Abstract
Since 2010, the UK has pursued a policy of austerity characterised by public spending cuts and welfare changes. There has been speculation – but little actual research – about the effects of this policy on health inequalities. This paper reports on a case study of local health inequalities in the local authority of Stockton-on-Tees in the North East of England, an area characterised by high spatial and socio-economic inequalities. The paper presents baseline findings from a prospective cohort study of inequalities in mental health and mental wellbeing between the most and least deprived areas of Stockton-on-Tees. This is the first quantitative study to explore local mental health inequalities during the current period of austerity and the first UK study to empirically examine the relative contributions of material, psychosocial and behavioural determinants in explaining the gap. Using a stratified random sampling technique, the data was analysed using multi-level models that explore the gap in mental health and wellbeing between people from the most and least deprived areas of the local authority, and the relative contributions of material, psychosocial and behavioural factors to this gap. The main findings indicate that there is a significant gap in mental health between the two areas, and that material and psychosocial factors appear to underpin this gap. The findings are discussed in relation to the context of the continuing programme of welfare changes and public spending cuts in the UK.
Keywords: Social determinants, Multilevel models, Survey, Mental wellbeing, United Kingdom, Welfare, Social inequality
Highlights
-
•
Exploring local inequalities, mental health and wellbeing, and austerity.
-
•
Stockton-on-Tees has the widest health inequalities in England.
-
•
Findings indicate a mental health gap between the most and least deprived areas.
-
•
Multi-level models show that material and psychosocial factors are key.
-
•
Multiple factors combine and interact to impact on mental health and wellbeing.
Background
Following the collapse of the global financial markets in 2007, the initial months of 2008 witnessed the US and European governments entering into an unprecedented public rescue package for the banking sector (Gamble, 2009). This followed concern that whole national economies would collapse – and indeed the financial crisis resulted in the longest period of global recession in the post-war era (Gamble, 2009). The common European response to the ensuing increase in national debt and increased unemployment has been the new politics of austerity, which has seen widespread programmes of public spending cuts (Kitson, Martin & Tyler, 2011). Subsequently, since 2010, the UK government has pursued the implementation of lower public spending and market led growth to reduce the national deficit. Public services, investment in public infrastructure and expenditure on welfare have been significantly reduced (Kitson et al., 2011).
Previous research has shown that such significant changes in the economy can have important negative implications for population health and inequalities in health with increases in suicides, rates of mental ill health and chronic illnesses (Barr et al., 2012, Stuckler and Basu, 2013). Unemployment increases during economic downturns and is itself strongly associated with greater morbidity and mortality (Bambra, 2011), particularly mental health problems, such as depression and stress (Janlert, 1997, Hagquist et al., 2000), suicide and suicide attempts (Platt, 1986, Newman and Bland, 2007, Lewis and Sloggett, 1998). Recessions are also characterised by an increase in job insecurity and ‘precarious’ employment, both of which are associated with higher rates of stress, and mental ill-health (Ferrie, Shipley, Stansfeld & Marmot, 2002).
Studies have found however, that there are important national policy variations in the effects of recessions and economic downturns on population health. For example, Stuckler and Basu (2013) found that the population health effects of recessions vary significantly by policy context with those countries (such as Iceland and the USA) which responded to the financial crisis of 2007 with an economic stimulus, faring much better – particularly in terms of mental health and suicides – than those countries (e.g. Spain, Greece and the UK) which chose to pursue a policy of austerity. Similarly, Hopkins (2006) found that in Thailand and Indonesia, where social welfare spending decreased during the Asian recession of the late 1990s, mortality rates increased. However, in Malaysia, where no cut-backs occurred, mortality rates were unchanged (Hopkins, 2006). Similarly, Stuckler, Basu, Suhrcke, Coutts and McKee (2009) study of 26 European countries concluded that greater spending on social welfare could considerably reduce suicide rates during periods of economic downturn.
Further, the economic effects of austerity are not distributed evenly within a country or population, either spatially or socially. Within the UK, some areas (such as the north-east of England and more deprived local authorities) have experienced greater public budget reductions and been more affected by changes to welfare benefits than others (Beatty & Fothergill, 2016). This has disproportionately impacted on the availability of key services in these areas, widening social inequalities within them and spatial inequalities between them and other areas (Pearce, 2013, Bambra and Garthwaite, 2015). Health inequalities are intimately linked to social inequalities and so a widening of social inequality, as a result of austerity, may lead to a further exacerbation of social and spatial health inequalities. This of course also includes inequalities in mental health.
However, there has been little research to date into the effects of austerity on health inequalities and most of it has mainly focused on the effects at a national population level (Suhrcke & Stuckler, 2012). There have been little consideration of the effects on health inequalities at the regional or local levels (Bambra, 2013). There is particularly a gap in terms of the effects on inequalities in mental health. This paper is the first to address this gap in the literature by exploring local inequalities in mental health and wellbeing during a time of austerity via a case study of the local authority of Stockton-on-Tees, a local authority in the North-East of England. It is also the first UK study to empirically examine the relative contribution of material, psychosocial and behavioural factors to inequalities in mental health. The primary aim of the research is to establish the magnitude of inequalities in mental health and wellbeing, and the role of different explanatory factors (material, psychosocial, and behavioural) in explaining it, between people living in the most and least deprived areas of the local authority within the context of austerity.
Inequalities in mental health and mental wellbeing
There are ongoing debates around how we conceptualise both mental health and mental wellbeing. Huppert (2009) argues that mental well-being incorporates feeling good (hedonic well-being) and functioning effectively (eudaimonic wellbeing). Whilst feeling good involves aspects such as happiness, interest in life, confidence and engagement, functioning effectively is about having a sense of purpose, feeling in control of life, and the ability to create positive relationships. Mental health and wellbeing can be seen as a pathway through which determinants of health, including deprivation and poverty, impact on physical health. Alongside this, however, they also need to be seen as outcomes in their own right, not just as mediators of this relationship between deprivation and physical ill-health (Rogers and Pilgrim, 2003).
Both physical and mental health follow a social gradient; the more advantaged people are in social and economic terms, the better their health (Scrambler, 2012). There are particularly large gaps between the extremes of the social hierarchy with people from the highest socio-economic backgrounds living longer (on average 7 years) and with longer amounts of their life disability-free (on average 17 years more) than people from the lowest socioeconomic backgrounds (Marmot, 2010). Alongside the link between socioeconomic class and physical health, the link between social deprivation and mental health is also well-established (Williams, 2002). A person׳s mental health is shaped by the environment he or she is living in (Curtis & Jones, 1998), and as such it is also of importance to consider the complex interactions between places and the people living in them, and their resulting impact on health. Significant gradients and health gaps also exist between areas with differences of up to 9 years in life expectancy between the most and least deprived areas of the UK (ONS, 2015).
Poor mental health is both a cause and a consequence of social inequality. The social consequences of living in poverty, including the impact of unemployment, underemployment, debt, poor living conditions, and living in areas with high levels of deprivation, can increase vulnerability to developing mental ill-health (Pilgrim & Rogers, 1999). Additionally, people who are experiencing mental distress, and those who have been labelled with mental health problems, are at increased risk of poverty, due for instance to risks around discrimination in the workplace preventing people from being able to secure and maintain employment (Evans-Lacko, Knapp, McCrone, Thornicroft & Mojtabai, 2013). Further, welfare changes as a result of austerity have disproportionately affected disability and ill-health related benefits, effectively bringing about a reduction in incomes for people who are unable to work as a result of ill-health.
Explaining health inequalities
Three main theories have been documented to account for health inequalities: materialist, psychosocial, and behavioural/cultural (Bartley, 2008).
Materialist explanations
Materialist explanations of health inequalities focus on the relationship between social structure and health, linking ill-health with the distribution of resources and inequalities in power (Williams, 2003). Material determinants factors include income, employment and level of education, and factors relating to the physical environment, such as poor quality housing and living in areas with high levels of deprivation, crime, and pollution. Cohort studies have linked poorer health with poverty, unemployment, and low income (Bartley, 2008).
Psychosocial explanations
Psychosocial explanations of health inequalities introduce the concept of relative deprivation: “What matters is where we stand in relation to others in our own society” (Wilkinson & Pickett, 2010: 25), placing emphasis on how people experience inequality and the emotional response to it which can give rise to acute and chronic levels of stress. Over time stress has an impact on the body, leading ultimately to physical and mental ill-health (Marmot & Wilkinson, 2006).
Behavioural explanations
Behavioural accounts of health inequalities focus on the things individuals do that are damaging to their health, and how certain groups of people are more likely to engage in health-damaging behaviours. So, for instance, smoking, drinking alcohol, poor diet and lack of exercise have all been found to be more prevalent amongst people from deprived areas than affluent ones (Marmot, 2010). Consumption of high amounts of alcohol appears to be a particular risk factor for mental ill health (WHO & Calouste Foundation, 2014).
Methods
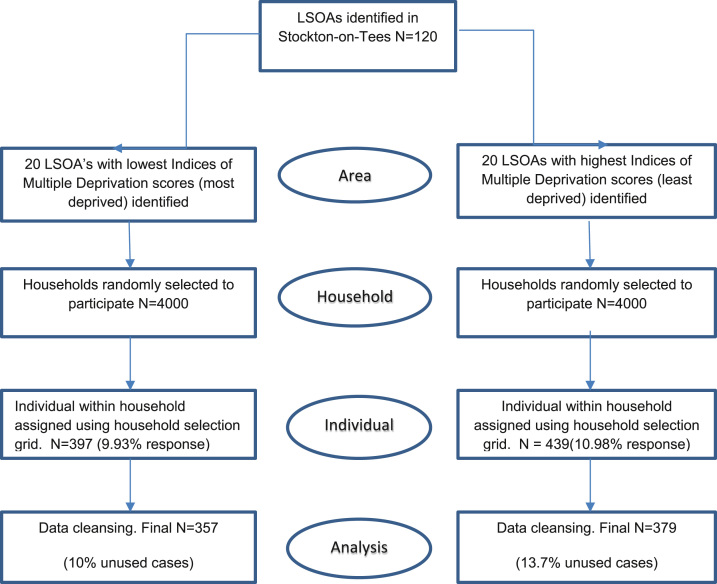
The ‘Local Health Inequalities in an Age of Austerity: The Stockton-on-Tees Study’ is a mixed method, interdisciplinary case study that aims to explore key debates around localised health inequalities in an age of austerity. Using a case study approach provides the opportunity to advance research into health inequalities by combining the methods and insights of different disciplines to study the localised effects of the social and spatial determinants of health. This paper presents the baseline findings from a prospective cohort survey comparing the health gap in Stockton-on-Tees. The gap is examined using a random baseline sample of adults aged over 18, split between participants from the 20 most to 20 least deprived lower super output areas (Fig. 1). LSOAs are small areas of relatively even size, with around 1500 people in each area; there are 32,484 LSOAs in England (Dept for Communities and Local Government, 2011). The aim of the project is to analyse health inequalities between the most and least deprived areas of the local authority during austerity, and how any changes in the underpinning social determinants (material, behavioural, and psychosocial) might explain any such changes. This paper focuses on inequalities in mental health and mental wellbeing.
Fig. 1.
Maps of Stockton-on-Tees including most and least deprived neighbourhoods.
Stockton-on-Tees was chosen as the site for analysis because it has the highest spatial health inequalities in England both for men (at a 17.3 year difference in life expectancy at birth) and for women (11.4 year gap in life expectancy) (Public Health England, 2015). This makes it a particularly important site to analyse health inequalities during austerity. Stockton-on-Tees has a population of 191,600 residents (Census, 2011). The population is overwhelmingly white (93.4%) although there is a small Asian/Asian British population (Indian 0.8%, Pakistani 1.6%, Bangladeshi 0.1%, Chinese 0.5%) (Census, 2011). Stockton has high levels of social inequality, with some areas of the local authority with very low levels of deprivation (e.g. Ingleby Barwick) and others with high levels of deprivation (e.g. Hardwick). These areas are often in close proximity to one another (as shown in Fig. 1). Deprivation overall is higher than the national average e.g. 21.9% of children live in poverty compared to 19.2% nationally (Public Health England, 2015).
Sampling strategy
Fig. 2 shows the sampling strategy for the survey. To identify the lowest and highest areas of deprivation in Stockton, we looked at the 120 lower super output areas (LSOA) in the local authority of Stockton on Tees, selecting the 20 with the lowest index of Multiple Deprivation (IMD) scores from 2010 and the 20 with the highest IMD scores (IMD range 1.54–74.5) (Dept for Communities and Local Government, 2011). The IMD is a summary measure of relative deprivation for each lower layer super output area (LSOA) in England. The IMD is published at the level of LSOA and is formed by pulling together 38 individual indicators that are situated within 7 broader domains: income deprivation; employment deprivation; health deprivation and disability; education, skills, and training deprivation; barriers to housing and services; living environment deprivation; and crime. The IMD provides an overall score by drawing together weighted scores from each of these domains. The scores for each LSOA are then ranked so that there is a relative deprivation score for each LSOA in England. This allows different LSOAs to be compared (Dept for Communities and Local Government, 2011).
Fig. 2.
Sampling strategy for the survey.
Participants were sampled initially by household, and then at the individual level, using a multi-stage randomised sampling strategy (Fig. 2). Within this approach, a sample of areas are drawn up (initially larger areas are selected and then progressively smaller ones until a sample of households are randomly selected within the areas). Individuals within the household were then randomly selected using a selection grid (Devaus, 1991). One individual within each household was selected in this manner.
Sample size
The sample size was based on a conservative power calculation which utilised a range of validated health outcome measures (EQ5D, SF8 PCS, SF8 MCS) and which assumed a 5% difference between the least and most deprived areas, and allowed for a 20% attrition rate between baseline and first follow-up and a further 5% attrition at all other follow ups, giving a final predicted sample size of 400 (200 in each group). A sample of 800 at baseline would ensure that, given attrition, there would be sufficient respondents in the follow-up waves to undertake statistical analysis. 20,013 eligible addresses were identified from the 40 study LSOAs, using the most recent Office for National Statistics postcode lookup tables. The amount of eligible addresses ranged from 313 to 1380 addresses per LSOA. Using a stratified random sampling technique, we created a sample of 200 target households in each of the 40 LSOAs. Assuming a 10% response rate, 8000 households (4000 most and least deprived) were sent study invitation letters (200 per LSOA) in April and May 2014.
A total of 836 participants completed the baseline survey between April and June 2014: 397 in the most deprived areas and 439 in the least deprived areas. Participating individuals were sent a £10 high street voucher as a thank you for taking part.
The baseline survey included questions on health, mental health, demographics and the social determinants of health – covering material, psychosocial, and behavioural factors. Questions were matched whenever possible to those used in other surveys (such as the General Household Survey), to enable national level comparisons to be made. The mental health scales used were validated instruments of mental health: the Warwick Edinburgh Mental Well Being Scale (WEMWBS) and the SF8.
A pilot survey of the questionnaire was completed in December 2013 and January 2014 with a random sample of 24 households in two non-study areas: the 21st most and 21st least deprived lower super output areas.
Outcome variables
Two measures were used to assess mental health: the Warwick Edinburgh Mental Wellbeing Scale and the SF8. The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) is a 14 point scale that considers both hedonic and eudaimonic aspects of well-being and asks respondents to self-report their experience of each of the statements over the past two weeks. It has been well-validated for use in the general population and has moderate to high levels of construct validity (Tennant, Fishwick, Platt, Joseph & Stewart-Brown, 2006). The WEMWBS has 14 statements with 5 possible answers that are scaled from ‘none of the time’ up to ‘all of the time’. The scale gives the individual a total score (up to a maximum of 70); this score is used as the dependent variable and is treated as a continuous variable.
The SF8 instrument provides a measure of physical and mental health and provides a separate score for both physical (SF8-PCS) and mental (SF8-MCS) health. This analysis focuses on the mental health component of the measure (SF8-MCS). The SF8 is a condensed version of the SF36 and has 8 questions; the participant is asked to report how much each question has applied to them over the past 30 days.
Explanatory variables
Explanatory variables were separated into four categories: material socioeconomic variables; material physical environment variables; psychosocial variables and behavioural variables. These capture the different determinants of health within the three main theories of health inequalities (as outlined earlier). For example, the survey questions on psychosocial factors captured domestic, community and workplace aspects of the psychosocial environment, whilst material socioeconomic variables covered factors such as income, education, employment and benefit receipt.
Statistical analysis
Following the data cleansing process, 736 participants remained in the final analysis. Certain variables were excluded from the analysis where there was too much missing data. This included for instance the questions related to participants׳ experiences in employment, as the survey had lots of respondents who were not in paid work. In the final analysis there were 357 respondents from the most deprived LSOAs and 379 from the least deprived (Fig. 2).
Analysis focused on establishing: (1) the magnitude of inequalities in mental health and mental wellbeing (as measured by WEMWBS and SF8MCS); (2) the associations between the individual explanatory variables and mental health outcomes; and (3) the relative explanatory contribution of each of the leading theories of health inequalities (material, psychosocial and behavioural) to the inequality gap. The analysis focuses on the gap in the two mental health scores between respondents from the most and least deprived areas. This inequality gap is labelled as ‘deprivation’ in the analysis.
Multilevel models were applied to explore the mean gap in mental health between the most and the least deprived areas, controlling for potential clustering within the lower super output areas. The model building exercise involved an initial process of univariate analysis with individual variables, where the most important variables for each category were first determined separately. Multi-variate analysis was then based on an initial combination of all the significant variables in the univariate models. The multilevel models were then used to calculate the percentage contribution of material, psychosocial and behavioural factors to mental health inequalities between the most and the least deprived areas.
A similar approach was used by Stuckler, Basu, Suhrcke, Coutts and McKee (2009) in regards to socio-economic inequalities in health in Norway, and Copeland, Kasim, and Bambra (2015) with respect to the North–South health divide. The reference model for each health outcome is a multilevel model containing only the indicator for the most and least deprived areas together with age and gender, while an adjusted model contains other factors in addition to those originally included in the reference model. Prior to a formal inference about the associations and the contributions of the factors (material/psychosocial/behavioural), likelihood ratio testing was used to pre-select relevant variables for each of the factors. In total, 11 multi-level models were fitted to the data in order to investigate the contribution of each of the factors to mental health inequalities between the most and least deprived areas.
The direct and indirect contributions were calculated. We use ‘direct contribution’ to denote the sole contribution of the category of determinant (e.g. material socioeconomic) to the inequality gap between the most and least deprived areas, after removing the effect of the other categories. We use ‘indirect contribution’ to refer to the contribution of the combination of the categories to the inequality gap.
Results
Baseline characteristics
Baseline characteristics of the sample including socio-demographic factors and material, psychosocial and behavioural variables are outlined in Table 1. It is of note that participants who took part in the survey were older than the general population, with one third of respondents from the least deprived areas, and one quarter from the most deprived areas, over the age of 65. Therefore there were also lots of participants who were not currently in paid employment, many as a result of being past retirement age: 31% (N=112) of those from the most deprived areas were retired, and 38% (N=142) from the least deprived. There were very high numbers of respondents from both areas who were in receipt of some form of benefit, however this was because the measure also incorporated the state pension and child benefit. In relation to housing and the neighbourhood, some key differences included that a quarter (26%) of participants in the deprived areas reported problems with damp in the home (compared to 3% from the least deprived areas). 29% of respondents from the most deprived areas also reported crime in the neighbourhood (compared to 6% in the least deprived areas. Smoking rates differed significantly between the two areas, with 37% of participants in the deprived areas smoking compared to 10% in the least deprived, although alcohol use was more prevalent in the least deprived areas. As expected there were large differences in median net household incomes between participants from both areas (£26000–£28600 for participants from the least deprived areas and £10400–£13000 for those from the most deprived areas). This compares to a United Kingdom median household income of £22,880 for the period 2012/3 (ONS, 2014).
Table 1.
Characteristics of the sample (after missing data exclusions): sociodemographic, material, psychosocial and behavioural variables.
| Variables Categories |
Number (%) |
|
|---|---|---|
| Least deprived | Most deprived | |
| Age | ||
| Under 25s | 15 (4.0) | 37 (10.4) |
| 25–49 | 131 (34.6) | 131 (36.7) |
| 50–64 | 110 (29.0) | 95 (26.6) |
| 65 and over | 123 (32.5) | 94 (26.3) |
| Gender | ||
| Male | 163 (43.0) | 147 (41.2) |
| Female | 216 (57.0) | 210 (58.8) |
| Marital status | ||
| Married | 223 (58.8) | 91 (25.5) |
| Single | 67 (17.7) | 142 (39.8) |
| Divorced | 39 (10.3) | 58 (16.2) |
| Widowed | 39 (10.3) | 41 (11.5) |
| Ethnicity | ||
| White | 362 (95.5) | 341 (95.8) |
| Asian or Asian British | 10 (2.6) | 0 (0.0) |
| Socioeconomic | ||
| Highest educational level | ||
| Higher or First degree | 101 (26.6) | 17 (4.8) |
| Higher diplomas/A-Levels or Equivalent | 107 (28.2) | 39 (10.9) |
| GCSE or Equiv | 87 (23.0) | 139 (38.9) |
| Entry level/No formal qualifications | 84 (22.2) | 162 (45.4) |
| Housing tenure | ||
| Own outright | 195 (51.5) | 61 (17.1) |
| Mortgage or loan | 138 (36.4) | 37 (10.4) |
| Rent | 44 (11.6) | 255 (71.4) |
| Live rent free | 2 (0.5) | 4 (1.1) |
| Household receipt of benefits | 267 (70.4) | 312 (87.4) |
| Household receipt of housing benefit | 16 (4.2) | 194 (54.3) |
| Workless household | 143 (37.7) | 238 (66.7) |
| Current job skill type | ||
| Professional | 43 (11.3) | 10 (2.8) |
| Unskilled | 27 (7.1) | 42 (11.8) |
| Work status | ||
| Participant in paid employment | 184 (48.5) | 89 (24.9) |
| Retired | 142 (37.5) | 112 (31.4) |
| Unemployeda | 53 (14.0) | 156 (43.7) |
| Household annual income (Mode) | £36400–£41600 | £10400–£13000 |
| Household annual income (Median) | £26000–£28600 | £10400–£13000 |
| Physical environment | ||
| Problems with damp in the home | 10 (2.6) | 95 (26.6) |
| Home is too dark | 31 (8.2) | 63 (17.6) |
| Home is not warm enough in winter | 27 (7.1) | 72 (20.2) |
| Problems with neighbourhood noise | 42 (11.1) | 86 (24.1) |
| Problems with pollution | 13 (3.4) | 46 (12.9) |
| Problems with crime | 24 (6.3) | 105 (29.4) |
| Psychosocial | ||
| Neighbourhood safety perception | ||
| Very safe | 209 (55.1) | 108 (30.3) |
| Safe | 141 (37.2) | 132 (37) |
| Unsafe | 23 (6.1) | 73 (20.4) |
| Very unsafe | 6 (1.6) | 44 (12.3) |
| Lacking companionship | ||
| Hardly ever | 288 (76) | 241 (67.5) |
| Some of the time | 70 (18.5) | 76 (21.3) |
| Often | 21 (5.5) | 40 (11.2) |
| Feeling left out | ||
| Hardly ever | 320 (84.4) | 250 (70) |
| Some of the time | 47 (12.4) | 66 (18.5) |
| Often | 12 (3.2) | 41 (11.5) |
| Feeling isolated | ||
| Hardly ever | 312 (82.3) | 256 (71.7) |
| Some of the time | 54 (14.2) | 60 (16.8) |
| Often | 13 (3.4) | 41 (11.5) |
| Behavioural | ||
| Respondents who smoke | 39 (10.3) | 132 (37) |
| Respondents who drink alcohol | 299 (78.9) | 211 (59.1) |
| Frequency of physical exercise | ||
| Every day | 113 (29.8) | 129 (36.1) |
| Most days | 65 (17.2) | 44 (12.3) |
| Couple of times a week | 79 (20.8) | 42 (11.8) |
| Once a week | 14 (3.7) | 15 (4.2) |
| Less than once a week | 13 (3.4) | 14 (3.9) |
| Never | 95 (25.1) | 113 (31.7) |
‘Unemployed’ incorporates all individuals of working age who are not in employment, including those classed as unemployed, unable to work due to ill-health or disability, or looking after the home/family.
Inequalities in mental health and wellbeing
The reference models explore the gap in WEMWBS and SF8 MCS between respondents from the most to least deprived areas of Stockton, adjusted for age and gender (Table 2). The estimated inequality gap in WEMWBS is 5.04 (3.42, 6.66). The estimated inequality gap in SF8 MCS is 3.80 (2.35, 5.25). People have better mental health scores in the least deprived areas when compared to their counterparts in the most deprived areas.
Table 2.
Inequality gap in Stockton-on-Tees for SF8 MCS and WEMWBS: estimates of fixed effects.
| Parameter | Estimate |
95% Confidence interval |
||
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| SF8 | Intercept | 50.90 | 48.59 | 53.21 |
| Gender | 1.96 | 0.49 | 3.44 | |
| Age | −0.04 | −0.08 | 0.01 | |
| Deprivation | 3.80 | 2.35 | 5.25 | |
| WEMWBS | Intercept | 49.10 | 46.52 | 51.68 |
| Gender | 1.31 | −0.33 | 2.96 | |
| Age | 0.01 | −0.04 | 0.05 | |
| Deprivation | 5.04 | 3.42 | 6.66 | |
WEMWBS and SF8-MCS models: associations between mental health outcomes and the final explanatory variables
Table 3 shows the results from the final models used to investigate the associations between the health outcomes (WEMWBS and SF8-MCS) and the different material, psychosocial and behavioural factors. These were the key factors that remained in each model following the process of model reduction using likelihood ratio testing. Only one question on material socioeconomic factors, two questions on material physical environment factors, five questions on psychosocial factors and one behavioural question remained in the final model for the SF8 MCS. People living in polluted areas have lower SF8 MCS scores than those living in non-polluted areas. Also, people living in homes that are too dark have significantly lower mental health scores. A positive significant association was found between happiness and mental wellbeing. Increasing feelings of lacking companionship, isolation and feeling left out were negatively associated with SF8 MCS score. The more unsafe people feel walking alone in the neighbourhood after dark, the lower the mental health score. People that use alcohol had higher SF8 MCS scores than non-drinkers.
Table 3.
Association between mental health outcomes and the explanatory factors based on the variables selected using likelihood ratio test. Point estimates and its associated 95% confidence intervals.
| Factors | Variables | SF8 MCS | WEMWBS |
|---|---|---|---|
| Deprivation | .09 (−1.25,1.42) | .07 (−1.64,1.79) | |
| Age | −.01 (−.05,.03) | .02 (−.02,.06) | |
| Gender | .77 (−.47,2.01) | −.19 (−1.49,1.10) | |
| Material socioeconomic | Housing tenure (Reference group=people who rent their homes) | ||
| Own outright | −1.48 (−3.80,0.82) | ||
| Buy with mortgage | −3.13 (−5.42,0.84) | ||
| Live rent free | 3.34 (−3.73,10.41) | ||
| Household income | .23 (.09,.38) | ||
| Household housing benefit (Yes/No) | −3.21 (−5.30,1.12) | ||
| Is the Individual in paid employment (Yes/No) | 1.22 (−.15,2.60) | ||
| Material physical environment | The home is dark (Yes/No) | −2.58 (−4.35,−.82) | |
| Pollution/Environmental problems (Yes/No) | −2.23 (−4.42,−.04) | −2.93 (−5.26,−.61) | |
| Psychosocial | Happiness scale | 1.76 (1.39,2.13) | 2.89(2.51,3.26) |
| Feeling unsafe walking alone after dark | −.90 (−1.63,−.17) | ||
| Frequency of lacking companionship | −1.45 (−2.80,−.10) | ||
| Frequency of feeling isolated from others | −1.66 (−3.24,−.08) | ||
| Frequency of feeling left out | −2.46 (−4.03,−.89) | −2.93 (−4.11,1.76) | |
| Behavioural | Frequency of physical exercise | .56 (.25,.87) | |
| Alcohol use (Yes/No) | 1.40 (.06,2.73) | 2.82 (1.42,4.23) | |
| Random effects | Covariance parameter | Estimate (Std.Error) | Estimate (Std.Error) |
| Residuals | 62.85(3.33) | 64.21(3.45) | |
| LSOA | 0.04(0.63) | 7.29(2.47) |
For the Yes/No response variables, ‘No’ is the reference group.
The analysis of WEMWBS shows similar results as the SF8 MCS score for the variables in the models that were important to both mental health outcome measures. Additionally, for the WEMWBS, compared to people who rent their homes, people who are buying their home with the help of a mortgage have lower wellbeing scores. Those in households that are in receipt of housing benefit have significantly lower WEMWBS scores than those who are not in receipt of housing benefit. Increasing household income was associated with increasing wellbeing. Finally, increasing levels of physical exercise were associated with higher WEMWBS scores.
Percentage contribution of material, psychosocial and behavioural determinants to inequalities in mental health
Table 4 shows the percentage reduction in the inequality gap due to the different categories of mental health determinant. The full model (M11) with all the factors accounts for 98.55% reduction in inequality gap in WEMWBS, and 97.76% in the SF8 mental health score, between people from the most and least deprived parts of Stockton-on-Tees. The percentage change of each model is calculated by:
Table 4.
Percentage contribution of material, psychosocial and behavioural models to the inequality gap.
| Model |
SF8 MCS baseline causal model |
WEMWBS baseline causal model |
||
|---|---|---|---|---|
| Estimate | % Change | Estimate | % Change | |
| M0: D | 3.80(2.35, 5.25) | 5.04(3.42, 6.66) | ||
| M1: D+MP | 3.07(1.61, 4.54) | 19.13 | 4.56(2.93, 6.19) | 9.48 |
| M2: D+MS | 3.02(1.50, 4.54) | 20.5 | 0.87(−1.27, 3.01) | 82.79 |
| M3: D+ P | 1.06(−0.21, 2.34) | 72.01 | 2.60(1.28, 3.92) | 48.43 |
| M4: D+B | 3.37(1.89, 4.85) | 11.2 | 4.29(2.67, 5.92) | 14.8 |
| M5: D+B+P | 0.75(−0.55, 2.04) | 80.38 | 1.91(0.59, 3.23) | 62.03 |
| M6: D+MS+MP | 2.36(0.83, 3.88) | 37.95 | 0.44(−1.70,2.58) | 91.25 |
| M7: D+MS+MP+B | 2.14(0.60, 3.68) | 43.7 | 0.46(−1.66, 2.57) | 90.9 |
| M8: D+MS+MP+P | 0.27(−1.06, 1.60) | 92.85 | 0.15(−1.59, 1.90) | 96.9 |
| M9: D+MS+B+P | 0.44(−0.89, 1.78) | 88.31 | 0.30(−1.41, 2.02) | 93.99 |
| M10. D+MP+B+P | 0.37(−0.93, 1.67) | 90.14 | 1.69(0.36, 3.01) | 66.55 |
| M11: D+MS+MP+P+B | 0.08(−1.25, 1.42) | 97.76 | 0.07(−1.64, 1.79) | 98.55 |
D – deprivation; MP – material physical environment; MS – material socioeconomic; B – behavioural; P – psychosocial.
100*(Reference Model M0−Adjusted Model)/Reference Model.
So for instance the percentage change of Model 1 is calculated as 100*(3.80−3.07)/3.80=19.13%. By comparing the different models in Table 4, we are then able to estimate the direct and the indirect contribution of the different categories to the inequality gaps. For example, the direct effect of psychosocial factors to the inequality gap in SF8 MCS is 54.06%, this is worked out by subtracting the percentage change of the model without psychosocial variables in it (43.7%) from the total percentage change from the full model (97.76%) i.e. the difference between the percentage reduction of model M11 and model M7.
The direct contribution of material, psychosocial and behavioural factors to the inequality gap in WEMWBS are 36.51%, 7.61% and 1.61% respectively. Among the material factors, socioeconomic factors explained 32% of the health inequality whilst the material physical environment factors explained 4.56%. Material factors contributed the biggest reduction in the estimated inequality gap whilst behavioural factors contributed the least. The indirect effect of the factors is estimated as 52.81%, based on the difference between the total reduction in equality gap from model M11 and the sum of the individual factors contributions (i.e. 98.55 – 36.51 – 7.61 – 1.61). Whilst material socioeconomic factors contribute the most to inequalities in mental wellbeing in Stockton, there are very high indirect effects. This suggests that the presence of the behavioural and psychosocial factors outlined in the model will aggravate the impact of material factors on the gap in mental wellbeing. So for instance, for an individual who feels unhappy and does not engage in physical exercise regularly, this will exacerbate the impact that being in receipt of housing benefit has on mental wellbeing. Psychosocial factors appear to contribute most to the gap in SF8 MCS score in Stockton on Tees, at 54.07% of direct effects. Material factors were secondary in importance (17.38%) to psychosocial factors, although there were also still fairly large indirect effects. Behavioural factors had the lowest contribution in both health outcomes (1.61% for WEMWBS and 4.91% for SF8 MCS).
Discussion
This paper has sought to explore the inequality gap in mental health and wellbeing between people from the most and least deprived areas of the local authority of Stockton-on-Tees, and what is causing this gap. A social determinants model has been applied, exploring the relative contributions of material (incorporating material physical environment and material socioeconomic), psychosocial and behavioural determinants of mental health and wellbeing. Two outcome measures have been used, the SF8-MCS and the WEMWBS. The results demonstrate that there is a significant gap for both of these measures; this gap is slightly more pronounced in the WEMWBS. Living in less deprived areas affords considerable protection towards mental health and mental wellbeing, and people who live in these areas are likely to score significantly higher on mental health measures.
This is consistent with the substantial research base evidencing inequalities in mental health (Marmot, 2010). Consistent associations have been found between mental ill health and low income, low education; low social status; unemployment; and poorer material circumstances (Melzer, Fryers & Jenkins, 2004). The literature suggests that it is not only individual factors (such as having a higher income or better housing) that impacts on the relationship between living in a more affluent area and better mental health, but also the context of the area itself which could be protective including such things as the physical environment (e.g. there is better access to green space in more affluent areas), opportunity structures (e.g. better access to healthcare services or education or childcare), or the economic environment (e.g. availability of better jobs) (Bambra, 2016).
Our research has also shown that material and psychosocial factors are the most important determinants of the divide in mental health and wellbeing in Stockton on Tees. However, there was a difference between the two mental health measures in terms of which category had the biggest direct effect on the outcome. With the SF8 score, psychosocial factors contributed most to the gap (54%), whereas in the WEMWBS it was material factors that took precedence (37%). Psychosocial variables such as social isolation were particularly important in the SF8. Participants in the most deprived areas, who tended to be slightly younger, seemed more isolated and lacking in companionship than those in the least deprived areas. These are social problems that are often associated with the mental health of older people (Cattan, White, Bond & Learmouth, 2005). As such, our findings suggest that either deprivation is strongly associated with social isolation in addition to age, or that the older participants in the most deprived areas were feeling so much more isolated than their counterparts in the least deprived.
There was some overlap in the final variables left within the two models; pollution was important for both mental health measures, alongside alcohol use, how often the individual felt left out, and the self-reported happiness measure. Although happiness as a concept is not measured in the WEMWBS, one would expect there may be some association between the happiness scale as a predictor and mental wellbeing as an outcome: happiness is a feature of emotional wellbeing (Westerhof & Keyes 2010). Where factors such as household income and receipt of housing benefit were crucial in the WEMWBS, these material factors became less important in the SF8 and were replaced with whether the individual was in paid employment. Finally, for the WEMWBS, we found that compared to people who rented their homes, people who were buying their home with the help of a mortgage had lower wellbeing scores. Although some of the housing literature describes home owners as having higher wellbeing in contrast to renters (Filakti & Fox, 1995), in the United Kingdom home ownership is a large heterogeneous sector (Searle, Smith & Cook, 2009). As such owner occupiers exhibit an uneven health profile (Smith, Easterlow & Munro, 2004). Our findings reflect this diversity, suggesting that home ownership can be problematic for mental wellbeing.
It can be argued that the SF8 may be a less robust measure than the WEMWBS. The SF8 is a condensed version of the SF-36. The SF-36 is a measure of 8 health concepts that cover: physical functioning; role limitations because of physical health problems; bodily pain; social functioning; general mental health (psychological distress and psychological wellbeing); role limitations because of emotional problems; vitality (energy/fatigue); general health perceptions. The shorter SF8 covers the same health concepts but uses single item questions for each category as opposed to several (Ware & Sherbourne, 1992). Whilst the shorter SF8 scale reduces the burden on respondent and interviewer, and is a more cost-effective scale within a larger survey, it carries the downside of being less sensitive and of being prone to distortion from bias (Bowling, 2005). There are only three questions that relate to mental health in the SF8, compared to the 14 in the WEMWBS; as such the latter scale may be a more precise tool.
Another possible reason for the divergence lies in the scales themselves; they are measuring slightly different things and were chosen for the study because they were different. The WEMWBS covers both eudemonic and hedonic aspects of wellbeing. These relate to feeling good (hedonic well-being) and functioning effectively (eudemonic wellbeing). Whilst feeling good involves aspects such as interest in life, confidence and engagement, functioning effectively is about having a sense of purpose, feeling in control of life, and the ability to create positive relationships (Huppert, 2009). Whilst the WEMWBS scale covers both eudemonic and hedonic functioning, the SF8 seems to have a greater focus on issues related to functioning – role limitations because of emotional problems, and the ability to get involved in social activities. The SF8 also asks people to rate their general mental health, which the WEMWBS does not. The scales therefore differ in what they are measuring, and as such this may be why their determinants have differed.
The third possibility is that both material and psychosocial factors are key in explaining the gap in mental health and mental wellbeing between people from more and less deprived areas during austerity. The statistical analysis shows that there are very large indirect effects in the WEMWBS (53%), and smaller, although still substantial, indirect effects in the SF8 (21%). This suggests that those different factors are working together in determining outcomes. Having a low income, and living in an area that is deprived and may have problems with pollution for instance, can make people unhappy, unwell, and can prevent people from being able to engage in activities that can make them feel included in life and connected with others. It is the combination and interaction of factors such as these, working alongside each other, that have a cumulative impact on mental health and can seriously undermine people׳s wellbeing. Within psychosocial models of health inequalities, it is ongoing, chronic levels of stress that ultimately exert an impact on the body, leading to physical and mental ill-health (Brunner, Marmot & Wilkinson, 2006). It is not difficult to see how living in poverty, with all of the challenges that this brings to people, can lead to chronic stress.
Our research has identified that behavioural indicators are the least important of the categories determining the inequality gap in mental health and wellbeing. This is true for both mental health measures. This is important, as much public health activity focused on reducing health inequalities tends to lean towards behavioural interventions and individual behaviour change. This shift towards a focus on the individual has been labelled as ‘lifestyle drift’ (Hunter, Popay, Tannahill, Whitehead & Elson, 2009: 3). Increasing physical activity is a much-used piece of advice given to people to improve their mental wellbeing (e.g. NHS, 2014a), alongside ‘eating healthy’ and drinking less alcohol as a means to combat depression (NHS, 2014b). We have found that although behavioural factors such as exercise play a role in mental health and wellbeing, they seem to have a far smaller direct impact than either structurally based material factors or psychosocial components. The participants in our study who drank alcohol actually had better mental health scores than the non-drinkers, although this may have been related to people abstaining from alcohol use as a result of physical health problems. It may have also been related to the context in which participants consumed alcohol: meeting up with friends in a pub may, for some, serve as a protective factor because of the added social benefits incurred from this. It does, however, need to be recognised that the study used general measures of mental health and wellbeing. It may be the case that the determinants of more clinical indicators of poor mental health may differ from the determinants of general mental health and wellbeing identified in this study. There is, for instance, a strong link between alcohol consumption, depression, and suicide (WHO & Calouste Foundation, 2014), although socioeconomic factors appear to have comparable effects on both mental wellbeing and mental health problems (Huppert, 2009).
Previous international research on welfare changes has shown that where welfare services are cut, this increases inequalities in mortality and morbidity: whilst overall population health is generally unaffected, cuts in welfare have a detrimental impact on the health of the poorest (Krieger et al., 2008, Blakely et al., 2008, Shaw et al., 2005). Across England there has been an increase in indicators of poor mental health since 2010, and evidence nationally of widening inequalities in mental health (Barr, Kinderman & Whitehead, 2015). Whilst population mental health usually declines during an economic recession and then recovers, this has not been the case in the current period. Mental health continues to be affected, including an increase in rates of suicides, with 2013 witnessing the highest male suicide rate since 2001 (ONS, 2015). The largest increase in poor mental health (including suicides, self-reported mental health problems and anti-depressant prescription rates) have been in the most deprived areas, leading to increasing inequalities in mental health (Barr, Taylor-Robinson et al., 2015).
Whilst the baseline findings of this study cannot demonstrate temporal changes during the period of austerity, our findings lend support to the argument that socioeconomic factors play a significant role in driving inequalities in mental health and mental wellbeing at a localised level. There are already substantial inequalities between people from the most and least deprived areas of the local authority, and as such, any increase in deprivation amongst the poorest (for example as a result of welfare changes) may further impact on these inequalities. Health profiles on Stockton-on-Tees have identified that since 2010, the life expectancy gap between the most and least deprived areas has worsened in the local authority (Public Health England, 2015). This would suggest that health inequalities have indeed grown since the onset of austerity. Whether inequalities in mental health and mental wellbeing change during austerity will be examined further in the follow-up waves of the Stockton on Tees cohort study.
Strengths and limitations
This study employed a random sample, it used a comprehensive questionnaire that incorporated multiple validated measures of health and the determinants of health, and it was administered on a face to face basis. However, the study is not without limitations. Firstly, the sample size is only moderate at 836 (although this is well within power for the analysis). Secondly, it relies on self-reported health measures (although there is a strong association between self-reported health and more objective outcomes including mortality). Thirdly, whilst validated measures of mental health and well-being are used, it is recognised that there are other ways to measure mental health. For instance, rates of suicide, prescriptions of anti-depressant use and self-reported mental health problems (as opposed to the more general measures of mental wellbeing and mental health employed in this study) have been used in other research exploring inequalities in mental health (e.g. Barr, Taylor-Robinson et al., 2015). The survey measures employed here to measure mental health and mental wellbeing may be more responsive to the impact of economic disadvantage, preceding any potential subsequent rises in indicators of mental ill-health such as self-reported mental health problems.
Another limitation within the study was the age of respondents, which was generally older than the general population. Findings need to be interpreted with this in mind and it is partly a result of who is prepared to engage in survey research. Whilst incidents of ill-health increase with age, mental wellbeing may be U-shaped over people׳s lives (Blanchflower & Oswald, 2008). As such a slightly younger sample may have led to lower overall wellbeing scores. Ethnicity was not explored as Stockton-on-Tees is a very white local authority and there were too few respondents from a non-white background. Marital status was also not included within the analysis as it did not fit conceptually within the framework employed. It was a further limitation that we were unable to include the information that related to employment type and work based psychosocial stressors as it would have resulted in a significantly smaller sample for analysis.
Finally, this study relates only to one place – Stockton-on-Tees – at one point in time. As it is a cross-sectional study it is unknown how long participants had lived in the area and therefore their length of exposure to the area characteristics is unknown. The local authority has the highest gap in life expectancy between people the most and least deprived areas in the whole of England and the results may not be generalisable, although the local authority has similar levels of deprivation to that found in places such as Wakefield and Leeds in the north of England and Southampton in the south (Public Health England, 2016).
Conclusion
This study has provided a comprehensive baseline analysis of local inequalities in mental health and wellbeing between the most and least deprived areas of Stockton-on-Tees in a time of austerity. There is significant social and health inequality in Stockton. Our baseline results provide evidence of a significant gap in mental health between people from the most and least deprived areas of the local authority, and which factors are most important in determining these differences. It shows that the material and psychosocial factors are the most important determinants of the gap. This is in contrast to much of current public health policy where behavioural factors are privileged as the key determinants. The baseline survey has provided information on these health inequalities at a set point in time, however with social inequality looking likely to rise further under austerity, subsequent waves of the survey will identify whether the gap in mental health subsequently increases in Stockton-on-Tees and if so whether this is due to any changes in the different determinants.
Acknowledgements
This research is part of a five year project studying health inequalities in Stockton-on-Tees which is funded by a Leverhulme Trust Research Leadership Award held by Professor Clare Bambra (reference RL-2012-006).
Contributor Information
K. Mattheys, Email: kate.mattheys@durham.ac.uk.
C. Bambra, Email: clare.bambra@durham.ac.uk.
J. Warren, Email: jonathan.warren@durham.ac.uk.
A. Kasim, Email: a.k.kasim@durham.ac.uk.
N. Akhter, Email: nasima.akhter@durham.ac.uk.
References
- Bambra C. Oxford University Press; Oxford: 2011. Work, worklessness and the political economy of health. [DOI] [PubMed] [Google Scholar]
- Bambra C. ‘All in it together’? Health inequalities, austerity and the ‘great recession’. In: Wood C., editor. Health in austerity. Demos Collection; London: 2013. p. 36. [Google Scholar]
- Bambra C. Policy Press; Bristol: 2016. Health divides: where you live can kill you. [Google Scholar]
- Bambra C., Garthwaite K. Austerity, welfare reform and the English health divide. Area. 2015;47(3):341–343. [Google Scholar]
- Barr B., Taylor-Robinson D., Scott-Samuel A. Suicides associated with the 2008–10 economic recession in England: time trend analysis. British Medical Journal. 2012;345:e5142. doi: 10.1136/bmj.e5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr B., Kinderman P., Whitehead P. Trends in mental health inequalities in England during a period of recession, austerity and welfare reform 2004–2013. Social Science and Medicine. 2015;147:324–331. doi: 10.1016/j.socscimed.2015.11.009. [DOI] [PubMed] [Google Scholar]
- Barr B., Taylor-Robinson D., Stuckler D., Loodstra R., Reeves A., Whitehead M. ‘First, do no harm’: are disability assessments associated with adverse trends in mental health? A longitudinal ecological study. Journal of Epidemology and Community Health. 2015;0:1–7. doi: 10.1136/jech-2015-206209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartley M. Polity Press; Cambridge: 2008. Health inequality: an introduction to theories, concepts and methods. [Google Scholar]
- Beatty C., Fothergill S. Sheffield: Centre for Regional Economic and Social Research Sheffield Hallam University; 2016. The uneven impact of welfare reform. The financial losses to places and people.〈http://www.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/welfare-reform-2016_1.pdf〉 Accessed 21.3.16. [Google Scholar]
- Blakely T., Tobias M., Atkinson J. Inequalities in mortality during and after restructuring of the New Zealand economy: repeated cohort studies. BMJ. 2008;336:371–375. doi: 10.1136/bmj.39455.596181.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchflower D.G., Oswald A.J. Is well-being U-shaped over the life cycle? Social Science and Medicine. 2008;66(8):1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Bowling A. Just one question: if one question works, why ask several? Journal of Epidemiology and Community Health. 2005;59:342–345. doi: 10.1136/jech.2004.021204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner E., Marmot M. Social organisation, stress and health. In: Marmot M., Wilkinson R., editors. Social Determinants of Health. Oxford University Press; Oxford: 2006. 2006. [Google Scholar]
- Cattan M., White M., Bond J., Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Society. 2005;25:41–67. doi: 10.7748/nop.17.1.40.s11. [DOI] [PubMed] [Google Scholar]
- Copeland A., Kasim A., Bambra C. Grim up north or northern grit? Recessions and the english spatial health divide (1991–2010) Journal of Public Health. 2015;37:34–39. doi: 10.1093/pubmed/fdu019. [DOI] [PubMed] [Google Scholar]
- Curtis S., Jones I.R. Is there a place for geography in the analysis of health inequality? Sociology of Health and Illness. 1998;20(5):645–672. [Google Scholar]
- Dept for Communities and Local Government (2011). English indices of deprivation 2010. 〈https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/6871/1871208.pdf〉 Accessed 12.10.15.
- Devaus D.A. UCL Press Ltd.; London: 1991. Surveys in social research. [Google Scholar]
- Evans-Lacko S., Knapp M., McCrone P., Thornicroft G., Mojtabai R. The mental health consequences of the recession: economic hardship and employment of people with mental health problems in 27 European Countries. PLoS One. 2013;8(7):e69792. doi: 10.1371/journal.pone.0069792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrie J.E., Shipley M.J., Stansfeld S.A., Marmot M.G. Effects of chronic job insecurity and change in job security on self-reported health, minor psychiatric morbidity, physiological measures, and health related behaviours in British civil servants: the Whitehall II study. Journal of Epidemiology and Community Health. 2002;56:450–454. doi: 10.1136/jech.56.6.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filakti H., Fox J. Differences in mortality by housing tenure and by car access. Population Trends. 1995;81:27–30. [PubMed] [Google Scholar]
- Gamble A. Palgrave; Basingstoke: 2009. The spectre at the feast: capitalist crisis and the politics of recession. [Google Scholar]
- Hagquist C., Silburn S.R., Zurbrick S.R., Lindberg G., Ringbäck W.G. Suicide and mental health problems among Swedish youth in the wake of the 1990s recession. International Journal of Social Welfare. 2000;9:211–219. [Google Scholar]
- Hopkins S. Economic stability and health status: evidence from East Asia before and after the 1990s economic crisis. Health Policy. 2006;75:347–357. doi: 10.1016/j.healthpol.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Hunter, D.J., Popay, J., Tannahill, C., Whitehead, M., and Elson, T. (2009). Lessons learned from the past. Shaping a different future. Marmot Review Working Committee 3 Cross-cutting sub-group report. 〈https://www.instituteofhealthequity.org/projects/the-marmot-review-working-committee-3-report/working-committee-3-final-report.pdf〉 Accessed 11.11.15.
- Huppert T.A. Psychological well-being: evidence regarding its causes and consequences. Applied Psychology: Health and Well-being. 2009;1(2):137–164. [Google Scholar]
- Janlert U. Unemployment as a disease and diseases of the unemployed. Scandinavian Journal of Work, Environment Health. 1997:79–83. [PubMed] [Google Scholar]
- Kitson M., Martin R., Tyler P. The geographies of austerity. Cambridge Journal of Regions, Economy and Society. 2011;4:289–302. [Google Scholar]
- Krieger N., Rehkopf D.H., Chen J.T., Waterman P.D., Marcelli E., Kennedy M. The fall and rise of US inequities in premature mortality: 1960–2002. Plos Medicine. 2008;5:227–241. doi: 10.1371/journal.pmed.0050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G., Sloggett A. Suicide, deprivation and unemployment: record linkage study. BMJ. 1998;317:1283–1286. doi: 10.1136/bmj.317.7168.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. University College; London: 2010. Fair society, healthy lives: the marmot review. [Google Scholar]
- Marmot M., Wilkinson R. Oxford University Press; Oxford: 2006. Social determinants of health. [Google Scholar]
- Melzer D., Fryers T., Jenkins R. Psychology Press; Hove: 2004. Social inequalities and the distribution of the common mental disorders. [Google Scholar]
- Newman S.C., Bland R.C. Case-control study of unemployment and parasuicide. Comprehensive Psychiatry. 2007;48(6):511–515. doi: 10.1016/j.comppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- NHS (2014a). Five steps to mental wellbeing. 〈http://www.nhs.uk/Conditions/stress-anxiety-depression/Pages/improve-mental-wellbeing.aspx〉 Accessed 01.06.15.
- NHS (2014b). Healthy eating and depression. 〈http://www.nhs.uk/Conditions/stress-anxiety-depression/Pages/healthy-diet-depression.aspx〉 Accessed 01.06.15.
- Office for National Statistics (2011). Census: Aggregate data (England and Wales) [computer file]. UK Data Service Census Support. Downloaded from: 〈http://infuse.ukdataservice.ac.uk〉; Accessed 03.05.16.
- ONS (2014). Households below average income: an analysis of the income distribution 1994/95–2012/13. DWP. 〈https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/325416/households-below-average-income-1994-1995-2012-2013.pdf〉 Accessed 06.04.16.
- ONS (2015). Inequality in healthy life expectancy at birth by national deciles of area deprivation: England, 2011 to 2013. Available at: 〈http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-392673〉 Accessed 05.04.2015.
- Pearce J. Commentary. Environment and Planning A. 2013;45:2030–2045. [Google Scholar]
- Pilgrim D., Rogers A. Open University Press; Buckingham: 1999. A sociology of mental health and illness. [Google Scholar]
- Platt S. Parasuicide and unemployment. British Journal of Psychiatry. 1986;149:401–405. doi: 10.1192/bjp.149.4.401. [DOI] [PubMed] [Google Scholar]
- Public Health England (2015). Stockton-on-Tees health profile 2015. APHO. 〈http://www.apho.org.uk/resource/item.aspx?RID=50336〉 Accessed 01.10.15.
- Public Health England (2016). Health profiles. 〈http://fingertips.phe.org.uk/profile/health-profiles/data#page/8/gid/3007000/pat/6/par/E12000004/ati/101/are/E07000032〉 Accessed 09.03.16.
- Rogers, A, Pilgrim, D (2003). Mental Health and Inequality.
- Scrambler G. Health inequalities. Sociology of Health and Illness. 2012;34(1):130–146. doi: 10.1111/j.1467-9566.2011.01387.x. [DOI] [PubMed] [Google Scholar]
- Searle B.A., Smith S.J., Cook N. From housing wealth to well-being? Sociology of Health and Illness. 2009;31(1):112–127. doi: 10.1111/j.1467-9566.2008.01113.x. [DOI] [PubMed] [Google Scholar]
- Shaw C., Blakely T., Atkinson J., Crampton P. Do social and economic reforms change socioeconomic inequalities in child mortality? A case study: New Zealand 1981–1999. Journal of Epidemiology and Community Health. 2005;59(8):638–644. doi: 10.1136/jech.2004.032466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.J., Easterlow D., Munro M. Housing for health: does the market work? Environment and Planning A. 2004;36:579–600. [Google Scholar]
- Stuckler D., Basu S., Suhrcke M., Coutts A., McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. 2009;374:315–323. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- Stuckler D., Basu S. Penguin Books Ltd.; London: 2013. The body economic. why austerity kills. [Google Scholar]
- Suhrcke M., Stuckler D. Will the recession be bad for our health? It depends. Social Science and Medicine. 2012;74:647–653. doi: 10.1016/j.socscimed.2011.12.011. [DOI] [PubMed] [Google Scholar]
- Tennant, R., Fishwick, R., Platt, S., Joseph, S., and Stewart-Brown, S. (2006). Monitoring positive mental health in Scotland: validating the Affectometer 2 scale and developing the Warwick-Edinburgh Mental Well-being Scale. 〈http://www.healthscotland.com/documents/2327.aspx〉 Accessed in April 2014.
- Ware J.E., Sherbourne C.D. The MOS 36-Item short-form health survey (SF-36): 1. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Westerhof J.J., Keyes C.L.M. Mental illness and mental health: the two continua model across the lifespan. Journal of Adult Development. 2010;17(2):110–119. doi: 10.1007/s10804-009-9082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, Calouste Foundation . WHO; Geneva: 2014. Social determinants of mental health. [Google Scholar]
- Wilkinson R., Pickett K. Penguin; London: 2010. The spirit level: why equality is better for everyone. [Google Scholar]
- Williams G.H. The determinants of health: structure, context and agency. Sociology of Health and Illness. 2003;25:131–154. [PubMed] [Google Scholar]
- Williams J. Social inequalities and mental health. In: Newnes C., Holmes G., Dunn C., editors. This is madness: a critical look at psychiatry and the future of mental health services. PCCS Books; Ross on Wye: 2002. [Google Scholar]