Abstract
Lymphatic vessels are essential for the uptake of fluid, immune cells, macromolecules, and lipids from the interstitial space. During lung transplant surgery, the pulmonary lymphatic vessel continuum is completely disrupted, and, as a result, lymphatic drainage function is severely compromised. After transplantation, the regeneration of an effective lymphatic drainage system plays a crucial role in maintaining interstitial fluid balance in the lung allograft. In the meantime, these newly formed lymphatic vessels are commonly held responsible for the development of immune responses leading to graft rejection, because they are potentially capable of transporting antigen-presenting cells loaded with allogeneic antigens to the draining lymph nodes. However, despite remarkable progress in the understanding of lymphatic biology, there is still a paucity of consistent evidence that demonstrates the exact impacts of lymphatic vessels on lung graft function. In this review, we examine the current literature related to roles of lymphatic vessels in the pathogenesis of lung transplant rejection.
Keywords: graft rejection, lymphangiogenesis, lung diseases
The lymphatic system is a specialized component of human vasculature that comprises an elaborate network of vessels in which lymph fluid flows unidirectionally toward the heart. Lymphatic vessels are integral for the uptake of fluid, macromolecules, immune cells, and lipids from the interstitial space (1). The formation of lymphatic vessels, or lymphangiogenesis, is critical during embryonic development; however, it should generally be quiescent in adults except in certain conditions, such as inflammation, tumor metastasis, and wound healing (2–4). Studies spanning multiple organ types have indicated that lymphatic vessels are also associated with induction of allograft tolerance as well as rejection after transplantation.
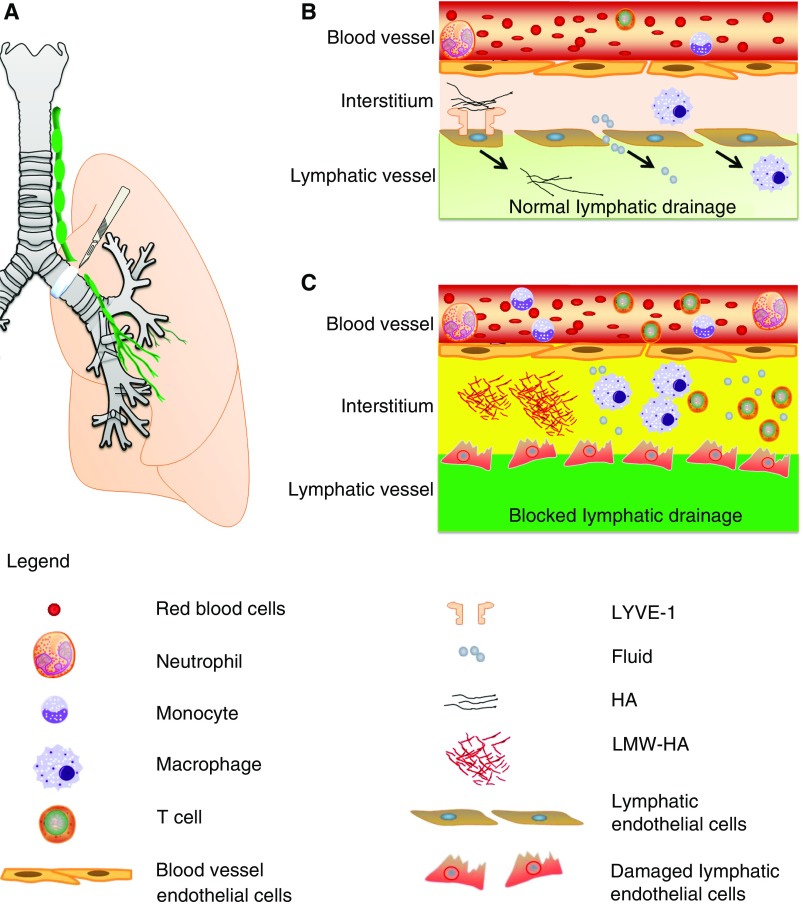
Lung transplantation is the only viable option for patients suffering from otherwise untreatable end-stage pulmonary diseases, including chronic obstructive pulmonary disease (COPD), cystic fibrosis, and pulmonary fibrosis (5). Although the lung graft survival rate has improved gradually over time, the long-term outcomes after lung transplantation lag considerably behind those of other solid organ transplantations (6). Despite prophylactic immunosuppression, acute rejection still occurs in the first postoperative year in approximately half of lung transplant recipients, who will ultimately succumb to bronchiolitis obliterans syndrome or chronic allograft rejection within 5 years after transplant (7). Lung transplantation restores respiratory airflow and vascular circulation of the graft through airway, pulmonary arterial, and venous anastomoses, although the morphological and functional integrity of the graft are not entirely preserved (8). The pulmonary lymphatic vessels are vital anatomical structures indispensable for pulmonary physiology, but they are inevitably interrupted during transplant surgery, and, as such, their functions are utterly compromised (Figure 1A).
Figure 1.
Interrupted pulmonary lymphatic drainage and its pathological outcomes in lung transplant. (A) Lymphatic vessel (green) is inevitably interrupted during lung transplant surgery. (B) Under physiological condition, lymphatic vessels maintain tissue homeostasis by draining excessive fluid, immune cells, and hyaluronan (HA) from the interstitial space. (C) Lymphatic drainage is blocked after lung transplant. During rejection, there are aberrant accumulations of fluid and low-molecular-weight HA (LMW-HA). In addition, an increased presence of immune cells is observed in the lung interstitium. LYVE = lymphatic vessel endothelial hyaluronan receptor.
During the past 2 decades, great strides have been made in elucidating the consequences of lymphatic vessel dysfunction and the therapeutic implications of promoting or inhibiting lymphatic vessel regeneration in various pathological conditions (9). Despite tremendous progress in the understanding of lymphatic biology, a key question remains unresolved: how exactly does lymphatic drainage affect lung graft function? In this review, we highlight findings that show a critical link between lymphatic vessels and outcomes of lung transplantation.
Lymphatic Vessels and Pulmonary Fluid Transport
The network of pulmonary lymphatic vessels is uniquely designed to drain extravasates from capillary beds and is integral to the maintenance of tissue fluid homeostasis. The initial lymphatics, also known as lymphatic capillaries, are the entry points for lymph fluid to the lymphatic system (10). Structurally, they are closed-ended microvessels composed of a single layer of overlapping oak leaf–shaped lymphatic endothelial cells (LECs) (11). The initial lymphatics lack a continuous basement membrane and are not surrounded by pericytes, but they are directly attached to the adjacent tissues via anchoring filaments to maintain vessel patency (12). Running along respiratory bronchioles, the initial lymphatics gradually merge into progressively larger muscular collecting lymphatics and ultimately drain into the right lymphatic duct and the thoracic duct (10). Under physiological conditions, continuously generated transcapillary fluid is efficiently drained through lymphatics (Figure 1B). When capillary fluid efflux is increased and/or lymphatic drainage is diminished, microvascular filtration exceeds lymphatic transport capacity, thereby causing edema (Figure 1C). Both of these two issues are tightly associated with lung transplant.
Lungs retrieved from brain dead organ donors are still the major source of lung grafts (13). Multiple studies suggest that before lung procurement, brain death initiates a complex process including hemodynamic, inflammatory, and sympathetic changes in the lung, which lead to elevated pulmonary capillary pressure and increased capillary barrier permeability (14). It has also been shown that alveolar macrophages are activated in response to brain death, and their long-term presence in the grafts after lung transplantation could contribute to fluid retention through pathological cellular crosstalk with alveolar epithelial cells (15–17). Worse still, the severed lymphatic vessels from donor lungs are not surgically reconnected to the recipients’, due to technical limitations. Consequently, there is a complete disruption of lymphatic flow. Indeed, during the first postoperative week, patients oftentimes develop pulmonary edema (18). Notably, studies have shown in mouse and canine lung transplant models that spontaneous recovery of pulmonary lymphatic flow between lung grafts and lymph nodes occurs in the second to the third post-transplant week in the absence of rejection (19–21). This explains that clinically, pulmonary edema gradually resolves on its own in most lung transplant recipients when rejection is properly controlled. In contrast, 10 to 25% of lung recipients develop primary graft dysfunction, a devastating condition characterized by severe lung edema with diffuse alveolar injury (22). The underlying pathomechanism of persistent edema in primary graft dysfunction is not completely understood and might be associated with interruption of normal lymphatic flow (23). In addition to its direct physical impact on alveolar space, the edema fluid contains potent surfactant inhibitors such as albumin and fibrinogen, which induce collapse of the alveoli (24). Consequently, there are significant alterations of gas exchange capacity, and lung function is inevitably impaired.
There have been multiple preclinical studies examining the efficacy of therapeutic lymphangiogenesis in facilitating the resolution of edema. In particular, therapeutic lymphangiogenesis is achieved by application of exogenous vascular endothelial growth factor (VEGF)-C, a member in the VEGF family that activates VEGF receptor (VEGFR)-2 and -3. Local administration of plasmid DNA encoding VEGF-C leads to reduced lymphedema by inducing lymphangiogenesis in a rabbit ear and a mouse tail model (25). Likewise, adenoviral vector–mediated gene transfer of VEGF-C has been shown to restore lymphatic vessel functionality and promote lymphatic drainage in a porcine lymphedema model (26). To avoid potential angiogenic effects and blood vessel leakiness, mutant forms of VEGF-C with exclusive binding affinity for VEGFR-3 on LECs (human VEGF-C156S or rat VEGF-C152S) have been tested and shown to increase lymphangiogenesis in a lymphedema mouse model and a rat myocardial infarction model, resulting in improved fluid balance (27, 28). Conversely, deletion of VEGF-C in mice results in prenatal death with lymphatic vessel defects and severe fluid retention (29), and inhibition of VEGFR-3 signaling causes conspicuous edema in mouse models of chronic airway and intestinal inflammation (2, 30). Although not directly tested in the setting of lung transplantation, the evidence above clearly favors the use of interventions that restore physiological lymphatic flow after lung transplant to control interstitial fluid volume and possibly reverse post-transplant lung edema.
Lymphatic Vessels and Immune Responses
The lung is constantly exposed to a large number of inhaled foreign antigens. To minimize the damaging impacts caused by such challenges, the lung has evolved to form tightly controlled immune responses to preserve its integrity (31). After lung transplantation, however, the induction of alloimmune responses against donor lung tissue should be dampened to achieve long-term graft survival.
Along with maintaining fluid equilibrium, lymphatic vessels also fulfill prominent roles in regulating immune responses by transporting soluble antigens and leukocytes (32). The role of lymphatic vessels in lung transplant rejection remains a much-debated topic, the complexity of which is highlighted by findings that lymphatic vessels could be either pathogenic or protective (Table 1). Current knowledge about the functions of lymphatic vessels in transplant immunology is generally gained from observations made in corneal transplant. After corneal transplantation, lymphangiogenesis develops and provides a conduit for antigen-presenting cells (APCs) trafficking from grafts to adjacent lymph nodes, which elicits alloimmune responses and exacerbates allograft rejection (33). Accordingly, inhibiting postoperative lymphangiogenesis improves corneal graft survival (34).
Table 1.
Experimental and clinical studies of lymphatic vessels in lung transplant rejection
| Species | Observations |
|---|---|
| Mouse | Orthotopic left lung transplant (model of acute rejection) |
| Decreased density of LYVE-1+ and VEGFR-3+/PROX-1+ lymphatic vessels in rejected grafts | |
| VEGF-C156S treatment induces lymphangiogenesis and alleviates established rejection (19) | |
| Rat | Heterotopic tracheal transplant (model of obliterative bronchiolitis) |
| Signs of lymphatic endothelial cell damage and loss of subepithelial LYVE-1+ lymphatic vessels in allografts | |
| Increased density of LYVE-1+, VEGFR-3+ lymphatic vessels in the airway wall of the allografts | |
| Overexpressing VEGF-C protects airway epithelium but aggravates airway occlusion in the allografts | |
| Blocking VEGF-C signaling by VEGFR-3-Ig inhibits lymphangiogenesis and attenuates airway occlusion (73) | |
| Canine | Left lung transplant (model of acute rejection) |
| In the absence of rejection, pulmonary lymphatic drainage is spontaneously restored 2–4 wk after transplant | |
| Reestablished pulmonary lymphatic drainage is disrupted again with the onset of acute rejection (20) | |
| Human | No change in the density of Podoplanin+ or LYVE-1+/VEGFR-3+ lymphatic vessels in lung tissue from patients with CLAD compared with control subjects (74) |
| No change in the density of Podoplanin+ lymphatic vessels in sequential transbronchial biopsies before and after alleviation of acute rejection (19) | |
| Increased density of PROX-1+ lymphatic vessels in transbronchial biopsies from patients with acute rejection (75) |
Definition of abbreviations: CLAD = chronic lung allograft dysfunction; LYVE = lymphatic vessel endothelial hyaluronan receptor; PROX = Prospero Homeobox; VEGF = vascular endothelial growth factor; VEGFR = vascular endothelial growth factor receptor.
Different from vascularized solid organs, such as lung and heart, the cornea is an immune-privileged tissue devoid of blood and lymphatic supplies under normal conditions (35). Therefore, experimental findings that indicate the deleterious impacts of increased lymphatic vessel growth and the overwhelming benefits of blocking lymphangiogenesis in corneal transplant rejection might not be completely applicable to other transplant settings. For example, sequential biopsies reveal that human kidney grafts with a density of lymphatic vessels higher than 6.5/mm2 within areas of cellular infiltrates have better kidney functional outcomes than those with lower lymphatic vessel density 1 year after transplantation (36). Similarly, human cardiac allografts with higher densities of lymphatic vessels half a month after transplant are less susceptible to severe rejection during the first postoperative year (37). In addition, rejection in a rat heart allograft transplantation model is associated with decreased lymphatic vessel density and increased cellular infiltrates (38). Previous research in other organs is further supported by our recent observation that the absence of lymphatic vessels is linked to immune cell infiltration and graft failure in an orthotopic mouse lung transplant model (19).
Interestingly, preclinical studies suggest that severe rejection, characterized by diffuse infiltrates of mononuclear cells, could be detected within the first postoperative week (39, 40), although lymphatic continuity between lung grafts and draining lymph nodes is not reestablished until a later stage (20). Furthermore, experimental findings from both mouse and canine lung transplant models suggest that there is minimal pulmonary lymphatic drainage when rejection takes place (19, 20). The chronological sequence clearly depicts that immune cell infiltration and rejection occur before restoration of lymphatic continuum. Because the severance of lymphatic vessels inevitably blocks the route of APCs to the recipient’s lymph nodes, how is the antigenic material from the lung grafts presented in the first place to initiate the immune responses? In mouse cardiac transplantation, secondary lymphoid organs from the recipient are indispensable in the initiation of graft rejection (41). Different from the heart, a previous study shows that antigen-loaded APCs are able to directly prime T cells in the lung without traveling to the draining lymph nodes (42). Furthermore, it is recently reported in an orthotopic mouse lung transplant model that acute lung rejection still occurs in recipients completely devoid of secondary lymphoid organs (43), providing a compelling argument that the presence of lymphatic vessels is not necessary for acute lung rejection.
A considerable amount of current literature shows the potential of prolymphangiogenic therapy in restraining immune response rather than perpetuating it. For instance, transgenic delivery of VEGF-C or intracutaneous administration of VEGF-C156S recombinant protein prevents inflammatory cell infiltration in skin inflammation (44, 45). Similarly, stimulating lymphangiogenesis effectively attenuates inflammation associated with myocardial infarction and colitis (28, 30). In contrast, inhibition of lymphangiogenesis is associated with retention of inflammatory cells within the site of injury (30). Consistent with the above findings, we recently showed that therapeutically induced lymphangiogenesis via VEGF-C156S effectively alters the inflammatory milieu associated with lung rejection by reducing the number of macrophages and T cells in the grafts (19). All the evidence collectively supports the notions that inadequate lymphatic drainage contributes to abnormal cellular infiltration, and prolymphangiogenic therapies modulate immune cell infiltration and mitigate the alloresponse.
Lymphatic and Hyaluronan Drainage
Hyaluronan (HA), also called hyaluronic acid, is a naturally occurring glycosaminoglycan. It is a key component of extracellular matrix abundantly distributed throughout the body. Physiologically, HA is produced as a high-molecular-weight (HMW) polymer at the plasma membrane by HA synthases 1, 2, and 3 (46). In response to tissue damage, the large linear polymers of HA can be broken down by hyaluronidases and/or reactive oxygen species into low-molecular-weight (LMW) bioactive fragments (47). HA serves miscellaneous, sometimes conflicting, functions, and its properties are distinctively influenced by its size. HMW-HA (>500 kD) is essential for lung interstitium by providing the structural integrity for normal lung tissue (48). In addition, experimental studies have shown that HMW-HA is protective against lung injury induced by smoke inhalation and sepsis (49, 50). On the other hand, LMW-HA (<500 kD) functions as a danger signal to trigger a perpetual sequence of inflammatory responses via CD44 and toll-like receptors 2 and 4 (46, 51). As a result, a host of proinflammatory mediators, such as monocyte chemoattractant protein-l and CC chemokine ligand 5, accumulate and further exacerbate the initial injury (52).
Elevated HA presence has been demonstrated in several lung disorders, such as asthma, pulmonary fibrosis, and COPD (53–55). It has also been shown that there is augmented HA deposition and fragmentation in plasma, bronchoalveolar lavage fluid, and lung tissue from patients with acute and chronic lung transplant rejection (19, 56–60), although HA production could be efficiently reduced by corticosteroids (61). The significance of HA in lung transplant rejection is further substantiated by findings that not only is LMW-HA directly connected to maturation of dendritic cells and disruption of established tolerance (59, 60) but also blockage of LMW-HA clearance aggravates the rejection response (19). In addition, HA is a hydrophilic molecule and functions to regulate water homeostasis. Accordingly, prolonged HA deposition causes notable water immobilization and may further exacerbate the initial tissue edema in the lung grafts.
Other than draining interstitial tissue fluid and transporting immune cells, lymphatic vessels preserve HA equilibrium by clearing HA fragments. In fact, approximately 85% of HA turnover takes place through lymphatics. HA binds to lymphatic vessel endothelial hyaluronan receptor (LYVE)-1 on LECs and is subsequently carried away via lymphatic vessels to be catabolized in lymph nodes and liver (62, 63). A recent study shows that vigorous uptake of HA by LECs depends on an abundant presence of LYVE-1 for durable engagement and that multiple LYVE-1 receptors are needed to secure the HA binding process (64).
Interestingly, the heightened presence of LMW-HA during acute lung injury is only temporary and resolves spontaneously over time when there are a sufficient number of LYVE-1–positive lymphatic vessels and intact lymphatic continuum (65, 66). In contrast, lung rejection is manifested by a persistent and progressive buildup of LMW-HA, suggesting that there may be deficient LMW-HA removal in rejected lung grafts. We have recently shown in an orthotopic mouse lung transplant model that there is a pronounced loss of pulmonary lymphatic vessels immunopositive for LYVE-1, VEGFR-3, and Prospero Homeobox (PROX)-1 (markers of LECs) along with aberrant accumulation of LMW-HA during allograft rejection. Moreover, therapeutic stimulation of lymphangiogenesis with VEGF-C156S suppresses established lung rejection and promotes LMW-HA clearance from the rejected lung grafts. As further evidence, blocking HA from binding to LYVE-1 via LYVE-1 function–blocking antibodies results in failed LMW-HA removal through lymphatic vessels and nullifies the therapeutic benefits generated by VEGF-C156S (19). Collectively, these findings underscore the detrimental impacts of LMW-HA accumulation on lung graft survival and the essential role of functional lymphatic vessels in HA clearance.
Future Perspectives
There has been remarkable progress in the identification of lymphatic-specific markers, characterization of LECs, and understanding of lymphatic function. These exceptional discoveries lead to the continued unraveling of mechanisms regulating physiological and pathological development of lymphatic vasculature. It is clear from the foregoing description that research into lung rejection may also benefit directly from enhanced insights into the complex biology of lymphatics.
Lymphatic imaging is a valuable approach for experimental research and clinical investigation of various medical conditions (67). Compared with conventional imaging modalities, including computed tomography and magnetic resonance imaging, multiphoton intravital microscopy (MP-IVM) possesses an unrivalled ability to continuously monitor biological events at the cellular level, and it is rapidly expanding our knowledge of the immune system (68). Its application has already generated substantial impacts on lung transplant research regarding neutrophil trafficking behaviors (69). Together with the use of transgenic lymphatic reporter mice, MP-IVM could be a promising technique for real-time exploration of the distinct attributes of lymphatics in the lung. In addition, MP-IVM will be a powerful tool to decipher the origin of LECs in lung grafts. Determination of their origin not only provides us with clues about their changes during rejection but also is extremely useful to evaluate the effects of prolymphangiogenic therapy.
It is worth mentioning that therapeutically induced lymphatic regeneration through pharmacological treatments may take days or even weeks to be fully functional and is not able to reestablish the lymphatic continuum immediately after surgery to save the lung grafts from the initial injury. Nonetheless, identification and preclinical testing of small molecules with potent prolymphangiogenic properties could improve our understanding regarding roles of the lymphatic vasculature in acute allograft rejection and advance the drug development process, with possible patient application in a wide spectrum of diseases.
It is not known whether anastomosis between donor and recipient lymphatic vessels could be beneficial for lung graft survival, but much could be learned from the surgical breakthrough that physically reconnects lymphatic vessels during intestinal transplant. Preclinical studies have demonstrated that microsurgical lymphatic reconstruction improves the long-term survival of small bowel grafts (70, 71). Similar to the lung, the gastrointestinal tract is constantly challenged by a diversity of foreign antigens (72). Because the efficacy of lymphatic anastomosis has been shown in intestinal transplantation, it is entirely conceivable that comparable benefits could be achieved in lung transplant as well. Therefore, future experimental endeavors should focus on developing a microsurgical lung transplant model with reestablished lymphatic drainage and examining the significance of such physiological connection.
Conclusions
In summary, accumulating evidence demonstrates that acute lung rejection develops in the absence of secondary lymphoid organs, and therapeutic induction of lymphangiogenesis could be beneficial for lung graft survival. Future investigations that use modern imaging modalities will shed light on the changes of lymphatics during lung transplant rejection. Finally, strategies to promptly restore physiological pulmonary lymphatic drainage by potent prolymphangiogenic molecules or surgical interventions may serve as valid therapeutic options to improve outcomes in recipients of lung transplants.
Supplementary Material
Footnotes
Supported by National Institutes of Health grants R21 HL119902 and R01 HL130275 (S.E.-C.).
Author Contributions: Y.C. and S.E.-C. drafted the manuscript; K.L., A.M.L., and G.V. contributed to manuscript revision.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Betterman KL, Harvey NL. The lymphatic vasculature: development and role in shaping immunity. Immunol Rev. 2016;271:276–292. doi: 10.1111/imr.12413. [DOI] [PubMed] [Google Scholar]
- 2.Baluk P, Tammela T, Ator E, Lyubynska N, Achen MG, Hicklin DJ, Jeltsch M, Petrova TV, Pytowski B, Stacker SA, et al. Pathogenesis of persistent lymphatic vessel hyperplasia in chronic airway inflammation. J Clin Invest. 2005;115:247–257. doi: 10.1172/JCI22037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martínez-Corral I, Olmeda D, Diéguez-Hurtado R, Tammela T, Alitalo K, Ortega S. In vivo imaging of lymphatic vessels in development, wound healing, inflammation, and tumor metastasis. Proc Natl Acad Sci USA. 2012;109:6223–6228. doi: 10.1073/pnas.1115542109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamashita M, Mouri T, Niisato M, Kowada K, Kobayashi H, Chiba R, Satoh T, Sugai T, Sawai T, Takahashi T, et al. Heterogeneous characteristics of lymphatic microvasculatures associated with pulmonary sarcoid granulomas. Ann Am Thorac Soc. 2013;10:90–97. doi: 10.1513/AnnalsATS.201209-078OC. [DOI] [PubMed] [Google Scholar]
- 5.Arcasoy SM, Kotloff RM. Lung transplantation. N Engl J Med. 1999;340:1081–1091. doi: 10.1056/NEJM199904083401406. [DOI] [PubMed] [Google Scholar]
- 6.Yusen RD, Shearon TH, Qian Y, Kotloff R, Barr ML, Sweet S, Dyke DB, Murray S. Lung transplantation in the United States, 1999-2008. Am J Transplant. 2010;10:1047–1068. doi: 10.1111/j.1600-6143.2010.03055.x. [DOI] [PubMed] [Google Scholar]
- 7.Trulock EP, Christie JD, Edwards LB, Boucek MM, Aurora P, Taylor DO, Dobbels F, Rahmel AO, Keck BM, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: twenty-fourth official adult lung and heart-lung transplantation report-2007. J Heart Lung Transplant. 2007;26:782–795. doi: 10.1016/j.healun.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Griffith BP, Magee MJ, Gonzalez IF, Houel R, Armitage JM, Hardesty RL, Hattler BG, Ferson PF, Landreneau RJ, Keenan RJ. Anastomotic pitfalls in lung transplantation. J Thorac Cardiovasc Surg. 1994;107:743–753; discussion 753–754. [PubMed] [Google Scholar]
- 9.Adamczyk LA, Gordon K, Kholova I, Meijer-Jorna LB, Telinius N, Gallagher PJ, van der Wal AC, Baandrup U. Lymph vessels: the forgotten second circulation in health and disease. Virchows Archiv. 2016;469:3–17. doi: 10.1007/s00428-016-1945-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schraufnagel DE. Lung lymphatic anatomy and correlates. Pathophysiology. 2010;17:337–343. doi: 10.1016/j.pathophys.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 11.Tammela T, Alitalo K. Lymphangiogenesis: molecular mechanisms and future promise. Cell. 2010;140:460–476. doi: 10.1016/j.cell.2010.01.045. [DOI] [PubMed] [Google Scholar]
- 12.Baluk P, Fuxe J, Hashizume H, Romano T, Lashnits E, Butz S, Vestweber D, Corada M, Molendini C, Dejana E, et al. Functionally specialized junctions between endothelial cells of lymphatic vessels. J Exp Med. 2007;204:2349–2362. doi: 10.1084/jem.20062596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Raemdonck D, Neyrinck A, Verleden GM, Dupont L, Coosemans W, Decaluwé H, Decker G, De Leyn P, Nafteux P, Lerut T. Lung donor selection and management. Proc Am Thorac Soc. 2009;6:28–38. doi: 10.1513/pats.200808-098GO. [DOI] [PubMed] [Google Scholar]
- 14.Avlonitis VS, Wigfield CH, Kirby JA, Dark JH. The hemodynamic mechanisms of lung injury and systemic inflammatory response following brain death in the transplant donor. Am J Transplant. 2005;5:684–693. doi: 10.1111/j.1600-6143.2005.00755.x. [DOI] [PubMed] [Google Scholar]
- 15.Watts RP, Thom O, Fraser JF.Inflammatory signalling associated with brain dead organ donation: from brain injury to brain stem death and posttransplant ischaemia reperfusion injury J Transplant 2013. 2013:521369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nayak DK, Zhou F, Xu M, Huang J, Tsuji M, Hachem R, Mohanakumar T. Long-term persistence of donor alveolar macrophages in human lung transplant recipients that influences donor-specific immune responses. Am J Transplant. 2016;16:2300–2311. doi: 10.1111/ajt.13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peteranderl C, Morales-Nebreda L, Selvakumar B, Lecuona E, Vadász I, Morty RE, Schmoldt C, Bespalowa J, Wolff T, Pleschka S, et al. Macrophage-epithelial paracrine crosstalk inhibits lung edema clearance during influenza infection. J Clin Invest. 2016;126:1566–1580. doi: 10.1172/JCI83931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan SU, Salloum J, O’Donovan PB, Mascha EJ, Mehta AC, Matthay MA, Arroliga AC. Acute pulmonary edema after lung transplantation: the pulmonary reimplantation response. Chest. 1999;116:187–194. doi: 10.1378/chest.116.1.187. [DOI] [PubMed] [Google Scholar]
- 19.Cui Y, Liu K, Monzon-Medina ME, Padera RF, Wang H, George G, Toprak D, Abdelnour E, D’Agostino E, Goldberg HJ, et al. Therapeutic lymphangiogenesis ameliorates established acute lung allograft rejection. J Clin Invest. 2015;125:4255–4268. doi: 10.1172/JCI79693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruggiero R, Fietsam R, Jr, Thomas GA, Muz J, Farris RH, Kowal TA, Myles JL, Stephenson LW, Baciewicz FA., Jr Detection of canine allograft lung rejection by pulmonary lymphoscintigraphy. J Thorac Cardiovasc Surg. 1994;108:253–258. [PubMed] [Google Scholar]
- 21.Ruggiero R, Muz J, Fietsam R, Jr, Thomas GA, Welsh RJ, Miller JE, Stephenson LW, Baciewicz FA., Jr Reestablishment of lymphatic drainage after canine lung transplantation. J Thorac Cardiovasc Surg. 1993;106:167–171. [PubMed] [Google Scholar]
- 22.Lee JC, Christie JD. Primary graft dysfunction. Proc Am Thorac Soc. 2009;6:39–46. doi: 10.1513/pats.200808-082GO. [DOI] [PubMed] [Google Scholar]
- 23.Belmaati E, Jensen C, Kofoed KF, Iversen M, Steffensen I, Nielsen MB. Primary graft dysfunction; possible evaluation by high resolution computed tomography, and suggestions for a scoring system. Interact Cardiovasc Thorac Surg. 2009;9:859–867. doi: 10.1510/icvts.2009.207852. [DOI] [PubMed] [Google Scholar]
- 24.Nitta K, Kobayashi T. Impairment of surfactant activity and ventilation by proteins in lung edema fluid. Respir Physiol. 1994;95:43–51. doi: 10.1016/0034-5687(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 25.Yoon YS, Murayama T, Gravereaux E, Tkebuchava T, Silver M, Curry C, Wecker A, Kirchmair R, Hu CS, Kearney M, et al. VEGF-C gene therapy augments postnatal lymphangiogenesis and ameliorates secondary lymphedema. J Clin Invest. 2003;111:717–725. doi: 10.1172/JCI15830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lähteenvuo M, Honkonen K, Tervala T, Tammela T, Suominen E, Lähteenvuo J, Kholová I, Alitalo K, Ylä-Herttuala S, Saaristo A. Growth factor therapy and autologous lymph node transfer in lymphedema. Circulation. 2011;123:613–620. doi: 10.1161/CIRCULATIONAHA.110.965384. [DOI] [PubMed] [Google Scholar]
- 27.Saaristo A, Veikkola T, Tammela T, Enholm B, Karkkainen MJ, Pajusola K, Bueler H, Ylä-Herttuala S, Alitalo K. Lymphangiogenic gene therapy with minimal blood vascular side effects. J Exp Med. 2002;196:719–730. doi: 10.1084/jem.20020587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henri O, Pouehe C, Houssari M, Galas L, Nicol L, Edwards-Lévy F, Henry JP, Dumesnil A, Boukhalfa I, Banquet S, et al. Selective stimulation of cardiac lymphangiogenesis reduces myocardial edema and fibrosis leading to improved cardiac function following myocardial infarction. Circulation. 2016;133:1484–1497; discussion 1497. doi: 10.1161/CIRCULATIONAHA.115.020143. [DOI] [PubMed] [Google Scholar]
- 29.Karkkainen MJ, Haiko P, Sainio K, Partanen J, Taipale J, Petrova TV, Jeltsch M, Jackson DG, Talikka M, Rauvala H, et al. Vascular endothelial growth factor C is required for sprouting of the first lymphatic vessels from embryonic veins. Nat Immunol. 2004;5:74–80. doi: 10.1038/ni1013. [DOI] [PubMed] [Google Scholar]
- 30.D’Alessio S, Correale C, Tacconi C, Gandelli A, Pietrogrande G, Vetrano S, Genua M, Arena V, Spinelli A, Peyrin-Biroulet L, et al. VEGF-C-dependent stimulation of lymphatic function ameliorates experimental inflammatory bowel disease. J Clin Invest. 2014;124:3863–3878. doi: 10.1172/JCI72189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hasenberg M, Stegemann-Koniszewski S, Gunzer M. Cellular immune reactions in the lung. Immunol Rev. 2013;251:189–214. doi: 10.1111/imr.12020. [DOI] [PubMed] [Google Scholar]
- 32.Schraufnagel DE. Lung lymphatics: why should a clinician care? Ann Am Thorac Soc. 2013;10:148–149. doi: 10.1513/AnnalsATS.201302-029ED. [DOI] [PubMed] [Google Scholar]
- 33.Dietrich T, Bock F, Yuen D, Hos D, Bachmann BO, Zahn G, Wiegand S, Chen L, Cursiefen C. Cutting edge: lymphatic vessels, not blood vessels, primarily mediate immune rejections after transplantation. J Immunol. 2010;184:535–539. doi: 10.4049/jimmunol.0903180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cursiefen C, Cao J, Chen L, Liu Y, Maruyama K, Jackson D, Kruse FE, Wiegand SJ, Dana MR, Streilein JW. Inhibition of hemangiogenesis and lymphangiogenesis after normal-risk corneal transplantation by neutralizing VEGF promotes graft survival. Invest Ophthalmol Vis Sci. 2004;45:2666–2673. doi: 10.1167/iovs.03-1380. [DOI] [PubMed] [Google Scholar]
- 35.Cursiefen C, Chen L, Dana MR, Streilein JW. Corneal lymphangiogenesis: evidence, mechanisms, and implications for corneal transplant immunology. Cornea. 2003;22:273–281. doi: 10.1097/00003226-200304000-00021. [DOI] [PubMed] [Google Scholar]
- 36.Stuht S, Gwinner W, Franz I, Schwarz A, Jonigk D, Kreipe H, Kerjaschki D, Haller H, Mengel M. Lymphatic neoangiogenesis in human renal allografts: results from sequential protocol biopsies. Am J Transplant. 2007;7:377–384. doi: 10.1111/j.1600-6143.2006.01638.x. [DOI] [PubMed] [Google Scholar]
- 37.Geissler HJ, Dashkevich A, Fischer UM, Fries JW, Kuhn-Regnier F, Addicks K, Mehlhorn U, Bloch W. First year changes of myocardial lymphatic endothelial markers in heart transplant recipients. Eur J Cardiothorac Surg. 2006;29:767–771. doi: 10.1016/j.ejcts.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 38.Soong TR, Pathak AP, Asano H, Fox-Talbot K, Baldwin WM., III Lymphatic injury and regeneration in cardiac allografts. Transplantation. 2010;89:500–508. doi: 10.1097/TP.0b013e3181c73c34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iken K, Liu K, Liu H, Bizargity P, Wang L, Hancock WW, Visner GA. Indoleamine 2,3-dioxygenase and metabolites protect murine lung allografts and impair the calcium mobilization of T cells. Am J Respir Cell Mol Biol. 2012;47:405–416. doi: 10.1165/rcmb.2011-0438OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krupnick AS, Lin X, Li W, Higashikubo R, Zinselmeyer BH, Hartzler H, Toth K, Ritter JH, Berezin MY, Wang ST, et al. Central memory CD8+ T lymphocytes mediate lung allograft acceptance. J Clin Invest. 2014;124:1130–1143. doi: 10.1172/JCI71359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lakkis FG, Arakelov A, Konieczny BT, Inoue Y. Immunologic ‘ignorance’ of vascularized organ transplants in the absence of secondary lymphoid tissue. Nat Med. 2000;6:686–688. doi: 10.1038/76267. [DOI] [PubMed] [Google Scholar]
- 42.Constant SL, Brogdon JL, Piggott DA, Herrick CA, Visintin I, Ruddle NH, Bottomly K. Resident lung antigen-presenting cells have the capacity to promote Th2 T cell differentiation in situ. J Clin Invest. 2002;110:1441–1448. doi: 10.1172/JCI16109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gelman AE, Li W, Richardson SB, Zinselmeyer BH, Lai J, Okazaki M, Kornfeld CG, Kreisel FH, Sugimoto S, Tietjens JR, et al. Cutting edge: acute lung allograft rejection is independent of secondary lymphoid organs. J Immunol. 2009;182:3969–3973. doi: 10.4049/jimmunol.0803514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huggenberger R, Siddiqui SS, Brander D, Ullmann S, Zimmermann K, Antsiferova M, Werner S, Alitalo K, Detmar M. An important role of lymphatic vessel activation in limiting acute inflammation. Blood. 2011;117:4667–4678. doi: 10.1182/blood-2010-10-316356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huggenberger R, Ullmann S, Proulx ST, Pytowski B, Alitalo K, Detmar M. Stimulation of lymphangiogenesis via VEGFR-3 inhibits chronic skin inflammation. J Exp Med. 2010;207:2255–2269. doi: 10.1084/jem.20100559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jiang D, Liang J, Noble PW. Hyaluronan as an immune regulator in human diseases. Physiol Rev. 2011;91:221–264. doi: 10.1152/physrev.00052.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Monzon ME, Fregien N, Schmid N, Falcon NS, Campos M, Casalino-Matsuda SM, Forteza RM. Reactive oxygen species and hyaluronidase 2 regulate airway epithelial hyaluronan fragmentation. J Biol Chem. 2010;285:26126–26134. doi: 10.1074/jbc.M110.135194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ruppert SM, Hawn TR, Arrigoni A, Wight TN, Bollyky PL. Tissue integrity signals communicated by high-molecular weight hyaluronan and the resolution of inflammation. Immunol Res. 2014;58:186–192. doi: 10.1007/s12026-014-8495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang PM, Syrkina O, Yu L, Dedaj R, Zhao H, Shiedlin A, Liu YY, Garg H, Quinn DA, Hales CA. High MW hyaluronan inhibits smoke inhalation-induced lung injury and improves survival. Respirology. 2010;15:1131–1139. doi: 10.1111/j.1440-1843.2010.01829.x. [DOI] [PubMed] [Google Scholar]
- 50.Liu YY, Lee CH, Dedaj R, Zhao H, Mrabat H, Sheidlin A, Syrkina O, Huang PM, Garg HG, Hales CA, et al. High-molecular-weight hyaluronan--a possible new treatment for sepsis-induced lung injury: a preclinical study in mechanically ventilated rats. Crit Care. 2008;12:R102. doi: 10.1186/cc6982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scheibner KA, Lutz MA, Boodoo S, Fenton MJ, Powell JD, Horton MR. Hyaluronan fragments act as an endogenous danger signal by engaging TLR2. J Immunol. 2006;177:1272–1281. doi: 10.4049/jimmunol.177.2.1272. [DOI] [PubMed] [Google Scholar]
- 52.McKee CM, Penno MB, Cowman M, Burdick MD, Strieter RM, Bao C, Noble PW. Hyaluronan (HA) fragments induce chemokine gene expression in alveolar macrophages: the role of HA size and CD44. J Clin Invest. 1996;98:2403–2413. doi: 10.1172/JCI119054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vignola AM, Chanez P, Campbell AM, Souques F, Lebel B, Enander I, Bousquet J. Airway inflammation in mild intermittent and in persistent asthma. Am J Respir Crit Care Med. 1998;157:403–409. doi: 10.1164/ajrccm.157.2.96-08040. [DOI] [PubMed] [Google Scholar]
- 54.Bjermer L, Lundgren R, Hällgren R. Hyaluronan and type III procollagen peptide concentrations in bronchoalveolar lavage fluid in idiopathic pulmonary fibrosis. Thorax. 1989;44:126–131. doi: 10.1136/thx.44.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dentener MA, Vernooy JH, Hendriks S, Wouters EF. Enhanced levels of hyaluronan in lungs of patients with COPD: relationship with lung function and local inflammation. Thorax. 2005;60:114–119. doi: 10.1136/thx.2003.020842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rao PN, Zeevi A, Snyder J, Spichty K, Habrat T, Warty V, Dauber J, Paradis I, Duncan S, Pham S, et al. Monitoring of acute lung rejection and infection by bronchoalveolar lavage and plasma levels of hyaluronic acid in clinical lung transplantation. J Heart Lung Transplant. 1994;13:958–962. [PubMed] [Google Scholar]
- 57.Riise GC, Scherstén H, Nilsson F, Ryd W, Andersson BA. Activation of eosinophils and fibroblasts assessed by eosinophil cationic protein and hyaluronan in BAL: association with acute rejection in lung transplant recipients. Chest. 1996;110:89–96. doi: 10.1378/chest.110.1.89. [DOI] [PubMed] [Google Scholar]
- 58.Riise GC, Kjellström C, Ryd W, Scherstén H, Nilsson F, Mårtensson G, Andersson BA. Inflammatory cells and activation markers in BAL during acute rejection and infection in lung transplant recipients: a prospective, longitudinal study. Eur Respir J. 1997;10:1742–1746. doi: 10.1183/09031936.97.10081742. [DOI] [PubMed] [Google Scholar]
- 59.Todd JL, Wang X, Sugimoto S, Kennedy VE, Zhang HL, Pavlisko EN, Kelly FL, Huang H, Kreisel D, Palmer SM, et al. Hyaluronan contributes to bronchiolitis obliterans syndrome and stimulates lung allograft rejection through activation of innate immunity. Am J Respir Crit Care Med. 2014;189:556–566. doi: 10.1164/rccm.201308-1481OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tesar BM, Jiang D, Liang J, Palmer SM, Noble PW, Goldstein DR. The role of hyaluronan degradation products as innate alloimmune agonists. Am J Transplant. 2006;6:2622–2635. doi: 10.1111/j.1600-6143.2006.01537.x. [DOI] [PubMed] [Google Scholar]
- 61.Zhang W, Watson CE, Liu C, Williams KJ, Werth VP. Glucocorticoids induce a near-total suppression of hyaluronan synthase mRNA in dermal fibroblasts and in osteoblasts: a molecular mechanism contributing to organ atrophy. Biochem J. 2000;349:91–97. doi: 10.1042/0264-6021:3490091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Banerji S, Ni J, Wang SX, Clasper S, Su J, Tammi R, Jones M, Jackson DG. LYVE-1, a new homologue of the CD44 glycoprotein, is a lymph-specific receptor for hyaluronan. J Cell Biol. 1999;144:789–801. doi: 10.1083/jcb.144.4.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Laurent UB, Dahl LB, Reed RK. Catabolism of hyaluronan in rabbit skin takes place locally, in lymph nodes and liver. Exp Physiol. 1991;76:695–703. doi: 10.1113/expphysiol.1991.sp003536. [DOI] [PubMed] [Google Scholar]
- 64.Lawrance W, Banerji S, Day AJ, Bhattacharjee S, Jackson DG. Binding of hyaluronan to the native lymphatic vessel endothelial receptor LYVE-1 is critically dependent on receptor clustering and hyaluronan organization. J Biol Chem. 2016;291:8014–8030. doi: 10.1074/jbc.M115.708305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Teder P, Vandivier RW, Jiang D, Liang J, Cohn L, Puré E, Henson PM, Noble PW. Resolution of lung inflammation by CD44. Science. 2002;296:155–158. doi: 10.1126/science.1069659. [DOI] [PubMed] [Google Scholar]
- 66.Meinecke AK, Nagy N, Lago GD, Kirmse S, Klose R, Schrödter K, Zimmermann A, Helfrich I, Rundqvist H, Theegarten D, et al. Aberrant mural cell recruitment to lymphatic vessels and impaired lymphatic drainage in a murine model of pulmonary fibrosis. Blood. 2012;119:5931–5942. doi: 10.1182/blood-2011-12-396895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sevick-Muraca EM, Kwon S, Rasmussen JC. Emerging lymphatic imaging technologies for mouse and man. J Clin Invest. 2014;124:905–914. doi: 10.1172/JCI71612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ishii T, Ishii M. Intravital two-photon imaging: a versatile tool for dissecting the immune system. Ann Rheum Dis. 2011;70:i113–i115. doi: 10.1136/ard.2010.138156. [DOI] [PubMed] [Google Scholar]
- 69.Kreisel D, Nava RG, Li W, Zinselmeyer BH, Wang B, Lai J, Pless R, Gelman AE, Krupnick AS, Miller MJ. In vivo two-photon imaging reveals monocyte-dependent neutrophil extravasation during pulmonary inflammation. Proc Natl Acad Sci USA. 2010;107:18073–18078. doi: 10.1073/pnas.1008737107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kellersmann R, Zhong R, Gao ZH, Garcia B, Zhang Z, Kiyochi H, Xing JJ, Grant D. Beneficial effects of microsurgical lymphatic reconstruction after intestinal transplantation in rats. Transplant Proc. 1998;30:2642. doi: 10.1016/s0041-1345(98)00764-7. [DOI] [PubMed] [Google Scholar]
- 71.Szymula von Richter TP, Baumeister RG, Hammer C. Microsurgical reconstruction of the lymphatic and nerve system in small bowel transplantation: the rat model, first results. Transpl Int. 1996;9:S286–289. doi: 10.1007/978-3-662-00818-8_71. [DOI] [PubMed] [Google Scholar]
- 72.Steele L, Mayer L, Berin MC. Mucosal immunology of tolerance and allergy in the gastrointestinal tract. Immunol Res. 2012;54:75–82. doi: 10.1007/s12026-012-8308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krebs R, Tikkanen JM, Ropponen JO, Jeltsch M, Jokinen JJ, Ylä-Herttuala S, Nykänen AI, Lemström KB. Critical role of VEGF-C/VEGFR-3 signaling in innate and adaptive immune responses in experimental obliterative bronchiolitis. Am J Pathol. 2012;181:1607–1620. doi: 10.1016/j.ajpath.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 74.Traxler D, Schweiger T, Schwarz S, Schuster MM, Jaksch P, Lang G, Birner P, Klepetko W, Ankersmit HJ, Hoetzenecker K.The lymphatic phenotype of lung allografts in patients with bronchiolitis obliterans syndrome and restrictive allograft syndrome Transplantation[online ahead of print] 10 May 2016DOI: 10.1097/TP.0000000000001263 [DOI] [PubMed] [Google Scholar]
- 75.Dashkevich A, Heilmann C, Kayser G, Germann M, Beyersdorf F, Passlick B, Geissler HJ. Lymph angiogenesis after lung transplantation and relation to acute organ rejection in humans. Ann Thorac Surg. 2010;90:406–411. doi: 10.1016/j.athoracsur.2010.03.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.