Abstract
Background
Early-life exposure to traffic-related air pollution exacerbates childhood asthma, but it is unclear what role it plays in asthma development.
Methods
The association between exposure to primary mobile source pollutants during pregnancy and during infancy and asthma incidence by ages 2 through 6 was examined in the Kaiser Air Pollution and Pediatric Asthma Study, a racially diverse birth cohort of 24,608 children born between 2000 and 2010 and insured by Kaiser Permanente Georgia. We estimated concentrations of mobile source fine particulate matter (PM2.5, μg/m3), nitrogen oxides (NOX, ppb), and carbon monoxide (CO, ppm) at the maternal and child residence using a Research LINE-source dispersion model for near-surface releases. Asthma was defined using diagnoses and medication dispensings from medical records. We used binomial generalized linear regression to model the impact of exposure continuously and by quintiles on asthma risk.
Results
Controlling for covariates and modeling log-transformed exposure, a 2.7-fold increase in first year of life PM2.5 was associated with an absolute 4.1% (95% CI 1.6%, 6.6%) increase in risk of asthma by age 5. Quintile analysis showed an increase in risk from the first to second quintile, but similar risk across quintiles 2–5. Risk differences increased with follow-up age. Results were similar for NOX and CO and for exposure during pregnancy and the first year of life due to high correlation.
Conclusions
Results provide limited evidence for an association of early-life mobile source air pollution with childhood asthma incidence with a steeper concentration–response relationship observed at lower levels of exposure.
Keywords: asthma, air pollution, traffic, birth cohort, pregnancy
INTRODUCTION
It is well established that exposure to ambient air pollution exacerbates childhood asthma, and some evidence suggests it may also play a role in asthma development.1,2 Exposure to air pollution during pregnancy and early life is associated with changes in immune programming and response as well as respiratory system development.3–5 One active area of research focuses on whether exposure to air pollution specifically from traffic causes childhood asthma.6–10 Results from recent epidemiologic studies suggest that there may be an association, with effect estimates for individual pollutants and exposure in different developmental windows ranging in magnitude and strength.11–18
We conducted a large retrospective birth cohort study, the Kaiser Air Pollution and Pediatric Asthma (KAPPA) Study, to assess whether exposure to air pollution from mobile sources during pregnancy or the first year of life is associated with risk of childhood asthma. Examining this question in the well-defined KAPPA cohort provided several advantages. The high proportion of African American children allowed us to examine a population subgroup disproportionately affected by asthma19 and underrepresented in studies of this kind. Objective measures of asthma diagnosis and medication dispensings obtained through medical records avoided reliance on parental-reported asthma. We estimated exposure to mobile source pollution (fine particulate matter [PM2.5], nitrogen oxides [NOX] and carbon monoxide [CO]) using prospectively collected residential locations of mothers and their children and spatially resolved estimates of pollutant concentrations derived from traffic emissions, meteorology, and measurements from air quality monitoring stations.
METHODS
Study Population
The KAPPA Study is a birth cohort of children born between 2000 and 2010 enrolled in Kaiser Permanente Georgia (KPGA) Health Maintenance Organization (HMO) for at least the first year of life (allowing up to 90 day gaps in enrollment). This study was approved by the Emory University and KPGA Institutional Review Boards. KAPPA members resided in metropolitan Atlanta, Georgia, an area that includes approximately 22,000 square kilometers, and were followed from birth until September 2013 or until their enrollment in KPGA ended if that occurred first. Information on demographic characteristics, geocoded residential history, diagnoses, and medication dispensings is available for all children from KPGA medical records. Additional information is available for 89% of children from linked maternal KPGA records, and for 76% of children from birth certificates.
Among the 24,608 children in the KAPPA cohort, 23,100 had estimates of air pollution exposure during the first year of life and of those 19,951 had estimates of prenatal air pollution exposure (eFigure 1 details exclusions). Date of conception was estimated using gestational age at birth (in weeks) from the birth certificate. For the 6,025 children for whom gestational age was unavailable, we assumed a full term gestational age of 40 weeks. Consistent with obstetric convention, we assumed conception to occur at gestational day 14 for both calculations.
Air Pollution Exposure Estimates
Annual average estimates of mobile source contributed PM2.5, NOX, and CO were modeled for years 2002–2011 at 250 meter resolution using a Research LINE-source dispersion model for near-surface releases (RLINE).20 The air quality model is described in more detail elsewhere.21 Briefly, RLINE modeling was completed using 2010 emissions inputs created by Atlanta Regional Commission’s Atlanta Roadside Emissions Exposure Study (AREES)22 and 2002–2011 meteorologic inputs from the meteorologic processors of AERMOD.23 Emission inputs for 2010 for 43,712 road links in the study area were based on factors such as road type, and traffic volume and composition and were scaled for years 2002–2011 by average emissions because the road network remained stable over the study period. The RLINE estimates were calibrated using stationary monitoring data to account for overestimation of spatial gradients. CO and NOX were calibrated directly to measured concentrations whereas PM2.5 was calibrated to source impacts estimated from speciated PM2.5 measurements using a CMB-GC approach24 since mobile source PM2.5 constitutes a small proportion of total PM2.5. Estimated pollutant concentrations for 2010 are shown in Figure 1 and eFigure 2. The spatial gradient was similar for the entire study period, but concentrations decreased over time.
Figure 1.
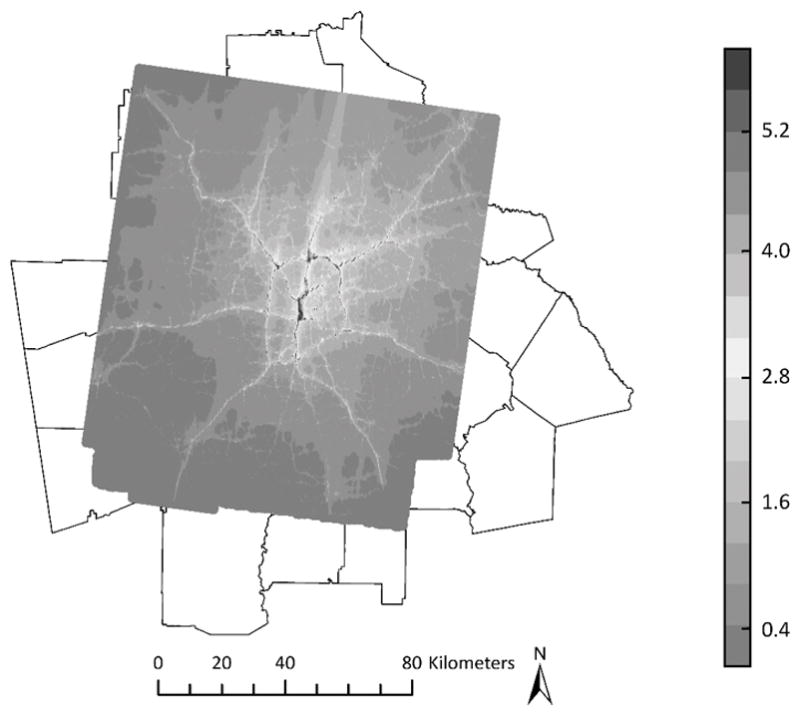
2010 PM2.5 (μg/m3) concentrations contributed by primary mobile sources
The calibrated annual average RLINE estimates for each 250 m grid and mother and child residential histories were used to estimate exposure to mobile source PM2.5, NOX, and CO during pregnancy and during the first year of life. Time-weighting was used to account for changes in residential locations and calendar years during the exposure window (i.e., assigned exposures were time-weighted averages of year- and grid-specific pollutant concentrations). Because only annual pollutant averages from RLINE were used to assign exposure, there was no seasonal variation captured by the exposure assignments; the use of year-specific annual averages did incorporate broad long-term time trends. Exposure windows in our cohort spanned from 1999 to 2011, but pollution estimates were only available for 2002 to 2011. Due to the similarity of the spatial patterns over this period, 2002 estimates were applied to years 1999 to 2001. We conducted sensitivity analyses excluding children with exposure periods before 2002.
Asthma Classification
We defined asthma as at least one asthma diagnosis (ICD-9 493.XX) and one asthma-related medication dispensing (including steroid and non-steroid asthma controllers and relievers) after the first year of life. We assessed cumulative asthma incidence by ages 2 through 6, so once a child was classified as having asthma, they were classified as asthmatic at every subsequent age. Due to the variability in case definitions for early-life incident asthma among studies using medical records to define disease,25–28 we completed a sensitivity analysis using 13 alternative asthma case definitions.29 Asthma in early life is often transient30 so we also completed an analysis to assess whether air pollution is associated with lasting asthma phenotypes. For this analysis, we examined the outcome of persistent asthma, classified as a child with incident asthma who also had evidence of asthma in the past year (at least 1 asthma diagnosis or 1 asthma-related medication dispensing) at each follow-up age. Children with incident asthma, but without evidence of asthma morbidity in the past year were excluded from this analysis. While we examined asthma by several ages, we had an a priori interest in asthma by age 5. Asthma diagnoses become more reliable as children approach age 531 making it an important age threshold in the field of asthma research, so we conducted sensitivity analyses on the subset followed until age 5 (n=8,592).
Covariate Information
We considered the following covariates: sex, race, ethnicity, maternal asthma (defined as at least one asthma diagnosis (ICD-9 493.XX) during a mother’s enrollment in KPGA), maternal age, parental education, maternal marital status, neighborhood socioeconomic status (SES), birth year and city region. We anticipated SES would be an important confounder in analyses due to the spatial assignment of pollution exposure, strong spatial pattern of SES, and the association between lower SES and asthma. To control for SES, we obtained demographic clusters created by Georgia Department of Public Health from data on 25 variables from the 2010 U.S. Census.32 These clusters categorize census block groups into 18 categories that broadly range from low to high SES (eFigure 3) and were used to characterize neighborhood SES at child residence at birth.
City region was not an a priori variable of interest, but was strongly related to air pollutant concentrations and was included in models due to concerns about residual confounding by SES. Although the demographic clusters characterize block group level SES, we noted that the same cluster could include inner city areas as well as areas outside the urban core (eFigure 3), and that there may be important differences between individuals classified as the same demographic cluster but who resided in more and less urban areas of Atlanta. In an effort to improve exchangeability we controlled for three city regions: inside the I-285 highway encircling the city of Atlanta, ≤16 kilometers (km) outside I-285, and >16 km outside I-285 (eFigure 4).
Statistical Analysis
We assessed the impact of prenatal and first year of life air pollution exposure on cumulative asthma incidence in subsequently longer follow-up periods using binomial generalized linear regression with robust variance estimation: 1–2 year risk, 1–3 year risk, 1–4 year risk, 1–5 year risk, and 1–6 year risk. Each analysis assessed asthma incidence by the age of interest among children enrolled in KPGA until at least that age. Because 33% of children in KAPPA have siblings in the cohort, we implemented models using generalized estimating equations with an exchangeable correlation structure to account for correlation among siblings. Adjusted models included birth year to control for potential confounding by temporal trends, but its inclusion resulted in some model convergence issues due to the sensitivity of binomial models to predicted probabilities approaching the boundary values of p. Results from models that alternatively controlled for time using cubic splines on birthdate with one knot per year were virtually identical and are presented when models including birth year did not converge. Convergence issues were attributable to fewer than five children with extreme predicted probabilities; exclusion of these children also yielded similar results. For presentation, we opted to change the time control slightly in order to preserve the sample size across analyses. Due to high correlation, prenatal and first year of life exposures were modeled separately. We assessed potential effect measure modification by race, sex, and maternal asthma on the additive scale by adding product terms to models and by stratified analyses.
All exposure distributions were highly skewed so we explored modeling exposure in three ways: by quintile, as a continuous linear variable, and as a natural log-transformed continuous variable. To further explore the concentration response, we used generalized additive models with loess smoothers for the pollution exposure. Because some children had gaps in residence data we completed a sensitivity analysis excluding children missing at least 90 days of residence data during exposure windows.
In a secondary analysis, we used Cox proportional hazards regression assessing asthma incidence by age 5 defining failure time in days. This approach was selected to examine multiplicative effects (estimated in previous studies) and to use censoring to allow children who were not followed to age 5 to contribute available follow-up time to the analysis. Analyses and figures were completed in SAS 9.3 (SAS Institute Inc., Cary, NC), R 3.1,33 and ArcMap 10.1 by ESRI (®).
RESULTS
The study population was racially diverse (35% African American) with relatively high SES (Table 1). The number of children followed to each age decreased with follow-up age (Table 1). This was due to HMO attrition and the fact that children born in later years were too young to be included in certain age-specific analyses due to follow-up ending in 2013 (i.e., administrative censoring). The distribution of first year of life exposure to mobile source PM2.5 is shown in Figure 2. Distribution shapes were similar for NOX and CO and also for prenatal exposures. Pollution from traffic represents a small proportion of total PM2.5 and the vast majority of NOX and CO; hence PM2.5 levels shown in Figure 2 are lower than would be expected in studies of total PM2.5. There were high correlations between exposure to mobile source PM2.5, NOX, and CO within each exposure window (rs>0.97) and also between prenatal and first year of life exposure (rs>0.90). Exposure distributions were virtually identical between children who remained insured by KPGA and children whose HMO enrollment ended. Children without asthma were slightly more likely than children with asthma to be lost to follow-up (e.g. 18% vs. 16% between ages 3 and 4).
Table 1.
KAPPA cohort characteristics
| Children with first year of life exposure data | Children with prenatal exposure data | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Characteristic | n (%) | Median first year of life | n (%) | Median prenatal | ||||
|
|
|
|||||||
| PM2.5 (μg/m3) | NOX (ppb) | CO (ppm) | PM2.5 (μg/m3) | NOX (ppb) | CO (ppm) | |||
| Cohort | 23,100 | 1.41 | 55.5 | 0.59 | 19,951 | 1.49 | 59.4 | 0.62 |
| Sex | ||||||||
| Female | 11,330 (49) | 1.42 | 55.6 | 0.59 | 9,748 (49) | 1.49 | 59.4 | 0.62 |
| Male | 11,770 (51) | 1.41 | 55.5 | 0.59 | 10,203 (51) | 1.49 | 59.5 | 0.62 |
| Race/Ethnicity | ||||||||
| Black | 7,995 (35) | 1.32 | 50.8 | 0.54 | 7,220 (36) | 1.40 | 54.6 | 0.57 |
| White | 9,034 (39) | 1.37 | 54.3 | 0.57 | 8,467 (42) | 1.45 | 58.0 | 0.60 |
| Other a | 2,771 (12) | 1.69 | 65.6 | 0.70 | 2,643 (13) | 1.78 | 69.6 | 0.73 |
| Unknown race | 3,300 (14) | 1.54 | 61.6 | 0.63 | 1,621 (8) | 1.70 | 69.7 | 0.69 |
| Hispanic ethnicity | 1,839 (8) | 1.42 | 54.2 | 0.60 | 1,759 (9) | 1.51 | 58.7 | 0.63 |
| Maternal education | ||||||||
| <12th grade | 285 (1) | 1.50 | 59.9 | 0.63 | 280 (1) | 1.60 | 65.3 | 0.68 |
| High school/GED | 2,605 (11) | 1.25 | 48.6 | 0.52 | 2,524 (13) | 1.32 | 52.3 | 0.54 |
| Some college or more | 13,442 (58) | 1.42 | 55.9 | 0.59 | 13,113 (66) | 1.51 | 60.4 | 0.62 |
| Missing | 6,768 (29) | 1.45 | 57.3 | 0.60 | 4,034 (20) | 1.56 | 61.1 | 0.64 |
| Maternal asthma | ||||||||
| Yes | 2,488 (11) | 1.39 | 54.4 | 0.58 | 2,419 (12) | 1.46 | 57.9 | 0.60 |
| No | 17,998 (78) | 1.41 | 55.5 | 0.59 | 17,532 (88) | 1.50 | 59.6 | 0.62 |
| Missing | 2,614 (11) | 1.44 | 57.3 | 0.60 | 0 | – | – | – |
| Neighborhood Socioeconomic Status b | ||||||||
| Highest SES | 14,401 (62) | 1.28 | 49.9 | 0.53 | 12,626 (63) | 1.36 | 53.6 | 0.56 |
| Urban/Suburban | 2,293 (10) | 2.38 | 93.2 | 0.96 | 1,925 (10) | 2.53 | 100.4 | 1.01 |
| Rural, average to low SES | 1,130 (5) | 0.95 | 37.7 | 0.40 | 974 (5) | 1.02 | 41.5 | 0.43 |
| Lowest SES | 5,272 (23) | 1.65 | 64.2 | 0.68 | 4,423 (22) | 1.74 | 68.9 | 0.71 |
| City Region | ||||||||
| Metro Atlanta c | 2,425 (11) | 2.24 | 87.0 | 0.91 | 2,030 (10) | 2.35 | 92.0 | 0.95 |
| ≤16 km from metro Atlanta | 9,894 (43) | 1.57 | 62.0 | 0.64 | 8,449 (42) | 1.67 | 66.5 | 0.68 |
| >16 km from metro Atlanta | 10,781 (47) | 1.14 | 45.0 | 0.49 | 9,472 (47) | 1.22 | 48.8 | 0.51 |
| Kaiser Permanente enrollment duration d | ||||||||
| Enrolled until age 2 | 17,960 (78) | 1.41 | 55.5 | 0.59 | 15,631 (78) | 1.49 | 59.6 | 0.62 |
| Enrolled until age 3 | 14,251 (62) | 1.42 | 56.0 | 0.59 | 12,434 (62) | 1.50 | 60.4 | 0.62 |
| Enrolled until age 4 | 10,999 (48) | 1.44 | 57.5 | 0.60 | 9,620 (48) | 1.54 | 62.3 | 0.63 |
| Enrolled until age 5 | 8,592 (37) | 1.46 | 59.0 | 0.60 | 7,521 (38) | 1.57 | 64.5 | 0.64 |
| Enrolled until age 6 | 6,629 (29) | 1.49 | 61.4 | 0.62 | 5,806 (29) | 1.59 | 66.7 | 0.65 |
| Cumulative asthma incidence e | ||||||||
| Age 2 | 1,994 (11) | 1.37 | 54.6 | 0.57 | 1,731 (11) | 1.45 | 58.6 | 0.60 |
| Age 3 | 2,627 (18) | 1.39 | 55.0 | 0.58 | 2,316 (19) | 1.47 | 59.4 | 0.60 |
| Age 4 | 2,650 (24) | 1.42 | 56.8 | 0.59 | 2,309 (24) | 1.51 | 61.4 | 0.61 |
| Age 5 | 2,465 (29) | 1.47 | 58.9 | 0.60 | 2,132 (28) | 1.55 | 64.0 | 0.63 |
| Age 6 | 2,149 (32) | 1.51 | 61.6 | 0.62 | 1,854 (32) | 1.59 | 67.1 | 0.66 |
SES indicates socioeconomic status, GED general educational development.
Includes Asian, American Indian, Alaska Native, Native Hawaiian or other Pacific Islander, and children identifying with more than one racial group
Neighborhood socioeconomic status was classified at census block group spatial resolution using child residence at time of birth and described using demographic clusters created by Georgia Department of Public Health32
Metro Atlanta defined as inside the I-285 perimeter of Atlanta
Reduction in sample size across follow-up reflects the shorter follow-up time available for children born in later years of the study (e.g., a child born in 2010 could be at most 3 years old at the time KAPPA follow-up ended in September 2013) as well as health maintenance organization enrollment attrition over time.
Cumulative asthma incidence (at least one asthma diagnosis (ICD-9 493.XX) and one asthma-related medication dispensing after the first year of life) calculated among children enrolled until each follow-up age
Figure 2.
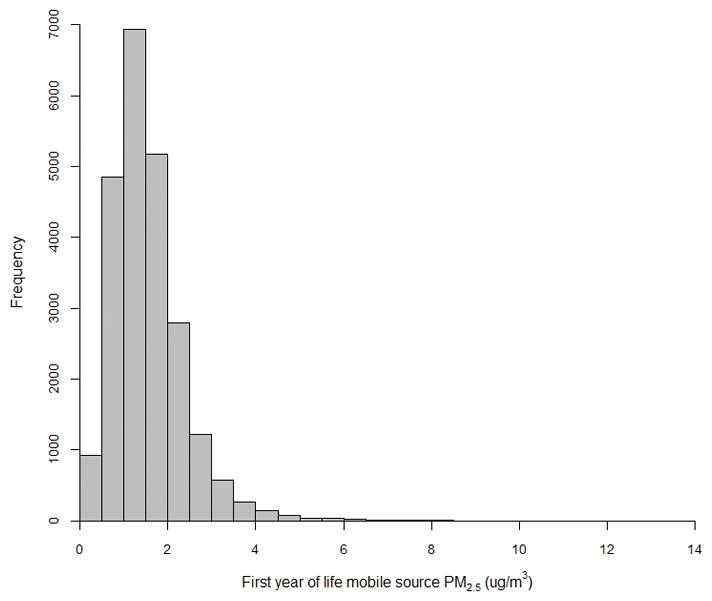
Distribution of first year of life mobile source PM2.5 (n=23,100) (range from 0.06 μg/m3 to 13.8 μg/m3)
Proximity to the city center was the strongest determinant of residential exposure to mobile source pollution in this cohort (Table 1). Due to the concentration of highways inside the city core (Figure 1), exposure decreased with increasing distance from the city center. Exposure distributions were similar between white and black children in our cohort. There was a high burden of asthma diagnoses and medication dispensings in the KAPPA cohort, with 32% of children receiving both a diagnosis and medication by age 6 (Table 1). Spatially, asthma risk increased with increasing distance from city center (28% in metro Atlanta vs. 33% >16 km outside metro Atlanta) and was highest among children born in rural neighborhoods (35%) and lowest among children born in urban/suburban neighborhoods (28%).
Due to the high correlation between pollutants, associations between mobile source PM2.5, NOx, and CO and asthma incidence were very similar for first year of life and prenatal exposures. Thus, we focus on results for first year of life mobile source PM2.5 with results for other exposures provided in the online supplement. Ethnicity, maternal age, parental education, and maternal marital status did not impact results and were dropped from adjusted models. When modeling first year of life exposure by quintile, using the lowest quintile as the reference group, there was evidence of an increase in asthma risk with every exposure quintile. However, risk increased most strongly from the first to second quintile and leveled off thereafter (Figure 3 for follow-up through age 5). We observed a similar pattern of the largest changes in risk occurring at the lowest exposure levels, as shown in smooth concentration response curves (eFigure 5). This log-linear shape of the exposure-response, the skewed exposure distributions, and QIC (quasilikelihood under the independence model criterion) goodness of fit statistics suggested that modeling log-transformed exposure was a better fit for these data than modeling a linear continuous exposure. Consequently, we modeled exposure as a natural log-transformed continuous variable in our main analyses (rather than as a continuous linear variable).
Figure 3.
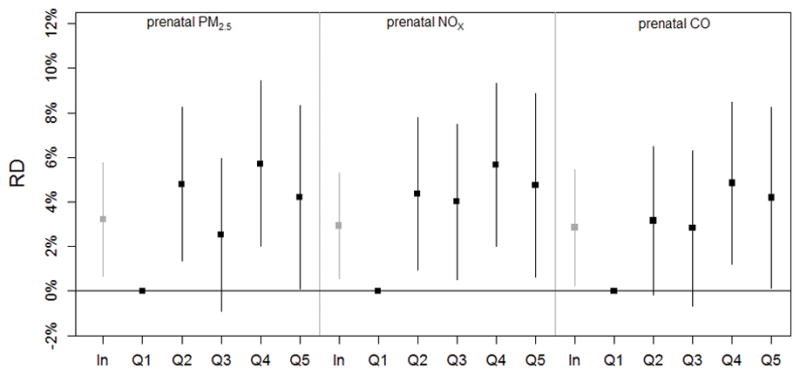
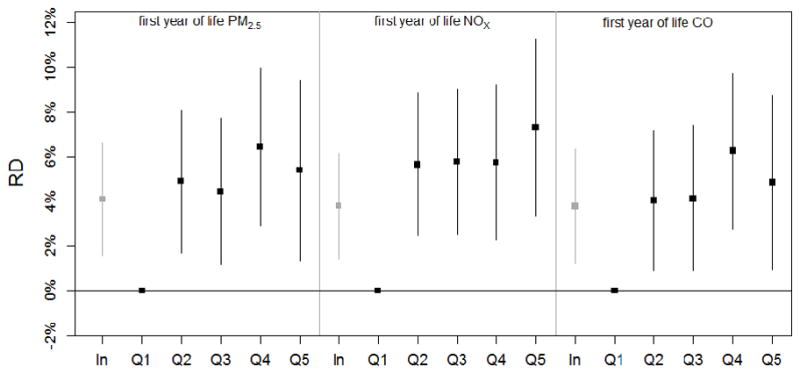
Adjusted risk differences and 95% confidence intervals for incident asthma by age 5 and prenatal (n=7,520) and first year of life (n=8,591) mobile source PM2.5, NOX, and CO: per natural log increase and by quintile (Q1–Q5). Numeric results corresponding to this figure are listed in Table 2, eTable 1, and eTable 3.
Unadjusted models suggested a decrease in asthma risk with an increase in mobile source PM2.5 (Table 2). Models adjusted for sex, race, maternal asthma, birth year, neighborhood SES, and city region demonstrated a positive association between mobile source PM2.5 and asthma risk, with risk differences increasing with follow-up age (Table 2). Control for neighborhood SES, followed by city region, had the largest impact on estimated risk differences; other covariates had little impact on results. Point estimates of the risk differences were highest for follow-up ages 5 and 6. When first year of life PM2.5 increased by a factor of 2.7 (a natural log increase), risk of asthma by age 2 increased by an absolute 1.2% (95% CI=0.0%, 2.3%) while risk of asthma by age 5 increased by an absolute 4.1% (95% CI=1.6%, 6.6%). Results were similar when excluding children with exposure windows missing 90 days or more of residence data or in years without air quality estimates (excluding <7% and <30% respectively). When we modeled pollutant concentrations linearly (without log transformation) adjusted risk differences were also positive but more compatible with the null than the log-transformed exposure results (eTable 2).
Table 2.
Risk differences and 95% confidence intervals for prenatal and first year of life mobile source PM2.5 and asthma incidence
| Prenatal exposure, RD per natural log increasea | ||
|---|---|---|
|
| ||
| Cohort | Unadjusted RD (95% CI) | Adjusted RD (95% CI) |
| Age 2 | −0.007 (−0.017, 0.002) | 0.015 (0.003, 0.027) |
| Age 3 | −0.008 (−0.021, 0.005) | 0.018 (0.002, 0.035) |
| Age 4 | −0.008 (−0.025, 0.009) | 0.023 (0.001, 0.044) |
| Age 5 | 0.001 (−0.019, 0.021) | 0.032 (0.007, 0.058) |
| Age 6 | 0.005 (−0.019, 0.029) | 0.035 (0.006, 0.065) |
|
| ||
| First year of life exposure, RD per natural log increasea | ||
|
| ||
| Cohort | Unadjusted RD (95% CI) | Adjusted RD (95% CI) |
|
| ||
| Age 2 | −0.008 (−0.016, 0.001) | 0.012 (0.000, 0.023) |
| Age 3 | −0.009 (−0.021, 0.004) | 0.019 (0.003, 0.034)b |
| Age 4 | −0.008 (−0.024, 0.007) | 0.025 (0.004, 0.046) |
| Age 5 | 0.005 (−0.014, 0.024) | 0.041 (0.016, 0.066) |
| Age 6 | 0.002 (−0.021, 0.024) | 0.035 (0.005, 0.064) |
RD indicates risk difference, CI confidence interval. Adjusted models control for child sex, child race, maternal asthma, birth year, neighborhood socioeconomic status, and city region.
This represents the absolute change in risk per 2.7-fold increase in mobile source PM2.5 concentration (μg/m3)
birth year replaced by cubic splines on date of birth with 1 knot per year.
The strongest predictors of childhood asthma were maternal asthma, male sex, and black race. When controlling for all other covariates, the risk of asthma by age 5 was an absolute 13.8% (95% CI=10.7%, 16.8%) higher among children whose mothers have asthma compared to children whose mothers do not have asthma or for whom asthma status was unknown, 8.7% (95% CI=6.9%, 10.6%) higher in males than females, and 5.7% (95% CI=3.2%, 8.2%) higher in black children than white children.
We observed no consistent evidence of additive interaction between the exposures and race, sex, or maternal asthma when assessed by adding product terms to models, although power for this assessment was limited. When stratifying by race, there was a 5.3% (1.7%, 8.9%) increase in asthma risk by age 5 among white children and a 4.8% (0.5%, 9.1%) increase among black children per natural log increase in PM2.5. In analyses restricted to children of mothers without asthma, there was a 4.1% (95% CI=1.2%, 6.9%) increase in risk of asthma by age 5 (n=6,606) per natural log increase in exposure. Models restricted to children whose mothers have asthma were less precise (n=1,140; RD (95% CI) 2.7% (−5.2%, 10.7%)). In models stratified by sex, estimates for females tended to be slightly higher than estimates for males, however confidence intervals largely overlapped. For example, by age 5 a natural log increase in PM2.5 was associated with a 4.7% (95% CI=1.4%, 8.0%) increase in risk among girls and a 2.7% (95% CI=−1.1%, 6.6%) increase in risk among boys.
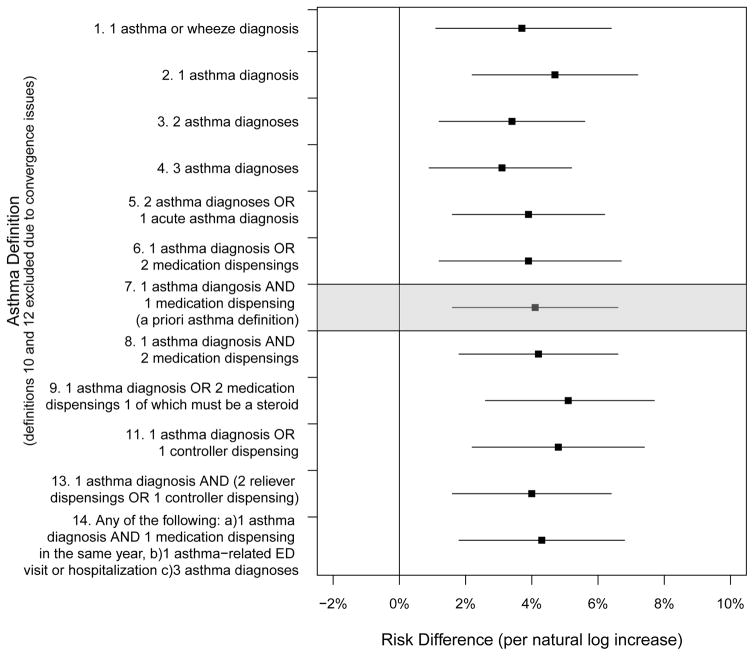
There was some variation in estimates, but conclusions were consistent when different asthma case definitions were applied (Figure 4). When modeling a natural log increase in mobile source PM2.5, the smallest risk difference was a 3.1% (95% CI=0.9%, 5.2%) increase in asthma risk by age 5 when asthma was defined as three asthma diagnoses. The largest risk difference resulted from defining asthma as one asthma diagnosis or two medication dispensings, one of which must be a steroid and demonstrated a 5.1% (95% CI=2.6%, 7.7%) increase in risk by age 5. When examining the outcome of persistent asthma by age 5 (excluding those with apparent transient asthma), there was a tendency for risk differences to be slightly larger than for incident asthma, but results were similar (eTable 4, eFigure 6).
Figure 4.
First year of life mobile source PM2.5 and incident asthma by age 5 among children enrolled through age 5 (n=8,591), comparing different outcome definitions (per natural log increase in μg/m3). Numeric results corresponding to this figure are listed in eTable 5.
Cox proportional hazards regression was completed using the 22,987 children in the KAPPA cohort with information on first year of life exposure data who were enrolled in KPGA until at least their first birthday. At age 5, adjusted model results indicated an elevated asthma hazard ratio associated with a natural log increase in mobile source PM2.5 (HR (95% CI) 1.16 (1.07, 1.26)).
DISCUSSION
In this large retrospective cohort study of children enrolled in the Kaiser Permanente Georgia HMO, we observed some positive associations between mobile source air pollution at the child’s early life residence and asthma incidence. Our results were sensitive to modeling decisions and control for covariates with results of some models providing no evidence of an association.
A 2010 study by Clark and colleagues in British Columbia is arguably the most similar study to ours, based its use of administrative data to define the cohort, asthma classification from medical records, and focus on prenatal and first year of life exposure.13 When exposure was defined using a land-use regression model based on pollutant sampling data, they observed associations between NO2, NO, CO, and black carbon and asthma onset between ages 3 and 4, but little evidence of associations with total PM2.5. Their black carbon results, indicative of traffic PM2.5, and our mobile source PM2.5 results, based on traffic data emissions, are consistent in that they provide some support for an association between early life traffic exposure and asthma incidence. Comparison of effect estimates across studies is challenging due to variation in population characteristics, pollution levels, focus on primary or total PM concentrations, and age at which asthma was examined. Additionally, our study is the first to assess absolute, rather than relative, changes in asthma risk. The risk difference was chosen for this study based on our interest in absolute changes in risk as well as a desire to assess additive interaction due to its relevance to public health.34 We note that when we estimated multiplicative changes using hazard ratios, which benefited from additional power due to the use of censoring, the results also indicated a positive association between traffic pollution and asthma incidence.
We estimated pollution exposure in the KAPPA study using longitudinal residence data and fine-scale pollutant estimates that account for traffic patterns, particle composition, and meteorology and that utilize data from stationary air pollution monitors for calibration. These estimates incorporate changes in residence; 36% of children in our analyses changed residences at least once during the period between conception and the first birthday.35 This is a refinement over previous studies that have used residence at birth as a proxy for residence throughout early life.12,14 Because mobile source PM2.5, NOX, and CO were highly correlated, exposure estimates should be considered indicators of traffic exposure more generally. Estimated risk differences may be indicating the impact of other unmeasured traffic pollutants. We anticipate some exposure measurement error due to the use of modeled exposure. Our research question focused on ambient pollution from traffic, but if ambient traffic pollution causes asthma it would be through the pathway of personal exposure which is additionally impacted by housing air exchange rates and time-activity patterns. There is some evidence in the literature suggesting that not accounting for time-activity patterns may be less of a concern for estimating personal exposures to pregnant women than other populations.36,37
We investigated study hypotheses in the KPGA population, a primarily urban population in the southeastern U.S. with high asthma rates, a large African American population, and access to healthcare. Although results may not generalize well to distinctly different populations, our association estimates are of similar magnitude to those previously reported in the literature, suggesting that the pediatric asthma associations that have been observed with traffic are not highly specific to a particular population. One limitation of the KAPPA study is the lack of detailed data on individual-level SES, early life environment, and clinical testing to differentiate atopic and non-atopic asthma phenotypes. The KAPPA study has high loss to follow-up (e.g., 22% of children are lost by age two years) which impacted power and contributed to model convergence issues. Children without prior diagnosis of asthma were slightly more likely to be lost to follow-up, but loss to follow-up was not associated with air pollution exposure, lessening our concerns about the impact of selection bias. Similar to the difficulties in a previous study,13 the high correlation between prenatal and first year of life exposure estimates prevented us from determining the relative importance of exposure during each of these periods.
Although we used comprehensive medical record data for outcome classification, outcome measurement error stemming from inherent difficulties in early-life asthma diagnosis is a limitation of our study. We made the decision to define asthma incidence as at least one asthma diagnosis and one asthma-related medication dispensing after investigating different ways to define asthma in this cohort.29 This definition ensures that a child classified as asthmatic has had a doctor diagnose their condition as asthma and also has some evidence of respiratory symptoms requiring medication. Sensitivity analyses using alternative asthma case definitions and the outcome of persistent asthma demonstrated that our results were robust to changes in disease classification. Because asthma symptoms in early life are often transient,30 the outcome of persistent asthma is perhaps more directly relevant to the public health burden of disease.
Confounding by SES-related factors acted in the opposite direction from what we expected. We anticipated unadjusted models would be biased in the positive direction since children from the lowest SES groups often have the most asthma and also frequently live in the most polluted areas.19,38 Surprisingly, our unadjusted results showed negative associations between mobile source air pollution and asthma. Descriptive analyses revealed a strong spatial pattern in our data; increasing distance from the city center was associated with increasing asthma rates and decreasing pollution. It seems likely to us that our crude results were confounded by SES and also by factors other than air pollution that change with distance from the city center (e.g., health care utilization). While we believe adjustment for neighborhood SES and city region increased the validity of our results, the sensitivity of results to control for these contextual variables warrants caution in interpretation.
We present results for natural log-transformed pollutant concentrations, and while it is common to log transform skewed exposures, this is usually not performed in air pollution epidemiology studies which rarely have such skewed exposure distributions. The highly skewed exposure distributions in this study are due to high concentrations among the children living closest to the highways. The results of the quintile analyses were generally consistent with a log-linear exposure-response shape, showing the greatest changes in risk at the low end of the exposure distribution (Figure 3); the difference in risk between the first and fifth quintiles was not much larger than the difference in risk between the first and second, third or fourth quintiles. This is perhaps less convincing than would be an observed monotonic dose response, but there is evidence from other areas of air pollution epidemiology that for some health outcomes the concentration response has a supralinear shape.39–43
The results of this study suggest that in the KAPPA cohort, the risk of asthma increased an absolute 1.2% to 4.1% (depending on follow-up age) per natural log increase in mobile source PM2.5, with similar effect estimates for NOX and CO. Our results were sensitive to certain modeling decisions, specifically how exposure was modeled and what contextual variables were controlled. Taken as a whole, our results provide limited evidence for an association between early-life mobile source air pollution exposure and childhood asthma incidence.
Supplementary Material
Acknowledgments
Sources of Funding: US EPA grant R834799, NIH/NICHD R03HD084884-01, NIH T32HD052460, NIOSH 5T03OH008609
US EPA grant R834799, NIH/NICHD Grant R03HD084884-01, NIH Reproductive, Perinatal, & Pediatric Training Grant T32HD052460, NIOSH Environmental Epidemiology Training Grant 5T03OH008609. This publication’s contents are solely the responsibility of the grantee and do not necessarily represent the official view of the US EPA. Further US EPA does not endorse the purchase of any commercial products or services mentioned in the publication.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest for this work.
Availability of Data and Code: The computing code can be obtained by contacting the first or last author. The data are not available because they include personal identifiers and medical information that cannot be released.
References
- 1.Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, Mills IC, Maynard RL. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology. 2012;17(6):887–98. doi: 10.1111/j.1440-1843.2012.02195.x. [DOI] [PubMed] [Google Scholar]
- 2.Tzivian L. Outdoor air pollution and asthma in children. J Asthma. 2011;48(5):470–81. doi: 10.3109/02770903.2011.570407. [DOI] [PubMed] [Google Scholar]
- 3.Peden DB. Development of atopy and asthma: candidate environmental influences and important periods of exposure. Environ Health Perspect. 2000;108(Suppl 3):475–82. doi: 10.1289/ehp.00108s3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kajekar R. Environmental factors and developmental outcomes in the lung. Pharmacol Ther. 2007;114(2):129–45. doi: 10.1016/j.pharmthera.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Pinkerton KE, Joad JP. The mammalian respiratory system and critical windows of exposure for children’s health. Environ Health Perspect. 2000;108(Suppl 3):457–62. doi: 10.1289/ehp.00108s3457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salam MT, Islam T, Gilliland FD. Recent evidence for adverse effects of residential proximity to traffic sources on asthma. Curr Opin Pulm Med. 2008;14(1):3–8. doi: 10.1097/MCP.0b013e3282f1987a. [DOI] [PubMed] [Google Scholar]
- 7.Bråbäck L, Forsberg B. Does traffic exhaust contribute to the development of asthma and allergic sensitization in children: findings from recent cohort studies. Environ Health. 2009;8:17. doi: 10.1186/1476-069X-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gasana J, Dillikar D, Mendy A, Forno E, Ramos Vieira E. Motor vehicle air pollution and asthma in children: A meta-analysis. Environ Res. 2012;117(0):36–45. doi: 10.1016/j.envres.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, Matheson M, Dharmage SC. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy. 2015;70(3):245–56. doi: 10.1111/all.12561. [DOI] [PubMed] [Google Scholar]
- 10.HEI Panel on the Health Effects of Traffic-Related Air Pollution. HEI Special Report 17. Boston, Mass: Health Effects Institute; 2010. Traffic-Related Air Pollution: A Critical Review of the Literature on Emissions, Exposure, and Health Effects. [Google Scholar]
- 11.Gruzieva O, Bergstrom A, Hulchiy O, Kull I, Lind T, Melen E, Moskalenko V, Pershagen G, Bellander T. Exposure to air pollution from traffic and childhood asthma until 12 years of age. Epidemiology. 2013;24(1):54–61. doi: 10.1097/EDE.0b013e318276c1ea. [DOI] [PubMed] [Google Scholar]
- 12.Carlsten C, Dybuncio A, Becker A, Chan-Yeung M, Brauer M. Traffic-related air pollution and incident asthma in a high-risk birth cohort. Occup Environ Med. 2011;68(4):291–5. doi: 10.1136/oem.2010.055152. [DOI] [PubMed] [Google Scholar]
- 13.Clark NA, Demers PA, Karr CJ, Koehoorn M, Lencar C, Tamburic L, Brauer M. Effect of early life exposure to air pollution on development of childhood asthma. Environ Health Perspect. 2010;118(2) doi: 10.1289/ehp.0900916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, Oldenwening M, Smit HA, Brunekreef B. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010;181(6):596–603. doi: 10.1164/rccm.200906-0858OC. [DOI] [PubMed] [Google Scholar]
- 15.Deng Q, Lu C, Li Y, Sundell J, Dan N. Exposure to outdoor air pollution during trimesters of pregnancy and childhood asthma, allergic rhinitis, and eczema. Environ Res. 2016;150:119–127. doi: 10.1016/j.envres.2016.05.050. [DOI] [PubMed] [Google Scholar]
- 16.Krämer U, Sugiri D, Ranft U, Krutmann J, von Berg A, Berdel D, Behrendt H, Kuhlbusch T, Hochadel M, Wichmann H-E, Heinrich J. Eczema, respiratory allergies, and traffic-related air pollution in birth cohorts from small-town areas. J Dermatol Sci. 2009;56(2):99–105. doi: 10.1016/j.jdermsci.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 17.Oftedal B, Nystad W, Brunekreef B, Nafstad P. Long-term traffic-related exposures and asthma onset in schoolchildren in Oslo, Norway. Environ Health Perspect. 2009;117(5):839–44. doi: 10.1289/ehp.11491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heinrich J, Guo F, Fuertes E. Traffic-related air pollution exposure and asthma, hayfever, and allergic sensitisation in birth cohorts: a systematic review and meta-analysis. Geoinfor Geostat: An Overview. 2016;4(4) [Google Scholar]
- 19.Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001--2009. MMWR Morb Mortal Wkly Rep. 2011;60(17):547–52. [PubMed] [Google Scholar]
- 20.Community Modeling and Analysis System. [Accessed September 28, 2015];R-LINE: A Research LINE-source dispersion model for near-surface releases. https://www.cmascenter.org/r-line/
- 21.Zhai X, Russell A, Sampath P, Mulholland J, Kim B-U, Kim Y, D’Onofrio D. Calibrating R-LINE model results with observational data to develop annual mobile source air pollutant fields at fine spatial resolution: Application in Atlanta. Atmos Environ. 2016;147:446–457. [Google Scholar]
- 22.Atlanta Regional Commission. [Accessed May 6, 2016];AREES - Near Road Emissions. http://atlantaregional.com/environment/air/arees-near-road-emissions.
- 23.Cimorelli AJ, Perry SG, Venkatram A, Weil JC, Paine RJ, Wilson RB, Lee RF, Peters WD, Brode RW. AERMOD: A dispersion model for industrial source applications. Part I: general model formulation and boundary layer characterization. J Appl Meteorol. 2005;44(5):682–693. [Google Scholar]
- 24.Marmur A, Unal A, Mulholland JA, Russell AG. Optimization-based source apportionment of PM2. 5 incorporating gas-to-particle ratios. Environ Sci Technol. 2005;39(9):3245–54. doi: 10.1021/es0490121. [DOI] [PubMed] [Google Scholar]
- 25.Black MH, Smith N, Porter AH, Jacobsen SJ, Koebnick C. Higher prevalence of obesity among children with asthma. Obesity (Silver Spring) 2012;20(5):1041–7. doi: 10.1038/oby.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Black MH, Zhou H, Takayanagi M, Jacobsen SJ, Koebnick C. Increased asthma risk and asthma-related health care complications associated with childhood obesity. Am J Epidemiol. 2013;178(7):1120–8. doi: 10.1093/aje/kwt093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li DK, Chen H, Odouli R. Maternal exposure to magnetic fields during pregnancy in relation to the risk of asthma in offspring. Arch Pediatr Adolesc Med. 2011;165(10):945–50. doi: 10.1001/archpediatrics.2011.135. [DOI] [PubMed] [Google Scholar]
- 28.Getahun D, Strickland D, Zeiger RS, Fassett MJ, Chen W, Rhoads GG, Jacobsen SJ. Effect of chorioamnionitis on early childhood asthma. Arch Pediatr Adolesc Med. 2010;164(2):187–92. doi: 10.1001/archpediatrics.2009.238. [DOI] [PubMed] [Google Scholar]
- 29.Pennington AF, Strickland MJ, Freedle KA, Klein M, Drews-Botsch C, Hansen C, Darrow LA. Evaluating early-life asthma definitions as a marker for subsequent asthma in an electronic medical record setting. Pediatr Allergy Immunol. 2016;27(6):591–6. doi: 10.1111/pai.12586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stewart LJ. Pediatric asthma. Prim Care. 2008;35(1):25–40. vi. doi: 10.1016/j.pop.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 31.National Asthma Education and Prevention Program. Expert Panel Report 3. Full Report 2007: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: U.S. Department of Health and Human Services. National Institutes of Health. National Heart Lung and Blood Institute; 2007. NIH Publication Number 10–4051. [Google Scholar]
- 32.Georgia Department of Public Health, Office of Health Indicators for Planning (OHIP) [Accessed 4/11/2016];Online Analytical Statistical Information System: Demographic Clusters of Georgia: Accessing the Georgia Deparmtent of Public Health’s Data Warehouse. https://oasis.state.ga.us/gis/demographiccluster/DemoClusters2011.htm.
- 33.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. http://www.R-project.org. [Google Scholar]
- 34.Rothman KJ, Greenland S, Walker AM. Concepts of interaction. Am J Epidemiol. 1980;112(4):467–70. doi: 10.1093/oxfordjournals.aje.a113015. [DOI] [PubMed] [Google Scholar]
- 35.Pennington AF, Strickland MJ, Klein M, Zhai X, Russell AG, Hansen C, Darrow LA. Measurement error in mobile source air pollution exposure estimates due to residential mobility during pregnancy. J Expo Sci Environ Epidemiol. 2016 doi: 10.1038/jes.2016.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iniguez C, Ballester F, Estarlich M, Llop S, Fernandez-Patier R, Aguirre-Alfaro A, Esplugues A. Estimation of personal NO2 exposure in a cohort of pregnant women. Sci Total Environ. 2009;407(23):6093–9. doi: 10.1016/j.scitotenv.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 37.Nethery E, Brauer M, Janssen P. Time-activity patterns of pregnant women and changes during the course of pregnancy. J Expo Sci Environ Epidemiol. 2009;19(3):317–24. doi: 10.1038/jes.2008.24. [DOI] [PubMed] [Google Scholar]
- 38.Rowangould GM. A census of the US near-roadway population: public health and environmental justice considerations. Transportation Research Part D. 2013;25:59–67. [Google Scholar]
- 39.Apte JS, Marshall JD, Cohen AJ, Brauer M. Addressing Global Mortality from Ambient PM2. 5. Environ Sci Technol. 2015;49(13):8057–66. doi: 10.1021/acs.est.5b01236. [DOI] [PubMed] [Google Scholar]
- 40.Marshall JD, Apte JS, Coggins JS, Goodkind AL. Blue Skies Bluer? Environ Sci Technol. 2015;49(24):13929–36. doi: 10.1021/acs.est.5b03154. [DOI] [PubMed] [Google Scholar]
- 41.Smith KR, Peel JL. Mind the gap. Environ Health Perspect. 2010;118(12):1643–5. doi: 10.1289/ehp.1002517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pope CA, 3rd, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE, Thun MJ. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation. 2009;120(11):941–8. doi: 10.1161/CIRCULATIONAHA.109.857888. [DOI] [PubMed] [Google Scholar]
- 43.Ostro B. Outdoor air pollution: assessing the environmental burden of disease at national and local levels. In: Pruss-Ustun A, Campbell-Lendrum D, Corvalan C, Woodward A, editors. Environmental Burden of Disease Series, No. 5. Geneva: World Health Organization; 2004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.