Abstract
Objective
To investigate whether a novel, task-specific training intervention that focused on correcting pain-producing movement patterns was feasible and whether it would improve hip and knee kinematics, pain, and function in women with patellofemoral pain.
Design
Prospective, non-randomized, within-group, double baseline, feasibility intervention study.
Subjects
Twenty-five women with patellofemoral pain were enrolled.
Intervention
The intervention, delivered 2×/week for 6 weeks, consisted of supervised, high-repetition practice of daily weight-bearing and recreational activities. Activities were selected and progressed based on participants’ interest and ability to maintain optimal alignment without increasing pain.
Main measures
Primary feasibility outcomes were recruitment, retention, adherence, and treatment credibility (Credibility/Expectancy Questionnaire). Secondary outcomes assessing intervention effects were hip and knee kinematics, pain (visual analog scale: current, average in past week, maximum in past week), and function (Patient-Specific Functional Scale).
Results
Twenty-five participants were recruited and 23 were retained (92% retention). Self-reported average daily adherence was 79% and participants were able to perform their prescribed home program correctly (reduced hip and knee frontal plane angles) by the second intervention visit. On average, treatment credibility was rated 25 (out of 27) and expectancy was rated 22 (out of 27). Hip and knee kinematics, pain, and function improved following the intervention when compared to the control phase.
Conclusions
Based on the feasibility outcomes and preliminary intervention effects, this task-specific training intervention warrants further investigation and should be evaluated in a larger, randomized clinical trial.
Keywords: anterior knee pain, kinematics, physical therapy, gait retraining
Introduction
Chronic patellofemoral joint pain (pain around the knee cap; patellofemoral pain) is a common, persistent,[1] and potentially debilitating musculoskeletal pain condition, affecting women to a greater extent than men.[2, 3] One proposed contributing factor is a movement pattern termed “dynamic knee valgus” (inward movement of the knee during weight bearing).[4] Characterized by increased hip adduction, hip medial rotation and knee lateral rotation, dynamic knee valgus theoretically increases patellofemoral joint stress, which over time results in tissue injury and pain.
Interventions aimed at reducing dynamic knee valgus typically address impairments thought to contribute to the movement pattern, specifically decreased hip abductor and external rotator muscle strength. Most hip muscle strengthening programs incorporate weight-bearing exercises that are described as “functional”,[5, 6, 7, 8, 9] however, movement typically is not addressed as an outcome measure or as a guiding principle of the intervention. Findings from previous studies demonstrating that joint kinematics were improved during a single limb squat after only a few minutes of movement instruction[10] and during running after a “gait retraining” intervention[11, 12] suggest that training to correct pain-producing movement patterns, in the absence of specific muscle strengthening, may be beneficial. Furthermore, training in tasks that are important to an individual may enhance motivation and adherence.[13]
Task-specific training is a well-supported motor learning concept that has resulted in improved outcomes in people with chronic hemiparesis post stroke,[14] and task-specific training that focuses on correcting pain-producing posture and movement patterns (task-specific movement training) is currently being evaluated for efficacy in people with low back pain (ClinicalTrials.gov #NCT02027623).
The critical next step is to determine whether task-specific movement training as a stand-alone intervention can be accomplished and whether participants with patellofemoral pain will find the intervention credible and adhere to the program. Typical physical therapy intervention programs for treatment of patients with patellofemoral pain involve a multimodal approach.[15] As such, a program that focuses solely on training optimal movement across daily tasks may be viewed with skepticism. Also unknown is whether task-specific movement training will result in improvements in kinematics, pain and function.
The primary purpose of this study was to determine the feasibility of a task-specific movement training intervention for women who have patellofemoral pain and dynamic knee valgus. In addition, we tested whether the effects of the intervention on health-related outcomes of kinematics, pain, and function were greater than the effects due to the passage of time.
Methods
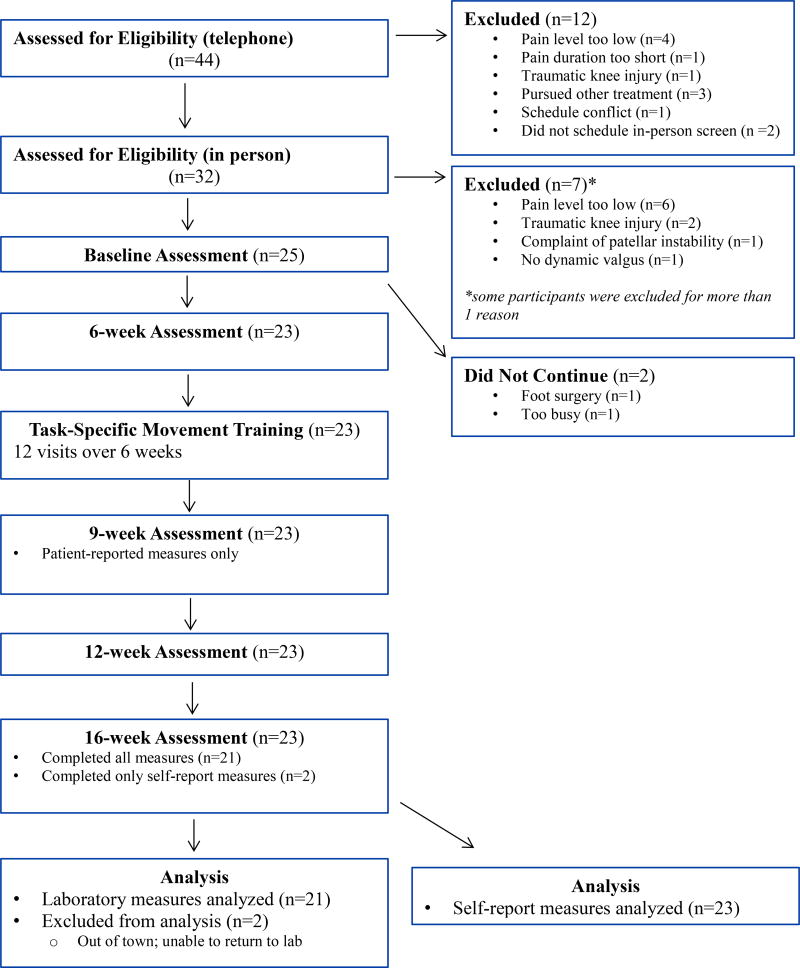
This study was approved by the Institutional Review Board at Saint Louis University (protocol #24433), and written informed consent was obtained from each participant. The study was a prospective, non-randomized, within-group, double-baseline, feasibility intervention study. Figure 1 depicts an overview of the study design.
Figure 1.
Study Flow Diagram
Female participants with chronic (> 2 months)[16] patellofemoral pain who were between the ages of 18 and 40 were recruited from the St. Louis metropolitan area through word-of-mouth referrals and through flyers posted in the community. Recruitment took place between October, 2014 and December, 2015.
Targeted enrollment was 25 participants. An a priori power analysis tested the null hypothesis that the mean changes in health-related outcomes from the control phase were equal to the mean changes during the intervention phase and were based on two-sided tests at the 0.05 level of significance. Standard deviations (SDs) were assumed to be similar to those reported in our preliminary data[10] (kinematics) and by Crossley et al[17] (pain). Assuming that 17 participants completed the study (allowing for a 30% dropout rate), the study would have power of 0.80 or above to detect clinically meaningful differences in change for the health-related outcomes of hip adduction (4.5°) and pain (2 points for visual analog scale).
To be included in the study, participants had to have pain originating from the patellofemoral articulation (behind or around the patella) that was rated (average daily pain) at least 3/10 on an 11-point numeric pain scale.[10] Pain had to be present during 2 of 3 provocation tests (resisted quadriceps contraction, single limb squat, step down). Participants also had to demonstrate observable dynamic knee valgus during a single limb squat test, defined according to previously published criteria,[10, 18] to be an appropriate candidate for the intervention.
Exclusion criteria were body mass index (BMI) greater than 30 kg/m2 (due to kinematic methodology), a history or current report of knee ligament, tendon or cartilage injury, patellar instability or dislocation, prior knee surgery, known pregnancy, and neurological involvement that would influence movement patterns.
Potential participants were screened by telephone for pain and demographic criteria, and eligible participants underwent a clinical screening examination by the principal investigator (a physical therapist with 27 years of experience) Palpation was performed to rule out pain originating from the patellar tendon, quadriceps tendon, tibiofemoral joint, meniscii, or synovial plicae. Participants completed a visual analog scale, a 100-mm line with a left anchor of “no pain” and a right anchor of “worst imaginable pain,” to confirm the presence of pain in response to the 3 provocation tests. For the visual assessment of dynamic knee valgus, participants performed approximately 5 trials of a single-limb squat on the involved (most painful) limb. If in the majority of trials the frontal plane knee angle (abduction) increased by 10° or more during the descent phase of the squat, the subject was classified as having “observable dynamic knee valgus.”[10, 18] Height and body mass data were obtained.
Assessments
Participants underwent full assessments at Baseline, 6 weeks (pre-intervention), 12 weeks (post-intervention), and 16 weeks. At each assessment, participants completed questionnaires to assess pain, function, and activity level.[19] To quantify movement patterns, 3-dimensional kinematic data and 2-dimensional video data were obtained while participants performed single limb squat, stair ascent, stair descent, sit to stand and stand to sit tasks. Additional measures included performance-based function, isometric hip muscle strength, and hip and ankle range of motion. At 9 weeks (mid-intervention), participants completed self-report measures of pain and function. Because the primary purpose of this study was to determine feasibility and preliminary effects of the intervention, only data from pre-planned primary and secondary outcome measures obtained at Baseline, 6 weeks, and 12 weeks are reported in this manuscript.
Intervention
The intervention, grounded in principals of motor skill learning,[20] consisted of supervised repetitive practice of functional daily tasks, with a focus on maintaining optimal limb alignment during movement.[21] A detailed description of the intervention is provided in the Appendix. One physical therapist, a certified orthopaedic clinical specialist with 24 years of experience, delivered the intervention in twelve 45 minute sessions (2×/week for 6 weeks).
At the first visit, the physical therapist followed a standardized script to introduce the intervention and inform participants of its rationale: that maintaining optimal alignment during daily activities could improve loading at the patellofemoral joint, and ultimately decrease pain. Participants were then instructed in key concepts of optimal movement: maintain a level pelvis (no contralateral hip drop), a level trunk (no side bending), and keep the knee over the second toe (no knee valgus/or medial rotation). Next, participants practiced moving optimally during several tasks, after which they completed a credibility/expectancy questionnaire[22] to assess their beliefs about the potential success of the intervention. At the beginning of the second intervention visit, to test whether participants understood and could demonstrate the key concepts, digital video recorded participants as they performed 3 trials of a single limb squat.
During each subsequent visit participants were trained in 4 common pain-provoking activities: single limb squats, double limb squats, standing up from/sitting down in a chair, and ascending/descending stairs. As the intervention progressed, participants were trained in 2–3 tasks specific to their sport, leisure or work activities (e.g. running, bicycling, jumping/cutting). These tasks were identified through the Patient-specific Functional Scale questionnaire[23] administered at Baseline, which asked participants to choose three meaningful activities that they have difficulty with or are unable to do because of their patellofemoral pain. Training for specific tasks was initiated once the common activities could be performed without increased pain while maintaining optimal alignment. During the intervention sessions, the number of repetitions for each task was not standardized; all participants practiced tasks for a given amount of time (~5–10 minutes each) based on their tolerance (symptoms and fatigue).
Feedback was tailored for each subject, starting with verbal cuing and progressing to visual (e.g. mirror) and tactile (e.g. therapist’s manual assistance) feedback when necessary. Feedback was not standardized across participants, as the goal was to achieve optimal alignment regardless of the method. As soon as the participant demonstrated correct performance of a task, feedback was decreased and participants were asked to assess their own performance.
Tasks were progressed when participants could maintain proper alignment without increasing pain (verbal numeric pain rating). Gradations of each task accommodated individual participant capabilities and allowed for task progression. Examples included increasing step height, squat depth, movement speed, and movement duration, as well as decreasing chair height and changing surface stability (see Appendix). During each session, the therapist documented the tasks, the time spent practicing each task, the grade of each task, and the feedback required. To monitor the tolerability of the intervention, the participant’s current pain level was assessed using a numeric pain rating scale at the beginning of each intervention session. Participants were instructed to report any increase in symptoms during execution of each task. If a task could not be performed at the given difficulty due to increased pain or incorrect movement, the task was downgraded.
As a home program, participants were instructed to incorporate optimal movement into all daily activities. In addition, they were instructed to complete five repetitions of 2–3 tasks each day as a way to reinforce the key concepts of optimal movement.
Participants completed a daily adherence log. For each day, participants indicated the percentage of the day they adhered to their home program as instructed (0–100%)[24] using a visual analog scale. The therapist collected the log at each intervention visit.
Because adherence to any intervention requires that patients 1) know what they are supposed to do, and 2) are able to execute the intervention as prescribed, at the beginning of each intervention session participants were asked to verbalize key concepts for correct performance of each task, after which they performed the task. Scoring for verbalization was “independent” (able to verbalize concepts without verbal cues) or “dependent” (requires verbal cues or demonstration of concept); scoring for performance was “independent”, “with verbal cues”, “with verbal cues and physical assist”, or “unable to perform.”[25]
To further document the participant’s independence in performing the activities, video images of a single limb squat obtained at the second intervention visit were compared to those from Baseline. On each image representing the deepest part of the squat, two dimensional hip and knee frontal plane projection angles were measured by an investigator blinded to the time point. The hip frontal plane projection angle is 90 minus the angle formed by a line connecting the anterior superior iliac spines of the pelvis and a line bisecting the femur. The knee frontal plane projection angle is 180 minus the angle formed by a line bisecting the femur and a line bisecting the tibia (Fig 2, Supplementary Data).[26] Increasing angles correspond to increasing dynamic knee valgus. The angle measurements were averaged across the 3 trials for each time point.
Primary Outcome (Feasibility) Measures
The outcome measures used to assess feasibility were 1) number of participants recruited (goal: n=25) and percent retained (goal: 70%), and 2) adherence to corrected movement patterns. The adherence goals were that participants would report an average daily adherence to the correct movement pattern of >75%, a value set slightly higher than published adherence ranges (55%–69%) for people with knee osteoarthritis,[27] and demonstrate improved movement performance (decreased frontal plane projection angles) during a single limb squat at the second intervention visit compared to Baseline. Treatment credibility was assessed using the Credibility-Expectancy questionnaire,[22] a 6-item Likert scale questionnaire with three items related to credibility (how logical I think the treatment is) and three items related to expectancy (the extent to which I expect the treatment to reduce symptoms). Items are on a 9-point scale except two of the expectancy items (11-point scale). Ratings from the 11-point items were transformed to a 9-point scale prior to analysis. Ratings on the 3 credibility items were summed to obtain a credibility score (possible range: 3 to 27); ratings on the 3 expectancy items were summed to obtain an expectancy score (possible range: 3 to 27).
Secondary Outcome (Preliminary Efficacy) Measures
Three-dimensional hip and knee kinematics were obtained during a single limb squat using an 8-camera, motion analysis system and previously established methods.[10, 28] Retro-reflective markers were placed on the pelvis and lower extremities to define a set of coordinate axes for each segment. Following marker placement, a static standing trial was captured followed by 3 trials of a single limb squat on the involved limb. Participants were allowed 2–3 practice trials to become accustomed to the task. The a priori kinematic variables of interest were the hip adduction angle, hip medial rotation angle, and knee lateral rotation angle at the time of peak knee flexion.
Current pain, average pain during the past week, and maximum pain during the past week were assessed using a visual analog scale. Function was assessed using the Patient-specific Functional Scale[29], a questionnaire that asked participants to choose 3 activities that they are unable to do or have difficulty doing because of their patellofemoral pain. Subjects rated their ability to perform the activity on a scale of 0 to 10, where 0 is unable to perform and 10 is able to perform without restriction.
Additional Outcome Measures
Additional measures that were obtained but were not part of the pre-planned statistical analysis, and thus are not reported in this manuscript, included hip and knee kinematics during stair ascent, stair descent, sit to stand, and stand to sit tasks, patient-reported function (Anterior Knee Pain Scale[30]), performance-based function (Y balance test[31], hexagon agility test[32]), isometric hip muscle strength (lateral rotators, gluteus medius, hip extensors), passive range of motion (hip medial rotation, hip lateral rotation, ankle dorsiflexion), and a clinical measure of femoral anteversion (Craig’s test[33]).
Statistical Analysis
Descriptive statistics were calculated for participant characteristics and feasibility outcome measures. Retention was calculated as the percentage of enrolled participants who completed the study. Self-report ratings of daily adherence for each participant were averaged across all days of the intervention phase. Adherence values were averaged across all participants. Hip and knee frontal plane projection angles during the single limb squat were compared between Baseline and the second intervention visit using a paired student’s t-test. Credibility and expectancy ratings were averaged across all participants.
Preliminary efficacy outcomes were compared across time points using a mixed linear model repeated measures analysis of variance with an autoregressive covariance structure. For each variable, an a priori statistical contrast tested whether the change during the intervention phase (6 weeks to 12-weeks) was equal to the change during the control phase (Baseline to 6 weeks). Visual analog scale data were rank-transformed prior to the analysis. Continuous data are represented as mean (SD).
Results
Participant characteristics are displayed in Table 1.
Table 1.
Participant Characteristics
| All Enrolled Participants (n=25) Mean (SD) |
Range (min-max) n=25 |
Participants Included in Analysis (n=23) Mean (SD) |
Range (min-max) n=23 |
|
|---|---|---|---|---|
| Age (years) | 21.7 (3.5) | 18 – 36 | 21.8 (3.7) | 18 – 36 |
| BMI (kg/m2) | 22.3 (2.1) | 17.5 – 26.6 | 22.2 (2.0) | 17.5 – 26.6 |
| Pain Duration (years) | 4.3 (3.5) | 0.5 – 11 | 4.1 (3.4) | 0.5 – 10 |
| Pain Level: average past week (NPRS) | 3.7 (1.0) | 2–6 | 3.7 (1.0) | 2–6 |
| Pain Level: maximum past week (NPRS) | 6.2 (1.0) | 3–8 | 6.2 (1.1) | 3–8 |
| Habitual Physical Activity: work index* | 2.3 (0.5) | 1.3 – 3.4 | 2.3 (0.5) | 1.3 – 3.4 |
| Habitual Physical Activity: sport index* | 2.8 (0.7) | 1.3 – 4.3 | 2.8 (0.6) | 1.5 – 4.3 |
| Habitual Physical Activity: leisure index* | 2.9 (0.5) | 2.0 – 4.0 | 2.9 (0.5) | 2.0 – 3.5 |
| Involved (tested) Side (n) | Left (11) Right (14) | Left (11) Right (12) | ||
| Bilateral Pain (n) | Bilateral (22) Unilateral (3) | Bilateral (20) Unilateral (3) | ||
| Frequency of Activities Limited by Pain# (n) | Running (19) Stairs (16) Squatting (12) Prolonged Sitting (10) | Running (18) Stairs (14) Squatting (12) Prolonged Sitting (9) | ||
| Previous Physical Therapy Treatment for Patellofemoral Pain (n) | 10 | 10 |
n = number of participants; SD = Standard Deviation; NPRS = numeric pain rating scale (0 = no pain, 10 = worst imaginable pain)
Habitual Physical Activity[19] (Range for each index: 1–5, where 1 = inactive and 5 = highly active)
Most frequently reported activities limited by pain, as noted on the Patient-specific Functional Scale[29]
Primary Outcomes (Feasibility)
Twenty-five participants were recruited and enrolled in the study. Twenty-three participants completed the study yielding a retention rate of 92% (Fig. 1). All 23 participants completed all 12 intervention visits. The average number of days for the intervention phase was 44.8 (6.3), and the average number of days for the control phase was 39.4 (6.6) (p<.001). Self-reported daily adherence to the home program was, on average, 78.6 (13.5) %. At the second intervention visit compared to Baseline, improvements were detected in the frontal plane projection angles of the hip (15.5 (7.0)° vs. 20.1 (5.1)°, p=.006) and knee (−2.3 (5.9)° vs. 7.6 (7.1)°, p<.001), demonstrating that participants were able to perform the intervention as prescribed. The average credibility score was 25.0 (2.2) (range: 19 to 27). The average expectancy score was 21.9 (3.9) (range: 11.6 to 27).
Secondary Outcomes (Preliminary Efficacy)
The change during the intervention phase was greater than the change during the control phase (Table 2) for hip adduction, hip medial rotation and knee lateral rotation during the single limb squat, with all kinematics improving following intervention.
Table 2.
Secondary Outcome Measures
| Baseline Mean (SD) (n = 23) |
6 weeks Mean (SD) (n = 23) |
12 weeks Mean (SD) (n = 23) |
Change: Baseline to 6 weeks (control phase) Mean (CI) |
Change: 6 weeks to 12 weeks (intervention phase) Mean (CI) |
P-Value* | |
|---|---|---|---|---|---|---|
| Hip Adduction/Abduction Angle (°)# | 17.0 (5.1) | 17.9 (5.8) | 8.4 (6.7) | 0.9 (4.5) | −9.5 (6.0) | <0.0001 |
| Hip Medial/Lateral Rotation Angle (°)# | −0.7 (6.1) | −0.7 (5.6) | −7.5 (6.1) | 0.03 (6.0) | −6.8 (6.8) | <0.0001 |
| Knee Medial/Lateral Rotation Angle (°)# | 4.1 (5.3) | 4.2 (5.3) | 9.1 (4.9) | 0.2 (4.0) | 4.9 (5.8) | <0.0001 |
| Current Pain (VAS)‡ | 21.7 (17.4) | 18.3 (17.9) | 4.7 (8.6) | −3.4 (−10.7 to 3.9) | −13.7 (−21.4 to −5.9) | <0.0001 |
| Average Pain-Past Week (VAS)‡ | 29.1 (16.6) | 28.6 (18.0) | 9.9 (9.3) | −0.5 (−5.3 to 4.4) | −18.7 (−27.0 to −10.4) | <0.0001 |
| Maximum Pain-past week (VAS)‡ | 48.5 (20.7) | 42.7 (20.8) | 17.1 (14.4) | −5.8 (−12.4 to 0.8) | −25.6 (−35.4 to −15.8) | <0.0001 |
| Patient-specific Functional Scale§ (Total Score) | 5.8 (1.4) | 5.9 (1.3) | 8.5 (0.9) | 0.1 (−0.6 to 0.9) | 2.6 (2.0 to 3.1) | <0.0001 |
SD = Standard Deviation; CI = 95% Confidence Interval
P-Value comparing change between Baseline and 6 weeks to change between 6 weeks and 12 weeks
Angle at peak knee flexion during single limb squat (+ values: adduction, medial rotation)
VAS = Visual Analog Scale (100 mm line where 0 = no pain and 100 = worst imaginable pain)
Patient-Specific Functional Scale (rate 3 activities; range: 0–10, where 0 = unable to perform and 10 = no limitations; total score = average of 3 activities)
The change during the intervention phase was greater than the change during the control phase (Table 2) for current pain, average pain during the past week, maximum pain during the past week, and function, with all patient-reported outcome measures improving following intervention.
Discussion
Our results indicate that a rehabilitation intervention comprised solely of task-specific movement training is feasible to implement in a sample of young women who have patellofemoral pain and dynamic knee valgus. We were able to recruit our targeted number of participants and retain a higher than expected percentage over the course of the study. Participants found the intervention to be credible and, on average, reported a daily adherence to their home program that exceeded our goal of 75%. In addition, the intervention yielded improvements in kinematics, pain and function, suggesting that this treatment paradigm impacts the variables of interest and should be tested in a larger, randomized trial.
Several study limitations should be noted. This was designed as a feasibility intervention study and any conclusions about efficacy are preliminary. We enrolled women who were relatively young, healthy, and active. While our study sample was fairly homogeneous, it is representative of a large group of people who have patellofemoral pain[34]. Nonetheless, we do not know if these results would be achieved if the sample was more heterogeneous. Because our study did not have a comparison group, we cannot say whether the effects of this intervention are superior to those of another intervention or to those of attention alone. Finally, we assumed that participants practiced moving optimally during activities throughout the day as instructed. While they reported a high level of adherence to the instructions, we have no objective data to indicate how participants moved throughout their day.
With respect to recruitment, our study targeted women between the ages of 18 and 40 years, however, the average age of our participants was 22 years, likely because the study took place at a university and many of the participants responded to flyers posted on campus. The proximity to the testing and intervention facility might have encouraged student involvement, and students might have been incentivized by the advertised remuneration for participating. Alternatively, our participants, seeking to return to meaningful activities, might have been highly motivated to receive treatment for their painful condition. Patellofemoral pain is common in young, active women,[34] often limiting participation, not only in high-level activities, but also in routine activities of daily living. On average, the duration of symptoms reported by our sample was 4+ years, and limitations were reported in basic activities such as stair climbing and prolonged sitting. That said, patellofemoral pain is present in older individuals and may be linked to patellofemoral osteoarthritis.[35] As such, expanding the sample to include a wider age range may be important for future studies. Enrolling a broader sample, however, may require different recruitment strategies.
Retention over the course of the study was higher than expected, given a relatively high participation burden of 4 laboratory assessments and 12 intervention visits. Twenty-three out of 25 participants completed the study, attending all 12 intervention visits. Several factors may have contributed to our high retention. Intervention visits were scheduled around participants’ class/work obligations, and for student participants the visits took place in close proximity to classes. Accommodating participants’ schedules is essential for maximizing retention [36], and this would need to be considered for studies that enroll non-student participants who have additional obligations and live farther from the study site. High retention also could be due in part to the motivation of the participants. As mentioned, these were young active women, eager to return to activity. Additionally, participants may have developed a personal connection to the physical therapist who administered the intervention, which could have enhanced retention.[37] Based on their high credibility and expectancy ratings, participants “bought” the intervention paradigm.
With respect to adherence to the prescribed home program, on average, participants reported daily adherence values of greater than 75%, which is higher than reported home exercise program adherence ranges (55%–69%) for people with knee osteoarthritis.[27] The high adherence in the current study may be attributed in part to the fact that our participants were young, motivated, and they understood what they were supposed to do and were able to do it. All participants correctly verbalized the key concepts of optimal movement, and they demonstrated improved movement (reduced hip and knee frontal plane projection angles) during the single limb squat by the start of the second intervention visit. Further, task progression was based on optimal alignment, and all participants had some level of task progression. Another reason for high adherence might have been the intervention paradigm itself. Ten participants had received previous physical therapy for treatment of patellofemoral pain (Table 1), which typically focused on knee and/or hip muscle strengthening exercises, with a similarly-focused home exercise program. Although some of these participants reported an initial decrease in pain with their previous treatment, they indicated that they stopped doing their home exercises, after which the pain returned. Others reported that pain returned as soon as they resumed typical activities. The current intervention focused on maintaining optimal movement during tasks that were meaningful to participants, which could have enhanced their motivation.[38] Additionally, the “home program” was to incorporate optimal movement during all daily tasks; participants did not have to find time in their day to complete a separate exercise program. Convenience is an important contributor to adherence[39] and might be especially important for participants who are not as motivated to exercise (e.g. older, less active individuals).
Our health-related outcomes, although secondary, suggest that task-specific training focused on changing pain-producing movement patterns might be an effective intervention for people with patellofemoral pain. During a single-limb squat, hip and knee kinematics improved after the intervention, compared to the control phase, indicating that the movement-focused intervention effectively targeted hip and knee joint movement. Although the clinical significance of the kinematic improvements is not known, all improvements were greater than the between-day standard error of measurement for each variable.[28] Furthermore, small changes in lower extremity joint motion (5–10°) have been associated with moderate changes in patellofemoral joint loading.[40] Participants reported improvements in pain and function following the intervention, a finding that could be explained by improved kinematics. During the intervention, tasks were progressed only if the participant was able to maintain proper alignment without increasing pain. The repeated task-specific practice incorporating optimal movement may have resulted in improved patellofemoral joint loading and reduced pain, thereby contributing to participants’ improved functional status. However, alternative mechanisms of pain reduction cannot be ruled out.
Based on the study results, a task-specific movement training intervention for treatment of patellofemoral pain is feasible and should be tested more rigorously in a larger randomized clinical trial comparing this intervention to a typical multimodal intervention.[15] The recruitment, retention and adherence methods employed in this study are acceptable for use in a future trial that includes both sexes. The intervention protocol, which focused solely on task-specific movement training, would be implemented as described, given that participants reported that the intervention was credible, they adhered to it, and the therapist was able to progress tasks appropriately for each participant. The comparison intervention would address impairments in hip and knee strength and lower extremity flexibility.[15] Our health-related outcome measures were stable over time and responsive to change following this intervention. As such, these outcome measures would be appropriate for use in a future trial, with the addition of multiple follow-up assessments.
Supplementary Material
Two-dimensional hip and knee frontal plane projection angles were used as a method of quantifying dynamic knee valgus during treatment sessions. Hip angle = 90-α; Knee angle = 180-β. Larger values represent greater dynamic knee valgus.
Clinical Messages.
A rehabilitation intervention comprised solely of task-specific movement training is feasible to implement in young women who have patellofemoral pain and dynamic knee valgus, based on positive outcomes for recruitment, retention, adherence, and treatment credibility.
Task-specific movement training may improve kinematics, pain and function in women with patellofemoral pain and dynamic knee valgus, however the efficacy of the intervention must be tested in a larger, randomized trial.
Acknowledgments
The authors would like to acknowledge Angela Reitenbach and Anna DiStaulo for their assistance with participant recruitment, data collection and data processing.
Sources of Funding
This project was supported by the NIH/National Center for Advancing Translational Sciences (NCATS) grant UL1 TR000448, Washington University, Institute for Clinical and Translational Sciences CTSA #705 and the Orthopaedic Section of the American Physical Therapy Association.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to disclose.
Contributors
GS was the principal investigator and oversaw all aspects of the study (intellectual, practical, and dissemination).
BY participated in the development and execution of the intervention protocol, data interpretation, and writing/editing this manuscript.
KS contributed to the study design, statistical analysis, data interpretation, and writing/editing this manuscript.
CL contributed to the study design, development of the intervention, data interpretation, and writing/editing this manuscript.
LV contributed to the study design, development of the intervention, data interpretation, and writing/editing this manuscript.
References
- 1.Nimon G, Murray D, Sandow M, Goodfellow J. Natural history of anterior knee pain: a 14- to 20-year follow-up of nonoperative management. J Pediatr Orthop. 1998;18:118–22. [PubMed] [Google Scholar]
- 2.DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–24. doi: 10.1177/036354658601400307. [DOI] [PubMed] [Google Scholar]
- 3.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639–46. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 5.Boling MC, Bolgla LA, Mattacola CG, Uhl TL, Hosey RG. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2006;87:1428–35. doi: 10.1016/j.apmr.2006.07.264. [DOI] [PubMed] [Google Scholar]
- 6.Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33:647–60. doi: 10.2519/jospt.2003.33.11.647. [DOI] [PubMed] [Google Scholar]
- 7.Nakagawa TH, Muniz TB, Baldon Rde M, Dias Maciel C, de Menezes Reiff RB, Serrao FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22:1051–60. doi: 10.1177/0269215508095357. [DOI] [PubMed] [Google Scholar]
- 8.Collins N, Crossley K, Beller E, Darnell R, McPoil T, Vicenzino B. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Bmj. 2008;337:a1735. doi: 10.1136/bmj.a1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferber R, Bolgla L, Earl-Boehm JE, Emery C, Hamstra-Wright K. Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: a multicenter randomized controlled trial. J Athl Train. 2015;50:366–77. doi: 10.4085/1062-6050-49.3.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salsich GB, Graci V, Maxam DE. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther. 2012;42:1017–24. doi: 10.2519/jospt.2012.4231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clinical biomechanics (Bristol, Avon) 2012;27:1045–51. doi: 10.1016/j.clinbiomech.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45:691–6. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 13.Salbach NM, Mayo NE, Wood-Dauphinee S, Hanley JA, Richards CL, Cote R. A task-orientated intervention enhances walking distance and speed in the first year post stroke: a randomized controlled trial. Clin Rehabil. 2004;18:509–19. doi: 10.1191/0269215504cr763oa. [DOI] [PubMed] [Google Scholar]
- 14.Birkenmeier RL, Prager EM, Lang CE. Translating animal doses of task-specific training to people with chronic stroke in 1-hour therapy sessions: a proof-of-concept study. Neurorehabil Neural Repair. 2010;24:620–35. doi: 10.1177/1545968310361957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crossley KM, van Middelkoop M, Callaghan MJ, Collins NJ, Rathleff MS, Barton CJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions) Br J Sports Med. 2016;50:844–52. doi: 10.1136/bjsports-2016-096268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kannus P, Natri A, Paakkala T, Jarvinen M. An outcome study of chronic patellofemoral pain syndrome. Seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. 1999;81:355–63. doi: 10.2106/00004623-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815–22. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- 18.Harris-Hayes M, Steger-May K, Koh C, Royer NK, Graci V, Salsich GB. Classification of lower extremity movement patterns based on visual assessment: reliability and correlation with 2-dimensional video analysis. J Athl Train. 2014;49:304–10. doi: 10.4085/1062-6050-49.2.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–42. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 20.Hubbard IJ, Parsons MW, Neilson C, Carey LM. Task-specific training: evidence for and translation to clinical practice. Occup Ther Int. 2009;16:175–89. doi: 10.1002/oti.275. [DOI] [PubMed] [Google Scholar]
- 21.Hoffman SL, Johnson MB, Zou D, Harris-Hayes M, Van Dillen LR. Effect of classification-specific treatment on lumbopelvic motion during hip rotation in people with low back pain. Man Ther. 2011;16:344–50. doi: 10.1016/j.math.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of behavior therapy and experimental psychiatry. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 23.Chatman AB, Hyams SP, Neel JM, Binkley JM, Stratford PW, Schomberg A, Stabler M. The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Phys Ther. 1997;77:820–9. doi: 10.1093/ptj/77.8.820. [DOI] [PubMed] [Google Scholar]
- 24.Van Dillen LR, Norton BJ, Sahrmann SA, Evanoff BA, Harris-Hayes M, Holtzman GW, Earley J, Chou I, Strube MJ. Efficacy of classification-specific treatment and adherence on outcomes in people with chronic low back pain. A one-year follow-up, prospective, randomized, controlled clinical trial. Man Ther. 2016;24:52–64. doi: 10.1016/j.math.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris-Hayes M, Holtzman GW, Earley JA, Van Dillen LR. Development and preliminary reliability testing of an assessment of patient independence in performing a treatment program: standardized scenarios. J Rehabil Med. 2010;42:221–7. doi: 10.2340/16501977-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scholtes SA, Salsich GB. A dynamic valgus index that combines hip and knee angles: Assessment of utility in females with patellofemoral pain. Int J Sports Phys Ther. 2017;12:333–40. [PMC free article] [PubMed] [Google Scholar]
- 27.Bennell KL, Campbell PK, Egerton T, Metcalf B, Kasza J, Forbes A, Bills C, Gale J, Harris A, Kolt GS, Bunker SJ, Hunter DJ, Brand CA, Hinman RS. Telephone Coaching to Enhance a Home-Based Physical Activity Program for Knee Osteoarthritis: A Randomized Clinical Trial. Arthritis Care Res (Hoboken) 2017;69:84–94. doi: 10.1002/acr.22915. [DOI] [PubMed] [Google Scholar]
- 28.Graci V, Van Dillen LR, Salsich GB. Gender differences in trunk, pelvis and lower limb kinematics during a single leg squat. Gait Posture. 2012;36:461–6. doi: 10.1016/j.gaitpost.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiotherapy Canada. 1995;47:258–63. [Google Scholar]
- 30.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–63. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 31.Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4:92–9. [PMC free article] [PubMed] [Google Scholar]
- 32.Beekhuizen KS, Davis MD, Kolber MJ, Cheng MS. Test-retest reliability and minimal detectable change of the hexagon agility test. J Strength Cond Res. 2009;23:2167–71. doi: 10.1519/JSC.0b013e3181b439f0. [DOI] [PubMed] [Google Scholar]
- 33.Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Joint Surg [Am] 1992;74:820–30. [PubMed] [Google Scholar]
- 34.Crossley KM, Stefanik JJ, Selfe J, Collins NJ, Davis IS, Powers CM, McConnell J, Vicenzino B, Bazett-Jones DM, Esculier JF, Morrissey D, Callaghan MJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50:839–43. doi: 10.1136/bjsports-2016-096384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schiphof D, van Middelkoop M, de Klerk BM, Oei EH, Hofman A, Koes BW, Weinans H, Bierma-Zeinstra SM. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis) Osteoarthritis Cartilage. 2014;22:631–8. doi: 10.1016/j.joca.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Bower P, Brueton V, Gamble C, Treweek S, Smith CT, Young B, Williamson P. Interventions to improve recruitment and retention in clinical trials: a survey and workshop to assess current practice and future priorities. Trials. 2014;15:399. doi: 10.1186/1745-6215-15-399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brueton VC, Stevenson F, Vale CL, Stenning SP, Tierney JF, Harding S, Nazareth I, Meredith S, Rait G. Use of strategies to improve retention in primary care randomised trials: a qualitative study with in-depth interviews. BMJ Open. 2014;4:e003835. doi: 10.1136/bmjopen-2013-003835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Essery R, Geraghty AW, Kirby S, Yardley L. Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil. 2016:1–16. doi: 10.3109/09638288.2016.1153160. [DOI] [PubMed] [Google Scholar]
- 39.Dobson F, Bennell KL, French SD, Nicolson PJ, Klaasman RN, Holden MA, Atkins L, Hinman RS. Barriers and Facilitators to Exercise Participation in People with Hip and/or Knee Osteoarthritis: Synthesis of the Literature Using Behavior Change Theory. Am J Phys Med Rehabil. 2016;95:372–89. doi: 10.1097/PHM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 40.Liao TC, Yang N, Ho KY, Farrokhi S, Powers CM. Femur Rotation Increases Patella Cartilage Stress in Females with Patellofemoral Pain. Med Sci Sports Exerc. 2015;47:1775–80. doi: 10.1249/MSS.0000000000000617. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two-dimensional hip and knee frontal plane projection angles were used as a method of quantifying dynamic knee valgus during treatment sessions. Hip angle = 90-α; Knee angle = 180-β. Larger values represent greater dynamic knee valgus.