Abstract
Substance use (SU) stigma is one factor contributing to unmet need for SU treatment. Additionally, theory suggests that women and single parents who use substances experience enhanced stigma because they do not adhere to normative social expectations. This study examines differences in perceived stigma by gender and parenthood among those with unmet need for SU treatment using the 2003-2010 National Survey of Drug Use and Health (N = 1,474). Results indicate that women are more likely to report stigma as a barrier to treatment compared with men, though the interaction between gender and parenthood is not significant. We find that married parents report the highest level of stigma. We situate our findings in past health-related stigma research. We suggest that these results shed a light on stigma, particularly as it relates to family status, as a contributing factor to differences regarding SU treatment utilization. Finally, we raise a provocative question concerning social status and anticipated stigma.
Keywords: family health, family theory, gender and family, quantitative, single parents
Substance use (SU) problems, including illicit substance use and at-risk alcohol use, have serious consequences both for the individual and the family (Substance Abuse and Mental Health Services Administration [SAMHSA], 2012). Beyond the health ramifications that the individual user endures, children growing up in homes where one or more parent(s) engage in SU may be exposed to domestic violence, child welfare involvement, and residential instability (VanDeMark et al., 2005). Research also indicates that children of parents with SU problems are more likely to develop substance-related problems as adolescents and adults (Lam et al., 2007; Seljamo et al., 2006). However, there is hope; SU treatment significantly reduces the negative outcomes associated with parental SU including a reduced likelihood that children will experience SU problems as adults (Haggerty, Skinner, Fleming, Gainey, & Catalano, 2008).
Despite the positive benefits of SU treatment, few individuals receive treatment. Unmet need for SU treatment, (commonly referred to as the SU treatment gap) is defined as needing treatment for SU, but not receiving treatment at a specialty facility (Epstein, 2002; Woodward et al., 1996). According to the National Survey of Drug Use and Health (NSDUH), 99% of Americans who meet the criteria for alcohol or SU disorders fall into this treatment gap (Grella, Stein, Weisner, Chi, & Moos, 2010; SAMHSA, 2011; Storbjörk & Ullman, 2012). Additionally, this unmet need for treatment is experienced unevenly across different groups and is greater among women than men (Green, 2006; Holmila & Raitasalo, 2005; Wu & Ringwalt, 2004). Though women comprise approximately one third of the population affected by SU problems, women are consistently less likely than men to utilize SU treatment services, even after controlling for the higher rates of SU among men and problem severity (Cohen, Feinn, Arias, & Kranzler, 2007; Greenfield, Back, Lawson, & Brady, 2010; Schmidt, Tam, & Mj, 2007).
Research has shown that female users and parents experience a number of additional barriers to receiving treatment including maternal responsibilities (as mothers are more likely to be single parents), lack of child care while in treatment, disadvantages in economic resources, less social/partner-support, and possibly greater social stigma (Brady & Ashley, 2005; Greenfield et al., 2007; Taylor, 2010). While many factors impede an individual's ability to seek SU treatment, recent research has begun to focus on the role of stigma in help-seeking behaviors among those with SU problems. SU is especially stigmatizing as it is commonly viewed as an issue associated with a lack of self-control and low moral character (Corrigan, Watson, & Miller, 2006; Hegarty & Golden, 2008; Martin, Pescosolido, & Tuch (2000); Schomerus et al., 2011). The current analysis seeks to examine the possible gender differences in social stigma as a barrier to SU treatment and to focus on the role of the family, both parental and marital status, as contributing to or alleviating perceived stigma as a barrier to SU treatment.
Background
Health-Related Stigma
Goffman's (1963) seminal work described stigma as “an attribute that is deeply discrediting,” which reduces its bearer “from a whole and usual person to a tainted, discounted one” (Goffman 1963, p. 3). Although stigma can refer to a variety of attributes, health-related stigma has emerged as a significant player in health behavior and outcomes research. Health-related stigma is defined as status loss and discrimination informed by negative attitudes and stereotypes based on health-related conditions (Link & Phelan, 2001). Two types of stigmas that individuals with a need for SU treatment may face include enacted stigma and perceived (or felt) stigma. Enacted stigma refers to overt rejection and discrimination and may include denial of housing, medical services, social isolation, and verbal and physical assaults (White, Evans, & Lamb, 2009). Perceived stigma is a multidimensional concept that encompasses feelings of shame or embarrassment about having a stigmatized health condition as well as anticipation, and fear of, encountering enacted stigma (Carricaburu & Pierret, 1995; Scambler, 2009).
Goffman (1963) also differentiated between discredited and discreditable stigmas. Discredited stigma results from an obvious attribute that can readily be observed and thus the associated stigma is unavoidable. However, a discreditable stigma is a hidden attribute that is not readily apparent. Individuals possessing discreditable attributes often fear disclosure and may seriously alter their behaviors to avoid being identified or to “pass” for nonstigmatized. Similarly, Link (1987) and Link, Cullen, Struening, Shrout, & Dohrenwend (1989) noted in their “modified labeling theory” that secrecy, treatment avoidance, and treatment delay are defensive mechanisms employed as a result of perceived stigma; individuals with stigmatized conditions, including SU, may forgo treatment to avoid the diagnostic label that solidifies them as a member of a stigmatized group.
The reasons behind SU stigma range from reactions to the negative consequences of drug use to attributions of danger and blame (Lloyd, 2013). Jones et al. (1984) argued that not all stigmatizing conditions are treated equally and theorized six dimension of stigma that affect the extent to which a condition may be stigmatized. The most highly stigmatized conditions are related to the dimensions of etiology (personal responsibility), concealability (the extent to which it can be hidden), and peril (dangerousness) (Jones et al., 1984). With regard to etiology, the behavioral component of SU makes it especially vulnerable to stigmatization and likely contributes to the wide spread acceptance of SU as rooted in poor moral character (Baumohl, Speiglman, Swartz, & Stahl, 2003). With regard to concealability, SU is similar to other progressive illnesses, in that as one's SU increases, the physical toll on the body increases and the ability to conceal one's SU decreases. Finally, SU is strongly associated with peril; individuals engaged in various forms of SU are viewed by many as dangerous (Cunningham, Sobell, & Chow, 1993; Martin et al., 2000; Phelan, Link, Stueve, & Pescosolido, 2000). Previous research indicates that SU disorders are viewed as the most dangerous psychological disorders when compared with other serious mental illnesses (Link, Phelan, Bresnahan, Stueve, & Pescosolido, 1999; Pescosolido, Monahan, Link, Stueve, & Kikuzawa, 1999). To be fair, the link between SU and danger is not without merit; research suggests that crime and violence are more frequent among individuals with high levels of SU (Moore, Easton, & McMahon, 2011). This relationship between SU and harm helps rationalize the stigma of SU disorders.
Though the study of SU stigma and health outcomes is still relatively new, numerous studies have identified SU stigma as a significant predictor of low levels of health services utilization, poor mental and physical health outcomes, and high levels of risk behaviors (Cole, Logan, & Walker, 2011; Frischknecht et al., 2011; Kulesza, Larimer, & Rao, 2013; Latkin, Davey-Rothwell, Yang, & Crawford, 2012). The SU treatment research is replete with studies in which individuals list concern about stigma, privacy, and/or being labeled “alcoholic” or “addict” as primary contributors to treatment avoidance and delay (Cohen et al., 2007; Keyes et al., 2010; Rae Olmsted et al., 2011; Semple, Grant, & Patterson, 2005; White et al., 2009). Researchers have documented that concerns about privacy and stigma often lead individuals to engage in selective disclosure, treatment avoidance, and treatment delay in order to avoid diagnostic labeling (Palamar, 2012; Saunders, Zygowicz, & D'Angelo, 2006; Semple et al., 2005).
Motherhood and Substance Use Stigma
Research suggests that various types of stigma may intersect with other attributes of the individual, leading to higher levels of stigmatization for certain segments of the population (Logie, James, Tharao, & Loutfy, 2011). Researchers argue that the single most important factor that distinguishes the SU and treatment experiences of men and women is the experience of increased stigmatizing attitudes toward female substance users (Covington, 2000). Attitudes toward SU may be one way in which proscribed gender norms and traditional gendered expectations are enforced (Anderson, 2010; Peralta & Jauk, 2011). Women who do not conform to socially defined standards of feminine behavior are subjected to negative sanctions for their transgressions including views of female users as dirty, masculine, and sexually available (Anderson, 2010; Boyd, 2004; Parks & Scheidt, 2000).
The greater stigma that women with SU problems experience may be specifically rooted in a woman's socially defined role as mother and wife (Anderson, 2010; Boyd, 2004; Peralta & Jauk, 2011). Indeed, negative sereo-types of female users contradict women's normative roles as submissive, chaste, and nurturing caregivers (Fagan, 1994). This caregiving role is an essential aspect of the gendered role traditionally applied to women, especially those with children. Within the gendered perspective, concerns about SU among women stem from the perception that an intoxicated woman is unable to fulfill her primary socially defined role of caregiver. Therefore, women with SU-related problems are particularly vulnerable to stigmatization (Erickson, Butters, McGillicuddy, & Hallgren, 2000; Heidensohn, 2002; Worrall, 2002), having transgressed against social codes of behavior and having violated traditional expectations of the roles of wife, mother, and family nurturer (Ettorre, 2007; Fagan, 1994).
Substance using mothers must constantly live in fear that the label of ‘unfit mother’ will be applied to them (Boyd, 2004; Linnemann, 2009), thereby possibly increasing stigma as a barrier to SU treatment. The label of unfit mother, once applied, can carry serious consequences for women, including criminal charges and forfeiture of parental rights (Boyd, 2004; Linnemann, 2009). This stigma related to SU and motherhood may push her toward “passing” strategies, avoiding treatment in order to elude the negative social label, and social stigma, that comes with an official diagnosis (Brady & Ashley, 2005; Green, 2006). Research supports this idea of mothers attempting to “pass”; many pregnant women and new mothers report being afraid that their SU will be discovered and they will lose parental rights (Jessup, Humphreys, Brindis, & Lee, 2003).
These fears associated with the diagnosis of a SU disorder are not unwar-ranted among pregnant women and new mothers. Women who are parenting or pregnant have been the object of criminal prosecution in numerous states for years (Murphy, 2014). Most recently, on April 29, 2014, Tennessee became the first state in the country to authorize the incarceration of women who use drugs while pregnant (“Title 39,” 2014). Although these laws were originally passed in an attempt to deter pregnant women from using substances, they are counterproductive to SU treatment utilization. Numerous health associations, including, but not limited to, the American Medical Association (1990; Chervenak & McCullough, 1991), the American Academy of Pediatrics (1990), and the American Public Health Association (1990) have released statements pointing to the likelihood that criminal prosecution of substance using pregnant women will result in greater avoidance of SU treatment and prenatal care. Although it is impossible to summarize the dozens of statements published by various associations regarding the criminalization of SU while pregnant, the following quote from the American Society of Addiction Medicine's Policy Statement on Chemically Dependent Women and Pregnancy summarizes the general consensus:
Criminal prosecution of chemically dependent women will have the overall result of deterring such women from seeking both prenatal care and chemical dependency treatment, thereby increasing, rather than preventing harm to children and to society as a whole. (2005)
Parenthood, Martial Status, and Substance Use Stigma
SU stigma is magnified in the context of parenthood
The peril, or dangerousness, dimension of social stigma may be particularly relevant when considering SU and the presence of children. Though some studies have shown an association between SU and negative effects on children and the family unit (Barnard & McKeganey, 2004; Walsh, MacMillan, & Jamieson, 2003), parents suffering from substance-related problems are painted with a broad, stereotypical brush. Combining data collected from numerous studies, Klee (1998) reports that health professionals frequently describe parents with SU problems as “selfish and uncaring, irresponsible, distracted, neglectful, intolerant, irritable and aggressive, no(t engaging in) child-centered activity, (and) put(ting) drugs before (their) child” (p. 439). The possibility of facing enacted stigma from health care providers provides a strong incentive to avoid seeking treatment among parents with SU problems.
Furthermore, according to socialization theories, a two-parent household is the ideal environment for child rearing (David, Demo, & Acock, 1996), thus individuals who do not conform to the traditional, heterosexual, two-parent ideal family structure face various forms of social stigma (Lansford, Ceballo, Abbey, & Stewart, 2001; Lauster & Easterbrook, 2011). For single parents who engage in various forms of SU, the social stigma of single parenthood may enhance feelings of stigma overall. Although single parents may face multiple barriers to SU treatment (i.e., economic and child care burdens), the intersection of single parenthood stigma and SU stigma may further decrease one's likelihood to seek treatment services.
Hypotheses
A thorough search of the literature has uncovered that no quantitative investigation has been published to validate these theoretical propositions regarding gender, parenthood status, marital status, and stigma. Previous research has indicated that SU stigma as a barrier to treatment does exist among women (Greenfield et al., 2007), but an analysis of stigma as a barrier which compares men and women with respect to has yet to be conducted. Furthermore, an investigation of how family structure may affect SU stigma is also missing from the literature. Understanding the factors that increase perceived stigma as a barrier to SU treatment will facilitate providing adequate treatment and incentivizing substance users to seek treatment. This analysis addresses this gap in research, conducting an empirical analysis to examine gender differences in stigma as a barrier to SU treatment, and examining the potential role that parenthood and marital status may play in this relationship.
Based on theory and past research, we believe that women will be more likely to report social stigma as a barrier to SU treatment. Furthermore, taking into account the traditional expectations of motherhood and family structure, we expect that mothers and single parents will report more stigma-related barriers than father or married parent families.
Hypothesis 1: Women with unmet need for SU treatment will report greater stigma-related barriers than men with unmet need.
Hypothesis 2: Parents with unmet need for SU treatment will report greater stigma-related barriers than nonparents with unmet need.
Hypothesis 3: Parenthood is significantly more likely to be associated with stigma for women compared with men among those with unmet need for SU treatment.
Hypothesis 4: Never-married parents are more likely to report stigma as a barrier to SU treatment than married or formerly married parents with unmet need for SU treatment.
Data and Method
Data for this study were drawn from the public use file of the 2003-2010 NSDUH (SAMHSA, 2004-2011). The NSDUH is conducted on an annual basis to provide nationally representative data on the incidence and prevalence of drug, alcohol, and tobacco use by persons 12 years and older, within the United States. The NSDUH covers topics such as illicit drug use, alcohol use, substance abuse treatment history, and perceived need for treatment. The survey is conducted using face-to-face interview techniques at the respondent's home. To ensure confidentiality, questions concerning SU and mental health are completed using computer-assisted interview technology. A more detailed description of the sampling methodology for the NSDUH survey is publically available (Morton, Martin, Chromy, Hirsch, & Ridenhour, 2011).
The NSDUH only inquires about SU stigma in the context of barriers to treatment and as such, only participants with unmet need are asked about stigma concerns. For the purpose of this research, the target population included individuals older than the age of 18 years with unmet need for SU treatment. Unmet need is defined as a personal recognition for treatment by the individual and a failure to seek out such treatment. Listwise deletion was used if the respondent is missing on any of the research variables, resulting in dropping approximately 6% of the sample. Listwise deletion is seen as an appropriate method to handle missingness, when there is less than 10% missing in the sample (Allison, 2001). The final sample size is 1,474 cases.
Criterion Variable
The criterion variable, perceived stigma as a barrier to SU treatment, was constructed using responses to the following question: “Which of these statements explain why you did not seek the treatment you needed for your use of [substance]?” Respondents were given 14 options from which they could choose one or more reasons for not receiving treatment. Consistent with previous research, which has utilized the NSDUH data set to examine treatment-seeking behaviors and stigma (Alang, 2014; Brown et al., 2010; Mojtabai, Olfson, & Mechanic, 2002; SAMHSA, 2009; Townsend, Gearing, & Polyanskaya, 2012), a combination of the following three options were used to create the criterion variable for this study: (a) You did not want others to find out that you needed treatment (yes/no), (b) You were concerned that getting treatment or counseling might cause your neighbors or community to have a negative opinion of you (yes/no), (c) You were concerned that getting treatment or counseling might have a negative effect on your job (yes/no). An affirmative response to one or more of these items is coded as a report of stigma as a barrier to treatment (stigma = 1, no stigma = 0). Additionally, sensitivity analyses took into account that individuals were allowed to respond affirmatively to multiple barriers by examining stigma as a count variable and also examining differences among individuals who reported only stigma-related barriers to those who reported stigma and other related barriers. Results indicated no significant differences (not shown).
Predictor Variables
The predictor variables of interest include sex, marital status, and parenthood status. Sex and marital statuses are based on self-report; marital status is coded as never married, married (reference), and formerly married (divorced, widowed, and separated). Parenthood status is defined as having one or more of the respondent's own children, less than 18 years of age, living in the household at the time of the survey administration. Controls include race (non-Hispanic White and non-White or Hispanic, referred to herein out as White and non-White), education (less than high school, high school education, and at least some college), age, which is measured using four age groups (18 to 20 years old, 21 to 25 years old, 26 to 34 years old, and 35 years old or older), and income. Total family income is measured using seven categories; less than $10,000, $10,000 to $19,999, $20,000 to $29,999, $30,000 to $39,999, $40,000 to $49,999, $50,000 to $74,999, and $75,000 or more and is treated as continuous.
The hypotheses identified above are examined using nested logistic regression and are evaluated with STATA software (ver. 11; StataCorp., 2009). This statistical method was chosen to account for the binary nature of the criterion variable. Model 1 tests Hypotheses 1 and 2 by regressing our focal predictor variables (sex, parenthood status, and marital status) on stigma (stigma = 1). Model 2 includes the sociodemographic control variables to determine if a relationship exists between the predictor and criterion variable after controlling for these factors. Last, Hypotheses 3 and 4, whether the association between parenthood and stigma varies by marital status or sex, are evaluated by including interactions in Model 3.
Results
Table 1 contains descriptive statistics for the analytic sample and also broken down by sex and parenthood status. Significance tests were conducted using chi-square tests and t tests and indicate significant differences between men and women. Consistent with Hypothesis 1, among those with unmet need for SU treatment, we find that women are more likely than men to report stigma as a barrier to treatment (26.3% of women and 20.2% of men, p < .01). Additionally, we find that women are more likely to be parents compared with men (44.9% of women are parents compared with 36.9% of men p < .01) and are more likely to be formerly married compared with men (18.6% of women compared with 13.2% of men, p < .05). However, there are no significant differences in stigma by parenthood status (p = .34, not shown), between mothers and nonmothers (p = .42), or between fathers and nonfathers (p = .92, not shown). Additionally, there are no significant differences in stigma by marital status (p = .11, not shown). Thus, our descriptive statistics find support for Hypothesis 1, women are more likely to report stigma as a barrier to treatment compared with men, but fail to find support for Hypotheses 2, 3, and 4. Examining the control variables, we find that women are more educated compared with men (41.3% of women had at least some college compared with 31.2% of men, p < .01), but have lower incomes (3.5 for women compared with 3.8 for men p < .01). Examining demographic characteristics, women are more likely to be White (67.5% of women are White and 56.4% of men are White, p < .001) and younger (25% of women are in between the ages of 18 and 20 years compared with 18.4% of men, p < .01). Additionally, we find that men are more likely than women to report unmet need for SU treatment, 41.5% of the sample and 58.5% are men (final column). Appendix Table A1 contains study characteristics broken down by drug type.
Table 1.
Percentages and Means for Study Variables Among Individuals With Unmet Need for Substance Use Treatment by Sex and Parenthood Status, NSDUH, 2003-2010.a,b
| Women | Men | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Mothers | Nonmothers | Total | Fathers | Nonfathers | Total | Total | |
| Stigma (%) | 27.6 | 25.2 | 26.3** | 20.1 | 20.2 | 20.2 | 22.7 |
| Sex (%) | |||||||
| Men | 58.5 | ||||||
| Women | 41.5 | ||||||
| Parent (%) | 100.0 | 0.0 | 44.9*** | 100.0 | 0.0 | 36.9 | 40.2 |
| Marital status (%) | |||||||
| Never married | 53.1 | 71.5 | 63.2 | 54.4 | 74.1 | 66.8 | 65.3 |
| Married | 26.2 | 11.6 | 18.1 | 35.8 | 10.7 | 20.0 | 19.2 |
| Formerly married | 20.7 | 16.9 | 18.6* | 9.7 | 15.3 | 13.2 | 15.5 |
| Race (%) | |||||||
| Other | 37.1 | 28.8 | 32.5 | 52.5 | 38.4 | 43.6 | 39.0 |
| White | 62.9 | 71.2 | 67.5*** | 47.5 | 61.6 | 56.4 | 61.0 |
| Family income | 3.7 | 3.4 | 3.5** | 4.1 | 3.7 | 3.8 | 3.7 |
| (0.12) | (0.11) | (0.08) | (0.11) | (0.09) | (0.07) | (0.05) | |
| Education (%) | |||||||
| School | 31.6 | 21.4 | 26.0*** | 41.2 | 28.1 | 32.9 | 30.1 |
| High school | 36.4 | 29.7 | 32.7 | 38.7 | 34.2 | 35.8 | 34.5 |
| Some college | 32.0 | 49.0 | 41.3** | 20.1 | 37.7 | 31.2 | 35.4 |
| Age (%) | |||||||
| 18 to 20 years | 20.7 | 28.5 | 25.0* | 21.4 | 16.7 | 18.4 | 21.2 |
| 21 to 25 years | 39.3 | 40.4 | 39.9 | 36.5 | 38.8 | 37.9 | 38.7 |
| 26 to 34 years | 19.3 | 8.9 | 13.6 | 19.5 | 15.8 | 17.2 | 15.7 |
| 35 or older | 20.7 | 22.3 | 21.6 | 22.6 | 28.7 | 26.5 | 24.4 |
| Household size | 4.0 | 2.4 | 3.1 | 4.3 | 2.4 | 3.1 | 3.1 |
| (0.07) | (0.06) | (0.05) | (0.06) | (0.05) | (0.05) | (0.04) | |
| N | 275 | 337 | 612 | 318 | 544 | 862 | 1,474 |
Note. NSDUH = National Survey of Drug Use and Health.
χ2 tests of independence and t tests are used to determine significant differences between men and women.
Standard errors for continuous variables in parentheses.
p < .1.
p < .05.
p < .01.
p < .001.
Multivariate Analyses
The general patterns found above are examined in multivariate logistic regression. Table 2 presents odds ratios (ORs) and 95% confidence intervals (CIs) predicting perceived stigma as a barrier to SU treatment. Model 1 contains the main predictor variables, sex, parenthood status, and marital status and confirms the findings from the descriptive results. Sex is significantly associated with reporting greater stigma as a reason for unmet need; women have 44% greater odds of reporting stigma as a barrier to SU treatment compared with men (p < .01). Additionally, we now find that formerly married individuals have lower odds of reporting stigma than married individuals (OR = 0.61, p < .05). However, there are no differences by parenthood status. Model 2 adds our socioeconomic and demographic control variables. Controlling for these variables partially accounts for the significant sex differences in perceived stigma, OR for women is reduced from 1.44 to 1.32 (p < .05).
Table 2.
Logistic Regression Predicting Stigma as a Barrier to SU Treatment Among Those With Unmet.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | ||||||
| Men | ||||||
| Women | 1.44** | [1.12, 1.84] | 1.32* | [1.01, 1.71] | 1.27 | [0.91, 1.79] |
| Parent | 1.01 | [0.78, 1.31] | 1.49* | [1.05, 2.12] | 2.61** | [1.29, 5.31] |
| Marital status | ||||||
| Married | ||||||
| Never married | 0.83 | [0.61, 1.14] | 0.91 | [0.63, 1.33] | 1.51 | [0.84, 2.72] |
| Formerly married | 0.61* | [0.40, 0.95] | 0.70 | [0.44, 1.11] | 0.95 | [0.46, 1.94] |
| Parent × women | 1.11 | [0.66, 1.88] | ||||
| Parent × never | ||||||
| Married | 0.42* | [0.21, 0.86] | ||||
| Parent × formerly | ||||||
| Married | 0.72 | [0.28, 1.84] | ||||
| Race | ||||||
| Other | ||||||
| White | 1.42* | [1.07, 1.87] | 1.40* | [1.06, 1.86] | ||
| Family income | 1.15*** | [1.07, 1.23] | 1.16*** | [1.08, 1.24] | ||
| Education | ||||||
| Less than high school | ||||||
| High school | 1.40+ | [0.99, 2.00] | 1.36+ | [0.95, 1.93] | ||
| Some college | 2.47*** | [1.74, 3.51] | 2.37*** | [1.67, 3.37] | ||
| Age | ||||||
| 18 to 20 years | ||||||
| 21 to 25 years | 0.96 | [0.67, 1.36] | 0.94 | [0.66, 1.34] | ||
| 26 to 34 years | 1.15 | [0.73, 1.79] | 1.11 | [0.71, 1.74] | ||
| 35 or older | 0.80 | [0.50, 1.28] | 0.79 | [0.49, 1.28] | ||
| Household size | 0.88* | [0.77, 1.00] | 0.87* | [0.76, 0.99] | ||
| Model fit | ||||||
| Statistics | ||||||
| Model chi-square | 12.76* | 92.15*** | 98.95*** | |||
| Pseudo R2 | 0.008 | 0.058 | 0.063 | |||
Note. SU = substance use; OR = odds ratio; CI = confidence interval.
p < .1.
p < .05.
p < .01.
p < .001.
In Model 2, we also find significant relationships between the sociodemo-graphic control variables and perceived stigma as a barrier to SU treatment. Higher total family income is associated with a greater likelihood to report stigma as a barrier to SU treatment (OR = 1.15, p < .000). Compared with those with less than a high school degree, those with at least some college have nearly two and a half times to the odds of reporting stigma as a reason for unmet need (OR = 2.47, p < .001). Examining the demographic characteristics, we find that Whites have 42% (p < .05) higher odds of reporting stigma as barrier to treatment compared with non-Whites. Sex differences on the descriptive variables and the mediation of the sex difference once controls are added to the model suggest that the greater likelihood for women to perceive stigma as a barrier to SU treatment is partially due to their higher educational attainment and greater likelihood of being White. Additionally, we found that being formerly married is no longer significant once sociodemo-graphic controls are included. This appears to be due to the greater likelihood to have lower socioeconomic status (SES) among formerly married individuals compared with married individuals.
Model 3 tests Hypothesis 3 that parenthood is significantly more likely to be associated with stigma for women compared with men and Hypothesis 4 that never married parents have greater stigma then married parents. This is done by including interaction terms between sex and parenthood status and between parenthood and marital status. The interaction between sex and parenthood is not significant and fails to support our third hypothesis. Parenthood does not significantly interact with gender, however in additional analyses (see Appendix, Table A2) we examine parenthood and gender additively by creating four separate groups; mothers, nonmothers, fathers, and nonfathers. We find that compared with mothers, nonmothers and nonfathers both are less likely to experience stigma as a barrier to treatment (OR = 0.64, p < .05 and .51, p < .001, respectively). Additionally, fathers are less likely to experience stigma as a barrier to treatment than mothers, but this fails to reach significance (OR = 0.71, p = .09). Thus, we fail to find support for Hypothesis 3.
Model 3 also indicates that the interaction between parent and never married is significant and indicates that, contrary to Hypothesis 4, never married parents experience less stigma than married parents (OR = 0.42, p < .05). This interaction is depicted in Figure 1, which displays the predicted log odds of experiencing stigma as a barrier to unmet need among our different groups of parent and marital status. Indeed, married parents are the most likely to report stigma as a barrier to SU treatment than any of the other parent and marital status groups. Care should be taken in interpreting the association of stigma for the formerly married group by parenthood status given their small sample size (only 85 formerly married respondents are parents) and large CIs.
Figure 1.
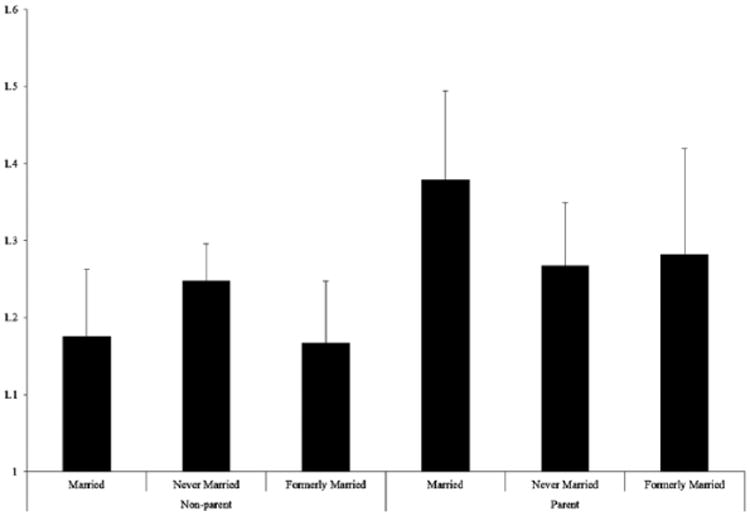
Predicted log odds of stigmas a barrier among those with unmet need, by parent and marital status. NSDUH, 2003-2010.
Note. NSDUH = National Survey of Drug Use and Health.
Discussion
Social stigma remains a strong barrier to SU treatment utilization, despite the medicalization of the condition more than 60 years ago (American Psychiatric Association, 1952). The goal of this analysis was to provide empirical support for sex differences in the role of perceived stigma as a barrier to SU treatment and examine the extent that this association was moderated by parenthood. This article tested the hypothesis that substance using women would report more stigma-related barriers to treatment than men. The stricter norms concerning SU among women was suspected to increase the strength of the perceived stigma experienced by women with unmet need for SU treatment and manifest itself in perceived stigma acting as a stronger barrier to SU treatment for women than for men.
Indeed, we find that women were more likely to report perceived stigma as a barrier to SU treatment compared with men. Women with unmet need had 44% greater log odds of reporting perceived stigma as a reason that they did not seek SU treatment in the last year. However, these sex differences were partially accounted for by our controls, especially race and education. Compared with men, women with unmet need were more likely to be White and have a higher education, both of which were positively associated with perceived stigma as a barrier to SU treatment. We also find support for our second hypothesis, which examined whether parenthood was associated with a greater likelihood of indicating that stigma was a barrier to receiving SU treatment, after controls for sociodemographic characteristics are included in the model; parents have 49% greater odds of reporting stigma compared with nonparents.
Our third model illustrates that the association between parenthood and stigma is not significantly different for men compared with women. Although our third hypothesis was not supported in the interaction model, further analysis (see Appendix, Table 2A) supported this association additively. The combined effects of greater stigma among women and parents results in mothers experiencing the most stigma compared with father, nonmothers, or nonfathers. However, the difference between mothers and fathers fails to reach significance, both fathers and mothers experience greater stigma than their nonparent counterparts. This highlights the impact of how gender roles and family status affect individual's ability to seek SU treatment when they are in need of it. Additionally, it underscores how parenthood status should be addressed in attempting to decrease stigma and increase utilization of treatment. Addressing this seems especially pertinent given the negative health outcomes found for children who have substance using parents (Osborne & Berger, 2009). Though female focused interventions specifically focus on family and are usually the targets for interventions when parent status is considered, this analysis also demonstrates that fathers experience greater stigma as well.
Concerning our fourth hypothesis, this analysis revealed surprising results; individuals who are married parents were more likely to report stigma as a barrier to SU treatment than never married parents. Although these results were unexpected, they are consistent with findings in Model 2, individuals with nonmarginalized statuses are more likely to report stigma as a barrier to SU treatment. In Model 2, we see that individuals who identify as White, have higher levels of education, and report higher incomes are more likely to report stigma as a barrier to SU treatment as well. One way to interpret these findings is that individuals with higher social status may be more concerned about possible status loss from seeking treatment compared with those with lower social status. Consequently, treatment avoidance based on stigma-related barriers may vary based on the amount of social status a person feels she or he has to lose (Ojeda & Bergstresser, 2008). Alternatively, it could be that individuals who already face various other forms discriminations and stigmas (single parents, non-Whites, those with lower SES) may be less sensitive to SU stigma compared with those who do not face stigma based on these group memberships.
Our findings concerning marginalized and nonmarginalized populations present a new and provocative question for stigma researchers: Does higher social status increase anticipated stigma? Although nonmarginalized populations may anticipate more social stigma, much research indicates that more marginalized populations experience greater enacted stigma (Hartwell, 2004; Logie et al., 2011; Loutfy et al., 2012; Storholm et al., 2013). Our finding can be significantly informed by fundamental cause theory. Although much of the focus in fundamental cause theory research has been on SES, in a recent volume of the American Journal of Public Health, Hatzenbuehler et al. (2013) argued that stigma should also be considered as a “fundamental cause of population health inequalities.” In their seminal work on the theory, Link and Phelan (1995) argue that flexible resources play a central role in the relationship between SES and health outcomes. Flexible resources, such as money, knowledge, power, prestige, and beneficial social connections, can be deployed to avoid risk or to adopt protective strategies to reduce negative outcomes. Thus, it is reasonable to consider that, access to various social resources may protect nonmarginalized persons from actually experiencing enacted stigma, but leave those without these resources at greater risk for experiencing enacted stigma. Although individuals with more flexible resources may employ these resources to avoid enacted stigma, this same access to resources is threatened by the possibility of enacted stigma; thus, fear of facing enacted stigma and losing social status may act to increase the extent that perceived stigma affects treatment seeking. A comparison of anticipated stigma and enacted stigma among these two groups would facilitate our understanding of the ways in which social status may affect stigma experiences.
Limitations and Conclusions
Though this is the first study to empirically examine sex difference in perceived stigma as a barrier to SU treatment, it is not without its limitations. The first limitation is that treatment was defined as only using formal treatment, which understates the extent that individuals with SU problems seek treatment. Though formal treatment is consistently associated with positive outcomes among this population (Grella et al., 2010; Storbjörk & Ullman, 2012), formal treatment is only one pathway to the treatment of substance-related disorders. Popular alternatives to formal treatment include 12-step programs, such as Alcoholics Anonymous, and attempts at self-recovery (natural recovery) (Humphreys et al., 2004; Tucker & Simpson, 2011). It is possible that stigma and discrimination are strong among recovering substance users who decide to forgo formal treatment options in favor of other treatment options; however, the present study was not able to tease out those who relied on self-help organizations rather than formal substance treatment and thus was unable to examine the extent to which the stigma-related barriers informed choices of treatment modalities.
Second, this research is only cross-sectional and implies associations only. Longitudinal data would allow researchers to examine how changes in stigma are associated with treatment seeking behaviors would be ideal. Future longitudinal research could expand our understanding by including individuals who ultimately did seek treatment, formal and informal, which would allow for a better assessment of the extent to which stigma affects decisions on the type of treatment one chooses and its effects on treatment delay. Unfortunately, a representative data set which would allow for longitudinal analysis of stigma and treatment-seeking behavior is not currently available. The NSDUH data set, stigma questions are only asked among those with unmet need, thus this data can only be used to examine stigma as a barrier to treatment among those with unmet need.
Furthermore, our analyses do not take into account various other barriers that parents or women may face. Treatment seeking requires not only the desire to receive treatment and the access to such services but also on the availability of a wide range of resources. For parents, the lack of availability of facilities that provide child care services may be an important barrier to SU treatment. Most SU treatment programs do not allow for parents to bring their children with them, do not provide child care services, nor do they help arrange for temporary guardianship while the parent is in treatment. Our analysis was not able to disentangle the complex relationship between perceived stigma and these structural barriers that many parents face. Future stigma research would benefit from a comparison of traditional treatment facilities and those that cater specifically to the needs of parents, especially mothers.
Similarly, our definition of stigma directly relies on barriers to seeking treatment and does not address the complex relationship of stigma. A continuous measure could provide a more nuanced understanding of the phenomenon in question. In many areas of stigma research, scales which provide continuous measures are avalable includingthe Berger Scale for HIV stigma (Berger, Ferrans, & Lashley, 2001), the Perceived Devaluation Discrimination Scale for Mental Illness Stigma (Link, Mirotznik, & Cullen, 1991). Although researchers are currently developing continuous scales to measure substance abuse stigma among current substance users (Palamar, Kiang, & Halkitis, 2011), data related to this topic are not currently available in nationally representative data. However, because participants were allowed to select more than one reason as to why they did not seek treatment, we used a negative binomial, with the number of stigma-related barriers as a count variable, to examine our hypothesis as well (n = 1,139 for 0, n = 220 for 1, n = 95 for 2, and n = 20 for 3 stigma barriers). Because the results of the negative binomial regression model were not different from the original outcome (not shown), and because prior research provides a basis for the dichotomous use of the NSDUH stigma variables (Alang, 2014; Brown et al., 2010; Mojtabai et al., 2002; SAMHSA, 2009; Townsend et al., 2012), we have chosen to only include the dichotomous stigma variable for publication.
Although effective treatment for substance-related disorders are widely available, adults with need for these services underutilize them (Cohen et al., 2007). Understanding barriers to treatment utilization is necessary in developing accessible treatment opportunities. Any examination of treatment utilization, avoidance, or delay must begin with an acknowledgment that stigma, SU, and SU treatment are complex social phenomenon. Decisions to seek treatment are influenced by a variety of factors including social stigma, economic status, clinical settings, familial relationships, and personal dispositions. The extent to which these factors individually inform the decision to seek, avoid, or delay treatment is not easily untangled. This research has added to the understanding of treatment-seeking behaviors; illustrating that parenthood status and marital status are important to understanding differences in stigma as a barrier to SU treatment.
Acknowledgments
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number F31DA037106. The content is solely the responsibilityof the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix
Table A1.
Percentages and Means for Study Variables Among Individuals With Unmet Need for Substance Abuse Treatment by Drug of Choice. NSDUH, 2003-2010.a
| Alcohol 23.5 | Depressantsb | Stimulantsc | Heroin | Marijuana | Otherd | |
|---|---|---|---|---|---|---|
| Stigma (%) | 27.9 | 26.2 | 27.0 | 21.1 | 15.2 | |
| Sex (%) | ||||||
| Men | 62.2 | 46.4 | 496.0 | 45.9 | 60.3 | 56.7 |
| Women | 38.8 | 54.6 | 50.4 | 54.1 | 39.7 | 43.3 |
| Parent (%) | 37.6 | 39.6 | 36.3 | 32.4 | 43.3 | 48.9 |
| Marital status (%) | ||||||
| Never married | 65.7 | 70.0 | 67.1 | 75.7 | 75.5 | 68.0 |
| Married | 18.8 | 16.1 | 16.4 | 13.5 | 15.4 | 15.2 |
| Formerly married | 15.5 | 13.9 | 16.4 | 10.8 | 9.2 | 16.9 |
| Race (%) | ||||||
| Other | 38.2 | 21.1 | 33.4 | 29.7 | 42.7 | 48.9 |
| White | 61.8 | 78.9 | 66.6 | 70.3 | 57.3 | 51.1 |
| Family income | 3.8 (0.06) | 3.8 (0.12) | 3.7 (0.11) | 3.2 (0.31) | 3.5 (0.10) | 3.4 (0.16) |
| Education (%) | ||||||
| Less than high school | 28.1 | 30.4 | 31.1 | 29.7 | 32.3 | 34.3 |
| High school | 34.2 | 35.4 | 36.3 | 37.8 | 34.4 | 40.4 |
| Some college | 37.7 | 34.3 | 32.6 | 32.4 | 33.3 | 25.3 |
| Age (%) | ||||||
| 18 to 20 years | 19.8 | 27.9 | 22.2 | 27.0 | 32.3 | 34.8 |
| 21 to 25 years | 40.0 | 44.3 | 37.2 | 35.1 | 42.2 | 32.0 |
| 26 to 34 years | 15.5 | 13.6 | 13.8 | 18.9 | 14.9 | 14.6 |
| 35 or older | 24.7 | 14.3 | 26.8 | 18.9 | 10.6 | 18.5 |
| Household size | 3.0 (0.04) | 3.1 (0.07) | 3.0 (0.07) | 3.2 (0.25) | 3.2 (0.06) | 3.3 (0.10) |
| N | 1,027 | 280 | 347 | 37 | 436 | 178 |
Note. NSDUH = National Survey of Drug Use and Health.
Standard errors for continuous variables in parentheses.
Depressants include any analgesics, tranquilizers, or sedatives used for nonmedical purposes.
Stimulants include cocaine, crack cocaine, amphetamines, and other stimulant used for recreational purposes.
Other includes hallucinogens and inhalants.
Table A2.
Logistic Regression Predicting Stigma as a Barrier to SU Treatment Among Those With Unmet Need. NSDUH, 2003-2010.
| Model 1 | ||
|---|---|---|
|
|
||
| OR | 95% CI | |
| Sex and parenthood status | ||
| Mothers | ||
| Fathers | 0.71+ | [0.31, 1.11] |
| Nonmothers | 0.64* | [0.20, 1.07] |
| Nonfathers | 0.51** | [0.09, 0.92] |
| Marital status | ||
| Married | ||
| Never married | 0.91 | |
| Formerly married | 0.70 | [0.53, 1.28] |
| Race | [0.24, 1.16] | |
| Other | ||
| White | 1.42* | |
| Family income | 1.15*** | [1.14, 1.69] |
| Education | [1.08, 1.21] | |
| Less than high school | ||
| High school | 1.40+ | |
| Some college | 2.47*** | [1.05, 1.76] |
| Age | [2.12, 2.82] | |
| 18 to 20 years | ||
| 21 to 25 years | 0.95 | |
| 26 to 34 years | 1.14 | [0.60, 1.31] |
| 35 or older | 0.79 | [0.69, 1.59] |
| Household size | 0.88* | [0.32, 1.27] |
| Model fit statistics | [0.75, 1.01] | |
| Model chi-square | 92 31*** | |
| Pseudo R2 | 0.058 | |
Note. NSDUH = National Survey of Drug Use and Health; SU = substance use; OR = odds ratio; CI = confidence interval.
p < .1.
p < .05.
p < .01.
p < .001.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Alang S. Are there disparities in causes of perceived unmet need for mental health care?. Paper presented at the Academy Health Annual Research Meeting; San Diego, CA. 2014. Jun, [Google Scholar]
- Allison PD. Missing data. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- American Academy of Pediatrics. Committee on substance abuse: Drug-exposed infants. Elk Grove Village, IL: Author; 1990. No. 0031-4005. [PubMed] [Google Scholar]
- American Medical Association. Treatment versus criminalization: Physician role in drug addiction during pregnancy. Chicago, IL: Author; 1990. [Google Scholar]
- American Psychiatric Association. Mental disorders: Diagnostic and statistical manual. Arlington, VA: Author; 1952. [Google Scholar]
- American Public Health Association. Illicit drug use by pregnant women. Washington, DC: Author; 1990. [Google Scholar]
- American Society of Addiction Medicine. Public policy statement on chemically dependent women and pregnancy. Chevy Chase, MD: Author; 2005. [Google Scholar]
- Anderson ML. Thinking about women: Sociological perspectives on sex and gender. 9th. Upper Saddle River, NJ: Prentice Hall; 2010. [Google Scholar]
- Barnard M, McKeganey N. The impact of parental problem drug use on children: What is the problem and what can be done to help? Addiction. 2004;99:552–559. doi: 10.1111/j.1360-0443.2003.00664.x. [DOI] [PubMed] [Google Scholar]
- Baumohl J, Speiglman R, Swartz JA, Stahl R. Substance abuse and welfare policy at the new century. Contemporary Drug Issues. 2003;30(Spring-Summer):501–537. [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Boyd SC. From witches to crack whores: Women, drug law, and policy. Rev. Durham: Carolina Academic Press; 2004. [Google Scholar]
- Brady TM, Ashley OS. Women in substance abuse treatment: Results from the Alcohol and Drug Services Study (ADSS) Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2005. [Google Scholar]
- Brown C, Conner KO, Copeland VC, Grote N, Beach S, Battista D, Reynolds CF. Depression stigma, race, and treatment seeking behavior and attitudes. Journal of Community Psychology. 2010;38:350–368. doi: 10.1002/jcop.20368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carricaburu D, Pierret J. From biographical disruption to biographical reinforcement: The case of HIV-positive men. Sociology of Health & Illness. 1995;17:65–88. [Google Scholar]
- Chervenak FA, McCullough LB. Legal intervention during pregnancy. Journal of the American Medical Association. 1991;265:1953. doi: 10.1001/jama.265.15.1953. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Cole J, Logan TK, Walker R. Social exclusion, personal control, self-regulation, and stress among substance abuse treatment clients. Drug and Alcohol Dependence. 2011;113:13–20. doi: 10.1016/j.drugalcdep.2010.06.018. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, Miller FE. Blame, shame, and contamination: The impact of mental illness and drug dependence stigma on family members. Journal of Family Psychology. 2006;20:239–246. doi: 10.1037/0893-3200.20.2.239. [DOI] [PubMed] [Google Scholar]
- Covington SS. Helping women recover: A comprehensive integrated treatment model. Alcohol Treatment Quarterly. 2000;18:99–111. [Google Scholar]
- Cunningham JA, Sobell LC, Chow VM. What's in a label? The effects of substance types and labels on treatment considerations and stigma. Journal of Studies on Alcohol. 1993;54:693–699. doi: 10.15288/jsa.1993.54.693. [DOI] [PubMed] [Google Scholar]
- David H, Demo DH, Acock AC. Family structure, family process, and adolescent well-being. Journal of Research on Adolescence. 1996;6:457–488. [Google Scholar]
- Epstein J. Substance dependence, abuse, and treatment: Findings from the 2000 National Household Survey on Drug Abuse. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2002. [Google Scholar]
- Erickson PG, Butters J, McGillicuddy P, Hallgren A. Crack and prostitution: Gender, myths, and experiences. Journal of Drug Issues. 2000;30:767–788. [Google Scholar]
- Ettorre E. Revisioning women and drug use: Gender, power and the body. Hampshire, England: Palgrave MacMillan; 2007. [Google Scholar]
- Fagan J. Women and drugs revisited: Female participation in the cocaine economy. Journal of Drug Issues. 1994;24:179–225. [Google Scholar]
- Frischknecht U, Beckmann B, Heinrich M, Kniest A, Nakovics H, Kiefer F, et al. Herman D. The vicious circle of perceived stigmatization, depressiveness, anxiety, and low quality of life in substituted heroin addicts. European Addiction Research. 2011;17:241–249. doi: 10.1159/000328637. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- Green CA. Gender and use of substance abuse treatment services. Alcohol Research and Health. 2006;29:55–62. [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatric Clinics of North America. 2010;33:339–355. doi: 10.1016/j.psc.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, et al. Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Stein JA, Weisner C, Chi F, Moos R. Predictors of longitudinal substance use and mental health outcomes for patients in two integrated service delivery systems. Drug and Alcohol Dependence. 2010;110:92–100. doi: 10.1016/j.drugalcdep.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty KP, Skinner M, Fleming CB, Gainey RR, Catalano RF. Long-term effects of the focus on families project on substance use disorders among children of parents in methadone treatment. Addiction. 2008;103:2008–2016. doi: 10.1111/j.1360-0443.2008.02360.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartwell S. Triple stigma: Persons with mental illness and substance abuse problems in the criminal justice system. Criminal Justice Policy Review. 2004;15:84–99. [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegarty P, Golden AM. Attributional beliefs about the controllability of stigmatized traits: Antecedents or justifications of prejudice? Journal of Applied Social Psychology. 2008;38:1023–1044. [Google Scholar]
- Heidensohn F. Gender and crime. In: Maguire M, Morgan R, Reiner R, editors. The Oxford handbook of criminology. 3rd. Oxford, England: Oxford University Press; 2002. pp. 457–490. [Google Scholar]
- Holmila M, Raitasalo K. Gender differences in drinking: Why do they still exist? Addiction. 2005;100:1763–1769. doi: 10.1111/j.1360-0443.2005.01249.x. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Wing S, McCarty D, Chappel J, Gallant L, Haberle B, et al. Weiss R. Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy. Journal of Substance Abuse Treatment. 2004;26:151–158. doi: 10.1016/S0740-5472(03)00212-5. [DOI] [PubMed] [Google Scholar]
- Jessup MA, Humphreys JC, Brindis CD, Lee KA. Extrinsic barriers to substance abuse treatment among pregnant drug dependent women. Journal of Drug Issues. 2003;33:285–304. [Google Scholar]
- Jones EE, Farina A, Hastorf AH, Markus H, Miller DT, Scott RA. Social stigma: The psychology of marked relationships. New York, NY: Freeman; 1984. [Google Scholar]
- Keyes KM, Hatzenbuehler ML, McLaughlin KA, Link B, Olfson M, Grant BF, Hasin D. Stigma and treatment for alcohol disorders in the United States. American Journal of Epidemiology. 2010;172:1364–1372. doi: 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klee H. Drug-using parents: Analysing the stereotypes. International Journal of Drug Policy. 1998;9:437–448. [Google Scholar]
- Kulesza M, Larimer ME, Rao D. Substance use related stigma: What we know and the way forward. Journal of Addictive Behaviors Therapy & Rehabilitation. 2013;2:782. doi: 10.4172/2324-9005.1000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam WKK, Cance JD, Eke AN, Fishbein DH, Hawkins SR, Williams JC. Children of African-American mothers who use crack cocaine: Parenting influences on youth substance use. Journal of Pediatric Psychology. 2007;32:877–887. doi: 10.1093/jpepsy/jsm015. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Ceballo R, Abbey A, Stewart AJ. Does family structure matter? A comparison of adoptive, two-parent biological, single-mother, stepfather, and stepmother households. Journal of Marriage and Family. 2001;63:840–851. [Google Scholar]
- Latkin C, Davey-Rothwell M, Yang Jy, Crawford N. The relationship between drug user stigma and depression among inner-city drug users in Baltimore, MD. Journal of Urban Health. 2013;90:147–156. doi: 10.1007/s11524-012-9753-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauster N, Easterbrook A. No room for new families? A field experiment measuring rental discrimination against same-sex couples and single parents. Social Problems. 2011;58:389–409. [Google Scholar]
- Link BG. Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review. 1987;52:96–112. [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review. 1989;54:400–423. [Google Scholar]
- Link BG, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: Can negative consequences of mental illness labeling be avoided? Journal of Health and Social Behavior. 1991;32:302–320. [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: Labels, causes, dangerousness, and social distance. American Journal of Public Health. 1999;89:1328–1333. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnemann T. Mad men, meth moms, moral panic: Gendering meth crimes in the Midwest. Critical Criminology. 2009;18:95–110. [Google Scholar]
- Lloyd C. The stigmatization of problem drug users: A narrative literature review. Drugs. 2013;20:85–95. [Google Scholar]
- Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: A qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLOS Medicine. 2011;8(11) doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loutfy M, Logie C, Zhang Y, Blitz S, Margolese S, Tharao W, et al. Raboud J. Gender and ethnicity differences in HIV-related stigma experienced by people living with HIV in Ontario, Canada. PLOS One. 2012;7(12) doi: 10.1371/journal.pone.0048168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JK, Pescosolido BA, Tuch SA. Of fear and loathing: The role of “disturbing behavior,” labels, and causal attributions in shaping public attitudes toward people with mental illness. Journal of Health and Social Behavior. 2000;41:208–223. [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Moore BC, Easton CJ, McMahon TJ. Drug abuse and intimate partner violence: A comparative study of opioid-dependent fathers. American Journal of Orthopsychiatry. 2011;81:218–227. doi: 10.1111/j.1939-0025.2011.01091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton KB, Martin PC, Chromy JR, Hirsch EL, Ridenhour JL. 2010 National Survey on Drug Use and Health sample design report. Research Triangle Park, NC: RTI International; 2011. [Google Scholar]
- Murphy AS. A survey of state fetal homicide laws and their potential applicability to pregnant women who harm their own fetuses. Indiana Law Journal. 2014;89 Retrieved from http://www.repository.law.indiana.edu/cgi/viewcontent.cgi?article=11110&context=ilj. [Google Scholar]
- Ojeda VD, Bergstresser SM. Gender, race-ethnicity, and psychosocial barriers to mental health care: An examination of perception and attitudes among adults reporting unmet need. Journal of Health and Social Behavior. 2008;49:317–334. doi: 10.1177/002214650804900306. [DOI] [PubMed] [Google Scholar]
- Osborne C, Berger LM. Parental substance abuse and child well-being: A consideration of parents' gender and coresidence. Journal of Family Issues. 2009;30:341–370. [Google Scholar]
- Palamar JJ. A pilot study examining perceived rejection and secrecy in relation to illicit drug use and associated stigma. Drug and Alcohol Review. 2012;31:573–579. doi: 10.1111/j.1465-3362.2011.00406.x. [DOI] [PubMed] [Google Scholar]
- Palamar JJ, Kiang MV, Halkitis PN. Development and psycho-metric evaluation of scales that assess stigma associated with illicit drug users. Substance Use & Misuse. 2011;46:1457–1467. doi: 10.3109/10826084.2011.596606. [DOI] [PubMed] [Google Scholar]
- Parks K, Scheidt D. Male bar drinkers' perspective on female bar drinkers. Sex Roles. 2000;43:927–941. [Google Scholar]
- Peralta RL, Jauk D. A brief feminist review and critique of the sociology of alcohol-use and substance-abuse treatment approaches. Sociology Compass. 2011;5:882–897. [Google Scholar]
- Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. American Journal of Public Health. 1999;89:1339–1345. doi: 10.2105/ajph.89.9.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Stueve A, Pescosolido BA. Public conceptions of mental illness in 1950 and 1996: What is mental illness and is it to be feared? Journal of Health and Social Behavior. 2000;41:188–207. [Google Scholar]
- Rae Olmsted KL, Brown JM, Vandermaas-Peeler JR, Tueller SJ, Johnson RE, Gibbs DA. Mental health and substance abuse treatment stigma among soldiers. Military Psychology. 2011;23:52–64. [Google Scholar]
- Saunders SM, Zygowicz KM, D'Angelo BR. Person-related and treatment-related barriers to alcohol treatment. Journal of Substance Abuse Treatment. 2006;30:261–270. doi: 10.1016/j.jsat.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Scambler G. Health-related stigma. Sociology of Health and Illness. 2009;31:441–455. doi: 10.1111/j.1467-9566.2009.01161.x. [DOI] [PubMed] [Google Scholar]
- Schmidt L, Tam T, Mj L. Understanding the substance abuse treatment gap. Washington, DC: Center for Substance Abuse Treatment, SAMHSA; 2007. [Google Scholar]
- Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol and Alcoholism. 2011;46:105–112. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
- Seljamo S, Aromaa M, Koivusilta L, Rautava P, Sourander A, Helenius H, Sillanpää M. Alcohol use in families: A 15-year prospective follow-up study. Addiction. 2006;101:984–992. doi: 10.1111/j.1360-0443.2006.01443.x. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Grant I, Patterson TL. Utilization of drug treatment programs by methamphetamine users: The role of social stigma. American Journal on Addiction. 2005;14:367–380. doi: 10.1080/10550490591006924. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software (Version 11) College Station, TX: Author; 2009. Computer software. [Google Scholar]
- Storbjörk J, Ullman S. A prospective study of mortality up to eight years after starting treatment for alcohol and drug problems in Stockholm County: 2000–2008. Addiction Research & Theory. 2012;20:402–413. [Google Scholar]
- Storholm ED, Halkitis PN, Kupprat SA, Hampton MC, Palamar JJ, Brennan-Ing M, Karpiak S. HIV-related stigma as a mediator of the relation between multiple-minority status and mental health burden in an aging HIV-positive population. Journal of HIV/AIDS & Social Services. 2013;12:9–25. doi: 10.1080/15381501.2013.767557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health. In: SAMSHA, editor. Inter-university Consortium for Political and Social Research (ICPSR) Rockville, MD: Author; 2004-2011. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Alcohol treatment: Need, utilization, and barriers. Rockville, MD: Author; 2009. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of national findings. Rockville, MD: Author; 2011. (NSDUH Series H-41). HHS Publication No. [SMA] 11-4658. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of national findings. Rockville, MD: Author; 2012. (NSDUH Series H-44). HHS Publication No. [SMA] 12-4713. [Google Scholar]
- Taylor OD. Barriers to treatment for women with substance use disorders. Journal of Human Behavior in the Social Environment. 2010;20:393–409. [Google Scholar]
- Title 39. General Assembly of the State of Tennessee. 2014 Retrieved from http://state.tn.us/sos/acts/108/pub/pc0820.pdf.
- Townsend L, Gearing RE, Polyanskaya O. Influence of health beliefs and stigma on choosing internet support groups over formal mental health services. Psychiatric Services. 2012;63:370–376. doi: 10.1176/appi.ps.201100196. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Simpson CA. The recovery spectrum: From self-change to seeking treatment. Alcohol Research & Health. 2011;33:371–379. [PMC free article] [PubMed] [Google Scholar]
- VanDeMark NR, Russell LA, O'Keefe M, Finkelstein N, Noether CD, Gampel JC. Children of mothers with histories of substance abuse, mental illness, and trauma. Journal of Community Psychology. 2005;33:445–459. [Google Scholar]
- Walsh C, MacMillan HL, Jamieson E. The relationship between parental substance abuse and child maltreatment: Findings from the Ontario health supplement. Child abuse & Neglect. 2003;27:1409–1425. doi: 10.1016/j.chiabu.2003.07.002. [DOI] [PubMed] [Google Scholar]
- White WL, Evans AC, Lamb R. Reducing addiction related social stigma. Counselor. 2009;10:52–58. [Google Scholar]
- Woodward A, Epstein J, Gfroerer J, Melnick D, Thoreson R, Willson D. The drug abuse treatment gap: Recent estimates. Health Care Financing Review. 1996;18(3):5–17. [PMC free article] [PubMed] [Google Scholar]
- Worrall A. Rendering women punishable: The making of a penal crisis. In: Carlen P, editor. Women and Punishment: The struggle for justice. Cullompton, England: Willan; 2002. pp. 47–56. [Google Scholar]
- Wu LT, Ringwalt CL. Alcohol dependence and use of treatment services among women in the community. American Journal of Psychiatry. 2004;161:1790–1797. doi: 10.1176/appi.ajp.161.10.1790. [DOI] [PMC free article] [PubMed] [Google Scholar]


