Abstract
Design
Mapping Review
Introduction
Although published literature and evidence to support medical practice is becoming more abundant, it is not known how well available evidence supports the full spectrum of hand therapy practice.
Purpose of the study
The aim of this mapping review was to identify strengths/gaps in available literature as compared to the hand therapy scope of practice to guide future research.
Methods
A systematic search and screening was conducted to identify evidence published from 2006-2015. Descriptive data from 191 studies were extracted and the diagnoses, interventions, and outcomes used in the literature were compared to the hand therapy scope of practice.
Results
Osteoarthritis, tendon surgeries, and carpal tunnel syndrome were most frequently studied. Exercise, education, and orthotic interventions were most common, each used in more than 100 studies; only 12 studies used activity-based interventions. Primary outcome measures included range of motion, pain/symptoms, strength, and functional status.
Discussion
Abundant high-quality research exists for a portion of the hand therapy scope of practice; however, there is a paucity of evidence for numerous diagnoses and interventions.
Conclusions
More evidence is needed for complex diagnoses and activity-based interventions, as well as behavioral and quality-of-care outcomes.
Level of evidence
N/A
Keywords: scoping review, hand therapy, interventions, outcome measures
Introduction
Orthopedic injuries and disorders of the upper extremity have a world-wide prevalence of 26.9%.1 Whether caused by overuse or a traumatic incident, upper extremity musculoskeletal disorders often negatively impact an individual’s ability to participate in meaningful play, work, and leisure activities. Hand therapy strives to increase functional capacity and quality of life for individuals with upper extremity disorders;2 however, maximizing quality of care and achieving positive outcomes depends on adequate available evidence. As such, the American Society of Hand Therapists (ASHT) has endorsed the use of evidence-based practice in a position paper on Hand Therapists’ Practice.3 Fortunately, a wealth of evidence has been published in the area of upper extremity rehabilitation in hand therapy specific journals.4 Additionally, several Cochrane systematic reviews have focused on commonly treated diagnoses in hand therapy, such as distal radius fracture5 and carpal tunnel syndrome.6-8
Despite adequate avenues for publishing hand therapy related evidence, it is important to examine to what extent the currently available evidence supports the full scope of practice for hand therapy. In 2011, a review examined all research articles published in the Journal of Hand Therapy through the lens of the World Health Organization’s International Classification of Function.9 At that time, research for hand therapy interventions focused on body function and structures with very little evaluation from an activities, participation or environment perspective. While valuable, this previous review was limited in scope as it only evaluated evidence from one journal. Moreover, there was no assessment of the diagnoses being studied to determine if research evidence was representative of the full scope of hand therapy practice. There have been no other comprehensive examinations of published literature in upper extremity rehabilitation that compares available research evidence to contemporary practice.
Mapping reviews have been used to compare research and practice in order to illuminate gaps and guide research priorities. In the field of developmental medicine, mapping reviews were used to identify gaps in the measurement of long term outcomes for patients with cerebral palsy, as well as demonstrate the need for more rigorous outcome measures following surgical procedures.10,11 Though a mapping review in gerontology, the need for further research related to influenza, falls, osteoporosis, fractures, and mobility was established.12 Another mapping review was used to determine recommendations for improving the fieldwork experience for occupational therapy students.13 Similar to these reviews, the hand therapy profession may benefit from a comprehensive examination of existing research literature as it compares to practice.
Purpose of the study
As a type of scoping review, a mapping review provides an overarching representation of the available literature within a field.14,15 When conducted in a systematic way, mapping reviews are an effective method to communicate the breadth of knowledge on a particular topic and to identify gaps in the overall evidence that can guide priorities for research.15 Thus, the purpose of this mapping review was to identify gaps and research priorities by examining all current literature on the treatment of distal upper extremity musculoskeletal disorders as compared to the ASHT scope of practice.16
The review sought to answer the following questions: Where, by whom, and at what level of evidence is hand therapy relevant research being conducted? What professionals are providing hand therapy relevant interventions in published research? To what extent is evidence available across all diagnostic and intervention categories described in the ASHT scope of practice? What types of outcomes measures are being used in research to evaluate the effectiveness of hand therapy interventions? What gaps exists in current research evidence related to diagnoses, types of interventions, and outcome measures in hand therapy?
Methods
Comprehensive searches were conducted in PubMed, CINAHL, and SPORTDiscus for human studies published in English between January of 2006 and December of 2015 that included interventions for distal upper extremity musculoskeletal disorders. An audit of all medical subheadings (MeSH) and corresponding CINAHL headings was conducted to identify potentially relevant indexing terms across three search categories (i.e., diagnoses, interventions, clinicians). In addition to indexing terms, key words were identified for all diagnoses and interventions from the ASHT scope of practice,16 as well as key words for the primary hand therapy professions. Table 1 provides a list of all indexing terms and key words within each category used in the search for this mapping review. Only those articles that appeared in all three search categories were included. In addition to database searches, titles and abstracts for all articles published in the Journal of Hand Therapy between the years 2006 and 2015 were screened for inclusion.
Table 1.
Indexing terms and keywords used within each of the three search categories.
| Search Categories | Indexing Terms | Keywords |
|---|---|---|
| Musculoskeletal Diagnoses of the Forearm, Wrist & Hand | MeSH: wounds and injuries, arm injuries, hand injuries, sprains and strains, tendon injuries, peripheral nerve injuries, musculoskeletal diseases, hand deformities, joint diseases, muscular diseases, contracture, musculoskeletal pain, rheumatic disease | Arthroplasty, burn, carpal tunnel syndrome, distal radius fracture, distal radial fracture, dequervain, dupuytren, extensor tendon repair, flexor tendon repair, mallet finger, nerve repair, osteoarthritis, rheumatoid arthritis, tenolysis, tenosynovitis, tendonitis, trigger finger, ulnar collateral ligament repair, gamekeeper thumb, skier thumb, boutonniere deformity, swan neck deformity, edema, burn |
| CINAHL/SPORTDiscus: hand fractures, finger flexor tendons, finger joint, carpal joints | ||
|
| ||
| Interventions | MeSH: therapeutics, complementary therapies, mind-body therapies, laser therapy, physical therapy modalities, prosthesis fitting, rehabilitation, activities of daily living, occupational therapy | exercise, therapeutic activity, hand writing, work hardening, work conditioning, manual therapy, orthosis, orthotic, joint protection, range of motion, mobilization, massage, myofascial release, contrast bath, cryotherapy, diathermy, fluidotherapy, hot pack, iontophoresis, electrical stimulation, paraffin, phonophoresis, ultrasound, whirlpool, biofeedback, compression therapy, desensitization, scar management, taping, kinesiotape, wound care |
| CINAHL/SPORTDiscus: therapeutic exercise, alternative therapies, mindbody techniques, combined modality therapy, orthoses | ||
|
| ||
| Clinicians | MeSH: N/A | occupational therapy, occupational therapist, physical therapy, physical therapist, physiotherapy, physiotherapist, hand therapy, hand therapist |
| CINAHL/SPORTDiscus: physical therapy, occupational therapy, hand therapy | ||
Articles were systematically reviewed in a multi-stage screening and selection process. All results were initially screened by title to eliminate articles evaluating treatment for conditions unrelated to the distal upper extremity (e.g., Achilles tendon). Duplicate results were removed and two raters independently screened the abstracts of remaining records to identify studies meeting two general inclusion criteria: 1) involved a musculoskeletal or orthopedic diagnosis of the distal upper extremity, and 2) evaluated or discussed interventions within the scope of hand therapy practice. Full texts were located for articles meeting general inclusion criteria and read by two reviewers. Any full text for which consensus was not reached by the reviewers was read by a third reviewer who determined final eligibility. Final inclusion was not restricted by level of evidence to ensure that the results of this review were based on all available literature.
Using REDCap,17 the following descriptive data were extracted from included studies: publication year, geographic region in which the study was conducted, author profession(s), treating provider(s), study design, participant age, diagnosis, intervention, and outcome. For ease of analysis, study interventions from the ASHT scope of practice16 were organized into seven categories: education, exercise, activity, manual techniques, physical agent modalities, orthotics, and miscellaneous (Table 2). Similarly, outcomes were organized into five categories informed by the International Classification of Functioning, Disability, and Health,9 including: body structure/pathology, pain/symptoms, function/performance, and behavioral/psychosocial. A sixth outcome category, quality of care, included any outcomes associated with the process of care itself. Figure 1 details specific outcome measures within each category. In addition to these categories, the use of standardized questionnaires (e.g., disabilities of the arm, shoulder, and hand; DASH) and other patient-reported outcome (PRO) measures was identified.
Table 2.
Intervention categories developed for data extraction and article analysis from the interventions identified in the ASHT position paper on scope of practice.
| Categories | Interventions |
|---|---|
| Education | Patient/family education, ADL/adaptive/assistive/ergonomic device training, orthotic/prosthetic training, joint protection, energy conservation, nutrition instruction, home exercise program, ergonomic and activity modification, compensatory techniques, wellness education |
|
| |
| Exercise | Exercise without clear functional implication (e.g., range of motion, tendon glides, strengthening) |
|
| |
| Activity | Functional activity, therapeutic activity, work hardening, work conditioning, handwriting |
|
| |
| Manual Techniques | Manual therapy, joint mobilization, nerve mobilization, edema mobilization, myofascial release, therapeutic massage, scar management, hypertrophic/keloid management, pressure therapy, scar mobilization/massage techniques, skin management |
|
| |
| Modalities | Contrast bath, cryotherapy, diathermy, fluidotherapy, hot packs, iontophoresis, laser/light therapy, NMES/electric stimulation, paraffin, phonophoresis, TENS, ultrasound, whirlpool |
|
| |
| Orthosis/Prosthetics | Orthotic design/selection/fitting/fabrication, fabrication of temporary prosthetic for functional activities |
|
| |
| Miscellaneous | Biofeedback, compression therapy, desensitization, sensory re-education, taping techniques, wound care management, design/selection of adaptive/assistive/ergonomic devices |
Figure 1.
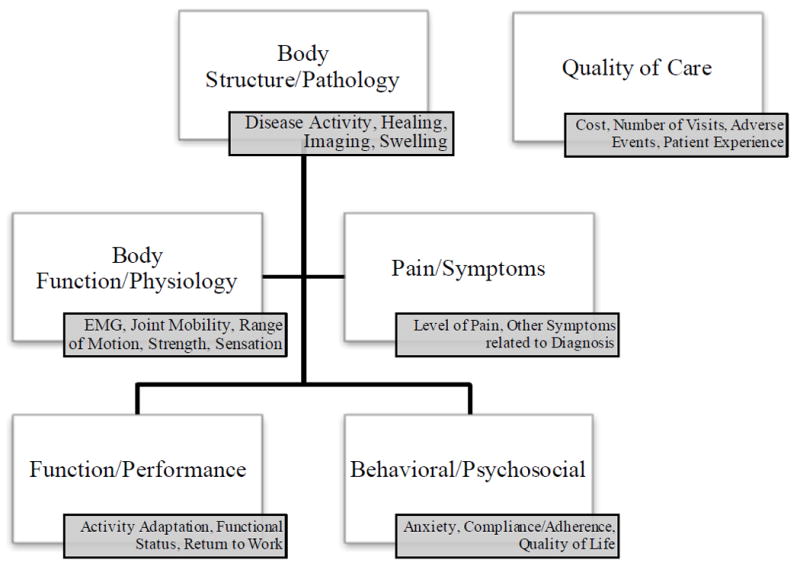
Categories of outcomes used in the included studies, with examples of primary outcome measures included within each category.
To answer the questions driving this mapping review, frequencies were calculated and cross-tabulations were conducted to evaluate relationships among the data categories. Comparison assessment included an evaluation of study designs by diagnoses to identify the strengths, or gaps, in research quality for various conditions treated in hand therapy. Relationships among intervention types to diagnoses, and intervention types to outcome measures were also examined. Multiple consensus meetings were held among the authors to review the data and identify gaps in evidence relative to the diagnoses, interventions, and outcomes identified in the ASHT scope of practice.16
Results
The database search yielded 9,079 results, which were reduced to 1,010 abstracts after initial screening. A total of 283 abstract were identified for full-text read through and 33 additional articles were added through the hand search of the Journal of Hand Therapy. Following full-text review, a total of 191 articles met the criteria for final inclusion. Primary reasons for exclusion of articles were studies that evaluated treatment for genetic or systemic conditions not specific to the distal upper extremity, focused on clinical measurement validation or reliability in a contrived or laboratory setting, or involved interventions outside the scope of hand therapy. A detailed flow diagram of study search, screening, and selection results is presented in Figure 2.
Figure 2.
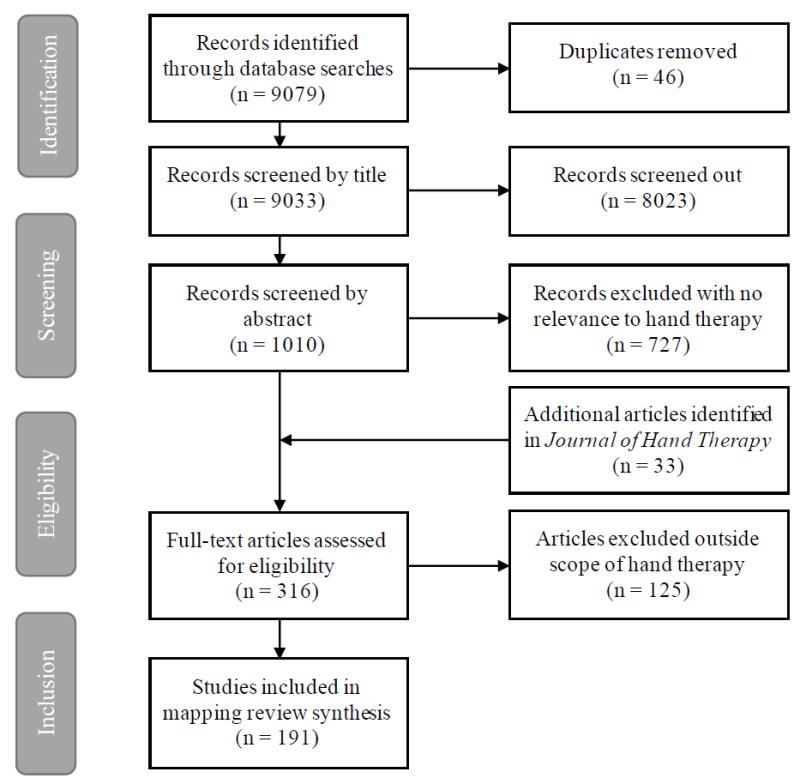
Flow of records and articles through the review process.
Characteristics of the Literature
Up to 2013, the number of articles published each year steadily increased, beginning with only 8 publications in 2006 to a peak of 28 articles in 2013 (Figure 3). In 2014, there was a sharp decline in publications by almost 50%, with only 15 and 16 articles published in 2014 and 2015, respectively. More than 65% of the studies were conducted in North American and European Countries (i.e., 35.6% and 30.9%). A smaller percentage of articles were noted from Australia/New Zealand (13.1%) and Eurasia/Middle Eastern countries (9.95%), with only three publications originating in Africa or South America. Although the author professions couldn’t be identified in nearly one-third of the articles, professions with the largest representation as authors were physicians (22.8%), occupational therapists (22.8%), and physical therapists (16.2%). Similarly, most of the articles (53.9%) did not specify the qualifications of the interventionist; however, occupational therapists (23.5%) and physical therapists (17.2%) were most frequently identified in those studies that did provide this detail. Randomized trials (n=64) were most common, followed by prospective cohort studies (n=29) and case series/studies (n=25). There were 18 systematic reviews, but only one meta-analysis. Qualitative studies represented 4.7% (n=9) of the articles and included three qualitative case studies, five phenomenological studies, and one grounded theory study. The remaining study designs were each represented by less than 10% of the articles in this review.
Figure 3.
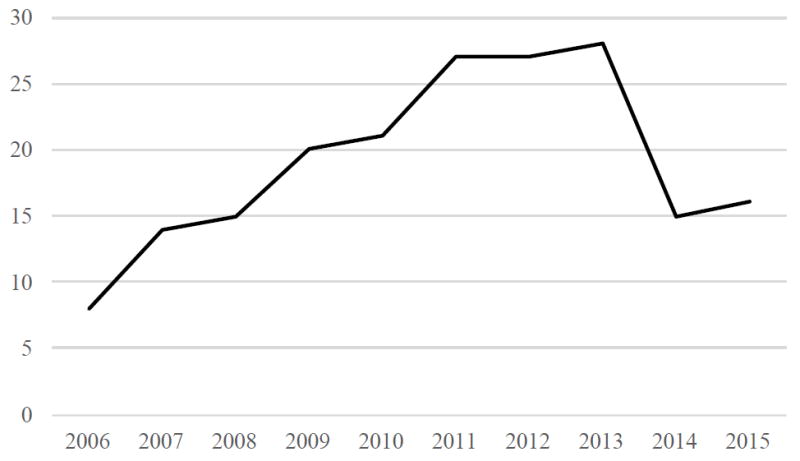
Trend for the number of articles relevant to hand therapy published each year across a 10-year period from 2006-2015.
More than two-thirds of the articles included adults (68.6%) while only five articles included participants exclusively under the age of 18; the remaining articles did not specify the age of participants. Diagnoses most frequently evaluated were osteoarthritis (16.1%); tendon surgeries, including flexor/extensor tendon repairs and transfers (15.6%); and carpal tunnel syndrome (15.2%). Rheumatoid arthritis, distal radius fractures, and other joint pathologies (e.g., Dupuytren’s contracture, metacarpophalangeal joint avulsion, carpal instability, joint laxity, volar plate injuries) were each a focus in 8% to 10% of the studies. There were relatively few articles focused on arthroplasty (n=7), trauma and pain syndromes (n=6), work related disorders/repetitive overuse syndromes (n=6), burns (n=5), amputations (n=4), or hand transplants (n=2).
The number of studies that included an intervention in each of the six main categories is presented in Figure 4. Exercise was the most frequently used intervention, included in 72.3% of studies. In contrast, the fewest number of articles explored activity-based interventions (6.3%). More than half of the studies included education or orthotic-based interventions. Within the education category, home exercise programs were the primary type of intervention (81.1%), followed by orthotic/prosthetic training. Within orthotic-based interventions, three-fourths of the articles investigated the use of custom-made orthotics. Manual techniques were included in about one-fourth of the total articles, with joint mobilization, nerve mobilization, and scar management each appearing in approximately 30% of those studies. Physical agent modalities were discussed in 18.8% of the articles in this review, one-third of which evaluated ultrasound and one-quarter examined the use of low-level laser therapy. Additional miscellaneous interventions included sensory re-education, wound care/management, desensitization techniques, compression therapy, biofeedback techniques, and taping techniques; each used in fewer than 10 studies.
Figure 4.
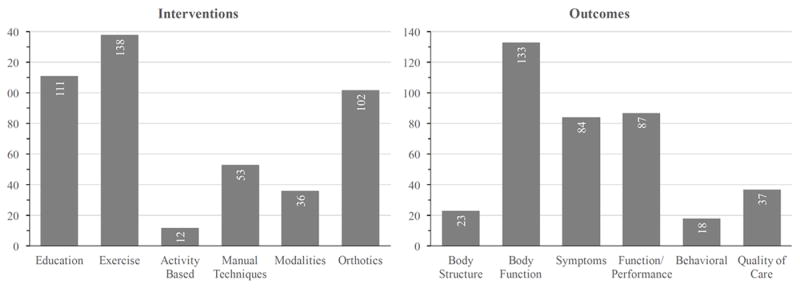
Frequency of studies (n=191) including an intervention and outcome measure within each of the primary categories.
Across the included studies, the number of articles measuring outcomes in each category is also presented in Figure 4. Body function/physiology outcomes were most frequently used (69.6%), followed by pain/symptoms outcomes and function/performance outcomes. Quality of care, body structure/pathology, and behavioral/psychosocial outcomes were least commonly measured. The most common specific outcomes measures used in studies were range of motion (20.4%), pain/symptom severity (17.6%), strength (17.6%), and general measures of functional status (17.4%). PRO measures were used in nearly three-fourths of the studies, with half of the articles using standardized questionnaires. Of all studies using PRO, the DASH or QuickDASH was the most commonly used standardized questionnaire (32.1%), followed by a Visual Analog Pain Scale (21.4%). The Boston Carpal Tunnel Questionnaire and the Australian/Canadian Osteoarthritis Hand Index were each used in approximately 10% of the studies that collected PRO.
Interrelations of the Characteristics of the Literature
Figure 5 depicts the study designs by diagnoses, providing an easy way to identify strengths and gaps in currently the available evidence for each diagnosis. Consistent with descriptive findings, the largest number of high-quality designs (e.g., systematic reviews and randomized trials) are available for the most frequently studied diagnoses (e.g., carpal tunnel syndrome, osteoarthritis, tendon injuries). In contrast, there are relatively few studies at the higher levels of evidence for diagnoses that may be less common and typically more complex, including arthroplasty, amputation, traumas, and hand transplants.
Figure 5.
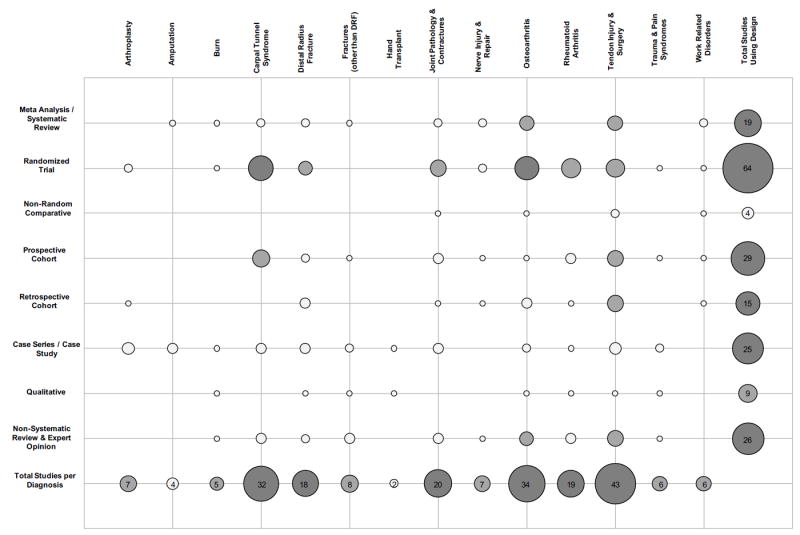
Total number of published articles for each diagnosis by study design, with larger circles indicating higher frequencies. (Note: dark grey indicates 15 or more studies, light grey indicates 5-14 studies, white indicates less than 5 studies)
The frequency of studies using each intervention type by diagnosis is presented in Table 3. With exception of nerve injuries/repairs, exercise interventions were used in more than half of the studies across all diagnoses. Similarly, patient education was included in more than half of all studies for each diagnosis with exception of nerve injury/repair and trauma/pain syndromes. Orthotic-based interventions were used in all studies for individuals with amputations and arthroplasties, and nearly all studies treating patients with fractures other than distal radius fracture and joint pathologies/contractures. Modalities, manual techniques, and activity-based interventions were used in less than half of the studies across all individual diagnoses. In fact, activity-based interventions were only used or mentioned in articles within 9 of the 14 diagnostic groups.
Table 3.
Frequency (percentage) of studies by diagnosis that used an individual intervention within each primary intervention category.
| Diagnosis | Education | Exercise | Activity-Based | Manual Techniques | Physical Agent Modalities | Orthotics |
|---|---|---|---|---|---|---|
| Amputation | 4 (100%) | 4 (100%) | 1 (25%) | 2 (50%) | 2 (50%) | 4 (100%) |
| Arthroplasty | 5 (71%) | 6 (86%) | 2 (29%) | 3 (43%) | 1 (14%) | 7 (100%) |
| Burn | 3 (60%) | 4 (80%) | 1 (20%) | 2 (40%) | 1 (20%) | 2 (40%) |
| Carpal Tunnel Syndrome | 17 (53%) | 22 (69%) | - | 16 (50%) | 13 (41%) | 15 (47%) |
| Distal Radius Fracture (DRF) | 12 (67%) | 13 (72%) | - | 2 (11%) | 2 (11%) | 5 (28%) |
| Fractures (Other than DRF) | 5 (63%) | 4 (50%) | 1 (13%) | 1 (13%) | 1 (13%) | 7 (88%) |
| Hand Transplant | 1 (50%) | 2 (100%) | 1 (50%) | 1 (50%) | 1 (50%) | 1 (50%) |
| Joint Pathology and Contracture | 10 (50%) | 13 (65%) | 1 (5%) | 3 (15%) | 2 (10%) | 19 (95%) |
| Nerve Injury/Repair | 2 (29%) | 3 (43%) | - | 1 (14%) | - | 1 (14%) |
| Osteoarthritis | 18 (53%) | 25 (74%) | - | 15 (44%) | 13 (38%) | 13 (38%) |
| Rheumatoid Arthritis | 14 (74%) | 15 (79%) | 1 (5%) | 7 (37%) | 4 (21%) | 9 (47%) |
| Tendon Injuries & Surgeries | 32 (74%) | 35 (81%) | 2 (5%) | 7 (16%) | 3 (7%) | 5 (77%) |
| Trauma and Pain Syndromes | 2 (33%) | 4 (67%) | 2 (33%) | 2 (33%) | 2 (33%) | 3 (50%) |
| Work-Related / Repetitive Syndromes | 5 (83%) | 5 (83%) | - | 2 (33%) | 1 (17%) | 2 (33%) |
Note. Bold indicates category with highest frequency within each diagnosis
There were slight variations in the type of outcome measures used across the intervention categories (Figure 6). Measures of body function (e.g., range of motion, strength) were most commonly paired with all interventions, being used more than two-thirds of the time. Measures of activity and functional performance were used in about half of the studies across all intervention categories. However, functional performance measures were used much more frequently with activity-based interventions than with other intervention types. Symptoms and pain reports were used more frequently with manual techniques and physical agent modalities (i.e., 66.0% and 63.7%, respectively), as compared to approximately only one-third of the time for other intervention types. Quality measures had more limited use, but most frequently appeared with orthotic and educational interventions. Behavioral outcomes (e.g., anxiety, quality of life) were rarely measured, but most frequently matched with educational interventions. The frequency of studies using PRO measures in combination with the different intervention types ranged from 58.3% to 84.9%, with studies using activity-based and orthotic interventions using PROs least frequently.
Figure 6.
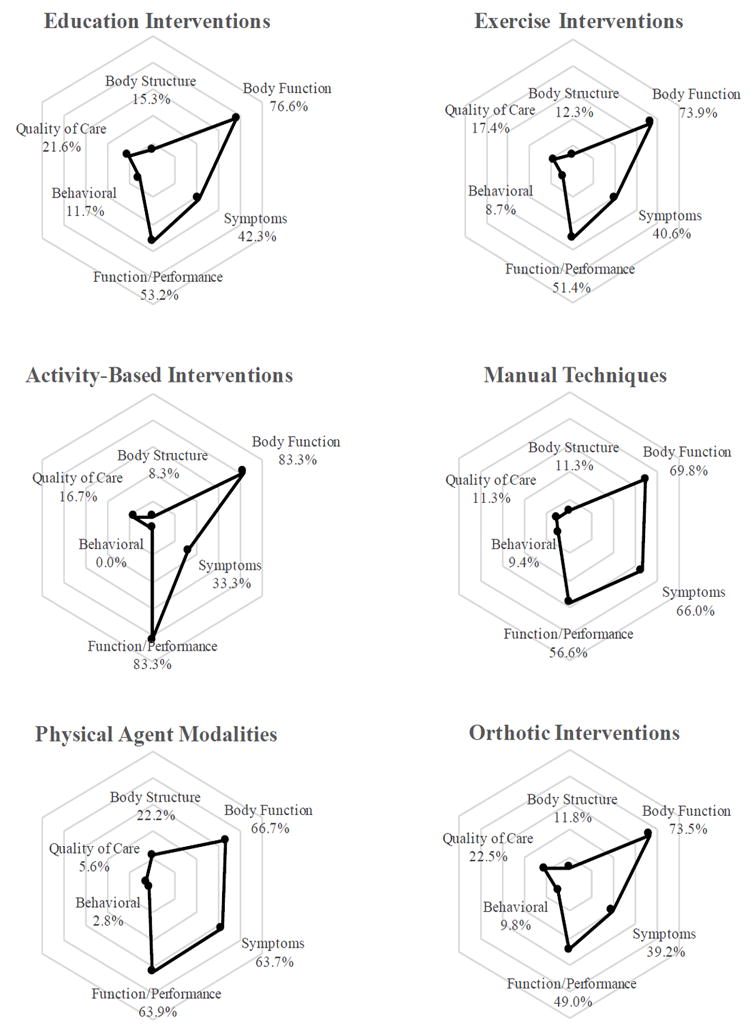
Percentage of studies measuring each outcome type within the six intervention categories. Variations in outcome measure usage by intervention are represented by differing shapes across the six web charts.
Discussion
To ensure the field of hand therapy continues its tradition as an evidence-based rehabilitation specialty, it is advantageous to compare the available literature on distal upper extremity rehabilitation to the scope of practice.16 As such, this mapping review aimed to describe the current content of the available literature, identify gaps, and provide suggestions for research and practice to enhance the evidence base for the profession. Evidence exists for a wide-range of diagnoses treated by hand therapists and for the many common interventions provided within hand therapy. However, there are multiple diagnoses and interventions for which evidence is either sparse or of low-quality. Additionally, this review illuminated opportunities for increasing evidence related to various types of outcome measures within hand therapy.
While a large number of articles pertaining to rehabilitation distal upper extremity disorders have been published in the last ten years, the number of studies in recent years has declined. Moreover, the majority of studies were conducted in North American and European countries. The recent decline in studies and lack of diversification may be an impediment to the global advancement of hand therapy. Additionally, although there were as many therapists as doctors conducting the studies, the majority of articles did not specify the clinical qualifications of either the authors or the individual(s) providing the intervention. Reporting the clinical background of the authors and intervenors in future studies will help inform the translation and successful implementation of findings from the literature into practice. Most importantly, it is essential for therapists to participate in the conduct of research to support hand therapy practice.
Current evidence is primarily focused on osteoarthritis, tendon surgeries, and carpal tunnel syndrome. Given the prevalence of these disorders, it is important to continue expanding the scope and quality of evidence in these areas; however, it is also vital to build evidence for the treatment of other disorders within the hand therapy scope of practice. For example, therapeutic treatment following both arthroplasty and nerve injuries and repairs was only discussed in 3.3% of articles. Similarly, the relatively few research articles on hand transplants and amputations, as well as the low level of evidence may be reflective of the rarity of these conditions; however, the lack of evidence highlights an important area for increased research on interventions and outcomes for these disorders.
Although a large proportion of the total studies available used high-level study designs, the level of evidence is not equally distributed across all diagnoses. For the highly researched diagnoses, an impressive number of meta-analyses and systematic reviews were discovered, providing clinicians with resources to guide clinical decision making. However, clinical guidance is more limited due to a lack of high-level studies for individuals with arthroplasty, rheumatoid arthritis, trauma and pain syndromes, burn, nerve injury and repair, and work-related disorders/repetitive overuse syndromes.
Current research foci for interventions may not be in line with priorities and patterns in contemporary hand therapy practice. Based on this mapping review, exercise and orthotics interventions appear to be a strong priority in current research, with less attention to other intervention types and exceedingly few studies evaluating activity-based interventions. In a recent practice analysis of hand therapists and other clinicians treating upper quadrant disorders, manual therapy techniques and education were both the most frequently used interventions and rated most critically important.18 Furthermore, respondents to that practice survey indicated slightly more frequent use of exercise than functional activities, but rated both equally as important.18
Although there is an abundance of evidence regarding exercise, education, and orthotic interventions, it is necessary to expand research to other interventions that are important in practice. Specifically, there is a need to increase the evaluation of manual techniques and functional, activity-based interventions. Given the preponderance of occupational therapists within the hand therapy profession, increasing evidence for the latter may be exceptionally vital as activity-based interventions are a keystone within occupational therapy practice.19 In fact, up to 85% of hand therapists indicate they use occupation-based interventions in their practice.20 A few recent studies have begun to provide evidence for activity-based interventions in upper extremity rehabilitation.21,22 However, as this review indicates that there are only one-tenth as many studies evaluating activity-based techniques as compared to exercise and other interventions.
Similar to a need to expand evidence for activity-based interventions, there may be a need to expand the use of functional performance and activity-based outcome measures. Just under half of the literature included in this review measured performance of functional activities. Although performance measures appeared with similar frequency to pain and symptom measures, these outcomes were overshadowed by measurement of body function (e.g., range of motion, muscle strength) and/or tissue physiology. Although potentially important as direct outcome for manual techniques, modalities, and exercise interventions, measures of body function may not be proxies for more direct measures of occupational performance. Measuring quality of care outcomes is another gap in the literature, reported in less than 20% of the articles in this review. As the push for the delivery of cost-efficient, high-quality care continues, more research that evaluates both effectiveness and quality of care will be necessary.23,24 Moreover, with a call for an increased focus on integrative health,25 evaluating the effectiveness of hand therapy interventions by their direct or indirect impact on quality of life, behavioral, and psychosocial outcomes is exceptionally timely.26,27
Multiple limitations are inherent when conducting a mapping review. Most notably, because the purpose of a mapping review is to describe the extent and nature of existing literature, this review did not evaluate the quality of individual studies, nor did this review provide any qualitative summary regarding the effectiveness of specific interventions. Second, in order to make the mapping process feasible, this review was limited to musculoskeletal disorders of the distal upper extremity. As such, it does not provide insight into the available literature for conditions of the elbow/shoulder or for systemic disorders involving multiple body segments that are also treated by hand therapists. Given this restricted focus, some studies that included information related to the distal region may have been screened out in the early stages of review. Next, data extraction was limited to the information provided within the text of each article, which limited and potentially biased the findings in this review. Specifically, more interventions or outcomes may have been included in individual studies than what was reported. Additionally, it was often difficult to identify the professional background of the authors and intervenors. Finally, because data were extracted, categorized, and interpreted based on the ASHT scope of practice, an American practice perspective is heavily represented, and the findings of this study may not be generalizable to hand therapy practice in other countries.
Conclusions
This mapping review was conducted to understand the representation of diagnoses, interventions, outcomes, and study methodologies within currently available hand therapy related literature over the last 10 years. This review identified strengths and gaps in the current literature as it relates to the full hand therapy scope of practice and current practice patterns. Specifically, there is an abundance of evidence available for commonly treated diagnoses, such as carpal tunnel syndrome, osteoarthritis, and tendon injuries. However, there are only limited, low-quality reports for more involved diagnoses, including amputations, hand transplants, and traumatic injuries. Across all diagnoses, there is an abundance of literature investigating exercise, orthotic, and educational interventions, but relatively few studies using activity-based interventions. Measurement of body function (e.g., range of motion, strength) is exceedingly common, whereas the evaluation of other types of outcomes is more limited. To ensure evidence is available to support all areas within the hand therapy scope of practice, more research is needed regarding complex musculoskeletal disorders and for activity-based interventions. Moreover, an increased focus on the impact of hand therapy on functional/activity performance, behavioral, and quality of care outcomes would strengthen the evidence-base for hand therapy practice.
Highlights.
There is an abundance of evidence available for commonly treated diagnoses, such as, carpal tunnel syndrome, osteoarthritis, and tendon injuries; however, there are only limited, low-quality reports for more involved diagnoses, including amputations, hand transplants, and traumatic injuries.
Across all diagnoses, there is an abundance of literature investigating exercise, orthotic, and educational interventions, but relatively few studies using activity-based interventions.
Patient reported outcome measures have high-use within the literature; however, measurement of body function (e.g., range of motion) is exceedingly more common than measurement of activity performance and other participation-based metrics.
More research is needed for complex musculoskeletal disorders and to support activity-based interventions, and an increased focus on the impact of hand therapy on functional/activity performance, behavioral, and quality of care outcomes would strengthen the evidence-base for hand therapy practice.
Acknowledgments
Work on this review was partially supported by Grant No. K12–HD055929, National Institute of Child Health and Human Development/National Institute of Neurological Disorders and Stroke Rehabilitation Research Career Development Program. The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Huisstede BM, Bierma-Zeinstra SM, Koes BW, Verhaar JA. Incidence and prevalence of upper-extremity musculoskeletal disorders. A systematic appraisal of the literature. BMC musculoskeletal disorders. 2006;7:7. doi: 10.1186/1471-2474-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dimick MP, Caro CM, Kasch MC, et al. 2008 practice analysis study of hand therapy. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2009;22(4):361–375. doi: 10.1016/j.jht.2009.06.001. quiz 376. [DOI] [PubMed] [Google Scholar]
- 3.Young KS, Krueger R, Goldie Staines K, DeAngelis C, Coker D, Bash D, Hardy M. A Position Paper on Evidence-Based Practice in Hand Therapy. American Society of Hand Therapists; 2013. [Google Scholar]
- 4.Flowers K, LaStayo PC. And On We Go To the Next 25 Years. Journal of Hand Therapy. 2012;25(1):1–2. doi: 10.1016/j.jht.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Handoll HH, Elliott J. Rehabilitation for distal radial fractures in adults. The Cochrane database of systematic reviews. 2015;(9) doi: 10.1002/14651858.CD003324.pub3. CD003324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huisstede BM, Hoogvliet P, Randsdorp MS, Glerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. Part I: effectiveness of nonsurgical treatments--a systematic review. Arch Phys Med Rehabil. 2010;91(7):981–1004. doi: 10.1016/j.apmr.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 7.Page MJ, O’Connor D, Pitt V, Massy-Westropp N. Exercise and mobilisation interventions for carpal tunnel syndrome. The Cochrane database of systematic reviews. 2012;(6) doi: 10.1002/14651858.CD009899. Cd009899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters S, Page MJ, Coppieters MW, Ross M, Johnston V. Rehabilitation following carpal tunnel release. The Cochrane database of systematic reviews. 2016;2(2) doi: 10.1002/14651858.CD004158.pub3. CD004158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jette AM. Toward a common language for function, disability, and health. Physical therapy. 2006;86(5):726–734. [PubMed] [Google Scholar]
- 10.Kembhavi G, Darrah J, Payne K, Plesuk D. Adults with a diagnosis of cerebral palsy: a mapping review of long-term outcomes. Developmental medicine and child neurology. 2011;53(7):610–614. doi: 10.1111/j.1469-8749.2011.03914.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilson NC, Chong J, Mackey AH, Stott NS. Reported outcomes of lower limb orthopaedic surgery in children and adolescents with cerebral palsy: a mapping review. Developmental medicine and child neurology. 2014;56(9):808–814. doi: 10.1111/dmcn.12431. [DOI] [PubMed] [Google Scholar]
- 12.Roberts ME, Hooper BR, Wood WH, King RM. An international systematic mapping review of fieldwork education in occupational therapy. Canadian journal of occupational therapy Revue canadienne d’ergotherapie. 2015;82(2):106–118. doi: 10.1177/0008417414552187. [DOI] [PubMed] [Google Scholar]
- 13.Winthrop Rose B, Kasch MC, Aaron DH, Stegink-Jansen CW. Does hand therapy literature incorporate the holistic view of health and function promoted by the World Health Organization? Journal of hand therapy : official journal of the American Society of Hand Therapists. 2011;24(2):84–87. doi: 10.1016/j.jht.2010.12.003. quiz 88. [DOI] [PubMed] [Google Scholar]
- 14.Hammick M. A BEME review: a little illumination. Med Teach. 2005;27(1):1–3. doi: 10.1080/01421590500046858. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 16.Cricchio M, McVeigh K, Lee M, Clancy S, Kane E, Bash D, Winthrop Rose B. A Position Paper on Hand Therapists’ Scope of Practice. American Society of Hand Therapists; 2011. [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keller JL, Caro CM, Dimick MP, Landrieu K, Fullenwider L, Walsh JM. Thirty years of hand therapy: The 2014 practice analysis. JOURNAL OF HAND THERAPY. 2016;29(3):222–234. doi: 10.1016/j.jht.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 19.Roll SC. Current Evidence and Opportunities for Expanding the Role of Occupational Therapy for Adults With Musculoskeletal Conditions. American Journal of Occupational Therapy. 2016;71(1):7101170010p7101170011–7101170010p7101170015. doi: 10.5014/ajot.2017.711002. [DOI] [PubMed] [Google Scholar]
- 20.Grice KO. The use of occupation-based assessments and intervention in the hand therapy setting - A survey. J Hand Ther. 2015;28(3):300–305. doi: 10.1016/j.jht.2015.01.005. quiz 306. [DOI] [PubMed] [Google Scholar]
- 21.Hardison ME, Roll SC. Factors Associated With Success in an Occupational Rehabilitation Program for Work-Related Musculoskeletal Disorders. The American Journal of Occupational Therapy. 2017;71(1):7101190040p7101190041–7101190040p7101190048. doi: 10.5014/ajot.2016.023200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Che Daud AZ, Yau MK, Barnett F, Judd J, Jones RE, Muhammad Nawawi RF. Integration of occupation based intervention in hand injury rehabilitation: A Randomized Controlled Trial. J Hand Ther. 2016;29(1):30–40. doi: 10.1016/j.jht.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 23.Pergolotti M, Lavery J, Reeve BB, Dusetzina SB. Examining Variation in Occupational Therapy Costs and Potential Decreases in Service Use Due to a Reduced Therapy Cap. American Journal of Occupational Therapy. 2016;70(4_Supplement_1):7011510180p7011510181–7011510180p7011510181. [Google Scholar]
- 24.Leland NE, Crum K, Phipps S, Roberts P, Gage B. Advancing the Value and Quality of Occupational Therapy in Health Service Delivery. The American Journal of Occupational Therapy. 2015;69(1):6901090010p6901090011–6901090010p6901090017. doi: 10.5014/ajot.2015.691001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Briggs JP, Killen J. Perspectives on complementary and alternative medicine research. JAMA. 2013;310(7):691–692. doi: 10.1001/jama.2013.6540. [DOI] [PubMed] [Google Scholar]
- 26.Hardison ME, Roll SC. Mindfulness Interventions in Physical Rehabilitation: A Scoping Review. The American Journal of Occupational Therapy. 2016;70(3):7003290030p7003290031–7003290030p7003290039. doi: 10.5014/ajot.2016.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stonner MM, Mackinnon SE, Kaskutas V. Predictors of Disability and Quality of Life With an Upper-Extremity Peripheral Nerve Disorder. American Journal of Occupational Therapy. 2016;71(1):7101190050p7101190051–7101190050p7101190058. doi: 10.5014/ajot.2017.022988. [DOI] [PubMed] [Google Scholar]


