Abstract
Music therapy has been employed as a therapeutic intervention to facilitate healing across a variety of clinical populations. There is theoretical and empirical evidence to suggest that individuals with trauma exposure and Posttraumatic Stress Disorder (PTSD), a condition characterized by enduring symptoms of distressing memory intrusions, avoidance, emotional disturbance, and hyperarousal, may derive benefits from music therapy. The current narrative review describes the practice of music therapy and presents a theoretically-informed assessment and model of music therapy as a tool for addressing symptoms of PTSD. The review also presents key empirical studies that support the theoretical assessment. Social, cognitive, and neurobiological mechanisms (e.g., community building, emotion regulation, increased pleasure, anxiety reduction) that promote music therapy’s efficacy as an adjunctive treatment for individuals with posttraumatic stress are discussed. It is concluded that music therapy may be a useful therapeutic tool to reduce symptoms and improve functioning among individuals with trauma exposure and PTSD, though more rigorous empirical study is required. In addition, music therapy may help foster resilience and engage individuals who struggle with stigma associated with seeking professional help. Practical recommendations for incorporating music therapy into clinical practice are offered along with several suggestions for future research.
Keywords: Music Therapy, PTSD, Posttraumatic Stress, Trauma
Introduction
“One good thing about music, when it hits, you feel no pain.”
-Bob Marley, Trench Town Rock
Music holds a ubiquitous role in our society (McDermott & Houser, 2005) and the creation and consumption of music represents a universal human activity (Rentfrow & Gosling, 2003). Of note, the role of group music making as an evolutionary advantage has long been considered and questioned (Darwin, 1859). Specifically, acoustic synchronization likely served as a mechanism to enhance likelihood of reproductive success (Cross, 2009) and as a way to communicate, build cohesion, and foster cooperation with others (McDermott & Houser, 2005; Disanayake, 2009).
There is a long and rich tradition of using music to cultivate resilience and facilitate healing in the wake of violence and oppression. Songs and chanted hymns often accompanied physical labor endured by American slaves to coordinate movement and boost resolve to complete arduous tasks (Gregory, 1997). The introduction of communal music-making activities to adolescent groups in post-apartheid South Africa led to self-reported reduction of anxiety, stress, and fear in the wake of community violence (Pavlicevic, 1999). These historical accounts of healing with music are complimented by research demonstrating that emotional responses to music are neurally mediated, such that listening to music activates brain structures involved in reward, pleasure, and emotional processing (e.g. insula, ventral medial prefrontal cortex, ventral striatum, amygdala, hippocampus; Koelsch 2009). Further, group music making has been shown to help solidify an individual’s sense of identity within their perceived social group (Gregory, 1997). More recently, trauma researchers and clinicians have been promoting the use of alternative and less verbally-intensive treatment modalities for trauma survivors involving body movement and creative arts (e.g. Garrido, Baker, Davidson, Moore, & Wasserman, 2015; Van der Kolk, 2014; Van Westrhenen & Fritz, 2014).
A Brief Overview of Music Therapy in the United States
Music has increasingly become internationally recognized as an intervention to be employed with clinical populations. In the United States, the creation of the National Association for Music Therapy and the Certification Board of Music Therapists led to the standardization and emergence of accredited music therapy programs in the early 1950s. Music therapy is now nationally disseminated across a variety of settings including hospitals, youth centers, schools, and prisons (American Music Therapy Association; AMTA).
Music therapy in the United States must be practiced by accredited music therapists certified by the Certification Board and can serve as an adjunctive therapeutic program or stand on its own (AMTA). Mental health providers must refer clients to music therapists if they want to incorporate music therapy into treatment. The therapist then formulates a treatment plan that can involve musical improvisation, listening exercises, singing, music making, the playing of an instrument, and a discussion of the emotions conveyed through a piece of music heard by the patient (Bonde & Wigram, 2002).
A music therapist offers a tailored structure to shape and develop the course of therapy (AMTA). For instance, the patient can create his own music with the therapist’s guidance as a way of expressing emotions (Hurt-Thaut, 2009) or the therapist can present the patient with a song and encourage him to sing along or introduce their own words (Sacks, 2007). There exist multiple theoretical approaches to the implementation of music therapy (Davis, Gfeller, & Thaut, 2008), including both product- and process-oriented music making (Crowe, 2007) emphasis on social integration via music (Voigt, 2003) and the Guided Imagery in Music technique, which involves listening to selected music in order to elicit imagery, symbols, and deep, potentially unconscious feelings (Maack & Nolan, 1999). Group or communal music therapy is intended to bring together individuals with a shared experience (e.g. military service, communal trauma) to work together via group discussion or improvisation (DeNora, 2002). Clearly, music therapy can be extremely structured and widely varied across a range of instruments, mediums, and methods of expression (Bensimon, Amir, & Wolf, 2008). More recently, it has been employed in the treatment of individuals with trauma exposure and Posttraumatic Stress Disorder (PTSD; e.g. MacIntosh, 2003; Orth, 2001; Heidenreich, 2005).
Music Therapy, Trauma, and PTSD
In a large epidemiological study of nearly 6,000 U.S. citizens, 60% of men and 51% of women experienced at least one traumatic event in their lifetime, with 8% experiencing PTSD (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). PTSD is characterized by an inability to recover from a reaction of stress by one month following exposure to a traumatic event (American Psychiatric Association (APA), 2013). Symptoms can include re-experiencing the event, intrusive memories of the event, prolonged emotional distress and physiological reactivity after exposure to trauma-related stimuli, avoidance of trauma-related thoughts and external reminders, negative alterations in mood and cognition (e.g. anhedonia, constricted affect, social detachment, persistent negative trauma-related emotions and beliefs), and alterations in arousal and reactivity (e.g. hyperarousal, irritable and aggressive behavior, exaggerated startle response; APA, 2013). Many individuals who experience trauma do not meet full criteria for PTSD (e.g. Kessler et. al, 1995). However, many trauma-exposed individuals still experience residual posttraumatic stress symptoms that negatively impact their quality of life (Thomas et al., 2010) as well as increased risk for other mental health conditions such as depression and problematic substance use (Thomas et. al, 2010; Campbell et al., 2007).
A number of evidence-based interventions are available for the treatment of PTSD, including Trauma-Focused Cognitive Behavioral Therapy (TF-CBT; Cohen, Kliethermes, Mannarino, & Murray, 2012), Cognitive Processing Therapy (CPT; Foa et al., 1999), Eye Movement Desensitization and Reprocessing Therapy (EMDR; Pitman et al., 1996 but see Schubert & Lee, 2009), and Prolonged Exposure (PE; Resick, Monson, & Chard, 2007). However, these therapies are time-intensive, require highly specialized and lengthy clinical training and supervision, and have been associated with high levels of attrition, perhaps due to the intensity of the therapeutic methods, which focus on re-telling of the index trauma (Zayfert & Deviva, 2004). Indeed, in a meta-analysis examining the efficacy of treatments for PTSD, attrition rates for exposure therapy, cognitive therapy (e.g. CBT or CPT), combination exposure and cognitive therapy, and EMDR were 20%, 22%, 27%, and 19%, respectively (Hembree, Foa, Dorfan, Street, Kowalski, & Tu, 2003). Finally, clinical psychologists (Ph.D. or Psy.D. level mental health providers) who perform these treatments tend to be less accessible in the community because of the significant training and case management burdens.
Music therapy may offer a more accessible and less stigmatizing therapeutic option for treating posttraumatic stress. Extant evidence that music therapy reduces stress and anxiety in other clinical populations (e.g., children; Westrhenen & Fritz, 2014; Gold, Voracek, & Wigram, 2004; individuals with depression; Guétin, et al., 2009; Erkkila, et al., 2011; Alzheimer’s patients; Svansdottir & Snaedal, 2006) suggests it may have the potential to improve clinical and functional outcomes and foster resilience among individuals struggling with posttraumatic stress. Indeed, music is evidenced to reduce emotional distress (Gross & Jazaieri 2014), foster social connectedness (Gregory, 1997), and improve overall wellbeing (Bonde & Wigram, 2002). However, integrated examination of the theoretical mechanisms and processes with empirical evidence for music therapy for PTSD pathology is currently limited. Accordingly, the objectives of this review are twofold:
The primary objective of this narrative review is to provide a theoretical overview of the key mechanisms of music therapy that support its use as a tool for posttraumatic stress and offer practical resources and recommendations for clinicians and researchers.
The secondary objective is to examine what little empirical literature is available regarding the impact of music therapy on clinical (e.g. depression, health, PTSD symptoms) and functional (e.g. wellbeing, interpersonal relationships) outcomes among individuals with symptoms of posttraumatic stress and link this evidence to our discussion of theoretical mechanisms of music therapy.
Method
Literature searches were conducted using Google Scholar, PubMed, and Web of Science for peer-reviewed articles using the search terms “music therapy” and “music therapy for PTSD,” along with “stress,” “anxiety,”, and “trauma.” A total of 25 articles were selected for further review based on their relevance to the search terms. Criteria for inclusion in the empirical review were (1) adult subjects of 18 years of age or older, (2) established assessment of exposure to trauma or serious adversity, (3) use of a music therapy intervention to address symptoms of posttraumatic stress, and (4) a pre-post-test (prospective) design. Four studies met the above criteria and were thus included in the current empirical review (See Table 1). Of note, additional studies that did not meet inclusion criteria for our empirical review have examined the efficacy of various musical interventions with different trauma-exposed populations (e.g., children with complex trauma, individuals affected by sexual abuse and war). These studies provide additional theoretical support for the use of music therapy to address trauma, and are thus incorporated into our theoretical review.
Table 1.
Empirical Studies Examining Music Therapy for PTSD and Related Symptoms
| Study | Design | n | Age | Approach | Effect Size | Outcomes |
|---|---|---|---|---|---|---|
| Bensimon, Amir, & Wolf, 2008 | Observational pre-post study; no control | 6 | 20–23 | Group drumming therapy; 16, 90 minute sessions | none reported | Improved feelings of self-worth and reduction of isolation |
| Carr et al., 2011 | Randomized control trial | 17 | 18–65 | Subjects given CBT alone or CBT w/additional 10 weeks music therapy | p = .004 | Significant reduction of posttraumatic stress symptoms |
| Hernandez-Ruiz, 2005 | Randomized control trial | 28 | Mean age = 35 | 5 days of group therapy. Music and progressive relaxation script for half of the participants | p < .001 | Improved sleep quality and reduced anxiety symptoms |
| Gold et al., 2014 | Exploratory randomized control trial | 113 | N/A | Music therapy for half the participants; variable length of treatment | d = 0.33 | Reduction in anxiety within-group. No change in depression or social relationship satisfaction. |
Theoretical Review
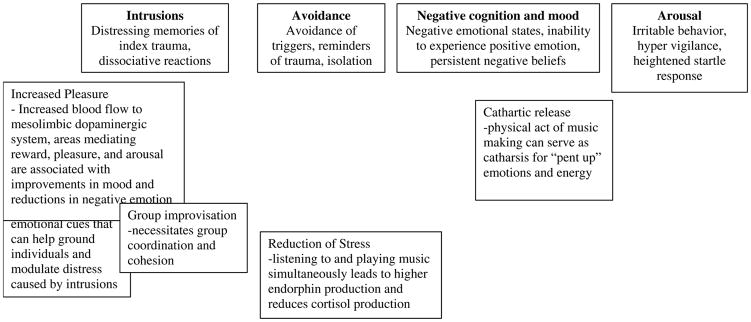
Figure 1 offers a theoretical conceptualization of how key mechanisms of music therapy apply to manifestations of DSM-5 PTSD symptom clusters and how these mechanisms can facilitate treatment of posttraumatic stress and promote functional recovery. Of note, Criterion A refers to the traumatic event itself, wherein the individual is exposed to death, the threat of death, serious injury or the threat of serious injury, and sexual violence or the threat or sexual violence (American Psychiatric Association, 2013).
Figure 1.
Mechanisms and processes of music therapy function to address the four PTSD symptom clusters: intrusions, avoidance, negative alterations in cognition and mood, and arousal and reactivity. Specifically, mechanisms and processes of music therapy work synergistically to capitalize on the many ways music can exercise a positive psychological and physiological impact on individual wellbeing.
Symptom Cluster B: Intrusions
Symptom cluster B is characterized by distressing memories of the index trauma, nightmares, dissociative reactions such as flashbacks, and intense psychological or physiological distress following exposure to cues associated with the index trauma. Music therapy has implications for addressing emotionally and physiologically distressing intrusions, given the unique connections between music and our experience of emotion (Juslin & Sloboda, 2001). Music may address emotion dysregulation associated with intrusive memories that leave individuals feeling triggered and distressed (Volkman, 1993). For instance, music can help ground someone in the present moment when faced with an intrusive or distressing reminder (Carr et al., 2011), and is commonly used a grounding technique in Dialectical Behavior Therapy, a therapeutic approach that specifically targets emotion dysregulation (Brantley, McKay, & Wood, 2007).
Symptom Cluster C: Avoidance
Many individuals with posttraumatic stress go to great lengths to avoid distressing memories, thoughts, feelings, or cues associated with their index trauma (APA, 2013). Avoidance of these reminders can exert dramatic negative impacts on an individuals’ social and emotional wellbeing. Group music making, accessed via group music therapy, can serve as a stand-in social process to address avoidant behavior and provide positive corrective experiences. Through group music making and group music therapy, individuals must coordinate so the music is cohesive, fostering connectivity (Gregory, 1997) and work collaboratively with others, particularly if the group uses musical improvisation, which demands active engagement (Orth & Verburgt, 1998; Volkman, 1993). Ultimately, group music therapy can allow patients to increase their social engagement in a safe space. The intended effect is to help patients, in-vivo, become comfortable with social experiences until they can eventually rejoin their community in a functional way (Carr et al., 2011; Bensimon et al., 2008).
Group music therapy outlets have been theorized to help individuals experiencing posttraumatic stress to connect with others and reduce detachment and isolation (Pavlicevic, 1999). Among low-income youth populations, where social or emotional problems linked to chronic and traumatic stress are common (Veenema, 2001), group music making serves as a non-verbal activity that can lead to significant improvements in social and emotional health (Ho, Tsao, Bloch, & Zeltzer, 2010). Further, veterans with PTSD who completed music therapy reported greater feelings of connectivity and empathy, noting they felt closer with members of their community whom they had previously avoided (Bensimon et al., 2008).
Symptom Cluster D: Negative Alterations in Cognition and Mood
Symptom cluster D encompasses a wide range of symptoms, including but not limited to persistent negative emotional states, an inability to experience positive emotions, feelings of detachment or alienation from others, and persistent and exaggerated negative beliefs about oneself and the world. Many mechanisms that operate in music therapy (e.g. communal music making, listening to music, playing an instrument) have been shown to have positive effects on symptoms associated with this cluster.
Music can shape how an individual emotionally experiences and interprets a moment or event. In a study by Boltz (2001), participants were presented with three ambiguous film clips accompanied by pre-determined positive, negative, or neutral music. Immediately after viewing the clips, subjects were asked to extrapolate the film’s ending and evaluate the different traits and motivations of the characters. The results revealed that relative to the control group (who heard no music), music influenced the subjects’ interpretation and memory of the film in a mood congruent fashion. Such findings suggest that music is deeply connected to our emotional processing and might serve as a potential avenue for patients to access their feelings.
Emotional responses to music correlate with physiological functioning, a response that has been measured by changes in the sympathetic (Iwanaga & Tsukamoto, 1997) and parasympathetic nervous systems (Krumhansl, 1997), and by changes in neural activity (Panksepp, 1997). Studies have also shown that music activates changes in the mesolimbic dopaminergic system, an area of the brain that mediates the experience of pleasure, reward, and arousal (Goldstein, 1980; Swanson, 1982; Wise, 2004). Indeed, fMRI neuroimaging studies have found that music increases the cerebral blood flow to areas of the brain associated with reward and reinforcement of pleasurable behaviors (e.g., nucleus accumbens and ventral tegmental area; Goldstein, 1980; Menon & Levitin, 2005; Swanson, 1982; Wise, 2004).
Accordingly, negative feelings such as anger, guilt, shame, fear, and anxiety may be addressed by music’s ability to activate reward pathways in the brain and suppress the release of stress hormones (Chanda & Levitin, 2013; Cepeda, 2006, Thayer & Levenson, 1983). Music may also help those with anhedonia or muted emotional experiences, as it can access neural pathways to emotion previously down-regulated in response to the index trauma (DeNora, 2002; Saarikallio & Erkkila, 2007).
Music can increase the release of endorphins to the brain, boosting positive feelings while reducing fear, self-awareness, and sadness, improving one’s overall emotional state (Chanda & Levitin, 2013; McNeil, 1995). The sense of community and group cohesion fostered in group music therapy can reduce feelings of isolation and estrangement (McNeil, 1995). Indeed, while threat of social rejection has been shown to activate neural “alarms” (e.g. the amygdala), cues that indicate safety, group care, integration, and support activate areas of the brain affiliated with reward (e.g. ventromedial prefrontal cortex and posterior cingulate cortex) and increase the production of stress reducing hormones (e.g. oxytocin and endogenous opioids; Eisenberger & Cole, 2012). Studies have also shown that engagement with music is correlated with increased self-esteem and the reduction of feelings of worthlessness, particularly in younger populations (Haines, 1989).
Symptom Cluster E: Arousal and Reactivity
Manifestations of symptoms in Cluster E can include irritable behavior and difficulty with anger management, recklessness, hypervigilance, exaggerated startle responses, problems concentrating, and difficulty sleeping. Individuals who have participated in drumming therapy reported that the physicality of drumming alleviated anger, frustration, and the negative abundance of energy that is characteristic of posttraumatic stress (Bensimon et al., 2008), while others reported that the action of hitting a drum was a cathartic release (Carr et al., 2011). Intensive drumming allows for release of physical energy and can serve as a constructive vent for emotions linked to arousal such as rage, sadness, anger, guilt, or frustration. At the end of a therapy session in which this aggression is expressed, individuals often reported feeling calmer and had greater ease reconnecting with others (Bensimon et al., 2008; Carr et al., 2011). Finally, listening to and playing music have also been shown to reduce the production of the stress hormone cortisol (Swanson, 1982; Wise, 2004).
Examination of Empirical Studies
Only four empirical studies examining the role of music therapy in the treatment of PTSD were identified using the literature review methods described in the methods section. Of these four studies, only one randomized-controlled trial among adults has directly examined music therapy using PTSD-specific symptom outcome measures. Carr et al., (2011) recruited 17 patients with PTSD from a specialized clinic that provided Trauma-Focused CBT. Patients discharging from the clinic with persistent levels of posttraumatic stress, as measured by the Impact of Events Scale (Horowitz, Wilner, & Alvarez, 1979), were recruited to participate in the study. Of those eligible, half were randomly assigned to receive an additional ten weeks of music therapy consisting of one, one-hour session of group improvisational instrumental therapy provided weekly. The control group was not offered music therapy or any other intervention. Compared to the control group, patients in the music therapy condition demonstrated a significantly greater reduction in posttraumatic stress symptoms as evidenced by their total IES score upon treatment completion (Carr et al., 2011).
Hernandez-Ruiz (2005) examined targeted symptoms of PTSD (e.g. poor sleep and anxiety) as well as common symptomatic correlates (i.e. depression) among a sample of twenty-eight abused women in a domestic violence shelter. Participants were randomly assigned to receive a music therapy treatment or no therapeutic intervention while in the shelter. Over five consecutive days, both the control and experimental group regularly completed surveys measuring their anxiety, sleep quality, and depression. The experimental group received a music therapy treatment, which consisted of a musical recording coupled with a progressive muscle-relaxation script. Results indicated that the music therapy group showed a greater pre-post reduction in anxiety (State-Trait Anxiety Inventory (STAI); Spielberger, 2010), and significantly improved sleep quality (Pittsburgh Sleep Quality Index; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). No differences in depression were reported.
Another randomized controlled trial examined the effects of music therapy on symptoms of PTSD including anxiety, depression, and social relationship satisfaction among prison inmates (Gold et al., 2014). One hundred and thirteen inmates were randomly assigned standard therapeutic treatment or group music therapy (e.g. playing in bands, instrumental tuition, recording music, music improvisation, songwriting) two to three times a week for at least two weeks and up to ten weeks or until the inmate was released from the prison. Self-report measures were used to assess symptoms of anxiety (STAI), depression (Hospital Anxiety and Depression Scale; Zigmond & Snaith, 1983), and social relationship satisfaction (Quality of Life Enjoyment and Satisfaction Questionnaire; Endicott, Nee, Harrison, & Blumenthal, 1993). Variable inmate discharge dates and scheduling limitations of the prison meant that the only viable results from this experiment came from post hoc tests of within-group changes from baseline to 2 weeks in the music therapy group. Inmates in the music therapy group demonstrated significant with-in group reductions in anxiety (Gold et al., 2014). No significant changes were noted for depression or social relationship satisfaction.
A non-controlled pre-post examination of music therapy for military veterans with PTSD looked at the efficacy of group drumming therapy (Bensimon et al., 2008). The sample included six male subjects aged 20–23 who had experienced traumatic events during military service and had a diagnosis of PTSD. They participated in group drumming music therapy for 16 weekly 90-minute sessions. The researchers measured the changes in the group dynamic by conducting content analysis from recordings of qualitative interviews (Fetterman, 1989) and peer debriefing sessions (Lincoln & Guba, 1985). Additional therapist observations indicated a significant reduction of specific symptoms including isolation, lack of connectedness, avoidance of traumatic memories, rage, and anxiety (Bensimon et al., 2008).
The research design and methodology employed in these studies face several limitations. The first two studies (Carr et al., & Hernandez-Ruiz, 2005), compared music therapy to no treatment (i.e., treatment as usual – receiving standard care and services) rather than a 3rd, alternative treatment. One possibility is that the additional treatment and contact with staff afforded by being in the experimental, music therapy conditions improved outcomes rather than music therapy itself. The latter two studies (Bensimon et al., 2008; Gold et al., 2014) employed a within-subjects design which yielded evidence of feasibility and offered a “proof of concept” for using music therapy for PTSD, but were not methodologically rigorous enough to draw definitive conclusions.
In conclusion, music therapy touches multiple symptomatic clusters that present in patients with trauma and PTSD. Given the current body of evidence, it appears that it might be best suited to addressing symptom cluster D, that of negative affect and mood alterations. However, it would be beneficial to see future studies focus on the impact of music therapy for specifically addressing arousal, intrusions, and avoidance, since little available evidence, both in the theoretical review and empirical research presented here, supports the use of music therapy for addressing these symptom clusters directly. Further PTSD is a highly heterogeneous condition (Hodge et al., 2016), and by one report, there are 636,120 possible ways to have or meet criteria for DSM-5 PTSD (20 symptoms across 4 symptom clusters; Galatzer-Levy & Bryant, 2013). Accordingly, additional study is required to determine how different subtypes of PTSD (e.g., complex trauma) might respond to music therapy.
Discussion
Examination of the extant literature yielded theoretical evidence and scant yet compelling empirical evidence to suggest that music, when employed as a therapeutic tool via music therapy, may address and reduce prominent symptoms of posttraumatic stress, including emotionally-dysregulating intrusions, avoidance, negative alterations in mood, and arousal and high reactivity. However, with only four known methodologically sound studies among adults, further empirical study is required before music therapy can be included among the canon of evidence-based treatments for posttraumatic stress. Specifically, extant studies compared music therapy to treatment as usual (i.e., did not have active control conditions) and thus limits the extent to which music therapy can be determined effective.
Music Therapy, Resilience, Posttraumatic Growth, and Treatment Process
Resilience has been defined as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of threat” (American Psychological Association, 2013). Music therapy may be considered a resilience-enhancing intervention as it can help trauma-exposed individuals harness their ability to recover elements of normality in their life following great adversity.
Resilience is related to posttraumatic growth (i.e., the experience of positive change after enduring a traumatic event; Tedeschi & Calhoun, 2004), and is cultivated through processes that reduce stress and fear, increase self-confidence, and foster social support (Southwick, Pietrzack, Tsai, & Krystal, 2015). These mechanisms are also addressed by music therapy (Goldstein, 1980; Bonde & Wigram, 2002; Thomas et al., 2010). As discussed in this review, music has been shown to reduce cortisol levels and subjective reports of stress (Chanda & Levitin, 2013; Cepeda, 2006, Thayer & Levenson, 1983), increase dopamine release (Goldstein, 1980; Swanson, 1982; Wise, 2004), and foster connectedness to one’s community (Gregory, 1997), all of which can directly combat many symptoms present among individuals with posttraumatic stress. Both music therapy and resilience-enhancing interventions (e.g. mindfulness training, positive cognitive reappraisal; Southwick et al., 2015) address many of the same symptoms and utilize the same mechanisms for recovery, suggesting important links between treatments that might support music therapy’s efficacy in addressing PTSD symptoms.
Areas for Future Research
Several questions remain that warrant further study. In studies examining music therapy for symptoms of posttraumatic stress, dosing parameters varied widely. To better understand how to utilize music therapy, clinicians will need more information about the frequency and duration of music therapy required for an optimal response. There is also little understanding of which elements of music therapy interventions are critical for their effectiveness. For instance, do group musical activities confer more benefits than solitary ones? Do certain personality traits or symptom presentations benefit more from group musical activities? Do more active musical activities (e.g., drumming, song writing) confer benefits that are superior to physically passive activities (e.g., music listening)?
Researchers should further examine how music therapy functions as both an adjunctive and standalone treatment. It would be useful to know if music therapy has greater effects on reducing symptoms of PTSD if it is applied in conjunction with existing evidence-based treatments, or if it is sufficient as a treatment on its own. Future research could examine the impact of music therapy as a standalone intervention when access to mental health care may be limited or significant barriers to care are present (e.g., stigma, costs, accessibility, disability). Specifically, music therapy may help engage individuals in therapeutic settings who might otherwise be unwilling to seek traditional talk-therapies.
Another notable challenge to pursuing further study is the difficulty identifying the impact of music therapy across a wide range of clinical subpopulations that experience posttraumatic stress (e.g. veterans, refugees, prisoners, children, victims of war, victims of abuse, etc.). Additional lines of inquiry should examine the impact of music therapy on posttraumatic stress as a function of key individual differences, including but not limited to age, gender, index trauma (e.g. sexual, combat, terrorism, natural disaster), complex or isolated trauma, socioeconomic background, and existing musical ability or training. For instance, individuals with high music ability may become frustrated and increasing self-critical in the music therapy experience. Future studies might also consider use of neuroimaging technologies to determine areas of the brain most directly impacted by music therapy, which could in turn, lend support to its use in addressing specific symptomatic clusters of PTSD (e.g., down-regulation of the corticolimbic system). A logical future research initiative might also explore how music therapy’s impact varies across different clinical subpopulations and determine recommendations for whom, when, and how can it be most effective. Additionally, the wide range of methods through which music therapy is employed (active engagement, receptive listening, instruments versus vocalization, etc.) warrants deeper examination regarding efficacy for different clinical subgroups.
PTSD is a highly comorbid condition and affected individuals are at dramatically increased risk for co-occurring anxiety and substance use disorders (Kessler et al., 2005). Future research should examine how music therapy can improve mental health outcomes more generally for high-risk populations that experience anxiety, substance use disorders, and other challenging conditions (e.g., homelessness) in addition to posttraumatic stress. Application of music therapy for the transdiagnostic treatment of psychological disorders with connections to posttraumatic stress would highlight whether it could address symptoms present in other common co-occurring conditions.
Practical Clinical Recommendations
In the United States, at the time of writing, music therapy is considered a reimbursable service under Medicare; private insurances may also cover the costs. Prices vary widely for music therapists working independently, but the costs may be mitigated if the music therapist is employed by a mental health clinic, hospital, or community health organization that offers comprehensive care that includes music therapy (AMTA).
A music therapist must have a bachelor’s or master’s degree in music therapy, 1200 hours of clinical training, be certified by the Certification Board of Music Therapists (a national certification) and may also need additional licenses as required by a state to practice psychotherapy (Office of the Professions; AMTA). A music therapist is trained to assess their clients’ needs and tailor each therapeutic experience to those needs.
Clinicians who wish to integrate music therapy into their patient’s treatment plan are encouraged to explore the resources in Appendix A. If a clinician decides to pursue music therapy for their patient, they must refer that patient to a board-certified music therapist. They may do this by contacting the AMTA National Office to request a list of referrals or looking through their online directory.
While the use of music therapy requires a licensed music therapist to administer it, clinicians need not be music therapists to augment care with music. Playing music during therapy or encouraging the patient to develop a playlist of soothing music could utilize music without being considered formal music therapy. It is recommended that clinicians who wish to incorporate music into treatment possess a basic knowledge of the physiological and psychological impact of music and consistently solicit feedback from patients in a collaborative manner. Clinicians can also consult with music therapists regarding how they might incorporate music into their practices with individual patients. Further, some individuals may not consider themselves musical, and lack interest or confidence which may influence the extent to which they benefit from the approach. Understanding individual and contextual factors that may influence a patient’s experience of music can help clinicians make more appropriately targeted referrals to music therapists as well.
Conclusion
Individuals who experience symptoms of PTSD could gain from further research into music therapy as a treatment option to improve functioning and foster resilience. Increased knowledge about the direct impact of music therapy on PTSD symptoms could also increase the number of tools available to clinicians who aim to offer better holistic care. It is our hope that this review will inspire further study and eventually afford music therapy a place within clinicians’ repertoires of available evidence-based treatment options for PTSD.
Supplementary Material
Acknowledgments
Support for this research was provided in part by a VA Rehabilitation Research and Development (RR&D) Career Development Award – 2 granted to Dr. Heinz.
References
- American Music Therapy Association (1983–2013) History of music therapy. 2015 Mar; Retrieved from http://www.musictherapy.org/about/history/
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- Bensimon M, Amir D, Wolf Y. Drumming through trauma: Music therapy with post-traumatic soldiers. The Arts in Psychotherapy. 2008;35:34–48. [Google Scholar]
- Boltz M. Musical soundtracks as a schematic influence on the cognitive processing of filmed events. Music Perception: An Interdisciplinary Journal. 2001;18(4):427–454. [Google Scholar]
- Bonde LO, Wigram T. A comprehensive guide to music therapy: Theory, clinical practice, research, and training. London, England: Jessica Kingsley Publishers; 2002. [Google Scholar]
- Brantley J, McKay M, Wood J. The dialectical behavior therapy skills workbook: Practical DBT exercises for learning mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. 1. Oakland, CA: New Harbinger; 2007. [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu CF, Yano EM, Kirchner JE, Chan D, Chaney EF. Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine. 2007;22(6):711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr C, d’Ardenne P, Sloboda A, Scott C, Wang D, Priebe S. Group music therapy for patients with persistent post-traumatic stress disorder—an exploratory randomized controlled trial with mixed methods evaluation. Psychology and Psychotherapy: Theory, Research, and Practice, The British Psychological Society. 2011:1–24. doi: 10.1111/j.2044-8341.2011.02026.x. [DOI] [PubMed] [Google Scholar]
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews. 2006;19(2) doi: 10.1002/14651858.CD004843.pub2. [DOI] [PubMed] [Google Scholar]
- Chanda ML, Levitin DJ. The neurochemistry of music. Trends in Cognitive Sciences. 2013;17(4):179–193. doi: 10.1016/j.tics.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Kliethermes M, Murray LA. Trauma focused CBT for youth with complex trauma. Child Abuse and Neglect. 2012;36(6):528–541. doi: 10.1016/j.chiabu.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross I. The nature of music and its evolution. In: Hallam S, Cross I, Thaut M, editors. The oxford handbook of music psychology. New York, NY: Oxford University Press; 2009. pp. 3–14. [Google Scholar]
- Crowe B. Music therapy for children, adolescents, and adults with mental disorders. Silver Spring, MD: American Music Therapy Association; 2007. pp. 204–205. [Google Scholar]
- Davis WB, Gfeller KE, Thaut MH. An introduction to music therapy: Theory and practice. Silver Spring, MD: American Music Therapy Association; 2008. [Google Scholar]
- Disanayake E. Root, leaf, blossom, or bole: Concerning the origin and adaptive function of music. In: Stephen M, Colwyn T, editors. Communicative Musicality. Oxford: Oxford University Press; 2009. pp. 17–30. [Google Scholar]
- Darwin C. On the origin of species by means of natural selection, or, the preservation of favoured races in the struggle for life. London, England: John Murray, Albemarle Street; 1859. [Google Scholar]
- DeNora T. Vaillancourt, Guylaine (2012). Music therapy; A community approach to social justice. The Arts in Psychotherapy. 2002;39(3):173–178. [Google Scholar]
- Eisenberger NI, Cole SW. Social neuroscience and health: neurophysiological mechanisms linking social ties with physical health. Nature Neuroscience. 2012;15(5) doi: 10.1038/nn.3086. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: A new measure. Psychopharmacological Bulletin. 1993;29(2):321–326. [PubMed] [Google Scholar]
- Erkkila J, Punkanen M, Fachner J, Ala-Ruona E, Pontio I, Tervaniemi M, et al. Individual music therapy for depression: randomized controlled trial. The British Journal of Psychiatry. 2011;199(2):132–139. doi: 10.1192/bjp.bp.110.085431. [DOI] [PubMed] [Google Scholar]
- Fetterman DM, editor. Ethnography: Step-by-step. Vol. 17. New York, NY: Sage Publications; 2010. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67(2):194. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Garrido S, Baker FA, Davidson JW, Moore G, Wasserman S. Music and trauma: the relationship between music, personality, and coping style. Frontiers in Psychology. 2015;6 doi: 10.3389/fpsyg.2015.00977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Bryant RA. 636,120 Ways to Have Posttraumatic Stress Disorder. Perspectives on Psychological Science. 2013;8:651–662. doi: 10.1177/1745691613504115. [DOI] [PubMed] [Google Scholar]
- Gregory AH. The roles of music in society: The ethnomusicological perspective. In: Hargreaves David J, North Adrian C., editors. The social psychology of music. New York, NY, US: Oxford University Press; 1997. pp. 123–140. [Google Scholar]
- Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: An affective science perspective. Clinical Psychological Science. 2014;2(4):387–401. [Google Scholar]
- Gold C, Assmus J, Hjornevik K, Qvale G, Brown F, Hansen A, Waage L, Stige B. Music therapy for prisoners: Pilot randomized controlled trial and implications for evaluating psychosocial interventions. International Journal of Offender Therapy and Comparative Criminology. 2014;58(12):1520–1539. doi: 10.1177/0306624X13498693. [DOI] [PubMed] [Google Scholar]
- Gold C, Voracek M, Wigram T. Effects of music therapy for children and adolescents with psychopathology: a meta-analysis. Journal of Child Psychiatry. 2004;45(6):1054–1063. doi: 10.1111/j.1469-7610.2004.t01-1-00298.x. [DOI] [PubMed] [Google Scholar]
- Goldstein A. Thrills in response to music and other stimuli. Physiological Psychology. 1980;8:171–207. [Google Scholar]
- Guetin S, Portet F, Picot MC, Pommié C, Messaoudi M, Djabelkir L, et al. Effect of music therapy on anxiety and depression in patients with Alzheimer’s type dementia: Randomized, controlled study. Dementia and Geriatric Cognitive Disorders. 2009;28:36–46. doi: 10.1159/000229024. [DOI] [PubMed] [Google Scholar]
- Haines JH. The effects of music therapy on the self-esteem of emotionally-disturbed adolescents. Music Therapy. 1989;8(1):78–91. [Google Scholar]
- Heidenreich V. Music therapy in war-affected areas. Intervention. 2005;3:129–134. [Google Scholar]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowalski J, Tu X. Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress. 2003;16(6):555–562. doi: 10.1023/B:JOTS.0000004078.93012.7d. [DOI] [PubMed] [Google Scholar]
- Hernández-Ruiz E. Effect of music therapy on the anxiety levels and sleep patterns of abused women in shelters. Journal of Music Therapy. 2005;42(2):140–158. doi: 10.1093/jmt/42.2.140. [DOI] [PubMed] [Google Scholar]
- Ho P, Tsao JC, Bloch L, Zeltzer LK. The impact of group drumming on social-emotional behavior in low-income children. Evidence-Based Complementary and Alternative Medicine. 2011 doi: 10.1093/ecam/neq072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodge CW, Yehuda R, Castro CA, McFarlane AC, Vermetten E, Jetly R, et al. Unintended consequences of changing the definition of posttraumatic stress disorder in DSM-5: Critique and call for action. Jama Psychiatry. 2016;73(7):750–752. doi: 10.1001/jamapsychiatry.2016.0647. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosomatic medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hurt-Thaut C. Clinical practices in music therapy. In: Hallam S, Cross I, Thaut M, editors. The Oxford Handbook of Music Psychology. New York, NY: Oxford University Press; 2009. [Google Scholar]
- Iwanaga M, Tsukamoto M. Effects of excitative and sedative music on subjective and physiological relaxation. Perception and Motor Skills. 1997;85(1):287–296. doi: 10.2466/pms.1997.85.1.287. [DOI] [PubMed] [Google Scholar]
- Juslin PN, Sloboda JA. Music and emotion: Theory and research. New York, NY: Oxford University Press; 2001. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koelsch S. A neuroscientific perspective on music therapy. Annals of the New York Academy of Sciences. 2009;1169(1):374–384. doi: 10.1111/j.1749-6632.2009.04592.x. [DOI] [PubMed] [Google Scholar]
- Krumhansl CL. An exploratory study of musical emotions and psychophysiology. Canadian Journal of Experimental Psychology. 1997;51:336–352. doi: 10.1037/1196-1961.51.4.336. [DOI] [PubMed] [Google Scholar]
- Lincoln YS, Guba EG. Naturalistic inquiry. Vol. 75. New York, NY: Sage; 1985. [Google Scholar]
- Maack C, Nolan P. The effects of guided imagery and music therapy on reported change in normal adults. Journal of Music Therapy. 1999;36(1):39–55. doi: 10.1093/jmt/36.1.39. [DOI] [PubMed] [Google Scholar]
- Macintosh HB. Sounds of healing: Music in group work with survivors of sexual abuse. The Arts in Psychotherapy. 2003;30:17–23. [Google Scholar]
- Menon V, Levitin DJ. The rewards of music listening: response and physiological connectivity of the mesolimbic system. Neuroimage. 2005;28(1):175–184. doi: 10.1016/j.neuroimage.2005.05.053. [DOI] [PubMed] [Google Scholar]
- McDermott J, Hauser M. The origins of music: Innateness, uniqueness, and evolution. Music Perception: An Interdisciplinary Journal. 2005;23(1):29–59. [Google Scholar]
- McNeil WH. Keeping together in time: Dance and drill in human history. Cambridge, MA: Harvard University Press; 1995. [Google Scholar]
- Orth J, Verburgt J. Arts Therapists, Refugees, and Migrants: Reaching Across Borders. 1998. One Step Beyond; p. 80. [Google Scholar]
- Orth J. Between abandoning and control: Structure, security and expression in music therapy with traumatized refugees in a psychiatric clinic. In: Verwey M, editor. Trauma and empowerment. Berlin: VWB, Verlag fur Wissandschaft und Bildung; 2001. pp. 189–197. [Google Scholar]
- Panksepp J. The affective cerebral consequence of music: Happy vs sad effects on the EEG and clinical implications. International Journal of Arts Medicine. 1997;5(1):18–27. [Google Scholar]
- Pavlicevic M. Music therapy improvisation groups with adults: Towards de-stressing in South Africa. South African Journal of Psychology. 1999;29(2):94–99. [Google Scholar]
- Pitman RK, Orr SP, Altman B, Longpre RE, Poiré RE, Macklin ML. Emotional processing during eye movement desensitization and reprocessing therapy of Vietnam veterans with chronic posttraumatic stress disorder. Comprehensive psychiatry. 1996;37(6):419–429. doi: 10.1016/s0010-440x(96)90025-5. [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy: Veteran/military version: Therapist and patient materials manual. Washington, DC: Department of Veterans Affairs; 2014. [Google Scholar]
- Rentfrow PJ, Gosling SD. The do re mi’s of everyday life: The structure and personality correlates of music preferences. Journal of Personality and Social Psychology. 2003;84:1236–1256. doi: 10.1037/0022-3514.84.6.1236. [DOI] [PubMed] [Google Scholar]
- Saarikallio S, Erkkila J. The role of music in adolescents’ mood regulation. Psychology of Music. 2007;35(1):88–109. [Google Scholar]
- Sacks O. Musicophilia. New York, NY: Vintage Books; 2007. [Google Scholar]
- Schubert S, Lee CW. Adult PTSD and its treatment with EMDR: A review of controversies, evidence, and theoretical knowledge. Journal of EMDR Practice and Research. 2009;3(3):117–132. [Google Scholar]
- Spielberger CD. State-Trait anxiety inventory. Hoboken, NJ: John Wiley & Sons, Inc; 2010. [Google Scholar]
- Southwick SM, Pietrzack R, Tsai J, Krystal JH. Resilience: an update. PTSD Research Quarterly. 2015;25(4):1–10. [Google Scholar]
- Svansdottir HB, Snaedal J. Music therapy in moderate and severe demential of Alzheimer’s type: a case-control study. International Psychogeriatrics. 2006;18(4):613–621. doi: 10.1017/S1041610206003206. [DOI] [PubMed] [Google Scholar]
- Swanson LW. The projections of the ventral tegmental area and the adjacent regions: a combined fluorescent retrograde tracer and immunofluorescence study in the rat. Brain Research Bulletin. 1982;9:321–353. doi: 10.1016/0361-9230(82)90145-9. [DOI] [PubMed] [Google Scholar]
- Romo R, Gifford L. A cost-benefit analysis of music therapy in a home hospice. Nursing Economics. 2007;25(6):353. [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological inquiry. 2004;15(1):1–18. [Google Scholar]
- Thayer JF, Levenson RW. Effects of music on psychophysiological responses to a stressful film. Psychomusicology. 1983;3:44–52. [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functioning impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry. 2010;67(6):614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- Thompson WF. The Origins of Music. In: Thompson WF, editor. Music, thought, and feeling: Understanding the psychology of music. New York, NY: Oxford University Press; 2008. [Google Scholar]
- Van der Kolk B. The body keeps the score: Brain, mind, body, and the healing of trauma. New York, NY, US: Penguin Books; 2014. [Google Scholar]
- Van Westrhenen N, Fritz E. Creative arts therapy as treatment for child trauma: An overview. The Arts in Psychotherapy. 2014;41(5):527–534. [Google Scholar]
- Veenema TG. Children’s exposure to community violence. Journal of Nursing Scholarship. 2001;33(2):167–173. doi: 10.1111/j.1547-5069.2001.00167.x. [DOI] [PubMed] [Google Scholar]
- Voigt M. Orff music therapy: An overview. Voices: A World Forum for Music Therapy. 2003;3(3) doi: 10.15845/voices.v313.134. [DOI] [Google Scholar]
- Volkman S. Music therapy and the treatment of trauma-induced dissociative disorders. The Arts in Psychotherapy. 1993;20(3):243–251. [Google Scholar]
- Wise RA. Dopamine, learning and motivation. Nature Reviews Neuroscience. 2004;5:483–494. doi: 10.1038/nrn1406. [DOI] [PubMed] [Google Scholar]
- Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. Journal of Traumatic Stress. 2004;17(1):69–73. doi: 10.1023/B:JOTS.0000014679.31799.e7. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta psychiatrica Scandinavia. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.