Abstract
The burden of depression in men is high. Current diagnostic criteria may not fully capture men’s experience with depression. Descriptions of the heterogeneity in depression among men are lacking. The purpose of the study was to characterize latent subtypes of major depression and changes in these subtypes among men receiving citalopram in Level 1 of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial. Latent transition analysis was applied to data from 387 men who completed baseline and Week 12 study visits in Level 1 of STAR*D. Items from the self-report version of the Quick Inventory of Depressive Symptomatology were used as indicators of latent depression subtypes. Four statuses were identified at baseline and Week 12. Baseline statuses were Mild (10% of men), Moderate (53%), Severe with Psychomotor Slowing (20%), and Severe with Psychomotor Agitation (17%). At Week 12, the statuses were Symptom Resolution (41%), Mild (36%), Moderate (18%), and Severe with Psychomotor Slowing (5%). Men in the Mild status were most likely to transition to Symptom Resolution (probability = 69%). Men in the Severe with Agitation status were least likely to transition to Symptom Resolution (probability = 0%). This work highlights the need to not focus solely on summary rating scores but to also consider patterns of symptoms when treating depression.
Keywords: major depressive disorder, depression subtypes, latent transition analysis, STAR*D
Introduction
Major depressive disorder is a substantial public health problem, with considerable morbidity and mortality. The 12-month prevalence of a major depressive episode among adult men in the United States is approximately 5% (Substance Abuse and Mental Health Services Administration, 2013). This is likely an underestimate since it is thought that current diagnostic criteria do not adequately capture men’s experience with depression (Martin, Neighbors, & Griffith, 2013). It is also possible that the lower incidence of diagnosed depression in men reflects men’s tendency to deny illness and not seek treatment in order to preserve their masculinity (Addis & Mahalik, 2003). Despite the substantial burden of depression in men, it is often overlooked, with most research on sex differences focusing on women’s risk (Addis, 2008). As a result of depression commonly being interpreted as a women’s disorder, there is a poor understanding of how to best identify and treat men with depression (Ogrodniczuk & Oliffe, 2011). Successful recognition and treatment of depression in men is important, particularly because men are four times more likely than women to die from suicide and mood disorders such as depression are thought to be a major contributor to suicide risk (National Center for Injury Prevention and Control, 2013; Office of the U.S. Surgeon General and National Action Alliance for Suicide Prevention, 2012).
Sex differences have been documented in many aspects of depression, including rates, severity, symptoms, risk factors, and course. Men experience depression less often and less severely than women (Angst et al., 2002; Kendler & Gardner, 2014; Marcus et al., 2008; Substance Abuse and Mental Health Services Administration, 2013; E. A. Young et al., 2009). Men are more likely than women to endorse externalizing symptoms such as anger and aggression, substance abuse, and risky behavior but less likely to endorse stress, irritability, sleep problems, and lack of interest in previously enjoyable activities (Martin et al., 2013). Men are also more likely than women to have melancholic depression (Hildebrandt, Stage, & Kragh-Soerensen, 2003) but less likely to experience somatic, atypical, and anxiety symptoms (Lamers et al., 2010; Schuch, Roest, Nolen, Penninx, & de Jonge, 2014; Silverstein, 2002) and to have less transitions between subtypes (Rodgers, Ajdacic-Gross, et al., 2014). Risk factors for major depression for men include failure in financial and occupational goals, legal issues, and lowered self-worth (Kendler & Gardner, 2014).
Despite the well-documented sex differences in depression, these differences are not always considered in research on heterogeneity in depression. While symptom heterogeneity is expected for both men and women with major depression, little research has been done to characterize subtypes of depression in men and in changes in subtypes with treatment. An enhanced understanding of empirically derived depression subtypes and how these subtypes change over time is necessary for improving screening, treatments, and service delivery for men. This study used latent transition analysis (LTA), a person-centered modeling approach, to describe depression subtypes for men and examine changes in subtypes after receiving citalopram treatment in Level 1 of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial. Specifically, the objectives were to (a) characterize subtypes based on patterns of depression symptoms at the beginning of a treatment trial and (b) examine changes in these subtypes, including changes in the descriptive nature of each subtype, and how men move between subtypes, over 12 weeks of treatment.
Method
The institutional review board at the University of Massachusetts Medical School determined that this secondary data analysis was not human subjects research as defined by Department of Health and Human Services and Food and Drug Administration regulations.
Study Participants
In STAR*D, men and women with moderate-to-severe nonpsychotic major depression were originally enrolled from 41 sites (primary care and outpatient psychiatry) and participated in this pragmatic clinical trial designed to assess the effectiveness of a variety of pharmacological and psychosocial treatments (Rush et al., 2004). Enrollment occurred between July 2001 and April 2004 (n = 4,041). The protocol called for all participants to receive citalopram for at least 12 weeks during Level 1 of the trial. Using the publicly available, de-identified STAR*D data set from the National Institute of Mental Health, the present analysis was restricted to the Level 1 “evaluable sample (Rush et al., 2004; Trivedi et al., 2006)” of 1,044 men. The “evaluable sample” included participants whose baseline Hamilton Rating Scale of Depression (Hamilton, 1960) score was at least 14 and who completed at least one postbaseline visit (Trivedi et al., 2006). Although study visits occurred more frequently (baseline, 2, 4, 6, 9, and 12 weeks), the current study was restricted to men who completed the baseline and 12-week visits (n = 408), as necessary for this longitudinal analysis. The sample was further restricted to those with complete information on important study variables. The final study sample included 387 men.
Measures
Indicators of Latent Subtypes
The individual items from the self-report version of the Quick Inventory of Depressive Symptomatology (QIDS-SR16) served as indicator variables of latent depression subtype. The QIDS-SR16 measures depression severity and contains 16 items corresponding to the nine Diagnostic and Statistical Manual of Mental Disorders–Fourth edition (DSM-IV) symptom criterion domains for major depressive disorder (Rush et al., 2003). These items (scored 0 to 3) were collected at baseline and at Week 12. The time referent for most items was the previous 7 days with an exception for questions relating to changes in weight. The time referent for weight change variables was the previous 14 days. Because a symptom meets the DSM-IV threshold for major depressive disorder if scored 2 or above (Nierenberg et al., 2010), each item was dichotomized with scores ≤1 denoting the absence of a DSM-IV criterion symptom and ≥2 signifying presence. Although the QIDS-SR16 specifies that only one of the appetite items and only one of the weight items should be scored, all four items were included to adequately capture appetite increase, appetite decrease, weight increase, and weight decrease.
Analysis
The analysis was conducted in several stages. The first step was to compare the men who were included with those who were ineligible for the current study. Means and standard deviations were calculated for continuous variables and proportions for categorical variables. A 5% absolute difference in prevalence estimates was used to identify noteworthy differences between those included and excluded. Next, the basic latent status model for transitions between baseline and Week 12 of the trial was developed. An iterative process was used to identify the correct number of latent depression subtypes. This process involved fitting multiple basic LTA models with different numbers of statuses or subtypes (ranging from 2 to 7). The Akaike information criterion (Akaike, 1987) and Bayesian information criterion (Schwarz, 1978) were used in addition to the interpretability of the subtypes to decide the number of statuses because LTA models have very large degrees of freedom and extreme sparseness (Collins & Lanza, 2010). The difference G2 test (Collins & Lanza, 2010) was employed to rule out the assumption of measurement invariance of the qualitative nature of the statuses at baseline and 12 weeks. This was accomplished by comparing a model allowing variation between baseline and Week 12 item-response probabilities to a model constraining the item-response probabilities for both time points. Analyses were conducted using PROC LTA (Lanza & Collins, 2008; Lanza, Dziak, Huang, Wagner, & Collins, 2015) in SAS 9.3 (SAS Institute, Inc., Cary, NC).
Results
As summarized in Table 1, men who were included in this analysis were similar to those who were excluded in terms of demographic and clinical characteristics at baseline. The 387 men included in this analysis had a mean age of 44.6 years (SD = 12.5). Seventy-eight percent of these men were White (n = 303). The mean QIDS-SR16 score at baseline was 15.3 (SD = 3.9), which is indicative of moderate depression. Anxiety disorders were the most common psychiatric comorbidity. Approximately 29% of men had social phobia (n = 110), making it the most prevalent comorbid anxiety disorder. The prevalence of the depression symptoms measured by the QIDS-SR16 at baseline and Week 12 is reported in Table 2. At baseline, the majority of the included men were experiencing sleep-onset insomnia (63.6%), had midnocturnal insomnia (70.0%), sad mood (80.6%), impaired concentration (56.9%), lack of interest (58.4%), and fatigue (63.1%) but midnocturnal insomnia (61.2%) was the only depression symptom experienced by a majority by Week 12.
Table 1.
Baseline Demographic and Clinical Characteristics of Men Participating in STAR*D Level 1, by Inclusion Status.
| Characteristic | Included, n = 387 | Excluded, n = 657 | p |
|---|---|---|---|
| Age at study entry, M (SD) | 44.6 (12.5) | 42.3 (12.6) | .004 |
| Race, n (%) | |||
| White | 303 (78.3) | 519 (79.0) | .871 |
| Black or African American | 62 (16.0) | 98 (14.9) | |
| Other | 22 (5.7) | 40 (6.1) | |
| Hispanic, n (%) | 31 (8.0) | 58 (8.8) | .648 |
| Age at onset, M (SD) | 27.3 (14.7) | 26.5 (14.2) | .394 |
| Number of depressive episodes before baseline, M (SD) | 7.9 (12.8) | 6.5 (10.3) | .088 |
| Depression severity (QIDS-SR16) at baseline, M (SD) | 15.3 (3.9) | 15.8 (4.0) | .059 |
| Psychiatric comorbidities, n (%) | |||
| Generalized anxiety disorder | 74 (19.3) | 118 (18.3) | .689 |
| Posttraumatic stress disorder | 78 (20.4) | 127 (19.8) | .812 |
| Bulimia | 26 (6.7) | 44 (6.8) | .973 |
| Social phobia | 110 (28.8) | 182 (28.2) | .831 |
| Obsessive–compulsive disorder | 44 (11.5) | 83 (12.8) | .518 |
| Panic disorder | 42 (11.0) | 75 (11.6) | .753 |
| Psychosis | 48 (12.5) | 103 (15.9) | .138 |
| Agoraphobia | 35 (9.1) | 79 (12.2) | .129 |
| Alcohol abuse/dependence | 67 (17.5) | 118 (18.2) | .789 |
| Drug abuse/dependence | 38 (9.9) | 68 (10.5) | .749 |
| Somatization disorder | 3 (0.8) | 7 (1.1) | .636 |
| Hypochondriasis | 6 (1.6) | 29 (4.5) | .012 |
Note. STAR*D = Sequenced Treatment Alternatives to Relieve Depression; QIDS-SR16 = Quick Inventory of Depressive Symptomatology.
Table 2.
Frequency of QIDS-SR16 Items at Baseline and Week 12 for Eligible Men Participating in Level 1 of STAR*D (n = 387).
| QIDS-SR16 items | Baseline, n (%) | Week 12, n (%) |
|---|---|---|
| Sleep-onset insomnia | 246 (63.6) | 125 (32.3) |
| Midnocturnal insomnia | 271 (70.0) | 237 (61.2) |
| Early morning insomnia | 180 (46.5) | 95 (24.6) |
| Hypersomnia | 38 (9.8) | 37 (9.6) |
| Sad mood | 312 (80.6) | 93 (24.0) |
| Decreased appetite | 80 (20.7) | 22 (5.7) |
| Increased appetite | 41 (10.6) | 25 (6.5) |
| Decreased weight | 52 (13.4) | 11 (2.8) |
| Increased weight | 27 (7.0) | 18 (4.7) |
| Impaired concentration | 220 (56.9) | 77 (19.9) |
| Negative view of self | 179 (46.3) | 65 (16.8) |
| Suicidal ideation | 51 (13.2) | 19 (4.9) |
| Lack of interest | 226 (58.4) | 70 (18.1) |
| Fatigue | 244 (63.1) | 69 (17.8) |
| Psychomotor retardation | 126 (32.6) | 46 (11.9) |
| Psychomotor agitation | 130 (33.6) | 59 (15.3) |
Note. QIDS-SR16 = Quick Inventory of Depressive Symptomatology; STAR*D = Sequenced Treatment Alternatives to Relieve Depression.
A four-status LTA model fit the data best at both baseline and Week 12. The fit statistics used in determining the most appropriate model are reported in Supplementary Table 1. The item-response probabilities of the symptoms characterizing each status are displayed in Table 3. At baseline, the subtypes were Mild Depression, Moderate Depression, Severe Depression with Psychomotor Slowing, and Severe Depression with Psychomotor Agitation. At Week 12, the Mild, Moderate, and Psychomotor Slowing subtypes were still present but a Symptom Resolution subtype had emerged. The results of the G2 difference test are reported in Supplementary Table 1. The G2 difference test suggested that measurement invariance of the overall item-response probabilities across time could not be assumed, meaning that the subtypes were qualitatively different at each time ( − = 117.53, degrees of freedom = 64, p < .0001). After thoroughly considering the interpretation of each individual subtype at each time, however, measurement invariance was assumed for the Mild, Moderate, and Psychomotor Slowing subtypes between baseline and Week 12.
Table 3.
Item-Response Probabilities From Four-Status Latent Transition Analysis of QIDS-SR16 Indicators With Measurement Invariance on the Conditional Probabilities for the Mild, Moderate, and Severe With Psychomotor Slowing Subtypes at Baseline and Week 12.
| Baseline latent subtypes |
Week 12 latent subtypes |
|||||||
|---|---|---|---|---|---|---|---|---|
| QIDS-SR16 items | Mild | Moderate | Severe with Psychomotor Slowing | Severe with Psychomotor Agitation | Symptom Resolution | Mild | Moderate | Severe with Psychomotor Slowing |
| Sleep-onset insomnia | .35 | .56 | .82 | .83 | .13 | .35 | .56 | .82 |
| Midnocturnal insomnia | .71 | .69 | .83 | .76 | .39 | .71 | .69 | .83 |
| Early morning insomnia | .35 | .34 | .66 | .86 | .00 | .35 | .34 | .66 |
| Hypersomnia | .05 | .15 | .12 | .00 | .09 | .05 | .15 | .12 |
| Sad mood | .11 | .84 | .89 | .89 | .06 | .11 | .84 | .89 |
| Decreased appetite | .05 | .07 | .44 | .49 | .00 | .05 | .07 | .44 |
| Increased appetite | .07 | .17 | .08 | .00 | .00 | .07 | .17 | .08 |
| Decreased weight | .04 | .07 | .16 | .34 | .01 | .04 | .07 | .16 |
| Increased weight | .05 | .10 | .06 | .00 | .03 | .05 | .10 | .06 |
| Impaired concentration | .59 | .51 | .93 | .59 | .01 | .59 | .51 | .93 |
| Negative self-view | .41 | .47 | .76 | .41 | .02 | .41 | .47 | .76 |
| Suicidal ideation | .03 | .15 | .24 | .03 | .02 | .03 | .15 | .24 |
| Lack of general interest | .72 | .51 | .81 | .72 | .00 | .72 | .51 | .81 |
| Fatigue | .63 | .57 | .96 | .63 | .00 | .63 | .57 | .96 |
| Psychomotor retardation | .27 | .21 | .86 | .27 | .00 | .27 | .21 | .86 |
| Psychomotor agitation | .62 | .26 | .45 | .62 | .00 | .62 | .26 | .45 |
Note. QIDS-SR16 = Quick Inventory of Depressive Symptomatology.
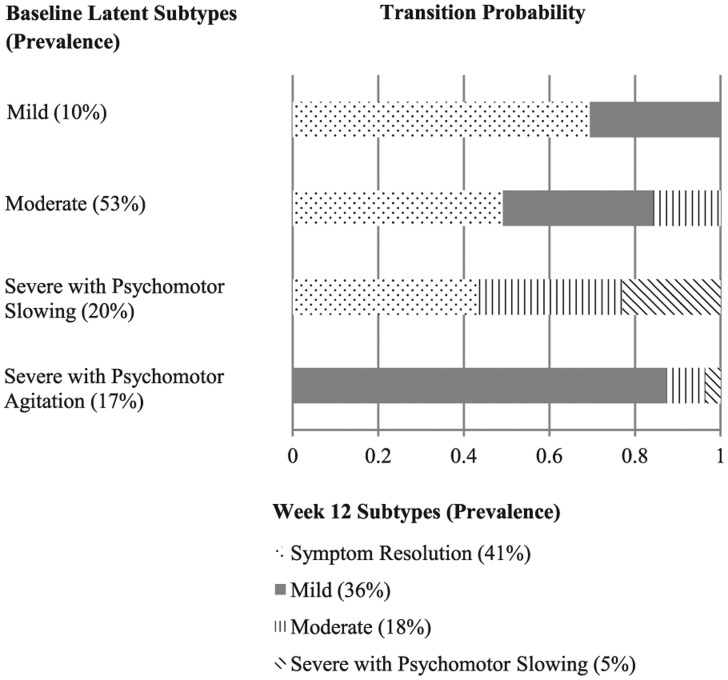
Figure 1 reports the prevalence of depression subtypes at baseline and 12 weeks and the transition probabilities derived from the LTA. At baseline, the prevalence of the Mild subtype was 10%. Fifty-three percent of men belonged to the Moderate subtype. The prevalence of the Severe with Psychomotor Slowing subtype was 20% at baseline. Seventeen percent were classified as belonging to Severe with Psychomotor Agitation. Members of the Mild subtype at baseline were the most likely to transition to the Symptom Resolution subtype, with a 69% chance of making this transition. None of those in the Severe with Psychomotor Agitation subtype transitioned to the Symptom Resolution subtype at Week 12. Men in the Severe with Psychomotor Slowing subtype were least likely to transition to a less severe subtype, with a 23% chance of remaining in the Severe with Psychomotor Slowing subtype at Week 12. Conversely, men in the Mild subtype at baseline were the least likely to move into a more severe subtype, with none transitioning to the Moderate or Severe with Psychomotor Slowing subtype. Overall, 41% of men were likely to be in the Symptom Resolution subtype at Week 12.
Figure 1.
Probabilities of transitioning in subtype membership from baseline to Week 12.
Discussion
This study explored changes in depression subtypes for men through 12 weeks of citalopram treatment using a person-centered analytic approach. Using LTA, four latent depression subtypes were identified at baseline. Depression severity and psychomotor disturbances were common distinguishing features of the subtypes. At Week 12, a Symptom Resolution subtype emerged and Severe Depression with Psychomotor Agitation was no longer identified as a subtype. The majority of men were likely to transition into subtypes characterized by fewer dominant symptoms than at baseline. Such nuances in transitions are lost when operationalizing treatment success as a summary rating scale score of meeting criteria for complete symptom remission.
The finding that severe depression subtypes were further differentiated by psychomotor symptoms agrees with previous work noting psychomotor disturbances in depression for men (Alexandrino-Silva et al., 2013; Schrijvers, Hulstijn, & Sabbe, 2008). A separate latent class analysis also identified a latent subtype distinguished by psychomotor retardation (Rodgers, Grosse Holtforth, et al., 2014). Experiencing psychomotor retardation or agitation is one of the criteria for the melancholic specifier of major depressive disorder in DSM-5 (American Psychiatric Association, 2013). Despite previous work focused on psychomotor agitation and retardation, it remains unclear if both symptoms are core features of melancholia only or are shared across subtypes (Benazzi, 2002). Furthermore, agitation is also associated with mood switching in unipolar depression (Iwanami et al., 2015) and with comorbid substance dependence (Leventhal et al., 2011), highlighting the need to determine how to improve treatment to resolve specific symptoms.
After 12 weeks of citalopram treatment, men who started in the Severe with Psychomotor Slowing subtype had the lowest chances of improving. This is consistent with previous work demonstrating that psychomotor retardation is related to greater depression severity (Calugi et al., 2011), poor response to citalopram (McGrath et al., 2008), and impairment of social functioning (K. S. Young, Parsons, Stein, & Kringelbach, 2015). Psychomotor retardation appears to involve the hypothalamic–pituitary–adrenal axis, basal ganglia, and prefrontal cortex (Frank et al., 2011). It is also associated with differential treatment response, with improvements seen in depression with psychomotor retardation when treated with fluoxetine and sertraline but not with citalopram (Buyukdura, McClintock, & Croarkin, 2011). These complex connections suggest potential areas for targeted treatment. Targeting antidepressant treatment to specific symptoms may improve the likelihood of remitting.
Identifying subtypes of depression in men may improve the understanding of variations in treatment response. Psychotherapy is widely believed to be preferred by women, possibly because of culturally reinforced gender roles that emphasize stoicism and limit men’s willingness to express emotions (Emslie, Ridge, Ziebland, & Hunt, 2006; Houle et al., 2013; Oliffe & Phillips, 2008). Some have suggested modifications to cognitive-behavioral therapy for men, yet a recent review reveals little evidence to support such changes (Spendelow, 2015). With respect to pharmacological treatments, response may vary by sex. Men in STAR*D were less likely than women to remit with citalopram (E. A. Young et al., 2009). Further study to understand which treatments may be more effective for specific depression subtypes in men is warranted.
Several limitations of this work must be considered. Because the primary goal of this analysis was to evaluate transitions in latent depression subtypes, men were required to have complete data on the baseline and 12-week visits. While it is somewhat reassuring that sociodemographic and clinical characteristics between men included in this analysis were similar to those excluded, selection bias cannot be completely ruled out. Although the inclusion criteria of STAR*D was more representative of people seeking outpatient depression treatment than most clinical trials (Wisniewski et al., 2009), it is known that men are reluctant to seek mental health treatment (Elhai, Patrick, Anderson, Simons, & Frueh, 2006; Oliver, Pearson, Coe, & Gunnell, 2005; O’Loughlin et al., 2011). Men also appear to be reluctant to participate in National Institutes of Health–funded clinical trials (The Center for Information & Study on Clinical Research Participation, 2012). Men adhering to traditional forms of masculinity may wish to remain self-reliant and might avoid seeking treatment until their depression becomes too difficult to ignore (Johnson, Oliffe, Kelly, Galdas, & Ogrodniczuk, 2012). Given this reluctance, psychomotor agitation and retardation might be overrepresented in the current study sample since psychomotor disturbances may push men to seek treatment. It is thus unclear whether it would be appropriate to generalize these findings beyond a similar group of men engaged in treatment.
Psychomotor disturbances and the other depression symptoms used as indicators of the latent depression status variable were self-reported measures. Relying on self-reported measures could lead to inaccurately estimated symptoms and response bias. Future research should incorporate objective measures of the cognitive and motor behaviors associated with psychomotor functioning. Biological factors such as neuroendocrine dysfunction and telomerase activity have also been proposed to explain sex differences in depression (Rodgers et al., 2015; Simon et al., 2015). A preliminary study of serum testosterone (T) levels has suggested that T levels may be associated with the classic DSM depression specifiers, with men with atypical depression showing lower average T levels than men with melancholic depression (Rodgers et al., 2015). While the role of such factors remains debatable, additional research which integrates patient-reported outcomes with objective and biological measures is warranted. Furthermore, while this is one of the largest samples to use LTA for changes in men’s depression subtypes, the size of this sample did prevent us from having adequate power to examine potential sociodemographic and clinical correlates of subtypes and transitions between subtypes. Future work should also investigate factors such as age, comorbidities, and functional impairment in characterizing depression subtypes.
It is possible that the QIDS-SR16 does not measure all of the symptoms that men with depression may experience. Previous research has reported that men are more likely to exhibit externalizing behaviors and that their depression symptoms can include anger and irritability, risk-taking behaviors, and substance abuse (Martin et al., 2013). These experiences are not part of the DSM criteria for major depression and are not assessed by the QIDS-SR16 or other commonly used depression assessment instruments (Möller-Leimkühler, Bottlender, Strauss, & Rutz, 2004). Given the post hoc nature of this work, it was not possible to explore aspects of theoretical models of men’s depression, for example, the masked depression or the gendered responding frameworks (Addis, 2008). Additionally, the length of participation in Level 1 of STAR*D and the timing of the assessments should also be taken into account when interpreting these results. The QIDS-SR16 captures information about the prior 1 to 2 weeks and thus might miss some changes in depression symptoms. The 12-week trial period might also not have been sufficiently long enough to identify all the transitions between subtypes that may happen with antidepressant treatment.
These limitations notwithstanding, these results are notable for numerous reasons. This is one of the first studies to examine changes in men’s depression subtypes during known treatment. While women are more likely to be diagnosed as having depression, the burden of depression in men is high and is probably underestimated. Given that men’s experiences of depression appear to differ from women’s in ways that may not be elucidated in traditional subgroup analyses, it is important to consider sex differences when studying and treating depression. This work also demonstrates the potential of LTA for characterizing discrete changes among the multiple aspects of a disease. This approach is particularly important in mental health, where pathophysiologic causes of disorders such as depression are unknown (Correll & Carbon, 2014) and where disorders are currently defined by heterogeneous symptoms which are likely not disease-specific.
Supplementary Material
Footnotes
Authors’ Note: This article presents an analysis of a preexisting data set, the National Institute of Mental Health–supported STAR*D limited access data set, version 3. This data set is available from the National Institute of Mental Health by contacting nimhdatasets@mail.nih.gov. More information is available at http://www.nimh.nih.gov/funding/clinical-trials-for-researchers/datasets/nimh-procedures-for-requesting-data-sets.shtml.
Declaration of Conflicting Interests: The author(s) declared the following conflicts of interest with respect to the research, authorship, and/or publication of this article: No competing financial interests exist for Drs. Dumenci and Ulbricht. Dr. Rothschild has received research support from St. Jude Medical, AssureRx, Alkermes, Janssen, and Takeda; has served as a consultant to AbbVie, Allergan, GlaxoSmithKline, Eli Lilly, OmniCare, Pfizer, and Sunovian; has received royalties from UpToDate, from UMass Medical School for the Rothschild Scale for Antidepressant Tachyphylaxis (RSAT)TM; and from American Psychiatric Press, Inc. for HYPERLINK “http://www.appi.org/SearchCenter/Pages/SearchDetail.aspx?ItemId=8857” Psychoneuroendocrinology: The Scientific Basis of Clinical Practice (2003), HYPERLINK “http://www.appi.org/SearchCenter/Pages/SearchDetail.aspx?ItemId=62292” Clinical Manual for Diagnosis and Treatment of Psychotic Depression (2009), HYPERLINK “http://www.appi.org/SearchCenter/Pages/SearchDetail.aspx?ItemId=62366” The Evidenced-Based Guide to Antipsychotic Medications (2010), and The Evidenced-Based Guide to Antidepressant Medications (2011). Dr. Lapane has received research support from Merck, Cubist, and the National Institutes of Health (Contract: HHSN268201000020C). She serves as a consultant to GlaxoSmithKline and Janssen.
Dr. Dumenci has received research support from the National Cancer Institute (5R01CA140151). Dr. Rothschild has received research support from the National Institute of Mental Health (5U01MH062624). Dr. Lapane has received support from the National Institute of Aging (1R21AG046839-01).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplementary material is available for this article online.
References
- Addis M. E. (2008). Gender and depression in men. Clinical Psychology: Science and Practice, 15, 153-168. [Google Scholar]
- Addis M. E., Mahalik J. R. (2003). Men, masculinity, and the contexts of help seeking. American Psychologist, 58, 5-14. [DOI] [PubMed] [Google Scholar]
- Akaike H. (1987). Factor analysis and AIC. Psychometrika, 52, 317-332. [Google Scholar]
- Alexandrino-Silva C., Wang Y.-P., Carmen Viana M., Bulhões R. S., Martins S. S., Andrade L. H. (2013). Gender differences in symptomatic profiles of depression: Results from the São Paulo Megacity Mental Health Survey. Journal of Affective Disorders, 147, 355-364. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: Author. [Google Scholar]
- Angst J., Gamma A., Gastpar M., Lépine J.-P., Mendlewicz J., Tylee A. (2002). Gender differences in depression: Epidemiological findings from the European DEPRES I and II studies. European Archives of Psychiatry and Clinical Neuroscience, 252, 201-209. [DOI] [PubMed] [Google Scholar]
- Benazzi F. (2002). Psychomotor changes in melancholic and atypical depression: Unipolar and bipolar-II subtypes. Psychiatry Research, 112, 211-220. [DOI] [PubMed] [Google Scholar]
- Buyukdura J. S., McClintock S. M., Croarkin P. E. (2011). Psychomotor retardation in depression: Biological underpinnings, measurement, and treatment. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 35, 395-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calugi S., Cassano G. B., Litta A., Rucci P., Benvenuti A., Miniati M., . . . Frank E. (2011). Does psychomotor retardation define a clinically relevant phenotype of unipolar depression? Journal of Affective Disorders, 129, 296-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Center for Information & Study on Clinical Research Participation. (2012). During participation: Proportion of study volunteers by gender in clinical research studies. Retrieved from https://www.ciscrp.org/education-center/charts-and-statistics/during-participation/
- Collins L. M., Lanza S. T. (2010). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Hoboken, NJ: John Wiley. [Google Scholar]
- Correll C. U., Carbon M. (2014). Efficacy of pharmacologic and psychotherapeutic interventions in psychiatry: To talk or to prescribe: Is that the question? JAMA Psychiatry, 71, 624-626. [DOI] [PubMed] [Google Scholar]
- Elhai J. D., Patrick S. L., Anderson S., Simons J. S., Frueh B. C. (2006). Gender- and trauma-related predictors of use of mental health treatment services among primary care patients. Psychiatric Services, 57, 1505-1509. [DOI] [PubMed] [Google Scholar]
- Emslie C., Ridge D., Ziebland S., Hunt K. (2006). Men’s accounts of depression: Reconstructing or resisting hegemonic masculinity? Social Science & Medicine, 62, 2246-2257. [DOI] [PubMed] [Google Scholar]
- Frank E., Cassano G. B., Rucci P., Thompson W. K., Kraemer H. C., Fagiolini A., . . . Forgione R. N. (2011). Predictors and moderators of time to remission of major depression with interpersonal psychotherapy and SSRI pharmacotherapy. Psychological Medicine, 41, 151-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt M. G., Stage K. B., Kragh-Soerensen P. (2003). Gender differences in severity, symptomatology and distribution of melancholia in major depression. Psychopathology, 36, 204-212. [DOI] [PubMed] [Google Scholar]
- Houle J., Villaggi B., Beaulieu M.-D., Lespérance F., Rondeau G., Lambert J. (2013). Treatment preferences in patients with first episode depression. Journal of Affective Disorders, 147, 94-100. [DOI] [PubMed] [Google Scholar]
- Iwanami T., Maeshima H., Baba H., Satomura E., Namekawa Y., Shimano T., . . . Arai H. (2015). Psychomotor agitation in major depressive disorder is a predictive factor of mood-switching. Journal of Affective Disorders, 170, 185-189. [DOI] [PubMed] [Google Scholar]
- Johnson J. L., Oliffe J. L., Kelly M. T., Galdas P., Ogrodniczuk J. S. (2012). Men’s discourses of help-seeking in the context of depression. Sociology of Health & Illness, 34, 345-361. [DOI] [PubMed] [Google Scholar]
- Kendler K. S., Gardner C. O. (2014). Sex differences in the pathways to major depression: A study of opposite-sex twin pairs. American Journal of Psychiatry, 171, 426-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers F., de Jonge P., Nolen W. A., Smit J. H., Zitman F. G., Beekman A. T. F., Penninx B. W. J. H. (2010). Identifying depressive subtypes in a large cohort study: Results from the Netherlands Study of Depression and Anxiety (NESDA). Journal of Clinical Psychiatry, 71, 1582-1589. [DOI] [PubMed] [Google Scholar]
- Lanza S. T., Collins L. M. (2008). A new SAS procedure for latent transition analysis: Transitions in dating and sexual risk behavior. Developmental Psychology, 44, 446-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S. T., Dziak J. J., Huang L., Wagner A., Collins L. M. (2015). Proc LCA & Proc LTA users’ guide (Version 1.3.2). Retrieved from https://methodology.psu.edu/
- Leventhal A. M., Gelernter J., Oslin D., Anton R. F., Farrer L. A., Kranzler H. R. (2011). Agitated depression in substance dependence. Drug and Alcohol Dependence, 116, 163-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus S. M., Kerber K. B., Rush A. J., Wisniewski S. R., Nierenberg A., Balasubramani G. K., . . . Trivedi M. H. (2008). Sex differences in depression symptoms in treatment-seeking adults: Confirmatory analyses from the Sequenced Treatment Alternatives to Relieve Depression study. Comprehensive Psychiatry, 49, 238-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin L. A., Neighbors H. W., Griffith D. M. (2013). The experience of symptoms of depression in men vs women: Analysis of the National Comorbidity Survey Replication. JAMA Psychiatry, 70, 1100-1106. [DOI] [PubMed] [Google Scholar]
- McGrath P. J., Khan A. Y., Trivedi M. H., Stewart J. W., Morris D. W., Wisniewski S. R., . . . Rush A. J. (2008). Response to a selective serotonin reuptake inhibitor (citalopram) in major depressive disorder with melancholic features: A STAR*D report. Journal of Clinical Psychiatry, 69, 1847-1855. [DOI] [PubMed] [Google Scholar]
- Möller-Leimkühler A. M., Bottlender R., Strauss A., Rutz W. (2004). Is there evidence for a male depressive syndrome in inpatients with major depression? Journal of Affective Disorders, 80, 87-93. [DOI] [PubMed] [Google Scholar]
- National Center for Injury Prevention and Control. (2013). Fatal injury reports, national and regional, 1999-2013. Retrieved from http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html
- Nierenberg A. A., Husain M. M., Trivedi M. H., Fava M., Warden D., Wisniewski S. R., . . . Rush A. J. (2010). Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: A STAR*D report. Psychological Medicine, 40, 41-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the U.S. Surgeon General and National Action Alliance for Suicide Prevention. (2012). 2012 National strategy for suicide prevention: Goals and objectives for action. Washington, DC: Author. [Google Scholar]
- Ogrodniczuk J. S., Oliffe J. L. (2011). Men and depression. Canadian Family Physician/Médecin de Famille Canadien, 57, 153-155. [PMC free article] [PubMed] [Google Scholar]
- Oliffe J. L., Phillips M. J. (2008). Men, depression and masculinities: A review and recommendations. Journal of Men’s Health, 5, 194-202. [Google Scholar]
- Oliver M. I., Pearson N., Coe N., Gunnell D. (2005). Help-seeking behaviour in men and women with common mental health problems: Cross-sectional study. British Journal of Psychiatry, 186, 297-301. [DOI] [PubMed] [Google Scholar]
- O’Loughlin R. E., Duberstein P. R., Veazie P. J., Bell R. A., Rochlen A. B., Fernandez y, Garcia E., Kravitz R. L. (2011). Role of the gender-linked norm of toughness in the decision to engage in treatment for depression. Psychiatric Services, 62, 740-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers S., Ajdacic-Gross V., Müller M., Hengartner M. P., Grosse Holtforth M., Angst J., Rössler W. (2014). The role of sex on stability and change of depression symptom subtypes over 20 years: A latent transition analysis. European Archives of Psychiatry and Clinical Neuroscience, 264, 577-588. [DOI] [PubMed] [Google Scholar]
- Rodgers S., Grosse Holtforth M., Hengartner M. P., Müller M., Aleksandrowicz A. A., Rössler W., Ajdacic-Gross V. (2015). Serum testosterone levels and symptom-based depression subtypes in men. Frontiers in Psychiatry, 6, 61. doi: 10.3389/fpsyt.2015.00061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers S., Grosse Holtforth M., Müller M., Hengartner M. P., Rössler W., Ajdacic-Gross V. (2014). Symptom-based subtypes of depression and their psychosocial correlates: A person-centered approach focusing on the influence of sex. Journal of Affective Disorders, 156, 92-103. [DOI] [PubMed] [Google Scholar]
- Rush A. J., Fava M., Wisniewski S. R., Lavori P. W., Trivedi M. H., Sackeim H. A., . . . Niederehe G. (2004). Sequenced treatment alternatives to relieve depression (STAR*D): Rationale and design. Controlled Clinical Trials, 25, 119-142. [DOI] [PubMed] [Google Scholar]
- Rush A. J., Trivedi M. H., Ibrahim H. M., Carmody T. J., Arnow B., Klein D. N., . . . Keller M. B. (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54, 573-583. [DOI] [PubMed] [Google Scholar]
- Schrijvers D., Hulstijn W., Sabbe B. G. C. (2008). Psychomotor symptoms in depression: A diagnostic, pathophysiological and therapeutic tool. Journal of Affective Disorders, 109, 1-20. [DOI] [PubMed] [Google Scholar]
- Schuch J. J. J., Roest A. M., Nolen W. A., Penninx B. W. J. H., de Jonge P. (2014). Gender differences in major depressive disorder: Results from the Netherlands study of depression and anxiety. Journal of Affective Disorders, 156, 156-163. [DOI] [PubMed] [Google Scholar]
- Schwarz G. E. (1978). Estimating the dimension of a model. Annals of Statistics, 6, 461-464. [Google Scholar]
- Silverstein B. (2002). Gender differences in the prevalence of somatic versus pure depression: A replication. American Journal of Psychiatry, 159, 1051-1052. [DOI] [PubMed] [Google Scholar]
- Simon N. M., Walton Z. E., Bui E., Prescott J., Hoge E., Keshaviah A., . . . Wong K. K. (2015). Telomere length and telomerase in a well-characterized sample of individuals with major depressive disorder compared to controls. Psychoneuroendocrinology, 58, 9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spendelow J. S. (2015). Cognitive-behavioral treatment of depression in men: Tailoring treatment and directions for future research. American Journal of Men’s Health, 9, 94-102. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2013). Results from the 2012 National Survey on Drug Use and Health: Mental Health findings. Retrieved from http://www.samhsa.gov/data/NSDUH/2k12MH_FindingsandDetTables/2K12MHF/NSDUHmhfr2012.htm
- Trivedi M. H., Rush A. J., Wisniewski S. R., Nierenberg A. A., Warden D., Ritz L., . . . Fava M. (2006). Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice. American Journal of Psychiatry, 163, 28-40. [DOI] [PubMed] [Google Scholar]
- Wisniewski S. R., Rush A. J., Nierenberg A. A., Gaynes B. N., Warden D., Luther J. F., . . . Trivedi M. H. (2009). Can phase III trial results of antidepressant medications be generalized to clinical practice? A STAR*D report. American Journal of Psychiatry, 166, 599-607. [DOI] [PubMed] [Google Scholar]
- Young E. A., Kornstein S. G., Marcus S. M., Harvey A. T., Warden D., Wisniewski S. R., . . . Rush A. J. (2009). Sex differences in response to citalopram: A STAR*D report. Journal of Psychiatric Research, 43, 503-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young K. S., Parsons C. E., Stein A., Kringelbach M. L. (2015). Motion and emotion: Depression reduces psychomotor performance and alters affective movements in caregiving interactions. Frontiers in Behavioral Neuroscience, 9, 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.