Abstract
Objective
To describe an approach that allows for a streamlined assessment and accurate differentiation of most patients with itch in primary care and to provide an update on the available nonpharmacologic, topical, and systemic therapies.
Sources of information
MEDLINE (Ovid) and PubMed were searched for the key words itch or pruritus. Searches were refined for each cause and treatment by adding appropriate key words, and subsequent hand searches of the references of retrieved literature were performed.
Main message
A good body of evidence from high-quality trials does not exist for treatment of pruritus, and the treatments that do exist are inconsistent in their success. The dominant causes of generalized itch are xerosis and eczema. Most patients will improve with nonpharmacologic therapy including frequent moisturization. If this avenue fails, further investigations are warranted to help guide subsequent treatment with any of the many cause-specific topical and systemic approaches available.
Conclusion
Chronic itch can be debilitating for patients. The approach described allows for a streamlined assessment and accurate differentiation of most patients with itch in primary care.
Pruritus is the most common cutaneous symptom, yet it is difficult to diagnose and manage. Visible skin lesions are not always present, and itch might be a dermatologic manifestation of any of a broad array of systemic diseases. Although itch most commonly results from xerosis (dry skin) or eczema, the systemic differential diagnosis reaches as far as cirrhosis, hematologic disorders, infection, drug reactions, and malignancy. Frequently ignored, pruritus has the potential to severely compromise quality of life. Chronic itch can be just as debilitating as chronic pain.1 Nocturnal scratching in atopic dermatitis, for example, might considerably impair sleep and cause fatigue and irritability.2
We describe an approach that allows for a streamlined assessment and accurate differentiation of most patients with itch in primary care. We also provide an update for the available nonpharmacologic, topical, and systemic therapies.
Case description
Mr B. is a 78-year-old widower who comes into your comprehensive family medicine office in December for assessment of generalized itch he has had for 2 months. “I’ve been itchy ever since I flew back from vacationing in the tropics,” he describes. “It’s been driving me wild and keeping me up at night.” Mr B. lives in a retirement home and has a healthy family and social life. He frequently helps take care of his 7-year-old granddaughter, he mentions, who has always had sensitive skin but “has also been a lot more rash-y these past few weeks.” You interview and examine him, and as you walk out the door he adds, “Oh, Doc … my partner also says I’ve been more yellow than usual. I thought it was the tan at first, but the colour might be sticking around!”
Sources of information
We searched MEDLINE (Ovid) and PubMed for the key words itch or pruritus. We refined our search for each cause and treatment approach by adding appropriate key words, and we performed subsequent hand searches of the references of retrieved literature.
Main message
History.
As with any medical complaint, it is imperative to listen to and empathize with the patient’s narrative. Like pain, pruritus is subjective. There are specific aspects of the history, however, that will help a conscientious clinician narrow the differential diagnosis between the types of itch (Table 1).3–5 Ask about the location, onset, and timing of itch. Ask about medications, personal care products, family, travel, and psychiatric history. Perform a comprehensive review of systems; weight changes, fatigue, night sweats, or other constitutional symptoms, for example, might point to thyroid dysfunction or malignancy. Pruritus in the context of other cohabitants with itch, on the other hand, might suggest an insect bite reaction or scabies.
Table 1.
Types of itch
| ITCH TYPE | DESCRIPTION |
|---|---|
| Systemic | Itch from noncutaneous organ systems (eg, cholestasis, kidney disease, myeloproliferative disorders, hyperthyroidism)
|
| Psychogenic | Itch from a disorder of the mind (eg, delusions of parasitosis, formication)
|
| Neuropathic | Itch from central or peripheral nerve damage (eg, postherpetic neuralgia, brachioradial pruritus, notalgia paresthetica)
|
| Pruritoceptive | Dermatologic itch (eg, xerosis, scabies, urticaria, reactions to insect bite)
|
Is the pruritus localized or generalized?
A careful physical examination should be performed. Look for primary lesions. Chronic rubbing and scratching can result in nonspecific lesions that include lichenification, prurigo nodules, and excoriations. Attempts to identify a primary cause for these lesions can be difficult.
The foremost divide in the differential diagnosis is the distribution of pruritus—that is, whether the itch is localized or generalized. If pruritus is localized, a primary skin lesion will often point to a particular diagnosis. A skin biopsy might be helpful. A dermatomal distribution, possibly with pain, burning, or loss of sensation, is especially suggestive of a neuropathic pathogenesis. A history of herpes zoster, for instance, might indicate postherpetic neuralgia.
The differential diagnosis for generalized pruritus without primary lesions, on the other hand, is broad and often requires a more comprehensive history and investigation. Generalized pruritus might or might not have a primary skin lesion. It is important to note, for example, that the primary wheals of urticaria are fleeting and thus easy to miss. Although xerosis must first be ruled out, the absence of primary skin lesions otherwise indicates that the clinician must tailor the physical examination toward the findings of systemic disease. It is important to evaluate for signs such as the stigmata of chronic liver disease, conjunctival pallor, thyromegaly, splenomegaly, and lymphadenopathy.
Red flag symptoms.
Unfortunately, pruritus is sometimes the cutaneous herald of more severe systemic disease. Systemic illness is the cause in 14% to 24% of patients with pruritus without a primary dermatologic origin.6 Constitutional symptoms might point to underlying malignancy or infection. A high-risk substance or sexual history might implicate HIV or hepatitis C infection. Polydipsia and polyuria could point to diabetes mellitus. Kidney or renal disease might lead to uremic pruritus, and temperature intolerance could signify thyroid dysfunction. Mood changes, disproportionate worry, or obsessive patterns might suggest a psychiatric cause of itch.
Laboratory and special tests.
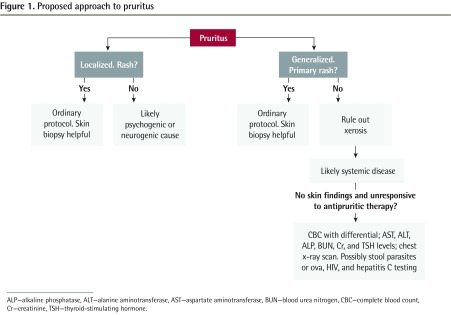
There is consensus that more extensive investigation should be reserved for patients who are both without physical findings of skin disease and unresponsive to a short course of antipruritic therapy.7 If indicated, however, evaluation should include the tests in Figure 1.
Figure 1.
Proposed approach to pruritus
ALP—alkaline phosphatase, ALT—alanine aminotransferase, AST—aspartate aminotransferase, BUN—blood urea nitrogen, CBC—complete blood count, Cr—creatinine, TSH—thyroid-stimulating hormone.
Management.
Whenever possible, treatment should be directed at the primary cause of itch. Nonpharmacologic, topical, and systemic therapies are available (Table 2). However, a robust body of evidence from randomized controlled trials (RCTs) does not exist for treatment of pruritus, and the treatments that do exist are inconsistent in their success even when appropriate for the cause of the itch.
Table 2.
Summary of interventions and the most appropriate indications
| CLASS | INTERVENTION | INDICATION | LEVEL OF EVIDENCE* |
|---|---|---|---|
| Nonpharmacologic therapies | Moisturization | All patients | III |
| Cool environment | All patients | III | |
| Avoid irritants | All patients | III | |
| Break itch-scratch cycle | All patients | III | |
| Behavioural therapy, relaxation, stress reduction | All patients, but especially for atopic dermatitis and other chronic itch | II | |
| Topical therapies | Corticosteroids | Inflammatory dermatoses | I |
| Calcineurin inhibitors | Inflammatory dermatoses | I | |
| Capsaicin | Localized itch (eg, neuropathic) | III | |
| Menthol | Localized itch (eg, neuropathic) | III | |
| Pramoxine or eutectic mixture of lidocaine and prilocaine | Postburn, uremic, or neuropathic pruritus | II | |
| Doxepin | Atopic dermatitis | I | |
| Systemic therapies | Nonsedating antihistamines | Urticaria, insect bite reactions, mastocytosis, drug reactions | I |
| First-generation antihistamines | Nocturnal itch | III | |
| μ-Opioid receptor antagonists | Cholestatic pruritus, chronic urticaria, atopic dermatitis | I | |
| κ-Opioid receptor agonists | Opiate-induced pruritus, uremic pruritus | I | |
| SSRIs (paroxetine, fluvoxamine, sertraline) | Palliative care | I | |
| Atopic dermatitis, systemic lymphoma, solid carcinoma, uremic pruritus, cholestatic pruritus | II | ||
| Doxepin | Atopic dermatitis, HIV-related pruritus, allergic cutaneous reactions, urticaria | II | |
| Anticonvulsants (gabapentin, pregabalin) | Uremic pruritus | I | |
| Neuropathic pruritus, idiopathic pruritus | II | ||
| Ursodeoxycholic acid | Intrahepatic cholestasis of pregnancy | I | |
| Oral immunosuppressants (cyclosporine, azathioprine, mycophenolate mofetil) | Inflammatory dermatoses | I | |
| Corticosteroids | Inflammatory dermatoses | I |
SSRI—selective serotonin reuptake inhibitors.
Level I evidence requires at least 1 properly conducted randomized controlled trial, systematic review, or meta-analysis. Level II evidence includes other comparison trials, non-randomized, cohort, case-control, or epidemiologic studies, and preferably more than 1 study. Level III evidence includes expert opinion or consensus statements.
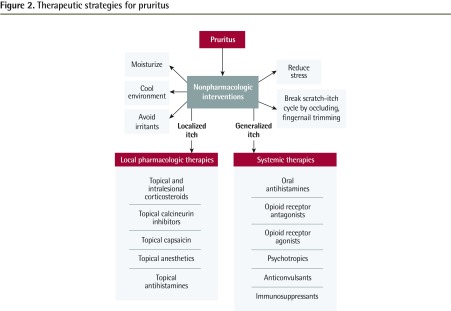
Nonpharmacologic interventions: Although management must be tailored to the cause of pruritus, there are several interventions that might benefit most patients. Frequent moisturization is helpful to restore the skin barrier, especially as xerosis can both cause and exacerbate pruritus. Transepidermal water loss correlates with itch intensity and reflects skin barrier function. It might be minimized by consistent moisturization.8 Patients should avoid overbathing and overdrying their skin with soaps and cleansers. These first interventions are simple but crucial, as most itch is due to xerosis and eczema.
Interestingly, warmer temperatures lower the threshold of receptors to pruritic stimuli.9 Patients should use lighter clothing and run lukewarm water when bathing. Moisturization with a refrigerated emollient often helps considerably. Skin irritants such as wool should be avoided. The itch-scratch cycle should also be broken, for example by occluding pruritic areas and trimming fingernails.
Behavioural therapy is also effective in the management of itch from atopic dermatitis and other causes.10–13 In behavioural therapy, participants learn to consciously suppress the reflex to scratch through distraction and habit reversal.14
Local pharmacologic therapies: In localized skin disease, topical preparations are beneficial. While not directly antipruritic, topical and intralesional corticosteroids can improve both inflammation and associated itch in inflammatory dermatoses. It is likely that the antipruritic effects of topical calcineurin inhibitors are also a result of their anti-inflammatory properties.15 Both topical steroids and calcineurin inhibitors can help itch in conditions such as atopic dermatitis, psoriasis, and lichen planus. They can also help to break the itch-scratch cycle in patients with secondary lesions such as prurigo nodularis or lichen simplex chronicus.
Topical capsaicin causes a burning sensation. It activates and depletes various cutaneous ion channels and leads to lasting desensitization to pain and pruritus alike.16 Despite its common use historically, a 2010 systematic review by Gooding et al found no good RCT evidence for the use of topical capsaicin in pruritus of any origin.17 Nonetheless, evidence for capsaicin use continues to grow for localized neuropathic itch.16,18–20
Topical menthol, on the other hand, causes a cooling sensation. The mechanism by which topical menthol alleviates pruritus is unknown, but it might mimic cool temperatures in heightening the threshold for pruritic stimuli. There is expert consensus that menthol might be effective in low concentrations (less than 5%).21 It is an irritant at higher concentrations.
Topical anesthetics such as pramoxine cream or the eutectic mixture of lidocaine and prilocaine cream might be beneficial in postburn, uremic, and neuropathic pruritus.22
Although topical antihistamines are frequently prescribed for pruritus, a 2010 review by Eschler and Klein found mixed evidence to support their use.23 Only topical doxepin, a tricyclic antidepressant and a potent H1 and H2 receptor antagonist, has RCT evidence supporting use for atopic dermatitis.24
Systemic therapies: Oral H1 antihistamines such as hydroxyzine and diphenhydramine are often the first line of treatment for generalized itch. However, the evidence for their use is limited mainly to histamine-mediated conditions.25 Histamine is the dominant mediator for pruritus only with insect bite reactions, urticaria, mastocytosis, and drug reactions. Within these conditions, nonsedating antihistamines are often more effective owing to better adherence.26 First-generation antihista-mines are more likely to be sedating, but for this reason they often benefit patients suffering from nocturnal itch even if the itch is not mediated by histamine.27
Antagonization of μ-opioid receptors in the central nervous system can relieve itch by disinhibiting the effect of pain-transmitting neurons on pruritoceptive neurons. μ-Opioid receptor antagonists such as naloxone, nalmefene, and naltrexone have RCT evidence for use in itch from cholestasis, chronic urticaria, and atopic dermatitis.28
Agonization of κ-opioid receptors in the central nervous system by butorphanol or nalfurafine, on the other hand, can directly inhibit itch, especially in opiate-induced itch.29 Nalfurafine, for example, while not yet approved in Canada, has increasingly robust RCT evidence for efficacy and safety in uremic pruritus.30–32
There are several psychotropic medications that might have benefit in itch.33 The selective serotonin reuptake inhibitors paroxetine and sertraline both have RCT evidence for their use in various systemic causes of itch. Paroxetine might be helpful in severe pruritus of nondermatologic origin (eg, in palliative patients with advanced neoplastic disease).34 Low-dose sertraline might be beneficial for uremic or cholestatic pruritus.35–37 Paroxetine or fluvoxamine both have some evidence for use in refractory itch from atopic dermatitis, systemic lymphoma, and solid carcinoma.38
The tricyclic antidepressant doxepin might also be useful in treating chronic pruritus of atopic dermatitis, HIV-related pruritus, pruritus associated with allergic cutaneous reactions, and urticaria refractory to conventional H1 antihistamine therapy.39,40 In addition to its topical use in cream form, doxepin also has a place in systemic therapy because of its potent antihistaminergic effects and has some RCT evidence for use in uremic itch.41
The anticonvulsants gabapentin and pregabalin might be particularly useful in idiopathic, uremic, and neuropathic itch (eg, brachioradial pruritus or notalgia paresthetica, and perhaps even prurigo nodularis).42 Interestingly, the promise both anticonvulsant agents show lends support to the neuropathic origin of uremic pruritus.
Oral immunosuppressants such as cyclosporine, azathioprine, and mycophenolate mofetil have efficacy in itch from inflammatory conditions such as atopic dermatitis.43,44 Systemic corticosteroids might also be used to settle inflammation in severe cases of chronic pruritus.45
Ursodeoxycholic acid has RCT evidence for use in itch from intrahepatic cholestasis of pregnancy, although it seems to have a small benefit size.46,47
Cromolyn sodium, zinc sulfate, omega-3 fatty acid, and montelukast have small RCTs that support their use in uremic itch.48 However, the results need to be confirmed by larger studies.
As is the case with pain, placebo might improve pruritic symptoms. Van Laarhoven et al published a creative and elegant meta-analysis in 2015 investigating the magnitude of the effects on itch of oral and injected placebo. They reported a mean itch reduction of 24%. Their analysis included 4141 patients treated with placebo, out of 12 218 total trial participants drawn from 70 trials on atopic dermatitis, psoriasis, urticaria, and an assortment of other dermatologic conditions.49 Many therapies for pruritus are supported only by poorly powered studies, thus placebo or self-resolution with general measures might be an underappreciated aspect in itch therapy. It could well be that “time in divided doses,” Sir William Osler’s favourite prescription, should be combined with moisturization and the general measures listed in Figure 2 as a universal first-line therapy for undifferentiated itch.
Figure 2.
Therapeutic strategies for pruritus
Pruritus in palliative care.
While pruritus is not one of the most prevalent complaints in palliative care populations, it is frustrating for patients and puzzling for providers. A 2013 Cochrane intervention review by Xander et al determined that the literature did not reveal an optimal approach to pruritus in palliative care. Unsurprisingly, they suggest that the pathophysiology of pruritus should guide the treatment plan.50 When itch compromises quality of life, the underlying cause of the pruritus should be investigated in order to tailor management. In patients with HIV-associated pruritus, weak evidence points to the nonsteroidal anti-inflammatory drug indomethacin as the most effective agent. Gabapentin and nalfurafine have been shown to ameliorate pruritus in patients suffering from chronic kidney disease. Rifampin and flumecinol, a hepatic enzyme inducer, might be recommended for patients with cholestatic pruritus owing to a low incidence of adverse effects. Paroxetine might be beneficial in alleviating pruritus of various causes for palliative care patients. Although the 2013 Cochrane review found these various interventions to be effective in the treatment of specific forms of pruritus, it found insufficient evidence to direct concrete guidelines for the management of pruritus in palliative care.50
Case resolution
On further questioning, Mr B. has no other historical red flags for systemic disease. On examination, Mr B. has no primary skin lesions. He has no localized disease that might suggest a pathogenesis shared with his granddaughter such as scabies or insect bite reaction. In terms of his new “yellow” colour, he does have some persistent pigment darkening from recent sun exposure, but no scleral icterus or jaundice. His skin is generally dry. You recommend nonpharmacologic measures including moisturization and shorter, less frequent bathing. His itch has resolved by the time he visits you again in the clinic the following month.
Conclusion
The dominant causes of generalized itch are xerosis and eczema. Most patients will improve with nonpharmacologic therapy including frequent moisturization. If this avenue fails, the investigations outlined in Figure 1 are warranted to help guide subsequent treatment by the many cause-specific topical and therapeutic approaches available (Table 2 and Figure 2).
EDITOR’S KEY POINTS
Itch is the most common cutaneous symptom, yet it poses considerable difficulty in diagnosis and management. Although pruritus most commonly results from xerosis (dry skin) or eczema, the differential diagnosis is broad and the evidence for many treatments is limited. As a result, patients with itch often suffer for extended periods of time without an understanding of the cause or appropriate therapy.
The authors outline an approach to the assessment and treatment of patients with pruritus in primary care. Conducting a careful history and examination, differentiating between localized and generalized pruritus, identifying primary lesions if they exist, and recognizing red flag symptoms can be helpful in identifying the cause of pruritus and guiding treatment.
Many patients will benefit from nonpharmacologic therapies including frequent moisturization, avoiding overbathing, behavioural therapy, and breaking the itch-scratch cycle. Various topical and systemic therapies are available that could help patients who do not benefit from nonpharmacologic measures.
Footnotes
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
Cet article se trouve aussi en français à la page 925.
Contributors
Both authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Kini SP, DeLong LK, Veledar E, McKenzie-Brown AM, Schaufele M, Chen SC. The impact of pruritus on quality of life: the skin equivalent of pain. Arch Dermatol. 2011;147(10):1153–6. doi: 10.1001/archdermatol.2011.178. Epub 2011 Jun 16. [DOI] [PubMed] [Google Scholar]
- 2.Arndt J, Smith N, Tausk F. Stress and atopic dermatitis. Curr Allergy Asthma Rep. 2008;8(4):312–7. doi: 10.1007/s11882-008-0050-6. [DOI] [PubMed] [Google Scholar]
- 3.Twycross R, Greaves MW, Handwerker H, Jones EA, Libretto SE, Szepietowski JC, et al. Itch: scratching more than the surface. QJM. 2003;96(1):7–26. doi: 10.1093/qjmed/hcg002. [DOI] [PubMed] [Google Scholar]
- 4.Nowak DA, Wong SM. DSM-5 update in psychodermatology. Skin Therapy Lett. 2016;21(3):4–7. [PubMed] [Google Scholar]
- 5.Yosipovitch G, Greaves MW, Schmelz M. Itch. Lancet. 2003;361(9358):690–4. doi: 10.1016/S0140-6736(03)12570-6. [DOI] [PubMed] [Google Scholar]
- 6.Reamy BV, Bunt CW, Fletcher S. A diagnostic approach to pruritus. Am Fam Physician. 2011;84(2):195–202. [PubMed] [Google Scholar]
- 7.Greco PJ, Ende J. Pruritus: a practical approach. J Gen Intern Med. 1992;7(3):340–9. doi: 10.1007/BF02598094. [DOI] [PubMed] [Google Scholar]
- 8.Lee CH, Chuang HY, Shih CC, Jong SB, Chang CH, Yu HS. Transepidermal water loss, serum IgE and beta-endorphin as important and independent biological markers for development of itch intensity in atopic dermatitis. Br J Dermatol. 2006;154(6):1100–7. doi: 10.1111/j.1365-2133.2006.07191.x. [DOI] [PubMed] [Google Scholar]
- 9.Yosipovitch G, Patel TS. Pathophysiology and clinical aspects of pruritus. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick’s dermatology in general medicine. 8th edition. New York, NY: McGraw-Hill; 2012. pp. 1146–57. [Google Scholar]
- 10.Gieler U, Kupfer J, Niemeier V, Brosig B, Stangier U. Atopic eczema prevention programs—a new therapeutic concept for secondary prevention. Dermatol Psychosom. 2000;1:138–47. [Google Scholar]
- 11.Staab D, Von Rueden U, Kehrt R, Erhart M, Wenninger K, Kamtsiuris P, et al. Evaluation of a parental training program for the management of childhood atopic dermatitis. Pediatr Allergy Immunol. 2002;3(2):84–90. doi: 10.1034/j.1399-3038.2002.01005.x. [DOI] [PubMed] [Google Scholar]
- 12.Evers AW, Duller P, de Jong EM, Otero ME, Verhaak CM, Van der Valk PG, et al. Effectiveness of a multidisciplinary itch-coping training programme in adults with atopic dermatitis. Acta Derm Venereol. 2009;89(1):57–63. doi: 10.2340/00015555-0556. [DOI] [PubMed] [Google Scholar]
- 13.Bathe A, Matterne U, Dewald M, Grande T, Weisshaar E. Educational multidisciplinary training programme for patients with chronic pruritus. Acta Derm Venereol. 2009;89(5):498–501. doi: 10.2340/00015555-0684. [DOI] [PubMed] [Google Scholar]
- 14.Rosenbaum MS, Ayllon T. The behavioral treatment of neurodermatitis through habit-reversal. Behav Res Ther. 1981;19(4):313–8. doi: 10.1016/0005-7967(81)90052-8. [DOI] [PubMed] [Google Scholar]
- 15.Ständer S, Schürmeyer-Horst F, Luger TA, Weisshaar E. Treatment of pruritic diseases with topical calcineurin inhibitors. Ther Clin Risk Manag. 2006;2(2):213–8. doi: 10.2147/tcrm.2006.2.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papoiu AD, Yosipovitch G. Topical capsaicin. The fire of a ‘hot’ medicine is reignited. Expert Opin Pharmacother. 2010;11(8):1359–71. doi: 10.1517/14656566.2010.481670. [DOI] [PubMed] [Google Scholar]
- 17.Gooding SM, Canter PH, Coelho HF, Boddy K, Ernst E. Systematic review of topical capsaicin in the treatment of pruritus. Int J Dermatol. 2010;49(8):858–65. doi: 10.1111/j.1365-4632.2010.04537.x. [DOI] [PubMed] [Google Scholar]
- 18.Boyd K, Shea SM, Patterson JW. The role of capsaicin in dermatology. Prog Drug Res. 2014;68:293–306. doi: 10.1007/978-3-0348-0828-6_12. [DOI] [PubMed] [Google Scholar]
- 19.Zeidler C, Lüling H, Dieckhöfer A, Osada N, Schedel F, Steinke S, et al. Capsaicin 8% cutaneous patch: a promising treatment for brachioradial pruritus? Br J Dermatol. 2015;172(6):1669–71. doi: 10.1111/bjd.13501. Epub 2015 Apr 13. [DOI] [PubMed] [Google Scholar]
- 20.Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Am Acad Dermatol. 1995;32(2 Pt 1):287–9. doi: 10.1016/0190-9622(95)90152-3. [DOI] [PubMed] [Google Scholar]
- 21.Patel T, Ishiuji Y, Yosipovitch G. Menthol: a refreshing look at this ancient compound. J Am Acad Dermatol. 2007;57(5):873–8. doi: 10.1016/j.jaad.2007.04.008. Epub 2007 May 10. [DOI] [PubMed] [Google Scholar]
- 22.Young TA, Patel TS, Camacho F, Clark A, Freedman BI, Kaur M, et al. A pramoxine-based anti-itch lotion is more effective than a control lotion for the treatment of uremic pruritus in adult hemodialysis patients. J Dermatolog Treat. 2009;20(2):76–81. doi: 10.1080/09546630802441218. [DOI] [PubMed] [Google Scholar]
- 23.Eschler DC, Klein PA. An evidence-based review of the efficacy of topical antihistamines in the relief of pruritus. J Drugs Dermatol. 2010;9(8):992–7. [PubMed] [Google Scholar]
- 24.Drake LA, Fallon JD, Sober A. Relief of pruritus in patients with atopic dermatitis after treatment with topical doxepin cream. The Doxepin Study Group. J Am Acad Dermatol. 1994;31(4):613–6. doi: 10.1016/s0190-9622(94)70225-x. [DOI] [PubMed] [Google Scholar]
- 25.Yosipovitch G, Bernhard JD. Clinical practice. Chronic pruritus. N Engl J Med. 2013;368(17):1625–34. doi: 10.1056/NEJMcp1208814. [DOI] [PubMed] [Google Scholar]
- 26.Charlesworth EN, Beltrani VS. Pruritic dermatoses: overview of etiology and therapy. Am J Med. 2002;113(Suppl 9A):25S–33S. doi: 10.1016/s0002-9343(02)01434-1. [DOI] [PubMed] [Google Scholar]
- 27.Lavery MJ, Stull C, Kinney MO, Yosipovitch G. Nocturnal pruritus: the battle for a peaceful night’s sleep. Int J Mol Sci. 2016;17(3):425. doi: 10.3390/ijms17030425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phan NQ, Bernhard JD, Luger TA, Ständer S. Antipruritic treatment with systemic μ-opioid receptor antagonists: a review. J Am Acad Dermatol. 2010;63(4):680–8. doi: 10.1016/j.jaad.2009.08.052. Epub 2010 May 11. [DOI] [PubMed] [Google Scholar]
- 29.Phan NQ, Lotts T, Antal A, Bernhard JD, Ständer S. Systemic kappa opioid receptor agonists in the treatment of chronic pruritus: a literature review. Acta Derm Venereol. 2012;92(5):555–60. doi: 10.2340/00015555-1353. [DOI] [PubMed] [Google Scholar]
- 30.Wikström B, Gellert R, Ladefoged SD, Danda Y, Akai M, Ide K, et al. Kappa-opioid system in uremic pruritus: multicenter, randomized, double-blind, placebo-controlled clinical studies. J Am Soc Nephrol. 2005;16(12):3742–7. doi: 10.1681/ASN.2005020152. Epub 2005 Oct 26. [DOI] [PubMed] [Google Scholar]
- 31.Kumagai H, Ebata T, Takamori K, Miyasato K, Muramatsu T, Nakamoto H, et al. Efficacy and safety of a novel κ-agonist for managing intractable pruritus in dialysis patients. Am J Nephrol. 2012;36(2):175–83. doi: 10.1159/000341268. Epub 2012 Aug 3. [DOI] [PubMed] [Google Scholar]
- 32.Inui S. Nalfurafine hydrochloride to treat pruritus: a review. Clin Cosmet Investig Dermatol. 2015;8:249–55. doi: 10.2147/CCID.S55942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tennyson H, Levine N. Neurotropic and psychotropic drugs in dermatology. Dermatol Clin. 2001;19(1):179–97. doi: 10.1016/s0733-8635(05)70239-4. [DOI] [PubMed] [Google Scholar]
- 34.Zylicz Z, Krajnik M, Sorge AA, Costantini M. Paroxetine in the treatment of severe non-dermatological pruritus: a randomized, controlled trial. J Pain Symptom Manage. 2003;26(6):1105–12. doi: 10.1016/j.jpainsymman.2003.05.004. [DOI] [PubMed] [Google Scholar]
- 35.Chan KY, Li CW, Wong H, Yip T, Chan ML, Cheng HW, et al. Use of sertraline for antihistamine-refractory uremic pruritus in renal palliative care patients. J Palliat Med. 2013;16(8):966–70. doi: 10.1089/jpm.2012.0504. Epub 2013 Jun 18. [DOI] [PubMed] [Google Scholar]
- 36.Mayo MJ, Handem I, Saldana S, Jacobe H, Getachew Y, Rush AJ. Sertraline as a first-line treatment for cholestatic pruritus. Hepatology. 2007;45(3):666–74. doi: 10.1002/hep.21553. [DOI] [PubMed] [Google Scholar]
- 37.Thébaut A, Habes D, Gottrand F, Rivet C, Cohen J, Debray D, et al. Sertraline as an additional treatment for cholestatic pruritus in children. J Pediatr Gastroenterol Nutr. 2017;64(3):431–5. doi: 10.1097/MPG.0000000000001385. [DOI] [PubMed] [Google Scholar]
- 38.Ständer S, Böckenholt B, Schürmeyer-Horst F, Weishaupt C, Heuft G, Luger TA, et al. Treatment of chronic pruritus with the selective serotonin re-uptake inhibitors paroxetine and fluvoxamine: results of an open-labelled, two-arm proof-of-concept study. Acta Derm Venereol. 2009;89(1):45–51. doi: 10.2340/00015555-0553. [DOI] [PubMed] [Google Scholar]
- 39.Smith PF, Corelli RL. Doxepin in the management of pruritus associated with allergic cutaneous reactions. Ann Pharmacother. 1997;31(5):633–5. [PubMed] [Google Scholar]
- 40.Greene SL, Reed CE, Schroeter AL. Double-blind crossover study comparing doxepin with diphenhydramine for the treatment of chronic urticaria. J Am Acad Dermatol. 1985;12(4):669–75. doi: 10.1016/s0190-9622(85)70092-8. [DOI] [PubMed] [Google Scholar]
- 41.Pour-Reza-Gholi F, Nasrollahi A, Firouzan A, Nasli Esfahani E, Farrokhi F. Low-dose doxepin for treatment of pruritus in patients on hemodialysis. Iran J Kidney Dis. 2007;1(1):34–7. [PubMed] [Google Scholar]
- 42.Matsuda KM, Sharma D, Schonfeld AR, Kwatra SG. Gabapentin and pregabalin for the treatment of chronic pruritus. J Am Acad Dermatol. 2016;75(3):619–25.e6. doi: 10.1016/j.jaad.2016.02.1237. Epub 2016 May 17. [DOI] [PubMed] [Google Scholar]
- 43.Simon D, Bieber T. Systemic therapy for atopic dermatitis. Allergy. 2014;69(1):46–55. doi: 10.1111/all.12339. Epub 2013 Dec 20. [DOI] [PubMed] [Google Scholar]
- 44.Schmitt J, Schmitt N, Meurer M. Cyclosporin in the treatment of patients with atopic eczema—a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2007;21(5):606–19. doi: 10.1111/j.1468-3083.2006.02023.x. [DOI] [PubMed] [Google Scholar]
- 45.Weisshaar E, Szepietowski JC, Darsow U, Misery L, Wallengren J, Mettang T, et al. European guideline on chronic pruritus. Acta Derm Venereol. 2012;92(5):563–81. doi: 10.2340/00015555-1400. [DOI] [PubMed] [Google Scholar]
- 46.Palma J, Reyes H, Ribalta J, Hernández I, Sandoval L, Almuna R, et al. Ursodeoxycholic acid in the treatment of cholestasis of pregnancy: a randomized, double-blind study controlled with placebo. J Hepatol. 1997;27(6):1022–8. doi: 10.1016/s0168-8278(97)80146-8. [DOI] [PubMed] [Google Scholar]
- 47.Chappell LC, Gurung V, Seed PT, Chambers J, Williamson C, Thornton JG, et al. Ursodeoxycholic acid versus placebo, and early term delivery versus expectant management, in women with intrahepatic cholestasis of pregnancy: semifactorial randomised clinical trial. BMJ. 2012;344:e3799. doi: 10.1136/bmj.e3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pongcharoen P, Fleischer AB., Jr An evidence-based review of systemic treatments for itch. Eur J Pain. 2016;20(1):24–31. doi: 10.1002/ejp.766. Epub 2015 Sep 28. [DOI] [PubMed] [Google Scholar]
- 49.Van Laarhoven AI, van der Sman-Mauriks IM, Donders AR, Pronk MC, van de Kerkhof PC, Evers AW. Placebo effects on itch: a meta-analysis of clinical trials of patients with dermatological conditions. J Invest Dermatol. 2015;135(5):1234–43. doi: 10.1038/jid.2014.522. Epub 2014 Dec 1. [DOI] [PubMed] [Google Scholar]
- 50.Xander C, Meerpohl JJ, Galandi D, Buroh S, Schwarzer G, Antes G, et al. Pharmacological interventions for pruritus in adult palliative care patients. Cochrane Database Syst Rev. 2013;(6):CD008320. doi: 10.1002/14651858.CD008320.pub2. [DOI] [PubMed] [Google Scholar]