Abstract
Objectives
To examine whether self-stigma mediates the relationship between perceived stigma and quality of life, self-esteem and general functioning among outpatients with depression, schizophrenia, anxiety and obsessive-compulsive disorder (OCD).
Design
Cross-sectional survey.
Setting
Outpatient clinics at a tertiary psychiatric hospital in Singapore.
Participants
280 outpatients with a primary clinical diagnosis of either schizophrenia, depression, anxiety or OCD.
Methods
Data were collected in relation to self-stigma, perceived stigma, self-esteem, functioning and quality of life. In order to examine the mediating role of self-stigma on the relationship between perceived stigma and psychosocial outcomes, bootstrapping mediation analyses were used.
Results
Mediation analyses revealed that the relationship between perceived stigma and psychosocial outcomes was subject to the effects of self-stigma among the overall sample. Separate mediation analyses were conducted by diagnoses and showed differences in the mediating effects of self-stigma. Among the whole sample and the subsample with OCD, self-stigma mediated the relationship between perceived stigma and all psychosocial outcomes. For those with anxiety, depression and schizophrenia, the mediating effects of self-stigma were present in all relationships except (1) perceived stigma with physical health in the anxiety sample, (2) perceived stigma with social relationships in the depression sample and (3) perceived stigma with physical health in the schizophrenia sample.
Conclusions
The mediating effects of self-stigma on the relationship between perceived stigma and various psychosocial outcomes are evident and differ across diagnoses. Interventions to address and reduce the effects of self-stigma along with targeted treatments and psychoeducation to assist people with mental illness overcome or better manage self-stigma while providing them the skills to counteract public stigma are needed.
Keywords: mental health, adult psychiatry, public health
Strengths and limitations of this study.
This was a cross-sectional study that adopted a convenient sampling strategy to recruit outpatients with a clinical primary diagnosis of longer than 1 year of schizophrenia, depression, anxiety or obsessive-compulsive disorder.
The mediating role of self-stigma on the relationship between perceived stigma and psychosocial outcomes was examined using bootstrapping mediation analyses.
This is the first study to explore the mediating effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes across psychiatric disorders among a multiethnic Asian sample.
The study has some limitations, including social desirability bias, the cross-sectional design and limited generalisability due to inclusion criteria.
Introduction
Historically, the word ‘stigma’ originates from a Greek term which refers to a ‘mark or brand’. Goffman1 later defined stigma as ‘an attribute that is deeply discrediting’, which reduces someone ‘from a whole and usual person to a tainted, discounted one’ (p3). He goes on to say that stigma is fundamentally a social phenomenon rooted in social relationships that is shaped by the culture and structure of society. While stigma is universal and has no boundaries, it is commonly associated with mental illness. More specifically, Johnstone2 believes ‘people suffering from mental illness and other mental health problems are among the most stigmatized, discriminated against, marginalized, disadvantaged and vulnerable members of society’ (p.200).
In relation to mental illness, stigma is a multifaceted construct that involves feelings, attitudes and behaviours.3 Stigma has been theorised and conceptualised in different ways and from different perspectives. Social cognitive models4 depict stigma as comprising three main components: negative stereotypes (negative beliefs about a particular group), prejudice (agreeing with these negative stereotypes) and discrimination (the behavioural consequence of prejudice).5 Link and Phelan6 adopt a sociological perspective where stigma exists when four interrelated components occur: (1) labelling, (2) negative attributes, (3) separation and (4) status loss and discrimination.
Mental illness stigma can present in four main ways: personal stigma, perceived stigma, self-stigma and structural stigma.5 7 Personal stigma refers to an individual’s stigmatising attitudes and beliefs about people with mental illness, whereby they endorse prejudice and discrimination against them.5 Perceived stigma is the perceived attitudes of others towards people with mental illness.8 Self-stigma or internalised stigma is the process by which people with mental illness accept the negative attitudes of others towards them, then internalise and apply these beliefs to themselves.9–11 Finally structural stigma refers to the prejudice and discrimination by policies, laws and constitutional practices, which intentionally or unintentionally disadvantage people with mental illness.5 12
While stigma can present in different ways, it has been proposed that certain types of stigma will present before others. Link et al13 theorised that public stigma may lead people with mental illness to develop self-stigma, where both forms of stigma have the potential to cause detrimental effects on people with mental illness. Vogel et al14 substantiated this theory when they examined the relationship between public stigma and self-stigma over a 3-month period and found that public stigma is internalised as self-stigma over time, and higher initial public stigma predicted higher subsequent self-stigma. These findings support previous research postulated by modified labelling theory, which has consistently been used to explain the relationship between perceived and self-stigma.13
These types of stigma can have various ramifications for people with mental illness. Negative public attitudes towards people with mental illness can result in delays in treatment-seeking or avoiding treatment altogether,15 while public and perceived stigma are negatively associated with work and role functioning,16 self-esteem17 and quality of life.16 Similarly, self-stigma has also consistently been linked to poorer outcomes among people with mental illness, including reduced quality of life and life satisfaction,18 difficulties obtaining employment and/or housing,19 treatment adherence20 and self-esteem21; self-stigma has also been associated with an increase in symptom severity,22 positive symptoms23 24 and negative symptoms.23 25
In Singapore, a multiethnic city-state in Southeast Asia, there has been increased interest in the stigma of mental illness due to a recent focus on destigmatisation and mental health promotion initiatives. A recent population-wide mental health literacy study revealed there is considerable personal stigma towards people with mental illness, where 89% of people endorsed that people with a mental illness could get better if they wanted to.26 A second study, among psychiatric outpatients with anxiety, depression, obsessive-compulsive disorder (OCD) and schizophrenia, revealed that 43.6% experienced moderate to high self-stigma, while there was a significant negative relationship between quality of life, self-esteem and general functioning and self-stigma.27 These recent studies highlight the magnitude of personal stigma towards and self-stigma among people with mental illness, and the devastating consequences of stigma on outcomes for people with mental illness.
While it is evident how the various types of stigma can have negative impacts on people with mental illness, less is known about how one or more of these types of stigma may influence or affect another. In a recent study among Chinese outpatients with and without psychotic disorders, Kao and colleagues28 examined the mediating role of self-stigma on the relationship between perceived stigma and psychosocial outcomes. Results revealed that self-stigma mediated the effects of perceived stigma on outcomes including self-esteem, depressive symptoms and quality of life.
Given that we already know self-stigma is negatively associated with various psychosocial outcomes including quality of life, self-esteem and general functioning, among psychiatric outpatients in Singapore,27 this raises the questions as to whether this self-stigma influences or mediates the relationship between perceived stigma and psychosocial outcomes. Also given the majority of research to date has focused on depression and schizophrenia,29 there is a need to further explore the effects of stigma on other disorders such as OCD and anxiety. In order to address some of these gaps in the existing literature and to more clearly delineate the relationship between perceived and self-stigma, the current study aimed to examine whether self-stigma mediates the relationship between perceived stigma and quality of life, self-esteem and functioning, among outpatients with anxiety, depression, OCD and schizophrenia.
Methods
Participants and recruitment
This cross-sectional study recruited patients seeking treatment at outpatient and affiliated clinics of the Institute of Mental Health (IMH), the only tertiary psychiatric care hospital in Singapore. Recruitment was conducted between May 2014 and September 2015 and required respondents to meet the following inclusion criteria: Singapore citizens or permanent residents, aged 21–65 years, belonging to Chinese, Malay or Indian ethnicity (the three main ethnic groups in Singapore), capable of providing consent, literate in the English language, and having a clinical primary diagnosis of longer than 1 year of either schizophrenia, depression or anxiety spectrum disorders, or OCD, as determined by a psychiatrist, using the International Classification of Diseases Ninth Revision (ICD-9) criteria. Patients with intellectual disabilities, who were not fluent in English and those who had been seeking treatment at IMH for less than 1 year were excluded. The study employed a convenience sampling strategy to recruit participants using multiple methods and referral sources. Posters informing attending patients of the ongoing study, its eligibility criteria and contact details of the study team were placed in the clinic waiting areas. Psychiatrists and other healthcare professionals were also informed of the study and requested to refer eligible patients. Ethical approval was obtained from the Domain Specific Review Board of the National Healthcare Group, Singapore, and written informed consent was obtained from all respondents.
Measures
Sociodemographic information was collected from all respondents, including age, gender, ethnicity, education, marital and employment status. Medical record reviews were also undertaken to confirm each respondent’s primary diagnosis, age of onset, comorbid psychiatric disorders and number of hospitalisations resulting from their mental illness.
Internalized Stigma of Mental Illness scale
Self-stigma was measured using the Internalized Stigma of Mental Illness (ISMI) scale, which comprises five subscales: alienation, stereotype endorsement, discrimination experience, social withdrawal and stigma resistance.30 The self-report scale uses a 4-point Likert scale from strongly disagree to strongly agree to rate each of the 29 items, which included statements such as ‘Having a mental illness has spoiled my life’ and ‘People without mental illness could not possibly understand me’. As the stigma resistance subscale has not been included in the ISMI total score in several previous studies, given its relatively weak correlation to the other ISMI subscales and its lack of internal consistency,23 30 it was excluded from this analysis. Subscale and total scores were calculated by adding the item scores together and then dividing by the number of answered items. The Cronbach’s alpha in our sample was 0.93.
Devaluation-Discrimination Scale
Perceived public stigma was measured using the 12-item Devaluation-Discrimination Scale, which assesses self-reported stereotype awareness through perceived discrimination and devaluation subscales.31 The scale asks respondents the extent to which they agree or disagree with statements indicating that most people devalue individuals who have used psychiatric treatment. Examples include ‘Most people believe that entering a psychiatric hospital is a sign of personal failure’ and ‘Most people think less of a person after he/she has been hospitalized for a mental illness’. Items are answered on a 6-point response scale from strongly agree (1) to strongly disagree (6). After reverse-scoring items 1, 3, 4, 7, 8 and 11, all item scores are then summed and divided by the total number of items answered. The internal consistency was good among the current sample (Cronbach’s alpha=0.81).
WHO Quality of Life-BREF
The WHO Quality of Life-BREF is a 26-item quality of life scale that measures self-reported overall quality of life and general health. It also measures four distinct quality of life domains—physical health, psychological health, social relationships and environmental aspects—over the 2 weeks prior to the interview.32 All items are constructed on variations of a 5-point Likert scale, with scores from 1 to 5, enquiring on ‘how much’, ‘how completely, ‘how often’, ‘how good’ or ‘how satisfied’ the individual felt. Scores for the four domains are calculated by taking the mean of all items within the domain and multiplying by 4 and then linearly transforming it to a 0–100 scale. For missing items, the mean of other items in the domain is substituted; however, if more than two items were missing from the domain, the domain score was not calculated. Domain scores are scaled in a positive direction, with higher scores denoting higher quality of life except for items 3, 4 and 26, which need to be reverse-scored. The Cronbach’s alpha in our sample for each of the four domains was 0.81 for physical health, 0.84 for psychological health, 0.63 for social relationships and 0.78 for environment.
Rosenberg’s Self-Esteem Scale
Rosenberg’s Self-Esteem Scale (RSES) is a short, 10-item scale that measures self-reported global self-worth by measuring positive and negative feeling about one’s self. Using a 4-point Likert scale from strongly agree (1) through to strongly disagree (4), respondents indicate how strongly they agree or disagree with each of the statements. Negative items are reverse-scored and higher scores indicate greater self-esteem.33 There were two cases with missing items and these were excluded from the analysis. The RSES displayed good internal consistency (Cronbach’s alpha=0.84).
Global Assessment of Functioning
The Global Assessment of Functioning scale34 assesses severity of illness in psychiatry in terms of overall functioning, which takes into account impairments in psychological, social and occupational/school functioning in the month prior to the interview. The scale ranges from 0 (inadequate information) to 100 (superior functioning). The 100-point scale is divided into 10-point intervals, each of which has verbal anchors describing symptoms and functioning pertaining to that interval. Scores between 91 and 100 indicate optimal mental health and coping capabilities, while a score in the 1–10 range may be considered suicidal and incapable of maintaining minimal personal hygiene. Trained raters and members of the study team started at either the top or the bottom of the scale and went up/down the list until the most accurate description of functioning for the individual was reached as per the rater’s judgement.
Statistical analysis
Analysis was performed using SPSS V.21. Mediation (indirect) effects were tested using the PROCESS macro for SPSS developed by Hayes.35 Descriptive statistics were calculated to provide an overview of the sociodemographic, clinical and psychosocial (self-stigma, perceived stigma, self-esteem, functioning and quality of life) characteristics of the sample by the four diagnoses: anxiety, depression, OCD and schizophrenia. Analysis of variance (ANOVA) followed by the appropriate post-hoc tests were conducted to identify significant difference in the means of each psychosocial variable across the four diagnostic groups. The psychosocial variables were normally distributed; hence, the associations between these were examined using Pearson’s correlation.
The mediation (indirect) effect model hypothesised in this study is illustrated in figure 1, which examines the mediating role of self-stigma, and is similar to that reported by Kao et al.28 The relationships between perceived stigma (independent variable) and psychosocial outcomes such as self-esteem, functioning and quality of life (depicted by four domains: physical health, psychological health, social relationships and environment) (dependent variables) without controlling for self-stigma (mediator variable) are referred to as total effects and denoted by ‘z’. The relationships between perceived stigma and the psychosocial outcomes controlling for self-stigma are referred to as direct effects denoted by ‘z*’. Indirect effects denoted by ‘xy’ refer to the relationships between perceived stigma and the psychosocial outcomes with self-stigma as the mediator. Applying the PROCESS macro, it conducts bias-corrected bootstrapping through random sampling with replacement from the data set to create pseudo-bootstrap samples, which produce point estimates for the mediation effects as well as their bias-corrected and accelerated 95% CI. The study used 5000 bootstrap samples. When the CI does not contain 0, it could be inferred that the mediation effect of the proposed mediator is statistically significant.36 The mediation analyses were controlled for age, age of onset, gender, ethnicity, marital status, education, employment, comorbid psychiatric disorders and hospitalisation history.
Figure 1.
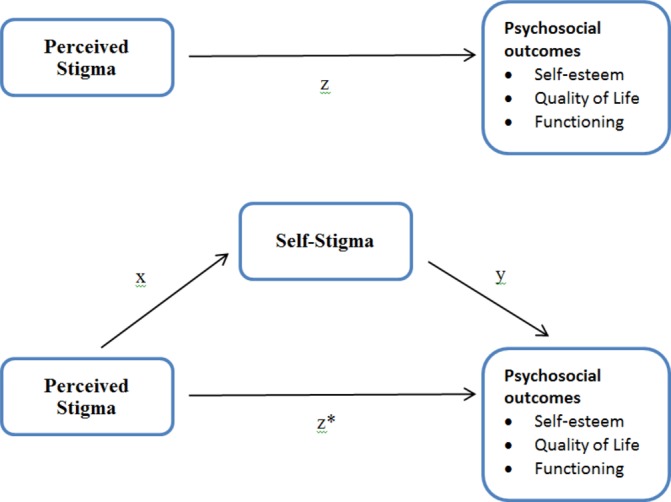
Mediation effect model.
The entire sample was first used to test the mediation effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes. Thereafter, we examined the four diagnostic groups separately to explore if there were any differences in mediation effects between diagnoses.
Results
The sociodemographic and clinical characteristics of the sample (n=280) are presented in table 1. The majority of respondents were male (54.6%), of Chinese ethnicity (53.6%), never married (63.1%) and employed (55.7%). The mean age of the respondents was 38.9 years (SD=11.6 years).
Table 1.
Sample characteristics by diagnosis
| Anxiety, n (%) |
Depression, n (%) |
OCD, n (%) |
Schizophrenia, n (%) |
Total sample, n (%) |
|
| Gender | |||||
| Male | 41 (57.7) | 36 (48.6) | 38 (62.3) | 38 (51.4) | 153 (54.6) |
| Female | 30 (42.3) | 38 (51.4) | 23 (37.7) | 36 (48.6) | 127 (45.4) |
| Ethnicity | |||||
| Chinese | 50 (70.4) | 25 (33.8) | 49 (80.3) | 26 (35.1) | 150 (53.6) |
| Malay | 10 (14.1) | 25 (33.8) | 6 (9.8) | 24 (32.4) | 65 (23.2) |
| Indian/Others | 11 (15.5) | 24 (2.4) | 6 (9.8) | 24 (32.4) | 65 (23.2) |
| Marital status | |||||
| Never married | 51 (71.8) | 23 (31.1) | 50 (82.0) | 52 (71.2) | 176 (63.1) |
| Married | 14 (19.7) | 24 (32.4) | 6 (9.8) | 14 (19.2) | 58 (20.8) |
| Separated/divorced/widowed | 6 (8.5) | 27 (36.5) | 5 (8.2) | 7 (9.6) | 45 (16.1) |
| Education | |||||
| Primary and below | 3 (4.2) | 6 (8.2) | 1 (1.6) | 9 (12.2) | 19 (6.8) |
| Secondary or O/N *level | 13 (18.3) | 28 (38.4) | 18 (29.5) | 34 (45.9) | 93 (33.3) |
| A level/diploma | 43 (60.6) | 26 (35.6) | 28 (45.9) | 27 (36.5) | 124 (44.4) |
| University | 12 (16.9) | 13 (17.8) | 14 (23.0) | 4 (5.4) | 43 (15.4) |
| Employment status | |||||
| Employed | 42 (59.2) | 40 (54.1) | 37 (60.7) | 37 (50.0) | 156 (55.7) |
| Unemployed | 17 (24) | 8 (36.4) | 17 (27.9) | 29 (39.2) | 90 (32.1) |
| Student/home maker/retired | 12 (16.9) | 7 (9.5) | 7 (11.5) | 8 (10.8) | 34 (12.1) |
| Hospitalisation | |||||
| Yes | 9 (12.9) | 28 (39.4) | 25 (42.4) | 61 (88.4) | 123 (45.7) |
| No | 61 (87.1) | 43 (60.6) | 34 (57.6) | 8 (11.6) | 146 (54.3) |
| Comorbid psychiatric disorder | |||||
| Yes | 38 (53.5) | 25 (33.8) | 36 (59.0) | 11 (14.9) | 110 (39.3) |
| No | 33 (46.5) | 49 (66.2) | 25 (41.0) | 63 (85.1) | 170 (60.7) |
| Age (mean, SD) | 33.6 (10.9) | 42.2 (10.8) | 32.5 (9.45) | 43.0 (10.4) | 38.9 (11.6) |
| Age of onset of illness | 28.8 (9.42) | 35.6 (10.8) | 25.4 (10.0) | 25.7 (7.94) | 29.5 (10.4) |
*O/N level is the equivalent to up to 11 years of education
OCD, obsessive-compulsive disorder.
The psychosocial characteristics of the sample are presented in table 2. ANOVA on the psychosocial variables yielded significant differences among the diagnostic groups, with the exception of self-stigma which was not different across diagnoses. Post-hoc tests revealed that the mean self-esteem scores were higher in participants with schizophrenia than depression. Participants with schizophrenia had lower mean perceived stigma and physical health scores as compared with the other diagnostic groups, while they had higher mean psychological health and social relationships scores as compared with those with depression. The results were significant and reported at p<0.05. To determine the correlations between the various stigma and psychosocial measures, Pearson’s correlations were performed (table 3). Results showed that perceived stigma, self-stigma, self-esteem, quality of life and functioning were significantly associated with each other.
Table 2.
Stigma and psychosocial outcomes among people with mental illness by disorder
| Mean (SD) | Anxiety | Depression | OCD | Schizophrenia | Total sample |
| ISMI | 2.23 (0.56) | 2.44 (0.55) | 2.41 (0.49) | 2.41 (0.52) | 2.37 (0.54) |
| DDS | 48.5 (9.52) | 49.0 (8.96) | 48.1 (10.0) | 42.5 (11.6) | 46.9 (10.4) |
| RSES | 26.5 (6.31) | 25.4 (5.34) | 25.6 (5.67) | 27.7 (4.13) | 26.3 (5.45) |
| GAF | 55.9 (15.9) | 50.0 (17.6) | 53.33 (13.5) | 54.3 (16.0) | 53.4 (16.0) |
| WHOQOL-BREF | |||||
| Physical health | 53.4 (13.3) | 50.4 (11.8) | 51.4 (14.0) | 60.4 (11.5) | 54.0 (13.2) |
| Psychological health | 49.1 (15.0) | 47.1 (16.4) | 48.6 (15.7) | 54.2 (16.1) | 49.8 (16.0) |
| Social relationships | 54.5 (22.6) | 48.8 (24.6) | 53.6 (21.6) | 59.8 (18.8) | 54.2 (22.3) |
| Environmental | 63.5 (16.9) | 56.5 (17.9) | 61.6 (16.1) | 63.1 (15.1) | 61.1 (16.7) |
DDS, Devaluation-Discrimination Scale (perceived stigma); GAF, Global Assessment of Functioning; ISMI, Internalized Stigma of Mental Illness Scale (self-stigma); OCD, Obsessive-compulsive disorder; RSES, Rosenberg’s Self-Esteem Scale; WHOQOL-BREF, WHO Quality of Life-BREF.
Table 3.
Correlations among study variables
| Self-stigma | Perceived stigma | Self-esteem | Physical health | Psychological health | Social relationships | Environmental | GAF | |
| Self-stigma | – | |||||||
| Perceived stigma | 0.269 | – | ||||||
| Self-esteem | −0.576 | −0.305 | – | |||||
| Quality of life | ||||||||
| Physical health | −0.316 | −0.309 | 0.483 | – | ||||
| Psychological health | −0.518 | −0.313 | 0.659 | 0.646 | – | |||
| Social relationships | −0.453 | −0.280 | 0.511 | 0.520 | 0.604 | – | ||
| Environmental | −0.512 | −0.180 | 0.535 | 0.529 | 0.645 | 0.553 | – | |
| GAF | −0.401 | −0.133 | 0.434 | 0.419 | 0.462 | 0.454 | 0.497 | – |
All correlations are significant at the 0.001 level (two-tailed).
GAF, Global Assessment of Functioning.
The results of the mediation analyses are presented in table 4. Among the overall sample, the significant (p<0.05) total effects (z) of perceived stigma on self-esteem, functioning, physical health, psychological health, social relationships and environment were −0.187, –0.302, −0.330, –0.506, −0.626 and −0.450, respectively. When self-stigma was entered simultaneously into the model (z*), the direct effects (z*) of perceived stigma on psychosocial outcomes decreases to −0.062, –0.873, −0.187, –0.192, −0.291 and −0.155, respectively, implying the negative effects of perceived stigma on the psychosocial outcomes had weakened. In other words, the relationship between perceived stigma and the psychosocial outcomes is subjected to the effects of self-stigma.
Table 4.
Mediating effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes
| Outcomes | Total effects | Direct effects | Indirect effects | Mediation ratio‡ | ||||
| z | SE | z* | SE | xy | SE | CI | ||
| Total sample | ||||||||
| Self-esteem | −0.186*** | 0.032 | −0.061* | 0.028 | −0.126† | 0.021 | (−0.170 to –0.089) | 0.674 |
| Functioning | −0.299** | 0.095 | −0.085 | 0.097 | −0.214† | 0.046 | (−0.316 to –0.136) | 0.716 |
| Quality of life | ||||||||
| Physical health | −0.332*** | 0.076 | −0.192** | 0.080 | −0.140† | 0.037 | (−0.225 to –0.077) | 0.422 |
| Psychological health | −0.510*** | 0.094 | −0.196* | 0.088 | −0.314† | 0.052 | (−0.429 to –0.223) | 0.616 |
| Social relationships | −0.623*** | 0.130 | −0.289* | 0.131 | −0.335† | 0.069 | (−0.492 to –0.218) | 0.537 |
| Environmental | −0.450*** | 0.097 | −0.158 | 0.094 | −0.292† | 0.054 | (−0.407 to –0.193) | 0.650 |
| Anxiety | ||||||||
| Self-esteem | −0.298*** | 0.066 | −0.119 | 0.068 | −0.179† | 0.050 | (−0.297 to –0.094) | 0.601 |
| Functioning | −0.458* | 0.198 | −0.213 | 0.230 | −0.245† | 0.131 | (−0.560 to –0.028) | 0.536 |
| Quality of life | ||||||||
| Physical health | −0.499** | 0.160 | −0.384* | 0.190 | −0.115 | 0.119 | (−0.357 to 0.120] | |
| Psychological health | −0.613*** | 0.170 | −0.306 | 0.189 | −0.307† | 0.116 | (−0.588 to –0.114) | 0.501 |
| Social relationships | −0.918*** | 0.254 | −0.541 | 0.290 | −0.377† | 0.170 | (−0.793 to –0.112) | 0.411 |
| Environmental | −0.604** | 0.208 | −0.062 | 0.212 | −0.543† | 0.187 | (−0.966 to –0.246) | 0.898 |
| Depression | ||||||||
| Self-esteem | −0.199* | 0.080 | −0.097 | 0.075 | −0.103† | 0.051 | (−0.225 to –0.022) | 0.515 |
| Functioning | −0.444* | 0.219 | −0.213 | 0.214 | −0.231† | 0.128 | (−0.561 to –0.040) | 0.521 |
| Quality of life | ||||||||
| Physical health | −0.420** | 0.144 | −0.300 | 0.145 | −0.120† | 0.067 | (−0.296 to –0.020) | 0.286 |
| Psychological health | −0.590* | 0.242 | −0.250 | 0.217 | −0.340† | 0.149 | (−0.690 to –0.097) | 0.576 |
| Social relationships | −0.777* | 0.373 | −0.499 | 0.381 | −0.279 | 0.200 | (−0.782 to 0.019] | |
| Environmental | −0.707** | 0.244 | −0.454 | 0.239 | −0.253† | 0.131 | (−0.573 to –0.051) | 0.358 |
| OCD | ||||||||
| Self-esteem | −0.155* | 0.078 | −0.059 | 0.067 | −0.096† | 0.046 | (−0.196 to –0.016) | 0.621 |
| Functioning | −0.237 | 0.177 | −0.120 | 0.179 | −0.117† | 0.076 | (−0.309 to –0.036) | 0.493 |
| Quality of life | ||||||||
| Physical health | −0.370 | 0.199 | −0.244 | 0.203 | −0.126† | 0.083 | (−0.377 to –0.014) | 0.341 |
| Psychological health | −0.347 | 0.208 | −0.129 | 0.195 | −0.218† | 0.115 | (−0.495 to –0.038) | 0.630 |
| Social relationships | −0.582* | 0.276 | −0.241 | 0.243 | −0.342† | 0.165 | (−0.705 to –0.061) | 0.587 |
| Environmental | −0.325 | 0.214 | −0.153 | 0.211 | −0.173† | 0.088 | (−0.417 to –0.042) | 0.531 |
| Schizophrenia | ||||||||
| Self-esteem | −0.115* | 0.051 | −0.006 | 0.046 | −0.109† | 0.039 | (−0.204 to –0.046) | 0.949 |
| Functioning | 0.085 | 0.182 | 0.216 | 0.199 | −0.130† | 0.095 | (−0.370 to –0.018) | −1.528 |
| Quality of life | ||||||||
| Physical health | −0.129 | 0.144 | −0.077 | 0.160 | −0.052 | 0.072 | (−0.243 to 0.071] | |
| Psychological health | −0.539** | 0.187 | −0.251 | 0.187 | −0.288† | 0.113 | (−0.575 to –0.109) | 0.535 |
| Social relationships | −0.266 | 0.214 | −0.032 | 0.228 | −0.234† | 0.120 | (−0.543 to –0.042) | 0.879 |
| Environmental | −0.251 | 0.166 | −0.062 | 0.176 | −0.189† | 0.105 | (−0.480 to –0.029) | 0.753 |
The relationships between perceived stigma and the psychosocial outcomes controlling for self-stigma are referred to as direct effects denoted by z*.
*Significant at p value <0.05, **significant at p value <0.01, ***significant at p value <0.001.
†CI does not contain 0.
‡Ratio of the indirect effect to the total effect.
OCD, obsessive-compulsive disorder.
After conducting separate mediation analyses on each of the four diagnostic groups, the results presented in table 4 suggest that the mediating effects of self-stigma differed by diagnosis. Among the whole sample and the subsample with OCD, self-stigma mediated the relationship between perceived stigma and all psychosocial outcomes. For those with anxiety, depression and schizophrenia, the mediating effects of self-stigma were present in all relationships except (1) perceived stigma with physical health in the anxiety sample, (2) perceived stigma with social relationships in the depression sample and (3) perceived stigma with physical health in the schizophrenia sample. The controlled variables that were significant in each of the mediation analyses are presented in online supplementary table 1.
bmjopen-2017-018228supp001.pdf (48KB, pdf)
Discussion
To our knowledge, this is the first study to examine the mediating effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes among a multiethnic Asian sample of outpatients with anxiety, depression, OCD and schizophrenia. Results revealed significant differences in stigma and psychosocial mean scores across diagnostic groups. Furthermore, results showed that self-stigma mediated the effects of perceived stigma on psychosocial outcomes including self-esteem, quality of life and functioning. Differences in the mediation effect were also observed when the sample was split by diagnostic groups, with self-stigma having no mediating effect on several psychosocial outcomes.
Across the different diagnostic groups, we observed significant differences in mean self-stigma, perceived stigma and psychosocial scores. Overall, those with depression had higher self and perceived stigma scores and lower psychosocial scores compared with other diagnostic groups. More specifically, mean self-esteem, psychological health and social relationships scores were significantly lower among those with depression compared with those with schizophrenia. Research has shown that self-stigma is associated with increased depression,37 which may partly explain the current findings. On the other hand, schizophrenia is associated with a lack of insight or awareness38 and may also be a contributing factor. There is a dearth of research exploring differences in self and perceived stigma and psychosocial outcomes across psychiatric disorders, and given the obvious differences observed in the current study this warrants further exploration in the future to ascertain why such differences may occur.
Mediation analysis revealed that while perceived stigma and self-stigma are distinct constructs, they are related. The current study specifically examined how self-stigma mediates the relationship between perceived stigma and quality of life, self-esteem and functioning. Among the overall sample we observed the mediating effects of self-stigma, whereby it reduced the effects of perceived stigma on self-esteem, quality of life and functioning, and higher self-stigma scores were associated with lower scores among the psychosocial outcome measures. In other words, the effects of perceived stigma on these psychosocial outcomes are mediated by internalising public stigma among those with mental illness. Our findings are in line with Kao et al,28 who also observed the effects of perceived stigma on psychosocial outcomes was mediated by self-stigma. These findings highlight the importance and impact self-stigma can have for people with mental illness and its predictive influence on psychosocial outcomes. Given that self-stigma is the internalisation of public beliefs and stigmatising views,39 40 efforts to dispel misconceptions relating to mental illness among the general population are needed. At the same time, counteracting the negative effects of self-stigma among people with mental illness is also needed. Mittal et al41 undertook a review of strategies to reduce self-stigma among people with mental illness and concluded that two prominent approaches for self-stigma reduction emerged. The first being interventions that attempt to alter the stigmatising beliefs and attitudes of those experiencing self-stigma, while the second related to enhancing coping skills through improvements in self-esteem, empowerment and help-seeking behaviour; given the findings of this study, such interventions need to be considered for the local population.
When the sample was split by diagnostic groups, distinct differences in the effects of self and perceived stigma were observed. The mediating effects of self-stigma among those with anxiety and depression was not dissimilar to that observed for the overall sample. There was no mediating effect of self-stigma on the physical health quality of life domain for those with anxiety, nor was there a mediating effect on the social relationships quality of life domain for those with depression. Items within the physical health domain ask about tangible aspects of physical health such as pain, the need for medical treatment to function, ability to get around, energy levels and satisfaction with sleep, ability to perform daily living activities, and capacity for work. So while perceived stigma is a significant predictor of the physical health domain and people with anxiety may internalise stigmatising views, it was found that this relationship was not influenced by self-stigma.
The same applies for those with depression and the social relationships domain, whereby perceived stigma is negatively associated with this quality of life domain, yet the relationship is not influenced by self-stigma. Interestingly, while the mean social relationships score was significantly lower among those with depression (vs schizophrenia), self-stigma did not appear to be an influencing factor. It is possible that while those with depression had higher mean self and perceived stigma scores, self-stigma did not affect their social relationships, but rather the impact of what others think (perceived stigma) is more influential to social relationships. Contrary to this, however, longitudinal evidence has shown that self-stigma has a stronger effect on the psychosocial outcomes of people with mental illness compared with perceived stigma.11 Given that little is known about the effects of stigma on various psychosocial outcomes over time, and how this may in fact influence the mediating effects of self-stigma on these outcomes, this warrants further exploration in the future to better understand the complex interplays between these constructs.
Among those with schizophrenia, both self-stigma and perceived stigma did not have a significant effect on physical health-related quality of life. Although people with schizophrenia may experience perceived or self-stigma, perceived stigma is not associated with physical health-related quality of life, and self-stigma does not mediate the relationship between perceived stigma and this psychosocial outcome. These findings suggest it is likely that other factors such as symptom severity or coping methods may influence physical health-related quality of life among those with schizophrenia. Therefore, while it is important to address self-stigma given that it does influence the relationship between perceived stigma and most psychosocial outcomes, people with different mental illnesses may perceive or experience stigma in unique ways. Previous literature has also shown that self-stigma is negatively associated with quality of life among those with schizophrenia,27 42 and this further compounds the impact it can have on this and other psychosocial outcomes.
Unlike other mental illnesses such as depression or schizophrenia, there has been substantially less literature published on stigma relating to OCD, and therefore little is known about the magnitude or impact of stigma on psychosocial outcomes for people with OCD. Among those with OCD in the current sample, while the mediating effects of self-stigma were present, perceived stigma was not associated with any of the psychosocial outcomes. That is, while perceived stigma does not seem to have an impact on the psychosocial outcomes of people with OCD, self-stigma still has a mediating effect and further reduces the impact perceived stigma has on self-esteem, quality of life and functioning. It is difficult to postulate why this lack of association would be observed, and to our knowledge there is no empirical evidence that has previously explored this. Some possible explanations are proposed. It could be that people with OCD disassociate the disorder from negative public conceptions of ‘mental illness’ and perceive OCD as a less serious or dangerous condition,43 and consequently perceived stigma has no effects on psychosocial outcomes. Similarly it could be that those with OCD learn to distinguish between OCD thoughts and real thoughts, resulting in these people being able to reduce self-stigma by disassociating the OCD from oneself.43 An alternative explanation could be that public stigma towards OCD in Singapore is lower compared with other disorders,26 which may result in less perceived and self-stigma among those with the disorder. Finally while OCD refers to unwanted recurrent and persistent thoughts, urges, or impulses and/or repetitive behaviours that an individual feels driven to perform,44 these thoughts or behaviours can relate to a broad range of areas. It is therefore possible that this subgroup with OCD forms quite a heterogeneous group in terms of their specific OCD symptoms, which may result in variance in the extent to which they experience self or perceived stigma. Given the impact of stigma on people with OCD is hugely understudied and that findings from the current study highlight distinct differences in the mediating effects of self-stigma on the relationship of perceived stigma and psychosocial outcomes, further research is needed to explore this phenomenon further.
It is important to note that this study is not without its limitations. Stigma and psychosocial variables were all self-reported, which can result in social desirability bias. The cross-sectional design of our study precluded any causal inferences being made. Furthermore, while the majority of investigations exploring mediation are based on cross-sectional designs, there are certain limitations to this study design, particularly in capturing true mediation processes,45 and these should be considered when interpreting the study findings. In addition, sampling was also based on convenient sampling methods among a heterogeneous group of patients with anxiety, depression, OCD and schizophrenia, and was also restricted to English-speaking patients, aged 21–65, who were seeking care at IMH, and therefore our results may not be generalisable to all patients with mental illness in Singapore. The primary clinical diagnoses of the disorders were determined by a psychiatrist, using the ICD-9 criteria, which has been superseded by ICD-10. Consequently, the two versions use slightly different criteria for classification of mental disorders, and therefore it is possible that in some instances those with an ICD-9 diagnosis in the current study would be diagnosed somewhat differently, or possibly excluded, according to ICD-10 classifications. As the primary aim of the study was to explore the types and extent of stigma experienced by people with mental illness, we did not collect information on severity of illness or physical comorbidities, which may impact perceived stigma, self-stigma or psychosocial outcomes. Accordingly, it would be beneficial to further explore the effects of symptom severity and physical comorbidities on stigma and psychosocial outcomes in the future. Finally, as this was a treatment-seeking population, it is possible that the extent of perceived and self-stigma may be inflated or may not be a true reflection of these types of stigma among people with mental illness.
Despite these limitations, this is to our knowledge the first study to explore the mediating effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes across psychiatric disorders among a multiethnic Asian sample. Findings have highlighted that the relationship between perceived stigma and various psychosocial outcomes was subjected to the effects of self-stigma, while the effects of perceived and self-stigma differ across diagnoses.
While perceived stigma contributes to self-stigma, both types of stigma can have pernicious effects on various outcomes for people with mental illness. Given that self-stigma mediates the relationship between perceived stigma and various psychosocial outcomes, and that existing literature has shown self-stigma is considered a risk factor for poorer mental health prognosis,46 it is important that interventions aim to address and reduce the effects of self-stigma among people with mental illness. There is a need for targeted treatments and psychoeducation that aim to assist people with mental illness overcome or better manage self-stigma while providing them the skills to counteract public stigma.11
The repercussions of self and/or perceived stigma are also often responsible for delayed help-seeking or treatment avoidance and further exemplify the damaging effects stigma can have for people with mental illness. A better understanding of how these different stigma constructs relate to each other over time, and how they might differ across disorders, will provide important information and guidance for designing interventions at the individual and societal level aimed at reducing stigma associated with mental illness and will aid to reduce barriers to help-seeking.14
Supplementary Material
Footnotes
Contributors: LP was responsible for the study design, data collection and verification, and wrote the manuscript. YWL and EA were involved in the data analysis and interpretation and provided inputs into the manuscript. SP and JAV were involved in data collection and clean-up, and provided inputs and edits to the manuscript. SAC and MS supervised the overall study and provided intellectual inputs on the manuscript.
Competing interests: None declared.
Patient consent: Obained.
Ethics approval: National Healthcare Group Domain Specific Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are not available for online access; however, readers who wish to gain access to the data can write to the senior author (MS) at mythily@imh.com.sg with their requests. Access can be granted subject to the Institutional Review Board (IRB) and the research collaborative agreement guidelines. This is a requirement mandated for this research study by our IRB and funders.
References
- 1. Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York: Simon and Schuster Inc, 1963. [Google Scholar]
- 2. Johnstone MJ. Stigma, social justice and the rights of the mentally ill: challenging the status quo. Aust N Z J Ment Health Nurs 2001;10:200–9. 10.1046/j.1440-0979.2001.00212.x [DOI] [PubMed] [Google Scholar]
- 3. Penn DL, Martin J. The stigma of severe mental illness: Some potential solutions for a recalcitrant problem. Psychiatr Q 1998;69:235–47. 10.1023/A:1022153327316 [DOI] [PubMed] [Google Scholar]
- 4. Corrigan PW. Mental Health Stigma as Social Attribution: Implications for Research Methods and Attitude Change. Clinical Psychology: Science and Practice 2000;7:48–67. 10.1093/clipsy.7.1.48 [DOI] [Google Scholar]
- 5. Rusch N, Thornicroft G. Does stigma impair prevention of mental disorders? The British Journal of Psychiatry 2014;204:249–51. 10.1192/bjp.bp.113.131961 [DOI] [PubMed] [Google Scholar]
- 6. Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Sociol 2001;27:363–85. 10.1146/annurev.soc.27.1.363 [DOI] [Google Scholar]
- 7. Overton SL, Medina SL. The Stigma of Mental Illness. Journal of Counseling & Development 2008;86:143–51. 10.1002/j.1556-6678.2008.tb00491.x [DOI] [Google Scholar]
- 8. Griffiths KM, Batterham PJ, Barney L, et al. . The generalised anxiety stigma scale (GASS): psychometric properties in a community sample. BMC Psychiatry 2011;11:184–93. 10.1186/1471-244X-11-184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Corrigan P, Watson A. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002;1:16–20. [PMC free article] [PubMed] [Google Scholar]
- 10. Corrigan PW, Watson AC, Barr L et al. . The Self–Stigma of Mental Illness: Implications for Self–Esteem and Self–Efficacy. J Soc Clin Psychol 2006;25:875–84. 10.1521/jscp.2006.25.8.875 [DOI] [Google Scholar]
- 11. Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res 2004;129:257–65. 10.1016/j.psychres.2004.08.003 [DOI] [PubMed] [Google Scholar]
- 12. Pescosolido BA, Martin JK. The Stigma Complex. Annu Rev Sociol 2015;41:87–116. 10.1146/annurev-soc-071312-145702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Link BG, Cullen FT, Struening E, et al. . A modified labeling theory approach to mental disorders: An empirical assessment. Am Sociol Rev 1989;54:400–23. 10.2307/2095613 [DOI] [Google Scholar]
- 14. Vogel DL, Bitman RL, Hammer JH, et al. . Is stigma internalized? The longitudinal impact of public stigma on self-stigma. J Couns Psychol 2013;60:311–6. 10.1037/a0031889 [DOI] [PubMed] [Google Scholar]
- 15. Corrigan P, Pw C. How stigma interferes with mental health care. Am Psychol 2004;59:614–25. 10.1037/0003-066X.59.7.614 [DOI] [PubMed] [Google Scholar]
- 16. Alonso J, Buron A, Rojas-Farreras S, et al. . Perceived stigma among individuals with common mental disorders. J Affect Disord 2009;118:180–6. 10.1016/j.jad.2009.02.006 [DOI] [PubMed] [Google Scholar]
- 17. Cy O, Lee BO. Relationship between perceived stigma, coping orientations, self esteem and quality of life in patients with schizophrenia. Asia Pac J Public Health 2015;27:1932–41. [DOI] [PubMed] [Google Scholar]
- 18. Świtaj P, Wciórka J, Smolarska-Świtaj J, et al. . Extent and predictors of stigma experienced by patients with schizophrenia. European Psychiatry 2009;24:513–20. 10.1016/j.eurpsy.2009.06.003 [DOI] [PubMed] [Google Scholar]
- 19. Wahl OF. Mental Health Consumers’ Experience of Stigma. Schizophr Bull 1999;25:467–78. 10.1093/oxfordjournals.schbul.a033394 [DOI] [PubMed] [Google Scholar]
- 20. Fung KMT, Tsang HWH, Chan F. Self-stigma, stages of change and psychosocial treatment adherence among Chinese people with schizophrenia: a path analysis. Soc Psychiatry Psychiatr Epidemiol 2010;45:561–8. 10.1007/s00127-009-0098-1 [DOI] [PubMed] [Google Scholar]
- 21. Vauth R, Kleim B, Wirtz M, et al. . Self-efficacy and empowerment as outcomes of self-stigmatizing and coping in schizophrenia. Psychiatry Res 2007;150:71–80. 10.1016/j.psychres.2006.07.005 [DOI] [PubMed] [Google Scholar]
- 22. Wws M, Cfm W. Cognitive insight and casual attribution in the development of self-stigma among individuals with schizophrenia. Psychiatr Serv 2006;57:1800–2. [DOI] [PubMed] [Google Scholar]
- 23. Lysaker PH, Davis LW, Warman DM, et al. . Stigma, social function and symptoms in schizophrenia and schizoaffective disorder: Associations across 6 months. Psychiatry Res 2007;149:89–95. 10.1016/j.psychres.2006.03.007 [DOI] [PubMed] [Google Scholar]
- 24. Yanos PT, Roe D, Markus K, et al. . Pathways Between Internalized Stigma and Outcomes Related to Recovery in Schizophrenia Spectrum Disorders. Psychiatric Services 2008;59:1437–42. 10.1176/ps.2008.59.12.1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lysaker PH, Vohs JL, Tsai J. Negative symptoms and concordant impairments in attention in schizophrenia: Associations with social functioning, hope, self-esteem and internalized stigma. Schizophr Res 2009;110:165–72. 10.1016/j.schres.2009.01.015 [DOI] [PubMed] [Google Scholar]
- 26. Subramaniam M, Abdin E, Picco L, et al. . Stigma towards people with mental disorders and its components – a perspective from multi-ethnic Singapore. Epidemiology and Psychiatric Sciences 2016:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Picco L, Pang S, Lau YW, et al. . Internalized stigma among psychiatric outpatients: Associations with quality of life, functioning, hope and self-esteem. Psychiatry Res 2016;246:500–6. 10.1016/j.psychres.2016.10.041 [DOI] [PubMed] [Google Scholar]
- 28. Kao Y-C, Lien Y-J, Chang H-A, et al. . Evidence for the indirect effects of perceived public stigma on psychosocial outcomes: The mediating role of self-stigma. Psychiatry Res 2016;240:187–95. 10.1016/j.psychres.2016.04.030 [DOI] [PubMed] [Google Scholar]
- 29. Grant JB, Bruch CP, Batterham PJ, et al. . perceived and self-stigma towards anxiety and depression. Epidemiology and Psychiatric Sciences 2016;25:247–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Boyd Ritsher J, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res 2003;121:31–49. 10.1016/j.psychres.2003.08.008 [DOI] [PubMed] [Google Scholar]
- 31. Link BG. Understanding Labeling Effects in the Area of Mental Disorders: An Assessment of the Effects of Expectations of Rejection. Am Sociol Rev 1987;52:96–112. 10.2307/2095395 [DOI] [Google Scholar]
- 32. World Health Organization. The World Health Organisation Quality of Life (WHOQOL)-BREF: World Health Organisation, 2004. [Google Scholar]
- 33. Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press, 1965. [Google Scholar]
- 34. Dufton BD, Siddique CM. Measures in the day hospital: I. The Global Assessment of Functioning Scale. Int J Part Hosp 1992;8:41–9. [PubMed] [Google Scholar]
- 35. Hayes A. An Introduction to Mediation, Moderation, and Conditional Process Analyses: A Regression-Based Approach. New York: Guilford, 2013. [Google Scholar]
- 36. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput 2004;36:717–31. 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- 37. Manos RC, Rusch LC, Kanter JW, et al. . Depression Self-Stigma as a Mediator of the Relationship Between Depression Severity and Avoidance. J Soc Clin Psychol 2009;28:1128–43. 10.1521/jscp.2009.28.9.1128 [DOI] [Google Scholar]
- 38. David AS. Insight and psychosis. Br J Psychiatry 1990;156:798–808. 10.1192/bjp.156.6.798 [DOI] [PubMed] [Google Scholar]
- 39. Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med 2010;71:2150–61. 10.1016/j.socscimed.2010.09.030 [DOI] [PubMed] [Google Scholar]
- 40. Vogel DL, Wade NG, Hackler AH et al. . Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. J Couns Psychol 2007;54:40–50. 10.1037/0022-0167.54.1.40 [DOI] [Google Scholar]
- 41. Mittal D, Sullivan G, Chekuri L, et al. . Empirical Studies of Self-Stigma Reduction Strategies: A Critical Review of the Literature. Psychiatric Services 2012;63:974–81. 10.1176/appi.ps.201100459 [DOI] [PubMed] [Google Scholar]
- 42. Cavelti M, Kvrgic S, Beck E-M, et al. . Self-stigma and its relationship with insight, demoralization, and clinical outcome among people with schizophrenia spectrum disorders. Compr Psychiatry 2012;53:468–79. 10.1016/j.comppsych.2011.08.001 [DOI] [PubMed] [Google Scholar]
- 43. Fennell D, Liberato ASQ. Learning to Live with OCD: Labeling, the Self, and Stigma. Deviant Behav 2007;28:305–31. 10.1080/01639620701233274 [DOI] [Google Scholar]
- 44. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition: American Psychiatric Association, 2013. [Google Scholar]
- 45. Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychol Methods 2007;12:23–44. 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- 46. National Institute of Mental Health Strategic Plan. Washington DC: US Department of Health & Human Services, 2008. Report No.: NIH Publication No. 08–6368. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018228supp001.pdf (48KB, pdf)


