Abstract
Central nervous system involvement in Behçet's disease (Neuro-Behçet's disease: NBD) has been reported to present diverse clinical and pathological manifestations. A few cases presenting with neurological symptoms preceding other systemic features are difficult to be diagnosed. Here we suggest the clinical benefit of brain biopsy with a case of NBD initially presenting neurological symptoms.
Keywords: Neuro-Behçet's disease, Magnetic resonance imaging, Brain biopsy
Highlights
-
•
We report one case of neuro-Behçet's disease (NBD).
-
•
He presented with neurological symptoms without other preceding features.
-
•
Brain biopsy was useful to diagnose him with NBD.
-
•
Clinical utility of brain biopsy in NBD is suggested.
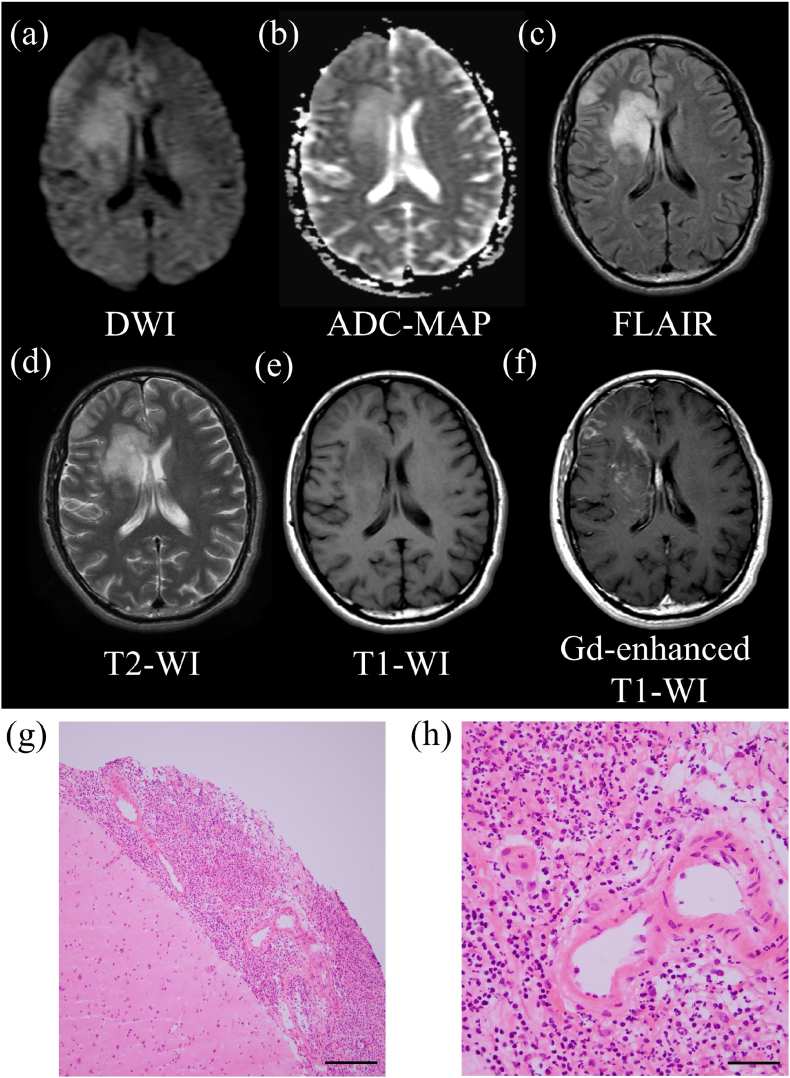
A 41-year-old man was admitted to our hospital with a fever and disturbance of consciousness. On a physical examination, he presented with a fever of 38.1 °C, headache, disorientation, hypersensitivity to touch, and pain on left side of the body. No skin, mucosa, or ophthalmologic lesions were observed. A blood test revealed an erythrocyte sedimentation rate (ESR) of 40 mm (1 h), white blood cells 8920/μL, and C-reactive protein (CRP) 4.2 mg/dL. Other blood tests for infectious disease such as syphilis, tuberculosis, cytomegalovirus, and human immunodeficiency virus were all negative. On a cerebrospinal fluid (CSF) examination, his total protein was 129.4 mg/dL, cell count 112/mm3 (mononuclear cells 95%, polynuclear cells 5%), and IL-6421 pg/mL. Human leukocyte antigen (HLA)-B51 was positive. Brain magnetic resonance imaging (MRI) showed tumefactive hyperintensity in the right frontal lobe and meninges on diffuse-weighted image (DWI), fluid-attenuated inversion recovery (FLAIR), and T2-weighted imaging (T2-WI) (Fig. 1a, c, d), an increased apparent diffusion coefficient (ADC) value (Fig. 1b), and hypointensities on T1-WI (Fig. 1e) with gadolinium enhancement in the cortex, meninges, and deep subcortical area presenting as tumor-like lesions (Fig. 1f).
Fig. 1.
a–f. Axial brain MRI. Tumefactive hyperintensity in the right frontal lobe and meninges on DWI (a), FLAIR (c), and T2-WI (f) with increased ADC values (b). Tumefactive hypointensity in the lesion on T1-WI (e), showing enhancement in the cortex, meninges, and deep subcortical area on gadolinium-enhanced T1-WI (f). g, h. Histopathology of biopsied right frontal lobe and meninges (Hematoxylin-Eosin staining). Inflammation of the meninges with intact brain parenchyma. Scale bar: 500 μm (g). Inflammatory infiltration of neutrophils around the blood vessels. Scale bar: 100 μm (h).
DWI: diffusion-weighted image, ADC-MAP: apparent diffusion coefficient map, FLAIR: fluid-attenuated inversion recovery, T2-WI: T2-weighted imaging, T1-WI: T1-weighted imaging, Gd-enhanced T1-WI: gadolinium-enhanced T1-WI.
A brain biopsy was considered to be necessary to exclude the possibility of a brain tumor or other diseases presenting with tumor-like lesions. A biopsy of the lesion was taken from the right frontal lobe with enhanced meninges. The histopathology showed perivascular infiltration of neutrophils in the meninges (Fig. 1g: × 40 and 1 h: × 200), while the brain parenchyma was intact (Fig. 1g).
This case did not meet the International Consensus Recommendation criteria for a Neuro-Behçet's disease (NBD) diagnosis (Kalra et al. J Neurol 2014) [1] because no oral or genital ulcerations, uveitis, or cutaneous lesions were noted. However, perivascular infiltration of neutrophils in the meninges suggested the possibility of a diagnosis of NBD. The patient was treated with intravenous methylprednisolone therapy (1000 mg/day) for 3 days and oral prednisolone therapy (1.0 mg/kg/day), which was reduced by 5 mg after 1 week. About eight months later, the patient presented with uveitis, genital ulcers, and intestinal inflammation in addition to the recurrence of the brain lesions. He was ultimately diagnosed with NBD.
We searched medical literature using PubMed (https://www.ncbi.nlm.nih.gov/pubmed/) with following words: “Behçet's disease”, “Neuro-Behçet's disease”, “Biopsy”, “Autopsy”, “Histopathology”, without limit of publication date. As a result, NBD has been reported to present with diverse clinical and pathological manifestations. Although the brain stem is the most common lesion site in NBD [2], tumor-like lesions have been also reported [3]. About 3% of patients have been also reported to develop neurological symptoms initially, followed by other systemic features in their clinical course [2]. A histopathological examination revealed perivascular neutrophilic infiltration with gliosis in autopsied NBD patients' brains [4]. In cases presenting with neurological symptoms preceding other systemic features, it is difficult to diagnose NBD based only on the clinical presentation and neuroimaging findings. Although the International Consensus Recommendation criteria for a Neuro-Behçet's disease (NBD) diagnosis suggested nervous system biopsy would be useful when all other diagnostic avenues have been exhausted [1], no previous papers have reported the brain biopsy in a case with NBD initially presenting neurological symptoms. In our case, a brain biopsy was helpful for his diagnosis and treatment.
Author contributions to the manuscript
Hiroki Yamada, Dr—Study concept and design, acquisition of data, analysis and interpretation and critical revision of the manuscript for important intellectual content.
Kazuyuki Saito, Dr-, PhD—Acquisition of data, analysis and interpretation and critical revision of the manuscript for important intellectual content.
Mitsuhiko Hokari, Dr—Acquistion of data (biopsy).
Shuta Toru, Dr-, PhD—Critical revision of the manuscript for important intellectual content, and study supervision.
None of the authors declare conflict of interest.
All human studies have been reviewed by the appropriate ethics committee.
References
- 1.Kalra S., Silman A., Akman-Demir G. Diagnosis and management of Neuro-Behçet's disease: international consensus recommendations. J Neurol. 2014;261:1662–1676. doi: 10.1007/s00415-013-7209-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akman-Demir G., Serdaroglu P., Tasçi B. Clinical patterns of neurological involvement in Behçet disease: evaluation of 200 patients. Brain. 1999;122:2171–2182. doi: 10.1093/brain/122.11.2171. [DOI] [PubMed] [Google Scholar]
- 3.Noel N., Hutié M., Wechsler B. Pseudotumoural presentation of neuro-Behcet's disease: case series and review of literature. Rheumatology. 2012;51:1216–1225. doi: 10.1093/rheumatology/ker449. [DOI] [PubMed] [Google Scholar]
- 4.Arai Y., Kohno S., Takahashi Y. Autopsy case of neuro-Behçet's disease with multifocal neutrophilic perivascular inflammation. Neuropathology. 2006;26:579–585. doi: 10.1111/j.1440-1789.2006.00734.x. [DOI] [PubMed] [Google Scholar]