)' to 'extremely (4)'. The total mood disturbance (TMD) is a composite overall score which is calculated by adding the scores across the four categories of tension, anger, fatigue and depression and subtracting the score for vigour. The total ranges from 20 to 108. An increased TMD score indicates a deterioration of mood. 4Environmental Symptoms Questionnaire (ESQ): a standardized form containing 68 questions relating to all body systems. Responses consist of six graded answers ranging from 'not at all' to 'extreme'. 5Neurobehavioral evaluation system (NES): a series of computerized tests designed to provide quantitative neurobehavioral outcomes which measures performance, such as sustained attention (response latency), coding speed, and visuomotor accuracy. 6Instrument co‐ordination analyser (ICA): This is a tool used in the selection of trainee pilots, and measures multiple task abilities. It It simulates simplified cockpit tasks with controls for the altitude, direction, and speed. It is used to test for coordination, psychomotor function, spatial discrimination, fine coordination, and stress resistance. 7Critical flicker/fusion frequency: this tests measures the frequency at which a flickering light is perceived as a steady light source. Changes are thought to be indicative of alterations in central nervous system activation, or fatigue. 8Critical instability tracking tests: this test is used to measure the ability of the participant to control a displayed error signal using a joystick. It is a first‐order, compensatory tracking task.
Additional outcomes
Santos 1993 (RCT) reported only on adverse effects, which the study authors attributed to the drug regime used. They report 1 case of "nervosismo" (anxiety) and discomfort in a participant who took 500 mg of mefloquine every 4 weeks (31 participants in this study arm).
Additionally, Weiss 1995 reported on mean number of symptoms reported per participant. This includes all spontaneously reported symptoms, and included diarrhoea, stomach pains, nausea, fever and headache. No significant differences were found between the multivitamin (placebo) group and the mefloquine groups. Pearlman 1980 reported that "there was no clinical evidence of drug toxicity in the 990 study participants, nor were there significant changes in the measured biochemical parameters". However, they did not actively seek out adverse events, and did not describe how causality was assessed (Table 7). Davis 1996 reports on events occurring in the first week of the study (when both groups had received 1 placebo tablet) and the relative risk of those symptoms worsening over time, for symptoms including headache, lethargy, abdominal pain, diarrhoea, cough and nausea. Diarrhoea increased transiently with mefloquine compared to placebo, there was no difference in the other symptoms. Schlagenhauf 1997 was a cross‐over randomized controlled trial including 23 participants. They report one withdrawal due to dizziness, diarrhoea, and flu‐like symptoms and three volunteers spontaneously reported minor sleep‐related adverse events, including insomnia, unpleasant dreams, superficial sleep, and early awakening. These events all occurred in the mefloquine loading dose phase.
Petersen 2000 had important differences in the numbers of exposed/non‐exposed participants and was at high risk of bias. Sensitivity analysis removing this trial did not alter the overall results.
Appendix 5. Mefloquine versus doxycycline: other outcomes and groups of symptoms
Groups of symptoms
RCTs
Ohrt 1997 reported the overall number of adverse events, and Schlagenhauf 2003 reported the overall number of mild, moderate and severe events, and no differences were found between groups (2 RCTs, 429 participants). Both trials also grouped symptoms together by body system, Schlagenhauf 2003 found that mefloquine users were more likely to experience both moderate (RR 1.56, 95% CI 1.09 to 2.22; 306 participants) and severe (RR 8.00, 95% CI 1.01 to 63.19; 306 participants) 'neuropsychological' adverse effects. However, there was no difference between groups in the number of neuropsychological adverse events overall (RR 1.26, 95% CI 0.91 to 1.75; 2 trials; 429 participants).
Cohort studies
In cohort studies reporting grouped adverse effects, there was no difference between groups for the overall number of adverse effects (RR 0.93, 95% CI 0.74 to 1.17; 12 cohort studies, 13,576 participants). There was also no difference between groups in the only cohort study that reported adverse events (RR 1.39, 95% CI 1.17 to 1.65; 668 participants).
Mefloquine users were more likely to experience 'constitutional' adverse effects (RR 3.53, 95% CI 1.92 to 6.49; 1 study; 684 participants) and 'neuropsychologic' adverse effects (RR 5.48, 95% CI 2.49 to 12.05; 3 studies; 4568 participants). They were less likely to experience gastrointestinal (RR 0.33, 95% CI 0.19 to 0.58; 3 studies; 5190 participants), genitourinary (RR 0.05, 95% CI 0.01 to 0.19; 1 study; 684 participants) or skin and subcutaneous (RR 0.08, 95% CI 0.02 to 0.32; 2 studies; 1915 participants) effects.
Other outcomes
RCTs
Schlagenhauf 2003 reported the Profile of Moods States (POMS) and a quality of life questionnaire, and found no significant differences between groups. Weiss 1995 reported on the mean number of symptoms reported per participant, which included diarrhoea, stomach pains, nausea, fever and headache, but we were unable to reliably include these data.
Cohort studies
Jute 2007, Rack 2005 and Rieckmann 1993 were additional cohort studies including users of both mefloquine and atovaquone‐proguanil but did not present their data in a way that could be included in meta‐analyses.
Jute 2007 was a cross‐sectional cohort study which included 17 users of mefloquine and 16 users of doxycycline and reported that "no significant adverse effects were reported by any users of chemoprophylaxis". Rack 2005 included 167 mefloquine users and 16 users of doxycycline and reported that "side effects were reported by 80 (28.9%) of 276 travelers with malaria prophylaxis, which affected the journey in 27 (9.8%) cases. In users of mefloquine, the most common side effects were central nervous system problems, such as headache, dizziness, sleep disorders,and emotional lability (53 of 167 [31.7%]).These kinds of side effects occurred significantly more often with mefloquine than with other antimalarial drugs (31.7% vs 8.6%, p < .01). Of those patients on atovaquone/proguanil and doxycycline, gastrointestinal side effects were most frequent (15.1% and 25%, respectively). Dermatologic problems occurred significantly more often with doxycycline than with any other antimalarial drug (12.5% vs 1.5%, p < .01)." Rieckmann 1993 included 40 mefloquine users and 115 doxycycline users and reported that "mefloquine was well tolerated and no dizziness or neurotoxicity was observed, the incidence of gastrointestinal disturbance was 24.5%".
Mavrogordato 2012 included a categorical measure of adherence to the drug regime which we could not combine for meta‐analysis. The study included 12 mefloquine users and six doxycycline users.
Appendix 6. Mefloquine versus atovaquone‐proguanil: other outcomes and groups of symptoms
Groups of symptoms
RCTs
Of the RCTs, Overbosch 2001 reported an increase in any adverse effect (RR 1.40, 95% CI 1.18 to 1.66; 976 participants), and 'any moderate or severe adverse effect' with mefloquine (RR 1.84, 95% CI 1.34 to 2.53; 976 participants). Schlagenhauf 2003 reported the overall number of mild, moderate and severe events, and no differences were found between groups. Schlagenhauf 2003 also grouped symptoms together by body system: 'gastrointestinal', 'neuropsychological', 'skin and subcutaneous' and 'skin and vaginal'. The only statistically significant finding was an increase in moderate 'neuropsychological' symptoms with mefloquine (RR 1.88, 95% CI 1.29 to 2.73; 317 participants).
Cohort studies
Of the cohort studies, mefloquine users were more likely to experience 'cardiovascular' adverse effects (RR 7.32, 95% CI 1.06 to 50.42; 1 cohort study, 316 participants), 'constitutional' adverse effects (RR 13.53, 95% CI 1.89 to 96.60; 1 cohort study, 477 participants), 'gastrointestinal' adverse effects (RR 1.99, 95% CI 1.09 to 3.60; 2 cohort studies, 793 participants) and 'neuropsychologic' adverse effects (RR 8.48, 95% CI 3.18 to 22.62; 3 cohort studies, 1021 participants). Overall participants who took mefloquine were more likely to experience any adverse effect (RR 2.40, 95% CI 1.84 to 3.13; 10 cohort studies; 5404 participants). Although there was moderate statistical heterogeneity among trials (I² statistic = 65%), the direction of the effect was consistent.
Other outcomes
RCTs
Two RCTs reported other outcomes which could be used as proxy measures of psychological adverse effects. These are described in the table below.
| Study ID | Mefloquine participants | Drug comparator(s) (n) | Outcome(s) measured | Results reported |
| Schlagenhauf 2003 | 153 | Atovaquone‐proguanil (164), doxycycline (153) |
|
POMS: Reports no statistically significant differences between groups. Quality of life questionnaire: Reports no statistically significant differences between groups |
| van Riemsdijk 2002 | 58 | Atovaquone‐proguanil (61) |
|
POMS: "Significant deterioration on the domains of depression, anger, fatigue, and vigor. The TMD increased by 7.52 points (95% confidence interval, 3.32 to 11.71 points)" NES: Both groups showed improvement between the first and second measurement. No differences were observed between groups |
1Profile of Mood States (POMS): a validated questionnaire designed to measure feelings in five domains: tension, depression, anger, fatigue, and vigor. Answers are graded ranging from 'not at all (0)' to 'extremely (4)'. The total mood disturbance (TMD) is a composite overall score which is calculated by adding the scores across the four categories of tension, anger, fatigue and depression and subtracting the score for vigour. The total ranges from 20 to 108. An increased TMD score indicates a deterioration of mood. 2Quality of life questionnaire: participants were asked to grade 13 positive statements (for example, 'I can enjoy my everyday life') on scale of 1 ('not at all true') to 6 ("true") 3Neurobehavioral evaluation system (NES): a series of computerized tests designed to provide quantitative neurobehavioral outcomes which measures performance, such as sustained attention (response latency), coding speed, and visuomotor accuracy.
Cohort studies
Schneider 2013 analysed a large UK General Practice research database for incident cases of 'neuropsychiatric' disorders including anxiety, stress‐related disorders or psychosis, depression, epilepsy or peripheral neuropathies during or after antimalarial drug use. There was no difference between mefloquine or atovaquone‐proguanil for incident cases of depression, epilepsy, neuropathy or 'anxiety or stress‐related disorders or psychosis' in 'current' or 'past' users. The authors did not present their data in a way which we could include within meta‐analysis.
Napoletano 2007 reports the number of 'neuropsychiatric' and 'gastrointestinal' adverse effects reported in each group. 'Neuropsychiatric' symptoms accounted for 44% of symptoms reported by mefloquine users, and 12% of symptoms reported by users of atovaquone‐proguanil. They report a higher incidence of both 'neuropsychiatric' and 'gastrointestinal' symptoms in mefloquine users (data not provided).
Jute 2007 and Rack 2005 were additional cohort studies including users of both mefloquine and atovaquone‐proguanil but did not present their data in a way which could be included within meta‐analysis.
Jute 2007 was a cross‐sectional cohort study which included 17 users of mefloquine and one user of atovaquone‐proguanil and reported that "no significant adverse effects were reported by any users of chemoprophylaxis". Rack 2005 included 167 mefloquine users and 86 users of atovaquone‐proguanil and reported that "side effects were reported by 80 (28.9%) of 276 travelers with malaria prophylaxis, which affected the journey in 27 (9.8%) cases. In users of mefloquine, the most common side effects were central nervous system problems, such as headache, dizziness, sleep disorders,and emotional lability (53 of 167 [31.7%]).These kinds of side effects occurred significantly more often with mefloquine than with other antimalarial drugs (31.7% vs 8.6%, p < .01). Of those patients on atovaquone/proguanil and doxycycline, gastrointestinal side effects were most frequent (15.1% and 25%, respectively). Dermatologic problems occurred significantly more often with doxycycline than with any other antimalarial drug (12.5% vs 1.5%, p < .01)".
Mavrogordato 2012 included a categorical measure of adherence to the drug regime which we could not combine within meta‐analysis. The study included 12 mefloquine users and 11 users of atovaquone‐proguanil.
Appendix 7. Mefloquine versus chloroquine: other outcomes and groups of symptoms
Groups of symptoms
Four RCTs and 12 cohort studies compared participants reporting any adverse symptom. The results are mixed with mefloquine users less likely to report any adverse event in the few small RCTs (RR 0.59, 95% CI 0.42 to 0.83; three RCTs trials; 641 participants), and more likely to report any adverse effect in the cohort studies (RR 1.43, 95% CI 1.19) to 1.73; 11 cohort studies, 63,286 participants).
Within cohort studies, mefloquine users were more likely to report 'gastrointestinal' symptoms (RR 2.88, 95% CI 1.09 to 7.57; 1 cohort study, 3822 participants), 'neuropsychologic' symptoms (RR 2.12, 95% CI 1.24 to 3.60; 2 cohort studies, 3965 participants), and 'skin and subcutaneous' symptoms (RR 1.27, 95% CI 1.08 to 1.50; 2 cohort studies, 53,550 participants).
Other outcomes
Boudreau 1993 also reported outcomes which could be used as proxy markers of psychological or neurological adverse effects, including the POMS (a validated questionnaire designed to measure feelings in five domains: tension, depression, anger, fatigue, and vigor), environmental symptoms questionnaire (ESQ) (a standardized form containing 68 questions relating to all body systems. Responses consist of six graded answers ranging from 'not at all' to 'extreme') and a sleep assessment. They reported as follows:
POMS: "On day 4, depression was significantly greater in the loading dose mefloquine group. At week 6, depression, tension and anger were significantly greater in the mefloquine group. No differences were found between groups for vigour, fatigue or confusion."
ESQ: "On day 4, significant differences were found for depression, dizziness, co‐ordination off for both mefloquine groups... eye irritability was more common in the chloroquine group... During week 6: depression, nausea, hands shaking higher in mefloquine weekly group and irritability higher in both [mefloquine] groups."
Sleep assessment: no group differences (in total sleep time) were statistically significant, however, both mefloquine groups slept less (about 20 minutes less per night).
Data and analyses
Comparison 1. Mefloquine versus placebo/non users.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinical cases of malaria | 9 | 1908 | Risk Ratio (M‐H, Random, 95% CI) | 0.09 [0.04, 0.19] |
| 2 Malaria; episodes of parasitaemia in semi‐immune populations | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Trials reporting number of participants with parasitaemia | 3 | 414 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.06, 0.55] |
| 2.2 Trials reporting number of episodes of parasitaemia | 2 | 510 | Risk Ratio (M‐H, Random, 95% CI) | 0.05 [0.00, 5.25] |
| 3 Serious adverse events or effects (all studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 RCTs (adverse events) | 6 | 1221 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.14, 3.53] |
| 3.2 Cohort studies (adverse effects) | 2 | 1167 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.39, 24.11] |
| 4 Discontinuations due to adverse effects (all studies) | 7 | 1130 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.55, 4.88] |
| 4.1 RCTs (adverse effects) | 7 | 1130 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.55, 4.88] |
| 5 Nausea (all studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 RCTs (adverse events) | 2 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.05, 1.73] |
| 5.2 Cohort studies (adverse events) | 3 | 1901 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [1.42, 2.43] |
| 6 Vomiting (all studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 RCTs (adverse events) | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.50, 1.19] |
| 6.2 Cohort studies (adverse events) | 2 | 1167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.45, 1.21] |
| 7 Abdominal pain (all studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 RCTs (adverse events) | 3 | 550 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.84, 1.40] |
| 7.2 Cohort studies (adverse events) | 2 | 1167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.66, 1.42] |
| 8 Diarrhoea (all studies) | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 RCTs (adverse events) | 4 | 589 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.32, 1.62] |
| 8.2 Cohort studies (adverse events) | 3 | 1901 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.93, 1.68] |
| 9 Headache (all studies) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 RCTs (adverse events) | 5 | 791 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.71, 0.99] |
| 9.2 Cohort studies (adverse events) | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.63, 4.26] |
| 10 Dizziness (all studies) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 RCTs (adverse events) | 3 | 452 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.90, 1.17] |
| 10.2 Cohort studies (adverse events) | 3 | 1901 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.80 [1.29, 2.49] |
| 11 Abnormal dreams (all studies) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Cohort studies (adverse events) | 2 | 931 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.15, 4.80] |
| 12 Insomnia (all studies) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Cohort studies (adverse events) | 2 | 931 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [1.06, 2.02] |
| 13 Anxiety (all studies) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Cohort studies (adverse events) | 2 | 931 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.67, 2.21] |
| 14 Depressed mood (all studies) | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 14.1 Cohort studies (adverse events) | 3 | 1901 | Risk Ratio (M‐H, Random, 95% CI) | 2.43 [0.65, 9.07] |
| 15 Abnormal thoughts and perceptions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 Cohort studies (adverse events) | 1 | 970 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.77 [0.79, 42.06] |
| 16 Pruritis (all studies) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 RCTs (adverse events) | 3 | 609 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.60, 1.24] |
| 16.2 Cohort studies (adverse events) | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.71 [1.58, 28.55] |
| 17 Visual impairment (all studies) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 RCTs (adverse events) | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.66, 1.46] |
| 17.2 Cohort studies (adverse events) | 1 | 970 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.27, 3.19] |
| 18 Vertigo (all studies) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 RCTs (adverse events) | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.78, 1.34] |
| 19 Other adverse events (RCTs) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Arthralgia | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.02, 5.48] |
| 19.2 Back pain | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 1.61] |
| 19.3 Blurred vision | 1 | 208 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.89] |
| 19.4 Cough | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.71, 1.14] |
| 19.5 Constipation | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.53, 1.11] |
| 19.6 Decreased appetite | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.95, 1.28] |
| 19.7 Falls | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.82, 1.43] |
| 19.8 Fatigue | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.14, 5.86] |
| 19.9 Gastritis | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.10, 10.98] |
| 19.10 Myalgia | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [0.36, 6.57] |
| 19.11 Rash | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.04, 2.30] |
| 19.12 Respiratory tract infection | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.63 [1.04, 6.61] |
| 19.13 Sore throat | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.04, 2.75] |
| 19.14 Unsteadiness | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.74, 1.52] |
| 19.15 Weakness | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.96, 1.17] |
| 20 Other adverse effects (cohort studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Agitation | 1 | 734 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.61, 1.82] |
| 20.2 Altered spatial perception | 1 | 970 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.4 [0.57, 153.97] |
| 20.3 Confusion | 1 | 734 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.25, 1.78] |
| 20.4 Loss of appetite | 1 | 970 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.54, 1.50] |
| 20.5 Mouth ulcers | 1 | 970 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.39, 2.56] |
| 20.6 Palpitations | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.06 [0.44, 147.68] |
| 20.7 Tingling | 1 | 970 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.59, 6.24] |
Comparison 2. Mefloquine versus doxycycline.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinical cases of malaria (RCTs) | 4 | 744 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.35, 5.19] |
| 2 Serious adverse events or effects (all studies) | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 RCTs (adverse events) | 3 | 682 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.01, 8.16] |
| 2.2 Cohort studies (adverse effects) | 3 | 3722 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [0.23, 10.24] |
| 3 Discontinuations due to adverse effects (all studies) | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 RCTs | 4 | 763 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.41, 2.87] |
| 3.2 Cohort studies | 10 | 10165 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.54, 1.55] |
| 4 Nausea (all studies) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Cohort studies (adverse effects) | 5 | 2683 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.30, 0.45] |
| 4.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.71 [0.75, 9.74] |
| 4.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.06, 2.43] |
| 5 Vomiting (all studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Cohort studies (adverse effects) | 4 | 5071 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.12, 0.27] |
| 5.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.19, 21.84] |
| 6 Abdominal pain (all studies) | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Cohort studies (adverse effects) | 4 | 2569 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.09, 1.07] |
| 6.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 1.65 [0.74, 3.70] |
| 6.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.83, 2.18] |
| 7 Diarrhoea (all studies) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Cohort studies (adverse effects) | 5 | 5104 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.11, 0.73] |
| 7.2 RCTs (adverse events) | 2 | 376 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.78, 1.29] |
| 7.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 3.58 [1.69, 7.59] |
| 8 Dyspepsia (all studies) | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Cohort studies (adverse effects) | 5 | 5104 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.09, 0.74] |
| 9 Headache (all studies) | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Cohort studies (adverse effects) | 5 | 3322 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.50, 2.92] |
| 9.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 2.31 [1.25, 4.27] |
| 9.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 2.45 [1.38, 4.34] |
| 10 Dizziness (all studies) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1 Cohort studies (adverse effects) | 5 | 2633 | Risk Ratio (M‐H, Random, 95% CI) | 3.49 [0.88, 13.75] |
| 10.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 3.05 [1.30, 7.16] |
| 10.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 2.40 [1.47, 3.90] |
| 10.4 Retrospective healthcare record analysis (adverse events) | 1 | 354959 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.62, 0.73] |
| 11 Abnormal dreams (all studies) | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Cohort studies (adverse effects) | 4 | 2588 | Risk Ratio (M‐H, Random, 95% CI) | 10.49 [3.79, 29.10] |
| 11.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.07, 15.89] |
| 11.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 4.33 [2.08, 9.00] |
| 12 Insomnia (all studies) | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Cohort studies (adverse effects) | 4 | 3212 | Risk Ratio (M‐H, Random, 95% CI) | 4.14 [1.19, 14.44] |
| 12.2 RCTs (adverse events) | 1 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 2.03 [0.65, 6.40] |
| 12.3 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Random, 95% CI) | 4.54 [2.09, 9.83] |
| 12.4 Retrospective healthcare record analysis (adverse events) | 1 | 354959 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.43, 0.49] |
| 13 Anxiety (all studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Cohort studies (adverse effects) | 3 | 2559 | Risk Ratio (M‐H, Fixed, 95% CI) | 18.04 [9.32, 34.93] |
| 13.2 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.74 [1.99, 38.40] |
| 13.3 Retrospective healthcare record analysis (adverse events) | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.47, 0.56] |
| 14 Depressed mood (all studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Cohort studies (adverse effects) | 2 | 2445 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.43 [5.21, 25.07] |
| 14.2 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.27 [1.82, 21.62] |
| 14.3 Retrospective healthcare record analysis (adverse events) | 2 | 376024 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.51, 0.60] |
| 15 Abnormal thoughts and perceptions | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 Cohort studies (adverse effects) | 2 | 2445 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.60 [0.92, 47.20] |
| 15.2 Retrospective healthcare record analyses (adverse events) | 2 | 376024 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.26, 0.66] |
| 16 Pruritis (all studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Cohort studies (adverse effects) | 2 | 1794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.30, 0.91] |
| 16.2 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.69 [0.93, 7.78] |
| 17 Photosensitivity (all studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Cohort studies (adverse effects) | 2 | 1875 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.05, 0.11] |
| 17.2 Cohort studies (adverse events) | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.49] |
| 18 Yeast infection (all studies) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Cohort studies (adverse effects) | 1 | 1761 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.06, 0.16] |
| 18.2 Cohort studies (adverse events) | 1 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.06, 0.63] |
| 19 Visual impairment (all studies) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Cohort studies (adverse effects) | 2 | 1875 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.37 [1.41, 3.99] |
| 20 Other adverse effects (cohort studies) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Alopecia | 2 | 1875 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.44 [1.96, 6.03] |
| 20.2 Asthenia | 1 | 1761 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.89, 3.76] |
| 20.3 Balance disorder | 1 | 1761 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.87 [1.48, 5.59] |
| 20.4 Decreased appetite | 1 | 734 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.42, 3.64] |
| 20.5 Fatigue | 2 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.03, 1.77] |
| 20.6 Hypoaesthesia | 2 | 2445 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.48 [3.01, 43.70] |
| 20.7 Malaise | 1 | 734 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.11, 0.71] |
| 20.8 Mouth ulcers | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.02, 11.42] |
| 20.9 Palpitations | 1 | 1761 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.76 [0.16, 48.91] |
| 20.10 Tinnitus | 1 | 684 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.20 [0.39, 133.30] |
| 21 Other adverse events (RCTs) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 Constipation | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.19, 21.84] |
| 21.2 Cough | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.28, 1.01] |
| 21.3 Decreased appetite | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.56 [1.24, 10.20] |
| 21.4 Malaise | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.88, 4.69] |
| 21.5 Palpitations | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.19, 21.84] |
| 21.6 Pyrexia | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.85 [1.09, 7.42] |
| 21.7 Sexual dysfunction | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.05 [0.33, 28.51] |
| 21.8 Somnolence | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.19, 21.84] |
| 22 Other adverse events (cohort studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 Adjustment disorder | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.40, 0.45] |
| 22.2 Confusion | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [0.24, 19.49] |
| 22.3 Convulsions | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.45, 0.75] |
| 22.4 Hallucinations | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.08, 0.45] |
| 22.5 Paranoia | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.10, 1.63] |
| 22.6 Palpitations | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 13.44 [1.73, 104.38] |
| 22.7 Panic attacks | 1 | 21065 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.16 [0.55, 31.49] |
| 22.8 PTSD | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.53, 0.64] |
| 22.9 Rash | 1 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.50, 2.94] |
| 22.10 Suicidal ideation | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.31, 0.47] |
| 22.11 Suicide | 2 | 376024 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.32, 4.56] |
| 22.12 Tinnitus | 1 | 354959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.61, 0.71] |
| 23 Adherence (cohort studies) | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 Adherence during travel | 13 | 15583 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [1.12, 1.18] |
| 23.2 Adherence in the post‐travel period | 4 | 840 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.95, 1.22] |
Comparison 3. Mefloquine versus atovaquone‐proguanil.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinical cases of malaria (RCTs) | 2 | 1293 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Serious adverse events or effects (all studies) | 3 | 3591 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.08, 23.22] |
| 2.1 Cohort studies | 3 | 3591 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.08, 23.22] |
| 3 Discontinuations due to adverse effects (all studies) | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 RCTs | 3 | 1438 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [1.53, 5.31] |
| 3.2 Cohort studies | 9 | 7785 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [1.83, 4.08] |
| 4 Nausea (all studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.72 [1.52, 4.86] |
| 4.2 Cohort studies (adverse effects) | 7 | 3509 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.50 [1.54, 4.06] |
| 5 Vomiting (all studies) | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.49, 3.50] |
| 5.2 Cohort studies (adverse effects) | 3 | 2180 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.08, 4.09] |
| 6 Abdominal pain (all studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.52, 1.56] |
| 6.2 Cohort studies (adverse effects) | 7 | 3509 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.38, 1.07] |
| 7 Diarrhoea (all studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.60, 1.47] |
| 7.2 Cohort studies (adverse effects) | 7 | 3509 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.53, 1.35] |
| 8 Mouth ulcers (all studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.70, 3.00] |
| 8.2 Cohort studies (adverse effects) | 2 | 783 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.04, 0.37] |
| 9 Headache (all studies) | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.99, 2.99] |
| 9.2 Cohort studies (adverse effects) | 8 | 4163 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.42 [1.71, 6.82] |
| 10 Dizziness (all studies) | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.99 [2.08, 7.64] |
| 10.2 Cohort studies (adverse effects) | 8 | 3986 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.83 [2.23, 6.58] |
| 10.3 Retrospective healthcare record analysis (adverse events) | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [1.04, 1.46] |
| 11 Abnormal dreams (all studies) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 2.04 [1.37, 3.04] |
| 11.2 Cohort studies (adverse effects) | 7 | 3848 | Risk Ratio (M‐H, Random, 95% CI) | 6.81 [1.65, 28.15] |
| 12 Insomnia (all studies) | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.42 [2.56, 7.64] |
| 12.2 Cohort studies (adverse effects) | 8 | 3986 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.29 [4.37, 12.16] |
| 12.3 Retrospective healthcare record analysis (adverse events) | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [1.06, 1.44] |
| 13 Anxiety (all studies) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.12 [1.82, 20.66] |
| 13.2 Cohort studies (adverse effects) | 4 | 2664 | Risk Ratio (M‐H, Fixed, 95% CI) | 10.10 [3.48, 29.32] |
| 13.3 Retrospective healthcare record analysis (adverse events) | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [1.28, 1.85] |
| 14 Depressed mood (all studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.78 [1.71, 19.61] |
| 14.2 Cohort studies (adverse effects) | 6 | 3624 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.02 [3.56, 18.07] |
| 14.3 Retrospective healthcare record analysis (adverse events) | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.93 [1.56, 2.38] |
| 15 Abnormal thoughts and perceptions (all studies) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 Cohort studies (adverse effects) | 3 | 2433 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.30, 7.42] |
| 15.2 Retrospective healthcare record analysis (adverse events) | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.69, 12.97] |
| 16 Pruritis (all studies) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.60, 2.70] |
| 16.2 Cohort studies (adverse effects) | 3 | 1824 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.07 [0.40, 10.68] |
| 17 Visual impairment (all studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 RCTs (adverse effects) | 1 | 976 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.88, 4.73] |
| 17.2 Cohort studies (adverse effects) | 2 | 1956 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.29, 4.72] |
| 18 Other adverse effects (cohort studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Allergic reaction | 1 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.04, 14.48] |
| 18.2 Alopecia | 1 | 1469 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.55 [0.30, 70.01] |
| 18.3 Asthenia | 2 | 1956 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.84 [0.26, 13.12] |
| 18.4 Balance disorder | 1 | 1469 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.86 [0.19, 44.19] |
| 18.5 Cough | 1 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.08, 2.92] |
| 18.6 Disturbance in attention | 3 | 1363 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.45 [1.84, 10.77] |
| 18.7 Dyspepsia | 2 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.17, 1.46] |
| 18.8 Fatigue | 2 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.62 [0.47, 45.56] |
| 18.9 Hypoaesthesia | 2 | 1946 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.45 [0.93, 21.26] |
| 18.10 Loss of appetite | 1 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.33, 1.43] |
| 18.11 Muscle pain | 1 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.57 [0.45, 127.80] |
| 18.12 Palpitations | 3 | 2180 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.34 [0.73, 15.26] |
| 18.13 Photosensitization | 2 | 718 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.10, 4.92] |
| 18.14 Pyrexia | 1 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.28 [0.24, 75.57] |
| 18.15 Rash | 2 | 711 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.15, 6.09] |
| 18.16 Restlessness | 1 | 487 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.24 [0.32, 84.52] |
| 18.17 Slight illness | 1 | 487 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.83 [0.36, 93.84] |
| 18.18 Somnolence | 1 | 487 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.21, 11.40] |
| 18.19 Tinnitus | 1 | 477 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.31 [0.13, 42.64] |
| 18.20 Circulatory disorders | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.38 [0.36, 114.01] |
| 19 Other adverse events (cohort studies) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Adjustment disorder | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.76 [1.54, 2.02] |
| 19.2 Confusion | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.04, 25.96] |
| 19.3 Convulsions | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.79, 2.30] |
| 19.4 Hallucinations | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.08, 0.79] |
| 19.5 Paranoia | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.76 [0.08, 36.72] |
| 19.6 PTSD | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.51 [1.93, 3.26] |
| 19.7 Suicidal ideation | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.03, 2.77] |
| 19.8 Suicide | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.06, 7.78] |
| 19.9 Tinnitus | 1 | 49419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.21, 1.68] |
| 20 Adherence (RCTs) | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 20.1 van Riemsdijk 2002 | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.02] |
| 20.2 Overbosch 2001; during travel | 1 | 966 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.95, 1.01] |
| 20.3 Overbosch 2001; post‐travel | 1 | 966 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.74, 0.85] |
| 21 Adherence (cohort studies) | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 21.1 During travel | 6 | 5577 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.86, 1.34] |
| 21.2 Post‐travel | 2 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.64, 1.23] |
3.1. Analysis.
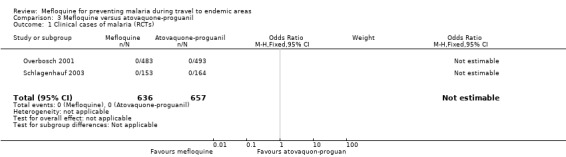
Comparison 3 Mefloquine versus atovaquone‐proguanil, Outcome 1 Clinical cases of malaria (RCTs).
Comparison 4. Mefloquine versus chloroquine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinical cases of malaria (RCTs) | 4 | 877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.28, 0.52] |
| 2 Serious adverse events or effects (all studies) | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 RCTs | 4 | 1000 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.77 [0.32, 23.85] |
| 2.2 Cohort studies | 6 | 79257 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.62, 2.07] |
| 3 Discontinuations due to adverse effects (all studies) | 11 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 RCTs | 3 | 815 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.61, 4.18] |
| 3.2 Cohort studies in short‐term travellers | 6 | 55397 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.78, 1.26] |
| 3.3 Cohort studies in longer term occupational travellers | 2 | 6085 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.97 [2.41, 3.66] |
| 4 Nausea (all studies) | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Cohort studies (adverse effects) | 6 | 58984 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.89, 1.68] |
| 4.2 RCTs (adverse events) | 1 | 359 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.57, 1.79] |
| 5 Vomiting (all studies) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Cohort studies (adverse effects) | 5 | 5577 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.78, 1.40] |
| 5.2 RCTs (adverse events) | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.36, 3.49] |
| 6 Abdominal pain (all studies) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Cohort studies (adverse effects) | 4 | 5440 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.22] |
| 6.2 RCTs (adverse events) | 2 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.37, 1.36] |
| 7 Diarrhoea (all studies) | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Cohort studies (adverse effects) | 5 | 5577 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.74, 0.95] |
| 7.2 RCTs (adverse events) | 3 | 772 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.46, 1.50] |
| 8 Headache (all studies) | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Cohort studies (adverse effects) | 6 | 56998 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.53, 1.34] |
| 8.2 RCTs (adverse events) | 3 | 772 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.61, 1.31] |
| 9 Dizziness (all studies) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Cohort studies (adverse effects) | 5 | 58847 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [1.34, 1.70] |
| 9.2 RCTs (adverse events) | 2 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.35, 1.46] |
| 10 Abnormal dreams (all studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Cohort studies (adverse effects) | 4 | 2845 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.10, 1.33] |
| 10.2 RCTs (adverse events) | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.70 [1.05, 6.95] |
| 11 Insomnia (all studies) | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Cohort studies (adverse effects) | 5 | 56952 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [0.73, 4.51] |
| 11.2 RCTs (adverse events) | 1 | 359 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.76, 1.84] |
| 12 Anxiety (all studies) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Cohort studies (adverse effects) | 3 | 3408 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.30 [4.37, 9.09] |
| 13 Depressed mood (all studies) | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Cohort studies (adverse effects) | 5 | 58855 | Risk Ratio (M‐H, Random, 95% CI) | 3.14 [1.15, 8.57] |
| 14 Abnormal thoughts and perceptions | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Cohort studies (adverse effects) | 4 | 4831 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.49 [2.65, 11.35] |
| 15 Pruritis (all studies) | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 15.1 Cohort studies (adverse effects) | 2 | 55544 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.92, 1.40] |
| 15.2 RCTs (adverse events) | 2 | 413 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.03, 2.93] |
| 16 Visual impairment (all studies) | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 16.1 Cohort studies (adverse effects) | 5 | 58847 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.50, 2.44] |
| 16.2 RCTs (adverse events) | 1 | 210 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.63] |
| 17 Vertigo (all studies) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Cohort studies (adverse effects) | 1 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.05, 23.43] |
| 18 Cohort studies in travellers; prespecified adverse effects | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 18.1 Vertigo | 1 | 746 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.05, 23.43] |
| 18.2 Nausea | 5 | 56847 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.94, 2.13] |
| 18.3 Vomiting | 4 | 3440 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.55, 1.42] |
| 18.4 Abdominal pain | 3 | 3303 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.74, 1.30] |
| 18.5 Diarrhoea | 4 | 3440 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.57, 2.64] |
| 18.6 Headache | 5 | 54861 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.48, 2.65] |
| 18.7 Dizziness | 4 | 56710 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.10, 2.10] |
| 18.8 Abnormal dreams | 3 | 708 | Risk Ratio (M‐H, Random, 95% CI) | 4.21 [0.57, 31.33] |
| 18.9 Insomnia | 4 | 54815 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.40, 6.10] |
| 18.10 Anxiety | 2 | 1271 | Risk Ratio (M‐H, Random, 95% CI) | 3.94 [0.53, 29.48] |
| 18.11 Depressed mood | 4 | 56710 | Risk Ratio (M‐H, Random, 95% CI) | 2.49 [0.75, 8.31] |
| 18.12 Abnormal thoughts or perceptions | 3 | 2694 | Risk Ratio (M‐H, Random, 95% CI) | 4.42 [1.58, 12.40] |
| 18.13 Pruritis | 1 | 53407 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.94, 1.48] |
| 18.14 Visual impairment | 4 | 56710 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.55, 0.79] |
| 19 Other adverse effects (cohort studies) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Altered spatial perception | 1 | 2032 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.16 [1.55, 6.45] |
| 19.2 Alopecia | 1 | 2137 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.27, 2.25] |
| 19.3 Asthenia | 3 | 3408 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [0.97, 2.40] |
| 19.4 Balance disorder | 1 | 2137 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.59 [2.15, 6.00] |
| 19.5 Confusion | 1 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.11, 36.31] |
| 19.6 Decreased appetite | 1 | 2032 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.87, 1.57] |
| 19.7 Fatigue | 1 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.37 [0.57, 9.80] |
| 19.8 Hypoaesthesia | 1 | 2137 | Risk Ratio (M‐H, Fixed, 95% CI) | 20.26 [1.23, 333.93] |
| 19.9 Irritability | 1 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.75 [0.28, 80.59] |
| 19.10 Mouth ulcers | 2 | 55439 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [1.01, 1.87] |
| 19.11 Paraesthesia | 2 | 2778 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.22 [1.27, 3.89] |
| 19.12 Palpitations | 3 | 3408 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.71 [0.91, 24.26] |
| 19.13 Photosensitization | 2 | 2662 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.52, 1.53] |
| 19.14 Restlessness | 1 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.74 [0.65, 34.46] |
| 19.15 Slight illness | 1 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.65 [0.64, 10.87] |
| 19.16 Somnolence | 1 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.08 [0.37, 100.36] |
| 19.17 Yeast infection | 1 | 2137 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.53, 2.49] |
| 20 Other adverse events (RCTs) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Abdominal distension | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.64, 15.27] |
| 20.2 Anger | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.07, 1.55] |
| 20.3 Disturbance in attention | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.16 [0.61, 16.47] |
| 20.4 Irritability | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.45, 2.64] |
| 20.5 Loss of appetite | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.35, 3.25] |
| 20.6 Malaise | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.85] |
| 20.7 Mood altered | 1 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.29, 4.34] |
| 21 Pregnancy related outcomes (RCTs) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 Spontaneous abortions | 1 | 2334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.36, 1.79] |
| 21.2 Still births | 1 | 2334 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.67, 1.52] |
| 21.3 Congenital malformations | 1 | 2334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Adherence (cohort studies) | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 22.1 Short‐term travellers | 3 | 852 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.90, 1.13] |
| 22.2 Short‐term travellers: after return | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.54, 1.87] |
| 22.3 Longer‐term occupational travellers | 2 | 5777 | Risk Ratio (M‐H, Random, 95% CI) | 2.02 [1.80, 2.26] |
4.17. Analysis.
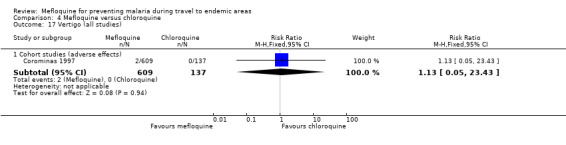
Comparison 4 Mefloquine versus chloroquine, Outcome 17 Vertigo (all studies).
Comparison 5. Mefloquine versus currently used regimens; by study design.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Nausea; effects | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 2.72 [1.52, 4.86] |
| 1.2 Cohort studies | 11 | 5973 | Risk Ratio (M‐H, Random, 95% CI) | 1.72 [0.78, 3.77] |
| 2 Abdominal pain; effects | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.52, 1.56] |
| 2.2 Cohort studies | 9 | 4494 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.27, 0.87] |
| 3 Diarrhoea; effects | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.60, 1.47] |
| 3.2 Cohort studies | 10 | 7648 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.28, 1.34] |
| 4 Headache; effects | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 1.72 [0.99, 2.99] |
| 4.2 Cohort studies | 9 | 5592 | Risk Ratio (M‐H, Random, 95% CI) | 2.19 [1.22, 3.93] |
| 5 Dizziness; effects | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 3.99 [2.08, 7.64] |
| 5.2 Cohort studies | 9 | 4606 | Risk Ratio (M‐H, Random, 95% CI) | 3.17 [1.58, 6.35] |
| 6 Abnormal dreams; effects | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 2.04 [1.37, 3.04] |
| 6.2 Cohort studies | 7 | 4543 | Risk Ratio (M‐H, Random, 95% CI) | 7.30 [2.51, 21.18] |
| 7 Insomnia; effects | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 4.42 [2.56, 7.64] |
| 7.2 Cohort studies | 9 | 5299 | Risk Ratio (M‐H, Random, 95% CI) | 5.70 [2.83, 11.47] |
| 8 Anxiety; effects | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 6.12 [1.82, 20.66] |
| 8.2 Cohort studies | 4 | 3390 | Risk Ratio (M‐H, Random, 95% CI) | 15.26 [8.66, 26.89] |
| 9 Depressed mood; effects | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 5.78 [1.71, 19.61] |
| 9.2 Cohort studies | 6 | 4236 | Risk Ratio (M‐H, Random, 95% CI) | 7.82 [3.79, 16.12] |
| 10 Abnormal thoughts or perceptions; effects | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1 Cohort studies | 3 | 3045 | Risk Ratio (M‐H, Random, 95% CI) | 4.20 [0.81, 21.87] |
| 11 Pruritis; effects | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.60, 2.70] |
| 11.2 Cohort studies | 3 | 2034 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.16, 4.76] |
| 12 Visual impairment; effects | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 RCTs | 1 | 976 | Risk Ratio (M‐H, Random, 95% CI) | 2.04 [0.88, 4.73] |
| 12.2 Cohort studies | 3 | 2560 | Risk Ratio (M‐H, Random, 95% CI) | 2.06 [1.05, 4.02] |
| 13 Adherence; during travel | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 RCTs | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.02] |
| 13.2 Cohort studies | 11 | 12131 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.03, 1.30] |
| 14 Adherence; after return | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 14.1 Cohort studies | 4 | 1221 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.92, 1.17] |
5.1. Analysis.
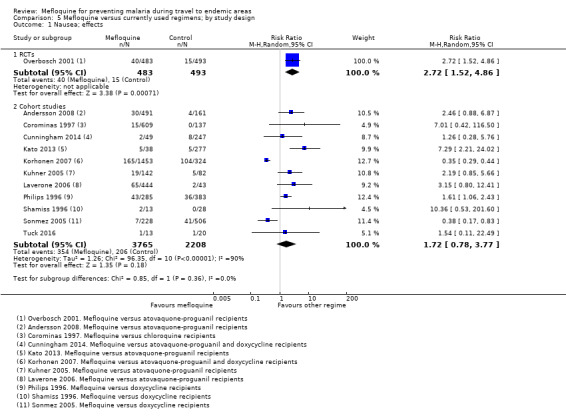
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 1 Nausea; effects.
5.2. Analysis.
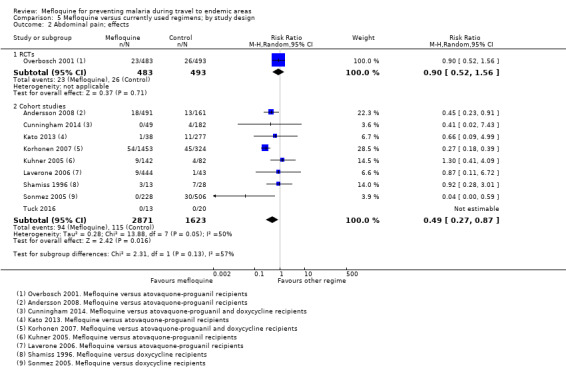
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 2 Abdominal pain; effects.
5.3. Analysis.
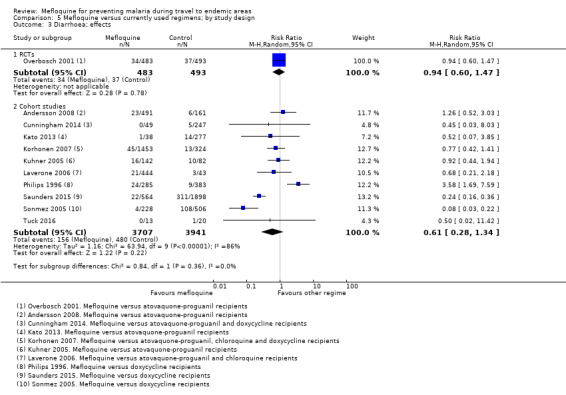
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 3 Diarrhoea; effects.
5.10. Analysis.
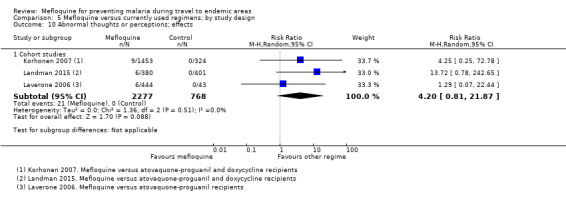
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 10 Abnormal thoughts or perceptions; effects.
5.11. Analysis.
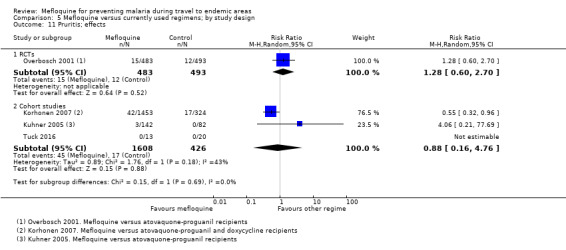
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 11 Pruritis; effects.
5.12. Analysis.
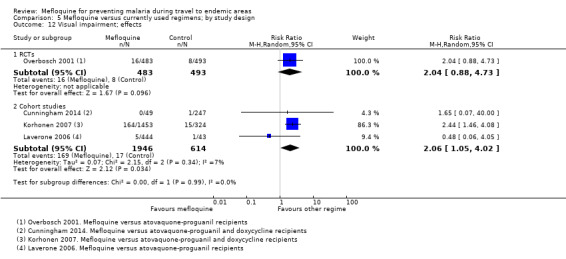
Comparison 5 Mefloquine versus currently used regimens; by study design, Outcome 12 Visual impairment; effects.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Albright 2002.
| Methods | Design: retrospective cohort study. Study dates: November 1997 to January 2000 Malaria transmission pattern and local antimalarial drug resistance: various destinations, not specified. Adverse event monitoring: one off telephone interview with parents whose children had previously been prescribed antimalarial prophylaxis. |
|
| Participants | Number enrolled: 177 fit inclusion criteria and interviewed, 190 contacted Inclusion criteria: children aged ≤ 13 years who visited the travel clinic at the Children’s Memorial Hospital in Chicago within the study dates. Subjects who were not on other medications. Exclusion criteria: "...data were only included if the child was living with the interviewed parent while taking the antimalarial". "Unwillingness to participate in the study and language barriers". Factors influencing drug allocation: "children... instructed to take mefloquine or chloroquine for malaria prophylaxis". Country of recruitment: USA. Country of malaria exposure: various; Africa 58%, Central or South America 21%, India 12% or Eastern Asia 9%. Duration of exposure to malaria: various, not specified. Type of participants: travellers |
|
| Interventions | 1. Mefloquine* 2. Chloroquine* *dosing regimen not specified |
|
| Outcomes | 1. Adverse effects; any, nausea, vomiting, diarrhoea, headache, insomnia, abnormal dreams 2. Serious adverse effects 3. Discontinuations of study drug due to adverse effects |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex and destination of travel were recorded, but were not reported across prophylactic regimens 2. Selection of participants into the study: low Non‐response rate 1.6% 3. Measurement of interventions: moderate The prescription was provided by a travel clinic, but participants were asked to recall if they discontinued their medication 2.8 to 28 months after visiting 4. Departures from intended interventions: serious Information was collected up to 2 years after taking the drug. No information was captured on switches. 5. Missing data: low All information was collected at one time point, there were no losses to follow‐up. 6. Measurement of outcomes: serious The outcome measure was subjective, participants and personnel were not blinded. 7. Selection of the reported results: low All outcomes included in the introduction were reported in the results 8. Other: low "The authors had no financial or other conflicts of interest to disclose" |
Andersson 2008.
| Methods | Design: prospective cohort study Study dates: March 2004 to November 2006 Malaria transmission pattern and local antimalarial drug resistance: malaria attack rate of 44% with P falciparum in another similar study at the time Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 690 soldiers sent questionnaire, 609 respondents Inclusion criteria: all Swedish soldiers deployed to Liberia within the study dates Exclusion criteria: none stated. Factors influencing drug allocation: "...mefloquine was prescribed to almost all soldiers in the first two contingents and to about two‐thirds in the last three contingents. The remaining soldiers were recommended atovaquone/ proguanil. The latter group consisted mainly of those with body weight < 70 kg and those who had already experienced adverse events with mefloquine. No other drug regimes were used". Country of recruitment: Sweden Country of malaria exposure: Liberia Duration of exposure to malaria: 6 months Type of participants: military |
|
| Interventions | 1. Mefloquine* 2. Atovaquone‐proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse events; any, nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams nightmares, insomnia sleep disturbance, depression 2. Serious adverse events; serious 3. Adverse events; other (concentration difficulties, mouth ulcers, fever, muscle pain) 4. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 5. Clinical cases of malaria 6. Overall satisfaction with the drug 7. Whether they would take the drug again 8. Measures of adherence to the drug regimen (data provided on aggregate) |
|
| Notes | Funding sources: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Information on potential confounders is not provided across prophylactic groups 2. Selection of participants into the study: moderate 609/690 (88%) response rate 3. Measurement of interventions: low All participants were issued with the study drug. 4. Departures from intended interventions: low Switches were recorded and reported 5. Missing data: serious Outcomes were reported from 3 of 5 cohorts. No information was provided for 2 remaining cohorts. 6. Measurement of outcomes: serious The outcome measure was subjective, participants and personnel were not blinded. 7. Selection of the reported results: low All outcomes prespecified in the introduction were reported. 8. Other: moderate Study sponsor not mentioned, but 2 study authors worked for GlaxoSmithKline |
Arthur 1990.
| Methods | Design: RCT Study dates: June to August 1988 Malaria transmission pattern and local drug resistance: local chloroquine resistance Adverse event monitoring: blood taken at induction and at days 57 and 70 of treatment. Interviews regarding side effects when sera taken. Stool sample at induction, at end of exercise and at any time participants sought medical care. |
|
| Participants | Number enrolled: 270 Inclusion criteria: soldiers (aged 18 to 40 years), awaiting deployment to Thailand Exclusion criteria: previous history of gastrointestinal illness Country of recruitment: USA Country of malaria exposure: Thailand Duration of exposure to malaria: 5 weeks Type of participants: soldiers, non‐immune |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet) once weekly, starting 1 week before travel and continuing throughout the period of deployment.* 2. Doxycycline (1 capsule containing doxycycline hyclate 100 mg) once daily, starting 1 week before travel and continuing throughout the period of deployment* Co‐interventions: Both groups given doxycycline 100mg daily for suppression of P falciparum and primaquine 45 mg weekly for elimination of liver hypnozoites for 6 weeks on return to the USA. *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Serious adverse event 3. Adverse events; diarrhoea 4. Discontinuation of study drug due to adverse effects 5. Measures of adherence to the drug regimen Outcomes assessed not included in the review: 6. Laboratory tests; enteric pathogens 7. Adverse events; nausea, vomiting, headache, dizziness (data provided on aggregate) |
|
| Notes | Funding sources: Pfizer Inc supplied active and placebo doxycycline; Hoffman‐La Roche Inc supplied active and placebo mefloquine | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Volunteers were assigned from a computer generated random number list to receive daily doxycycline or weekly mefloquine" |
| Allocation concealment (selection bias) | Unclear risk | Comment: Unclear how the tablets were labelled and whether allocation concealment occurred |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "Soldiers receiving mefloquine also received identical appearing doxycycline placebo capsules daily, and those receiving daily doxycycline received weekly mefloquine placebo tablets" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no explanation of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | High risk | "Of the 270 volunteers who were deployed, 253 were correctly taking the assigned study malaria prophylaxis on arrival in Korat" Comment: Reasons for not taking medication were not reported. Method of detection for malaria, frequency and duration of follow‐up were not reported |
| Incomplete outcome data (attrition bias); safety | Low risk | Comment: 17 participants (6%) were not "correctly taking the prophylaxis on arrival to Korat" and were excluded from the analysis. Data were not stratified by time point |
| Selective reporting (reporting bias); efficacy | Low risk | "None of the soldiers developed malaria" |
| Selective reporting (reporting bias); safety | Unclear risk | Comment: data for general side effects (e.g. headaches) were presented for the study population but not for each group |
| Other bias | Unclear risk | Comment: study sponsor not mentioned |
Belderok 2013.
| Methods | Design: prospective cohort study Study dates: October 2006 to October 2007 Malaria transmission pattern and local antimalarial drug resistance: various destinations, not specified Adverse event monitoring: not performed |
|
| Participants | Number enrolled: 945 Inclusion criteria: People aged ≥ 18 years were eligible if they were planning to travel for 1 to 13 weeks to one or more malaria‐endemic countries. Exclusion criteria: None stated Factors influencing drug allocation: "Dutch national guidelines for travelers’ health advice" Country of recruitment: Netherlands Regions of malaria exposure: various; Asia 48%, Africa 30% and Latin America 22% Duration of exposure to malaria: various; 49% ≤ 13 days, 35% 14 to 28 days and 9% ≥ 29 days Type of participants: travellers |
|
| Interventions | 1. Mefloquine: taken 3 weeks prior to arrival, during trip and for 4 weeks after return, dose and frequency of dose not specified 2. Atovaquone‐proguanil: 1 day prior to arrival, during trip and for 7 days after return, dose and frequency of dose not specified 3. Proguanil: On day of arrival, during trip and for 4 weeks after return, dose and frequency of dose not specified |
|
| Outcomes |
Included in the review: 1. Measures of adherence to the drug regime Outcomes assessed not included in the review: 2. Clinical cases of malaria 3. Predictors of adherence to malaria prophylaxis 4. Use of antimosquito preventive measures |
|
| Notes | Funding sources: The Amsterdam Academic Collaborative Center on Public Health is financially supported by the Netherlands Organization for Health Research and Development (ZonMw; grant number 7115 0001, http://www.zonmw.nl/nl/) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Length of stay, travel destination, age and sex were not reported across groups 2. Selection of participants into the study: moderate Non‐response rates were not reported 3. Measurement of interventions: low Participants made daily diary entries during travel 4. Departures from intended interventions: low Participants made daily diary entries during travel 5. Missing data: low Information was collected at one time point 6. Measurement of outcomes: moderate Outcome assessors were not blinded, methods were comparable across groups 7. Selection of the reported results: low Outcomes were reported for 610/620 participants 8. Other: low Government funding |
Boudreau 1991.
| Methods | Design: RCT Study dates: July 1983 to March 1984 Malaria transmission pattern and local antimalarial drug resistance: "in this area we believe the efficacy of chloroquine prophylaxis at the time of the study was negligible" Adverse event monitoring: "at each 2 week visit… history of symptoms over the previous fortnight was obtained. Patients were asked about fever, chills, headache, nausea, vomiting, diarrhoea, anorexia, rash, myalgia and dysuria or abnormally coloured urine". Laboratory studies were performed at baseline and at 6 weeks in participants who had not developed malaria |
|
| Participants | Number enrolled: 501 Inclusion criteria: "Only males 21 years of age or over were accepted" Exclusion criteria: "All participants were required to have a negative malaria smear (after examination of 200 fields on thick smear) on entry into the study". "...the use of other antimalarials or antibiotics" Country of recruitment: Cambodia Country of malaria exposure: Cambodia Duration of exposure to malaria: ongoing in semi immune population, 14 week study period Type of participants: Thai gem miners with a degree of immunity |
|
| Interventions |
Included in review comparisons: 1. Mefloquine (2 x 250 mg tablet) fortnightly for 14 weeks* 2. Chloroquine (1 x 300 mg tablet) weekly* Not included in review comparisons: 3. Fansidar (2 x 500 mg sufadoxine and 25 mg pyrimethamine) fortnightly and chloroquine (1 x 300 mg tablet) weekly* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Adverse events; other (myalgias, rash) Outcomes assessed not included in the review: 3. Laboratory tests; haematocrit, complete blood count, transaminase levels, total and direct bilirubin, alkaline phosphatase, blood urea nitrogen 4. Adverse events; headache, anorexia, fever, chills, nausea, diarrhoea or vomiting (data provided on aggregate) |
|
| Notes | Funding sources: Support for this study was from the USA Army Medical Research and Development Command | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Assignment… is a 4:3:2 ratio" Comment: method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details of allocation concealment were reported |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Unclear risk | "Every two weeks in a double blind fashion one of the investigators administered five tablets to each subject" Comment: not mentioned whether placebo tablets had an identical appearance |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no mention of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | "Only 194 patients completed the study until positivity or end of the 14 weeks observation period". "Therefore of the original 501 enrollees, 63 were discarded due to positivity at week 0 and 104 were discarded since they never returned beyond week 0". Comment: Losses to follow‐up during the study was not reported across groups |
| Incomplete outcome data (attrition bias); safety | Unclear risk | "Only 194 patients completed the study until positivity or end of the 14 weeks observation period...Any subject missing one appointment was excluded from the study though each subject's records up to the time of exclusion were entered into the survival analysis...After 3 weeks post treatment and a negative malaria smear some patients wishing to continue were reentered under a new study number and were assigned a double blind randomized treatment" |
| Selective reporting (reporting bias); efficacy | Unclear risk | Comment: number of people contracting malaria in each group and person‐weeks in the study were reported |
| Selective reporting (reporting bias); safety | Unclear risk | "There were no significant differences in frequency of complaints among the study groups for headache, anorexia, fever, chills, nausea, diarrhoea, or vomiting". Comment: Data for specific adverse events not reported. Methods section states participants were asked about dysuria and abnormally coloured urine, but this was not reported in the results |
| Other bias | Low risk | Support for this study was from the USA Army Medical Research and Development Command |
Boudreau 1993.
| Methods | Design: RCT Study dates: not mentioned Malaria transmission pattern and local antimalarial drug resistance: not applicable Adverse event monitoring: "At each visit, the subject answered two computerised questionnaires (the Environmental Symptoms Questionnaire and the Profile of Mood States) [and] a physician interview was performed" |
|
| Participants | Number enrolled: 359 Inclusion criteria: "males at least 18 years old, met military weight standards, were available for weekly administration of medications and monitoring during the 13 week study period, and were willing to give informed consent" Exclusion criteria: "treatment with beta‐blocking agents or other cardiotropic drugs, underlying chronic disease, history of cardiac arrhythmia, medical history of psychiatric or neurological problems within the last 5 years, anaemia or impaired hepatic or renal function. Women were excluded from participation in the study due to the risk of teratogenicity involved when the drug is used in early pregnancy" Country of recruitment: USA Country of malaria exposure: not applicable Duration of exposure to malaria: not applicable Type of participants: military, non‐travellers |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet), larium 228 mg base (F Hoffman La Roche) weekly for 11 weeks 2. Mefloquine (1 x 250 mg tablet), larium 228 mg base (F Hoffman La Roche) weekly for 11 weeks, with loading dose of 1 x 250 mg tablet daily for 3 days during the first week 3. Chloroquine (1 x 300 mg tablet), 300 mg base (F Hoffman La Roche) weekly for 11 weeks |
|
| Outcomes |
Included in the review: 1. Adverse events; nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams, insomnia 2. Adverse events; other (irritability, poor concentration, anger, moodiness, abdominal distension, anorexia, environmental symptoms questionnaire (ESQ), sleep assessment, Profile of Mood States questionnaire) Outcomes assessed not included in the review: 3. Laboratory tests: haemoglobin, haematocrit, platelets, white blood cell count, alanine aminotransferase, blood urea nitrogen and creatinine 4. Analysis of the dizziness index on the ESQ 5. Spontaneous comments on the ESQ (data provided on aggregate) |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...military personnel were assigned to drug groups in a ratio of approximately 3:3:1…stratification was performed by major subordinate command so that equal proportions of each study group would be represented in each MSC" Comment: not mentioned how the randomisation code was generated |
| Allocation concealment (selection bias) | Unclear risk | Comment: method allocation concealment not mentioned |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "...the ‘double dummy’ method of blinding was employed with either chloroquine or mefloquine placebos administered with active drug… In addition, during the first week of the study, on days two and three, a single mefloquine tablet or placebo was administered. Both drugs and placebos had an extremely bitter taste... identical placebo tablets" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no description provided of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | Unclear risk | Comment: 15 medical withdrawals are reported within the study. It is unclear whether these are the only losses to follow up which occurred, or whether they occurred in the mefloquine loading dose group or weekly administration group. |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | High risk | ‘table 5 outlines the percent of the group with symptoms only when significance was demonstrated’ ‘selected haematology and biochemistry tests were performed… no significant differences were noted among the three drugs when comparing the mean values’ Comment: data is not fully reported for ‘other symptoms’; only significant results are reported for the ESQ, and data for spontaneous comments on the ESQ are not reported; data is not fully reported for the POMS. |
| Other bias | Unclear risk | Comment: study sponsor not mentioned, but the lead author is attributed to ‘Pharmaceutical Systems Incorporated’ |
Bunnag 1992.
| Methods | Design: RCT Study dates: July 1987 to January 1988 Malaria transmission pattern and local antimalarial drug resistance: "a malaria endemic area". Reports chloroquine, sulfadoxine‐pyrimethamine and quinine resistance within Thailand at the time of the study. Adverse event monitoring: "volunteers asked about adverse events at each visit (weeks 4, 9, 14, 19, 24, 28)...starting week 14, volunteers reporting adverse events were interviewed by members of the hospital team; most of them were also seen by principal investigators" |
|
| Participants | Number enrolled: 605 randomized, 3 excluded because of baseline parasitaemia Inclusion criteria: "...healthy male volunteers, aged between 16 and 60, living in this area, were recruited" Exclusion criteria: "persons with a known history of allergy against sulphonamides, with an evidence illness of fever, or which a positive blood film (with or without symptomatic malaria) were excluded" Country of recruitment: Thailand Country of malaria exposure: Thailand Duration of exposure to malaria: trial duration 24 weeks Type of participants: Thai residents in a malaria‐endemic area (presumed semi‐immune) |
|
| Interventions |
Included in the review: 1. Mefloquine (1 tablet containing 125 mg mefloquine) once weekly, double dose during first 4 weeks* 2. Chloroquine (1 tablet containing 300 mg chloroquine) once weekly* 3. Placebo Not included in the review: 4. Fansifem (1 tablet containing 125 mg mefloquine, 250 mg sulfadoxine, 12.5 mg pyrimethamine) once weekly, double dose during first 2 weeks* 5. Fansidar (1 tablet containing 500 mg sulfadoxine, 25 mg pyrimethamine) once weekly* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Adverse events; any 3. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 4. Laboratory tests; haematocrit, white blood cell count and neutrophil count |
|
| Notes | Funding sources: "The project was jointly organized and conducted by the Malaria Division, Department of Communicable Disease, Ministry of Public Health; the Hoffman‐La Roche company, Basel, Switzerland; and The Faculty of Tropical Medicines, Mahidol University, Bangkok" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Eligible volunteers were randomly assigned to treatment groups" Comment: method of random sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | "The tablets were identical in appearance; they were packed in numbered blister packs and were in addition labelled weeks 1‐24... the coded test drugs for weeks 1‐4 were given to every subject" Comment: no mention of concealed opaque envelopes or central allocation |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "A randomised double blind trial…the tablets were identical in appearance; they were packed in numbered blister packs" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no explanation provided of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | "Of the 605 subjects originally randomised, 3 were excluded because of baseline parasitaemia... Although some of the volunteers left the study for personal reasons (moving away from the area)" Comment: numbers lost to follow up have not been reported |
| Incomplete outcome data (attrition bias); safety | Unclear risk | "94% (116/123) in the mefloquine group and 98% (119/121) in the placebo group were included for adverse event reporting" "Although some of the volunteers left the study for personal reasons (moving away from the area)" Comment: numbers lost to follow‐up were not reported |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: Malaria cases were fully reported |
| Selective reporting (reporting bias); safety | High risk | Comment: Data were collected but not reported for adherence to drug regimen. Data were provided on aggregate across all time points. The number of adverse events were reported but not types or severity |
| Other bias | High risk | "The project was jointly organized and conducted by the Malaria Division, Department of Communicable Disease, Ministry of Public Health; the Hoffman‐La Roche company, Basel, Switzerland; and The Faculty of Tropical Medicines, Mahidol University, Bangkok" |
Corominas 1997.
| Methods | Design: retrospective cohort study Study dates: June 1992 to July 1994 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 1511 questionnaires distributed, 1054 respondents Inclusion criteria: travellers who visited areas with a risk of malaria infection who were travelling on short trips < 6 weeks duration Exclusion criteria: none mentioned Factors influencing drug allocation: The fact of participating in this study did not change at all the typical prophylaxis when performing, which followed the usual criteria (Google Translate = "El hecho de participar en este estudio no cambio en absoluto el tipico de profilaxis al realizar, que siguio los criterios habituales" Country of recruitment: Spain Country of malaria exposure: various, not specified Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine (1 x 250 mg tablet) weekly, starting 1 week prior to travel, during the trip and 4 weeks following return from the malaria‐endemic area 2. Chloroquine (5 mg/kg) weekly, starting 1 week prior to travel, during the trip and 4 weeks following return from the malaria‐endemic area Outcomes assessed not included in the review: 3. Chloroquine and proguanil (chloroquine base 5 mg/kg, once weekly plus proguanil 100 mg daily, if weight < 55 kg and 200 mg daily if weight > 55 kg) starting 1 week prior to travel, during the trip and 4 weeks following return from the malaria‐endemic area |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, vertigo, visual impairment, nausea, vomiting, abdominal pain, diarrhoea, insomnia, anxiety, depression, pruritis 2. Adverse effects; other (irritability) 3. Discontinuations of study drugs due to adverse effects Outcomes assessed not included in the review: 4. Mean number of symptoms reported per traveller 5. Adverse effects; other, incidence < 1% (amnesia, tremor, paraesthesia, seizures, hyper‐reflexia, drowsiness, asthenia, nervousness, difficulty concentrating, mouth ulcers, acne, cardiac rhythm disturbance) |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Sex was reported across groups. No other confounders were reported 2. Selection of participants into the study: serious 1054/1511 (70%) response rate 3. Measurement of interventions: low The antimalarial prescription was provided by a travel clinic which also performed the study 4. Departures from intended interventions: moderate Discontinuations were reported across groups. It is unclear if information regarding switches was obtained 5. Missing data: low All participants were included in the analysis. All information was included at one time point 6. Measurement of outcomes: serious Comment: the outcome measure was subjective, participants and personnel were not blinded 7. Selection of the reported results: moderate The analysis of the relationship of symptoms by weight was reported only for mefloquine 8. Other: no information No information was provided regarding the study sponsor |
Cunningham 2014.
| Methods | Design: cross‐sectional cohort study Study dates: questionnaire emailed July 2012, reminder emails were circulated at 8 and 12 weeks Malaria transmission pattern and local antimalarial drug resistance: various destinations, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 579 questionnaires emailed, 327 responses Inclusion criteria: all Foreign and Commonwealth Office staff posted to a malaria‐endemic area Exclusion criteria: none stated Factors influencing drug allocation: "prophylaxis based on the Advisory Committee on Malaria Prevention in UK Travellers (ACMP) guidelines" Country of recruitment: various, not specified Country of malaria exposure: various, not specified Duration of exposure to malaria: 0 to 3 months N = 16 (4.9%), 4 to 6 months N = 26 (8.0%), 7 to 12 months N = 46 (14.1%), 13 to 36 months N = 75 (22.9%), > 36 months N = 167 (51.1%) Type of participants: UK Foreign and Commonwealth Office staff |
|
| Interventions | 1. Mefloquine* 2. Atovaquone‐proguanil* 3. Doxycycline* 4. Chloroquine* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; psychiatric disorders (abnormal dreams) 2. Adverse effects; other (skin sensitivity, indigestion, other psychological) Outcomes assessed not included in the review: 3. Clinical cases of malaria 4. Background knowledge of malaria 5. Attitudes regarding malaria prophylaxis 6. Use of personal protective measures 7. Impact of pregnancy on malaria prevention 8. Measures of adherence to drug regimen (data provided on aggregate) |
|
| Notes | Funding sources: not mentioned Communications with study authors: the study authors provided us with access to the full original data set. Thedata set differed from findings in the published version of the paper, and we were unable to determine the cause for differences. The included figures were from the full data set |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate No information on confounders was provided across prophylaxis groups 2. Selection of participants into the study: serious Response rate for the survey was 56.5% 3. Measurement of interventions: moderate Participants were asked to self‐report which medications they were prescribed. Compliance rate was 25% 4. Departures from intended interventions: serious No questions were included in the questionnaire regarding switches between chemoprophylactic regimens 5. Missing data: low All participants were included in the analysis 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: low The entire questionnaire was provided in full, all outcomes included were reported 8. Other: no information Study sponsor not mentioned |
Davis 1996.
| Methods | Design: RCT Study dates: not mentioned Malaria transmission pattern and local antimalarial drug resistance: not applicable Adverse event monitoring: daily self‐reported diary. Three medical check ups for laboratory and other tests |
|
| Participants | Number enrolled: 106 randomized, 95 completed all study procedures Inclusion criteria: "healthy adult staff and students at teaching hospitals in Perth, Western Australia" Exclusion criteria: "Those with a past history of psychiatric conditions, or neurological, cardiac, hepatic or renal disease were excluded, as were pregnant or breastfeeding females and those with a known allergy to, or taking medication known to interact with quinolone drugs. None of the subjects had taken mefloquine in the 3 months before the study" Country of recruitment: Australia Country of malaria exposure: not applicable Duration of follow up: 7 weeks Type of participants: non‐immune non‐travellers |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet), with placebo dose followed 1 week later by 250 mg mefloquine weekly, active treatment duration 4 weeks 2. Placebo, 1 tablet weekly, duration 5 weeks |
|
| Outcomes |
Included in the review: 1. Measure of adherence to the drug regimen 2. Adverse events: other outcome measures (symbol digit modalities test, digit span forwards and backwards test, ECG, hearing loss at 6kHz) Outcomes assessed not included in the review: 3. Laboratory tests: serum glucose, insulin, ionized calcium, phosphate, magnesium and albumin concentrations 4. Adverse events: headache, lethargy, abdominal pain, diarrhoea, cough, nausea; study reports events occurring in the first week (after both groups had received placebo) and the relative risk of symptoms worsening over time |
|
| Notes | Funding sources: "We thank… F. Hoffman La Roche & Co. for financial support" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...allocation… was by a random number code generated by independent Fremantle Hospital Pharmacy staff" |
| Allocation concealment (selection bias) | Low risk | "...who kept the code strictly confidential until the last volunteer had completed the protocol" |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "Tablets were prepared in individually numbered but otherwise unlabelled containers... identical placebo tablets…" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Allocation of active or placebo formulation was by a random number code generated by independent Freemantle hospital staff who kept the code strictly confidential" Comment: not mentioned whether outcomes assessors were blinded |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | Low risk | "Of 106 randomised volunteers, 95 (90%) completed all study procedures... eight subjects withdrew after initial assessment and three after the second. Follow‐up of these individuals revealed no toxicity in those allocated mefloquine" |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | High risk | Comment: not all symptoms were reported, only those occurring in > 10% of participants in both groups. Absolute numbers of participants experiencing each symptom after mefloquine/placebo commenced not provided, only relative risk of symptoms worsening over time |
| Other bias | High risk | "We thank… F. Hoffman La Roche & Co. for financial support" |
Eick‐Cost 2017.
| Methods | Design: Retrospective cohort study Study dates: 1 January 2008 to 30 June 2013 Malaria transmission pattern and local antimalarial drug resistance: Various, not specified Adverse event monitoring: Data collected retrospectively from the Defense Medical Surveillance System, the Pharmacy Data Transaction Service and the Theater Medical Data Store |
|
| Participants | Number enrolled: 367,840 Inclusion criteria: Active component service members who filled a prescription for mefloquine, doxycycline or atovaquone‐proguanil Exclusion criteria: Doxycycline and atovaquone‐proguanil prescriptions were excluded if the service member previously or concurrently received mefloquine. Doxycycline prescriptions were restricted to 100 mg, once daily, tabular form, minimum 30 day prescription Factors influencing drug allocation: Not specified Country of recruitment: USA Country of malaria exposure: Various, not specified Duration of exposure to malaria: Various, not specified Type of participants: Military |
|
| Interventions | 1. Mefloquine (250 mg weekly) 2. Atovaquone‐ proguanil* 3. Doxycycline (100 mg, tabular form, daily dose, 30 day minimum prescription) *dosing regimen not specified |
|
| Outcomes | 1. Adverse events (anxiety disorders, depressive disorders, psychoses, insomnia, vertigo) 2. Adverse events; other (adjustment disorders, post‐traumatic stress disorder, tinnitus, suicidal ideation, convulsions, hallucinations, paranoia, confusion) |
|
| Notes | Funding source: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Identified confounders were measured and not balanced across groups 2. Selection of participants into the study: low Start of intervention and start of follow‐up coincided for most participants. Retrospective medical records were used, therefore there were no non‐responders 3. Measurement of interventions: moderate Information regarding drug prescriptions were obtained from a medical database, without any verification that users took the prescription 4. Departures from intended interventions: serious Discontinuations and switches between prophylactic regimes were not recorded in the database 5. Missing data: low All records in the research database were included in the analysis 6. Measurement of outcomes: moderate Participants and outcome assessors (physicians) were not blinded. However, information was collected anonymously and on aggregate. Participants were unaware of their participation at the time of seeking healthcare 7. Selection of the reported results: low Outcome data were reported for all outcomes prespecified for analysis 8. Other: no information No information was available regarding the study sponsor. |
Goodyer 2011.
| Methods | Design: prospective cohort study Study dates: December 2004 to April 2006 Malaria transmission pattern and local antimalarial drug resistance: various destinations, not specified Adverse event monitoring: "a post travel questionnaire… approximately 1 week after they were due to complete their course of medication" |
|
| Participants | Number enrolled: 252 recruited, 185 completed pre‐ and post‐travel questionnaires Inclusion criteria: "...to be eligible, travelers had to be at least 18 years of age and to have been prescribed or supplied... an antimalarial medication as a result of planned travel for a duration of 28 days or less." Exclusion criteria: "travelers participating in other prospective clinical research or observational studies, pregnant travelers or travelers planning to get pregnant during the study were excluded" Factors influencing drug allocation: "Treatment choice was solely at the discretion of the traveler and practitioner" Country of recruitment: UK Country of malaria exposure: various, not reported Duration of exposure to malaria: various, median 14 days (interquartile range 9 to 20) Type of participants: travellers |
|
| Interventions | 1. Mefloquine* 2. Atovaquone‐proguanil* 3. Doxycycline* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Any adverse effects 2. Measures of adherence to the drug regimen Outcomes assessed not included in the review: 3. Relative importance of factors in choice of antimalarial drugs, for both healthcare professionals and travellers |
|
| Notes | Funding sources: "The study was commissioned and paid for by GlaxoSmithKline" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate "There were statistically significant differences in mean age" Several other confounders were not reported across groups 2. Selection of participants into the study: moderate No information is provided regarding people who did not wish to participate 3. Measurement of interventions: low The antimalarial prescription was provided by a travel clinic which also performed the study 4. Departures from intended interventions: moderate No information was captured regarding switches between interventions of interest 5. Missing data: serious 185/252 participants completed the pre‐ and post‐travel questionnaire. Interim loss to follow up 27% 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate The number of reported side effects was reported, but not the types or severity 8. Other: serious Funded by GlaxoSmithKline; the role of the study sponsor was not made clear |
Hale 2003.
| Methods | Design: RCT Study dates: not mentioned Malaria transmission pattern and local antimalarial drug resistance: "the 20‐week cumulative incidence of reinfection by P. falciparum to be nearly 100%". No mention of local drug resistance patterns Adverse event monitoring: "...during the prophylaxis and follow‐up phases, health workers visited the subjects 3 times weekly. Subjects with physical complaints were examined by a study physician the next day or on an emergent basis, as needed. Hematologic analysis was done on days 4 and 10 after starting the loading dose phase and during weeks 4, 8, 12, and 15. Biochemical analysis was done during weeks 4, 8, 12, and 15" |
|
| Participants | Number enrolled: 530 enrolled and completed radical cure regimen. 509 participants took at least 1 dose of the weekly study drug or placebo and comprised the full intention‐to‐treat data set Inclusion criteria: "Inclusion criteria included the following: age of 18–60 years (men) or 50–60 years (women); lack of significant systemic illness as determined by history, physical examination, and clinical laboratory test results (including negative results of a urine pregnancy test for women); and absence of seizures or other neuropsychiatric illness (past or present)" Exclusion criteria: "The high rate of pregnancy and breast‐feeding in women aged 18–49 years precluded their enrollment... G6PD deficiency accounted for 179 of 338 exclusions" Country of recruitment: Ghana Country of malaria exposure: Ghana Duration of exposure to malaria: trial duration 12 weeks Type of participants: Ghanain residents, semi‐immune |
|
| Interventions |
Included in the review: 1. Mefloquine (1 x 250 mg tablet, salt), weekly, with supervised 3 day loading dose* 2. Placebo, with supervised 3 day loading dose* Not included in the review: 3. Tafenoquine (1 x 25 mg tablet, base), weekly, with supervised 3 day loading dose* 4. Tafenoquine (1 x 50 mg tablet, base), weekly, with supervised 3 day loading dose* 5. Tafenoquine (1 x 100 mg tablet, base), weekly, with supervised 3 day loading dose* 6. Tafenoquine (1 x 200 mg tablet, base), weekly, with supervised 3 day loading dose* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1.Clinical cases of malaria 2. Adverse events; any, abdominal pain, diarrhoea, headache 3. Adverse events; other (gastritis, back pain, myalgia, polyarthralgia/arthralgia, respiratory tract infection, sore throat, rash) 4. Discontinuation of study drug due to adverse effects Outcomes assessed not included in the review: 5. Laboratory tests; haematological and biochemical analyses |
|
| Notes | Funding sources: USA Army Medical Materiel Development | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The randomization code was generated in blocks of 11 numbers" Comment: not mentioned how randomization code was produced |
| Allocation concealment (selection bias) | Unclear risk | "Code numbers were assigned according to the chronological order of appearance of the subjects at screening. Study drugs were prepackaged and prelabeled with a unique study number according to the randomization code" Comment: no mention of opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Unclear risk | "A ‘double‐dummy’ design allowed double‐blind administration of tafenoquine and mefloquine active drugs and their corresponding placebos" "A placebo (tafenoquine placebo, GlaxoSmith‐Kline; mefloquine placebo, Hoffmann‐La Roche) served as the negative comparator" Comment: does not report that the tablets were identical |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "All slides positive for the presence of malaria causing parasites, and an equal number of randomly selected slides with negative results were reevaluated by a second (blinded) microscopist." Comment: no other mention of outcome assessors being blinded and does not report that the researchers were blinded |
| Incomplete outcome data (attrition bias); efficacy | Low risk | "Data analysis for efficacy used 2 data sets: the 'full, intent‐to‐treat' data set (n=509), comprising all subjects who took at least 1 dose of the weekly study drug or placebo, and the 'per‐protocol' data set (n=428), comprising those subjects who strictly fulfilled the protocol criteria" |
| Incomplete outcome data (attrition bias); safety | Low risk | Comment: The safety and tolerability analyses included data for all participants who received at least 1 dose of the study drug or placebo (N = 513) |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: total number of participants with positive blood smear result at any time during prophylaxis was reported. Clinical cases of malaria were reported |
| Selective reporting (reporting bias); safety | High risk | "There were 9 serious adverse events in the study... No serious adverse events were considered by study physicians to be related to the study drug, and no deaths occurred" Comment: Data for serious adverse events were not attributed to the drug regimen. No information was provided on how causality was assessed |
| Other bias | High risk | Acknowledgement of "Philip Pickford and Rachel Moate (GlaxoSmithKline), for statistical and editorial advisement" |
Hill 2000.
| Methods | Design: retrospective cohort study Study dates: June 1989 to May 1991 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire. "Any reported illness was followed up by telephone interview about the nature of the illness, during which time more complete information was obtained using standardized questions" |
|
| Participants | Number enrolled: 869 participants enrolled, 822 completed follow‐up Inclusion criteria: all individuals attending the International Traveler’s Medical Service at the University of Connecticut Health Center and traveling for ≤ 90 days Exclusion criteria: none mentioned Factors influencing drug allocation: "prior to travel each person was given extensive counseling and written material on the prevention of malaria and traveler’s diarrhea. They were given prescriptions for prophylactic antimalarials" Country of recruitment: USA Country of malaria exposure: Various: Indian subcontinent 21%, central and east Africa 20%, South America 16%, Southeast Asia 14%, West Africa 10%, Central America and Mexico 10%, North Africa 65, East Asia 6%, Carribean 5%, Southern Africa 5%, Middle East 3% Duration of exposure to malaria: median 19 days (up to 90 days) Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Chloroquine* Not included in the review: 2. Chloroquine‐proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Any adverse effects 2. Discontinuations of study drug due to adverse effects 3. Measures of adherence to the drug regime Outcomes assessed not included in the review: 4. Clinical cases of malaria 5. Adverse events (provided for entire cohort, not by type of malaria prophylaxis) 6. Adverse effects; other (all gastrointestinal disorders, all nervous system disorders ‐ no comparative data provided) 7. Illness during and following travel |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex, destination and duration of travel were measured but not reported across groups 2. Selection of participants into the study: moderate Non‐response rate was not reported. 3. Measurement of interventions: low The antimalarial prescription was provided by a travel clinic which also performed the study 4. Departures from intended interventions: moderate Information was provided on discontinuations, but no information was captured on switches between interventions 5. Missing data: low Information on adverse effects was available for all participants who ever filled the prescription for the study drug (571/612, 93%) 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate It is unclear which questions were included in the questionnaire. Information was provided on aggregate 8. Other: no information No information provided on study sponsor |
Hoebe 1997.
| Methods | Design: retrospective cohort study Study dates: January to June 1995 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: one‐off telephone interview between 4 and 20 weeks post‐travell |
|
| Participants | Number enrolled: 454 eligible travellers, 300 successfully contacted and agreed to participate Inclusion criteria: subjects who visited the travel vaccination service of the regional public health institute in Maastricht if they had returned from their journey to tropical countries between 4 and 20 weeks previously. The group of non‐users was formed by people who travelled either to tropical countries without malaria risk or to cities in malarious areas, and by travellers who were prescribed an antimalarial drug but did not commence use Exclusion criteria: participants who had a serious adverse reaction to mefloquine in the first week Country of recruitment: Netherlands Region of malaria exposure: various; Asia, Africa, South America Duration of exposure to malaria: mean ˜3 weeks (range 1 to 9 weeks) Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine (1 x 250 mg tablet) weekly, taken 1 week prior to leaving, during travel and 4 weeks after departure 2. Non‐users of antimalarials Not included in the review: 3. Proguanil (1 x 100 mg tablet) twice daily, taken during travel and 4 weeks after departure |
|
| Outcomes | 1. Adverse events; any, nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams, insomnia, anxiety, depression, pruritis 2. Adverse events; other (palpitations, severity of symptoms, time point of symptoms in relation to drug taking) 3. Discontinuations of study drug due to adverse effects 4. Measure of adherence to the drug regimen |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Travel destination varies significantly between users of mefloquine and non‐users of prophylaxis (6.7% America mefloquine versus 29.0% non‐users) 2. Selection of participants into the study: low 13/454 (2.8%) of travellers successfully contacted refused to participate 3. Measurement of interventions: low Prescription was provided by a travel clinic which also performed the study, and discontinuations were reported 4. Departures from intended interventions: moderate No information regarding switches been interventions of interest was reported 5. Missing data: moderate "If somebody discontinued drug use within a certain period, symptoms that occurred in the following period were not counted" Comment: Mefloquine has a half life of 17 to 21 days 6. Measurement of outcomes: moderate "The participants were specifically asked about symptoms instead of adverse effects...To hide our focus on symptoms as adverse effects of the drugs, participants were informed that the aim of the study was to investigate symptoms during travelling. We structured the questionnaire so that the interviewers asked about symptoms first and drug use last, in order to blind them to the drug used when addressing symptoms" 7. Selection of the reported results: low All prespecified outcomes were reported. 8. Other: no information Funding source was not mentioned |
Jute 2007.
| Methods | Design: cross‐sectional cohort study Study dates: 2003 Malaria transmission pattern and local antimalarial drug resistance: during the dry season (considered a low risk malaria season). Local chloroquine/proguanil resistance Adverse event monitoring: Patient self‐reported questionnaire |
|
| Participants | Number enrolled: 90 questionnaires distributed, 68 responses Inclusion criteria: "all expatriate employees at the mine" Exclusion criteria: non mentioned Country of recruitment: Mali Country of malaria exposure: Mali Duration of exposure to malaria: various, not specified Type of participants: long‐term expatriates |
|
| Interventions |
Included in the review: 1. Mefloquine 2. Doxycycline 3. Atovaquone‐proguanil Not included in the review: 4. Chloroquine‐proguanil |
|
| Outcomes | 1. Adverse effects; any | |
| Notes | Study sponsor not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Sex was recorded but not reported across chemoprophylaxis groups. Duration of travel was not reported. Destination of travel was set by the study design. 2. Selection of participants into the study: serious 68/90 response rate (76%) 3. Measurement of interventions: no information It was unclear whether information on participants chemoprophylaxis was taken from medical records or patient self‐reporting 4. Departures from intended interventions: moderate No information regarding switches between interventions of interest were reported. Discontinuations were reported 5. Missing data: low All information was collected at one time point 6. Measurement of outcomes: serious The outcome measure was subjective. There was no mention of participants or outcome assessors being blinded. 7. Selection of the reported results: no information No information was provided regarding which topics were included within the questionnaire 8. Other: no information Funding source was not mentioned |
Kato 2013.
| Methods | Design: cross‐sectional cohort study Study dates: June 2009 to June 2011 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 1119 eligible travellers, 316 enrolled Inclusion criteria: "travelers who visited Hibiya Clinic, and requested antimalarial drugs for malaria chemoprophylaxis from June 2009 to June 2011" Exclusion criteria: none mentioned Factors influencing drug allocation: "The choice of anti‐malarial drug was supported by sufficient explanation about the advantages and disadvantages (efficacy, method, duration, side effect, cost and approval) of each drug" Country of recruitment: Japan Region of malaria exposure: various (n): East Africa 76, West Africa 63, South Africa 50, Southeast Asia 36, Central Africa 36, South Pacific 21, South America 16, India 8, North Africa 5, Central America 1 Duration of exposure to malaria: mean 20.0 ± 9.6 days in the atovaquone‐proguanil group and 59.0 ± 15.9 days in the mefloquine group Type of participants: travellers |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet, Mephaquin; Mepha) weekly, starting 1 week prior to arrival, during the stay, and continuing for 4 weeks after leaving the endemic area 2. Atovaquone‐proguanil (1 tablet containing 250 mg atovaquone and 100 mg proguanil, Malarone; GlaxoSmithKline) daily, starting 2 days prior to arrival, during the stay, and for 1 week after leaving the endemic area |
|
| Outcomes | 1. Adverse effects (any vertigo/dizziness, nausea, abdominal pain, diarrhoea, headache, insomnia, depression, any cardiovascular, any gastrointestinal, any psychoneurotic, allergic reaction) 2. Discontinuations of study drug due to adverse effects |
|
| Notes | Funding sources: not mentioned Communications with the study authors: the study authors provided us with disaggregated study data for the following outcomes: vertigo/dizziness, nausea, abdominal pain, diarrhoea, headache, insomnia, depression. Because we did not get receive the full disaggregated data set, we also retained this study in the analysis of groups of symptoms |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate PTravellers in the mefloquine group were significantly younger than travellers in the A/P group (p=0.01)" 2. Selection of participants into the study: serious "316 of 1119 travelers (28.2 %) were enrolled" 3. Measurement of interventions: low The prescription has been provided by travel clinic which also performed the study and discontinuations have been reported 4. Departures from intended interventions: moderate No information was available regarding switches between interventions of interest 5. Missing data: low One participant in the mefloquine group appears to be missing from the adverse events analysis. No reason was given 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: low Study authors provided us with disaggregated study data for individual outcomes 8. Other: serious "The authors wish to acknowledge that Makoto Ono and Tomoko Kawamura of GlaxoSmithKline are highly appreciated for conducting Data Management and Statistics Analysis of this study" |
Korhonen 2007.
| Methods | Design: prospective cohort study Study dates: 1 August 2005 to 31 July 2006. Malaria transmission pattern and local antimalarial drug resistance: various, chloroquine resistance specified by country of destination Adverse event monitoring: "Peace Corps medical staff in these countries were provided surveys for distribution during mandatory in‐country volunteer training sessions" |
|
| Participants | Number enrolled: 2701 (6216 Peace Corps volunteers during the time period) Inclusion criteria: "all Peace Corps countries with malaria risk" Exclusion criteria: none mentioned Factors influencing drug allocation: "Volunteers are provided chemoprophylaxis (either chloroquine, mefloquine, doxycycline, or atovaquone/proguanil)... medical officers can provide alternative chemoprophylaxis regimens for volunteers when adverse events or other factors require the cessation of any medication" Country of recruitment: various Country of malaria exposure: various Duration of exposure to malaria: "6 months or longer" Type of participants: Peace Corps volunteers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Chloroquine* 3. Doxycycline* 4. Atovaquone‐proguanil* *dosing regimen not specified |
|
| Outcomes | 1. Adverse effects; any (mild, moderate, severe, sought medical advice), nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams, insomnia, depression, anxiety, visual disturbance 2. Adverse effects; other (unsteadiness, hair loss, weakness, itchy skin, photosensitivity, yeast infection) 3. Serious adverse effects 4. Discontinuations of study drug due to adverse effects |
|
| Notes | Funding sources: "CK and PJ are employed by the Peace Corps, which has a significant number of volunteers taking anti‐malarial medications. There were no other financial disclosures" Communications with study authors: The study authors provided us with access to the disaggregated study data for the specific symptoms mentioned above. The questionnaire in the paper allowed participants to describe side effects from the antimalarial they were currently taking, and any regimen they had previously used. For non‐serious side effects, in line with the original paper, we only included side effects for the subject's original regimen. Where subjects had previously taken more than one regimen, we only include side effects for whichever regimen to which the participant attributed the greater number of side effects; this affected 70/2701 participants. This analysis resulted in a decrease in the effect size for side effects attributed to mefloquine. For serious side effects (hospitalizations) and discontinuations we included all participants entries for all regimens. In addition, our denominator differed from the original paper because we did not exclude participants who had been in post for fewer than six months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate "The questionnaire did not collect demographic information because of privacy concerns" Comment: destination has been reported, but not by type of antimalarial chemoprophylaxis. Duration was set by the study design 2. Selection of participants into the study: serious "A total of 2701 surveys were received yielding a response rate of 43%" 3. Measurement of interventions: moderate Participants were asked to self‐report which prophylaxis they were currently taking and had previously taken 4. Departures from intended interventions: moderate Switches between interventions of interest were reported. Approximately 1/3 of study participants had switched prophylactic regimens 5. Missing data: low We were able to include all participants in the study analysis because we had access to the original data set 6. Measurement of outcomes: serious "If respondents identified any adverse event, the survey instructed them to self‐report which drug they believed caused the adverse event" Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: low We were able to include all results in the analysis because we had access to the original data set 8. Other: low No evidence of pharmaceutical company funding |
Kuhner 2005.
| Methods | Design: prospective cohort study Study dates: 2000 to 2003 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: retrospective patient self‐reporting questionnaire |
|
| Participants | Number enrolled: 495 enrolled, 284 response rate Inclusion criteria: unclear. Users of the travel medicine department of the lower Saxony regional health office in Hanover, Germany Exclusion criteria: None mentioned Factors influencing drug allocation: "the prescriptions of medications followed individual consultation" Country of recruitment: Germany Country of malaria exposure: various, not specified Duration of exposure to drug: atovaquone‐proguanil mean 2.6 weeks, mefloquine mean 7 weeks Type of participants: short‐term travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Atovaquone‐proguanil* Not included in the review: 3. Chloroquine‐proguanil* 4. Chloroquine (not included in the study analysis) *dosing regimen not specified |
|
| Outcomes | 1. Adverse effects; any, nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams, insomnia, pruritis 2. Adverse effects; other (concentration difficulties, palpitations, circulation disorders, rash) 3. Discontinuations of study drug due to adverse effects |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Sex, age and duration of travel were reported but not balanced across groups 2. Selection of participants into the study: serious 284/495 (59.8%) response rate 3. Measurement of interventions: low The prescription was provided by a travel clinic which also performed the study; switches and discontinuations were recorded and reported. 4. Departures from intended interventions: moderate No information was provided regarding switches between prophylactic regimens 5. Missing data: low All information was collected at one time point 6. Measurement of outcomes: serious The outcome measure was subjective. There was no mention of outcome assessors being blinded 7. Selection of the reported results: moderate Insufficient information was provided regarding the questionnaire to know whether all outcomes were reported 8. Other: no information Study sponsor not mentioned |
Landman 2015.
| Methods | Design: prospective cohort study Study dates: 19 August to 30 September 2013 Malaria transmission pattern and local antimalarial drug resistance: various Adverse event monitoring: participant self‐reported questionnaire |
|
| Participants | Number enrolled: 3207 emails sent, 1184 unique, valid responses received Inclusion criteria: "(volunteers in) Peace Corps offices of all 23 countries with active posts in the Africa region to all active Volunteers in‐country" Exclusion criteria: Volunteers serving in Ethiopia, Kenya, Tanzania, Namibia, Botswana, South Africa Region of recruitment: African region except Ethiopia, Kenya, Tanzania, Namibia, Botswana, South Africa Factors influencing drug allocation: "all prophylaxis options (mefloquine, doxycycline, atovaquone‐proguanil) [are] equally available... They are instructed to individualize their choice of agent based on area‐specific recommendations, drug contraindications and precautions, drug tolerance, and dosing schedule" Country of malaria exposure: various: Togo (3.7%), Sierra Leone (6.3%), Uganda (7.8%), Liberia (5.6%), Malawi (2.0%), Cameroon (11.4%), Benin (10.2%), Burkina Faso (1.9%), Zambia (6.0%), Mozambique (4.5%), Ghana (10.8%), Rwanda (5.4%), Gambia (4.4%), Madagascar (11.1%), Swaziland (2.3%) Duration of exposure to malaria: various, not specified Type of participants: Peace Corps volunteers |
|
| Interventions | 1. Mefloquine* 2. Atovaquone‐proguanil* 3. Doxycycline* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, vertigo, headache, abnormal dreams, insomnia, anxiety, depression, psychosis 2. Adverse effects; other (any neuropsychiatric disorder, any gastrointestinal disorder, any skin or subcutaneous disorder, limb numbness, tinnitus, 'constitutional', genitourinary) 3. Measures of adherence to the drug regimen Outcomes assessed not included in the review: 4. Reasons for non‐adherence (not ascribed to prophylactic regimen, provided on aggregate), 5. Malaria knowledge 6. Health behaviours |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate The age, sex and BMI of included participants was not recorded. The destination and duration of travel was not reported by prophylactic regimen 2. Selection of participants into the study: serious 1184/3248 (36%) response rate 3. Measurement of interventions: moderate Travellers were asked to self‐report which prophylaxis they were taking at various time points during treatment 4. Departures from intended interventions: serious "Two hundred seventy‐six (35%) respondents reported having changed prophylaxis at some point during their service" Comment: this was not provided by prophylactic regimen 5. Missing data: low 703/781 (90%) participants reported data for adherence; 733/781 (94%) participants reported data for adverse events. Data were only included from the 2015 version of the publication 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: low All outcomes prespecified in the methods section were reported 8. Other: no information Study sponsor not mentioned |
Laver 2001.
| Methods | Design: cross‐sectional cohort study Study dates: February 2000 Malaria transmission pattern and local antimalarial drug resistance: "during February 2000, which was a peak period of malaria transmission in Zimbabwe" Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 660 Inclusion criteria: Passengers in Harare and Victoria Falls international airport during February 2000 Exclusion criteria: "Children under the age of 18 were excluded on the assumption that parents probably influence their health seeking behavior... Excluded, were travelers from the African continent and VIP travelers who exited through special departure lounges" Factors influencing drug allocation: no infromation provided Country of recruitment: Zimbabwe Country of malaria exposure: Zimbabwe Duration of exposure to malaria: various: 1 week or less, N = 317; 8 days to 2 weeks, N = 144; 15 days to 4 weeks, N = 90; > 4 weeks, N = 41 Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Doxycycline* 3. Chloroquine* Not included in the review: 4. Proguanil* 5. Dapsone and pyrimethamine* 6. Chloroquine and proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 2. Sources of pre‐travel health advice 3. Knowledge about malaria transmission 4. Knowledge about malaria prevention 5. Threat and risk perception |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Sex (P < 0.008), education (P < 0.022), previous episodes of malaria (P < 0.001) and access to pre‐travel advice (P < 0.001) were all significantly associated with reduced compliance at the significance value set by the study. None of these factors were adjusted for in the analysis 2. Selection of participants into the study: moderate "The nonresponse rate was about 10% (n = 65), with the main reason being the short transit time" 3. Measurement of interventions: low Participants were asked to self‐report which prophylactic regimen they were taking while they were still taking it 4. Departures from intended interventions: moderate No information was provided regarding switches between prophylactic regimens 5. Missing data: low Adherence information was not available for 4/595 participants 6. Measurement of outcomes: serious The outcome measure was based on participant self‐reporting; participants and personnel were not blinded. 7. Selection of the reported results: moderate There was insufficient information provided to know what questions were asked regarding adherence 8. Other: low "The authors had no financial or other conflicts of interest to disclose" |
Laverone 2006.
| Methods | Design: retrospective cohort study Study dates: 1 January 2003 to 31 December 2004 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: "An anonymous survey in a post‐travel situation" |
|
| Participants | Number enrolled: 1176 agreed to participate, 1237 approached Inclusion criteria: "travellers who had already completed their journey for which they had undergone immunization prophylaxis and who had returned to complete their vaccination schedule" Exclusion criteria: none mentioned Factors influencing drug allocation: "offered health advice following the World Health Organization guidelines for international travel" Country of recruitment: Italy Regions of malaria exposure: 97 countries: 39 states in Africa, 25 in Asia, 16 in North and Central America, 8 in South America, 6 in Europe and 3 in Oceania Duration of exposure to malaria: 1 to 7 days, 8.9%; 8 to 14 days, 30.1%; 15 to 21 days, 34.6%; 22 to 30 days, 16.8%; > 30 days, 8.9%; not available 0.7% Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Atovaquone‐proguanil* 3. Chloroquine* Not included in the review: 4.Chloroquine‐proguanil* 5. Proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, visual impairment (blurred vision), nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams (nightmares), insomnia, anxiety (anxiety disorder), depression, psychosis (hallucinations) 2. Adverse effects; other (slight illness, tiredness, restlessness, drowsiness, palpitations, weakness, photosensitization, mental confusion, rash) Outcomes assessed not included in the review: 3. Adverse effects; other, incidence < 1% (liver pain, aerophagy, rise in transaminase levels, gastrointestinal disturbance, epistaxis, fever) 4. Compliance with vaccinations 5. Side effects from vaccinations 6. Occurrence of health problems and unforeseen events during travel in the countries visited 7. Attention to avoiding potentially risky food and drink |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Demographic information was collected, but provided on aggregate for the entire cohort 2. Selection of participants into the study: low 1176 of 1237 (95.1%) response rate 3. Measurement of interventions: serious Participants were asked to self‐report which prophylactic regimen they had used, up to over 12 months since travelling 4. Departures from intended interventions: serious No switches were reported, and this information was not sought in the questionnaire 5. Missing data: low 642/646 (99%) participants were included in the analysis 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: low The questionnaire was provided in full, and all outcomes were reported 8. Other: no information No information was provided regarding the study sponsor |
Lobel 2001.
| Methods | Design: cross‐sectional cohort study Study dates: 13 July to 9 August 1997 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 6633 respondents, 5626 met inclusion criteria Inclusion criteria: "travelers departing Nairobi, or Mombasa, Kenya, from July 13 to August 9, 1997, on flights to Europe, including London, Paris, Frankfurt, Amsterdam, and Rome" Exclusion criteria: residents of African countries, individuals who had remained in Africa for more than 1 year, individuals who visited only non malarious areas, including Nairobi and Lesotho Factors influencing drug allocation: no information available Region of recruitment: Nairobi or Mombasa, Kenya Region of malaria exposure: Nairobi or Mombasa, Kenya Duration of exposure to malaria: < 5 weeks Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Doxycycline* 3. Chloroquine* Not included in the review: 4. Chloroquine‐proguanil* 5. Proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, 2. Serious adverse outcomes 3. Adverse effects; other (neuropsychologic, gastrointestinal, respiratory) 4. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 5. Pre‐travel medical advice 6. Compliance with antimosquito measures 7. Self‐treatment of presumed malaria |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate The number of travellers and country of origin was reported, but was not adjusted for in the analysis. Sex, age and duration of stay were reported on aggregate. 2. Selection of participants into the study: serious Response rate 6633/15,487 (43%) 3. Measurement of interventions: low Participants were asked to provide information regarding their prophylactic regimen during their flight home, while they should have still been using it 4. Departures from intended interventions: moderate No information was available regarding switches between alternative prophylactic regimens 5. Missing data: low 4934/4982 (99%) participants included in adverse event reporting 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate There was insufficient information provided regarding the questions included in the questionnaire. Symptoms were grouped together to report outcomes 8. Other: low "The authors had no financial or other conflicts of interest to disclose" |
Mavrogordato 2012.
| Methods | Design: retrospective cohort study Study dates: October to December 2005, with a 2 year follow‐up Malaria transmission pattern and local antimalarial drug resistance: "Malaria endemic area. Local chloroquine/proguanil resistance" Adverse event monitoring: Not clear |
|
| Participants | Number enrolled: 33 Inclusion criteria: not explicitly stated. Participants were travellers who took part in a scientific survey and rafting expedition in Ethiopia between October and December 2005 Exclusion criteria: none stated Country of recruitment: various, participants were from "a non‐malarious area, mainly the UK" Country of malaria exposure: Ethiopia Duration of exposure to malaria: 3 months Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine, dose not specified, during travel and 4 weeks after return 2. Atovaquone‐proguanil, dose not specified, during travel and for 1 week after return 3. Doxycycline, dose not specified, during travel and 4 weeks after return Not included in the review: 4. Chloroquine‐proguanil, dose not specified, during travel and 4 weeks after return |
|
| Outcomes |
Included in the review: 1. Measures of adherence to the drug regimen Outcomes assessed not included in the review: 2. Clinical cases of malaria 3. Adverse effects (information not provided by drug class) 4. Factors influencing choice of prophylaxis |
|
| Notes | Funding sources: Work was supported by the Biomedical Research Centre (Grant RG561620 to AMLL) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Demographic information is provided for the entire cohort 2. Selection of participants into the study: low No participants refused to participate in the study. Start of follow‐up began at the start of travel and not at the start of treatment, but this was judged to have a low impact on monitoring self‐reported adherence 3. Measurement of interventions: low Intervention status was determined by one of the participants on the expedition 4. Departures from intended interventions: low There are no documented switches between interventions of interest 5. Missing data: low Two people (6%) were lost to follow‐up in respect to data on efficacy. No participants were lost to follow‐up when monitoring adherence 6. Measurement of outcomes: serious Adherence was monitored by the medical officer on the trip, and reporting may have been influenced by social desirability bias 7. Selection of the reported results: low All prespecified outcomes have been reported 8. Other: low Government funding |
Meier 2004.
| Methods | Design: retrospective cohort study Study dates: 1 January 1990 and 31 December 1999 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: incident cases of depression, psychoses and panic attacks severe enough to require hospitalisation, referral to a specialist or specific pharmacological treatment within the UK general practice research database |
|
| Participants | Number enrolled: 35,370 Inclusion criteria: "men and women aged 17‐79 years who received between one and four prescriptions for mefloquine, proguanil and/or chloroquine, or subjects who received one prescription only for doxycycline... we included only those subjects who medical record contained a code indicating that the person received the drug for malaria prophylaxis within 1 week of the prescription date e.g. ‘travel advice’ or ‘prophylactic drug use’" Exclusion criteria: "participants who received the study drugs on a longer‐term basis...subjects had to be enrolled in the database for at least 12 months before the date of the first prescription for a study drug and had to have had some recorded activity (diagnoses or drug prescriptions) after the prescription(s) for an antimalarial drug... subjects with a history of alcoholism" Country of recruitment: UK Country of malaria exposure: various, not specified Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Doxycycline* Not included in the review: 3. Chloroquine‐proguanil* 4. Proguanil* 5. Chloroquine* (data reported combined with proguanil and chloroquine‐proguanil) *dosing regimen not specified |
|
| Outcomes | 1. Serious adverse events 2. Adverse events; psychiatric disorders (depression, psychosis) 3. Adverse events; other (panic attacks, suicide) |
|
| Notes | Funding sources: "This study was funded by an unconditional grant by F. Hoffmann‐La Roche Ltd, Basel, Switzerland" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Women and those aged 40 to 49 years were at higher risk of depression but this was not adjusted for in the analysis. Risk ratio estimates for psychoses and panic attacks could not be adjusted for because numbers were too small for the multivariate model. Data on destination and duration of travel were not available 2. Selection of participants into the study: low Recruitment onto the General Practice Research Database was unlikely to be related to exposure or outcome 3. Measurement of interventions: moderate "Antimalarial drugs can be used for malaria prophylaxis, for treatment of an acute malaria infection, or as a reserve drug… In order to distinguish these options, we included only those subjects whose medical records contained a code indicating ‘travel advice’ or ‘prophylactic drug use’" 4. Departures from intended interventions: serious Discontinuations and switches between prophylactic regimens were not recorded in this database 5. Missing data: low All participants in the research database were included in the analysis 6. Measurement of outcomes: moderate "...we reviewed all computer records of potential cases and included or excluded cases on the available clinical information, blinded to exposure status" Comment: general practitioners diagnosing patients would have been aware of their exposure status 7. Selection of the reported results: low Information on all outcomes prespecified in the methods section were reported for all participants. 8. Other: serious Funded by Roche pharmaceuticals |
Napoletano 2007.
| Methods | Design: retrospective cohort study Study dates: 1 October 2005 to 30 June 2006 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: telephone questionnaire to all travellers to tropical countries for whom antimalarial chemoprophylaxis was prescribed |
|
| Participants | Number enrolled: 1906 questionnaires returned Inclusion criteria: participants staying in high risk malarial areas, aged between 18 and 65 years, with no severe underlying disease (e.g. heart disease, diabetes) with an available phone number Exclusion criteria: immigrants (due to potential difficulty in linguistic communication) Country of recruitment: Italy Country of malaria exposure: various: Kenya, Tanzania/Zanzibar, India, Madagascar, Brazil, other countries of South America, South Africa, Senegal, Mali, Myanmar, Ghana, Congo, and others Duration of exposure to malaria: mean stay 2 weeks Type of participants: Travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Chloroquine* 3. Atovaquone + proguanil* 4. Doxycycline* Not included in the review: 5. Chloroquine + proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any 2. Serious adverse effects 3. Adverse effects; other (any gastrointestinal, any neuropsychiatric) 4. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 5. Clinical cases of malaria 6. Eating habits during travel |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Demographic information was provided on aggregate for the entire cohort 2. Selection of participants into the study: moderate Non‐response rates to the questionnaire were not reported 3. Measurement of interventions: moderate The prescription was provided by several travel clinics which also performed the study. However, it was unclear whether this information was used to determine intervention status or relied on participant self‐reporting 4. Departures from intended interventions: low Discontinuations were reported, with detailed reasons for discontinuations. No switches to alternative regimens were reported 5. Missing data: low All participants were included in the analysis 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: low The methods section makes clear which outcomes were being assessed; all outcomes were reported 8. Other: no information No information was provided regarding the study sponsor |
Nosten 1994.
| Methods | Design: RCT Study dates: January 1987 to November 1990 Malaria transmission pattern and local antimalarial drug resistance: "in an area of seasonal malaria transmission... mefloquine and quinine resistance is increasing in this area, and the proportion of recrudescent infections is rising" Adverse event monitoring: trial occurred over two phases. Phase 1: Weekly basic observations and simple symptom questionnaire. ECG, haematological and biochemical tests were done fortnightly. Children born to women in the trial were assessed at birth and at 3, 6, 12, and 24 months. Phase 2: weekly basic observations and expanded simple symptom questionnaire. ECG and blood tests were performed at baseline, at midstudy and at term. Each delivery was supervised. Additional assessments at 1 week and 2 and 9 months for children born to women in the trial |
|
| Participants | Number enrolled: 339 Inclusion criteria: "Women attending the weekly clinic were admitted to the study if they were at > 20 weeks of estimated gestation" Exclusion criteria: Not mentioned Region of recruitment: Thai‐Burmese border Region of malaria exposure: Thai‐Burmese border Duration of exposure to malaria: ongoing exposure in a semi‐immune population, monitored until delivery Type of participants: Pregnant Thai residents in malaria‐endemic area (presumed semi‐immune) |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet, Lariam; Hoffmann‐La Roche) weekly for 4 weeks, then 125 mg weekly until delivery, with 500 mg base loading dose in phase 1 but not phase 2 2. Placebo (1 tablet) weekly until delivery |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Episodes of parasitaemia 3. Serious adverse events (including childhood deaths) 4. Adverse events; vertigo, visual impairment (visual abnormalities), nausea, vomiting, abdominal pain, headache, dizziness, pruritis 5. Adverse events; other (weakness, anorexia, cough, falls, constipation, unsteadiness) 6. Discontinuation of study drug due to adverse effects 7. Adverse pregnancy outcomes (spontaneous abortions, still births, congenital malformations) Outcomes assessed not included in the review: 8. Laboratory tests; haematologic (full blood count, haematocrit) and biochemical (creatinine, blood urea, transaminases, alkaline phosphatase, albumin, globulin) 9. Outcomes related to pregnancy; weight gain during follow‐up, complications of labour, mean duration of labour, maternal anaemia 10. Fetal outcomes; mean birth weight, percent premature, fetal distress 11. Infant follow up; mean age at which children could crawl, sit, walk or talk, Romberg test |
|
| Notes | Funding sources: United Nations Development Programme/World Bank/World Health Organization Special Programme for Research and Training in Tropical Diseases; Wellcome Trust of Great Britain; Praevention Foundation. The Hague (to FLK) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...women were randomized to receive either mefloquine…or placebo" Comment: unclear what method of randomization was used |
| Allocation concealment (selection bias) | Unclear risk | "...the investigators were unaware of the randomisation" Comment: no mention of method used to conceal allocation |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "...double blind...women were randomised to receive either mefloquine…or identical placebo" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "...the investigators were unaware of the randomisation" |
| Incomplete outcome data (attrition bias); efficacy | Low risk | Comment: total number of participants with positive blood smear result at any time during prophylaxis was reported. Clinical cases of malaria were reported" |
| Incomplete outcome data (attrition bias); safety | High risk | "Ten women (8%) in phase I (3 mefloquine, 7 placebo) and 18 (8%) in phase II (9 in each group) dropped out of the study. The main reason was the discomfort of blood sampling (26 cases) and, in 1 case, pruritus attributed to mefloquine" Comment: 28 women dropped out but reasons were provided for only 27 women; numbers were not provided across groups |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: all episodes of parasitaemia and clinical cases of malaria were reported |
| Selective reporting (reporting bias); safety | High risk | Comment: Data on adverse effects were reported for only participants from phase 2 of the trial (220/339 women). Fifteen symptoms were listed in the comparative table, but the narrative states "twenty questions were asked". Romberg test results were not reported. Biochemical, haematological and ECG parameters were not reported other than "there were no differences" |
| Other bias | Low risk | Funding: United Nations Development Programme/World Bank/World Health Organization Special Programme for Research and Training in Tropical Diseases; Wellcome Trust of Great Britain; Praevention Foundation. The Hague (to FLK) |
Ohrt 1997.
| Methods | Design: RCT Duration of study: May to July 1994 Malaria transmission pattern and local drug resistance: "P. falciparum resistant to sulfadoxine‐pyrimethamine and both P falciparum and P vivax resistant to chloroquine" Adverse event monitoring: symptoms reported in the first week of the study, daily questioning about symptoms, exit questionnaire |
|
| Participants | Number enrolled: 204 Inclusion criteria: "All soldiers from military posts that were considered to have high malaria attack rates" Exclusion criteria: history of frequent travel, allergy to one of the study drugs, glucose‐6‐phosphate dehydrogenase deficiency, history of underlying illness Country of recruitment: Indonesia Country of malaria exposure: Indonesia Duration of exposure to malaria: Study duration was approximately 13 weeks Type of participants: military, semi‐immune (60% of participants had prior exposure to malaria) |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet, containing the equivalent of 228 mg mefloquine base) once weekly (after a loading dose of 250 mg per day for 3 days).* 2. Doxycycline hyclate (1 x 100 mg capsule) once daily* 3. Placebo* Co‐interventions: All soldiers were given doxycycline tablets for 4 to 6 weeks to enable clearance of sulfadoxine‐pyrimethamine from the blood before study prophylaxis began. All participants received radical treatment for pre‐existing malaria parasites in the blood and liver prior to beginning study prophylaxis. *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Adverse events; any, nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, insomnia, abnormal dreams 3. Serious adverse events 4. Adverse events; other (all gastrointestinal, all neurologic, constipation, anorexia, fever, malaise, skin related, cough, somnolence, palpitations, sexual dysfunction) 5. Discontinuation of study drug due to adverse effect Outcomes assessed not included in the review: 6. Exit questionnaire (incomplete data reported) |
|
| Notes | Funding source: Pfizer Indonesia supplied active and placebo doxycycline; F. Hoffman‐La Roche supplied active and placebo mefloquine, and gave financial support; USA Army Medical Research and Materiel Command gave financial support; USA Naval Medical Research and Development Command gave financial support | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Block randomization was used (block size, 15)" Comment: Used a randomization code, but it was not stated how it was generated |
| Allocation concealment (selection bias) | Unclear risk | "The randomization code was stored in individual envelopes in a locked box at the study site...Drugs were packaged into weekly ziplock plastic bags" Comment: Unclear whether the investigators or participants would foresee assignment. There was no mention of central allocation, sequentially numbered drug containers or sequentially numbers opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "Drugs were packaged into weekly zipper‐lock plastic bags: each bag contained a mefloquine or mefloquine placebo tablet and a blister pack of seven doxycycline or doxycycline placebo capsules (double‐dummy technique)" The placebo medication had an "identical appearance" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The randomisation code was stored in individual envelopes in a locked box at the study site. All investigators and study personnel did not have access to or know the randomisation code throughout the study" |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | "Sixteen of the 204 participants did not complete the study" Comment: It was unclear whether the duration of follow up included the post‐prophylaxis period to monitor for relapses |
| Incomplete outcome data (attrition bias); safety | High risk | Exit questionnaire: "Only data from persons who were still receiving the study drug at the time of the questionnaire were included" Comment: numbers not reported |
| Selective reporting (reporting bias); efficacy | Low risk | "The primary end point for efficacy was the first occurrence of malaria, as documented by a positive malaria smear" Comment: all cases of malaria were reported. |
| Selective reporting (reporting bias); safety | High risk | Comment: Not all data were reported from the exit questionnaire; the study reports "...the only statistically significant finding". Data on adverse symptoms were not reported for the placebo group |
| Other bias | Low risk | "Neither of the pharmaceutical companies that provided support played any role in the gathering, analysing or interpreting the data" |
Overbosch 2001.
| Methods | Design: RCT Duration of study: April to October 1999 Malaria transmission pattern and local drug resistance: not mentioned Adverse event monitoring: "evaluated 7, 28 and 60 days after return to obtain information about a targeted list of adverse events" |
|
| Participants | Number enrolled: 1013 Inclusion criteria: "travellers aged ≥ 3 years and weighing ≥ 11 kg with planned travel of ≤ 28 days to a malaria‐endemic area" Exclusion criteria: "poor general health; drug hypersensitivity (to atovaquone, chloroquine or proguanil); history of alcoholism, seizures or psychiatric or severe neurological disorders; generalized psoriasis; severe blood disorders; pregnancy/lactation; renal, hepatic or cardiac dysfunction; clinical malaria within previous 12 months; travel to malaria endemic area within previous 60 days" Countries of recruitment: Canada, Germany, Netherlands, South Africa, UK Regions of malaria exposure: various malaria‐endemic destinations (79% Africa, 6% South America) Mean duration of exposure to malaria: 2.5 weeks Type of participants: travellers, non‐immune |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet; or alternatively ¼, ½ or ¾ of a tablet, according to body weight) once weekly, starting 1 to 3 weeks before travel and continuing for 4 weeks after travel* 2. Atovaquone‐proguanil (1 combined tablet containing 250 mg atovaquone and 100 mg proguanil hydrochloride; or alternatively 1 to 3 combined tablets for children according to body weight, each tablet containing 62.5 mg atovaquone and 25 mg proguanil hydrochloride) once daily, starting 1 to 2 days before travel and continuing for 1 week after leaving the malaria‐endemic area* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria (antibody to blood‐stage malaria parasites) 2. Adverse events; any 3. Serious adverse events 4. Adverse effects; any (moderate or severe), visual impairment, nausea, vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams, insomnia, anxiety, depression, pruritis 5. Adverse effects; other (mouth ulcers) 6. Discontinuation of study drug due to adverse effects 7. Measures of adherence to the drug regimen Outcomes assessed not included in the review: 8. Laboratory tests; haematology (haemoglobin level, white blood cell count and platelet count) and chemistry (creatinine and alanine aminotransferase) |
|
| Notes | Funding source: GlaxoSmithKline "Subjects were enrolled in study MAL30010"‐ Enrollment criteria and study conduct were described in a separate publication (Høgh 2000) which refers to a different study population (atovaquone‐proguanil versus chloroquine‐proguanil). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated code was used to randomly assign a treatment number" (Høgh 2000) |
| Allocation concealment (selection bias) | Low risk | "Treatment codes were provided to investigators in opaque sealed envelopes, to be opened only if knowledge of study drug assignment was required for management of a medical emergency" (Høgh 2000) |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "For each active drug, capsules or film‐coated tablets were identical in appearance to the matching placebo" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "All subjects and study personnel remained blinded to treatment assignment with 5 exceptions. Two subjects in the atovaquone‐proguanil group and 3 in the mefloquine group lost their study drug during their return trip from a malaria‐endemic area, and the investigator broke the blind to enable completion of postexposure prophylaxis with active drug" |
| Incomplete outcome data (attrition bias); efficacy | Low risk | "A total of 963 subjects completed the 60‐day follow‐up period and had efficacy information recorded. A total of 915 subjects had paired serum samples available for serological testing" Comment: 963/976 (randomized and received first dose of study drug) = 98.7%. 915/976 = 93.75%. Reasons for leaving the study early were reported and numbers were balanced across groups |
| Incomplete outcome data (attrition bias); safety | Unclear risk | Comment: 96.35% of randomized participants were included in adverse event reporting. Reasons for leaving the study early were reported and numbers were balanced across groups |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: Full clinical details were provided for every episode in which an episode of malaria was considered (4 cases) |
| Selective reporting (reporting bias); safety | High risk | Comment: Data on adverse symptoms were not reported for the placebo group due to a shorter duration of follow‐up. Data were collected 7, 28 and 60 days after travel. However, data were only presented for 7 days after return |
| Other bias | High risk | Funding: GlaxoSmithKline It was not made clear whether the interpretation of the study findings was independent of the study sponsor |
Pearlman 1980.
| Methods | Design: RCT Study dates: unclear, during 1977 Malaria transmission pattern and local antimalarial drug resistance: "subjects were resident in an area highly endemic for P. vivax and chloroquine resistant P. falciparum" Adverse event monitoring: "a physician visited the study area each week and conducted a sick call for participating and nonparticipating villagers...Between physician visits, residents were taken to a nearby health centre for serious medical problems" |
|
| Participants | Number enrolled: 990 Inclusion criteria: "All eligible and consenting villagers over 10 years of age were included in the study" Exclusion criteria: "Female villagers of childbearing age (15‐44 years) were not considered for inclusion" Country of recruitment: The Bhu Phram Valley, Thailand Country of malaria exposure: The Bhu Phram Valley, Thailand Duration of exposure to malaria: study duration 26 weeks Type of participants: Thai residents, semi‐immune |
|
| Interventions | 1. Mefloquine (1 x 180 mg tablet, children 22 to 35 kg ½ dose) weekly 2. Mefloquine (1 x 360 mg tablet, children 22 to 35 kg ¼ dose) weekly 3. Mefloquine (1 x 360 mg tablet, children 22 to 35 kg ¼ dose) every 2 weeks 4. Placebo (1 x tablet) weekly Co‐interventions: "Those who had experienced falciparum parasitemias were given a therapeutic dose of sulfadoxine (1,500 mg)‐pyrimethamine (75 mg), and those with vivax or malariae parasitemias were treated with the standard regimen of chloroquine (1,500 mg over a 3‐day period), followed by primaquine, 15 mg daily for 14 days, for those study subjects known to be G‐6‐PD normal" |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Episodes of parasitaemia 3. Adverse events; any Outcomes assessed not included in the review: 4. Laboratory tests; haematocrit, white cell count, white cell differential, serum glutamic oxaloacetic transaminase, alkaline phosphatase and blood urea nitrogen |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Assignment to one of six treatment groups was made on a stratified random number basis" Comment: no details of how random numbers were generated |
| Allocation concealment (selection bias) | Unclear risk | "In the course of this visit, the technician opened a sealed, numbered envelope, gave the enclosed tablets, and observed the subject swallow them" Comment: no mention of the envelope being opaque |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "Each subject received two tablets each week (medication, placebo or a combination) in order to maintain the double blind nature of the study" "All tablets were identical in appearance" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but not clear how this was achieved |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | "Nine hundred and ninety nine subjects began the 25‐week field trial and 856 completed it (86.5%). 160/189 (85%) of the mefloquine 180 mg weekly group, 169/191 (88%) of the mefloquine 360 mg weekly, 158/184 (86%) of the mefloquine 360 mg fortnightly and 36/44 (82%) of the placebo group completed the trial" Comment: reasons for losses to follow‐up were not reported |
| Incomplete outcome data (attrition bias); safety | Low risk | "There was no clinical evidence of drug toxicity in the 990 study participants, nor were there significant changes in the biochemical parameters" |
| Selective reporting (reporting bias); efficacy | Low risk | "Table 2 shows the number of subjects in each group who completed the study, the number infected with P. falciparum, and the number of episodes of asexual parasitemia" |
| Selective reporting (reporting bias); safety | High risk | "There was no clinical evidence of drug toxicity in the 990 study participants" Comment: it was unclear whether all events that occurred during the 6 month trial period were included |
| Other bias | Unclear risk | Comment: study sponsor not reported |
Petersen 2000.
| Methods | Design: retrospective cohort study Study dates: 1 May 1996 to 30 April 1998 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 5446 questionnaires mailed, 4158 respondents Inclusion criteria: "travellers 18 years old or older, who were not pregnant and had no previous adverse reactions to any of the prescribed drugs" Exclusion criteria: none mentioned Factors influencing drug allocation: "the standard recommendations to Danish travelers were followed" Country of recruitment: Denmark Country of malaria exposure: various, not specified Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Chloroquine* Not included in the review: 3. Chloroquine + proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse events; any 2. Serious adverse outcomes 3. Adverse effects; visual impairment (blurred vision), nausea, vomiting, abdominal pain, diarrhoea, dizziness, depression 4. Adverse effects; other (loss of appetite, strange thoughts, tingling, altered spatial perception, mouth ulcers) Outcomes assessed not included in the review: 5. Discontinuation of study drug due to adverse effects (data reported on aggregate) 6. Measure of adherence to the drug regimen (data reported on aggregate) 7. Duration in days of symptoms |
|
| Notes | Funding sources: Not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate The questionnaire collected information regarding age, body weight and gender, destination and duration of travel but these were not reported 2. Selection of participants into the study: serious Response rate 4158/5446 (76.3%) 3. Measurement of interventions: low The prescription was provided by a travel clinic which also performed the study, and switches and discontinuations have been recorded and reported 4. Departures from intended interventions: moderate Discontinuations were reported. Although changes in prophylaxis were mentioned, it was unclear whether participants were analysed according to original or subsequent prophylactic grouping 5. Missing data: low 4020/4158 (97%) of participants are included in the analysis for adverse events 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded. It was unclear whether the questionnaire implied causality to the drug regimen 7. Selection of the reported results: moderate The questionnaire included demographic information, but this was not reported. All results were reported according to short‐term or long‐term users of prophylaxis, which was not specified in the methods section 8. Other: no information No information is provided regarding the study sponsor |
Philips 1996.
| Methods | Design: cross‐sectional cohort study Study dates: November 1993 to October 1994 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient questionnaire sent 2 weeks after travellers return |
|
| Participants | Number enrolled: 741 respondents, 918 questionnaires sent Inclusion criteria: "...travelers were asked to participate in the study when they attended TMVC clinics in Adelaide or Melbourne for pretravel consultation. If either doxycycline or mefloquine malaria chemoprophylaxis was recommended for part, or whole, of their itinerary, permission was sought to have them receive a mailed questionnaire" Exclusion criteria: "...under 18 years old, if doxycycline was recommended at doses other than 100mg daily, if other antimalarials were to be used during the intended journey, or if a traveller was not returning home in under 6 months" Factors influencing drug allocation: "Unless a contraindication existed for one or the other drug, the choice of which one to take was left to the traveler, the physician having already discussed, at some length, the different regimens, cost, and commonly reported adverse effects" Country of recruitment: Australia Region of malaria exposure: various (Southeast Asia, Africa, South Asia (India), Pacific) Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions | 1. Mefloquine* 2. Doxycycline* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse events; any, nausea/vomiting, abdominal pain, diarrhoea, headache, dizziness, abnormal dreams, insomnia, anxiety 2. Serious adverse events 3. Adverse events; other (mood change, palpitations, itching, rash, red skin, vaginal itch) 4. Adverse effects; any 5. Adverse effects; abdominal pain, diarrhoea 6. Discontinuation of study drug due to adverse effects 7. Measure of adherence to the drug regimen Outcomes assessed not included in the review 8. Reasons for choice of antimalarial drug regimen |
|
| Notes | Funding sources: "Thanks to Roche and Pfizer pharmaceutical companies for their financial support" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Identified confounders were measured and reported across groups. Mefloquine users were more likely to be female and had longer duration of treatment 2. Selection of participants into the study: serious Response rate 668 of 918 (73%) 3. Measurement of interventions: low The prescription was provided by a travel clinic which also performed the study; discontinuations were recorded and reported 4. Departures from intended interventions: moderate Discontinuations were recorded. It was unclear whether information regarding switches was recorded 5. Missing data: low All information was collected at one time point and all participants were included in the analysis 6. Measurement of outcomes: serious Comment: The outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: serious Information was reported for all adverse events recorded, but participants' assessment of causality to the study drug was only reported for two side effects 8. Other: serious "Sponsored by Roche and Pfizer pharmaceuticals" The role of the study sponsor was not made clear |
Potasman 2002.
| Methods | Design: RCT Study dates: unclear Malaria transmission pattern and local antimalarial drug resistance: not applicable Adverse event monitoring: "Two days after drug ingestion, a second EEG was performed, and a blood sample for mefloquine level was obtained...Travelers were given forms on which to record adverse effects that appeared within 48 hours after drug intake" |
|
| Participants | Number enrolled: 90 Inclusion criteria: not explicitly mentioned, included travellers from the Bnia Zion medical centre, Haifa, Israel Exclusion criteria: "Travelers younger than 18 years; with a history of epilepsy or depression, known allergy to mefloquine, cardiac conduction block; using beta‐blockers; or who were pregnant...Travelers with an abnormal baseline EEG (unifocal or repetitive bursts)" Country of recruitment: Israel Country of malaria exposure: not applicable Duration of follow up: 48 hours Type of participants: non‐travellers |
|
| Interventions | 1. Mefloquine (1 x Mephaquine 250 mg tablet, Mepha, Aesch, Switzerland) one dose 2. Mefloquine (1 x Larium 250 mg tablet, Roche, Basel, Switzerland) one dose 3. Placebo |
|
| Outcomes | 1. Adverse events; any 2. Adverse events; other (neuropsychiatric, abnormal EEG 48 hours after ingestion) |
|
| Notes | Funding sources: "Partially funded by Mepha Ltd, Aesch, Switzerland" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Eligible travelers were randomly assigned to one of three groups" "Randomization and statistical tests were carried out using Statmate and InStat" |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Unclear risk | "Participants were unaware of their group assignment until they completed their tests" Comment: methods used to blind participants not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "EEG pairs (pre‐ and post‐mefloquine) were examined separately by two senior neurologists who were unaware of group allocation" |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | Unclear risk | Comment: data were provided for all participants who were not excluded on the basis of abnormal baseline EEG |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | Unclear risk | "Adverse effects, mainly gastrointestinal and neuropsychiatric were noted in 26 travellers" Comment: specific nature of each adverse effect is not noted per group |
| Other bias | High risk | Partially funded by Mepha Ltd, Aesch, Switzerland. Comment: the role of the study sponsor was not clear |
Rack 2005.
| Methods | Design: retrospective cohort study Study dates: July 2003 to June 2004 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 794 Inclusion criteria: Travellers who were visiting five popular tropical regions or countries. Exclusion criteria: aged < 18 years, travelling for more than 2 months, and major acute or chronic diseases Country of recruitment: Germany Country of malaria exposure: Kenya/Tanzania, Senegal/Gambia, India/Nepal, Thailand, Brazil Duration of exposure to malaria: various, mean duration of travel 23.9 days Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Doxycycline* 3. Atovaquone‐proguanil* 4. Chloroquine* Not included in the review: 5. Chloroquine‐proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Narrative description of adverse effects Outcomes assessed not included in the review: 2. Risk behaviours during travel 3. Illness during travel 4. Seeking medical care owing to illness or accident 5. Accidents during travel |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Demographic information was provided for the entire cohort, not by prophylactic regimen 2. Selection of participants into the study: moderate Numbers of participants choosing not to participate in the study were not reported 3. Measurement of interventions: serious Participants were asked to self‐report which prophylaxis they took after return. The time after return was not specified 4. Departures from intended interventions: no information There was insufficient information provided to determine whether the questionnaire contained information regarding discontinuations or switches 5. Missing data: moderate Follow up was obtained for 658 (83%) travellers 6. Measurement of outcomes: serious There was insufficient information on the questionnaire about how adverse effects were sought and if outcome measures were objective. There was no mention of blinding of outcome assessors 7. Selection of the reported results: moderate There was insufficient information provided regarding the questionnaire to determine if all questions were reported. Side effects were grouped to report symptoms 8. Other: no information No information was provided regarding the study sponsor |
Rieckmann 1993.
| Methods | Design: cohort study Study dates: 1989 Malaria transmission pattern and local antimalarial drug resistance: higher levels of P falciparum than P vivax locally. Local chloroquine and primaquine resistance Adverse event monitoring: unclear |
|
| Participants | Number enrolled: 349 Inclusion criteria: Unclear Exclusion criteria: Unclear Country of recruitment: Australia Country of malaria exposure: Papua New Guinea Duration of exposure to malaria: 3 to 13 week training exercises Type of participants: Soldiers |
|
| Interventions |
Included in the review: 1. Mefloquine (1 x 250 mg weekly) 2. Doxycycline (1 x 100 mg tablet, daily, starting one day before deployment and continuing until 3 days after return) Not included in the review: 3. Doxycycline + primaquine 4. Doxycycline + chloroquine |
|
| Outcomes |
Included in the review: 1. Narrative description of adverse effects Outcomes assessed not included in the review:: 2. Clinical cases of malaria |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate No demographic information was provided 2. Selection of participants into the study: moderate Numbers of participants choosing not to participate in the study not reported 3. Measurement of interventions: low All participants were soldiers who were issued with medication 4. Departures from intended interventions: moderate No information was provided regarding discontinuations or switches 5. Missing data: moderate No losses to follow‐up or treatment withdrawals were reported, but the paper does not clearly state that none occurred 6. Measurement of outcomes: serious There was insufficient information on how adverse effects were sought and if outcome measures were objective. There was no mention of blinding outcome assessors 7. Selection of the reported results: moderate There was insufficient information provided regarding the questionnaire to determine if all questions were reported. Side effects were grouped to report symptoms. 8. Other: no information No information is provided regarding the study sponsor |
Rietz 2002.
| Methods | Design: cross‐sectional cohort study Study dates: June to December 2000 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 491 Inclusion criteria: "visitors over fifteen who were travelling to South or Central America, Africa, India or South‐East Asia, including China, and who were not suffering from any chronic illness" Exclusion criteria: none mentioned Factors influencing drug allocation: "After talking to the doctor, the doctor wrote whether malaria prophylaxis had been decided on and if so which kind" Country of recruitment: Sweden Region of malaria exposure: various, including South or Central America, Africa, India or Southeast Asia, including China Duration of exposure to malaria: "most were abroad between two to four weeks" Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Chloroquine* 3. Non‐users Not included in the review: 4. Chloroquine‐proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse events; any, seriously negative effect on the journey 2. Adverse effects; any 3. Adverse effects; other (neuropsychiatric, skin problems) Outcomes assessed not included in the review: 4. Importance attached to prophylaxis 5. Whether travellers had any anxiety about side effects prior to taking prophylaxis |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex, destination and duration of travel data were collected but not reported across groups. BMI was not measured 2. Selection of participants into the study: serious Response rate 62% 3. Measurement of interventions: low The prescription was provided by a travel clinic which also performed the study 4. Departures from intended interventions: moderate Discontinuations were reported, but not across groups. Switches were not recorded 5. Missing data: low All participants who completed both questionnaires were included in the analysis 6. Measurement of outcomes: moderate The outcome measure was subjective; participants and personnel were not blinded. Participants were asked to report all symptoms, and which they felt were due to prophylaxis 7. Selection of the reported results: moderate Symptoms were grouped to report outcomes 8. Other: low Source of funding not mentioned. "competing interests: none declared" |
Salako 1992.
| Methods | Design: RCT Study dates: July 1987 to June 1988 Malaria transmission pattern and local antimalarial drug resistance: "holoendemic for malaria... at the time of the trial, chloroquine resistance was not a problem" Adverse event monitoring: "study participants were seen weekly up to week 28". Interview with study personnel for events such as "fever, chills, malaise, nausea and vomiting, rashes and other symptoms and signs that could be regarded as adverse events" |
|
| Participants | Number enrolled: 567 Inclusion criteria: "...adult males aged 16 to 60 years, judged healthy on clinical grounds (no history of any illness and physical examination revealed no evidence of an acute or chronic illness). The patients were not on any drugs" Exclusion criteria: "...known hypersensitivity to sulphonamides, antimalarial drug treatment in the preceeding four weeks, presence of chronic debilitating disease and inability to attend regularly for follow up" Country of recruitment: Nigeria Country of malaria exposure: Nigeria Duration of exposure to malaria: study duration 24 weeks Type of participants: Nigerian residents, semi‐immune. |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet, Hoffman‐La Roche) weekly for 4 weeks followed by 1 x 125 mg tablet weekly for 20 weeks, total duration 24 weeks* 2. Chloroquine (1 x 300 mg base tablet, Hoffman‐La Roche) weekly, total duration 24 weeks* 3. Placebo, 1 tablet (Hoffman‐La Roche) weekly, total duration 24 weeks* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Episodes of parasitaemia 3. Adverse events; any, abdominal pain, diarrhoea, headache, dizziness, pruritis, visual impairment (blurred sight) 4. Serious adverse events 5. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 6. Laboratory tests; white blood cell counts, haematocrit, serum glutamic oxaloacetic transaminase and serum glutamic‐pyruvic transaminase 7. Adverse events: rash, muscle stiffness (occurred in < 1% of study participants) |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...subjects were allocated randomly into five groups on the basis of a pre‐determined randomisation list" Comment: no mention of how the list was generated |
| Allocation concealment (selection bias) | Unclear risk | "...blister packs containing a total of 24 tablets were provided for each subject ...The packs and tablets were identical in appearance and were labelled with the appropriate double‐blind number" Comment: no mention of opaque sealed envelopes or central allocation |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "The packs and tablets were identical in appearance" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no description provided of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | Low risk | Comment: numbers lost to follow up were provided across groups, with reasons provided. 107/113 (95%) mefloquine recipients, 103/115 (90%) chloroquine recipients and 101/114 (89%) placebo recipients completed the trial |
| Incomplete outcome data (attrition bias); safety | Low risk | Comment: reports "number of individuals suffering adverse events during the trial". Numbers lost to follow up were provided across groups, with reasons provided. 107/113 (95%) mefloquine recipients, 103/115 (90%) chloroquine recipients and 101/114 (89%) placebo recipients completed the trial |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: clinical cases of malaria and episodes of parasitaemia are reported for all participants |
| Selective reporting (reporting bias); safety | Unclear risk | "No change of clinical relevance occurred in any of the groups in the above laboratory tests" Comment: there was insufficient information available regarding the collection of adverse events to determine whether the reported list included all events or only a targeted list. Data not fully reported for blood tests |
| Other bias | Unclear risk | Comment: study sponsor not mentioned, but four of the authors are attributed to F Hoffman‐La Roche |
Santos 1993.
| Methods | Design: RCT Study dates: August 1982 to January 1983 Malaria transmission pattern and local antimalarial drug resistance: region considered hyperendemic. P falciparum resistant to chloroquine and “high prevalence of multiresistant Plasmodium falciparum transmission” Adverse event monitoring: during the initial screening visit, weekly visits, and a final visit at study end, participants were asked about illnesses, mainly about signs and symptoms compatible with malaria, and blood tests were done, including haematocrit and leucocyte count |
|
| Participants | Number enrolled: 122 Inclusion criteria: "volunteer soldiers and civilians aggregated to the 5th Battalion of Engineering and Construction in a community in Porto Velho" Exclusion criteria: aged < 12 years and > 55 years, pregnancy, people with debilitating disease, people who took antimalarial drugs in the previous four weeks and people with allergy to sulphonamides Country of recruitment: Brazil Country of malaria exposure: Brazil Duration of exposure to malaria: Mean duration within study (across groups) 16.9 weeks Type of participants: Brazilian soldiers and civilians, semi‐immune |
|
| Interventions |
Included in review comparisons: 1. Mefloquine (2 x 250 mg tablets, Roche) every 4 weeks* 2. Mefloquine (1 x 250 mg tablet, Roche) every 2 weeks* 3. Placebo Not included in review comparisons: 4. Fansidar* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Adverse effects; any, anxiety Outcomes assessed not included in the review: 3. Laboratory tests; haematocrit, white blood cell counts, serum glutamic oxaloacetic transaminase and serum glutamic‐pyruvic transaminase |
|
| Notes | Funding sources: Laboratory Roche provided mefloquine and “support” for conducting the study. Comando do 5o Batalhão de Engenharia e Construção, Porto Velho, RO, provided laboratory and field installations | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: described as a randomized controlled trial, but no details were given on the sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of allocation concealment provided |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "Each week... participants ingested 4 tablets of equal appearance, contained in sealed envelopes" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Each week... participants ingested 4 tablets of equal appearance, contained in sealed envelopes, with a code pre‐determined for each individual and not opened after the completion of the study" Comment: no mention of blinding of outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | High risk | "120 participants were initially recruited (30 in each group). Six of them were then excluded and were not included in the analysis. 8 participants left the area of study (one after the 10th week and 7 after the 11th week of exposure)" Outcomes were included in the analysis, and were substituted by eight new participants. With these six excluded participants and eight substituted participants, final sample size was 122. Comment: participants were not followed up beyond the active phase of treatment for relapses |
| Incomplete outcome data (attrition bias); safety | Unclear risk | Comment: reasons for losses to follow‐up were not reported |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: all cases of malaria were reported |
| Selective reporting (reporting bias); safety | Unclear risk | Comment: there was insufficient information provided regarding the method of adverse effects monitoring to determine whether all outcomes had been reported |
| Other bias | High risk | Roche provided mefloquine and “support” for conducting the study |
Saunders 2015.
| Methods | Design: retrospective cohort study Study dates: January to June 2007 Malaria transmission pattern and local antimalarial drug resistance: "malaria risk and transmission patterns have been known to shift rapidly in Afghanistan" Adverse event monitoring: "A retrospective, anonymous survey was completed by soldiers returning to Fort Drum, NY from Afghanistan" |
|
| Participants | Number enrolled: 2601 surveys distributed, 2351 (90%) returned Inclusion criteria: none mentioned Exclusion criteria: none mentioned Factors influencing drug allocation: "oral mefloquine 250 mg per week was the primary alternative to doxycycline... In some cases, mefloquine was chosen as the first‐line therapy based on either perceived advantages in compliance, unit force protection, and/or operational concerns" Country of recruitment: USA Country of malaria exposure: Afghanistan Duration of exposure to malaria: various, not specified Type of participants: military |
|
| Interventions | Included in review comparisons: 1. Mefloquine* 2. Doxycycline* Not included in review comparisons: 3. Atovaquone‐proguanil* (data on adverse events not collected; data on compliance not reported) *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, vomiting, diarrhoea 2. Adverse effects; other (heartburn/dyspepsia) 3. Discontinuations of study drug due to adverse effects 4. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 5. Clinical cases of malaria 6. Adverse effects: numbers not reported in both groups (nausea, headache, dizziness, abnormal dreams, insomnia, depression, photosensitivity, rash, loss of appetite, pain and/or difficulty swallowing, vaginitis, lightheadedness, nervousness, ringing in ears, chills) 7. Use of personal protective measures to prevent mosquito bites |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Information was provided on duration of deployment, area of deployment, sex, age group and rank across regimens. Area deployed in Afghanistan and sex were different across groups. No adjustment for confounders was made in the analysis 2. Selection of participants into the study: low Response rate 2351/2601 surveys (90%) 3. Measurement of interventions: moderate Participants were asked to self‐report which prophylaxis was used on return to the USA. It is unclear if participants were still receiving the intervention at this time 4. Departures from intended interventions: serious "There were 520 respondents (25.2%) reporting more than one medication used to prevent malaria over the course of the deployment" 5. Missing data: low Analysis included 1898/2011 (94.4%) respondents for doxycycline, 564/596 (94.6%) respondents for mefloquine 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded. Different criteria were used to assess adverse effects related to mefloquine and doxycycline 7. Selection of the reported results: serious There was insufficient information provided regarding the questionnaire to determine whether all included outcomes were reported. Data for doxycycline were provided by severity gradings but not for mefloquine 8. Other: no information No information is provided regarding the study sponsor |
Schlagenhauf 1997.
| Methods | Design: cross‐over RCT Study dates: 1993 to 1994 Malaria transmission pattern and local antimalarial drug resistance: not applicable Adverse event monitoring: "Throughout dosing, the participants were monitored and questioned regarding their general well‐being. The participants were seen 1) prior to taking any medication, 2) at the end of the first week (during which the loading dose was administered, 3) one week before testing, and 4) on the testing day itself when they were asked to report any changes from normal and questioned with regard to any symptoms experienced while taking the drug" |
|
| Participants | Number enrolled: 23 Inclusion criteria: "conducted with trainee pilots attending the Swiss Civil Aviation School during the classroom phases of their study" Exclusion criteria: "history of a seizure disorder; psychosis or severe depression; known allergy or sensitivity to mefloquine or related compounds; concurrent use of cardioactive medication; compromised renal or hepatic function; pregnancy or the intention to become pregnant within three months of mefloquine use; use of mefloquine in the preceding two months, and use of hypnotics or tranquillizers during the two weeks prior to testing and alcohol within 12 hr of testing" Country of recruitment: Switzerland Country of malaria exposure: not applicable Duration of follow up: 4 weeks Type of participants: Swissair trainee pilots, did not travel |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet) given daily on 3 consecutive days followed from day 8 by once a week administration of 1 tablet for three consecutive weeks 2. Placebo (1 tablet) given daily on 3 consecutive days followed from day 8 by once a week administration of one tablet for 3 consecutive weeks |
|
| Outcomes |
Included in the review: 1. Adverse events; any 2. Discontinuations of study drug due to adverse effects 3. Adverse events; other outcomes (instrument co‐ordination analyser, sleep assessment, sway, neurobehavioural evaluation system, profile of mood states) |
|
| Notes | Funding sources: This study was sponsored by the F. Hoffmann La Roche Tropical Medicine Unit (Basel, Switzerland) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of randomization not reported |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Unclear risk | Comment: described as double blind but no mention of whether placebo was identical to the active formulation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no description of who was blinded and how |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | Unclear risk | "There was one withdrawal due to dizziness, diarrhea, and flu‐like symptoms and three volunteers spontaneously reported minor sleep‐related AEs (adverse events), including insomnia, unpleasant dreams, superficial sleep, and early awakening. These events all occurred in the mefloquine loading dose phase" Comment: not clear whether this withdrawal was included in the data analysis |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | High risk | "The individual Environmental Symptom Questionnaire (ESQ) symptoms were also analyzed and items selected for their relevance to mefloquine administration were assessed by Cochran's Q test for related samples" Comment: intra‐individual changes in scores were obtained during the study, but outcomes were presented as means across groups. Data from the ESQ were not reported, only "no significant differences". Data for the Profile of Mood States questionnaire was presented in a graph with no standard deviations |
| Other bias | High risk | This study was sponsored by the F. Hoffmann La Roche Tropical Medicine Unit (Basel, Switzerland). The role of the study sponsor was not clear |
Schlagenhauf 2003.
| Methods | Design: RCT Study dates: 1998 to 2001 Malaria transmission pattern and local drug resistance: not mentioned Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 674 Inclusion criteria: adult travellers aged 18 to 70 years, with planned travel of 1 to 3 weeks to a malaria‐endemic area, and consulting at a travel clinic ≥ 17 days before departure Exclusion criteria: glucose‐6‐phosphate dehydrogenase deficiency, history of severe adverse events with any of the four study drugs or a contra‐indication for their use, pregnancy or unwillingness to adhere to reliable contraception, history of seizures, psychiatric disorders, severely impaired renal or hepatic function, concurrent or recent vaginal infections or bacterial enteric disorders, a history of photosensitivity, or unwillingness to adhere to the study protocol Countries of recruitment: Switzerland, Germany and Israel Region of malaria exposure: sub‐Saharan Africa Duration of exposure to malaria: 1 to 3 weeks Type of participants: travellers |
|
| Interventions | 1. Mefloquine (1 capsule containing mefloquine hydrochloride 274.09 mg, equivalent to mefloquine 250 mg base) once weekly, starting 17 days before travel and continuing for 4 weeks after travel* 2. Chloroquine‐proguanil (1 combined capsule containing chloroquine diphosphatase 161.21 mg, equivalent to chloroquine 100 mg base; and 200 mg proguanil hydrochloride) once daily, starting 17 days before travel and continuing for 4 weeks after travel* 3. Doxycycline (1 capsule containing doxycycline monohydrate 100 mg) once daily, starting 17 days before travel and continuing for 4 weeks after travel* 4. Atovaquone‐proguanil (1 combined capsule containing 250 mg atovaquone and 100 mg proguanil hydrochloride) once daily, starting 17 days before travel and continuing for 1 week after travel* *matched placebo for each treatment arm |
|
| Outcomes |
Included in the review: 1. Adverse events; any 2. Serious adverse events 3. Adverse events; other ('gastrointestinal', 'skin symptoms', 'neuropsychological') ‐ any severity, mild, moderate, severe 4. Discontinuation of study drug due to adverse effects 5. Adverse events; other outcomes (profile of mood states, quality of life score) |
|
| Notes | Funding sources: GlaxoSmithKline supplied atovaquone‐proguanil and gave financial support; Zeneca supplied chloroquine‐proguanil; Pfizer supplied doxycycline; Roche supplied mefloquine and gave financial support | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was from a computer generated table of numbers in permuted blocks of five" |
| Allocation concealment (selection bias) | Unclear risk | "Participants were allocated treatment sequentially in order of study numbers. Allocation concealment was by sealed envelope" Comment: not reported whether envelopes were opaque |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "The drugs were provided as identical capsule blister packs in weekly cards" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: Described as double blind but no mention of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | High risk | Comment: Method of detection for malaria, frequency and duration of follow up were not reported |
| Incomplete outcome data (attrition bias); safety | Unclear risk | "Adverse events were analysed in 623 participants who completed questionnaires at recruitment and at least one of the follow up periods" "Data was collected during recruitment and at follow up 13‐11 days before departure, 6‐4 days before departure and 7‐14 days after departure" Comment: it was unclear how many participants provided data at each time point |
| Selective reporting (reporting bias); efficacy | Low risk | "No cases of malaria were reported for any study arm" |
| Selective reporting (reporting bias); safety | High risk | "Adverse events were analysed in 623 participants who completed questionnaires at recruitment and at least one of the follow up periods" "Data was collected during recruitment and at follow up 13‐11 days before departure, 6‐4 days before departure and 7‐14 days after departure" Comment: Data were presented on aggregate across multiple time points |
| Other bias | High risk | Funding: Pfizer, GlaxoSmithKline, Roche, and Zeneca provided the drugs free of charge. GlaxoSmith Kline and Roche provided research grants. "Competing interests: PS has received speakers’ honorariums and travel expenses from Roche and GlaxoSmithKline. She acted as a consultant to Roche in a drug safety database evaluation. RS has received speakers’ honorariums and travel expenses from GlaxoSmithKline, Roche, and Pfizer. He is also a member of the advisory board of GlaxoSmithKline for malaria prophylaxis related questions. BB has received a speaker’s honorarium and travel expenses from GlaxoSmithKline. HN has received speakers’ honorariums and travel expenses from GlaxoSmithKline on different occasions. He has been principal or coinvestigator in several vaccine trials sponsored by GlaxoSmithKline" |
Schneider 2013.
| Methods | Design: retrospective cohort study Study dates: 1 January 2001 and 1 October 2009 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: Incident cases of a neuropsychiatric disorder including anxiety, stress‐related disorders or psychosis, depression, epilepsy or peripheral neuropathies during or after anti‐malarial drug use within the UK general practice research database |
|
| Participants | Number enrolled: Not available Inclusion criteria: "We identified in the general practice research database all patients who had ≥ 1 prescription of mefloquine, chloroquine and/or proguanil or atovaquone/proguanil between January 1, 2001 and October 1, 2009, and who had a pre‐travel consultation within 1 week of the prescription" Exclusion criteria: "We only included subjects who used anti‐malarial drugs for malaria prophylaxis... Furthermore, individuals had at least 12 months of information on prescribed drugs and medical diagnoses before the first prescription date for a study drug. In addition, subjects had recorded activity (diagnoses or drug prescriptions) at any time after the prescription for an anti‐malarial drug to include only subjects who returned to the UK. We excluded all patients with a diagnosis of malaria prior to the start of anti‐malarial drug use, patients with a history of cancer, alcoholism, rheumatoid arthritis; or with an outcome of interest prior to using anti‐malarial drugs. The date of the first neuropsychiatric disorder was the index date for each case" Country of recruitment: UK Country of malaria exposure: various, not specified Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions |
Included in review comparisons: 1. Mefloquine* 2. Atovaquone‐proguanil* Not included in review comparisons: 3. Chloroquine‐proguanil* 4. Unexposed (case‐control design) *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse events; psychiatric disorders (anxiety, depression, psychosis) 2. Adverse events; other ('anxiety or stress related disorders or psychosis', epilepsy, neuropathy, phobia, panic attack) |
|
| Notes | Funding sources: F. Hoffmann‐La Roche Ltd., Basel, Switzerland | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex and BMI were measured but only reported for people experiencing adverse events 2. Selection of participants into the study: moderate "We excluded all patients with a personal history of recorded neuropsychiatric disorders from the study population, but family history is not consistently recorded in the database" 3. Measurement of interventions: moderate "We only included subjects who used anti‐malarial drugs for malaria prophylaxis. We identified prescriptions for which the GP recorded ‐ within a week of the anti‐malarial drug prescription ‐ specific codes indicating that the person received the prescription for malaria prophylaxis, such as 'travel advice' or “prophylactic drug use” 4. Departures from intended interventions: serious It is possible that participants discontinued or switched medication and this would not have been captured in the study 5. Missing data: moderate The study did not report the total number of participants, only those who experienced adverse events 6. Measurement of outcomes: moderate General practitioners diagnosing patients would have been aware of their exposure status 7. Selection of the reported results: moderate Data for anxiety, stress‐related disorders and psychosis were reported on aggregate 8. Other: serious Study was sponsored by Roche. The role of the funding source was not made clear |
Schwartz 1999.
| Methods | Design: cross‐sectional cohort study Study dates: October 1995 to April 1998 Malaria transmission pattern and local antimalarial drug resistance: "both P. falciparum and P. vivax are hyperendemic" Adverse event monitoring: "...we directly contacted all travelers for complete follow‐up and assessment of compliance. Fifty travelers taking primaquine completed a questionnaire regarding side effects" |
|
| Participants | Number enrolled: 158 Inclusion criteria: Israelis participating in rafting trips in Southern Ethiopia Exclusion criteria: none mentioned Country of recruitment: Israel Country of malaria exposure: Ethiopia Duration of exposure to malaria: 14 to 20 days Type of participants: travellers |
|
| Interventions |
Included in review comparisons: 1. Mefloquine (1 x 250 mg tablet) weekly, Starting 1 week prior to departure, during travel and for 4 weeks after return 2. Doxycycline (1 x 100 mg tablet) daily Not included in review comparisons: 3. Primaquine 15 mg daily for travellers with body weight < 70 kg and 30 mg for those weighing > 70 kg, starting 1 day prior to departure and continuing for up to 2 days after departure 4. Hydroxychloroquine* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 2. Clinical cases of malaria 3. Measure of adherence to the drug regimen (not fully reported) 4. Adverse effects; any (methods of detection different for primaquine versus other regimens) |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex and BMI were not reported for any participants. Destination and duration of travel was roughly equivalent across all groups 2. Selection of participants into the study: moderate Subjects were selected on the basis of their travel destination. Start of follow up and start of intervention coincide. No non‐responses were reported 3. Measurement of interventions: moderate "Prior to the trip, participants consulted one of a number of travel clinics in Israel, among them our clinic" Comment: it was unclear how intervention status was ascertained for participants who visited other clinics 4. Departures from intended interventions: low Two discontinuations (158 participants) were reported 5. Missing data: serious "In addition, we directly contacted all travelers for complete follow‐up and assessment of compliance. Fifty travelers taking primaquine completed a questionnaire regarding side effects" It was unclear how information on discontinuations and side effects were obtained for participants who did not take primaquine" 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: serious "In addition, we directly contacted all travelers for complete follow‐up and assessment of compliance. Fifty travelers taking primaquine completed a questionnaire regarding side effects" It was unclear how information on discontinuations and side effects was obtained for participants who did not take primaquine 8. Other: no information No information was provided regarding the study sponsor |
Shamiss 1996.
| Methods | Design: cross‐sectional cohort study Study dates: not mentioned Malaria transmission pattern and local antimalarial drug resistance: not applicable Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 45 Inclusion criteria: none mentioned Exclusion criteria: none mentioned Factors influencing drug allocation: "Prior knowledge about the side effect profile of mefloquine forced us to prescribe doxycycline 100 mg daily for aviators and mefloquine 250 mg weekly for non‐aviator crew" Country of recruitment: Israel Country of malaria exposure: Rwanda and Zaire Duration of exposure to malaria: "biweekly flights to and from Rwanda to Zaire with an average of 4 hours stay in the field over a period of 2 months" Type of participants: military |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet) weekly, starting on the day of travel (< 12 hours before the first flight) and continuing until 4 weeks after return 2. Doxycycline (1 x 100 mg tablet) daily, starting on the day of travel (< 12 hours before the first flight) and continuing until 4 weeks after return |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, nausea, abdominal pain, dizziness 2. Adverse effects; other (fatigue) 3. Discontinuations of study drug due to adverse effects 4. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 5. Clinical cases of malaria |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Sex and BMI were not measured. Destination and duration of travel were set by the study design 2. Selection of participants into the study: low "Prior knowledge about the side effects profile of mefloquine forced us to prescribe doxycycline 100 mg daily for aviators and mefloquine 250 mg weekly for non‐aviator aircrew up to 1 mo after the last return" All participants completed questionnaires. 3. Measurement of interventions: low Type of prophylaxis used was set by the job of the included participants 4. Departures from intended interventions: low "Two non‐aviators were dropped from the study because of receiving the wrong prescription" 5. Missing data: low "Two non‐aviators were dropped from the study because of receiving the wrong prescription" Information was provided for the remaining 43 participants. 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate "...the questionnaire included questions about compliance, side effects attributed to chemoprophylaxis, and any illness after return" No information was provided regarding illness after return. 8. Other: no information No information is provided regarding the study sponsor |
Sharafeldin 2010.
| Methods | Design: retrospective cohort study Study dates: July 2006 to December 2008 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: "Participants… were sent an informative email asking them to complete a web‐based questionnaire" |
|
| Participants | Number enrolled: 242 students sent questionnaire, 180 respondents Inclusion criteria: "all medical students who had performed an elective abroad between July 2006 and December 2008, who had visited countries where hepatitis A is endemic, and who had notified the student registrar to obtain study credits" Exclusion criteria: none mentioned Factors influencing drug allocation: "...students are free to visit [our occupational health department] or any other travel clinic including the LUMC in‐hospital travel clinic or their general practitioner" Country of recruitment: Netherlands Country of malaria exposure: none mentioned Duration of exposure to malaria: mean duration of stay = 74 days (range 10 to 224 days ) Type of participants: travellers |
|
| Interventions |
Included in review comparisons: 1. Mefloquine* 2. Atovaquone‐proguanil* 3. Doxycycline* Not included in review comparisons: 4. Primaquine* 5. Proguanil* 6. Chloroquine* (no data reported) *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any 2. Serious adverse outcomes 3. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 4. Clinical cases of malaria 5. Risk of infection with bloodborne viruses 6. Health risks while abroad 7. Health problems experienced whilst abroad 8. Health problems experienced on return |
|
| Notes | Funding sources: There was no dedicated funding for this project | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex, destination and duration of travel were measured but information not provided across groups. BMI was not measured 2. Selection of participants into the study: serious Response rate 180/242 (74.4%) 3. Measurement of interventions: serious "...six students did not remember which prophylaxis had been prescribed" Students were asked to self‐report which prophylaxis they took an average of 235 days after completing their trip 4. Departures from intended interventions: moderate "Eight students who used mefloquine (20%) stopped the drug prematurely as did ten students on atovaquone‐proguanil (16%) and the student on doxycycline. Only two of these students switched to another prophylaxis" 5. Missing data: low "none of the questionnaires was incomplete" All participants were included in the analysis 6. Measurement of outcomes: serious The outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate Insufficient information was provided on how data on adverse effects were sought 8. Other: low "There was no dedicated funding for this project" |
Sonmez 2005.
| Methods | Design: prospective cohort study Study dates: April 2002 to October 2003 Malaria transmission pattern and local antimalarial drug resistance: "20% of recent cases were due to P. falciparum' 'chloroquine resistant P. falciparum" Adverse event monitoring: "common questionnaires were used to investigate the compliance to and side effects of both regimes" |
|
| Participants | Number enrolled: 1400 soldiers worked in the region Inclusion criteria: "...all Turkish soldiers were examined in detail and serum samples were taken before heading for the region" Exclusion criteria: "...none of the participants had any chronic disease" Factors influencing drug allocation: "The preference of the preventive regime was related to the availability of the drugs... the prophylaxis was started with doxycycline, which was at hand in March 2002. Then again the soldiers who came after July 2002 were given mefloquine" Country of recruitment: Afghanistan Country of malaria exposure: Afghanistan Duration of exposure to malaria: "The average time of presence for a single soldier in Kabul region was approx. 6 month [sic]" Type of participants: military |
|
| Interventions | 1. Mefloquine* 2. Doxycycline* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Serious adverse effects 2. Adverse effects; any, nausea, vomiting, abdominal pain, diarrhoea, headache, insomnia, dyspepsia, anorexia Outcomes assessed not included in the review: 3. Clinical cases of malaria |
|
| Notes | Funding sources: Not mentioned Communications with study author: Sonmez 2005 no longer had access to the original study data. However, the study authors confirmed that for table 1: "The comparisons of the number of side effects of both regimes" the number of side effects for specific symptoms e.g. nausea was equivalent to the number of soldiers reporting that side effect. In addition, the authors were able to clarify a discrepancy in the original text: the paper states "27 mefloquine takers (41.2%) reported 43 side effects at the 2nd week of prophylaxis". The total number of mefloquine participants was 228; 41.2% equates to 94 participants. The authors confirmed that the correct figure was 27 mefloquine users (11%). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age of participants was balanced across groups. Destination and duration of travel were set by the study design. Sex and BMI were not reported 2. Selection of participants into the study: serious 734 soldiers returned questionnaires (52.2%) 3. Measurement of interventions: low All soldiers were issued with prophylaxis 4. Departures from intended interventions: low Switches between prophylactic regimens were not possible 5. Missing data: low The data were collected at 2 time points. The reported denominator for each time point was the same 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate There was insufficient information provided to be sure that all outcomes included in the questionnaire were reported 8. Other: no information No information was provided regarding the study sponsor |
Sossouhounto 1995.
| Methods | Design: RCT Study dates: January 1989 to June 1989 Malaria transmission pattern and local antimalarial drug resistance: "region endemic for P. falciparum malaria" Adverse event monitoring: "participants had access to a village health center, where they could notify personnel of any malaise or side effects. Clinical examinations and parasitologic tests were performed every 4 weeks. Blood counts were carried out at the end of weeks 4, 19 and 24" |
|
| Participants | Number enrolled: 500 Inclusion criteria: "five‐hundred male volunteers, aged 16‐60 years, who were residents of a local village, were randomly assigned" Exclusion criteria: none mentioned Country of recruitment: Adzope region, Ivory Coast Country of malaria exposure: Adzope region, Ivory Coast Duration of exposure to malaria: study duration 20 weeks Type of participants: Ivory Coast residents, semi‐immune |
|
| Interventions |
Included in review comparisons: 1. Mefloquine (1 x 250 mg tablet) weekly in weeks 1 to 4, (1 x 125 mg tablet) weekly in weeks 5 to 20 2. Chloroquine (1 x 300 mg tablet) weekly for 20 weeks 3. Placebo (1 tablet) weekly for 20 weeks Not included in review comparisons: 4. Fansidar 5. Fansifem |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Episodes of parasitaemia 3. Serious adverse events 4. Adverse events: any, diarrhoea, headache, pruritis Outcomes assessed not included in the review: 5. Laboratory tests; haematocrit and white blood cell count 6. Adverse events: other (leukopenia, malaise; did not occur in any study participants) |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Five‐hundred male volunteers… were randomised" Comment: Method of randomization was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of allocation concealment was provided |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "double blind". "The medications and placebo were identical in appearance" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no information was provided on how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | Low risk | "Four hundred and ninety‐nine subjects were evaluated for safety (at least one tablet taken and one visit) as well as for efficacy" Comment: 499/500 (99.8%) participants included in the analysis |
| Incomplete outcome data (attrition bias); safety | Low risk | "Four hundred and ninety‐nine subjects were evaluated for safety (at least one tablet taken and one visit) as well as for efficacy" Comment: 499/500 (99.8%) participants included in the analysis |
| Selective reporting (reporting bias); efficacy | Low risk | Comment: all outcomes prespecified in the methods section were reported |
| Selective reporting (reporting bias); safety | Unclear risk | "Blood counts were carried out at the end of weeks 4, 19 and 24" Comment: blood counts were reported only for one participant who developed reversible leukopenia |
| Other bias | Unclear risk | Comment: no information provided regarding the study sponsor |
Steffen 1993.
| Methods | Design: cohort study Study dates: Malpro 1‐ April 1985 to July 1988, Malpro 2‐ July 1988 to December 1991 Malaria transmission pattern and local antimalarial drug resistance: various, not stated Adverse event monitoring: self‐completed questionnaires were distributed and collected by cabin crews to all passengers returning on charter planes |
|
| Participants | Number enrolled: 145,003 Inclusion criteria: not explicitly stated. This trial includes two publications, Steffen 1993 states "All passengers returning on charter planes from Mombasa, Kenya, to Europe", whereas Steffen 1990 states "all passengers flying back to Europe from East Africa (Kenya) or West Africa (9 countries)". Data have been included from Steffen 1993 Exclusion criteria: "All travellers who stayed longer than one year in tropical Africa were excluded, as were those who did not spend the main part of their visit in East Africa (Kenya, Tanzania and Uganda)" Country of recruitment: not applicable Region of malaria exposure: East Africa (Kenya, Tanzania, Uganda) Duration of exposure to malaria: various, not stated Type of participants: travellers |
|
| Interventions |
Included in review comparisons: 1. Mefloquine* 2. Chloroquine (1 x 300 mg tablet) weekly Not included in review comparisons: 3. Chloroquine (1 x 600 mg tablet) weekly 4. Proguanil* 5. Chloroquine + proguanil* 6. Pyrimethamine + sulfadoxine* 7. Non‐users (this population was asked about side effects (adverse effects) and instead answered regarding adverse events *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Serious adverse effects 2. Adverse effects; any (mild, moderate or severe), visual impairment, nausea, headache, dizziness, insomnia, depression, pruritis 3. Adverse effects; other ('other skin', medical consultations due to side effects, incapacitation due to side effects, 'cutaneous', 'redness of the skin', consulted a doctor) 4. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 5. Clinical cases of malaria 6. Measures taken against mosquito bites 7. Sources of pre‐travel health information 8. Places visited in tropical Africa |
|
| Notes | Funding sources: "This study was sponsored by F. Hoffman‐La Roche Ltd, Basel, Switzerland" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex and BMI were not reported across different prophylactic groups 2. Selection of participants into the study: moderate "In Malpro 1, 80.1% of all passengers completed the in‐flight questionnaire… in Malpro 2 the response rate [was] 83.9%" 3. Measurement of interventions: low Passengers were asked to self‐report which malaria prophylaxis was used. Data were collected on the journey home, meaning it was likely that passengers were still taking this medication 4. Departures from intended interventions: low Handschin 1997: "2.9% of passengers changed the prophylactic regimen during the observation period" 5. Missing data: moderate Malpro 1 losses to follow‐up 4.1%, Malpro 2 losses to follow‐up 14.1% 6. Measurement of outcomes: moderate The outcome measure was subjective; participants and personnel were not blinded. Serious adverse events were verified independently 7. Selection of the reported results: serious Data on non‐serious side effects were not included from Malpro 1‐ 31% of participants (44,667) were not included 8. Other: serious The study was funded by Roche. The role of the study sponsor was not made clear |
Steketee 1996.
| Methods | Design: quasi‐RCT Study dates: September 1987 to June 1990 Malaria transmission pattern and local antimalarial drug resistance: "primarily P falciparum (> 90%), some P malariae and minimal P ovale... High levels of Plasmodium falciparum resistance to CQ... sensitivity of P. falciparum to mefloquine was documented" Adverse event monitoring: "At the time of each dose, a questionnaire was administered to record symptoms including fever and reported drug side effects since the last visit" |
|
| Participants | Number enrolled: 4220 Inclusion criteria: "...consecutive attenders at first antenatal clinic visit were enrolled at three sites… At a fourth side, consecutive attenders in their first and second pregnancy were enrolled" Exclusion criteria: "At this site [fourth site, government district hospital] women with two or more pregnancies were not enrolled because of the large number of patients attending the clinic and the limited number of study staff" Country of recruitment: Malawi Country of malaria exposure: Malawi Duration of exposure to malaria: Ongoing in semi‐immune population ‐ monitored from enrolment for various periods of time Type of participants: pregnant Malawian residents, semi‐immune |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet) weekly, with a single loading dose of 750 mg 2. Chloroquine (1 x 300 mg tablet) weekly, with a loading dose 25 mg of base/kg given as a divided dose over 2 days 3. Chloroquine (1 x 300 mg tablet) weekly |
|
| Outcomes |
Included in the review: 1. Episodes of parasitaemia 2. Adverse events; any 3. Serious adverse events 4. Discontinuations of study drug due to adverse effects 5. Adverse pregnancy outcomes; still births, abortions Outcomes assessed not included in the review: 6. Frequency of placental malarial infection 7. Frequency of prematurity or intra‐uterine growth retardation 8. Frequency of maternal febrile illness or anaemia 9. Likelihood of infant acquisition of malarial infection |
|
| Notes | Funding sources: "This work was supported and made possible by the Africa Bureau, Office of Operations and New Initiatives and the Office of Analysis, Research and Technical Support, the USAID through the Africa Child Survival initiative… The Global Program on AIDS, World Health Organisation provided support for the HIV testing and evaluation portion of this study" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Systematic assignment of regimens was done based on the clinic and day of enrolment… All women making their first antenatal clinic on a given day were assigned to the same regimen; the following day, enrolled women were assigned to the following regimen" |
| Allocation concealment (selection bias) | High risk | "Systematic assignment of regimens was done based on the clinic and day of enrolment… All women making their first antenatal clinic on a given day were assigned to the same regimen; the following day, enrolled women were assigned to the following regimen" |
| Blinding of participants and personnel (performance bias) Adverse effects/events | High risk | Comment: no mention of participants being blinded to which prophylactic regimen they were taking |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "All blood smear examinations were done with the microscopist blinded to the study subject’s antimalarial regimen" Comment: No mention of outcome assessors being blinded to the treatment regimen used when assessing safety outcomes |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | "Among the 4187 enrolled women, 3380 (81%) [were analysed]… 94 did not have an initial blood smear result for comparison, 89 left the study area before follow up, 397 delivered before the follow up visit, 133 missed their appropriate follow up visit, and 94 did not have documented adherence to the drug regimen" Comment: numbers lost to follow up were not reported across groups |
| Incomplete outcome data (attrition bias); safety | High risk | "A total of 4101 women had information available after their first dose and 2976 women had information available after their dose at four weeks" Comment: reasons for missing data were not reported |
| Selective reporting (reporting bias); efficacy | Unclear risk | "Only P falciparum infections were of interest for this study… when P malariae alone was identified these infections were excluded from the analysis" "For the purposes of malaria prevention and infant outcome we analysed the group of women… only if they were enrolled in the study for six or more weeks and had received the appropriate amount of medication during their participation" "A total of 1,790 women delivered in study health facilities had received proper dosing on their antimalarial regimen, and had their peripheral blood examined" Comment: women who had reported fever during pregnancy, and during the 2 weeks prior to delivery was reported, but not reported across antimalarial drug regimens |
| Selective reporting (reporting bias); safety | High risk | "All other complaints e.g. weakness, heart palpitations accounted for less than 15% of reported symptoms" Comment: Data were collected weekly but only reported after the first and the fourth dose |
| Other bias | Low risk | "This work was supported and made possible by the Africa Bureau, Office of Operations and New Initiatives and the Office of Analysis, Research and Technical Support, the USAID through the Africa Child Survival initiative… The Global Program on AIDS, World Health Organisation provided support for the HIV testing and evaluation portion of this study" |
Stoney 2016.
| Methods | Design: Prospective cohort study Study dates: 2009 to 2011 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: "...participants were asked to complete a survey each week during travel and a post‐travel survey within 2–4 weeks after return" |
|
| Participants | Number enrolled: 628 participants completed all three surveys, 370 included in the analysis Inclusion criteria: "Travelers were included from among all those enrolled if they received a prescription for chemoprophylaxis, traveled to at least one malaria‐endemic area, and completed pre‐ and post‐travel surveys and at least one during‐travel survey" Exclusion criteria: "To complete the study in a reasonable amount of time, only participants with shorter durations of travel (approximately 2 months) were included" Factors influencing drug allocation: "Several different medications are available for malaria chemoprophylaxis, depending on the traveler’s destination and medical history" Country of recruitment: USA Country of malaria exposure: India (13%), Tanzania (8%), Kenya (7%), South Africa (7%), and Haiti (7%) Duration of exposure to malaria: median travel duration 13 days Type of participants: travellers |
|
| Interventions |
Included in the review: 1. Mefloquine* 2. Doxycycline* 3. Atovaquone‐proguanil* 4. Chloroquine* Not included in the review: 5. Primaquine* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse effects; any, headache, abnormal dreams 'intense nightmares', any gastrointestinal 2. Discontinuations of study drug due to adverse effects 3. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 4. Clinical cases of malaria 5. Reasons for non‐compliance with chemoprophylaxis (data provided on aggregate), 6. Use of personal protective measures for malaria prevention |
|
| Notes | Funding sources: "This work was supported by a cooperative agreement [1 U19CI000508‐01] between the Centers for Disease Control and Prevention and Boston Medical Center" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex, destination and duration of travel were recorded but figures were not reported across prophylactic regimens 2. Selection of participants into the study: moderate No information was provided regarding travellers who did not wish to participate in the study 3. Measurement of interventions: low "The type of chemoprophylaxis prescribed were collected from data entered by clinicians into patients’ medical records" 4. Departures from intended interventions: moderate No switches or discontinuations were reported. It was unclear whether this information was captured in the questionnaire 5. Missing data: low 364/370 (98%) participants were included in the analysis 6. Measurement of outcomes: serious Comment: the outcome measure was subjective, participants and personnel were not blinded 7. Selection of the reported results: moderate Insufficient information provided on how data on adverse effects were obtained to determine whether all outcomes had been reported 8. Other: low Government funding |
Tan 2017.
| Methods | Design: retrospective cohort study Study dates: 18 July to 16 September 2016 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 8931 Inclusion criteria: Returned Peace Corps volunteers (RPCV) who served between 1995 and 2014 and had an e‐mail address in Peace Corps' RPCV database Exclusion criteria: None mentioned Factors influencing drug allocation: none specified Country of recruitment: USA Country of malaria exposure: various, not specified Duration of exposure to malaria: various, not specified Type of participants: returned Peace Corps volunteers |
|
| Interventions | 1. Mefloquine* 2. Doxycycline* 3. Atovaquone‐proguanil* 4. Chloroquine* *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 2. "Questions about medications before, during, or after Peace Corps, as well as habits such as drinking" |
|
| Notes | Funding source: "this research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Important confounders were measured but not been reported across groups. Duration and destination of travel were not measured 2. Selection of participants into the study: serious 8931/47,238 potential respondents included (13% response rate) 3. Measurement of interventions: serious Participants were asked to self‐report which chemoprophylaxis they had taken at least 2 years after they had finished the course 4. Departures from intended interventions: serious Limited information was provided regarding switches between interventions. Participants were asked to self‐report this information at least 2 years after finishing treatment 5. Missing data: low Information on adherence was reported for all participants who answered this question (5026 respondents/5055 who reported taking malaria prophylaxis) 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate There was insufficient information provided to be sure that all outcomes included in the questionnaire were reported 8. Other: low "This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors" |
Terrell 2015.
| Methods | Design: cross‐sectional cohort study Study dates: 2012 and 2013 Malaria transmission pattern and local antimalarial drug resistance: "...high risk of malaria (mainly P. falciparum) in Kenya, although the risk is assessed as very low in Nairobi and in the highlands above 2,500 m... widespread resistance to chloroquine" Adverse event monitoring: "...questionnaire‐based, two‐arm cohort study" |
|
| Participants | Number enrolled: 2032 completed questionnaires available, 220 failed to indicate which drug they were taking Inclusion criteria: all military personnel on deployment to Kenya who travelled on one of three main body flights on their return to the UK Exclusion criteria: none mentioned Factors influencing drug allocation: "...the choice of drugs considered in this study was limited to mefloquine or doxycycline... participants were free to use another drug should they experience unacceptable adverse effects or where there was an occupational reason" Country of recruitment: UK Country of malaria exposure: Kenya Duration of exposure to malaria: "The majority of participants spent approximately 6 weeks in Kenya with a small number spending a few weeks longer if they filled an administrative role" Type of participants: military |
|
| Interventions |
Included in review comparisons: 1. Mefloquine* 2. Doxycycline* Not included in review comparisons: 3. Atovaquone‐proguanil* (results not included in the analysis) *dosing regimen not specified |
|
| Outcomes |
Included in the review : 1. Adverse effects; any 2. Measure of adherence to the drug regimen Outcomes assessed not included in the review: 3. Clinical cases of malaria 4. Impact of adverse effects on self‐reported ability to work |
|
| Notes | Funding sources: "The research was not sponsored by any external body" After we submitted the review for peer referee, the author sent us a spreadsheet containing numbers of events relating to a variety of symptoms after the review had been submitted for publication. These data are not included in the review and will require some clarification over how they were collected to allow us to assess risk of bias. This additional information will be considered in future updates. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate "Although not formally recorded, each unit can be assumed to be composed of similar populations in terms of number, age, gender, occupation, and general health" 2. Selection of participants into the study: serious "Completion rates were consistently poor throughout the study period with only 150 to 250 questionnaires returned per tranche of around 1,000 troops" 3. Measurement of interventions: low Participants were asked to self‐report which medication they were on while still taking the medication" 4. Departures from intended interventions: moderate "...[participants] were invited to complete the questionnaire for whichever drug they took for the longer period" 5. Missing data: moderate "2,032 completed questionnaires available for analysis of which 10.8% (220) failed to indicate which drug they were taking" 6. Measurement of outcomes: serious The outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: serious "In both arms, some participants indicated that they had experienced an adverse effect but did not report how it had impacted upon their ability to work. They were excluded from the final analysis" Mefloquine: 71 participants, doxycycline: 67 participants 8. Other: low "The research was not sponsored by any external body" |
Tuck 2016.
| Methods | Design: cohort study Study dates: 15 to 22 February 2015 Malaria transmission pattern and local antimalarial drug resistance: not specified Adverse event monitoring: patient self‐reported questionnaire |
|
| Participants | Number enrolled: 115 (337 eligible) Inclusion criteria: all land‐based members of a UK military expedition to Sierra Leone Exclusion criteria: none specified Country of recruitment: Sierra Leone Country of malaria exposure: Sierra Leone Duration of exposure to malaria: not specified Type of participants: military |
|
| Interventions | 1. Mefloquine 2. Doxycycline 3. Atovaquone‐proguanil |
|
| Outcomes |
Included in the review: 1. Adverse effects: any, nausea, abdominal pain, diarrhoea, dizziness, insomnia 'disturbed sleep', pruritis, indigestion, mouth ulcers, lethargy 2. Measure of adherence to the drug regime |
|
| Notes | Funding source: unfunded | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Age, sex and BMI were not measured. Demographic information not reported across groups 2. Selection of participants into the study: serious 151 (46.3%) returned survey forms 3. Measurement of interventions: low Participants were asked to self‐report which medication they were taking while taking it 4. Departures from intended interventions: moderate Switches between groups were recorded. 8/151 recipients had medications switched due to unacceptable adverse effects. It was unclear to which drug adverse effects were attributed. 5. Missing data: low Data were reported for all survey respondents. 6. Measurement of outcomes: serious The outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate There was insufficient information provided to be sure that all outcomes included in the questionnaire were reported 8. Other: low "This audit was unfunded" |
van Riemsdijk 1997.
| Methods | Design: prospective cohort study Study dates: 24 February to 24 May 1994 Malaria transmission pattern and local antimalarial drug resistance: various, not stated Adverse event monitoring: participant self‐reporting questionnaire |
|
| Participants | Number enrolled: 1791 eligible and willing to co‐operate, data obtained from 1501 participants. Inclusion criteria: "...persons who visited the Travel Clinic in the period between 24 February and 24 May, 1994, and who had an anticipated date of return to the Netherlands before the end of the study period, and who had given informed consent" Exclusion criteria: none stated Country of recruitment: Rotterdam, Netherlands Region of malaria exposure: various; Africa, South America, Asia or the Middle East Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions |
Included in review comparisons: 1. Mefloquine (1 x 250 mg tablet) weekly 2. Non‐users of antimalarials Not included in review comparisons: 3. Proguanil (1 x 200 mg tablet) daily |
|
| Outcomes |
Included in the review: 1. Adverse events; nausea, diarrhoea, dizziness, abnormal dreams, insomnia, anxiety, depression, visual impairment 2. Adverse events; other (agitation, confusion) Outcomes assessed not included in the review: 3. Profile of mood states (only reported in comparison with proguanil) |
|
| Notes | Funding sources: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Counfounding: low Identified confounders were measured and balanced across groups 2. Selection of participants into the study: moderate 1501/1791 (86% response rate) 3. Measurement of interventions: moderate Comment: the prescription was provided by a travel clinic which also performed the study but no information regarding switches and discontinuations were recorded or reported 4. Departures from intended interventions: moderate No information was provided on discontinuations or switches 5. Missing data: moderate 1227/1449 (85%) participants were included in the analysis; chloroquine‐proguanil users were not included. The number of non‐users decreased from 392 to 340 without explanation 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate It was clear what was asked in the questionnaire. Information was sought on the severity of adverse events but this was not reported 8. Other: no information No information was provided regarding the study sponsor |
van Riemsdijk 2002.
| Methods | Design: RCT Malaria transmission pattern and local drug resistance: not mentioned Study dates: unclear Adverse event monitoring: baseline evaluation prior to travel, and follow up date 7 days after the participant left the endemic area and two scheduled telephone conversations |
|
| Participants | Number enrolled: 140 Inclusion criteria: travellers aged ≥ 3 years and weighing ≥ 11 kg with planned travel ≤ 28 days to a malaria‐endemic area (Overbosch 2001) Exclusion criteria: In the published report "We excluded those who had risk factors for concentration impairment (e.g. use of opioids, hypnotics, or tranquillizers or use of alcohol 4 hours before testing)" Within Høgh 2000 (unclear if the same exclusion criteria were applied): poor general health; drug hypersensitivity (to atovaquone, chloroquine or proguanil); history of alcoholism, seizures, psychiatric disorders, severe neurological disorders, severe blood disorders; renal, hepatic or cardiac dysfunction; clinical malaria within previous 12 months; travel to malaria‐endemic area within previous 60 days; risk factors for concentration impairment (e.g. use of opioids, hypnotics, or tranquillizers; or use of alcohol 4 hours before testing) Country of recruitment: Rotterdam Travel Clinic, Netherlands Regions of malaria exposure: various malaria endemic destinations (66% in Africa, 13% South America, 24% other) Mean duration of exposure to malaria: 19 days Type of participants: travellers, non‐immune |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet; or ¼, ½ or ¾ of a tablet, according to body weight) once weekly, starting 7 days before travel and continuing for 4 weeks after travel* 2. Atovaquone‐chloroguanil (1 combined tablet containing 250 mg atovaquone and 100 mg proguanil hydrochloride; or alternatively 1 to 3 combined children's tablets according to body weight, each tablet containing 62.5 mg atovaquone and 25 mg proguanil hydrochloride) once daily, starting 1 to 2 days before travel and continuing for 1 week after leaving the malaria‐endemic area* *matched placebo for each treatment arm |
|
| Outcomes | 1. Adverse events; other outcomes (profile of mood states, neurobehavioural evaluation system) 2. Measures of adherence to the drug regimen 3. Discontinuations of the study drug due to adverse effects |
|
| Notes | Funding source: Netherlands Inspectorate for Healthcare gave financial support 'independently performed in a sample of patients from one center that participated in the MAL30010 multicenter clinical trial'‐ Enrollment criteria and study conduct were described in a separate publication (Høgh 2000) which refers to a different study population (atovaquone‐proguanil versus chloroquine‐proguanil). 'This study was planned and performed independently from the trial by other researchers and without knowledge of its results.' 'Subjects were separately recruited and asked for consent during the initial screening visit of the trial.' |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated code was used to randomly assign a treatment number to the three bottles of study drug for every individual. At all sites consecutively enrolled individuals who satisfied all entry criteria received the next treatment number" (Høgh 2000) |
| Allocation concealment (selection bias) | Low risk | "Treatment codes were provided to investigators in opaque sealed envelopes, to be opened only if knowledge of study drug assignment was required for management of a medical emergency" (Høgh 2000) |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Unclear risk | "To mask differences between the dosing regimes, placebo tablets were used... All placebo treatment regimens were identical to the aforementioned scheme for the active ingredient of mefloquine and atovaquone plus chloroguanide" Comment: did not mention whether the placebo and intervention tablets were identical in appearance |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The assessments were made by researchers who were unaware of the treatment allocation" |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | High risk | "We enrolled a total of 140 subjects in the cohort, 119 of whom completed the follow up" Comment: Those who did not complete follow up were not included in the subsequent statistical analysis. The proportion of participants who did not complete the study due to adverse outcomes varied significantly between groups (67% mefloquine and 33% atovaquone plus chloroguanide) |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | Low risk | "Data were collected on concurrent medications, as well as subject’s use of coffee, alcohol and illicit drugs" "stratification for sex and adjustment for potential confounders such as smoking and the use of coffee and tea did not affect the result" Comment: these data were not presented |
| Other bias | Low risk | Funding: "For this study came from the Inspectorate for Health Care. Glaxo Wellcome kindly provided us with the treatment allocation codes after completion of the study. No financial support, however, was received from any pharmaceutical company" |
Vuurman 1996.
| Methods | Design: RCT Study dates: not mentioned Malaria transmission pattern and local antimalarial drug resistance: not applicable Adverse event monitoring: "After each driving test, subjects [described]... the presence and severity of adverse effects ‐ drowsiness, weakness, headache, fatigue, nervousness, nausea, dizziness and memory disturbance" |
|
| Participants | Number enrolled: 42 Inclusion criteria: "...[volunteers] were medically screened by routine blood chemistry and haematology tests, a physical examination including an 12‐lead ECG recording, and urine tests for pregnancy and drugs of abuse" Exclusion criteria: "...clinically relevant abnormalities in any blood test; far‐field, binocular visual acuity that deviated by more than 0.65 dioptres from normal, corrected or uncorrected; known hypersensitivity to any drug; history of any serious gastrointestinal, hepatic, renal neurologic or psychiatric disorder; evidence of drug or alcohol abuse, excessive alcohol or nicotine use; blood donation or participation in a drug trial within the prior 2 months; and for premenopausal females, pregnancy, lactation or failure to exercise reliable birth control" Country of recruitment: Netherlands Country of malaria exposure: not applicable Duration of follow up: 30 days Type of participants: non‐exposed Dutch nationals |
|
| Interventions | 1. Mefloquine (1 x 250 mg tablet) weekly, with loading dose of one tablet daily for 3 days in week 1 2. Placebo (1 tablet) weekly, with identical loading regimen of placebo tablets |
|
| Outcomes | 1. Adverse events; any, nausea, diarrhoea, headache, dizziness 2. Adverse events; other (fatigue) 3. Discontinuations of study drug due to adverse effects 4. Adverse events; other outcome measures (critical flicker/fusion frequency, critical instability tracking test, standardized stabilimetry method of the International Society of Posturography, tests of driving performance) |
|
| Notes | Funding sources: "The study was sponsored by F. Hoffmann‐La Roche Ltd" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The study followed a randomised, 2‐arm, double‐blind, parallel group design" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | "The study followed a randomised, 2‐arm, double‐blind, parallel group design" Comment: method of allocation concealment not described |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Low risk | "They received mefloquine 250 mg or placebo in identically appearing tablets" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: described as double blind but no description of how this was achieved for researchers and outcome assessors |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | Low risk | Comment: dropouts were reported. 2/20 participants dropped out of the mefloquine group, one due to adverse effects related to the study drug |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | High risk | "...subjects used 10 cm visual‐analogue scales to describe their mood in three dimensions – 'Alertness', 'Contentedness', and 'Calmness'” Comment: outcomes relating to these descriptions were not reported. The study reports "events occurring more than once" in each group |
| Other bias | High risk | "The study was sponsored by F. Hoffmann‐La Roche Ltd" |
Waner 1999.
| Methods | Design: cross‐sectional cohort study Study dates: April to May 1996 Malaria transmission pattern and local antimalarial drug resistance: "a high risk Malaria area... Chloroquine‐resistant P. falciparum malaria" Adverse event monitoring: "In‐flight self administered questionnaires were distributed and completed by travelers on flights returning to Johannesburg International Airport" |
|
| Participants | Number enrolled: 4035 questionnaires distributed, 3051 returned Inclusion criteria: All travelers boarding the only commercial airline serving this area during April and May 1996 were included in the survey Exclusion criteria: None mentioned Country of recruitment: South Africa Country of malaria exposure: South Africa Duration of exposure to malaria: various, not specified Type of participants: travellers |
|
| Interventions |
Included in review comparisons: 1. Mefloquine* 2. Doxycycline* 3. Chloroquine* Not included in review comparisons: 4. Chloroquine‐proguanil* 5. Proguanil* *dosing regimen not specified |
|
| Outcomes |
Included in review comparisons: 1. Adverse effects; any Outcomes assessed not included in the review: 2. Sources of information on malaria prior to visit, 3. Use of personal protective measures against mosquitoes, 4. Measures of adherence to the drug regimen (information provided on aggregate), 5. Travellers knowledge of malaria symptoms |
|
| Notes | Funding sources: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Confounding: moderate Sex of travellers was not provided by prophylactic regimen. Destination of travel was set by the study design. BMI of travellers and duration of travel were not recorded 2. Selection of participants into the study: serious Response rate 3051/4035 (75%) 3. Measurement of interventions: low Travellers were asked to self‐report which prophylactic regimen they were taking while still using the drug 4. Departures from intended interventions: moderate No discontinuations or switches were reported. This information was not included in the questionnaire 5. Missing data: low Outcome data were available for 973/978 mefloquine recipients and 80/80 doxycycline recipients 6. Measurement of outcomes: serious Comment: the outcome measure was subjective; participants and personnel were not blinded 7. Selection of the reported results: moderate Insufficient information provided on how data on adverse effects were obtained to determine whether all outcomes were reported 8. Other: no information No information was provided regarding the study sponsor. |
Weiss 1995.
| Methods | Design: RCT Study dates: April to July 1993 Malaria transmission pattern and local antimalarial drug resistance: "Incidence of new cases of falciparum malaria during the rainy seasons has been measured at 90% in adults. P. falciparum accounts for > 95% of all malaria in Saradidi" Adverse event monitoring: "Each subject was visited daily at home by an assigned field worker, who asked about symptoms of malaria or drug side effects, obtained malaria smears, or administered drug doses if the subject was not at school" |
|
| Participants | Number enrolled: 169 Inclusion criteria: aged 9 to 14 years. "Screening consisted of a physical examination, a urine pregnancy test for girls, and blood tests for complete blood cell count; blood urea nitrogen, serum alanine aminotransferase, and glucose‐6 phosphate dehydrogenase (G6PD) levels; and hemoglobin electrophoresis" Exclusion criteria: none mentioned Country of recruitment: Saradidi Rural Health Project, Nyanza province, Kenya on the shores of Lake Victoria Country of malaria exposure: Saradidi Rural Health Project, Nyanza province, Kenya on the shores of Lake Victoria Duration of exposure to malaria: study duration 4 months Type of participants: Kenyan residents, semi‐immune |
|
| Interventions | 1. Melfoquine (1 x 125 mg tablet) weekly, with a second dose given on the third day of the study, equal to their usual weekly medication. 2. Doxycycline (1 x 50 mg tablet) daily 3. Primaquine 4. Multivitamin (1 x tablet containing vitamin A, 2500 IU, thiamine, 1 mg, riboflavin, 0.5 mg, nicotinamide, 7.5 mg, ascorbic acid, 15 mg, vitamin 0 3, 250 IU) daily Co‐interventions: After baseline malaria smears, all subjects received curative therapy for preexisting malaria: 7 days of quinine bisulfate, 300 mg three times daily, and doxycycline, 50 mg twice daily. The first dose of prophylactic drug was given starting the day after curative therapy finished |
|
| Outcomes |
Included in the review: 1. Clinical cases of malaria 2. Episodes of parasitaemia 3. Discontinuations of study drug due to adverse effects Outcomes assessed not included in the review: 4. Laboratory tests; complete blood cell counts, blood urea nitrogen and serum alanine aminotransferase 5. Mean number of symptoms reported per subject: nausea, abdominal pain, diarrhoea, headache, fever |
|
| Notes | Funding sources: Financial support: USA Naval Medical Research and Development Command (work unit no. 623002A.81 0.00 J0 I.HFX. J433). Kenya Medical Research Institute. USA Army Medical Research and Materiel Command Provisional (contract no. DAMDI7‐92‐V‐20J2) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Students from each village school were separately randomized, to control for geographic variation in malaria transmission" Comment: no description of how randomization was performed |
| Allocation concealment (selection bias) | Unclear risk | "All medications were in brown envelopes and were administered 7 days each week by I field worker at each school" Comment: no mention of whether envelopes were sealed or if field workers had access to their content |
| Blinding of participants and personnel (performance bias) Adverse effects/events | Unclear risk | Comment: no mention of whether participants were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "None of the malaria slide readers knew which drugs the subjects were taking. None of the field workers visiting the homes daily to ask about symptoms or clinical staff evaluating and treating subjects at the Saradidi Clinic knew which drugs the subjects were taking. If there was concern about a drug side effect, the clinical staff would consult the medical monitor, who would break the code for that subject. This occurred only four times during the studies" |
| Incomplete outcome data (attrition bias); efficacy | Unclear risk | N/A |
| Incomplete outcome data (attrition bias); safety | Unclear risk | Comment: number included in the safety analysis not reported |
| Selective reporting (reporting bias); efficacy | Unclear risk | N/A |
| Selective reporting (reporting bias); safety | Unclear risk | Comment: mean number of symptoms reported per subject during 11 weeks of the study were reported. A targeted list of symptoms was reported, with everything else included in ‘all other’. It was unclear what this list included |
| Other bias | Low risk | Financial support: USA Naval Medical Research and Development Command (work unit no. 623002A.81 0.00 J0 I.HFX. J433). Kenya Medical Research Institute. USA Army Medical Research and Materiel Command Provisional (contract no. DAMDI7‐92‐V‐20J2) |
Wells 2006.
| Methods | Design: retrospective cohort study Study dates: January 2002 to December 31 2002 Malaria transmission pattern and local antimalarial drug resistance: various, not specified Adverse event monitoring: "The study cohort was electronically linked to the Standardized Inpatient Data Record (SIDR) and the Health Care Service Record (HCSR) to identify hospitalization... We analyzed any‐cause hospitalization (excluding complications of pregnancy, childbirth, and the puerperium, congenital anomalies, and certain conditions originating in the perinatal period)" |
|
| Participants | Number enrolled: 397442 Inclusion criteria: "All active‐duty US service members during the period January 1, 2002, and December 31, 2002, as reported by the Defense Manpower Data Center (DMDC), Monterey, CA. The mefloquine prescribed group was defined as service members who had been prescribed a minimum of seven mefloquine tablets beginning in 2002 and who were identified as having been deployed at some point during the same time period. We used two reference groups. The first reference group was comprised of service members who had duty zip codes for either Europe or Japan at some time during 2002 and had no evidence of having been deployed from October 1, 2001 through the individual’s period of observation... The second reference group consisted of US service members who were identified as having been deployed for a minimum of 1 month during 2002" Exclusion criteria: "Both reference groups were restricted to individuals who had no evidence of having received a prescription for mefloquine or chloroquine or a doxycycline prescription for more than 14 tablets.’ ‘Individuals who could not be followed a minimum of 2 months were excluded from the study" Country of recruitment: USA Country of malaria exposure: various, not specified Duration of exposure to malaria: various, not specified Type of participants: military |
|
| Interventions | 1. Mefloquine* 2. Non‐users of antimalarials *dosing regimen not specified |
|
| Outcomes |
Included in the review: 1. Adverse events; serious (any hospitalization, hospitalizations due to vertiginous syndromes, migraine, dizziness and giddiness, anxiety disorders, somatoform disorders, mood disorders, PTSD, substance use disorders, personality disorders, nystagmus or adjustment reaction) Outcomes assessed not included in the review: 2. Hospitalizations coded according to classification system: infectious/parasitic, neoplasms, endocrine, nutritional, metabolic, blood and blood‐forming organs, mental disorders, nervous system, circulatory system, respiratory system, digestive system, genitourinary system, skin and subcutaneous tissues, musculoskeletal and connective tissue, ill‐defined conditions, injury and poisoning |
|
| Notes | Funding sources: "This represents report 05–05, supported by the Department of Defense, under work unit no. 60002" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Other bias | Unclear risk |
1. Counfounding: moderate BMI, destination and duration of travel have not been recorded 2. Selection of participants into the study: serious "Follow‐up time began on return from deployment for mefloquine‐prescribed members, and for the deployed reference group, on assignment to Europe or Japan, or January 1, 2002, whichever occurred last for the Europe/Japan reference group" Start of follow up began a long time after start of intervention 3. Measurement of interventions: serious Surrogate measure used for mefloquine exposure. There was a possiblity that some participants in the second deployed reference group took mefloquine 4. Departures from intended interventions: moderate "Both reference groups were restricted to individuals who had no evidence of having received a prescription for mefloquine or chloroquine or a doxycycline prescription for more than 14 tablets" 5. Missing data: moderate "Individuals who could not be followed a minimum of 2 months were excluded from the study" Comment: number of participants in this group not reported 6. Measurement of outcomes: low The outcome measure (hospitalizations) was objective 7. Selection of the reported results: low All prespecified outcomes were reported 8. Other: low Government funding |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abraham 1999 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely |
| Adera 1995 | Cohort study. R eported on efficacy but no other relevant outcomes |
| Adshead 2014 | Single arm cohort study |
| Angelin 2014 | No relevant outcomes reported |
| Anonymous 1991 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Anonymous 1998 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Anonymous 1998a | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Anonymous 2005 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Anonymous 2009 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Artaso 2004 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Arthur 1990a | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Banerjee 2001 | No relevant outcomes reported |
| Barbero Gonzalez 2003 | No relevant outcomes reported |
| Barrett 1996 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely |
| Berger 1998 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Berman 2004 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Bernado 1994 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Bijker 2014 | This trial evaluated chemoprophylaxis plus sporozoite immunization |
| Bjorkman 1991 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Black 2007 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Blanke 2003 | Cohort study. R eported on efficacy but no other relevant outcomes |
| Botella de Maglia 1999 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Bourgeade 1990 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Brenier‐Pinchart 2000 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Brisson 2012 | No relevant outcomes reported |
| Bruguera 2007 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Burke 1993 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Caillon 1992 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Carme 1997 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely |
| Castot 1988 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Cave 2003 | No relevant outcomes reported |
| Charles 2007 | No relevant outcomes reported |
| Chin 2016 | No relevant outcomes reported |
| Clifford 2009 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Clift 1996 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Clyde 1976 | Single‐arm cohort study |
| Cobelens 1997 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Cohen 1997 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Conget 1993 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Conrad 1997 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Corbett 1996 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely |
| Coulaud 1986 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Croft 1996 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Croft 1997 | RCT. C ompared mefloquine with a regimen that is no longer used routinely |
| Del Cacho 2001 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely |
| Dia 2010 | No relevant outcomes reported |
| Durrheim 1999 | Cohort study. Compare d mefloquine with a regimen that is no longer used routinely |
| Eamsila 1993 | Cohort study. Compare d mefloquine with a regimen that is no longer used routinely |
| El Jaoudi 2010 | Single arm cohort study |
| Fernando 2016 | No relevant outcomes reported |
| Fujii 2007 | Single arm cohort study |
| Hamer 2008 | No relevant outcomes reported |
| Hellgren 1990 | No relevant outcomes reported |
| Hopperus 1996 | Single arm cohort study |
| Jaspers 1996 | Single arm cohort study |
| Jensen 1998 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Karbwang 1991 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| Karbwang 1991a | Mefloquine was used as a combination regimen with sulph adoxine and pyrimethamine |
| Khaliq 2001 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Kimura 2006 | No relevant outcomes reported |
| Kitchener 2003 | No relevant outcomes reported |
| Kitchener 2005 | Cohort study. A llocation to study drug was based on the occurrence of adverse effects |
| Kok 1997 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Kollaritsch 2000 | Single arm cohort study |
| Kozarsky 1993 | Single arm cohort study |
| Landry 2006 | Single arm cohort study |
| Lapierre 1983 | Single arm cohort study |
| Lim 2005 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Lobel 1993 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely. C hloroquine users we re not clearly separated from users of chloroquine‐proguanil |
| Looareesuwan 1987 | No relevant outcomes reported |
| MacArthur 2002 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Malvy 2006 | Cohort study. R eported on efficacy but no other relevant outcomes |
| Marcy 1996 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Massey 2007 | No relevant outcomes reported |
| Matsumura 2005 | Single arm cohort study |
| Meszaros 1996 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Michel 2007 | Cohort study. R eported on efficacy but no other relevant outcomes |
| Mimica 1983 | No relevant outcomes reported |
| Mizuno 2006 | Single arm cohort study |
| Mizuno 2010 | Single arm cohort study |
| Moon 2011 | No relevant outcomes reported |
| Morales de Naime 1989 | No relevant outcomes reported |
| Munawar 2012 | Single arm cohort study |
| Mølle 2000 | Cohort selected on basis of adverse events |
| Namikawa 2008 | No relevant outcomes reported |
| Nasveld 2010 | RCT. C ompared mefloquine with a regimen which is not used routinely |
| Nevin 2010 | No relevant outcomes reported |
| Nevin 2012 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Nosten 1990 | RCT. Did not include a comparator; compared alternate mefloquine doses |
| Nosten 1999 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| Nwokolo 2001 | Cohort study. Compared mefloquine with a regimen that is no longer used routinely |
| Olanrewaju 2000 | Single arm cohort study |
| Ollivier 2004 | Single arm cohort study |
| Peetermans 2001 | Cohort study. Compared mefloquine with a regimen that is no longer used routinely |
| Peragallo 1999 | Cohort study. Compared mefloquine with a regimen that is no longer used routinely |
| Peragallo 2002 | Single arm cohort study |
| Peragallo 2014 | Single arm cohort study |
| Philips 1994 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Phillips 1996 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Phillips‐Howard 1998 | Cohort study. Compared mefloquine with a regimen that is no longer used routinely |
| Pistone 2007 | No relevant outcomes reported |
| Port 2011 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| Potasman 2000 | Cohort selected on basis of adverse events |
| Quinn 2016 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Reisinger 1989 | RCT. C ompared mefloquine with a regimen that is no longer use d routinely |
| Rieckmann 1974 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| Rieke 1993 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Ries 1993 | Not a randomiz ed or cohort study e.g. case report or case control study |
| Ringqvist 2015 | Cohort selected on basis of adverse events |
| Rombo 1993 | RCT. C ompared mefloquine with a regimen that is no longer used routinely |
| Rønn 1998 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| Sallent 1997 | No relevant outcomes reported |
| Schlagenhauf 1996 | Single arm cohort study |
| Scott 1993 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Smail 1991 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Smoak 1997 | Single arm cohort study |
| Suriyamongkol 1991 | Single arm cohort study |
| Tansley 2010 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| ter Kuile 1993 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Todd 1997 | No relevant outcomes reported |
| Turner 2014 | No relevant outcomes reported |
| Valerio 2005 | No relevant outcomes reported |
| Van Genderen 2007 | No participants received mefloquine prophylaxis |
| Van Grootheest 1999 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| van Riemsdijk 2004 | Single arm cohort study |
| Venturini 2011 | Single arm cohort study |
| Wagner 1986 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Wallace 1996 | Field study in which troops switched extensively between mefloquine and doxycycline. Unable to attribute side effects to either prophylactic regimen |
| Weinke 1991 | Cohort selected on basis of adverse events |
| White 2016 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Win 1985 | Mefloquine not used at a prophylactic dose (e.g. treatment dose or i ntermittent preventive treatment of malaria in pregnancy dose) |
| Winstanley 1999 | Not a research study of malaria prophylaxis e.g. letter to the editor or editorial |
| Wolters 1997 | Cohort study. C ompared mefloquine with a regimen that is no longer used routinely |
Differences between protocol and review
In the protocol we planned to use a modified version of the ACROBAT‐NRSI tool (now referred to as ROBINS‐I) (ACROBAT‐NSRI tool). In the full review we used the original version.
In the protocol we stated that we would include "clinical cases of malaria, diagnosed by PCR or microscopy". In the full review we included trials in which the methods of detection for malaria were unclear, or different (one RCT which tested for antibodies to a circumsporozoite protein four weeks after travel). This change occurred due to difficulties in establishing diagnoses of malaria in short‐term travellers. No cases of malaria occurred in any study arm in any of these additionally included studies.
In the full review we did not include comparisons with regimens that are currently not routinely used or single‐arm cohort studies. These are planned to be analysed in separate systematic reviews (Rodrigo 2016; Tickell‐Painter 2017).
Differences between 2015 review and this review update
We amended the review title from 'Drugs for preventing malaria in travellers' to 'Mefloquine for preventing malaria during travel to endemic areas.
We rewrote the protocol. Criteria for included studies, methods, and outcomes were revised. The was externally peer refereed by two editors.
The scope of the review changed to cover only efficacy and safety of mefloquine. The search was updated. The types of studies were changed to include non‐RCTs/cohort studies for analysis of safety. The control arm was changed to include placebo or no intervention, as well as the commonly used alternatives of atovaquone‐proguanil, doxycycline, and chloroquine. Types of participants were changed to include all adults and children, including pregnant women (now includes immune and partially‐ immune participants). We altered the inclusion of adverse outcomes; we included measures of adherence to the drug regime and adverse pregnancy outcomes. We modified the 'Risk of bias' assessment to include methods of assessment for non‐randomized trials and risk of bias in conduct and reporting of adverse events and adverse effects.
We did not include any analysis of deaths, suicides, or parasuicides attributable to mefloquine prophylaxis; these are addressed in a separate review (Tickell‐Painter 2017).
The author team changed from Jacquerioz FA and Croft AM to Tickell‐Painter M, Mayaan N, Saunders R, Pace C, and Sinclair D.
Contributions of authors
Maya Tickell‐Painter (MTP) and David Sinclair (DS) performed title and abstract and full text screening of the search results. MTP and Nicola Mayaan assessed the methodological quality of trials and extracted and analysed data. MTP completed the first draft of the review. DS, Cheryl Pace and Rachel Saunders provided advice on content and methodology. All authors approved the final version for publication.
Sources of support
Internal sources
Liverpool School of Tropical Medicine, UK.
External sources
-
Department for International Development, UK.
Grant: 5242
Declarations of interest
NM was contracted by the Cochrane Infectious Diseases Group (CIDG) as a freelance consultant to work on this review and previously worked for Enhanced Reviews Ltd, a company that conducts systematic reviews mostly for the public sector. NM is currently employed by Cochrane Response, an evidence services unit operated by Cochrane.
CP has been involved in aspects of clinical trial management for trials of antimalarials (other than mefloquine) where the study drug has been supplied free of charge by the manufacturer.
David Sinclair was employed at Liverpool School of Tropical Medicine as an author and editor with the CIDG, funded through a grant from the UK Department for International Development.
RS was employed at Liverpool School of Tropical Medicine as an author with the CIDG, funded through a grant from the UK Department for International Development.
MTP was employed at Liverpool School of Tropical Medicine as an author with the CIDG, funded through a grant from the UK Department for International Development.
Unchanged
References
References to studies included in this review
Albright 2002 {published data only}
- Albright TA, Binns HJ, Katz BZ. Side effects of and compliance with malaria prophylaxis in children. Journal of Travel Medicine 2002;9(6):289‐92. [DOI] [PubMed] [Google Scholar]
Andersson 2008 {published data only}
- Andersson H, Askling HH, Falck B, Rombo L. Well‐tolerated chemoprophylaxis uniformly prevented Swedish soldiers from Plasmodium falciparum malaria in Liberia, 2004‐2006. Military Medicine 2008;173(12):1194‐8. [DOI] [PubMed] [Google Scholar]
Arthur 1990 {published data only}
- Arthur JD, Echeverria P, Shanks GD, Karwacki J, Bodhidatta L, Brown JE. A comparative study of gastrointestinal infections in United States soldiers receiving doxycycline or mefloquine for malaria prophylaxis. American Journal of Tropical Medicine and Hygiene 1990;43(6):608‐13. [DOI] [PubMed] [Google Scholar]
Belderok 2013 {published data only}
- Belderok SM, Hoek A, Roeffen W, Sauerwein R, Sonder GJ. Adherence to chemoprophylaxis and Plasmodium falciparum anti‐circumsporozoite seroconversion in a prospective cohort study of Dutch short‐term travelers. PLoS ONE 2013;8(2):e56863. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boudreau 1991 {published data only}
- Boudreau EF, Pang LW, Chaikummao S, Witayarut C. Comparison of mefloquine, chloroquine plus pyrimethamine‐sulfadoxine (Fansidar), and chloroquine as malarial prophylaxis in eastern Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 1991; Vol. 22, issue 2:183‐9. [PubMed]
Boudreau 1993 {published data only}
- Boudreau E, Schuster B, Sanchez J, Novakowski W, Johnson R, Redmond D, et al. Tolerability of prophylactic Lariam regimens. Tropical Medicine and Parasitology 1993;44(3):257‐65. [PubMed] [Google Scholar]
Bunnag 1992 {published data only}
- Bunnag D, Malikul S, Chittamas S, Chindanond D, Harinasuta T, Fernex M, et al. Fansimef for prophylaxis of malaria: a double‐blind randomized placebo controlled trial. Southeast Asian Journal of Tropical Medicine and Public Health 1992; Vol. 23, issue 4:777‐82. [PubMed]
Corominas 1997 {published data only}
- Corominas N, Gascon J, Mejias T, Caparros F, Quinto L, Codina C, et al. Adverse drug reactions associated to the antimalarial chemoprophylaxis. Medicina Clinica 1997;108(20):772‐5. [PubMed] [Google Scholar]
Cunningham 2014 {published and unpublished data}
- Cunningham J, Horsley J, Patel D, Tunbridge A, Lalloo DG. Compliance with long‐term malaria prophylaxis in British expatriates. Travel Medicine and Infectious Disease 2014;12(4):341‐8. [DOI] [PubMed] [Google Scholar]
Davis 1996 {published data only}
- Davis TM, Dembo LG, Kaye‐Eddie SA, Hewitt BJ, Hislop RG, Batty KT. Neurological, cardiovascular and metabolic effects of mefloquine in healthy volunteers: a double‐blind, placebo‐controlled trial. British Journal of Clinical Pharmacology 1996;42(4):415‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eick‐Cost 2017 {published data only}
- Eick‐Cost A, Hu Z, Rohrbeck P, Clark L. Neuropsychiatric outcomes after mefloquine exposure among U.S. military service members. American Journal of Tropical Medicine and Hygiene 2017;96(1):159‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodyer 2011 {published data only}
- Goodyer L, Rice L, Martin A. Choice of and adherence to prophylactic antimalarials. Journal of Travel Medicine 2011;18(4):245‐9. [DOI] [PubMed] [Google Scholar]
Hale 2003 {published data only}
- Hale BR, Owusu‐Agyei S, Fryauff DJ, Koram KA, Adjuik M, Oduro AR, et al. A randomized, double‐blind, placebo‐controlled, dose‐ranging trial of tafenoquine for weekly prophylaxis against Plasmodium falciparum. Clinical Infectious Diseases 2003;36(5):541‐9. [DOI] [PubMed] [Google Scholar]
Hill 2000 {published data only}
- Hill DR. Health problems in a large cohort of Americans traveling to developing countries. Journal of Travel Medicine 2000;7(5):259‐66. [DOI] [PubMed] [Google Scholar]
Hoebe 1997 {published data only}
- Hoebe C, Munter J, Thijs C. Adverse effects and compliance with mefloquine or proguanil antimalarial chemoprophylaxis. European Journal of Clinical Pharmacology 1997;52(4):269‐75. [DOI] [PubMed] [Google Scholar]
Jute 2007 {published data only}
- Jute S, Toovey S. Knowledge, attitudes and practices of expatriates towards malaria chemoprophylaxis and personal protection measures on a mine in Mali. American Journal of Tropical Medicine and Hygiene 2007;5(1):40‐3. [DOI] [PubMed] [Google Scholar]
Kato 2013 {published and unpublished data}
- Kato T, Okuda J, Ide D, Amano K, Takei Y, Yamaguchi Y. Questionnaire‐based analysis of atovaquone‐proguanil compared with mefloquine in the chemoprophylaxis of malaria in non‐immune Japanese travelers. Journal of Infection and Chemotherapy 2013;19(1):20‐3. [DOI] [PubMed] [Google Scholar]
Korhonen 2007 {published and unpublished data}
- Korhonen C, Peterson K, Bruder C, Jung P. Self‐reported adverse events associated with antimalarial chemoprophylaxis in peace corps volunteers. American Journal of Preventine Medicine 2007;33(3):194‐9. [DOI] [PubMed] [Google Scholar]
Kuhner 2005 {published data only}
- Kuhner S, Drager‐Hoppe HS, Dreesman J. Malaria chemoprophylaxis ‐ A survey on drug‐related adverse events. Medizinische Welt 2005;56(1‐2):51‐5. [Google Scholar]
Landman 2015 {published data only}
- Landman KZ, Tan KR, Arguin PM. Adherence to malaria prophylaxis among Peace Corps volunteers in the Africa region, 2013. Travel Medicine and Infectious Disease 2015;13(1):61‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landman KZ, Tan KR, Arguin PM. Knowledge, attitudes, and practices regarding antimalarial chemoprophylaxis in U.S. Peace Corps volunteers ‐ Africa, 2013. Morbidity and Mortality Weekly Report 2014;63(23):516‐7. [PMC free article] [PubMed] [Google Scholar]
Laver 2001 {published data only}
- Laver SM, Wetzels J, Behrens RH. Knowledge of malaria, risk perception, and compliance with prophylaxis and personal and environmental preventive measures in travelers exiting Zimbabwe from Harare and Victoria Falls International airport. Journal of Travel Medicine 2001;8(6):298‐303. [DOI] [PubMed] [Google Scholar]
Laverone 2006 {published data only}
- Laverone E, Boccalini S, Bechini A, Belli S, Santini MG, Baretti S, et al. Travelers' compliance to prophylactic measures and behavior during stay abroad: Results of a retrospective study of subjects returning to a travel medicine center in Italy. Journal of Travel Medicine 2006;13(6):338‐44. [DOI] [PubMed] [Google Scholar]
Lobel 2001 {published data only}
- Lobel HO, Baker MA, Gras FA, Stennies GM, Meerburg P, Hiemstra E, et al. Use of malaria prevention measures by North American and European travelers to East Africa. Journal of Travel Medicine 2001;8(4):167‐72. [DOI] [PubMed] [Google Scholar]
Mavrogordato 2012 {published data only}
- Mavrogordato A, Lever AM. A cluster of Plasmodium vivax malaria in an expedition group to Ethiopia: Prophylactic efficacy of atovaquone/proguanil on liver stages of P. vivax. Journal of Infection 2012;65(3):269‐74. [DOI] [PubMed] [Google Scholar]
Meier 2004 {published data only}
- Meier CR, Wilcock K, Jick SS. The risk of severe depression, psychosis or panic attacks with prophylactic antimalarials. Drug Safety 2004;27(3):203‐13. [DOI] [PubMed] [Google Scholar]
Napoletano 2007 {published data only}
- Napoletano G, Bissoli P, Bisoffi Z, Todescato A, Gottardello L, Costa S, et al. Malaria chemoprophylaxis ‐ Follow up of returned travellers of Veneto Region, Italy. Giornale Italiano di Medicina Tropicale 2007;12(1‐4):13‐9. [Google Scholar]
Nosten 1994 {published data only}
- Nosten F, Ter Kuile F, Maelankiri L, Chongsuphajaisiddhi T, Nopdonrattakoon L, Tangkitchot S, et al. Mefloquine prophylaxis prevents malaria during pregnancy: A double‐blind, placebo‐controlled study. Journal of Infectious Diseases 1994;169(3):595‐603. [DOI] [PubMed] [Google Scholar]
Ohrt 1997 {published data only}
Overbosch 2001 {published data only}
- Overbosch D, Schilthuis H, Bienzle U, Behrens RH, Kain KC, Clarke PD, et al. Atovaquone‐proguanil versus mefloquine for malaria prophylaxis in nonimmune travelers: results from a randomized, double‐blind study. Clinical Infectious Diseases 2001;33(7):1015‐21. [DOI] [PubMed] [Google Scholar]
Pearlman 1980 {published data only}
- Pearlman EJ, Doberstyn EB, Sudsok S, Thiemanun W, Kennedy RS, Canfield CJ. Chemosuppressive field trials in Thailand. IV. The suppression of Plasmodium falciparum and Plasmodium vivax parasitemias by mefloquine (WR 142,490, A 4‐quinolinemethanol). Americal Journal of Tropical Medicine and Hygiene 1980;29(6):1131‐7. [PubMed] [Google Scholar]
Petersen 2000 {published data only}
- Petersen E, Ronne T, Ronn A, Bygbjerg I, Larsen SO. Reported side effects to chloroquine, chloroquine plus proguanil, and mefloquine as chemoprophylaxis against malaria in Danish travelers. Journal of Travel Medicine 2000;7(2):79‐84. [DOI] [PubMed] [Google Scholar]
Philips 1996 {published data only}
- Phillips MA, Kass RB. User acceptability patterns for mefloquine and doxycycline malaria chemoprophylaxis. Journal of Travel Medicine 1996;3(1):40‐5. [DOI] [PubMed] [Google Scholar]
Potasman 2002 {published data only}
- Potasman I, Weller B. Does mefloquine prophylaxis affect electroencephalographic patterns?. American Journal of Medicine 2002;112(2):147‐9. [DOI] [PubMed] [Google Scholar]
Rack 2005 {published data only}
- Rack J, Wichmann O, Kamara B, Gunther M, Cramer J, Schonfeld C, et al. Risk and spectrum of diseases in travelers to popular tourist destinations. Journal of Travel Medicine 2005;12(5):248‐53. [DOI] [PubMed] [Google Scholar]
Rieckmann 1993 {published data only}
- Rieckmann KH, Yeo AE, Davis DR, Hutton DC, Wheatley PF, Simpson R. Recent military experience with malaria chemoprophylaxis. Medical Journal of Australia 1993;158(7):446‐9. [DOI] [PubMed] [Google Scholar]
Rietz 2002 {published data only}
- Rietz G, Petersson H, Odenholt I. Many travellers suffer of side‐effects of malaria prophylaxis. Lakartidningen 2002;99(26‐7):2939‐44. [PubMed] [Google Scholar]
Salako 1992 {published data only}
- Salako LA, Adio RA, Walker O, Sowunmi A, Sturchler D, Mittelholzer ML, et al. Mefloquine‐sulphadoxine‐pyrimethamine (Fansimef, Roche) in the prophylaxis of Plasmodium falciparum malaria: A double‐blind, comparative, placebo‐controlled study. Annals of Tropical Medicine and Parasitology 1992;86(6):575‐81. [DOI] [PubMed] [Google Scholar]
Santos 1993 {published data only}
- Santos JB, Prata A, Wanssa E. Mefloquine chemoprophylaxis of malaria in the Brazilian Amazonia. Revista da Sociedade Brasileira de Medicina Tropical 1993;26(3):157‐62. [DOI] [PubMed] [Google Scholar]
Saunders 2015 {published data only}
- Saunders DL, Garges E, Manning JE, Bennett K, Schaffer S, Kosmowski AJ, et al. Safety, tolerability, and compliance with long‐term antimalarial chemoprophylaxis in American soldiers in Afghanistan. American Journal of Tropical Medicine and Hygiene 2015;93(3):584‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schlagenhauf 1997 {published data only}
- Schlagenhauf P, Lobel H, Steffen R, Johnson R, Popp K, Tschopp A, et al. Tolerance of mefloquine by SwissAir trainee pilots. American Journal of Tropical Medicine and Hygiene 1997;56(2):235‐40. [DOI] [PubMed] [Google Scholar]
Schlagenhauf 2003 {published data only}
- Schlagenhauf P, Johnson R, Schwartz E, Nothdurft HD, Steffen R. Evaluation of mood profiles during malaria chemoprophylaxis: a randomized, double‐blind, four‐arm study. Journal of Travel Medicine 2009;16(1):42‐45. [DOI] [PubMed] [Google Scholar]
- Schlagenhauf P, Tschopp A, Johnson R, Nothdurft HD, Beck B, Schwartz E, et al. Tolerability of malaria chemoprophylaxis in non‐immune travellers to sub‐Saharan Africa: multicentre, randomised, double blind, four arm study. BMJ 2003;327(7423):1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schneider 2013 {published data only}
- Schneider C, Adamcova M, Jick SS, Schlagenhauf P, Miller MK, Rhein HG, et al. Antimalarial chemoprophylaxis and the risk of neuropsychiatric disorders. Travel Medicine and Infectious Disease 2013;11(2):71‐80. [DOI] [PubMed] [Google Scholar]
- Schneider C, Adamcova M, Jick SS, Schlagenhauf P, Miller MK, Rhein HG, et al. Use of anti‐malarial drugs and the risk of developing eye disorders. Travel Medicine and Infectious Disease 2014;12(1):40‐7. [DOI] [PubMed] [Google Scholar]
Schwartz 1999 {published data only}
- Schwartz E, Regev‐Yochay G. Primaquine as prophylaxis for malaria for nonimmune travelers: A comparison with mefloquine and doxycycline. Clinical Infectious Diseases 1999;29(6):1502‐6. [DOI] [PubMed] [Google Scholar]
Shamiss 1996 {published data only}
- Shamiss A, Atar E, Zohar L, Cain Y. Mefloquine versus doxycycline for malaria prophylaxis in intermittent exposure of Israeli Air Force aircrew in Rwanda. Aviation, Space, and Environmental Medicine 1996;67(9):872‐3. [PubMed] [Google Scholar]
Sharafeldin 2010 {published data only}
- Sharafeldin E, Soonawala D, Vandenbroucke JP, Hack E, Visser LG. Health risks encountered by Dutch medical students during an elective in the tropics and the quality and comprehensiveness of pre‐and post‐travel care. BMC Medical Education 2010;10:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sonmez 2005 {published data only}
- Sonmez A, Harlak A, Kilic S, Polat Z, Hayat L, Keskin O, et al. The efficacy and tolerability of doxycycline and mefloquine in malaria prophylaxis of the ISAF troops in Afghanistan. Journal of Infectious Diseases 2005;51(3):253‐8. [DOI] [PubMed] [Google Scholar]
Sossouhounto 1995 {published data only}
- Sossouhounto RT, Soro BN, Coulibaly A, Mittelholzer ML, Stuerchler D, Haller L. Mefloquine in the prophylaxis of P. Falciparum malaria. Journal of Travel Medicine 1995;2(4):221‐4. [DOI] [PubMed] [Google Scholar]
Steffen 1993 {published data only}
- Handschin JC, Wall M, Steffen R, Sturchler D. Tolerability and effectiveness of malaria chemoprophylaxis with mefloquine or chloroquine with or without co‐medication. Journal of Travel Medicine 1997;4(3):121‐7. [DOI] [PubMed] [Google Scholar]
- Steffen R, Fuchs E, Schildknecht J, Naef U, Funk M, Schlagenhauf P, et al. Mefloquine compared with other malaria chemoprophylactic regimens in tourists visiting east Africa. Lancet 1993;341(8856):1299‐303. [DOI] [PubMed] [Google Scholar]
- Steffen R, Heusser R, Machler R, Bruppacher R, Naef U, Chen D, et al. Malaria chemoprophylaxis among European tourists in tropical Africa: use, adverse reactions, and efficacy. Bulletin of the World Health Organization 1990;68(3):313‐22. [PMC free article] [PubMed] [Google Scholar]
Steketee 1996 {published data only}
- Steketee RW, Wirima JJ, Hightower AW, Slutsker L, Heymann DL, Breman JG. The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity, and intrauterine growth retardation in rural Malawi. American Journal of Tropical Medicine and Hygiene 1996;55(Suppl 1):33‐41. [DOI] [PubMed] [Google Scholar]
- Steketee RW, Wirima JJ, Slutsker L, Breman JG, Heymann DL. Comparability of treatment groups and risk factors for parasitemia at the first antenatal clinic visit in a study of malaria treatment and prevention in pregnancy in rural Malawi. American Journal of Tropical Medicine and Hygiene 1996;55(Suppl 1):17‐23. [DOI] [PubMed] [Google Scholar]
- Steketee RW, Wirima JJ, Slutsker L, Khoromana CO, Heymann DL, Breman JG. Malaria treatment and prevention in pregnancy: Indications for use and adverse events associated with use of chloroquine or mefloquine. American Journal of Tropical Medicine and Hygiene 1996;55(Suppl 1):50‐6. [DOI] [PubMed] [Google Scholar]
- Steketee RW, Wirima JJ, Slutsker L, Roberts JM, Khoromana CO, Heymann DL, et al. Malaria parasite infection during pregnancy and at delivery in mother, placenta, and newborn: efficacy of chloroquine and mefloquine in rural Malawi. American Journal of Tropical Medicine and Hygiene 1996;55(Suppl 1):24‐32. [DOI] [PubMed] [Google Scholar]
- Steketee RW, Wirima JJ, Slutsker WL, Khoromana CO, Breman JG, Heymann DL. Objectives and methodology in a study of malaria treatment and prevention in pregnancy in rural Malawi: the Mangochi Malaria Research Project. American Journal of Tropical Medicine and Hygiene 1996;55(Suppl 1):8‐16. [DOI] [PubMed] [Google Scholar]
Stoney 2016 {published data only}
- Stoney RJ, Chen LH, Jentes ES, Wilson ME, Han PV, Benoit CM, et al. Malaria prevention strategies: adherence among Boston area travelers visiting malaria‐endemic countries. American Journal of Tropical Medicine and Hygiene 2016;94(1):136‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2017 {published data only}
- Tan KR, Henderson S, Williamson J, Ferguson RW, Wilkinson TM, Jung P, et al. Long term health outcomes among returned Peace Corps volunteers after malaria prophylaxis, 1995‐2014. Travel Medicine and Infectious Disease 2017;17:50‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Terrell 2015 {published data only}
- Terrell AG, Forde ME, Firth R, Ross DA. Malaria chemoprophylaxis and self‐reported impact on ability to work: mefloquine versus doxycycline. Journal of Travel Medicine 2015;22(6):383‐8. [DOI] [PubMed] [Google Scholar]
Tuck 2016 {published data only}
- Tuck J, Williams J. Malaria protection in Sierra Leone during the Ebola outbreak 2014/15; The UK military experience with malaria chemoprophylaxis Sep 14‐Feb 15. Travel Medicine and Infectious Diseases 2016;14(5):471‐4. [DOI] [PubMed] [Google Scholar]
van Riemsdijk 1997 {published data only}
- Riemsdijk MM, Klauw MM, Heest JA, Reedeker FR, Ligthelm RJ, Herings RM, et al. Neuro‐psychiatric effects of antimalarials. European Journal of Clinical Pharmacology 1997;52(1):1‐6. [DOI] [PubMed] [Google Scholar]
van Riemsdijk 2002 {published data only}
- Riemsdijk MM, Sturkenboom MC, Ditters JM, Ligthelm RJ, Overbosch D, Stricker BH. Atovaquone plus chloroguanide versus mefloquine for malaria prophylaxis: a focus on neuropsychiatric adverse events. Clinical Pharmacology and Therapeutics 2002;72(3):294‐301. [DOI] [PubMed] [Google Scholar]
Vuurman 1996 {published data only}
- Vuurman EF, Muntjewerff ND, Uiterwijk MM, Veggel LM, Crevoisier C, Haglund L, et al. Effects of mefloquine alone and with alcohol on psychomotor and driving performance. European Journal of Clinical Pharmacology 1996;50(6):475‐82. [DOI] [PubMed] [Google Scholar]
Waner 1999 {published data only}
- Waner S, Durrhiem D, Braack LE, Gammon S. Malaria protection measures used by in‐flight travelers to South African game parks. Journal of Travel Medicine 1999;6(4):254‐7. [DOI] [PubMed] [Google Scholar]
Weiss 1995 {published data only}
- Weiss WR, Oloo AJ, Johnson A, Koech D, Hoffman SL. Daily primaquine is effective for prophylaxis against falciparum malaria in Kenya: Comparison with mefloquine, doxycycline, and chloroquine plus proguanil. Journal of Infectious Disease 1995;171(6):1569‐75. [DOI] [PubMed] [Google Scholar]
Wells 2006 {published data only}
- Wells TS, Smith TC, Smith B, Wang LZ, Hansen CJ, Reed RJ, et al. Mefloquine use and hospitalizations among US service members, 2002‐2004. American Journal of Tropical Medicine and Hygiene 2006;74(5):744‐9. [PubMed] [Google Scholar]
References to studies excluded from this review
Abraham 1999 {published data only}
- Abraham C, Clift S, Grabowski P. Cognitive predicators of adherence to malaria prophylaxis regimens on return from a malarious region: protective study. Social Science and Medicine 1999;48(11):1641‐54. [DOI] [PubMed] [Google Scholar]
Adera 1995 {published data only}
- Adera T, Wolfe MS, McGuire‐Rugh K, Calhoun N, Marum L. Risk factors for malaria among expatriates living in Kampala, Uganda: The need for adherence to chemoprophylactic regimens. American Journal of Tropical Medicine and Hygiene 1995;52(3):207‐12. [DOI] [PubMed] [Google Scholar]
Adshead 2014 {published data only}
- Adshead S. The adverse effects of mefloquine in deployed military personnel. Journal of the Royal Naval Medical Service 2014;100(3):232‐7. [PubMed] [Google Scholar]
Angelin 2014 {published data only}
- Angelin M, Evengard B, Palmgren H. Travel health advice: Benefits, compliance, and outcome. Scandinavian Journal of Infectious Diseases 2014;46(6):447‐53. [DOI] [PubMed] [Google Scholar]
Anonymous 1991 {published data only}
- Anonymous. Mefloquine ‐ A new antimalarial. Drug and Therapeutics Bulletin 1991;29(13):51‐2. [PubMed] [Google Scholar]
Anonymous 1998 {published data only}
- Anonymous. Medication‐associated depression. WHO Drug Information 1998;12(2):81. [Google Scholar]
Anonymous 1998a {published data only}
- Anonymous. Mefloquine effectiveness impaired by high withdrawal rates. WHO Drug Information 1998;12(1):7‐8. [Google Scholar]
Anonymous 2005 {published data only}
- Anonymous. Mefloquine: Revised patient information. WHO Drug Information 2005;19(2):119. [Google Scholar]
Anonymous 2009 {published data only}
- Anonymous. Mefloquine: interstitial pneumonia: rare events. Prescrire International 2009;18(102):167. [PubMed] [Google Scholar]
Artaso 2004 {published data only}
- Artaso Irigoyen B, Langarica Eseverri M, Campos Mangas MC. Mefloquine‐induced acute psychosis. Psiquiatria Biologica 2004;11(4):164‐6. [Google Scholar]
Arthur 1990a {published data only}
- Arthur JD, Shanks GD, Echeverria P. Mefloquine prophylaxis. Lancet 1990;335(8695):972. [DOI] [PubMed] [Google Scholar]
Banerjee 2001 {published data only}
- Banerjee D, Stanley PJ. Malaria chemoprophylaxis in UK general practitioners traveling to South Asia. Journal of Travel Medicine 2001;8(4):173‐5. [DOI] [PubMed] [Google Scholar]
Barbero Gonzalez 2003 {published data only}
- Barbero Gonzalez A, Alvarez de Toledo Saavedra F, Esteban Fernandez J, Pastor‐Sanchez R, Gil de Miguel A, Rodriguez Barrios JM, et al. Management of vaccinations and prophylaxis of international travellers from community pharmacy (VINTAF Study). Atencion Primaria 2003;32(5):276‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barrett 1996 {published data only}
- Barrett PJ, Emmins PD, Clarke PD, Bradley DJ. Comparison of adverse events associated with use of mefloquine and combination of chloroquine and proguanil as antimalarial prophylaxis: postal and telephone survey of travelers. British Medical Journal 1996;313(7056):525‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berger 1998 {published data only}
- Berger A. Science commentary: protection against malaria. British Medical Journal 1998;317(7171):1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berman 2004 {published data only}
- Berman J. Toxicity of commonly‐used antimalarial drugs. Travel Medicine and Infectious Disease 2004;2(3‐4):171‐84. [DOI] [PubMed] [Google Scholar]
Bernado 1994 {published data only}
- Bernardo M, Parellada E. Mefloquine and severe psychiatric disorder. Medicina Clinica 1994;102(15):596. [PubMed] [Google Scholar]
Bijker 2014 {published data only}
- Bijker EM, Schats R, Obiero JM, Behet MC, Gemert GJ, Vegte‐Bolmer M, et al. Sporozoite immunization of human volunteers under mefloquine prophylaxis is safe, immunogenic and protective: a double‐blind randomized controlled clinical trial. PLoS ONE 2014;9(11):e112910. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjorkman 1991 {published data only}
- Bjorkman A, Steffen R, Armengaud M, Picot N, Piccoli S. Malaria chemoprophylaxis with mefloquine. Lancet 1991;337(8755):1479‐80. [DOI] [PubMed] [Google Scholar]
Black 2007 {published data only}
- Black J. Lariam and Halfan. Journal of the Royal Society of Medicine 2007;100(8):355‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blanke 2003 {published data only}
- Blanke CH. Increased malaria‐morbidity of long‐term travellers due to inappropriate chemoprophylaxis recommendations. Tropical Doctor 2003;33(2):117‐9. [DOI] [PubMed] [Google Scholar]
Botella de Maglia 1999 {published data only}
- Botella de Maglia J, Espacio Casanovas A. Prevention of malaria. Revista Clínica Española 1999;199(8):549‐50. [PubMed] [Google Scholar]
Bourgeade 1990 {published data only}
- Bourgeade A, Tonin V, Keudjian F, Levy PY, Faugere B. Accidental mefloquine poisoning. Presse Medicale 1990;19(41):1903. [PubMed] [Google Scholar]
Brenier‐Pinchart 2000 {published data only}
- Brenier‐Pinchart MP, Brion JP, Issartel B, Barro C, Pinel C, Ambroise‐Thomas P. Glucose‐6‐phosphate dehydrogenase deficiency and hemoglobinuric biliary fever after taking mefloquine. Presse Medicale 2000;29(3):142. [PubMed] [Google Scholar]
Brisson 2012 {published data only}
- Brisson M, Brisson P. Compliance with antimalaria chemoprophylaxis in a combat zone. American Journal of Tropical Medicine and Hygiene 2012;86(4):587‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruguera 2007 {published data only}
- Bruguera M, Herrera S. Acute hepatitis associated with mefloquine therapy. Gastroenterologie Hepatologie 2007;30(2):102‐3. [DOI] [PubMed] [Google Scholar]
Burke 1993 {published data only}
- Burke BM. Mefloquine. Lancet 1993;341(8860):1605‐6. [DOI] [PubMed] [Google Scholar]
Caillon 1992 {published data only}
- Caillon E, Schmitt L, Moron P. Acute depressive symptoms after mefloquine treatment. American Jounal of Psychiatry 1992;149(5):712. [DOI] [PubMed] [Google Scholar]
Carme 1997 {published data only}
- Carme B, Peguet C, Nevez G. Compliance with and tolerance of mefloquine and chloroquine + proguanil malaria chemoprophylaxis in French short‐term travellers to sub‐Saharan Africa. Tropical Medicine and International Health 1997;2(10):953‐6. [DOI] [PubMed] [Google Scholar]
- Carme B, Peguet C, Nevez G. Malaria chemoprophylaxis: tolerance and compliance with mefloquine and proguanil/chloroquine combination in French tourists. Bulletin de la Societe de Pathologie Exotique 1997;90(4):273‐6. [PubMed] [Google Scholar]
Castot 1988 {published data only}
- Castot A, Garnier R. The secondary effects of mefloquine. Concours Medical 1988;110(43):4003. [Google Scholar]
Cave 2003 {published data only}
- Cave W, Pandey P, Osrin D, Shlim DR. Chemoprophylaxis use and the risk of malaria in travelers to Nepal. Journal of Travel Medicine 2003;10(2):100‐5. [DOI] [PubMed] [Google Scholar]
Charles 2007 {published data only}
- Charles BG, Blomgren A, Nasveld PE, Kitchener SJ, Jensen A, Gregory RM, et al. Population pharmacokinetics of mefloquine in military personnel for prophylaxis against malaria infection during field deployment. European Journal of Clinical Pharmacology 2007;63(3):271‐8. [DOI] [PubMed] [Google Scholar]
Chin 2016 {published data only}
- Chin BS, Kim JY, Gianella S, Lee M. Travel pattern and prescription analysis at a single travel clinic specialized for yellow fever vaccination in South Korea. Infection and Chemotherapy 2016;48(1):20‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clifford 2009 {published data only}
- Clifford D, Brew B, Cinque P, Gorelik L, Bennett D, Panzara MA, et al. Design of a clinical trial of mefloquine in patients with progressive multifocal leukoencephalopathy. 25th Congress of the European Committee for Treatment and Research in Multiple Sclerosis; 2009 Sep 9‐12; Dusseldorf Germany. Dusseldorf, 2009:S87.
Clift 1996 {published data only}
- Clift S, Grabowski P. Malaria prophylaxis and the media. Lancet 1996;348(9023):344. [DOI] [PubMed] [Google Scholar]
Clyde 1976 {published data only}
- Clyde DF, McCarthy VC, Miller RM, Hornick RB. Suppressive activity of mefloquine in sporozoite‐induced human malaria. Antimicrobial Agents and Chemotherapy 1976;9(3):384‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cobelens 1997 {published data only}
- Cobelens FG, Thiel PP. There is no evidence of more symptoms with mefloquine than with other drugs in malaria prophylaxis. Nederlands Tijdschrift voor Geneeskunde 1997;141(16):794‐5; author reply 796. [PubMed] [Google Scholar]
Cohen 1997 {published data only}
- Cohen J. Mefloquine prophylaxis ‐ revisited. Australian Family Physician 1997;26(8):909. [PubMed] [Google Scholar]
Conget 1993 {published data only}
- Conget JJ, Navarro M, Navarro P, Corachan M. Prophylaxis with mefloquine and changes in thyroidal hormones. Medicina Clinica 1993;100(13):516. [PubMed] [Google Scholar]
Conrad 1997 {published data only}
- Conrad KA, Kiser WR. Response to doxycycline vs. mefloquine. Military Medicine 1997;162(6):iii. [PubMed] [Google Scholar]
Corbett 1996 {published data only}
- Corbett EL, Doherty JF, Behrens RH. Adverse events associated with mefloquine. Study in returned travelers confirms authors' findings. British Medical Journal 1996;313(7071):1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coulaud 1986 {published data only}
- Coulaud JP. Chemoprophylaxis of malaria. Medecine et Maladies Infectieuses 1986;16(12):746. [Google Scholar]
Croft 1996 {published data only}
- Croft AM, World MJ. Neuropsychiatric reactions with mefloquine chemoprophylaxis. Lancet 1996;347(8997):326. [DOI] [PubMed] [Google Scholar]
Croft 1997 {published data only}
- Croft AM, Clayton TC, World MJ. Side effects of mefloquine prophylaxis for malaria: an independent randomized controlled trial. Transactions of the Royal Society of Tropical Medicine and Hygiene 1997;91(2):199‐203. [DOI] [PubMed] [Google Scholar]
Del Cacho 2001 {published data only}
- Cacho Ma E, Martinez M, Tuset M, Biarnes C, Mejias T, Gascon J, et al. Advice program for travelers about antimalarial prohilaxis. Atencion Farmaceutica 2001;3(3):171‐6. [Google Scholar]
Dia 2010 {published data only}
- Dia A, Gautret P, Adheossi E, Bienaime A, Gaillard C, Simon F, et al. Illness in French travelers to Senegal: Prospective cohort follow‐up and sentinel surveillance data. Journal of Travel Medicine 2010;17(5):296‐302. [DOI] [PubMed] [Google Scholar]
Durrheim 1999 {published data only}
- Durrheim DN, Gammon S, Waner S, Braack LE. Antimalarial prophylaxis‐‐use and adverse events in visitors to the Kruger National Park. Suid‐Afrikaanse Tydskrif vir Geneeskunde 1999;89(2):170‐5. [PubMed] [Google Scholar]
Eamsila 1993 {published data only}
- Eamsila C, Singharaj P, Yooyen P, Chatnugrob P, Nopavong Na Ayuthya A, Webster HK, et al. Prevention of Plasmodium falciparum malaria by Fansimef and Lariam in the northeastern part of Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 1993;24(4):672‐6. [PubMed] [Google Scholar]
El Jaoudi 2010 {published data only}
- Jaoudi R, Benziane H, Khabbal Y, Elomri N, Lamsaouri J, Cherrah Y. Long‐term malaria prophylaxis with mefloquine: a study of adverse drug reactions. Therapie 2010;65(5):439‐45. [DOI] [PubMed] [Google Scholar]
Fernando 2016 {published data only}
- Fernando SD, Dharmawardana P, Semege S, Epasinghe G, Senanayake N, Rodrigo C, et al. The risk of imported malaria in security forces personnel returning from overseas missions in the context of prevention of re‐introduction of malaria to Sri Lanka. Malaria Journal 2016;15(1):144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fujii 2007 {published data only}
- Fujii T, Kaku K, Jelinek T, Kimura M. Malaria and mefloquine prophylaxis use among Japan ground self‐defense force personnel deployed in East Timor. Journal of Travel Medicine 2007;14(4):226‐32. [DOI] [PubMed] [Google Scholar]
Hamer 2008 {published data only}
- Hamer DH, Ruffing R, Callahan MV, Lyons SH, Abdullah AS. Knowledge and use of measures to reduce health risks by corporate expatriate employees in western Ghana. Journal of Travel Medicine 2008;15(4):237‐42. [DOI] [PubMed] [Google Scholar]
Hellgren 1990 {published data only}
- Hellgren U, Angel VH, Bergqvist Y, Arvidsson A, Forero‐Gomez J, Rombo L. Plasma concentrations of sulfadoxine‐pyrimethamine and of mefloquine during regular long term malaria prophylaxis. Transactions of the Royal Society of Tropical Medicine and Hygiene 1990;84(1):46‐9. [DOI] [PubMed] [Google Scholar]
Hopperus 1996 {published data only}
- Hopperus Buma AP, Thiel PP, Lobel HO, Ohrt C, Ameijden EJ, Veltink RL, et al. Long‐term malaria chemoprophylaxis with mefloquine in Dutch marines in Cambodia. Journal of Infectious Diseases 1996;173(6):1506‐9. [DOI] [PubMed] [Google Scholar]
Jaspers 1996 {published data only}
- Jaspers CA, Hopperus Buma AP, Thiel PP, Hulst RA, Kager PA. Tolerance of mefloquine chemoprophylaxis in Dutch military personnel. American Journal of Tropical Medicine and Hygiene 1996;55(2):230‐4. [DOI] [PubMed] [Google Scholar]
Jensen 1998 {published data only}
- Jensen JJ. Mefloquine: neuropsychiatric adverse effects are often severe and persistent long after withdrawal of the drug. Ugeskrift for Laeger 1998;160(16):2413. [PubMed] [Google Scholar]
Karbwang 1991 {published data only}
- Karbwang J, Molunto P, Bangchang KN, Banmairuroi V, Bunnag D, Harinasuta T. Pharmacokinetics of prophylactic mefloquine. Southeast Asian Journal of Tropical Medicine and Public Health 1991;22(4):519‐22. [PubMed] [Google Scholar]
Karbwang 1991a {published data only}
- Karbwang J, Bangchang KN, Supapojana A, Bunnag D, Harinasuta T. Pharmacokinetics of prophylactic mefloquine in Thai healthy volunteers. Southeast Asian Journal of Tropical Medicine and Public Health 1991;22(1):68‐71. [PubMed] [Google Scholar]
Khaliq 2001 {published data only}
- Khaliq Y, Gallicano K, Carignan CT, Cooper C, McCarthy A. Pharmacokinetic interaction between mefloquine and ritonavir in healthy volunteers. British Journal of Clinical Pharmacology 2001;51(6):591‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kimura 2006 {published data only}
- Kimura M, Kawakami K, Hashimoto M, Hamada M. Malaria prevention and stand‐by emergency treatment among Japanese travelers. Travel Medicine and Infectious Disease 2006;4(2):81‐5. [DOI] [PubMed] [Google Scholar]
Kitchener 2003 {published data only}
- Kitchener S, Nasveld P, Russell B, Elmes N. An outbreak of malaria in a forward battalion on active service in East Timor. Military Medicine 2003;168(6):457‐9. [PubMed] [Google Scholar]
Kitchener 2005 {published data only}
- Kitchener SJ, Nasveld PE, Gregory RM, Edstein MD. Mefloquine and doxycycline malaria prophylaxis in Australian soldiers in East Timor. Medical Journal of Australia 2005;182(4):168‐71. [DOI] [PubMed] [Google Scholar]
Kok 1997 {published data only}
- Kok PW, Puls FT, Zonderland HD. Not more symptoms with mefloquine use than with other drugs in malaria prophylaxis. Nederlands Tijdschrift Voor Geneeskunde 1997;141(18):898. [PubMed] [Google Scholar]
Kollaritsch 2000 {published data only}
- Kollaritsch H, Karbwang J, Wiedermann G, Mikolasek A, Na‐Bangchang K, Wernsdorfer WH. Mefloquine concentration profiles during prophylactic dose regimens. Wiener Klinische Wochenschrift 2000;112(10):441‐7. [PubMed] [Google Scholar]
Kozarsky 1993 {published data only}
- Kozarsky P, Eaton M. Use of mefloquine for malarial chemoprophylaxis in its first year of availability in the United States. Clinical Infectious Diseases 1993;16(1):185‐6. [DOI] [PubMed] [Google Scholar]
Landry 2006 {published data only}
- Landry P, Iorillo D, Darioli R, Burnier M, Genton B. Do travelers really take their mefloquine malaria chemoprophylaxis? Estimation of adherence by an electronic pillbox. Journal of Travel Medicine 2006;13(1):8‐14. [DOI] [PubMed] [Google Scholar]
Lapierre 1983 {published data only}
- Lapierre J, Devant J, Coquelin B, Faurant C, Galal AA. Results of an experiment on chemoprophylaxis of malaria using mefloquine in Cambodia (Cambodia‐Thai border region). Bulletin de la Societe de Pathologie Exotique et de ses Filiales 1983;76(4):357‐63. [PubMed] [Google Scholar]
Lim 2005 {published data only}
- Lim DS. Dermatology in the military: An East Timor study. International Journal of Dermatology 2005;44(4):304‐11. [DOI] [PubMed] [Google Scholar]
Lobel 1993 {published data only}
- Lobel HO, Bernard KW, Williams SL, Hightower AW, Patchen LC, Campbell C. Effectiveness and tolerance of long‐term malaria prophylaxis with mefloquine. Need for a better dosing regimen. JAMA 1991;265(3):361‐4. [PubMed] [Google Scholar]
- Lobel HO, Miani M, Eng T, Bernard KW, Hightower AW, Campbell CC. Long‐term malaria prophylaxis with weekly mefloquine. Lancet 1993;341(8849):848‐51. [DOI] [PubMed] [Google Scholar]
Looareesuwan 1987 {published data only}
- Looareesuwan S, White NJ, Warrell DA, Forgo I, Schwartz DE, et al. Studies of mefloquine bioavailability and kinetics using a stable isotope technique: comparison of Thai patients with falciparum malaria and healthy Caucasian volunteers. British Journal of Clinical Pharmacology 1987;24(1):37‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacArthur 2002 {published data only}
- MacArthur JR, Parise ME, Steketee RW. Relationships between mefloquine blood levels, gender, and adverse reactions. American Journal of Tropical Medicine and Hygiene 2002;66(5):445; author reply 446‐7. [DOI] [PubMed] [Google Scholar]
Malvy 2006 {published data only}
- Malvy D, Pistone T, Rezvani A, Lancon F, Vatan R, Receveur MC, et al. Risk of malaria among French adult travellers. Travel Medicine and Infectious Disease 2006;4(5):259‐69. [DOI] [PubMed] [Google Scholar]
Marcy 1996 {published data only}
- Marcy SM, Wilson ME. Malaria prophylaxis in young children and pregnant women. Pediatric Infectious Disease Journal 1996;15(1):101‐2. [Google Scholar]
Massey 2007 {published data only}
- Massey P, Durrheim DN, Speare R. Inadequate chemoprophylaxis and the risk of malaria. Australian Family Physician 2007;36(12):1058‐60. [PubMed] [Google Scholar]
Matsumura 2005 {published data only}
- Matsumura T, Fujii T, Miura T, Koibuchi T, Endo T, Nakamura H, et al. Questionnaire‐based analysis of mefloquine chemoprophylaxis for malaria in a Japanese population. Journal of Infection and Chemotherapy 2005;11(4):196‐8. [DOI] [PubMed] [Google Scholar]
Meszaros 1996 {published data only}
- Meszaros K. Acute psychosis caused by mefloquine prophylaxis?. Canadian Journal of Psychiatry 1996;41(3):196. [PubMed] [Google Scholar]
Michel 2007 {published data only}
- Michel R, Ollivier L, Meynard JB, Guette C, Migliani R, Boutin JP. Outbreak of malaria among policemen in French Guiana. Military Medicine 2007;172(9):977‐81. [DOI] [PubMed] [Google Scholar]
Mimica 1983 {published data only}
- Mimica I, Fry W, Eckert G, Schwartz DE. Multiple‐dose kinetic study of mefloquine in healthy male volunteers. Chemotherapy 1983;29(3):184‐7. [DOI] [PubMed] [Google Scholar]
Mizuno 2006 {published data only}
- Mizuno Y, Kudo K, Kano S. Chemoprophylaxis according to the guidelines on malaria prevention for Japanese overseas travellers. Southeast Asian Journal of Tropical Medicine and Public Health 2006;37(Suppl 3):11‐4. [PubMed] [Google Scholar]
Mizuno 2010 {published data only}
- Mizuno Y, Kudo K, Kano S. Mefloquine chemoprophylaxis against malaria in Japanese travelers: Results of a study on adverse effects. Tropical Medicine and Health 2010;38(3):103‐6. [Google Scholar]
Moon 2011 {published data only}
- Moon J, Deye G, Miller L, Fracisco S, Miller RS, Tosh D, et al. Malaria infection in individuals taking mefloquine does not induce antibody response to MSP142. 58th Annual Meeting of the American Society of Tropical Medicine and Hygiene; 2009 November 18‐22; Washington, USA. Washington, USA: American Journal of Tropical Medicine and Hygiene, 2009; Vol. 81:156‐7.
- Moon JE, Deye GA, Miller L, Fracisco S, Miller RS, Tosh D, et al. Plasmodium falciparum infection during suppressive prophylaxis with mefloquine does not induce an antibody response to merozoite surface protein‐1(42). American Journal of Tropical Medicine and Hygiene 2011;84(5):825‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morales de Naime 1989 {published data only}
- Morales de Naime L, Kosidub H, Martínez Iturriza L. Prophylactic malaria with pyrimethamine, sulfadoxine and mefloquine [Paludismo tratamiento profiláctico con pirimetamina, sulfadoxina y mefloquina]. Medicina Interna 1989;5(3‐4):125‐37. [Google Scholar]
Munawar 2012 {published data only}
- Munawar CM, Khan TP, Hyder MF. Effect of mefloquine on eye. Pakistan Journal of Medical and Health Sciences 2012;6(2):340‐2. [Google Scholar]
Mølle 2000 {published data only}
- Mølle I, Christensen KL, Hansen PS, Dragsted UB, Aarup M, Mads Buhl R. Use of medical chemoprophylaxis and antimosquito precautions in Danish malaria patients and their traveling companions. Journal of Travel Medicine 2000;7(5):253‐8. [DOI] [PubMed] [Google Scholar]
Namikawa 2008 {published data only}
- Namikawa K, Kikuchi H, Kato S, Takizawa Y, Konta A, Iida T, et al. Knowledge, attitudes, and practices of Japanese travelers towards malaria prevention during overseas travel. Travel Medicine and Infectious Disease 2008;6(3):137‐41. [DOI] [PubMed] [Google Scholar]
Nasveld 2010 {published data only}
- Dow GS, McCarthy WF, Reid M, Smith B, Tang D, Shanks GD. A retrospective analysis of the protective efficacy of tafenoquine and mefloquine as prophylactic anti‐malarials in non‐immune individuals during deployment to a malaria‐endemic area. Malaria Journal 2014;13(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasveld PE, Edstein MD, Reid M, Brennan L, Harris IE, Kitchener SJ, et al. Randomized, double‐blind study of the safety, tolerability, and efficacy of tafenoquine versus mefloquine for malaria prophylaxis in nonimmune subjects. Antimicrobial Agents and Chemotherapy 2010;54(2):792‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nevin 2010 {published data only}
- Nevin RL. Mefloquine prescriptions in the presence of contraindications: Prevalence among US military personnel deployed to Afghanistan, 2007. Pharmacoepidemiology and Drug Safety 2010;19(2):206‐10. [DOI] [PubMed] [Google Scholar]
Nevin 2012 {published data only}
- Nevin RL. Biased measurement of neuropsychiatric adverse effects of pediatric mefloquine treatment. Pediatric Infectious Diseases Journal 2012;31(1):102; author reply 102‐3. [DOI] [PubMed] [Google Scholar]
Nosten 1990 {published data only}
- Nosten F, Karbwang J, White NJ, Honeymoon, Na Bangchang K, Bunnag D, et al. Mefloquine antimalarial prophylaxis in pregnancy: dose finding and pharmacokinetic study. British Journal of Clinical Pharmacology 1990;30(1):79‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nosten 1999 {published data only}
- Nosten F, Vincenti M, Simpson J, Yei P, Thwai KL, Vries A, et al. The effects of mefloquine treatment in pregnancy. Clinical Infectious Diseases 1999;28(4):808‐15. [DOI] [PubMed] [Google Scholar]
Nwokolo 2001 {published data only}
- Nwokolo C, Wambebe C, Akinyanju O, Raji AA, Audu BS, Emodi IJ, et al. Mefloquine versus proguanil in short‐term malaria chemoprophylaxis in sickle cell anaemia. Clinical Drug Investigation 2001;21(8):537‐44. [Google Scholar]
Olanrewaju 2000 {published data only}
- Olanrewaju I W, Lin L. Mefloquine chemoprophylaxis in Chinese railway workers on contract in Nigeria. Journal of Travel Medicine 2000;7(3):116‐9. [DOI] [PubMed] [Google Scholar]
Ollivier 2004 {published data only}
- Ollivier L, Tifratene K, Josse R, Keundjian A, Boutin JP. The relationship between body weight and tolerance to mefloquine prophylaxis in non‐immune adults: results of a questionnaire‐based study. Annals of Tropical Medicine and Parasitology 2004;98(6):639‐41. [DOI] [PubMed] [Google Scholar]
Peetermans 2001 {published data only}
- Peetermans WE, Wijngaerden E. Implementation of pretravel advice: Good for malaria, bad for diarrhoea. Acta Clinica Belgica 2001;56(5):284‐8. [DOI] [PubMed] [Google Scholar]
Peragallo 1999 {published data only}
- Peragallo MS, Sabatinelli G, Sarnicola G. Compliance and tolerability of mefloquine and chloroquine plus proguanil for long‐term malaria chemoprophylaxis in groups at particular risk (the military). Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93(1):73‐7. [DOI] [PubMed] [Google Scholar]
Peragallo 2002 {published data only}
- Peragallo MS, Croft AM, Kitchener SJ. Malaria during a multinational military deployment: the comparative experience of the Italian, British and Australian Armed Forces in East Timor. Transactions of the Royal Society of Tropical Medicine and Hygiene 2002;96(5):481‐2. [DOI] [PubMed] [Google Scholar]
Peragallo 2014 {published data only}
- Peragallo MS, Sarnicola G, Boccolini D, Romi R, Mammana G. Risk assessment and prevention of malaria among Italian troops in Afghanistan, 2002 to 2011. Journal of Travel Medicine 2014;21(1):24‐32. [DOI] [PubMed] [Google Scholar]
Philips 1994 {published data only}
- Phillips M. Antimalarial mefloquine. Medical Journal of Australia 1994;161(3):227‐8. [DOI] [PubMed] [Google Scholar]
Phillips 1996 {published data only}
- Phillips M. Adverse events associated with mefloquine. Women may be more susceptible to adverse events. British Medical Journal 1996;313(7071):1552‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Phillips‐Howard 1998 {published data only}
- Phillips‐Howard PA, Steffen R, Kerr L, Vanhauwere B, Schildknecht J, Fuchs E, et al. Safety of mefloquine and other antimalarial agents in the first trimester of pregnancy. Journal Travel Medicine 1998;5(3):121‐6. [DOI] [PubMed] [Google Scholar]
Pistone 2007 {published data only}
- Pistone T, Guibert P, Gay F, Malvy D, Ezzedine K, Receveur MC, et al. Malaria risk perception, knowledge and prophylaxis practices among travellers of African ethnicity living in Paris and visiting their country of origin in sub‐Saharan Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 2007;101(10):990‐5. [DOI] [PubMed] [Google Scholar]
Port 2011 {published data only}
- Port A, Cottrell G, Dechavanne C, Briand V, Bouraima A, Guerra J, et al. Prevention of malaria during pregnancy: assessing the effect of the distribution of IPTp through the national policy in Benin. American Journal of Tropical Medicine and Hygiene 2011;84(2):270‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Potasman 2000 {published data only}
- Potasman I, Beny A, Seligmann H. Neuropsychiatric problems in 2,500 long‐term young travelers to the tropics. Journal of Travel Medicine 2000;7(1):5‐9. [DOI] [PubMed] [Google Scholar]
Quinn 2016 {published data only}
- Quinn JC. Better approach needed to detect and treat military personnel with adverse effects from mefloquine. BMJ 2016;352:i838. [DOI] [PubMed] [Google Scholar]
Reisinger 1989 {published data only}
- Reisinger EC, Horstmann RD, Dietrich M. Tolerance of mefloquine alone and in combination with sulfadoxine‐pyrimethamine in the prophylaxis of malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1989;83(4):474‐7. [DOI] [PubMed] [Google Scholar]
Rieckmann 1974 {published data only}
- Rieckmann KH, Trenholme GM, Williams RL, Carson PE, Frischer H, Desjardins RE. Prophylactic activity of mefloquine hydrochloride (WR 142490) in drug‐resistant malaria. Bulletin of the World Health Organization 1974;51(4):375‐7. [PMC free article] [PubMed] [Google Scholar]
Rieke 1993 {published data only}
- Rieke B, Fleischer K. Permanent health impairment after staying in malaria areas. Versicherungsmedizin 1993;45(6):197‐202. [PubMed] [Google Scholar]
Ries 1993 {published data only}
- Ries S. Cerebral spasm during malaria prophylaxis with mefloquine. Deutsche Medizinische Wochenschrift 1993;118(51‐2):1911‐2. [PubMed] [Google Scholar]
Ringqvist 2015 {published data only}
- Ringqvist A, Bech P, Glenthøj B, Petersen E. Acute and long‐term psychiatric side effects of mefloquine: a follow‐up on Danish adverse event reports. Travel Medicine and Infectious Disease 2015;13(1):80‐8. [DOI] [PubMed] [Google Scholar]
Rombo 1993 {published data only}
- Rombo L, Angel VH, Friman G, Hellgren U, Mittelholzer ML, Sturchler D. Comparative tolerability and kinetics during long‐term intake of Lariam and Fansidar for malaria prophylaxis in nonimmune volunteers. Tropical Medicine and Parasitology 1993;44(3):254‐6. [PubMed] [Google Scholar]
Rønn 1998 {published data only}
- Rønn AM, Rønne‐Rasmussen J, Gøtzsche PC, Bygbjerg IC. Neuropsychiatric manifestations after mefloquine therapy for Plasmodium falciparum malaria: comparing a retrospective and a prospective study. Tropical Medicine and International Health 1998;3(2):83‐8. [DOI] [PubMed] [Google Scholar]
Sallent 1997 {published data only}
- Sallent LV. Anti‐malarial prophylaxis: The role of the general practitioner. Atencion Primaria 1997;20(10):558‐62. [PubMed] [Google Scholar]
Schlagenhauf 1996 {published data only}
- Schlagenhauf P, Steffen R, Lobel H, Johnson R, Letz R, Tschopp A, et al. Mefloquine tolerability during chemoprophylaxis: focus on adverse event assessments, stereochemistry and compliance. Tropical Medicine and International Health 1996;1(4):485‐94. [DOI] [PubMed] [Google Scholar]
Scott 1993 {published data only}
- Scott R. Malaria chemoprophylaxis. South African Medical Journal 1993;83(11):861. [PubMed] [Google Scholar]
Smail 1991 {published data only}
- Smail A, Ducroix JP, Cohen G, Baillet J. Current malaria prophylactic therapy for travellers servicemen. La Semaine des Hopitaux de Paris 1991;67(40‐41):1824‐7. [Google Scholar]
Smoak 1997 {published data only}
- Smoak BL, Writer JV, Keep LW, Cowan J, Chantelois JL. The effects of inadvertent exposure of mefloquine chemoprophylaxis on pregnancy outcomes and infants of US Army servicewomen. Journal of Infectious Disease 1997;176(3):831‐3. [DOI] [PubMed] [Google Scholar]
Suriyamongkol 1991 {published data only}
- Suriyamongkol V, Timsaad S, Shanks GD. Mefloquine chemoprophylaxis of soldiers on the Thai‐Cambodian border. Southeast Asian Journal of Tropical Medicine and Public Health 1991;22(4):515‐8. [PubMed] [Google Scholar]
Tansley 2010 {published data only}
- Tansley R, Lotharius J, Priestley A, Bull F, Duparc S, Mohrle J. A randomized, double‐blind, placebo‐controlled study to investigate the safety, tolerability, and pharmacokinetics of single enantiomer (+)‐mefloquine compared with racemic mefloquine in healthy persons. American Journal of Tropical Medicine and Hygiene 2010;83(6):1195‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
ter Kuile 1993 {published data only}
- ter Kuile FO, Nosten F, Luxemburger C, White NJ. Mefloquine prophylaxis. Lancet 1993;342(8870):551. [DOI] [PubMed] [Google Scholar]
Todd 1997 {published data only}
- Todd GD, Hopperus Buma AP, Green MD, Jaspers CA, Lobel HO. Comparison of whole blood and serum levels of mefloquine and its carboxylic acid metabolite. American Journal of Tropical Medicine and Hygiene 1997;57(4):399‐402. [DOI] [PubMed] [Google Scholar]
Turner 2014 {published data only}
- Turner C, Sabin C, Chiodini P, Bhagani S, Johnson M, Zuckerman J. Cross‐sectional study investigating the prescription, adherence and tolerability of malaria prophylaxis in HIV‐positive travellers. 3rd Joint Conference of the British HIV Association, BHIVA with the British Association for Sexual Health and HIV, BASHH Liverpool United Kingdom; 2014 April 1‐4; Liverpool, UK. Liverpool, UK: HIV Medicine, 2014; Vol. 15:127.
Valerio 2005 {published data only}
- Valerio L, Martinez O, Sabria M, Esteve M, Urbiztondo L, Roca C. High‐risk travel abroad overtook low‐risk travel from 1999 to 2004: Characterization and trends in 2,622 Spanish travelers. Journal of Travel Medicine 2005;12(6):327‐31. [DOI] [PubMed] [Google Scholar]
Van Genderen 2007 {published data only}
- Genderen PJ, Koene HR, Spong K, Overbosch D. Atovaquone‐proguanil versus mefloquine for malaria prophylaxis in nonimmune travelers: Results from a randomized, double‐blind study. Journal of Travel Medicine 2007;14(2):92‐5. [Google Scholar]
Van Grootheest 1999 {published data only}
- Grootheest AC, Puijenbroek EP, Heeringa M. Adverse effects of mefloquine: Agitation undermines objective assessment. Pharmaceutisch Weekblad 1999;134(4):114‐6. [Google Scholar]
van Riemsdijk 2004 {published data only}
- Aarnoudse AL, Schaik RH, Dieleman J, Molokhia M, Riemsdijk MM, Ligthelm RJ, et al. MDR1 gene polymorphisms are associated with neuropsychiatric adverse effects of mefloquine. Clinical Pharmacology and Therapeutics 2006;80(4):367‐74. [DOI] [PubMed] [Google Scholar]
- Riemsdijk MM, Ditters JM, Sturkenboom MC, Tulen JH, Ligthelm RJ, Overbosch D, et al. Neuropsychiatric events during prophylactic use of mefloquine before travelling. British Journal of Clinical Pharmacology 2002;58(6):441‐5. [DOI] [PubMed] [Google Scholar]
- Riemsdijk MM, Sturkenboom MC, Ditters JM, Tulen JH, Ligthelm RJ, Overbosch D, et al. Low body mass index is associated with an increased risk of neuropsychiatric adverse events and concentration impairment in women on mefloquine. British Journal of Clinical Pharmacology 2004;57(4):506‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Venturini 2011 {published data only}
- Venturini E, Chiappini E, Mannelli F, Bonsignori F, Galli L, Martino M. Malaria prophylaxis in African and Asiatic children traveling to their parents' home country: A Florentine study. Journal of Travel Medicine 2011;18(3):161‐4. [DOI] [PubMed] [Google Scholar]
Wagner 1986 {published data only}
- Wagner WH. Fight against malaria ‐ chemotherapy and immunoprophylaxis. Part 1. Chemotherapy. Arzneimittel Forschung 1986;36(1):1‐9. [PubMed] [Google Scholar]
Wallace 1996 {published data only}
- Sánchez JL, DeFraites RF, Sharp TW, Hanson RK. Mefloquine or doxycycline prophylaxis in US troops in Somalia. Lancet 1993;341(8851):1021‐2. [DOI] [PubMed] [Google Scholar]
- Wallace MR. Malaria among United States troops in Somalia. American Journal of Medicine 1996;100(1):49‐55. [DOI] [PubMed] [Google Scholar]
Weinke 1991 {published data only}
- Weinke T, Trautmann M, Held T, Weber G, Eichenlaub D, Fleischer K, et al. Neuropsychiatric side effects after the use of mefloquine. American Journal of Tropical Medicine and Hygiene 1991;45(1):86‐91. [DOI] [PubMed] [Google Scholar]
White 2016 {published data only}
- White C. UK troops to continue to receive mefloquine despite concern over adverse events. BMJ 2016;354:i5030. [DOI] [PubMed] [Google Scholar]
Win 1985 {published data only}
- Win K, Thwe Y, Lwin TT, Win K. Combination of mefloquine with sulfadoxine‐pyrimethamine compared with two sulfadoxine‐pyrimethamine combinations in malaria chemoprophylaxis. Lancet 1985;2(8457):694‐5. [DOI] [PubMed] [Google Scholar]
Winstanley 1999 {published data only}
- Winstanley P, Behrens R. Malaria prophylaxis with mefloquine: Neurological and psychiatric adverse drug reactions. Prescribers' Journal 1999;39(3):161‐5. [Google Scholar]
Wolters 1997 {published data only}
- Wolters BA, Bosje T, Luinstra‐Passchier MJ. Not more problems with mefloquine compared to other antimalarial prophylactics. Nederlands Tijdschrift voor Geneeskunde 1997;141(7):331‐4. [PubMed] [Google Scholar]
Additional references
ACROBAT‐NSRI tool
- Sterne JAC, Higgins JPT, Reeves BC on behalf of the development group for ACROBAT‐NRSI. A Cochrane Risk Of Bias Assessment Tool: for Non‐Randomized Studies of Interventions (ACROBAT‐NRSI). Version 1.0.0 [September 2014]. Available from: http://www.riskofbias.info [Accessed September 2017].
Behrens 2015
- Behrens R, Neave P, Jones P. Imported malaria among people who travel to visit friends and relatives: is current UK policy effective or does it need a strategic change?. Malaria Journal 2015;14:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Briand 2009
- Briand V, Bottero J, Noël H, Masse V, Cordel H, Guerra J, et al. Intermittent treatment for the prevention of malaria during pregnancy in Benin: a randomized, open‐label equivalence trial comparing sulfadoxine‐pyrimethamine with mefloquine. Journal of Infectious Diseases 2009;200(6):991‐1001. [DOI] [PubMed] [Google Scholar]
Bukiwra 2014
- Bukirwa H, Unnikrishnan B, Kramer CV, Sinclair D, Nair S, Tharyan P. Artesunate plus pyronaridine for treating uncomplicated Plasmodium falciparum malaria. Cochrane Database of Systematic Reviews 2014, Issue 3. [DOI: 10.1002/14651858.CD006404.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2015a
- Centers for Disease Control and Prevention. Malaria biology. 2015. www.cdc.gov/malaria/about/biology (accessed September 2017).
CDC 2015b
- Centers for Disease Control and Prevention. Drugs for malaria prevention table. Travelers' health. 2015. Yellow book. wwwnc.cdc.gov/travel/diseases/malaria (accessed September 2017).
Covidence 2017 [Computer program]
- Veritas Health Innovation. Covidence. Version accessed prior to 4 October 2017. Melbourne, Australia: Veritas Health Innovation, 2017.
Croft 2005
- Croft AM. Malaria: prevention in travellers. BMJ Clinical Evidence 2010;2010:0903. [PMC free article] [PubMed] [Google Scholar]
EMA 2014
- European Medicines Agency. PRAC recommendations on signals adopted at the PRAC meeting of 3‐6 March 2014. EMA/PRAC/65788/2014. ema.europa.eu/docs/en_GB/document_library/PRAC_recommendation_on_signal/2014/03/WC500163626.pdf (accessed prior to 19 September 2017).
eMC 2015a
- electronic Medicines Compendium. Summary of product characteristics: Larium. medicines.org.uk/emc/medicine/1701#UNDESIRABLE_EFFECTS 2015 (accessed September 2017).
eMC 2015b
- electronic Medicines Compendium. Glossary. medicines.org.uk/emc/glossary/#SPC 2015 (accessed September 2017).
FDA 2013
- USA Food, Drug Administration. FDA drug safety communication: mefloquine. fda.gov/drugs/drugsafety/ucm362227.htm 2013 (accessed September 2017).
González 2014
- González R, Hellgren U, Greenwood B, Menéndez C. Mefloquine safety and tolerability in pregnancy: a systematic literature review. Malaria Journal 2014;13:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
González 2014a
- González R, Mombo‐Ngoma G, Ouédraogo S, Kakolwa MA, Abdulla S, Accrombessi M, et al. Intermittent preventive treatment of malaria in pregnancy with mefloquine in HIV‐negative women: a multicentre randomized controlled trial. PLoS Medicine 2014;11(9):e1001733. [DOI] [PMC free article] [PubMed] [Google Scholar]
Handschin 1997
- Handschin JC, Wall M, Steffen R, Stürchler D. Tolerability and effectiveness of malaria chemoprophylaxis with mefloquine or chloroquine with or without co‐medication. Journal of Travel Medicine 1997;4(3):121‐7. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 [updated March 2011]. http://training.cochrane.org/handbook. The Cochrane Collaboration, 2011. Available at www.cochrane‐handbook.org, (accessed prior to 19 September 2017).
Høgh 2000
- Høgh B, Clarke PD, Camus D, et al. Atovaquone‐proguanil versus chloroquine‐proguanil for malaria prophylaxis in non‐immune travellers: a randomised, double‐blind study. Lancet 2000;356:1888‐94. [DOI] [PubMed] [Google Scholar]
ICH 1994
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). Clinical safety data management: definitions and standards for expedited reporting E2A. 1994. ICH harmonised tripartite guideline. https://www.imim.cat/media/upload/arxius/MEDIA436.pdf (accessed prior to 19 September 2017).
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. training.cochrane.org/handbook (accessed prior to 19 September 2017).
Loke 2007
- Loke YK, Price D, Herxheimer A. Systematic reviews of adverse effects: framework for a structured approach. BMC Medical Research Methodology 2007;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Loke 2011
- Loke YK, Price D, Herxheimer A. Chapter 14: Adverse effects. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 [updated March 2011]. training.cochrane.org/handbook. The Cochrane Collaboration, 2011. Available at www.cochrane‐handbook.org, (accessed prior to 19 September 2017).
McCarthy 2015
- McCarthy S. Malaria prevention, mefloquine neurotoxicity, neuropsychiatric illness, and risk‐benefit analysis in the Australian Defence Force. Journal of Parasitology Research 2015;2015:287651. [DOI: 10.1155/2015/287651] [DOI] [PMC free article] [PubMed] [Google Scholar]
MedDRA 2016
- Medical Dictionary for Regulatory Activities. Introductory guide MedDRA version 19.0. 2016. International Federation of Pharmaceutical Manufacturers and Associations. meddra.org/sites/default/files/guidance/file/intguide_19_0_english.pdf (accessed September 2017).
Meremikwu 2008
- Meremikwu MM, Donegan S, Esu E. Chemoprophylaxis and intermittent treatment for preventing malaria in children. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD003756.pub3] [DOI] [PubMed] [Google Scholar]
Muanda 2015
- Muanda FT, Chaabane S, Boukhris T, Santos F, Sheehy O, Perreault S, et al. Antimalarial drugs for preventing malaria during pregnancy and the risk of low birthweight: a systematic review and meta‐analysis of randomized and quasi‐randomized trials. BMC Medicine 2015;13:193. [DOI: 10.1186/s12916-015-0429-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 2014
- Murray CJ, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384(9947):1005‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nevin 2015
- Nevin R. Rational risk‐benefit decision‐making in the setting of military mefloquine policy. Journal of Parasitology Research 2015;2015:260106. [DOI: 10.1155/2015/260106] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oniyangi 2006
- Oniyangi O, Omari AA. Malaria chemoprophylaxis in sickle cell disease. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD003489.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
PHAC 2014
- Public Health Agency of Canada. Canadian recommendations for the prevention and treatment of malaria. Canada Communicable Disease Report. 2014. publications.gc.ca/collections/collection_2014/aspc‐phac/HP40‐102‐2014‐eng.pdf (accessed September 2017).
PHE 2015
- Public Health England Advisory Committee for Malaria Prevention for UK Travellers. Guidelines for malaria prevention in travellers from the UK. 2015. gov.uk/government/publications/malaria‐prevention‐guidelines‐for‐travellers‐from‐the‐uk (accessed September 2017).
Radeva‐Petrova 2014
- Radeva‐Petrova D, Kayentao K, ter Kuile F, Sinclair D, Garner P. Drugs for preventing malaria in pregnant women in endemic areas: any drug regimen versus placebo or no treatment. Cochrane Database of Systematic Reviews 2014, Issue 10. [DOI: 10.1002/14651858.CD000169.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reeves 2011
- Reeves BC, Deeks JJ, Higgins JPT, Wells GA. Chapter 13: Including non‐randomized studies. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 [updated March 2011]. training.cochrane.org/handbook (accessed prior to 19 September 2017).
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rodrigo 2016
- Rodrigo C, Rajapakse S, Fernando S. Primaquine or tafenoquine for preventing malaria in people travelling to or living in endemic areas. Cochrane Database of Systematic Reviews 2016, Issue 6. [DOI: 10.1002/14651858.CD012242] [DOI] [Google Scholar]
Schlagenhauf 2003
- Schlagenhauf P, Tschopp A, Johnson R, Nothdurft HD, Beck B, Schwartz E, et al. Tolerability of malaria chemoprophylaxis in non‐immune travellers to sub‐Saharan Africa: multicentre, randomised, double blind, four arm study. BMJ 2003;327(7423):1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schlagenhauf 1999
- Schlagenhauf P. Mefloquine for malaria chemoprophylaxis 1992‐1998: a review. Journal of Travel Medicine 1999;6(2):122‐33. [DOI] [PubMed] [Google Scholar]
Schlagenhauf 2010
- Schlagenhauf P, Adamcova M, Regep L, Schaerer MT, Rhein HG. The position of mefloquine as a 21st century malaria chemoprophylaxis. Malaria Journal 2010;9:357. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shanks 2005
- Shanks GD, Edstein MD. Modern malaria chemoprophylaxis. Drugs 2005;65(12):2091‐110. [DOI] [PubMed] [Google Scholar]
Tickell‐Painter 2017
Treiber 2010
- Treiber M, Wernsdorfer G, Wiedermann U, Congpuong K, Wernsdorfer WH. Sensitivity to artemisinin, mefloquine and quinine of Plasmodium falciparum in northwestern Thailand. Wiener Klinische Wochenschrift 2010;122(Suppl 3):52‐6. [DOI] [PubMed] [Google Scholar]
Treiber 2011
- Treiber M, Wernsdorfer G, Wiedermann U, Congpuong K, Sirichaisinthop J, Wernsdorfer WH. Sensitivity of Plasmodium vivax to chloroquine, mefloquine, artemisinin and atovaquone in north‐western Thailand. Wiener Klinische Wochenschrift 2011;123(Suppl 1):20‐5. [DOI] [PubMed] [Google Scholar]
UK Parliament 2016
- UK Parliament 2016. Commons select committee, UK Parliament. 'Larium should be 'drug of last resort' for troops'. parliament.uk/business/committees/committees‐a‐z/commons‐select/defence‐committee/news‐parliament‐2015/lariam‐report‐published‐16‐17/ (accessed September 2017).
Warrell 2002
- Warrell D, Gilles H. Essential Malariology. 4th Edition. New York: CRC Press, 2002. [Google Scholar]
WHO 2015
- World Health Organization. Guidelines for the treatment of malaria. 2015. who.int/malaria/publications/atoz/9789241549127/en/ (accessed September 2017).
WHO 2016
- World Health Organization. World malaria report 2016. http://www.who.int/malaria/publications/world‐malaria‐report‐2016/en/ (accessed September 2017).
WHO 2017
- World Health Organization. Malaria, International travel and health. Chapter 7. who.int/ith/2017‐ith‐chapter7.pdf?ua=1 2017 (accessed 19 September 2017).
WHO‐ART 2008
- Uppsala Monitoring Centre. WHO adverse reaction terminology (WHO‐ART). https://www.who‐umc.org/vigibase/services/learn‐more‐about‐who‐art/ (accessed prior to 19 September 2017).
References to other published versions of this review
Jacquerioz 2007
- Jacquerioz FA, Croft AM. Drugs for preventing malaria in travellers. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD006491] [DOI] [PubMed] [Google Scholar]
Jacquerioz 2009
- Jacquerioz FA, Croft AM. Drugs for preventing malaria in travellers. Cochrane Database of Systematic Reviews 2009, Issue 10. [DOI: 10.1002/14651858.CD006491.pub2] [DOI] [PubMed] [Google Scholar]
Jacquerioz 2015
- Jacquerioz FA, Croft AM. Drugs for preventing malaria in travellers. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD006491.pub3] [DOI] [PubMed] [Google Scholar]


