The United States is experiencing an unprecedented epidemic of opioid overdose deaths. Illicit heroin is an obvious culprit in the crisis and compelling evidence shows synthetic opioids, especially fentanyl, are having a major impact (Frank and Pollack, 2017). Fentanyl is a prescribed medication that is 50–100 times more potent than morphine. Fentanyl in the recreational (ie, non-medical) drug market is not diverted pharmaceuticals but is illicitly manufactured in Asian laboratories and trafficked via the Internet. Unscrupulous drug dealers are mixing fentanyl with heroin and most users are unaware of their fentanyl exposure.
An alarming new development in the opioid crisis is the increasing availability and misuse of novel synthetic opioids (NSOs) (Prekupec et al, 2017). NSOs include analogs of fentanyl and structurally distinct non-fentanyl compounds, which act as μ-opioid receptor agonists. NSOs are used as standalone products, heroin adulterants, or constituents of counterfeit pain pills. The role of NSOs in opioid overdose deaths is difficult to determine, because the substances are not detected by standard toxicology screens, which rely on immunoassays sensitive to heroin, its metabolites, and chemically related compounds. Fentanyl can be detected with a separate immunoassay, but fentanyl analogs may cross-react with the antibody; thus, identifying analogs requires sophisticated analytical methods such as mass spectrometry. In a study examining the presence of fentanyl analogs in opioid overdose deaths, 17% of cases that tested positive by fentanyl immunoassay were found to contain fentanyl analogs (eg, acetylfentanyl) when subjected to confirmatory testing with mass spectrometry (Petersen et al, 2016). Medical examiners and forensic toxicologists do not routinely check for the presence of NSOs; thus, the contribution of the substances to overdose deaths could be grossly underestimated.
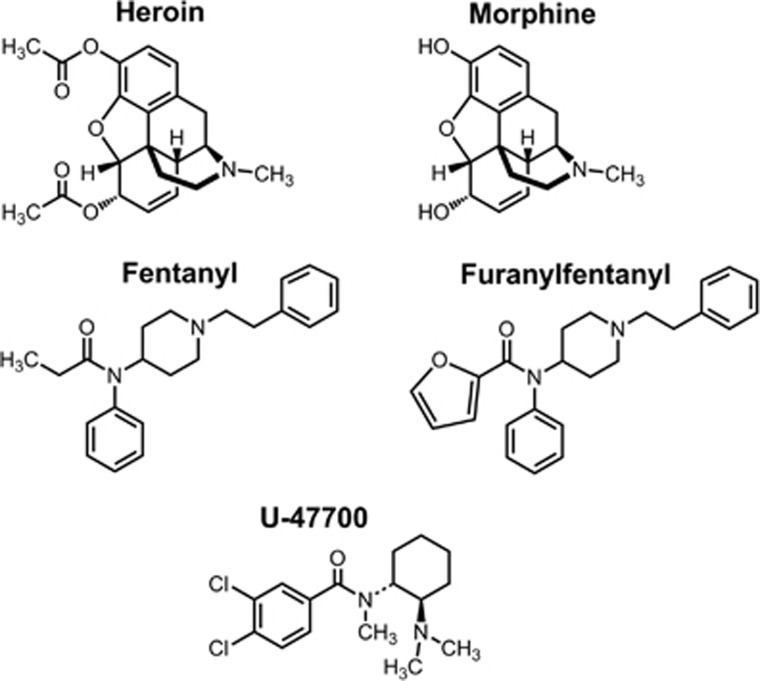
N-phenyl-N-[1-(2-phenylethyl)-4-piperidinyl]-2-furamide (furanylfentanyl) and 3,4-dichloro-N-[(1R,2R)-2-(dimethylamino)cyclohexyl]-N-methylbenzamide (U-47700) are prime examples of NSOs linked to analytically confirmed overdose deaths (Mohr et al, 2016) (see Figure 1 for structures). Furanylfentanyl is a fentanyl analog with a furan ring on the carboxamide moiety, whereas U-47700 is a non-fentanyl compound developed in the 1970s as a potential analgesic. Little information is available about the pharmacology and toxicology of furanylfentanyl, U-47700, or other NSOs, most of which were discovered decades ago. There is an immediate need for in vitro studies examining the potency and efficacy of NSOs in cells expressing μ-, δ-, and κ-opioid receptors. In addition, in vivo studies are warranted to investigate analgesic and reinforcing effects of the drugs in animal models, including opioid receptor knock out mice. The degree to which NSOs produce life-threatening adverse effects such as respiratory depression is largely unexplored.
Figure 1.
Chemical structures of heroin, morphine, fentanyl, N-phenyl-N-[1-(2-phenylethyl)-4-piperidinyl]-2-furamide (furanylfentanyl) and 3,4-dichloro-N-[(1R,2R)-2-(dimethylamino)cyclohexyl]-N-methylbenzamide (U-47700).
Naloxone (ie, Narcan) is a competitive μ-opioid receptor antagonist that reverses the effects of heroin, fentanyl, and other opioids. Anecdotal evidence suggests that current naloxone dosing protocols (0.4–2 mg) are insufficient to rescue fentanyl overdose and previous research shows naloxone doses up to 20 mg were required to reverse the effects of fentanyl during an epidemic of overdose cases in Chicago during 2005–2006 (Schumann et al, 2008). Such observations may simply reflect the need for larger doses of naloxone to reverse high fentanyl doses, but could point to interaction of fentanyl with alternative non-opioid receptor targets after high doses. Whether greater-than-expected doses of naloxone are required to antagonize effects of highly potent NSO remains an open question. The recent emergence of the fentanyl analog, carfentanil, in the recreational drug market is especially troubling because this compound is 100 times more potent than fentanyl (Shoff et al, 2017). The potential risk from non-opioid compounds in the marketplace is well illustrated by 4-chloro-N-[(2Z)-1-[2-(4-nitrophenyl)ethyl]piperidin-2-ylidene]benzene-1-sulfonamide (W-18). Although initially touted as a highly potent opioid, recent evidence reveals that W-18 does not interact with μ-, δ-, or κ-opioid receptors; thus, effects of the drug will not be antagonized by naloxone (Huang et al, 2016).
To conclude, NSOs are contributing to the current epidemic of opioid overdose deaths. Basic research investigations aimed at characterizing the pharmacology and toxicology of NSO are needed as part of a comprehensive science-based response to the opioid crisis. In particular, preclinical studies are warranted to determine the sensitivity of analgesic, respiratory depressant, and lethal effects of fentanyl, carfentanil, and NSO to naloxone or other broader spectrum opioid antagonists such as levallorphan. Data from such studies will help to inform the public, influence drug scheduling decisions, and aid in strategies to remediate effects of the drugs in emergency and clinical settings.
Funding and disclosure
This work is generously funded by the Intramural Research Program of the National Institute on Drug Abuse (NIDA) for MHB and by research grants from NIDA (DA06241 and DA07242), the Mayday Fund, and the Peter F. McManus Charitable Trust to GWP. The authors declare no conflict of interest.
References
- Frank RG, Pollack HA (2017). Addressing the fentanyl threat to public health. N Eng J Med 376: 605–607. [DOI] [PubMed] [Google Scholar]
- Huang XP, Che T, Mangano T, Le Rouzic V, Pan YX, Majumdar S et al Pharmacology of W-18 and W-15. Preprint at http://www.biorxiv.org/content/early/2016/07/24/065623 (2016).
- Mohr AL, Friscia M, Papsun D, Kacinko SL, Buzby D, Logan BK (2016). Analysis of novel synthetic opioids U-47700, U-50488 and furanyl fentanyl by LC-MS/MS in postmortem casework. J Anal Toxicol 40: 709–717. [DOI] [PubMed] [Google Scholar]
- Peterson AB, Gladden RM, Delcher C, Spies E, Garcia-Williams A, Wang Y et al (2016). Increases in fentanyl-related overdose deaths—Florida and Ohio, 2013-2015. MMWR Morb Mortal Wkly Rep 65: 844–849. [DOI] [PubMed] [Google Scholar]
- Prekupec MP, Mansky PA, Baumann MH (2017). Misuse of novel synthetic opioids: a deadly new trend. J Addict Med 11: 256–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumann H, Erickson T, Thompson TM, Zautcke JL, Denton JS (2008). Fentanyl epidemic in Chicago, Illinois and surrounding Cook County. Clin Toxicol (Phila) 46: 501–506. [DOI] [PubMed] [Google Scholar]
- Shoff EN, Zaney ME, Kahl JH, Hime GW, Boland DM (2017). Qualitative identification of fentanyl analogs and other opioids in postmortem cases by UHPLC-Ion Trap-MSn. J Anal Toxicol 41: 484–492. [DOI] [PubMed] [Google Scholar]