Abstract
An infrequently studied question is how diverse combinations of built environment (BE) features relate to physical activity (PA) for older adults. We derived patterns of Geographical Information Systems- (GIS) measured BE features and explored how they accounted for differences in objective and self-reported PA, sedentary time, and BMI in a sample of older adults. Senior Neighborhood Quality of Life Study participants (N=714, aged 66–97 years, 52.1% women, 29.7% racial/ethnic minority) were sampled in 2005–2008 from the Seattle-King County, WA and Baltimore, MD-Washington, DC regions. Participants’ home addresses were geocoded, and net residential density, land use mix, retail floor area ratio, intersection density, public transit density, and public park and private recreation facility density measures for 1-km network buffers were derived. Latent profile analyses (LPAs) were estimated from these GIS-based measures. In multilevel regression models, profiles were compared on accelerometer-measured moderate-to-vigorous PA (MVPA) and sedentary time and self-reported PA, adjusting for covariates and clustering. Analyses were conducted in 2014–2015. LPAs yielded three profiles: low walkability/transit/recreation (L-L-L); mean walkability/transit/recreation (M-M-M); and high walkability/transit/recreation (H-H-H). Three PA outcomes were more favorable in the HHH than the LLL profile group (difference of 7.2 minutes/day for MVPA, 97.8 minutes/week for walking for errands, and 79.2 minutes/week for walking for exercise; all ps < 0.02). The most and least activity-supportive BE profiles showed greater differences in older adults’ PA than did groupings based solely on a 4-component walkability index, suggesting that diverse BE features are important for healthy aging.
Keywords: built environment, environment design, aging in place, obesity, active transportation, exercise
INTRODUCTION
Adults over 65 years of age represent a large (14%) and rapidly increasing proportion of the US population, growing by almost 25% since 20031. As for younger and middle-aged adults, regular physical activity (PA) and moderate-to-vigorous PA (MVPA) are important for improving cardiovascular fitness and as predictors of physiological risk factors (e.g., cardiovascular functioning, bone density, body mass index [BMI]) 2–4, morbidity (e.g., 5–9), and mortality (e.g., 10–12) in older adults. Aerobic PA guidelines for healthy older adults recommend ≥150-minutes per week of moderate or ≥75 minutes of vigorous PA, or an equivalent combination to prevent morbidities and reduce mortality related to cardiovascular disease, stroke, and metabolic dysregulation. 13,14 Despite these long-standing recommendations, national studies have estimated that few (< 9%) adults aged 60 and older meet them.15,16
Increasingly, research has linked built environment (BE) features to PA among adults in general (e.g., 17–21), and older adults specifically (e.g., 22–26). Indicators of greater neighborhood walkability (e.g., proximity to destinations, walkability index) have been linked to higher levels of overall PA and active transportation in older adults. 25–27 Other BE features, such as access to public transit access and recreation facilities may also contribute positively to the likelihood of engaging in active transportation and other PA among all adults (e.g., 22,28–32) including older adults (e.g., 27,33,34), suggesting these features may also be important aspects of the activity-supportiveness of neighborhoods.
Typically, examinations of associations between BE features and PA in older adults have focused either on only one feature or quantitative indicator (e.g., parks35 or pedestrian connectivity27) or the unique contribution of each feature after adjusting for the presence or level of other features (e.g., 33,36). These approaches, respectively, can yield relatively straightforward models that may fail to capture BE complexity or complex multivariable models that do not necessarily illustrate which patterns of features are relatively more supportive of PA. Clustering methods can reduce model complexity while using information from several BE indicators, but some methods present limitations. Conventional principal components analysis identifies groups of similar (correlated) indicators, rather than groups of similar observations. Traditional cluster analysis methods identify groups of similar observations, but place constraints on indicator scaling and don’t afford straightforward statistical comparisons among models. Supervised machine learning methods (e.g., support vector machines) can find groups of similar observations and allow for statistical comparisons, but they depend on the use of “training” sets of observations that have a priori known class memberships. Latent profile analysis (LPA) addresses these limitations by yielding a discrete set of model-derived clusters of observations with distinctive patterns (profiles) of indicator (BE feature) scores in each model and allows for statistical comparison of models of differing complexity. Feature patterns derived from LPA models using perceived (vs. GIS-measured) BE features have shown predictive utility for MVPA and transportation-related physical activity for younger and older adults22,37 and children38, and with GIS-measured features for adults aged 20–65. 39 Identifying feature patterns from objective measures conceptually associated with regular PA in adults over age 65 may help inform neighborhood designs that allow older adults remain relatively active and healthy.
The first major goal of the current study was to derive empirically defined latent profiles of seven GIS-measured BE features using pooled data from a sample of older adults residing in two U.S. metropolitan regions. The second major goal was to examine how neighborhood profiles were related to objectively measured MVPA (measuring total PA volume and intensity) and self-reported PA (measuring specific types of PA engaged in, e.g., walking for errands), objectively measured sedentary time, and BMI, which is related to both MVPA and overall health in older adults. We hypothesized that participants residing in neighborhoods characterized by an overall PA-supportive profile, compared to other profiles, would show higher PA, and lower sedentary time and BMI.
METHODS
This analysis used data from the Senior Neighborhood Quality of Life Study (SNQLS), an observational study examining relations between block group-level walkability and multiple health-related outcomes, including PA and BMI in adults over 65 years old. Detailed descriptions of the SNQLS study can be found elsewhere (e.g., 27). Briefly, Census block groups in metropolitan Seattle-King County, WA and Baltimore, MD-Washington DC regions were screened for the study based on the BE construct of walkability, with walkability defined by block-group-level net residential density, land use mix, street connectivity and retail floor area ratio40. Block groups were ranked based on potentially available participants, and then categorized based on region-specific median splits for walkability and Census-based median household income, which were then crossed yielding a 2 (lower walkability vs. higher walkability) x 2 (lower income vs. higher income) matrix of sampling strata or quadrants. A minimum of 13 block groups within each sampling quadrant were identified and participants were subsequently selected from these block groups. Participants (n = 714, 66–97 years old, 53.1% female, 29.3% ethnic minority), from whom informed consent was obtained, were systematically sampled and recruited across all 4 quadrants simultaneously over 12 months to prevent seasonal bias. At each of two time points six months apart, participants wore accelerometers over a 7-day period and completed questionnaires measuring socio-demographics and self-reported PA; data from the first time point were used here.
Neighborhood Environment Measures
For the current analysis, BE features were measured for the geographic area around each participant’s home, as residence-based measures may be more important than those for the BE of a person’s home block group. 40 Using geographic information systems (GIS) methods and software (ArcGIS 10.0; ESRI; Redlands, CA), the location of each participant’s residence was geocoded and a 1-km street-network buffer was computed around that location. Next, as described below, seven different BE features were quantified for each participant’s residence using this buffer.
Walkability Components
Neighborhood walkability comprises components representing pedestrian accessibility of destinations near the home. 40 The components are as follows: (1) net residential density—the ratio of residential dwelling units to land area devoted to residential land use within a buffer; (2) intersection density —the number of intersections with three or more legs divided by the total land area of the buffer—higher intersection density corresponds to shorter, more direct paths between destinations; (3) land use mix or the diversity and evenness of nearby and accessible destinations present in a buffer across five land use types (residential, retail/commercial, entertainment, food-related, and civic/institutional)—with normalized values ranging from 0 (indicating a single land use, most likely residential) to 1 (indicating an even distribution, i.e., 20% of parcel areas dedicated to each of 5 use types); and (4) retail floor area ratio (RFAR)—the ratio of retail building floor areas divided by retail parcel land areas—low RFAR indicates retail development likely to have substantial space devoted to parking, while high RFAR indicates smaller building setbacks typical of pedestrian-oriented designs. Individual walkability components were included in the latent profile analyses rather than a single walkability index score computed from the four components.
Public Transportation
Spatial datasets of transit stops and stations were obtained from regional repositories. Because the majority of participants did not have access to rail stops/stations, buffer-level bus and rail counts were combined to yield a single variable for total public transit density within each participant’s buffer defined as the number of stops/stations divided by the area of the buffer.
Recreation Environment
Using information collected from park departments, parcel data, and the Yellow Pages, SNQLS investigators enumerated recreation facilities after conducting a comprehensive assessment of parks, fitness centers, community recreation centers, swimming pools, yoga, and ballroom dance studios, among others, in each region. Parks were defined as freely accessible, improved and unimproved green spaces designated as parks by the above data sources. Private recreation facilities included places where physical activity could occur and required payment (e.g., golf courses, fitness facilities). Separate park density and recreation facility density variables were operationalized, respectively, as the number of park locations and number of private recreation locations divided by the area of the participant’s buffer.
Physical Activity, Sedentary, and Demographic Measures
Objectively-measured PA
Participants wore ActiGraph accelerometers (Pensacola, FL; models 7164 or 71256) on their right hip using an elastic belt during waking hours for 7 days to measure MVPA. Participants were asked to re-wear the accelerometer if < 5 valid days or < 66 valid hours across 7 days were obtained. Accelerometer data were scored using MeterPlus version 4.0 software (Santech, Inc.). For scoring MVPA, a ‘valid day’ was defined as ≥ 10 valid hours of wear, and a valid hour was < 30 consecutive zero values. The difference in the number of consecutive zeros used to define a valid hour affects the estimates of non-wear time and sedentary time most. A lower threshold used to define valid hour (i.e., fewer consecutive zeros) results in more non-wear time and less sedentary time daily. On valid days, we summed each minute < 100 counts/minute (cpm) to compute total sedentary minutes and the duration of moderate-to-vigorous intensity minutes was based on the Freedson cut-point for adults (≥1952 cpm). 41 We also examined “low light” intensity PA (100–1040 cpm) and “high light” intensity PA (1041–1951 cpm) 42. The average minutes of moderate-to-vigorous activity, low light, high light, and sedentary time per valid wearing day were examined independently in analyses. We also examined whether participants attained greater than 30 minutes per day on average, which approximates the 150 minutes per week guideline. ActiGraph accelerometers have produced reliable and valid estimates of sedentary time and PA in adults when compared to indirect calorimetry.43
Self-reported PA
Participants completed the Community Healthy Activities Model Program for Seniors (CHAMPS) physical activity questionnaire for older adults44, which assessed their usual amounts of various physical activities over the past 4 weeks. The CHAMPS asks participants to report the number of times per week they usually engage in a particular activity and the duration spent in each activity. Duration items have 6 response options ranging from less than 1 hr/week to 9 or more hr/week. The midpoint of each response option (e.g., 1–2.5 hr/week = 105 min) was used as the estimate of time spent in the activity. Time spent walking for errands was measured using a single item from the CHAMPS (walk to do errands), and walking for exercise was measured using the sum of three CHAMPS items (walk your dog, walk fast or briskly for exercise, walk uphill or hike uphill). The CHAMPS has shown good reliability (6-month stabilities [ICCs] = 0.58–0.67) and validity.40
Demographics
Participants reported demographic and personal characteristics including sex, age (years), race/ethnicity (non-Hispanic white versus non-white and/or Hispanic), annual household income (eleven levels from <$10,000 to >$100,000 USD), educational attainment (seven levels from 7th grade to completed graduate degree), number of motor vehicles divided by eligible drivers in household (continuous), marital or cohabitation status (married or living together versus other), number of people in household (continuous), and years at current address (continuous).
Analytic Approach
First we conducted a latent profile analysis (LPA) with seven BE feature indicators using Mplus 7.22. 45 LPA derives mutually exclusive profiles of observations (i.e., patterns) that maximize between-profile variance and minimize within-profile variance across the set of continuous indicators. Adjustment for non-independence was made via the Mplus TYPE=COMPLEX specification, with block groups specified as clusters (i.e., higher-level sampling units). LPA models were estimated using a dataset (n = 714) based on participants from both regions (Seattle/King County: n = 364; Baltimore/Washington, DC: n = 350). We derived solutions (models) ranging from 1 to 4 profiles. Selection of the final solution was based on consideration of model fit indices, subjective interpretability of the derived profiles, and within-profile sample sizes. Relative model fit and quality was judged using sample size-adjusted Bayesian Information Criterion (BIC) and model log likelihood values. Upon selection of the appropriate LPA solution, each respondent was assigned to the profile for which his/her analytically derived probability of membership was highest.
Next, we used generalized linear mixed models in SAS 9.4 to examine relations between final BE profiles (i.e., profile membership) and log-transformed accelerometer-measured MVPA, low light and high light PA, and sedentary time, self-reported walking for errands and walking for exercise, BMI (in PROC MIXED), and a dichotomous indicator of having met MVPA recommendations (< 150 min/week MVPA vs. ≥ 150 min/week MVPA; in PROC GLIMMIX). Respondents were treated as being nested within block groups, and block group-level intercepts were modeled as random effects. All regression models adjusted for sex, age, annual household income, education, race/ethnicity, motor vehicles divided by adults in household, marital status, number of people in household, and years at current address. In models using accelerometer-measured outcomes, we also adjusted for total hours of accelerometer wear time on all valid wear days. We present anti-logged model-adjusted means and standard error bars from analyses of log-transformed measures.
RESULTS
Table 1 presents descriptive statistics on participant demographic and personal characteristics, physical activity and sedentary times, and neighborhood environment factors
Table 1.
Percentages, Means, and Standard Deviations for Sample Characteristics for Older Adults from the Seattle-King County, WA and Baltimore, MD-Washington, DC Regions 2005–2008
| Variable | Percent | M | SD |
|---|---|---|---|
| Participant background characteristics | |||
| Age (in years) | 74.5 | 6.3 | |
| % Female | 52.1 | ||
| % Non-Hispanic White | 70.3 | ||
| Highest education level | |||
| Less than high school diploma/GED | 5.5 | ||
| Completed high school | 15.6 | ||
| Some college or vocational training | 29.8 | ||
| Completed college or university | 26.1 | ||
| Completed graduate degree | 23.1 | ||
| % Married or cohabiting | 56.8 | ||
| Annual income (in $1000) | 40–49a | 20–29, 70–79b | |
| Vehicles per adults in household | 0.9 | 0.4 | |
| Number of people in household | 1.8 | 0.8 | |
| Time at current residence (in years) | 24.8 | 15.5 | |
| BMI | 26.5 | 4.8 | |
| Accelerometer measures | |||
| Sedentary time (minutes/day) | 561.4 | 100.8 | |
| Low light PA (minutes/day) | 222.4 | 68.1 | |
| High light PA (minutes/day) | 29.8 | 21.5 | |
| MVPA (minutes/day) | 13.6 | 16.8 | |
| CHAMPS-based measuresc | |||
| Walking for errands (hours/week) | 0.6 | 1.3 | |
| Walking for exercise (hours/week) | 3.4 | 4.1 | |
| GIS-measured BE features | |||
| Residential density | 7.4 | 6.0 | |
| Intersection density | 63.1 | 23.0 | |
| Land use mix | 0.2 | 0.3 | |
| Retail floor area ratio | 0.2 | 0.2 | |
| Transit stop density | 15.6 | 10.6 | |
| Park density | 2.4 | 2.1 | |
| Recreation facility density | 3.4 | 4.9 | |
Notes.
Median response.
25th and 75th percentiles.
CHAMPS—Community Healthy Activities Model Program for Seniors questionnaire
Latent Profile Analyses
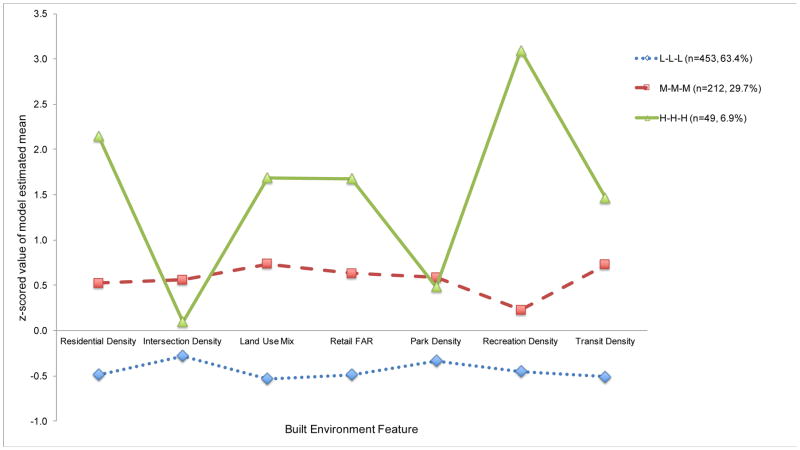
Model fit indices (i.e., BIC, log likelihood) indicated that a 4-profile solution (BIC = 20990.431, log likelihood = −10430.699) was better than a 3-profile solution (BIC = 21449.86, log likelihood = −10673.993); however, the 4-profile solution could not be clearly interpreted, so the 3-profile solution was selected. Figure 1 shows the patterns of standardized LPA-estimated profile-specific indicator means (Z-scores standardized with respect to the observed sample means and standard deviations) for the 3-profile solution.
Figure 1.
Patterns of latent profile analysis-estimated indicators means from 3-profile solution for older adults sampled from the Seattle-King County, WA and Baltimore, MD-Washington, DC regions 2005–2008. A z-score of +1.0 reflects an estimated mean that is 1 SD above the observed sample mean for that indicator. L-L-L = low walkability, low transit access, and low recreation access; M-M-M, medium levels of walkability, transit access, and recreation access; H-H-H, high levels of walkability, transit access, and recreation access.
In the 3-profile solution, the most common profile was labeled “low walkable, low transit access, low recreation access” (L-L-L) and comprised 63.4% (n = 453) of the participants. This profile was characterized by a combination of low values for residential density, land use mix, intersection density, with relatively low values on public transit access, and limited access to parks and private recreational facilities. The next most common profile was labeled “moderately-high walkability, moderately-high transit access, and moderately-high recreation access” (MH-MH-MH) and comprised 29.7% (n = 212) of participants. This profile was characterized by above average values (i.e., Z-scores of approximately 0.5) for all environmental indicators. The third most common profile was labeled “high walkable, high transit access, high recreation access” (H-H-H) and comprised 6.9% (n = 49) of participants. H-H-H was characterized by high Z-score values for residential density, land use mix, retail FAR, recreation density, and transit density.
Between-profile Differences in PA, Sedentary Time, and BMI
Accelerometer-measured PA and Sedentary Time
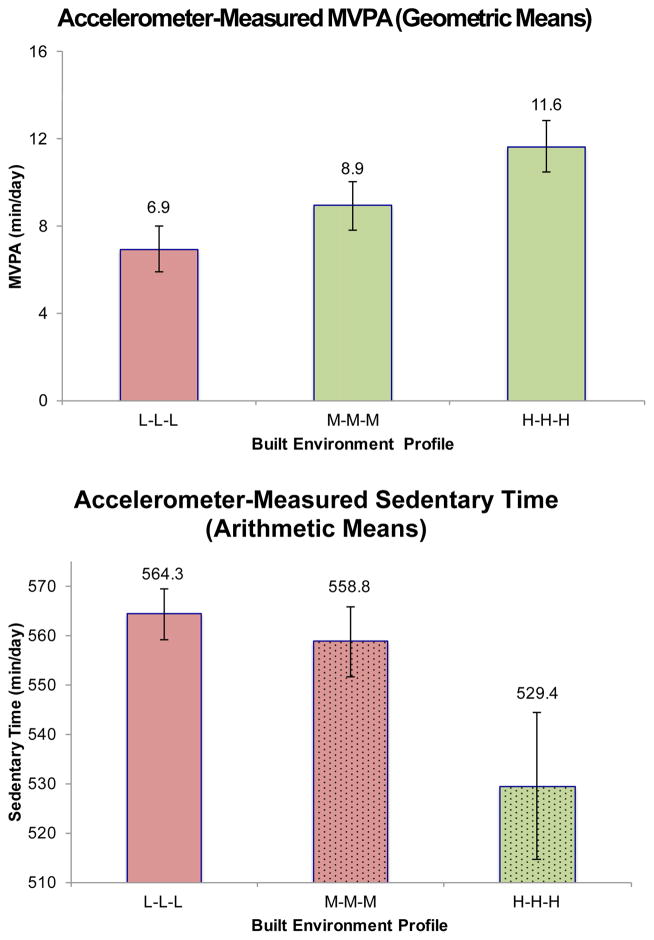
Figure 2 presents model-adjusted geometric means and standard errors for accelerometer-measured MVPA and arithmetic means and standard errors for sedentary behavior across latent profiles, along with results of pairwise between-profile comparisons of means from the linear mixed model analyses. Tests of overall between-profile differences were significant for MVPA minutes per day (p = .008). Participants in the L-L-L profile had an adjusted geometric mean of 6.9 MVPA min/day (adjusted raw score M = 11.6 min/day) which significantly differed from 8.9 MVPA min/day (adjusted raw M = 15.0 min/day) in the M-M-M profile and 11.6 min/day (adjusted raw M = 18.8 min/day) in H-H-H profile, p = .013 and p = .006, respectively. Participants in the M-M-M and H-H-H profiles did not differ significantly from each other (p = .167). Sedentary time differed significantly between the L-L-L and H-H-H profiles (adjusted raw M = 564.3 min/day vs. 529.4 min/day, p = .027); however, sedentary time for the M-M-M profile (adjusted raw M = 558.8 min/day) did not differ significantly from that for either the L-L-L profile (p = .511) or the H-H-H profile (p = .072). No significant between-profile differences were found for proportion of participants meeting MVPA recommendations (≥ 150 MVPA min/week). We also explored between-profile differences in “low light” intensity PA and “high light” intensity PA. None of these differences were statistically significant.
Figure 2.
Adjusted geometric means for accelerometer-derived MVPA and adjusted arithmetic means for sedentary time by latent profile for older adults sampled from the Seattle-King County, WA and Baltimore, MD-Washington, DC regions 2005–2008. MVPA and sedentary minutes per day values were adjusted for accelerometer wear time, sex, age, race/ethnicity, annual household income, educational attainment, number of motor vehicles and eligible drivers in household, marital or cohabitation status, number of people in household, and years at current address. Within each panel, non-significant comparisons are reflected across profiles by bars with matching colors or matching patterns.
Self-reported PA
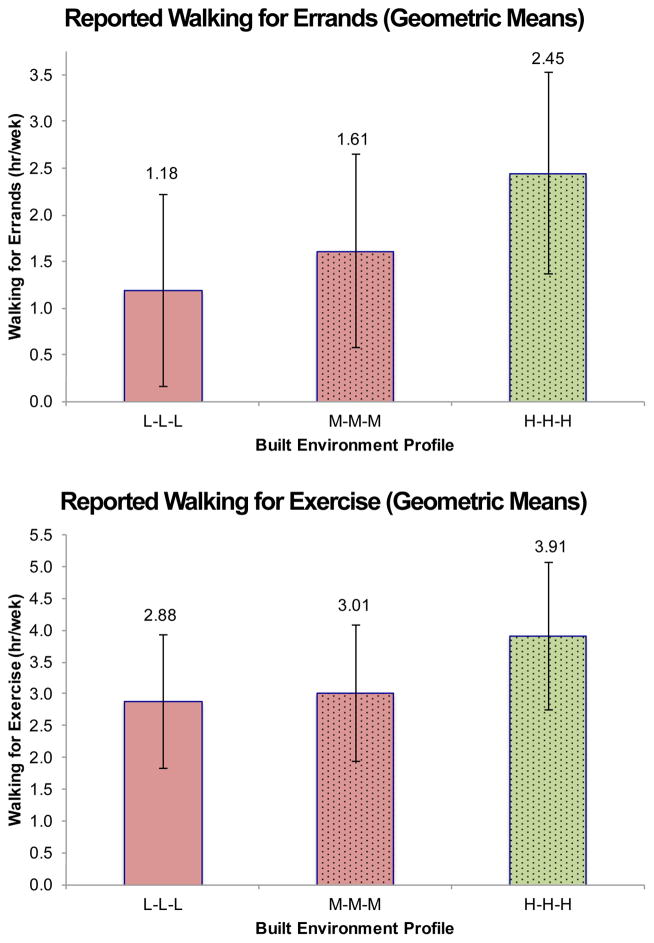
Figure 3 shows between-profile differences in hours per week of walking for errands and walking for exercise. All between-profile comparisons of logged values of walking for errands were statistically significant, with walking in the L-L-L group profile (adjusted geometric M = 1.18 hr/week; adjusted raw M = 0.34 hr/week) being significantly lower than in the M-M-M (adjusted geometric M = 1.61 hr/week; adjusted raw M = 0.92 hr/week) and the H-H-H (adjusted geometric M = 2.45 hr/week; adjusted raw M = 1.97 hr/week) profiles, and significantly lower in the M-M-M profile than in the H-H-H profile (all ps < .001). The ordering of profile means for walking for exercise was the same as that for walking for errands, but the pattern of significant differences was not. Only the difference between the L-L-L profile (adjusted geometric M = 2.85 hr/week; adjusted raw M = 3.27 hr/week) and the H-H-H profile (adjusted geometric M = 4.07 hr/week; adjusted raw M = 4.59 hr/week) was statistically significant (p = .017) for walking for exercise. The M-M-M profile (adjusted geometric M = 3.06 hr/week; adjusted raw M = 3.17 hr/week) did not differ significantly from either the L-L-L profile (p = .358) or the H-H-H profile (p = .064).
Figure 3.
Adjusted geometric means for CHAMPS-based measures of walking for errands and walking for exercise by latent profile for older adults sampled from the Seattle-King County, WA and Baltimore, MD-Washington, DC regions 2005–2008. Mean were adjusted for accelerometer wear time, sex, age, race/ethnicity, annual household income, educational attainment, number of motor vehicles and eligible drivers in household, marital or cohabitation status, number of people in household, and years at current address. Within each panel, non-significant comparisons are reflected across profiles by bars with matching colors or matching patterns.
BMI
Although profile means for BMI were ordered as expected (i.e., lowest in the H-H-H profile, highest in the L-L-L profile), they not differ significantly across profiles. The difference between the L-L-L profile (M = 26.9 kg/m2) and the H-H-H profile (M = 25.3 kg/m2) approached statistical significance (p = .058), but the L-L-L vs. M-M-M (M = 26.5 kg/m2) and M-M-M vs. H-H-H differences did not (p = .428 and p = .158, respectively).
DISCUSSION
The current analysis builds on previous work from SNQLS by examining a more diverse array of GIS-measured BE features than previously reported, including not only walkability-related features but also access to public transit, parks, and recreation facilities. It also builds upon previous work by the current authors relating LPA-derived profiles of objectively measured BE features to PA in younger adults39 and work examining how profiles of self-reported BE features relate to PA among younger adults22,37,46 and older adults22. Using seven diverse BE features, we derived three meaningful BE profiles with varying levels of activity-supportiveness. The profile corresponding to neighborhoods relatively unsupportive of PA comprised the most participants, while the profile corresponding to activity-supportive neighborhoods comprised the fewest. This finding, reflected in other analyses22,39,46, is consistent with low population densities and levels of transit and recreation access seen in U.S. cities, compared to cities in other countries.19,47,48
PA measures and BMI varied as expected in a gradient relation to the activity-supportiveness of neighborhood profiles. Participants in the least PA-supportive profile (L-L-L) consistently had lower levels of PA, and higher levels of sedentary time, than those in the most supportive profile (H-H-H). Differences between those in the moderately supportive profile (M-M-M) and those in the other profiles, however, were generally not significant. Average BMI values, while ordered as expected across profiles, did not significantly differ from each other.
In the quadrant-based analysis of SNQLS participants, those from high versus low (GIS-measured) walkability neighborhoods (defined by a 4-component walkability index at the block group level) differed by 2.5 min/day for accelerometer-measured MVPA, 31.4 min/week for self-reported active transportation (included walking, jogging/running, and biking), and by 0.9 points for BMI. 27 For MVPA min/day, self-reported time spent in active transportation (even with biking excluded), and BMI, the differences between the least and most activity-supportive profiles in the current analyses were nearly 2–3 times as large as the differences between walkability groups in the quadrant-based SNQLS analyses.
Potential alternative explanations for differences between the current findings and the quadrant-based findings include: (a) different operationalizations of neighborhood (1-km network buffer vs. Census block group)—areas defined by block group boundaries may be divided by barriers (e.g., freeways, rivers) rendering certain BE features inaccessible, and exclude features that are near a person’s home, but lie within an adjacent block group; (b) inclusion of transit, parks, and recreation facilities allowing for more complex BE patterns to emerge, offering a more complete portrayal of a neighborhood feature patterns; (c) differences between LPA grouping of BE features vs. a priori construction of feature combinations; or (d) some combination of these components.
Discussions of successful “aging in place”, i.e., older adults maintaining high levels of independence and quality of life without having to move out of their homes, now incorporate the BE surrounding the home (see 49 for a review). The neighborhood environment becomes particularly important for adults no longer in the workforce, with its impact magnified as mobility decreases due to physical disablement and/or loss of driving skills, heightening the relevance of proximity to destinations reachable without reliance on walking long distances, driving a private vehicle, or using limited-access public transit (e.g., “Dial-A-Ride”) programs. Designing communities with activity-supportive features or incorporating additional features into existing communities is especially important to an aging population because of the cost and risks associated with the relocation of older adults. 50 These improvements can also increase home values and decrease expenses related to car ownership, which can ease financial burdens associated with transition to an assisted living or long-term care facility, when or if it becomes necessary.51,52
Study strengths included a large sample of older adults from two regions in the US, objective measures of diverse neighborhood BE features, use of objective and self-reported outcomes in analyses. Limitations included a cross-sectional design and an inherent inability to establish causal relationships. Objective microscale features (e.g., sidewalk quality, safety from traffic) that could not be measured at the same geographic scale could have changed profile patterns. Based on U.S. Census estimates for adults aged 65 and older53, this sample was relatively highly educated, so caution may be warranted in generalizing these findings. Residential self-selection may attenuate relationships between BE features and health outcomes. While we did not adjust for residential self-section, this sample of older adults, on average, lived in their neighborhoods for over 24 years, mitigating this potential bias.
Conclusions
The results reported here add to an accumulating body of findings showing more comprehensive BE characterizations, as compared those relying on individual BE features, may better account for between-neighborhood differences in PA among older adults, indicating that local planning and policy decisions promoting healthy aging in place for this rapidly growing group should be informed by consideration of multiple BE features.
Highlights.
Latent profile analysis used to identify patterns of seven GIS-measured built environment features.
Three built environment feature profiles differing in activity-supportiveness emerged.
Older adults in most activity-supportive profile showed highest levels of MVPA.
Older adults in most activity-supportive profile showed highest levels of walking for errands and exercise.
Walkability plus transit and recreation access may contribute to healthy aging.
Footnotes
Conflicts of interest: This study was supported by the American Heart Association’s Beginning Grant in Aid (12BGIA9280017) and grant R01HL109222 from the National Heart, Lung, and Blood Institute. Study sponsors had no role in design or conduct of the study, preparation of the manuscript, or the decision to submit for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Administration on Aging-Administration for Community Living. A profile of older Americans: 2014. 2014. [Google Scholar]
- 2.Blumenthal JA, Emery CF, Madden DJ, et al. Cardiovascular and behavioral effects of aerobic exercise training in healthy older men and women. J Gerontol. 1989;44(5):M147–57. doi: 10.1093/geronj/44.5.m147. [DOI] [PubMed] [Google Scholar]
- 3.DiPietro L. Physical activity in aging: Changes in patterns and their relationship to health and function. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):13–22. doi: 10.1093/gerona/56.suppl_2.13. [DOI] [PubMed] [Google Scholar]
- 4.Pate RR, Taverno Ross SE, Liese AD, Dowda M. Associations among physical activity, diet quality, and weight status in US adults. Med Sci Sports Exerc. 2015;47(4):743–750. doi: 10.1249/MSS.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abbott RD, Rodriguez BL, Burchfiel CM, Curb JD. Physical activity in older middle-aged men and reduced risk of stroke: The Honolulu Heart Program. Am J Epidemiol. 1994;139(9):881–893. doi: 10.1093/oxfordjournals.aje.a117094. [DOI] [PubMed] [Google Scholar]
- 6.Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med. 1991;325(3):147–152. doi: 10.1056/NEJM199107183250302. [DOI] [PubMed] [Google Scholar]
- 7.Kelley GA, Sharpe Kelley K. Aerobic exercise and resting blood pressure in older adults: A meta-analytic review of randomized controlled trials. J Gerontol A Biol Sci Med Sci. 2001;56(5):M298–303. doi: 10.1093/gerona/56.5.m298. [DOI] [PubMed] [Google Scholar]
- 8.LaCroix AZ, Leveille SG, Hecht JA, Grothaus LC, Wagner EH. Does walking decrease the risk of cardiovascular disease hospitalizations and death in older adults? J Am Geriatr Soc. 1996;44(2):113–120. doi: 10.1111/j.1532-5415.1996.tb02425.x. [DOI] [PubMed] [Google Scholar]
- 9.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan GA, Seeman TE, Cohen RD, Knudsen LP, Guralnik J. Mortality among the elderly in the Alameda County Study: Behavioral and demographic risk factors. Am J Public Health. 1987;77(3):307–312. doi: 10.2105/ajph.77.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindsted KD, Tonstad S, Kuzma JW. Self-report of physical activity and patterns of mortality in Seventh-day Adventist men. J Clin Epidemiol. 1991;44(4–5):355–364. doi: 10.1016/0895-4356(91)90074-j. [DOI] [PubMed] [Google Scholar]
- 12.Paffenbarger RS, Jr, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328(8):538–545. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- 13.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: Recommendation from the American college of sports medicine and the American heart association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008. [Google Scholar]
- 15.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 16.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: Adults compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40(4):454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 17.Gebel K, Bauman AE, Petticrew M. The physical environment and physical activity: A critical appraisal of review articles. Am J Prev Med. 2007;32(5):361–369. doi: 10.1016/j.amepre.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Saelens BE, Handy SL. Built environment correlates of walking: A review. Med Sci Sports Exerc. 2008;40(7 Suppl):S550–66. doi: 10.1249/MSS.0b013e31817c67a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sallis JF, Saelens BE, Frank LD, et al. Neighborhood built environment and income: Examining multiple health outcomes. Soc Sci Med. 2009;68(7):1285–1293. doi: 10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Dyck D, Cardon G, Deforche B, Sallis JF, Owen N, De Bourdeaudhuij I. Neighborhood SES and walkability are related to physical activity behavior in Belgian adults. Prev Med. 2010;50(Suppl 1):S74–9. doi: 10.1016/j.ypmed.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 21.Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: A systematic review. Am J Prev Med. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams MA, Sallis JF, Conway TL, et al. Neighborhood environment profiles for physical activity among older adults. Am J Health Behav. 2012;36(6):757–769. doi: 10.5993/AJHB.36.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frank L, Kerr J, Rosenberg D, King A. Healthy aging and where you live: Community design relationships with physical activity and body weight in older Americans. J Phys Act Health. 2010;7(Suppl 1):S82–90. doi: 10.1123/jpah.7.s1.s82. [DOI] [PubMed] [Google Scholar]
- 24.Hall KS, McAuley E. Individual, social environmental and physical environmental barriers to achieving 10 000 steps per day among older women. Health Educ Res. 2010;25(3):478–488. doi: 10.1093/her/cyq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shigematsu R, Sallis JF, Conway TL, et al. Age differences in the relation of perceived neighborhood environment to walking. Med Sci Sports Exerc. 2009;41(2):314–321. doi: 10.1249/MSS.0b013e318185496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Cauwenberg J, De Bourdeaudhuij I, De Meester F, et al. Relationship between the physical environment and physical activity in older adults: A systematic review. Health Place. 2011;17(2):458–469. doi: 10.1016/j.healthplace.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 27.King AC, Sallis JF, Frank LD, et al. Aging in neighborhoods differing in walkability and income: Associations with physical activity and obesity in older adults. Soc Sci Med. 2011;73(10):1525–1533. doi: 10.1016/j.socscimed.2011.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen DA, McKenzie TL, Sehgal A, Williamson S, Golinelli D, Lurie N. Contribution of public parks to physical activity. Am J Public Health. 2007;97(3):509–514. doi: 10.2105/AJPH.2005.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diez Roux AV, Evenson KR, McGinn AP, et al. Availability of recreational resources and physical activity in adults. Am J Public Health. 2007;97(3):493–499. doi: 10.2105/AJPH.2006.087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freeland AL, Banerjee SN, Dannenberg AL, Wendel AM. Walking associated with public transit: Moving toward increased physical activity in the united states. Am J Public Health. 2013;103(3):536–542. doi: 10.2105/AJPH.2012.300912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rissel C, Curac N, Greenaway M, Bauman A. Physical activity associated with public transport use--a review and modelling of potential benefits. Int J Environ Res Public Health. 2012;9(7):2454–2478. doi: 10.3390/ijerph9072454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saelens BE, Vernez Moudon A, Kang B, Hurvitz PM, Zhou C. Relation between higher physical activity and public transit use. Am J Public Health. 2014;104(5):854–859. doi: 10.2105/AJPH.2013.301696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li F, Fisher KJ, Brownson RC, Bosworth M. Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. J Epidemiol Community Health. 2005;59(7):558–564. doi: 10.1136/jech.2004.028399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mowen A, Orsega-Smith E, Payne L, Ainsworth B, Godbey G. The role of park proximity and social support in shaping park visitation, physical activity, and perceived health among older adults. J Phys Act Health. 2007;4(2):167–179. doi: 10.1123/jpah.4.2.167. [DOI] [PubMed] [Google Scholar]
- 35.Kaczynski AT, Potwarka LR, Saelens BE. Association of park size, distance, and features with physical activity in neighborhood parks. Am J Public Health. 2008;98(8):1451–1456. doi: 10.2105/AJPH.2007.129064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kerr J, Norman G, Millstein R, et al. Neighborhood environment and physical activity among older women: Findings from the San Diego cohort of the Women’s Health Initiative. J Phys Act Health. 2014;11(6):1070–1077. doi: 10.1123/jpah.2012-0159. [DOI] [PubMed] [Google Scholar]
- 37.Adams MA, Sallis JF, Kerr J, et al. Neighborhood environment profiles related to physical activity and weight status: A latent profile analysis. Prev Med. 2011;52(5):326–331. doi: 10.1016/j.ypmed.2011.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kurka JM, Adams MA, Todd M, et al. Patterns of neighborhood environment attributes in relation to children’s physical activity. Health Place. 2015;34:164–170. doi: 10.1016/j.healthplace.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adams MA, Todd M, Kurka J, et al. Patterns of walkability, transit, and recreation environment for physical activity. Am J Prev Med. 2015;49(6):878–887. doi: 10.1016/j.amepre.2015.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place. 2010;16(2):175–190. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 42.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Welk GJ, Schaben JA, Morrow JR., Jr Reliability of accelerometry-based activity monitors: A generalizability study. Med Sci Sports Exerc. 2004;36(9):1637–1645. [PubMed] [Google Scholar]
- 44.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Muthén LK, Muthén BO. Mplus user’s guide. 1998–2014. [Google Scholar]
- 46.Adams MA, Ding D, Sallis JF, et al. Patterns of neighborhood environment attributes related to physical activity across 11 countries: A latent class analysis. Int J Behav Nutr Phys Act. 2013;10 doi: 10.1186/1479-5868-10-34. 34-5868-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adams MA, Frank LD, Schipperijn J, et al. International variation in neighborhood walkability, transit, and recreation environments using geographic information systems: The IPEN adult study. Int J Health Geogr. 2014;13 doi: 10.1186/1476-072X-13-43. 43-072X-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18(1):47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- 49.Levasseur M, Généreux M, Bruneau JF, et al. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: Results from a scoping study. BMC Public Health. 2015;15 doi: 10.1186/s12889-015-1824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rossen EK. Assessing older persons’ readiness to move to independent congregate living. Clin Nurse Spec. 2007;21(6):292–296. doi: 10.1097/01.NUR.0000299618.51722.19. [DOI] [PubMed] [Google Scholar]
- 51.Sallis JF, Spoon C, Cavill N, et al. Co-benefits of designing communities for active living: An exploration of literature. Int J Behav Nutr Phys Act. 2015;12 doi: 10.1186/s12966-015-0188-2. 30-015-0188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cortright J. [Accessed June 1, 2016];Walking the walk: How walkability raises home values in US cities. http://blog.walkscore.com/wp-content/uploads/2009/08/WalkingTheWalk_CEOsforCities.pdf.
- 53.Ryan CL, Bauman K. Educational Attainment in the United States: 2015. U.S. Census Bureau; (Population Characteristics Report No. P20-578) https://www.census.gov/content/dam/Census/library/publications/2016/demo/p20-578.pdf. [Google Scholar]