Abstract
We explore if the geographic variation in excess body-mass in Norway can be explained by socioeconomic status, as this has consequences for public policy. The analysis was based on individual height and weight for 198,311 Norwegian youth in 2011, 2012 and 2013, stemming from a compulsory screening for military service, which covers the whole population aged seventeen. These data were merged with municipality-level socioeconomic status (SES) variables and we estimated both ecological models and two-level models with a random term at the municipality level. Overweight was negatively associated with income, education and occupation at municipality level. Furthermore, the municipality-level variance in overweight was reduced by 57% in females and 40% in males, when SES factors were taken into account. This suggests that successful interventions aimed at reducing socioeconomic variation in overweight will also contribute to reducing the geographic variation in overweight, especially in females.
Keywords: Overweight, Body mass index, Socioeconomic factors, Neighborhood, Multilevel modeling, Geographic factors, Norway
Highlights
-
•
Overweight at the age of 17 is negatively associated with area-level SES in Norway.
-
•
SES could explain roughly half of the geographic variation in overweight in Norway.
-
•
SES factors were more important for geographic variation in overweight in females, than males.
1. Introduction
Worldwide, the proportion of overweight adults has increased from 29% among men and 30% among women in 1980 to 37% and 38%, respectively, in 2013 (Ng et al., 2014). Every second type II diabetes case, every fifth ischemic heart disease case and more than every third of certain types of cancers are attributable to excess body weight (WHO, 2000). The rise in overweight is not only limited to developed countries; overweight is now a problem among all age groups in developing countries as well (Ng et al., 2014).
There are considerable geographic variations in overweight within many countries. In Norway, the share of youth considered overweight varied between 14.8% and 28.3% across the 19 counties in 2013 (Norwegian Institute of Public Health, 2015). Like the geographic variation in other health outcomes, such geographic variations in overweight has received considerable attention and puzzled researchers, politicians and policy makers (Bjerkedal & Brevik, 2001; Department of Health (UK), 2004; Jullumstro & Eide, 2013; Norwegian Ministry of Health and Care Services, 2012; Smyth, 2015). Some countries have also introduced measures to reduce geographic variation in health. For example, in the UK the Government has set a Public Service Agreement target to address geographical inequalities in life expectancy, cancer, heart disease, stroke and related diseases (Department of Health, 2004). Also in Norway the municipalities, which are responsible for local public health, are obliged to keep an eye on geographical differences and suggest interventions when needed (Norwegian Ministry of Health and Care Services, 2012). However, an important question is whether steps could or should be taken to reduce the geographic variation in overweight, and the answer depends on the type of factors that contribute to it.
The aim of this paper is to contribute to this discussion by estimating how much of the geographic variation in overweight in Norway is explained by three indicators of socioeconomic resources (income, education, and occupational status), which in a number of studies have been associated with overweight. More specifically we estimate multilevel models with a random term at the municipality level and study how its variance is reduced when SES indicators are added. To our awareness such a study has not been carried out in any country earlier.
If socioeconomic factors contribute substantially to geographic variation in overweight, the implication is that reduction of SES variation in overweight – which is an important health policy goal in Norway and many other countries – will also reduce the geographic variation. For example, nationwide income supplementation to relatively poor people or general initiatives to reduce school dropout would also reduce the geographic variation. Conversely, if SES does not explain much of the geographic variation in overweight, it must be the result of other factors such as other individual characteristics (e.g. attitudes), neighborhood green space (Astell-Burt, Feng, & Kolt, 2014), or other aspects of the environment (unchangeable or man-made) not entirely determined by the SES of the population (e.g. fast food restaurants). Interventions to reduce the geographic differences would then have to be different from interventions aimed at reducing socioeconomic health inequalities.
We consider the socioeconomic resources in the municipality, indicated by average income, average education and occupational status. Information about corresponding individual level characteristics are not available. The associations between municipality-level socioeconomic resources and an individual's overweight will reflect two effects: first, own (or, for young people, parents’) SES may have an impact on an individual's weight; second, there may be an effect of the SES in the municipality on individual weight. As explained below, separation of those two contributions would be of some value from a policy perspective, but the data available to us did not allow this.
2. Data and methods
2.1. Data
Our study was based upon individual-level (but anonymized) data on height and weight of the Norwegian youth in 2011, 2012 and 2013. Height and weight was self-reported and supplied in an internet based military muster from the Norwegian Armed Forces. Since 2010 it has been compulsory for Norwegian citizens to provide this information, as part of a large questionnaire during the year they turn 17 (Fauske, 2011). Hence, the response rate is as high as 97%1. Individuals who become Norwegian citizens after the age of 17 years and individuals who do not finish school on time can fill out the form at an older age. We excluded all individuals who were over the age of 18 when answering the questions about height and weight (1.3% of females and 3.5% of males). Our study population comprised 90,568 females and 107,743 males2. We also have access to information about the individual's municipality of residence.
2.2. Variables
The dependent variable was overweight, defined as the body mass index (BMI, weight in kilograms divided by height in meters squared) being above 25 in adults. This limit accords with World Health Organization guidelines (World Health Organization, 1995). However, body mass changes substantially with age and our population consisted of individuals aged 16-18. Hence, we used age- and sex-specific overweight cut-off values to account for changing interpretation of BMI by age and sex in younger age groups (Cole, Bellizzi, Flegal, & Dietz, 2000).
The level of aggregation was the Norwegian municipalities, as defined the 1st of January 2014, and the analysis encompassed all 428 municipalities in the country. As recommended by Galobardes, Lynch, and Smith (2007), we included three aggregate measures to reflect the socioeconomic conditions in the area.These are median gross income in 2012, the share of the population above the age of 16 with college or university education in 2012, and the share of the population aged 15–74 who were in leading positions3 in 2012. A number of previous studies have demonstrated that the associations between income and health behaviors are non-linear (Ecob and Smith, 1999, Ettner, 1996), so we grouped the income variable into five categories.
As covariates we also include the share of the population aged 16–66 and the square root of the population size4. The reason for including population size is that it is a reasonable indicator of the degree of urbanity, which is positively associated with income. Living in an urban area has also been found to be negatively associated with the prevalence of overweight (Biehl et al., 2013). The age structure may affect the share of the population who are employed, and thus the average income in the population. Additionally, BMI tends to vary by age (Flegal, Carroll, Kuczmarski, & Johnson, 1998), which then again may have an impact on our sample through peer-effects (Trogdon, Nonnemaker, & Pais, 2008).
It is likely that the effects of socioeconomic factors on overweight may vary across the sexes. The possibility of such variation has rarely been analyzed from a multilevel perspective (Wen & Maloney, 2014). A few studies have indicated that women, on the whole, may be more influenced by area-level contexts than men (King, Kavanagh, Jolley, Turrell, & Crawford, 2006). However, other studies have found stronger associations between composite measures of neighborhood disadvantage and mortality among men than among women (Kravdal, 2010). We ran a Chow test based on a logit model and found that the coefficients (both at the individual- and area-level) varied significantly by sex. This further supports sex-stratified analyses.
Finally, we controlled for 1-year age groups at the individual level and response year.
2.3. Statistical analysis
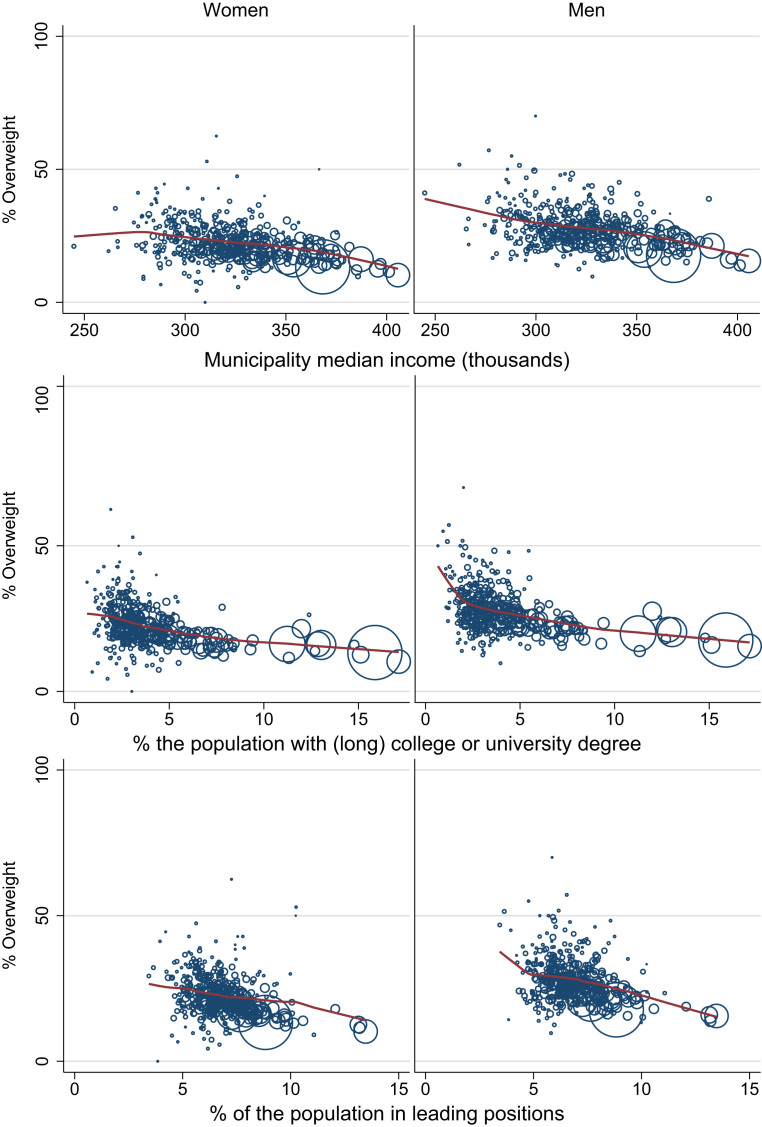
In the first step, we generated descriptive graphs of the associations between overweight prevalence in the municipality and the three socioeconomic variables, based on locally weighted regressions with a bandwidth of 0.8 to place less emphasis on the outliers.
In the second step, we estimated two-level logistic models, where the dependent variable was the binary overweight variable at the individual level. The models were of the form:
| (1) |
where i indexes the individuals, j indexes the 428 municipalities, y is the overweight status for individual i in municipality j, A is the age group, and T response year. X is a vector of the municipality-level variables. Ϛj is a random intercept which is assumed to be independent across municipalities’ j and independent of the other covariates in the models. The variance of this random term is a measure of the between-municipality variation in the dependent variable, which is not explained by the variables included in the model. We estimate the proportional change in the variance (PCV) by the formula (Merlo et al., 2006):
where VA is the variance of the random term in the initial model and VB is the corresponding variance in the expanded model. The PCV expresses how much of the variation in overweight across municipalities that can be explained by the additional covariates included in the expanded model.
We report marginal effects (ME) based on each regression. These were calculated for each variable fixing the other variables at their whole sample mean values. Furthermore, the municipality-level random effects were all set to zero, i.e. the MEs for each variable were calculated for an average municipality.
3. Results
Overweight was more common among males than among females (Table 1). The mean number of respondents per municipality was lower among the overweight compared with non-overweight; however, no difference was found by age. In both females and males, the overweight prevalence was higher in 2013 than in 2011 and 2012. Those who were overweight generally came from municipalities with lower income, lower education and fewer in leading positions. In addition, overweight was more common in municipalities with smaller populations.
Table 1.
Summary statistics of the estimation sample.
| Females | Males | |||
|---|---|---|---|---|
| BMI groups | Non-OW | OW | Non-OW | OW |
| Number | 73,323 | 17,245 | 81,728 | 26,015 |
| % | 80.96 | 19.04 | 75.85 | 24.15 |
| Mean number of respondents per municipality | 3164.2 | 2451.5 | 3116.3 | 2439.5 |
| Age (mean) | 16.8 | 16.8 | 17.0 | 17.0 |
| Response year by BMI group (%) | ||||
| 2011 | 81.8 | 18.2 | 76.0 | 24.0 |
| 2012 | 80.8 | 19.2 | 77.4 | 22.6 |
| 2013 | 80.2 | 19.8 | 74.4 | 25.6 |
| Municipality level variables | ||||
| Share of the population aged 16-66 | 0.677 | 0.673 | 0.677 | 0.673 |
| Median income | 342,696 | 337,355 | 342,353 | 337,640 |
| Share of the population with high education | 0.072 | 0.062 | 0.071 | 0.062 |
| Share of the population in leading positions | 0.077 | 0.074 | 0.077 | 0.074 |
| Mean municipality population | 98,782 | 74,091 | 97,179 | 73,865 |
OW: overweight.
Fig. 1 displays the smoothed value from the locally weighted regressions of the associations between percent overweight at the municipality level and each of the SES variables. Fig. 1 also displays bubble-plots where the size of the bubbles correspond with the population size in the municipality.
Fig. 1.
municipality-level overweight on municipality-level characteristics from locally weighted regressions.
We observe first that there were negative associations between the share of the population who were overweight and the median income at the municipality level, the share of the population with a university degree, and the share of the population in leading positions (Fig. 1). Furthermore, the municipalities with the largest populations (the largest circles) were also the populations with the highest incomes, most educated populations and greatest share in leading positions. Correspondingly, the inhabitants in the municipalities with the largest populations were also less overweight, both among males and females at the age of 16–18. Finally, we observe that the patterns in each figure were similar in females and males, i.e. those municipalities that had low prevalence of overweight in females also had low prevalence in males, and vice versa.
In model 1 – adjusted for individual age, age structure in the municipality and population size- the variance of the municipality random term was 0.038 in females and 0.042 in males (Table 2). Two-thirds of the observations in a normal distribution are between one standard deviation below and one standard deviation above the average. These results therefore mean that 1/3 of the population live in municipalities where the log odds of overweight was more than about √(0.04) below or above the average, i.e. where the overweight probability was more than about 20% below or above the average.
Table 2.
Variance of the municipality-level random term from two-stage regressions in females and males.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variance | p-Value | Variance | p-Value | Variance | p-Value | Variance | p-Value | Variance | p-Value | |
| Females | ||||||||||
| Variance of the municipality level random term | 0.03765 | <0.001 | 0.02764 | <0.001 | 0.02485 | <0.001 | 0.01756 | <0.001 | 0.01636 | <0.001 |
| Proportional change in variance (PCV) | 26.59% | 34.00% | 53.37% | 56.56% | ||||||
| Males | ||||||||||
| Variance of the municipality level random term | 0.04174 | <0.001 | 0.03281 | <0.001 | 0.02844 | <0.001 | 0.02934 | <0.001 | 0.02509 | <0.001 |
| Proportional change in variance (PCV) | 21.40% | 31.87% | 29.72% | 39.88% | ||||||
Model 1 covariates: age, response year, share of the population aged 16-66, and population (squared).
Model 2 covariates: age, response year, share of the population aged 16-66, population (squared), and median income.
Model 3 covariates: age, response year, share of the population aged 16-66, population (squared), and share of the population with high education.
Model 4 covariates: age, response year, share of the population aged 16-66, population (squared), and share of the population in leading positions.
Model 5 covariates: age, response year, share of the population aged 16-66, population (squared), median income, share of the population with high education, and share of the population in leading positions.
When SES variables were added (alone) in model 2, 3 and 4, the municipality random term decreased for both sexes. In females the “share in leading positions” had the largest impact on the variation in overweight across municipalities, by reducing the variation with 53%. In males, the “share with high education” was most important as it reduced variation in overweight by 32%. In both females and males, median income was the least important variable in terms of explaining geographic variation in overweight in Norway. The three SES variables were included jointly in model 5 (Table 2). Fifty-seven percent of the variance in overweight across municipalities -among females- could be explained by the three SES variables. In males the corresponding proportion was 40%.
Table 3 shows the marginal effects (ME), which were calculated based on the two-level logit model. The ME for the categorical variables (i.e. age, response year, median income) shows the discrete change from base level (reference category). The ME for the continuous variables (i.e. population age, population (squared), share with high income and share in leading positions) shows the change when the continuous variables change by one unit.
Table 3.
Marginal effects of the individual level and municipality-level characteristics from two-stage regressions in females and males.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | p-Value | Coef. | p-Value | Coef. | p-Value | Coef. | p-Value | Coef. | p-Value | |
| Females | ||||||||||
| Age | ||||||||||
| 16 | Base group | Base group | Base group | Base group | Base group | |||||
| 17 | −0.00688 | 0.025 | −0.00702 | 0.023 | −0.00690 | 0.025 | −0.00694 | 0.025 | −0.00700 | 0.024 |
| 18 | 0.02480 | <0.001 | 0.02477 | <0.001 | 0.02467 | <0.001 | 0.02473 | <0.001 | 0.02465 | <0.001 |
| Response year | ||||||||||
| 2011 | Base group | Base group | Base group | Base group | Base group | |||||
| 2012 | 0.01074 | 0.001 | 0.01073 | 0.001 | 0.01078 | 0.001 | 0.01089 | 0.001 | 0.01085 | 0.001 |
| 2013 | 0.01692 | <0.001 | 0.01693 | <0.001 | 0.01694 | <0.001 | 0.01707 | <0.001 | 0.01702 | <0.001 |
| Municipality level variables | ||||||||||
| Share of the population aged 16–66 | −0.30903 | 0.011 | −0.06000 | 0.632 | −0.15204 | 0.183 | −0.15028 | 0.163 | −0.03723 | 0.748 |
| Population (squared) | −0.00019 | <0.001 | −0.00014 | <0.001 | −0.00002 | 0.504 | −0.00012 | <0.001 | −0.00007 | 0.034 |
| Median income | ||||||||||
| Low | Base group | Base group | ||||||||
| Medium low | −0.01067 | 0.077 | −0.00655 | 0.214 | ||||||
| Medium | −0.02194 | 0.001 | −0.01244 | 0.030 | ||||||
| Medium high | −0.02734 | 0.002 | −0.01113 | 0.171 | ||||||
| High | −0.05547 | <0.001 | −0.01993 | 0.035 | ||||||
| Share of the population with high educ. | −0.81747 | <0.001 | −0.29239 | 0.034 | ||||||
| Share of the population in leading pos. | −1.33920 | <0.001 | −0.88939 | <0.001 | ||||||
| Males | ||||||||||
| Age | ||||||||||
| 16 | Base group | Base group | Base group | Base group | Base group | |||||
| 17 | −0.02982 | <0.001 | −0.02992 | <0.001 | −0.02997 | <0.001 | −0.03006 | <0.001 | −0.03007 | <0.001 |
| 18 | −0.00127 | 0.777 | −0.00140 | 0.757 | −0.00165 | 0.714 | −0.00174 | 0.700 | −0.00179 | 0.692 |
| Response year | ||||||||||
| 2011 | Base group | Base group | Base group | Base group | Base group | |||||
| 2012 | −0.01187 | <0.001 | −0.01191 | <0.001 | −0.01188 | <0.001 | −0.01183 | <0.001 | −0.01188 | <0.001 |
| 2013 | 0.01740 | <0.001 | 0.01745 | <0.001 | 0.01750 | <0.001 | 0.01760 | <0.001 | 0.01757 | <0.001 |
| Municipality level variables | ||||||||||
| Share of the population aged 16-66 | −0.14477 | 0.285 | 0.13447 | 0.337 | 0.03110 | 0.806 | 0.00328 | 0.980 | 0.15655 | 0.240 |
| Population (squared) | −0.00024 | <0.001 | −0.00019 | <0.001 | −0.00004 | 0.344 | −0.00018 | <0.001 | −0.00007 | 0.069 |
| Median income | ||||||||||
| Low | Base group | Base group | ||||||||
| Medium low | −0.00354 | 0.600 | 0.00010 | 0.987 | ||||||
| Medium | −0.01773 | 0.014 | −0.00815 | 0.228 | ||||||
| Medium high | −0.03735 | <0.001 | −0.01861 | 0.053 | ||||||
| High | −0.05578 | <0.001 | −0.01840 | 0.112 | ||||||
| Share of the population with high educ. | −0.98829 | <0.001 | −0.58650 | 0.001 | ||||||
| Share of the population in leading pos. | −1.21166 | <0.001 | −0.52766 | 0.022 | ||||||
Age was significantly and negatively associated with the probability of individual overweight in females and males in each model 1–5 (Table 3). In both females and males those who responded in 2013 were significantly more likely to be overweight than those who responded in 2011. Median income was significantly and negatively associated with overweight (Model 2; Table 3). Overweight was also significantly associated with education and share in leading positons at the municipality level (Model 3–4; Table 3). When all SES variables were included in Model 5 both the share with high education and the share in leading positions remained significant.
To explore the robustness of the findings we repeated our analysis with a few modifications. First, in the multilevel approach larger municipalities contributes more to the estimated variance compared with the smaller municipalities. To explore whether or not our findings were strongly influenced by the large municipalities, we omitted the five largest municipalities and reran the models. The variation explained by SES -in the model including all SES variables (model 5)- was 48% in females and 37% in males. Second, we ran models with share living in urban areas as a control variable instead of population size. This did not alter our findings. Third, we grouped the education variable and the occupational status variable to allow for non-linear effects, which had little or no impact on the estimated variances. Fourth, we entered a number of additional SES variables like unemployment rate, mean income and education stratified by sex. More of the random term was explained when more SES variables were included. However, these models also suffered from multicollinearity (resulting in wide confidence intervals and big changes in the values and signs of the coefficients when additional variables were entered into the model), which made the interpretation of the coefficients difficult.
Finally, gestation and early infancy are critical periods for health and overweight development in adolescence and adulthood (Currie and Almond, 2011, Dietz, 1994). To explore this association we ran models controlling for median income and mean education in the municipality at the time when each individual was born5. We did not have information corresponding about occupational status at birth. In females, inclusion of income at birth reduced the variance in overweight with 27%, which was almost identical to the reduction observed when income in 2012 was added. Inclusion of education at birth reduced the variance in overweight in females with 32%, compared with 34% when education in 2012 was added. In men, the corresponding numbers were 26% at birth and 21% in 2012, 29% for education at birth and 32% for education at in 2012. Finally, we ran models including all SES variables at the time of birth and in 2012. In females, 59% of the variance was explained, compared with 57% in the models including SES in 2012 only. In men, the comparable numbers were 41% and 40%, respectively.
4. Discussion
We found negative and significant associations between overweight and education at the municipality level in Norway among both females and males. Similar negative associations were found for occupation and median income at the municipality level. The study also showed that these three socioeconomic variables in total could explain 57% and 40% of the variation in overweight across municipalities in females and males, respectively.
The association between individual body mass index and area-level socio-economic resources supports findings reported in previous studies. A number of these studies have used composite indicators of SES (Adams et al., 2009, Chen and Truong, 2012, Do et al., 2007, Feng and Wilson, 2015, Sundquist et al., 1999, Wen and Maloney, 2014), while other studies have looked specifically at area-level income (Cetateanu and Jones, 2014, King et al., 2006), area-level education (Harrington & Elliott, 2009) or area-level occupational status (Cetateanu & Jones, 2014). A Canadian study, which included school-aged children, used individual-level SES variables in addition to area-level income, occupation and education. This study found that both individual- and area-level SES variables were negatively associated with individual BMI (Janssen, Boyce, Simpson, & Pickett, 2006). However, the mentioned studies explore the associations between high BMI and area-level SES; they do not estimate how much of the geographic variation in high BMI that could be explained by SES. To our awareness, our study provides the first estimates of this.
The study was based on an extensive register data source, which provided information on height and weight among women and men in 428 Norwegian municipalities. However, there are limitations that need to be taken into consideration when interpreting the findings. First, our measure of overweight was based on BMI, which has been criticized because it does not incorporate measures of body fat, which is an independent predictor of ill health (Burkhauser & Cawley, 2008). Second, and related to this, there may be measurement errors: if BMI is mis-measured (as it was based on self-reported height and weight), and if the level of mis-measurement is associated with SES, our coefficients might be biased. Finally, there may be reverse causality and omitted variables, either at the individual- or area-level, and the implications of this are discussed in more detail below.
4.1. Potential mechanisms explaining the findings
It is reasonable to assume that the environmental factors linking SES and overweight largely reflect differences in diet6 and physical activity7 (Janssen et al., 2006). The possible pathways are reviewed below, with attention both to the effects of individual (parental) SES and those of area-level SES (net of individual SES). As mentioned, we pick up both types of effects when municipality-level SES is included alone.
4.1.1. Effect of individual (parents) level SES
A number of studies considering the importance of individual-level SES have found high-BMI to be associated with income, education and occupation (Biehl et al., 2013, Elstad, 2013, Kinge et al., 2015, McLaren, 2007). Income could affect BMI, for example by affecting resources available to buy certain types of food and to participate in leisure-time physical activities. Furthermore, a number of studies have suggested that education enables people to integrate healthy behaviors into their daily routine, which may give them better health outcomes, and educated people are also more likely to pass on healthy habits to their children (Atella and Kopinska, 2014, Laitinen et al., 1995, Mirowsky and Ross, 1998). Also occupation has been argued to influence body mass, as low status jobs are often associated with lack of autonomy, which might for example make it difficult to manage time effectively to adopt a healthy lifestyle (Wardle, Waller, & Jarvis, 2002). This may further contribute to different ideals for body weight depending on occupational status (McLaren, 2007).
4.1.2. Effect of area-level SES
A number of studies on dietary choices and physical activity suggest that there is an effect of area-level SES variables net of individual characteristics. Area-level SES may have an impact on individual behavior by setting the social norm for health behaviors and then influence all individuals in the area. In addition, area-level SES may have implications for the built and institutional environment, which then again influence the behavior of most individuals in an area.
One such factor might be decreased neighborhood opportunities for physical activity in low-SES areas (Black and Macinko, 2008, Kavanagh et al., 2005), (Gordon-Larsen, Nelson, Page, & Popkin, 2006), (Wilson, Kirtland, Ainsworth, & Addy, 2004). A number of studies have also found diet, e.g. consumption of sweets and soft drinks, to be influenced by area SES. (Janssen et al., 2006), (Shohaimi et al., 2004, Turrell et al., 2004), (Diez-Roux et al., 1999).
More of the geographic variation could be explained by SES among women than men (according to a comparison of point estimates). This supports studies which suggest a stronger connection between neighborhood socioeconomic capital for women than for men (Do et al., 2007). Moreover, some researchers have hypothesized that the neighborhood environment may be generally more important for women than for men (King et al. 2006), as women traditionally spent more time in the home and were thus more exposed to the neighborhood (Robert, 1999). Such effects might be less relevant in our case, and when it comes to neighborhood SES in particular, findings have been mixed. Indeed, some authors have concluded that effects on mortality may be strongest among men (Kravdal 2010). Thus, it was not obvious what one should expect to find with respect to the importance of municipality SES for overweight, and with a focus on proportion explained (compared to other factors that include other types of community characteristics), predictions would be even harder to make.
4.2. Implications and suggestions for further research
Our findings suggest that SES contribute much to the geographic variation in overweight. Leaving aside the possibility of endogeneity problems,8 this means that socioeconomic resources are important determinants of overweight and are distributed unevenly across the country. Hence, successful attempts to reduce the socioeconomic variation will also reduce the geographic variation.
If it is a goal to reduce the social variation in overweight, and if low individual income and education are important determinants of overweight, interventions to prevent high-school drop-out or move people out of poverty – regardless of geographic location– may be effective measures. One could also try to reduce the effect of having low education or income, for example by providing certain health-promoting goods to individuals in low SES groups. Successful interventions of these two types will necessarily have a larger impact on overweight rates in areas where incomes and educational levels tend to be low and overweight therefore most common. In other words, the geographic variation will automatically be reduced.
The motive behind such attempts to reduce socioeconomic variation in overweight, through general interventions that are not specially targeted towards low-SES areas, would be that the returns to interventions would be just as good in the less disadvantaged areas. Stated differently, by helping the same number of people with the same low education and income in high SES areas, one could achieve as much in terms of less overweight. However, this argument would not hold if more people could be helped for the same amount of money in the most disadvantaged areas, for example because of scale advantages in poverty reduction. In that case, it would make good sense to steer some of the efforts to reduce social variation specifically towards low-SES areas, and if that is done, the geographic variation would be even more strongly reduced than if the efforts to reduce the social variation are not geographically targeted in this way.
Similarly, if overweight instead is influenced by the socioeconomic resources in the community rather than of the individual, it would be sound from a social equality perspective to direct interventions towards the low-SES areas in particular. The reduction in overweight might be as good if similar initiatives were taken elsewhere, but one would then support people that were not in quite as bad situation at the outset. Our data did not allow us to assess the importance of individual- versus community-level effects.9
To summarize, successful attempts to reduce social inequalities in high body mass would also lead to smaller geographic variation, especially if the interventions to some extent are targeted towards low-SES areas.
This argument hinges on the assumption that the estimates reflect causal effects of SES and not that some factors influence both SES and overweight. Though it would be valid, in theory, also if a change in SES for some reason is accompanied by corresponding changes in these factors. We control for population size and age structure, however there are potential omitted variables that could explain our findings. These are first, individual factors such as chronic conditions or discount rate (the rate of time preference) (Komlos et al., 2004, Morris, 2007), which may both affect the BMI of individuals and also their employment status. And second, omitted area variables such as the local schools, which may influence children's diet and body mass in addition to later life SES (Eide and Showalter, 1998, Jaime and Lock, 2009, Simon et al., 2008). Hence, a challenge for further research could be to exogenously identify variation in the socioeconomic factors to explore its impact on overweight across and within areas.
The other main message from this study is that roughly half of the geographic variation in Norway could not be explained by income, education and occupation. The unexplained part could be a result of other population characteristics, such as attitudes, and marital status, operating either at the individual- or aggregate level. In addition, it could be explained by the built environment (not entirely determined by the socioeconomic resources) like the availability of parks and bike lanes. Finally, it could be explained by the unchangeable physical environment (Kravdal et al., 2015), latitude and distance from the sea (affecting e.g. local food traditions) being examples. Hence, to fully understand geographic variation in overweight, more research needs to be done to explore the consequences of including other variables than SES in these models.
To conclude, income, education and occupation were important variables for explaining geographic variation in overweight (among women in particular). This is important from a health policy perspective, as it means that interventions to reduce social inequalities in overweight most likely also will help to reduce the geographic inequalities.
Footnotes
This number was obtained from personal communication with staff at the Norwegian Armed Forces.
A few individuals answered the question about height and weight twice (at 17 and 18). However, we do not have the opportunity to correct for this in our data. To check whether or not this has an impact on our results we reran the analysis, excluding those who are 18. It does not alter the findings and we kept the 18-year olds in our analyses.
Leading positons are here defined according to the Norwegian Standard for Classification of Occupations (STYRK). All codes that start with the number 1 are leading positions or politicians.
Some of the data used in this publication are based on the Norwegian Social Science Data Services Municipality Database. The Norwegian Social Science Data Services is not responsible for data analysis or interpretation done here.
The birth year varied across the sample. To avoid that these variables were affected by changes across time in relative level of education and income, we included the income and education in 1995 for all individuals. This was the median birth year in the sample.
Strict definitions of diets that contribute to overweight are hard to find, though there is much knowledge about dietary choices that increase the likelihood of weight gain. For example, the consumption of energy-dense and high-fat diets, beverages containing high amounts of sugar, large portion sizes and fast food have been associated with high BMI (Black and Macinko, 2008, The Norwegian Directorate of Health, 2015)
Physical activity is the only way to increase caloric expenditure that can be modified through behavior (Black & Macinko, 2008). National authorities encourage individuals to engage in regular physical activity at least 30 minutes per day. However, to maintain a healthy weight after weight reduction the advice is 60–90 min per day (The Norwegian Directorate of Health, 2015).
Caused by, for example, factors that affect both SES and BMI.
Even if information on individual socioeconomic resources were available, separation of these two types of effects would be difficult not least because of unobserved individual characteristics affecting the chance of moving to or remaining in low-SES areas, and because the resources in the community have implications in the longer run for the individual resources.
Contributor Information
Jonas Minet Kinge, Email: Jonas.Minet.Kinge@fhi.no.
Ólöf Anna Steingrímsdóttir, Email: OlofAnna.Steingrimsdottir@fhi.no.
Bjørn Heine Strand, Email: BjornHeine.Strand@fhi.no.
Øystein Kravdal, Email: oystein.kravdal@econ.uio.no.
References
- Adams R.J., Howard N., Tucker G., Appleton S., Taylor A.W., Chittleborough C.…Wilson D.H. Effects of area deprivation on health risks and outcomes: a multilevel, cross-sectional, Australian population study. International Journal of Public Health. 2009;54(3):183–192. doi: 10.1007/s00038-009-7113-x. [DOI] [PubMed] [Google Scholar]
- Astell-Burt T., Feng X., Kolt G. Greener neighborhoods, slimmer people? Evidence from 246 920 Australians. International Journal of Obesity. 2014;38(1):156–159. doi: 10.1038/ijo.2013.64. [DOI] [PubMed] [Google Scholar]
- Atella V., Kopinska J. Body weight, eating patterns, and physical activity: the role of education. Demography. 2014;51(4):1225–1249. doi: 10.1007/s13524-014-0311-z. [DOI] [PubMed] [Google Scholar]
- Biehl A., Hovengen R., Grøholt E.-K., Hjelmesæth J., Strand B.H., Meyer H.E. Adiposity among children in Norway by urbanity and maternal education: a nationally representative study. BMC Public Health. 2013;13(1):842. doi: 10.1186/1471-2458-13-842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjerkedal T., Brevik J.I. [Geographic variation in body mass index measured among men born in Norway between 1967 and 1980] Tidsskrift for Den Norske Laegeforening. 2001;121(30):3505–3508. [PubMed] [Google Scholar]
- Black J.L., Macinko J. Neighborhoods and obesity. Nutrition Reviews. 2008;66(1):2–20. doi: 10.1111/j.1753-4887.2007.00001.x. [DOI] [PubMed] [Google Scholar]
- Burkhauser R.V., Cawley J. Beyond BMI: the value of more accurate measures of fatness and obesity in social science research. Journal of Health Economics. 2008;27(2):519–529. doi: 10.1016/j.jhealeco.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Cetateanu A., Jones A. Understanding the relationship between food environments, deprivation and childhood overweight and obesity: evidence from a cross sectional England-wide study. Health & Place. 2014;27:68–76. doi: 10.1016/j.healthplace.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D.-R., Truong K. Using multilevel modeling and geographically weighted regression to identify spatial variations in the relationship between place-level disadvantages and obesity in Taiwan. Applied Geography. 2012;32(2):737–745. [Google Scholar]
- Cole, T. J., Bellizzi, M. C., Flegal, K. M., & Dietz, W. H. (2000). Establishing a standard definition for child overweight and obesity worldwide: international survey, 320. [DOI] [PMC free article] [PubMed]
- Currie J., Almond D. Human capital development before age five. Handbook of Labor Economics. 2011;4:1315–1486. [Google Scholar]
- Department of Health . Department of Health; 2004. Tackling health inequalities: the spearhead group of Local authorities and primary care trusts. [Google Scholar]
- Department of Health (UK) Department of Health; London: 2004. Reid announces'Spearhead’ PCTs to tackle health inequalities. [Google Scholar]
- Dietz W.H. Critical periods in childhood for the development of obesity. The American Journal of Clinical Nutrition. 1994;59(5):955–959. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- Diez-Roux A.V., Nieto F.J., Caulfield L., Tyroler H.A., Watson R.L., Szklo M. Neighbourhood differences in diet: the Atherosclerosis Risk in Communities (ARIC) Study. Journal of Epidemiology and Community Health. 1999;53(1):55–63. doi: 10.1136/jech.53.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do D.P., Dubowitz T., Bird C.E., Lurie N., Escarce J.J., Finch B.K. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using the NHANES III survey (1988–1994) Economics Human Biology. 2007;5(2):179–203. doi: 10.1016/j.ehb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecob R., Smith G.D. Income and health: what is the nature of the relationship? Social Science & Medicine. 1999;48(5):693–705. doi: 10.1016/s0277-9536(98)00385-2. [DOI] [PubMed] [Google Scholar]
- Eide E., Showalter M.H. The effect of school quality on student performance: a quantile regression approach. Economics Letters. 1998;58(3):345–350. [Google Scholar]
- Elstad J.I. Research Review of Social Inequalities in Health in Norway; 2013. The hierarchical diffusion model and the changing patterns in health-related habits in Norway since the 1970s. [Google Scholar]
- Ettner S.L. New evidence on the relationship between income and health. Journal of Health Economics. 1996;15(1):67–85. doi: 10.1016/0167-6296(95)00032-1. [DOI] [PubMed] [Google Scholar]
- Fauske M.F. Forsvarets forskningsinstitutt (FFI); 2011. Jeg vil inn i Forsvaret–hvem er jeg?”–en kvantitativ studie. [Google Scholar]
- Feng X., Wilson A. Do neighbourhood socioeconomic circumstances not matter for weight status among Australian men? Multilevel evidence from a household survey of 14 691 adults. BMJ Opening. 2015;5(9) doi: 10.1136/bmjopen-2014-007052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K.M., Carroll M.D., Kuczmarski R.J., Johnson C.L. Overweight and obesity in the United States: prevalence and trends, 1960-1994. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 1998;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- Galobardes B., Lynch J., Smith G.D. Measuring socioeconomic position in health research. British Medical Bulletin. 2007;81(1):21–37. doi: 10.1093/bmb/ldm001. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P., Nelson M.C., Page P., Popkin B.M. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Harrington D.W., Elliott S.J. Weighing the importance of neighbourhood: a multilevel exploration of the determinants of overweight and obesity. Social Science Medicine. 2009;68(4):593–600. doi: 10.1016/j.socscimed.2008.11.021. [DOI] [PubMed] [Google Scholar]
- Jaime P.C., Lock K. Do school based food and nutrition policies improve diet and reduce obesity? Preventive Medicine. 2009;48(1):45–53. doi: 10.1016/j.ypmed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Janssen I., Boyce W.F., Simpson K., Pickett W. Influence of individual-and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. The American journal of clinical nutrition. 2006;83(1):139–145. doi: 10.1093/ajcn/83.1.139. [DOI] [PubMed] [Google Scholar]
- Jullumstro, F. S., & Eide, S. S. (2013). [Thicker in the village] in Norwegian. NRK. Retrieved from: 〈http://www.nrk.no/ho/tjukkere-pa-bygda-1.11278453〉.
- Kavanagh A.M., Goller J.L., King T., Jolley D., Crawford D., Turrell G. Urban area disadvantage and physical activity: a multilevel study in Melbourne, Australia. Journal of Epidemiology and Community Health. 2005;59(11):934–940. doi: 10.1136/jech.2005.035931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King T., Kavanagh A.M., Jolley D., Turrell G., Crawford D. Weight and place: a multilevel cross-sectional survey of area-level social disadvantage and overweight/obesity in Australia. International Journal of Obesity. 2006;30(2):281–287. doi: 10.1038/sj.ijo.0803176. [DOI] [PubMed] [Google Scholar]
- Kinge J.M., Strand B.H., Vollset S.E., Skirbekk V. Educational inequalities in obesity and gross domestic product: evidence from 70 countries. Journal of Epidemiology and Community Health. 2015 doi: 10.1136/jech-2014-205353. (jech-2014-205353) [DOI] [PubMed] [Google Scholar]
- Komlos J., Smith P.K., Bogin B. Obesity and the rate of time preference: is there a connection? Journal of Biosocial Science. 2004;36(02):209–219. doi: 10.1017/s0021932003006205. [DOI] [PubMed] [Google Scholar]
- Kravdal Ø. The importance of community education for individual mortality: a fixed-effects analysis of longitudinal multilevel data on 1.7 million Norwegian women and men. Journal of Epidemiology and Community Health. 2010;64(12):1029–1035. doi: 10.1136/jech.2008.081034. [DOI] [PubMed] [Google Scholar]
- Kravdal Ø., Alvær K., Bævre K., Kinge J.M., Meisfjord J.R., Steingrímsdóttir Ó.A.…Strand B.H. How much of the variation in mortality across Norwegian municipalities is explained by the socio-demographic characteristics of the population? Health & Place. 2015;33:148–158. doi: 10.1016/j.healthplace.2015.02.013. [DOI] [PubMed] [Google Scholar]
- Laitinen S., Räsänen L., Viikari J., Åkerblom H.K. Diet of Finnish children in relation to the family’s socio-economic status. Scandinavian Journal of Public Health. 1995;23(2):88–94. doi: 10.1177/140349489502300203. [DOI] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiologic Reviews. 2007;29(1):29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Merlo J., Chaix B., Ohlsson H., Beckman A., Johnell K., Hjerpe P.…Larsen K. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. Journal of Epidemiology and Community Health. 2006;60(4):290–297. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J., Ross C.E. Education, personal control, lifestyle and health A human capital hypothesis. Research on Aging. 1998;20(4):415–449. [Google Scholar]
- Morris S. The impact of obesity on employment. Labour Economics. 2007;14(3):413–433. [Google Scholar]
- Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C.…Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014 doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwegian Institute of Public Health. (2015). About Norhealth. Retrieved from 〈http://www.fhi.no/artikler/?id=112322〉.
- Norwegian Ministry of Health and Care Services. (2012). The Public Health Act. ACT-2011-06-24-29. Norwegian Ministry of Health and Care Services, Retrieved from 〈http://www.ub.uio.no/ujur/ulovdata/lov-20110624-029-eng.pdf〉.
- Robert S.A. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annual Review of Sociology. 1999:489–516. [Google Scholar]
- Shohaimi S., Welch A., Bingham S., Luben R., Day N., Wareham N.…Khaw K.-T. Residential area deprivation predicts fruit and vegetable consumption independently of individual educational level and occupational social class: a cross sectional population study in the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk) Journal of Epidemiology and Community Health. 2004;58(8):686–691. doi: 10.1136/jech.2003.008490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon P.A., Kwan D., Angelescu A., Shih M., Fielding J.E. Proximity of fast food restaurants to schools: do neighborhood income and type of school matter? Preventive Medicine. 2008;47(3):284–288. doi: 10.1016/j.ypmed.2008.02.021. [DOI] [PubMed] [Google Scholar]
- Smyth, L. (2015). Mark Regan: 'There’s huge health inequality between Northern Ireland and England’. Belfast Telegraph.
- Sundquist J., Malmström M., Johansson S.-E. Cardiovascular risk factors and the neighbourhood environment: a multilevel analysis. International Journal of Epidemiology. 1999;28(5):841–845. doi: 10.1093/ije/28.5.841. [DOI] [PubMed] [Google Scholar]
- The Norwegian Directorate of Health. (2015). Dietary advice from The Norwegian Directorate of Health [in Norwegian]. Oslo: The Norwegian Directorate of Health. Retrieved from 〈https://helsedirektoratet.no/folkehelse/kosthold-og-ernering/kostrad-fra-helsedirektoratet〉.
- Trogdon J.G., Nonnemaker J., Pais J. Peer effects in adolescent overweight. Journal of Health Economics. 2008;27(5):1388–1399. doi: 10.1016/j.jhealeco.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Turrell G., Blakely T., Patterson C., Oldenburg B. A multilevel analysis of socioeconomic (small area) differences in household food purchasing behaviour. Journal of Epidemiology and Community Health. 2004;58(3):208–215. doi: 10.1136/jech.2003.011031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J., Waller J., Jarvis M.J. Sex differences in the association of socioeconomic status with obesity. American Journal of Public Health. 2002;92(8):1299–1304. doi: 10.2105/ajph.92.8.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M., Maloney T.N. Neighborhood socioeconomic status and BMI differences by immigrant and legal status: evidence from Utah. Economics Human Biology. 2014;12:120–131. doi: 10.1016/j.ehb.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2000. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. [PubMed] [Google Scholar]
- Wilson D.K., Kirtland K.A., Ainsworth B.E., Addy C.L. Socioeconomic status and perceptions of access and safety for physical activity. Annals of Behavioral Medicine. 2004;28(1):20–28. doi: 10.1207/s15324796abm2801_4. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1995). Physical status: The use of and interpretation of anthropometry, Report of a WHO Expert Committee. [PubMed]