Abstract
Introduction
The U.S. spends more than any other country on health care, yet Americans have lower life expectancy than most industrialized countries. Recent studies suggest that lower expenditures on social policies in the U.S. may contribute to less favorable trends in life expectancy. This study tests the hypothesis that greater social spending will be positively associated with life expectancy across the countries of the Organisation of Economic Co-operation and Development and that the magnitude of these associations will outweigh those between government healthcare spending and life expectancy.
Methods
In 2016, longitudinal data on six domains of social expenditures for the U.S. and 19 other wealthy nations between 1980 and 2010 were used to estimate the associations between prior year expenditures on education, family, unemployment, incapacity, old age and active labor market programs, and period life expectancy using fixed effects models.
Results
Controlling for a wide set of confounders and government healthcare expenditures, a 1% increase in prior year education expenditures was associated with 0.160 (95% CI=0.033, 0.286) of a year gain in life expectancy, whereas a 1% increase in prior year incapacity benefit expenditures was associated with 0.168 (95% CI=0.003, 0.333) of a year gain in life expectancy. Counterfactual models suggest that if the U.S. were to increase expenditures on education and incapacity to the levels of the country with the maximum expenditures, life expectancy would increase to 80.12 years.
Conclusions
The U.S. life expectancy lag may be considerably smaller if U.S. expenditures on education and incapacity programs were comparable with those in other high-income countries.
INTRODUCTION
The U.S. spends more than any other country on health care, yet Americans have worse health and lower life expectancy than most industrialized countries. In 2016, the U.S. ranked 42nd in global life expectancy, below most other industrialized nations. Proposed explanations include differences in health care, behavior, and the built environment, all of which appear to play some role but do not fully explain the U.S. health disadvantage.1 Recently, focus has shifted towards the potential role of social policy, with reports suggesting that lower social expenditures in the U.S. relative to peer nations may contribute to less favorable life expectancy trends. As yet, however, few studies have examined whether higher social expenditures lead to life expectancy gains.
Emerging research from within the U.S. provides evidence that social expenditures may bring benefits to health. In a recent study, a higher ratio of state social welfare spending relative to healthcare spending was associated with significant improvements in a variety of health outcomes.2,3 Cross-national evidence suggests that several social programs may have positive associations with health including parental leave, child allowances and subsidized child care,4–6 unemployment benefits, and education.7–10 Experimental evidence from the U.S. also suggests that social programs, such as intensive early childhood interventions,11 might bring some benefits to health, whereas other social investments such as welfare reform,12 housing relocation,13 and small class sizes14 had both positive and negative health effects. Interestingly, experimental evidence from the Oregon Health Study shows that randomized assignment to Medicaid among uninsured Americans led to no significant improvement in physical health.15
There are at least three potential mechanisms through which social expenditures may lead to better population health. First, higher social spending may insure individuals against poverty, which may in turn translate into better health outcomes and lower risk of death. Second, social spending may promote human capital investment by increasing access to early childhood programs, education, and training, which may translate into better health in the long run. Third, social spending may provide reliable safeguards that reduce chronic stress pathways linked to hypothalamic–pituitary–adrenal axis dysregulation and subsequent metabolic, cardiovascular, and inflammatory changes.
This study uses data from the U.S. and 19 other wealthy nations to examine whether greater social spending is associated with larger gains in life expectancy. Associations with health are examined across six domains of social spending, accounting for confounding with government healthcare spending. The contribution to life expectancy gains of spending on social welfare relative to spending on health care is also evaluated. The central hypothesis of the study is that greater social spending will be positively associated with life expectancy across the countries of the Organisation of Economic Co-operation and Development (OECD) and that the magnitude of these associations will outweigh those between government healthcare spending and life expectancy.
METHODS
Study Sample
Data were drawn from the OECD Social Expenditure Database, which provides yearly data on social spending as a percentage of gross domestic product (GDP) spanning 1980 to 2010 for 20 countries: Austria, Belgium, Canada, Denmark, Finland, France, Germany, Greece, Ireland, Italy, Japan, Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, Switzerland, United Kingdom, and the U.S. Data on Australia and Luxembourg were also available, but were excluded from the analysis as they did not cover all years and variables required for the analysis.
Measures
Data are provided for six domains which represent the largest social expenditures across nations and include both cash and in-kind public spending: education, family, unemployment, incapacity, old age, and active labor market programs (ALMP). Education is the sum of public spending on all levels from pre-primary to tertiary education. Family consists of primarily child allowances and credits, childcare support, income support during leave, and sole parent payments. Unemployment includes unemployment benefit compensation and early retirement programs. Incapacity covers care services, disability benefits, benefits accruing from occupational injury and accident legislation, employee sickness payments, and home-help and residential services for the working aged. Old age largely comprises spending on early retirement pensions and home-help and residential services for the elderly. ALMP includes expenditures on employment services, training, employment incentives, integration of the disabled, direct job creation, and start-up incentives.
Data were drawn from the OECD Health database, which provides internationally harmonized data on period life expectancy derived from the WHO Mortality database. Period life expectancy measures the average number of years that a person can be expected to live from birth, assuming that age-specific mortality levels remain constant.
All models included a linear time trend centered around the first year of observation, GDP per capita in millions of U.S. dollars adjusted for inflation (base year 2010), unemployment rates measured as the percentage of unemployed out of the total labor force, income inequality measured using the Gini coefficient, and variables for the percentage of the population age <15 (reference), 15–64, and ≥65 years.
Statistical Analysis
A fixed effects design was employed to address confounding by unmeasured differences between countries that are stable over time but might also be correlated with life expectancy.16–18 Fixed effects models compare differences in life expectancy across years within countries, exploiting only within-country variation in social expenditures for estimation. The basic model specification was as follows:
| (1) |
where yit is a measure of life expectancy for country i at time t, β0 is the intercept, Xitβ is a country-level measure of social expenditures and other covariates for country i at time t, υi is the unobserved time-invariant characteristics of each country, and εit is the residual for a country in a given year.
A test for serial correlation between successive time points was conducted using Stata’s xtserial command.19 The null hypothesis of no first-order autocorrelation was rejected at a significance level of 0.07. Therefore, models were fit specifying a first-order autoregressive process. Specifying a first-order autoregessive process models the error term in equation (1) as ρεi,t−1+ ηit., where the absolute value of ρ (rho, the autocorrelation coefficient) is <1 and ηit is independent and identically distributed with mean 0 and variance σ2η. To account for potential delays in the effect of a given expenditure, models were fit including contemporaneous, 1- and 2-year lags of social expenditures. These analyses show the largest effect sizes at t−1, pointing to a 1-year lag as the preferred temporal specification of the relationship between social spending and life expectancy. All SEs were clustered at the country level. Two-tailed tests with an α of 0.05 were used throughout. Analysis was conducted in Stata, version 13 and included use of the margins command suite.
RESULTS
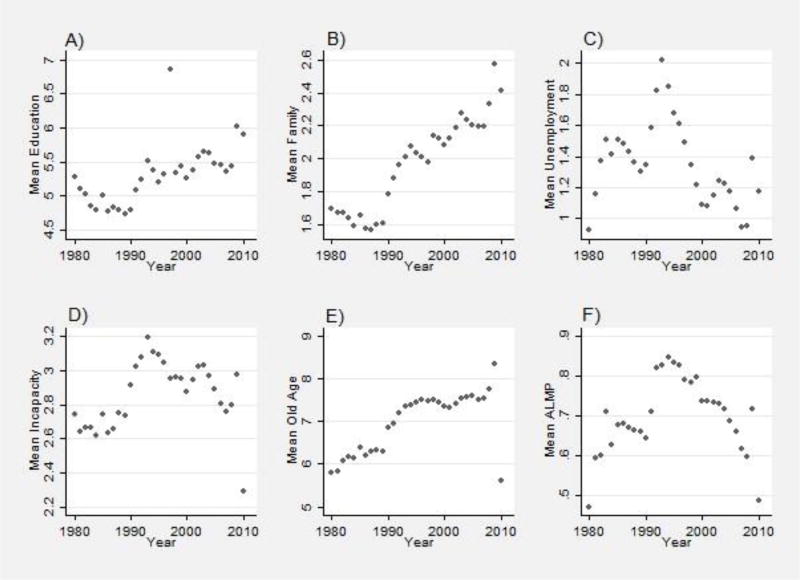
Figure 1 shows time trends in the six domains of social expenditure. There has been considerable temporal variation. Expenditures on education, family, and incapacity showed declines from 1980 to 1990, while old age, ALMP, and unemployment expenditures increased during this period. From 1990 to 2000, spending in all domains increased. Although spending in education, family, and old-age benefits continued to increase from 2000 to 2010, spending in unemployment, incapacity, and ALMP declined over the same period.
Figure 1.
Pooled sample mean of social expenditures as a percentage of GDP by year, OECD countries, 1980–2010.
GDP, gross domestic product; OECD, Organisation of Economic Co-operation and Development
Table 1 shows that within countries there have been substantial changes in expenditures in each domain. For example, expenditures on education were as low as 3.5% for New Zealand in 1986 in contrast to 7.2% in 2010. In the UK, family expenditures were 1.9% of GDP in 1990 compared with 3.9% in 2009, the year with the highest family expenditure. Expenditures varied considerably between countries as well (Appendix Figure 1). For example, maximum expenditures on family benefits was 0.8% of GDP in the U.S. in 2002 compared with 4.85% in 1992 in Sweden. It is worth noting that the U.S. had the lowest average expenditures across all domains, while Sweden had the highest (not shown).
Table 1.
Country-specific Minimum and Maximum Social Expenditures as a Percentage of GDP Between 1980 and 2010
| Country | Education | Family | Unemployment | Incapacity | Old age | ALMP | N(Years) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Min | Max | Min | Max | Min | Max | Min | Max | Min | Max | Min | Max | ||
| Austria | 5.01 | 6.25 | 2.54 | 3.34 | 0.40 | 1.29 | 3.15 | 4.13 | 8.93 | 11.96 | 0.26 | 0.85 | 30 |
| Belgium | 3.03 | 6.57 | 2.21 | 3.05 | 2.42 | 3.69 | 2.27 | 3.78 | 5.93 | 8.10 | 1.02 | 1.41 | 30 |
| Canada | 4.77 | 7.88 | 0.50 | 1.13 | 0.57 | 2.35 | 0.85 | 1.38 | 2.90 | 4.37 | 0.27 | 0.65 | 31 |
| Denmark | 5.70 | 8.74 | 2.57 | 3.90 | 1.73 | 5.27 | 3.15 | 5.16 | 6.67 | 8.44 | 0.71 | 1.91 | 30 |
| Finland | 4.77 | 7.65 | 1.85 | 4.42 | 0.65 | 4.74 | 3.33 | 5.55 | 5.12 | 10.20 | 0.73 | 1.63 | 31 |
| France | 4.38 | 5.90 | 2.33 | 3.31 | 0.00 | 2.32 | 1.84 | 2.90 | 7.64 | 12.33 | 0.60 | 1.24 | 30 |
| Germany | 4.43 | 5.06 | 1.55 | 2.32 | 0.50 | 1.89 | 3.06 | 4.18 | 6.83 | 10.24 | 0.51 | 1.48 | 31 |
| Greece | 1.77 | 4.09 | 0.18 | 1.43 | 0.22 | 0.72 | 0.83 | 1.83 | 4.63 | 11.10 | 0.06 | 0.40 | 30 |
| Ireland | 4.22 | 6.50 | 1.07 | 4.35 | 0.70 | 3.33 | 1.28 | 2.64 | 2.56 | 4.88 | 0.62 | 1.33 | 31 |
| Italy | 3.95 | 4.96 | 0.58 | 1.64 | 0.37 | 1.36 | 1.94 | 2.59 | 8.01 | 14.17 | 0.23 | 0.70 | 31 |
| Japan | 3.43 | 5.67 | 0.36 | 0.96 | 0.31 | 0.72 | 0.75 | 1.15 | 3.11 | 10.93 | 0.16 | 0.43 | 31 |
| Netherlands | 4.84 | 6.37 | 1.24 | 2.50 | 1.04 | 3.85 | 3.54 | 6.97 | 5.17 | 6.34 | 0.55 | 1.55 | 31 |
| New Zealand | 3.50 | 7.24 | 1.91 | 3.55 | 0.23 | 1.89 | 1.28 | 3.10 | 4.13 | 7.69 | 0.26 | 0.88 | 31 |
| Norway | 5.35 | 7.99 | 1.80 | 3.63 | 0.19 | 1.41 | 3.63 | 7.03 | 5.09 | 8.04 | 0.34 | 1.31 | 31 |
| Portugal | 3.09 | 5.79 | 0.59 | 1.51 | 0.17 | 1.37 | 2.15 | 3.01 | 3.04 | 10.65 | 0.16 | 0.77 | 30 |
| Spain | 3.22 | 5.01 | 0.15 | 1.52 | 1.68 | 4.69 | 2.28 | 2.74 | 4.59 | 8.45 | 0.18 | 0.86 | 31 |
| Sweden | 5.56 | 7.51 | 2.95 | 4.85 | 0.37 | 2.71 | 4.39 | 6.37 | 7.70 | 10.71 | 0.97 | 2.82 | 31 |
| Switzerland | 4.51 | 5.83 | 0.93 | 1.46 | 0.07 | 1.43 | 2.30 | 4.53 | 6.70 | 12.09 | 0.19 | 0.81 | 30 |
| United Kingdom | 4.37 | 5.60 | 1.92 | 3.88 | 0.39 | 2.10 | 1.26 | 3.07 | 3.96 | 7.43 | 0.22 | 0.83 | 30 |
| U.S. | 4.76 | 5.77 | 0.42 | 0.78 | 0.23 | 1.12 | 1.24 | 1.73 | 5.00 | 6.12 | 0.11 | 0.27 | 31 |
| Pooled N | 1.77 | 8.73 | .154 | 4.85 | 0.07 | 5.27 | 0.75 | 7.03 | 2.56 | 14.17 | 0.06 | 2.82 | 31 |
OECD, Organisation of Economic Co-operation and Development; ALMP, active labor market programs; Pooled N, average across full sample of country-years; GDP, gross domestic product
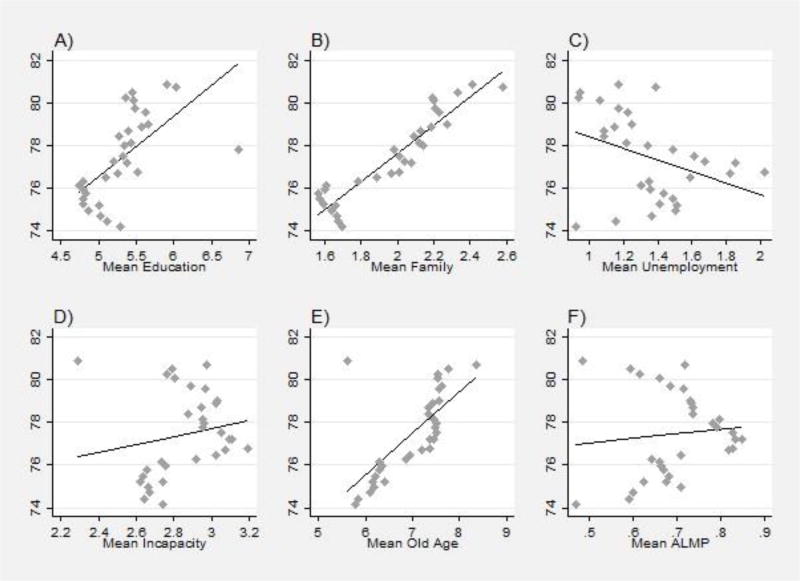
Figure 2 plots life expectancy against social expenditures as percentage of GDP, superimposing a local linear smoother upon the data points. With the exception of unemployment, the bivariate relationship between social spending and life expectancy is positive.
Figure 2.
Life expectancy by social expenditures as a percentage of GDP with local linear smooth, OECD countries, 1980–2010.
GDP, gross domestic product; OECD, Organisation of Economic Co-operation and Development
Table 2 provides estimates from fixed effects models with each domain listed separately. The purpose of this table is to test the hypothesis that greater social spending will be positively associated with life expectancy and that the magnitude of observed associations will outweigh those between government healthcare spending and life expectancy. Greater expenditures in the previous year on education (Model 1: b=0.177, 95% CI=0.060, 0.294, p<0.001) and incapacity (Model 1: b=0.292, 95% CI=0.154, 0.429, p<0.001) were associated with significant gains in life expectancy. Results in Model 2, show that estimates of lagged education and incapacity expenditures remained significant in models that simultaneously controlled for all domains of social expenditures (b=0.165, 95% CI=0.045, 0.286, p<0.01, and b=0.172, 95% CI=0.010, 0.334, p<0.05, respectively). Estimates in Model 3 show that these results were also robust to additional controls for government healthcare expenditures (b=0.160, 95% CI=0.033, 0.286, p<0.05, and b=0.168, 95% CI=0.003, 0.333, p<0.05, respectively).
Table 2.
Fixed Effects Models of Life Expectancy on Lagged Social Expenditures as a Percentage of GDP and Relevant Controls, OECD Countries, 1980–2010
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Separate | Simultaneous | Simultaneous with healthcare expenditures |
||||
|
|
||||||
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Education | 0.177 | 0.060, 0.294 | 0.165 | 0.045, 0.286 | 0.160 | 0.033, 0.286 |
| Family | 0.120 | −0.074, 0.314 | −0.041 | −0.296, 0.214 | −0.048 | −0.308, 0.211 |
| Unemployment | 0.082 | −0.064–0.228 | 0.054 | −0.132, 0.241 | 0.053 | −0.134, 0.240 |
| Incapacity | 0.292 | 0.154, 0.429 | 0.172 | 0.010, 0.334 | 0.168 | 0.003, 0.333 |
| Old age | −0.015 | −0.106, 0.076 | −0.090 | −0.204, 0.024 | −0.095 | −0.213, 0.024 |
| ALMP | 0.198 | −0.050, 0.447 | 0.127 | −0.187, 0.440 | 0.132 | −0.184, 0.448 |
| Country-years | 252 | 327 | 328 | |||
| Countries | 20 | 20 | 20 | |||
Notes: Estimate unit is years of life expectancy. Model 1 includes predictor variables separately and full set of controls (Gini, GDP per capita, unemployment rate, population age distribution, and continuous year). Model 2 includes predictor variables simultaneously and full set of controls. Model 3 includes predictor variables simultaneously, full set of controls, and government healthcare expenditures.
OECD, Organisation of Economic Co-operation and Development; ALMP, active labor market programs; GDP, gross domestic product
To contextualize these findings, the parameter estimates for prior year education and incapacity expenditures are applied to the U.S. case with an observed value of 78.5 in 2009. If the U.S. were to increase education spending from 5.4% of GDP to 8.7% of GDP (the pooled sample maximum), life expectancy would increase 0.53 years. Increasing incapacity spending from 1.71% of GDP to 7.0% of GDP (the pooled sample maximum) would result in an increase of 0.89 years in life expectancy. In total, these increases in education and incapacity benefits would increase U.S. life expectancy to 80.12 years. Again, the specification of these models presumes such expenditures occur the year prior to observation of the outcome.
Given its relatively low rates of social spending and life expectancy, models were replicated excluding the U.S. The sensitivity of results to the exclusion of Southern European nations, which differ from Northern European nations in terms of economic performance and history of development, were also tested. Appendix Table 1 (Columns 1 and 2) shows the results of these sensitivity analyses. Overall, this table shows that coefficients were nearly identical as for the total sample. Results were also robust in models that did not include government-mandated private expenditures (Column 3) and that incorporated total fertility rate, net migration, and population size as additional demographic controls (Column 4).
DISCUSSION
Life expectancy is a key indicator of population health and human development. Results from this study show that investments in education and incapacity programs contribute to gains in life expectancy and may contribute to the smaller gains in life expectancy observed in the U.S. relative to other wealthy nations. These findings suggest that social policies may be important determinants of health and life expectancy and may offer an important pathway to improving population health.
In this study, the associations between population health and prior year spending on education and incapacity were stronger than between population health and spending on health care. Although positive, the association with government healthcare spending was small in magnitude and not statistically significant in models that controlled for all domains. These findings support the conclusions of Bradley et al.2,3 that spending on social policy may be more effective at improving health than spending targeted strictly to health. This finding might be because of the fact that the impact of investments in areas of health care known to be effective, such as hypertension or cholesterol control, is overshadowed by increasing costs in medical technologies or drugs that may be less effective. For example, evidence suggests that faster uptake of new and more expensive prescription drugs is an important contributor to higher per capita spending in the U.S. relative to other OECD countries that employ stricter health technology assessments requiring clear evidence of the value of new drugs.21 Although widely publicized, the proposition that costly medical technologies ultimately increase U.S. longevity has been challenged by findings suggesting that the beneficial effects observed in RCTs are not found when implemented outside of the laboratory environment. For a comprehensive treatment of the limitations of, and effective companions and alternatives to, RCT-based evidence see the National Academy of Medicine’s 2008 report which addressed this and related issues.20
Findings for education are in line with a wealth of evidence suggesting that more schooling and higher educational attainment is associated with better health. Education is crucial to labor market success,22–27 and may promote healthier behavioral choices28 and increase access to social networks, power and prestige, health care, and other mechanisms conducive to better health.29 Studies of the Perry School Program in Michigan and The Abecedarian program in North Carolina show consistent benefits of intensive early education programs on educational, labor market, and cognitive outcomes, all of which predict better health later in life.30,31 Studies have also shown that compulsory education laws led to reductions in mortality and improvements in health,11,32 although evidence is contradictory for some countries, such as Britain and France.33,34 Overall, these results are in line with the hypothesis that larger investments in education may lead to gains in life expectancy. Increased spending in education may also signal investments to improve the quality of education,29 although there is limited evidence on whether these improvements translate into health benefits.
Results for incapacity benefits are difficult to interpret. One possibility is that incapacity spending addresses the social and economic consequences of poor health and disability, which may revert back into benefits to life expectancy. For example, financial resources may help incapacitated individuals to effectively manage illness, above and beyond the diagnoses and treatments covered under healthcare spending. This could explain why similar associations were not observed with unemployment or old-age benefits, which, although also a form of income replacement, are not targeted at the already ill and disabled. Even if some specific components of family, unemployment, old-age pensions, and ALMP may lead to health gains, the current mix of funding allocation across these programs may not translate into gains in life expectancy.
Limitations
This study has several strengths, but some limitations should be considered. First, life expectancy is driven heavily by infant mortality and there are cross-national differences in the reporting of such deaths that could introduce measurement error. Although this may be the case, alternative measures such as survival are likely to disproportionately reflect the impact of health care rather than the broad-based impacts of social expenditures that serve as the focus of this investigation. Moreover, because these models include country fixed effects, they do not compare infant mortality between countries, but rather examine variation over time within countries alone. Together, these factors minimize potential measurement-related biases.
Second, this analysis investigates the short-term associations between social policy and life expectancy. Preliminary analyses suggest a 1-year delay in the effect of expenditures on longevity. That said, life expectancy reflects a series of health advantages and insults that accumulate over multiple points in the life course. The association between spending and life expectancy the following year will not accurately capture the full and long-term associations with health and mortality of social investments over a lifetime. In particular, investments early in life might lead to long-run benefits for health that only materialize decades later. Future studies should explore this question using individual-level data linked to aggregate expenditures throughout the life course.
Finally, although time trends and a variety of confounders were included, social expenditure variation may also partly reflect unaccounted for demand-side changes. Trends in social expenditures similarly reflect a complex pattern of supplyside factors related to the adjustment of eligibility and coverage restrictions. For example, mid-1990s welfare reform in the U.S. led to a shift of Americans from welfare rolls to Supplementary Security Income. Likewise, in many other OECD countries, pension reforms have affected old-age expenditures just as benefits and duration caps affected unemployment expenditures. This study does not capture the myriad impacts of these types of reforms; however, it does provide a sense of how overall changes in social expenditure arising from these policy changes relate to life expectancy and helps to set the agenda for future research on the subject. Another limitation is that these estimates do not capture changes in the quality of predictors or outcomes. In other words, little can be gleaned from these data about the caliber of education or life satisfaction during years-of-life gained. Lastly, research on poverty and inequality suggests that more universal social expenditures have stronger outcome-improvement effects than targeted benefits.38,39 The present analysis, though, does not tell whether the magnitude of the observed effects are larger (or smaller) as spending levels increase.
Notwithstanding the limitations, these results have important implications for policy. Life expectancy gains in the U.S. have slowed significantly in recent decades, even though other wealthy nations have continued to enjoy significantly larger gains. This has left the U.S. farther and farther down the rankings relative to peer nations.1,36 The fact that increased education and incapacity spending are favorably associated with life expectancy gains suggests that the comparatively low spending levels in these areas may have contributed to this large and growing lag in U.S. life expectancy.
CONCLUSIONS
This study advances knowledge on the relevance of health policy vis-a-vis other policy domains. Empirical work has paid considerable attention to the relationship between population health and healthcare policy.3,37–42 This is understandable given the intuitive link between health care and health. Yet, these findings support prior evidence that health care explains only a fraction of gains in life expectancy.43,44 Furthermore, the position of the U.S. in international life expectancy rankings does not seem to have benefited from increasingly higher overall spending on health care.1,36 These results suggest that the disproportionate focus on healthcare policy could shift attention away from other policies outside health care that may improve health and reduce mortality in the U.S. and that conceiving social policy as health policy may constitute a promising approach to improving population health.
Supplementary Material
Acknowledgments
Dr. Avendano was supported by the National Institute on Aging (award number R01AG040248), and the European Union’s Horizon2020 research and innovation program under grant agreements 633666 (Lifepath) and 667661 (MINDMAP). Dr. Reynolds received no grant support for the study. The funding agencies did not participate in the design or conduct of the study; in the collection, analysis, or interpretation of the data; in the preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Avendano M, Kawachi I. Why Do Americans Have Shorter Life Expectancy and Worse Health Than Do People in Other High-Income Countries? Annu Rev Public Health. 2014;35:307–325. doi: 10.1146/annurev-publhealth-032013-182411. https://doi.org/10.1146/annurev-publhealth-032013-182411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradley EH, Canavan M, Rogan E, et al. Variation In Health Outcomes: The Role Of Spending On Social Services, Public Health and Health Care, 2000–2009. Health Aff (Millwood) 2016;35(5):760–768. doi: 10.1377/hlthaff.2015.0814. https://doi.org/10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- 3.Bradley EH, Elkins BR, Herrin J, Elbel B. Health and social services expenditures: associations with health outcomes. BMJ Qual Saf. 2011;20(10):826–831. doi: 10.1136/bmjqs.2010.048363. https://doi.org/10.1136/bmjqs.2010.048363. [DOI] [PubMed] [Google Scholar]
- 4.Burstrom B, Whitehead M, Clayton S, Fritzell S, Vannoni F, Costa G. Health inequalities between lone and couple mothers and policy under different welfare regimes - the example of Italy, Sweden and Britain. Soc Sci Med. 2010;70(6):912–920. doi: 10.1016/j.socscimed.2009.11.014. https://doi.org/10.1016/j.socscimed.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Heymann J, Raub A, Earle A. Creating and Using New Data Sources to Analyze the Relationship Between Social Policy and Global Health: The Case of Maternal Leave. Public Health Rep. 2011;126(3):127–134. doi: 10.1177/00333549111260S317. https://doi.org/10.1177/00333549111260S317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lundberg O, Yngwe MÅ, Stjärne MK, et al. The role of welfare state principles and generosity in social policy programmes for public health: an international comparative study. Lancet. 2008;372(9650):1633–1640. doi: 10.1016/S0140-6736(08)61686-4. https://doi.org/10.1016/S0140-6736(08)61686-4. [DOI] [PubMed] [Google Scholar]
- 7.Cylus J, Glymour MM, Avendano M. Health Effects of Unemployment Benefit Program Generosity. Am J Public Health. 2015;105(2):317–323. doi: 10.2105/AJPH.2014.302253. https://doi.org/10.2105/AJPH.2014.302253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cylus J, Glymour MM, Avendano M. Do generous unemployment benefit programs reduce suicide rates? A state fixed-effect analysis covering 1968–2008. Am J Epidemiol. 2014;180(1):45–52. doi: 10.1093/aje/kwu106. https://doi.org/10.1093/aje/kwu106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grytten JSI, Sørensen RJ. Educated mothers, healthy infants. The impact of a school reform on the birth weight of Norwegian infants 1967–2005. Soc Sci Med. 2014;105:84–92. doi: 10.1016/j.socscimed.2014.01.008. https://doi.org/10.1016/j.socscimed.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Kim AS, Jennings ET. Effects of U.S. States’ Social Welfare Systems on Population Health. Policy Stud J. 2009;37(4):745–767. https://doi.org/10.1111/j.1541-0072.2009.00333.x. [Google Scholar]
- 11.Muennig P. Can universal pre-kindergarten programs improve population health and longevity? Mechanisms, evidence, and policy implications. Soc Sci Med. 2015;127:116–123. doi: 10.1016/j.socscimed.2014.08.033. https://doi.org/10.1016/j.socscimed.2014.08.033. [DOI] [PubMed] [Google Scholar]
- 12.Wilde ET, Rosen Z, Couch K, Muennig PA. Impact of welfare reform on mortality: an evaluation of the Connecticut jobs first program, a randomized controlled trial. Am J Public Health. 2014;104(3):534–538. doi: 10.2105/AJPH.2012.301072. https://doi.org/10.2105/AJPH.2012.301072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessler RC, Duncan GJ, Gennetian LA, et al. Associations of housing mobility interventions for children in high-poverty neighborhoods with subsequent mental disorders during adolescence. JAMA. 2014;311(9):937–948. doi: 10.1001/jama.2014.607. https://doi.org/10.1001/jama.2014.607. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Muennig P, Johnson G, Wilde ET. The effect of small class sizes on mortality through age 29 years: evidence from a multicenter randomized controlled trial. Am J Epidemiol. 2011;173(12):1468–1474. doi: 10.1093/aje/kwr011. https://doi.org/10.1093/aje/kwr011. [DOI] [PubMed] [Google Scholar]
- 15.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. https://doi.org/10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gangl M. Causal Inference in Sociological Research. Annu Rev Sociol. 2010;36:21–47. https://doi.org/10.1146/annurev.soc.012809.102702. [Google Scholar]
- 17.Halaby CN. Panel models in sociological research: Theory into practice. Annu Rev Sociol. 2004;30:507–544. https://doi.org/10.1146/annurev.soc.30.012703.110629. [Google Scholar]
- 18.Winship C, Morgan SL. The estimation of causal effects from observational data. Ann Rev Sociol. 1999;25:659–706. https://doi.org/10.1146/annurev.soc.25.1.659. [Google Scholar]
- 19.Drukker DM. Testing for serial correlation in linear panel-data models. Stata J. 2003;3(2):168–177. [Google Scholar]
- 20.National Academy of Medicine. Evidence-based medicine and the changing nature of health care: 2007 IOM annual meeting summary. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 21.Kanavos P, Ferrario A, Vandoros S, Anderson GF. Higher U.S. branded drug prices and spending compared to other countries may stem partly from quick uptake of new drugs. Health Aff (Millwood) 2013;32(4):753–761. doi: 10.1377/hlthaff.2012.0920. https://doi.org/10.1377/hlthaff.2012.0920. [DOI] [PubMed] [Google Scholar]
- 22.Becker GS. Human Capital: A Theoretical and Empirical Analysis, with Special Reference to Education. New York, NY: Columbia University Press; 1967. [Google Scholar]
- 23.Mincer J. Schooling, Experience, and Earnings. New York, NY: Columbia University Press; 1974. [Google Scholar]
- 24.Ashenfelter OaAK. Estimating the Returns to Schooling Using a New Sample of Twins. Am Econ Rev. 1994;84:1157–1173. [Google Scholar]
- 25.Allmindinger J. Educational Systems and Labor Market Outcomes. Eur Sociol Rev. 1989;5(3):231–250. https://doi.org/10.1093/oxfordjournals.esr.a036524. [Google Scholar]
- 26.Gangl M. Changing Labour Markets and Early Career Outcomes: Labour Market Entry in Europe Over the Past Decade. Work Employ Soc. 2002;16(1):67–90. https://doi.org/10.1177/09500170222119254. [Google Scholar]
- 27.Müller W, Gangl M, editors. Transitions from Education to Work in Europe: The Integration of Youth into EU Labour Markets. Oxford, England: Oxford University Press; 2003. https://doi.org/10.1093/0199252475.001.0001. [Google Scholar]
- 28.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29(1):1–28. doi: 10.1016/j.jhealeco.2009.10.003. https://doi.org/10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glymour MM, Avendano M, Kawachi I. Socioeconomic Status and Health. In: Berkman LF, Kawachi I, Glymour MM, editors. Social Epidemiology. 2. New York, NY: Oxford University Press; 2014. pp. 17–62. https://doi.org/10.1093/med/9780195377903.003.0002. [Google Scholar]
- 30.Muennig P, Robertson D, Johnson G, Campbell F, Pungello EP, Matthew Neidell P. The Effect of an Early Education Program on Adult Health: The Carolina Abecedarian Project Randomized Controlled Trial. Am J Public Health. 2011;101(3):512–516. doi: 10.2105/AJPH.2010.200063. https://doi.org/10.2105/AJPH.2010.200063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell F, Conti G, Heckman JJ, et al. Early Childhood Investments Substantially Boost Adult Health. Science. 2014;343(6178):1478–1485. doi: 10.1126/science.1248429. https://doi.org/10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lleras-Muney A. The Relationship Between Education and Adult Mortality in the United States. Rev Econ Stud. 2005;72(1):189–221. https://doi.org/10.1111/0034-6527.00329. [Google Scholar]
- 33.Clark D, Royer H. The Effect of Education on Adult Mortality and Health: Evidence from Britain. Am Econ Rev. 2013;103(6):2087–2120. doi: 10.1257/aer.103.6.2087. https://doi.org/10.1257/aer.103.6.2087. [DOI] [PubMed] [Google Scholar]
- 34.Albouy V, Lequien L. Does compulsory education lower mortality? J Health Econ. 2009;28(1):155–168. doi: 10.1016/j.jhealeco.2008.09.003. https://doi.org/10.1016/j.jhealeco.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 35.Eberstadt N. The U.S. Infant Mortality Problem in an International Perspective. Washington, DC: The AEI Press; 1995. [Google Scholar]
- 36.Denney JT, McNown R, Rogers RG, Doubilet S. Stagnating Life Expectancies and Future Prospects in an Age of Uncertainty. Soc Sci Q. 2013;94(2):445–461. doi: 10.1111/j.1540-6237.2012.00930.x. https://doi.org/10.1111/j.1540-6237.2012.00930.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anand S, Ravallion M. Human Development in Poor Couontries - On the Role of Private Income and Publc Services. J Econ Perspect. 1993;7(1):133–150. https://doi.org/10.1257/jep.7.1.133. [Google Scholar]
- 38.Cochrane AL, Leger ASS, Moore F. Health service “input” and mortality “output” in developed countries (Reprinted from Journal of Epidemiology and Community Health vol 32, pg 200–205, 1968) J Epidemiol Community Health. 1997;51(4):344–348. doi: 10.1136/jech.51.4.344. https://doi.org/10.1136/jech.51.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elola J, Daponte A, Navarro V. Health Indicators and the Organization of Health Care Systems in Western Europe. Am J Public Health. 1995;85(10):1397–1401. doi: 10.2105/ajph.85.10.1397. https://doi.org/10.2105/AJPH.85.10.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Houweling TA, Caspar AE, Looman WN, Mackenbach JP. Determinants of under-5 mortality among the poor and the rich: a cross-national analysis of 43 developing countries. Int J Epidemiol. 2005;34(6):1257–1265. doi: 10.1093/ije/dyi190. https://doi.org/10.1093/ije/dyi190. [DOI] [PubMed] [Google Scholar]
- 41.Mays GP, Smith SA. Evidence links increases in public health spending to declines in preventable deaths. Health Aff (Millwood) 2011;30(8):1585–1593. doi: 10.1377/hlthaff.2011.0196. https://doi.org/10.1377/hlthaff.2011.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Terrelonge SC. For Health, Strength, and Daily Food: The Dual Impact of Remittances and Public Health Expenditure on Household Health Spending and Child Health Outcomes. J Dev Stud. 2014;50(10):1397–1410. https://doi.org/10.1080/00220388.2014.940911. [Google Scholar]
- 43.Raphael D, Bryant T. The state’s role in promoting population health: public health concerns in Canada, USA, UK, and Sweden. Health Policy. 2006;78(1):39–55. doi: 10.1016/j.healthpol.2005.09.002. https://doi.org/10.1016/j.healthpol.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 44.Bambra C, Fox D, Scott-Samuel A. Towards a politics of health. Health Promot Int. 2005;20(2):187–193. doi: 10.1093/heapro/dah608. https://doi.org/10.1093/heapro/dah608. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.