Abstract
Introduction
There is a high prevalence of inactive adults in the UK, and many suffer from conditions such as cardiovascular disease (CVD) or poor mental health. These coexist more frequently in areas of higher socioeconomic deprivation. There is a need to test the effectiveness, acceptability and sustainability of physical activity programmes. Active Herts uses novel evidence-based behaviour change techniques to target physical inactivity.
Methods and analysis
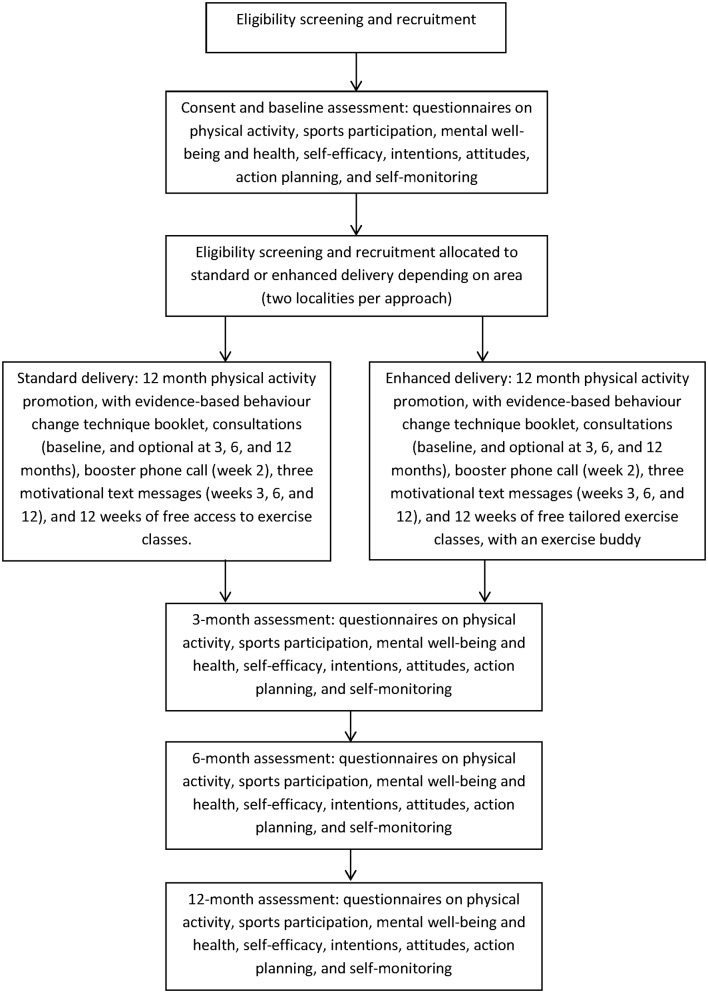
Active Herts is a community physical activity programme for inactive adults aged 16+ with one or more risk factors for CVD and/or a mild to moderate mental health condition. This evaluation will follow a mixed-methods longitudinal (baseline, and 3-month, 6-month and 12-month follow-ups) design. Pragmatic considerations mean delivery of the programme differs by locality. In two areas programme users will receive a behaviour change technique booklet, regular consultations, a booster phone call, motivational text messages and signposting to 12 weeks of exercise classes. In another two areas programme users will also receive 12 weeks of free tailored exercise classes, with optional exercise ‘buddies’ available. An outcome evaluation will assess changes in physical activity as the primary outcome, and sporting participation, sitting, well-being, psychological capability and reflective motivation as secondary outcomes. A process evaluation will explore the views of stakeholders, delivery staff and programme leads. Economic evaluation will examine the programme costs against the benefits gained in terms of reduced risk of morbidity.
Ethics and dissemination
This study was been approved by the Faculty of Medicine and Health Sciences Research Ethics Committee at the University of East Anglia. Informed written consent will be obtained from programme users in the evaluation. Results will be published in peer-reviewed journals, presented at conferences, and shared through the study website and local community outlets.
Trial registration number
ClinicalTrials.gov ID number: NCT03153098.
Keywords: physical activity programme, behaviour change, inactive adults, behaviour change techniques, com-b
Strengths and limitations of this study.
The Active Herts programme is designed with the latest behaviour change theory and techniques in both the materials for programme users and the training for delivery staff.
The Active Herts programme targets individuals in areas of deprivation with existing health issues that would benefit most from lifestyle changes.
The main limitation is that due to pragmatic considerations participants will receive the two different delivery approaches based on their place of residence and not through randomisation.
A secondary limitation is that due to financial constraints and the scale of recruitment (aiming for maximum reach), it is not possible to include an objective measure of physical activity.
Introduction
Physical inactivity is responsible for 6% of deaths globally, making it the fourth leading risk factor for mortality worldwide.1 Being active is protective against cardiovascular disease (CVD), type 2 diabetes and cancer,2 3 with strong evidence that exercise is an effective treatment for depression.4 In England, 63% of men and 59% of women report participating in the recommended weekly levels of 150 min of moderate to vigorous physical activity,5 yet objectively measured data suggest just 6% of men and 4% of women meet this level.6 Further, only 34% of men and 24% of women meet the guidelines for muscle-strengthening exercises on two or more days per week.7 The Active People Survey from Sport England in 2015–2016 found that only 36% of adults (41% of men and 32% of women) report taking part in sport once a week, with the figure decreasing to 18% for sporting participation on three or more occasions weekly.
Overall physical activity and sporting participation needs to be improved in the UK, but inactivity is even more prevalent in low-socioeconomic status (SES) adults and those suffering from major disease. Lower SES adults are less likely to participate in vigorous and moderate-intensity physical activity and walking.8 They are also more likely to perceive the opportunities to be active in their local environment more negatively shown through physical activity-related factors such as attractiveness, safety and how congested roads are.8 Furthermore, lower SES adults are also less likely to perceive themselves as overweight or try to lose weight, which in turn lessens the chances of them participating in physical activity as a weight control strategy.9 Additionally, those suffering from CVD and a combination of CVD and type 2 diabetes report lower levels of physical activity and greater sedentary behaviour in terms of television watching.10 Overall, those living in low SES areas and/or with ongoing diseases are an important target to increase physical activity through intervention.
The Active Herts programme will attempt to address adult inactivity by drawing on the latest evidence analysing how to support inactive adults to be more physically active. A recent systematic review has shown that interventions in inactive adults show statistically significant small to moderate effect sizes postintervention and small but still statistically significant effect sizes for at least 6 months after intervention contact has finished (follow-up).11 12 This review also analysed the behaviour change techniques (BCT13) that were associated with effective interventions and highlighted several approaches that can be used to heighten the likelihood of programmes and interventions producing meaningful changes in physical activity. It was found that practising the performance of physical activity and gradually increasing its intensity were effective for physical activity change at both postparticipation and follow-up. Additionally, postparticipation effectiveness was associated with being shown how to be more active and with ‘Biofeedback’ (using heart rate monitors to judge exercise intensity), and effectiveness at follow-up was associated with creating detailed plans to be active, receiving instructions on particular exercises (this may include during exercise classes), rewarding oneself for progress and utilising prompts or cues to exercise.11
While understanding which techniques are effective when attempting to intervene with an inactive population to increase physical activity is important, so too is the communication style in which the techniques are delivered.14 Motivational interviewing has been shown to be an effective communication method with which to change several health behaviours including physical activity (eg, ref 15). Used in combination, BCTs and motivational interviewing can target key determinants of behaviour, which can be understood in terms of the individual’s Capability (physical and psychological), Opportunity (social and physical) and Motivation (reflective and automatic) (COM-B16) to be more active. The selected BCTs in this programme can be mapped onto and, therefore, target all six aspects of the COM-B.17 Research has shown that the COM-B model explains a large amount of variance in physical activity participation, highlighting psychological capability and reflective motivation as key drivers.18 In this work, psychological capability was formed of components such as action planning and self-monitoring, and reflective motivation was formed of components such as intentions and self-efficacy.18
The purpose of the Active Herts programme is to support engagement in physical activity and promote well-being in inactive adults with elevated risk of CVD and/or mental health concerns living in four areas of the English county of Hertfordshire where need is the highest. Pragmatic delivery considerations mean the programme will use two different approaches, with each being delivered in two different localities. The first will provide programme users with an initial consultation, followed by 12 weeks of exercise sessions, and further support in person or by phone throughout a 12-month period (‘standard delivery’). The second approach will include additional support in the form of optional exercise buddies and free tailored exercise organised by the programme staff themselves (‘enhanced delivery’). The aim of this paper is to report the Active Herts programme methods in terms of their content, delivery, staff training and evaluation. The following are the objectives of the evaluation:
Primary objective
The primary objective is to observe whether the Active Herts programme increases physical activity with (enhanced delivery) and without (standard delivery) additional support from exercise buddies and free access to tailored exercise classes.
Secondary objectives
to observe whether the Active Herts programme increases health and mental well-being with (enhanced delivery) and without (standard delivery) additional support from exercise buddies and tailored exercise classes
to explore the relative cost-effectiveness of the two delivery approaches
to explore which components from the two different delivery approaches are particular drivers of their effectiveness and what the barriers may be that prevent these models from achieving their potential.
Methods and analysis
Design
This evaluation includes a qualitative process evaluation and an outcome evaluation. The quantitative study will follow a longitudinal (baseline, and 3-month, 6-month and 12-month follow-ups) observational design, with comparison of the two different delivery methods employed in different localities. The design of the evaluation is illustrated in figure 1. This protocol is reported according to the Transparent Reporting of Evaluations with Nonrandomized Designs19 guidelines and with reference to the Template for Intervention Description and Replication20 checklist.
Figure 1.
Active Herts programme design.
Programme users
The inclusion criteria for participation in the Active Herts programme are inactive adults aged 16 and over who have one or more risk factors for CVD. Inactivity is classed as participating in less than one episode of 30 min of physical activity per week on a regular basis. Additional risk factors for CVD include diabetes, hypertension, high cholesterol, obesity (body mass index (BMI) >30 or BMI >28 if one or more comorbidities) and/or smoking. Programme users who are inactive with a mild to moderate mental health condition may also take part. Those with a severe mental health condition can do so if their general practitioner (GP), Mind (a mental health charity) or Improving Access to Psychological Therapies consultant deems them suitable for the programme. An additional criterion for inclusion in the evaluation was the ability to give informed consent for their data to be used.
Eligible adults will live in one of four Hertfordshire districts (Broxbourne, Stevenage, Hertsmere and Watford). The wider economic value for health from sport participation in Hertfordshire is £461.6 million. Inactivity (excluding costs related to obesity and mental health) is also costing the health economy between £1.1 and £1.4 million per year in the four focus districts of Active Herts. The districts contain the highest number of deprived Lower Super Output Areas in Hertfordshire and are in the five highest rates of under 75 mortality rate from CVD (2%–3%), adult obesity (8%–10%) and diabetes (4%–6%). A life expectancy gap of 6–9.6 years exists between the most and least deprived areas across these districts.21 Less than 50% of this population participate in 30 min of physical activity once per week.
Programme users will be primarily recruited into the programme through 23 GP services throughout the four localities: five in Broxbourne, five in Hertsmere, seven in Stevenage and six in Watford. A Mind well-being centre in each location will also refer into the programme. Hertfordshire residents who meet the inclusion criteria can also access the programme through self-referral. As this programme is Sport England-funded and local authority-funded with a focus on delivery, power calculations were not deemed necessary and all eligible programme users are invited to engage in the evaluation. The objective is to provide as many eligible residents as possible with access to this programme over the 3-year life of the project, with a minimum expectation of engagement from 1500 programme users.
Programme and evaluation materials and procedure
The content of the Active Herts programme has been based on the review11 12 discussed to include BCTs found to be present in effective physical activity interventions, with the exception of ‘Biofeedback’ as giving each participant heart rate monitors in a programme of this size is unfeasible. Many of the BCTs are included in the booklet given to programme users used by ‘Get Active Specialists’ (GAS) during their consultations with programme users, and target all six facets of the COM-B model of behaviour change17 (see table 1). Programme users in both delivery groups will receive the same content in terms of an initial 45 min consultation with a GAS (with additional consultations at 3, 6 and 12 months), an Active Herts booklet, a 2-week booster call and access to activities in their local area. All programme contacts in person and by phone will be on a one-to-one basis. Aside from access to a range of free group activity sessions over the first 12 weeks, there are no additional incentives for programme users to attend consultation.
Table 1.
Programme content specified by behaviour change techniques and linked to constructs of the COM-B model
| Programme component | Behaviour change technique | COM-B construct targeted | Content |
| Booklet (both groups) | Pros and cons | Reflective motivation | A page asking whether exercise is good for you and programme users are given two blank columns to fill out with possible advantages and disadvantages of becoming more active. They are then asked how confident they feel about becoming active on a scale of 1–10. |
| Problem solving | Psychological capability*; reflective motivation | Programme users are asked to think about their current situation and to list the things that might be currently stopping them from being active and how they might overcome them. | |
| Goal setting | Reflective motivation | Programme users are given the opportunity to set short-term (2 weeks), medium-term (3 months) or long-term (12 months) goals, and then rate how confident they are of achieving each one from 1 to 10. | |
| Action planning | Psychological capability; reflective motivation | A page allowing programme users to complete sections referring to their plans to becoming more active in terms of what they are going to do, where they are going to do it, when they are going to do it and who they are going to do it with. A second page allows them to explore their time management by mapping out the week in terms of morning, afternoons and evenings. | |
| Relapse prevention | Psychological capability*; reflective motivation | In contrast to the problem-solving page which focuses on current problems, this page explains how even the most habitual exercisers can struggle at times. Programme users are asked to think about situations in the future that may affect their progress and then about options to avoid or cope with these situations. | |
| Self-monitoring of behaviour; information about emotional consequences |
Psychological capability; reflective motivation |
Programme users are given an exercise and activity diary to track their progress and highlight their engagement. A table contains columns for the date, activities completed, time in minutes, enjoyment level (from 1 (low) to 10 (high)) and how they felt after completing the activity. The table contains several rows so programme users can track this over time. | |
| Information about health consequences: information on emotional consequences | Psychological capability; reflective motivation | A page summarises the health and emotional benefits of being active in a positively framed manner. For example, did you know that being active can ‘help you manage high blood pressure’ and ‘make you feel good and improve your mental health’? | |
| Instruction on how to perform the behaviour | Psychological capability* | Programme users are given the national exercise guidelines for moderate and vigorous activity. Additionally information is given for examples of moderate and vigorous activity, how to break up long periods of sitting, how to improve balance to reduce the chance of falls and an example of how these activities can fit into everyday life. | |
| Self-reward | Automatic motivation | Programme users are told the importance of rewarding themselves for the effort they make towards their activity goals. Examples are then given of how to reward themselves in ways that are healthy and free. For example, ‘listen to music’ or ‘have a nice relaxing bath’. Self-reward is also discussed briefly during the goal-setting page when thinking about what success looks like. | |
| Consultation (both groups) | Social support unspecified; social support emotional | Social opportunity; automatic motivation | Programme users are given an initial 45 min consultation in person one-to-one where motivational interviewing and health coaching are used to structure the session to fit participant needs, move them towards becoming more active, signposting activities and discussing goals and plans, while providing emotional support. This is then repeated in subsequent consultation meetings at 3, 6 and 12 months. The additional consultations will vary between 15 and 30 min and are optional based on participant needs. |
| Credible source | Social opportunity*; automatic motivation | Expert Get Active Specialists who are trained in motivational interviewing and behaviour change, with specialist knowledge of obesity, diabetes, exercise referral and mental health, will discuss becoming more active in a favourable light with programme users. | |
| Verbal persuasion about capability | Reflective motivation | Programme users will set goals and the Get Active Specialists will encourage participants’ belief in their ability to fulfil those goals and make long-term change. | |
| Focus of past success | Reflective motivation | During the consultation programme users will set physical activity goals and the Get Active Specialists will discuss previous success or progress. | |
| Exercise sessions (both groups) | Instruction on how to perform the behaviour; demonstration of the behaviour; behavioural practice/rehearsal | Social opportunity; psychological capability | Programme users can choose to attend 12 weeks of exercise classes either referred to them (standard delivery) or organised as bespoke sessions (enhanced delivery) by the Get Active Specialists. These will involve detailed instruction on how to perform a range of exercises (eg, yoga, pilates, light to moderate-intensity circuit training). During these classes programme users will be given demonstrations of the correct way to perform the activities and provided with ample opportunity to practise and gain confidence in performing the exercises. |
| Graded tasks | Physical capability | During the exercise classes, exercise specialists will encourage programme users to start slowly and build up intensity throughout the 12 weeks. | |
| Booster call (both groups) | Social support unspecified; verbal persuasion about capability; prompts and cues | Social opportunity; reflective motivation; physical opportunity | Programme users receive a phone call at 2 weeks, which is approximately 5 min in duration, prompting them to keep working towards their physical activity goals and stating that they are capable of achieving them. |
| Test messages (both groups) | Social support unspecified; verbal persuasion about capability; prompts and cues | Social opportunity; reflective motivation; physical opportunity | A text message is sent to programme users at 2, 6 and 12 weeks prompting them to keep working towards their physical activity goals and stating that they are capable of achieving them. |
| Exercise buddies and tailored exercise classes (enhanced delivery only) | Social support practical and emotional | Social opportunity; automatic motivation | For programme users in the enhanced delivery areas, Get Active Specialists will also run and/or organise a range of exercise classes based on the preferences of programme users, where they may also be paired with an exercise buddy to help them attend the exercise classes and provide emotional support if needed. |
*Denotes that a BCT was not explicitly linked to a COM-B construct in the consensus study from Cane et al,17 but the authors believe this BCT will impact this area.
BCT, behaviour change technique; COM-B, capability, opportunity and motivation.
Get Active Specialists
One GAS has been employed in each of the four localities for the 3-year duration of the programme. The specialists will work with local GPs and Mind centres to recruit eligible programme users. The specialists all have a minimum of level 3 Register of Exercise Professional and GP Exercise Referral qualifications. The GAS will be further trained so that conversations with programme users can be user-led, involving open-ended questions, which allow programme users to take ownership of setting their own goals, plans and rewards for progress. Consequently, the specialists will receive the following training specific to this programme:
2-day ‘British Heart Foundation: Promoting health behaviour change – A solution focused approach’ course (http://www.bhfactive.org.uk/training-and-events-item/506/index.html)
3-day ‘The Wright Foundation: Obesity and Diabetes’ course (http://www.wrightfoundation.com/spec_ob_di.php)
3-day ‘The Wright Foundation: Level four mental health’ course (http://www.wrightfoundation.com/spec_men.php)
2-day workshop, followed by quarterly 1-day boosters, on motivational interviewing, health coaching and behaviour change led by a Chartered Sport and Exercise and Health Psychologist and Research Fellow (AC, NH)
the two specialists working in the localities with the potential to provide exercise buddies will also attend a 1-day recruiting and retaining volunteer course organised by volunteer centres, Hertfordshire (http://www.volunteeringherts.org.uk/index.php/events/details/12-recruiting-and-retaining-volunteers).
Assessment of fidelity
To ensure fidelity of programme delivery, a number of measures will be put in place. The GAS will record a random sample of consultations and review the audio among themselves, project lead and at quarterly booster sessions with the trainers. The specialists will score each consultation with the Motivational Interviewing Treatment Integrity coding scheme (MITI22) and a checklist of BCTs. The MITI will score the specialists on five domains core to motivational interviewing: evocation—the GAS works proactively to evoke the participant’s own reasons for change; collaboration—the GAS actively fosters and encourages power sharing in the interaction; autonomy/support—the GAS adds significantly to the feeling and meaning of the participant’s expression of autonomy; direction—the GAS resists the righting reflex, yet generally does not miss opportunities to direct participant towards the target behaviour; and empathy—the GAS shows evidence of deep understanding of the participant’s point of view. Every 3 months throughout the duration of the evaluation, the GAS and project lead will meet for booster sessions with a Chartered Sport and Exercise and Health Psychologist and Research Fellow (AC, NH) to review recorded consultations, recap training, discuss any barriers to successful delivery and highlight what is working well.
Outcome measures
Primary outcomes
Physical activity will be measured with the International Physical Activity Questionnaire (IPAQ23). Six questions will assess the level of vigorous and moderate-intensity physical activity and walking of each participant over the last week by asking the amount of time spent being active and on how many days for each, with the minimum being 10 min at a time. The IPAQ allows a metabolic equivalent of task (MET) score to be calculated for each activity type by weighing its energy requirements, with 3.3 METs for walking, 4 METs for moderate-intensity activity and 8 METs for vigorous-intensity activity. A total activity MET score can then be calculated accounting for intensity.24 The IPAQ also asks one question about how much time is spent sitting on a weekday over the last 7 days. An additional two questions will ask about sporting participation over the last week by asking the amount of time spent doing sports and on how many days, with the minimum being 10 min at a time.
Secondary outcomes
Mental well-being will be measured using the Warwick Edinburgh Mental Well-being Scale,25 a 14-item scale exploring thoughts and feelings over the last 2 weeks. Programme users are presented with items such as ‘I’ve been feeling useful’ or ‘I’ve been thinking clearly’, and must rate themselves on a scale from 1 ‘None of the time’ to 5 ‘All of the time’.
Perceptions of health will be measured using the EuroQol EQ-5D-5L,26 which has five domains focusing on mobility, self-care, usual activities, pain/discomfort and anxiety/depression, with one question per domain. Each question has five options to choose from, ranging from no problems to inability to function. An additional question also asks how good or bad programme users perceive their health to be on a scale ranging from 0 (the worst health you can imagine) to 100 (the best health you can imagine).
COM-B measures
All of the COM-B-related scales were validated in a previous study18 and produce a mean score apart for self-efficacy, which produces a total score. Self-monitoring will be measured by two items, which ask programme users to rate how much they agree with statements such as ‘I constantly monitored myself whether I exercise frequently enough’ on a scale from 1 ‘Completely disagree’ to 4 ‘Totally agree’, retrospectively over the past week.27
Action planning will be measured by four items about when, where, how and how often programme users make detailed plans regarding physical activity on a scale from 1 ‘Completely disagree’ to 4 ‘Totally agree’, retrospectively over the past week.28
Self-efficacy will be measured with the Physical Exercise Self-Efficacy Scale,29 which consists of five items exploring programme users’ ability to carry out their behavioural intentions in the face of challenges, such as ‘even when I feel tense’. The items will be measured on a scale from 1 (Very uncertain) to 4 (Very certain).
Intentions will be measured using three items,30 each referring to the amount of physical activity the individual intends to do over the next week, with statements such as ‘I expect to take part in regular physical activity over the next week’. Each item is rated on a 7-point scale from 1 (Strongly disagree) to 7 (Strongly agree).
Attitudes will be measured using four items,30 each referring to the participant’s attitudes towards physical activity in terms of how harmful, healthy, enjoyable and boring they view it on a set of 7-point scales anchored by positive and negative views (eg, 1=very unhealthy to 7=very healthy).
Analytical methods
Outcomes evaluation
The outcomes evaluation will be based on a comparison between recorded values at baseline for the primary and secondary outcomes and those captured at the various follow-up points. The association between exposure to the programme and changes in the primary and secondary outcomes between baseline and postparticipation will be examined using repeated-measures multiple regression models, with covariates including follow-up time point, and whether each participant is in a ‘standard delivery’ or ‘enhanced delivery’ area. An interaction term will be fitted to identify if trends in outcomes by follow-up point differ between the two area types. Differences in baseline characteristics of programme users between the ‘standard’ and ‘enhanced’ delivery areas will be tested using either an independent-samples t-test or a Mann-Whitney U test depending on whether the variable being tested follows a normal distribution. Any potential confounding factors associated with variant characteristics of the two sets of programme users will be adjusted for by inclusion as covariates in the models. If changes in the primary outcome are found, additional regression models will explore whether these changes are driven by changes in COM-B-related measures.
Loss to follow-up is a common problem in this form of evaluation, and the sample of programme users providing data at all follow-up points is likely to differ from those with lower engagement in the evaluation. Depending on the degree of loss to follow-up, a complete case analysis will be undertaken and the results compared with an analysis of all data available, whereby simple mean imputation will be used in the case of missing values. Should the results from the two models show substantial variation, then multiple imputation techniques will be employed.
Process evaluation
A process evaluation is a systematic method of collecting, analysing and using information to understand the functioning of a programme or intervention by examining implementation, mechanisms of impact and contextual factors.31 A process evaluation of Active Herts will take place in three phases, with each phase exploring a different theme. Data will be collected in the form of one-to-one interviews with stakeholders, group interviews with the GAS and focus groups with programme users. Stakeholders interviewed will include commissioners, higher programme management, project delivery partners and health service practitioners.
The initial phase will focus on areas related to the set-up of Active Herts, including developments in the method of recruitment or delivery of the programme, barriers and facilitators to reaching the target audience, partnership working, and engagement with primary and secondary care. The second phase will explore deviations in the programme delivery from those planned, potential mechanisms by which the programme works, and external factors that may influence the programme. A final phase will take on a reflective focus looking back over the programme and considering what worked well and what did not, identifying examples of best practice. It will also consider the future sustainability of Active Herts, including exit routes for programme users and continuation of the programme where appropriate. In all phases, other emerging themes will be explored as identified during the process.
Economic evaluation
The economic evaluation will examine the costs of delivery of the Active Herts programme against the benefits gained in terms of reduced risk of morbidity from a range of chronic conditions, the risk of which is associated with physical inactivity. The ratio of costs to effects—that is, ‘the incremental cost-effectiveness ratio’ (ICER)—will be assessed against a ‘cost-effectiveness threshold’, representing the opportunity cost of spending the money. In the UK, the National Institute for Health and Care Excellence uses a threshold range of £20 000–30 000; if interventions are within this area of cost-effectiveness or below, then they are considered ‘cost-effective’ or good ‘value for money’.
This evaluation will use version 2 (November 2016) of the Sport England MOVES model, a tool for conducting economic analysis of physical activity programmes and interventions developed by the Health Economics Group at the University of East Anglia. The MOVES tool will be used to monetarise the reduced disease burden associated with participation in Active Herts by comparing their predicted disease risk against that of a similar cohort of the population not participating in any programme. The MOVES model will link changes in physical activity (using increases in physical activity energy expenditure due to the programme) with changes in disease prevalence over time for depression, diabetes, stroke, coronary heart disease, dementia, colorectal cancer, breast cancer and hip fracture. The model then assesses the financial return to the National Health Service (NHS) (treatment costs saved) and the health impacts (quality-adjusted life years (QALYs) gained) in the ‘enhanced delivery’ compared with the ‘standard delivery’ area, which are used to calculate indicators of cost-effectiveness: ICER, NHS return on investment and QALYs return on investment.
Ethics and dissemination
All programme users will be provided with a participant information and consent form. Informed written consent will be obtained from all programme users in the evaluation. The results of this study will be published in peer-reviewed journals, presented at national and international conferences, and shared through the study website, and local public health and community sport partnership forums and newsletters.
Discussion
Inactivity is a major issue in England, with large health and economic burdens associated with not participating in the recommended amount of activity. This programme targets inactive adults with additional health problems in areas that would benefit the most from a community physical activity programme. Pragmatic considerations mean that the form of programme delivery differs across programme areas, providing a comparison in the form of a natural experiment. Active Herts incorporates the latest evidence of the BCTs that work both during the participation in the programme and over the longer term to aid sustainable behaviour change. These evidence-based techniques will be combined with an effective delivery approach in motivational interviewing and health coaching that allow discussions to be participant-led so that the programme users take ownership over their goals, progress and rewards. Additionally, this evaluation will measure key drivers of physical activity from the most up-to-date behaviour change theory (COM-B), allowing evaluation of whether physical activity has increased and why. This will provide the basis with which to refine a scalable intervention that could be more robustly tested in a randomised controlled trial.
Supplementary Material
Acknowledgments
The authors would like to thank Adan Freeman and Joe Capon, the project officers, and Fiona Deans, the project manager from Herts Sports Partnership, and the public health lead, Piers Simey, from Hertfordshire County Council. The authors would also like the thank the Get Active Specialists (Lee Bruce, Alison Goodchild, Hannah Marsh and Andrew Rix).
Footnotes
Contributors: NH prepared the draft versions and final manuscript. AC read and provided feedback on the drafts, and approved the final manuscript. APJ prepared the analysis and evaluation sections, read and provided feedback on the drafts, and approved the final manuscript. LB read and provided feedback on the drafts, and approved the final manuscript.
Funding: This work was supported by Sport England (ref: 2015000295), Broxbourne Borough Council, East and North Herts CCG, Herts Valley CCG, Hertfordshire Public Health, Herts Mind Network, Mind in Mid Herts, and Herts Sports Partnership.
Competing interests: None declared.
Ethics approval: This study has been approved by both the Faculty of Medicine and Health Sciences Research Ethics Committee at University of East Anglia (ref: 20152016–28) and by the University of Hertfordshire Health and Human Science Ethics Committee with Delegated Authority (protocol number: LMS/PGR/UH/02427).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Global Recommendations on Physical Activity for Health: World Health Organization, 2010. http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/ (accessed 9 Mar 2017). [PubMed] [Google Scholar]
- 2. Barengo NC, Antikainen R, Borodulin K, et al. Leisure-time physical activity reduces total and cardiovascular mortality and cardiovascular disease incidence in older adults. J Am Geriatr Soc 2017;65:504–10. 10.1111/jgs.14694 [DOI] [PubMed] [Google Scholar]
- 3. Bauman AE. Updating the evidence that physical activity is good for health: an epidemiological review 2000-2003. J Sci Med Sport 2004;7:6–19. 10.1016/S1440-2440(04)80273-1 [DOI] [PubMed] [Google Scholar]
- 4. Schuch FB, Vancampfort D, Richards J, et al. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res 2016;77:42–51. 10.1016/j.jpsychires.2016.02.023 [DOI] [PubMed] [Google Scholar]
- 5. Sporting future – first annual report. 2017. https://www.gov.uk/government/publications/sporting-future-first-annual-report (accessed 9 Mar 2017).
- 6. NHS health and social care information centre. Statistics on obesity, physical activity and diet. 2014. http://content.digital.nhs.uk/catalogue/PUB13648/Obes-phys-acti-diet-eng-2014-rep.pdf (accessed 9 Mar 2017).
- 7. Health and social care information centre. The health survey for England. 2013. http://content.digital.nhs.uk/catalogue/PUB13218 (accessed 9 Mar 2017).
- 8. Giles-Corti B, Donovan RJ. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prev Med 2002;35:601–11. 10.1006/pmed.2002.1115 [DOI] [PubMed] [Google Scholar]
- 9. Wardle J, Griffith J. Socioeconomic status and weight control practices in British adults. J Epidemiol Community Health 2001;55:185–90. 10.1136/jech.55.3.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cassidy S, Chau JY, Catt M, et al. Cross-sectional study of diet, physical activity, television viewing and sleep duration in 233,110 adults from the UK Biobank; the behavioural phenotype of cardiovascular disease and type 2 diabetes. BMJ Open 2016;6:e010038 10.1136/bmjopen-2015-010038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Howlett N, Trivedi D, Troop N, et al. What are the most effective behaviour change techniques to promote physical activity and/or reduce sedentary behaviour in inactive adults? A systematic review and meta-analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Howlett N, Trivedi D, Troop NA, et al. What are the most effective behaviour change techniques to promote physical activity and/or reduce sedentary behaviour in inactive adults? A systematic review protocol. BMJ Open 2015;5:e008573 10.1136/bmjopen-2015-008573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 14. Chater AC. The power of language andemotion in specialist obesity services. Eur Health Psychol 2016;18:184–8. [Google Scholar]
- 15. Rubak S, Sandbaek A, Lauritzen T, et al. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract 2005;55:305–12. [PMC free article] [PubMed] [Google Scholar]
- 16. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cane J, Richardson M, Johnston M, et al. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol 2015;20:130–50. 10.1111/bjhp.12102 [DOI] [PubMed] [Google Scholar]
- 18. Howlett N, Schulz J, Trivedi D, et al. A prospective study exploring the construct and predictive validity of the COM-B model for physical activity. 2017. Journal of Health Psychology. [DOI] [PubMed] [Google Scholar]
- 19. Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 2004;94:361–6. 10.2105/AJPH.94.3.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 21. Public health profiles. Health profile. 2014. http://fingertipsreports.phe.org.uk/health-profiles/2014/e10000015.pdf
- 22. Moyers T, Martin T, Manuel J, et al. Revised global scales:Motivational interviewing treatment integrity 3.1.1. Albuquerque, NM: University of New Mexico, 2010. [Google Scholar]
- 23. Booth ML, Ainsworth BE, Pratt M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;195:3508–1381. [DOI] [PubMed] [Google Scholar]
- 24. International physical activity questionnaire website. Guidelines for data processing and analysis of the international physical activity questionnaire (IPAQ). 2005. https://sites.google.com/site/theipaq/scoring-protocol (accessed 9 Mar 2017). [PubMed]
- 25. Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5:63 10.1186/1477-7525-5-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337–43. 10.3109/07853890109002087 [DOI] [PubMed] [Google Scholar]
- 27. Sniehotta FF, Scholz U, Schwarzer R, et al. Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. Int J Behav Med 2005;12:244–55. 10.1207/s15327558ijbm1204_5 [DOI] [PubMed] [Google Scholar]
- 28. Sniehotta FF, Schwarzer R, Scholz U, et al. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol 2005;35:565–76. 10.1002/ejsp.258 [DOI] [Google Scholar]
- 29. Schwarzer R, Renner B. Health-specific self-efficacy scales. 2009. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.386.5658&rep=rep1&type=pdf (accessed 9 Mar 2017).
- 30. Francis JJ, Eccles MP, Johnston M, et al. Constructing questionnaires based on the theory of planned behaviour. A manual for health services researchers 2004. http://openaccess.city.ac.uk/1735/1/TPB%20Manual%20FINAL%20May2004.pdf (accessed 9 Mar 2017). [Google Scholar]
- 31. Bauman A, Nutbeam D. Evaluation in a nutshell: a practical guide to the evaluation of health promotion programs: Mcgraw hill, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.