Abstract
Rotator cuff tear has been a known entity for orthopaedic surgeons for more than two hundred years. Although the exact pathogenesis is controversial, a combination of intrinsic factors proposed by Codman and extrinsic factors theorized by Neer is likely responsible for most rotator cuff tears. Magnetic resonance imaging remains the gold standard for the diagnosis of rotator cuff tears, but the emergence of ultrasound has revolutionized the diagnostic capability. Even though mini-open rotator cuff repair is still commonly performed, and results are comparable to arthroscopic repair, all-arthroscopic repair of rotator cuff tear is now fast becoming a standard care for rotator cuff repair. Appropriate knowledge of pathology and healing pattern of cuff, strong and biological repair techniques, better suture anchors, and gradual rehabilitation of postcuff repair have led to good to excellent outcome after repair. As the healing of degenerative cuff tear remains unpredictable, the role of biological agents such as platelet-rich plasma and stem cells for postcuff repair augmentation is still under evaluation. The role of scaffolds in massive cuff tear is also being probed.
Keywords: biomechanics, pathoanatomy, rehabilitation, rotator cuff
Relevant anatomic details
Rotator cuff tendons form confluence with the joint capsule and coracohumeral ligament, and insert on the humeral tuberosity. The subscapularis (SC) is the largest and strongest cuff muscle with the upper 60% of the insertion being tendinous, and the lower 40% being muscular with footprint attachment varying from 24 to 40 mm in the superoinferior and 16–20 mm in the mediolateral directions. The supraspinatus (SS), infraspinatus (IS), and teres minor (TM) are inserted over the superior, middle, and inferior facets on to the greater tuberosity with a mean anteroposterior length of 37.8 mm, mean medial–lateral distance of 14.7 mm, and mean area of 6.2 cm2.Dugas et al1 suggested that the restoration of this footprint might increase the likelihood of normal healing and subsequent normal function. The SS muscle has two bellies, namely, anterior and posterior. The anterior belly has a larger physiologic cross-sectional area (140 ± 43 mm2) and a smaller tendon cross-sectional area (26.4 ± 11.3 mm2) as compared with the posterior belly, which has a smaller cross-sectional area (62 ± 25 mm2) but a larger tendon cross-sectional area (31.2 ± 10.1 mm2). The anterior belly has an intramuscular fusiform core tendon, whereas the posterior belly is strap like with no intramuscular tendon.2 Therefore, the peculiar anatomy of the anterior muscle with a larger belly, a fusiform cross section, and an intramuscular fusiform core tendon is responsible for the major contractile force generation by the SS and is primarily responsible for arm abduction and humeral head depression.2 It may also help explain why many patients who have SS tear with intact anterior tendon on the footprint retain their ability to flex forward and abduct their arm. Therefore, incorporation of the anterior tendon into rotator cuff tendon repair is an important aspect to enable transmission of the major portion of contractile loads, which subsequently improves functional outcome.2 On the downside, stronger leading edge of the SS forms the stress riser zone between the anterior and remaining mid-posterior fibres. This may explain why more than 90% of degenerative tears start and propagate from this junction. The IS tendon bends in its insertion anteriorly and covers the largest part of the greater tuberosity compared with the SS insertion.3 Histologically, there are five interlocked distinct layers of the SS and IS tendons.4, 5 Differential anatomy between various layers initiates stress risers and can cause intrasubstance tears that are two times as common as bursal- or articular-side tears. Robust collagen on the bursal side makes it more resistant to tensile stress. Therefore, the stress-failure point of the articular side is half of bursal side.6, 7, 8
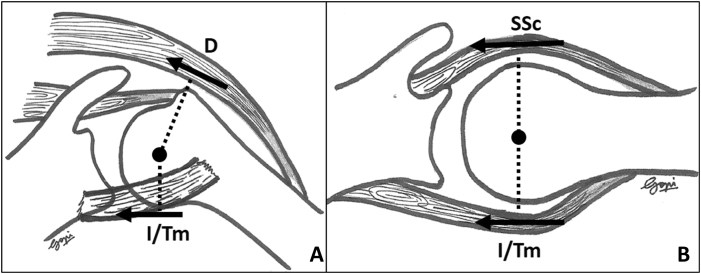
The primary function of the rotator cuff is to keep the head of the humerus depressed and centred into the glenoid fossa permitting a single centre of rotation, while allowing efficient abduction or forward elevation of the arm.9, 10 This centring in the glenoid by the cuff is achieved by balancing the force couples around the glenohumeral joint. A force couple is a pair of forces that act on an object and cause it to rotate. The shoulder joint has two force couples, namely, coronal and transverse (Fig. 1). The coronal force couple, which was first described by Inman et al,11 is a result of the balance of moments created by the deltoid versus inferior rotator cuff (IS, SC, and TM). The coronal force couple is said to be balanced only if the line of action of the rotator cuff force is below the centre of rotation of the humeral head so that it can oppose the moment created by the deltoid muscle. A balanced coronal force couple maintains adequate fulcrum for the glenohumeral joint motion. The transverse force couple, which was described by Burkhart,12, 13 is a balanced moment between the anterior SC and posterior IS–TM muscles. Burkhart emphasized the role of transverse force couple, which is imbalanced in massive cuff tear wherein the large tears of the SS gradually involve the IS too, in weakening the posterior cuff. This leads to imbalanced transverse as well as coronal force couples, leading to posterosuperior migration of the head and inability to maintain stable fulcrum of motion. Parsons et al14 in their study on nine cadaveric human shoulders emphasized that peak joint reaction forces (JRFs) drop by 10–11% in case of incomplete or complete tear of the SS. However, the peak abduction angle attained was almost similar to intact shoulder as concavity compression through the action of remaining cuff was sufficient to provide a fixed fulcrum for concentric rotation of the glenohumeral joint. However, the peak JRF further dropped by another 50% when tear propagated into the posteroinferior cuff. This disrupts the transverse force couple, and the deltoid is unable to achieve maximum abduction. Burkhart12, 13 established that restoration of transverse and coronal force couples by partial repair of tendons (IS and SC) in case of massive cuff tear can give surprisingly good results.
Fig. 1.
(A) Coronal force couple. (B) Transverse force couple. D = deltoid muscle force; I/Tm = infraspinatus/teres minor muscle force; SSc = subscapularis muscle force.
Aetiology of cuff tear
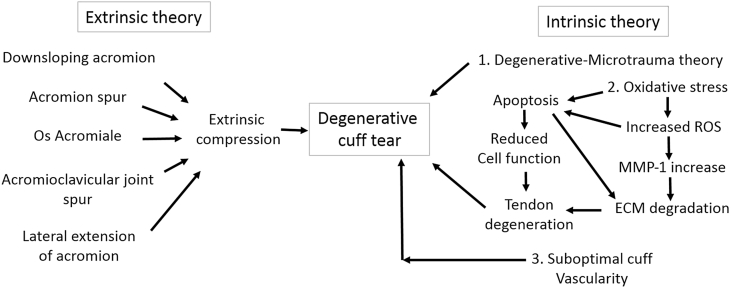
Cuff tears are either traumatic or degenerative. Traumatic tears are due to significant trauma, whereas degenerative tears are far more frequent and multifactorial in aetiology. The rotator cuff is weakened by both extrinsic and intrinsic factors, leading to gradual failure of tendon with or without superimposed acute injury, which finally results in full-thickness tear (Fig. 2).
Fig. 2.
Summary of extrinsic and intrinsic pathways of rotator cuff tear. ECM = extracellular matrix; MMP-1 = matrix metalloproteinase-1; ROS = reactive oxygen species.
Extrinsic theory
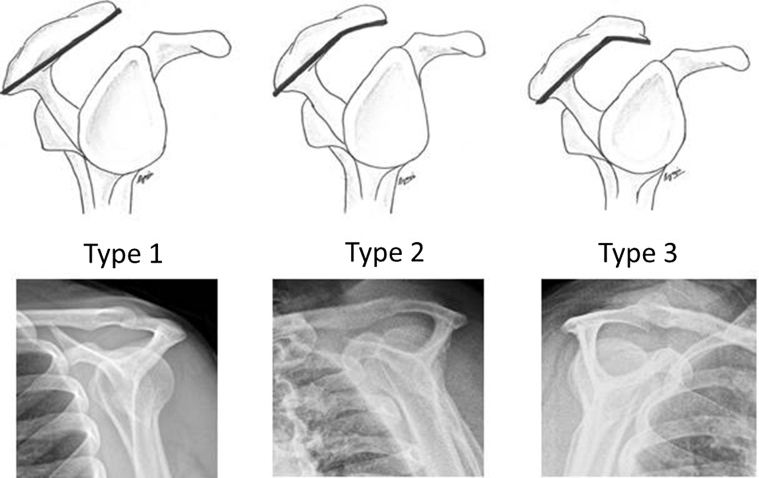
Neer's classic work advocated extrinsic factors for rotator cuff tendon failure in which during forward elevation of the shoulder, the anterior part of the cuff abuts against the coracoacromial (CA) arch and leads to impingement, tendonitis, and tear.15 Neer's theory got a boost when Bigliani et al16 proposed that downsloping acromion in the sagittal plane can impinge upon the anterior cuff, and could cause cuff tear. Bigliani et al classified the acromial morphology into three types, namely, type I (flat undersurface), type II (curved), and type III (hooked); (Fig. 3). Several authors confirmed close relationship between hooked acromion and cuff tear.17, 18, 19, 20 Wang et al21 concluded that patients with Bigliani type II and type III acromion are poor responders to conservative treatment for impingement syndrome. Various other factors such as the presence of acromial spur,22, 23 acromion slope,24, 25 CA ligament,26, 27, 28 os acromiale,29, 30, 31 and acromioclavicular joint spur32, 33 also contribute towards extrinsic compression. Recently, Nyffeler et al introduced the acromion index as a measurement of lateral extension of the acromion, which is associated with a higher incidence of rotator cuff disease.34 Balke et al35 also reported that lateral extension of the acromion (acromial index) and low lateral acromial angle are associated with a higher incidence of cuff tear. However, extrinsic theory of tendon failure has failed to explain the tears happening in the IS tendon or articular-side tear.36 While these extrinsic factors in isolation or in combination certainly seem to be playing an important role in the pathogenesis of SS tear, the consistency in relationship is yet to be proven due to the lack of quality of available data.
Fig. 3.
Bigliani's classification of acromion undersurface with corresponding supraspinatus outlet view radiograph.
Intrinsic theory
The intrinsic theory proposed by Codman encompasses multiple possible mechanisms that occur within the rotator cuff tendon to initiate the cuff tear.37
The commonest accepted theory is based on the degenerative-microtrauma model, which proposes that age-related degeneration compounded with repetitive microtrauma/loads leads to a partial tear that gradually converts into a full-thickness tear. Yamaguchi et al38, 39 proved that there is 50% chance of cuff tear after the age of 60, and Hashimoto et al40 reported that the rate of tear increases from 13% to 51% from the age of 50 to 80, suggesting that it could be a normal attrition process. With advancing age, the cuff undergoes several internal changes, such as collagen disorganization and thinning, myxoid and hyaline degeneration, fatty infiltration, and vascular proliferation.40 In a rat model, Plate et al41 demonstrated that advanced age leads to collagen fibre disorganization and structural changes, which potentially affect the rotator cuff tendon-to-bone healing. In addition, the type II collagen variant at the fibrocartilage junctions of the tendon that is primarily responsible for compressive load converts into type III. This decreases the capability of the tendon to withstand compressive loads and predisposes it for a tear. The degenerative process also leads to muscle atrophy and fatty infiltration, which is a part of the reparative process.42 This leads to loss of strength in the muscle and could render the outcome of the cuff repair unfavourable.43, 44 Budoff et al45 further stated that contractile overload leads to intrinsic damage to the tendon.
Another possible intrinsic theory is of oxidative stress in the local environment. The oxidative stress is perhaps produced due to repetitive injury followed by the reparative process. This oxidative stress induces tenocyte apoptosis due to excess levels of reactive oxygen species (ROS) that damages the tendon.46, 47, 48 Other inflammatory mediators that are found to be high during the process of oxidative stress are a local concentration of metalloproteases [matrix metalloprotease-1 (MMP-1), MMP-3, and MMP-13], cyclooxygenase-2 (COX-2), and prostaglandin E2. MMPs probably mediate the process of apoptosis and alter collagen structure, whereas COX-2 and prostaglandin E2 might be responsible for pain associated with cuff tear.49 Soslowsky et al emphasized that oxidative stress environment is further influenced by inflammatory mediators that alter tendon gene expression and histopathology of tendon due to repetitive injury.50, 51 Within 4 months of the onset of a tear, there is a drastic decrease in procollagen alpha-1-positive tendon cells in the tendon margin, which are responsible for tendon healing.52 Lundgreen et al53 evaluated the potential of the SS muscle in the partial and full-thickness SS tear groups and proved that the muscle in full-thickness tear showed reduced muscle proliferative capacity and satellite cells, muscle fibre atrophy, and loss of myosin heavy-chain content as compared with the partial thickness group.
Many authors have also investigated the role of cuff vascularity in cuff tear. Traditionally, the area 10–15 mm proximal to the SS tendon insertion is thought to be the site of critical ischaemia or hypovascular zone.54 Benjamin et al55 asserted that histological transition from tendon to calcified fibrocartilage during tendon-to-bone insertion leads to hypovascular zones in tendon and is also responsible for ruptures and poor healing of tendon after repair. However, the existence of such an area was challenged by Moseley and Goldie56 in cuff specimens. Rudzki et al57 demonstrated that cuff vascularity is significantly less after the age of 40 as compared with those under the age of 40, especially on the medial articular side. This might explain Codman's theory that lesion peel off starts on the medial articular side of the cuff probably due to decreasing vascularity in ageing tendons. Rudzki et al also demonstrated that cuff perfusion improves after exercise. Walch et al58 proposed the internal impingement mechanism of the undersurface as a cause of tendon failure in the posterior SS and the anterior IS along with posterosuperior labral tears in throwing athletes or those involved in overhead sports with extreme abduction and external rotation.
To conclude, intrinsic mechanism of cuff tear appears to be a complex process involving various inflammatory mediators (MMPs, prostaglandins, COX, ROS, and protein kinase, etc.), the apoptotic process, and tissue remodelling. In future, fundamental knowledge of such pathways would open newer channels of pharmacologic therapies that may be locally or systemically delivered to stimulate reparative process.
Pathology and pathomechanics
According to Codman, degenerative cuff tears initiate in the anterior fibres of SS as a peel-off lesion 7 mm behind the biceps pulley or in the SS tendon at a stress riser junction.59 However, Kim et al60 suggested that the most common site of the lesion is 15 mm behind the biceps tendon (BT). Nimura et al61 carried out a study on capsular attachment of the SS and IS, and reported that the thinnest part of the capsule lies 11 mm behind the anterior SS tendon, which may cause tears to begin posteriorly. The constant presence of peel-off lesion induces reactive changes on the footprint in the form of sclerosis and small cysts that can be easily recognized on plain X-ray. Peel-off lesion may heal, remain unchanged, or enlarge.62 Gradually, the peel-off lesion extends to the bursal surface and finally appears as a rim rent (pinhole) in the anterior SS. Interestingly, a small peel-off lesion is enough to weaken the SS centring effect leading to secondary impingement and initiation of Neer's bursal lesion on the anterior facet of the SS.63 This progressive enlargement of the peel-off lesion to full-thickness pinhole may take several months to years and then forms a small crescent-shaped tear. Meanwhile, progressive loss of the centring effect and impingement leads to four-stage acromial changes as observed by Uhthoff et al.28 First, there is a loss of acromial areolar tissue. Then the CA ligament and its footprint thickens, and the CA ligament shows fibrillation. Finally, there is loss of CA ligament footprint with balding of the acromial undersurface. Full-thickness tears do not heal and progress slowly unless compounded/aggravated by an acute traumatic event.52, 60, 64, 65, 66 Because the anterior strong part of tendon resists anterior tear migration, the progression of tear is usually posterior. During later stages, the tear becomes deep U or later L shaped due to capsular contracture and muscle–tendon unit pull.63 Posteriorly, the IS tendon subluxates backward and down. The long head of the BT undergoes hypertrophy and starts to fray. Anteriorly, the capsule–coracohumeral complex, which merges together, contracts and pulls the anterior SS tendon leading to the coracohumeral's forward subluxation towards the coracoid. Later, the anterior SS tendon stretches and uproots completely, thus exposing the BT with subsequent damage to the biceps pulley. This can cause BT rupture or subluxation over the SC, causing tear in the superior border of the SC. Finally, the SS retracts up to the glenoid due to continued capsular contracture and pull by muscle, the IS also ruptures and subluxates further inferiorly, and the SC tear proceeds further. This exposes the head and is termed classic “bald head tear” sign, which imbalances coronal and transverse force couples pushing the head cranially.63 However small is the cuff tear, cartilage degeneration begins in the glenohumeral joint.67 Later, rotator cuff arthropathy sets in with massive cuff tears.
Small degenerative tears of the SS are well tolerated functionally as long as the rotator cable is maintained, and the anterior strong SS tendon remains intact.14, 68 However, full-thickness tear involving complete SS tendon affects abduction and humeral rotational capability.69 Extension of the tear posteriorly or anteriorly into the IS or SC tendons, respectively, significantly alters glenohumeral JRFs and disrupts transverse force couple, forcing the head of the humerus to migrate superiorly.14, 70
Natural history of full-thickness cuff tear
Partial thickness cuff tears can heal (10%) or become smaller (10%) but 53% propagate and 28% become full-thickness tears.62 Full-thickness tears do not heal spontaneously and the majority (36–50%) progress in size gradually.66, 71, 72 Larger tears (>1–1.5 cm) have a greater rate of progression along with a higher incidence of muscle atrophy and fatty infiltration.73 Increase in tear size is associated with fatty infiltration into the muscle belly. In an ultrasonographic study of 251 full-thickness cuff tear, Kim et al60 suggested that with every 5-mm increase in the size of tear (either length or width), the odds of fatty infiltration double. Kim et al also suggested that tears that did not involve the anterior fibres of the SS had less risk of fatty infiltration. This could be due to the intact rotator cable suggested by Burkhart et al.74 Intact rotator cable enables the SS muscle to function optimally, avoiding muscle atrophy and fatty infiltration. Fatty infiltration, muscle atrophy, and BT changes are faster in newly symptomatic cuff tears.71 Moderate fatty infiltration appears after an average of 3 years and severe changes occur after 5 years of cuff tear.75, 76 The IS fatty infiltration is an indicator of multitendon tear.77 When the size of a cuff tear remains constant, patient may remain clinically asymptomatic or may complain of mild pain with intact active elevation. Onset of pain or worsening pain, with or without accompanying weakness in active arm elevation usually signals increasing size of cuff tear.
Classification
Many classifications exist in the literature for better understanding of tear patterns and their possible treatment options.78, 79, 80 All these classification systems consider one of the following factors: size, shape, retraction; however, none is comprehensive. Recently, the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine Shoulder Committee has recommended that the rotator cuff tear classification system takes the following five factors into account: location, extension, pattern, fatty atrophy, and retraction.81
Management of full-thickness cuff tear
While managing a cuff tear, certain factors are taken in account before repair.
-
•
Traumatic versus degenerative tears.
-
•
Asymptomatic and symptomatic cuff tears.
-
•
Patients and their demographic factors.
-
•
Reparability of the cuff.
Traumatic versus degenerative tears
In patients with traumatic full-thickness cuff tear with loss of active elevation, repair could be undertaken soon after oedema and inflammation subside and before the cuff retracts medially. The repair of traumatic cuff tear provides good result, but there is weak evidence in favour of early repair.82, 83
Asymptomatic versus symptomatic chronic reparable tear
A large number of cuff tear patients are asymptomatic and are two times as common as symptomatic ones.84 Keeping symptoms and function in mind, there are three broad categories of patients with “potentially reparable chronic full-thickness cuff tear”: (1) asymptomatic and functionally compensated, (2) mildly symptomatic but functionally compensated, and (3) functionally decompensated.
Asymptomatic and functionally compensated
Diagnosis of this category is usually made when bilateral ultrasound is performed to assess the health of the contralateral side in a patient with another shoulder symptomatic cuff tear. According to the recent American Academy of Orthopaedic Surgeons (AAOS) group recommendation, such asymptomatic cuff tears should be left alone and can be monitored under regular follow-up.83
Mildly symptomatic but functionally compensated
Patients in this category present with pain but retain ability to elevate the arm actively enough to perform activities of daily living (ADLs).57 Burkhart64, 85 suggested that despite having anatomic deficiency in the cuff structure, such functionally compensated patients have functionally optimal cuff probably due to intact rotator cable, which provides balanced force couple in the coronal and axial planes, maintaining the head centred into the glenoid. Pain may arise not only due to torn cuff but also due to multifactorial causes such as impingement, subacromial bursitis, BT affection, cartilage degeneration, and scapular muscle dysfunction. Pain can be managed by activity modification, analgesics, steroid injection, and focused physical therapy aiming at strengthening the remaining normal cuff and scapular muscles. Once the pain subsides, these patients may not require any surgical intervention. Nonetheless, patients in the “Asymptomatic and Functionally Compensated” and “Mildly Symptomatic but Functionally Compensated” categories should be informed about inevitable cuff tear enlargement in due course, which may be few months to years.65 In addition, prolonged inactivity in the dysfunctional part of the cuff leads to fatty infiltration and atrophy of muscle and further medial retraction with possible delamination of the tendon.60, 75, 76 Because of delamination and medial retraction, late repairs become technically challenging and anatomical footprint restoration may not be possible without tension that may affect the functional and structural outcomes of the repair.86, 87 A study by Zingg et al88 looked at the outcome of nonoperative management of 19 patients with massive cuff tear involving two or three tendons for 4 years. They concluded that the physical therapy could maintain satisfactory shoulder function in all patients. However, there was a substantial increase in the size of the tear, fatty infiltration, and osteoarthritis; in addition, four of the eight tear that were initially reparable, became irreparable. There is still ambiguity in the literature about the accurate treatment protocol for these asymptomatic and mildly symptomatic cuff tears. The rate of progression of an asymptomatic cuff tear is not precisely known and so may not justify immediate surgical repair; however, leaving it alone will convert a repairable tear into an irreparable tear in due course. Therefore, the patients must remain aware of informed neglect and its consequences if they choose the conservative line of treatment.
Painful and functionally decompensated
Patients of this category present with pain and inability to elevate the arm with severely compromised ADL. They can be given a trial of analgesics and physical therapy for few weeks. If they regain active elevation, with minimal pain and are able to perform ADL comfortably, they can be kept on regular follow-up to detect further enlargement of tear size, retraction, fatty infiltration, and atrophy using serial ultrasound sonography or magnetic resonance imaging (MRI). Later, they should be managed electively as discussed earlier. If they fail to recover within few weeks, surgical restoration of torn cuff at the footprint is advisable.83
Patients and their demographic factors
Age has been proved to be the most important predictor of clinical and radiological outcomes after the rotator cuff repair, as age is a predictor of tissue viability, and therefore, probably predicts success of cuff repair. Many studies have shown that the success of cuff repair decreases with advancing age especially after 65 years, and retear rates may be higher after 65 years.89, 90, 91, 92 Rhee et al93 in their report on 238 patients aged between 60 and 79 years concluded that patients over the age of 70 have higher rates of retear (51.1% vs. 39.8%) than those under the age of 70; however, the rate is not statistically significant. An interesting evidence using univariate analysis on factors affecting the cuff healing by Chung et al94 and Oh et al95 established that age is an important predictor in estimating cuff healing. However, multivariate analysis proved that fatty degeneration and tear characteristics showed a significant relation with cuff healing than age.94, 95 The AAOS Committee too finds weak evidence against age.83 Therefore, although age remains the most significant factor in determining the outcome of cuff repair, amount of fatty infiltration and muscle atrophy may also provide a guide to the age cut-off.
Reparability of the cuff
A cuff tear is considered to be irreparable when it cannot be closed adequately with proper footprint coverage or when its closure will indeed result in postoperative retear. Large or massively retracted cuff tears may not be reparable. If preoperative radiograph reveals anterosuperior migration or acromiohumeral distance less than 6 mm, chronically retracted two-tendon tear that may not be reparable is indicated.96 In such cases, MRI would be certainly helpful to assess the number of tendon involvement, retraction, fatty infiltration, and atrophy, and the surgeon may take all the factors into account before attempting surgical repair. Reparability also depends on size and shape of the tear. Davidson and Burkhart97 and Burkhart13 suggested a practical way to assess the shape and possible reparability of a tear. Type 1 tears are crescent shaped and can be repaired end to end on to the footprint with good to excellent prognosis. Type 2 tears are either L or U shaped and can be managed by side-to-side repair or margin convergence with good to excellent prognosis. Type 3 tears are massively retracted tears larger than 2 × 2 cm in the coronal–sagittal dimensions that may need extensive mobilization or interval slides, and may end up with partial repair. These repairs carry fair to good prognosis if transverse force couples are satisfactorily restored. Type 4 tears are associated with rotator cuff arthropathy, and may later require reverse arthroplasty.
Various surgical techniques of cuff repair
The following are the surgical techniques available, but their outcome is debatable:
-
•
Open/arthroscopic-assisted mini-open/all-arthroscopic technique.
-
•
Open transosseous/single row (SR)/classical double row (DR)/suture bridge DR transosseous equivalent (TOE) technique.
-
•
Subacromial bursectomy with/without acromioplasty.
Open/arthroscopic-assisted mini-open/all-arthroscopic technique
Rotator cuff tear can be repaired by direct open/arthroscopic-assisted mini-open repair or all-arthroscopic technique. The direct open technique (deltoid detachment) has been criticized in terms of more postoperative pain and stiffness as compared with arthroscopic techniques. However, many authors have refuted such claims.98, 99 Despite the deltoid dehiscence as an occasional disastrous complication of open cuff repair,100, 101 the long-term results of repair by the three listed techniques are comparable.102, 103, 104, 105, 106, 107, 108, 109 Currently, there is no consensus among shoulder surgeons about which technique offers superiority in terms of technique and outcome. Nonetheless, whichever technique is opted for cuff repair, it should involve certain principle of rotator cuff repair (Table 1).
Table 1.
Principles of rotator cuff repair.
| 1. Confirmation of cuff tear, manage pathologies of the biceps, labrum, and cartilage, if any. 2. Define the size and geography of the tear: how many tendons are involved? What type (crescent, or U or L shaped)? 3. Subacromial bursectomy, with or without acromioplasty. 4. Check the reducibility of the tendon at the footprint, whether it can be brought to footprint without tension. 5. Mobilization of tendon by peritendon release/interval/capsule release; if tendon is not reducible at footprint without tension. 6. Footprint preparation. 7. Repair of tendon with sutures and anchors or by transosseous technique. 8. Closely supervised and individualized rehabilitation programme. |
Open transosseous/SR/DR/TOE suture bridge technique
The controversy continues regarding the most optimal method to repair the cuff. Park et al110 stated that transosseous techniques restore better contact area and interface pressure over footprint as compared with anchor techniques that may be more helpful in tendon–tuberosity healing. They also demonstrated that even the DR technique restores only 50% of contact area and 80% of contact pressure as compared with the transosseous technique. Nonetheless, clinical results of open transosseous, suture anchor, and TOE techniques are comparable.111, 112 Currently, the transosseous technique is increasingly being performed arthroscopically with good results similar to other anchor-related techniques.113
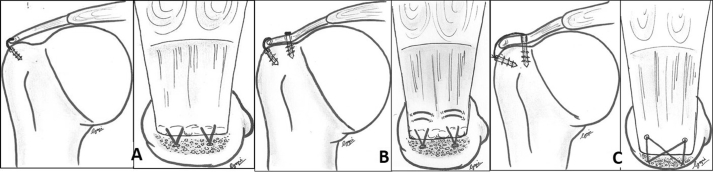
Technically, SR technique is simpler, quicker, inflicts less trauma to tendon margins, cheaper, and easier to revise. On the downside, the SR technique has smaller contact area and pressures, and the repaired tendon is allowed to heal over the smaller area, which theoretically predisposes SR repair to poor healing potential (Fig. 4A).114, 115 Despite theoretical shortcomings, good clinical and structural outcomes are reported throughout the literature with SR technique.114, 116, 117 Few studies have reported good clinical outcome with SR technique but higher rerupture at the end of 2 years.114, 115, 117, 118
Fig. 4.
Diagrammatic representation of (A) single row, (B) double row, and (C) transosseous equivalent suture anchor repair.
Classic DR technique with medial and lateral row of anchors was introduced with the aim of re-establishing the anatomical mediolateral footprint restoration, which enables better healing at the tendon–bone junction (Fig. 4B).119 DR repair encompasses restoration of a larger medial–lateral footprint area near the anatomical footprint with improved initial strength and stiffness, decreased least gap formation and strain as compared with SR or transosseous repair.120, 121, 122 However, classic DR is criticized for increased operative time, complexity of the procedure, and higher cost of more implants used without having any major added clinical advantage over SR. In addition, presence of excess implant at the footprint renders repair of retear difficult.123, 124, 125, 126 Although DR repair is stated to provide superior fixation properties, it can fail at the medial row (type 2 failure) near the musculotendinous junction.127, 128, 129
In DR TOE or suture bridge technique, suture ends bridge over the lateral cuff margin, thereby compressing the cuff over the footprint without passage of sutures through lateral stump (Fig. 4C). This spares the lateral edge of tendon from another set of sutures passing through the substance and probably preserves the vascularity of tendon.130, 131 Recent studies have reported similar results with TOE with respect to DR technique.132 However, TOE too has shown the medial tendon rupture tendency.90 TOE is comparable with DR in complexity of the procedure, cost, longer operative time, and morbidity.
Although SR, DR, and TOE present similar clinical results, many studies have shown that DR and TOE have better structural healing rates.133, 134, 135, 136 In a recent study by Mihata et al,137 the retear rates after arthroscopic rotator cuff repair were 10.8%, 26.1%, and 4.7%, respectively, for the SR, DR, and TOE techniques. In the subcategory of large and massive rotator cuff tears, the retear rate in the TOE group (7.5%) was significantly less than that in the SR group (62.5%, p < 0.001) and the DR group (41.7%, p < 0.01). Table 2 summarizes the outcome difference observed in various studies between SR and DR.133, 134, 135, 136 It appears that SR repair is sufficient for small- to medium-sized tears, but DR or TOE may be superior in large tears especially when structural integrity is concerned. A better structural integrity would perhaps ensure better structural and functional outcomes in the long term.133, 134, 135, 136
Table 2.
Clinical and structural outcomes of SR versus DR rotator cuff repair in various recent systematic reviews and meta-analysis.
| Author, y | Type of study | Comparative groups | Outcome |
|---|---|---|---|
| DeHaan et al (2012)133 | Systematic review of seven Level I and Level II studies | SR vs. DR |
Clinical outcome: No difference Structural outcome: Less retear in DR (27% vs. 43.1%) |
| Sheibani-Rad et al (2013)135 | Meta-analysis of five Level I studies | SR vs. DR | No difference in clinical and structural outcomes |
| Mascarenhas et al (2014)134 | Systematic review of eight Level I and Level II studies | SR vs. DR | DR provides superior structural healing to SR |
| Xu et al (2014)136 | Meta-analysis of nine Level I studies | SR vs. DR |
For small- and medium-sized tear: No difference in clinical and structural outcomes. For large-sized tear: DR better than SR |
DR = double row; SR = single row.
Subacromial decompression
Whether to perform acromioplasty or not is still a matter of debate. There are surgeons who strongly advocate it irrespective of the type of acromion and there are those who oppose it. Surgeons who advocate acromioplasty suggest that it improves CA arch morphology by preventing further compression over the cuff, improves visualization for cuff repair, and provides better healing response due to bleeding bone in the subacromial space.15, 138, 139 Those who oppose acromioplasty propose that the CA ligament is an important structure to prevent superior migration of the head and is contraindicated in massive cuff tear.140 In addition, even while performing arthroscopic acromioplasty, there can be damage to deltoid attachment.141
The emerging current consensus is that if the acromion is of type 3 or if it has downward-projecting acromial spur, acromioplasty is desirable as it clears the subacromial space from downward-protruding spurs or tip of type 3 acromion, which can endanger the integrity of the repaired cuff.21, 142 Because the results of cuff repair with or without acromioplasty in type I and II acromion are similar, type 1 and 2 should be left alone.142, 143 Perhaps, routine acromioplasty is not indicated anymore.83, 144
Factors influencing the outcome after cuff repair
There are surgical and patient factors that affect the outcome of cuff repair surgery. Surgical factors include open versus arthroscopic repair, SR versus DR, standard tuberosity preparation versus cancellous bone exposed (crimson Duvet), acromioplasty, etc. Many such surgical factors have already been discussed earlier with evidence for and against them. There is no evidence in the literature for or against the use of type of anchors and their outcome due to the limited availability of studies. Most surgeons continue to perform the standard tuberosity preparation. However, Snyder and Burns145 recommended the crimson duvet technique, which involves the exposure of the cancellous bone at the tuberosity lateral to the anchor placement, which helps in marrow and blood exudation over cuff that supposedly helps in healing.145 Milano et al146 conducted a prospective randomized study on 80 patients, with or without microfracture over the tuberosity during cuff repair. There was no clinical difference between the two groups, and they did not find any significant difference in the overall radiological healing between the two groups. However, a subgroup analysis on the large tears of the SS and IS revealed statistically significant healing in the microfracture group. Therefore, although performing a microfracture may be fine, a cautious approach is required as overzealous tuberosity preparation may affect the cortical fixation of anchor especially in an osteoporotic bone. Patient factors include age, smoking, body mass index (BMI), diabetes, osteoporosis, chronicity of tear, and tear characteristics. Many of them are modifiable, and some are not. Smoking has always been associated with poor healing properties of tissue. Galatz et al147 in an experiment on rats (nicotine vs. saline group) noted that nicotine delays tendon–bone healing. In their study, rats in the nicotine group had poorer type I collagen expression and inferior mechanical properties (chronic inflammation and decreased cell proliferation). Baumgarten et al148 noted that smokers had a higher risk of rotator cuff tear as compared with nonsmokers with dose-dependent and time-dependent relationship between smoking and rotator cuff tears, whereas Carbone et al149 noted that the severity of cuff tear increases with more numbers of cigarettes smoked. Diabetes is known to affect healing by affecting the microvasculature. Bedi et al150 found that diabetic rats have less fibrocartilage, less organized collagen, and more advanced glycosylated end product at the tendon–bone interface, and these animals demonstrated significantly reduced ultimate load to failure and stiffness of rotator cuff. Abate et al151 proved that diabetics are more prone to age-related degenerative disorder of cuff tendons and bursitis as compared with controls. Chen et al152 and Clement et al153 concluded that patients with diabetics show slower improvements after cuff surgery compared with nondiabetic patients. Higher BMI or obesity reportedly does not have a negative influence on rotator cuff outcome.142, 154 Chronicity of tear may affect the repair outcome. Cho and Rhee155 reported complete healing rates of 83% and 71% in patients who underwent surgery for tear within 1 year and after more than 1 year, respectively, but this difference was not statistically significant. A study by Charousset et al118 suggested that healing rates in patients who underwent surgery within 1 year are far better than those who underwent surgery after more than 1 year (60% and 26%, respectively; p < 0.05). However, we believe that chronicity may play an indirect role in repair outcome as it affects the quality of muscle and tendon unit with a higher degree of atrophy, fatty infiltration, lamination, and retraction. Tear characteristics directly affect the repair outcome. Many studies have shown that small- and medium-sized tears carry greater chance of healing as compared with large and massive tears,118, 137, 155, 156 and if two or more tendons are involved in tear, it reduces the chance of healing and leads to poor outcome.156, 157, 158 Tendons with poor quality are more prone to nonhealing at the tuberosity as compared with the healthy cuff tissue.83, 156, 157 Tendons with higher fatty infiltration index (>1) or Goutallier grade 2 and above do affect healing rates significantly.118, 155, 159 Lastly, osteoporosis too may affect the anchor-holding property and tendon healing on to the tuberosity.118
Rehabilitation
Apart from biological and surgical factors, the outcome of rotator cuff repair may also depend on how well rehabilitation programme is executed. Allowing healing of the repaired cuff on to the footprint while minimizing the stiffness and muscle atrophy is the goal of rehabilitation. Various rehabilitation protocols have been designed around the fundamentals of tendon–bone healing potential. Table 3 summarizes the three histological phases of rotator cuff healing on to the footprint.160 The first two phases lasts for 4–6 weeks, and remodelling starts after 6 weeks. During remodelling, type 3 collagen is replaced by type 1 collagen and cuff heals on to the footprint with scar-tissue formation. Further, natural tendon-to-bone transition including unmineralized and mineralized fibrocartilage is not recreated during remodelling phase.161 Furthermore, in animal models, mature healing and remodelling of the tissue does not reach maximal tensile strength before 12–16 weeks.162 Therefore, it is advisable to avoid isometric strengthening of the cuff before 3 months.
Table 3.
Histological process of rotator cuff healing on to the footprint.
| Phase | Microscopic process |
|---|---|
| 1 | Inflammation: Inflammatory cells, platelets, and fibroblast migrate at the site |
| 2 | Proliferation: Cellular proliferation and matrix deposition and yield of type 3 collagen |
| 3 | Remodelling: Gradual conversion of type 3 collagen into type 1 and scar formation |
Traditionally, immediate mobilization was started after rotator cuff repair to prevent stiffness.163, 164, 165 However, there were concerns regarding increased retear rates, which led to the adoption of delayed rehabilitation protocol.166, 167 Although complete immobilization may lead to low scar volume,168 many studies recommend a brief period of immobilization in mild abduction as it improves collagen strength, orientation and viscoelastic properties, and vascularity of repair tissue in comparison with immediate mobilization.169, 170 In addition, early mobilization may lead to increased micromotion at the repair site and gap formation leading to poor healing of cuff. Besides, most retears develop with 3–6 months of repair, which further supports the concept of initial immobilization.171, 172 However, whether it has to be a slow and protective or accelerated rehabilitation continues to be a matter of debate. Table 4 summarizes the outcome of various studies on rehabilitation protocol.173, 174, 175, 176, 177 The arm position during immobilization may also play a role in tendon healing. Slight abduction at shoulder may improve the vascularity and minimize the tension at the repaired site.169
Table 4.
Clinical and structural outcomes in the early and delayed rehabilitation groups after arthroscopic rotator cuff repair in various RCTs, systematic reviews, and meta-analysis.
| Author, y | Type of study | Comparative group characteristics (early vs. delayed rehabilitation) | Outcome |
|---|---|---|---|
| Cuff and Pupello (2012)173 | RCT, 64 patients | Crescent tear; TOE repair |
Functional result: No difference between the two groups Structural result: Better healing rate in the delayed group (91% vs. 85%, p > 0.5) |
| Lee et al (2012)176 | Comparative study, 68 patients | Medium–large-sized tear; SR repair |
Functional result: Better recovery in 3 months but no difference at 1 year Structural result: Better healing of cuff in the delayed rehabilitation group vs. the aggressive group (91.2 % vs. 76.7 %, p = 0.105) |
| Keener et al (2014)174 | RCT, 124 patients | Small–medium-sized tears; TOE repair | No difference in functional or structural outcome |
| Kluczynski et al (2014)175 | Systematic review and meta-analysis, 28 studies | Small–large-sized tear; TO, SR, DR repairs |
Risk of retear was high for tear size > 5 cm in the early group vs. the late group repaired by DR (56.4% vs. 20%, p = 0.002; RR = 2.82) and for all repair methods combined (52.2% vs. 22.6%, p = 0.01; RR = 2.31) |
| Ross et al (2014)177 | Review of seven studies (RCTs and other types) | All types of tear and repair | The accelerated group has a trend for better pain, ROM, and functional scores, but slightly higher retear rates as compared with the slow rehabilitation group |
DR = double row; RCT = randomized controlled trial; ROM = range of motion; SR = single row; TO = transosseous; TOE = transosseous equivalent; RR = relative risk.
Perhaps, it may be wise at times to individualize the rehabilitation programme according to patient's need. With the quality of currently available literature, we feel that it may be prudent to adhere to delayed rehabilitation programme if the tear size is large, the quality of repaired tissue is poor, or SR repair is performed for large-sized tear to minimize the risk of retear. Patients who are at risk of developing postoperative stiffness, especially patients with diabetes or calcific tendonitis, can be allowed to perform early passive table slides as recommended by Koo et al.178
Recent advances in cuff repair
Current research is aimed at facilitating the healing process after cuff repair, especially in degenerative tears where healing is unpredictable. Present research on the use of growth factors (bone morphogenetic protein, fibroblast growth factor, platelet-derived growth factor, and transforming growth factor), stem-cell augmentation of tendon healing, and rotator cuff repair, or gene therapy is underway.179, 180 Platelet-rich plasma (PRP) in postrepair cuff has been studied by many authors, but contrasting results were reported, with some studies suggesting beneficial effect181, 182 and some suggesting no effect of PRP in healing response.183, 184, 185 A systematic review involving five studies on PRP by Chahal et al186 failed to demonstrate any beneficial effect of PRP, whereas a meta-analysis involving seven studies by Zhang et al187 showed some benefit in small- to medium-sized tear but no effect in healing large to massive tears. The role of scaffold or augmentation patches, which are derived from mammalian extracellular matrix (human, porcine, bovine, and equine), synthetic co-polymers (poly-l-lactide, polycarbonate, polyurethane urea), and other combinations, is being extensively evaluated in large to massive cuff tear to compensate for defects. Scaffold not only mechanically reinforces defective part of the tendon but also stimulates the intrinsic healing potential of tendon. Several studies have shown promising short-term results using scaffolds in massive tear.188, 189, 190, 191 A prospective randomized study by Barber et al188 in two group of patients with two-tendon tear greater than 3 cm, with and without augmentation patch, resulted in statistically significant improvement in pain and movement scores in the augmentation group at the mean of 14.5 months. Bond et al189 using human dermal matrix graft (GRAFTJACKET) in 16 patients achieved encouraging results in massive and irreparable cuff tears at the mean follow-up of 26.8 months. Ciampi et al190 showed good results using polypropylene patch in patients with massive posterosuperior massive cuff tear at the end of 36 months. They also showed graft incorporation on MRI evaluation. Another study by Proctor191 on 18 patients with large to massive cuff tear who underwent repair with poly-l-lactic acid synthetic patch showed intact repair at 42 months in 78% cases.191 However, there is still a long way to go before the use of scaffold becomes practical in massive tears.
Conclusion
Although constant research in rotator cuff pathology and treatment has made considerable progress in the last two decades, there is still a long way to go in improving the outcome of rotator cuff repair especially in large and massive cuff tears. The treatment of the cuff repair should be individualized according to the age, tear characteristics, chronicity, repair integrity, and individualized rehabilitation, which would ensure better structural healing and functional outcome. Well-designed, large, prospective, randomized, controlled trials in the areas of operative versus nonoperative treatment, SR versus DR, slow versus delayed rehabilitation are the need of the hour to improve the long-term outcome of rotator cuff repair. Future research will focus on scaffolds and biological agents to ensure better healing of large degenerative cuff tear.
Conflicts of interest
Dr Vivek Pandey and Dr W. Jaap Willems are the authors of the manuscript and have no conflicts of interest.
Acknowledgements
We are thankful to Dr. Gopinath, resident orthopaedics, KMC Manipal for the drawings provided for the article.
References
- 1.Dugas J.R., Campbell D.A., Warren R.F., Robie B.H., Millett P.J. Anatomy and dimensions of rotator cuff insertions. J Shoulder Elbow Surg. 2002;11:498–503. doi: 10.1067/mse.2002.126208. [DOI] [PubMed] [Google Scholar]
- 2.Roh M.S., Wang V.M., April E.W., Pollock R.G., Bigliani L.U., Flatow E.L. Anterior and posterior musculotendinous anatomy of the supraspinatus. J Shoulder Elbow Surg. 2000;9:436–440. doi: 10.1067/mse.2000.108387. [DOI] [PubMed] [Google Scholar]
- 3.Mochizuki T., Sugaya H., Uomizu M. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008;90:962–969. doi: 10.2106/JBJS.G.00427. [DOI] [PubMed] [Google Scholar]
- 4.Clark J.M., Harryman D.T., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713–725. [PubMed] [Google Scholar]
- 5.Sonnabend D.H., Yu Y., Howlett C.R., Harper G.D., Walsh W.R. Laminated tears of the human rotator cuff: a histologic and immunochemical study. J Shoulder Elbow Surg. 2001;10:109–115. doi: 10.1067/mse.2001.112882. [DOI] [PubMed] [Google Scholar]
- 6.Lee S.B., Nakajima T., Luo Z.P., Zobitz M.E., Chang Y.W., An K.N. The bursal and articular sides of the supraspinatus tendon have a different compressive stiffness. Clin Biomech (Bristol, Avon) 2000;15:241–247. doi: 10.1016/s0268-0033(99)00086-8. [DOI] [PubMed] [Google Scholar]
- 7.Luo Z.P., Hsu H.C., Grabowski J.J., Morrey B.F., An K.N. Mechanical environment associated with rotator cuff tears. J Shoulder Elbow Surg. 1998;7:616–620. doi: 10.1016/s1058-2746(98)90010-6. [DOI] [PubMed] [Google Scholar]
- 8.Nakajima T., Rokuuma N., Hamada K., Tomatsu T., Fukuda H. Histologic and biomechanical characteristics of the supraspinatus tendon: reference to rotator cuff tearing. J Shoulder Elbow Surg. 1994;3:79–87. doi: 10.1016/S1058-2746(09)80114-6. [DOI] [PubMed] [Google Scholar]
- 9.Saha A.K. Dynamic stability of the glenohumeral joint. Acta Orthop Scand. 1972;42:476–483. doi: 10.3109/17453677108989066. [DOI] [PubMed] [Google Scholar]
- 10.Basmajian J.V., Bazant F.J. Factors preventing downward dislocation of the adducted shoulder joint. An electromyographic and morphological study. J Bone Joint Surg Am. 1959;41A:1182–1186. [PubMed] [Google Scholar]
- 11.Inman V.T., Saunders J.B., Abbott L.C. Observations of the function of the shoulder joint. 1944. Clin Orthop Relat Res. 1996:3–12. doi: 10.1097/00003086-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart S.S. Partial repair of massive rotator cuff tears: the evolution of a concept. Orthop Clin North Am. 1997;28:125–132. doi: 10.1016/s0030-5898(05)70270-4. [DOI] [PubMed] [Google Scholar]
- 13.Burkhart S.S. A stepwise approach to arthroscopic rotator cuff repair based on biomechanical principles. Arthroscopy. 2000;16:82–90. doi: 10.1016/s0749-8063(00)90133-6. [DOI] [PubMed] [Google Scholar]
- 14.Parsons I.M., Apreleva M., Fu F.H., Woo S.L. The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J Orthop Res. 2002;20:439–446. doi: 10.1016/S0736-0266(01)00137-1. [DOI] [PubMed] [Google Scholar]
- 15.Neer C.S., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 16.Bigliani L.U., Morrison D.S., April E.W. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:216. [Google Scholar]
- 17.Bigliani L.U., Ticker J.B., Flatow E.L., Soslowsky L.J., Mow V.C. The relationship of acromial architecture to rotator cuff disease. Clin Sports Med. 1991;10:823–838. [PubMed] [Google Scholar]
- 18.Epstein R.E., Schweitzer M.E., Frieman B.G., Fenlin J.M., Jr., Mitchell D.G. Hooked acromion: prevalence on MR images of painful shoulders. Radiology. 1993;187:479–481. doi: 10.1148/radiology.187.2.8475294. [DOI] [PubMed] [Google Scholar]
- 19.Nicholson G.P., Goodman D.A., Flatow E.L., Bigliani L.U. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1–11. doi: 10.1016/s1058-2746(96)80024-3. [DOI] [PubMed] [Google Scholar]
- 20.Worland R.L., Lee D., Orozco C.G., SozaRex F., Keenan J. Correlation of age, acromial morphology, and rotator cuff tear pathology diagnosed by ultrasound in asymptomatic patients. J South Orthop Assoc. 2003;12:23–26. [PubMed] [Google Scholar]
- 21.Wang J.C., Horner G., Brown E.D., Shapiro M.S. The relationship between acromial morphology and conservative treatment of patients with impingement syndrome. Orthopedics. 2000;23:557–559. doi: 10.3928/0147-7447-20000601-12. [DOI] [PubMed] [Google Scholar]
- 22.Hamid N., Omid R., Yamaguchi K., Steger-May K., Stobbs G., Keener J.D. Relationship of radiographic acromial characteristics and rotator cuff disease: a prospective investigation of clinical, radiographic, and sonographic findings. J Shoulder Elbow Surg. 2012;21:1289–1298. doi: 10.1016/j.jse.2011.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogawa K., Yoshida A., Inokuchi W., Naniwa T. Acromial spur: relationship to aging and morphologic changes in the rotator cuff. J Shoulder Elbow Surg. 2005;14:591–598. doi: 10.1016/j.jse.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Banas M.P., Miller R.J., Totterman S. Relationship between the lateral acromion angle and rotator cuff disease. J Shoulder Elbow Surg. 1995;4:454–461. doi: 10.1016/s1058-2746(05)80038-2. [DOI] [PubMed] [Google Scholar]
- 25.Hawkins R.J., Kennedy J.C. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151–158. doi: 10.1177/036354658000800302. [DOI] [PubMed] [Google Scholar]
- 26.Chambler A.F., Pitsillides A.A., Emery R.J. Acromial spur formation in patients with rotator cuff tears. J Shoulder Elbow Surg. 2003;12:314–321. doi: 10.1016/s1058-2746(03)00030-2. [DOI] [PubMed] [Google Scholar]
- 27.Soslowsky L.J., An C.H., DeBano C.M., Carpenter J.E. Coracoacromial ligament: in situ load and viscoelastic properties in rotator cuff disease. Clin Orthop Relat Res. 1996:40–44. doi: 10.1097/00003086-199609000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Uhthoff H.K., Hammond D.I., Sarkar K., Hooper G.J., Papoff W.J. The role of the coracoacromial ligament in the impingement syndrome. A clinical, radiological and histological study. Int Orthop. 1988;12:97–104. doi: 10.1007/BF00266972. [DOI] [PubMed] [Google Scholar]
- 29.Hutchinson M.R., Veenstra M.A. Arthroscopic decompression of shoulder impingement secondary to os acromiale. Arthroscopy. 1993;9:28–32. doi: 10.1016/s0749-8063(05)80341-x. [DOI] [PubMed] [Google Scholar]
- 30.Ryu R.K., Fan R.S., Dunbar W.H., 5th The treatment of symptomatic os acromiale. Orthopedics. 1999;22:325–328. doi: 10.3928/0147-7447-19990301-09. [DOI] [PubMed] [Google Scholar]
- 31.Warner J.J., Beim G.M., Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg Am. 1998;80:1320–1326. doi: 10.2106/00004623-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 32.Gohlke F., Barthel T., Gandorfer A. The influence of variations of the coracoacromial arch on the development of rotator cuff tears. Arch Orthop Trauma Surg. 1993;113:28–32. doi: 10.1007/BF00440591. [DOI] [PubMed] [Google Scholar]
- 33.Petersson C.J., Gentz C.F. Ruptures of the supraspinatus tendon. The significance of distally pointing acromioclavicular osteophytes. Clin Orthop Relat Res. 1983:143–148. [PubMed] [Google Scholar]
- 34.Nyffeler R.W., Werner C.M., Sukthankar A., Schmid M.R., Gerber C. Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am. 2006;88:800–805. doi: 10.2106/JBJS.D.03042. [DOI] [PubMed] [Google Scholar]
- 35.Balke M., Schmidt C., Dedy N., Banerjee M., Bouillon B., Liem D. Correlation of acromial morphology with impingement syndrome and rotator cuff tears. Acta Orthop. 2013;84:178–183. doi: 10.3109/17453674.2013.773413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ko J.Y., Huang C.C., Chen W.J., Chen C.E., Chen S.H., Wang C.J. Pathogenesis of partial tear of the rotator cuff: a clinical and pathologic study. J Shoulder Elbow Surg. 2006;15:271–278. doi: 10.1016/j.jse.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 37.Codman E.A. Complete rupture of the supraspinatus tendon. Operative treatment with report of two successful cases. 1911. Boston Med Surg J. 1911;164:708–710. doi: 10.1016/j.jse.2010.10.031. [DOI] [PubMed] [Google Scholar]
- 38.Tempelhof S., Rupp S., Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–299. doi: 10.1016/s1058-2746(99)90148-9. [DOI] [PubMed] [Google Scholar]
- 39.Yamaguchi K., Ditsios K., Middleton W.D., Hildebolt C.F., Galatz L.M., Teefey S.A. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699–1704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 40.Hashimoto T., Nobuhara K., Hamada T. Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin Orthop Relat Res. 2003:111–120. doi: 10.1097/01.blo.0000092974.12414.22. [DOI] [PubMed] [Google Scholar]
- 41.Plate J.F., Brown P.J., Walters J. Advanced age diminishes tendon-to-bone healing in a rat model of rotator cuff repair. Am J Sports Med. 2014;42:859–868. doi: 10.1177/0363546513518418. [DOI] [PubMed] [Google Scholar]
- 42.Goutallier D., Postel J.M., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994:78–83. [PubMed] [Google Scholar]
- 43.Gerber C., Schneeberger A.G., Hoppeler H., Meyer D.C. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007;16:691–696. doi: 10.1016/j.jse.2007.02.122. [DOI] [PubMed] [Google Scholar]
- 44.Rokito A.S., Cuomo F., Gallagher M.A., Zuckerman J.D. Long-term functional outcome of repair of large and massive chronic tears of the rotator cuff. J Bone Joint Surg Am. 1999;81:991–997. doi: 10.2106/00004623-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Budoff J.E., Nirschl R.P., Ilahi O.A., Rodin D.M. Internal impingement in the etiology of rotator cuff tendinosis revisited. Arthroscopy. 2003;19:810–814. doi: 10.1016/s0749-8063(03)00732-1. [DOI] [PubMed] [Google Scholar]
- 46.Droge W. Oxidative stress and aging. Adv Exp Med Biol. 2003;543:191–200. doi: 10.1007/978-1-4419-8997-0_14. [DOI] [PubMed] [Google Scholar]
- 47.Yuan J., Murrell G.A., Trickett A., Landtmeters M., Knoops B., Wang M.X. Overexpression of antioxidant enzyme peroxiredoxin 5 protects human tendon cells against apoptosis and loss of cellular function during oxidative stress. Biochim Biophys Acta. 2004;1693:37–45. doi: 10.1016/j.bbamcr.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 48.Yuan J., Murrell G.A., Wei A.Q., Wang M.X. Apoptosis in rotator cuff tendinopathy. J Orthop Res. 2002;20:1372–1379. doi: 10.1016/S0736-0266(02)00075-X. [DOI] [PubMed] [Google Scholar]
- 49.Tsuzaki M., Guyton G., Garrett W. IL-1 beta induces COX2, MMP-1, -3 and -13, ADAMTS-4, IL-1 beta and IL-6 in human tendon cells. J Orthop Res. 2003;21:256–264. doi: 10.1016/S0736-0266(02)00141-9. [DOI] [PubMed] [Google Scholar]
- 50.Perry S.M., McIlhenny S.E., Hoffman M.C., Soslowsky L.J. Inflammatory and angiogenic mRNA levels are altered in a supraspinatus tendon overuse animal model. J Shoulder Elbow Surg. 2005;14:79S–83S. doi: 10.1016/j.jse.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 51.Soslowsky L.J., Thomopoulos S., Tun S. Neer Award 1999. Overuse activity injures the supraspinatus tendon in an animal model: a histologic and biomechanical study. J Shoulder Elbow Surg. 2000;9:79–84. [PubMed] [Google Scholar]
- 52.Hamada K., Tomonaga A., Gotoh M., Yamakawa H., Fukuda H. Intrinsic healing capacity and tearing process of torn supraspinatus tendons: in situ hybridization study of alpha 1 (I) procollagen mRNA. J Orthop Res. 1997;15:24–32. doi: 10.1002/jor.1100150105. [DOI] [PubMed] [Google Scholar]
- 53.Lundgreen K., Lian O.B., Engebretsen L., Scott A. Lower muscle regenerative potential in full-thickness supraspinatus tears compared to partial-thickness tears. Acta Orthop. 2013;84:565–570. doi: 10.3109/17453674.2013.858289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lindblom K. On pathogenesis of ruptures of the tendon aponeurosis of the shoulder joint. Acta Radiol. 1939;20:563–577. [Google Scholar]
- 55.Benjamin M., Evans E.J., Copp L. The histology of tendon attachments to bone in man. J Anat. 1986;149:89–100. [PMC free article] [PubMed] [Google Scholar]
- 56.Moseley H.F., Goldie I. The arterial pattern of the rotator cuff of the shoulder. J Bone Joint Surg Br. 1963;45:780–789. [PubMed] [Google Scholar]
- 57.Rudzki J.R., Adler R.S., Warren R.F. Contrast-enhanced ultrasound characterization of the vascularity of the rotator cuff tendon: age- and activity-related changes in the intact asymptomatic rotator cuff. J Shoulder Elbow Surg. 2008;17:96S–100S. doi: 10.1016/j.jse.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 58.Walch G., Boileau P., Noel E., Donell S.T. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992;1:238–245. doi: 10.1016/S1058-2746(09)80065-7. [DOI] [PubMed] [Google Scholar]
- 59.Codman E.A. The pathology associated with the rupture of the supraspinatus tendon. Ann Surg. 1931;93:348–359. doi: 10.1097/00000658-193101000-00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim H.M., Dahiya N., Teefey S.A. Location and initiation of degenerative rotator cuff tears: an analysis of three hundred and sixty shoulders. J Bone Joint Surg Am. 2010;92:1088–1096. doi: 10.2106/JBJS.I.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nimura A., Kato A., Yamaguchi K. The superior capsule of the shoulder joint complements the insertion of the rotator cuff. J Shoulder Elbow Surg. 2012;21:867–872. doi: 10.1016/j.jse.2011.04.034. [DOI] [PubMed] [Google Scholar]
- 62.Yamanaka K., Matsumoto T. The joint side tear of the rotator cuff. A followup study by arthrography. Clin Orthop Relat Res. 1994:68–73. [PubMed] [Google Scholar]
- 63.Bunker T. Rotator cuff disease. Curr Orthop. 2002;16:223–233. [Google Scholar]
- 64.Burkhart S.S. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10:4–19. doi: 10.1016/s0749-8063(05)80288-9. [DOI] [PubMed] [Google Scholar]
- 65.Mall N.A., Kim H.M., Keener J.D. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92:2623–2633. doi: 10.2106/JBJS.I.00506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yamaguchi K., Tetro A.M., Blam O., Evanoff B.A., Teefey S.A., Middleton W.D. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
- 67.Feeney M.S., O'Dowd J., Kay E.W., Colville J. Glenohumeral articular cartilage changes in rotator cuff disease. J Shoulder Elbow Surg. 2003;12:20–23. doi: 10.1067/mse.2003.128565. [DOI] [PubMed] [Google Scholar]
- 68.Halder A.M., O'Driscoll S.W., Heers G. Biomechanical comparison of effects of supraspinatus tendon detachments, tendon defects, and muscle retractions. J Bone Joint Surg Am. 2002;84-A:780–785. doi: 10.2106/00004623-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 69.Oh J.H., Jun B.J., McGarry M.H., Lee T.Q. Does a critical rotator cuff tear stage exist? A biomechanical study of rotator cuff tear progression in human cadaver shoulders. J Bone Joint Surg Am. 2011;93:2100–2109. doi: 10.2106/JBJS.J.00032. [DOI] [PubMed] [Google Scholar]
- 70.Mura N., O'Driscoll S.W., Zobitz M.E. The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: a biomechanical study. J Shoulder Elbow Surg. 2003;12:179–184. doi: 10.1067/mse.2003.9. [DOI] [PubMed] [Google Scholar]
- 71.Moosmayer S., Tariq R., Stiris M., Smith H.J. The natural history of asymptomatic rotator cuff tears: a three-year follow-up of fifty cases. J Bone Joint Surg Am. 2013;95:1249–1255. doi: 10.2106/JBJS.L.00185. [DOI] [PubMed] [Google Scholar]
- 72.Safran O., Schroeder J., Bloom R., Weil Y., Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710–714. doi: 10.1177/0363546510393944. [DOI] [PubMed] [Google Scholar]
- 73.Tashjian R.Z. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589–604. doi: 10.1016/j.csm.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 74.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: an anatomic description of the shoulder's “suspension bridge”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 75.Melis B., DeFranco M.J., Chuinard C., Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010;468:1498–1505. doi: 10.1007/s11999-009-1207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Melis B., Nemoz C., Walch G. Muscle fatty infiltration in rotator cuff tears: descriptive analysis of 1688 cases. Orthop Traumatol Surg Res. 2009;95:319–324. doi: 10.1016/j.otsr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 77.Melis B., Wall B., Walch G. Natural history of infraspinatus fatty infiltration in rotator cuff tears. J Shoulder Elbow Surg. 2010;19:757–763. doi: 10.1016/j.jse.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 78.DeOrio J.K., Cofield R.H. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563–567. [PubMed] [Google Scholar]
- 79.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990:64–74. [PubMed] [Google Scholar]
- 80.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990:81–86. [PubMed] [Google Scholar]
Further reading
- 81.Arce G., Bak K., Bain G. Management of disorders of the rotator cuff: Proceedings of the ISAKOS Upper Extremity Committee Consensus Meeting. Arthroscopy. 2013;29:1840–1850. doi: 10.1016/j.arthro.2013.07.265. [DOI] [PubMed] [Google Scholar]
- 82.Mall N.A., Lee A.S., Chahal J. An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy. 2013;29:366–376. doi: 10.1016/j.arthro.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 83.Pedowitz R.A., Yamaguchi K., Ahmad C.S. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on: optimizing the management of rotator cuff problems. J Bone Joint Surg Am. 2012;94:163–167. [PubMed] [Google Scholar]
- 84.Minagawa H., Yamamoto N., Abe H. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop. 2013;10:8–12. doi: 10.1016/j.jor.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Burkhart S.S. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992:144–152. [PubMed] [Google Scholar]
- 86.Gladstone J.N., Bishop J.Y., Lo I.K., Flatow E.L. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–728. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 87.Kuzel B.R., Grindel S., Papandrea R., Ziegler D. Fatty infiltration and rotator cuff atrophy. J Am Acad Orthop Surg. 2013;21:613–623. doi: 10.5435/JAAOS-21-10-613. [DOI] [PubMed] [Google Scholar]
- 88.Zingg P.O., Jost B., Sukthankar A., Buhler M., Pfirrmann C.W., Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89:1928–1934. doi: 10.2106/JBJS.F.01073. [DOI] [PubMed] [Google Scholar]
- 89.Boileau P., Brassart N., Watkinson D.J., Carles M., Hatzidakis A.M., Krishnan S.G. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 90.Cho N.S., Yi J.W., Lee B.G., Rhee Y.G. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38:664–671. doi: 10.1177/0363546509350081. [DOI] [PubMed] [Google Scholar]
- 91.Choi S., Kim M.K., Kim G.M., Roh Y.H., Hwang I.K., Kang H. Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg. 2014;23:1675–1681. doi: 10.1016/j.jse.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 92.Le B.T., Wu X.L., Lam P.H., Murrell G.A. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014;42:1134–1142. doi: 10.1177/0363546514525336. [DOI] [PubMed] [Google Scholar]
- 93.Rhee Y.G., Cho N.S., Yoo J.H. Clinical outcome and repair integrity after rotator cuff repair in patients older than 70 years versus patients younger than 70 years. Arthroscopy. 2014;30:546–554. doi: 10.1016/j.arthro.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 94.Chung S.W., Oh J.H., Gong H.S., Kim J.Y., Kim S.H. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39:2099–2107. doi: 10.1177/0363546511415659. [DOI] [PubMed] [Google Scholar]
- 95.Oh J.H., Kim S.H., Kang J.Y., Oh C.H., Gong H.S. Effect of age on functional and structural outcome after rotator cuff repair. Am J Sports Med. 2010;38:672–678. doi: 10.1177/0363546509352460. [DOI] [PubMed] [Google Scholar]
- 96.Goutallier D., Le Guilloux P., Postel J.M., Radier C., Bernageau J., Zilber S. Acromio humeral distance less than six millimeter: its meaning in full-thickness rotator cuff tear. Orthop Traumatol Surg Res. 2011;97:246–251. doi: 10.1016/j.otsr.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 97.Davidson J., Burkhart S.S. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy. 2010;26:417–424. doi: 10.1016/j.arthro.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 98.Vastamaki H., Vastamaki M. Postoperative stiff shoulder after open rotator cuff repair: a 3- to 20-year follow-up study. Scand J Surg. 2014;103:263–270. doi: 10.1177/1457496913514383. [DOI] [PubMed] [Google Scholar]
- 99.Williams G., Jr., Kraeutler M.J., Zmistowski B., Fenlin J.M., Jr. No difference in postoperative pain after arthroscopic versus open rotator cuff repair. Clin Orthop Relat Res. 2014;472:2759–2765. doi: 10.1007/s11999-014-3715-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bigliani L.U., Cordasco F.A., McIlveen S.J., Musso E.S. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am. 1992;74:1505–1515. [PubMed] [Google Scholar]
- 101.Sher J.S., Iannotti J.P., Warner J.J., Groff Y., Williams G.R. Surgical treatment of postoperative deltoid origin disruption. Clin Orthop Relat Res. 1997:93–98. [PubMed] [Google Scholar]
- 102.Aleem A.W., Brophy R.H. Outcomes of rotator cuff surgery: what does the evidence tell us? Clin Sports Med. 2012;31:665–674. doi: 10.1016/j.csm.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 103.Bartl C., Kouloumentas P., Holzapfel K. Long-term outcome and structural integrity following open repair of massive rotator cuff tears. Int J Shoulder Surg. 2012;6:1–8. doi: 10.4103/0973-6042.94304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Buess E., Steuber K.U., Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy. 2005;21:597–604. doi: 10.1016/j.arthro.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 105.Kang L., Henn R.F., Tashjian R.Z., Green A. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007;23:573–582. doi: 10.1016/j.arthro.2007.01.011. 582.e1–e2. [DOI] [PubMed] [Google Scholar]
- 106.Lindley K., Jones G.L. Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthop (Belle Mead NJ) 2010;39:592–600. [PubMed] [Google Scholar]
- 107.Mohtadi N.G., Hollinshead R.M., Sasyniuk T.M., Fletcher J.A., Chan D.S., Li F.X. A randomized clinical trial comparing open to arthroscopic acromioplasty with mini-open rotator cuff repair for full-thickness rotator cuff tears: disease-specific quality of life outcome at an average 2-year follow-up. Am J Sports Med. 2008;36:1043–1051. doi: 10.1177/0363546508314409. [DOI] [PubMed] [Google Scholar]
- 108.Morse K., Davis A.D., Afra R., Kaye E.K., Schepsis A., Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36:1824–1828. doi: 10.1177/0363546508322903. [DOI] [PubMed] [Google Scholar]
- 109.Nho S.J., Shindle M.K., Sherman S.L., Freedman K.B., Lyman S., MacGillivray J.D. Systematic review of arthroscopic rotator cuff repair and mini-open rotator cuff repair. J Bone Joint Surg Am. 2007;89:127–136. doi: 10.2106/JBJS.G.00583. [DOI] [PubMed] [Google Scholar]
- 110.Park M.C., Cadet E.R., Levine W.N., Bigliani L.U., Ahmad C.S. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33:1154–1159. doi: 10.1177/0363546504273053. [DOI] [PubMed] [Google Scholar]
- 111.Behrens S.B., Bruce B., Zonno A.J., Paller D., Green A. Initial fixation strength of transosseous-equivalent suture bridge rotator cuff repair is comparable with transosseous repair. Am J Sports Med. 2012;40:133–140. doi: 10.1177/0363546511426071. [DOI] [PubMed] [Google Scholar]
- 112.Maier D., Jaeger M., Izadpanah K. [Open transosseous reconstruction of the rotator cuff: clinical outcome, influencing factors and complications] Chirurg. 2012;83:1068–1077. doi: 10.1007/s00104-012-2399-2. [Article in German] [DOI] [PubMed] [Google Scholar]
- 113.Kuroda S., Ishige N., Mikasa M. Advantages of arthroscopic transosseous suture repair of the rotator cuff without the use of anchors. Clin Orthop Relat Res. 2013;471:3514–3522. doi: 10.1007/s11999-013-3148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 115.Tuoheti Y., Itoi E., Yamamoto N. Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med. 2005;33:1869–1874. doi: 10.1177/0363546505278256. [DOI] [PubMed] [Google Scholar]
- 116.Ide J., Maeda S., Takagi K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy. 2005;21:1090–1098. doi: 10.1016/j.arthro.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 117.Sugaya H., Maeda K., Matsuki K., Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 118.Charousset C., Bellaiche L., Kalra K., Petrover D. Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older? Arthroscopy. 2010;26:302–309. doi: 10.1016/j.arthro.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 119.Lo I.K., Burkhart S.S. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035–1042. doi: 10.1016/j.arthro.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 120.Baums M.H., Spahn G., Steckel H., Fischer A., Schultz W., Klinger H.M. Comparative evaluation of the tendon-bone interface contact pressure in different single- versus double-row suture anchor repair techniques. Knee Surg Sports Traumatol Arthrosc. 2009;17:1466–1472. doi: 10.1007/s00167-009-0771-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kim D.H., Elattrache N.S., Tibone J.E. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34:407–414. doi: 10.1177/0363546505281238. [DOI] [PubMed] [Google Scholar]
- 122.Waltrip R.L., Zheng N., Dugas J.R., Andrews J.R. Rotator cuff repair. A biomechanical comparison of three techniques. Am J Sports Med. 2003;31:493–497. doi: 10.1177/03635465030310040301. [DOI] [PubMed] [Google Scholar]
- 123.Aydin N., Kocaoglu B., Guven O. Single-row versus double-row arthroscopic rotator cuff repair in small- to medium-sized tears. J Shoulder Elbow Surg. 2010;19:722–725. doi: 10.1016/j.jse.2009.11.053. [DOI] [PubMed] [Google Scholar]
- 124.Franceschi F., Ruzzini L., Longo U.G. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254–1260. doi: 10.1177/0363546507302218. [DOI] [PubMed] [Google Scholar]
- 125.Koh K.H., Kang K.C., Lim T.K., Shon M.S., Yoo J.C. Prospective randomized clinical trial of single- versus double-row suture anchor repair in 2- to 4-cm rotator cuff tears: clinical and magnetic resonance imaging results. Arthroscopy. 2011;27:453–462. doi: 10.1016/j.arthro.2010.11.059. [DOI] [PubMed] [Google Scholar]
- 126.Saridakis P., Jones G. Outcomes of single-row and double-row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am. 2010;92:732–742. doi: 10.2106/JBJS.I.01295. [DOI] [PubMed] [Google Scholar]
- 127.Mazzocca A.D., Millett P.J., Guanche C.A., Santangelo S.A., Arciero R.A. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33:1861–1868. doi: 10.1177/0363546505279575. [DOI] [PubMed] [Google Scholar]
- 128.Trantalis J.N., Boorman R.S., Pletsch K., Lo I.K. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2008;24:727–731. doi: 10.1016/j.arthro.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 129.Yamakado K., Katsuo S., Mizuno K., Arakawa H., Hayashi S. Medial-row failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2010;26:430–435. doi: 10.1016/j.arthro.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 130.Christoforetti J.J., Krupp R.J., Singleton S.B., Kissenberth M.J., Cook C., Hawkins R.J. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg. 2012;21:523–530. doi: 10.1016/j.jse.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 131.Park M.C., Elattrache N.S., Ahmad C.S., Tibone J.E. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy. 2006;22:1360.e1–1360.e5. doi: 10.1016/j.arthro.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 132.Toussaint B., Schnaser E., Bosley J., Lefebvre Y., Gobezie R. Early structural and functional outcomes for arthroscopic double-row transosseous-equivalent rotator cuff repair. Am J Sports Med. 2011;39:1217–1225. doi: 10.1177/0363546510397725. [DOI] [PubMed] [Google Scholar]
- 133.DeHaan A.M., Axelrad T.W., Kaye E., Silvestri L., Puskas B., Foster T.E. Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports Med. 2012;40:1176–1185. doi: 10.1177/0363546511428866. [DOI] [PubMed] [Google Scholar]
- 134.Mascarenhas R., Chalmers P.N., Sayegh E.T. Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy. 2014;30:1156–1165. doi: 10.1016/j.arthro.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 135.Sheibani-Rad S., Giveans M.R., Arnoczky S.P., Bedi A. Arthroscopic single-row versus double-row rotator cuff repair: a meta-analysis of the randomized clinical trials. Arthroscopy. 2013;29:343–348. doi: 10.1016/j.arthro.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 136.Xu C., Zhao J., Li D. Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elbow Surg. 2014;23:182–188. doi: 10.1016/j.jse.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 137.Mihata T., Watanabe C., Fukunishi K. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39:2091–2098. doi: 10.1177/0363546511415660. [DOI] [PubMed] [Google Scholar]
- 138.Hawkins R.J., Misamore G.W., Hobeika P.E. Surgery for full-thickness rotator-cuff tears. J Bone Joint Surg Am. 1985;67:1349–1355. [PubMed] [Google Scholar]
- 139.Romeo A.A., Hang D.W., Bach B.R., Jr., Shott S. Repair of full thickness rotator cuff tears. Gender, age, and other factors affecting outcome. Clin Orthop Relat Res. 1999:243–255. [PubMed] [Google Scholar]
- 140.Su W.R., Budoff J.E., Luo Z.P. The effect of coracoacromial ligament excision and acromioplasty on superior and anterosuperior glenohumeral stability. Arthroscopy. 2009;25:13–18. doi: 10.1016/j.arthro.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 141.Green A., Griggs S., Labrador D. Anterior acromial anatomy: relevance to arthroscopic acromioplasty. Arthroscopy. 2004;20:1050–1054. doi: 10.1016/j.arthro.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 142.MacDonald P., McRae S., Leiter J., Mascarenhas R., Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: a multicenter, randomized controlled trial. J Bone Joint Surg Am. 2011;93:1953–1960. doi: 10.2106/JBJS.K.00488. [DOI] [PubMed] [Google Scholar]
- 143.Shin S.J., Oh J.H., Chung S.W., Song M.H. The efficacy of acromioplasty in the arthroscopic repair of small- to medium-sized rotator cuff tears without acromial spur: prospective comparative study. Arthroscopy. 2012;28:628–635. doi: 10.1016/j.arthro.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 144.Shi L.L., Edwards T.B. The role of acromioplasty for management of rotator cuff problems: where is the evidence? Adv Orthop. 2012;2012:467571. doi: 10.1155/2012/467571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Snyder S.J., Burns J. Rotator cuff healing and the bone marrow ‘‘crimson duvet’’ from clinical observations to science. Tech Shoulder Elbow Surg. 2009;10:130–134. [Google Scholar]
- 146.Milano G., Saccomanno M.F., Careri S., Taccardo G., De Vitis R., Fabbriciani C. Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy. 2013;29:802–810. doi: 10.1016/j.arthro.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 147.Galatz L.M., Silva M.J., Rothermich S.Y., Zaegel M.A., Havlioglu N., Thomopoulos S. Nicotine delays tendon-to-bone healing in a rat shoulder model. J Bone Joint Surg Am. 2006;88:2027–2034. doi: 10.2106/JBJS.E.00899. [DOI] [PubMed] [Google Scholar]
- 148.Baumgarten K.M., Gerlach D., Galatz L.M. Cigarette smoking increases the risk for rotator cuff tears. Clin Orthop Relat Res. 2010;468:1534–1541. doi: 10.1007/s11999-009-0781-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Carbone S., Gumina S., Arceri V., Campagna V., Fagnani C., Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg. 2012;21:56–60. doi: 10.1016/j.jse.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 150.Bedi A., Fox A.J., Harris P.E. Diabetes mellitus impairs tendon-bone healing after rotator cuff repair. J Shoulder Elbow Surg. 2010;19:978–988. doi: 10.1016/j.jse.2009.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Abate M., Schiavone C., Salini V. Sonographic evaluation of the shoulder in asymptomatic elderly subjects with diabetes. BMC Musculoskelet Disord. 2010;11:278. doi: 10.1186/1471-2474-11-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chen A.L., Shapiro J.A., Ahn A.K., Zuckerman J.D., Cuomo F. Rotator cuff repair in patients with type I diabetes mellitus. J Shoulder Elbow Surg. 2003;12:416–421. doi: 10.1016/s1058-2746(03)00172-1. [DOI] [PubMed] [Google Scholar]
- 153.Clement N.D., Hallett A., MacDonald D., Howie C., McBirnie J. Does diabetes affect outcome after arthroscopic repair of the rotator cuff? J Bone Joint Surg Br. 2010;92:1112–1117. doi: 10.1302/0301-620X.92B8.23571. [DOI] [PubMed] [Google Scholar]
- 154.Namdari S., Baldwin K., Glaser D., Green A. Does obesity affect early outcome of rotator cuff repair? J Shoulder Elbow Surg. 2010;19:1250–1255. doi: 10.1016/j.jse.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 155.Cho N.S., Rhee Y.G. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1:96–104. doi: 10.4055/cios.2009.1.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gulotta L.V., Nho S.J., Dodson C.C., Adler R.S., Altchek D.W., MacGillivray J.D. Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: part II—prognostic factors for clinical and radiographic outcomes. J Shoulder Elbow Surg. 2011;20:941–946. doi: 10.1016/j.jse.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 157.Nho S.J., Shindle M.K., Adler R.S., Warren R.F., Altchek D.W., MacGillivray J.D. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009;18:697–704. doi: 10.1016/j.jse.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 158.Tashjian R.Z., Hollins A.M., Kim H.M. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med. 2010;38:2435–2442. doi: 10.1177/0363546510382835. [DOI] [PubMed] [Google Scholar]
- 159.Voigt C., Bosse C., Vosshenrich R., Schulz A.P., Lill H. Arthroscopic supraspinatus tendon repair with suture-bridging technique: functional outcome and magnetic resonance imaging. Am J Sports Med. 2010;38:983–991. doi: 10.1177/0363546509359063. [DOI] [PubMed] [Google Scholar]
- 160.Gulotta L.V., Rodeo S.A. Growth factors for rotator cuff repair. Clin Sports Med. 2009;28:13–23. doi: 10.1016/j.csm.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 161.Carpenter J.E., Thomopoulos S., Flanagan C.L., DeBano C.M., Soslowsky L.J. Rotator cuff defect healing: a biomechanical and histologic analysis in an animal model. J Shoulder Elbow Surg. 1998;7:599–605. doi: 10.1016/s1058-2746(98)90007-6. [DOI] [PubMed] [Google Scholar]
- 162.Sonnabend D.H., Howlett C.R., Young A.A. Histological evaluation of repair of the rotator cuff in a primate model. J Bone Joint Surg Br. 2010;92:586–594. doi: 10.1302/0301-620X.92B4.22371. [DOI] [PubMed] [Google Scholar]
- 163.Brislin K.J., Field L.D., Savoie F.H., 3rd Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007;23:124–128. doi: 10.1016/j.arthro.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 164.Liem D., Lichtenberg S., Magosch P., Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007;89:1770–1776. doi: 10.2106/JBJS.F.00749. [DOI] [PubMed] [Google Scholar]
- 165.Tauro J.C. Stiffness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006;22:581–586. doi: 10.1016/j.arthro.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 166.Koo S.S., Burkhart S.S. Rehabilitation following arthroscopic rotator cuff repair. Clin Sports Med. 2010;29:203–211. doi: 10.1016/j.csm.2009.12.001. vii. [DOI] [PubMed] [Google Scholar]
- 167.Parsons B.O., Gruson K.I., Chen D.D., Harrison A.K., Gladstone J., Flatow E.L. Does slower rehabilitation after arthroscopic rotator cuff repair lead to long-term stiffness? J Shoulder Elbow Surg. 2010;19:1034–1039. doi: 10.1016/j.jse.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 168.Galatz L.M., Charlton N., Das R., Kim H.M., Havlioglu N., Thomopoulos S. Complete removal of load is detrimental to rotator cuff healing. J Shoulder Elbow Surg. 2009;18:669–675. doi: 10.1016/j.jse.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 169.Rathbun J.B., Macnab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg Br. 1970;52:540–553. [PubMed] [Google Scholar]
- 170.Thomopoulos S., Williams G.R., Soslowsky L.J. Tendon to bone healing: differences in biomechanical, structural, and compositional properties due to a range of activity levels. J Biomech Eng. 2003;125:106–113. doi: 10.1115/1.1536660. [DOI] [PubMed] [Google Scholar]
- 171.Kluger R., Bock P., Mittlbock M., Krampla W., Engel A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med. 2011;39:2071–2081. doi: 10.1177/0363546511406395. [DOI] [PubMed] [Google Scholar]
- 172.Miller B.S., Downie B.K., Kohen R.B. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med. 2011;39:2064–2070. doi: 10.1177/0363546511413372. [DOI] [PubMed] [Google Scholar]
- 173.Cuff D.J., Pupello D.R. Prospective randomized study of arthroscopic rotator cuff repair using an early versus delayed postoperative physical therapy protocol. J Shoulder Elbow Surg. 2012;21:1450–1455. doi: 10.1016/j.jse.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 174.Keener J.D., Galatz L.M., Stobbs-Cucchi G., Patton R., Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014;96:11–19. doi: 10.2106/JBJS.M.00034. [DOI] [PubMed] [Google Scholar]
- 175.Kluczynski M.A., Nayyar S., Marzo J.M., Bisson L.J. Early versus delayed passive range of motion after rotator cuff repair: a systematic review and meta-analysis. Am J Sports Med. 2014 Oct 8 doi: 10.1177/0363546514552802. pii: 0363546514552802. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 176.Lee B.G., Cho N.S., Rhee Y.G. Effect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: aggressive versus limited early passive exercises. Arthroscopy. 2012;28:34–42. doi: 10.1016/j.arthro.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 177.Ross D., Maerz T., Lynch J., Norris S., Baker K., Anderson K. Rehabilitation following arthroscopic rotator cuff repair: a review of current literature. J Am Acad Orthop Surg. 2014;22:1–9. doi: 10.5435/JAAOS-22-01-1. [DOI] [PubMed] [Google Scholar]
- 178.Koo S.S., Parsley B.K., Burkhart S.S., Schoolfield J.D. Reduction of postoperative stiffness after arthroscopic rotator cuff repair: results of a customized physical therapy regimen based on risk factors for stiffness. Arthroscopy. 2011;27:155–160. doi: 10.1016/j.arthro.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 179.Isaac C., Gharaibeh B., Witt M., Wright V.J., Huard J. Biologic approaches to enhance rotator cuff healing after injury. J Shoulder Elbow Surg. 2012;21:181–190. doi: 10.1016/j.jse.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 180.Nixon A.J., Watts A.E., Schnabel L.V. Cell- and gene-based approaches to tendon regeneration. J Shoulder Elbow Surg. 2012;21:278–294. doi: 10.1016/j.jse.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 181.Jo C.H., Shin J.S., Lee Y.G. Platelet-rich plasma for arthroscopic repair of large to massive rotator cuff tears: a randomized, single-blind, parallel-group trial. Am J Sports Med. 2013;41:2240–2248. doi: 10.1177/0363546513497925. [DOI] [PubMed] [Google Scholar]
- 182.Randelli P., Arrigoni P., Ragone V., Aliprandi A., Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elbow Surg. 2011;20:518–528. doi: 10.1016/j.jse.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 183.Bergeson A.G., Tashjian R.Z., Greis P.E., Crim J., Stoddard G.J., Burks R.T. Effects of platelet-rich fibrin matrix on repair integrity of at-risk rotator cuff tears. Am J Sports Med. 2012;40:286–293. doi: 10.1177/0363546511424402. [DOI] [PubMed] [Google Scholar]
- 184.Castricini R., Longo U.G., De Benedetto M. Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: a randomized controlled trial. Am J Sports Med. 2011;39:258–265. doi: 10.1177/0363546510390780. [DOI] [PubMed] [Google Scholar]
- 185.Rodeo S.A., Delos D., Williams R.J., Adler R.S., Pearle A., Warren R.F. The effect of platelet-rich fibrin matrix on rotator cuff tendon healing: a prospective, randomized clinical study. Am J Sports Med. 2012;40:1234–1241. doi: 10.1177/0363546512442924. [DOI] [PubMed] [Google Scholar]
- 186.Chahal J., Van Thiel G.S., Mall N. The role of platelet-rich plasma in arthroscopic rotator cuff repair: a systematic review with quantitative synthesis. Arthroscopy. 2012;28:1718–1727. doi: 10.1016/j.arthro.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 187.Zhang Q., Ge H., Zhou J., Cheng B. Are platelet-rich products necessary during the arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. PLoS One. 2013;8:e69731. doi: 10.1371/journal.pone.0069731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Barber F.A., Burns J.P., Deutsch A., Labbe M.R., Litchfield R.B. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy. 2012;28:8–15. doi: 10.1016/j.arthro.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 189.Bond J.L., Dopirak R.M., Higgins J., Burns J., Snyder S.J. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJack et al lograft: technique and preliminary results. Arthroscopy. 2008;24:403–409. doi: 10.1016/j.arthro.2007.07.033. e401. [DOI] [PubMed] [Google Scholar]
- 190.Ciampi P., Scotti C., Nonis A. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears: a 3-year follow-up study. Am J Sports Med. 2014;42:1169–1175. doi: 10.1177/0363546514525592. [DOI] [PubMed] [Google Scholar]
- 191.Proctor C.S. Long-term successful arthroscopic repair of large and massive rotator cuff tears with a functional and degradable reinforcement device. J Shoulder Elbow Surg. 2014;23:1508–1513. doi: 10.1016/j.jse.2014.01.010. [DOI] [PubMed] [Google Scholar]