Abstract
Objectives
Episodes of agitation are frequent in intoxicated patients who have a substance use disorder, a psychiatric disorder or both (dual diagnosis). For managing the agitation, it is necessary to act promptly in a safe environment and addressing any underlying etiology. Inhaled loxapine improves symptoms of agitation in adults with psychiatric disorders (eg, schizophrenia) within 10 minutes of administration. Recently, some reports have documented the usefulness of loxapine in dual diagnoses patients with agitation. However, the efficacy of loxapine in intoxicated patients has not been deeply addressed.
Methods
This report describes a case series of 12 patients (with addiction or dual disorder) who received inhaled loxapine for symptoms of psychomotor agitation during intoxication with different substances (eg, alcohol, cannabis, or cocaine) at 1 center in Spain.
Results
Data from 12 patients were reviewed, 5 patients were attended at the emergency room, 4 at the addiction and dual diagnosis unit, and 3 were treated during hospitalization for detoxification. All patients were under effects of substances. They had substance use disorder (including cannabis, cocaine, alcohol, hypnotics, and hallucinogens), and almost all (90%) presented 1 or more psychiatric disorders. One dose of inhaled loxapine was effective in 9 patients (75%), and in 3 patients, a second dose was required. Only mild dizziness was reported in 1 patient after the second dose.
Conclusions
The acute agitation was effectively and quickly managed with inhaled loxapine in all intoxicated patients and enabled the appropriate clinical evaluation of the agitated state and the patient's management.
Key Words: agitation, inhaled loxapine, emergency, substance use disorders, mental disorders
Substance use disorders (SUDs) and psychiatric disorders (or even both diagnoses, namely dual diagnosis) are a frequent factor for agitation episodes in intoxicated patients.1–5 Substance intoxication is one of the main etiologies of psychomotor agitation according to several expert consensus.4,6,7 Intoxicated patients in a state of psychomotor agitation are common users of emergency departments. Their management includes providing a safe environment, managing agitation to enable appropriate clinical evaluation of the agitated state, and addressing the underlying etiology.
To allow a safe management of the agitated patient is necessary a “quick intervention,” including nonpharmacological and pharmacological strategies.8 Pharmacological treatment consists in achieving patient's tranquilization and includes mainly benzodiazepines or antipsychotics, which are chosen depending on the absence or presence of psychotic symptoms.3 Low doses of neuroleptics are recommended for intoxications in agitated patients with history of alcohol and sedative use, whereas benzodiazepines are preferred if there is a suspicion of substance intoxication other than alcohol (eg, with amphetamines, cocaine, or phencyclidine).3 Nevertheless, antipsychotics are preferred over benzodiazepines for patients with a known psychiatric disorder (schizophrenia, schizoaffective disorder, bipolar disorder), because they address the underlying disease.3,5
There are few data on the use of antipsychotics, other than haloperidol, for agitation secondary to intoxication in patients with underlying psychiatric pathology.3,5,9 New intramuscular formulations for antipsychotics provide faster effect, but they are invasive and are not well received by most of the patients.10 The most frequent complications of rapid tranquilization depend on the pharmacologic profile but also can derive from the interactions with other addictive substances or the existence of subjacent diseases.9 Thus, complications from sedatives reside in their long duration of action and the risk of lethality in overdose, especially when they are combined with other medications or alcohol.3 On the other hand, the use of antipsychotics may result in extrapyramidal adverse effects, QTc prolongation, arrhythmias, potential serotonin syndrome, and neuroleptic malignant syndrome.11 Furthermore, antipsychotics can also reduce the seizure threshold and should be used with caution in patients who are prone to seizures (including patients undergoing alcohol or sedative-hypnotic withdrawal)12 and not to mention that antipsychotics are related to metabolic syndrome.13 Hence, there is a need for treatments with a good safety profile and low drug interactions, with fast onset but enough duration of action, easy to administer, and nontraumatic.7
As a new alternative, inhaled loxapine has demonstrated to reduce mild to moderate agitation in 10 minutes in patients with schizophrenia or bipolar disorder.14–16 Response rates observed with inhaled loxapine were similar to those observed with the intramuscular administration of other antipsychotics.17 Inhaled loxapine may have a role in the treatment of substance-induced agitation, but data on the use of inhaled loxapine in intoxicated patients are lacking.18 Recently, a case series of 14 agitated patients with dual diagnosis has been described; 4 patients presented an intoxication state and were treated with inhaled loxapine (9.1 mg) for symptoms of agitation. Inhaled loxapine was rapid, effective, and well accepted in all patients presenting with acute agitation and facilitated the cooperation of the patient and an adequate management of the disease.19 Although, it is important to point out that inhaled loxapine was used as off-label in that report, as has been used in other diagnoses such as borderline personality disorder.20
The current report aims to extend the experience with inhaled loxapine to 12 intoxicated patients attending the emergency service and the addiction and dual diagnosis unit at 1 center in Spain. All patients had a SUD, and almost all patients had an underlying psychiatric disorder. Inhaled loxapine was used to treat agitation.
CASES
Cases include 12 patients in an intoxicated state and were treated with inhaled loxapine; those patients were attended at the emergency room (ER) (n = 5), at the addiction and dual diagnosis unit (n = 4), or during hospitalization for detoxification (n = 3) at the Hospital of Vall de Hebron in Barcelona, Spain, from December 2014 to April 2016.
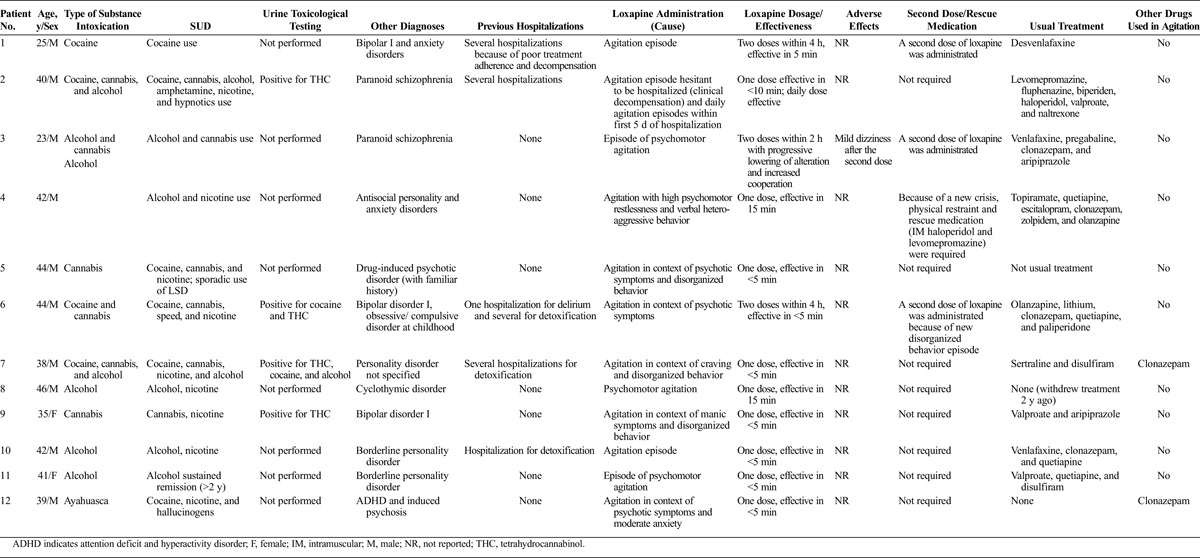
All patients presented a SUD, namely nicotine (n = 9; 75.0%), alcohol (n = 7; 58.3%), cannabis (n = 6; 50.0%), cocaine (n = 6; 50.0%), and others (amphetamines [n = 2; 16.7%], hypnotics [n = 1; 8.3%], and hallucinogens [n = 1; 8.3%]). Almost all (9/10; 90%) presented 1 or more psychiatric disorders according to Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, including personality disorder (n = 4; 33.3%), bipolar I disorder (n = 3; 25%), schizophrenia (n = 2; 16.7%), psychotic disorder (n = 1; 8.3%), cyclothymic disorder (n = 1; 8.3%), or anxiety disorder (n = 2; 16.7%). Patients presented at the center in a state of substance intoxication due to alcohol (n = 7; 58.3%), cannabis (n = 6; 50.0%), cocaine (n = 4; 33.3%), or ayahuasca (n = 1; 8.3%), which was confirmed by urine toxicological testing in 4 patients (Table 1). One dose of inhaled loxapine was effective in 9 patients (75%) within 5 to 15 minutes after administration (<5 minutes in 8 patients; 66.7%). In 3 patients (no. 1, no. 3, and no. 6), a second dose was required between 2 and 4 hours after the first one. Clonazepam treatment was started concomitantly with loxapine for the agitation episode, because of the appearance of abstinence or anxiety, in 2 patients (no. 7 and no. 12). A third patient (no. 4) required physical restraint and rescue medication (intramuscular haloperidol and levomepromazine). No other rescue medication was needed during the acute episodes of agitation. Only mild dizziness was reported in 1 patient after the second dose. A daily dose of loxapine was effective for the treatment of daily agitation episodes during the first 5 days of hospitalization in 1 patient (no. 2).
TABLE 1.
Patient Characteristics and Treatment Response
Vital signs and other parameters were monitored during the medical intervention according to the hospital protocol for agitation. No alterations were detected on vital signs or other hemodynamic parameters.
DISCUSSION
To date, there are scarce clinical data on the use of inhaled loxapine in intoxicated patients because usually intoxication or having a positive drug screening was exclusion criteria in clinical trials that evaluated inhaled loxapine as treatment for agitation. The current study constitutes a report on the effectiveness and safety of inhaled loxapine in patients presenting with agitation during substance-related intoxication.
Inhaled loxapine was well received by the patient and reduced the perception of coercion or forced medication, enabling the patient's cooperation. In most cases, only 1 dose was needed to calm the patients, which was effective within minutes in a considerable proportion of them. A 66.7% (n = 8) of patients did not require an additional dose (n = 3, 25%) or rescue medication (n = 1) within 24 hours. These rates are comparable with those reported in the clinical trials with inhaled loxapine in patients with schizophrenia (60.9%) or bipolar disorders (61.5%).15,16 A regimen with a benzodiazepine was initiated, concomitantly with inhaled loxapine, in 2 cases. After control of acute agitation symptoms, patients received regular treatment immediately, and in these 2 cases, clonazepam was deemed the most appropriate treatment for their underlying disorder. The advantages of inhaled loxapine over the antipsychotic medication used traditionally reside in the route of administration, which is equivalent to the intravenous and faster than the intramuscular one but has better tolerability and is more patient friendly. Inhaled loxapine was well tolerated in these case series, and there were no reporting of respiratory signs/symptoms.
The most prevalent substances used were alcohol, cannabis, and cocaine use (apart from tobacco), and these were the most consumed substances causing intoxication. There is plenty of published literature on the abuse of cocaine,21 alcohol,22 or cannabis23 as correlated to agitation episodes in patients with SUD and dual diagnosis and represent a major public health problem and a cause of concern in the emergency and outpatient facilities.24
For a better management of the patient, it is important to determine what specific substances the patient have been consuming, and the use of urine (or blood) toxicology screening tests is an important aid at the ER.25 However, the results of the test screening are not always a determining factor, and the substance might not be detectable through the routine analysis.2 In the current study, the substance intoxication was detectable in 4 cases, but it was not assessed in the other 8 cases because of several reasons (the patient referred active consumption at admission, or the urine sampling was not feasible). Specific clinical signs and symptoms are also helpful, particularly psychomotor agitation is frequent in patients with stimulant intoxication (induced by cocaine or amphetamine) or alcohol-intoxicated patients, and in these patients, the use of a neuroleptic is recommended.
This article should be analyzed focusing in limitations, especially because it is a small case series and the use of inhaled loxapine as off-label in some cases. Nevertheless, the use of some medications as off-label in psychiatry and SUD is frequent26 and inhaled loxapine has been administered as off-label in some reports, for example in borderline personality disorder20 and in dual diagnoses patients.21 Finally, effectiveness was not evaluated with a standard instrument but only with clinical assessment (considering tranquilization and use of additional medication or doses).
Conclusively, inhaled loxapine would have a role in agitation related to substance intoxication, especially in dual diagnosis patients, improving cooperation and outcomes at the ER. Therefore, we may comment (and recommend) that this medication is a useful tool in drug users who are agitated and intoxicated at the same time. Although, usual contraindications of this medication have always to be taken into consideration (eg, respiratory diseases). These case series are illustrative of the real world at the emergency and psychiatric services and substantiate the effectiveness and safety of inhaled loxapine for treating agitation, enabling the appropriate clinical evaluation of the agitated state and the adequate management of the intoxicated patients attended at our hospital. Studies with a higher sample of intoxicated patients who consume different and multiple types of drugs are needed to better characterize the potential interactions of loxapine.
Footnotes
Conflicts of Interest and Source of Funding: Carlos Roncero has received fees to give lectures for Janssen-Cilag, Ferrer-Brainfarma, Pfizer, Indivior, Lundbeck, Otsuka, Servier, GSK, Rovi, Astra, Gilead, MSD, Sanofi, and Exeltis. He has received financial compensation for his participation as a board member of Janssen-Cilag, Lundbeck, Gilead, MSD, Indivior, and Mundipharma. He has carried out the PROTEUS project, which was funded by a grant from Reckitt-Benckiser/Indivior. He received a medical education grant for Gilead.
Dr Ros-Cucurull has received fees to give talks for Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Lilly, Servier, Rovi, and Juste. She has received financial compensation for projects with Lundbeck, Esteve, Pfizer, Rovi, Exeltis, and Servier. She has received financial compensation for her participation as a board member of Janssen-Cilag. She has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict.
Dr Palma-Álvarez has received fees to give talks for Mundipharma and Exeltis.
Dr Abad has no conflicts of interest.
Dr Fadeuilhe has received fees to gives talks for Ferrer and Otsuka.
Dr Casas has received fees to give talks for Janssen-Cilag, Bristol-Mayers Squibb, Ferrer-Brainfarma, Pfizer, Reckitt-Benckiser, Lundbeck, Otsuka, Servier, Lilly, Shire, GSK, Rovi, and Adamed. He has received financial compensation for his participation as a member of the Janssen-Cilag, Lilly, Shire, Lundbeck, Otsuka, Ferrer, and Rovi board. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Dr Grau-López has received fees to give talks for Janssen-Cilag, Lundbeck, Servier, Otsuka, and Pfizer.
An unrestricted grant for medical writing assistance (A. Del Campo, Pivotal SL) was provided by Ferrer International.
REFERENCES
- 1.MacDonald K, Wilson MP, Minassian A, et al. A retrospective analysis of intramuscular haloperidol and intramuscular olanzapine in the treatment of agitation in drug- and alcohol-using patients. Gen Hosp Psychiatry 2010;32(4):443–445. [DOI] [PubMed] [Google Scholar]
- 2.Weaver MF, Hopper JA, Gunderson EW. Designer drugs 2015: assessment and management. Addict Sci Clin Pract 2015;10:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the american association for emergency psychiatry project Beta psychopharmacology workgroup. West J Emerg Med 2012;13(1):26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nordstrom K, Zun LS, Wilson MP, et al. Medical evaluation and triage of the agitated patient: consensus statement of the american association for emergency psychiatry project Beta medical evaluation workgroup. West J Emerg Med 2012;13(1):3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothschild AJ. Substance-related psychomotor agitation. In: Rothschild AJ, ed. The Evidence-Based Guide to Antipsychotic Medications. Washington, DC: American Psychiatric Publishing Inc; 2010:125–143. [Google Scholar]
- 6.Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series. Treatment of behavioral emergencies. Postgrad Med 2001; (Spec No):1–88. [PubMed] [Google Scholar]
- 7.Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatry 2016;17(2):86–128. [DOI] [PubMed] [Google Scholar]
- 8.Nordstrom K, Allen MH. Alternative delivery systems for agents to treat acute agitation: progress to date. Drugs 2013;73(16):1783–1792. [DOI] [PubMed] [Google Scholar]
- 9.Gudin JA, Mogali S, Jones JD, et al. Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgrad Med 2013;125(4):115–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson MP, Minassian A, Bahramzi M, et al. Despite expert recommendations, second-generation antipsychotics are not often prescribed in the emergency department. J Emerg Med 2014;46(6):808–813. [DOI] [PubMed] [Google Scholar]
- 11.Stanniland C, Taylor D. Tolerability of atypical antipsychotics. Drug Saf 2000;22(3):195–214. [DOI] [PubMed] [Google Scholar]
- 12.Haddad PM, Dursun SM. Neurological complications of psychiatric drugs: clinical features and management. Hum Psychopharmacol 2008;23(Suppl 1):15–26. [DOI] [PubMed] [Google Scholar]
- 13.Ko YK, Soh MA, Kang SH, et al. The prevalence of metabolic syndrome in schizophrenic patients using antipsychotics. Clin Psychopharmacol Neurosci 2013;11(2):80–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen MH, Feifel D, Lesem MD, et al. Efficacy and safety of loxapine for inhalation in the treatment of agitation in patients with schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2011;72(10):1313–1321. [DOI] [PubMed] [Google Scholar]
- 15.Kwentus J, Riesenberg RA, Marandi M, et al. Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord 2012;14(1):31–40. [DOI] [PubMed] [Google Scholar]
- 16.Lesem MD, Tran-Johnson TK, Riesenberg RA, et al. Rapid acute treatment of agitation in individuals with schizophrenia: multicentre, randomised, placebo-controlled study of inhaled loxapine. Br J Psychiatry 2011;198(1):51–58. [DOI] [PubMed] [Google Scholar]
- 17.Citrome L. Aerosolised antipsychotic assuages agitation: inhaled loxapine for agitation associated with schizophrenia or bipolar disorder. Int J Clin Pract 2011;65(3):330–340. [DOI] [PubMed] [Google Scholar]
- 18.de Berardis D, Fornaro M, Orsolini L, et al. The role of inhaled loxapine in the treatment of acute agitation in patients with psychiatric disorders: a clinical review. Int J Mol Sci 2017;18(2):pii: E349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roncero C, Ros-Cucurull E, Grau-Lopez L, et al. Effectiveness of inhaled loxapine in dual-diagnosis patients: a case series. Clin Neuropharmacol 2016;39(4):206–209. [DOI] [PubMed] [Google Scholar]
- 20.Kahl KG, Negt P, Wollmer A, et al. Inhaled loxapine for acute treatment of agitation in patients with borderline personality disorder: a case series. J Clin Psychopharmaco 2015;35(6):741–743. [DOI] [PubMed] [Google Scholar]
- 21.Roncero C, Daigre C, Grau-López L, et al. An international perspective and review of cocaine-induced psychosis: a call to action. Subst Abus 2014;35(3):321–327. [DOI] [PubMed] [Google Scholar]
- 22.Verelst S, Moonen PJ, Desruelles D, et al. Emergency department visits due to alcohol intoxication: characteristics of patients and impact on the emergency room. Alcohol Alcohol 2012;47(4):433–438. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JM, Wu CY, Winder GS, et al. The effects of cannabis on inpatient agitation, aggression, and length of stay. J Dual Diagn 2016;12(3–4):244–251. [DOI] [PubMed] [Google Scholar]
- 24.Mena G, Giraudon I, Álvarez E, et al. Cocaine-related health emergencies in Europe: a review of sources of information, trends and implications for service development. Eur Addict Res 2013;19(2):74–81. [DOI] [PubMed] [Google Scholar]
- 25.Bagøien G, Morken G, Zahlsen K, et al. Evaluation of a urine on-site drugs of abuse screening test in patients admitted to a psychiatric emergency unit. J Clin Psychopharmacol 2009;29(3):248–254. [DOI] [PubMed] [Google Scholar]
- 26.Barral C, Ros-Cucurull E, Roncero C. Off-label prescription in dual diagnosis [article in Spanish]. Revista de Patología Dual 2014;1(3):10 Available at http://www.patologiadual.es/profesional_revista.html. [Google Scholar]


