Key Points
Question
What are lifetime risks of cardiovascular disease (CVD) according to educational attainment?
Findings
This population-based observational study found that in men, lifetime CVD risks from 45 through 85 years ranged from 59.0% for grade school to 42.2% for graduate/professional school education; in women, from 50.8% to 28.0%, respectively. Educational attainment was inversely associated with lifetime CVD risks, regardless of other important socioeconomic characteristics.
Meaning
Our findings emphasize the need for further efforts to reduce CVD inequalities related to educational disparities.
This population-based observational study estimates lifetime risks of cardiovascular disease according to categories of educational attainment.
Abstract
Importance
Estimates of lifetime risk may help raise awareness of the extent to which educational inequalities are associated with risk of cardiovascular disease (CVD).
Objective
To estimate lifetime risks of CVD according to categories of educational attainment.
Design, Setting, and Participants
Participants were followed from 1987 through December 31, 2013. All CVD events (coronary heart disease, heart failure, and stroke) were confirmed by physician review and International Classification of Diseases codes. A total of 13 948 whites and African Americans who were 45 to 64 years old and free of CVD at baseline were included from 4 US communities (Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and suburbs of Minneapolis, Minnesota). The data analysis was performed from June 7 to August 31, 2016.
Exposures
Educational attainment.
Main Outcomes and Measures
We used a life table approach to estimate lifetime risks of CVD from age 45 through 85 years according to educational attainment. We adjusted for competing risks of death from underlying causes other than CVD.
Results
The sample of 13 948 participants was 56% female and 27% African American. During 269 210 person-years of follow-up, we documented 4512 CVD events and 2401 non-CVD deaths. Educational attainment displayed an inverse dose-response relation with cumulative risk of CVD, which became evident in middle age, with the most striking gap between those not completing vs completing high school. In men, lifetime risks of CVD were 59.0% (95% CI, 54.0%-64.1%) for grade school, 52.5% (95% CI, 47.7%-56.8%) for high school education without graduation, 50.9% (95% CI, 47.3%-53.9%) for high school graduation, 47.2% (95% CI, 41.5%-52.5%) for vocational school, 46.4% (95% CI, 42.8%-49.6%) for college with or without graduation, and 42.2% (95% CI, 36.6%-47.0%) for graduate/professional school; in women, 50.8% (95% CI, 45.7%-55.8%), 49.3% (95% CI, 45.1%-53.1%), 36.3% (95% CI, 33.4%-39.1%), 32.2% (95% CI, 26.0%-37.3%), 32.8% (95% CI, 29.1%-35.9%), and 28.0% (95% CI, 21.9%-33.3%), respectively. Educational attainment was inversely associated with CVD even within categories of family income, income change, occupation, or parental educational level.
Conclusions and Relevance
More than 1 in 2 individuals with less than high school education had a lifetime CVD event. Educational attainment was inversely associated with the lifetime risk of CVD, regardless of other important socioeconomic characteristics. Our findings emphasize the need for further efforts to reduce CVD inequalities related to educational disparities.
Introduction
Inequalities in cardiovascular disease (CVD), which is the leading cause of death in the world, are due in part to inequalities in socioeconomic status such as education, occupation, and income, and present a major and persistent public health challenge across industrialized nations. Educational inequality is one of the most important socioeconomic factors contributing to CVD. Greater education tends to be associated with healthier behaviors, occupations with healthier working conditions, and better access to health care. Because education is typically completed by young adulthood, educational inequality may affect risk of CVD early in the life course and thus increase the probability of premature death. Therefore, interventions to correct educational inequalities at the community or individual level may not only reduce CVD rates but also improve life expectancy.
One way to convey the importance of educational attainment is to calculate the lifetime risk of CVD according to educational levels. Lifetime risk estimates, that is, absolute risks through various ages, can readily convey the burden of CVD in a population and potentially increase public awareness, as demonstrated for lifetime risk of breast cancer. Yet, to our knowledge, there has been no study so far estimating lifetime risks of CVD according to educational attainment.
We evaluated the association between educational attainment and CVD risk by estimating the lifetime risks of CVD (coronary heart disease, heart failure, and stroke) in a large biracial cohort study. In addition, we also assessed how other important socioeconomic factors (income, occupation, and parental education) were related to the association between educational attainment and lifetime CVD risk.
Methods
Study Design, Setting, and Population
The Atherosclerosis Risk in Communities (ARIC) study is an ongoing population-based prospective study of CVD. In 1987 through 1989, the ARIC study recruited and examined 15 792 mostly white or African American men and women aged 45 to 64 years from 4 US communities. The participants were reexamined in 1996 through 1998 (visit 4, 80% return). See eMethods in the Supplement for additional details. The institutional review boards of the collaborating institutions (University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Wake Forest Baptist Medical Center, Winston-Salem, North Carolina; University of Mississippi Medical Center, Jackson, Mississippi; University of Minnesota, Minneapolis, Minnesota; and Johns Hopkins University, Baltimore, Maryland) approved the study protocol, and each participant provided written informed consent.
Risk Factor Measurements
The main exposure of interest was self-reported educational attainment, ascertained at ARIC baseline, and categorized into 6 levels: (1) grade school, (2) high school without graduation, (3) high school with graduation, (4) vocational school, (5) college with or without graduation, and (6) graduate or professional school.
We assessed other potential CVD risk factors as follows: socioeconomic status; family income (<$5000, $5000-$7999, $8000-$11 999, $12 000-$15 999, $16 000-$23 999, $24 000-$34 999, $35 000-$49 999, or >$50 000); occupation for the longest period (“precision jobs” [mechanic, repairman, construction worker, or craftsman], “service jobs” [hairdresser, domestic, restaurant, or security], “machine-operating jobs” [driver, machine operator, sanitation, or laborer], “technical and sales jobs” [technician, sales, or clerical], “professional and managerial jobs,” and “homemaker”); and parental educational attainment (using the aforementioned levels). See eMethods in the Supplement for additional details.
Confirmation of CVD
We defined incident CVD events as coronary heart disease, heart failure, and stroke. ARIC staff contacted participants annually by telephone to capture all hospitalizations and deaths related to possible CVD. See eMethods in the Supplement for additional details.
Statistical Analysis
SAS version 9.3 software (SAS Institute Inc) was used for statistical analyses. All statistical tests were 2 sided and P < .05 was regarded as significant.
We excluded participants who self-reported prebaseline CVD (coronary heart disease, heart failure, or stroke) or had electrocardiographic evidence of prebaseline coronary heart disease (n = 1553) and participants whose data on educational attainment or outcome status were missing (n = 291). After exclusions, 13 948 participants were available for these analyses.
Participants were observed from age at baseline to age at CVD event, age at last follow-up contact, or December 31, 2013, whichever came first. We included the first-ever coronary heart disease, heart failure, or stroke event as the incident CVD event. We estimated remaining lifetime risks of CVD using a modified version of survival analysis. See eMethods in the Supplement for additional details. Results unadjusted and adjusted for competing risks in relation to educational attainment and lifetime risk of CVD are given in the eTable in the Supplement. We also estimated the lifetime risk of CVD according to family income, occupation, and parental educational attainment and evaluated the associations of these variables and individual educational attainment jointly with the lifetime CVD risk. After identical exclusions as described herein, 13 128 participants (94%) had baseline income data. Similarly, 9381, 9609, and 8963 participants who were free of CVD at that time completed the visit 4 questionnaire on income, occupation, and parental education, respectively, among whom we estimated lifetime risk of CVD from age 55 to 85 years.
In sensitivity analyses, we also evaluated the association between educational attainment and lifetime risk of CVD by stratifying on CVD risk factors (family income [<$35 000 vs ≥$35 000], occupation [occupations with the 3 highest vs 3 lowest lifetime risks of CVD], parental educational attainment [non–high school graduates vs high school graduates], marital status, smoking status [current vs former vs never], drinking status [current vs former vs never], physical inactivity, diet [healthy diet score ≤1 vs healthy diet score ≥2], obesity, hypertension, diabetes, hypercholesterolemia, subclinical atherosclerosis, left ventricular hypertrophy, and chronic kidney disease). Next, we estimated lifetime risks of CVD according to family income at visit 4 instead of visit 1. Finally, we also evaluated the association between educational attainment and lifetime risks of CVD by stratifying birth years (individuals born before 1935 [55-64 years at baseline] vs after 1935 [45-54 years]) to assess birth cohort effects.
Results
Educational Attainment and Risk Factors for CVD
As presented in Table 1, individuals with a higher educational attainment were likely to have higher socioeconomic status and were less likely to have unhealthy lifestyle factors, health impairments, and subclinical organ damage. Those with higher educational attainment were more likely to be current drinkers, but current drinkers with lower educational attainment consumed more alcohol.
Table 1. Baseline Characteristics of Participants According to Educational Attainment, Atherosclerosis Risk in Communities, 1987 Through 1989.
| Parametera | Educational Attainment (N = 13 948) |
P Value for Trend | |||||
|---|---|---|---|---|---|---|---|
| Grade School | High School Without Graduation | High School With Graduation | Vocational School | College With or Without Graduation | Graduate/ Professional School |
||
| Participants, No. (%) | 1237 (8.9) | 1889 (13.5) | 4545 (32.6) | 1179 (8.5) | 3644 (26.1) | 1454 (10.4) | |
| Socioeconomic status, % | |||||||
| Female | 48.1 | 61.0 | 63.8 | 51.8 | 53.3 | 44.1 | <.001 |
| African American | 56.7 | 41.2 | 17.7 | 21.1 | 18.2 | 34.7 | <.001 |
| Married | 69.2 | 72.3 | 83.8 | 81.9 | 84.4 | 84.1 | <.001 |
| Family income ≤$35 000 | 92.4 | 82.7 | 57.9 | 53.5 | 34.3 | 26.9 | <.001 |
| Blue collar workersb | 26.9 | 19.0 | 13.3 | 19.1 | 4.9 | 1.5 | <.001 |
| Parental education less than high school graduationc | 92.2 | 83.0 | 64.2 | 60.5 | 41.8 | 37.7 | <.001 |
| Health insurance | 70.5 | 81.1 | 92.9 | 93.5 | 95.0 | 97.0 | <.001 |
| Lifestyle factors | |||||||
| Current smoker, % | 33.3 | 34.2 | 26.8 | 25.1 | 21.9 | 15.1 | <.001 |
| Current drinker, % | 33.0 | 38.7 | 57.1 | 62.5 | 69.1 | 65.3 | <.001 |
| Alcohol consumption, mean (SD), g/wkd | 106.0 (181.2) | 91.9 (138.1) | 71.8 (121.4) | 73.1 (109.2) | 72.5 (104.2) | 71.3 (100.3) | <.001 |
| Physical activity, mean (SD), MET-h/week | 5.2 (8.9) | 6.5 (10.0) | 9.5 (12.2) | 10.3 (12.2) | 12.9 (14.0) | 14.6 (15.4) | <.001 |
| Healthy diet score, mean (SD) | 1.7 (0.9) | 1.8 (1.0) | 1.9 (0.9) | 1.9 (1.0) | 2.0 (0.9) | 2.1 (1.0) | <.001 |
| Health conditions | |||||||
| Obesity, % | 34.9 | 34.3 | 25.9 | 25.5 | 22.3 | 20.8 | <.001 |
| BMI, mean (SD) | 28.8 (6.0) | 28.6 (5.8) | 27.4 (5.3) | 27.3 (5.0) | 27.0 (4.8) | 26.9 (4.6) | <.001 |
| Hypertension, % | 50.3 | 40.0 | 30.5 | 27.1 | 26.0 | 26.1 | <.001 |
| Systolic blood pressure, mean (SD), mmHg | 147.9 (20.5) | 144.6 (19.4) | 141.0 (18.0) | 140.2 (17.2) | 138.7 (16.7) | 138.6 (16.8) | <.001 |
| Diabetes, % | 19.0 | 14.9 | 9.8 | 8.2 | 7.7 | 7.6 | <.001 |
| Fasting blood glucose level, mean (SD), mg/dL | 112.1 (41.9) | 110.2 (40.6) | 105.9 (33.7) | 103.8 (26.1) | 103.1 (27.3) | 102.2 (25.8) | <.001 |
| Hypercholesterolemia, % | 28.9 | 27.4 | 26.6 | 25.1 | 23.8 | 20.8 | <.001 |
| Total cholesterol level, mean (SD), mg/dL | 217.4 (44.0) | 217.0 (42.9) | 217.1 (41.4) | 212.2 (41.8) | 211.4 (41.4) | 208.8 (38.2) | <.001 |
| Subclinical organ damage, % | |||||||
| Carotid intima media thickness >0.9 mm or plaque | 49.1 | 41.3 | 33.3 | 36.2 | 32.1 | 31.6 | <.001 |
| Left ventricular hypertrophy | 5.0 | 2.5 | 1.7 | 1.6 | 1.2 | 2.0 | <.001 |
| Chronic kidney disease | 2.0 | 1.5 | 1.0 | 0.9 | 0.8 | 0.6 | .002 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MET, metabolic equivalent of task.
SI conversion factors: To convert blood glucose to millimoles per liter, multiply by 0.0555; to convert total cholesterol to millimoles per liter, multiply by 0.0259.
Each factor except parental educational attainment was available from at least 13 003 participants (93%). These factors were not used for lifetime risk calculation but presented just to show participants’ characteristics.
Data from 9741 participants at visit 4.
Data from 9607 participants at visit 4.
Mean alcohol intake only among current drinkers.
Educational Attainment and Lifetime Risk of CVD
During 1987 through 2013, 13 948 participants (6108 men and 7840 women) provided 269 210 person-years of observation. During the follow-up, we documented 4512 incident CVD (coronary heart disease, heart failure, or stroke) events and 2401 non-CVD deaths. The overall lifetime risks to age 85 years of CVD were 48.6% (95% CI, 46.5%-50.4%) for white men, 34.3% (95% CI, 32.3%-36.2%) for white women, 51.8% (95% CI, 47.8%-55.1%) for African American men, and 44.8% (95% CI, 41.6%-47.6%) for African American women.
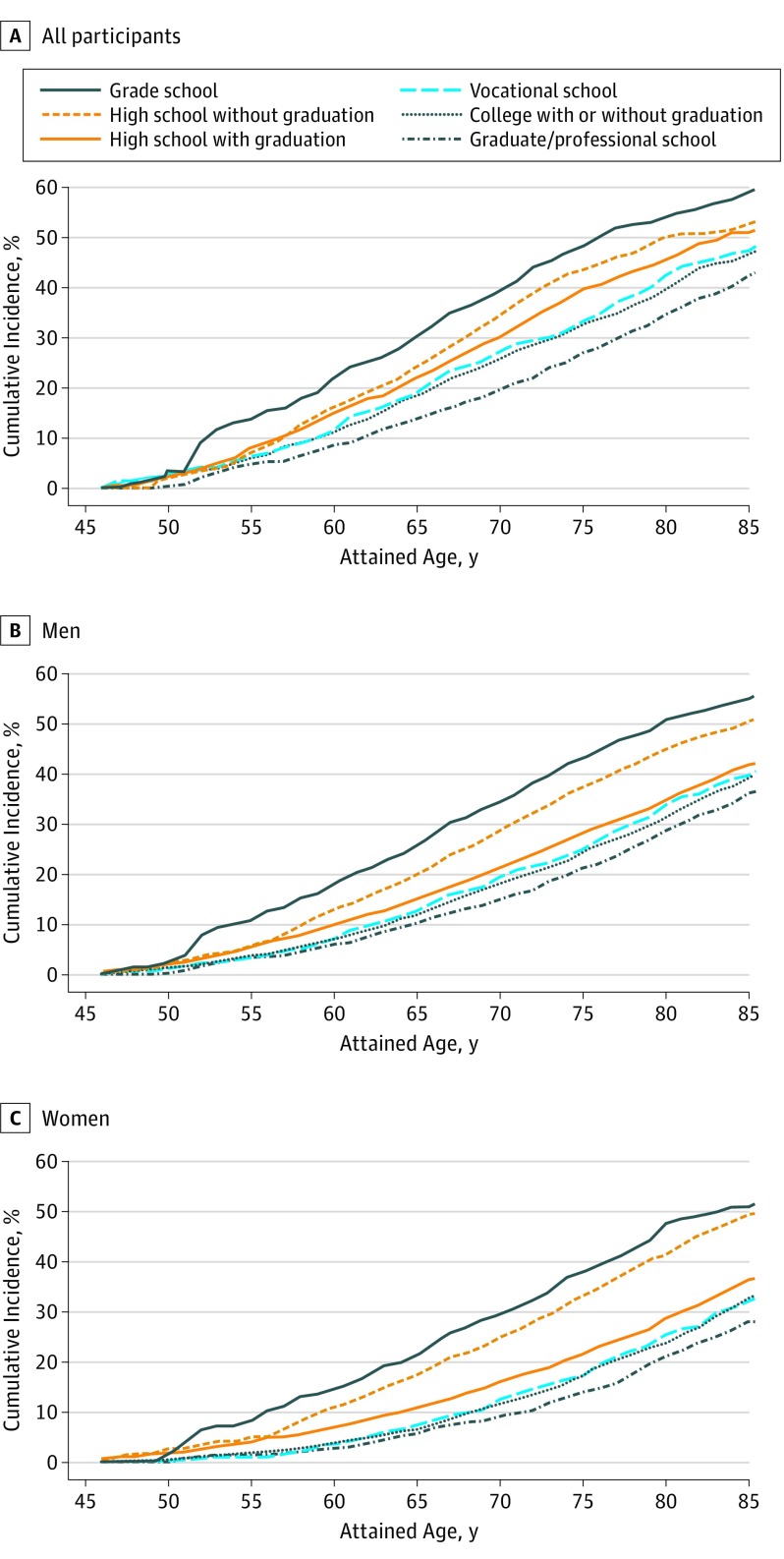
The lifetime risks of CVD after age 45 years according to educational attainment are given in Table 2 and illustrated in Figure 1. Educational attainment displayed inverse dose-response relations with lifetime risks of CVD in both men and women. Lifetime risk estimates though 85 years were 55.0% (95% CI, 51.4%-58.6%) in all participants, 59.0% (95% CI, 54.0%-64.1%) in men, and 50.8% (95% CI, 45.7%-55.8%) in women for the lowest attainment (grade school) and 36.1% (95% CI, 31.9%-39.7%) in all participants, 42.2% (95% CI, 36.6%-47.0%) in men, and 28.0% (95% CI, 21.9%-33.3%) in women for the highest attainment (graduate/professional school). Through age 65 years, the cumulative CVD risk estimates were 25.6% (95% CI, 21.2%-30.0%) in all participants, 30.2% (95% CI, 23.5%-36.9%) in men, and 21.2% (95% CI, 15.6%-26.9%) in women for the lowest educational attainment vs 10.1% (95% CI, 8.3%-12.0%) in all participants, 13.8% (95% CI, 10.9%-16.6%) in men, and 5.6% (95% CI, 3.5%-7.7%) in women for the highest educational attainment. Race-specific educational attainment showed similar inverse dose-response relations with lifetime CVD risks (eFigure 1 in the Supplement). A wide gap in the lifetime risks of CVD was observed between those without high school graduation vs with high school graduation, particularly in women. In all participants, the lifetime risks of CVD from 45 through 85 years were 51.9% (95% CI, 49.5%-54.1%) for non–high school graduates and 39.9% (95% CI, 38.4%-41.2%) for high school graduates; in men, 54.9% (95% CI, 51.5%-58.1%) and 47.4% (95% CI, 45.2%-49.3%); and in women, 49.4% (95% CI, 46.2%-52.3%) and 33.8% (95% CI, 31.9%-35.6%), respectively (eFigure 2 in the Supplement).
Table 2. Risk of Cardiovascular Disease (CVD) to Various Ages According to Educational Attainment at 45 Years.
| Age, y | CVD Risk, % (95% CI) | |||||
|---|---|---|---|---|---|---|
| Grade School | High School Without Graduation | High School With Graduation | Vocational School | College With or Without Graduation | Graduate/Professional School | |
| All | ||||||
| 55 | 10.7 (6.3-15.1) | 5.7 (3.5-7.9) | 5.4 (4.0-6.9) | 3.4 (1.5-5.3) | 3.6 (2.6-4.7) | 3.3 (2.0-4.6) |
| 65 | 25.6 (21.2-30.0) | 20.0 (17.4-22.6) | 15.0 (13.4-16.6) | 12.7 (10.1-15.2) | 11.8 (10.5-13.2) | 10.1 (8.3-12.0) |
| 75 | 43.1 (39.3-47.0) | 37.3 (34.6-39.9) | 28.2 (26.5-30.0) | 24.9 (22.0-27.8) | 24.4 (22.7-26.0) | 21.1 (18.7-23.4) |
| 85 (Lifetime risk) | 55.0 (51.4-58.6) | 50.5 (47.3-53.3) | 41.7 (39.5-43.8) | 39.7 (35.5-43.4) | 39.2 (36.6-41.4) | 36.1 (31.9-39.7) |
| Men | ||||||
| 55 | 13.6 (6.5-20.8) | 7.1 (3.6-10.6) | 8.0 (5.7-10.2) | 6.4 (2.4-10.3) | 6.0 (3.8-8.2) | 4.8 (2.7-6.9) |
| 65 | 30.2 (23.5-36.9) | 24.2 (19.9-28.4) | 22.0 (19.3-24.6) | 18.9 (14.3-23.5) | 18.4 (15.8-20.9) | 13.8 (10.9-16.6) |
| 75 | 48.1 (42.6-53.8) | 43.4 (39.2-47.5) | 39.6 (36.8-42.3) | 33.2 (28.3-37.9) | 32.5 (29.8-35.2) | 26.8 (23.3-30.2) |
| 85 (Lifetime risk) | 59.0 (54.0-64.1) | 52.5 (47.7-56.8) | 50.9 (47.3-53.9) | 47.2 (41.5-52.5) | 46.4 (42.8-49.6) | 42.2 (36.6-47.0) |
| Women | ||||||
| 55 | 8.2 (2.8-13.6) | 4.9 (2.1-7.8) | 3.9 (2.2-5.7) | 1.1 (0.0-2.3) | 1.9 (1.0-2.9) | 1.6 (0.2-2.9) |
| 65 | 21.2 (15.6-26.9) | 17.4 (14.1-20.6) | 10.8 (8.9-12.8) | 7.3 (4.9-9.7) | 6.5 (5.2-7.9) | 5.6 (3.5-7.7) |
| 75 | 37.9 (32.6-43.1) | 33.2 (29.8-36.6) | 21.5 (19.4-23.7) | 17.2 (13.8-20.4) | 17.4 (15.5-19.3) | 13.8 (10.8-16.8) |
| 85 (Lifetime risk) | 50.8 (45.7-55.8) | 49.3 (45.1-53.1) | 36.3 (33.4-39.1) | 32.2 (26.0-37.3) | 32.8 (29.1-35.9) | 28.0 (21.9-33.3) |
Figure 1. Risk Estimates of Cardiovascular Disease From Age 45 to 85 Years According to Educational Attainment, 1987 Through 2013.
Joint Associations
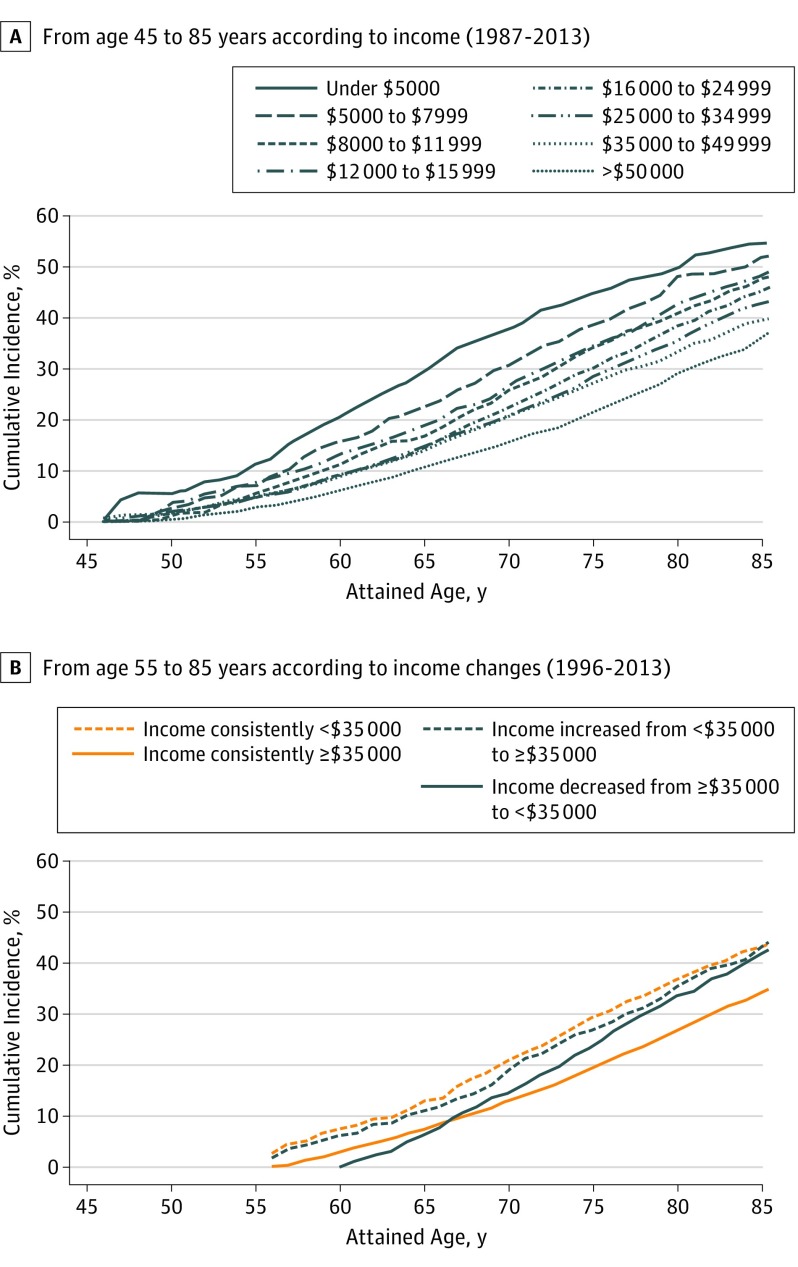
As shown in Figure 2A, family income also showed inverse dose-response relations with lifetime risk of CVD. For example, lifetime risks of CVD at age 45 to 85 years were 45.2% (95% CI, 42.1%-48.0%) for those with annual income of $16 000-23 999, 39.5% (95% CI, 36.5-42.3%) for $35 000-49 999, and 36.2% (95% CI, 33.3-38.7%) for more than $50 000. We also assessed the association of income changes from visit 1 to visit 4 with lifetime CVD risk from 55 to 85 years (Figure 2B). Lifetime risks of CVD were 45.6% (95% CI, 40.8%-51.6%) for individuals with income consistently less than $35 000, 45.9% (95% CI, 39.7%-52.4%) for those whose income increased from less than $35 000 to $35 000 or more, 44.1% (95% CI, 38.7%-49.2%) for those whose income decreased from $35 000 or more to less than $35 000, and 36.3% (95% CI, 34.5%-37.9%) for individuals whose income was consistently at least $35 000. However, those whose income decreased from at least $35 000 to less than $35 000 had the most rapid increase in lifetime CVD risk between 55 and 85 years (compare slopes in Figure 2B).
Figure 2. Risk Estimates of Cardiovascular Disease .
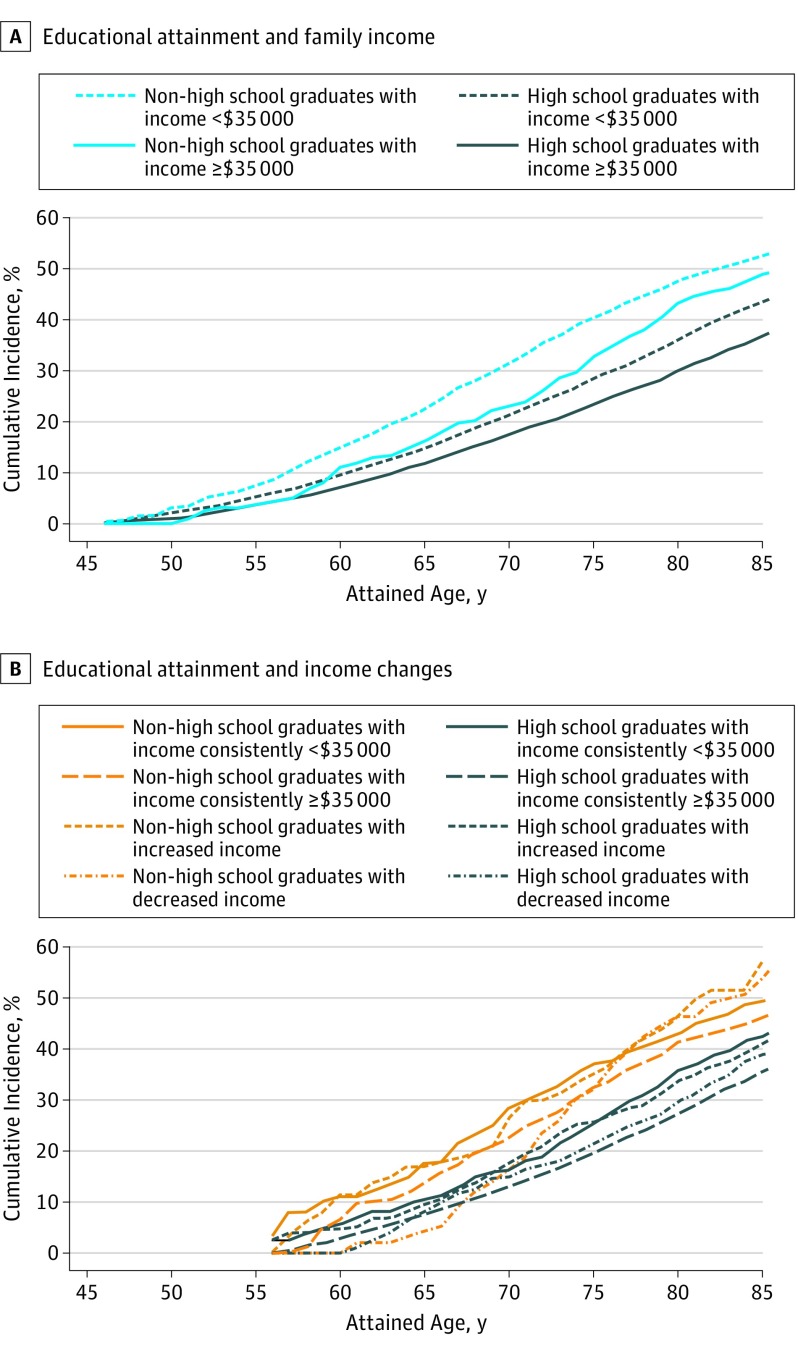
As shown in Figure 3, high school graduates had lower lifetime risks of CVD than non–high school graduates, regardless of their family income or income changes. Lifetime risks from 45 to 85 years were 52.4% (95% CI, 49.8%-54.9%) for non–high school graduates with family income less than $35 000, 48.7% (95% CI, 41.5%-54.8%) for non–high school graduates with income of at least $35 000, 43.3% (95% CI, 41.2%-45.2%) for high school graduates with income less than $35 000, and 36.7% (95% CI, 34.5%-38.6%) for high school graduates with income of at least $35 000. The cumulative risk of CVD for non–high school graduates whose income decreased from at least $35 000 to less than $35 000 increased more during their remaining life course, and their lifetime risk was 53.7% (95% CI, 45.1%-61.8%). In contrast, the cumulative risk for those with more than high school education whose income decreased from at least $35 000 to less than $35 000 had a less steep rise in lifetime CVD risk, and their lifetime risk was 38.8% (95% CI, 31.8%-45.1%).
Figure 3. Risk Estimates of Cardiovascular Disease to Age 85 Years Estimated Jointly by Educational Attainment (Non–High School vs High School Graduates) and Family Income or Income Changes.
A, Educational attainment and family income (<$35 000 vs ≥$35 000). B, Educational attainment and income changes (individuals consistently <$35 000 vs those whose income increased from <$35 000 to ≥$35 000 vs those whose income decreased from ≥$35 000 to <$35 000 vs those consistently ≥$35 000).
We also assessed the associations of occupation and parental educational attainment with lifetime risks of CVD (eFigure 3 in the Supplement). Lifetime risks of CVD were higher successively for “precision jobs,” “service jobs,” “machine-operating jobs,” “technical and sales jobs,” “professional and managerial jobs,” and “homemaker.” Parental educational attainment showed an inverse dose-response relation with lifetime risks of CVD. Participants who were at least high school graduates had lower lifetime risks of CVD than non–high school graduates, regardless of their occupation or their parental educational attainment (eFigure 4 in the Supplement).
Sensitivity Analysis
Analyses stratified by CVD risk factors all showed similar inverse dose-response relations between educational attainment and lifetime risk of CVD (data not shown). Income data at visit 4 showed an inverse dose-response relation with CVD lifetime risk from 55 to 85 years similar to that for visit 1 income (eFigure 5 in the Supplement). Finally, lifetime risks of CVD in individuals born before and after 1935 showed similar inverse-dose response relations with educational attainment, but differences of lifetime CVD risks between education levels appeared smaller in the older age category (eFigure 6 in the Supplement).
Discussion
Principal Findings
Educational attainment showed an inverse dose-response relation with lifetime risk of CVD. Men and women with the lowest education level had lifetime CVD risks of approximately 60% and 50%, respectively, while those with the highest education level had approximately 40% and 30% lifetime CVD risks (ie, 20% lower “attributable risk” in the highest educational attainment group). This gap in cumulative risk was already evident during middle age. Individuals with more than a high school education had a lower lifetime risk than those with less educational attainment, regardless of their income, income change, occupation, or parental educational attainment. Although socioeconomic disparities in CVD risk are well established, this is the first estimate of how these disparities translate into lifetime CVD risk in a US cohort.
Interpretation and Public Health Implications
Allowing for variability by CVD risk factor, the following 2 mechanisms have been proposed for an association between educational attainment and CVD risk. First, CVD risk factors plausibly mediate the association of low education with CVD and greater education contributes to cognitive skills, problem-solving ability, learned effectiveness, personal control, and economic resources. In fact, educational attainment in ARIC was correlated with other socioeconomic status variables and CVD risk factors. In this scenario, interventions to enhance high educational attainment might be effective. Second, some CVD risk factors may also operate as confounding factors, rather than as mediators, between low educational attainment and CVD. For example, disabilities, including learning disabilities, may make educational achievements difficult and at the same time increase lifestyle-related CVD risk. Under this scenario, we may have overestimated the association between educational attainment and lifetime CVD risk to some extent. It seems unlikely however that reverse causality (ie, subclinical CVD leading to lower educational attainment) played a big role in this or similar studies, as most educational attainment is finished before chronic diseases become prevalent, and we excluded participants with a clinical history of CVD.
The lifetime risk method cannot directly assess which intermediate risk factors explain the association of education with lifetime CVD risk. However, our Table 1 and multiple publications have shown that people with less formal education tend to have poorer CVD risk factor levels. In prior publications, the major risk factors explain much of the association between education and CVD.
A previous study estimated that the lifetime risks of CVD of individuals aged 45 years who had at least 2 major risk factors (smoking, hypertension, diabetes, and hypercholesterolemia) were approximately 60% for men and 50% for women, respectively, which correspond to lifetime CVD risks for ARIC men and women with the lowest education level. In contrast, lifetime CVD risks for ARIC men and women with the highest education level were similar to those for men with only hypertension or women without any major risk factor. Thus, strategies targeting individuals with lower educational attainment for CVD risk factor prevention, as well as early CVD risk factor management, might also be beneficial for correction of inequalities in CVD.
A noteworthy finding of the present study is that educational inequalities were associated with inequalities in CVD even at young middle age. In fact, educational inequalities have been shown to relate to the rate of atherosclerosis progression even in youth. This may also suggest the importance of education for correction of inequalities in CVD.
Income, occupation, and parental educational attainment are also important socioeconomic determinants of CVD and life expectancy. However, those who completed more than high school education had a lower lifetime risk of CVD, regardless of their income, occupation, or parental educational attainment compared with those who did not complete high school. These results may suggest that whereas inequalities in CVD may be in part due to variation in income, occupation, and parental education levels, an individual’s own educational attainment, and the associated health knowledge and behaviors that education promotes, may be a critical socioeconomic determinant of CVD risk.
Income increase during middle age appeared not to be associated with CVD cumulative risk. It could be that low income at younger ages might have exposed individuals to CVD risk factors to the extent that they developed atherosclerosis, and even if they earned more money later, they might not have been able to reverse their risk trajectory. In contrast, income decrease appeared to accelerate CVD cumulative risk. We speculate that an income decrease might have led to an unhealthier lifestyle and less access to better health resources. However, CVD cumulative risk for individuals in those with high educational attainment appeared to be less affected by income change. Those with higher educational attainment might have pursued a healthy lifestyle regardless of their personal economic changes. Thus, these findings seem to reinforce the importance of education in lifetime CVD risk.
Our result about the association between occupations and CVD risk is similar to a previous finding. Homemakers had the lowest lifetime risk of CVD, probably because homemakers in the present study included mainly women and in general women have a lower risk of CVD than men.
Limitations
Some limitations of our study need to be mentioned. Estimates of lifetime risks of CVD should be interpreted carefully because they may be to some degree confounded by other CVD risk factors, although as mentioned, most risk factors would be considered mediators rather than confounders. Even with such a proviso, our estimates of lifetime risk can help in elucidating the association between education and CVD risk. A second potential limitation is that estimates of lifetime risk are subject to birth cohort effects and therefore can change over time. For example, older participants would have been in grade school (or even have completed their education) during the Depression. The youngest would have been born by the end of the Second World War, and thus in many parts of the country they would have attended racially segregated schools. Although the relative importance of level of education may still be the same, where or how much the biggest benefits occur in terms of CVD risk may have changed over time, as shown in the present study. Finally, we had no information on the age at which participants completed their education. Although we may presume that most participants completed grade school and high school at similar ages, they might have completed any higher education at different ages. In addition, we surveyed educational attainment only at ARIC baseline. Thus, we cannot completely negate the possibility that some participants might have had further education even after age 45 years, during follow-up. It is unclear whether this missing information might have affected our findings.
Conclusions
For the first time, to our knowledge, we report the population CVD burden for various categories of educational attainment using lifetime risk estimates. More than 1 in 2 individuals with less than high school education had a CVD event during his or her lifetime. Educational attainment was inversely associated with the lifetime risk of CVD, regardless of other important socioeconomic characteristics. Our findings emphasize the need for further efforts to reduce CVD inequalities related to educational disparities.
eMethods
eReferences
eTable. Unadjusted and Adjusted Risk (%) of Cardiovascular Disease (95% Confidence Interval) to Various Ages According to Educational Attainment at Age 45 among all participants
eFigure 1. Race-specific risk estimates of cardiovascular disease from age 45 to 85 years, non-high school vs. high school graduates (1987–2013)
eFigure 2. Risk estimates of cardiovascular disease from age 45 to 85 years, non-high school vs. high school graduates (1987–2013)
eFigure 3. Risk estimates of cardiovascular disease from age 55 to 85 years according to (A) occupations and (B) parental educational attainment (1996–2013)
eFigure 4. Risk estimates of cardiovascular disease from age 55 to 85 years in estimated jointly by educational attainment (non-high school vs. high school graduates) and (A) occupations (precision, service or machine operating job vs. homemaking or technical and sales or professional and managerial job) or (B) parental educational attainment (non-high school vs. high school graduates) (1996–2013)
eFigure 5. Risk estimates of cardiovascular disease from age 55 to 85 years according to (A) income at visit 4, and (B) jointly by educational attainment (non-high school vs. high school graduates) and family income (<$35,000 vs. ≥$35,000), (1987–2013)
eFigure 6. Risk estimates of cardiovascular disease according to educational attainment for participants born (A) before and (B) after 1935
References
- 1.Mackenbach JP, Cavelaars AE, Kunst AE, Groenhof F. Socioeconomic inequalities in cardiovascular disease mortality; an international study. Eur Heart J. 2000;21(14):1141-1151. [DOI] [PubMed] [Google Scholar]
- 2.Havranek EP, Mujahid MS, Barr DA, et al. ; American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council . Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873-898. [DOI] [PubMed] [Google Scholar]
- 3.McCarthy M. Tackling social factors is key in reducing cardiovascular disease, say US heart doctors. BMJ. 2015;351:h4333. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Health 2020: education and health through the life-course. http://www.euro.who.int/__data/assets/pdf_file/0007/324619/Health-2020-Education-and-health-through-the-life-course-en.pdf?ua=1. Accessed November 1, 2016.
- 5.Hoeymans N, Smit HA, Verkleij H, Kromhout D. Cardiovascular risk factors in relation to educational level in 36 000 men and women in the Netherlands. Eur Heart J. 1996;17(4):518-525. [DOI] [PubMed] [Google Scholar]
- 6.Kilander L, Berglund L, Boberg M, Vessby B, Lithell H. Education, lifestyle factors and mortality from cardiovascular disease and cancer: a 25-year follow-up of Swedish 50-year-old men. Int J Epidemiol. 2001;30(5):1119-1126. [DOI] [PubMed] [Google Scholar]
- 7.Yan LL, Liu K, Daviglus ML, et al. . Education, 15-year risk factor progression, and coronary artery calcium in young adulthood and early middle age: the Coronary Artery Risk Development in Young Adults study. JAMA. 2006;295(15):1793-1800. [DOI] [PubMed] [Google Scholar]
- 8.Woolf SH, Braveman P. Where health disparities begin: the role of social and economic determinants—and why current policies may make matters worse. Health Aff (Millwood). 2011;30(10):1852-1859. [DOI] [PubMed] [Google Scholar]
- 9.Pearson TA, Palaniappan LP, Artinian NT, et al. ; American Heart Association Council on Epidemiology and Prevention . American Heart Association guide for improving cardiovascular health at the community level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730-1753. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353(9147):89-92. [DOI] [PubMed] [Google Scholar]
- 11.Feuer EJ, Wun LM, Boring CC, Flanders WD, Timmel MJ, Tong T. The lifetime risk of developing breast cancer. J Natl Cancer Inst. 1993;85(11):892-897. [DOI] [PubMed] [Google Scholar]
- 12.ARIC Investigators The Atherosclerosis Risk in Communities (ARIC) study: design and objectives. Am J Epidemiol. 1989;129(4):687-702. [PubMed] [Google Scholar]
- 13.Folsom AR, Alonso A, Misialek JR, et al. . Parathyroid hormone concentration and risk of cardiovascular diseases: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2014;168(3):296-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beiser A, D’Agostino RB Sr, Seshadri S, Sullivan LM, Wolf PA. Computing estimates of incidence, including lifetime risk: Alzheimer’s disease in the Framingham Study: the Practical Incidence Estimators (PIE) macro. Stat Med. 2000;19(11-12):1495-1522. [DOI] [PubMed] [Google Scholar]
- 15.Woolf SH, Johnson RE, Phillips RL Jr, Philipsen M. Giving everyone the health of the educated: an examination of whether social change would save more lives than medical advances. Am J Public Health. 2007;97(4):679-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Din-Dzietham R, Liao D, Diez-Roux A, et al. . Association of educational achievement with pulsatile arterial diameter change of the common carotid artery: the Atherosclerosis Risk in Communities (ARIC) study, 1987-1992. Am J Epidemiol. 2000;152(7):617-627. [DOI] [PubMed] [Google Scholar]
- 17.Huisman M, Kunst AE, Bopp M, et al. . Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365(9458):493-500. [DOI] [PubMed] [Google Scholar]
- 18.Gupta R, Gupta VP, Ahluwalia NS. Educational status, coronary heart disease, and coronary risk factor prevalence in a rural population of India. BMJ. 1994;309(6965):1332-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmerman EB, Woolf SH, Haley A Understanding the Relationship Between Education and Health: a Review of the Evidence and an Examination of Community Perspectives. Bethesda, MD: National Institute of Health, Office of Behavioral and Social Sciences Research; 2015. [Google Scholar]
- 20.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4, pt 1):1973-1998. [DOI] [PubMed] [Google Scholar]
- 21.Suadicani P, Hein HO, Gyntelberg F. Strong mediators of social inequalities in risk of ischaemic heart disease: a six-year follow-up in the Copenhagen Male study. Int J Epidemiol. 1997;26(3):516-522. [DOI] [PubMed] [Google Scholar]
- 22.Nordahl H, Rod NH, Frederiksen BL, et al. . Education and risk of coronary heart disease: assessment of mediation by behavioral risk factors using the additive hazards model. Eur J Epidemiol. 2013;28(2):149-157. [DOI] [PubMed] [Google Scholar]
- 23.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308(17):1795-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chetty R, Stepner M, Abraham S, et al. . The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750-1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kvaavik E, Glymour M, Klepp KI, Tell GS, Batty GD. Parental education as a predictor of offspring behavioural and physiological cardiovascular disease risk factors. Eur J Public Health. 2012;22(4):544-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luckhaupt SE, Calvert GM; Centers for Disease Control and Prevention . Prevalence of coronary heart disease or stroke among workers aged <55 years—United States, 2008-2012. MMWR Morb Mortal Wkly Rep. 2014;63(30):645-649. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eReferences
eTable. Unadjusted and Adjusted Risk (%) of Cardiovascular Disease (95% Confidence Interval) to Various Ages According to Educational Attainment at Age 45 among all participants
eFigure 1. Race-specific risk estimates of cardiovascular disease from age 45 to 85 years, non-high school vs. high school graduates (1987–2013)
eFigure 2. Risk estimates of cardiovascular disease from age 45 to 85 years, non-high school vs. high school graduates (1987–2013)
eFigure 3. Risk estimates of cardiovascular disease from age 55 to 85 years according to (A) occupations and (B) parental educational attainment (1996–2013)
eFigure 4. Risk estimates of cardiovascular disease from age 55 to 85 years in estimated jointly by educational attainment (non-high school vs. high school graduates) and (A) occupations (precision, service or machine operating job vs. homemaking or technical and sales or professional and managerial job) or (B) parental educational attainment (non-high school vs. high school graduates) (1996–2013)
eFigure 5. Risk estimates of cardiovascular disease from age 55 to 85 years according to (A) income at visit 4, and (B) jointly by educational attainment (non-high school vs. high school graduates) and family income (<$35,000 vs. ≥$35,000), (1987–2013)
eFigure 6. Risk estimates of cardiovascular disease according to educational attainment for participants born (A) before and (B) after 1935