Abstract
Purpose
To measure the waste generation and lifecycle environmental emissions from cataract surgery via phacoemulsification in a recognized resource-efficient setting.
Setting
Two tertiary care centers of the Aravind Eye Care System in southern India.
Design
Observational case series.
Methods
Manual waste audits, purchasing data, and interviews with Aravind staff were used in a hybrid environmental lifecycle assessment framework to quantify the environmental emissions associated with cataract surgery. Kilograms of solid waste generated and midpoint emissions in a variety of impact categories (eg, kilograms of carbon dioxide equivalents).
Results
Aravind generates 250 grams of waste per phacoemulsification and nearly 6 kilograms of carbon dioxide-equivalents in greenhouse gases. This is approximately 5% of the United Kingdom’s phaco carbon footprint with comparable outcomes. A majority of Aravind’s lifecycle environmental emissions occur in the sterilization process of reusable instruments because their surgical system uses largely reusable instruments and materials. Electricity use in the operating room and the Central Sterile Services Department (CSSD) accounts for 10% to 25% of most environmental emissions.
Conclusions
Results show that surgical systems in most developed countries and, in particular their use of materials, are unsustainable. Ophthalmologists and other medical specialists can reduce material use and emissions in medical procedures using the system described here.
In most developed countries, surgery in general uses a significant amount of single-use disposable instruments and generates large quantities of waste.1–3 The resulting emissions contribute directly and indirectly to public health impacts, including respiratory impacts and global warming or climate change.4–6 The National Health Services are responsible for 3% of the United Kingdom’s greenhouse gases,7 and in the United States, the healthcare sector produces 10% of total greenhouse gases and 9% of the U.S. criteria air pollutants.6 Climate change is already having a profound effect on public health, resulting in increased frequency and severity of flooding and droughts, greater insecurity of food systems, and an increase in disease vectors such as mosquitoes and ticks.8 A larger proportion of these impacts fall on developing countries such as India where environmental and economic conditions make it difficult to mitigate the effects of climate change and where emissions from material production or electronic waste treatment result in emissions such as air particulates, heavy metals, and toxic compounds that directly affect health.8,9
Cataracts are the leading cause of blindness and visual impairment worldwide, making cataract surgery one of the most commonly performed surgical procedures.10 Cataract surgery in the U.K. emits 180 kilograms (kg) of carbon dioxide (CO2)-equivalents per eye, with more than one half of those emissions originating from the procurement of largely disposable medical equipment.11 Globally, the cost of cataract surgery frequently impedes access for those who need it most.12,13 In its mission to eradicate unnecessary blindness, the Aravind Eye Care System, in the southern Indian state of Tamil Nadu, has developed an innovative and effective model of care centered on time efficiency and resource efficiency. Aravind performs 1000 surgeries per working day. Sixty percent of these surgeries are delivered at minimum or no cost to the patient and with better outcomes and lower complication rates than the U.K.13,14 The Avarind model is recognized for its financial and social success,15,16 although it has not yet been studied for its environmental footprint.
As healthcare professionals worldwide become more aware of and concerned for the public health implications of climate change and excessive resource use, efficient care delivery models must be better understood and promoted.8,17–19 Aravind, with its assembly-line model for surgery and its use of reusable instruments, serves as an example of more sustainable, efficient cataract surgery. This study analyzes Aravind’s material use from phaco-emulsification cataract surgery and quantifies the resulting environmental effects and costs through environmental lifecycle assessment (LCA).
MATERIALS AND METHODS
Data Collection
Data were collected at Aravind Eye Hospital in Pondicherry, India, between November 2014 and February 2015. This project obtained institutional review board exemption because no individual patient data were collected. Material flow analysis was performed by observing the flow of materials through the operating room. Lists of the materials used in surgery, their prices, quantities, and estimated lifespans were obtained from Aravind’s purchasing department and interviews with midlevel ophthalmic personnel. The weight of each surgical instrument and tool was measured directly. Data on waste disposal routes and associated costs or profits were obtained from Aravind’s housekeeping department and direct observation, and information on the sterilization processes was obtained from Aravind’s CSSD. Waste audits, in which waste from each stream was separated by material type and weighed, were performed on all phacoemulsification cases from 1 operating room on the same day with a typical caseload (93 cases). An on-site visit to the regional biomedical waste incinerator confirmed treatment and disposal of waste from this specific waste stream. Surgical demographics, including number of surgeries and staffing levels, were obtained from Aravind’s surgical database and the midlevel ophthalmic personnel administrator.
Data on the hospital’s overall use of water and electricity were obtained from Aravind’s engineering department. Water consumption and treatment was allocated to a single phacoemulsification based on floor area of the operating rooms and the CSSD, and then by total number of all surgeries performed in a single year. Electricity use was calculated using the power ratings from all equipment and lighting found in the operating room, and an average duration of 9 minutes, from a patient entering the operating room to the patient leaving the operating room. Ventilation and air conditioning was calculated by subtracting the per-operating room electricity use from Aravind’s total annual records and allocating the remainder to the total floor area of air-conditioned space. These assumptions will likely overestimate the actual water and electricity consumption in the operating room for a single phacoemulsification. Electricity use for sterilization of reusable items was calculated using power ratings of sterilization and laundry equipment in the CSSD and the duration of equipment’s treatment cycles. These were allocated to the quantity of linens or trays treated per load. Aravind uses diesel generators to overcome gaps in the electrical grid. On-site emissions from the burning of diesel fuel were allocated as a percentage of total electricity use based on the amount of energy generated by the diesel generators (4% of Aravind’s kilowatt hours (kWh) per year).
Lifecycle Assessment
Lifecycle assessment is a tool used to quantify the emissions of a product or process throughout its lifecycle, from raw material extraction through use and disposal. Emissions to air, water, and soil are typically sorted into related categories (eg, greenhouse gases) and converted into similar units (eg, kg of CO2-equivalents) in what is known as midpoint reporting. In the case of cataract surgery, emissions include indirect sources (upstream might include emissions to water and air caused by the production of plastics for surgical materials, whereas downstream might include emissions to soil and water for landfilling of waste) and direct sources (eg, burning diesel fuel in generators onsite at Aravind).
The International Organization for Standardization20 has established guidelines for LCAs that are performed in 4 stages as follows: (1) goal and scope definition, (2) lifecycle inventory, (3) impact assessment, and (4) interpretation. For this LCA study, the functional unit, an essential component of stage 1, was the removal of cataract in 1 eye using phacoemulsification. The study boundaries encompass only the perioperative period, including preoperative cleaning and anesthesia of the eye and all activities performed within the operating room. The study boundaries do not include the patient preparation before entering the operating area or postoperative follow-ups. The production, use, and disposal of all surgical instruments and supplies are included in the LCA; however, capital equipment such as the phacoemulsification machine, operating microscope, and the building construction were not included because the effect of these items when allocated to a single case are typically negligible.4,5,16
The lifecycle inventory is a list of all the emissions associated with a single product. The lifecycle inventory for Aravind’s phaco-emulsification surgeries was created by matching the collected material, energy, and water-use data with global-based and Indian-based unit processes in the Ecoinvent database,21 an international emissions database containing thousands of products. Ecoinvent is known for its comprehensiveness and robustness and it has been used in previous studies of medicine.4,5,21,22 Aravind’s Pondicherry location constructed an on-site wetland to treat wastewater. Because most medical facilities do not use this wastewater treatment method, wastewater treatment is a tertiary concern of cataract care, and decentralized wastewater treatment systems are not well documented in existing LCA databases and literature. This system was modeled as a standard wastewater treatment plant with primary and secondary settlers, activated sludge aeration, and anaerobic digestion. A detailed list of the materials inventory and matching lifecycle inventory databases can be found in Supplemental Tables 1 and 2, available at http://jcrsjournal.org.
These emissions were characterized and combined into midpoint impact categories using the lifecycle impact (LCI) assessment method, the Tool for the Reduction and Assessment of Chemical and Other Environmental Impacts (TRACI) (version 2.1 v1.02, U.S., 2008) by the U.S. Environmental Protection Agency.23 This study reports the following impact categories: ozone depletion, greenhouse gas emissions, smog formation, acidification, eutrophication, carcinogenics, noncarcinogenics, respiratory effects, and ecotoxicity. This method was chosen because it will allow for a comparison with ongoing studies of cataract surgery in the U.S. Because TRACI is not explicitly a global method and there are no available India-specific lifecycle inventories or impact assessment methods at present, a sensitivity analysis (Supplemental Figure 1, available at: http://jcrsjournal.org) was also performed using the LCI assessment method CML-IA baseline (version 3.02, World 2000, developed by the Department of Industrial Ecology of Leiden University)A Greenhouse gas emissions matched exactly in both LCI assessment methods and the relative impacts for components of phacoemulsification matched in the categories of ozone depletion, smog, acidification, and eutrophication, thus validating the model used in this study. For more information on sensitivity analyses for this study, see Supplemental Figures 2 to 7 and Supplemental Table 3, available at: http://jcrsjournal.org. Embodied energy, or the amount of energy needed throughout a product’s lifecycle, was calculated using Cumulative Energy Demand (version 1.09).24
Emissions for pharmaceuticals were calculated using Economic Input-Output Life Cycle Assessment (EIO-LCA) and the TRACI method contained in the EIO-LCA tool because at present, there are no lifecycle impacts available for specific pharmaceutical agents.4 The EIO-LCA uses the transfer of money between economic sectors to assign emissions to a certain dollar value of spending. There are no EIO-LCA models available for pharmaceutical production in India; therefore, to make some estimate on the environmental emissions associated with pharmaceuticals, this study used the U.S. 2002 Producer model provided by Carnegie Mellon University’s free online tool.25 Aravind spends an average of $1.68 per phacoemulsification on perioperative pharmaceuticals. This value was converted into 2002 U.S. dollars (the units used in the most current EIO-LCA model) using U.S.-based producer price indexing. The values reported reflect LCI assessment impact categories with matching units, but exclude pharmaceutical impacts for the following categories: carcinogenics, noncarcinogenics, respiratory effects, and ecotoxicity.
RESULTS
During the 4-month study, Aravind performed 2942 cataract surgeries with phacoemulsification (Table 1). Metrics from surgical complications and outcomes during this period are on par with Aravind’s previously reported data and satisfactorily meet standards for ophthalmic surgeries in developed countries.
Table 1.
Patient characteristics during the study period.
| Metric | Value, n (%) |
|---|---|
|
| |
| Phacoemulsification | 2942 |
| Endophthalmitis | 1 (0.03) |
| Posterior capsule rupture | 4 (0.14) |
| Vitreous loss | 8 (0.27) |
| Inflammation (persistent) | 1 (0.03) |
| Vision better than 6/12 (20/40) | 2322 (79) |
| Wound complication | 0 (0) |
| Persistent corneal edema | 67 (2.3) |
| Hypopyon | 0 (0) |
| IOL decentration | 0 (0) |
| Descemet membrane detachment | 1 (0.03) |
| Significant cortex residual | 5 (0.17) |
IOL = intraocular lens
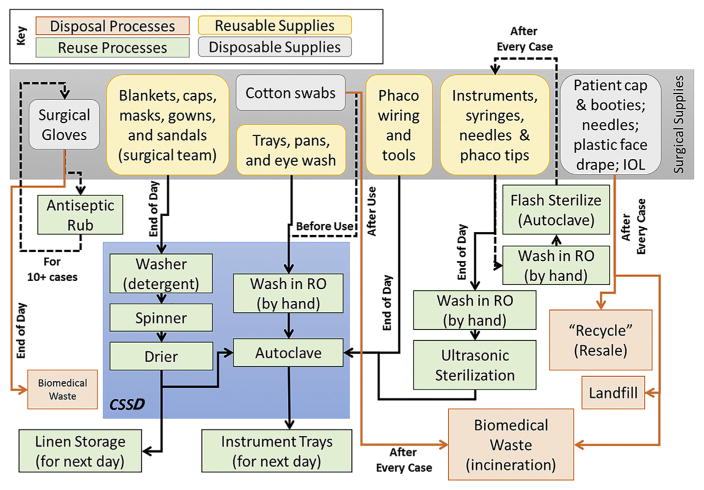
Figure 1 shows the flow of Aravind’s surgical materials through the operating room during which the single-use items, including patient face drape, patient cap and booties, some of the needles and blades, and the intraocular lens (IOL) packaging, are discarded to recycling (resale), landfill, or biomedical waste (incineration) after each phacoemulsification procedure. Stainless steel instruments, syringes, and the phaco tools that come in contact with the patient are removed from the operating room after every case, washed by hand in reverse-osmosis water, and sterilized in a 30-minute flash autoclave cycle (high-pressure steam). These autoclaved items are reused in the operating rooms the same day. At the end of the operating day, these instruments are washed by hand, sterilized via ultrasound, and autoclaved for a full 1-hour cycle in the CSSD. After they have dried, the instruments are stored for use on the next operating day. Other items, such as the phaco wiring and the larger instrument bins are sterilized only at the end of the day. The physician’s and midlevel ophthalmic personnel’s surgical gloves are sterilized between cases using an antiseptic gel and disposed of via the biomedical waste stream after approximately 10 cases. Other items, such as plastic table draping and the plastic cover for the phaco machine, are disposed of at the end of the operating day. The surgical team’s caps, masks, gowns, and sandals, as well as the patient blanket, are laundered at the end of the day by the CSSD. Aravind also uses all pharmaceuticals, including antibacterial eyedrops, local anesthetic, and a balanced salt solution on multiple patients until the bottle is empty or until the end of the operating day.
Figure 1.
Downstream material flow diagram for the surgical supplies used in Aravind’s phaco-emulsification cases (CSSD = Central Sterile Services Department; IOL = intraocular lens; RO = reverse osmosis).
Waste audits show that Aravind generates an average of 250 grams of waste per phacoemulsification. Two-thirds of this waste is recycled, whereas the remaining one third is split between landfilling and biomedical waste incineration. The landfilled waste products are scraps of paper or plastic too small to be recycled in the local market. The incinerated waste includes biohazardous materials such as used gauze, needles, blades, and used gloves. Over 20% of the waste by weight is the plastic face drape worn by patients during the surgery. Another 25% of the waste is the packaging and paper booklet of directions included with the IOL.
Lifecycle Assessment Results
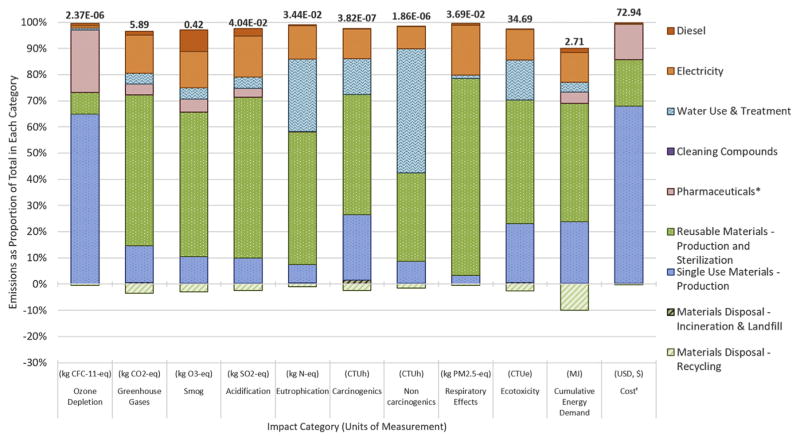
The environmental LCA showed that the reusable surgical instruments and their sterilization comprise more than one half of the emissions in all reported impact categories except ozone depletion, noncarcinogenic emissions, and cumulative energy demand (Figure 2 and Supplemental Tables 4 and 5 [available at: http://jcrsjournal.org]). The electricity use of the autoclaves and laundering equipment in the CSSD comprise the largest share of these emissions because these instruments are sterilized between each case. Single-use materials result in the largest portion of emissions related to ozone depletion, which can be traced back to the use of cotton gauze. Traditional cotton agricultural practices use large quantities of pesticides and fertilizers that can contribute to ozone depletion and other impact categories. Despite the minimum use of disposable supplies, over 60% of Aravind’s per-case variable expenditures are for single-use materials. Electricity and diesel consumption for lighting, equipment, and air conditioning compose 10% to 25% of all impact categories except ozone depletion and costs. Electricity comprises a larger portion of those categories related to the burning of fossil fuels, that is, greenhouse gases, smog formation, acidification, and respiratory impacts.
Figure 2.
Lifecycle environmental effects of an average phacoemulsification at Aravind Eye Hospital in Pondicherry, India. The mean value of total emissions is shown at the top of each impact category column. Costs do not include staff salaries, the IOL, water use, overhead, or capital equipment (* = pharmaceuticals were calculated using economic data in a U.S.-based model; CFC = carbofluorocarbons; CO2 = carbon dioxide; CTU = cumulative toxicity unit; h = human; e = environment; eq = equivalent; MJ = megajoules; O3 = ozone; PM2.5 = particulate matter less than 2.5 μm in diameter; USD = 2014 U.S. dollars).
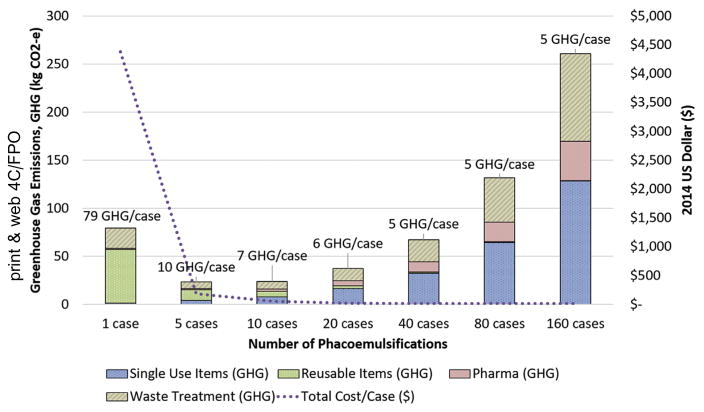
By decreasing the duration of each surgery and minimizing the turnaround time in the operating room, Aravind has decreased per-case electricity use and the associated financial and environmental costs (Figure 3). Short surgical duration and quick turnaround is safely implemented through extensive training of all staff and rigid sterilization protocols.
Figure 3.
Effect of surgical duration on energy use (grid electricity and diesel generators), greenhouse gas emissions from energy use, and costs for a single phacoemulsification at Aravind Eye Hospital (GHG = greenhouse gas; kWh = kilowatt hour).
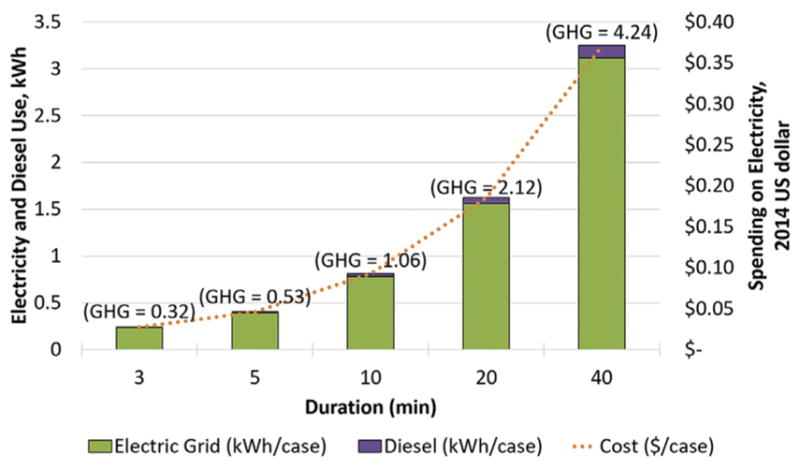
In Aravind’s case, short surgical duration allows for more surgeries to be performed each day, and because most of the surgical supplies are reusable, this minimizes the associated environmental footprint from material production. If Aravind were to dispose of all surgical supplies after a single case, the emissions from this phacoemulsification would be equivalent to performing approximately 40 phacoemulsification surgeries through the Aravind method (Figure 4). The more surgeries Aravind performs, the smaller their greenhouse gases and cost footprint, although the effects from the single-use devices and their disposal accrue with each case.
Figure 4.
Effect of patient throughput and material reuse on total greenhouse gas emissions and per case cost (2014 U.S. dollars) for phacoemulsification at Aravind Eye Hospital; does not include emissions associated with energy use, building construction, or capital equipment such as the phacoemulsification machine (CO2-e = carbon dioxide-equivalent; GHG = greenhouse gas).
Each phacoemulsification procedure at Aravind emits approximately 5% of the greenhouse gases of a phacoemulsification in the U.K. Excluding patient and staff travel, paper and ink, and food from the U.K. calculations (to ensure the boundaries match the present study), each phacoemulsification generates approximately 130 kg of CO2-equivalents, which is equivalent to the greenhouse gases of a passenger car driving 500 kilometer (km). Aravind’s 6 kg CO2-equivalents per phacoemulsification is equivalent to the same car driving just 23 km. Aravind’s model emits proportionally fewer greenhouse gases from the procurement of pharmaceuticals and the use of electricity in the building (Figure 5), which is likely because of the use of multiuse pharmaceuticals and the short surgical duration and quick turnaround time, although this comparison is limited by differences in carbon footprinting methods (the U.K. study uses a largely economic-based framework) and emissions variations by location (the Indian electric grid generally emits a greater proportion of greenhouse gases than the U.K. electric grid).
Figure 5.
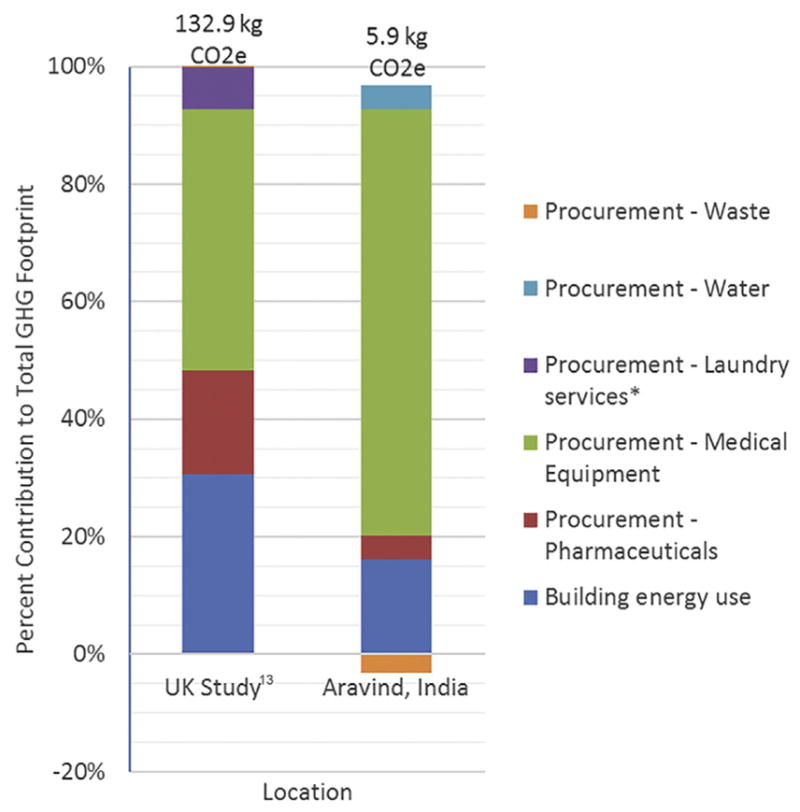
Comparison of greenhouse gas emissions for phacoemulsification in the U.K. and at Aravind based on economic subsectors, modified from Morris et al.,11 to account for different study boundaries (* = Aravind’s laundry services are included in the Procurement - Water category; CO2-e = carbon dioxide-equivalent; GHG = greenhouse gas).
DISCUSSION
The current cataract surgical rate in India is estimated at 5721 surgeries per million annually.16,26 Extrapolating the U.K. ’s per-case carbon footprint to India’s current surgical rate would result in 1.16 million metrictons of CO2-equivalents released annually. This is equivalent to nearly 250 000 passenger vehicles driven for 1 year and would require 30 million tree seedlings growing for 10 years to sequester this amount of carbon.27 If the Aravind model were used for these cases and they were all phacoemulsification cases, the footprint would be approximately 42 000 metric tons of CO2-equivalents per year, which is equivalent to 8900 vehicles and would require approximately 1.1 million seedlings to sequester. However, a majority of Aravind’s cataract surgeries are performed via manual small incision, which likely has an even smaller footprint than phacoemulsification because of the reduction in energy consumption and specialty instruments (phacoemulsifier).
The World Health Organization’s (WHO) Vision 2020 Initiative28 aims to eliminate avoidable blindness by 2020. To achieve this initiative, India’s surgical rate will be required to at least double.16,26,29 Climate change already affects Indian citizens and the predicted weather patterns of flooding and drought are only expected to worsen with increases in global greenhouse gases emissions.9 The WHO Vision 2020 Initiative would be best achieved using a surgical model with quality outcomes, reduced costs, and minimum adverse environmental and public health effects. Aravind attained such a model through a continual focus on resource efficiency.
Aravind’s high-volume approach increases patient throughput, reducing per capita expenditures on overhead and capital equipment while minimizing the environmental footprint associated with electricity and energy use. Each surgeon operates on 2 tables and is assisted by 4 highly trained midlevel ophthalmic personnel. The physician is responsible exclusively for the surgery, from open to close. While the physician operates on the first table, the midlevel ophthalmic personnel perform preoperative preparations on the second table. At the end of each case, the scope and phacoemulsification equipment is transferred to the second table while the surgeon and staff sterilize their gloves with an antiseptic solution. The first patient is then escorted from the operating room by 1 of the midlevel ophthalmic personnel, who also brings in the next patient for surgical preparation. By this method, Aravind provides 750 to 1500 surgeries per day.
High volume alone is not enough to minimize emissions. Over 50% of the U.K. ’s phacoemulsification carbon footprint originates in the procurement of supplies. By reusing surgical gowns, blankets, and instruments, Aravind reduces the environmental impacts and costs associated with the production of those items. Aravind has further reduced the impacts associated with sterilization by delineating between surgical supplies, which are contaminated and must be sterilized between each case (including the reusable instrument tray and the phaco tips) and surgical supplies, which do not pose a safety risk to the patient and can be sterilized or disposed of at the end of the operating day (including intraoperative pharmaceuticals, the plastic protectors on the phaco machine and tables, and the fluid collection bags attached to the phaco machine). In addition, Aravind uses a shorter autoclave cycle throughout the operating day, which reduces per-case energy consumption of sterilization. This also reduces the turnaround time for reusable instruments, thereby minimizing the total number of instruments required to meet the daily demand.
Healthcare services in developed countries are a major source of environmental emissions. In the U.K., the National Health Services is responsible for 3% of the U.K. ’s total greenhouse gas emissions.7 In the U.S., the healthcare sector emits nearly 10% of the U.S. ’s greenhouse gases and other air pollutants resulting in acid rain, smog formation, and respiratory impacts that adversely affect human health.6 A large portion of these emissions can be reduced through readily available resource efficiency measures, including optimizing the use of reusable instruments and supplies, maximizing single-use device reprocessing, promoting minimum waste and recycling practices, using energy-efficient appliances and air-handling systems, and investing in low-carbon energy sources.
Although most developed countries face greater regulatory barriers in replicating the Aravind model in its entirety, some ophthalmology groups in the U.S. already use similar efficiency measures. Some have minimized surgical duration by running 2 adjacent operating rooms simultaneously and minimizing physician’s nonoperative duties. Some facilities have minimized the items in their disposable custom packs (prepackaged kits of sterile surgical supplies) and switched to largely reusable surgical supplies.22 Other facilities use flash autoclaving, or, as it is more commonly known in the U.S., Immediate Use Sterile Supplies (IUSS). These instrument trays are sterilized but are not allowed to dry; as such, they cannot be stored and must be used the same day they are sterilized. Most regulatory bodies in the U.S. prohibit the use of IUSS unless it is recommended in the sterilization procedures produced by the instrument manufacturer. Although these regulatory restrictions are made with the purpose of increasing safety, their effect is theoretical and unproven, and they add energy burdens and expense to the process.
Although most regulations in developed countries are made with patient safety in mind, greater liability in countries such as the U.S. might drive resource use in operating rooms. Defensive medicine, not based on scientific evidence of infectious risk, adds to the cost and, therefore, environmental footprint of care.30 Policy changes would be required to implement other safe and effective efficiency measures used by Aravind, such as multiuse ophthalmic pharmaceuticals. Other issues, including the wider recycling of operating room waste and the reduction of packaging on ophthalmic surgical supplies, require changes from the waste management and medical device manufacturing industries, which can be encouraged by ophthalmologists and other healthcare professionals as well as purchasing officers.
Aravind is a dynamic eye care system that is constantly seeking ways to improve access and quality while reducing costs. Large hospitals in India (>100 beds) are required to install and maintain their own decentralized on-site waste-water treatment plants. At its Pondicherry location, Aravind uses a Decentralized Wastewater Treatment Systems-constructed wetland that creates treated water for use in gardening and toilet flushing, in addition to providing green space. Since this study was performed, Aravind has also installed solar photovoltaic panels on all the hospitals in its system, reducing the need for the carbon-intensive Indian electric grid and diesel generators, which create on-site emissions affecting air quality.
At present, Aravind is working with an IOL manufacturer, Aurolab, to reduce the paper waste from the IOL packaging and directions because this impact comprised one quarter of the waste (by weight) they generate in each phacoemulsification procedure. In addition, Aravind is installing 100 new vision centers by 2020. These vision centers are small facilities in remote and rural communities, serving approximately 45 000 to 50 000 people. They are managed by 2 midlevel ophthalmic personnel who perform basic screening tests and have a telemedicine link to a physician at an Aravind hospital. This increases patient access to care, including postoperative follow-up, while minimizing the patient’s travel (and thus carbon footprint).
Lifecycle assessment models contain uncertainties and the values reported here are not absolute, but rather represent an average in a range of potential emissions. A major limitation of this study is the dearth of lifecycle inventories and LCI assessment methods specifically for India. Organizations such as Ecoinvent, the Confederation of Indian Industry, and the India LCA Alliance are attempting to address this issue. In the meantime, the global emissions inventories and the North American impact assessment method used in this study might not be accurate for India. However, we tested the sensitivity of our results using a more global impact assessment method producing results on par with the primary, U.S.-based method. In addition, because of the lack of LCI data for pharmaceuticals, this study was forced to use a U.S.-based economic model to assign environmental emissions to the production and delivery of ophthalmic pharmaceuticals in India.
Despite these limitations, this study provided an estimate of the emissions associated with Aravind’s surgical model that can be compared with other approaches to phacoemulsification globally. Future work in ophthalmology will expand on this study to identify and test potential sustainability interventions in cataract surgery worldwide, and these study methods might be applied to other ophthalmic surgeries such as similar waste and environmental footprint studies of femtosecond laser–assisted cataract surgery. In addition, LCA methodology should be expanded to include a wider range of medical products and international locations, so that baseline assessments and evaluations of interventions can be performed more easily in other medical fields.
Supplementary Material
WHAT WAS KNOWN
Modern-day healthcare uses large quantities of resources resulting in substantial environmental emissions. The National Health Service is responsible for 3% of the U.K.’s climate-warming greenhouse gases, and the healthcare sector produces 10% of the U.S.’s greenhouse gases and 9% of the U.S.’s criteria air pollutants.
A single cataract surgery (phacoemulsification) in the U.K. releases the equivalent greenhouse gases of driving a passenger vehicle nearly 700 km.
WHAT THIS PAPER ADDS
The Aravind Eye Care System generated 0.25 kg of solid waste per phacoemulsification and approximately 6 kg of CO2-equivalent greenhouse gases (the same as driving a passenger vehicle at approximately 25 km), all with comparable-to-better patient outcomes and less spending.
If India’s ophthalmologists used the U.K.’s methods for phacoemulsification, cataract surgery in India would emit the same greenhouse gases as 250 000 passenger vehicles. This number would double if India fulfills the WHO’s Vision 2020 Initiative to meet the demand for cataract care.
Acknowledgments
Supported by a Fulbright-Nehru Academic and Professional Excellence Award through the United States –India Educational Foundation, New Delhi, India. Dr. Saeedi is supported by a Career Development Grant (No. K23 EY025014) from the U.S. National Institutes of Health, Bethesda, Maryland, USA. The sponsor or funding organization had no role in the design, conduct, or reporting of this research.
Footnotes
OTHER CITED MATERIAL: Department of Industrial Ecology. Universiteit Leiden. CML-IA Characterisation Factors, 2016. Available at: https://www.universiteitleiden.nl/en/research/research-output/science/cml-ia-characterisation-factors. Accessed September 25, 2017
The employees of Aravind Eye Care System helped collect data for this project.
Disclosure: None of the authors has a financial or proprietary interest in any material or method mentioned.
Supplemental material available at www.jcrsjournal.org.
References
- 1.Esaki RK, Macario A. Wastage of supplies and drugs in the operating room. Medscape Anesthesiology. 2009 [Google Scholar]
- 2.McGain F, Clark M, Williams T, Wardlaw T. Recycling plastics from the operating suite [letter] Anaesth Intensive Care. 2008;36:913–914. [PubMed] [Google Scholar]
- 3.Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste; surgeons venture through the trash can. [Accessed September 25, 2017];JAMA. 1992 267:2765–2768. Available at: http://infohouse.p2ric.org/ref/39/38843.pdf. [PubMed] [Google Scholar]
- 4.Thiel CL, Eckelman M, Guido R, Huddleston M, Landis AE, Sherman J, Shrake SO, Copley-Woods N, Bilec MM. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. [Accessed September 25, 2017];Environ Sci Technol. 2015 49:1779–1786. doi: 10.1021/es504719g. Available at: http://pubs.acs.org/doi/pdf/10.1021/es504719g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campion N, Thiel CL, DeBlois J, Woods NC, Landis AE, Bilec MM. Life cycle assessment perspectives on delivering an infant in the US. [Accessed September 25, 2017];Sci Total Environ. 2012 425:191–198. doi: 10.1016/j.scitotenv.2012.03.006. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3563327/pdf/nihms364803.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. [Accessed September 25, 2017];PLoS One. 2016 11(6):e0157014. doi: 10.1371/journal.pone.0157014. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4900601/pdf/pone.0157014.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sustainable Development Unit. Carbon Footprint Update for NHS in England 2012. Cambridge, UK: Sustainable Development Unit; 2013. [Accessed September 25, 2017]. Available at: http://www.sduhealth.org.uk/documents/carbon_footprint_summary_nhs_update_2013.pdf. [Google Scholar]
- 8.Wang H, Horton R. Tackling climate change: the greatest opportunity for global health [comment] [Accessed September 25, 2017];Lancet. 2015 386:1798–1799. doi: 10.1016/S0140-6736(15)60931-X. Available at: https://climatehealthcommission.files.wordpress.com/2015/04/commentaryrichard-horton-and-helena-wang.pdf. [DOI] [PubMed] [Google Scholar]
- 9.Narain S, Ghosh P, Saxena NC, Parikh J, Soni P. Climate Change: Perspectives From India. New Delhi, India: United Nations Development Programme; 2009. [Accessed September 25, 2017]. Available at: http://www.undp.org/content/dam/india/docs/undp_climate_change.pdf. [Google Scholar]
- 10.Bourne RRA, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Resnikoff S, Taylor HR on behalf of the Vision Loss Expert Group. Causes of vision loss worldwide, 1990–2010: a systematic analysis. [Accessed September 25, 2017];Lancet Glob Health. 2013 1:e339–e349. doi: 10.1016/S2214-109X(13)70113-X. Available at: http://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(13)70113-X.pdf. [DOI] [PubMed] [Google Scholar]
- 11.Morris DS, Wright T, Somner JEA, Connor A. The carbon footprint of cataract surgery. [Accessed September 25, 2017];Eye. 2013 27:495–501. doi: 10.1038/eye.2013.9. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3626018/pdf/eye20139a.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aravind S, Haripriya A, Sumara Taranum BS. Cataract surgery and intraocular lens manufacturing in India. Curr Opin Ophthalmol. 2008;19:60–65. doi: 10.1097/ICU.0b013e3282f2aaed. [DOI] [PubMed] [Google Scholar]
- 13.Vickers T, Rosen E. Driving Down the Cost of High-Quality Care: Lessons From the Aravind Eye Care System. London, UK: McKinsey and Co; 2011. [Accessed September 25, 2017]. Available at: http://www.aravind.org/content/Downloads/draravindinterview.pdf. [Google Scholar]
- 14.Haripriya A, Chang DF, Reena M, Shekhar M. Complication rates of phaco-emulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012;38:1360–1369. doi: 10.1016/j.jcrs.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 15.Rangan VK. Harvard Business School, case. 1993. The Aravind Eye Hospital, Madurai, India: in service for sight; pp. 593–598. (revised May 2009) [Google Scholar]
- 16.Le H-G, Ehrlich JR, Venkatesh R, Srinivasan A, Kolli A, Haripriya A, Ravindran RD, Thulasiraj RD, Robin AL, Hutton DW, Stein JD. A sustainable model for delivering high-quality efficient cataract surgery in southern India. [Accessed September 25, 2017];Health Aff (Millwood) 2016 35:1783–1790. doi: 10.1377/hlthaff.2016.0562. Available at: http://218.248.31.202/librarymain/files/journalcasestudies/SustainableModel.pdf. [DOI] [PubMed] [Google Scholar]
- 17.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, Friel S, Groce N, Johnson A, Kett M, Lee M, Levy C, Maslin M, McCoy D, McGuire B, Montgomery H, Napier D, Pagel C, Patel J, de Oliveira JA, Redclift N, Rees H, Rogger D, Scott J, Stephenson J, Twigg J, Wolff J, Patterson C. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 18.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859–869. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- 19.Venkatesh R, van Landingham SW, Khodifad AM, Haripriya A, Thiel CL, Ramulu P, Robin AL. Carbon footprint and cost–effectiveness of cataract surgery. Curr Opin Ophthalmol. 2016;27:82–88. doi: 10.1097/ICU.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 20.International Organization for Standardization. Environmental Management–Life Cycle Assessment –Principles and Framework. Geneva, Switzerland: ISO; 2006. [Accessed September 25, 2017]. (ISO 14040:2006). Summary Available at: https://www.iso.org/obp/ui/#iso:std:iso:14040:ed-2:v1:en. [Google Scholar]
- 21.Weidema BP, Bauer C, Hischier R, Mutel C, Nemecek T, Reinhard J, Vadenbo CO, Wernet G. Overview and methodology: data quality guideline for the ecoinvent database version 3. St. Gallen, Switzerland: Swiss Centre for Life Cycle Inventories; 2013. [Accessed September 25, 2017]. (Ecoinvent report no.1, vol. 3). Available at: http://vbn.aau.dk/ws/files/176769045/Overview_and_methodology.pdf. [Google Scholar]
- 22.Campion N, Thiel CL, Woods NC, Swanzy L, Landis AE, Bilec MM. Sustainable healthcare and environmental life-cycle impacts of disposable supplies: a focus on disposable custom packs. J Clean Prod. 2015;94:46–55. [Google Scholar]
- 23.Bare J. TRACI version 2.1. User’s guide. Washington DC: U.S, Environmental Protection Agency Office of Research and Development; 2012. [Accessed September 25, 2017]. Tool for the Reduction and Assessment of Chemical and Other Environmental Impacts (TRACI) Available at: https://nepis.epa.gov/Adobe/PDF/P100HN53.pdf. [Google Scholar]
- 24.Frischknecht R, Jungbluth N, Althaus H-J, Bauer C, Doka G, Dones R, Hischier R, Hellweg S, Humbert S, Kollner T, Loerincik Y, Margni M, Nemecek T. Ecoinvent report No. 3, v2.0. Dubendorf, Switzerland: Swiss Centre for Life Cycle Inventories; 2007. [Accessed September 25, 2017]. Implementation of Life Cycle Impact Assessment Methods. Available at: http://www.iaea.org/inis/collection/NCLCollectionStore/_Public/41/028/41028089.pdf. [Google Scholar]
- 25.Carnegie Mellon University. Green Design Institute. Economic Input-Output Life Cycle Assessment (EIO-LCA) [Accessed September 25, 2017];US 2002(428) model. Available at: http://www.eiolca.net/
- 26.Murthy GVS, Gupta SK, John N, Vashist P. Current status of cataract blindness and Vision 2020: the right to sight initiative in India. [Accessed September 25, 2017];Indian J Ophthalmol. 2008 56:489–494. doi: 10.4103/0301-4738.42774. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2612994/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.United States Environmental Protection Agency. [Accessed September 25, 2017];Greenhouse Gas Equivalencies Calculator. Available at: https://www.epa.gov/energy/greenhouse-gas-equivalencies-calculator.
- 28.World Health Organization. Global Initiative for the Elimination of Avoidable Blindness; Action Plan 2006–2011. Geneva, Switzerland: WHO; 2007. [Accessed September 25, 2017]. Vision 2020. The Right to Sight. Available at: http://apps.who.int/iris/bitstream/10665/43754/1/9789241595889_eng.pdf. [Google Scholar]
- 29.Foster A. Cataract and “Vision 2020–the right to sight” initiative [editorial] [Accessed September 25, 2017];Br J Ophthalmol. 2001 85:635–637. doi: 10.1136/bjo.85.6.635. Available at: http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1724020&blobtype=pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hermer LD, Brody H. Defensive medicine, cost containment, and reform. [Accessed September 25, 2017];J Gen Intern Med. 2010 25:470–473. doi: 10.1007/s11606-010-1259-3. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855004/pdf/11606_2010_Article_1259.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.