Key Points
Question
What clinical factors are associated with a major pathologic response following preoperative therapy for pancreatic ductal adenocarcinoma?
Findings
In this study of 583 patients with histopathologically confirmed pancreatic ductal adenocarcinoma who were treated with preoperative therapy, those with a pathologic complete response or less than 5% viable cancer cells had a significantly longer median survival duration (73.4 months vs 32.2 months). On multivariable logistic regression analysis, young age, low baseline cancer antigen 19-9 level, and the use of gemcitabine as a radiosensitizer were associated with a major pathologic response.
Meaning
The patient, treatment, and tumor-related factors identified in this study may define a group of patients most likely to experience a significant response to preoperative therapy.
Abstract
Importance
We previously demonstrated that a major pathologic response to preoperative therapy, defined histopathologically by the presence of less than 5% viable cancer cells in the surgical specimen, is an important prognostic factor for patients with pancreatic ductal adenocarcinoma. However, to our knowledge, the patients most likely to experience a significant response to therapy are undefined.
Objective
To identify clinical factors associated with major pathologic response in a large cohort of patients who underwent preoperative therapy and pancreatectomy for pancreatic ductal adenocarcinoma.
Design, Setting, and Participants
Retrospective review of a prospectively maintained database at University of Texas MD Anderson Cancer Center. The study included 583 patients with histopathologically confirmed pancreatic ductal adenocarcinoma who received preoperative therapy prior to pancreatectomy between 1990 and 2015.
Exposures
Preoperative therapy consisted of systemic chemotherapy alone (n = 38; 6.5%), chemoradiation alone (n = 261; 44.8%), or both (n = 284; 48.7%) prior to pancreatoduodenectomy (n = 514; 88.2%), distal pancreatectomy (n = 62; 10.6%), or total pancreatectomy (n = 7; 1.2%).
Main Outcomes and Measures
Clinical variables associated with a major pathologic response (pathologic complete response or <5% residual cancer cells) were evaluated using logistic regression.
Results
Among all patients, the mean (SD) age was 63.7 (9.2) years, and 53.0% were men. A major pathologic response was seen in 77 patients (13.2%) including 23 (3.9%) who had a complete pathologic response. The median overall survival duration was significantly longer for patients who had a major response than for those who did not (73.4 months vs 32.2 months, P < .001). On multivariate logistic regression, only age younger than 50 years, baseline serum cancer antigen 19-9 level less than 200 U/mL, and gemcitabine as a radiosensitizer were associated with a major response. The number of these positive factors was associated with the likelihood of a major response in a stepwise fashion (0, 7.5%; 1, 12.7%; 2, 16.9%; 3, 35.7%; P = .009).
Conclusions and Relevance
Although a major pathologic response occurs infrequently following preoperative therapy for pancreatic ductal adenocarcinoma, it is associated with a significantly improved prognosis. Of the patient- and treatment-related factors we analyzed, only young age, low baseline cancer antigen 19-9, and gemcitabine as a radiosensitizer were associated with a major pathologic response. Given its association with long-term survival, better predictors of response and more effective preoperative regimens should be aggressively sought.
This study identifies clinical factors associated with major pathologic response in a large cohort of patients who underwent preoperative therapy and pancreatectomy for pancreatic ductal adenocarcinoma.
Introduction
Recent practice guidelines have recognized the administration of chemotherapy and/or radiation therapy prior to pancreatectomy for localized pancreatic ductal adenocarcinoma (PDAC) as the preferred treatment strategy for patients with borderline resectable cancer and an acceptable treatment option for patients with potentially resectable cancer. Purported benefits of this approach include the selection of patients with favorable tumor biology and a physiologic profile appropriate for major surgery, early treatment of micrometastatic disease, facilitation of a margin-negative resection, and guaranteed delivery of all components of multimodality therapy. During the past 3 decades, refinement of the therapeutic regimens administered in the preoperative setting has permitted the rational use of potentially curative surgery in patients with anatomically advanced cancer and has contributed to a significant increase in overall survival duration following pancreatectomy.
The response of the primary tumor to preoperative therapy, measured histologically by the extent of residual carcinoma in the resected surgical specimen, represents an important prognostic factor for patients with PDAC, just as it does for patients with cancers of the breast, rectum, and esophagus. However, a pathologic complete response (pCR) occurs infrequently in PDAC relative to these other cancers. We previously identified only 6 of 223 patients (2.7%) treated with preoperative therapy and pancreatoduodenectomy who experienced a pCR, while another 36 patients (16.1%) had minimal residual tumor (ie, <5% viable cells) in the surgical specimen. Patients who had either a pCR or less than 5% residual cancer cells had a significantly longer survival duration than patients in whom the response to therapy was less robust (ie, 5%-100% residual cancer cells).
A complete understanding of the factors associated with a significant response to preoperative therapy would have profound clinical importance. These factors might suggest the underlying mechanisms by which treatment effect occurs. More practically, the presence of these factors might identify a group of patients for whom a multimodality strategy using preoperative therapy would be particularly appropriate. Several clinical features have been found to be predictive of pCR in patients with breast, rectal, and esophageal cancer. However, to our knowledge, factors associated with a significant treatment response have not been defined in PDAC.
In this study, we sought to identify clinical factors associated with a major pathologic response (pCR or <5% residual viable tumor cells) in a large cohort of patients who underwent preoperative therapy and pancreatectomy for PDAC at the University of Texas MD Anderson Cancer Center.
Methods
The institutional review board of the University of Texas MD Anderson Cancer Center, Houston, approved this retrospective study. Individual informed consent was waived. We used a prospectively maintained institutional pancreatic tumor database to identify all patients who received preoperative chemotherapy and/or chemoradiation (CRT) prior to pancreatectomy for PDAC between January 1990 and December 2015. Patients who received preoperative therapy prior to referral (n = 76) and those in whom histopathologic treatment effect was not recorded (n = 111) were excluded.
Staging
Prior to the initiation of preoperative therapy, all patients underwent comprehensive clinical and radiographic staging, including cross-sectional imaging of the abdomen and pelvis, a chest radiograph or chest computed tomography/magnetic resonance imaging scan, and laboratory studies, including serum cancer antigen (CA) 19-9 measurement. The most recent CA 19-9 level prior to initiation of preoperative therapy was used for this analysis. Tumor anatomy was classified as potentially resectable, borderline resectable, or locally advanced according to standardized radiographic criteria. A histopathologic diagnosis of PDAC was required for initiation of preoperative therapy.
Preoperative Therapy
Decisions regarding preoperative therapy were made as part of a multidisciplinary program, and treatments were administered either on or off protocol. Several preoperative treatment regimens were used during the study period. External-beam radiation therapy with concurrent 5-fluorouracil, capecitabine, or gemcitabine was generally delivered to a total of 50.4 Gy over 6 weeks or to a total of 30 Gy over 2 weeks. When both systemic chemotherapy and CRT were used, systemic chemotherapy was administered prior to CRT.
Surgical Technique
Within 4 to 8 weeks of completing all intended preoperative therapy, patients underwent repeated clinical and radiographic staging. Those without evidence of disease progression and with adequate performance status were considered for surgical resection. Pancreatoduodenectomy, distal pancreatectomy, or total pancreatectomy was performed according to standardized techniques.
Histopathologic Analysis
All surgical specimens were evaluated by dedicated gastrointestinal pathologists using a standardized protocol. R1 margin status was defined as evidence of cancer cells present at the inked bile duct, pancreatic neck, or superior mesenteric artery margin. The histopathologic response to preoperative therapy was measured as the percentage of residual viable cancer cells within the tumor. Based on our prior work, a pCR (no residual viable cancer cells) or less than 5% residual viable cancer cells were defined as evidence of a major pathologic response.
Postoperative Therapy and Follow-up
Following surgical resection, adjuvant therapy was administered selectively based on individual patient and tumor characteristics. Patients were typically evaluated initially every 3 to 4 months and then later every 6 months, with cross-sectional imaging, physical examination, and CA 19-9 analysis according to a standardized protocol. Locoregional recurrence was defined as the development of a new low-density mass in the region of the resected pancreas or new lymphadenopathy localized to the root of the mesentery occurring as a component of first failure following surgery.
Statistical Analysis
Clinical, demographic, and pathologic variables were compared among patients with less than 5% and at least 5% residual cancer cells. Categorical variables were compared using Pearson χ2, while continuous variables were compared using the Mann-Whitney U test. Next, demographic and clinical factors were investigated for their association with clinical response using univariate and multivariate logistic regression modeling. Factors included in the final model were determined using backward conditional regression. Finally, overall survival was calculated from the date of diagnosis to the date of death or last follow-up using the Kaplan-Meier method and compared between the 2 groups using the Mantel-Cox log-rank test. Curves were created using GraphPad Prism 6.0 (GraphPad Software Inc), and statistical analyses were performed using SPSS, version 24.0 (SPSS Inc), with statistical significance established at P < .05. The P value was 2-sided.
Results
A total of 583 patients with localized PDAC received preoperative chemotherapy (n = 38; 6.5%), CRT (n = 261; 44.8%), or both (n = 284; 48.7%) prior to pancreatectomy between 1990 and 2015 and had their tumor specimens graded for treatment effect. Most patients (n = 514; 88.2%) underwent pancreatoduodenectomy.
A major pathologic response to preoperative therapy was observed in the surgical specimens of 77 patients (13.2%); among them, 23 (3.9%) had no viable cells, and 54 (9.3%) had less than 5% viable cells. The specimens of the remaining 506 patients (86.8%) had at least 5% viable cells (Table 1). Patients who had a major pathologic response were younger (mean [SD] age, 61.5 [10.6] years vs 64.1 [9.0] years; P = .02) and more likely to present with a CA 19-9 level less than 200 U/mL (70.1% vs 56.9%, P = .03) than patients who did not, but the groups were similar in terms of the regimens they had received and their mean duration of therapy. Patients who had a major response were less likely to have undergone vascular resection than patients who did not, and their tumors were smaller and less likely to have positive margins, positive lymph nodes, lymphovascular invasion, or perineural invasion (Table 1). Patients with a major response were also less likely to have been treated with postoperative chemotherapy (18.2% vs 37.0%, P = .001).
Table 1. Complete Demographic, Clinical, and Pathologic Data for Patients Who Experienced a Major Pathologic Response (Less Than 5% Residual Cancer Cells) and Those Who Did Not (At Least 5% Residual Cancer Cells) Following Preoperative Therapy for PDAC.
| Characteristic | Major Pathologic Response, No. (%) | P Value | |
|---|---|---|---|
| Yes (<5% Residual Cells) (n = 77) |
No (≥5% Residual Cells) (n = 506) |
||
| Demographic/clinical | |||
| Mean age, y, (SD) | 61.5 (10.6) | 64.1 (9.0) | |
| Age, y | |||
| <50 | 11 (14.3) | 30 (5.9) | .02 |
| 50-70 | 51 (66.2) | 343 (67.8) | |
| >70 | 15 (19.5) | 133 (26.3) | |
| Male sex | 39 (50.6) | 270 (53.4) | .66 |
| CA 19-9 level, mean (SD), U/mL | 401 (1212) | 714 (109300) | .60 |
| CA 19-9 level <200 U/mL | 54 (70.1) | 288 (56.9) | .03 |
| Radiographic stage | |||
| Potentially resectable | 60 (77.9) | 365 (72.6) | .37 |
| Borderline resectable | 14 (18.2) | 96 (19.1) | |
| Locally advanced | 3 (3.9) | 42 (8.3) | |
| Preoperative therapies | |||
| Any chemotherapy | 43 (55.8) | 278 (54.9) | .72 |
| Any radiation therapy | 76 (98.7) | 476 (94.1) | .08 |
| Chemotherapy type | |||
| None | 34 (44.1) | 228 (45.1) | .81 |
| Gemcitabine | 3 (3.9) | 24 (4.7) | |
| Gemcitabine + other | 31 (40.3) | 188 (37.2) | |
| FOLFIRINOX | 8 (10.4) | 48 (9.5) | |
| Gemcitabine + nab-paclitaxel | 0 | 12 (2.4) | |
| Other | 1 (1.3) | 6 (1.2) | |
| Radiation dose | .29 | ||
| None | 1 (1.3) | 30 (5.9) | |
| Hypofractionated | 35 (45.5) | 237 (46.8) | |
| Standard fractionated | 39 (50.6) | 229 (45.3) | |
| Unknown | 2 (2.6) | 10 (2.0) | |
| Radiation sensitizer | .08 | ||
| Gemcitabine | 44 (57.1) | 216 (45.3) | |
| 5-FU/capecitabine | 31 (40.3) | 254 (53.3) | |
| Other | 2 (2.6) | 6 (1.3) | |
| Treatment interval, mean (SD), mo | 5.3 (2.5) | 5.2 (2.4) | .69 |
| Surgery | |||
| Type of surgery | |||
| Pancreatoduodenectomy | 70 (90.9) | 444 (87.7) | .51 |
| Distal pancreatectomy | 7 (9.1) | 55 (10.9) | |
| Total pancreatectomy | 0 | 7 (1.4) | |
| Surgery, y | |||
| 1990-1999 | 7 (9.1) | 45 (8.9) | .97 |
| 2000-2004 | 20 (26.0) | 119 (23.5) | |
| 2005-2009 | 21 (27.3) | 146 (28.9) | |
| 2010-2015 | 29 (37.7) | 196 (38.7) | |
| Vascular resection performed | 20 (26.0) | 247 (48.8) | <.001 |
| EBL, mL | |||
| <500 | 39 (50.6) | 217 (43.2) | .12 |
| 500-1000 | 29 (37.7) | 176 (35.1) | |
| >1000 | 9 (11.7) | 109 (21.7) | |
| Lymph nodes excised | |||
| <15 | 10 (13.0) | 92 (18.2) | .53 |
| 15-30 | 49 (63.6) | 300 (59.3) | |
| >30 | 18 (23.4) | 114 (22.5) | |
| Pathology | |||
| Mean tumor size, cm (SD) | 1.5 (1.6) | 2.8 (1.3) | <.001 |
| Differentiation | |||
| Well/moderate | 41 (53.2) | 335 (66.2) | <.001 |
| Poor | 15 (19.5) | 159 (31.4) | |
| Unknown | 21 (27.3) | 12 (2.4) | |
| R1 margin | 0 | 44 (8.7) | .02 |
| Positive LN status | 18 (23.4) | 280 (55.3) | <.001 |
| LNR | |||
| 0 | 59 (76.6) | 226 (44.7) | <.001 |
| ≤0.2 | 14 (18.2) | 217 (42.9) | |
| >0.2 | 4 (5.2) | 63 (12.5) | |
| Lymphovascular invasion | |||
| No | 63 (81.8) | 238 (47.0) | <.001 |
| Yes | 7 (9.1) | 220 (43.5) | |
| Unknown | 7 (9.1) | 48 (9.5) | |
| Perineural invasion | |||
| No | 48 (62.3) | 73 (14.4) | <.001 |
| Yes | 19 (24.7) | 401 (79.2) | |
| Unknown | 10 (13.0) | 32 (6.3) | |
| Postoperative therapy | |||
| Chemotherapy | 14 (18.2) | 186 (36.8) | .001 |
| Chemoradiation | 0 | 3 (0.6) | .48 |
| Outcomes | |||
| Follow-up, mean (SD), mo | 59.0 (43.4) | 39.4 (35.5) | <.001 |
| Locoregional recurrence | 9 (11.7) | 99 (19.6) | .08 |
| Overall survival | |||
| 5 y, % | 58.2 | 28.8 | <.001 |
| Median, mo | 73.4 | 32.2 | |
Abbreviations: CA, cancer antigen; EBL, estimated blood loss; FOLFIRINOX, 5-FU, leucovorin, oxaliplatin, irinoteca; LN, lymph node; LNR, lymph node ratio; PDAC, pancreatic ductal adenocarcinoma; 5-FU, 5-fluorouracil.
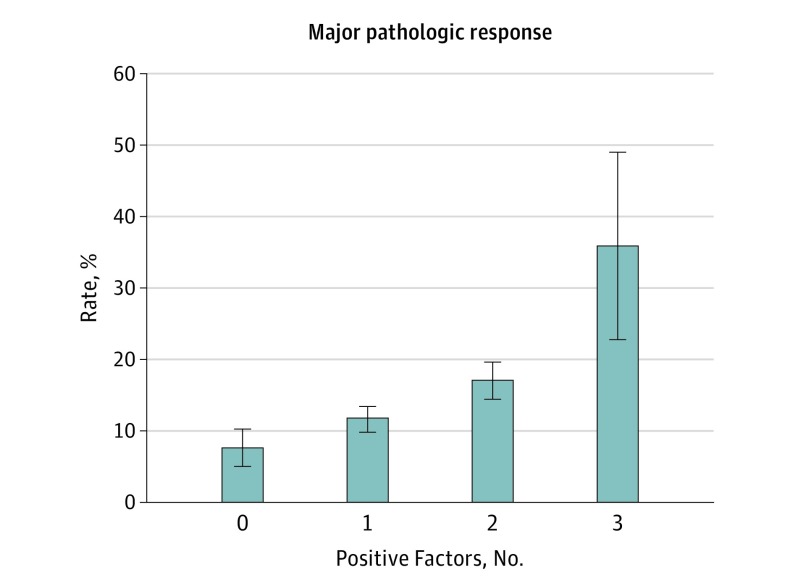
On univariate logistic regression, younger age, lower baseline CA 19-9 level, and the use of gemcitabine as a radiosensitizer were associated with a significant treatment effect (Table 2). No other treatment-related variables, including type of chemotherapy, dose of radiation, or duration of preoperative therapy, were associated with treatment effect. On multivariate logistic regression, age younger than 50 years, CA 19-9 level less than 200 U/mL, and gemcitabine as a radiosensitizer were associated with major response (Table 2). The number of predictive factors was associated with the rate of a major pathologic response in a stepwise fashion (0, 7.5%; 1, 12.7%; 2, 16.9%; 3, 35.7%; P = .009, Figure 1).
Table 2. Univariate and Multivariate Logistic Regression Analysis of Preoperative Predictors of Major Pathologic Response.
| Factor | Univariate, Odds Ratio (95% CI) | P Value | Multivariate, Odds Ratio (95% CI) | P Value |
|---|---|---|---|---|
| Demographic/clinical | ||||
| Age, y | ||||
| <50 | 1 [Reference] | NA | 1 [Reference] | NA |
| 50-70 | 0.41 (0.19-0.86) | .02 | 0.44 (0.20-0.98) | .04 |
| >70 | 0.31 (0.13-0.74), | <.01 | 0.28 (0.11-0.71) | <.01 |
| Male sex | 0.90 (0.56-1.45) | .66 | NA | NA |
| CA 19-9 level <200 U/mL | 1.70 (1.00-2.88) | .05 | 1.72 (1.00-2.98) | .05 |
| Radiographic stage | ||||
| Potentially resectable | 1 [Reference] | NA | NA | NA |
| Borderline resectable | 0.89 (0.48-1.66) | .71 | NA | NA |
| Locally advanced | 0.44 (0.13-1.45) | .17 | NA | NA |
| Preoperative therapies | ||||
| Any chemotherapy | 1.09 (0.67-1.78) | .72 | NA | NA |
| Any radiation therapy | 4.79 (0.64-35.63) | .13 | NA | NA |
| Chemotherapy type | ||||
| None | 1 [Reference] | NA | NA | NA |
| Gemcitabine | 0.86 (0.25-3.03) | .82 | NA | NA |
| Gemcitabine + other | 1.14 (0.67-1.93) | .63 | NA | NA |
| FOLFIRINOX | 1.15 (0.50-2.65) | .74 | NA | NA |
| Other | 1.15 (0.13-9.87) | .90 | NA | NA |
| Gemcitabine + nab-paclitaxel | NA | NA | NA | NA |
| Radiation dose | ||||
| None | 1 [Reference] | NA | NA | NA |
| Hypofractionated | 4.43 (0.59-33.5) | .15 | NA | NA |
| Standard fractionated | 5.11 (0.68-38.56) | .11 | NA | NA |
| Radiation sensitizer | ||||
| 5-FU/capecitabine | 1 [Reference] | NA | NA | NA |
| Gemcitabine | 1.67 (1.02-2.74) | .04 | 1.69 (1.02-2.82) | .04 |
| Other | NA | NA | NA | NA |
| Median treatment time interval, mo | 1.02 (0.93-1.12) | .69 | NA | NA |
| Surgery | ||||
| Type of surgery | ||||
| Pancreatoduodenectomy | 1 [Reference] | NA | NA | NA |
| Distal pancreatectomy | 0.81 (0.35-1.84) | .61 | NA | NA |
| Total pancreatectomy | NA | NA | NA | NA |
| Surgery, y | ||||
| 1990-1999 | 1 [Reference] | NA | NA | NA |
| 2000-2004 | 1.08 (0.43-2.73) | .87 | NA | NA |
| 2005-2009 | 0.93 (0.37-2.32) | .87 | NA | NA |
| 2010-2015 | 0.91 (0.39-2.31) | .91 | NA | NA |
Abbreviations: CA, cancer antigen; FOLFIRINOX, 5-FU, leucovorin, oxaliplatin, irinotecan; 5-FU, 5-fluorouracil; NA, not applicable.
Figure 1. Association With Number of Positive Predictive Factors and Odds of Developing a Major Pathologic Response Following Preoperative Therapy for Pancreatic Ductal Adenocarcinoma .
Error bars represent standard error.
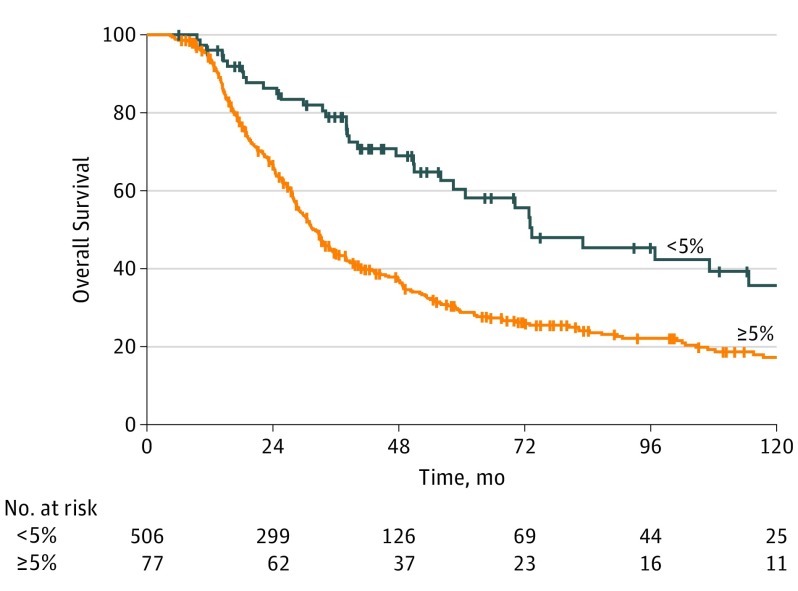
The median overall survival duration and 5-year overall survival rate of patients who had a major pathologic response were both significantly better (73.4 months and 58.2%, respectively) than those of patients who did not have a major response (32.2 months and 28.8%, respectively) (P < .001; Figure 2). In contrast, there was no significant difference in locoregional recurrence between the groups (11.7% vs 19.6%, P = .08).
Figure 2. Influence of Major Pathologic Response on Overall Survival in Patients With Pancreatic Ductal Adenocarcinoma Who Underwent Preoperative Therapy.
Table 3 reports the clinical profile of the 23 patients who had a pCR (0% viable cancer cells). None of these patients developed locoregional recurrence, but 4 of them (17.4%) developed distant recurrence: 2 in the lungs and 2 in the liver. In contrast, 9 of the 54 patients (16.7%) who had a major pathologic response but still had up to 5% residual cancer cells experienced locoregional recurrence as a component of first failure.
Table 3. Characteristics of 23 Patients With a Pathologic Complete Response.
| Demographic/Clinical | No. (%) |
|---|---|
| Age, mean (SD), y | 61.0 (10.2) |
| Male sex | 11 (47.8) |
| Median CA 19-9 level, U/mL | 39.5 |
| Radiographic stage | |
| Potentially resectable | 14 (60.9) |
| Borderline resectable | 8 (34.8) |
| Locally advanced | 1 (4.3) |
| Preoperative therapies | |
| Any chemotherapy | 13 (56.5) |
| Any radiation therapy | 23 (100.0) |
| Chemotherapy type | |
| None | 10 (43.5) |
| Gemcitabine | 1 (4.3) |
| Gemcitabine + other | 8 (34.8) |
| FOLFIRINOX | 4 (17.4) |
| Radiation dose | |
| Hypofractionated | 9 (39.1) |
| Standard fractionated | 14 (60.9) |
| Radiation sensitizer | |
| Gemcitabine | 11 (47.8) |
| Capecitabine/5-FU | 12 (52.2) |
| Mean treatment interval, mo | 6.3 (3.2) |
| Surgery | |
| Type of surgery | |
| Pancreatoduodenectomy | 20 (87.0) |
| Distal pancreatectomy | 3 (13.0) |
| Pathology | |
| R1 margin | 0 |
| Positive LN status | 1 (4.3) |
| Lymphovascular invasion | 0 |
| Perineural invasion | 0 |
| Postoperative therapy | |
| Chemotherapy | 2 (8.7) |
| Chemoradiation | 0 |
| Outcomes | |
| Follow-up, mo, (SD) | 57.0 (34.3) |
| Locoregional recurrence | 0 |
| Distant recurrence | 4 (17.4) |
| Median overall survival, mo | 83.1 |
Abbreviations: CA, cancer antigen; EBL, estimated blood loss; FOLFIRINOX, 5-FU, leucovorin, oxaliplatin, irinotecan; LN, lymph node; LNR, lymph node ratio; pCR, pathologic complete response; 5-FU, 5-fluorouracil.
Discussion
We have previously shown that patients with PDAC who receive preoperative chemotherapy and/or CRT and have less than 5% residual viable cancer cells have a favorable prognosis relative to patients who have at least 5% cells in their pancreatectomy specimens. In this study, we specifically sought to identify predictors of this response to therapy. Using a large data set of patients who received preoperative therapy during a 25-year period, we calculated a major pathologic response rate of only 13.2% and a pCR rate of only 3.9%. The median overall survival duration of patients who had a major response was 73.4 months. Importantly, we identified a patient-related factor (age), tumor-related factor (CA 19-9 level), and treatment-related factor (radiosensitizer) that were each independently associated with development of a major pathologic response.
The results of this study highlight the relative rarity of a pCR among patients with PDAC treated with existing preoperative therapy regimens. Indeed, the pCR rate of 3.9% reported here, remarkably similar to the 3.6% published in a 2010 meta-analysis of patients with PDAC, is striking when compared with rates in other cancers. For example, preoperative chemotherapy for breast cancer results in pCR rates ranging from 15% to 60% depending on the cancer subtype and the type of chemotherapy administered. Pathologic complete response is observed following preoperative CRT for rectal cancer in 15% to 27% of patients, and several clinical features and biomarkers are known to be predictive. Preoperative CRT for esophageal cancer led to an overall pCR rate of 29% in the CROSS trial, and the rate was higher in squamous cell carcinoma than in adenocarcinoma. Why pCR is substantially rarer in patients with PDAC is unknown, but at a minimum, this discrepancy points to the need for more effective therapeutics against this disease.
Whether a patient’s response to therapy is related to the underlying biology of the tumor, the cytotoxic efficacy of the treatment used against it, or an immunomodulating ability of its host remains unknown. Our findings suggest that response may be determined by all 3 of these factors. The association between clinical response and young age hints at the possibility of a genetic influence because both somatic and germline mutation status have been associated with pCR in other cancers. For example, breast cancers in patients with germline BRCA mutations demonstrate greater chemosensitivity and are associated with higher rates of pCR following neoadjuvant therapy, especially when platinum-based therapies are used. In PDAC, BRCA carriers have been found to be more sensitive to chemotherapies that lead to DNA damage, which is inefficiently repaired by cells lacking functional BRCA1 or BRCA2. Further research into the genetic and molecular influences on clinical and pathologic response to chemotherapy in PDAC is clearly needed.
Equally notable here was the limited number of treatment-related factors that were associated with clinical response. No chemotherapy regimen was found to be more effective than others in this regard nor was a longer treatment interval. Although the data set we used is likely limited in its power to analyze the association between CRT and response because almost all patients received CRT, the trend toward a higher rate of response in patients treated with radiation suggests its possible importance. Indeed, in this study, only 1 major pathologic response was observed in patients who received preoperative chemotherapy alone. Furthermore, only a handful of case reports describing pCR in response to chemotherapy exist in the literature, and other studies have also reported higher response rates after CRT than after chemotherapy. The possible importance of the dose-related ablative effects of radiation on the primary tumor is also suggested by the relatively high rates of response (9%-16%) reported with stereotactic body radiation, which enables higher doses of radiation to be delivered. Finally, our results also suggest that the chemotherapeutic agent used to sensitize the tumor to radiation may also be important. We had previously found that the radiosensitizer gemcitabine was associated with improved survival; this study suggests that an enhanced pathologic response may be the mechanism through which the improved outcome occurs.
That 5-fluorouracil, leucovorin, oxaliplatin, irinotecan (FOLFIRINOX) was not associated with a higher incidence of a major pathologic response might be surprising given its apparent association with improved resectability rates and longer survival durations. However, a 2016 systematic review of studies evaluating FOLFIRINOX for locally advanced PDAC reported a pooled pCR rate of only 7.1% in patients who underwent pancreatectomy, a rate identical to that reported here (4 of 56 patients who received FOLFIRINOX). Furthermore, it is worth noting that prior single-institution reports of patients who underwent pancreatectomy for locally advanced PDAC were likely enriched with patients who experienced a favorable response to preoperative therapy; in contrast, most patients herein were technically resectable at baseline and did not require a major response to become resectable.
It may also be surprising that only 34.5% of patients (n = 201 of 583) in this series received chemotherapy or chemoradiation following pancreatectomy. However, it must be recognized that the role of postoperative therapy for patients who have already received preoperative therapy remains poorly defined. We have historically administered postoperative therapy selectively in this setting, but in a 2015 review of our data, we found that the administration of systemic chemotherapy following preoperative therapy and pancreatectomy was associated with improved survival relative to observation. Whether this apparent benefit applies to patients who have had a major pathologic response or a pCR to preoperative therapy is unclear.
One question that remains is whether response of the primary tumor serves as an effective surrogate for response of the micrometastatic disease presumed present in almost all patients with PDAC. Our findings would suggest not entirely: although clinical response measured in the primary tumor was associated with improved survival, it did not guarantee cure. For example, one patient who had a pCR in the primary tumor specimen had viable cancer in a regional lymph node, and many patients who had a major pathologic response, including 17% of patients who had a pCR, developed distant recurrence following pancreatectomy. This phenomenon may be partially explained by differences in treatment effect induced by radiation (which primarily works locally) as opposed to treatment effect induced by chemotherapy (which has a systemic effect). Regardless, given the association between major pathologic response and long-term outcomes, such response may serve as a clinically relevant early end point in clinical trials.
Limitations
The main limitation of our study is its retrospective and single-institution design. Specifically, the results of this study may be influenced by our bias toward the preoperative administration of chemoradiation, although the role of radiation in the treatment of localized PDAC remains controversial. On the other hand, the strengths of the study are its relatively large sample size, the evaluation of a wide range of treatment regimens that allow for comparisons, use of a prospectively maintained database, and the availability of granular data to evaluate treatment-level factors and their association with a novel end point.
Conclusions
In summary, although pCR is a relatively rare outcome following preoperative therapy for PDAC, it is associated with a significantly improved prognosis. However, of the patient- and treatment-related factors we analyzed, only young age (patient), low baseline CA 19-9 level (biology), and gemcitabine as a radiosensitizer (treatment) were associated with a major pathologic response. Future studies should investigate the mechanisms by which pCR develops and focus on the identification of new therapeutic agents with greater cytotoxic potential.
References
- 1.National Comprehensive Cancer Network NCCN practice guidelines for pancreatic cancer. http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed March 1, 2016.
- 2.Khorana AA, Mangu PB, Berlin J, et al. Potentially curable pancreatic cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34(21):2541-2556. [DOI] [PubMed] [Google Scholar]
- 3.Cloyd JM, Katz MHG, Prakash L, et al. Preoperative therapy and pancreatoduodenectomy for pancreatic ductal adenocarcinoma: a 25-year single-institution experience. J Gastrointest Surg. 2017;21(1):164-174. [DOI] [PubMed] [Google Scholar]
- 4.Chuong MD, Frakes JM, Figura N, et al. Histopathologic tumor response after induction chemotherapy and stereotactic body radiation therapy for borderline resectable pancreatic cancer. J Gastrointest Oncol. 2016;7(2):221-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chatterjee D, Katz MH, Rashid A, et al. Histologic grading of the extent of residual carcinoma following neoadjuvant chemoradiation in pancreatic ductal adenocarcinoma: a predictor for patient outcome. Cancer. 2012;118(12):3182-3190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz MHG, Shi Q, Ahmad SA, et al. Preoperative modified FOLFIRINOX treatment followed by capecitabine-based chemoradiation for borderline resectable pancreatic cancer: alliance for clinical trials in oncology trial A021101. JAMA Surg. 2016;151(8):e161137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao Q, Rashid A, Gong Y, et al. Pathologic complete response to neoadjuvant therapy in patients with pancreatic ductal adenocarcinoma is associated with a better prognosis. Ann Diagn Pathol. 2012;16(1):29-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuerer HM, Newman LA, Smith TL, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17(2):460-469. [DOI] [PubMed] [Google Scholar]
- 9.Maas M, Nelemans PJ, Valentini V, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010;11(9):835-844. [DOI] [PubMed] [Google Scholar]
- 10.Lorenzen S, Thuss-Patience P, Al-Batran SE, et al. Impact of pathologic complete response on disease-free survival in patients with esophagogastric adenocarcinoma receiving preoperative docetaxel-based chemotherapy. Ann Oncol. 2013;24(8):2068-2073. [DOI] [PubMed] [Google Scholar]
- 11.Tan MC, Al Mushawah F, Gao F, et al. Predictors of complete pathological response after neoadjuvant systemic therapy for breast cancer. Am J Surg. 2009;198(4):520-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Armstrong D, Raissouni S, Price Hiller J, et al. Predictors of pathologic complete response after neoadjuvant treatment for rectal cancer: a multicenter study. Clin Colorectal Cancer. 2015;14(4):291-295. [DOI] [PubMed] [Google Scholar]
- 13.Huang R-W, Chao Y-K, Wen Y-W, et al. Predictors of pathological complete response to neoadjuvant chemoradiotherapy for esophageal squamous cell carcinoma. World J Surg Oncol. 2014;12:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang RF, Wang H, Lara A, et al. Development of an integrated biospecimen bank and multidisciplinary clinical database for pancreatic cancer. Ann Surg Oncol. 2008;15(5):1356-1366. [DOI] [PubMed] [Google Scholar]
- 15.Katz MHG, Pisters PWT, Evans DB, et al. Borderline resectable pancreatic cancer: the importance of this emerging stage of disease. J Am Coll Surg. 2008;206(5):833-846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunt K. Operative Standards for Cancer Surgery. Vol 1 Philadelphia, PA: Wolters Kluwer; 2015. [Google Scholar]
- 17.Liu L, Katz MH, Lee SM, et al. Superior mesenteric artery margin of posttherapy pancreaticoduodenectomy and prognosis in patients with pancreatic ductal adenocarcinoma. Am J Surg Pathol. 2015;39(10):1395-1403. [DOI] [PubMed] [Google Scholar]
- 18.Lee SM, Katz MHG, Liu L, et al. Validation of a proposed tumor regression grading scheme for pancreatic ductal adenocarcinoma after neoadjuvant therapy as a prognostic indicator for survival. Am J Surg Pathol. 2016;40(12):1653-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tzeng C-WD, Abbott DE, Cantor SB, et al. Frequency and intensity of postoperative surveillance after curative treatment of pancreatic cancer: a cost-effectiveness analysis. Ann Surg Oncol. 2013;20(7):2197-2203. [DOI] [PubMed] [Google Scholar]
- 20.Gillen S, Schuster T, Meyer Zum Büschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;7(4):e1000267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McFarland DC, Naikan J, Rozenblit M, Mandeli J, Bleiweiss I, Tiersten A. Changes in pathological complete response rates after neoadjuvant chemotherapy for breast carcinoma over five years. J Oncol. 2016;2016:4324863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bria E, Carbognin L, Furlanetto J, et al. Impact of neoadjuvant single or dual HER2 inhibition and chemotherapy backbone upon pathological complete response in operable and locally advanced breast cancer: Sensitivity analysis of randomized trials. Cancer Treat Rev. 2014;40(7):847-856. [DOI] [PubMed] [Google Scholar]
- 23.Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384(9938):164-172. [DOI] [PubMed] [Google Scholar]
- 24.Spolverato G, Pucciarelli S, Bertorelle R, De Rossi A, Nitti D. Predictive factors of the response of rectal cancer to neoadjuvant radiochemotherapy. Cancers (Basel). 2011;3(2):2176-2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Hagen P, Hulshof MCCM, van Lanschot JJB, et al. ; CROSS Group . Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074-2084. [DOI] [PubMed] [Google Scholar]
- 26.Jiang T, Shi W, Wali VB, et al. Predictors of chemosensitivity in triple negative breast cancer: an integrated genomic analysis. PLoS Med. 2016;13(12):e1002193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Isakoff SJ, Mayer EL, He L, et al. TBCRC009: a multicenter phase ii clinical trial of platinum monotherapy with biomarker assessment in metastatic triple-negative breast cancer. J Clin Oncol. 2015;33(17):1902-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arun B, Bayraktar S, Liu DD, et al. Response to neoadjuvant systemic therapy for breast cancer in BRCA mutation carriers and noncarriers: a single-institution experience. J Clin Oncol. 2011;29(28):3739-3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Byrski T, Gronwald J, Huzarski T, et al. Pathologic complete response rates in young women with BRCA1-positive breast cancers after neoadjuvant chemotherapy. J Clin Oncol. 2010;28(3):375-379. [DOI] [PubMed] [Google Scholar]
- 30.Lowery MA, Kelsen DP, Stadler ZK, et al. An emerging entity: pancreatic adenocarcinoma associated with a known BRCA mutation: clinical descriptors, treatment implications, and future directions. Oncologist. 2011;16(10):1397-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Golan T, Kanji ZS, Epelbaum R, et al. Overall survival and clinical characteristics of pancreatic cancer in BRCA mutation carriers. Br J Cancer. 2014;111(6):1132-1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gostimir M, Bennett S, Moyana T, Sekhon H, Martel G. Complete pathological response following neoadjuvant FOLFIRINOX in borderline resectable pancreatic cancer: a case report and review. BMC Cancer. 2016;16(1):786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boone BA, Steve J, Krasinskas AM, et al. Outcomes with FOLFIRINOX for borderline resectable and locally unresectable pancreatic cancer. J Surg Oncol. 2013;108(4):236-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartlapp I, Müller J, Kenn W, et al. Complete pathological remission of locally advanced, unresectable pancreatic cancer (LAPC) after intensified neoadjuvant chemotherapy. Onkologie. 2013;36(3):123-125. [DOI] [PubMed] [Google Scholar]
- 35.Valeri S, Borzomati D, Nappo G, Perrone G, Santini D, Coppola R. Complete pathological response after FOLFIRINOX for locally advanced pancreatic cancer: the beginning of a new era? case report and review of the literature. Pancreatology. 2014;14(5):425-430. [DOI] [PubMed] [Google Scholar]
- 36.Cloyd JM, Crane CH, Koay EJ, et al. Impact of hypofractionated and standard fractionated chemoradiation before pancreatoduodenectomy for pancreatic ductal adenocarcinoma. Cancer. 2016;122(17):2671-2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim SS, Nakakura EK, Wang ZJ, et al. Preoperative FOLFIRINOX for borderline resectable pancreatic cancer: is radiation necessary in the modern era of chemotherapy? J Surg Oncol. 2016;114(5):587-596. [DOI] [PubMed] [Google Scholar]
- 38.Moningi S, Dholakia AS, Raman SP, et al. The role of stereotactic body radiation therapy for pancreatic cancer: a single-institution experience. Ann Surg Oncol. 2015;22(7):2352-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferrone CR, Marchegiani G, Hong TS, et al. Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg. 2015;261(1):12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Conroy T, Desseigne F, Ychou M, et al. ; Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup . FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825. [DOI] [PubMed] [Google Scholar]
- 41.Rombouts SJ, Walma MS, Vogel JA, et al. Systematic review of resection rates and clinical outcomes after FOLFIRINOX-based treatment in patients with locally advanced pancreatic cancer. Ann Surg Oncol. 2016;23(13):4352-4360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roland CL, Katz MHG, Tzeng C-WD, et al. The addition of postoperative chemotherapy is associated with improved survival in patients with pancreatic cancer treated with preoperative therapy. Ann Surg Oncol. 2015;22(September)(suppl 3):S1221-S1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klinkenbijl JH, Jeekel J, Sahmoud T, et al. Adjuvant radiotherapy and 5-fluorouracil after curative resection of cancer of the pancreas and periampullary region: phase III trial of the EORTC gastrointestinal tract cancer cooperative group. Ann Surg. 1999;230(6):776-782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neoptolemos JP, Stocken DD, Friess H, et al. ; European Study Group for Pancreatic Cancer . A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350(12):1200-1210. [DOI] [PubMed] [Google Scholar]
- 45.Kalser MH, Ellenberg SS. Pancreatic cancer: adjuvant combined radiation and chemotherapy following curative resection. Arch Surg. 1985;120(8):899-903. [DOI] [PubMed] [Google Scholar]