Abstract
Introduction:
The analgesic effect of low-level laser therapy (LLLT) after mandibular third molar (MTM) extraction is controversial. The aim is to evaluate the effect of intraoral LLLT on postoperative pain after MTMs extraction.
Methods:
Thirty patients with bilateral symmetrical impacted MTMs underwent surgical extractions. Experimental and control sides were randomly selected to receive LLLT or placebo. Following suturing, a dental assistant applied 810 nm gallium aluminum arsenide (GaAlAs) at three points for 30 s each with a total energy of 9 J. Pain was recorded on a visual analog scale on the 7 successive days.
Results:
Data analyzed by IBM SPSS Statistics 23 for Windows with P ≤ 0.05 significance level. LLLT appeared to have a high significant effect on pain reduction; however, there was a mild increase in pain after the 4th day.
Conclusion:
Intraoral 810 nm GaAlAs is effective in reducing postoperative pain when a dose of 32.86 J/cm2 is used.
Keywords: Gallium aluminum arsenides, low-level laser therapy, pain, third molar extraction, visual analog scale
INTRODUCTION AND LITERATURE REVIEW
Extraction of mandibular impacted third molars is a common dental surgical procedure.[1,2,3,4,5,6] This may result in tissue trauma and inflammation, developing postoperative pain [Figure 1].[5,6,7,8] Pain peaks within the first 5 h and decreases over a week.[3,4,6,8] The management of postoperative pain by medications such as nonsteroidal anti-inflammatory drugs and corticosteroids has been reported.[4,9] However, their use is often associated with potential side effects, such as peptic ulcer disease, gastrointestinal bleeding and perforation, impaired renal function, allergic reactions, and inhibition of platelet function.[4,9] To minimize these side effects, there are alternative methods to control postoperative pain, such as surgical closure techniques with or without incorporation of drains, use of cryotherapy and laser application.[1,6,10,11,12,13]
Figure 1.
Sequel of tooth extraction
LASER is an acronym for Light Amplification by Stimulated Emission of Radiation. The energy output differentiates LASER into “hard” and “soft.” Hard lasers have large energy output and are used for cutting tissues, whereas soft lasers are low-level lasers that promote tissue healing.[11] Low-level laser therapy (LLLT) was discovered incidentally in attempt to treat cancerous cells with a ruby laser and it was found that it did not kill tumor cells instead it accelerated wound healing from which the concept of photobiomodulation developed.[14] Since then, laser therapy has been used in dentistry for different applications, wound healing, aphthous stomatitis, mucositis, neural regeneration, postherpetic neuralgia, synovitis, arthritis, tempromandibular joint pathology, acute abcesses, periapical granulomas, chronic orofacial pain, and bone regeneration.[13,15,16,17,18,19,20] LLLT analgesic effects are obtained by stimulating the synthesis of endogenous endorphins (β-endorphin), decreasing the inflammatory cytokines and enzymes, altering the pain threshold, inducing morphological neurons changes, reducing the mitochondrial membrane potential, and blocking the fast axonal flow leading to neural conduction blockage.[4,12] The anti-inflammatory effect is due to an increase of the phagocytic activity, the number and diameter of lymphatic vessels, decrease in the permeability of blood vessels and restoration of microcapillary circulation, normalizing the permeability of the vascular wall, and decreasing the edema [Figure 2].[2,4,6,12,13,17,20,21]
Figure 2.
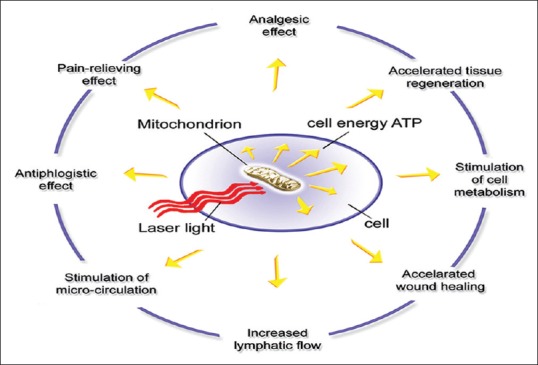
Mechanism of action of low-level laser therapy
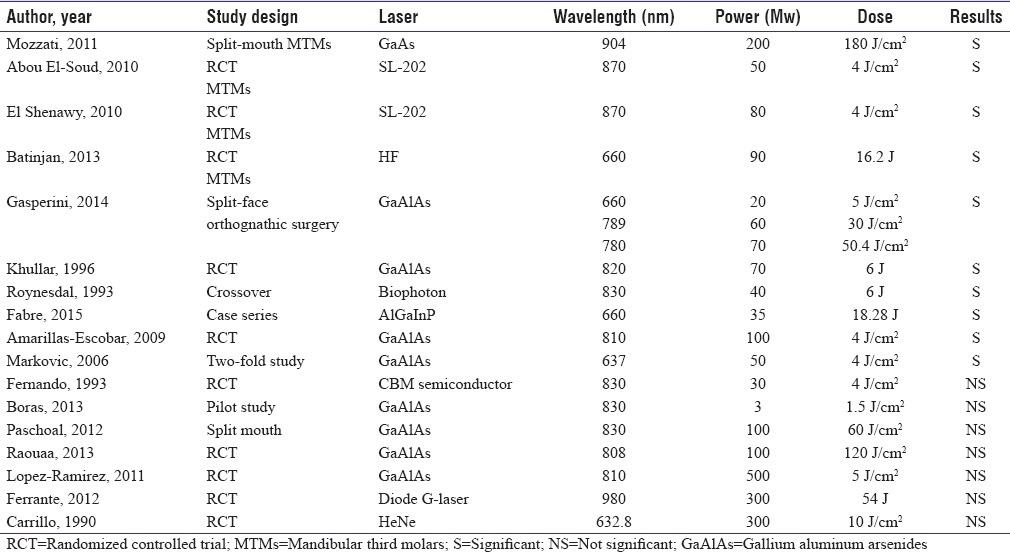
The effect of LLLT on pain reduction after third molars extractions is controversial [Table 1]. Some studies showed clinical significance in the reduction of postoperative pain and swelling when soft laser of 870 nm wavelength, energy output of 4 J/cm2, and constant power of 50 and 80 mW were used intraorally from a distance of 1 cm for 10 min after extraction.[8,9] Moreover, the use of gallium aluminum arsenide (GaAlAs) with wavelengths range from 660 nm to 904 nm and power of 35–200 mW for different time intervals showed clinical significance in pain reduction.[7,21,22,23,24,25,26] Another study reported that the intra- and extra-oral use of 810 nm wavelength and 4 J/cm2 energy output using continuous wave reduces postoperative pain, swelling, and trismus, a reduction that was not deemed statistically significant.[3] In addition, the intra- and extra-oral application of 660–789 nm GaAlAs laser with energy output of 21.6 J and 50.4 J, respectively, had a significant reduction in pain at days 1 and 3 postoperatively.[25] In contrast, other studies demonstrated no beneficial effects in pain reduction using LLLT after the removal of impacted mandibular third molars (MTMs).[4,6,11,23,27,28,29,30]
Table 1.
Summary of laser parameters used in other clinical trials studying the effect of low-level laser therapy on postsurgical pain
The lack of a standardized laser application methodology among studies with regard to the sample selection, sample size, control, and LLLT parameters had contributed to the controversial postoperative pain reduction effectiveness of LLLT. The purpose of this study is to evaluate the effect of intraoral LLLT on the postoperative pain following the extraction of MTMs.
The aims and objectives of this study are to understand:
The effect of LLLT on pain
The effect of age on pain
The effect of gender on pain
The effect of surgical difficulty on pain
The effect of LLLT on the number of postoperative analgesics used
The effect of LLLT on postoperative mouth opening.
SUBJECTS AND METHODS
The experimental design
This randomized, controlled, double-blind, prospective split-mouth clinical trial was conducted at Medical Laser Center Dental, Abu Dhabi, UAE, after obtaining an ethical approval from the Research Committee of Maktoum Bin Hamdan Dental University College. Thirty healthy patients with bilateral asymptomatic symmetrical impacted MTMs on orthopantomographs were included in the study [Figure 3]. An informed consent was discussed with each patient and signed by both the researcher and the patients. The exclusion criteria included the presence of systemic disease, chronic pain, neurological or psychiatric disorders, photosensitivity disorders, allergy to local anesthetics, acute pericoronitis, periodontal disease, pregnancy, breastfeeding, smoking, and the use of anti-inflammatory agents or analgesics 2 weeks before the study. The same oral surgeon performed two surgical extractions at 3-week interval for each patient [Figure 4]. The extraction sites were randomly assigned into experimental and control groups using a computer software (Random Allocation Software, Developed by M. Saghaei, MD., Department of Anesthesia, Isfahan University of Medical Sciences, Isfahan, Iran). A trained dental assistant applied GaAlAs diode laser of 810 nm and 0.1 W to the experimental sites immediately after suturing for a total of 9 J, while the contralateral extraction site served as a control receiving the same treatment except for the active laser beam [Figure 5]. Neither the surgeon nor the patients were aware of the side which received LLLT, and the records were saved by the dental assistant [Figure 6].
Figure 3.
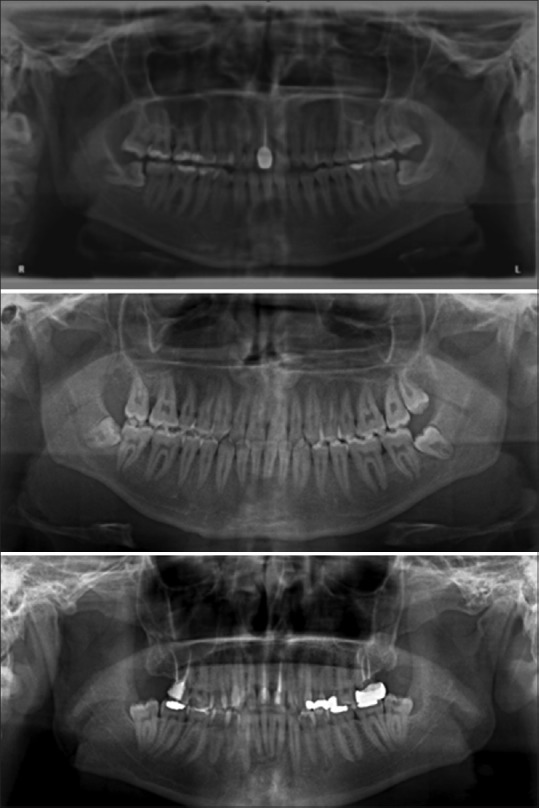
Orthopantomographs of some cases showing the bilateral symmetrical impacted mandibular third molars
Figure 4.

One oral surgeon performing the surgical extractions
Figure 5.

One dental assistant applying the laser beam
Figure 6.
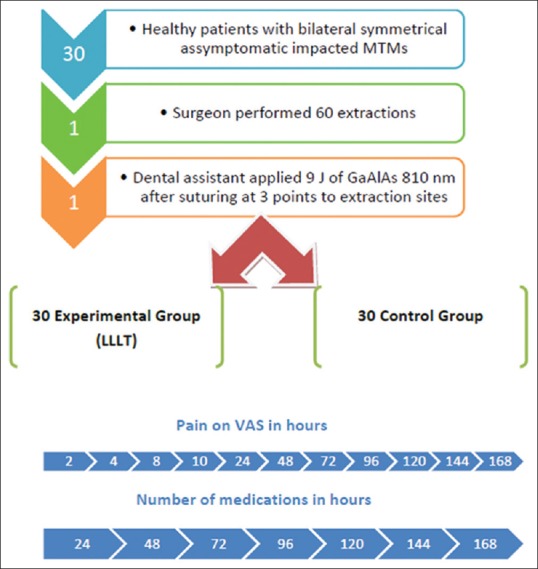
A diagram illustrating the experimental design
Experimental protocol
Preoperatively, gender and age were recorded as well as the degree of surgical extraction difficulty of impacted MTMs using the Pederson difficulty index.
Surgical protocol
Right and left MTMs surgical extractions were performed using a standardized technique. Patients received inferior alveolar, lingual, and buccal nerves blocks using two 1.8 ml carpules, each containing 2% lidocaine with epinephrine 1:80,000 (New Stetic S.A, Guarne, Colombia). A scalpal incision was made using blade number 15 (Bromed, Ontario, USA), full mucoperiosteal flap reflected with number 9 Molt Periosteal Elevator (Nordent, Illinois, USA). Buccal and distal bone was removed, as planned, with a number 8 round carbide bur (Dentsply, Ballaigues, Switzerland) attached to a low-speed surgical handpiece (NSK, Tokyo, Japan). Teeth were sectioned by a 703 fissure bur (Dentsply, Ballaigues, Switzerland) attached to the same handpiece using copious saline (0.9% sodium chloride, Jeddah, Saudi Arabia). Wound approximation was achieved using black braided nonresorbable 3/0 silk suture attached to 3/8 circle reverse cutting needle (SMI, Steinerberg, Belgium) [Figure 7]. Postoperatively, patients were prescribed oral Amoxicillin 500 mg every 8 h for 7 days and ibuprofen 400 mg taken orally every 6 h when needed.
Figure 7.

A photograph demonstrating the surgical armamentarium used in this clinical trial
Laser protocol
The GaAlAs diode laser device used (Elexxion Claros Pico, Radolfzell, Germany) and calibrated by Ophir Orion/TH with 30A-SH-V1 sensor head for validity and reliability. The device consisted of a display unit that allows for laser-specific indication selection, a foot pedal for activation control, rechargeable battery, and handpiece to which a Pico T laser applicator of 6 mm in diameter is attached for LLLT [Figure 8]. The Pico T applicator is cylindrical and has two ends, one to be applied on target tissues, while the other is fully threaded clockwise into the handpiece to deliver LLLT beam, otherwise if not completely threaded, laser beam will not emit. An active beep indicates the activation of the device, whether the Pico T is fully threaded or not [Figure 9].
Figure 8.

A photograph illustrating elexxion claros Pico laser device used. a: The display elements on the stand, b: The foot pedal for activation control, and c: The Pico T applicator fully threaded into the d: handpiece
Figure 9.

A photograph demonstrating a: the Pico T applicator unthreaded from the handpiece. b: The spot size of the Pico T applicator is 6 mm in diameter with a surface beam area of 0.28 cm2
Laser parameters
The irradiation parameters used in the study were the wavelength of 808 ± 10 nm, power of 100 mW, and pulse frequency of continuous waveform - 20,000 Hz. The spot size was 6 mm and the beam surface area was 0.28 cm2. On the other hand, the radiant exposure or fluence was 32.86 J/cm2 and the power density was 0.71 W/cm2. Furthermore, the applicator was placed at proximity to the soft tissue and applied for 30 s at three points occlusal, buccal, and lingual with the total time of 90 s and total energy of 9 J, 3 J at each point [Figure 10].
Figure 10.

Photographs of a clinical case showing the three postoperative positions of the Pico T applicator occlusal (a), buccal (b), and lingual (c) at proximity to the soft tissue after suturing
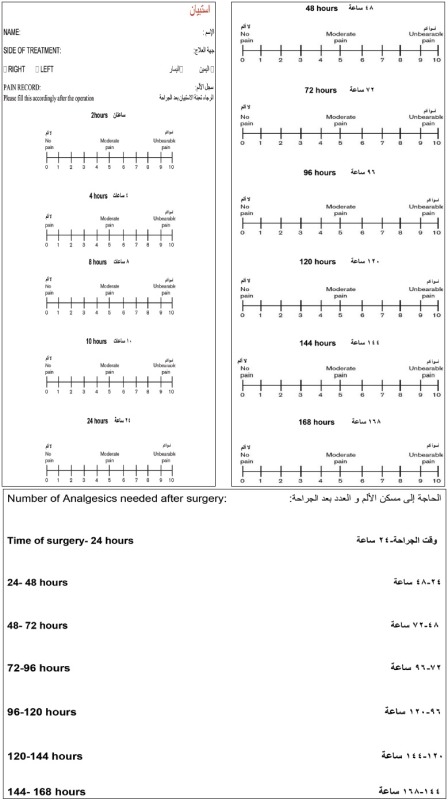
Postoperative evaluation of pain and interincisal opening
Pain intensity was recorded using a 10 cm visual analog linear scale whose scores are ranged from 0 as no pain to 10 which represents the worst possible pain [Figure 11]. Questionnaire 1 was distributed to patients who were instructed to mark the level of pain intensity postoperatively as a point on the visual analog scale at 2, 4, 8, 10 h after the surgery as well as the mornings of the first 7 successive days before taking any medication. In addition, patients were requested to record the number of analgesics taken daily. The interincisal opening was evaluated by measuring with a caliper the maximal opening between the right maxillary and right mandibular central incisors before surgery and immediately postoperatively and on the 7th day.
Figure 11.
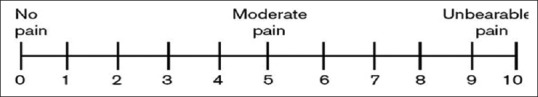
A schematic diagram shows the visual analog scale
Hypothesis and statistical analysis
The hypothesis of this clinical trial is that LLLT has an effect on postoperative pain after surgical extraction of MTMs.
Spearman's correlation is a nonparametric measure of the strength and direction of association that exists between two variables measured on at least an ordinal scale. The Mann–Whitney U-test is used to compare differences between two independent groups when the dependent variable is ordinal. Multiple regression was used to predict the value of a variable based on the value of two or more other variables. Multiple regression also allows to determine the overall fit of the model and the relative contribution of each of the predictors to the total variance explained. Paired sample t-test was used to compare two population means in the case of two samples that are correlated in case–control studies. IBM SPSS Statistics 23 for Windows (IBM Corp., United States) with a significance level of P ≤ 0.05 was used.
RESULTS
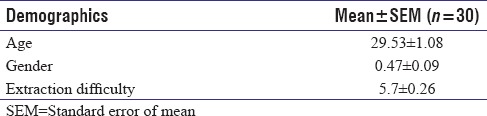
The clinical experiments were conducted from June 2016 to August 2016. Thirty patients participated in the study, 53.3% were female and 46.7% were male. The mean age of the patients included in this study was 29.5, 46.7% of the participants are at the ages of 19–29, and 53.3% of them are 30–39 years old. Moreover, the surgical difficulty scores of MTM extractions were recorded according to Pederson difficulty index. The extraction difficulty score ranges from 3 to 8 in this experimental study, and the average 5.7 indicates that surgical extractions were moderately difficult, 43.3% of the impacted third molars scored 3–5 on Pederson index and the remaining 56.7% scored 6–8 [Table 2]. The R2 (goodness of fit) and adjusted R2 figures indicate that approximately 88% of variance in pain is explained by age, gender, difficulty, and type of treatment. The F-ratio in ANOVA shows that the independent variables (age, gender, difficulty, and type of treatment) statistically significantly predict the dependent variable (pain), F (4, 55) = 100.975, P < 0.0005 (i.e., the regression model is a good fit of the data). The age of the patients has no significant effect on pain intensity levels (P > 0.05), whereas gender, surgical difficulty, and laser have significant effects on pain. Males experienced less pain intensity levels than females, in addition, the more the difficult the extraction the more the pain experienced.
Table 2.
Distribution of age, gender, and extraction difficulty
There is a significant correlation between LLLT and pain reduction, patients had less pain in the surgical sites treated with laser than the control sites. 88% of the pain scores was <1 at the laser sites, whereas 87% of the control sites scored pain from 2.29 to 6.14. Furthermore, LLLT appeared to have a high significant effect on pain reduction (P ≤ 0.05). Although there was a mild increase in pain intensity after the 4th day postoperatively [Figure 12]. The results of the study showed that on the 1st postoperative day, the average interincisal opening in the control group was 2.93 cm; in the laser group, it was 3.58 cm. On the 7th postoperative day, the average interincisal opening in the control group was 4.76 cm; in the laser group, it was 5.54 cm. Trismus in the LLLT group was significantly less than in the control group at the 1st and 7th postoperative days [Figure 13].
Figure 12.
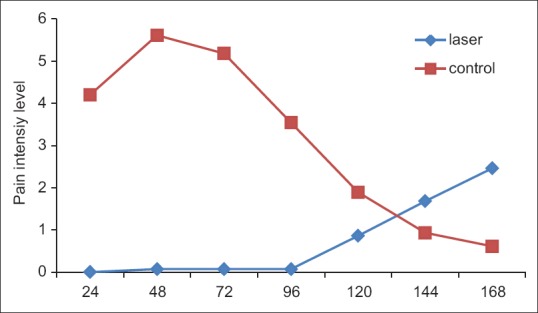
A graph illustrating the means of the pain intensity levels over time in the laser versus the control sides
Figure 13.
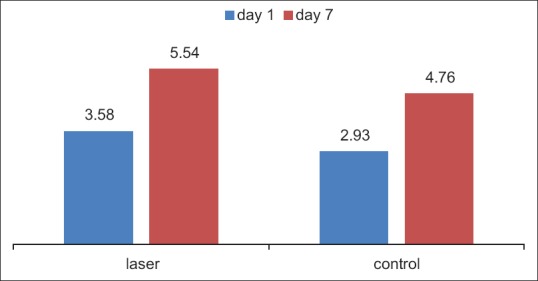
A graph showing the average difference in interincisal opening between the low-level laser therapy treated surgical sites and the control sites. It shows that the low-level laser therapy reduced trismus postoperatively
The differences in number of analgesics taken over time between the laser and the control sides using paired-samples t-test (P ≤ 0.05) demonstrated a significant difference in the number of rescue analgesics taken between both the laser and the control sides. The control sides demonstrated the peak number of analgesics taken at 48 h postoperatively with an average of 2.83 tablets and a standard error of the mean being 0.15, and then, the number of analgesics taken has gradually reduced over time. On the other hand, the laser sides did not require the intake of medications on the first 4 days postoperatively, and then interestingly, they started to take an average of one tablet afterward [Figure 14].
Figure 14.
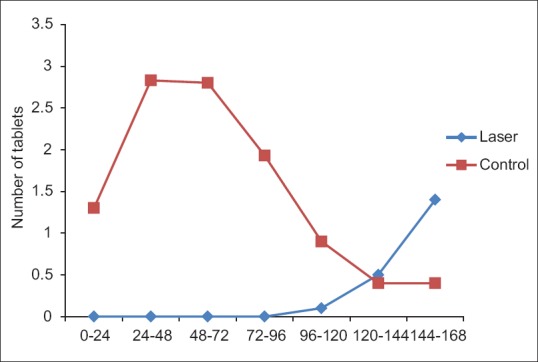
A graph illustrating the means of number of analgesics used over time in the laser versus the control sides
DISCUSSION
There is a growing interest in investigating the physiological effects of LLLT and its various clinical applications in orofacial pain, acute and chronic inflammation either as a single therapy or complementary therapy.[31,32] However, the lack of quality publications on the analgesic and anti-inflammatory effects of LLLT after the surgical removal of third molars, together with the obtained controversial results, calls into question its efficacy. So far, the parameters of ideal radiation for this purpose have not been determined due to the great diversity of variables such as the type of laser wavelength, power, pulse rate, time, and mode of application.[3,4,6,7,11,22,23,24,25,26,27,28,29,30] A local inflammation of a surgical wound does not take place immediately after surgery, but it appears gradually and reaches its peak between 24 and 48 h after the surgery.[3,33] Pain intensity and degree of inflammation can vary between patients. For this reason, the split-mouth design where the patient becomes his/her own control is able to avoid bias in the data collection. Moreover, a 3-week interval is allowed in between both extractions to allow for wound healing and to avoid the presence of any systemic effect of one side on the other.[18] In addition, one treatment of acute injuries or immediately postoperatively has clinically meaningful effects. Whereas for chronic pathologies, LLLT typically requires two or three treatments a week for several weeks to achieve clinical significance.[18,19,34] According to the results of our study, the clinical parameter of pain was reported by patients to be less at the sites treated with laser therapy than at the other control sites. This effect is in agreement with results of another study in which 10 patients treated with 904 nm GaAs laser applied immediately after the surgery and on days 3 and 5 postoperatively, with a total fluence of 180 J/cm2.[22]
In contrast, other split-mouth studies reported no significant reduction in pain using intraoral 830 nm GaAlAs once immediately after suturing as well as when applied more the one time.[6,11,29] Furthermore, a clinical trial demonstrated lower intensity of postoperative pain, swelling, and trismus in the laser treated group than in the control group, but the difference was not reported to be statistically significant, whereas there was a significant reduction in the number of rescue analgesic medications required in agreement with the results of this study.[3] However, in 2006, Markovic and Todorovic obtained a reduction of postoperative pain by applying the laser AsGaAl after the surgical removal of third molars.
This study was conducted with third molars in symmetrical positions with a similar degree of difficulty, so that each patient was his own control. Furthermore, a single surgeon performed all surgical procedures to avoid differences among different surgeon's skills, which might have influenced the results. A similar double-blind crossover study included 25 patients with bilateral identical impactions reported no significant effect of applying 6 J LLLT on postoperative pain and swelling except on the 2nd day.[23]
The HeNe laser was also used to investigate the effects of the LLLT in reducing pain, postoperative swelling, and trismus after a third molar extraction. There were no significant differences in the levels of pain and swelling between the laser group and control group. However, this laser allowed a significant reduction of trismus after 7 days in both groups.[28] The laser application following third molar extraction can be intraorally, extraorally, or both. In this study, the intraoral application was adopted to allow for maximum penetration and absorption at the surgical site 4–6 mm.[15,18,35]
Several studies reported the use of intraoral soft laser once immediately after third molar extraction at 1 cm distance from the surgical site and found a significant reduction in pain in agreement with this study.[7,8,9] On the other hand, the extra- and intra-oral application of GaAlAs demonstrated a significant reduction in swelling and pain after 24 h postoperatively following orthognathic surgery,[25] and in another study, the extra- and intra-oral application was used to verify the effectiveness of LLLT in improving sensory function after sagittal split osteotomy and resulted in a significant improvement in subjective sensory assessment.[24] In contrast, other studies reported no significant effects.[4,30]
Studies that have accurately measured beam irradiance and taken measurements at the target depth report successful tissue repair and anti-inflammatory effects in the range of 5–55 mW/cm2 at the target site. However, analgesia typically requires higher power densities, a systematic review of laboratory studies found power densities >300 mW/cm2 are necessary to inhibit nerve conduction in C-fibers and A-delta fibers. Therefore, the power density of 0.71 W/cm2 was used in this study.[18,35]
Pain reduction in acute conditions is achieved through inhibition of neural flow and high fluence, and greater power density is more effective. The fluence used in the study was 32.86 J/cm2. Wound healing and tissue regeneration require fairly low intensity and long time 2–6 J/cm2; reduction of inflammation is more effective with higher fluence 6–10 J/cm2, whereas acute pain may require 20–50 J/cm2.[18,35]
The age of the patients had no influence on the level of pain experienced in this clinical trial; nevertheless, a prospective study reported that older patients are at greater risk of postoperative complications and permanent sequelae.[36] It is believed that with an increasing age, bone become harder and brittle resulting in more pain, trismus, and swelling.[37]
Females were reported to have more pain intensity levels postsurgically than males as well as the more the surgical difficulty the more the pain experienced.[5,36,37,38,39]
On the other hand, the laser sides experienced no pain on the first 4 days postoperatively, and then interestingly, they started to experience mild pain afterward. A similar split-mouth study reported reduction in postoperative pain when 5 J/cm2 is used; but after the 4th day, the laser-treated sites experience more pain levels than the control sites.[6] This interesting finding can be due to a high dose of laser power density lead to delayed wound healing, and this can be managed by increasing the distance between the laser tip and the target tissue or by reducing the exposure time. Furthermore, the increase in pain might be due to a secondary infection, or because the laser effect wears off after 3 to 4 days and an additional application is required.[18,19,34]
CONCLUSION
The use of intraoral GaAlAs of 810 nm and 0.1 W is effective in reducing postoperative pain when a dose of 32.86 J/cm2 is used and less pain medications were required. Furthermore, there is no effect of age on the postoperative pain experienced; however, gender has an effect, females experience more pain than males. On the other hand, the more the difficult the surgical extraction the more the postoperative pain experienced.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
QUESTIONNAIRE
REFERENCES
- 1.Brignardello-Petersen R, Carrasco-Labra A, Araya I, Yanine N, Beyene J, Shah PS, et al. Is adjuvant laser therapy effective for preventing pain, swelling, and trismus after surgical removal of impacted mandibular third molars? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2012;70:1789–801. doi: 10.1016/j.joms.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 2.He WL, Yu FY, Li CJ, Pan J, Zhuang R, Duan PJ, et al. Asystematic review and meta-analysis on the efficacy of low-level laser therapy in the management of complication after mandibular third molar surgery. Lasers Med Sci. 2015;30:1779–88. doi: 10.1007/s10103-014-1634-0. [DOI] [PubMed] [Google Scholar]
- 3.Amarillas-Escobar ED, Toranzo-Fernández JM, Martínez-Rider R, Noyola-Frías MA, Hidalgo-Hurtado JA, Serna VM, et al. Use of therapeutic laser after surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2010;68:319–24. doi: 10.1016/j.joms.2009.07.037. [DOI] [PubMed] [Google Scholar]
- 4.Ferrante M, Petrini M, Trentini P, Perfetti G, Spoto G. Effect of low-level laser therapy after extraction of impacted lower third molars. Lasers Med Sci. 2013;28:845–9. doi: 10.1007/s10103-012-1174-4. [DOI] [PubMed] [Google Scholar]
- 5.Osunde OD, Saheeb BD. Effect of age, sex and level of surgical difficulty on inflammatory complications after third molar surgery. J Maxillofac Oral Surg. 2015;14:7–12. doi: 10.1007/s12663-013-0586-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.López-Ramírez M, Vílchez-Pérez MA, Gargallo-Albiol J, Arnabat-Domínguez J, Gay-Escoda C. Efficacy of low-level laser therapy in the management of pain, facial swelling, and postoperative trismus after a lower third molar extraction. A preliminary study. Lasers Med Sci. 2012;27:559–66. doi: 10.1007/s10103-011-0936-8. [DOI] [PubMed] [Google Scholar]
- 7.Rana M, Gellrich NC, Ghassemi A, Gerressen M, Riediger D, Modabber A, et al. Three-dimensional evaluation of postoperative swelling after third molar surgery using 2 different cooling therapy methods: A randomized observer-blind prospective study. J Oral Maxillofac Surg. 2011;69:2092–8. doi: 10.1016/j.joms.2010.12.038. [DOI] [PubMed] [Google Scholar]
- 8.Batinjan G, Zore Z, Čelebić A, Papić M, Gabrić Pandurić D, Filipović Zore I, et al. Thermographic monitoring of wound healing and oral health-related quality of life in patients treated with laser (aPDT) after impacted mandibular third molar removal. Int J Oral Maxillofac Surg. 2014;43:1503–8. doi: 10.1016/j.ijom.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Abou El-Soud N, El Shenawy H. A randomized double blind clinical study on the efficacy of low level laser therapy in reducing pain after simple third molar extraction. Maced J Med Sci. 2010;3:303–6. [Google Scholar]
- 10.El Shenawy H, Aboelsoud N, Zaki A, El Zawahry M, Shaibeta A. Postoperative pain control in patients after lower third molar extraction. J Am Sci. 2010;6:1068–72. [Google Scholar]
- 11.Fernando S, Hill CM, Walker R. A randomised double blind comparative study of low level laser therapy following surgical extraction of lower third molar teeth. Br J Oral Maxillofac Surg. 1993;31:170–2. doi: 10.1016/0266-4356(93)90118-g. [DOI] [PubMed] [Google Scholar]
- 12.Oliveira Sierra S, Melo Deana A, Mesquita Ferrari RA, Maia Albarello P, Bussadori SK, Santos Fernandes KP, et al. Effect of low-level laser therapy on the post-surgical inflammatory process after third molar removal: Study protocol for a double-blind randomized controlled trial. Trials. 2013;14:373. doi: 10.1186/1745-6215-14-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh LJ. The current status of low level laser therapy in dentistry. Part 1. Soft tissue applications. Aust Dent J. 1997;42:247–54. doi: 10.1111/j.1834-7819.1997.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 14.Mester E, Spiry T, Szende B, Tota JG. Effect of laser rays on wound healing. Am J Surg. 1971;122:532–5. doi: 10.1016/0002-9610(71)90482-x. [DOI] [PubMed] [Google Scholar]
- 15.Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, et al. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. 2015;68:217–69. doi: 10.1111/prd.12080. [DOI] [PubMed] [Google Scholar]
- 16.Moore K, Hira N, Kumar P, Jayakumar C, Ohshiro T. A double blind crossover trial of low level laser therapy in the treatment of post herpetic neuralgia. Laser Ther. 1989;2:7–9. [Google Scholar]
- 17.Albertini R, Villaverde AB, Aimbire F, Salgado MA, Bjordal JM, Alves LP, et al. Anti-inflammatory effects of low-level laser therapy (LLLT) with two different red wavelengths (660 nm and 684 nm) in carrageenan-induced rat paw edema. J Photochem Photobiol B. 2007;89:50–5. doi: 10.1016/j.jphotobiol.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Carroll JD, Milward MR, Cooper PR, Hadis M, Palin WM. Developments in low level light therapy (LLLT) for dentistry. Dent Mater. 2014;30:465–75. doi: 10.1016/j.dental.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Parker S. Verifiable CPD paper: Introduction, history of lasers and laser light production. Br Dent J. 2007;202:21–31. doi: 10.1038/bdj.2006.113. [DOI] [PubMed] [Google Scholar]
- 20.Raman A, Srividhya S, Kumar M, Laxman A, Kumar M, Kailasam S. Low level laser therapy: A concise review on its applications. J Indian Acad Oral Med Radiol. 2013;25:291–3. [Google Scholar]
- 21.Fabre HS, Navarro RL, Oltramari-Navarro PV, Oliveira RF, Pires-Oliveira DA, Andraus RA, et al. Anti-inflammatory and analgesic effects of low-level laser therapy on the postoperative healing process. J Phys Ther Sci. 2015;27:1645–8. doi: 10.1589/jpts.27.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mozzati M, Martinasso G, Cocero N, Pol R, Maggiora M, Muzio G, et al. Influence of superpulsed laser therapy on healing processes following tooth extraction. Photomed Laser Surg. 2011;29:565–71. doi: 10.1089/pho.2010.2921. [DOI] [PubMed] [Google Scholar]
- 23.Røynesdal AK, Björnland T, Barkvoll P, Haanaes HR. The effect of soft-laser application on postoperative pain and swelling. A double-blind, crossover study. Int J Oral Maxillofac Surg. 1993;22:242–5. doi: 10.1016/s0901-5027(05)80646-0. [DOI] [PubMed] [Google Scholar]
- 24.Khullar SM, Emami B, Westermark A, Haanaes HR. Effect of low-level laser treatment on neurosensory deficits subsequent to sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:132–8. doi: 10.1016/s1079-2104(96)80215-0. [DOI] [PubMed] [Google Scholar]
- 25.Gasperini G, Rodrigues de Siqueira IC, Rezende Costa L. Does low-level laser therapy decrease swelling and pain resulting from orthognathic surgery? Int J Oral Maxillofac Surg. 2014;43:868–73. doi: 10.1016/j.ijom.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 26.Markovic AB, Todorovic L. Postoperative analgesia after lower third molar surgery: Contribution of the use of long-acting local anesthetics, low-power laser, and diclofenac. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e4–8. doi: 10.1016/j.tripleo.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 27.Boras V, Richter I, Zorat N, Juras D, Barilo V, Rogulj A. Use of low level laser therapy in the treatment of persistent idiopathic orofacial pain and traumatic trigeminal neuropathy - A pilot study. J Regen Med Tissue Eng. 2013;2:5. [Google Scholar]
- 28.Carrillo JS, Calatayud J, Manso FJ, Barberia E, Martinez JM, Donado M, et al. A randomized double-blind clinical trial on the effectiveness of helium-neon laser in the prevention of pain, swelling and trismus after removal of impacted third molars. Int Dent J. 1990;40:31–6. [PubMed] [Google Scholar]
- 29.Paschoal MA, Santos-Pinto L. Therapeutic effects of low-level laser therapy after premolar extraction in adolescents: A randomized double-blind clinical trial. Photomed Laser Surg. 2012;30:559–64. doi: 10.1089/pho.2012.3243. [DOI] [PubMed] [Google Scholar]
- 30.Raouâa B, Samèh S, Nour BM, Abdellatif C, Jamil S. Effects of low-level-laser therapy versus corticotherapy on pain, trismus and edema after surgical removal of third mandibular molars: A comparative study. Family Med Med Sci Res. 2013;2:1–4. [Google Scholar]
- 31.Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49:107–16. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 32.Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA. Low-level laser therapy in acute pain: A systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg. 2006;24:158–68. doi: 10.1089/pho.2006.24.158. [DOI] [PubMed] [Google Scholar]
- 33.Farina R, Trombelli L. Wound healing of extraction sockets. Endod Topics. 2012;25:16–34. [Google Scholar]
- 34.Goyal M, Makkar S, Pasricha S. Low level laser therapy in dentistry. Int J Lasers Dent. 2013;3:82–8. [Google Scholar]
- 35.Pirnat S. Versatility of an 810 nm diode laser in dentistry: An overview. J Laser Health Acad. 2007;4:1–9. [Google Scholar]
- 36.Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: Postoperative complications and their risk factors. J Can Dent Assoc. 2007;73:325. [PubMed] [Google Scholar]
- 37.Osunde O, Saheeb B, Bassey G. Indications and risk factors for complications of lower third molar surgery in a Nigerian teaching hospital. Ann Med Health Sci Res. 2014;4:938–42. doi: 10.4103/2141-9248.144919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bali A, Bali D, Sharma A, Verma G. Is Pederson index a true predictive difficulty index for impacted mandibular third molar surgery? A meta-analysis. J Maxillofac Oral Surg. 2013;12:359–64. doi: 10.1007/s12663-012-0435-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Juodzbalys G, Daugela P. Mandibular third molar impaction: Review of literature anda proposal of a classification. J Oral Maxillofac Res. 2013;4:e1. doi: 10.5037/jomr.2013.4201. [DOI] [PMC free article] [PubMed] [Google Scholar]


