Abstract
During the past two decades, mindfulness meditation has gone from being a fringe topic of scientific investigation to being an occasional replacement for psychotherapy, tool of corporate well-being, widely implemented educational practice, and “key to building more resilient soldiers”. Yet the mindfulness movement and empirical evidence supporting it have not gone without criticism. Misinformation and poor methodology associated with past studies of mindfulness may lead public consumers to be harmed, misled, and disappointed. Addressing such concerns, the present article discusses the difficulties of defining mindfulness, delineates the proper scope of research into mindfulness practices, and explicates crucial methodological issues for interpreting results from investigations of mindfulness. For doing so, the authors draw upon their diverse areas of expertise to review the present state of mindfulness research, comprehensively summarizing what we do and do not know, while providing a prescriptive agenda for Contemplative Science, with a particular focus on assessment, mindfulness training, possible adverse effects, and intersection with brain imaging. Our goals are to inform interested scientists, the news media, and the public, in order to minimize harm, curb poor research practices, and staunch the flow of misinformation about the benefits, costs, and future prospects of mindfulness meditation.
Keywords and Phrases: mindfulness, meditation, psychotherapy, neuroimaging, contemplative science, adverse effects, media hype, misinformation
I. Introduction
Mindfulness is an umbrella term used to characterize a large number of practices, processes, and characteristics, largely defined in relation to the capacities of attention, awareness, memory/retention, and acceptance/discernment. While the term has its historical footing in Buddhism (cf. Bodhi, 2011; Dunne, 2011; Dreyfus, 2011; Gethin, 2011; Kabat-Zinn, 2011), it has achieved wide-ranging popularity in psychology, psychiatry, medicine, neuroscience, and beyond, initially through its central role in Mindfulness-based Stress Reduction (MBSR: Kabat-Zinn, 1990) -- an intervention/training ‘package’ introduced in the late 1970s as a complementary therapy for medically ailing individuals (Kabat-Zinn, 2011). The term mindfulness began to gain traction among scientists, clinicians, and scholars as the Mind and Life Institute emerged in 1987 and facilitated formal regular dialogues between the Dalai Lama and prominent scientists and clinicians, as well as regular summer research meetings, the latter starting in 2004 (Kabat-Zinn & Davidson, 2011). In the early 2000s, mindfulness saw an exponential growth trajectory that continues to this day (see Figure 1). The term mindfulness has a plethora of meanings; a reflection of its incredible popularity alongside considerable misinformation and misunderstanding, as well as preliminary support among a general lack of methodologically rigorous research.
Figure 1.
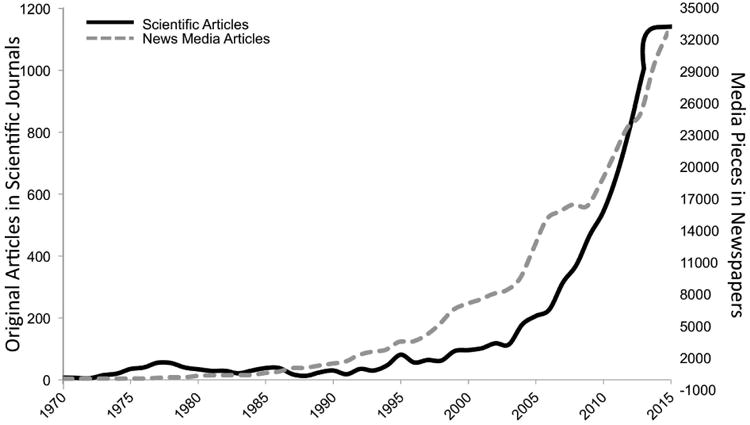
Scientific and news media articles on mindfulness and/or meditation by year from 1970 – 2015. Empirical scientific articles (black line) with the term “mindfulness” or “meditation” in the abstract, title, or keywords, published between 1970 and 2015 were searched using Scopus. Media pieces (dashed gray line) with the terms “mindfulness” or “meditation”, published in newspapers, using a similarity filter to minimize double-counting, published between 1970 and 2015 were searched using LexisNexis.
Mindfulness has become an extremely influential practice for a sizeable subset of the general public, constituting part of Google's business practices (Schaufenbuel, 2015), available as a standard psychotherapy via the National Health Service in the United Kingdom (see Coyne, 2015b), and most recently, part of standard education for approximately 6,000 school children in London (Rhodes, 2015). Additionally, it has become a major area of study across subdisciplines of psychological science, including Social/Personality (Brown & Ryan, 2003), Industrial/Organizational (Dane, 2011), Experimental (Jensen et al. 2012), Clinical (Dimidjian & Segal, 2015), Cognitive (Tang, et al. 2015), Health (Jain et al. 2007), Educational (Britton et al. 2014), and many others. As such, it is critical that we take the term (along with any ambiguities) and the methodological rigor (or lack thereof) with which it has been studied very seriously.
Over the past two decades, writings on mindfulness and meditation practices have saturated the public news media and scientific literature (see Figure 1). While not an isolated case, much popular media fails to accurately represent scientific examination of mindfulness (see e.g., Goyal et al., 2014), making rather exaggerated claims about the potential benefits of mindfulness practices (Gibbs, 2016; Gunderson, 2016). There have even been some portrayals of mindfulness as an essentially universal panacea for various types of human deficiencies and ailments (see e.g., Gunderson, 2016; Huffington, 2013).
As mindfulness has increasingly pervaded every aspect of contemporary society, so have misunderstandings about what it is, whom it helps, and how it affects the mind and brain. At a practical level, the misinformation and propagation of poor research methodology has potential led to people being harmed, cheated, disappointed, and/or disaffected. At a philosophical level, misunderstandings of the work and its implications could limit the potential utility of a method that proposes unique links between first-person data and third-person observations (cf. Lutz & Thompson, 2003). Further, research into a potentially promising arena may be halted for no reason other than that people have become tired of hearing about it (and therefore disinclined to pursue and/or fund it). While there have been many review articles written on mindfulness (e.g., Davidson & Kazniak, 2015; Dimidjian & Segal, 2015; Farb, 2014; Tang, Hölzel, & Posner, 2015), they cannot, by virtue of their limited scope (often focused on specific conditions or topics) and authorship (often limited to a short list of investigators, sometimes with clear conflicts of interest; see e.g., Coyne, 2015b), offer a balanced, consensus perspective. Going beyond prior reviews, the present work provides exposition of the varying definitions of mindfulness, reviews the status of empirical assessment of mindfulness, reviews potential adverse events, considers implications for contemporary clinical practice, discusses specific issues that arise when doing neuroimaging with meditating samples, and elaborates on potential neural differences associated with meditation practices of varying durations.
Two main topics are considered herein: (1) the problem of defining mindfulness and thus delineating the appropriate scope of research on mindfulness practices; and (2) methodological issues in mindfulness research. We provide (a) an overview of the current state in scientific knowledge; (b) a summary of consensus about what the currently available empirical findings do or do not conclusively show; and (c) a proposed prescriptive research agenda for making future scientific progress in understanding the consequences of mindfulness practices.
Our rationale for this expository approach stems from multiple major a priori considerations. We believe that much public confusion and media hype have stemmed from an undifferentiated use of the terms mindfulness and meditation. Each of these terms may refer to an ambiguously broad array of mental states and practices that are associated with a wide variety of secular and religious contexts (Davidson & Kaszniak, 2015; Goleman, 1988). Valid interpretation of empirical results from scientific research on such states and practices must take proper account of exactly what types of ‘mindfulness’ and ‘meditation’ are involved (see Section II.C). With current use of umbrella terms, a 5 minute meditation exercise from a popular phone application might be treated the same as a 3-month meditation retreat (both labeled as meditation) and a self-report questionnaire might be equated with the characteristics of someone who has spent decades practicing a particular type of meditation (both labeled as mindfulness).
Furthermore, there is a general failure among the public to recognize that scientific consensus is a complex process requiring considerable time, effort, debate, and (most importantly) data. Throughout the scientific process, the predominant view among scholars can vacillate between being in support of, being agnostic to, and being against, a given idea or theory (Shwed & Bearman, 2010). Eager journalists, academic press offices, and news media outlets – sometimes aided and abetted by researchers – have often over-interpreted initial tentative empirical results as if they were established facts. Moreover, statistically ‘significant’ differences have repeatedly been equated with clinical and/or practical significance (cf. Rosnow & Rosenthal, 1989). These critical considerations need to be incorporated constructively in the future development of best practices for conducting mindfulness research, and for promoting accurate scientific communication with the general public (Britton, 2016).
II. The Problematic Meaning of “Mindfulness”
Despite how it is often portrayed by the media (e.g., Huffington, 2013) and some researchers (Brown & Ryan, 2003), there is neither one universally accepted technical definition of “mindfulness” nor any broad agreement about detailed aspects of the underlying concept to which it refers (Bodhi, 2011; Dreyfus, 2011; Dunne, 2011; Gethin, 2011). Frequently, “mindfulness” simply denotes a mental faculty for being consciously aware and taking account of currently prevailing situations (Kabat-Zinn, 1990; Langer, 1989). At other times, “mindfulness” may refer to formal practice of sitting on a cushion in a specific posture and attending (more or less successfully) to the breath or some other focal object. Considerable disagreement about definitions is not uncommon in the study of complex constructs (for discussion of intelligence, see e.g., Neisser et al., 1996; for discussion of wisdom, see e.g., Walsh, 2015) and mindfulness is no exception. Mindfulness is typically considered to be a mental faculty relating to attention, awareness, retention/memory, and/or discernment (cf. Davidson & Kazniak, 2015), however, these multiple faculties are rarely represented in research practice (Goldberg et al. 2015; Manuel, Somohano, & Bohen, 2016). One of the most thoughtful and frequently invoked definitions, states that mindfulness is moment-to-moment awareness, cultivated by paying attention in a specific way, in the present moment, as non-reactively, non-judgmentally, and open-heartedly as possible (Kabat-Zinn, 1990; Kabat-Zinn, 2011). However, this definition has been described as one of convenience regarding those constructs most readily comprehensible to Western audiences (Kabat-Zinn, 2011).
Alternative semantic interpretations of ‘mindfulness’
Although concerted efforts have been made to provide consensus descriptions of mindfulness (Analayo, 2003; Bishop et al., 2004; Bodhi, 2011; Brown, Ryan, & Creswell, 2007; Grabovac, Lau, & Willett, 2011; Gunaratana, 2002; Hölzel et al., 2011; Malinowski, 2013; Shapiro et al., 2006; Vago & Silbersweig, 2012), there continue to be considerable variations regarding the meaning of ‘mindfulness’. The resulting debates within and across complementary scholarly disciplines that encompass the investigation and practice of mindfulness and meditation more generally are diverse and complex (cf. Contemporary Buddhism, 2011, Vol. 12, Issue 1; Psychological Inquiry, 2007, Vol. 18, Issue 4). Given such considerations, one should not be especially surprised that some people have refrained from accepting Kabat-Zinn's (1990) definition of “mindfulness,” or else have interpreted it in different, sometimes conflicting, ways. Kabat-Zinn (2011) himself has acknowledged that the term represents (to him) a much broader scope of concepts and practices than what his earlier (1990) definition might suggest.
Scientific implications of semantic ambiguity in the meaning of ‘mindfulness’
The ramifications of considerable semantic ambiguity in the meaning of mindfulness are multifarious. Any study that uses the term “mindfulness” must be scrutinized carefully, ascertaining exactly what type of “mindfulness” was involved, and what sorts of explicit instruction were actually given to participants for directing practice, if there was any practice involved. If the definition of mindfulness is based on self-report measures, one should be aware of the nuances of the various measures, how they relate to each other and/or conceptualizations of mindfulness (see Table 1; Sauer et al. 2013; Bergomi, Tschacher, & Kupper, 2013), as well as how different individuals might interpret the items on these measures (cf. Grossman & Van Dam, 2011). It should be further noted that self-reported mindfulness may not relate to the actual practice of mindfulness meditation (cf. Manuel, Somohano, & Bohen, 2016). When formal meditation was used in a study, one ought to consider whether a specifically defined type of mindfulness or other meditation (cf. Lutz et al. 2008) was the target practice (see e.g., Braun, 2013; McMahan, 2008). Additionally, while there is no single definition of mindfulness, it is important to examine whether the authors' specified definition is consistent with their study design (see Section II.C).
Table 1. Mindfulness measures.
| Publication Date | Name | Context | Citation Count1 | Factors |
|---|---|---|---|---|
| 2001 | Freiburg Mindfulness Inventory (FMI) | Buddhist Theory | 565 | 1 - General |
|
| ||||
| 2003 | Mindful Attention and Awareness Scale (MASS) | Self-Determination Theory | 5054 | 1 - Attentiveness & Awareness |
|
| ||||
| 2004 | Kentucky Inventory of Mindfulness Skills (KIMS) | Dialectical Behavior Therapy | 1449 | 1 – Observing |
| 2 – Describing | ||||
| 3 –Awareness | ||||
| 4 - Acceptance | ||||
|
| ||||
| 2006 | Five Facet Mindfulness Questionnaire (FFMQ) | CAMS-R, KIMS, FMI, SMQ, MAAS | 2660 | 1 – Nonreactivity |
| 2 – Observing | ||||
| 3 – Awareness | ||||
| 4 – Describing | ||||
| 5 - Nonjudging | ||||
|
| ||||
| 2006 | Toronto Mindfulness Scale (TMS) | Bishop et al. 2004 | 648 | 1 – Curiousity |
| 2 – De-centering | ||||
|
| ||||
| 2007 | Cognitive and Affective Mindfulness Scale, Revised (CAMS-R) | Buddhist Theory & Kabat-Zinn 1990 | 530 | 1 – Attention |
| 2 – Present Focus | ||||
| 3 – Acceptance | ||||
| 4 - Acceptance | ||||
|
| ||||
| 2008 | Philadelpha Mindfulness Scale (PHLMS) | Bishop et al. 2004 | 411 | 1 – Acceptance |
| 2 - Awareness | ||||
|
| ||||
| 2008 | Southhamptom Mindfulness Questionnaire (SMQ) | Kabat-Zinn 1990 and Cognitive Theory | 297 | 1 - General |
|
| ||||
| 2013 | State Mindfulness Scale (SMS) | Buddhist Theory | 35 | 1 – Body Mindfulness |
| 2 – Mind Mindfulness | ||||
Google Scholar, October 20th, 2016
II.A. Consequences of Semantic Ambiguity for Empirical Studies of ‘Mindfulness’
Although most mindfulness training has been derived from the original MBSR model (Kabat-Zinn, 1990), the intensity (hours per day) and duration (total time commitment) of participants' formal practice have varied considerably across different versions of training (Davidson & Kaszniak, 2015; Tang et al. 2007; Zeidan et al. 2011). The particular methods for teaching and practicing ‘mindful’ states have varied too. However, published journal abstracts and media reports about obtained results often gloss over such crucial variations, leading to inappropriate comparisons between what might be fundamentally different states, experiences, skills, and practices.
Different definitions of skilled expertise
The definitions of “novice” and “expert” or “adept” (with respect to those with meditation experience) have varied considerably from study to study. Some investigators have considered novices to be individuals with some but not extensive prior formal meditation experience (e.g., up to a few hundred hours of practice; Kozasa et al., 2012; Lutz, Dunne & Davidson, 2007). Others have applied a much stricter criterion, deeming novices only to be individuals with absolutely no prior meditation experience (e.g., Brewer et al., 2011). Further increasing this confusion, some approaches to investigating ‘mindfulness’ (e.g., Hayes, Strosahl, & Wilson, 1999; Linehan, 1993) do not require any systematic training to become ‘skilled’ in the practice, nor do they require participants to sustain a given experiential state (e.g., present-moment focus, or compassionate engagement) any longer than necessary to achieve a putative beneficial effect.
II.B. Consequences of Semantic Ambiguity for Theoretical Models of ‘Mindfulness’
According to proposed theoretical models of mindfulness, there are clear mental processes and brain mechanisms that might facilitate insight and adaptive personal change, such as psychological distancing/re-perceiving (Shapiro et al., 2006), decentering and inhibitory control (Vago & Silbersweig, 2012), non-conceptual discriminatory awareness (Brown et al., 2007), acceptance and reintegration (Hayes et al., 1999; Linehan, 1993), or focused attention, decentering, and meta-awareness (Lutz, Jha, Dunne, & Saron, 2015; Meyer, 2009). Some of these processes and/or outcomes may be evident on a continuum, suggesting gradual growth with practice over time, whereas others may emerge significantly only in experienced practitioners (i.e., individuals who have engaged in formal sitting meditation or other contemplative practices such as Hatha Yoga, over a lengthy period of time; e.g., van Vugt & Slagter, 2014). Potential changes to various cognitive capacities as a result of mindfulness practice is not specific to clinical contexts; it also informs the limits, capacities, and nature of various cognitive functions and how those functions might be modified. However, the aforementioned complexity, confounding, and confusion that surrounds empirical research on ‘mindfulness’ limits the potential of the method to inform broad questions and inform specific theories. The extent to which a specific model is supported or disconfirmed by particular sets of empirical data or systematic observations depends on the meaning of ‘mindfulness’ that inspired data acquisition. For example, it is nearly impossible to test whether de-centering has occurred if one has not obtained a measure of it. Support for a model will also depend on compliance with experimenter/clinician instructions (Davidson & Kaszniak, 2015). No one theoretical model (e.g., Garland, Farb, Goldin, & Fredrickson, 2015; Grabovac et al. 2011; Hölzel et al. 2011; Shapiro et al 2006; Vago & Silbersweig, 2012) can possibly describe, explain, and predict all of the phenomena stemming from the panoply of facets that ‘mindfulness,’ broadly construed, can have. Thus, it will be critical, going forward, to generate new integrative models and to track which data support which models.
II.C. Integrative Assessment
Consensus about the semantic ambiguity of ‘mindfulness’
‘Mindfulness’ does not constitute a unitary construct, though it frequently includes aspects of paying attention in a specific, sustained, non-judgmental way (Kabat-Zinn, 1990). Buddhist scholars suggest it often entails attention, awareness, memory/retention and discernment (cf. Bodhi, 2011; Dreyfus, 2011; Dunne, 2011; Gethin, 2011). Self-report measures often highlight attention, awareness, and acceptance or nonjudgment (rather than discernment; see Table 1). The field, broadly defined, seems to agree that mindfulness entails attention and awareness with some important qualifiers about the nature of those faculties. It is also evident that mindfulness is part of some broader collection of goals and attitudes (Gethin, 2011; Kabat-Zinn, 2011). From a historical perspective, the attitudes qualifying attention and awareness are those accompanying some higher pursuit (e.g., enlightenment), including recognition/awareness, tranquility, concentration, equanimity, energy, joy, and discrimination (Gethin, 2011). Ultimately, degree of fidelity to historical definitions may not necessarily matter to definitions of mindfulness applied in modern practice (Dreyfus, 2011; Gethin, 2011), though historical definitions can provide important context and insight into the nature of mindfulness practice and its potential mechanisms (cf. Kabat-Zinn, 2011). Finally, the type of mindfulness putatively measured by contemporary cross-sectional research is not necessarily the same as what contemporary mindfulness training/meditation seeks to cultivate (see Manuel et al. 2016), which itself can differ from the mindfulness practiced by long-term meditators in various contemplative traditions relative to one another (Grossman & Van Dam, 2011).
Prescriptive research agenda: Transcending the prevalent ambiguity
Given current confusion surrounding “mindfulness,” we urge scientists, practitioners, instructors, and the public news media to move away from relying on the broad, umbrella rubric of “mindfulness” and toward more explicit, differentiated, denotations of exactly what mental states, processes, and functions are being taught, practiced, and investigated. Towards this end, we have provided a non-exhaustive list of defining features for characterization of contemplative and meditation practices (see Table 2). We have divided these features into primary (i.e., critical to most practices) and secondary (i.e., only critical to some practices). While this list is non-exhaustive, common use of this list of descriptors (or a comparable list) would permit the field to move beyond the many ambiguities of definition it is currently facing. Other examples of fundamental feature lists can be found in both scientific (e.g., Lutz et al. 2015) and contemplative (e.g., Analayo, 2003) literatures. For those studies using self-report measures, we encourage users to list the exact measure and to discuss the aspects of ‘mindfulness’ that the utilized measure characterizes (see e.g., Table 1). These suggestions only address terminology and do not necessarily provide ways to overcome the variation in the panoply of contextual factors surrounding mindfulness and/or meditation practice (e.g., type and training of instructor, regularity of meetings, group vs. individual practice, home practice type and amount, etc.). To resolve issues surrounding the implementation of mindfulness and/or other meditation-based training/intervention, we recommend development of something similar to a CONSORT checklist (Moher, Schulz, Altman, 2001) that could be implemented across studies (see Table 3).
Table 2. Non-exhaustive list of defining features for characterization of meditation practice.
| Feature | Definition | Variation in Feature |
|---|---|---|
| Primary Features | ||
| Arousal | Extent of alertness, awakeness, etc. | Low, medium, high |
| Orientation (of Attention) | Where attention is directed | Inward vs. Outward vs. No Orientation |
| Spatial ‘dynamic’ (of Attention) | The quality of attention in space | Fixed (e.g., on an object or location) vs. Moving (e.g., as inthe Body Scan) |
| Temporal ‘dynamic’ (of Attention) | The quality of attention in time | Constant/Stable vs. Rhythmic/Sporadic |
| Object (of Attention) | Attention can be fixed on none, one, two, or many objects | Specific (i.e., defined object(s)) vs. Aspecific (i.e., no well-defined object(s)) vs. None (i.e., no object of attention) |
| Aperture (of Attention) | How ‘sharply’ the spotlight of attention is focused | Narrow vs. Intermediate vs. Diffuse |
| Effort | The extent to which one exerts energy to achieve other features | Low, medium, high |
|
| ||
| Secondary Features | ||
| Complementary Activity | Physical activity to facilitate desired feature(s) | Walking, Mantra recitation, Dancing, Rhythmic movement, etc. |
| Affective Valence | Emotional tone of practice | Positive vs. Neutral vs. Negative |
| Emotional Intention | A desired emotional state (to be cultivated) | Loving-kindness, compassion, forgiveness, generosity, etc. |
| Motivation/Goal | The rationale/reason for the practice | Wellness, mitigation of illness, self-improvement, enlightenment |
| Proficiency Required | Level of skill or expertise necessary | Low, medium, high |
| Posture | Physical orientation of body during practice | Horizontal (e.g., lying down) vs. Intermediate (e.g., sitting) vs. Vertical (e.g., standing) |
Table 3. Non-exhaustive list of study design features for a mindfulness-based intervention.
| Teacher Information |
|
| Practice Information |
|
| General Information |
|
| Participant Info |
|
| Conflicts of Interest |
|
III. Methodological Issues in Mindfulness Meditation Research
Complementing our commentary about the problematic meanings of ‘mindfulness,’ several major methodological issues in mindfulness meditation research should be considered as well. Such consideration is essential to achieve the present goals of providing a more balanced perspective on the pros and cons of practicing mindfulness, and on the weaknesses of currently available empirical findings about its efficacy. Specifically, we are concerned about four distinct but related types of issue: (1) insufficient construct validity in measures of mindfulness; (2) challenges to (clinical) intervention methodology; (3) potential adverse effects from practicing mindfulness; and (4) questionable interpretations of data from Contemplative Neuroscience concerning the mental processes and brain mechanisms underlying mindfulness.
Relation to the ‘Replication Crisis’ in Psychological Science
Worries over scientific integrity and reproducibility of empirical findings have recently come to the fore of both Psychological Science and wider swaths of other basic and applied sciences, receiving considerable attention in both the scientific literature (Button et al., 2013; Ioannidis, 2005, 2012; Miguel et al., 2014; Open Science Collaboration, 2012; Pashler & Wagenmakers, 2012) and public news media (Freedman, 2010; Johnson, 2014a, 2014b; Lehrer, 2010; Nyham, 2014). As part of these developments, debates regarding the efficacy and safety of treatment interventions have also embroiled the behavioral and neuropsychiatric sciences (Baker, McFall, & Shoham, 2008; Fanelli, 2010; Simmons, Nelson, & Simonsohn, 2011; Button et al., 2013; Ioannidis, 2005; Munafò, Stothart, & Flint, 2009; Yarkoni, Poldrack, Van Essen, & Wager, 2010). Although our present focus is on methodological issues to which mindfulness research is especially vulnerable, it is important to take account of this broader self-examination currently underway in the scientific community. Contemplative Science (i.e., the scientific study of contemplative practices including, but not limited to, mindfulness meditation), is particularly vulnerable to “hype” of various sorts (i.e., tendencies to tout exaggerated positive and negative claims).
III.A. Insufficient Construct Validity in Measuring Mindfulness
One of the disclaimers on offer here concerns construct validity in measuring mindfulness. For obvious reasons, this concern is crucial to our present objectives. Lacking reasonably validated mindfulness measures, one can neither properly determine how this mental faculty changes through instructions and guided practice, nor can one assess how increased mindfulness affects the cognitive capacities and/or symptoms of various mental and physical dysfunctions.
Difficulties in operationalizing and measuring mindfulness
Given the aforementioned absence of consensus regarding definitions of ‘mindfulness,’ the operationalization and measurement of mindfulness are challenging endeavors. These difficulties have propagated to affect both (1) mindfulness practice, and (2) assessments of mindfulness as a mental state or personality trait. Different researchers have implemented varying mindfulness training approaches across studies (e.g., Davidson, 2010), creating challenges for identifying common effects. We are especially concerned about attempts to measure mindfulness via self-report (see e.g., Grossman & Van Dam, 2011) because, as Figure 2 indicates, a large fraction of recent research studies has used questionnaires for their primary assessment of mindfulness (consistent with a broader trend towards measuring psychological constructs via self-report; e.g., Baumeister, Vohs, & Funder, 2007).
Figure 2.
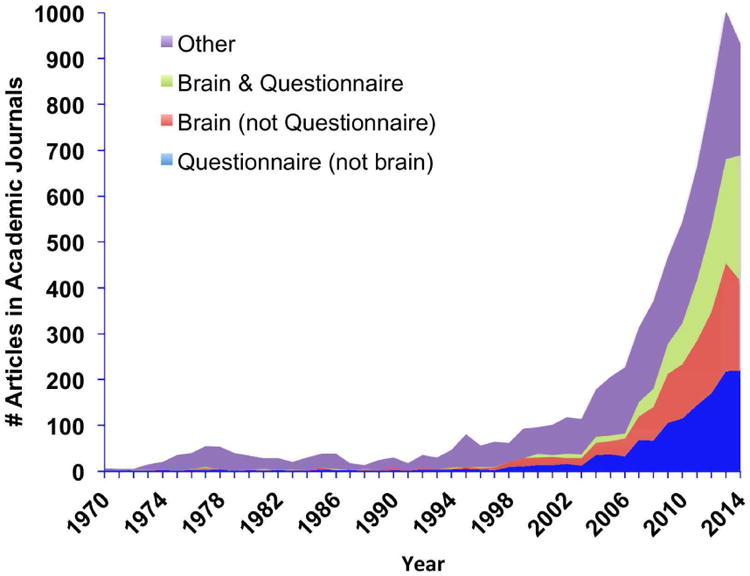
Articles in academic journals by content type. Scopus search limited to articles in academic journals only, published between 1970 and 2014, keywords “mindfulness” or “meditation” for overall search. Brain NOT Questionnaire and Questionnaire NOT Brain as additional key terms.
Problematic aspects of self-report questionnaires
A major challenge to construct validity in psychological assessment is due to reluctance of the field to move beyond logical positivism, a philosophical position that suggests theories are direct derivations of that which can be empirically observed (Green, 1992). Fueled by the prominence of behaviorism, which continues to play a prominent role in contemporary psychology (see e.g., Plaud, 2001), the logical positivistic approach posits that a given measure is equivalent to the construct it purports to measure. In contrast, an alternative, nonjustificationist view suggests that a given measure is merely an approximation of a construct (Embretson, 1983; Strauss & Smith, 2009). Importantly, philosophical views on construct validity can influence the ways that measures are designed and validated. One contemporary extension of logical positivism (which itself would reject the very idea of a construct) seems to be that nomothetic span (e.g., the extent to which a measure converges or diverges from other measures that are related or unrelated, respectively) is all that is needed for construct validity. In contrast to the positivistic view, construct representation (e.g., the psychological processes that give rise to responses on measures that purport to measure the construct) is critical to construct validity (Embretson, 1983; Strauss & Smith, 2009).
Questionnaire-based scales that purport to measure mindfulness offer, at best, modest evidence of nomothetic span. Mindfulness does reliably correlate with other constructs such as emotional intelligence, self-compassion, psychological symptoms, thought suppression, emotion regulation, alexithymia, dissociation, and absent-mindedness (e.g., Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). However, these findings may actually be suggestive of a lack of differentiation from broad features of personality and temperament; meta-analysis of mindfulness measures suggests a strong negative relationship to neuroticism and negative affect (Giluk, 2009). Alternatively, it may suggest that at least some measures of mindfulness relate to general vulnerabilities or skills that are developed across interventions. In other words, these vulnerabilities and/or skills may not be specifically related to mindfulness; an idea supported by increases in mindfulness across both MBSR and an active control condition (Goldberg et al. 2015).
Additional psychometric concerns, largely relating to construct representation, about self-report mindfulness also exist. Notably, several of these scales exhibit different factor structures and response properties between meditators and non-meditators (e.g., Christopher, Charoensuk, Gilbert, Neary, & Pearce, 2009; Van Dam, Earleywine, & Danoff-Burg, 2009), as well as before and after mindfulness training (e.g., Gu, Strauss, Crane, Barnhofer, Karl, Cavanaugh, & Kuyken, 2016). These findings suggest lack of equivalence on a common underlying latent variable, as well as change in how the items are interpreted. One possible reason for this has to do with demand characteristics; one who has practiced mindfulness meditation may understand and value items differently than someone who has not practiced (though see Baer, Samuel, & Lykins, 2011) – a potential conflation of desire to be ‘mindful’ with actually being ‘mindful’ (cf. Grossman, 2011). Of additional concern, mindfulness measures have not always favored the group one might expect to be more mindful; in one case, experienced meditators were less ‘mindful’ than binge-drinkers (Leigh, Bowen, & Marlatt, 2005). Moreover, mindfulness questionnaires do not always correlate with mindfulness meditation practice (Manuel et al. 2016) and the underlying latent variable influencing item response on certain scales may be reflective of some general feature such as inattentiveness (Van Dam et al. 2010).
Self-report based measures of mindfulness may be particularly vulnerable to limitations of introspection because participants may not know exactly which aspects of mental states should be taken into account when making personal assessments. Moreover, making ‘on-line’ judgments about degrees of mindfulness requires a special kind of multi-tasking (Meyer, 2009). In addition, social-desirability biases may be especially pronounced in self-reports about ‘mindfulness’. This is because participants/patients often learn to expect/value improved attention, equanimity, and so forth, while experimenters often fail to hide their hopes that participants will grow in their adeptness at these mental faculties (cf. Jensen, Vangkilde, Frokjaer, & Hasselbalch, 2012).
Consensus about construct validity in measuring ‘mindfulness’
Some promise exists towards more accurate mindfulness measures via subjective report of behavioral indicators (e.g., breath counting; Frewen, Evans, Maraj, Dozois, & Patridge, 2007; Frewen, Lundberg, MacKinley, & Wrath, 2011; Levinson, Stoll, Kindy, Merry, & Davidson, 2014). Yet potential pitfalls exist even in these new measures (Ring, Brener, Knapp, & Mailloux, 2015). Although some self-report questionnaire measures of mindfulness seem to be effective in revealing particular mental and physical changes associated with practicing mindfulness (e.g., Baer, 2011), how closely these measures track exactly what is taught during practice remains unclear. While some investigators have suggested that increased mindfulness improves the quality of participants' introspections (Lutz et al., 2007; Mrazek, Smallwood, & Schooler, 2012; Zanesco, King, MacLean, & Saron, 2013), this claim has not been well established (cf. Fox et al., 2012; Levinson et al., 2014; Sze, Gyurak, Yuan, & Levenson, 2010; Whitmarsh, Barendregt, Schoffelen, & Jensen, 2014). Nor is it entirely obvious how one could veridically establish such a claim, for doing so would require accurate ‘third-person’ evidence about the subjective contents of an introspector's ‘first-person’ consciousness (cf. Lutz, Lachaux, Martinerie, & Varela, 2002). Ironically, were it shown that mindfulness practice improves the quality of participants' introspections, this might deepen other problems in mindfulness research. For example, if mindfulness-based enhancements of introspective accuracy are real, such enhancements could increase honest responding, thereby exacerbating between group confounds.
Perhaps because of such pitfalls in introspection, many studies have focused instead on neurobehavioral performance, attempting to assess mindfulness indirectly (e.g., Brewer et al. 2011; Ferrarelli et al. 2013; Jha et al. 2007; Lao et al. 2016; Lutz et al. 2009; Sahdra et al. 2011). However, these studies have inconsistent and sometimes contradictory empirical findings about the effects of mindfulness training on various basic cognitive and behavioral capacities (e.g., Lao et al. 2016; Jha et al. 2007). Several studies that involved different types of mindfulness training have found modest improvements in the efficiency of attention, orienting, and executive cognitive control after varying types of practice (Jha, Krompinger, & Baime, 2007; Sahdra et al., 2011; Slagter et al., 2007; Tang et al., 2007; van den Hurk, Giommi, Gielen, Speckens, & Barendregt, 2010). Even when statistically significant, the magnitudes of observed cognitive effects stemming from mindfulness practices have been rather small (Chiesa, Calati, & Serretti, 2011; Sedlmeier et al., 2012).
Prescriptive research agenda: Measuring aspects of mindfulness
Given the cultural history and multitude of contextual variations in the term ‘mindfulness,’ scientific research on the aggregate of mental states labeled by it would benefit from redirecting attempts to directly measure mindfulness towards measuring supporting mental faculties. The situation is similar to the psychological study of ‘intelligence’. Because of complexities, historical efforts to obtain a single unitary measure of general intelligence evolved to studying particular cognitive capacities, that, in combination, may make people functionally more or less intelligent (cf. Neisser et al. 1996).
Paralleling such evolution, we recommend that future research on mindfulness aim to produce a body of work for describing and explaining what biological, emotional, cognitive, behavioral, and social, as well as other such mental and physical functions change with mindfulness training. There are two broadly useful contexts in which to approach this problem. The first is to use a multimodal approach wherein first- and third-person (i.e., neurobiological and/or behavioral) assessments are used to mutually inform and identify one another (cf. Lutz et al. 2002; Lutz et al. 2015). This comprises a more theory-driven approach to the problem of understanding mindfulness. A data-driven alternative might be comparable to how individuals in affective neuroscience have used advanced algorithms to integrate physiological and neurobiological signals towards understanding emotional states (cf. Kragel & LaBar, 2014). A second context is to focus on the indirect impact of mindfulness practice, such as how meditation practice might lead to more effective therapists via assessing patient outcome (cf. Grepmair et al., 2007) or how mindfulness might improve caregiver efficacy via assessment of significant others (cf. Singh et al., 2004). Another approach within this domain might be to examine how mindfulness practice can lead to changes in observable behaviors such as eating patterns or interpersonal exchanges (Papies, Pronk, Keesman, & Barsalou, 2015), the latter especially as reported by friends or partners of those undergoing mindfulness and/or meditation training (e.g., Birnie, Garland, & Carlson, 2010). In addition, researchers should situate future process models of mindfulness within extant rigorous theoretical frameworks for cognition and emotion whereby empirical predictions and falsifiable conceptual hypotheses can be tested (e.g., Meyer, 2009; van Vugt, Taatgen, Bastian, & Sackur, 2015; Vago & Silbersweig, 2012). Frameworks based on computational modeling may be especially helpful for such purposes (e.g., Anderson et al., 2004; Meyer & Kieras, 1999).
III.B. Challenges for Clinical Intervention Methodology
Numerous intervention studies have been conducted to assess whether, and by how much, practicing mindfulness may help alleviate various undesirable mental and physical conditions, including pain, stress, anxiety, depression, obesity, addiction, and others. Dimidjian and Segal (2015) estimate, using the NIH stage model for Clinical Science (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014), that only 30% of research using mindfulness-based interventions (MBIs) has moved beyond Stage 1 (Intervention Generation/Refinement). The majority (20%) of research beyond Stage 1 has been conducted at Stage 2a (Efficacy in research clinic: compared to wait-list control or treatment as usual) with a mere 9% (of the total) at Stage 2b (Efficacy in research clinic: compared to active control). Moreover, only 1% of all research has been conducted outside research contexts, a woefully inadequate research base to inform whether MBIs are ready for use in regular clinical practice, as is the case in the UK (Coyne, 2015b; 2016). As a result, some have blatantly stated that, “widespread use is premature” (Greenberg & Harris, 2012).
Haphazard variability across MBIs
Given the lack of consensus about what ‘mindfulness’ means and how it should be operationalized, MBIs have varied greatly in the diverse types of practice, methods of participant training, and duration of instructional courses associated with them. The ‘gold-standard model’ of a MBI has been the eight-week mindfulness-based stress reduction (MBSR; Kabat-Zinn, 1990) course, involving 20-26 hours of formal meditation training during 8 weekly group classes (1.5-2.5 hrs/class), one all-day (6 hr) class, and home practice (∼45 min/day, 6 days/week). Throughout the eight weeks, formal MBSR training has included an eclectic set of specific mindfulness practices – focused attention (FA) on the breath, open monitoring (OM) of awareness in ‘body-scanning’ (cf. Lutz, Slagter, Dunne, & Davidson, 2008), prosocial meditation (e.g., loving-kindness and compassion), and gentle Hatha Yoga.
‘Spin-off’ MBIs vary in content and form depending on the participant populations for which they were adapted and the accompanying idiosyncratic objectives of individual investigators (cf. Shonin, Van Gordin, & Griffiths, 2013). For example, interventions such as Mindfulness-Based Cognitive Therapy (MBCT; Segal et al., 2002) have incorporated aspects of cognitive behavioral therapy (Cognitive Behavioral Therapy, widely considered the most researched and empirically-based psychotherapy, focuses on the relationship between thoughts, emotions, and behaviors, most commonly with a focus on changing thought and behavioral patterns; Tolin, 2010). Notably, there are also a number of psychotherapies that draw on ‘mindful’ principles, but are more commonly associated with traditional cognitive behavioral therapy (cf. Hofmann & Asmundson, 2008); these include Acceptance and Commitment Therapy (ACT; Hayes et al. 1999) and Dialectical Behavior Therapy (DBT; Linehan et al. 1993). We focus our discussions of MBIs on those interventions that utilize formal meditation techniques (namely, derivatives of MBSR), as they arguably differ in origin from those interventions more closely tied to cognitive and/or behavioral therapy (cf. Dimidjian & Segal, 2015; Hayes, 2002; Kabat-Zinn, 2011; Robins, 2002). Moreover, interventions that formally employ meditation practices differ in therapeutic delivery from those that do not formally employ such practices, though this distinction has become muddied as mindfulness and meditation have enjoyed greater mainstream popularity.
The duration of MBIs have been altered dramatically to conform with brief training regimens that may involve as few as four 20-min sessions (e.g., Papies, Barsalou, & Custers, 2012; Zeidan, Emerson, Farris, Ray, Jung, McHaffie, & Coghill, 2015). Some newer MBIs have even implemented web-based or mobile applications for treatment delivery (Cavanaugh et al., 2013; Dimidjian et al., 2014; Lim, Condon, & DeSteno, 2015). Given the variety of practices that fall under the umbrella of MBI, the adoption of mindfulness as a prescriptive clinical treatment has not entailed a consistent type of intervention. While there is considerable variability in other practices of psychotherapy as well, specific classes of intervention (e.g., CBT) at least tend to have sufficient consistency with one another (in terms of content and format) to provide a basis for broad evaluation of their efficacy (cf. Tolin, 2010). In contrast, the varieties of interventions labeled as “mindful”, are as varied as the definitions of the construct (differing in content, meeting type/frequency, instructions, homework, readings, instructor/therapist training and accessibility, etc.). Extreme caution must be exercised when considering mainstream implementation of minimally-tested adaptations of more traditional MBIs (Dimidjian & Segal, 2015).
Misperceptions of therapeutic efficacy
Despite the preceding list of concerns, there is a common misperception in public and government domains that compelling clinical evidence exists for the broad and strong efficacy of mindfulness as a therapeutic intervention (e.g., Freeman, D. & Freeman, J, 2015; Coyne, 2016). Results from some clinical studies conducted over the past ten years have indicated that MBCT may be modestly helpful for some individuals with residual symptoms of depression (Eisendrath et al., 2008; Geschwind, Peeters, Huibers, van Os, & Wichers, 2012; van Aalderen et al., 2012). As a consequence of select results, published in high profile journals, MBCT is now officially endorsed by the American Psychiatric Association for preventing relapse in remitted patients who have had three or more previous episodes of depression. Moreover, the United Kingdom's National Institute for Health and Clinical Excellence now even recommends MBCT over other more conventional treatments (e.g., SSRIs) for preventing depressive relapse (Crane & Kuyken, 2012). Mitigating such endorsements, a recent meta-analysis found that MBSR did not generally benefit patients susceptible to relapses of depression (Strauss, Cavanagh, Oliver, & Pettman, 2014). Other meta-analysis have suggested general efficacy of MBIs for depressive and anxious symptoms (Hofmann et al. 2010), though head-to-head comparisons of MBIs to other evidence-based practices have resulted in mixed findings, some suggesting comparable outcomes, others suggesting MBIs might be superior in certain conditions, and others suggesting CBT is superior in certain conditions (e.g., Arch et al., 2013; Goldin et al. 2016; Manicavascar et al. 2011). There is also mixed evidence comparing MBIs to interventions such as progressive muscle relaxation (e.g., Agee et al. 2009; Jain et al. 2007). Direct comparisons of MBIs to empirically established treatments are limited.
In a recent review and meta-analysis commissioned by the US Agency for Healthcare Research and Quality (AHRQ), MBIs (compared to active controls) were found to have a mixture of only moderate, low, or no efficacy, depending on the disorder being treated. Specifically, the efficacy of mindfulness was only moderate in reducing symptoms of anxiety, depression, and pain. Also, efficacy was low in reducing stress and improving quality of life. There was no effect or insufficient evidence for attention, positive mood, substance abuse, eating habits, sleep, and weight control (Goyal et al., 2014). These and other limitations echoed those from a report issued just seven years earlier (Ospina et al., 2007). The lack of improvement over these seven years in the rigor of the methods used to validate MBIs is concerning; indeed if research does not extend beyond Stage 2A (comparison of MBI to wait-list control), it will be difficult, if not impossible, to ascertain whether MBIs are effective in the real world (cf. Dimidjian & Segal, 2015). On balance, much more research will be needed before we know for what mental and physical disorders, in which individuals, MBIs are definitively helpful.
Consensus about clinical intervention methodology
MBIs are sometimes misleadingly described as “comparable” to antidepressant medications (ADMs)(Goyal et al., 2014). Such comparability has been tentatively supported by results from studies examining MBIs vs. ADMs for depressive relapse in recurrent depression (Segal et al., 2010; Kuyken et al., 2015). Notably, there are large individual differences in efficacy: MBIs may be beneficial for some people, but instead may be ineffective or contraindicated for others (Dobkin, Irving, & Amar, 2011). Special care is therefore needed when interpreting results from clinical studies employing MBIs, many of which have lacked ‘active’ control conditions. Given the absence of scientific rigor in much clinical mindfulness research (Davidson & Kaszniak, 2015; Goyal et al., 2014), evidence for use of MBIs in clinical contexts should be considered preliminary.
The official standards of practice for MBSR exclude suicidality and the presence of any psychiatric disorder (Santorelli, 2014). Case-by-case exceptions are permissible by these standards if, and only if, an individual participant is willing and able to simultaneously maintain adequate medical treatment for the exclusionary condition or if an instructor has sufficient clinical training to manage the case at hand (Santorelli, 2014). The American Psychiatric Association (Shapiro, 1982), US National Institutes of Health (NIH) (NCCAM/NIH, 2014), and leading researchers in the field (Dobkin et al., 2011; Greenberg & Harris, 2012; Lustyk et al., 2009) have expressed concerns that meditation may be contraindicated under several circumstances. Numerous authors have recommended that Schizophrenia spectrum disorders, Bipolar disorder, Post-traumatic stress disorder, Depression, and risk-factors for psychosis (e.g., Schizoid personality disorder) are contraindications to participation in an MBI that is not specifically tailored to one of these conditions (Didonna & Gonzalez, 2009; Dobkin et al. 2012; Germer, 2005; Kuijpers et al. 2007; Lustyk et al. 2009; Manocha, 2000; Walsh & Roche, 1979; Yorston, 2001). The rationale for these contraindications is that without sufficient clinical monitoring, an intervention not designed to address these issues could lead to deterioration or worse. Such contraindications should be considered exclusionary criteria for regular clinical practice until substantially more evidence about the efficacy of various MBIs becomes available.
Prescriptive research agenda: Strengthening clinical intervention methods
Replication of earlier studies with appropriately randomized designs and proper active control groups will be absolutely crucial. In conducting this work, we recommend that researchers provide explicit detail of mindfulness measures (e.g., see Table 1), primary outcome measures, mindfulness/meditation practices (see Table 2), and intervention protocol (see Table 3). While active control groups for MBIs can be difficult to implement for a variety of reasons (Davidson & Kazniak, 2015), the problem is not insurmountable (see e.g., MacCoon et al. 2012) and has been resolved by those conducting more traditional psychotherapy research (e.g., Arch et al., 2013; Agee et al. 2009; Goldin et al. 2016; Jain et al. 2007; Manicavascar et al. 2011). Additionally, researchers must be explicit about the exact hypothesis they are testing (non-inferiority to an established treatment, superiority to an established treatment, etc.) and consider the various limitations that might accompany treatment designs (see e.g., Coyne, 2015a).
Because of potential confirmation biases (Rosnow, 2002) and allegiance effects (Martin, Garske, & Davis, 2000), clinical research ideally would involve multidisciplinary teams of investigators. These teams should consist not only of clinicians, but also basic research scientists, scholars from within classical mindfulness traditions, and scientists/scholars skeptical about mindfulness's efficacy. An especially compelling research strategy could involve adversarial collaboration (see e.g., Matzke et al., 2015). Moreover, future clinical studies should not rely merely on self-report and assessments by clinicians, but also incorporate biological and behavioral efficacy measures.
III.C. Harm, Adverse Effects, and Fallout of Meditation Practices
Much of the public news media has touted mindfulness as a universal panacea for what ails human kind (e.g., Chan, 2013; Firestone, 2013), overlooking the very real potential for several different types of harm. According to Directors of the National Center for Complementary and Integrative Medicine (NCCIH) at the National Institutes of Health (NIH), the biggest potentials for harm of complementary treatments (e.g., meditation) are “unjustified claims of benefit, possible adverse effects…and the possibility that vulnerable patients with serious diseases may be misled” (Briggs, & Killen, 2013). Identifying “harm”, “side effects”, or “adverse effects” is complicated by issues related to definitions and measurement, which will be addressed in turn.
Coming to terms with meditation-related adverse effects
An adverse effect or event (AE) is any unwanted, harmful effect that results from, but is not the stated goal of a given treatment. A side effect is any unexpected effect that is secondary to the intended effect of the treatment (Linden, 2013). An event can also be categorized a “side effect” if it is not described in the “product labeling”, “package insert”, “marketing or advertising” (NIA, 2011; OHRP, 2007) – descriptions that are often lacking for meditation practices (and behavioral interventions more generally, despite a comparable incidence of AEs to pharmacological treatments; Crawford et al., 2016; Linden, 2013; Mohr, 1995; Moos, 2005, 2012). Whether the result of correct or incorrect treatment, a treatment-emergent reaction may include the appearance of novel symptoms that did not exist before treatment, or the exacerbation or re-emergence of a pre-existing condition. Treatment non-response or deterioration of (target) illness may or may not be caused by the treatment (Linden, 2013) but requires both reporting and action.
Meditation-related experiences that were serious or distressing enough to warrant additional treatment or medical attention have been reported in more than 20 published case reports or observational studies. These reports document instances of meditation-related or “meditation-induced” (i.e., occurring in close temporal proximity to meditation and causally attributed to meditation by the practitioner, instructor, or both) psychosis, mania, depersonalization, anxiety, panic, traumatic-memory re-experiencing, and other forms of clinical deterioration (Boorstein, 1996; Carrington, 1977; Castillo, 1990; Chan-Ob, & Boonyanaruthee, 1999; Disayavanish, & Disayavanish, 1984; Epstein, & Lieff, 1981; Heide, & Borkovec, 1983; Kerr et al., 2011; Kornfield, 1979; Kuijpers et al., 2007; Kutz et al., 1985; Lomas et al., 2014; Miller, 1993; Nakaya, & Ohmori, 2010; Sethi, 2003; Shapiro, 1992; Shonin et al., 2014; Shonin et al, 2014; Van Nuys, 1973; VanderKooi, 1997; Walsh, & Roche, 1979; Yorston, 2001). Many of the aforementioned were case studies, case series, or observational studies, often without a control group. Only two were prospective (Shapiro, 1992; Shonin et al 2014). Detailed clinical histories were available for some of the subjects, but not all, which makes the question of pre-existing conditions difficult to evaluate. While qualitative reports and case studies are an appropriate and necessary first step in identifying potential AEs (Dimidjian, & Hollon, 2010), the need for AE assessments within more rigorous designs such as randomized controlled trials would provide more conclusive information.
Issues in the measurement of adverse effects
Since safety reporting is required for federally funded clinical trials, one might expect that the many National Institute of Health (NIH) funded mindfulness or meditation trials would be a rich source of information about potential adverse effects with causality assessment inherent in randomized controlled trial (RCT) design. However, most current methods for assessing AEs in meditation-related research are insufficient to produce an accurate estimate. Despite CONSORT requirements (Moher et al., 2001), and compared to 100% of pharmacology trials (Vaughan et al., 2014), less than 25% of meditation trials actively assess AEs (Goyal et al., 2014; Jonsson et al., 2014), relying instead on spontaneous reporting, which may underestimate AE frequency by more than 20-fold (Bent et al., 2006), and results in widely varying AE rates, even for similar trials (Kuyken et al., 2015; Kuyken et al., 2016; Williams et al., 2014). Different AE assessment methods (Vaughan et al., 2014) or specifically the lack of systematic AE assessment in meditation trials, has led not only to the hasty erroneous conclusion that meditation is free of AEs (Turner et al., 2011), but also that meditation interventions can act as a replacement to medication for mental illnesses such as depression and bipolar disorder (Annels et al., 2016; Strawn et al., 2016; Walton, 2014) with slogans such as, “meditate not medicate” (Annels et al., 2016). Furthermore, meditation-related AEs are discussed in many traditional (largely Buddhist) meditation guides (Buddhaghosa, 1991; Sayadaw, 1965; Wallace, 2011). Despite the assumption of “wide acceptance of minimal, if any, adverse events associated with meditation” (Turner et al., 2011), this assumption is largely based on a lack of research rather than substantive evidence.
Other potential risks of mindfulness meditation
The benefits and the safety of meditation are likely exaggerated beyond available evidence in a manner that increases “the possibility that vulnerable patients with serious diseases may be misled” (Briggs, & Killen, 2013). In the face of such exaggerated claims, patients may be diverted from pursuing other, more traditional activities (e.g., regular aerobic exercising) that typically yield physical and mental benefits (Cotman, Berchtold, & Christie, 2007; Penedo & Dahn, 2005) or standard treatments (e.g., psychotherapy, pharmacotherapy) that are better suited to dealing with particular psychiatric conditions. For example, in a recent meta-analysis of MBIs Strauss et al (2014) concluded, “…given the paucity of evidence in their favour, we would caution against offering MBIs as a first line intervention for people experiencing a primary anxiety disorder… findings from the current meta-analysis would suggest great caution if offering MBIs to this population as a first line intervention instead of a well-established therapy” (Strauss et al., 2014). In economics, as well as recent discussions of psychotherapy, this effect has been labeled an “opportunity cost” (i.e., time and money invested in a treatment approach that has little to no therapeutic benefit relative to the potential time/money that could have been invested in a treatment more likely to yield improvement; cf. Lilienfeld, Lynn, & Lohr, 2003). Given that relief from anxiety is probably one of most widely promoted benefits of mindfulness (see e.g., Hofmann et al. 2010), opportunity cost may be a widespread “side effect” of MBI hype.
Consensus about harm, adverse effects, and contraindications
To date, “official” clinical guidelines about the state of meditation-related risks are in their infancy and only a handful of organizations and regulatory agencies have issued any statements. The American Psychiatric Association first showed concern about meditation-related adverse effects in 1977, and commissioned a report on the topic with treatment guidelines (Shapiro, 1982). The APA also included descriptions of meditation-induced depersonalization and other clinically relevant problems in both the 4th and 5th editions of their Diagnostic and Statistical Manual of Mental Disorders (DSM; APA, 1994, 2013). The NIH states that “meditation could cause or worsen certain psychiatric problems” but does not provide any practice guidelines beyond a boilerplate disclaimer to “check with your doctor” before trying meditation (NCCIH, 2016).
Since neither meditation-writ-large nor meditation-based interventions are overseen by any regulatory agencies, most of the clinical guidelines and recommendations regarding risk and safety have been issued by the “Centers for Mindfulness”, creators of interventions, as well as various experts in the field. Many meditation researchers and clinicians have offered reviews of meditation-related risks, adverse effects or contraindications with recommendations for clinical guidelines (Dobkin et al., 2012; Fenwick, 1983; Greenberg, & Harris, 2012; Hanley et al., 2016; Lustyk et al., 2009; Shapiro, 1982; Shonin et al., 2014). The MBCT Implementation Resources (Kuyken et al 2012) is one of the first documents to list potential “risks to participants”, including increased likelihood of suicidality, depression, negative emotions, and flashbacks during meditation for individuals with trauma histories. At present, management strategies for potential risks have been largely limited to exclusion and informed consent. Both the University of Massachusetts Center for Mindfulness and the Oxford Mindfulness Centre have published recommended exclusion criteria for standard MBSR and MBCT, both excluding current suicidality and/or any current psychiatric disorder (Kuyken et al., 2012; Santorelli, 2014). In addition, many centers attempt to make clear that mindfulness is not intended to replace standard psychiatric care.
Prescriptive research agenda: Transcending adverse effects
The current guidelines, while preliminary, represent substantial progress in assessing and promoting safety of meditation-based interventions. On the measurement front, there have been signs of progress. A few MBI researchers have started to actively monitor AEs either through questionnaires or through clinician interviews (Kuyken et al., 2015; Kuyken et al., 2016; Williams et al., 2014). While these are typically limited to serious AEs (life-threatening or fatal events) or “deterioration” on pre-existing clinical outcomes that require clinical attention, such as increased depression or suicidality, this is a considerable improvement from passive monitoring.
In addition, a recent qualitative study of 60 Buddhist meditators and meditation teachers entitled “The Varieties of Contemplative Experience” (c.f. Rocha, 2014) also sought to improve knowledge of meditation-related experiences that are underreported, unexpected, “adverse”, or associated with significant levels of distress and functional impairment. While qualitative and retrospective, this study applied 11 of the 13 causality criteria (as outlined by the World Health Organization, Federal Drug Administration, and NIH; Agbabiaka et al., 2008; NIH, 2016; WHO, 2016), including interviews with meditation teachers (expert judgment). The study produced 60 categories of meditation-related experiences and 26 categories of “influencing factors” that may impact the duration, associated distress, and impairment of the experience. While the first study of its kind, it sets a foundation for testable hypotheses in future research. In addition, the 60 categories of meditation-related experiences are being converted into a measurement tool that can be used for systematic assessment across multiple studies and conditions. The codebook was inserted as an interview-based assessment into a recently-completed clinical dismantling trial of MBCT (NCT# 01831362) which can assess whether similar experiences occur in MBIs, as well as address the question of biological gradient (i.e., whether more exposure results in greater effects; Hill, 1965).
The large and growing body of empirical data on the psychological and neurobiological effects of meditation and related practices also represent a step forward to identifying potential mechanisms by which meditation-related effects, as well as AEs might occur. Knowledge of mechanism may help identify who is at risk. For example, there is some evidence that hyper-connectivity of the prefrontal cortex and limbic regions may result in affective and autonomic blunting which is characteristic of dissociation (Ketay et al., 2014; Sierra et al., 2002). Similarly, increased activity in the inferior parietal cortex, a common outcome of mindfulness training (Brefczynski-Lewis et al., 2007; Farb et al., 2007; Goldin, & Gross, 2010; Hasenkamp et al., 2012), might relate to depersonalization (disembodiment, loss of agency and self-other/self-world boundaries; Bunning, & Blanke, 2005). Others have created neurobiological models for specific meditation-related experiences, such as visual hallucinations, (Lindahl et al., 2014), sleep-related changes (insomnia; Britton et al., 2014), changes in sense of self (Dor-Ziderman et al., 2013) and altered perceptions of space and time (Berkovich-Ohana et al., 2013).
Research on adverse effects of treatments that share mechanisms with meditation should also be considered. For example, treatments that restrict environmental stimulation or narrative processing through internal sensory focus, such as Qigong (APA, 2000; Shan, 2000), autogenic training (Linden, 1990), and relaxation (Edinger, & Jacobsen, 1982), can precipitate similar AEs, such as autonomic hyperarousal, perceptual disturbances (Lindahl et al., 2014), traumatic memory re-experiencing (Brewin, 2015; Brewin et al., 2010; Miller, 1993), and psychosis (APA, 2000; Shan, 2000). Relaxation-induced panic or anxiety (RIP/RIA) is perhaps one of the most well documented phenomena with clear relevance to meditation (Adler et al., 1987; Cohen et al., 1985; Heide, & Borkovec, 1983).
III.D. Challenges for Investigating Mindfulness through Contemplative Neuroscience
As part of the burgeoning trend in research on mindfulness and meditation more generally (Figure 1), investigators have increasingly used methods from Cognitive Neuroscience (cf. Gazanniga & Mangun, 2014), especially functional magnetic-resonance imaging (fMRI). These methods yield visual depictions of participants' relative, regionally localized, brain activation during various types of cognitive task performance as well as the integrated functional neural networks of mental processing (including the default mode network; cf. Power et al. 2011). The investigation of mindfulness through such methods has also come to be known as Contemplative Neuroscience (e.g., Davidson & Lutz, 2008).
Limitations in depictions of brain activity based on neuroimaging
Representative pictures from fMRI and other neuroimaging methods do not clearly convey the complex – often fraught – chain of biological and computational steps that lead to inferences about changes in brain structure and function. They also neglect to highlight the fact that such inferences are frequently derived from averages obtained across groups of participants. Thus, when also accompanied by numerous other difficult experimental, statistical, and inferential challenges prevalent in psychological research, Contemplative Neuroscience has often led to overly simplistic interpretations of nuanced neurocognitive and affective phenomena. For example, psychologist Rick Hanson, in what is presumably an effort to explain how meditation has been shown to influence emotion regulation, correlated with alterations in amygdala activity (e.g., Goldin & Gross, 2010), has stated, “ In terms of amydgala activity, people seem to belong to one of three groups…the ones with a joyful amydgala – are more focused on promoting the good than on preventing the bad.” (Hanson, 2013, pp. 43-44). As a result of such oversimplifications, meditative benefits may be exaggerated and undue societal urgency to undertake mindfulness practices may be encouraged (e.g., Farias & Wikholm, 2015).
Problematic aspects of group-level neuroimaging analyses
Furthermore, results from neuroimaging during mindfulness practices and other types of meditation may be subject to unique confounds. Despite variability in different types of practice and meditative experiences, it is not uncommon for neuroimaging data obtained from diverse practitioners to be pooled in aggregated analyses (e.g., Luders et al., 2012; Luders, Kurth, Toga, Narr, & Gaser, 2013; Ferrarelli et al. 2013; Sperduti, Martinelli, & Piolino, 2012). Also complicating theoretical interpretation of their results and further adding to confounds associated with systematic individual differences, many neuroimaging studies have used cross-sectional designs, precluding possible inferences about underlying cause-and-effect relationships (cf. Tang et al., 2015).
Ancillary physical artifacts in neuroimaging data
Certain methodological confounds that plague neuroimaging studies in general, are of particular concern in studies of individuals who meditate. Physical artifacts involving head movements and cardio-respiratory effects are especially notable (Holmes, Solomon, Cappo, & Greenberg, 1983; Lutz, Greischar, Perlman, & Davidson, 2009; Reuter et al., 2015; Van Dijk, Sabuncu, & Buckner, 2012; Wallace, 1970; Wallace, Benson, & Wilson, 1971; cf. Lazar et al. 2000; Zeidan et al. 2011). If non-meditators are more restless or breathe more rapidly than experienced meditators during MRI sessions, there could be spurious group differences in some neuroimaging measurements (e.g., with respect to meditators, seemingly more brain gray-matter and brain activation in particular neuroanatomical regions; cf. Greene, Black, & Schlaggar, 2016). Systematic individual differences in cardio-respiratory activity between non-meditators and meditators are especially worrisome because of the so-called ‘vein-drain problem’ (Turner, 2002). It prevails especially in typical regions of differential brain activation. Enlarged blood vessels may lead to measurement artifacts (e.g., Boubela et al., 2015), which can be particularly pronounced in brain regions commonly identified as important for cognition and emotion (e.g., insular and anterior cingulate cortices).
Partially mitigating these concerns, meta-analyses of both structural and functional neuroimaging data have revealed differences in brain regions that tend to be consistent with the specific meditation practices under study (e.g., changes in brain regions associated with bodily awareness of mindfulness practitioners – for example, the insula and somatosensory cortices --and widespread recruitment of brain regions associated with vision during meditative visualization). Such findings, when supported by results from meta-analyses of multiple studies, are less likely to have stemmed merely from artifacts (Fox et al., 2014; Fox et al., 2016).
Practical vs. statistical significance of neuroimaging data
Statistical and theoretical approaches to calculating and interpreting effect sizes and associated confidence intervals have been well developed in behavioral and psychological research (Cumming, 2014). Yet calculating valid estimates of effect sizes in neuroimaging data is extremely difficult (Fox et al., 2014; Fox et al., 2016; Friston, 2012; Hupé, 2015). Consequently, the practical significance and clinical importance (e.g., diagnostic and/or therapeutic utility) of observed changes in brain structure and neural activity associated with practicing mindfulness is still elusive (cf. Castellanos, Di Martino, Craddock, Mehta, & Milham, 2013). Moreover, despite some agreement among investigators that mindfulness and other types of meditation affect the brain, we still do not know how their effects compare to other cognitive training methods in terms of practical significance.
Consensus about findings from Contemplative Neuroscience
Despite the many serious limitations mentioned previously, studies in Contemplative Neuroscience do allow some preliminary conclusions. Meta-analyses of neuroimaging data suggest modest changes in brain structure due to practicing mindfulness (Fox et al., 2014). Some concomitant modest changes also have been observed in neural function (e.g., Sperduti et al., 2012; Tomasino, Fregona, Skrap, & Fabbro, 2013; Fox et al., 2016; for a broad review, see Tang et al, 2015). Caution must exerted in interpreting these findings; similar changes have been observed following other forms of mental and physical skill acquisition, such as learning to play musical instruments and learning to reason, suggesting that they may not be unique to mindfulness or other popular types of meditation practice (cf. Draganski & May, 2008; Hyde et al., 2009; Mackey, Singley, & Bunge, 2013; Münte, Altenmüller, & Jäncke, 2002).
Prescriptive research agenda: Truth in advertising by Contemplative Neuroscience
Rather than contributing to further media hype, researchers in Contemplative Neuroscience must endeavor to communicate more accurately with other scientists, journalists, and the public about not only the potential benefits of mindfulness practices for mental processes and brain mechanisms, but also about the serious limitations of neuroimaging methods and data collected through them. We encourage contemplative neuroscientists to follow best practices in neuroimaging methods generally (cf. Nichols et al. 2017), but also to consider and accommodate unique issues that may arise while collecting brain data from meditating populations. These unique issues (e.g., different respiration rates, different cardiac activity, dramatically different demographic and life-style characteristics) may warrant unique data collection methods (e.g., cardiac-gated image acquisition) and/or analytic methods (e.g., removal of activity due to respiratory artifact), as well as very detailed demographic information. Particular attention should be paid to methodologically and/or statistically controlling potential contributions from a panoply of confounded variables (e.g., participant motivation, placebo effects, cardio-respiratory factors, head motion, history of psychopathology) that may underlie apparent group differences. This will be especially necessary where mindfulness studies compare results from long-term practitioners versus meditation-naïve participants. In contexts of comparing meditation experience, either between-groups, or within, some common metric should be used (cf. Hasenkamp & Barsalou, 2012). Researchers should stress specifically that individuals who already have meditated over many years, or who – though not yet experts – are personally attracted to meditation, may have characteristics that differentiate them from the general population even before experimentation (Mascaro, Rilling, Negi, & Raison, 2013). Prominent mention about the limitations and fraught nuances of statistical neuroimaging analyses should not be entirely neglected either. No amount of sophisticated statistical prowess can correct results from faulty or confounded methods: a fact to which researchers, scientists, and the public should regularly be reminded.
And, ultimately, the popular news media – inspired by honest, forthright, thorough cooperation with contemplative neuroscientists – must persuade the general public together with government funding agencies that multiple large, longitudinal, randomized-control trials (RCTs) that consider participant preferences concerning mindfulness practices are required, and should be funded. We need such trials in order to definitively determine the full benefits and costs of practicing mindfulness. Without future RCTs, prevalent widespread uncertainties surrounding past results from haphazard studies of mindfulness involving relatively small sample sizes (e.g., Button et al., 2013) and considerable variation in how neuroimaging methodologies have been implemented (Simmons et al., 2011) make it difficult to know the neural effects of mindfulness.
IV. Conclusion
Contemplative psychological scientists and neuroscientists, along with other researchers who study mental processes and brain mechanisms underlying the practice of mindfulness and related types of meditation, have a considerable amount of work to make meaningful progress. Much work should go toward improving the rigor of methods used, along with the accuracy of news-media publicity and eliminating public misunderstandings caused by past undue ‘Mindfulness Hype’. These efforts have to take place on several related fronts.
First, as mentioned before, the various possible meanings of ‘mindfulness’ have to be clarified. To deal with prevailing inherent semantic ambiguities, researchers should adopt more nuanced, precisely focused, terminology for referring to the various distinct mental and physical states as well as overt behaviors often associated with mentions of ‘mindfulness’ (see Table 2). In so far as future research involves self-report questionnaires about mindfulness, new ones that incorporate specific terminology (see e.g., Table 2) ought to be developed. Theoretical models formulated to account for data need also consider these new key terms.
Second, future studies of mindfulness should conform to lessons being learned from the ongoing ‘replication crisis’ in Psychological Science and other related scientific disciplines. For example, Pre-registered experiments and Open-Science replications of mindfulness are desirable. Additional discipline is especially needed in light of recent growing troublesome meta-analytic evidence that -- like some other ‘glitzy’ popular topics of psychological and neural investigations -- past mindfulness research has succumbed to these questionable practices (Coronado-Montoya et al., 2016).
Third, future clinical applications involving mindfulness-based interventions must seek to attain more uniformity and better control (see Table 3), especially where definitive answers have yet to be found. It is critical that those who conduct clinical research provide warnings regarding the extent to which their research findings generalize to clinical practice. Also, researchers and clinicians have to be put on guard, educated about, and encouraged to address the potential adverse effects stemming from mindfulness practices. Research on the nature and scope of potential adverse effects should receive considerable further attention and government funding, due to the public's rapidly increasing involvement in practicing mindfulness.
Fourth, as they continue to emerge through technological advances in neuroimaging methods, new findings from Contemplative Neuroscience about the mental processes and brain mechanisms of mindfulness practices must be reported with all due modesty. Their importation into protocols for future clinical practice must await proper vetting of the potential practical significance that may accompany them. This vetting process will have to deal diligently with the many aforementioned challenges that still remain to be surmounted by the Contemplative Neuroscience community.
Only with such diligent multi-pronged future endeavors may we hope to surmount the prior misunderstandings and past harms caused by pervasive Mindfulness Hype that has accompanied the Contemplative Science movement.
Acknowledgments
We dedicate this article to our dear friend and colleague, Cathy Kerr, who passed away unexpectedly during revision of this work. Cathy was among the key driving forces that led to this particular group forming and to our formal meeting in Amherst, MA in July, 2014. Cathy touched so many lives and had a profound influence on the variety of ways that many of us approach mindfulness and meditation research. She will be profoundly missed.
This article grew out of a series of conferences and workshops generously funded by the Mind and Life Institute. However, the views expressed here are those of the authors' alone, collectively, and do not necessarily represent the views or policies of the Mind and Life Institute nor any other organizations with which the authors are affiliated. We would further like to add that while all authors contributed to the article, it should be read as a majority consensus. In other words, not all authors strictly ascribe to all statements contained herein.
References
- Adler C, Craske M, Barlow D. Relaxation-induced panic: When resting isn't peaceful. Integrative Psychiatry. 1987;9:94–112. [Google Scholar]
- Agbabiaka TB, Savovic J, Ernst E. Methods for causality assessment of adverse drug reactions: a systematic review. Drug Safety. 2008;31:21–37. doi: 10.2165/00002018-200831010-00003. [DOI] [PubMed] [Google Scholar]
- Agee JD, Danoff-Burg S, Grant CA. Comparing brief stress management courses in a community sample: Mindfulness skills and progressive muscle relaxation. Explore: The Journal of Science and Healing. 2009;5:104–109. doi: 10.1016/j.explore.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Arch JJ, Ayers CR, Baker A, Almklov E, Dean DJ, Craske MG. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behaviour Research and Therapy. 2013;51:185–196. doi: 10.1016/j.brat.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Analayo B. Sattipatthana: The direct path to realization. Birmingham: Windhorse Publications; 2003. [Google Scholar]
- Anderson JR, Bothell D, Byrne MD, Douglas S, Lebiere C, Qin Y. An integrated theory of mind. Psychologial Review. 2004;111:1036–1060. doi: 10.1037/0033-295X.111.4.1036. [DOI] [PubMed] [Google Scholar]
- Annels S, Kho K, Bridge P. Meditate don't medicate: How medical imaging evidence supports the role of meditation in the treatment of depression. Radiography. 2016;22:e54–e58. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorder s (DSM IV) 4th. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4th. Arlington, VA: American Psychiatric Association; 2000. Text Revision (DSM-IV-TR) [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington VA: American Psychiatric Association; 2013. DSM-5. [Google Scholar]
- Baer RA. Measuring mindfulness. Contemporary Buddhism. 2011;12(1):241–261. http://doi.org/10.1080/14639947.2011.564842. [Google Scholar]
- Baer RA, Samuel DB, Lykins EL. Differential item functioning on the Five Facet Mindfulness Questionnaire is minimal in demographically matched meditators and nonmeditators. Assessment. 2011;18:3–10. doi: 10.1177/1073191110392498. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: The Kentucky inventory of mindfulness skills. Assessment. 2004;11:191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- Baker TB, McFall RM, Shoham V. Current status and future prospects of clinical psychology toward a scientifically principled approach to mental and behavioral health care. Psychological Science in the Public Interest. 2008;9(2):67–103. doi: 10.1111/j.1539-6053.2009.01036.x. http://doi.org/10.1111/j.1539-6053.2009.01036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett E. Mindfulness: The saddest trend of 2015. 2015 Jan 8; Retrieved from http://www.telegraph.co.uk/women/womens-life/11331034/Mindfulness-the-saddest-trend-of-2015.html.
- Baumeister RF, Vohs KD, Funder DC. Psychology as the Science of Self-Reports and Finger Movements: Whatever Happened to Actual Behavior? Perspectives on Psychological Science. 2007;2(4):396–403. doi: 10.1111/j.1745-6916.2007.00051.x. http://doi.org/10.1111/j.1745-6916.2007.00051.x. [DOI] [PubMed] [Google Scholar]
- Bent S, Padula A, Avins A. Better ways to question patients about adverse medical events. Annals of Internal Medicine. 2006;144(4):257. doi: 10.7326/0003-4819-144-4-200602210-00007. [DOI] [PubMed] [Google Scholar]
- Bergomi C, Tschacher W, Kupper Z. The assessment of mindfulness with self-report measures: Existing scales and open issues. Mindfulness. 2013;4:191–202. [Google Scholar]
- Berkovich-Ohana A, Dor-Ziderman Y, Glicksohn J, Goldstein A. Alterations in the sense of time, space, and body in the mindfulness-trained brain: a neurophenomenologically-guided MEG study. Frontiers in Psychology. 2013;4:912. doi: 10.3389/fpsyg.2013.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR) Psycho-Oncology. 2010;9:1004–1009. doi: 10.1002/pon.1651. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, N D, Carmody J, et al. Devins G. Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice. 2004;11(3):230–241. http://doi.org/10.1093/clipsy.bph077. [Google Scholar]
- Bodhi B. What does mindfulness really mean? A canonical perspective. Contemporary Buddhism: An Interdisciplinary Journal. 2011;12(1):19–39. [Google Scholar]
- Boorstein S. Clinical aspects of meditation. In: Scotton B, Chinen A, Battista J, editors. Textbook of Transpersonal Psychiatry and Psychology. New York: Basic Books; 1996. [Google Scholar]
- Boubela RN, Kalcher K, Huf W, Seidel EM, Derntl B, et al. Moser E. fMRI measurements of amygdala activation are confounded by stimulus correlated signal fluctuation in nearby veins draining distance brain regions. Scientific Reports. 2015;5:10499. doi: 10.1038/srep10499. http://doi.org/10.1038/srep10499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun E. The Birth of Insight: Meditation, Modern Buddhism, and the Burmese Monk Ledi Sayadaw. University of Chicago Press; 2013. [Google Scholar]
- Brefczynski-Lewis JA, Lutz A, Schaefer HS, Levinson DB, Davidson RJ. Neural correlates of attentional expertise in long-term meditation practitioners. Proceedings of the National Academy of Sciences. 2007;104:11483–11488. doi: 10.1073/pnas.0606552104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proceedings of the National Academy of Sciences. 2011;108(50):20254–20259. doi: 10.1073/pnas.1112029108. http://doi.org/10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR. Re-experiencing traumatic events in PTSD: new avenues in research on intrusive memories and flashbacks. European Journal of Psychotraumatology. 2015;6:27180. doi: 10.3402/ejpt.v6.27180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Gregory JD, Lipton M, Burgess N. Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychological Review. 2010;117:210–232. doi: 10.1037/a0018113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs J, Killen J. Perspectives on Complementary and Alternative Medicine Research. JAMA. 2013;310:691–692. doi: 10.1001/jama.2013.6540. [DOI] [PubMed] [Google Scholar]
- Britton WB. Scientific literacy as a foundational competency for teachers of mindfulness-based interventions. In: McCown D, Reibel DK, Miccozzi MS, editors. Resources for Teaching Mindfulness: A Cross-Cultural and International Handbook. New York: Springer; 2016. [Google Scholar]
- Britton WB, Lepp NE, Niles HF, Rocha T, Fisher N, Gold J. A randomized controlled pilot trial of classroom-based mindfulness meditation compared to an active control condition in 6th grade children. Journal of School Psychology. 2014;52:263–278. doi: 10.1016/j.jsp.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton WB, Lindahl JR, Cahn BR, Davis JH, Goldman RE. Awakening is not a metaphor: The effects of Buddhist meditation practices on basic wakefulness. Annals of the New York Academy of Sciences. 2014;1307(1):64–81. doi: 10.1111/nyas.12279. http://doi.org/10.1111/nyas.12279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. http://doi.org/10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Addressing fundamental questions about mindfulness. Psychological Inquiry. 2007;18(4):211–237. [Google Scholar]
- Buddhaghosa B. In: The Path of Purification. Nanamoli B, translator. Onalaska, WA: Buddhist Publication Society; 1991. [Google Scholar]
- Bugental FJ. The existential crisis in intensive psychotherapy. Psychotherapy: Theory, Research & Practice. 1965;2(1):16–20. http://doi.org/10.1037/h0088602. [Google Scholar]
- Bunning S, Blanke O. The out-of body experience: precipitating factors and neural correlates. Progress in Brain Research. 2005;150:331–350. doi: 10.1016/S0079-6123(05)50024-4. [DOI] [PubMed] [Google Scholar]
- Button KS, Ioannidis JP, Mokrysz C, Nosek BA, Flint J, Robinson ES, Munafò MR. Power failure: Why small sample size undermines the reliability of neuroscience. Nature Reviews Neuroscience. 2013;14(5):365–376. doi: 10.1038/nrn3475. [DOI] [PubMed] [Google Scholar]
- Carrington P. The Misuse of Meditation: Problems from Overmeditation to Freedom in Meditation. Garden City, NY: Anchor; Books: 1977. [Google Scholar]
- Castellanos FX, Di Martino A, Craddock RC, Mehta AD, Milham MP. Clinical applications of the functional connectome. Neuroimage. 2013;80:527–540. doi: 10.1016/j.neuroimage.2013.04.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo R. Depersonalization and meditation. Psychiatry Research: Neuroimaging Section. 1990;53:158–168. doi: 10.1080/00332747.1990.11024497. [DOI] [PubMed] [Google Scholar]
- Castonguay LG, Boswell JF, Constantino MJ, Goldfried MR, Hill CE. Training implications of harmful effects of psychological treatments. The American Psychologist. 2010;65(1):34–49. doi: 10.1037/a0017330. http://doi.org/10.1037/a0017330. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Strauss C, Cicconi F, Griffiths N, Wyper A, Jones F. A randomised controlled trial of a brief online mindfulness-based intervention. Behaviour Research and Therapy. 2013;51(9):573–578. doi: 10.1016/j.brat.2013.06.003. http://doi.org/10.1016/j.brat.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Chan AL. 20 Reasons To Love Mindfulness (According To Science) 2013 Retrieved January 5, 2016, from http://www.huffingtonpost.com/2013/04/08/mindfulness-meditation-benefits-health_n_3016045.html.
- Chan-Ob T, Boonyanaruthee V. Meditation in association with psychosis. Journal of the Medical Association of Thailand. 1999;82:925–930. [PubMed] [Google Scholar]
- Chiesa A, Calati R, Serretti A. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clinical Psychology Review. 2011;31(3):449–464. doi: 10.1016/j.cpr.2010.11.003. http://doi.org/10.1016/j.cpr.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Christopher MS, Charoensuk S, Gilbert BD, Neary TJ, Pearce KL. Mindfulness in Thailand and the United States: A case of apples versus oranges? Journal of Clinical Psychology. 2009;65(6):590–612. doi: 10.1002/jclp.20580. http://doi.org/10.1002/jclp.20580. [DOI] [PubMed] [Google Scholar]
- Cohen AS, Barlow DH, Blanchard EB. Psychophysiology of relaxation-associated panic attacks. Journal of Abnormal Psychology. 1985;94:96–101. doi: 10.1037//0021-843x.94.1.96. [DOI] [PubMed] [Google Scholar]
- Coronado-Montoya S, Levis AW, Kwakkenbos L, Steele RJ, Turner EH, Thombs BD. Reporting of positive results in randomized controlled trials of mindfulness-based mental health interventions. PLOS One. 2016 doi: 10.1371/journal.pone.0153220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotman CW, Berchtold NC, Christie LA. Exercise builds brain health: Key roles of growth factor cascades and inflammation. Trends in Neurosciences. 2007;30(9):464–472. doi: 10.1016/j.tins.2007.06.011. http://doi.org/10.1016/j.tins.2007.06.011. [DOI] [PubMed] [Google Scholar]
- Crane RS, Kuyken W. The Implementation of Mindfulness-Based Cognitive Therapy: Learning From the UK Health Service Experience. Mindfulness. 2012;4(3):246–254. doi: 10.1007/s12671-012-0121-6. http://doi.org/10.1007/s12671-012-0121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford MJ, Thana L, Farquharson L, Palmer L, Hancock E, Bassett P, et al. Parry GD. Patient experience of negative effects of psychological treatment: results of a national surveydagger. British Journal of Psychiatry. 2016;208:260–265. doi: 10.1192/bjp.bp.114.162628. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Way BM, Eisenberg NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosomatic medicine. 2007;69:560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Wiens S, Rotshtein P, Öhman A, Dolan RJ. Neural systems supporting interoceptive awareness. Nature Neuroscience. 2004;7(2):189–195. doi: 10.1038/nn1176. [DOI] [PubMed] [Google Scholar]
- Coyne J. Amazingly spun mindfulness trial in British Journal of Psychiatry: How to publish a null trial. 2015a Mar 30; [Web log post]. Retrieved from http://blogs.plos.org/mindthebrain/2015/03/30/amazingly-spun-mindfulness-trial-in-british-journal-of-psychiatry-how-to-publish-a-null-trial/
- Coyne J. Is mindfulness-based therapy ready for rollout to prevent relapse and recurrence in depression? [Web log post] 2015b May 20; Retrieved from http://blogs.plos.org/mindthebrain/2015/05/20/is-mindfulness-based-therapy-ready-for-rollout-to-prevent-relapse-and-recurrence-in-depression/
- Coyne J. Unintended consequences of universal mindfulness training for schoolchildren? 2016 Nov 16; [Web log post] Retrieved from http://blogs.plos.org/mindthebrain/2016/11/16/unintended-consequences-of-universal-mindfulness-training-for-schoolchildren/
- Cullen M. Mindfulness-Based Interventions: An Emerging Phenomenon. Mindfulness. 2011;2(3):186–193. http://doi.org/10.1007/s12671-011-0058-1. [Google Scholar]
- Cumming G. The new statistics: Why and how. Psychological Science. 2014;25:7–29. doi: 10.1177/0956797613504966. [DOI] [PubMed] [Google Scholar]
- Dane E. Paying Attention to Mindfulness and Its Effects on Task Performance in the Workplace. Journal of Management. 2011;37:997–1018. [Google Scholar]
- Davidson RJ. Empirical explorations of mindfulness: Conceptual and methodological conundrums. Emotion. 2010;10(1):8–11. doi: 10.1037/a0018480. http://doi.org/10.1037/a0018480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist. 2015;70(7):581–592. doi: 10.1037/a0039512. http://doi.org/10.1037/a0039512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, Lutz A. Buddha's brain: Neuroplasticity and meditation. IEEE Signal Processing Magazine. 2008;25:174–176. doi: 10.1109/msp.2008.4431873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JH, Vago DR. Can enlightenment be traced to specific neural correlates, cognition, or behavior? No, and (a qualified) Yes. Frontiers in Psychology. 2013;4:870. doi: 10.3389/fpsyg.2013.00870. http://doi.org/10.3389/fpsyg.2013.00870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desbordes G, Gard T, Hoge E, Hölzel B, Kerr C, Lazar S, Olendzski A, Vago DR. Moving beyond mindfulness: Defining equanimity as an outcome measure in meditation research. Mindfulness. 2014;6:356–272. doi: 10.1007/s12671-013-0269-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disayavanish C, Disayavanish P. Meditation-induced psychosis (in Thai) Journal of the Psychiatric Association of Thailand. 1984;29:1–12. [Google Scholar]
- Dimidjian S, Beck A, Felder JN, Boggs JM, Gallop R, Segal ZV. Web-based Mindfulness-based Cognitive Therapy for reducing residual depressive symptoms: An open trial and quasi-experimental comparison to propensity score matched controls. Behaviour Research and Therapy. 2014;63:83–89. doi: 10.1016/j.brat.2014.09.004. http://doi.org/10.1016/j.brat.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD. How would we know if psychotherapy were harmful? American Psychologist. 2010;65(1):21–33. doi: 10.1037/a0017299. http://doi.org/10.1037/a0017299. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Segal SV. Prospects for a clinical science of mindfulness-based intervention. American Psychologist. 2015;70(7):593–620. doi: 10.1037/a0039589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobkin PL, Irving JA, Amar S. For whom may participation in a Mindfulness-Based Stress Reduction Program be Contraindicated? Mindfulness. 2011;3(1):44–50. http://doi.org/10.1007/s12671-011-0079-9. [Google Scholar]
- Dor-Ziderman Y, Berkovich-Ohana A, Glicksohn J, Goldstein A. Mindfulness-induced selflessness: a MEG neurophenomenological study. Frontiers in Human Neuroscience. 2013;7:582. doi: 10.3389/fnhum.2013.00582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draganski B, May A. Training-induced structural changes in the adult human brain. Behavioural Brain Research. 2008;192(1):137–142. doi: 10.1016/j.bbr.2008.02.015. [DOI] [PubMed] [Google Scholar]
- Dreyfus G. Is mindfulness present-centered and non-judgmental? A discussion of the cognitive dimensions of mindfulness. Contemporary Buddhism. 2011;12:41–54. [Google Scholar]
- Dunne J. Toward an understanding of non-dual mindfulness. Contemporary Buddhism. 2011;12:71–88. [Google Scholar]
- Edinger J, Jacobsen R. The incidence and significance of relaxation treatment side effects. The Behavior Therapist. 1982;5:137–138. [Google Scholar]
- Edwards AL. The social desirability variable in personality assessment and research. VIII. Ft Worth, TX, US: Dryden Press; 1957. [Google Scholar]
- Eisendrath SJ, Delucchi K, Bitner R, Fenimore P, Smit M, McLane M. Mindfulness-Based Cognitive Therapy for treatment-resistant depression: A pilot study. Psychotherapy and Psychosomatics. 2008;77(5):319–320. doi: 10.1159/000142525. http://doi.org/10.1159/000142525. [DOI] [PubMed] [Google Scholar]
- Embretson S. Construct validity: Construct representation versus nomothetic span. Psychological Bulletin. 1983;93:179–197. [Google Scholar]
- Epstein M, Lieff J. Psychiatric complications of meditation practice. The Journal of Transpersonal Psychology. 1981;13:137–147. [Google Scholar]
- Fanelli D. “Positive” results increase down the hierarchy of the sciences. PLoS ONE. 2010;5(4):e10068. doi: 10.1371/journal.pone.0010068. http://doi.org/10.1371/journal.pone.0010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farah MJ. Neuroethics: The practical and the philosophical. Trends in Cognitive Sciences. 2005;9:34–40. doi: 10.1016/j.tics.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Farb N. From retreat center to clinic to boardroom? Perils and promises of the modern mindfulness movement. Religions. 2014;5(4):1062–1086. [Google Scholar]
- Farias M, Wikholm C. The Buddha Pill: Can meditation change you? Watkins Publishing 2015 [Google Scholar]
- Fenwick P. Can we still recommend meditation? British Medical Journal. 1983;287:1401. doi: 10.1136/bmj.287.6403.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrarelli F, Smith R, Dentico D, Riedner BA, Zenning C, Benca R, Lutz A, Davidson RJ, Tononi G. Experienced mindfulness meditators exhibit higher parietal-occipital EEG gamma activity during NREM sleep. PLoS ONE. 2013;8:e73417. doi: 10.1371/journal.pone.0073417. http://doi.org/10.1371/journal.pone.0073417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firestone L. Benefits of Mindfulness. 2013 Retrieved January 5, 2016, from http://www.psychologytoday.com/blog/compassion-matters/201303/benefits-mindfulness.
- Fox KCR, Dixon ML, Nijeboer S, Floman JL, Girn M, Lifshitz M, Ellamil M, Sedlmeier P, Christoff K. Functional neuroanatomy of meditation: A systematic review and meta-analysis of 78 functional neuroimaging investigations. Neuroscience & Biobehavioral Reviews. 2016;65:208–228. doi: 10.1016/j.neubiorev.2016.03.021. [DOI] [PubMed] [Google Scholar]
- Fox KCR, Nijeboer S, Dixon ML, Floman JL, Ellamil M, Rumak SP, et al. Christoff K. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neuroscience & Biobehavioral Reviews. 2014;43:48–73. doi: 10.1016/j.neubiorev.2014.03.016. http://doi.org/10.1016/j.neubiorev.2014.03.016. [DOI] [PubMed] [Google Scholar]
- Fox KCR, Zakarauskas P, Dixon M, Ellamil M, Thompson E, Christoff K. Meditation Experience Predicts Introspective Accuracy. PLoS ONE. 2012;7(9):e45370. doi: 10.1371/journal.pone.0045370. http://doi.org/10.1371/journal.pone.0045370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman DH. Lies, damned lies, and medical science. The Atlantic. 2010 Nov;306:76–84. [Google Scholar]
- Freeman D, Freeman J. New study shows mindfulness therapy can be as effective as antidepressants. The Guardian. 2015 Apr; Retrieved from: https://www.theguardian.com/science/blog/2015/apr/21/could-mindfulness-therapy-be-an-alternative-to-antidepressants.
- Frewen PA, Evans EM, Maraj N, Dozois DJA, Partridge K. Letting go: Mindfulness and negative automatic thinking. Cognitive Therapy and Research. 2007;32(6):758–774. http://doi.org/10.1007/s10608-007-9142-1. [Google Scholar]
- Frewen P, Lundberg E, MacKinley J, Wrath A. Assessment of response to mindfulness meditation: Meditation breath attention scores in association with subjective measures of state and trait mindfulness and difficulty letting go of depressive cognition. Mindfulness. 2011;2(4):254–269. http://doi.org/10.1007/s12671-011-0069-y. [Google Scholar]
- Friston K. Ten ironic rules for non-statistical reviewers. Neuroimage. 2012;61:1300–1310. doi: 10.1016/j.neuroimage.2012.04.018. [DOI] [PubMed] [Google Scholar]
- Gangadhar B, Kalyani B, Venkatasubramanian G, Arasappa R, Rao N, Kalmady S, et al. Vasudev M. Neurohemodynamic correlates of ′OM′ chanting: A pilot functional magnetic resonance imaging study. International Journal of Yoga. 2011;4(1):3. doi: 10.4103/0973-6131.78171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin PR, Fredrickson BL. Mindfulness broadens awareness and builds eudaimonic meaning: A process model of mindful positive emotion regulation. Psychological Inquiry. 2015;26:293–314. doi: 10.1080/1047840X.2015.1064294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland E, Gaylord S. Envisioning a future contemplative science of mindfulness: Fruitful methods and new content for the next wave of research. Complementary Health Practice Review. 2009;14(1):3–9. doi: 10.1177/1533210109333718. http://doi.org/10.1177/1533210109333718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzaniga MS. The ethical brain. The Dana Press; 2005. [Google Scholar]
- Gazzaniga MS, Mangun GR. The Cognitive Neurosciences. Fifth. MIT Press; 2014. [Google Scholar]
- Geschwind N, Peeters F, Huibers M, van Os J, Wichers M. Efficacy of mindfulness-based cognitive therapy in relation to prior history of depression: randomised controlled trial. The British Journal of Psychiatry. 2012;201(4):320–325. doi: 10.1192/bjp.bp.111.104851. http://doi.org/10.1192/bjp.bp.111.104851. [DOI] [PubMed] [Google Scholar]
- Gethin R. On some definitions of mindfulness. Contemporary Buddhism. 2011;12:263–279. [Google Scholar]
- Gibbs N, editor. Time. 2016. Sep, Mindfulness: The new science of health and happiness. [Google Scholar]
- Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2006;13(6):353–379. http://doi.org/10.1002/cpp.507. [Google Scholar]
- Giluk TL. Mindfulness, Big Five personality, and affect: A meta-analysis. Personality and Individual Differences. 2009;47:805–811. [Google Scholar]
- Goldberg SB, Wielgosz J, Dahl C, Shuyler B, MacCoon DS, Rosenkranz M, et al. Davidson RJ. Does the Five Facet Mindfulness Questionnaire measure what we think it does? Construct validity evidence from an active controlled randomized clinical trial. Psychological Assessment. 2015;28(8):1009–1014. doi: 10.1037/pas0000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10:83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2016;84:427–437. doi: 10.1037/ccp0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goleman D. The meditative mind: The varieties of meditative experience. New York: Tarcher; 1988. [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Shihab HM. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabovac A, Lau M, Willett B. Mechanisms of mindfulness: A Buddhist psychological model. Mindfulness. 2011;2:154–166. http://doi.org/10.1007/s12671-011-0054-5. [Google Scholar]
- Greenberg MT, Harris AR. Nurturing mindfulness in children and youth: Current state of research. Child Development Perspectives. 2012;6(2):161–166. [Google Scholar]
- Greene DJ, Black KJ, Schlaggar BL. Considerations for MRI study design and implementation in pediatric and clinical populations. Developmental Cognitive Neuroscience. 2016;18:101–112. doi: 10.1016/j.dcn.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grepmair L, Mitterlehner F, Loew T, Bachler E, Rother W, Nickel M. Promoting mindfulness in psychotherapists in training influences the treatment results of their patients: a randomized, double-blind, controlled study. Psychotherapy and Psychosomatics. 2007;76(6):332–338. doi: 10.1159/000107560. http://doi.org/10.1159/000107560. [DOI] [PubMed] [Google Scholar]
- Grossman P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology's (re)invention of mindfulness: Comment on Brown et al. (2011) Psychological Assessment. 2011;23(4):1034–1040. doi: 10.1037/a0022713. http://doi.org/10.1037/a0022713. [DOI] [PubMed] [Google Scholar]
- Grossman P, Van Dam NT. Mindfulness, by any other name…: trials and tribulations of sati in western psychology and science. Contemporary Buddhism. 2011;12(1):219–239. http://doi.org/10.1080/14639947.2011.564841. [Google Scholar]
- Gu J, Strauss C, Crane C, Barnhofer T, Karl A, Cavanaugh K, Kuyken W. Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychological Assessment. 2016;28:791–802. doi: 10.1037/pas0000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunaratana H. Mindfulness in Plain English. Boston: Wisdom; 2002. [Google Scholar]
- Gunderson G. The science is in, and meditation may be the next big business opportunity. Forbes. 2016 Jun 28; Retrieved from http://www.forbes.com/sites/garrettgunderson/2016/06/28/the-science-is-in-and-meditation-may-be-the-next-big-business-opportunity/#2f729c7123c0.
- Haberman C. A discredited vaccine study's continuing impact on public health. The New York Times. 2015 Feb 1; Retrieved from http://www.nytimes.com/2015/02/02/us/a-discredited-vaccine-studys-continuing-impact-on-public-health.html.
- Hanley A, Abell N, Osborn D, Roehrig A, Canto A. Mind the Gaps: Are Conclusions About Mindfulness Entirely Conclusive? Journal of Counseling & Development. 2016;94:103–113. [Google Scholar]
- Hanson R. Hardwiring happiness: The new brain science of contentment, calm, and confidence. New York: Harmony Books; 2013. [Google Scholar]
- Hasenkamp W, Barsalou LW. Effects of meditation experience on functional connectivity of distributed brain networks. Frontiers in Human Neuroscience. 2012 doi: 10.3389/fnhum.2012.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasenkamp W, Wilson-Mendenhall CD, Duncan E, Barsalou LW. Mind wandering and attention during focused meditation: A fine-grained temporal analysis of fluctuating cognitive states. NeuroImage. 2012;59(1):750–760. doi: 10.1016/j.neuroimage.2011.07.008. http://doi.org/10.1016/j.neuroimage.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY, US: Guilford Press; 1999. [Google Scholar]
- Heide F, Borkovec T. Relaxation-induced anxiety: paradoxical anxiety enhancement due to relaxation treatment. Journal of Consulting and Clinical Psychology. 1983;51:171–182. doi: 10.1037//0022-006x.51.2.171. [DOI] [PubMed] [Google Scholar]
- Hill AB. The Environment and Disease: Association or Causation? Proceedings of the Royal Society of Medicine. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- Holmes DS, Solomon S, Cappo BM, Greenberg JL. Effects of Transcendental Meditation versus resting on physiological and subjective arousal. Journal of Personality and Social Psychology. 1983;44(6):1245. doi: 10.1037//0022-3514.44.6.1245. [DOI] [PubMed] [Google Scholar]
- Hölzel B, Lazar S, Gard T, Schuman-Olivier Z, Vago D, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Horton R. The lessons of MMR. The Lancet. 2004;363(9411):747–749. doi: 10.1016/S0140-6736(04)15714-0. http://doi.org/10.1016/S0140-6736(04)15714-0. [DOI] [PubMed] [Google Scholar]
- Huffington A. Mindfulness, meditation, wellness and their connection to corporate America's bottom line. 2013 Mar 16; Retrieved December 23, 2015, from http://www.huffingtonpost.com/arianna-huffington/corporate-wellness_b_2903222.html.
- Hupé J. Statistical inferences under the Null hypothesis: Common mistakes and pitfalls in neuroimaging studies. Frontiers in Neuroscience. 2015;9:18. doi: 10.3389/fnins.2015.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde KL, Lerch J, Norton A, Forgeard M, Winner E, Evans AC, Schlaug G. Musical training shapes structural brain development. The Journal of Neuroscience. 2009;29(10):3019–3025. doi: 10.1523/JNEUROSCI.5118-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis JP. Why most published research findings are false. PLoS Medicine. 2005;2(8):e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis JP. Why science is not necessarily self-correcting. Perspectives on Psychological Perspectives on Psychological Science. 2012;7(6):645–654. doi: 10.1177/1745691612464056. [DOI] [PubMed] [Google Scholar]
- Jain S, Shapiro SL, Swanick S, Roesch SC, Mills PJ, Bell I, Schwartz GER. A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- Jensen CG, Vangkilde S, Frokjaer V, Hasselbalch SG. Mindfulness training affects attention--or is it attentional effort? Journal of Experimental Psychology General. 2012;141(1):106–123. doi: 10.1037/a0024931. http://doi.org/10.1037/a0024931. [DOI] [PubMed] [Google Scholar]
- Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cognitive, Affective & Behavioral Neuroscience. 2007;7(2):109–119. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- Johnson G. New truths that only one can see. The New York Times. 2014a Jan 21;:D1. [Google Scholar]
- Johnson G. When studies are wrong: A coda. The New York Times. 2014b Mar 7; Retrieved Decemeber 23, 2015, from http://www.nytimes.com/2014/03/07/science/when-studies-are-wrong-a-coda.html.
- Jonsson U, Alaie I, Parling T, Arnberg FK. Reporting of harms in randomized controlled trials of psychological interventions for mental and behavioral disorders: A review of current practice. Contemporary Clinical Trials. 2014;38(1):1–8. doi: 10.1016/j.cct.2014.02.005. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: The program of the Stress Reduction Clinic at the University of Massachusetts Medical Center. Dell Publishing; 1990. [Google Scholar]
- Kabat-Zinn J. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemporary Buddhism. 2011;12(1):281–306. [Google Scholar]
- Kabat-Zinn J, Davidson RJ. The mind's own physician: A scientific dialogue with the Dalai Lama on the healing power of meditation. Oakland, CA: New Harbinger; 2011. [Google Scholar]
- Kerr CE, Josyula K, Littenberg R. Developing an observing attitude: an analysis of meditation diaries in an MBSR clinical trial. Clinical Psychology & Psychotherapy. 2011;18(1):80–93. doi: 10.1002/cpp.700. http://doi.org/10.1002/cpp.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketay S, Hamilton HK, Haas BW, Simeon D. Face processing in depersonalization: an fMRI study of the unfamiliar self. Psychiatry Research. 2014;222:107–110. doi: 10.1016/j.pscychresns.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield J. Intensive insight meditation: A phenomenological study. The Journal of Transpersonal Psychology. 1979;11:41–58. [Google Scholar]
- Kozasa EH, Sato JR, Lacerda SS, Barreiros MAM, Radvany J, Russell TA, et al. Amaro E., Jr Meditation training increases brain efficiency in an attention task. NeuroImage. 2012;59(1):745–749. doi: 10.1016/j.neuroimage.2011.06.088. http://doi.org/10.1016/j.neuroimage.2011.06.088. [DOI] [PubMed] [Google Scholar]
- Kragel PA, LaBar KS. Advancing emotion theory with multivariate pattern classficaiton. Emotion Review. 2014;6:160–174. doi: 10.1177/1754073913512519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn TS. Scientific revolutions as changes of world view. In: Harding SG, editor. Can Theories be Refuted? Springer; Netherlands: 1976. pp. 133–154. [Google Scholar]
- Kuijpers HJ, van der Heijden FMMA, Tuinier S, Verhoeven WMA. Meditation-induced psychosis. Psychopathology. 2007;40(6):461–464. doi: 10.1159/000108125. http://doi.org/10.1159/000108125. [DOI] [PubMed] [Google Scholar]
- Kutz I, Leserman J, Dorrington C, Morrison CH, Borysenko JZ, Benson H. Meditation as an adjunct to psychotherapy. An outcome study. Psychotherapy & Psychosomatics. 1985;43:209–218. doi: 10.1159/000287881. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Crane R, Dalgleish T. Does mindfulness based cognitive therapy prevent relapse of depression? BMJ. 2012;345:e7194. doi: 10.1136/bmj.e7194. http://doi.org/10.1136/bmj.e7194. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Crane W, Williams JM. Mindfulness-Based Cognitive Therapy (MBCT) Implementation Resources. Oxford University, University of Exeter, Bangor University 2012 [Google Scholar]
- Kuyken W, Hayes R, Barrett B, Byng R, Dagleish T, Kessler D, et al. Byford S. Effectiveness and cost-effectivness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet. 2015;386:63–73. doi: 10.1016/S0140-6736(14)62222-4. [DOI] [PubMed] [Google Scholar]
- Langer EJ. Mindfulness. Perseus Books; 1989. [Google Scholar]
- Lao SA, Kissane D, Meadows G. Cognitive effects of MBSR/MBCT: A systematic review of neuropsychological outcomes. Consciousness & Cognition. 2016;45:109–123. doi: 10.1016/j.concog.2016.08.017. [DOI] [PubMed] [Google Scholar]
- Lazar SW, Bush G, Gollub RL, Fricchione GL, Khalsa G, Benson H. Functional brain mapping of the relaxation response and meditation. Neuroreport. 2000;111581(7) [PubMed] [Google Scholar]
- Lehrer J. The truth wears off. The New Yorker. 2010 Dec 13;13:52. [Google Scholar]
- Leigh J, Bowen S, Marlatt GA. Spirituality, mindfulness, and substance abuse. Addictive Behaviors. 2005;30:1335–1341. doi: 10.1016/j.addbeh.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Levinson DB, Stoll EL, Kindy SD, Merry HL, Davidson RJ. A mind you can count on: validating breath counting as a behavioral measure of mindfulness. Frontiers in Psychology. 2014;5 doi: 10.3389/fpsyg.2014.01202. http://doi.org/10.3389/fpsyg.2014.01202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilienfeld SO. Psychological Treatments That Cause Harm. Perspectives on Psychological Science. 2007;2(1):53–70. doi: 10.1111/j.1745-6916.2007.00029.x. http://doi.org/10.1111/j.1745-6916.2007.00029.x. [DOI] [PubMed] [Google Scholar]
- Lilienfled SO, Lynn SJ, Lohr JM. Science and pseudoscience in clincal psychology. New York: Guilford Press; 2003. [Google Scholar]
- Lim D, Condon P, Desteno D. Mindfulness and Compassion: An Examination of Mechanism and Scalability. PLoS ONE. 2015;10(2) doi: 10.1371/journal.pone.0118221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl JR, Kaplan C, Winget E, Britton WB. A Phenomenology of Meditation-Induced Light Experiences: Traditional Buddhist and Neurobiological Perspectives. Frontiers in Psychology. 2014;4:1–16. doi: 10.3389/fpsyg.2013.00973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden M. How to define, find and classify side effects in psychotherapy: from unwanted events to adverse treatment reactions. Clinical Psychology & Psychotherapy. 2013;20:286–296. doi: 10.1002/cpp.1765. [DOI] [PubMed] [Google Scholar]
- Linden W. Autogenic Training: A Clinical Guide. New York: Guilford; 1990. [Google Scholar]
- Linehan M. Cognitive behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Lomas T, Cartwright T, Edginton T, Ridge D. A qualitative analysis of experiential challenges associated with meditation practice. Mindfulness. 2014:1–13. http://doi.org/10.1007/s12671-014-0329-8.
- Luders E, Cherbuin N, Kurth F. Forever young(er): Potential age-defying effects of long-term meditation on gray matter atrophy. Frontiers in Psychology. 2015;5:1441. doi: 10.3389/fpsyg.2014.01551. http://doi.org/10.3389/fpsyg.2014.01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luders E, Thompson PM, Kurth F, Hong J, Phillips OR, Wang Y, et al. Toga AW. Global and regional alterations of hippocampal anatomy in long-term meditation practitioners. Human Brain Mapping. 2012;34(12):3369–3375. doi: 10.1002/hbm.22153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luders E, Kurth F, Toga AW, Narr KL, Gaser C. Meditation effects within the hippocampal complex revealed by voxel-based morphometry and cytoarchitectonic probabilistic mapping. Frontiers in Psychology. 2013;4:398. doi: 10.3389/fpsyg.2013.00398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukoff D, Lu FG, Turner R. Cultural considerations in the assessment and treatment of religious and spiritual problems. Psychiatric Clinics of North America. 1995;18:467–485. [PubMed] [Google Scholar]
- Lustyk M, Chawla N, Nolan R, Marlatt G. Mindfulness meditation in research: A discussion of safety issues and participant screening procedures. Advances in Mind-Body Medicine. 2009;24:20–30. [PubMed] [Google Scholar]
- Lutz A, Dunne JD, Davidson RJ. Meditation and the neuroscience of consciousness: An introduction. In: Zelazo PD, Moscovitch M, Thompson E, editors. The Cambridge handbook of consciousness. New York, NY, US: Cambridge University Press; 2007. pp. 499–551. [Google Scholar]
- Lutz A, Greischar LL, Perlman DM, Davidson RJ. BOLD signal in insula is differentially related to cardiac function during compassion meditation in experts vs. novices. Neuroimage. 2009;47(3):1038–1046. doi: 10.1016/j.neuroimage.2009.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Jha AP, Dunne JD, Saron CD. Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. American Psychologist. 2015;70(7):632–658. doi: 10.1037/a0039585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Lachaux JP, Martinerie J, Varela FJ. Guiding the study of brain dynamics by using first-person data: synchrony patterns correlate with ongoing conscious states during a simple visual task. Proceedings of the National Academy of Sciences. 2002;99(3):1586–1591. doi: 10.1073/pnas.032658199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends in Cognitive Sciences. 2008;12(4):163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Thompson E. Neurophenomenology integrating subjective experience and brain dynamics in the neuroscience of consciousness. Journal of Consciousness Studies. 2003;10:31–52. [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Wang HY, Sullivan JC, et al. Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour Research and Therapy. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey AP, Miller Singley AT, Bunge SA. Intensive reasoning training alters patterns of brain connectivity at rest. Journal of Neuroscience. 2013;33:4796–4803. doi: 10.1523/JNEUROSCI.4141-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malinowski P. Neural mechanisms of attentional control in mindfulness meditation. Frontiers in Human Neuroscience. 2013;7:8. doi: 10.3389/fnins.2013.00008. http://doi.org/10.3389/fnins.2013.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manicavasgar V, Parker G, Perich T. Mindfulness-based cognitive therapy vs cognitive behaviour therapy as a treatment for non-melancholic depression. Jouranl of Affective Disorders. 2011;130:138–144. doi: 10.1016/j.jad.2010.09.027. [DOI] [PubMed] [Google Scholar]
- Manuel JA, Somohano VC, Bowen S. Mindfulness practice and its relationship to the Five-Facet Mindfulness Questionnaire. Mindfulness. 2016 doi: 10.1007/s12671-016-0605-x. [DOI] [Google Scholar]
- Mantovani A, Simeon D, Urban N, Bulow P, Allart A, Lisanby S. Temporo-parietal junction stimulation in the treatment of depersonalization disorder. Psychiatry Research. 2011;186:138–140. doi: 10.1016/j.psychres.2010.08.022. [DOI] [PubMed] [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438–450. [PubMed] [Google Scholar]
- Mascaro JS, Rilling JK, Negi LT, Raison CL. Pre-existing brain function predicts subsequent practice of mindfulness and compassion meditation. Neuroimage. 2013;69:35–42. doi: 10.1016/j.neuroimage.2012.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matzke D, Nieuwenhuis S, van Rijn H, Slagter HA, van der Molen MW, Wagenmakers EJ. The effect of horizontal eye movements on free recall: a preregistered adversarial collaboration. Journal of Experimental Psychology General. 2015;144(1):e1–15. doi: 10.1037/xge0000038. http://doi.org/10.1037/xge0000038. [DOI] [PubMed] [Google Scholar]
- McCabe DP, Castel AD. Seeing is believing: The effect of brain images on judgments of scientific reasoning. Cognition. 2008;107(1):343–352. doi: 10.1016/j.cognition.2007.07.017. [DOI] [PubMed] [Google Scholar]
- McCown D, Reibel D, Micozzi MS. Teaching Mindfulness: A Practical Guide for Clinicians and Educators. New York: Springer; 2010. [Google Scholar]
- McMahan DL. The Making of Buddhist Modernism. Oxford University Press; 2008. [Google Scholar]
- Meyer DE. Presentation at Mind and Life XVIII: Attention, Memory and the Mind. Dharamsala, India: 2009. Apr, Multi-tasking, meditation, and contemplative practice. [Google Scholar]
- Meyer DE, Kieras DE. Precis to a practical unified theory of cognition and action: Some lessons from EPIC computational models of human multiple-task performance. In: Gopher D, Koriat A, editors. Attention and Performance XVII Cognitive Regulation of Performance: Interaction of Theory and Application. Cambridge, MA: MIT Press; 1999. pp. 17–88. [Google Scholar]
- Miguel E, Camerer C, Casey K, Cohen J, Esterling KM, Gerber A, et al. Van der Laan M. Promoting Transparency in Social Science Research. Science. 2014;343(6166):30–31. doi: 10.1126/science.1245317. http://doi.org/10.1126/science.1245317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J. The unveling of traumatic memories and emotions through mindfulness and concentration meditation: clinical implications and three case reports. Journal of Transpersonal Psychology. 1993;25:169–180. [Google Scholar]
- Moher D, Shulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. The Lancet. 2001;357(9263):1191–1194. [PubMed] [Google Scholar]
- Monteiro LM, Musten RF, Compson J. Traditional and contemporary mindfulness: Finding the middle path in the tangle of concerns. Mindfulness. 2014;6(1):1–13. http://doi.org/10.1007/s12671-014-0301-7. [Google Scholar]
- Moos RH. Iatrogenic effects of psychosocial interventions for substance use disorders: prevalence, predictors, prevention. Addiction. 2005;100:595–604. doi: 10.1111/j.1360-0443.2005.01073.x. [DOI] [PubMed] [Google Scholar]
- Moos RH. Iatrogenic effects of psychosocial interventions: treatment, life context, and personal risk factors. Substance Use & Misuse. 2012;47:1592–1598. doi: 10.3109/10826084.2012.705710. [DOI] [PubMed] [Google Scholar]
- Mrazek MD, Smallwood J, Schooler JW. Mindfulness and mind-wandering: Finding convergence through opposing constructs. Emotion. 2012;12(3):442–448. doi: 10.1037/a0026678. http://doi.org/10.1037/a0026678. [DOI] [PubMed] [Google Scholar]
- Munafò MR, Stothart G, Flint J. Bias in genetic association studies and impact factor. Molecular Psychiatry. 2009;14(2):119–120. doi: 10.1038/mp.2008.77. http://doi.org/10.1038/mp.2008.77. [DOI] [PubMed] [Google Scholar]
- Münte TF, Altenmüller E, Jäncke L. The musician's brain as a model of neuroplasticity. Nature Reviews Neuroscience. 2002;3(6):473–478. doi: 10.1038/nrn843. [DOI] [PubMed] [Google Scholar]
- Nakaya M, Ohmori K. Psychosis induced by spiritual practice and resolution of pre-morbid inner conflicts. German Journal of Psychiatry. 2010;13:161–163. [Google Scholar]
- NCCIH. NCCIH Clinical Research Toolbox: Data Safety Monitoring. National Center for Complementary and Integrative Medicine (NCCIH), National Institutes of Health (NIH) 2016 https://nccih.nih.gov/grants/toolbox#DSM.
- NCCIH. What the Science Says About Safety and Side Effects of Meditation. National Cennter for Complementary and Intrgrative Medicine (NCCIH), National Insitutes of health (NIH) 2016 https://nccih.nih.gov/health/meditation/overview.htm#hed5.
- Nederhof AJ. Methods of coping with social desirability bias: A review. European Journal of Social Psychology. 1985;15(3):263–280. http://doi.org/10.1002/ejsp.2420150303. [Google Scholar]
- Neff KD, Germer CK. A pilot study and randomized controlled trial of the Mindful Self-Compassion Program. Journal of Clinical Psychology. 2013;69(1):28–44. doi: 10.1002/jclp.21923. http://doi.org/10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- Neisser U, Boodoo G, Bouchard TJ, Boykin AW, Brody N, Ceci SJ, et al. Urbina S. Intelligence: Knowns and unknowns. American Psychologist. 1996;51:77–101. [Google Scholar]
- NIA. NIA Adverse Event and Serious Adverse Event Guidelines. National Institutes on Aging, National Insitutes of Health (NIH); 2011. [Google Scholar]
- Nichols TE, Das S, Eickhoff SB, Evans AC, Glatard T, Hanke M, et al. Yeo BTT. Best practices in data analysis and sharing in neuroimaging using MRI. Nature Neuroscience. 2017;20:299–303. doi: 10.1038/nn.4500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIH. Adverse Event and Serious Adverse Event Guidelines OHRP Guidance on Reviewing and Reporting Unanticipated Problems Involving Risks to Subjects or Others and Adverse Events, OHRP Guidance. National Insitutes of Health (NIH): Office for Human Research Protections, U.S. Department of health and Human Servcies; 2016. [Google Scholar]
- Nyham B. To get more out of science, show the rejected research. The New York Times. 2014 Sep 18; Retrieved January 1st, 2015 from http://www.nytimes.com/2014/09/19/upshot/to-get-more-out-of-science-show-the-rejected-research.html.
- OHRP. Guidance on Reviewing and Reporting Unanticipated Problems Involving Risks to Subjects or Others and Adverse Events: Office for Human Research Protections. US Department of Health and Human Services; 2007. [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: Unifying the discipline to improve public health. Clinical Psychological Science. 2014;2(1):22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Open Science Collaboration. An open, large-scale, collaborative effort to estimate the reproducibility of psychological science. Perspectives on Psychological Science. 2012;7(6):657–660. doi: 10.1177/1745691612462588. [DOI] [PubMed] [Google Scholar]
- Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, et al. Lassen TP. Rockville, MD: National Center for Complementary and Alternative Medicine; 2007. Meditation Practices for Health: State of the Researh (Evidence Report/Technology Assessment) Retrieved from http://www.ahrq.gov/downloads/pub/evidence/pdf/meditation/medit.pdf. [PMC free article] [PubMed] [Google Scholar]
- Papies EK, Barsalou LW, Custers R. Mindful attention prevents mindless impulses. Social Psychological and Personality Science. 2012;3(3):291–299. http://doi.org/10.1177/1948550611419031. [Google Scholar]
- Papies EK, Pronk TM, Keesman M, Barsalou LW. The benefits of simply observing: mindful attention modulates the link between motivation and behavior. Journal of Personality and Social Psychology. 2015;108(1):148–170. doi: 10.1037/a0038032. http://doi.org/10.1037/a0038032. [DOI] [PubMed] [Google Scholar]
- Pashler H, Wagenmakers E. Editors' introduction to the special section on replicability in psychological science: A crisis of confidence? Perspectives on Psychological Science. 2012;7(6):528–530. doi: 10.1177/1745691612465253. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Plaud JJ. Paradigms, promises, and the potential of clinical psychology. Journal of Clinical Psychology. 2001;57:1089–1102. doi: 10.1002/jclp.1079. [DOI] [PubMed] [Google Scholar]
- Power JD, Cohen AL, Nelson SM, Wig GS, Barnes KA, Church JA, et al. Petersen SE. Functional network organization of the human brain. Neuron. 2011;72:665–678. doi: 10.1016/j.neuron.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds S. 7 ways meditation supercharges your brain. 2015 Retrieved January 31, 2016 from: https://www.psychologytoday.com/blog/prime-your-graycells/201511/7ways-meditation-supercharges-your-brain.
- Reuter M, Tisdall MD, Qureshi A, Buckner RL, van der Kouwe AJ, Fischl B. Head motion during MRI acquisition reduces gray matter volume and thickness estimates. Neuroimage. 2015;107:107–115. doi: 10.1016/j.neuroimage.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes E. Mindfulness on trial. The Psychologist. 2015 Sep;28(9) Retrieved from https://thepsychologist.bps.org.uk/mindfulness-trial. [Google Scholar]
- Ring C, Brener J, Knapp K, Mailloux J. Effects of heartbeat feedback on beliefs about heart rate and heartbeat counting: a cautionary tale about interoceptive awareness. Biological Psychology. 2015;104:193–198. doi: 10.1016/j.biopsycho.2014.12.010. http://doi.org/10.1016/j.biopsycho.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Rocha T. The Dark Knight of the Soul. The Atlantic 2014 Jun 25; [Google Scholar]
- Rosnow RL. The nature and role of demand characteristics in scientific inquiry. Prevention & Treatment. 2002;5(1) http://doi.org/10.1037/1522-3736.5.1.537c. [Google Scholar]
- Rosnow RL, Rosenthal R. Statistical procedures and the justification of knowledge in psychological science. American Psychologist. 1989;44:1276–1284. [Google Scholar]
- Rustichini A. Neuroeconomics: What have we found, and what should we search for? Current Opinion in Neurobiology. 2009;19:672–677. doi: 10.1016/j.conb.2009.09.012. [DOI] [PubMed] [Google Scholar]
- Sahdra BK, MacLean KA, Ferrer E, Shaver PR, Rosenberg EL, Jacobs TL, et al. Saron CD. Enhanced response inhibition during intensive meditation training predicts improvements in self-reported adaptive socioemotional functioning. Emotion. 2011;11(2):299–312. doi: 10.1037/a0022764. [DOI] [PubMed] [Google Scholar]
- Santorelli S. Mindfulness-based stress reduction (MBSR): standards of practice. Worcester, MA, USA: Center for mindfulness in medicine, health care, and society, University of Massachusetts Medical School; 2014. [Google Scholar]
- Sauer S, Walach H, Schmidt S, Hinterberger T, Lynch S, Bussing A, Kohls N. Asessment of mindfulness: Review on state of the art. Mindfulness. 2013;4:3–17. [Google Scholar]
- Sayadaw M. In: The Progress of Insight: A Modern Pali Treatise on Buddhist Satipatthana Meditation. Nyanaponika Thera., translator. Kandy, Sri Lanka: Buddhist Publication Society; 1965. [Google Scholar]
- Schaufenbuel K. Why Google, Target, and General Mills are investing in mindfulness. Harvard Business Review. 2015 Dec 28; Retrieved from https://hbr.org/2015/12/why-google-target-and-general-mills-are-investing-in-mindfulness.
- Sedlmeier P, Eberth J, Schwarz M, Zimmermann D, Haarig F, Jaeger S, Kunze S. The psychological effects of meditation: A meta-analysis. Psychological Bulletin. 2012;138(6):1139–1171. doi: 10.1037/a0028168. http://doi.org/10.1037/a0028168. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, et al. Levitan RD. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry. 2010;67:1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford; 2002. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. Second. Guilford Press; 2012. [Google Scholar]
- Sethi S. Relationship of meditation and psychosis: case studies. Australian and New Zealand Journal of Psychiatry. 2003;37:382. doi: 10.1046/j.1440-1614.2003.11721.x. [DOI] [PubMed] [Google Scholar]
- Shan H. Culture-bound psychiatric disorders associated with Qigong practice in China. Hong Kong Journal of Psychiatry. 2000;10:12–14. [Google Scholar]
- Shapiro DH., Jr Overview: Clinical and physiological comparison of meditation with other self-control strategies. American Journal of Psychiatry. 1982;139(3):267–274. doi: 10.1176/ajp.139.3.267. [DOI] [PubMed] [Google Scholar]
- Shapiro DH., Jr Adverse effects of meditation: A preliminary investigation of long-term meditators. International Journal of Psychosomatics. 1992;39(1-4):62–67. [PubMed] [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. Journal of Clinical Psychology. 2006;62(3):373–86. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Sharf RH. Is mindfulness Buddhist? (and why it matters) Transcultural Psychiatry. 2014;52:470–484. doi: 10.1177/1363461514557561. [DOI] [PubMed] [Google Scholar]
- Shonin E, Van Gordin W, Griffiths MD. Mindfulness-based interventions: Towards mindful clinical integration. Frontiers in Psychology. 2013;4:194. doi: 10.3389/fpsyg.2013.00194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonin E, Van Gordon W, Griffiths MD. Are there risks associated with using mindfulness in the treatment of psychopathology? Clinical Practice. 2014;11:389–392. [Google Scholar]
- Shonin E, Van Gordon W, Griffiths MD. Cognitive behavioral therapy (CBT) and meditation awareness training (MAT) for the treatment of co-occurring schizophrenia with pathological gambling: a case study. International Journal of Mental Health and Addiction. 2014;12:181–196. [Google Scholar]
- Shonin E, Van Gordon W, Griffiths MD. Do mindfulness-based therapies have a role in the treatment of psychosis? Australian and New Zealand Journal of Psychiatry. 2014;48:124–127. doi: 10.1177/0004867413512688. [DOI] [PubMed] [Google Scholar]
- Shwed U, Bearman PS. The temporal structure of scientific consensus formation. American Sociological Review. 2010;75:817–840. doi: 10.1177/0003122410388488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sierra M, Senior C, Dalton J, McDonough M, Bond A, Phillips ML, et al. David AS. Autonomic response in depersonalization disorder. Archives of General Psychiatry. 2002;59:833–838. doi: 10.1001/archpsyc.59.9.833. [DOI] [PubMed] [Google Scholar]
- Siegling AB, Petrides KV. Measures of trait mindfulness: Convergent validity, shared dimensionality, and linkages to the five-factor model. Frontiers in Psychology. 2015;5:1164. doi: 10.3389/fpsyg.2014.01164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons JP, Nelson LD, Simonsohn U. False-Positive Psychology Undisclosed Flexibility in Data Collection and Analysis Allows Presenting Anything as Significant. Psychological Science. 2011 doi: 10.1177/0956797611417632. 0956797611417632. http://doi.org/10.1177/0956797611417632. [DOI] [PubMed]
- Singh NN, Lancioni GE, Winton ASW, Wahler RG, Singh J, Sage M. Mindful caregiving increases happiness among individuals with profound multiple disabilities. Research in Developmental Disabilities. 2004;25(2):207–218. doi: 10.1016/j.ridd.2003.05.001. http://doi.org/10.1016/j.ridd.2003.05.001. [DOI] [PubMed] [Google Scholar]
- Slagter HA, Lutz A, Greischar LL, Francis AD, Nieuwenhuis S, Davis JM, Davidson RJ. Mental training affects distribution of limited brain resources. PLoS Biology. 2007;5(6):e138. doi: 10.1371/journal.pbio.0050138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperduti M, Martinelli P, Piolino P. A neurocognitive model of meditation based on activation likelihood estimation (ALE) meta-analysis. Consciousness and Cognition. 2012;21(1):269–276. doi: 10.1016/j.concog.2011.09.019. [DOI] [PubMed] [Google Scholar]
- Stanley S. “Things said or done long ago are recalled and remembered”: The ethics of mindfulness in early Buddhism, psychotherapy and clinical psychology. European Journal of Psychotherapy & Counselling. 2013;15(2):151–162. http://doi.org/10.1080/13642537.2013.795338. [Google Scholar]
- Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-Based Interventions for People Diagnosed with a Current Episode of an Anxiety or Depressive Disorder: A Meta-Analysis of Randomised Controlled Trials. PLoS ONE. 2014;9(4):e96110. doi: 10.1371/journal.pone.0096110. http://doi.org/10.1371/journal.pone.0096110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strawn JR, Cotton S, Luberto CM, Patino LR, Stahl LA, Weber WA, et al. DelBello MP. Neural Function Before and After Mindfulness-Based Cognitive Therapy in Anxious Adolescents at Risk for Developing Bipolar Disorder. Journal of Child and Adolescent Psychopharmacology. 2016 doi: 10.1089/cap.2015.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundquist J, Lilja A, Palmer K, Memon AA, Wang X, Johansson LM, Sundquist K. Mindfulness group therapy in primary care patients with depression, anxiety and stress and adjustment disorders: randomised controlled trial. The British Journal of Psychiatry. 2014;114:150243. doi: 10.1192/bjp.bp.114.150243. http://doi.org/bjp.bp.114.150243. [DOI] [PubMed] [Google Scholar]
- Szalavitz M. Explaining why meditators may live longer. TIME. 2010 Dec 23; Retrieved from http://healthland.time.com/2010/12/23/could-meditation-extend-life-intriguing-possibility-raised-by-new-study/
- Sze JA, Gyurak A, Yuan JW, Levenson RW. Coherence between emotional experience and physiology: Does body awareness training have an impact? Emotion. 2010;10(6):803–814. doi: 10.1037/a0020146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nature Reviews Neuroscience. 2015;16(4):213–225. doi: 10.1038/nrn3916. http://doi.org/10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, et al. Posner MI. Short-term meditation training improves attention and self-regulation. Proc Nat Acad Sci USA. 2007;104(43):17152–17156. doi: 10.1073/pnas.0707678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VA, Daneault V, Grant J, Scavone G, Breton E, Roffe-Vidal S, et al. Beauregard M. Impact of meditation training on the default mode network during a restful state. Social Cognitive and Affective Neuroscience. 2013;8(1):4–14. doi: 10.1093/scan/nsr087. http://doi.org/10.1093/scan/nsr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF. Is cognitive-behavioral therapy more effective than other therapies?: A meta-analytic review. Clinical Psychology Review. 2010;30:710–720. doi: 10.1016/j.cpr.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Tomasino B, Fregona S, Skrap M, Fabbro F. Meditation-related activations are modulated by the practice needed to obtain it and by the expertise: An ALE meta-analysis study. Frontiers in Human Neuroscience. 2013;6:346. doi: 10.3389/fnhum.2012.00346. http://doi.org/10.3389/fnhum.2012.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner L, Singh K, Garrity C, Tsertsvadze A, Manheimer E, Wieland L, et al. Moher D. An evaluation of the completeness of safety reporting in reports of complementary and alternative medicine trials. BMC Complementary and Alternative Medicine. 2011;11:67. doi: 10.1186/1472-6882-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RP, Lukoff D, Barnhouse RT, Lu FG. Religious or spiritual problem. A culturally sensitive diagnostic category in the DSM-IV. Journal of Nervous and Mental Disease. 1995;183:435–444. doi: 10.1097/00005053-199507000-00003. [DOI] [PubMed] [Google Scholar]
- Turner R. How much cortex can a vein drain? Downstream dilution of activation-related cerebral blood oxygenation changes. Neuroimage. 2002;16:1062–1067. doi: 10.1006/nimg.2002.1082. [DOI] [PubMed] [Google Scholar]
- Vago DR, Silbersweig DA. Self-awareness, self-regulation, and Self-transcendence (S-ART): A framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in Human Neuroscience. 2012;6:1–30. doi: 10.3389/fnhum.2012.00296. http://doi.org/10.3389/fnhum.2012.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Aalderen JR, Donders ART, Giommi F, Spinhoven P, Barendregt HP, Speckens AEM. The efficacy of mindfulness-based cognitive therapy in recurrent depressed patients with and without a current depressive episode: a randomized controlled trial. Psychological Medicine. 2012;42(05):989–1001. doi: 10.1017/S0033291711002054. http://doi.org/10.1017/S0033291711002054. [DOI] [PubMed] [Google Scholar]
- Van Nuys D. Meditation, attention, and hypnotic susceptibility: A correlation study. International Journal of Clinical & Experimental Hypnosis. 1973;21:59–69. [Google Scholar]
- VanderKooi L. Buddhist teachers' experience with extreme mental states in Western meditators. Journal of Transpersonal Psychology. 1997;29:31–46. [Google Scholar]
- Van Dam NT, Earleywine M, Borders A. Measuring mindfulness? An Item Response Theory analysis of the Mindful Attention Awareness Scale. Personality and Individual Differences. 2010;49(7):805–810. http://doi.org/10.1016/j.paid.2010.07.020. [Google Scholar]
- Van Dam NT, Earleywine M, Danoff-Burg S. Differential item function across meditators and non-meditators on the Five Facet Mindfulness Questionnaire. Personality and Individual Differences. 2009;47(5):516–521. http://doi.org/10.1016/j.paid.2009.05.005. [Google Scholar]
- Van Dam NT, Hobkirk AL, Danoff-Burg S, Earleywine M. Mind Your Words: Positive and Negative Items Create Method Effects on the Five Facet Mindfulness Questionnaire. Assessment. 2012;19:198–204. doi: 10.1177/1073191112438743. [DOI] [PubMed] [Google Scholar]
- Van Dijk KRA, Sabuncu MR, Buckner RL. The influence of head motion on intrinsic functional connectivity MRI. NeuroImage. 2012;59(1):431–438. doi: 10.1016/j.neuroimage.2011.07.044. http://doi.org/10.1016/j.neuroimage.2011.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Hurk PAM, Giommi F, Gielen SC, Speckens AEM, Barendregt HP. Greater efficiency in attentional processing related to mindfulness meditation. Quarterly Journal of Experimental Psychology. 2010;63(6):1168–1180. doi: 10.1080/17470210903249365. [DOI] [PubMed] [Google Scholar]
- van Vugt MK, Slagter HA. Control over experience? Magnitude of the attentional blink depends on meditative state. Consciousness and Cognition. 2014;23:32–39. doi: 10.1016/j.concog.2013.11.001. http://doi.org/10.1016/j.concog.2013.11.001. [DOI] [PubMed] [Google Scholar]
- van Vugt MK, Taatgen NA, Bastian M, Sackur J. Proceedings of the International Conference in Cognitive Modeling. Groningen; Netherlands: 2015. Modeling mind-wandering: a tool to better understand distraction. [Google Scholar]
- van Waning A. The Less Dust the More Trust: Participating In The Shamatha Project, Meditation And Science. Lanham: Mantra Books; 2014. Reprint edition. [Google Scholar]
- Vaughan B, Goldstein MH, Alikakos M, Cohen LJ, Serby MJ. Frequency of reporting of adverse events in randomized controlled trials of psychotherapy vs. psychopharmacotherapy. Comprehensive Psychiatry. 2014;55:849–855. doi: 10.1016/j.comppsych.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace B. Stilling the Mind: Shamatha Teachings from Dudjom Lingpa's Vajra Essence. Boston: Wisdom Publications; 2011. [Google Scholar]
- Wallace RK. Physiological effects of transcendental meditation. Science. 1970;167(3926):1751–1754. doi: 10.1126/science.167.3926.1751. [DOI] [PubMed] [Google Scholar]
- Wallace RK, Benson H, Wilson AF. A wakeful hypometabolic physiologic state. American Journal of Physiology. 1971;221(3):795–799. doi: 10.1152/ajplegacy.1971.221.3.795. [DOI] [PubMed] [Google Scholar]
- Walsh R. What is wisdom? Cross-cultural and cross-disciplinary syntheses. Review of General Psychology. 2015;19:278–293. [Google Scholar]
- Walsh R, Roche L. Precipitation of acute psychotic episodes by intensive meditation in individuals with a history of schizophrenia. American Journal of Psychiatry. 1979;136:1085–1086. doi: 10.1176/ajp.136.8.1085. [DOI] [PubMed] [Google Scholar]
- Walton A. For Depression Treatment, Meditation Might Rival Medication. Forbes. 2014 Jan;7:1–3. [Google Scholar]
- Weisberg DS, Keil FC, Goodstein J, Rawson E, Gray JR. The Seductive Allure of Neuroscience Explanations. Journal of Cognitive Neuroscience. 2008;20(3):470–477. doi: 10.1162/jocn.2008.20040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. World Health Organization (WHO), Uppsala Monitoring Centre; 2016. The use of the WHO-UMC system for standardized case causaility assessment. http://who-umc.org. [Google Scholar]
- Whitmarsh S, Barendregt H, Schoffelen JM, Jensen O. Metacognitive awareness of covert somatosensory attention corresponds to contralateral alpha power. NeuroImage. 2014;85:803–809. doi: 10.1016/j.neuroimage.2013.07.031. http://doi.org/10.1016/j.neuroimage.2013.07.031. [DOI] [PubMed] [Google Scholar]
- Williams JM, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, et al. Russell IT. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. J Consult Clin Psychol. 2014;82:275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams R. Will Mindfulness Become Another Self-Help Fad? 2014 Oct 11; Retrieved March 29, 2015, from http://www.psychologytoday.com/blog/wired-success/201410/will-mindfulness-become-another-self-help-fad.
- Wilson TD, Reinhard DA, Westgate EC, Gilbert DT, Ellerbeck N, et al. Shaked A. Just think: The challenges of the disengaged mind. Science. 2014;345(6192):75–77. doi: 10.1126/science.1250830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarkoni T, Poldrack RA, Van Essen DC, Wager TD. Cognitive neuroscience 2.0: building a cumulative science of human brain function. Trends in Cognitive Sciences. 2010;14(11):489–496. doi: 10.1016/j.tics.2010.08.004. http://doi.org/10.1016/j.tics.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yorston G. Mania precipitated by meditation: a case report and literature review. Mental Health, Religion & Culture. 2001;4:209–214. [Google Scholar]
- Zanesco AP, King BG, MacLean KA, Saron CD. Executive control and felt concentrative engagement following intensive meditation training. Frontiers in Human Neuroscience. 2013;7 doi: 10.3389/fnhum.2013.00566. http://doi.org/10.3389/fnhum.2013.00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, Coghill RC. Mindfulness Meditation-Based Pain Relief Employs Different Neural Mechanisms Than Placebo and Sham Mindfulness Meditation-Induced Analgesia. Journal of Neuroscience. 2015;35(46):15307–15325. doi: 10.1523/JNEUROSCI.2542-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Martucci KT, Kraft RA, Gordon NS, Mchaffie JG, Coghill RC. Brain mechanisms supporting the modulation of pain by mindfulness meditation. Journal of Neuroscience. 2011;31(14):5540–5548. doi: 10.1523/JNEUROSCI.5791-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]


