Key Points
Question
Does Supplemental Nutrition Assistance Program (SNAP) participation reduce subsequent health care expenditures?
Findings
Using data from 4447 low-income adults who participated in the National Health Interview Survey (NHIS) and the Medical Expenditure Panel Survey (MEPS), we found that participation in SNAP was associated with lower health care expenditures by approximately $1400 per year.
Meaning
Programs that address food insecurity, such as SNAP, may reduce health care spending.
Abstract
Importance
Food insecurity is associated with high health care expenditures, but the effectiveness of food insecurity interventions on health care costs is unknown.
Objective
To determine whether the Supplemental Nutrition Assistance Program (SNAP), which addresses food insecurity, can reduce health care expenditures.
Design, Setting, and Participants
This is a retrospective cohort study of 4447 noninstitutionalized adults with income below 200% of the federal poverty threshold who participated in the 2011 National Health Interview Survey (NHIS) and the 2012-2013 Medical Expenditure Panel Survey (MEPS).
Exposures
Self-reported SNAP participation in 2011.
Main Outcomes and Measures
Total health care expenditures (all paid claims and out-of-pocket costs) in the 2012-2013 period. To test whether SNAP participation was associated with lower subsequent health care expenditures, we used generalized linear modeling (gamma distribution, log link, with survey design information), adjusting for demographics (age, gender, race/ethnicity), socioeconomic factors (income, education, Social Security Disability Insurance disability, urban/rural), census region, health insurance, and self-reported medical conditions. We also conducted sensitivity analyses as a robustness check for these modeling assumptions.
Results
A total of 4447 participants (2567 women and 1880 men) were enrolled in the study, mean (SE) age, 42.7 (0.5) years; 1889 were SNAP participants, and 2558 were not. Compared with other low-income adults, SNAP participants were younger (mean [SE] age, 40.3 [0.6] vs 44.1 [0.7] years), more likely to have public insurance or be uninsured (84.9% vs 67.7%), and more likely to be disabled (24.2% vs 10.6%) (P < .001 for all). In age- and gender-adjusted models, health care expenditures between those who did and did not participate in SNAP were similar (difference, $34; 95% CI, −$1097 to $1165). In fully adjusted models, SNAP was associated with lower estimated annual health care expenditures (−$1409; 95% CI, −$2694 to −$125). Sensitivity analyses were consistent with these results, also indicating that SNAP participation was associated with significantly lower estimated expenditures.
Conclusions and Relevance
SNAP enrollment is associated with reduced health care spending among low-income American adults, a finding consistent across several analytic approaches. Encouraging SNAP enrollment among eligible adults may help reduce health care costs in the United States.
This cohort study evaluates the association between participation in the SNAP program and reduced health care expenditures.
Introduction
Amid ever-increasing pressure to control societal health care costs, Americans with lower socioeconomic status consistently have worse health, and, often, higher health care expenditures. While the reasons for this are likely complex, an emerging body of research suggests that food insecurity, or the inability to consistently access nutritious food owing to cost, is one important reason. Conceptually, food insecurity may reduce dietary quality, force trade-offs between food and medical care, increase household stress, and sap cognitive “bandwidth” (the mental resources needed for complex chronic disease management).
The Supplemental Nutrition Assistance Program (SNAP) is the nation’s largest anti–food insecurity program, serving approximately 1 in 7 Americans. SNAP provides a monthly near-cash benefit to participants that supplements household budgets by allowing food purchases, with some restrictions (for example, SNAP cannot be used for alcohol). SNAP eligibility is set federally, but enrollment policies vary by state, and these policies can make it easier or harder to enroll, thus subtly encouraging or discouraging participation. SNAP is proven to reduce both the duration and severity of food insecurity episodes. Though SNAP is not a health program, there is growing interest among policy makers and clinicians about whether social programs such as SNAP may offer benefits in the health care sector. For example, the Centers for Medicare & Medicaid Services’ Accountable Health Communities intervention program will evaluate whether linking those with food insecurity to resources such as SNAP will affect health care expenditures.
The conceptual model of the relationship between food insecurity and health suggests several ways that programs to address food insecurity might reduce health care costs. In the long term, alleviating food insecurity may help reduce the incidence of chronic diet-sensitive conditions such as obesity and diabetes, and thus reduce their attendant effects on morbidity and mortality. In the short term, however, the prevalence of diabetes, obesity, coronary heart disease, and other chronic conditions is much greater than their incidence. Therefore, in the short-term, SNAP is most likely to improve health care expenditures by enhancing disease self-management, for example by off-loading food budgets to make available financial resources that can be spent on medications, reducing stress over subsistence needs, and freeing up cognitive bandwidth.
In this study, we sought to determine the relationship between SNAP program participation and health care costs over a 2-year period, accounting for factors that may influence the likelihood of participating in SNAP. We hypothesized that SNAP participation would be associated with lower subsequent health care expenditures.
Methods
Data Source and Study Sample
We used data from the 2011 National Health Interview Survey (NHIS) linked to Medical Expenditure Panel Survey (MEPS) 2012-2013 data. The NHIS is conducted by the National Center for Health Statistics as a nationally representative epidemiologic surveillance survey. Each year, the Agency for Healthcare Research and Quality generates a new cohort of MEPS participants from a subset of previous NHIS participants to gather health care expenditure data over a 2-year period. Trained interviewers conducted the surveys in English or Spanish. Self-reported expenditure data are both verified and supplemented using data from clinicians and payers. All adult (age ≥18 years) NHIS-MEPS participants were eligible for this study. Because SNAP is a means-tested program based on monthly income, which can fluctuate over the year, and similar to prior SNAP studies, we included participants as potentially eligible for SNAP if their annual income in the 2011 NHIS was below 200% of the federal poverty threshold for that year.
The Human Research Committee at Partners Healthcare exempted this analysis of deidentified data from human participants review.
Key Variables
SNAP Participation
The primary indicator of SNAP participation in this study was the following 2011 NHIS item: “At any time during the last calendar year, did you or any family members living here receive SNAP or food stamp benefits?” Those who responded affirmatively were categorized as participating in SNAP. Owing to limitations in duration of participation data, our analyses did not include duration or amount of benefits received.
Health Care Expenditures
The primary outcome for this study was total health care expenditures over the 2-year MEPS period (2012 through 2013). To aid understanding, we present annualized results in 2015 US dollars (using the Consumer Price Index, available at https://data.bls.gov:443/cgi-bin/cpicalc.pl). In MEPS, total health care expenditures are the actual amount of money either paid on behalf of the individual by a third party (costs, not charges) or spent by an individual as out-of-pocket costs.
Demographic, Socioeconomic, and Clinical Variables
We considered several factors that could confound the relationship between SNAP participation and health care expenditures. From the NHIS data, we extracted information on age (modeled with both a linear and quadratic term) gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and Asian/multiracial/other), household income as a percentage of the federal poverty level, educational attainment (less than high school diploma, high school diploma, greater than high school diploma), and whether one had applied for disability status. We categorized health insurance as private, Medicare (not including Medicare-Medicaid “dual eligibles”), other public (including Medicaid, dual eligibles, and Department of Veterans Affairs), and uninsured. To account for area variation in health care spending, we also included variables for census region (Northeast, Midwest, South, or West), and rural or urban location.
Because our conceptual model posited that the short-term effect, if any, of SNAP on health care expenditures could relate to disease management, we also included, from MEPS, self-reported presence or absence of several clinical conditions: obesity (body mass index >30), hypertension, coronary heart disease, diabetes mellitus, stroke, arthritis, and chronic obstructive pulmonary disease. Finally, we included an indicator of death during the study period.
Statistical Analysis
We first conducted descriptive statistics. Then we sought to determine the relationship between SNAP participation and subsequent health care expenditures. To do this, we adjusted for the observed covariates listed above. Because health care expenditure data generally contain many observations without any expenditures, but also observations with very high expenditures, we followed the approach proposed by Manning and Mullahy to determine the appropriate functional form for regression analysis, using a modified Park test. This led to selecting generalized linear regression with a gamma distribution and log link. For these analyses, we used the survey strata and sampling weights for NHIS-MEPS.
While standard regression can adjust for measured confounders, there may be unobserved characteristics that affect SNAP participation and health care expenditures. As a sensitivity analysis to address potential confounding by unrecorded factors, we used a technique called near/far matching (unpublished data, J.R., Michael Baiocchi, PhD, and S.B.; August 2017). A more detailed description of this approach is contained in the eAppendix in the Supplement, but in general, near/far matching can be thought of as filtering a cohort to find its most informative pairs—those who are very similar on measured characteristics (near) but are dissimilar (far) on the values of an instrumental variable (IV). An IV is one that, in some way, allocates treatment independently of the likelihood of experiencing the outcome, and thus is analogous to a randomized clinical trial. Finally, as an alternative to the IV-based analysis, we conducted an analysis using augmented inverse probability weighting (AIPW) (see the eAppendix in the Supplement for more detail).
For interpretation, we expressed results as the difference in US dollars spent per year, using the postestimation predictive margins command in Stata. To investigate factors that may confound the relationship between SNAP participation and health care expenditures, we created nested models to examine changes in the association seen by adjusting for different factors. To help understand policy implications of changing SNAP enrollment, we also evaluated the difference in expenditures between SNAP participation and nonparticipation for 2 groups who receive special emphasis in state budgets: those who are disabled and those who receive non-Medicare public health insurance, such as Medicaid. To determine whether there was support for our conceptual model, which posited that the short-term effects of SNAP participation would result from making illnesses easier to manage, we examined marginal predicted differences in health care expenditures for hypertension and coronary heart disease. These are 2 conditions where SNAP participation is particularly likely to affect management through dietary modification and making resources available for medications. We expected that differences between those who did and did not participate in SNAP would be greater for these conditions.
A 2-tailed P < .05 indicated statistical significance. Analyses were conducted in SAS, version 9.4 (SAS Institute Inc), Stata, version 14.0 (StataCorp LLC), and in R, version 3.3.1 (https://cran.r-project.org/), using the packages “nearfar” (https://cran.r-project.org/web/packages/nearfar/index.html) and “forestplot” (https://cran.r-project.org/web/packages/forestplot/forestplot.pdf).
Results
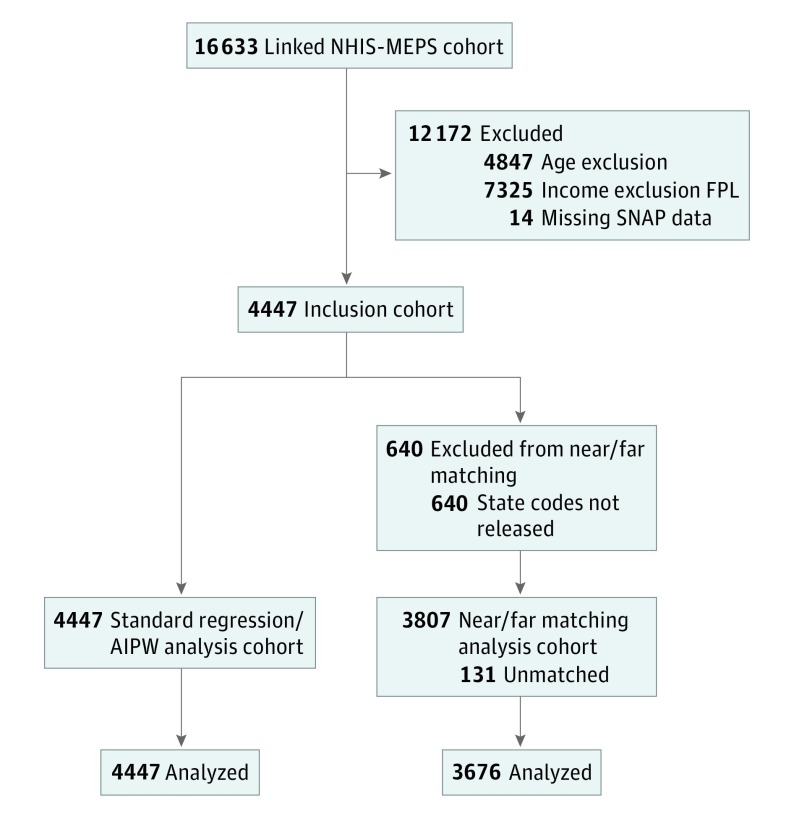
There were 4447 patients who met inclusion criteria (age >18 years, income <200% of federal poverty level, and information on SNAP participation) (Figure 1). Overall, as supported by the data reported in Table 1, there were significant demographic differences between those who did and did not report SNAP participation, with SNAP participants generally being younger, more likely to be a racial/ethnic minority, and poorer.
Figure 1. Study Flow Diagram.
Table 1. Demographic Characteristics of Included Study Participants by Participation in the SNAP Programa.
| Characteristic | No SNAP (n = 2558) |
SNAP (n = 1889) |
P Valueb |
|---|---|---|---|
| Age, mean (SE), y | 44.13 (0.7) | 40.29 (0.6) | <.001 |
| Female | 1383 (52.0) | 1184 (59.2) | <.001 |
| Race/ethnicity | <.001 | ||
| Non-Hispanic white | 689 (55.4) | 401 (45.0) | |
| Non-Hispanic black | 453 (11.6) | 657 (25.4) | |
| Hispanic | 1164 (25.0) | 739 (25.3) | |
| Asian/multi-ethnic/other | 252 (8.1) | 92 (4.3) | |
| Educational attainment | <.001 | ||
| <High school diploma | 841 (25.0) | 782 (36.4) | |
| High school diploma | 771 (32.0) | 599 (33.2) | |
| >High school diploma | 915 (43.1) | 476 (30.4) | |
| Income | <.001 | ||
| <100% FPL | 890 (32.1) | 1269 (62.9) | |
| 100%-149% FPL | 769 (29.0) | 395 (24.2) | |
| 150%-199% FPL | 899 (39.0) | 225 (12.9) | |
| Census region | .002 | ||
| Northeast | 381 (14.5) | 346 (17.5) | |
| Midwest | 366 (19.4) | 339 (23.0) | |
| South | 986 (39.8) | 799 (41.9) | |
| West | 825 (26.4) | 403 (17.6) | |
| Rural residence | 331 (16.7) | 328 (21.2) | .06 |
| Insurance | <.001 | ||
| Private | 664 (32.3) | 194 (15.1) | |
| Medicare | 301 (16.6) | 116 (6.5) | |
| Other public | 447 (14.9) | 881 (44.8) | |
| Uninsured | 1084 (36.1) | 643 (33.7) | |
| Died during study period | 27 (2.0) | 11 (1.3) | .34 |
| Reports disability | 250 (10.6) | 412 (24.2) | <.001 |
| Obesity | 771 (31.9) | 714 (38.6) | .003 |
| Hypertension | 835 (35.1) | 733 (39.1) | .06 |
| Heart disease | 329 (16.6) | 279 (17.5) | .54 |
| Diabetes | 263 (9.7) | 235 (12.0) | .09 |
| Stroke | 95 (4.5) | 113 (6.5) | .08 |
| Arthritis | 589 (28.8) | 525 (31.0) | .34 |
| Chronic obstructive pulmonary disease | 40 (2.6) | 57 (4.7) | .03 |
Abbreviations: FPL, federal poverty level; SNAP, Supplemental Nutrition Assistance Program.
Unless otherwise noted, data are number (weighted percentage) of participants.
P values are from χ2 tests for dichotomous variables and t tests for continuous variables.
In analyses adjusted only for age and gender, and likely still confounded by sociodemographics and selection issues, the annual mean expenditures for those who reported SNAP participation was $4628, compared with $4594 among those who did not report participation (difference, $34; 95% CI, −$1097 to $1165; P = .95) (Table 2).
Table 2. Estimated Differences in Annual Total Health Care Expenditure for 2015, Comparing Those Who Did and Did Not Participate in the SNAP Program.
| Characteristic | Difference (95% CI), $ |
|---|---|
| Age and gender adjusted | 34 (−1097 to 1165) |
| Fully adjusteda | −1409 (−2694 to −125) |
| Subgroups | |
| Insurance | |
| Private | −993 (−1902 to −84) |
| Medicare | −2709 (−5111 to −308) |
| Other public | −2544 (−5032 to −56) |
| Race/ethnicity | |
| Non-Hispanic white | −1853 (−3560 to −146) |
| Non-Hispanic black | −1255 (−2478 to −33) |
| Hispanic | −705 (−1336 to −74) |
| Disability status | |
| Not disabled | −943 (−1779 to −107) |
| Disabled | −3958 (−7796 to −119) |
| Comorbidities | |
| No hypertension | −689 (−1325 to −53) |
| Hypertension | −2654 (−5104 to −205) |
| No coronary heart disease | −860 (−1720 to −76) |
| Coronary heart disease | −4109 (−7971 to −247) |
Abbreviation: SNAP, Supplemental Nutrition Assistance Program.
Fully adjusted regression estimates from generalized linear model with gamma distribution and log link, incorporating survey design information, and adjusted for age, age squared, gender, race/ethnicity, region, rurality, insurance, education, income, disability, comorbidity, and death during study period. Full model can be found in the eAppendix in the Supplement.
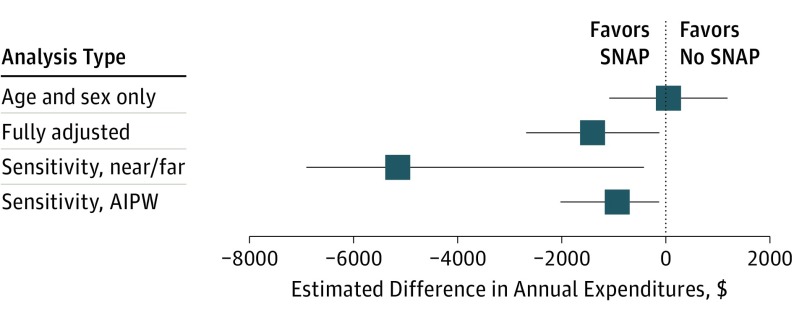
In generalized linear regression analyses adjusted for observed factors, SNAP participation was associated with a significant decrease in estimated expenditures: −$1409 per year in those who did, vs did not, report SNAP participation (95% CI, −$2694 to −$125; P = .03). The full model is detailed in eTable 3 in the Supplement. In sensitivity analyses, the results from both the near/far matching and AIPW techniques were qualitatively similar to the results from the generalized linear model, and both analyses found statistically significant differences in favor of SNAP (eTables 2-7 in the Supplement). Figure 2 presents a comparison of the effect estimates from the different analytic strategies.
Figure 2. Forest Plot Showing the Differences by Analysis Type in Estimated Mean (95% CI) Health Expenditures for Those Who Did and Did Not Receive Supplemental Nutrition Assistance Program (SNAP) Benefits.
Note that the estimands are slightly different across the methods: the fully adjusted regression estimates an effect conditional on the covariates; augmented inverse probability weighting (AIPW) estimates average treatment effect (ie, the effect of enrolling in SNAP for the entire population of adults with income <200% federal poverty level); and near/far instrumental variable analysis estimates local average treatment effect (ie, the effect in the marginal case where the instrument made the difference in receipt of SNAP benefits).
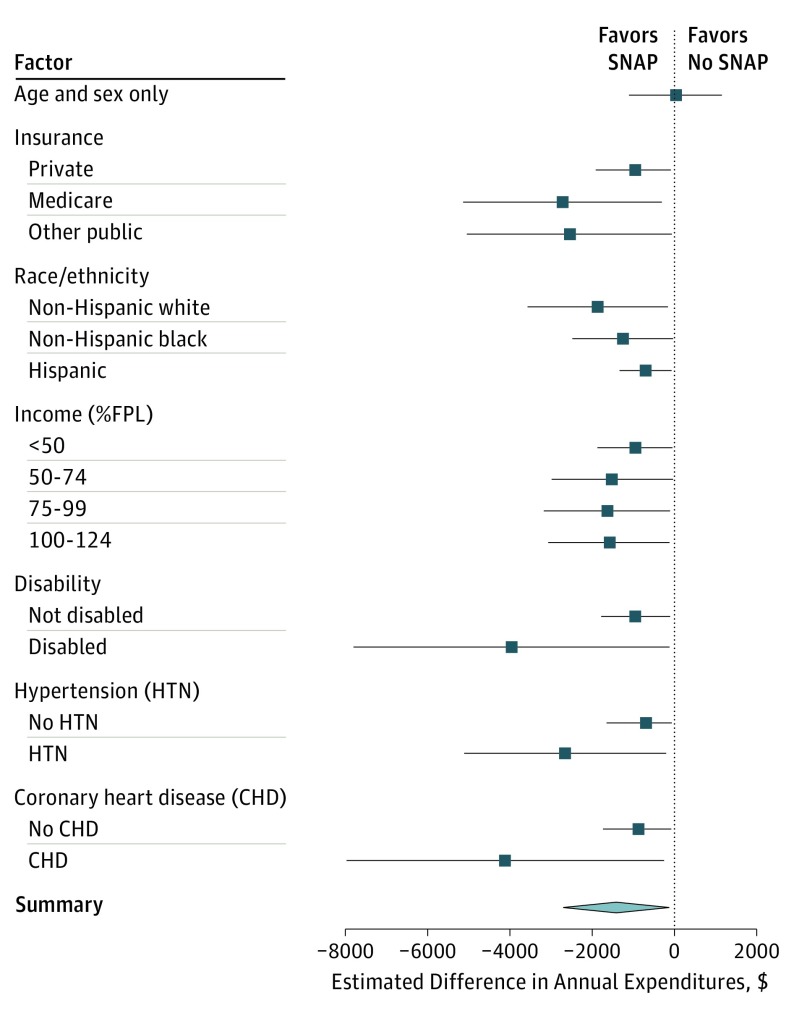
We next looked at differences by subgroup. By conducting a series of nested models, we found that age, insurance, disability, and comorbidity were likely important confounders of the relationship between SNAP participation and health care expenditures (eFigure 1 in the Supplement). In specific subgroups, estimated differences in health care expenditures between those who did and did not participate in SNAP were notably large in those who receive non-Medicare public health insurance such as Medicaid (−$2544; 95% CI, −5032 to −$56), those who are disabled (−$3958; 95% CI, −$7796 to −$107), those with hypertension (−$2654; 95% CI, −$5104 to −$205), and those with coronary heart disease (−$4109; 95% CI, −$7971 to −$247) (Figure 3).
Figure 3. Forest Plot Comparing the Mean (95% CI) Differences by Sociodemographic and Clinical Subgroups in Estimated Mean Health Expenditures for Those Who Did and Did Not Receive Supplemental Nutrition Assistance Program (SNAP) Benefits.
FPL indicates federal poverty level.
Discussion
In this study of NHIS-MEPS data from 2011 through 2013, we found that SNAP participation was associated with approximately $1400 per year per person lower subsequent health care expenditures in low-income adults. This represents approximately 30% of the unadjusted average annual expenditure in the study. Though the estimated amount saved varied somewhat by analytic approach, the finding of reduced health care expenditures associated with SNAP participation was robust across several different strategies, which made different modeling assumptions, and was estimated to be greater for participants with diet-sensitive conditions previously linked to food insecurity. For comparison, the average per-person SNAP benefit across the United States is $129 per month, or $1548 over a 12-month period.
This study is consistent with and expands our knowledge regarding the impact of SNAP on health and health care expenditures. The adjusted results reveal that unadjusted estimates are likely confounded by measurable factors such as age, insurance status, disability, and comorbidity. Prior studies have shown that food insecurity is associated with greater health care expenditures, and that SNAP participants are sicker and poorer than income-eligible nonparticipants, but it was unclear if food insecurity interventions could reduce health care costs. Furthermore, an emerging body of evidence suggests that interventions targeting food insecurity can improve cardiometabolic risk factors, which supports a potential mechanism (improved clinical control of chronic disease) for the observed findings.
The results of this study have several policy indications. Prioritizing ways to make it easier for eligible Americans to enroll in SNAP is likely to be a feasible way to help reduce health care costs. This may be of particular interest to states because of differences in the funding source between SNAP and health care costs. As an entitlement program, SNAP benefits are paid for by the federal government, while Medicaid, which would likely see some of the savings if health care costs are reduced, is paid for jointly by states and the federal government. Therefore, state policies regarding SNAP enrollment may help off-load state Medicaid budgets. Though not directly addressed here, the study’s findings also have implications for ongoing discussions about modifying SNAP, including eligibility restrictions, funding structure, and changes in benefit levels.
Although this study focused on health care expenditures, SNAP is a food insecurity and nutrition program, not a health care program. SNAP’s purpose is not to reduce health care expenditures, and we are of the opinion that its funding justification does not depend on affecting health care costs.
This study helps answer whether SNAP is associated with short-term changes in health care expenditures. Nevertheless, several questions remain unanswered, and represent promising directions for future work. Examining the trajectory of expenditures in the period before and after SNAP enrollment would add important detail to our understanding of SNAP effects. It is also important to develop a deeper understanding of the mechanism by which SNAP, and other food insecurity assistance programs, could lead to changes in health and health care expenditures. It is important to evaluate whether there is a “dose-response” relationship between duration of SNAP participation and expenditures, whether effects persist over longer periods of time, and whether longer evaluation periods can detect clinical changes, such as reduced incidence of diabetes or cardiovascular events. Finally, determining the health status of those who are eligible, but not enrolled in SNAP, will help determine what population-level effect expanded SNAP enrollment would be likely to have.
Limitations
The results of this study should be interpreted in light of several limitations. The data source did not have sufficient incident SNAP participants to permit a comparison of expenditures before and after SNAP enrollment or to allow for a difference-in-differences design. SNAP assessment occurred at a single point in time. Since low-income households often cycle on and off SNAP, this may have resulted in misclassification, either for those who later participated in SNAP, or, given lack of data on participation length, those who were only enrolled for a very brief period. Other sources of misclassification could include lack of information on eligibility criteria other than income (such as immigration status or assets), not reporting SNAP participation owing to stigma, or, for participants in California where SNAP is combined with Supplemental Security Income payments, not recognizing the source of their benefits. These types of misclassification would likely bias estimates to the null.
The methods used as sensitivity analyses have important limitations that are worth noting. While standard tests of the instruments we used were consistent with their validity, ultimately IV approaches rely on assumptions that cannot be empirically tested. The generalizability of the findings in the near/far analysis may have been limited because we were unable to incorporate survey design information into these analyses. However, since the matching process breaks the geographical link this may not be a significant issue. Though the estimates across the methods are qualitatively similar, the quantity estimated by the IV analysis is different from the standard regression analysis. The IV analyses do not estimate population-level effects but rather a local average treatment effect, or the change in outcome in those for whom the instrument made the difference in receipt of SNAP. Finally, the AIPW analyses are statistically less efficient than the maximum likelihood estimates from the standard regression. These limitations are, however, balanced by key strengths: the data are longitudinal, and the MEPS assessment of health care expenditures follows a rigorous methodology to capture both out-of-pocket and third-party expenditures.
Conclusions
Across several analytic approaches, including an IV approach that accounts for unmeasured confounding, SNAP participation was associated with lower subsequent health care expenditures for low-income adults. Helping to address food insecurity by making SNAP enrollment easier may be an important way to contain health care costs for vulnerable Americans.
eAppendix. Technical appendix and sensitivity analyses
eTable 1. Generalized Linear Regression, full model
eTable 2. Tests of IV
eTable 3. List of included states
eTable 4. post-‘Near/Far’ matching demographics, by ‘encouragement’ status
eTable 5. post-‘Near/Far’ Matching Two stage residual inclusion model
eTable 6. Balance statistics and overidentifying restrictions test for augmented inverse
probability weighted analyses
eTable 7. Auxiliary equations for augmented inverse probability weighting analyses
eReferences.
eFigure 1. Change in estimated difference between participating and not participating in SNAP, in a series of nested models to explore potential confounders
References
- 1.Agency for Healthcare Research and Quality 2014 National Healthcare Quality & Disparities Report. 2015. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr14/index.html. Accessed January 6, 2017.
- 2.Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high-need, high-cost patients: an urgent priority. N Engl J Med. 2016;375(10):909-911. [DOI] [PubMed] [Google Scholar]
- 3.Chetty R, Stepner M, Abraham S, et al. . The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750-1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093-3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berkowitz SA, Fabreau GE. Food insecurity: what is the clinician’s role? CMAJ. 2015;187(14):1031-1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkowitz SA, Gao X, Tucker KL. Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: results from the Boston Puerto Rican Health study. Diabetes Care. 2014;37(9):2587-2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berkowitz SA, Meigs JB, DeWalt D, et al. . Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303-310.e3. [DOI] [PubMed] [Google Scholar]
- 9.Carmichael SL, Yang W, Herring A, Abrams B, Shaw GM. Maternal food insecurity is associated with increased risk of certain birth defects. J Nutr. 2007;137(9):2087-2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castillo DC, Ramsey NL, Yu SS, Ricks M, Courville AB, Sumner AE. Inconsistent access to food and cardiometabolic disease: the effect of food insecurity. Curr Cardiovasc Risk Rep. 2012;6(3):245-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook JT, Frank DA, Berkowitz C, et al. . Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432-1438. [DOI] [PubMed] [Google Scholar]
- 12.Crews DC, Kuczmarski MF, Grubbs V, et al. ; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team . Effect of food insecurity on chronic kidney disease in lower-income Americans. Am J Nephrol. 2014;39(1):27-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. Food insecurity is associated with iron deficiency anemia in US adolescents. Am J Clin Nutr. 2009;90(5):1358-1371. [DOI] [PubMed] [Google Scholar]
- 14.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff (Millwood). 2015;34(11):1830-1839. [DOI] [PubMed] [Google Scholar]
- 15.Heflin C, Ziliak J. Food insufficiency, food stamp participation, and mental health. Soc Sci Q. 2008;89(3):706-727. [Google Scholar]
- 16.Heflin CM, Siefert K, Williams DR. Food insufficiency and women’s mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med. 2005;61(9):1971-1982. [DOI] [PubMed] [Google Scholar]
- 17.Lehnert T, Heider D, Leicht H, et al. . Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387-420. [DOI] [PubMed] [Google Scholar]
- 18.Mayer VL, McDonough K, Seligman H, Mitra N, Long JA. Food insecurity, coping strategies and glucose control in low-income patients with diabetes. Public Health Nutr. 2016;19(6):1103-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morales ME, Berkowitz SA. The relationship between food insecurity, dietary patterns, and obesity. Curr Nutr Rep. 2016;5(1):54-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreno G, Morales LS, Isiordia M, et al. . Latinos with diabetes and food insecurity in an agricultural community. Med Care. 2015;53(5):423-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22(7):1018-1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10(2):177-185. [DOI] [PubMed] [Google Scholar]
- 26.Wang EA, McGinnis KA, Goulet J, et al. ; Veterans Aging Cohort Study Project Team . Food insecurity and health: data from the Veterans Aging Cohort Study. Public Health Rep. 2015;130(3):261-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhargava V, Lee JS. Food insecurity and health care utilization among older adults in the United States. J Nutr Gerontol Geriatr. 2016;35(3):177-192. [DOI] [PubMed] [Google Scholar]
- 28.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6-9. [DOI] [PubMed] [Google Scholar]
- 29.United States Department of Agriculture Food and Nutrition Service Supplemental Nutrition Assistance Program (SNAP). 2016; https://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program-snap. Accessed February 26, 2016.
- 30.Service ER. SNAP Policy Database. 2016; https://www.ers.usda.gov/data-products/snap-policy-database/. Accessed January 6, 2017.
- 31.Gregory C, Ploeg MV, Andrews M, Coleman-Jensen A Supplemental Nutrition Assistance Program (SNAP) Participation Leads to Modest Changes in Diet Quality. Economic Research Service: Economic Research Report Number 147; 2013. https://www.ers.usda.gov/webdocs/publications/45059/36939_err147.pdf?v=41388. Accessed January 6, 2017.
- 32.Mabli J, Ohls J, Dragoset L, Castner L, Santos B Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Security. Prepared by Mathematica Policy Research for the U.S. Department of Agriculture, Food and Nutrition Service. 2013. https://www.fns.usda.gov/sites/default/files/Measuring2013.pdf. Accessed August 15, 2017.
- 33.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8-11. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention About the National Health Interview Survey. https://www.cdc.gov/nchs/nhis/about_nhis.htm. Accessed April 14, 2016.
- 35.Centers for Disease Control and Prevention 2011. Data Release. https://meps.ahrq.gov/mepsweb/. Accessed April 14, 2016.
- 36.Agency for Healthcare Research and Quality Medical Expenditure Panel Survey. https://meps.ahrq.gov/mepsweb/. Accessed April 14, 2016.
- 37.Harnack L, Oakes JM, Elbel B, Beatty T, Rydell S, French S. Effects of subsidies and prohibitions on nutrition in a food benefit program: a randomized clinical trial. JAMA Intern Med. 2016;176(11):1610-1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coleman-Jensen A, Nord M Food insecurity among households with working-age adults with disabilities. USDA Economic Research Report 2013;No. ERR-144. https://www.ers.usda.gov/publications/pub-details/?pubid=45040. Accessed August 15, 2017.
- 39.Coleman-Jensen A, Nord M Disability Is an Important Risk Factor for Food Insecurity. USDA, ERS. Amber Waves. https://www.ers.usda.gov/amber-waves/2013/may/disability-is-an-important-risk-factor-for-food-insecurity. Accessed August 15, 2017.
- 40.Sutherland JM, Fisher ES, Skinner JS. Getting past denial—the high cost of health care in the United States. N Engl J Med. 2009;361(13):1227-1230. [DOI] [PubMed] [Google Scholar]
- 41.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461-494. [DOI] [PubMed] [Google Scholar]
- 42.Baiocchi M, Small DS, Yang L, Polsky D, Groeneveld PW. Near/far matching: a study design approach to instrumental variables. Health Serv Outcomes Res Methodol. 2012;12(4):237-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130(2):270-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Glynn AN, Quinn KM. An introduction to the augmented inverse propensity weighted estimator. Polit Anal. 2010;18:36-56. [Google Scholar]
- 45.Service ER. Supplemental Nutrition Assistance Program FY14 through FY17 National View Summary. 2016; https://www.fns.usda.gov/sites/default/files/pd/34SNAPmonthly.pdf. Accessed January 6, 2017.
- 46.Tarasuk V, Cheng J, de Oliveira C, Dachner N, Gundersen C, Kurdyak P. Association between household food insecurity and annual health care costs. CMAJ. 2015;187(14):E429-E436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seligman HK, Lyles C, Marshall MB, et al. . A pilot food bank intervention featuring diabetes-appropriate food improved glycemic control among clients in three states. Health Aff (Millwood). 2015;34(11):1956-1963. [DOI] [PubMed] [Google Scholar]
- 48.Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177(2):244-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaiser Family Foundation Medicaid Spending per Enrollee (Full or Partial Benefit). 2016; http://www.kff.org/medicaid/state-indicator/medicaid-spending-per-enrollee/?currentTimeframe=0. Accessed December 9, 2016.
- 50.Imbens GW. Better LATE Than Nothing: Some Comments on Deaton (2009) and Heckman and Urzua (2009). National Bureau of Economic Research Working Paper Series. 2009;No. 14896.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Technical appendix and sensitivity analyses
eTable 1. Generalized Linear Regression, full model
eTable 2. Tests of IV
eTable 3. List of included states
eTable 4. post-‘Near/Far’ matching demographics, by ‘encouragement’ status
eTable 5. post-‘Near/Far’ Matching Two stage residual inclusion model
eTable 6. Balance statistics and overidentifying restrictions test for augmented inverse
probability weighted analyses
eTable 7. Auxiliary equations for augmented inverse probability weighting analyses
eReferences.
eFigure 1. Change in estimated difference between participating and not participating in SNAP, in a series of nested models to explore potential confounders