ABSTRACT
Introduction
Hockey Fans in Training (Hockey FIT) is a gender-sensitized weight loss and healthy lifestyle program. We investigated 1) feasibility of recruiting and retaining overweight and obese men into a pilot pragmatic randomized controlled trial and 2) potential for Hockey FIT to lead to weight loss and improvements in other outcomes at 12 wk and 12 months.
Methods
Male fans of two ice hockey teams (35–65 yr; body mass index ≥28 kg·m−2) located in Ontario (Canada) were randomized to intervention (Hockey FIT) or comparator (wait-list control). Hockey FIT includes a 12-wk active phase (weekly, coach-led group meetings including provision of dietary information, practice of behavior change techniques, and safe exercise sessions plus incremental pedometer walking) and a 40-wk minimally supported phase (smartphone app for sustaining physical activity, private online social network, standardized e-mails, booster session/reunion). Measurement at baseline and 12 wk (both groups) and 12 months (intervention group only) included clinical outcomes (e.g., weight) and self-reported physical activity, diet, and self-rated health.
Results
Eighty men were recruited in 4 wk; trial retention was >80% at 12 wk and >75% at 12 months. At 12 wk, the intervention group lost 3.6 kg (95% confidence interval, −5.26 to −1.90 kg) more than the comparator group (P < 0.001) and maintained this weight loss to 12 months. The intervention group also demonstrated greater improvements in other clinical measures, physical activity, diet, and self-rated health at 12 wk; most sustained to 12 months.
Conclusions
Results suggest feasible recruitment/retention of overweight and obese men in the Hockey FIT program. Results provide evidence for the potential effectiveness of Hockey FIT for weight loss and improved health in at-risk men and, thus, evidence to proceed with a definitive trial.
Key Words: MEN’S HEALTH, OVERWEIGHT/OBESITY, LIFESTYLE INTERVENTION, PHYSICAL ACTIVITY, HEALTH PROMOTION, WEIGHT LOSS
The worldwide prevalence of overweight (defined as a body mass index (BMI) of 25.0–29.9 kg·m−2) and obesity (defined as a BMI of ≥30.0 kg·m−2) is high and continuing to increase (25). It has been projected that there will be 65 million more obese adults in the United States by 2030, which also translates to increased rates of many preventable chronic diseases and increased economic burden (41). In 2011, the combined medical costs associated with treatment of chronic diseases resulting from obesity were estimated to increase by $48–66 billion per year in the United States alone (41).
In 2009–2010, the prevalence of overweight and obesity combined in the United States was disproportionately higher in middle-age men compared with women of the same age (79.5% in men vs 66% in women 40–59 yr of age) (11). In Canada in 2011, the national prevalence of overweight and obesity in adults (age, ≥18 yr) was also higher in men compared with women (overweight, 40.1% in men vs 27.1% in women; obese, 19.5% in men vs 17.1% in women) (39). A recent meta-analysis including studies from four different continents provides additional evidence for increased burden in men where results showed that men had higher all-cause mortality for every additional five BMI points greater than 25 kg·m−2 (relative to 22.5 to <25 kg·m−2) compared with women (35).
Excess body weight is a risk factor for chronic diseases including Type 2 diabetes, cardiovascular disease, osteoarthritis, and cancer (18). Physical inactivity and poor diet are associated with obesity and are key risk factors contributing to chronic disease burden (3). Health care costs associated with obesity increase significantly when combined with other lifestyle or behavioral risk factors, including physical inactivity (1). Furthermore, evidence suggests that poor diet is the lifestyle risk factor that contributes the most economic burden (33).
Interventions combining physical activity (PA), diet, and behavior change techniques have the strongest evidence for long-term weight change in men (30). Unfortunately, men are a hard-to-reach population who are often underrepresented in lifestyle weight loss interventions (26). Factors attracting men to participate in chronic disease prevention and management programs (i.e., lifestyle, weight management, or health promotion programs) include a group component with like-minded men, the presence of some form of competition, the use of humor to discuss sensitive health issues, and the inclusion of both dietary and PA components (12). Recent research has further supported the need to tailor programs to men to improve uptake and effectiveness (31). Research has shown that men may be more willing to participate in PA that is linked to sport, athleticism, and competition (4). Directly in line with these findings, studies have shown that weight management interventions situated in professional sports settings have been highly successful in men (4,16,20). These settings are traditionally male-dominated environments, which may help to offset the threat that “weight management” may pose to men’s identities or “masculine capital” (6), and can engage men through a strong sense of affiliation as a fan (19).
Hockey is an important part of Canadian culture; two-thirds of adult Canadians follow the game as a fan and 80% of Canadians identify hockey as a key part of what it means to be Canadian (24). In many areas, particularly small towns, amateur hockey (i.e., Major Junior hockey) is the primary fan base and often a rallying point in the community (24). Hockey Fans in Training (Hockey FIT) is a novel, gender-sensitized weight loss and healthy lifestyle program that engages men through being a fan of Major Junior hockey in Canada. Hockey FIT was adapted from Football Fans in Training (FFIT) (16,20) and then integrated with components of the HealtheStepsTM lifestyle prescription program, including eHealth technology support tools such as an online social network platform including only group members and their coaches (13).
In the current study, our primary objective was to examine the feasibility of recruiting and retaining men in Hockey FIT and the acceptability of the research procedures. Although there is strong evidence from FFIT that affiliation with professional football clubs provides a powerful draw to engage men in a lifestyle change program, it was unclear whether the same would be true with hockey in a North American setting. We hypothesized that 1) it would be feasible to recruit and retain men who are overweight or obese into the Hockey FIT program, and 2) trial procedures would be acceptable to most men. Secondary objectives were to determine the potential for Hockey FIT (vs control) to lead to weight loss and improvements in other health behaviors and health-related outcomes by 12 wk and whether improvements could be retained 12 months later. We hypothesized that Hockey FIT would lead to weight loss and improvements in health behaviors and other health-related outcomes in the short term, and that these improvements would be maintained in the longer term—providing support for the potential effectiveness of the Hockey FIT program.
METHODS
Trial Design
The full study protocol has been published elsewhere (14). Briefly, we conducted a pilot, pragmatic randomized controlled trial (pRCT; parallel groups, stratified by site) in Ontario, Canada. Eighty male fans of two ice hockey teams from the Ontario Hockey League (40 men from each of London and Sarnia) were recruited and randomized to either intervention (Hockey FIT) or comparator (wait-list control). Follow-up occurred at 12 wk (both groups) and 12 months (intervention group only to explore the sustainability of long-term change). Western University’s Health Sciences Research Ethics Board approved this study, and all participants provided written informed consent. The trial was registered on February 26, 2015, with ClinicalTrials.gov (identifier: NCT02396524).
Participants and Setting
Recruitment occurred using a variety of methods (e.g., hockey team e-mail blasts and social media accounts, study Web site (http://hockeyfansintraining.org/), posters, traditional media advertisements, word of mouth, direct contact at team arena). Eligible participants were male 35–65 yr old with a BMI of ≥28 kg·m−2 and met PA safety requirements (i.e., no risk indicated by the Physical Activity Readiness Questionnaire [36] or clearance from a health care provider). Age and BMI restrictions reflect evidence suggesting the following: 1) overweight/obese men in their mid-30s may experience an attitudinal shift in relation to their health, increasing their receptiveness to change health behaviors, and 2) men who are obese or at risk for becoming obese are more likely to want to lose weight (16). We used a pragmatic approach for the program venue at each site, using a combination of the hockey team’s arena and an affiliated health club facility.
Intervention Group: Hockey FIT Program
Overview
In the development of Hockey FIT, specific adaptations to FFIT included modifying program content to the North American context (e.g., language used in relation to education on healthy eating) and to hockey in particular (e.g., for the exercise component, off-ice hockey-related drills and conditioning exercises were incorporated). Components from HealtheStepsTM that were integrated into Hockey FIT included the following: 1) lifestyle prescriptions for healthy eating, PA (i.e., steps) and exercise, with the latter involving a simple fitness test that provided men with a target heart rate for exercise, and 2) eHealth technologies including the private and customizable online social network platform and the HealtheStepsTM smartphone app designed to help participants maintain their PA and exercise goals in the long term.
Twelve-week active phase
The Hockey FIT program was delivered over 12 weekly, 90-min sessions by Hockey FIT coaches (coach to participant ratio 2:20) from the central research team (see Gill et al. [14] for information on coach background and training). Program sessions comprised the following: 1) classroom-based teaching of behavior change techniques and simple information sharing on PA and healthy eating, delivered to encourage participant interaction and mutual learning, and 2) exercise sessions where men performed aerobic, strength, and flexibility exercises, incorporating their passion for hockey off the ice. Sessions were designed to appeal to men; they included elements of friendly competition and encouraged banter, humor, and peer support.
At the start of the program, more time was allocated to classroom education, but as the program progressed, more time was spent on group-based exercise. Twice throughout the program, participants completed the validated Step Test and Exercise Prescription to receive a personalized target heart rate to strive for during aerobic activities (22). In addition to the weekly in-person sessions, participants took part in an incremental pedometer-based walking program and they both set and tracked lifestyle prescriptions for PA (steps), exercise, and healthy eating. Incentives were also provided as part of the program to encourage program attendance and engagement (e.g., free promotional materials from hockey teams and attendance raffle for hockey-related prizes held during session 12).
Forty-week minimally supported phase
Participants were encouraged to continue with their lifestyle prescriptions and sustain their behavior changes with the support of free-of-charge eHealth tools: 1) HealtheSteps smartphone app providing tools to track and sustain PA (www.healthesteps.ca) and 2) Hockey FIT social network, a secure Web-based network tailored to each site and including only group members and coaches. Six standardized messages were sent using the online social network and by e-mail, to provide encouragement to sustain healthy lifestyle behaviors. A group reunion and booster session was held at month 9, where participants were invited to take part in a 60-min booster session and to attend a London Knights versus Sarnia Sting hockey game.
Comparator Group: Wait-List Control
Men were instructed to continue with usual daily activities without any restrictions from the research team and with minimal intervention (i.e., only contacted to schedule 12-wk measurements). Men were invited to start the Hockey FIT program at their respective sites after all 12-wk measurements were completed, approximately 4 months after the intervention group began the Hockey FIT program.
Feasibility and Acceptability
To address the feasibility of recruitment and retention, we examined the following: the length of time needed to recruit the desired sample size, the number of individuals who expressed interest but were not eligible, and of those who enrolled and were randomized, the number who withdrew before the follow-up measurement sessions, along with reasons. To address acceptability of the research procedures, we examined the following: the number of individuals who expressed interest and were eligible to participate but chose not to enroll, along with reasons, and the number of individuals who continued with baseline measurements after screening and eligibility.
Measurement
Trial outcome measures including measurement protocols are described in detail elsewhere (14). In brief, the planned primary outcome for the definitive trial was the difference between groups in mean weight loss (kg) and percentage weight change from baseline to 12 wk. For all outcomes (primary and secondary), we examined differences between groups at 12 wk and change within the intervention group to 12 months. Secondary outcome measures included the following:
Objectively measured clinical characteristics: BMI (calculated from weight and height; kg·m−2), waist circumference (cm), and resting systolic and diastolic blood pressure (BP; mm Hg)
Self-reported PA and sedentary time: average steps per day, measured using Yamax Digiwalker SW-200 pedometers and self-reported by participants using a 7-d paper log; total PA (metabolic equivalents MET·min·wk−1); and sedentary time (on a typical week day in minutes) measured using the International Physical Activity Questionnaire—Short Form (IPAQ) (7)
Self-reported eating and alcohol: healthful eating score, measured using Starting the Conversation questionnaire (27); fatty food score, as well as sugary food and fruit/vegetable consumption, measured using a modified version of the Dietary Instrument for Nutrition Education (DINE) (32) and following scoring outlined by Hunt et al. (20); and total alcohol consumption (units per week), measured using a 7-d recall diary (8)
Psychological and health-related quality of life: self-esteem score, measured using the Rosenberg Self-Esteem Scale (17); positive and negative affect scores, measured using the International Positive and Negative Affect Schedule—Short Form (37); and self-rated health, using the European Quality of Life–5 Dimensions Questionnaire–3 Levels (EQ-5D-3L) visual analog scale score (9).
Adverse Events
Adverse events were any injury/newly diagnosed health condition that occurred during the study regardless of whether it was related to participation in the study. Serious adverse events were those that required hospitalization, prolonged medical attention, or were immediately life threatening or fatal. Men were given a log for reporting adverse events and asked about these at the start of each Hockey FIT session and at all measurement sessions.
Randomization, Allocation, and Blinding
The randomization sequence was generated using SAS software version 9.4 (SAS Institute Inc., Cary, NC). Randomization was stratified by site (1:1 allocation; block size, 4) and concealed using sequentially numbered and sealed opaque envelopes. After baseline, a central research team member not involved in generating the sequence enrolled participants and assigned them to one of the two interventions. After allocation, all participants were told their weight and shown visually their BMI and associated risk on Health Canada’s BMI Nomogram (http://www.hc-sc.gc.ca/), and provided with copies of national guidelines for healthy eating (http://www.hc-sc.gc.ca/) and PA (http://www.csep.ca/). It was not possible to blind participants or coaches; however, objective measurement was used for our planned primary outcome (weight) and a blinded assessor conducted weight measurements in a separate, private area, to reduce the likelihood that group allocation would be revealed.
Sample Size
A sample size calculation for the definitive RCT was based on a 5% difference in weight loss between intervention and comparator at 12 months (20). Assuming an SD of 19.9%, 80% power, a 0.05 two-sided significance level, and a conservative 25% loss to follow-up estimate, 335 men in each arm (670 total) would be required. On the basis of the number of teams in the Ontario Hockey League, enrolling 17 sites was deemed reasonable for the definitive RCT, which reflects the need to recruit 40 men from each site. Therefore, a recruitment target of 40 men in each of the two sites (80 men total) was set for this pilot trial.
Statistical Analysis
We analyzed outcome data to examine the potential effectiveness of the Hockey FIT program on the basis of an intent-to-treat approach. We examined differences between groups in mean weight loss at 12 wk using a linear mixed-effects model, including all randomized participants per group assignment (i.e., including those with missing follow-up data and regardless of compliance with the intervention) and adjusted for age and site. We retained the baseline value as part of the outcome and constrained group means as equal because of randomization (i.e., no group term) (10). The model included terms for time (0, 12 wk), group (intervention, comparator)–time, age, and site (London, Sarnia). An advantage of the mixed-effects regression modeling approach is that it does not require each participant to have the same number of measurements provided that data are missing at random (i.e., after taking observed data into account, there are no systematic differences between participants with complete data as compared with those with missing data). This is also an assumption made by using most multiple imputation methods (10). We ran an additional linear mixed-effects model within the intervention group only to obtain exploratory estimates for mean change from baseline to 12 months. We followed the same approach for all continuous outcomes unless otherwise specified. Residuals from models were examined and subjected to assumptions checks.
Percentage of baseline weight was examined using an ANCOVA, and total PA from the IPAQ was analyzed using quantile regression; all models adjusted for age, site, and either baseline weight (weight model) or baseline total PA (total PA model). We also examined the likelihood of the intervention (vs comparator) achieving at least 5% weight loss at 12 wk using modified Poisson regression. We used generalized linear mixed-effects models adjusted for age and site for sugary foods and fruit/vegetable consumption (log-linear modified Poisson models), as well as for alcohol consumption (log-linear Poisson models).
To address participant dropout at 12 wk, we compared important baseline characteristics of men who attended the 12-wk measurement sessions (with valid weight data) with those who did not attend the 12-wk measurement sessions using independent-samples t-tests (continuous variables) and Fisher exact tests (categorical variables). In addition, we conducted a sensitivity analysis for our primary outcome (i.e., differences between groups in mean weight loss at 12 wk adjusting for age and site) by restricting our sample to include only “all-completers” (i.e., sample decreased from n = 80 to n = 63). Participants were deemed as all-completers if they attended the 12-wk measurement sessions and if the participant was in the intervention group; they also met the criteria to be classified as a “program completer” (i.e., attended ≥50% of in-person group sessions including at least one session in the final 6 wk). Interpretation of results is primarily based on estimation and associated 95% confidence intervals (CIs). Analyses were performed using SAS software version 9.4 (SAS Institute Inc.).
RESULTS
Participants were recruited during a 4-wk period. Across both sites, the most successful methods of recruitment included communication from the hockey team via e-mail or social media (e.g., Twitter) and word of mouth, where 40% and 36% of men were recruited, respectively. The remaining men were recruited through traditional media sources (14%), posters and handouts (9%), and other methods (1%). There were 105 individuals assessed for eligibility, of which 24 were excluded and 1 was eligible but did not enroll. The remaining 80 individuals were eligible, completed baseline measurements, and were allocated to either intervention or comparator. One individual withdrew after randomization because he was displeased with allocation to the comparator group. The intervention group began Hockey FIT within 3 wk of baseline measurement. The number of men not attending the 12-wk measurement sessions was similar between groups (intervention group, n = 7; comparator group, n = 6) along with reasons for withdrawal (see Fig. 1). Between 12 wk and 12 months (intervention group only), two individuals who had not attended the 12-wk measurement sessions returned to complete the 12-month measurement sessions and an additional five individuals were lost to follow-up. Overall, trial retention was >80% at 12 wk and >75% (intervention group only) at 12 months. Regarding program compliance, there were 10 men in the intervention group who were classified as “noncompleters” (i.e., attended <50% of sessions including none in the final 6 wk), but this did not preclude them from attending follow-up measurement sessions. For the remaining 30 men (i.e., program completers), the mean (SD) for percentage of sessions attended was 81.7% (13.7).
FIGURE 1.
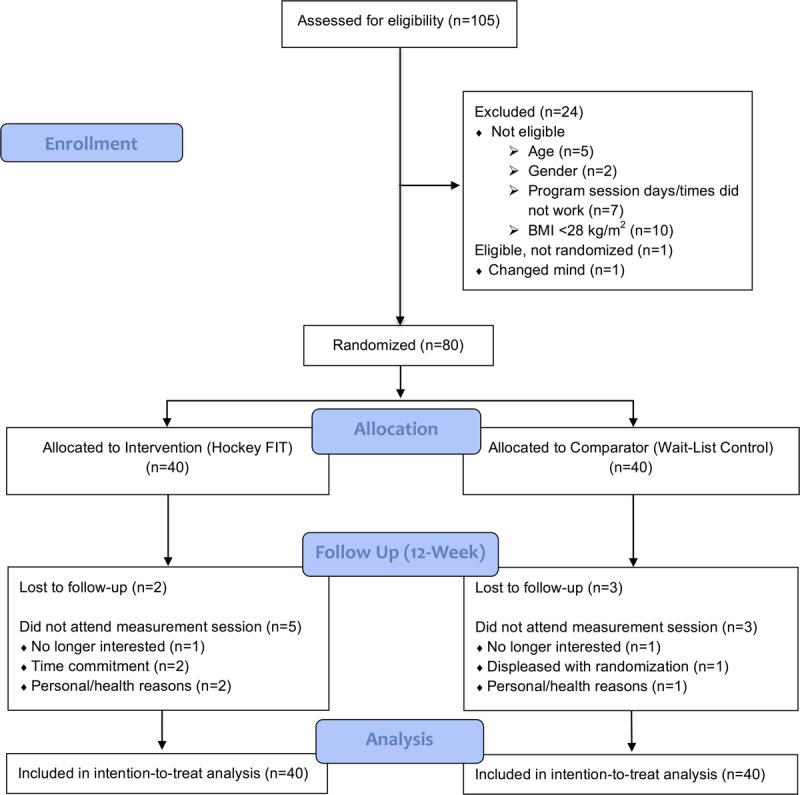
Study flow diagram to 12-wk follow-up (end of the intervention period).
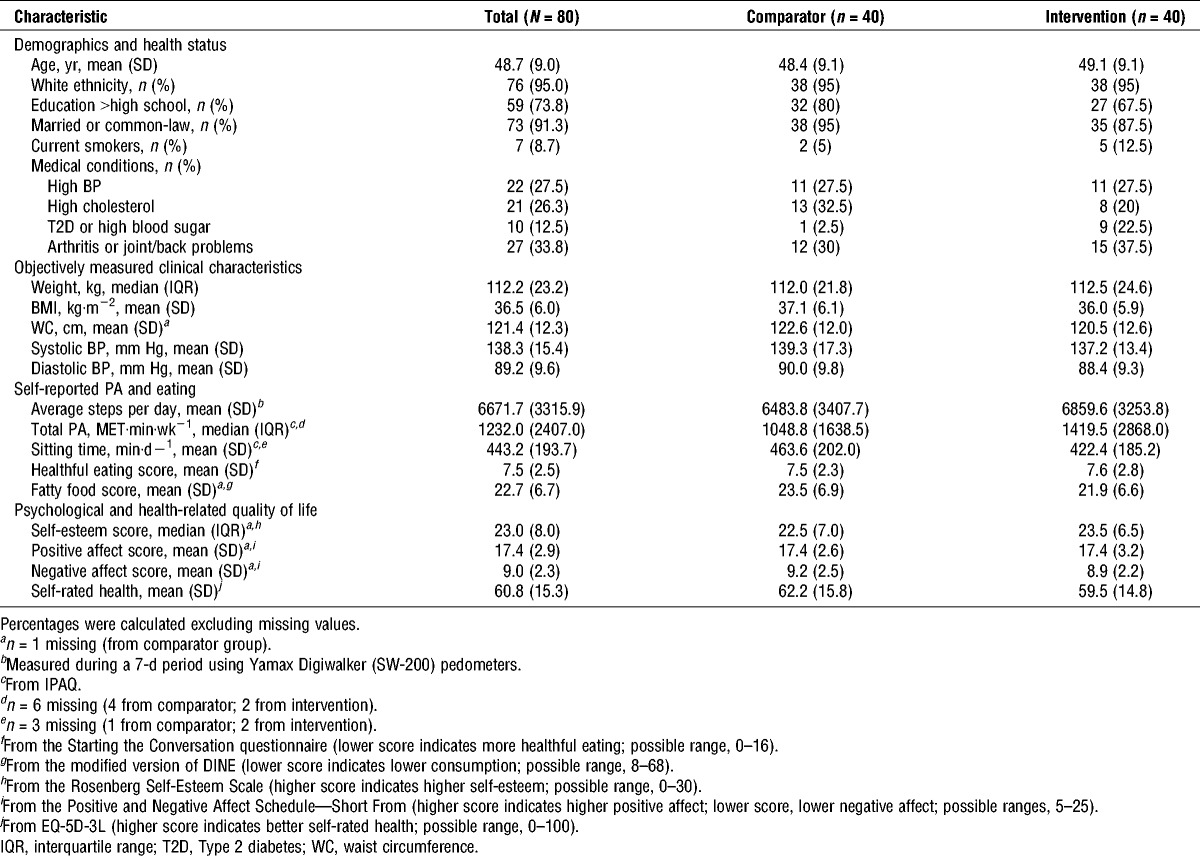
At baseline, groups were balanced on most demographic and health history characteristics, as well as study outcomes. Mean (SD) BMI values (36.5 (6.0)) correspond to obese class II (39); on average, participants reported daily step counts corresponding to a low active lifestyle (i.e., 5000–7499 steps per day) (38), and most participants consumed fruit/vegetables less than three times per day (see Table 1).
TABLE 1.
Baseline participant characteristics.
The detailed results for weight loss, percentage weight change from baseline, and weight loss of at least 5% are presented in Figure 2. The intervention group lost, on average, 3.58 kg more than the comparator group by 12 wk (95% CI for the difference between groups, −5.26 to −1.90; P < 0.001) and maintained weight loss to 12 months (mean change from baseline to 12 months within the intervention group, −3.96 (95% CI, −6.37 to −1.56)). This represents, on average, 3.04% more weight loss than the comparator group at 12 wk (95% CI for the difference between groups, −4.48 to −1.60; P < 0.001), and this percentage loss was maintained to 12 months (mean change from baseline to 12 months within the intervention group, −3.40 [95% CI, −5.56 to −1.25]). Furthermore, by 12 wk, 30% of men in the intervention group had achieved weight loss of 5% or more compared with only 3% of men in the comparator group. Accordingly, the intervention group had more than 10 times the likelihood of achieving weight loss of at least 5% compared with the comparator group (risk ratio (95% CI), 10.2 (1.4–73.5); P = 0.02). By 12 months, 17% of men in the intervention group had maintained weight loss of ≥5% since baseline. When we restricted the primary analysis to all-completers, the overall conclusions did not change; however, the difference between groups in mean weight loss (favoring the intervention group) increased (i.e., difference between groups in mean change (95% CI), −4.05 [−5.78 to −2.3] kg; P < 0.001).
FIGURE 2.
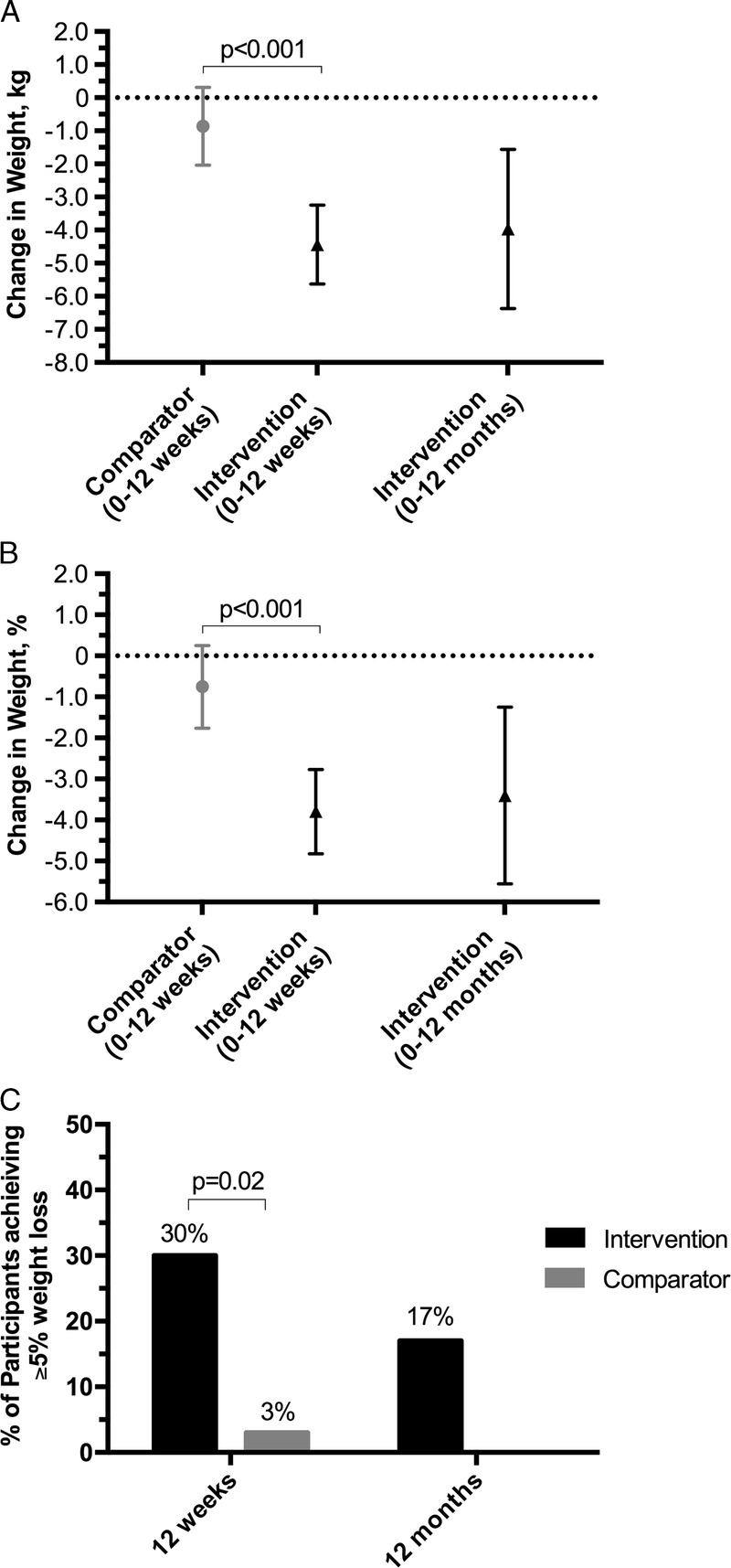
Effect of interventions on weight, percentage of baseline weight, and achieving clinically significant weight loss of at least 5%. A, Absolute weight change in kilograms. B, Percentage of baseline weight lost. C, Weight loss of at least 5% from baseline. From baseline (0 wk) to 12 wk, mean change in weight (kg) and percentage of baseline weight (%) were significantly different between the intervention and comparator groups—favoring the intervention group (i.e., greater weight loss and greater percentage of baseline weight lost). Within the intervention group, weight loss and percentage of baseline weight lost were maintained to 12 months. The intervention group had a significantly greater proportion of participants who achieved at least 5% weight loss by 12 wk compared with the comparator group. By 12 months, approximately half of the participants in the intervention group who had achieved at least 5% weight loss at 12 wk maintained this weight loss.
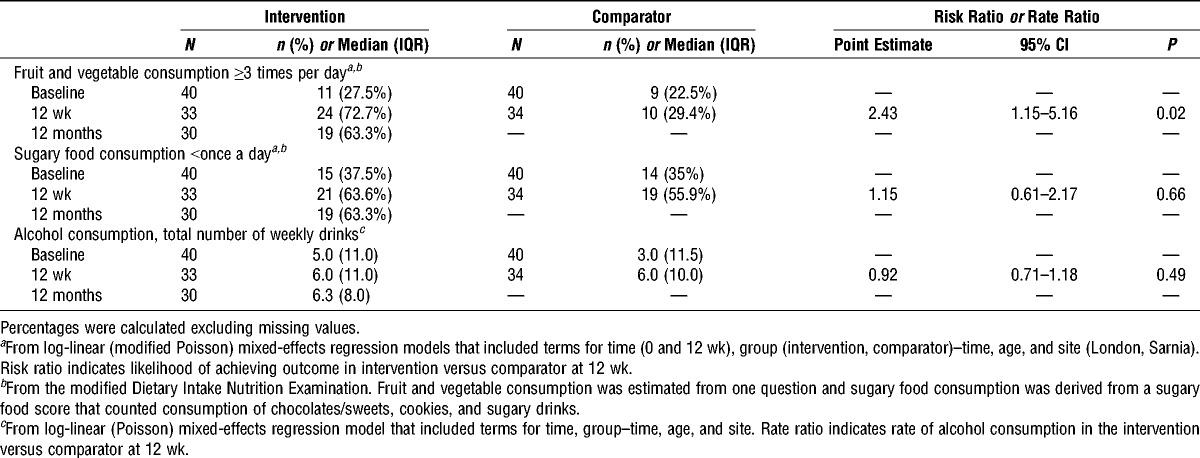
At 12 wk, we also found between-group differences favoring the intervention for BMI, waist circumference, systolic BP, steps per day, healthful eating, fatty food, and self-rated health. Although groups were similar in diastolic BP, sitting time, and self-esteem, improvements were observed within the intervention group at 12 wk. By 12 months, improvements were still observed within the intervention group for most of these outcomes. No statistically significant differences between groups were observed for either positive or negative affect or for total PA (see Table 2). At 12 wk, men in the intervention group were almost 2.5 times more likely to consume fruit and vegetables at least three times per day compared with men in the comparator group; however, groups had similar sugary food consumption and alcohol consumption (see Table 3).
TABLE 2.
Secondary continuous-level outcomes: changes from baseline to 12 wk and 12 months (intervention only) and differences between the intervention and comparator groups at 12 wk.
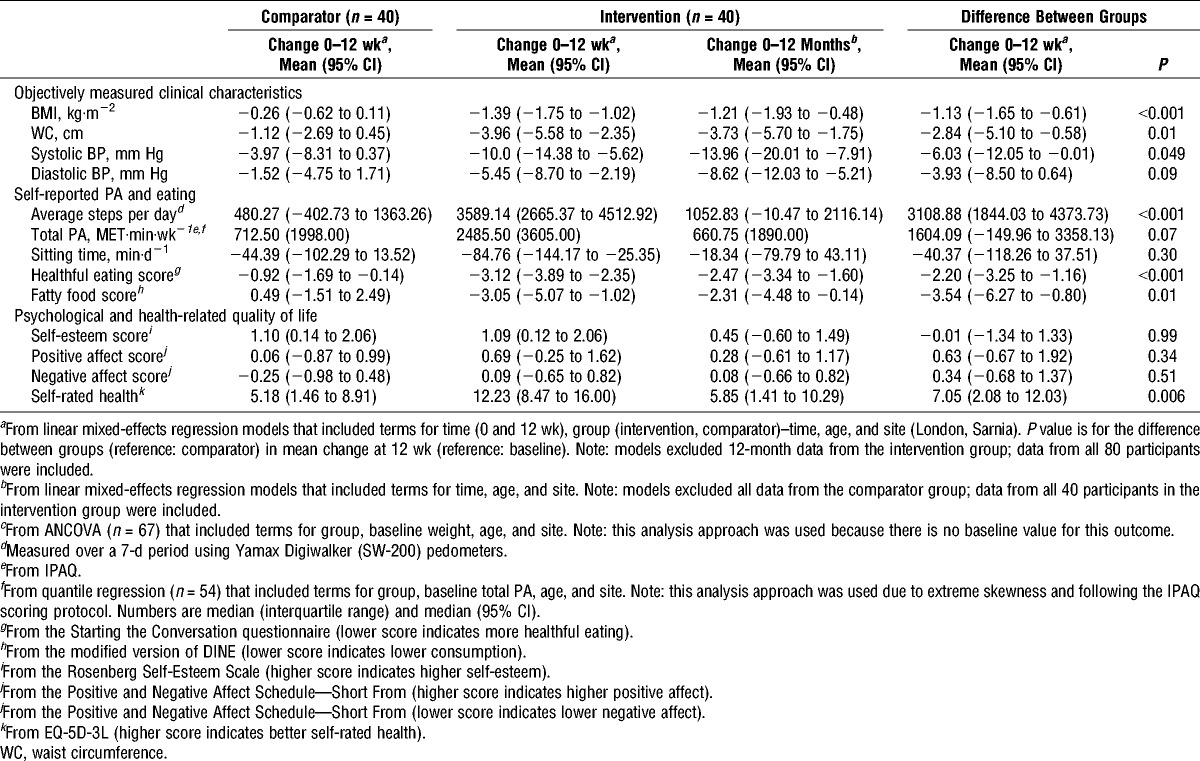
TABLE 3.
Secondary categorical-level outcomes: proportions achieving outcomes of interest at all time points and differences between the intervention and comparator groups at 12 wk.
For 12 wk (Hockey FIT active phase or control), there were no serious adverse events reported. Participants reporting any adverse event were numerically higher for intervention (11 (27.5%)) compared with those in the comparator group (1 (2.5%)); however, most adverse events (11/12) were musculoskeletal and only 2 (5%) were considered possibly or definitely related to the intervention.
Analyses comparing men who dropped out of the study by 12 wk (n = 13) with those who attended the 12-wk measurement sessions (n = 67) showed no statistically significant differences at baseline between groups on all characteristics examined including age, education, marital status, current medical conditions (high BP, high cholesterol), weight, BMI, steps per day, healthful eating, and self-rated health (data not shown).
DISCUSSION
Results from this pilot trial suggest feasibility of recruitment and retention of our target population (middle-age, overweight/obese male hockey fans), as well as acceptability of trial procedures. Recruitment of 80 eligible participants was completed in a short time frame using methods that were easy to implement and with no added costs. Trial retention was high at 12 wk (in both groups) and 12 months (intervention group only), and only one individual stated that he withdrew due to trial procedures (i.e., randomization).
Our results are provocative because we found that men who participated in the Hockey FIT program lost weight, increased their steps per day, and improved other clinical outcomes (e.g., systolic BP), their diet, and perceptions of their own health, to a greater extent compared with the controls. Furthermore, men were able to maintain most of these outcomes 12 months later, after a minimally supported phase, showing promise for long-term sustainability. When examining clinically significant weight loss of at least 5% (18), our results indicate that men participating in Hockey FIT were 10 times more likely to achieve this weight loss by 12 wk compared with the controls. Taken together, our results demonstrate excellent potential for the Hockey FIT program.
Four programs from England, Scotland, and Australia (5,20,28,34,43) engaged men through being fans of organized sports and showed increased PA and improvements in other health behaviors and outcomes (4). Similar to Hockey FIT, these approaches work with conceptions of masculine ideals rather than against them (4). Despite this being a pilot trial, we observed differences between groups at 12 wk for our planned primary outcome and for many secondary outcomes. When compared with the FFIT pilot (15), our retention rates observed at 12 wk and 12 months were similar, along with most of our main findings. Although similar to the FFIT pilot sample on most baseline characteristics, our sample had considerably lower levels of alcohol consumption and higher ratings of self-esteem, providing one possible explanation for our lack of differences found in these outcomes, in contrast to the FFIT pilot trial. Taken together, our findings suggest that we can achieve high retention rates and demonstrate the effectiveness of the Hockey FIT program in the planned definitive trial.
A systematic analysis for the Global Burden of Disease Study 2010 using data from 187 countries during a 20-yr period (1990–2010) found that gains in both life expectancy and healthy life expectancy were higher for women compared with men (40). As suggested by Baker et al. (2), to address the current global epidemic of chronic disease, we must direct attention to the health needs of both men and women, while recognizing the differences between them.
Although lifestyle interventions have been shown to reduce the risk of chronic disease, men are often underrepresented in such programs (12). In a review published in 2012, only 5% of RCTs of lifestyle weight loss interventions targeted men exclusively, and of studies that included both men and women, on average, only 27% of participants were male (26). Although development of interventions that consider the preferences of men is now receiving increased attention, recent reviews on male-only weight loss or weight-loss maintenance interventions (42), as well as interventions that include promotion of PA for adult men (4), have suggested the need for more high-quality research among diverse groups of men.
A limitation of this study includes the self-reported measurement of PA, diet, and alcohol consumption through self-administered questionnaires. Our decision to use these types of measures over more objective ones that are either much more expensive (e.g., accelerometers) or time-intensive (e.g., interviews) was based primarily on remaining pragmatic, particularly given that these are planned secondary outcomes for the definitive trial. We did use pedometers as one measure of PA; however, self-report was still required using a paper log. A planned improvement for the definitive trial is to use more sophisticated pedometers, which store data that can be downloaded to a computer, eliminating the self-reported component. This approach will strengthen our PA measurement but maintain the pragmatic nature of our trial.
Another limitation of this study is that there were 13 men who did return for the 12-wk measurement session. We analyzed the data using likelihood-based methods, which are well known to provide unbiased results under the more general assumption of missing at random (i.e., the probability of missing may depend not only on the covariates but also on the observed outcomes). This assumption is tenable because we did not find any differences between these men and the 67 who attended the 12-wk measurement sessions on characteristics such as age, weight, steps per day, healthful eating, and self-rated health. We did not adopt the method of last observation carried forward because it makes a very restrictive assumption that the outcome will be stable from the point of dropout to trial completion. One may still suspect that the data are missing not at random (i.e., the probability that a man did not return for measurement depends on his unobserved true weight). There are currently no good statistical methods without making even more assumptions for this situation (10).
It is possible that men allocated to the comparator group were disappointed with having to wait 4 months to receive the Hockey FIT program, which may have led some of these men to seek out alternatives to improve their health during the control period. In fact, improvements were seen within the control group in outcomes including healthy eating, self-esteem, and self-rated health. Although the trial itself may have influenced participants in the comparator group, this would only have made estimates in this study (i.e., differences between groups) more conservative. In our planned definitive trial, we will overcome this issue by using a cluster-randomized design, whereby all men enrolled at a given site will begin the program together at a defined date (i.e., the entire site is randomized to either intervention or comparator).
In this study, most men were white, employed, and married/living common-law, and about three-quarters had education greater than high school. Few were current smokers (<10%), which is lower than the estimated percentage of men in Canada who smoke (22.3% in 2011) (21), but the prevalence of self-reported Type 2 diabetes (5%) is similar to the estimated prevalence in Canada for men 40–49 yr old (ranging from 4.1% to 6.2%) (29). Thus, findings from this pilot study should be interpreted in context of these demographic and health characteristics. Future research includes determining how to engage a more diverse sample of men across the socioeconomic spectrum in the Hockey FIT program.
Our study had several strengths. In this study, we sought to reflect real-world conditions, in preparation for the definitive trial, where our goal will be to determine the effect of this program under conditions we expect it to be applied after research (23). Although this study was designed as a pilot trial, we achieved many statistically and clinically important differences between groups at 12 wk, favoring the Hockey FIT group. Importantly, we engaged at-risk men, a group of individuals who are typically a hard-to-reach population, and we achieved high rates of retention, including men in the intervention group after the 40-wk minimally supported phase. It is plausible that elements included in the minimally supported phase, including the smartphone app, the private online social network, the standardized encouragement messages, and the booster session, all contributed to both the retention rates and the positive results related to maintenance of outcomes in the intervention group. Alongside this pilot trial, we conducted a process evaluation, which will examine the acceptability of the Hockey FIT program, including both the active phase and the minimally supported phase, and inform program optimization (to be reported separately).
CONCLUSIONS
In conclusion, results from this study suggest that it is feasible to recruit and retain middle-age, overweight/obese men into a weight loss and healthy lifestyle program using sport fandom as a powerful draw, and that the research procedures used in this pilot trial were acceptable to most participants. Furthermore, Hockey FIT has the potential to lead to weight loss and improved health in middle-age overweight and obese men. Taken together, these results provide evidence to move forward with a definitive pRCT of the optimized Hockey FIT program.
Acknowledgments
We would like to thank the men who participated in this study, as well as the organizations who provided in-kind support for this study including the London Knights, the Sarnia Sting, and GoodLife Fitness. We would also like to thank staff and students who made important contributions to this study, including Roseanne Pulford, Wendy Blunt, Sasha Guay, Kendra Broad, Stephanie Muise, Nárlon Silva, Erin Shellington, Michael Gregory, Adam Gavarkovs, Ryan Scott, Sarah Hill, and Elizabeth Fryer. We would also like to thank Prof. Shaun Treweek for his advice and insight on the trial design for this study.
This study was funded by the Movember Foundation (Canadian Men’s Health & Wellbeing Innovation Challenge). Kate Hunt is funded by the UK Medical Research Council (MC_UU_12017/12).
The authors declare that the results of the present study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. In addition, the results of the present study do not constitute endorsement by the American College of Sports Medicine.
The authors declare no conflicts of interest.
REFERENCES
- 1.Alter DA, Wijeysundera HC, Franklin B, et al. Obesity, lifestyle risk-factors, and health service outcomes among healthy middle-aged adults in Canada. BMC Health Serv Res. 2012;12:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker P, Dworkin SL, Tong S, Banks I, Shand T, Yamey G. The men’s health gap: men must be included in the global health equity agenda. Bull World Health Organ. 2014;92(8):618–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. [DOI] [PubMed] [Google Scholar]
- 4.Bottorff JL, Seaton CL, Johnson ST, et al. An updated review of interventions that include promotion of physical activity for adult men. Sports Med. 2015;45(6):775–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brady AJ, Perry C, Murdoch DL, McKay G. Sustained benefits of a health project for middle-aged football supporters, at Glasgow Celtic and Glasgow Rangers Football Clubs. Eur Heart J. 2010;31(24):2966–8. [PubMed] [Google Scholar]
- 6.Bunn C, Wyke S, Gray CM, Maclean A, Hunt K. “Coz football is what we all have”: masculinities, practice, performance and effervescence in a gender-sensitised weight-loss and healthy living programme for men. Sociol Health Illn. 2016;38(5):812–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95. [DOI] [PubMed] [Google Scholar]
- 8.Emslie C, Lewars H, Batty GD, Hunt K. Are there gender differences in levels of heavy, binge and problem drinking? Evidence from three generations in the west of Scotland. Public Health. 2009;123(1):12–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 10.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. 2nd ed Hoboken (NJ): John Wiley & Sons; 2011. [Google Scholar]
- 11.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7. [DOI] [PubMed] [Google Scholar]
- 12.Gavarkovs AG, Burke SM, Petrella RJ. Engaging men in chronic disease prevention and management programs: a scoping review. Am J Mens Health. 2016;10(6):NP145–54. [DOI] [PubMed] [Google Scholar]
- 13.Gill DP, Blunt W, Bartol C, et al. HealtheSteps™ study protocol: a pragmatic randomized controlled trial promoting active living and healthy lifestyles in at-risk Canadian adults delivered in primary care and community-based clinics. BMC Public Health. 2017;17(1):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill DP, Blunt W, De Cruz A, et al. Hockey Fans in Training (Hockey FIT) pilot study protocol: a gender-sensitized weight loss and healthy lifestyle program for overweight and obese male hockey fans. BMC Public Health. 2016;16:1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gray CM, Hunt K, Mutrie N, Anderson AS, Treweek S, Wyke S. Weight management for overweight and obese men delivered through professional football clubs: a pilot randomized trial. Int J Behav Nutr Phys Act. 2013;10:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gray CM, Hunt K, Mutrie N, et al. Football Fans in Training: the development and optimization of an intervention delivered through professional sports clubs to help men lose weight, become more active and adopt healthier eating habits. BMC Public Health. 2013;13:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gray-Little B, Williams V, Hancock T. An item response theory analysis of the Rosenberg Self-Esteem Scale. Pers Soc Psychol Bull. 1997;23(5):443–51. [Google Scholar]
- 18.Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254–66. [DOI] [PubMed] [Google Scholar]
- 19.Hirt ER, Clarkson JJ. The psychology of fandom: understanding the etiology, motives, and implications of fanship. In: Kahle LR, Close AG, editors. Consumer Behavior Knowledge for Effective Sports and Event Marketing. New York (NY): Routledge/Taylor & Francis Group; 2011. pp. 59–85. [Google Scholar]
- 20.Hunt K, Wyke S, Gray CM, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet. 2014;383(9924):1211–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janz T. Current Smoking Trends. Statistics Canada; 2015. Available from: http://www.statcan.gc.ca/pub/82-624-x/2012001/article/11676-eng.htm. [Google Scholar]
- 22.Knight E, Stuckey MI, Petrella RJ. Validation of the step test and exercise prescription tool for adults. Can J Diabetes. 2014;38(3):164–71. [DOI] [PubMed] [Google Scholar]
- 23.Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ. 2015;350:h2147. [DOI] [PubMed] [Google Scholar]
- 24.Neuman K. Hockey in Canada—2012 Public Opinion Survey. The Environics Institute for Social Change. 2012. Available from: http://www.environicsinstitute.org/uploads/institute-projects/environics-institute-hockey-canada-2012-survey.pdf.
- 25.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring). 2012;20:1234–9. [DOI] [PubMed] [Google Scholar]
- 27.Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE. Starting the conversation performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med. 2011;40(1):67–71. [DOI] [PubMed] [Google Scholar]
- 28.Pringle A, Zwolinsky S, McKenna J, Daly-Smith A, Robertson S, White A. Effect of a national programme of men’s health delivered in English Premier League football clubs. Public Health. 2013;127(1):18–26. [DOI] [PubMed] [Google Scholar]
- 29.Public Health Agency of Canada. Diabetes in Canada. Ottawa: 2011.126. Available from: http://www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/index-eng.php.
- 30.Robertson C, Archibald D, Avenell A, et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess. 2014;18(35): v–vi, xxiii–xxix, 1–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robertson C, Avenell A, Boachie C, et al. Should weight loss and maintenance programmes be designed differently for men? A systematic review of long-term randomised controlled trials presenting data for men and women: the ROMEO project. Obes Res Clin Pract. 2016;10(1):70–84. [DOI] [PubMed] [Google Scholar]
- 32.Roe L, Strong C, Whitesdie C, Neil A, Mant D. Dietary intervention in primary care: validity of the DINE method for diet assessment. Fam Pract. 1994;11(4):375–81. [DOI] [PubMed] [Google Scholar]
- 33.Scarborough P, Bhatnagar P, Wickramasinghe KK, Allender S, Foster C, Rayner M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: an update to 2006–07 NHS costs. J Public Health (Oxf). 2011;33(4):527–35. [DOI] [PubMed] [Google Scholar]
- 34.Sealey RM, Twomey J, Pringle FA, Cheffins T, Gupta S. A 12-week lifestyle intervention for middle-aged, overweight men who are supporters of local sporting clubs. Aging Male. 2013;16(3):118–22. [DOI] [PubMed] [Google Scholar]
- 35.The Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can J Sport Sci. 1992;17(4):338–45. [PubMed] [Google Scholar]
- 37.Thompson ER. Development and validation of an internationally reliable short-form of the Positive and Negative Affect Schedule (PANAS). J Cross Cult Psychol. 2007;38(2):227–42. [Google Scholar]
- 38.Tudor-Locke C, Craig CL, Thyfault JP, Spence JC. A step-defined sedentary lifestyle index: <5000 steps/day. Appl Physiol Nutr Metab. 2013;38(2):100–14. [DOI] [PubMed] [Google Scholar]
- 39.Twells LK, Gregory DM, Reddigan J, Midodzi WK. Current and predicted prevalence of obesity in Canada: a trend analysis. CMAJ Open. 2014;2(1):E18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang H, Dwyer-Lindgren L, Lofgren KT, et al. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2071–94. [DOI] [PubMed] [Google Scholar]
- 41.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25. [DOI] [PubMed] [Google Scholar]
- 42.Young MD, Morgan PJ, Plotnikoff RC, Callister R, Collins CE. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes Rev. 2011;13(5):393–408. [DOI] [PubMed] [Google Scholar]
- 43.Zwolinsky S, McKenna J, Pringle A, Daly-Smith A, Robertson S, White A. Optimizing lifestyles for men regarded as “hard-to-reach” through top-flight football/soccer clubs. Health Educ Res. 2013;28(3):405–13. [DOI] [PubMed] [Google Scholar]


