Abstract
Background and Purpose
Black stroke survivors experience greater post-stroke disability than whites. Differences in post-acute rehabilitation may contribute to this disparity. Therefore, we estimated racial differences in rehabilitation therapy utilization, intensity and the number post-acute care settings in the first year after a stroke.
Methods
We used national Medicare data to study 186,168 elderly black and white patients hospitalized with a primary diagnosis of stroke in 2011. We tabulated the proportion of stroke survivors receiving physical, occupational and speech and language therapy in each post-acute care setting (inpatient rehabilitation facility, skilled nursing facility and home health agency), minutes of therapy, and number of transitions between settings. We then used generalized linear models to determine whether racial differences in minutes of physical therapy were influenced by demographics, comorbidities, thrombolysis, and markers of stroke severity.
Results
Black stroke patients were more likely to receive each type of therapy than white stroke patients. Compared to white stroke patients, black stroke patients received more minutes of physical therapy (897.8 vs. 743.4; p<0.01), occupational therapy (752.7 vs. 648.9; p<0.01), and speech and language therapy (865.7 vs. 658.1; p<0.01). There were no clinically significant differences in physical therapy minutes after adjustment. Blacks had more transitions (median 3, IQR (1–5)) than whites (median 2, IQR (1–5), p < 0.01).
Conclusions
There are no clinically significant racial differences in rehabilitation therapy utilization or intensity after accounting for patient characteristics. It is unlikely that differences in rehabilitation utilization or intensity are important contributors to racial disparities in post-stroke disability.
Each year 800,000 people in the US have a stroke, a leading cause of disability in the US.1, 2 The vast majority of stroke patients receive rehabilitation therapies during their stroke hospitalization and most continue to receive rehabilitation therapies as part of their post-acute care (PAC). Post-acute rehabilitation may occur in various types of settings, including: private residency home health, outpatient rehabilitation, institutions such as inpatient rehabilitation facilities (IRF) and skilled nursing facilities (SNF), and during the index stroke hospitalization itself. Observational studies have shown that more intense rehabilitation settings,3–5 higher intensity rehabilitation in comparable settings,6 and the use of outpatient and home therapy,7 are associated with reduced disability. Collectively, these studies suggest that more intense rehabilitation may reduce post-stroke disability.8
There are large racial disparities in stroke incidence and post-stroke disability. Blacks have twice as many strokes as whites and racial disparities in stroke incidence have worsened over time.9–11 National data has shown that community dwelling black stroke survivors experience on average, 25% more limitations in activities of daily living than whites stroke survivors.12 It is unknown when racial disparities in post-stroke disability emerge, but a prospective population based sample found that racial disparities in post-stroke disability are present one year after their stroke, suggesting that outcomes diverge in the first year.13 Despite the existence of marked racial disparities in post-stroke disability,12–14 little is known about the underlying mechanisms of this disparity.15 We hypothesize that black stroke patients receive less post-stroke rehabilitation therapies than white stroke patients. Our hypothesis is supported by the presence of marked geographic variability in PAC,16 coupled with racial segregation in the United States, potentially leading to differential PAC utilization. Additionally, among stroke patients discharged to institutional post-acute rehabilitation care, blacks are more likely to be discharged to the less intense rehabilitation environment, SNF, than the more intense IRF, compared to whites.17 Although prior studies have explored racial differences in post-acute rehabilitation care, they are limited to a single rehabilitation setting, solely focus on the initial discharge location, and are not nationally representative.17–19
We addressed these issues by conducting a comprehensive evaluation of rehabilitation therapies across all PAC settings for one year following a stroke using data from a population of Medicare fee-for-service recipients. To assess whether differences in PAC exist by race, we first considered utilization of PAC across all settings. We then explored whether there were racial differences in the intensity, defined as minutes of rehabilitation, within each setting. Finally, we explored whether the total number of PAC settings or the patterns of transition between settings differed between blacks and whites.
Methods
Stroke Patients
All Medicare fee-for-service patients aged 65 years or older admitted to an acute care hospital in 2011 with a primary diagnosis of ischemic stroke or intracerebral hemorrhage (ICD-9-CM 431, 433.×1, 434.×1, 436) were identified from the Medicare Inpatient file.20, 21 We included patients who were continuously enrolled in Medicare-fee-for service for 1 year after their stroke or until the time of their death. We excluded those with race/ethnicity other than black or white. Race was determined using the Medicare Beneficiary Summary File, which reports race from social security administration data.22
The Centers for Medicare & Medicaid Services Hierarchical Condition Categories (HCC) coding system was used to assign comorbidities to all patients at the time of their stroke hospitalization.23 We also identified life-sustaining treatments, including: gastrostomy, hemicraniectomy, ventriculostomy, tracheostomy, intubation, hemodialysis, and cardiopulmonary resuscitation, using procedure codes during the index hospitalization.24 Thrombolysis included (Intraenous (IV) tissue plasminogen activator (tPA) (DRG 559, MS-DRG 61-63 or ICD-9 procedure code 99.10), and acute intra-arterial treatment (IAT) (CPT codes 37184-6, 37201, 75896) identified using DRG and procedure codes were abstracted from the inpatient files. We abstracted length of hospitalization directly from the inpatient file.
Rehabilitation Services and Utilization
Medicare claims data are divided into standard analytic files based on the place of service. By combining data from the Inpatient (including acute hospitalization and IRF), SNF, Home Health, and Outpatient files, we captured all claims for each major rehabilitation setting. Inpatient rehabilitation facilities and inpatient stays were differentiated in the inpatient file based on provider numbers (3025-3099 or T R representing IRF and 0001-0879 representing acute hospitalizations). Files were linked using Medicare beneficiary IDs. We identified physical therapy (PT), occupational therapy (OT), and speech and language therapy (SLT) using CPT and revenue codes within one year of stroke admission (Supplemental Table I). Physical therapy was identified with revenue codes (042X), OT with revenue codes (043X), and SLT with revenue codes (044X).
For each therapy modality, minutes of therapy was estimated by cross-walking CPT codes to the American Medical Association’s average intra-service time (crosswalk included as Supplemental Table I). Because therapy in an institutional PAC setting is reimbursed as part of the overall facility fee, it is not necessarily reported with CPT codes, but rather rolled up into the overall facility record and summarized using revenue codes. To quantify therapy in institutional PAC settings, we created a two-stage cross walk. First, revenue codes and CPT codes were inconsistently, yet occasionally, listed on the same institutional claim. For these claims, we built a weighted average of the CPT-based time estimates to approximate the total amount of time for each revenue code. We then used this weighted time average for institutional claims that were limited to only revenue codes (Supplemental Table I). When both revenue codes and CPT codes were reported, we used the CPT code estimated time. We then estimated time in each therapy modality, total therapy time in each PAC setting, and the number of transitions between settings. Length of stay in SNF and IRF was abstracted from standard analytic files.
Analysis
Racial comparisons of demographics, comorbidities, hospital stay, and treatments were performed using descriptive statistics. First, we used chi-squared tests to compare, by race, the proportion of stroke patients who received each therapy modality and the proportion of stroke patients who received each therapy modality by rehabilitation setting. Second, we compared racial differences in the intensity of each therapy modality overall and by therapy setting among stroke patients who received each therapy modality of interest, using Wilcoxon Two-Sample Tests. For each therapy modality, we determined the minutes of therapy for each 10-day time epoch by race. We then used generalized linear models to explore racial differences in the amount of PT received in one year after accounting for age and sex, individual comorbidities, thrombolysis, and markers of stroke severity, which included length of stay, ICH (yes vs. no), and receipt of life-sustaining treatments. These analyses were repeated exploring minutes of PT in 30- and 90-days. A secondary analysis was performed to explore the impact of racial differences in opportunities for rehabilitation therapy. Specifically, we determined the number of minutes of post-stroke rehabilitation therapies across and within each setting after excluding stroke patients who died during their stroke hospitalizations or were discharged to hospice. We then repeated our generalized linear models to explore racial differences in the amount of PT received in one year after accounting for age and sex, all individual HCC comorbidities, and markers of stroke severity.
Lastly, we explored transitions across PAC settings. Given that PT was the most commonly used therapy, we identified the sequence of PT settings for each stroke patient by appending all facility claims for an individual after the index stroke over the course of the subsequent year. The total number of transitions reflected the number of settings where PT was received in the first year after the stroke. Transition patterns were summarized using directed graphs, while the number of transitions was compared by race using chi-squared tests. This study was approved by the University of Michigan Institutional Review Board. Analyses were completed in STATA 12.0 (College Station, TX) and SAS (Cary, NC).
Results
There were 186,168 elderly stroke patients in our sample. Black stroke patients were younger (77.3 vs. 80,4; p<0.01), more likely to be women, and had slightly more medical comorbidities (4.3 vs. 4.2; p<0.01) than white stroke patients (Table 1). The mean duration of hospitalization was longer among black stroke patients than white stroke patients (7.2 vs. 5.8 days; p<0.01). Black stroke patients were more likely than white stroke patients to undergo life-sustaining treatments, intubation, tracheostomy, gastrostomy tube insertion, hemodialysis, and cardiopulmonary resuscitation.
Table 1.
Stroke Patient Characteristics by Race
| Characteristics | White Stroke Patients, (n=164,398) %(n) |
Black Stroke Patients, (n=21,770) %(n) |
|---|---|---|
| Men | 41.3 (67,913) | 37.5 (8,160) |
| Age, Mean (SD) | 80.4 (8.2) | 77.3 (8.4) |
| Total number of comorbidities, Mean (SD) | 4.2 (2.3) | 4.3 (2.3) |
| Markers of Stroke Severity | ||
| Length of hospitalization, Mean (SD) | 5.8 (4.6) | 7.2 (6.6) |
| Intracerebral Hemorrhage | 11.1 (18,242) | 10.3 (2,249) |
| Gastrostomy Tube Insertion | 4.8 (7,816) | 9.3 (2,023) |
| Hemicraniectomy∞ | 0.6 (897) | 0.6 (123) |
| Ventriculostomy∞ | 0.01 (15) | 0.02 (5) |
| Tracheostomy | 0.6 (974) | 1.5 (1,326) |
| Intubation | 6.3 (10,314) | 8.2 (1,779) |
| Hemodialysis | 1.0 (1,686) | 4.4 (949) |
| Cardiopulmonary Resuscitation | 0.2 (451) | 0.6 (139) |
P is non-significant. All other p values are less than 0.001.
Rehabilitation Utilization
Table 2 shows the proportion of stroke patients who utilized each rehabilitation therapy in each setting. Black stroke patients received more of each type of therapy overall and in each specific setting than white stroke patients. Outpatient PT was the one exception. Black stroke patients were slightly less likely than white stroke patients to receive outpatient PT (22.6% vs. 23.4%; p=0.01). There were small differences in the hospital discharge location by race, predominantly due to slightly higher initial rates of SNF use in blacks (29.7% vs. 28.9%; p= 0.03) and home health (12.4% vs. 10.4%; p < 0.01), and the slightly lower rates of discharge home without PAC (31.6% vs. 34.0%; p < 0.01). There were no differences in initial discharge to IRF (24.0% vs. 24.0%; p = 0.95).
Table 2.
Stroke Rehabilitation Therapy Utilization by Race
| Description | White Stroke Patients, (n=164,398) % (n) |
Black Stroke Patients, (n=21,770) % (n) |
|---|---|---|
| Physical Therapy | ||
| Any setting | 85.4 (140,410) | 89.2 (19,420) |
| Hospital | 82.9 (136, 315) | 85.7 (18,646) |
| Inpatient Rehabilitation Facility | 22.3 (36,712) | 23.6 (5,139) |
| Skilled Nursing Facility | 37.6 (61,845) | 41.9 (9,124) |
| Home Health Agency | 34.9 (57,409) | 42.6 (9,273) |
| Outpatient Setting∞ | 23.4 (38,415) | 22.6 (4,923) |
| Occupational Therapy | ||
| Any setting | 77.6 (127,563) | 82.5 (17,964) |
| Hospital | 66.5 (109,387) | 70.0 (15,201) |
| Inpatient Rehabilitation Facility | 22.3 (36,582) | 23.5 (5,119) |
| Skilled Nursing Facility | 37.3 (61,346) | 41.6 (9,053) |
| Home Health Agency | 24.0 (39,504) | 28.8 (6,264) |
| Outpatient Setting∞ | 17.2 (28,222) | 17.9 (3,889) |
| Speech and Language Therapy | ||
| Any setting | 73.6 (120,923) | 77.6 (16, 901) |
| Hospital | 64.8 (106,513) | 67.6 (14,718) |
| Inpatient Rehabilitation Facility | 20.8 (34,186) | 22.1 (4,809) |
| Skilled Nursing Facility | 30.6 (50,331) | 34.9 (7,602) |
| Home Health Agency | 13.8 (22,637) | 16.9 (3,679) |
| Outpatient Setting∞ | 16.0 (26,279) | 16.6 (3,620) |
P=0.01. All other p values are less than 0.001.
Rehabilitation Intensity
In the first year after their strokes, patients who received therapy received a median of 759 (IQR 144–1893) minutes of PT, 662 (IQR 125–1665) minutes of OT, and 678 (IQR 117– 2173) minutes of SLT. Minutes of therapy were highly variable and right skewed; the mean minutes of therapy was much greater than the median minutes of therapy (Figure 1). The median minutes of therapy increased in the secondary analysis when the population was limited to patients who survived their hospitalization and were not discharged to hospice. In the first year after their stroke, these patients received a median of 871 (IQR 230– 2003) minutes of PT, 738 (IQR 179– 1746) minutes of OT and 831 (IQR 146– 2356) minutes of SLT.
Figure 1.
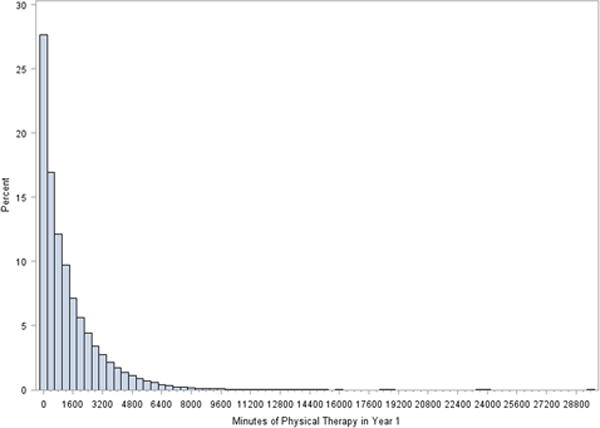
Minutes of Physical Therapy Received by Stroke Patients in the Year Following their Stroke
In the first year after their stroke, black stroke survivors had longer length of stay in SNF ((median 44 (IQR 21–83) vs. 40 (IQR 20–75, p<0.01)) and IRF ((median 17 (IQR 12–23) vs.16 (IQR 11-22), p<0.01)) than white stroke survivors. Table 3 shows the total minutes of each therapy and minutes of therapy in each setting by race among stroke patients who received therapy. Black stroke patients received more minutes of rehabilitation therapy than white stroke patients. Compared to white stroke patients, black stroke patients received a median of (897.8 vs. 743.4; p<0.01) minutes of PT, (752.7 vs. 648.9; p<0.01) minutes of OT, and (865.7 vs. 658.1; p<0.01) minutes of SLT. Black stroke patients received a greater amount of therapy in each setting compared to white stroke patients. With regards to the timing of post-stroke rehabilitation, overall white stroke patients received an average of 16 more minutes of therapy in the first 10 days post-stroke compared to black stroke patients. For every subsequent epoch of 10 days of therapy, black stroke patients received more therapy (Figure 2).
Table 3.
Intensity of Stroke Rehabilitation Therapy in the year following a stroke by Race
| Description | White Stroke Patients Median(IQR), mins/yr |
Black Stroke Patients Median(IQR), mins/yr. |
P value |
|---|---|---|---|
| Physical Therapy | |||
| Any setting | 743.4 (1729.6) | 897.8 (1782.8) | <0.01 |
| Hospital | 86.3 (115.4) | 86.8 (130.2) | <0.01 |
| Inpatient Rehabilitation Facility | 743.6 (728.8) | 772.2 (715.0) | 0.02 |
| Skilled Nursing Facility | 715.5 (1038.4) | 728.8 (990.4) | 0.61 |
| Home Health Agency | 441.4 (572.4) | 469.9 (598.08) | <0.01 |
| Outpatient Setting | 555.0 (969.0) | 539.0 (1016.2) | 0.06 |
| Occupational Therapy | |||
| Any setting | 648.9 (1528.9) | 752.7 (1598.3) | <0.01 |
| Hospital | 73.6 (88.7) | 75.5 (103.8) | <0.01 |
| Inpatient Rehabilitation Facility | 767.8 (742.4) | 808.4 (750.1) | <0.01 |
| Skilled Nursing Facility | 724.3 (1026.1) | 752.7 (1026.1) | 0.07 |
| Home Health Agency | 282.5 (414.6) | 312.4 (416.4) | <0.01 |
| Outpatient Setting | 570.0 (1066.00) | 600.0 (1094.0) | 0.09 |
| Speech and Language Therapy | |||
| Any setting | 658.1 (2020.2) | 865.7 (2294.6) | <0.01 |
| Hospital | 101.6 (161.2) | 117.1 (163.3) | <0.01 |
| Inpatient Rehabilitation Facility | 719.9 (1134.8) | 750.7 (1163.6) | <0.01 |
| Skilled Nursing Facility | 1046.0 (1649.3) | 1176.9 (1766.4) | <0.01 |
| Home Health Agency | 891.9 (1383.5) | 844.9 (1361.3) | 0.06 |
| Outpatient Setting | 485.0 (1119.0) | 473.5 (1115.5) | 0.18 |
Figure 2.
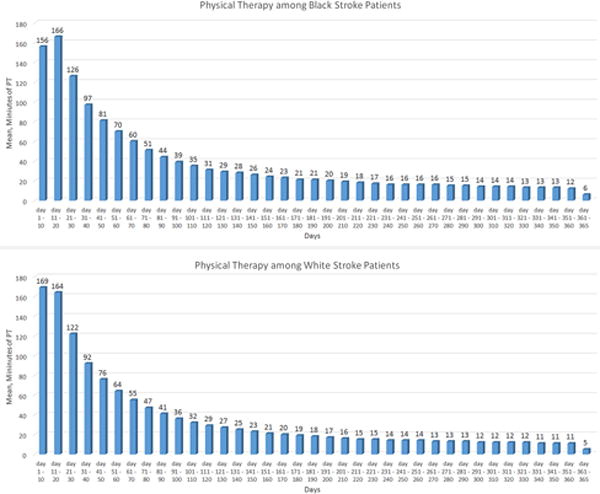
Distribution of Minutes of Physical Therapy by Days and Race among Stroke Patients in the Year Following their Stroke
Among stroke patients who received PT, after adjustments for demographics, comorbidities, thrombolysis, and markers of stroke severity, there was no racial difference in the amount of PT received in the 90 days or one year after their stroke (Supplemental Table II). Black stroke survivors received less PT within 30 days of their stroke than white stroke survivors. In secondary analysis, limited to patients who survived their hospitalization and were not discharged to hospice, black stroke survivors received slightly less PT at 30 days (20 minutes, 4%), 90 days (33 minutes, 4%) and 1 year (25 minutes, 2%) in the fully adjusted models.
Rehabilitation Transitions
The median number of transitions among stroke patients within the first year was 2 (IQR 1–5). Transitions were more common in blacks (mean 3.5, SD 3.3; median 3 IQR (1–5)) than whites (mean 3.0, SD 3.1; median 2 IQR (1–5), p < 0.01). There were multiple sequences of transitions in the stroke population, but there were no large racial differences in the transition patterns (Figure 3).
Figure 3.
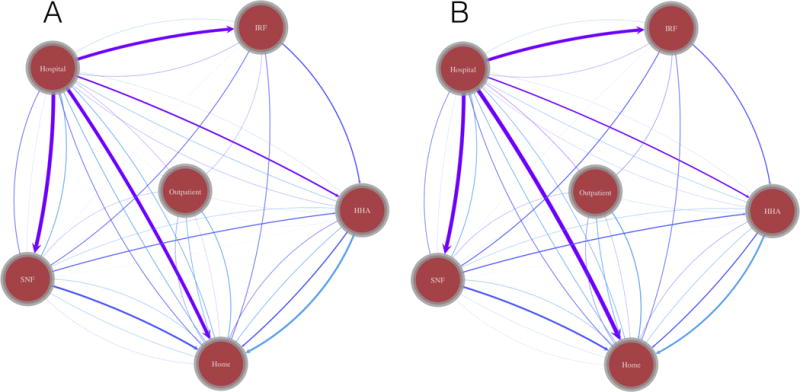
Transitions in care across Post-Acute Care Setting. A: White Stroke Patients. B: Black Stroke Patients
Discussion
For the first time, we report rehabilitation therapy utilization, intensity, and transitions across all PAC settings by elderly stroke patients for the year following their stroke. We found that stroke patients receive a substantial and variable amount of post-acute rehabilitation therapy in various settings. For example, over 85% of stroke patients received PT and those patients received a median of over 750 minutes of therapy in over 3 settings in the year following their stroke. While about a quarter of stroke patients received almost no rehabilitation therapy, thousands of stroke survivors received over 100 hours of therapy in the year after stroke. Contrary to our hypothesis, we found that there are no clinically significant differences in rehabilitation intensity or utilization after accounting for differences in patient characteristics.
Health disparities research has evolved from identifying and describing racial differences in health to exploring the drivers of disparities that can be used to guide interventions to encourage health equity. To date, the large race disparities in post-stroke disability remain unexplained.15 Our results suggest that differential utilization of rehabilitation therapies or time within rehabilitation therapies are unlikely to contribute to racial disparities in post-stroke disability among elderly stroke survivors. While we found that among stroke survivors who survive their hospitalization and are not discharged to hospice, blacks stroke patients receive slightly less PT than white stroke patients, the small magnitude (2% of annual) of this difference is unlikely to account for the much larger differences previously observed in post-stroke disability. We cannot, however, exclude the possibility that the quality of rehabilitation therapy varies by race and may contribute to post-stroke disability differences. However, given that rehabilitation therapy utilization and intensity are quite similar, very large racial differences in quality of care would be required to explain the large differences in functional outcomes. If utilization of rehabilitation therapies does not explain post-stroke racial disparities, what does? A wide variety of medical, social, and environmental factors may contribute to racial disparities in post-stroke outcomes. Of these possibilities, medical factors have been the most widely studied and while some racial differences exist, they are generally of small magnitude and unlikely to explain the wide differences in outcomes.25, 26 Further research is needed to understand racial differences in post-stroke disability.
Our data suggest one factor that may contribute to racial differences in post-stroke disability — discontinuous care and suboptimal transitions between settings. The median black stroke survivors received care in one more setting than the median white stroke survivor. Transitions across settings are a particularly vulnerable time for patients due to high rates of errors in medication, work-up, and incomplete transfer of medical information.27–29 The majority of data on care transitions are focused on one transition, from the hospital to home, and focus on outcomes such as hospital readmission.29 Lapses in quality of care may be even further increased in subsequent transitions or in patients with multiple transitions due to the increase in the number of opportunities for error and time from stroke. Further research to assess the consequences of care transitions in stroke patients, with particular attention to post-stroke disability, and strategies to optimize or decrease transitions are needed.
Our results have implications for initiatives designed to optimize the post-stroke continuum of care. The wide variation in the intensity of post-acute rehabilitation suggests that some stroke patients may be receiving too little post-acute rehabilitation therapy and/or others receiving too much. For example, we found that most stroke patients discharged home from a SNF do not receive home health services — a potential missed opportunity. Alternatively, strategies to decrease the numbers of transitions between settings may be of benefit to stroke survivors. Would a longer SNF stay directly transitioning to outpatient rehabilitation be preferable to a shorter stay with a bridge to outpatient rehabilitation via home health? Given that post-acute rehabilitation care is highly utilized, costly, and variable, determining the optimal intensity and setting of post-acute rehabilitation to reduce disability is important, particularly as Medicare explores changes to payments models.16
This study has limitations. We cannot directly measure stroke severity in administrative data, but given the lack of racial differences in stroke severity,30–32 this is unlikely to bias our findings. We do not know whether racial differences in recurrent stroke contribute to some of the observed racial differences. However, given the racial similarity of the transition patterns this is unlikely. Strokes were identified using ICD-9 codes which inaccurately classify some patients, but have been shown to have high positive predictive values supporting their use in stroke outcome studies.20, 33 It is possible that variation may exist in rehabilitation services among patients who do not have Medicare fee-for service insurance, as insurance status and coverage have influenced utilization of rehabilitation services.34, 35 Thus, our results should be cautiously extrapolated to middle aged stroke patients and those with other forms of insurance. We did not explore external factors that may impact PAC utilization. Some of these likely include payment models, PAC availability and hospital culture and should be considered in future studies.
In summary, black stroke patients undergo more frequent post-stroke transitions, but there are no clinically significant racial differences in the intensity of rehabilitation therapies in the year after a stroke. Further research is needed to explore alternate medical, social, and environmental factors, including transitions in care that may contribute to racial disparities in post-stroke disability.
Supplementary Material
Acknowledgments
Funding: This work was supported by the National Institute of Minority Health and Health Disparities (R01 MD008879) and National Institute of Aging at the National Institute of Health (U01AG032947). It was also supported by NIH/NINDS K23 NS073685 (Skolarus), NIH/NINDS K08NS082597 (Burke).
Footnotes
Disclosures: None
References
- 1.Feigin VL, Lawes CMM, Bennett DA, Anderson CS. Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurology. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics—2017 update: A report from the american heart association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kramer AM. Outcomes and costs after hip fracture and stroke: A comparison of rehabilitation settings. JAMA (Chicago, Ill) 1997;277:396–404. [PubMed] [Google Scholar]
- 5.Deutsch A, Granger CV, Heinemann AW, Fiedler RC, DeJong G, Kane RL, et al. Poststroke rehabilitation: Outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs. Stroke. 2006;37:1477–1482. doi: 10.1161/01.STR.0000221172.99375.5a. [DOI] [PubMed] [Google Scholar]
- 6.Lo AC, Guarino PD, Richards LG, Haselkorn JK, Wittenberg GF, Federman DG, et al. Robot-assisted therapy for long-term upper-limb impairment after stroke. New England Journal of Medicine. 2010;362:1772–1783. doi: 10.1056/NEJMoa0911341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Legg L. Rehabilitation therapy services for stroke patients living at home: Systematic review of randomised trials. The Lancet. 2004;363:352–356. doi: 10.1016/S0140-6736(04)15434-2. [DOI] [PubMed] [Google Scholar]
- 8.Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult stroke rehabilitation and recovery a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2016;47:e98–e169. doi: 10.1161/STR.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 9.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of Neurology. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and hispanic residents of an urban community: The northern manhattan stroke study. Am J Epidemiol. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 11.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, et al. Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater cincinnati/northern kentucky stroke study. Stroke. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burke JF, Freedman VA, Lisabeth LD, Brown DL, Haggins A, Skolarus LE. Racial differences in disability after stroke results from a nationwide study. Neurology. 2014;83:390–397. doi: 10.1212/WNL.0000000000000640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roth DL, Haley WE, Clay OJ, Perkins M, Grant JS, Rhodes JD, et al. Race and gender differences in 1-year outcomes for community-dwelling stroke survivors with family caregivers. Stroke. 2011;42:626–631. doi: 10.1161/STROKEAHA.110.595322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Differences in disability among black and white stroke survivors–united states, 2000–2001. MMWR Morb Mortal Wkly Rep. 2005;54:3–6. [PubMed] [Google Scholar]
- 15.Skolarus LE, Burke JF. Towards an understanding of racial differences in post-stroke disability. Current epidemiology reports. 2015;2:191–196. doi: 10.1007/s40471-015-0047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newhouse JP, Garber AM. Geographic variation in medicare services. New England Journal of Medicine. 2013;368:1465–1468. doi: 10.1056/NEJMp1302981. [DOI] [PubMed] [Google Scholar]
- 17.Freburger JK, Holmes GM, Ku L-JE, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in postacute rehabilitation care for stroke: An analysis of the state inpatient databases. Archives of Physical Medicine and Rehabilitation. 2011;92:1220–1229. doi: 10.1016/j.apmr.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horn SD, Deutscher D, Smout RJ, DeJong G, Putman K. Black-white differences in patient characteristics, treatments, and outcomes in inpatient stroke rehabilitation. Archives of Physical Medicine and Rehabilitation. 2010;91:1712–1721. doi: 10.1016/j.apmr.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 19.Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Archives of Physical Medicine and Rehabilitation. 2005;86:2081–2086. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Kumamaru H, Judd SE, Curtis JR, Ramachandran R, Hardy NC, Rhodes JD, et al. Validity of claims-based stroke algorithms in contemporary medicare data. Circulation: Cardiovascular Quality and Outcomes. 2014;7:611–619. doi: 10.1161/CIRCOUTCOMES.113.000743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tirschwell DL, Longstreth WT., Jr Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 22.Eicheldinger C. More accurate racial and ethnic codes for medicare administrative data. Health care financing review. 2008;29:27. [PMC free article] [PubMed] [Google Scholar]
- 23.Hhs-operated risk adjustment methodology meeting. 2016 Oct 1; https://www.cms.gov/CCIIO/Resources/Forms-Reports-and-Other-Resources/Downloads/RA-March-31-White-Paper-032416.pdf.
- 24.Burke JF, Skolarus LE, Adelman EE, Reeves MJ, Brown DL. Influence of hospital-level practices on readmission after ischemic stroke. Neurology. 2014;82:2196–2204. doi: 10.1212/WNL.0000000000000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dhamoon M, Sciacca R, Rundek T, Sacco R, Elkind M. Recurrent stroke and cardiac risks after first ischemic stroke the northern manhattan study. Neurology. 2006;66:641–646. doi: 10.1212/01.wnl.0000201253.93811.f6. [DOI] [PubMed] [Google Scholar]
- 26.Howard G, Kissela BM, Kleindorfer DO, McClure LA, Soliman EZ, Judd SE, et al. Differences in the role of black race and stroke risk factors for first vs recurrent stroke. Neurology. 2016;86:637–642. doi: 10.1212/WNL.0000000000002376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. Journal of General Internal Medicine. 2003;18:646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coleman EA, Smith JD, Raha D, Min S. Posthospital medication discrepancies: Prevalence and contributing factors. Archives of Internal Medicine. 2005;165:1842–1847. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
- 29.Coleman EA, Berenson RA. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Annals of Internal Medicine. 2004;141:533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 30.Hartmann A, Rundek T, Mast H, Paik M, Boden–Albala B, Mohr J, et al. Mortality and causes of death after first ischemic stroke the northern manhattan stroke study. Neurology. 2001;57:2000–2005. doi: 10.1212/wnl.57.11.2000. [DOI] [PubMed] [Google Scholar]
- 31.Kleindorfer D, Lindsell C, Alwell KA, Moomaw CJ, Woo D, Flaherty ML, et al. Patients living in impoverished areas have more severe ischemic strokes. Stroke. 2012;43:2055–2059. doi: 10.1161/STROKEAHA.111.649608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qian F, Fonarow GC, Smith EE, Xian Y, Pan W, Hannan EL, et al. Racial and ethnic differences in outcomes in older patients with acute ischemic stroke. Circulation: Cardiovascular Quality and Outcomes. 2013;6:284–292. doi: 10.1161/CIRCOUTCOMES.113.000211. [DOI] [PubMed] [Google Scholar]
- 33.Tirschwell DL, Longstreth W. Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 34.Skolarus LE, Burke JF, Morgenstern LB, Meurer WJ, Adelman EE, Kerber KA, et al. Impact of state medicaid coverage on utilization of inpatient rehabilitation facilities among patients with stroke. Stroke. 2014;45:2472–2474. doi: 10.1161/STROKEAHA.114.005882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skolarus L, Meurer W, Burke J, Bettger JP, Lisabeth L. Effect of insurance status on postacute care among working age stroke survivors. Neurology. 2012;78:1590–1595. doi: 10.1212/WNL.0b013e3182563bf5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


