Supplemental Digital Content is available in the text
Keywords: chlorhexidine, meta-analysis, total knee arthroplasty
Abstract
Background:
Surgical site infection is a devastating postoperative complication, and the occurrence ranges from 1% to 2% after total knee arthroplasty (TKA). The efficacy of the preoperative use of chlorhexidine for reducing infection has been debated. This meta-analysis aimed to examine the efficacy of the use of chlorhexidine to prevent surgical site infections after TKA.
Methods:
In February 2017, a systematic literature review was conducted using the following electronic databases: PubMed, EMBASE, Web of Science, Cochrane Database of Systematic Reviews, and the Google database. Data from randomized controlled trials (RCTs) and retrospective comparative study (RCS) that compared the use of chlorhexidine versus control washes to prep patients for TKA were retrieved. The primary endpoint was to compare the total incidence of infection with and without the use of chlorhexidine. The secondary outcomes were the incidence of infection in low-risk category patients, moderate-risk category patients, and high-risk category patients. After testing for publication bias and heterogeneity between studies, data were aggregated for random-effects modeling when necessary.
Results:
Four clinical trials that included 8787 patients (chlorhexidine group: n = 2615, control group: n = 6172) were ultimately included in the meta-analysis. Chlorhexidine was associated with a reduced total incidence of infection, corresponding to a reduction of 1.69% [risk ratio (RR) = 0.22; 95% confidence interval (95% CI) = 0.12–0.40; P = .000]. Similarly, chlorhexidine was associated with a reduction in the incidence of infection among patients in the moderate-risk category (RR, 0.18; 95% CI, 0.05–0.63; P = .007) and the high-risk category (RR, 0.13; 95% CI, 0.03–0.67; P = .014). There was no significant difference between the incidence of infection in low-risk category patients with chlorhexidine use compared with the use of control washes (RR, 0.60; 95% CI, 0.22–1.60; P = .330).
Conclusion:
The preoperative use of chlorhexidine could reduce the total incidence of infection and the incidence of infection in moderate-risk and high-risk category patients. The overall evidence and the number of included studies was limited; thus, a greater number of high-quality RCTs is still needed to further identify the effects of chlorhexidine on reducing the incidence of infection after TKA.
1. Introduction
Total knee arthroplasty (TKA) is one of the most successful procedures for decreasing pain and improving function in patients with end-stage knee osteoarthritis.[1] Nevertheless, site infection complications will prolong a treatment period that may last for several months. Infection is one of the most devastating postsurgical complications, and the rate of occurrence after TKA ranges from 1% to 2%.[2,3] Furthermore, the incidence reaches 10% in TKA revisions.[4] Sources of wound infection following TKA include airborne bacteria in the operating room and native skin flora.[5] Numerous methods have been developed for reducing the incidence of surgical site infections following TKA. Bathing with antiseptic agents on the evening before surgery is recommended by the Centers for Disease Control and Prevention and is the standard-of-care.[6] Chlorhexidine exerts its bactericidal effects through direct disruption of the organisms’ membrane permeability and is thus an effective broad-spectrum biocide agent.[7] Several studies have shown that chlorhexidine was efficacious to decrease postoperative infection risk.[8] However, another clinical trial did not support the routine administration of chlorhexidine for the prevention of surgical site infections.[7] A previous meta-analysis investigated the efficacy of the preoperative use of chlorhexidine to prevent surgical site infection in patients undergoing TKAs and total hip arthroplasties (THAs)[9]; however, because that study included both patients undergoing TKA and patients undergoing THA, we cannot determine whether chlorhexidine is certain to have exerted a significant influence on infection after TKA. Thus, we selected relevant studies from the electronic databases and used the summarized data to perform a meta-analysis to examine the effects of preoperative bathing with chlorhexidine on the incidence of surgical site infection after TKA.
2. Materials and methods
This meta-analysis was conducted in accordance with the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions[10] and was written in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) checklist.[11]
2.1. Search strategy and study selection
The following electronic databases were systematically searched from their inception through February 2017: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, and the Google database. The detailed PubMed search strategy was as follows: ((((chloraprep) OR chlorhexidine-isopropyl) OR chlorhexidine-alcohol)) AND (((((“Arthroplasty, Replacement, Knee”[Mesh]) OR TKR) OR TKA) OR total knee replacement) OR total knee arthroplasty). Meta-analysis was collected data from published papers and thus no ethical approval was need for this meta-analysis.
2.2. Eligibility criteria
-
1.
Participants: Patients who underwent TKA (including primary TKA and TKA revisions).
-
2.
Interventions: Chlorhexidine was used preoperatively for the intervention group.
-
3.
Comparisons: No chlorhexidine was used preoperatively for the comparison group.
-
4.
Outcomes: Total infection rate and incidence of surgical site infection stratified by risk category.
-
5.
Study design: RCTs and retrospective comparative study (RCS) were included.
2.3. Data extraction and outcome measures
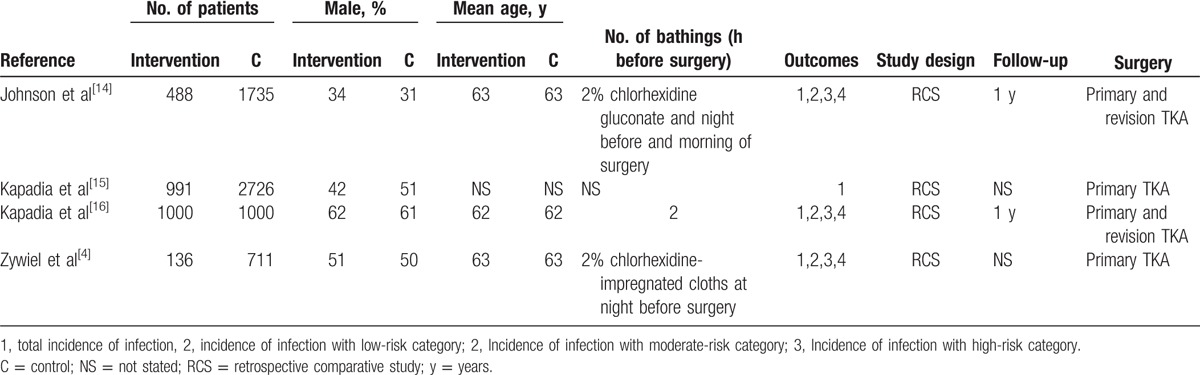
For each published study included in the meta-analysis, 2 authors independently extracted the following data: author, publication year, number of patients in the intervention and control groups, proportion of male patients, mean age of the patients, outcomes, duration of the follow-up period, and surgery type. Any disagreement was resolved by discussion. In the present meta-analysis, patient infection risk categories were classified according to the National Healthcare Safety Network surgical risk rating system.[12,13] The detailed information can be seen in Table 1.[4,14–16] The outcome measures were total infection rate, and the infection rate among low-risk, moderate-risk, and high-risk category patients. If the data were not reported numerically, we extracted the mean and standard deviation values using GetData Graph Digitizer software (Xinzhong Co, Beijing, China) as needed.[10]
Table 1.
The general characteristic of the included studies.
2.4. Risk of bias assessment
Two reviewers independently evaluated the risk of bias in non-RCTs according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions[10]; the assessment criteria were assessed by the Newcastle–Ottawa Scale (NOS) as previously described.[17]
2.5. Quality of evidence assessment
Two reviewers independently evaluated the quality of evidence assessment in accordance with the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology.[18] Assessment items included the following: risk of bias, inconsistency, indirectness, imprecision, and publication bias.[18,19] The quality of evidence of each result was classified as high, moderate, low, or very low. GRADE Pro software (Grade co. California) was used to construct summary tables for the included studies.
2.6. Statistical analysis
For dichotomous outcomes (total incidence of infection and the incidence of infection in low-risk, moderate-risk, and high-risk category patients), we calculated the risk ratio (RR) and the 95% confidence interval (CI). Heterogeneity was considered to be statistically significant if the I2 value was greater than 50%. A fixed-effects model was applied if the I2 value was less than 50%. All statistical analyses were conducted using Stata 12.0 (Stata Corp., College Station, TX). A P value less than .05 was considered statistically significant. Kappa values were used to measure the degree of agreement between the 2 reviewers and were rated as follows: fair, 0.40 to 0.59; good, 0.60 to 0.74; and excellent, 0.75 or higher.[20]
3. Results
3.1. Search results
The literature search and selection process are illustrated in Fig. 1. The initial search yielded 158 articles (PubMed = 92, Embase = 18, Web of Science = 32, Cochrane Library = 6, Google database = 10). After excluding duplications, 132 studies were examined. Next, 127 of the 132 studies were excluded on the basis of the inclusion criteria. One additional study was excluded, as it included both TKA and THA.[8] Finally, the remaining 4 clinical studies with 8787 patients (chlorhexidine group n = 2615, control group n = 6172) were included in this meta-analysis.[4,14–16]
Figure 1.
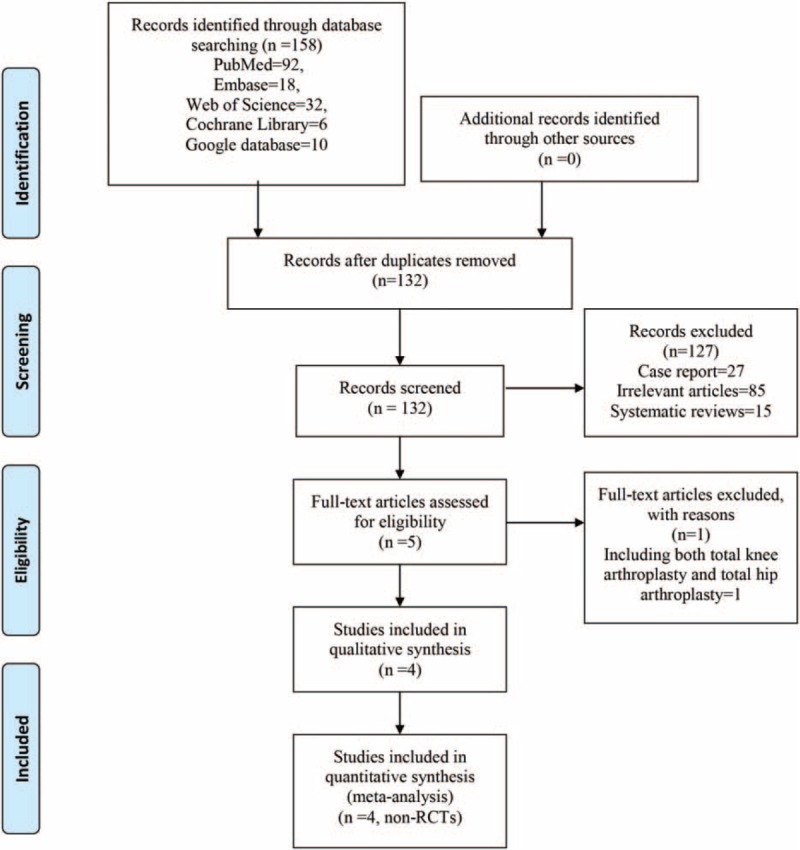
PRISMA flow chart of retrieved studies.
3.2. Study characteristics
Detailed baseline characteristics of the included studies are presented in Table 2. Four studies were included in the meta-analysis. All articles were published in English between 2011 and 2016. The sample sizes ranged from 136 to 2726 (total = 8787), and the mean ages ranged from 62 to 63 years. The follow-up period was 1 year in 2 studies and the rest 2 studies did not state the follow-up period.
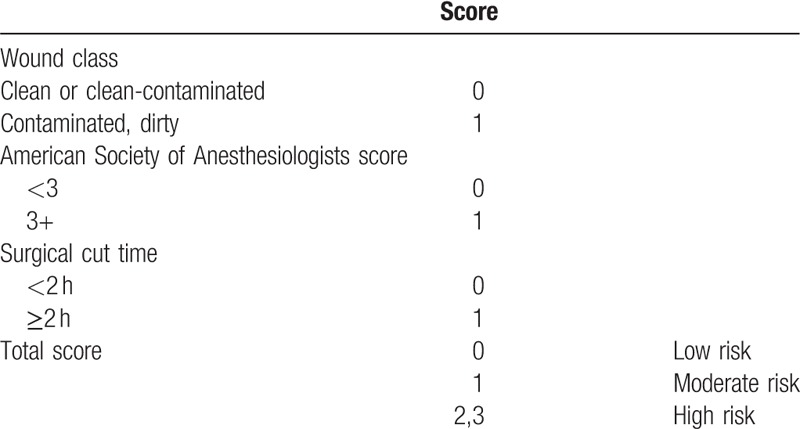
Table 2.
Patient infection risk categories according to the National Healthcare Safety Network surgical risk rating system.
3.3. Risk of bias among the included studies
Supplement S1 presents the details of the risk of bias assessment for each included study. The total scores of Johnson et al,[14] Kapadia et al,[15] Kapadia et al,[16] and Zywiel et al[4] were 18, 24, 17, and 23, respectively. The overall kappa value regarding the evaluation of risk of bias in the included RCS was 0.872, indicating an excellent degree of agreement between the 2 reviewers.
3.4. Quality of evidence assessment
A summary of the quality of the evidence as assessed according to the GRADE methodology is shown in Supplement S2. The level of evidence was classified as “low” according to the GRADE methodology for all outcomes including the total incidence of infection, and the incidence of infection in the low, moderate, and high-risk categories.
3.5. Total incidence of infection
Data regarding the total incidence of infection were available for 4 studies,[4,14–16] which included a total of 8787 patients. The pooled RR for all patients showed no significant heterogeneity (I2 = 0.0%, P = .824). Analysis revealed that the preoperative use of chlorhexidine could reduce the incidence of surgical site infections by 1.69% (RR, 0.22; 95% CI, 0.12–0.40; P = .000, Fig. 2).
Figure 2.
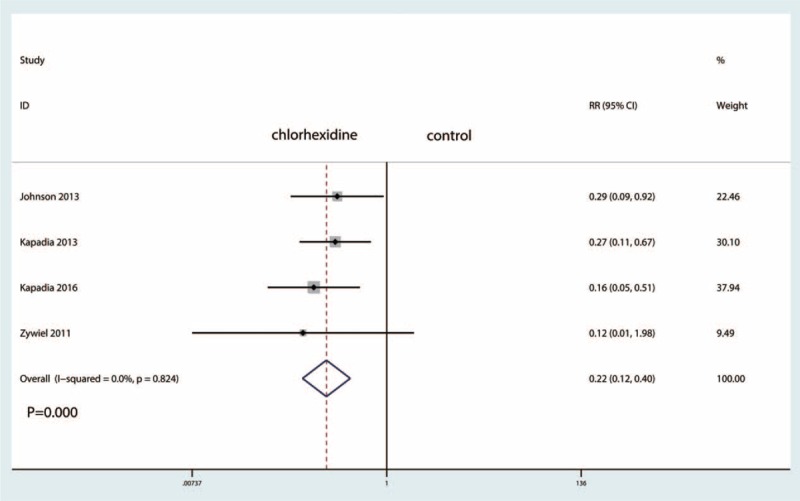
Forest plot comparing the total incidence of infection between the 2 groups.
3.6. Incidence of infection in low-risk category patients
The incidence of infection among low-risk category patients was examined in 3 trials,[4,14,16] which included a total of 2606 patients. The pooled RR for all patients revealed no significant heterogeneity (I2 = 0.0%, P = .858). The results showed that the preoperative use of chlorhexidine could reduce the incidence of infection in low-risk category patients by 0.52%. However, the difference was not statistically significant (RR, 0.60; 95% CI, 0.22–1.60; P = .330, Fig. 3).
Figure 3.
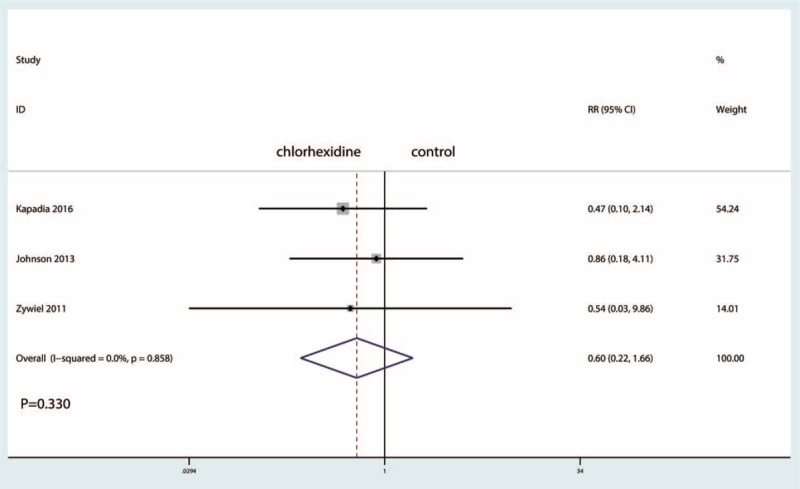
Forest plot comparing the incidence of infection in the low-risk category patients.
3.7. Incidence of infection in moderate-risk category patients
The incidence of infection among moderate-risk category patients was examined in 3 trials,[4,14,16] which included a total of 2985 patients. The pooled RR for all patients revealed no significant heterogeneity (I2 = 0.0%, P = .835). The results showed that the preoperative use of chlorhexidine could reduce the incidence of infection among moderate-risk category patients by 1.95% (RR, 0.18; 95% CI, 0.05–0.63; P = .007, Fig. 4).
Figure 4.
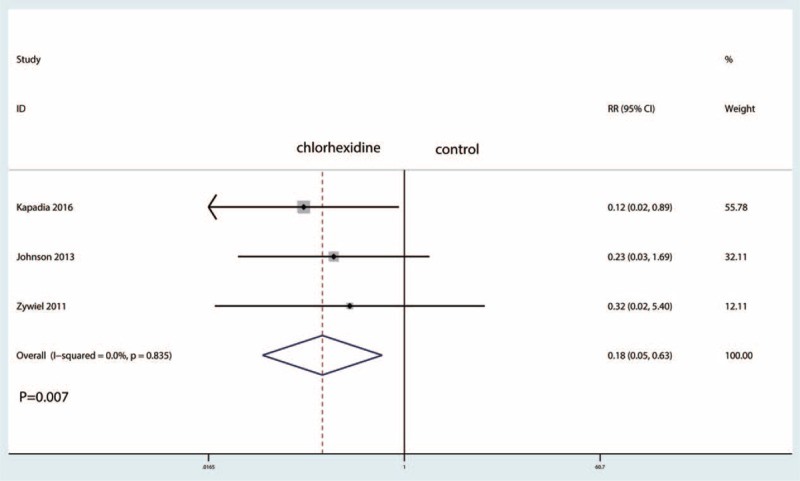
Forest plot comparing the incidence of infection in the moderate-risk category patients.
3.8. Incidence of infection among high-risk category patients
The incidence of infection among high-risk category patients was examined in 3 trials,[4,14,16] which included a total of 1186 patients. The pooled RR for all patients revealed no significant heterogeneity (I2 = 0.0%, P = .910). The results showed that the preoperative use of chlorhexidine could reduce the incidence of infection among high-risk category patients by 4.15% (RR, 0.13; 95% CI, 0.03–0.67; P = .014, Fig. 5).
Figure 5.
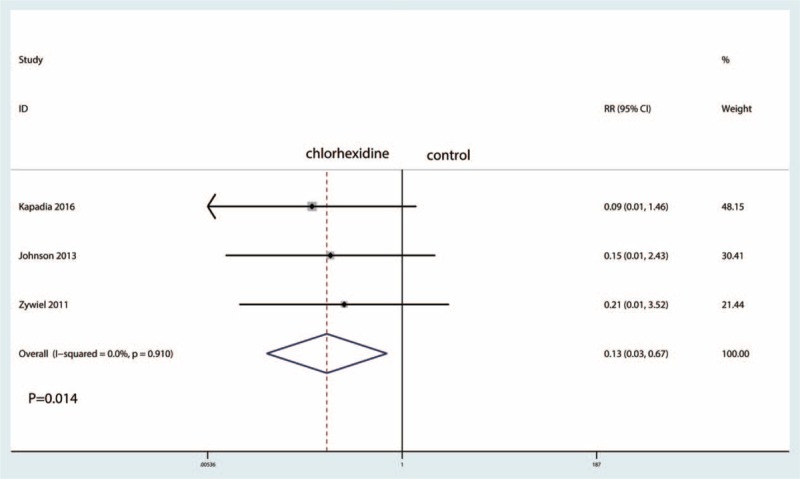
Forest plot comparing the incidence of infection in the high-risk category patients.
4. Discussion
To the best of our knowledge, this is the first systematic review and meta-analysis regarding the efficacy of the preoperative use of chlorhexidine for reducing the incidence of site infections after TKA. All included studies were RCS. The pooled results indicated that the preoperative use of chlorhexidine is effective for the prevention of surgical site infection and that the use of chlorhexidine could reduce the incidence of infection among moderate-risk and high-risk category patients. There was no significant difference in the incidence of infection among low-risk category patients with or without chlorhexidine use. The effect of chlorhexidine on the incidence of infection for the different infection risk category was further analyzed. There was no significant difference in the incidence of infection with or without chlorhexidine use in low-risk category patients (P > .05). The low-risk category included clean or clean-contaminated wounds, and the surgical cut time was always less than 2 hours. The final results indicated that the preoperative use of chlorhexidine could reduce the incidence of infection among moderate-risk and high-risk category patients by 1.95% and 4.15%, respectively. Thus, the antibiosis effects of chlorhexidine were most obvious in the high-risk category patients.
Although the benefit was conclusive, the level of evidence, which was undermined by the risk of bias and/or publication bias, was classified as “low,” indicating that the degree of benefit of chlorhexidine in preventing surgical site infections must be further studied. RCS may have potential selection risk of bias and cause large heterogeneity for the final outcomes. A major strength of the current analysis is the use of a comprehensive search with strict statistical calculations. Furthermore, number need to treat (NNT) was used to analyze the benefit of chlorhexidine for reducing the infection rate, and a quality of evidence assessment was performed to assess the quality of present evidence for the use of chlorhexidine to reduce the incidence of surgical site infection.
A considerable number of studies have addressed the accurate diagnosis and effective treatments for surgical site infections after TKA. Current strategies include showering or bathing the night before surgery, and washing the incision site before antiseptic skin preparation to prevent the peri-prosthetic infections.[4,14–16] However, there was inconclusive evidence regarding the optimal preoperative preparation.[4,14,16] Chlorhexidine's bactericidal effect results from the binding of cationic molecules found in the solution to the anionic molecules of the bacterial cell wall. The current meta-analysis indicated that the preoperative use of chlorhexidine could reduce the total infection rate by 1.69%. Eiselt [21] revealed that the rate of surgical site infections was 3.19% with the use of a povidone-iodine wash, and this rate decreased to 1.59% with the use of chlorhexidine cloths in orthopedic surgeries. Webster and Osborne[22] conducted a meta-analysis that found no clear evidence of benefit for preoperative showering or bathing with chlorhexidine over other the use of other wash products for reducing the incidence of surgical site infections. In 2015, an updated meta-analysis found similar results.[23] The conclusion of these meta-analyses is in opposition to the findings of the present meta-analysis, possibly due to differences in infection risk categories. Previous studies included all types of surgeries and did not differentiate between infection risk categories in determining the benefit of chlorhexidine.
One issue that should be considered when examining the use of chlorhexidine is the mean chlorhexidine skin concentration. Edmiston et al[24] revealed that using 4% chlorhexidine soap or a 2% chlorhexidine cloth is the optimal concentration on this skin. What is more, Kapadia et al[15] reported that the cost–benefit analysis of using chlorhexidine at their institution, per 1000 TKA patients, showed a net savings of approximately $2.1 million due to the costs of treating surgical site infections. However, only 1 study reported this outcome; thus, more clinical trials are needed to identify the economic savings of using chlorhexidine.
There were several limitations in this meta-analysis: only 4 RCS were included, which might have a selective risk of bias; the follow-up period was relatively short in the included studies, and the infection rate may have been thus underestimated; and publication bias may have existed due to the limited number of included studies.
5. Conclusion
The preoperative use of chlorhexidine could reduce the total incidence of infection and the incidence of infection in moderate-risk and high-risk category patients. In addition, chlorhexidine possesses greater economic-sparing effects than the washes used in the control group. The overall evidence and the number of included studies was limited; thus, more high-quality RCTs are still needed to further identify the efficacy of chlorhexidine for reducing the incidence of infection after TKA.
Supplementary Material
Footnotes
Abbreviations: CENTRAL = Cochrane Central Register of Controlled Trials, CI = confidence interval, GRADE = Grading of Recommendations, Assessment, Development and Evaluation, NNT = number need to treat, NOS = Newcastle–Ottawa Scale, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-analyses, RCS = retrospective comparative study, RCT = randomized controlled trials, RR = risk ratio, THA = total hip arthroplasty, THAs = total hip arthroplasties, TKA = total knee arthroplasty.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
References
- [1].Dong CC, Dong SL, He FC. Comparison of adductor canal block and femoral nerve block for postoperative pain in total knee arthroplasty: a systematic review and meta-analysis. Medicine 2016;95:e2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kurtz SM, Lau E, Schmier J, et al. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty 2008;23:984–91. [DOI] [PubMed] [Google Scholar]
- [3].Kurtz SM, Ong KL, Lau E, et al. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res 2010;468:52–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Zywiel MG, Daley JA, Delanois RE, et al. Advance pre-operative chlorhexidine reduces the incidence of surgical site infections in knee arthroplasty. Int Orthop 2011;35:1001–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Fairclough JA, Johnson D, Mackie I. The prevention of wound contamination by skin organisms by the pre-operative application of an iodophor impregnated plastic adhesive drape. J Int Med Res 1986;14:105–9. [DOI] [PubMed] [Google Scholar]
- [6].Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20:250–78. quiz 279-280. [DOI] [PubMed] [Google Scholar]
- [7].Franco LM, Cota GF, Pinto TS, et al. Preoperative bathing of the surgical site with chlorhexidine for infection prevention: systematic review with meta-analysis. Am J Infect Control 2017;45:343–9. [DOI] [PubMed] [Google Scholar]
- [8].Kapadia BH, Elmallah RK, Mont MA, et al. Clinical trial of preadmission chlorhexidine skin preparation for lower extremity total joint arthroplasty. J Arthroplasty 2016;31:2856–61. [DOI] [PubMed] [Google Scholar]
- [9].Cai Y, Xu K, Hou W, et al. Preoperative chlorhexidine reduces the incidence of surgical site infections in total knee and hip arthroplasty: a systematic review and meta-analysis. Int J Surg (London, England) 2017;39:221–8. [DOI] [PubMed] [Google Scholar]
- [10].Higgins JPT GS. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011. Available at: http://www.cochrane-handbook.org. access date 2011. [Google Scholar]
- [11].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed) 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 2004;32:470–85. [DOI] [PubMed] [Google Scholar]
- [13].Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 1991;91:152s–7s. [DOI] [PubMed] [Google Scholar]
- [14].Johnson AJ, Kapadia BH, Daley JA, et al. Chlorhexidine reduces infections in knee arthroplasty. J Knee Surg 2013;26:213–8. [DOI] [PubMed] [Google Scholar]
- [15].Kapadia BH, Johnson AJ, Issa K, et al. Economic evaluation of chlorhexidine cloths on healthcare costs due to surgical site infections following total knee arthroplasty. J Arthroplasty 2013;28:1061–5. [DOI] [PubMed] [Google Scholar]
- [16].Kapadia BH, Zhou PL, Jauregui JJ, et al. Does preadmission cutaneous chlorhexidine preparation reduce surgical site infections after total knee arthroplasty? Clin Orthop Relat Res 2016;474:1592–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [18].Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed) 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Guyatt GH, Oxman AD, Kunz R, et al. What is “quality of evidence” and why is it important to clinicians? BMJ (Clinical research ed) 2008;336:995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Eiselt D. Presurgical skin preparation with a novel 2% chlorhexidine gluconate cloth reduces rates of surgical site infection in orthopaedic surgical patients. Orthop Nurs 2009;28:141–5. [DOI] [PubMed] [Google Scholar]
- [22].Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev 2012;9:Cd004985. [DOI] [PubMed] [Google Scholar]
- [23].Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev 2015;Cd004985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Edmiston CE, Jr, Krepel CJ, Seabrook GR, et al. Preoperative shower revisited: can high topical antiseptic levels be achieved on the skin surface before surgical admission? J Am Coll Surg 2008;207:233–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


