Abstract
Bariatric surgery is an effective and durable treatment for individuals with obesity and its associated comorbidities. However, not all patients meet weight loss and/or cardiometabolic goals following bariatric surgery, suggesting that some people are “bariatric surgery resistant”. The reason for this resistance is unclear, but potential factors, such as adiposity-derived inflammation, insulin resistance, hyperglycemia, and aerobic fitness prior to surgery have been related to blunted surgery responsiveness. Exercise, diet, and/or pharmacology are effective at reducing inflammation and improving insulin action as well as physical function. Herein, we present data that supports the novel hypothesis that intervening prior to surgery can enhance disease resolution in people who are resistant to bariatric surgery.
Keywords: Bariatric surgery, insulin resistance, diet, exercise, pharmacology, weight loss surgery
Introduction
Nearly 34% of adults are obese (BMI ≥ 30 kg/m2) in the United States [1]. Obesity impacts public health as its associated comorbidities [2–4] result in higher health care costs [5] and lead to an elevated risk for all-cause mortality [6]. Thus, optimal therapies are drastically needed to combat obesity and reduce healthcare costs.
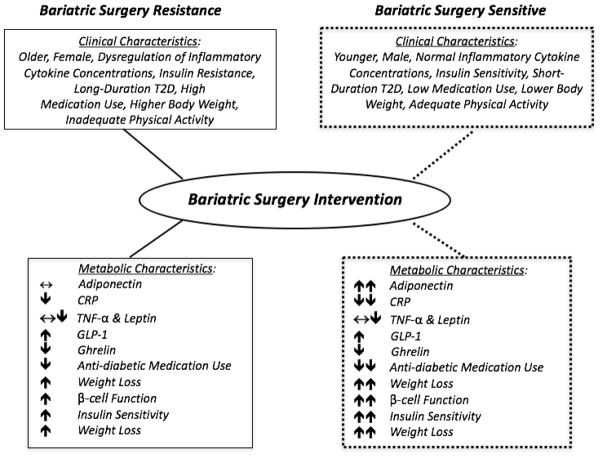
Lifestyle medicine, including diet and exercise, is established to induce meaningful weight loss and aerobic fitness for cardiometabolic benefit. However, long-term adherence to exercise and diet treatments are poor for the vast majority of patients. In fact, nearly 54% of people experiencing weight loss within the first year of lifestyle modification subsequently experience weight regain [7]. These observations suggest that alternative treatments are required to induce and maintain long-term weight loss. Medication is a reasonable adjunctive therapy to lifestyle treatment, but the optimal combination therapy remains unclear and no current therapies are approved for combination use [8–10]. Bariatric surgery, namely Roux-en-Y gastric bypass (RYGB) or Sleeve Gastrectomy (SG), is an effective treatment for individuals with obesity that often results in greater than 50% loss of excess body weight [11]. In addition, surgery decreases insulin resistance and improves pancreatic function, thereby conferring improved glucose regulation [11]. In fact, approximately 42% of individuals with T2D have remission following bariatric surgery [12–13], and nearly 60% of patients experience resolution of hypertension, hypercholesterolemia, hypertriglyceridemia, obstructive sleep apnea, and gastroesophageal reflux disease [14,15]. Unfortunately, not all patients undergoing bariatric surgery achieve these improvements in metabolic health. The exact reason for this large inter-subject variability to bariatric surgery outcomes is unclear, but pre-operative age, sex, race, body mass index (BMI), and diabetes status are reported determinants associated with non-responsiveness to surgery. Moreover, weight regain is a key underlying factor during the post-operative period that correlates with disease relapse. Herein, we review data in support of the novel hypothesis that pre-surgical interventions may reduce surgical complications, improve recovery and promote metabolic responsiveness post-operation. Thus, the present review will discuss current literature highlighting the clinical and physiologic underpinnings of “bariatric surgery resistant” individuals (Figure 1). In addition, this review will focus on the utility of exercise and diet before surgery as potential therapies that improve sensitivity to surgery and promote weight loss, glycemic control, and cardiometabolic health. Lastly, this review will provide a clinical perspective for optimization of pharmacological agent use to assist with additional weight loss and metabolic health.
Figure 1.
Summary of potential phenotype and mechanisms underlying the differences in patients with bariatric resistance versus bariatric sensitive before and after surgery. T2D = Type 2 diabetes. CRP = C-reactive protein. TNF-α = tumor necrosis factor-α. GLP-1 = glucagon-like peptide-1. GIP = glucose-dependent insulinotropic polypeptide.
Bariatric Surgery Resistance
Multi-factorial elements are associated with an individual’s resistance to bariatric surgery-induced weight loss and CVD risk reduction. Aging has been suggested to predict blunted weight loss after surgery [16–17]. When compared with adults ≥ 60 years, younger individuals experienced significantly greater weight loss at 1 and 5 years post bariatric surgery [18]. These findings may have clinical relevance as older individuals have a 3-fold higher risk of mortality from surgical complications than their younger counterparts [19]. Others have reported that older adults are at increased risk for sarcopenia and insulin resistance, potentially providing an explanation for increased surgical risk and attenuated weight loss with age [20–21]. Sex may also contribute to bariatric surgery resistance. Women have been reported to experience less weight loss than men [16]. Although this finding is consistent with “diet plus exercise” literature [22], it is worth considering that differences in hormones between men and women, including endogenous sex hormones, leptin, and ghrelin, could be in part related to bariatric surgery resistance due to their link to metabolic disease. A systematic review reported that high levels of testosterone is associated with a higher risk of T2D in women, independent of BMI and central adiposity, but lower risk in men [23]. Leptin concentrations vary between the sexes, as woman have higher concentrations of leptin per unit of fat mass than men [24]. Individuals who are obese are thought to be leptin resistant which alters eating behavior and satiety and could result in a greater caloric intake [25–26]. Women also have elevated ghrelin levels that are associated with a higher total fat mass, while in men, ghrelin is primarily related to central adiposity [27–28]. Given the link between ghrelin promoting insulin resistance [29], and the differential impact ghrelin has in women and men, it is possible that differences in ghrelin hormone profiles may explain why women have reduced weight loss responsiveness to bariatric surgery. Race/ethnicity are additional key clinical factor explaining bariatric surgery resistance. In particular, Hispanic and African American patients experience less weight loss following bariatric surgery than Caucasian patients [30–31]. This observation may be related to observations that Hispanic patients seem to have a higher genetic predisposition for metabolic syndrome, as evidence by the higher disease prevalence compared with African American and Caucasian patients. This suggests that race/ethnicity driven metabolic risk may explain attenuated responses to surgery [32–36]. Although not the purpose of the present review, it is important to consider that psychosocial factors including but not limited to eating behavior, eating disorders, mental illness, substance abuse, and socioeconomic status may also contribute to bariatric surgery resistance [37–40]. In summary, targeting metabolically modifiable risk factors with lifestyle medicine in high-risk populations may be beneficial for bariatric surgery resistant patients.
Independent of age, sex, and race/ethnicity, inflammation is an important etiological factor in obesity that promotes insulin resistance and may affect response to bariatric surgery [3–4]. In particular, increased white adipose tissue in the abdominal visceral region increases the expression of macrophages and inflammatory cytokines including TNF-α and interleukin-6 that in turn leads to elevated systemic inflammation [4, 41]. Moreover, increased inflammation in adipose tissue down-regulates adiponectin, which exacerbates systemic insulin responsiveness in tissues including skeletal muscle and liver. This is problematic as insulin resistance promotes β-cell dysfunction, endothelial dysfunction, hyperglycemia and increased risk for cardiovascular disease [3,4,42]. Bariatric surgery reduces pro-inflammatory cytokines in association with weight loss, and this reduced inflammation correlates with improved insulin sensitivity and brachial artery reactivity [42–44]. These findings are consistent with work by our group showing that individuals who had non-remission of T2D after bariatric surgery were characterized by smaller changes in C-reactive protein and adiponectin compared with those with remission [45]. Thus, pre-operative inflammation may be an important biomarker of bariatric surgery responsiveness [46]. Although others suggest that weight loss is at least partially responsible for changes in inflammation and elevated adiponectin levels [47–49], targeting inflammation has received little attention in the pre-surgical period. Whether reducing inflammation is an important aspect of bariatric surgery responsiveness to promote metabolic health improvement remains to be tested.
Additional factors that may affect individual responsiveness to bariatric surgery are insulin resistance and hyperglycemia. Insulin resistance is a complex physiological response caused by genetic and environmental factors that lead to dysregulation of metabolic control. Over time, the pancreas is unable to secrete compensatory levels of insulin to maintain glycemic control, thereby resulting in hyperglycemia. As such, it is currently unclear if insulin resistance per se, or the developed hyperglycemia explains attenuated bariatric surgery responses. Indeed, hyperglycemia has been shown to promote toxic effects on the pancreas and decrease insulin secretion capacity, as reflected by reductions in β-cell volume and alterations in pulsatile insulin release [50–51]. This would be consistent with recent work highlighting that pre-operative HbA1c > 10%, T2D duration, and anti-diabetes medication treatment all correlate with T2D non-remission following bariatric surgery [52–55]. Work by our group using the DiaREM score, which is a system to predict the probability of remission of T2D after RYGB surgery, supports the notion that the more severe forms of T2D status prior to surgery relates to non-remission state, even 10 years post-surgery [56]. These studies suggest that hyperglycemia at the time of bariatric surgery may itself play a role in bariatric surgery resistance, or it could be hypothesized that the physiologic factors regulating glucose, including insulin resistance or β-cell dysfunction, may be important targets to improve bariatric surgery outcomes. In support of this hypothesis, Gavin et al. recently reported that people with long duration T2D are characterized as being more insulin resistant prior to RYGB surgery, and thus, are more likely to have blunted T2D remission up to 3 months post-surgery [51]. We showed that long duration T2D is characterized by dampened reductions in HbA1c that were paralleled by having greater β-cell dysfunction prior to bariatric surgery than people with short-duration diabetes [57]. Collectively, these findings suggest that lowering glucose levels and/or improving insulin action prior to surgery can be an important therapeutic target for minimizing surgical complications and improving bariatric surgery sensitivity.
Bariatric Surgery Resistance May Be Associated with Surgical Outcomes
Targeting modifiable risk factors in the pre-operative period may reduce bariatric surgery resistance and possibly improve surgical outcomes. Intra- and post-operative complications from bariatric surgery occur in < 10% of procedures and include, but are not limited to, wound infections, anastomotic leak, and abdominal sepsis [58–59]. The exact reason why these surgical complications vary is unclear, but obesity-induced inflammation and/or hyperglycemia may relate to surgical complications, prolonged operating time, and length of stay. Evidence indicates that surgical risk is associated with the specific bariatric procedure (RYGB > SG) and the patient’s age, degree of obesity, and co-morbidities [59–60]. The Longitudinal Assessment of Bariatric Surgery Consortium (LABS) study reported that patients who had a history of deep-vein thrombosis, venous thromboembolism, and elevated BMI were at higher risk for post-surgical death, deep-vein thrombosis, venous thromboembolism, re-intervention, or failure to be discharged by 30 days post surgery [61]. Although no study to date has specifically linked inflammation, insulin resistance or hyperglycemia to the likelihood of bariatric surgery resistance, this prior work [59–61] suggests that there is a relationship between compromised cardiometabolic health and increased surgical risk. In fact, these findings are consistent with data showing that obesity is strongly related to individuals accumulating less than 150 minutes/week of moderate-to-vigorous physical activity and having low functional capacity. The physical inactivity reported in obese patients may be clinically relevant since the inability to climb 2 flights of stairs or walk 2 city blocks were some of the strongest predictors of blunted weight loss following bariatric surgery [17]. A recent meta-analysis corroborates this observation by showing that lower physical activity levels are associated with attenuated surgery-induced weight loss in bariatric patients [62]. Interestingly, McCullough et al. demonstrated that cardiorespiratory fitness (i.e. VO2max) < 15.8 ml/kg/min is associated with a longer operating time, intubation duration, and estimated blood loss during surgery as well as more frequent complications including unstable angina, myocardial infarction, and deep venous thrombosis [63]. Although no systematic studies have been conducted to establish a link between surgical complications and a blunted response to bariatric surgery, the intricate interplay of adiposity-derived inflammation, insulin resistance, and physical fitness needs to be better understood to identify their contributions to reduce surgical complications and rescue bariatric surgery resistance.
Exercise as a Pre-Surgical Therapy to Reset Metabolic Responsiveness
Current recommendations to increase aerobic fitness in adults include 150 minutes of moderate or 75 minutes of vigorous physical activity per week. However, < 10% of bariatric surgery candidates meet the activity recommendation prior to surgery [64] and, in turn, are categorized as having “very poor” cardiorespiratory fitness based on their VO2max [65]. This low level of physical activity may be an explanation for why some individuals have increased composite surgical complications risk. Increasing physical activity levels prior to bariatric surgery could attenuate risk, as Berglind et al. found that pre-surgical physical activity levels were positively associated with post-surgical physical activity levels [66]. Thus, increasing physical activity levels prior to surgery could facilitate a beneficial increase in post-surgery exercise behavior. In fact, over 40% of bariatric patients feel more ready to exercise 2 weeks prior to their surgery [64], and recent work suggests that exercise counseling combined with pedometery may increase physical activity levels approximately 6 months following surgery to a greater extent than standard medical care alone. Unfortunately, there are few randomized controlled trials evaluating the effectiveness of an exercise intervention prior to bariatric surgery. Baillot et al. conducted a semi-supervised endurance and strength training program for 12 weeks prior to surgery and showed that people completed 64.5% of total exercise sessions. The training program resulted in significant weight loss and improvements in both physical fitness, as assessed by a 6-minute walk, and quality of life [67]. These findings were later supported by use of a telehealth approach using a semi-supervised in-home endurance and strength program to increase physical fitness [68]. Whether this increase in fitness and/or strength prior to surgery leads to reduced insulin resistance, inflammation and improved surgical outcomes and responsiveness awaits investigation [11, 69]. Nevertheless, while no study has systematically tested pre-operative exercise interventions in bariatric patients, it has been well established that exercise can improve both insulin resistance [70–71] and inflammation [72–73] in adults across BMI categories. Furthermore, a number of recent randomized controlled trials have been conducted to investigate the effects of exercise imposed post-bariatric surgery to determine whether exercise can effectively promote greater weight loss, fitness, and cardiometabolic health when compared to standard of care alone. Shah et al. demonstrated that a 12 week exercise program following bariatric surgery improved glucose tolerance compared to standard care [74]. These findings are consistent with data highlighting that moderate intensity aerobic exercise increases insulin sensitivity and glucose effectiveness (i.e. the ability of glucose to facilitate glucose disposal) [75], along with increased VO2max and mitochondrial adaptation for fat oxidation during bariatric-induced weight loss [76]. Supervised endurance exercise or educational based programs with resistance exercise can also facilitate greater weight loss, improved muscle strength and increased fitness capacity [75–77], suggesting overall that exercise is an effective therapy to improve metabolic health in surgical patients. However, despite higher exercise volumes in the general population appearing to relate to improved glucose regulation [13, 78–79] and cardiometabolic health [80], there is a limitation in the existing body of work on the effects of exercise “dose” on cardiometabolic health maintenance over time as well as on the effectiveness of exercise for the prevention of weight regain. These are important clinical questions that are likely to improve medical practice.
Diet as a Pre-Surgical Therapy to Improve Metabolic Responsiveness
Many bariatric candidates are malnourished due to long-term overconsumption of energy with predominantly low nutrient dense foods, thus leading to low diet quality. Inflammation and insulin resistance are associated with the resulting micronutrient deficiencies (e.g. vitamin D, iron, zinc, vitamin B-12), putting patients at additional risk for resistance post bariatric surgery [81]. The detriment of micronutrient malnourishment on post-surgical outcomes needs to be considered, with requirements of up to 10% weight loss for patients prior to surgery by many surgical centers in the U.S. [82]. This pre-surgical weight loss has been suggested to shorten surgical time, reduce surgical complications, and elicit greater weight loss at 3, 6, and 12 months post surgery when compared with individuals who do not lose weight prior to surgery [83–84]. Independent of macronutrient composition, low calorie diets are the most commonly prescribed dietary interventions since creating the state of negative energy balance is an effective non-surgical venue to reduce body weight [85]. An important reason low-calorie diets are implemented is to optimize weight loss and increase subject safety during surgery, in particular due to the shrinking of the liver, which will be discussed below. Indeed, a very low calorie diet (defined as less than 800 kcal per day) implemented 2 weeks prior to bariatric surgery resulted in significantly fewer post-operative complications in the 30 days after surgery when compared to controls with no pre-operative dietary restrictions [86]. Furthermore, surgeons have reported operations to be easier in patients who have undergone pre-operative diet therapy [86]. However, it is worth noting that some studies report that despite significant amount of weight loss in the pre-surgical period, there was no enhanced weight loss at 24 [87] and 48 [88] months post-surgery compared with those who did not diet pre-surgery. In line with these findings, Pournaras et al. showed that a 2 week very low calorie diet prior to surgery elicited weight loss and improved insulin sensitivity in adults with T2D compared to patients who did not diet. Yet, the group who followed a very low calorie diet pre-operatively did not have greater weight loss or insulin sensitivity at 2 weeks or 1 year post-surgery [89]. Thus, although data indicate that surgery outcomes are beneficially affected by pre-operative diet-induced weight loss, additional work is required to determine if weight loss and/or metabolic health pre-surgery results in long-term health and well-being in the post-operative period.
Another reason the low-calorie diet is often utilized is to reduce liver size, as nearly 91% of people undergoing bariatric surgery have enlarged livers that are characterized by hepatic steatosis [90]. Enlarged and/or fatty liver is typically observed in individuals with large amounts of excessive body fat. This is problematic since enlarged fatty liver increases the risk of bleeding upon surgical manipulation and reduces operative visibility for the surgeon, thereby contributing to increased operative difficulty [91–92]. Fatty liver also correlates with increased rates of endogenous glucose production that contributes to fasting hyperglycemia and whole body insulin resistance [93]. Thus, dietary interventions that reduce liver size and elicit weight loss may be best for minimizing surgical complications. Edholm et al. evaluated the effectiveness of an 800–1100 kcal/day diet for 4 weeks prior to bariatric surgery, and reported an average weight loss of 7.5 kg, as well as a 12 and 40% decrease in liver volume and fat, respectively. The low calorie diet group had decreased surgical complexity as assessed by surgeons compared to individuals who did not undergo the diet intervention [94]. Brody et al. also studied the effectiveness of a 4 week 1200–1500 kcal/day diet that included specifically two 150 calorie high protein shakes per day during the pre-operative period. Dieting resulted in significant weight loss of approximately 3.1% and decreased left lateral liver volume by nearly 43% [95]. The response to a low calorie diet may be effected by time, as Colles et al. found that 2 weeks is the minimum amount of time for a very low calorie diet (<650 kcal/day) to induce decreased liver volume, while 6 weeks achieved greater reductions in liver size and visceral adipose tissue stores [96]. Thus, following a calorie-restricted diet as a pre-surgical intervention can reduce liver adiposity/size as well as insulin resistance. This in turn can translate to reduced surgical complications and improved surgical outcomes in bariatric candidates [93, 97–100].
One important limitation of following low calorie diets, and in particular the very low calorie liver-shrinking diets, relates to the disproportionally higher loss of skeletal muscle mass due to accentuated protein degradation and decreased rate of protein synthesis during periods of very low energy consumption [101]. Although, to date, no studies have specifically examined the relationship between skeletal muscle mass differences pre-operatively on the response to bariatric surgery, Dodson et al. reported that sarcopenia was an independent predictor of mortality following hepatic inter-arterial therapy [102]. Moreover, Psutka et al. showed that people characterized by sarcopenia were at increased risk of all-cause mortality after radical cystectomy for bladder cancer [103]. These findings suggest that skeletal muscle integrity may play an important role in post-surgical mortality. In fact, the loss of muscle mass from diet alone may be problematic for weight management during the post-operative period in the bariatric population as it results in significantly reduced resting metabolism [104–105], thereby affecting recovery from surgery as well as long-term weight loss.
Exercise is a therapy that can counteract the effects of diet on skeletal muscle loss. Ross et al. demonstrated that 60 minutes of aerobic exercise 5 days/week coupled with a low calorie diet resulted in significantly more adipose tissue loss and greater skeletal muscle mass preservation than diet alone [106], which may contribute to increased insulin sensitivity [107]. Yokoyama et al. showed that a 3 week calorie restrictive diet (i.e. 25–30 kcal/kg of ideal body weight) plus exercise for 5 days/week also reduces insulin resistance independent of weight loss when compared with diet alone in adults with T2D [108]. These improvements in insulin resistance were determined by HOMA-IR, thereby leaving a gap in our understanding of what insulin-sensitive tissue (i.e. liver, skeletal muscle, etc.) responds most to exercise plus diet in the bariatric population. However, Haus et al. reported that obese adults with impaired glucose tolerance who underwent a hypocaloric diet plus aerobic exercise for 12-weeks derived greater improvement in hepatic, not skeletal muscle, insulin sensitivity when measured by the euglycemic-hyperinsulinemic clamp with intralipid and stable isotope infusion compared with exercise alone [109]. These findings are consistent with other work [110], and suggest that while diet alone is likely an effective therapy for reducing the risk of surgical complications and potentially prolonged metabolic health, adding exercise attenuates risk of muscle loss that can affect long-term bariatric responses for metabolic health.
Pharmacology as a Pre-Surgical Therapy
Despite randomized clinical trials showing the efficacy of lifestyle modification on weight loss and fitness, subject adherence to diet and exercise remains difficult. If conventional approaches to improve glycemic control and weight with lifestyle do not work well or are not feasible, then pharmacological agents that target specific pathological defects contributing to obesity, insulin resistance, and β-cell dysfunction may be necessary for addressing bariatric surgery resistance in the pre-surgical patient. While a goal of surgery is to reduce the number of prescription medications patients are taking, implementing pharmacological interventions in the pre-operative phase may elicit physiological changes that allow patients to better respond to surgery. Nevertheless, health care providers should be cognoscente of their patients’ health status in the pre- and post-operative period in order to optimize health and well-being.
Four new weight loss agents with glycemic benefit have been approved for weight loss since 2012 and join orlistat for the long-term management of obesity. These therapies are generally recommended for patients who are obese or overweight (BMI ≥25 kg/m2) and who suffer from at least one weight-related complication, such as hypertension, T2D, or dyslipidemia. Orlistat is a gastric and pancreatic lipase inhibitor that blocks dietary fat absorption from the gastrointestinal system by ~30%. Both randomized trials and meta-analyses have demonstrated that orlistat treatment can produce weight loss and reduce the incidence of T2D in people with impaired glucose tolerance [111]. Several mechanisms have been proposed to account for the anti-diabetic effect of orlistat, such as improved insulin sensitivity, incomplete dietary fat digestion, partial stimulation of GLP-1 (glucagon like polypeptide-1) release, and decreases in visceral adiposity [112]. Phentermine-extended release (ER) topiramate, lorcaserin, and naltrexone-bupropion are additional medications that elicit weight loss, but do so by acting in the central nervous system to reduce appetite. Clinical trials have shown these medications are effective at reducing HbA1c as well as lowering the progression to T2D [113–118]. Finally, liraglutide, a GLP-1 receptor agonist that is approved for use in T2D, has also been approved for weight loss. Interestingly, GLP-1 (along with GIP, glucose-dependent insulinotropic peptide) is an incretin hormone that not only plays an important stimulatory role in meal-stimulated insulin secretion, but it also delays gastric emptying and reduces post-prandial glucose levels [119]. Subsequently, many studies have proposed GLP-1 therapy as a novel approach to promote glycemic control and weight loss in obese patients. In fact, Wood et al. showed that the use of GLP-1 receptor agonists combined with anti-diabetic medication prior to bariatric surgery resulted in greater T2D early remission rates and 6 year remission rates than when taking anti-diabetic medications alone [120]. This suggests that GLP-1 receptor agonists may promote metabolic health prior to surgery for enhanced metabolic responsiveness in the post-operative period. More work is needed to understand the effect of GLP-1 receptor agonists, with or without exercise/diet in the pre-surgical bariatric patient, as few studies have studied the combined treatment effects for metabolic health [121–122].
Insulin sensitizers work to improve the regulation of glucose in liver, skeletal muscle, and adipose tissue. Metformin is the most widely prescribed drug to treat hyperglycemia in people with T2D [8]. In fact, metformin is the first-line oral anti-diabetic medication recommended by the American Diabetes Association [123] that aids in blood glucose management and body weight reduction. Current evidence suggests that metformin increases whole-body insulin sensitivity through the suppression of hepatic gluconeogenesis and stimulation of peripheral (mainly skeletal muscle) glucose uptake through activation of adenosine monophosphate-kinase (AMPK) [8].
An older class of insulin sensitizers, the TZDs (thiazolidinediones), act as a ligand for the peroxisome proliferator-activated receptor (PPAR) γ. Although these agents are effective at improving both insulin sensitivity as well as improving/restoring pancreatic β-cell function [124], they often promote weight gain of approximately 2–5 kg [125] and are associated with significant side effects including increased risk for heart failure [126], bladder cancer [127] and bone loss [128–129] and thus, may not be ideal for the pre-surgical obese patient.
A new class of diabetes therapy worth mentioning is the SGLT-2 (sodium-dependent glucose co-transporter-2) inhibitors. This drug acts by blocking the reabsorption of approximately 90% of luminal glucose in the proximal tubule of the kidney. In addition, it has favorable effects on body weight with weight loss of 1.2 to 3.3 kg, in addition to significant impact on glycemic control and systolic blood pressure. Intriguingly, one agent in this class, empagliflozin, was shown to have improved atherosclerotic outcomes in patients at high risk or with known CVD [130]. However, the mechanism by which empagliflozin improves vascular outcomes has not been elucidated.
Sulfonylureas (SUs) are insulin secretagogues that increase pancreatic insulin secretion through the binding of receptors related to potassium channels on β-cells [50]. Unfortunately, SUs do not appear to work effectively in the long term and also carry a risk of promoting weight gain [131–133]. Thus, the role of SUs on preparing patients for surgery is unclear.
Taken together, determining the appropriate pharmacologic agent(s) to prescribe patients pre-operatively will likely vary based on the individual and their current health status, which also includes cost of therapy as the newer agents tend to be more expensive. Further prospective work is required to define an algorithm for the pre-bariatric surgery patient to foster weight loss and improve metabolic health to reduce surgical complications and improve metabolic responsiveness. Additional work will also be needed to be address how and if individuals should continue agents that promote weight loss even after surgery, particularly as people increase physical activity and improve nutrition. This will be important for optimizing life-long weight management, metabolic health, and well-being in the bariatric patient.
Clinical Perspective and Conclusion
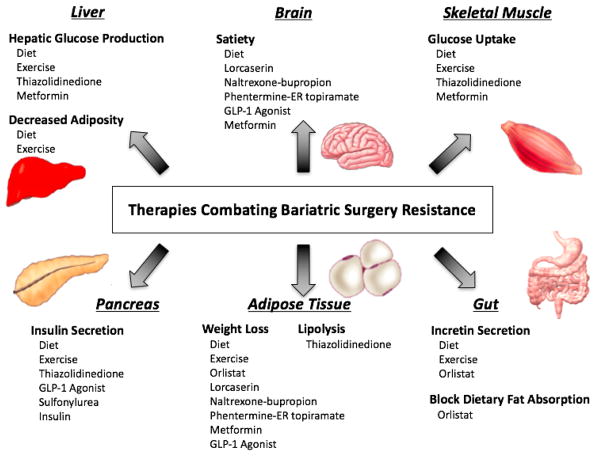
Bariatric surgery causes significant weight loss and improves cardiometabolic health. Individuals undergoing bariatric surgery have significantly lower body weight [87–89] and incidence of comorbidities including T2D and hypertriglyceridemia [134] that persists over time (e.g. 10 years). Post-operative interventions including diet [135], exercise [101], and pharmacotherapy [136] have been explored to a greater extent than pre-operative interventions and have shown to be efficacious. However, newer work highlights that some individuals receiving surgery are “bariatric surgery resistant” and experience blunted weight loss and cardiometabolic health and non-remission of T2D, suggesting the need to intervene prior to surgery. The notion of bariatric surgery resistance therefore raises several important clinical and public health knowledge gaps that need to be addressed. First, what are the characteristics predicting a person being “bariatric surgery resistant”? What treatment(s) may aid resistant individuals prior to surgery to reduce chances of surgical complication, minimize post-operative length of stay, as well as improve recovery in the immediate 30-day period after surgery? How will increasing bariatric surgery sensitivity relate to post-surgical responsiveness, health improvements, and preservation of co-morbidity resolutions? To date, the answers to these questions are unknown, highlighting critical gaps in our current knowledge. These gaps primarily include limited systematic evaluations of pre-operative interventions on improving post-operative outcomes like surgical outcomes, inflammation, insulin resistance, hyperglycemia, and aerobic fitness. We wrote this review to highlight these current gaps, propose hypotheses, and identify possible interventions prior to surgery. A targeted approach to answering these questions, however, may rest in recognition of the known clinical and metabolic determinants of those people likely to be bariatric surgery resistant. Subsequently, targeting tissue-specific modifiable risk factors including obesity, inflammation, hyperglycemia, insulin sensitivity and β-cell function with exercise, diet, and/or pharmacotherapy may be the first steps towards creating a long-life metabolic fitness program in the bariatric patient (Figure 2). Further work to better define the optimal combinations of lifestyle medicine and/or pharmacology for cardiometabolic health in bariatric patients prior to surgery remain to be determined. To date there are no systematic studies that have evaluated individual and/or combined lifestyle interventions prior to bariatric surgery on cardiometabolic outcomes. Thus, clinical trials are needed to understand the correct dose of exercise, diet and/or pharmacology to optimize health in the bariatric resistant patient prior to surgery. Ultimately, development of such a program will set forth a metabolic fitness program that increases the propensity for treatment and prevention of future T2D and CVD.
Figure 2.
Summary of lifestyle interventions and pharmaceutical agents that target potential mechanisms of bariatric surgery resistance across various tissues.
Acknowledgments
N.G. and S.K.M. were primarily responsible for writing the manuscript. A.P., S.K., A.W., and J.K., P.H. reviewed and edited the manuscript. We thank the members of the Applied Metabolism & Physiology Laboratory for helpful discussion on the manuscript.
Footnotes
CONFLICT OF INTEREST
N.G., A.P., S.K., A.W., J.K., P.H., and S.K.M. declare that they have no conflict of interest.
ETHNICAL APPROVAL STATEMENT
This article does not contain any studies with human participants or animals performed by any of the authors
INFORMED CONSENT STATEMENT
Does not apply.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McPhee JB, Schertzer JD. Immunometabolism of obesity and diabetes: microbiota link compartmentalized immunity in the gut to metabolic tissue inflammation. Clin Sci. 2015;129(12):1083–96. doi: 10.1042/CS20150431. [DOI] [PubMed] [Google Scholar]
- 3.Bastard JP, Maachi M, Lagathu C, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17(1):4–12. [PubMed] [Google Scholar]
- 4.Greenfield JR, Campbell LV. Insulin resistance and obesity. Clin Dermatol. 2004;22(4):289–95. doi: 10.1016/j.clindermatol.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28(5):822–31. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 6.Schelbert KB. Comorbidities of obesity. Prim Care. 2009;36(2):271–85. doi: 10.1016/j.pop.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Barte JC, ter Bogt NC, Bogers RP, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010;11(12):899–906. doi: 10.1111/j.1467-789X.2010.00740.x. [DOI] [PubMed] [Google Scholar]
- 8.Malin SK, Braun B. Impact of Metformin on Exercise-Induced Metabolic Adaptations to Lower Type 2 Diabetes Risk. Exerc Sport Sci Rev. 2016;44(1):4–11. doi: 10.1249/JES.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 9.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solomon TP, Thyfault JP. Type 2 diabetes sits in a chair. Diabetes Obes Metab. 2013;15(11):987–92. doi: 10.1111/dom.12105. [DOI] [PubMed] [Google Scholar]
- 11.Li JF, Lai DD, Lin ZH, Jiang TY, Zhang AM, Dai JF. Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis of randomized and nonrandomized trials. Surg Laparosc Endosc Percutan Tech. 2014;24(1):1–11. doi: 10.1097/SLE.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 12.Robinson AH, Adler S, Stevens HB, Darcy AM, Morton JM, Safer DL. What variables are associated with successful weight loss outcomes for bariatric surgery after 1 year? Surg Obes Relat Dis. 2014;10(4):697–704. doi: 10.1016/j.soard.2014.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malin SK, Solomon TP, Blaszczak A, Finnegan S, Filion J, Kirwan JP. Pancreatic beta-cell function increases in a linear dose-response manner following exercise training in adults with prediabetes. Am J Physiol Endocrinol Metab. 2013;305(10):E1248–54. doi: 10.1152/ajpendo.00260.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peluso L, Vanek VW. Efficacy of gastric bypass in the treatment of obesity-related comorbidities. Nutr Clin Pract. 2007;22(1):22–28. doi: 10.1177/011542650702200122. [DOI] [PubMed] [Google Scholar]
- 15.Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232(4):515–529. doi: 10.1097/00000658-200010000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma Y, Pagoto SL, Olendzki BC, et al. Predictors of weight status following laparoscopic gastric bypass. Obes Surg. 2006;16(9):1227–31. doi: 10.1381/096089206778392284. [DOI] [PubMed] [Google Scholar]
- 17.Hatoum IJ, Stein HK, Merrifield BF, Kaplan LM. Capacity for physical activity predicts weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring) 2009;17(1):92–99. doi: 10.1038/oby.2008.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sugerman HJ, DeMaria EJ, Kellum JM, Sugerman EL, Meador JG, Wolfe LG. Effects of bariatric surgery in older patients. Ann Surg. 2004;240(2):243–47. doi: 10.1097/01.sla.0000133361.68436.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002;236(5):576–82. doi: 10.1097/00000658-200211000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cleasby ME, Jamieson PM, Atherton PJ. Insulin resistance and sarcopenia: mechanistic links between common co-morbidities. J Endocrinol. 2016;229(2):67–81. doi: 10.1530/JOE-15-0533. [DOI] [PubMed] [Google Scholar]
- 21.Bijlsma AY, Meskers CG, van Heemst D, Westendorp RG, de Craen AJ, Maier AB. Diagnostic criteria for sarcopenia relate differently to insulin resistance. Age. 2013;35(6):2367–75. doi: 10.1007/s11357-013-9516-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hagobian TA, Evero N. Exercise and Weight Loss: What Is the Evidence of Sex Differences? Current Obesity Reports. 2013;2(1):86–92. [Google Scholar]
- 23.Ding EL, Song Y, Malik VS, Liu S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2006;295(11):1288–1299. doi: 10.1001/jama.295.11.1288. [DOI] [PubMed] [Google Scholar]
- 24.Hellstrom L, Wahrenberg H, Hruska K, Reynisdottir S, Arner P. Mechanisms behind gender differences in circulating leptin levels. J Intern Med. 2000;247(4):457–462. doi: 10.1046/j.1365-2796.2000.00678.x. [DOI] [PubMed] [Google Scholar]
- 25.Kennedy A, Gettys TW, Watson P, et al. The metabolic significance of leptin in humans: gender-based differences in relationship to adiposity, insulin sensitivity, and energy expenditure. J Clin Endocrinol Metab. 1997;82(4):1293–1300. doi: 10.1210/jcem.82.4.3859. [DOI] [PubMed] [Google Scholar]
- 26.Mantzoros CS. The role of leptin in human obesity and disease: a review of current evidence. Ann Intern Med. 1999;130(8):671–680. doi: 10.7326/0003-4819-130-8-199904200-00014. [DOI] [PubMed] [Google Scholar]
- 27.Faerch K, Borch-Johnsen K, Vaag A, Jorgensen T, Witte DR. Sex differences in glucose levels: a consequence of physiology or methodological convenience? The Inter99 study. Diabetologia. 2010;53(5):858–65. doi: 10.1007/s00125-010-1673-4. [DOI] [PubMed] [Google Scholar]
- 28.Makovey J, Naganathan V, Seibel M, Sambrook P. Gender differences in plasma ghrelin and its relations to body composition and bone - an opposite-sex twin study. Clin Endocrinol. 2007;66(4):530–37. doi: 10.1111/j.1365-2265.2007.02768.x. [DOI] [PubMed] [Google Scholar]
- 29.Purnell JQ, Weigle DS, Breen P, Cummings DE. Ghrelin levels correlate with insulin levels, insulin resistance, and high-density lipoprotein cholesterol, but not with gender, menopausal status, or cortisol levels in humans. J Clin Endocrinol Metab. 2003;88(12):5747–52. doi: 10.1210/jc.2003-030513. [DOI] [PubMed] [Google Scholar]
- 30.Anderson WA, Greene GW, Forse RA, Apovian CM, Istfan NW. Weight loss and health outcomes in African Americans and whites after gastric bypass surgery. Obesity. 2007;15(6):1455–63. doi: 10.1038/oby.2007.174. [DOI] [PubMed] [Google Scholar]
- 31.Parikh M, Lo H, Chang C, Collings D, Fielding G, Ren C. Comparison of outcomes after laparoscopic adjustable gastric banding in African-Americans and whites. Surg Obes Relat Dis. 2006;2(6):607–12. doi: 10.1016/j.soard.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 32.Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab. 2004;89(6):2590–94. doi: 10.1210/jc.2004-0339. [DOI] [PubMed] [Google Scholar]
- 33.Olson NC, Callas PW, Hanley AJ, et al. Circulating levels of TNF-alpha are associated with impaired glucose tolerance, increased insulin resistance, and ethnicity: the Insulin Resistance Atherosclerosis Study. J Clin Endocrinol Metab. 2012;97(3):1032–40. doi: 10.1210/jc.2011-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab. 2001;280(5):745–51. doi: 10.1152/ajpendo.2001.280.5.E745. [DOI] [PubMed] [Google Scholar]
- 35.Lindquist CH, Gower BA, Goran MI. Role of dietary factors in ethnic differences in early risk of cardiovascular disease and type 2 diabetes. Am J Clin Nutr. 2000;71(3):725–32. doi: 10.1093/ajcn/71.3.725. [DOI] [PubMed] [Google Scholar]
- 36.Conjeevaram HS, Kleiner DE, Everhart JE, et al. Race, insulin resistance and hepatic steatosis in chronic hepatitis C. Hepatology. 2007;45(1):80–87. doi: 10.1002/hep.21455. [DOI] [PubMed] [Google Scholar]
- 37.Gullick AA, Graham LA, Richman J, Kakade M, Stahl R, Grams J. Association of race and socioeconomic status with outcomes following laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2015;25(4):705–711. doi: 10.1007/s11695-014-1447-z. [DOI] [PubMed] [Google Scholar]
- 38.Lutfi R, Torquati A, Sekhar N, Richards WO. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc. 2006;20(6):864–867. doi: 10.1007/s00464-005-0115-8. [DOI] [PubMed] [Google Scholar]
- 39.Kinzl JF, Schrattenecker M, Traweger C, Mattesich M, Fiala M, Biebl W. Psychosocial predictors of weight loss after bariatric surgery. Obes Surg. 2006;16(12):1609–1614. doi: 10.1381/096089206779319301. [DOI] [PubMed] [Google Scholar]
- 40.van Hout GC, Verschure SK, van Heck GL. Psychosocial predictors of success following bariatric surgery. Obes Surg. 2005;15(4):552–560. doi: 10.1381/0960892053723484. [DOI] [PubMed] [Google Scholar]
- 41.Xu H, Barnes GT, Yang Q, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112(12):1821–30. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brethauer SA, Heneghan HM, Eldar S, et al. Early effects of gastric bypass on endothelial function, inflammation, and cardiovascular risk in obese patients. Surg Endosc. 2011;25(8):2650–59. doi: 10.1007/s00464-011-1620-6. [DOI] [PubMed] [Google Scholar]
- 43.Madsen EL, Rissanen A, Bruun JM, Skogstrand K, Tonstad S, Hougaard DM, Richelsen B. Weight loss larger than 10% is needed for general improvement of levels of circulating adiponectin and markers of inflammation in obese subjects: a 3-year weight loss study. Eur J Endocrinol. 2008;158(2):179–87. doi: 10.1530/EJE-07-0721. [DOI] [PubMed] [Google Scholar]
- 44.Heneghan HM, Huang H, Kashyap SR, et al. Reduced cardiovascular risk after bariatric surgery is linked to plasma ceramides, apolipoprotein-B100, and ApoB100/A1 ratio. Surg Obes Relat Dis. 2013;9(1):100–07. doi: 10.1016/j.soard.2011.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Malin SK, Bena J, Abood B, et al. Attenuated improvements in adiponectin and fat loss characterize type 2 diabetes non-remission status after bariatric surgery. Diabetes Obes Metab. 2014;16(12):1230–38. doi: 10.1111/dom.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hirsch FF, Pareja JC, Geloneze SR, Chaim E, Cazzo E, Geloneze B. Comparison of metabolic effects of surgical-induced massive weight loss in patients with long-term remission versus non-remission of type 2 diabetes. Obes Surg. 2012;22(6):910–17. doi: 10.1007/s11695-012-0589-0. [DOI] [PubMed] [Google Scholar]
- 47.Weyer C, Funahashi T, Tanaka S, et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab. 2001;86(5):1930–35. doi: 10.1210/jcem.86.5.7463. [DOI] [PubMed] [Google Scholar]
- 48.Arita Y, Kihara S, Ouchi N, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. 1999. Biochem Biophys Res Commun. 2012;425(3):560–64. doi: 10.1016/j.bbrc.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 49.Yang WS, Lee WJ, Funahashi T, et al. Weight reduction increases plasma levels of an adipose-derived anti-inflammatory protein, adiponectin. J Clin Endocrinol Metab. 2001;86(8):3815–19. doi: 10.1210/jcem.86.8.7741. [DOI] [PubMed] [Google Scholar]
- 50.Kahn SE, Cooper ME, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 2014;383(9922):1068–83. doi: 10.1016/S0140-6736(13)62154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gavin TP, Ernst JM, Caudill SE, et al. Insulin sensitivity is related to glycemic control in type 2 diabetes and diabetes remission after Roux-en Y gastric bypass. Surgery. 2014;155(6):1036–43. doi: 10.1016/j.surg.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 52.Vella A. Beta-Cell Function After Weight-Loss Induced by Bariatric Surgery. Physiology. 2014;29(2):84–5. doi: 10.1152/physiol.00003.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Torquati A, Lutfi R, Abumrad N, Richards WO. Is Roux-en-Y gastric bypass surgery the most effective treatment for type 2 diabetes mellitus in morbidly obese patients? J Gastrointest Surg. 2005;9(8):1112–8. doi: 10.1016/j.gassur.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 54.Hall TC, Pellen MG, Sedman PC, Jain PK. Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity. Obes Surg. 2010;20(9):1245–50. doi: 10.1007/s11695-010-0198-8. [DOI] [PubMed] [Google Scholar]
- 55.Wang GF, Yan YX, Xu N, et al. Predictive factors of type 2 diabetes mellitus remission following bariatric surgery: a meta-analysis. Obes Surg. 2015;25(2):199–208. doi: 10.1007/s11695-014-1391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mehaffey JH, Mullen MG, Mehaffey RL, et al. Type 2 diabetes remission following gastric bypass: does diarem stand the test of time? Surg Endosc. 2016 doi: 10.1007/s00464-016-4964-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khanna V, Malin SK, Bena J, et al. Adults with long-duration type 2 diabetes have blunted glycemic and beta-cell function improvements after bariatric surgery. Obesity (Silver Spring) 2015;23(3):523–26. doi: 10.1002/oby.21021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nguyen NQ, Game P, Bessell J, et al. Outcomes of Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding. World J Gastroenterol. 2013;19(36):6035–43. doi: 10.3748/wjg.v19.i36.6035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Steinbrook R. Surgery for severe obesity. N Engl J Med. 2004;350(11):1075–79. doi: 10.1056/NEJMp048029. [DOI] [PubMed] [Google Scholar]
- 60.Fernandez AZ, DeMaria EJ, Tichansky DS, et al. Experience with over 3,000 open and laparoscopic bariatric procedures: multivariate analysis of factors related to leak and resultant mortality. Surg Endosc. 2004;18(2):193–97. doi: 10.1007/s00464-003-8926-y. [DOI] [PubMed] [Google Scholar]
- 61.Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–54. doi: 10.1056/NEJMoa0901836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jacobi D, Ciangura C, Couet C, Oppert JM. Physical activity and weight loss following bariatric surgery. Obes Rev. 2011;12(5):366–77. doi: 10.1111/j.1467-789X.2010.00731.x. [DOI] [PubMed] [Google Scholar]
- 63.McCullough PA, Gallagher MJ, Dejong AT, et al. Cardiorespiratory fitness and short-term complications after bariatric surgery. Chest. 2006;130(2):517–25. doi: 10.1378/chest.130.2.517. [DOI] [PubMed] [Google Scholar]
- 64.Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self report vs. objective measures. Obesity. 2010;18(12):2395–97. doi: 10.1038/oby.2010.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Trivax JE, Gallagher MJ, Alexander DV, deJong AT, Kasturi G, Sandberg KR, Jafri SM, Krause KR, Chengelis DL, Moy J, Franklin BA, McCullough PA. Poor aerobic fitness predicts complications associated with bariatric surgery. Chest. 2005;128(4) doi: 10.1378/chest.130.2.517. [DOI] [PubMed] [Google Scholar]
- 66.Berglind D, Willmer M, Eriksson U, et al. Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obes Surg. 2015;25(1):119–25. doi: 10.1007/s11695-014-1331-x. [DOI] [PubMed] [Google Scholar]
- 67.Baillot A, Mampuya WM, Comeau E, Meziat-Burdin A, Langlois MF. Feasibility and impacts of supervised exercise training in subjects with obesity awaiting bariatric surgery: a pilot study. Obes Surg. 2013;23(7):882–91. doi: 10.1007/s11695-013-0875-5. [DOI] [PubMed] [Google Scholar]
- 68.Baillot A, Mampuya WM, Dionne IJ, Comeau E, Meziat-Burdin A, Langlois MF. Impacts of Supervised Exercise Training in Addition to Interdisciplinary Lifestyle Management in Subjects Awaiting Bariatric Surgery: a Randomized Controlled Study. Obes Surg. 2016 doi: 10.1007/s11695-016-2153-9. [DOI] [PubMed] [Google Scholar]
- 69.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 70.Henriksen EJ. Invited review: Effects of acute exercise and exercise training on insulin resistance. J Appl Physiol. 2002;93(2):788–796. doi: 10.1152/japplphysiol.01219.2001. [DOI] [PubMed] [Google Scholar]
- 71.Hawley JA. Exercise as a therapeutic intervention for the prevention and treatment of insulin resistance. Diabetes Metab Res Rev. 2004;20(5):383–393. doi: 10.1002/dmrr.505. [DOI] [PubMed] [Google Scholar]
- 72.Mathur N, Pedersen BK. Exercise as a mean to control low-grade systemic inflammation. Mediators Inflamm. 2008:6. doi: 10.1155/2008/109502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hopps E, Canino B, Caimi G. Effects of exercise on inflammation markers in type 2 diabetic subjects. Acta Diabetol. 2011;48(3):183–189. doi: 10.1007/s00592-011-0278-9. [DOI] [PubMed] [Google Scholar]
- 74.Shah M, Snell PG, Rao S, et al. High-volume exercise program in obese bariatric surgery patients: a randomized, controlled trial. Obesity. 2011;19(9):1826–34. doi: 10.1038/oby.2011.172. [DOI] [PubMed] [Google Scholar]
- 75.Coen PM, Tanner CJ, Helbling NL, et al. Clinical trial demonstrates exercise following bariatric surgery improves insulin sensitivity. J Clin Invest. 2015;125(1):248–57. doi: 10.1172/JCI78016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Coen PM, Menshikova EV, Distefano G, et al. Exercise and Weight Loss Improve Muscle Mitochondrial Respiration, Lipid Partitioning, and Insulin Sensitivity After Gastric Bypass Surgery. Diabetes. 2015;64(11):3737–50. doi: 10.2337/db15-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stegen S, Derave W, Calders P, Van Laethem C, Pattyn P. Physical fitness in morbidly obese patients: effect of gastric bypass surgery and exercise training. Obes Surg. 2011;21(1):61–70. doi: 10.1007/s11695-009-0045-y. [DOI] [PubMed] [Google Scholar]
- 78.Dube JJ, Allison KF, Rousson V, Goodpaster BH, Amati F. Exercise dose and insulin sensitivity: relevance for diabetes prevention. Med Sci Sports Exerc. 2012;44(5):793–99. doi: 10.1249/MSS.0b013e31823f679f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Houmard JA, Tanner CJ, Slentz CA, Duscha BD, McCartney JS, Kraus WE. Effect of the volume and intensity of exercise training on insulin sensitivity. J Appl Physiol. 2004;96(1):101–06. doi: 10.1152/japplphysiol.00707.2003. [DOI] [PubMed] [Google Scholar]
- 80.Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97(7):2482–88. doi: 10.1210/jc.2011-3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gletsu-Miller N, Wright BN. Mineral malnutrition following bariatric surgery. Adv Nutr. 2013;4:506–517. doi: 10.3945/an.113.004341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Baldry EL, Leeder PC, Idris IR. Pre-operative dietary restriction for patients undergoing bariatric surgery in the UK: observational study of current practice and dietary effects. Obes Surg. 2014;24(3):416–421. doi: 10.1007/s11695-013-1125-6. [DOI] [PubMed] [Google Scholar]
- 83.Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89. doi: 10.1007/s11695-011-0472-4. [DOI] [PubMed] [Google Scholar]
- 84.Alami RS, Morton JM, Schuster R, et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis. 2007;3(2):141–46. doi: 10.1016/j.soard.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 85.Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–73. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A, et al. Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: a randomized multicenter study. Arch Surg. 2011;146(11):1300–1305. doi: 10.1001/archsurg.2011.273. [DOI] [PubMed] [Google Scholar]
- 87.Huerta S, Dredar S, Hayden E, et al. Preoperative weight loss decreases the operative time of gastric bypass at a Veterans Administration hospital. Obes Surg. 2008;18(5):508–512. doi: 10.1007/s11695-007-9334-5. [DOI] [PubMed] [Google Scholar]
- 88.Martin LF, Tan TL, Holmes PA, Becker DA, Horn J, Bixler EO. Can morbidly obese patients safely lose weight preoperatively? Am J Surg. 1995;169(2):245–253. doi: 10.1016/s0002-9610(99)80145-7. [DOI] [PubMed] [Google Scholar]
- 89.Pournaras D, Nygren J, Hagstrom-Toft E, Arner P, Roux C, Thorell A. Improved glucose metabolism after gastric bypass: evolution of the paradigm. Surg Obes Relat Dis. 2016;12:1457–65. doi: 10.1016/j.soard.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 90.Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. J Hepatol. 2006;45(4):600–06. doi: 10.1016/j.jhep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 91.Nguyen NT, Longoria M, Gelfand DV, Sabio A, Wilson SE. Staged laparoscopic Roux-en-Y: a novel two-stage bariatric operation as an alternative in the super-obese with massively enlarged liver. Obes Surg. 2005;15(7):1077–81. doi: 10.1381/0960892054621062. [DOI] [PubMed] [Google Scholar]
- 92.van Wissen J, Bakker N, Doodeman HJ, Jansma EP, Bonjer HJ, Houdijk AP. Preoperative Methods to Reduce Liver Volume in Bariatric Surgery: a Systematic Review. Obes Surg. 2016;26(2):251–56. doi: 10.1007/s11695-015-1769-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yki-Jarvinen H. Fat in the liver and insulin resistance. Ann Med. 2005;37(5):347–56. doi: 10.1080/07853890510037383. [DOI] [PubMed] [Google Scholar]
- 94.Edholm D, Kullberg J, Haenni A, et al. Preoperative 4-week low-calorie diet reduces liver volume and intrahepatic fat, and facilitates laparoscopic gastric bypass in morbidly obese. Obes Surg. 2011;21(3):345–350. doi: 10.1007/s11695-010-0337-2. [DOI] [PubMed] [Google Scholar]
- 95.Brody F, Vaziri K, Garey C, et al. Preoperative liver reduction utilizing a novel nutritional supplement. J Laparoendosc Adv Surg Tech A. 2011;21(6):491–95. doi: 10.1089/lap.2010.0559. [DOI] [PubMed] [Google Scholar]
- 96.Colles SL, Dixon JB, Marks P, Strauss BJ, O’Brien PE. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am J Clin Nutr. 2006;84(2):304–11. doi: 10.1093/ajcn/84.1.304. [DOI] [PubMed] [Google Scholar]
- 97.Alvarado R, Alami RS, Hsu G, et al. The impact of preoperative weight loss in patients undergoing laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2005;15(9):1282–86. doi: 10.1381/096089205774512429. [DOI] [PubMed] [Google Scholar]
- 98.Dagogo-Jack S, Alberti GM. Management of diabetes mellitus in surgical patients. Diabetes Spectrum. 2002;15(1):44–48. [Google Scholar]
- 99.Gonzalez-Perez J, Sanchez-Leenheer S, Delgado AR, et al. Clinical impact of a 6-week preoperative very low calorie diet on body weight and liver size in morbidly obese patients. Obes Surg. 2013;23(10):1624–31. doi: 10.1007/s11695-013-0977-0. [DOI] [PubMed] [Google Scholar]
- 100.Rector RS, Warner SO, Liu Y, et al. Exercise and diet induced weight loss improves measures of oxidative stress and insulin sensitivity in adults with characteristics of the metabolic syndrome. Am J Physiol Endocrinol Metab. 2007;293(2):500–6. doi: 10.1152/ajpendo.00116.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Coen PM, Goodpaster BH. A role for exercise after bariatric surgery? Diabetes Obes Metab. 2016;18(1):16–23. doi: 10.1111/dom.12545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dodson RM, Firoozmand A, Hyder O, et al. Impact of sarcopenia on outcomes following intra-arterial therapy of hepatic malignancies. J Gastrointest Surg. 2013;17(12):2123–32. doi: 10.1007/s11605-013-2348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Psutka SP, Carrasco A, Schmit GD, et al. Sarcopenia in patients with bladder cancer undergoing radical cystectomy: impact on cancer-specific and all-cause mortality. Cancer. 2014;120(18):2910–18. doi: 10.1002/cncr.28798. [DOI] [PubMed] [Google Scholar]
- 104.Carbone JW, McClung JP, Pasiakos SM. Skeletal muscle responses to negative energy balance: effects of dietary protein. Adv Nutr. 2012;3(2):119–26. doi: 10.3945/an.111.001792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014;2(10):819–29. doi: 10.1016/S2213-8587(14)70034-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ross R, Pedwell H, Rissanen J. Effects of energy restriction and exercise on skeletal muscle and adipose tissue in women as measured by magnetic resonance imaging. Am J Clin Nutr. 1995;61(6):1179–1185. doi: 10.1093/ajcn/61.6.1179. [DOI] [PubMed] [Google Scholar]
- 107.Pan DA, Lillioja S, Kriketos AD, et al. Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes. 1997;46(6):983–988. doi: 10.2337/diab.46.6.983. [DOI] [PubMed] [Google Scholar]
- 108.Yokoyama H, Emoto M, Araki T, et al. Effect of aerobic exercise on plasma adiponectin levels and insulin resistance in type 2 diabetes. Diabetes Care. 2004;27(7):1756–58. doi: 10.2337/diacare.27.7.1756. [DOI] [PubMed] [Google Scholar]
- 109.Haus JM, Solomon TP, Marchetti CM, Edmison JM, Gonzalez F, Kirwan JP. Free fatty acid-induced hepatic insulin resistance is attenuated following lifestyle intervention in obese individuals with impaired glucose tolerance. J Clin Endocrinol Metab. 2010;95(1):323–27. doi: 10.1210/jc.2009-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tamura Y, Tanaka Y, Sato F, et al. Effects of diet and exercise on muscle and liver intracellular lipid contents and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab. 2005;90(6):3191–96. doi: 10.1210/jc.2004-1959. [DOI] [PubMed] [Google Scholar]
- 111.Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27(1):155–61. doi: 10.2337/diacare.27.1.155. [DOI] [PubMed] [Google Scholar]
- 112.Scheen AJ, Van Gaal LF. Combating the dual burden: therapeutic targeting of common pathways in obesity and type 2 diabetes. Lancet Diabetes Endocrinol. 2014;2(11):911–22. doi: 10.1016/S2213-8587(14)70004-X. [DOI] [PubMed] [Google Scholar]
- 113.Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95(2):297–308. doi: 10.3945/ajcn.111.024927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Garvey WT, Ryan DH, Henry R, et al. Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care. 2014;37(4):912–21. doi: 10.2337/dc13-1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Martin CK, Redman LM, Zhang J, et al. Lorcaserin, a 5-HT(2C) receptor agonist, reduces body weight by decreasing energy intake without influencing energy expenditure. J Clin Endocrinol Metab. 2011;96(3):837–45. doi: 10.1210/jc.2010-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo-controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. Obesity. 2012;20(7):1426–36. doi: 10.1038/oby.2012.66. [DOI] [PubMed] [Google Scholar]
- 117.Smith SR, Fujioka K, Gupta AK, et al. Combination therapy with naltrexone and bupropion for obesity reduces total and visceral adiposity. Diabetes Obes Metab. 2013;15(9):863–66. doi: 10.1111/dom.12095. [DOI] [PubMed] [Google Scholar]
- 118.Hollander P, Gupta AK, Plodkowski R, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36(12):4022–29. doi: 10.2337/dc13-0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Holst JJ, Vilsboll T, Deacon CF. The incretin system and its role in type 2 diabetes mellitus. Mol Cell Endocrinol. 2009;297(1–2):127–36. doi: 10.1016/j.mce.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 120.Wood GC, Gerhard GS, Benotti P, et al. Preoperative use of incretins is associated with increased diabetes remission after RYGB surgery among patients taking insulin: a retrospective cohort analysis. Ann Surg. 2015;261(1):125–128. doi: 10.1097/SLA.0000000000000588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Davies MJ, Bergenstal R, Bode B, et al. Efficacy of Liraglutide for Weight Loss Among Patients with Type 2 Diabetes: The SCALE Diabetes Randomized Clinical Trial. JAMA. 2015;314(7):687–99. doi: 10.1001/jama.2015.9676. [DOI] [PubMed] [Google Scholar]
- 122.Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE Maintenance randomized study. Int J Obes. 2013;37(11):1443–51. doi: 10.1038/ijo.2013.120. [DOI] [PubMed] [Google Scholar]
- 123.Rhee MK, Herrick K, Ziemer DC, et al. Many Americans have pre-diabetes and should be considered for metformin therapy. Diabetes Care. 2010;33(1):49–54. doi: 10.2337/dc09-0341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.DeFronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58(4):773–95. doi: 10.2337/db09-9028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2004;27(1):256–263. doi: 10.2337/diacare.27.1.256. [DOI] [PubMed] [Google Scholar]
- 126.Chaggar PS, Shaw SM, Williams SG. Review article: Thiazolidinediones and heart failure. Diab Vasc Dis Res. 2009;6(3):146–152. doi: 10.1177/1479164109338772. [DOI] [PubMed] [Google Scholar]
- 127.Dormandy J, Bhattacharya M, van Troostenburg de Bruyn AR PROactive investigators. Safety and tolerability of pioglitazone in high-risk patients with type 2 diabetes: an overview of data from PROactive. Drug Saf. 2009;32(3):187–202. doi: 10.2165/00002018-200932030-00002. [DOI] [PubMed] [Google Scholar]
- 128.Kahn SE, Haffner SM, Heise MA, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355(23):2427–2443. doi: 10.1056/NEJMoa066224. [DOI] [PubMed] [Google Scholar]
- 129.Dormandy JA, Charbonnel B, Eckland DJ, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366(9493):1279–1289. doi: 10.1016/S0140-6736(05)67528-9. [DOI] [PubMed] [Google Scholar]
- 130.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373(22):2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 131.Bennett WL, Maruthur NM, Singh S, et al. Comparative effectiveness and safety of medications for type 2 diabetes: an update including new drugs and 2-drug combinations. Ann Intern Med. 2011;154(9):602–13. doi: 10.7326/0003-4819-154-9-201105030-00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86. doi: 10.1001/jama.2013.281361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–83. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 135.McGrice M, Don Paul K. Interventions to improve long-term weight loss in patients following bariatric surgery: challenges and solutions. Diabetes Metab Syndr Obes. 2015;8:263–274. doi: 10.2147/DMSO.S57054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Stein J, Stier C, Raab H, Weiner R. Review article: The nutritional and pharmacological consequences of obesity surgery. Aliment Pharmacol Ther. 2014;40(6):582–609. doi: 10.1111/apt.12872. [DOI] [PubMed] [Google Scholar]