Cases of Middle East respiratory syndrome coronavirus, including travel-associated cases, continue to be reported. The risk of exportation of cases to the United States mandates that clinicians need to be vigilant to identify cases and implement infection control measures expeditiously.
Keywords: Middle East respiratory syndrome coronavirus, MERS-CoV, infection control, coronavirus
Abstract
Although much recent focus has been on the recognition of Ebola virus disease among travelers from West Africa, cases of Middle East respiratory syndrome coronavirus (MERS-CoV), including travel-associated cases, continue to be reported. US clinicians need to be familiar with recommendations regarding when to suspect MERS-CoV, how to make a diagnosis, and what infection control measures need to be instituted when a case is suspected. Infection control is especially critical, given that most cases have been healthcare-associated. Two cases of MERS-CoV were identified in the United States in May 2014; because these cases were detected promptly and appropriate control measures were put in place quickly, no secondary cases occurred. This paper summarizes information that US clinicians need to know to prevent secondary cases of MERS-CoV from occurring in the United States.
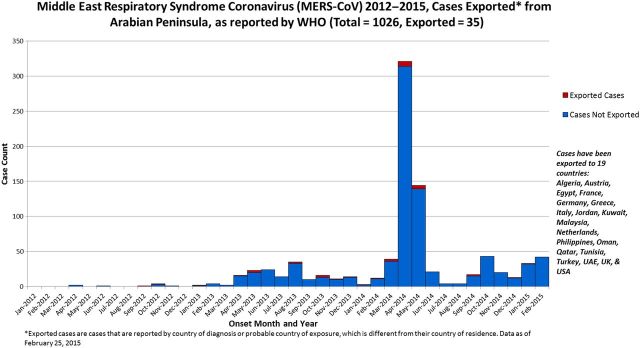
Although much recent focus has been appropriately placed on the recognition of Ebola virus disease in travelers returning from West Africa, the recent increase in cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection (including travel-associated cases) is also of concern [1, 2]. MERS-CoV is a novel virus first reported in Saudi Arabia in 2012. As of 25 February 2015, a total of 1026 laboratory-confirmed cases of MERS-CoV infection, including at least 376 deaths (36.7%), have been confirmed by the World Health Organization (WHO) (Figure 1) [2]. Between 1 August 2014 and 25 February 2015, there have been 172 cases (and 69 deaths) confirmed by WHO, with an additional 16 cases and 12 deaths pending WHO confirmation. All cases reported thus far have had a direct or indirect link through travel or residence to 9 countries in or near the Arabian Peninsula (Saudi Arabia, United Arab Emirates, Qatar, Oman, Jordan, Kuwait, Iran, Lebanon, and Yemen); at least 19 countries (including the United States) have had travel-associated cases (Figure 1). Most MERS-CoV patients have had fever, cough, and shortness of breath, often leading to severe respiratory complications (eg, pneumonia or acute respiratory distress syndrome) [3, 4]; some cases with mild or no symptoms (often tested as part of a contact investigation) have also been reported [5, 6]. Other reported symptoms include chills/rigors, headache, cough, dyspnea, myalgia, sore throat, coryza, dizziness, nausea/vomiting, diarrhea, and abdominal pain. Laboratory findings seen in some patients include leukopenia, lymphopenia, thrombocytopenia, thrombocytosis, and elevated levels of lactate dehydrogenase, alanine aminotransferase, and aspartate aminotransferase [3, 4]. In some MERS-CoV patients, coinfection with other respiratory pathogens has been reported [7, 8]; thus, identification of an alternative respiratory diagnosis should not rule out the possibility of MERS-CoV. The median age of persons with laboratory-confirmed MERS-CoV infection is 50 years, approximately 63% have been males, and approximately 18% have been healthcare workers [2]. Early on in the outbreak, a predominance of male patients and those with comorbidities was noted, and most cases had severe illness. However, as additional data are collected, the full spectrum of illness is becoming more clear, with a decrease in the percentage of severe cases and increase in asymptomatic cases, as well as a decline in the male-to-female ratio, median age, and case-fatality rate [9].
Figure 1.
Number of confirmed cases of Middle East respiratory syndrome coronavirus infection (including those that were travel-associated) reported by the World Health Organization as of 25 February 2015, by month and year of illness onset—worldwide, 2012–2015 [2].
MERS-CoV transmission is not fully understood; however, many cases have had exposure(s) to healthcare settings during the 14 days before symptom onset (the median incubation period is approximately 5 days, with a range of 2–14 days). Recent data highlight the likely role of camels as a source of human infection in some cases (eg, MERS-CoV has been found in camels in the region; MERS-CoV gene sequences in camels are similar to those in humans; camels have had antibodies to MERS-CoV or a MERS-CoV–like virus, suggesting previous MERS-CoV infection; and full gene sequencing has linked MERS-CoV identified in a camel to a patient who died of MERS-CoV) [10–15]. On 1 May and 11 May 2014, 2 cases of MERS-CoV infection were identified in Indiana and Florida, respectively [16, 17]. Both US cases were healthcare workers in Saudi Arabia and presented to hospitals in the United States with mild to moderate, nonspecific findings, where they were identified as having MERS-CoV by astute clinicians sensitized to the need to identify and test returning travelers with respiratory illnesses. Both patients were appropriately isolated and no secondary cases were identified despite extensive follow-up. These cases emphasize the importance of US clinicians’ becoming familiar with the clinical and epidemiologic features and actions needed to detect and manage MERS-CoV patients. The number of MERS cases has continued to increase; therefore, the risk of exportation of cases to the United States mandates that clinicians need to continue to be vigilant.
The Centers for Disease Control and Prevention (CDC) recommends evaluation for MERS-CoV infection for the following patients [18]:
Patients with fever and clinical or radiographic evidence of pneumonia or acute respiratory distress syndrome and either a history of travel from countries in or near the Arabian Peninsula (Bahrain; Iraq; Iran; Israel, the West Bank, and Gaza; Jordan; Kuwait; Lebanon; Oman; Qatar; Saudi Arabia; Syria; the United Arab Emirates; and Yemen) within 14 days before symptom onset, or close contact with a symptomatic traveler who developed fever and acute respiratory illness within 14 days after traveling from countries in the region.
Patients who are a member of a cluster of patients with severe acute respiratory illness (eg, fever and pneumonia requiring hospitalization) of unknown etiology in which MERS-CoV is being evaluated, in consultation with state and local health departments.
Patients with fever and symptoms of respiratory illness (eg, cough, shortness of breath) who have a history of being in a healthcare facility (as a patient, worker, or visitor) within 14 days before symptom onset in a country or territory in or near the Arabian Peninsula in which recent healthcare-associated cases of MERS-CoV have been identified.
Laboratory testing for suspected MERS-CoV cases in the United States can be performed using the CDC's real-time reverse transcription polymerase chain reaction assay [19]. Testing of multiple specimens from different sites (ie, nasopharyngeal swab, oropharyngeal swab, sputum, serum, and stool/rectal swab) at different times after symptom onset is recommended to maximize the probability of MERS-CoV detection. Lower respiratory tract specimens (eg, sputum or bronchoalveolar lavage) and serum should be tested when possible because MERS-CoV infection has sometimes been detected in lower respiratory specimens or serum when upper respiratory specimens had tested negative, including in the 2 US cases [16, 17]. Most state health department laboratories in the United States are approved for MERS-CoV testing; clinicians should contact their state or local health department when evaluating a patient for MERS-CoV infection. If testing is not available through coordination with state and local health departments, samples can be sent to the CDC for testing [18]. Serologic testing, which is useful for making a retrospective diagnosis, is only available in the United States at the CDC.
Healthcare-associated infections have played a major role in the transmission of MERS-CoV [4, 9, 20–23]. Based on the experience with severe acute respiratory syndrome (SARS) coronavirus patients and early data from MERS-CoV, strict infection control practices prevent spread of infection [24]. Thus, the CDC recommends implementation of screening and triage procedures for early recognition of potentially infected patients and prompt institution of infection control measures, including standard, contact, and airborne precautions (airborne precautions include care in an airborne infection isolation room, eye protection with goggles or face shield, and respiratory protection at least as protective as a fit-tested N95 filtering facepiece respirator that has been National Institute for Occupational Safety and Health certified), to prevent secondary cases in healthcare workers or other patients [18]. Healthcare workers exposed to aerosol-generating procedures (eg, sputum induction, intubation, and airway suctioning) appear to be at particularly high risk [23]. A high degree of respiratory protection (ie, including airborne precautions) is currently recommended by the CDC because data on MERS-CoV transmission are limited; these guidelines are similar to what was recommended during the SARS response and will be updated as additional information becomes available.
No specific vaccine or treatment is currently available for MERS-CoV. Many hospitalized patients become severely ill, with respiratory failure followed by multiorgan failure [8]. Clinical management focuses on supportive care [8, 16, 18]. In a small retrospective cohort study, 20 severely ill patients with MERS-CoV were treated with a combination of ribavirin and interferon alfa-2a, vs 24 patients in a comparison group. Improved survival in treated patients was noted at 14 days, but the results at 28 days were not statistically significant. A randomized controlled trial will be needed to determine if this treatment is of benefit [25].
No restrictions on travel to or from the Arabian Peninsula are recommended [26]. However, the CDC recommends that travelers protect themselves from MERS-CoV exposure by washing their hands frequently and avoiding close contact with ill persons. Given the emerging data on camels as a reservoir, the World Health Organization and the CDC recommend general hygiene measures (including regular handwashing before and after touching animals and avoiding contact with sick animals) for persons visiting farms, markets, or other places where animal contact is possible [26]. Consumption of raw or undercooked animal products, including camel milk, should also be avoided. Additional precautions that are recommended for persons at high risk for severe MERS (people with diabetes, kidney failure, chronic lung disease, or weakened immune systems) include avoiding contact with camels as well as consumption of raw camel milk and urine. In addition, people who are traveling to the region to provide healthcare services should review the CDC's infection control guidelines for MERS [26]. Travelers from the region with onset of fever or respiratory symptoms during their trip or within 14 days of leaving the region should seek medical care. Before presenting for care, patients should inform the healthcare facility of their recent travel so appropriate isolation measures can be implemented.
To prevent further introduction of cases of MERS-CoV into the United States, the CDC has developed guidance for US travelers to countries in or near the Arabian Peninsula about MERS-CoV, including information aimed at those attending mass gatherings, such as the Hajj and Umrah [26], and public health messages about MERS have been posted at US airports. The CDC has also conducted MERS outreach with community-based organizations, travel agencies, institutes of higher learning, and businesses for travelers to the Arabian Peninsula. The CDC has also shared guidance to rapidly identify MERS-CoV cases among travelers to the United States with airlines, US Customs and Border Protection, and the US Transportation Security Administration.
The CDC is working with international partners to conduct studies aimed at better understanding MERS-CoV transmission and risk factors for illness in community and hospital settings. As new information becomes available, the CDC will update its recommendations [18]. MERS-CoV and Ebola virus disease remind us all of the interconnectedness of the United States to the rest of the world. With the increase in global travel, we must remain alert for emerging infectious diseases to protect US residents and the world from these public health threats.
Notes
Acknowledgments. We acknowledge Huong Pham, Jessica Rudd, Aaron Curns, and Rebecca Dahl for their assistance with collection and compilation of epidemiologic data on Middle East respiratory syndrome cases.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Financial support. All authors completed this work as part of their official duties at the CDC.
Potential conflicts of interest. All authors: No potential conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Rha B, Rudd J, Feikin D, et al. Update on the epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, and guidance for the public, clinicians, and public health authorities—January 2015. MMWR Morb Mortal Wkly Rep 2015; 64:61–2. [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Coronavirus infections—disease oubreak news. Available at: http://www.who.int/csr/don/archive/disease/coronavirus_infections/en/ Accessed 25 February 2015.
- 3. Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis 2013; 13:752–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saad M, Omrani AS, Baig K, et al. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis 2014; 29:301–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Memish ZA, Al-Tawfiq JA, Assiri A, et al. Middle East respiratory syndrome coronavirus disease in children. Pediatr Infect Dis J 2014; 33:904–6. [DOI] [PubMed] [Google Scholar]
- 6. WHO MERS-CoV Research Group. State of knowledge and data gaps of Middle East respiratory syndrome coronavirus (MERS-CoV) in humans. PLoS Curr 2013; 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thomas HL, Zhao H, Green HK, et al. Enhanced MERS coronavirus surveillance of travelers from the Middle East to England. Emerg Infect Dis 2014; 20:1562–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arabi YM, Arifi AA, Balkhy HH, et al. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med 2014; 160:389–97. [DOI] [PubMed] [Google Scholar]
- 9. Al-Tawfiq JA, Memish ZA. Middle East respiratory syndrome coronavirus: epidemiology and disease control measures. Infect Drug Resist 2014; 7:281–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Raj VS, Farag EA, Reusken CB, et al. Isolation of MERS coronavirus from a dromedary camel, Qatar, 2014. Emerg Infect Dis 2014; 20:1339–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reusken CB, Haagmans BL, Muller MA, et al. Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect Dis 2013; 13:859–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Haagmans BL, Al Dhahiry SH, Reusken CB, et al. Middle East respiratory syndrome coronavirus in dromedary camels: an outbreak investigation. Lancet Infect Dis 2014; 14:140–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alagaili AN, Briese T, Mishra N, et al. Middle East respiratory syndrome coronavirus infection in dromedary camels in Saudi Arabia. MBio 2014; 5:e00884–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Azhar EI, El-Kafrawy SA, Farraj SA, et al. Evidence for camel-to-human transmission of MERS coronavirus. N Engl J Med 2014; 370:2499–505. [DOI] [PubMed] [Google Scholar]
- 15. Memish ZA, Cotten M, Meyer B, et al. Human infection with MERS coronavirus after exposure to infected camels, Saudi Arabia, 2013. Emerg Infect Dis 2014; 20:1012–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bialek SR, Allen D, Alvarado-Ramy F, et al. First confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in the United States, updated information on the epidemiology of MERS-CoV infection, and guidance for the public, clinicians, and public health authorities—May 2014. MMWR Morb Mortal Wkly Rep 2014; 63:431–6. [PMC free article] [PubMed] [Google Scholar]
- 17. Kapoor M, Pringle K, Kumar A, et al. Clinical and laboratory findings of the first imported case of Middle East respiratory syndrome coronavirus to the United States. Clin Infect Dis 2014; 59:1511–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. Middle East respiratory syndrome (MERS): information for health providers. Available at: http://www.cdc.gov/coronavirus/mers/hcp.html Accessed 17 January 2015.
- 19. Lu X, Whitaker B, Sakthivel SK, et al. Real-time reverse transcription-PCR assay panel for Middle East respiratory syndrome coronavirus. J Clin Microbiol 2014; 52:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Drosten C, Muth D, Corman VM, et al. An observational, laboratory-based study of outbreaks of Middle East respiratory syndrome coronavirus in Jeddah and Riyadh, Kingdom of Saudi Arabia, 2014. Clin Infect Dis 2015; 60:369–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maltezou HC, Tsiodras S. Middle East respiratory syndrome coronavirus: implications for health care facilities. Am J Infect Control 2014; 42:1261–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Assiri A, McGeer A, Perl TM, et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med 2013; 369:407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Memish ZA, Zumla AI, Assiri A. Middle East respiratory syndrome coronavirus infections in health care workers. N Engl J Med 2013; 369:884–6. [DOI] [PubMed] [Google Scholar]
- 24. Al-Abdallat MM, Payne DC, Alqasrawi S, et al. Hospital-associated outbreak of Middle East respiratory syndrome coronavirus: a serologic, epidemiologic, and clinical description. Clin Infect Dis 2014; 59:1225–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Omrani AS, Saad MM, Baig K, et al. Ribavirin and interferon alfa-2a for severe Middle East respiratory syndrome coronavirus infection: a retrospective cohort study. Lancet Infect Dis 2014; 14:1090–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Centers for Disease Control and Prevention. Travelers’ health. Available at: http://wwwnc.cdc.gov/travel/notices/alert/coronavirus-saudi-arabia-qatar Accessed 17 January 2015.