Abstract
Currently there are few evidence-based programs available for families of individuals with ASD during the transition to adulthood. The present study provided a preliminary evaluation of a multi-family group psychoeducation intervention using a randomized waitlist control design (n=41). Families in the intervention condition participated in Transitioning Together, an 8-week program designed to reduce family distress and improve social functioning for adolescents. Findings indicated significant improvements in parental depressive symptoms and problem solving from pre- to post-intervention for parents in the intervention condition but not for parents in the control condition. Social interactions also improved for youth in the intervention condition relative to controls. Parents reported satisfaction with the program and particularly valued the opportunity to interact with other families.
Keywords: autism spectrum disorder, adolescence, multi-family group psychoeducation, transition
Autism spectrum disorders (ASDs) affect an estimated 1 in 68 children in the US (Christensen et al., 2016), and can result in high levels of stress for all members in the family (Bishop-Fitzpatrick et al., 2015; Hayes & Watson, 2013; Orsmond & Seltzer, 2009). The adolescent years are particularly stressful, as families anticipate a loss of services following high school graduation (Lounds et al., 2007). This high level of parental worry is not surprising as outcomes are often poor during adulthood, with low rates of employment and independence (Henninger & Taylor, 2012; Howlin et al., 2004; Howlin & Moss, 2012), increased vulnerability for autism symptoms and behavior problems (Taylor & Seltzer, 2010) and loss of insurance and other services (Shattuck et al., 2012; Shattuck et al., 2011). Given the rapid increase of autism diagnoses since the 1990s (Gurney et al., 2003), there are high numbers of individuals with ASD graduating from high school and entering the adult world, creating an urgent need for interventions to support families during this critical period of transition. The present study aimed to address this gap in transition-focused services by evaluating a new intervention, Transitioning Together, a multi-family group psychoeducation program for adolescents with ASD and their families.
The high level of stress experienced by parents of children with ASD is well-documented (Abbeduto et al., 2004; Blacher & McIntyre, 2006; Eisenhower et al., 2005; Montes & Halterman, 2006, Smith et al., 2010); this stress is evident across the life course, with significant repercussions for parental health and well-being (Barker, Seltzer, & 2013). For example, parents of individuals with ASD have higher rates of depression (Weiss, 2002) and higher levels of negative mood compared to parents of children without disabilities (Smith et al., 2012). Further, there is an increase in maternal burden and a decrease in parent-child relationship quality for families of individuals with ASD following high school exit (Taylor & Seltzer, 2011a), making the adolescent period a time of particular risk for the family system.
The level of stress within the family system is important to consider not only for parental well-being, but also for the individual with ASD. In a review of studies of families of children with ID, Hastings and Lloyd (2007) argued that the challenges associated with caring for an individual with disabilities may create a family context where some level of negative emotional intensity, referred to as expressed emotion (EE), is to be expected. However, the presence of high EE in families may exacerbate or maintain behavior problems, suggesting that more research is needed to understand how to most effectively intervene to support families in maintaining positivity in the face of stress (Hastings & Lloyd, 2007). Consistent with this general literature, past longitudinal work with families of adolescents and adults with ASD has shown that when parents are warm and positive toward their children, the behavior problems and autism symptoms of their children are reduced (Smith et al., 2008; Woodman et al., 2016), whereas high levels of EE are associated with increases in these behaviors and symptoms (Greenberg et al., 2006, Baker et al., 2011). As such, interventions that reduce family distress and support positive parent-child relations have the potential to promote well-being not only for parents, but also for adolescents with ASD.
Although services for young children with disabilities have long considered the parent-child relationship as a critical factor in intervention programming (Singer et al., 2007), family-centered interventions later in the life course are only now emerging (Smith & Anderson, 2014). Of interventions for transition-aged youth with ASD that have included parents, very few have targeted parental well-being and the parent-child relationship. For instance, the Program for the Education and Enrichment of Relational Skills (PEERS) intervention has a strong evidence-base for improving social skills for students with ASD and includes parents as part of the intervention team but the program was not designed with family-wide well-being as an intervention target (Karst et al., 2014; Laugeson et al., 2015). There remains a high need for interventions for individuals with ASD that are designed to support the entire family system during the transition to adulthood.
One promising intervention approach for families of transition-aged youth with ASD, multi-family group psychoeducation, was developed based on research conducted with families of individuals with mental health conditions. Multi-family group psychoeducation has been shown to reduce family stress and improve outcomes in multiple clinical populations (e.g., asthma, cancer, mood disorders, schizophrenia; Chiquelho, Mendes, Relvas, & Sousa, 2011; Dixon et al., 2000; McFarlane et al., 2003; Ng et al., 2008; Young & Fristad, 2007). For example, in a study of family psychoeducation with adolescents with major depression, adolescents in the experimental group displayed more gains in social functioning and greater improvements in parent-child interactions relative to the control group (Sanford et al., 2006). Although the content and components of psychoeducation interventions vary by study and type of clinical condition, these programs all aim to reduce family distress and improve outcomes for all family members by providing (1) education on the clinical condition, (2) guided practice in problem-solving with others who have family members with similar diagnostic conditions, and (3) social support (McFarlane et al., 2002).
To begin to address this gap, as reported in BLINDED. (2012), we developed a curriculum (Transitioning Together) by first conducting a comprehensive review of the literature to create an outline of the curriculum and then holding a series of focus groups with key stakeholders (e.g., parents of adolescents with ASD, service providers) to gather input about the proposed program. Findings from the focus groups suggested that families have needs related to (1) increasing community activities and connections, (2) help with problem-solving, and (3) training in advocacy, reflecting strong alignment of end-user goals with the proposed curriculum developed from the research literature. Focus group participants also noted that family participation would be higher if there were activities for the adolescent with ASD and if practical solutions were being offered (BLINDED 2012). We subsequently refined the intervention curriculum based on the focus group feedback. Next, we completed a small pilot study of 10 families of adolescents with ASD who participated in this new multi-family group psychoeducation intervention; full detail regarding the focus group and pilot study can be found in BLINDED (2012). Although the sample was very small in size, statistically significant positive changes were observed in the parent-child relationship from pre-intervention to post-intervention (p <.05). Specifically, parents were rated by an independent rater as having higher levels of warmth toward their son or daughter following the intervention using the Five Minute Speech Sample (Magaña et al., 1986). Additionally, after the intervention, parents were also more likely to report being happy or proud of the child and had improved understanding of their child’s disability and the service system. Although we did not find significant changes in autism symptoms in this small pilot sample, parents felt more able to predict when their child would have a behavior problem from pre-intervention to post-intervention (BLINDED 2012). These pilot findings suggested that the multi-family group psychoeducation approach has promise for families with ASD, and a more robust and comprehensive evaluation of the intervention is needed. Based on the pilot findings, we developed a fully manualized intervention curriculum for Transitioning Together, focusing specifically on families of adolescents with high functioning ASD.
Present Study
The present randomized waitlist control study examined the effects of Transitioning Together for adolescents with high-functioning ASD and their families. We compared two groups, intervention condition vs waitlist control condition, on key outcomes of interest: parental well-being, parent-child relationship, and adolescent social functioning. Our primary research question was: is there a difference in change from pre to post for families in the intervention compared to families in the waitlist control condition on key outcome measures? We hypothesized that families who received the intervention, which included research-based education on the transition to adulthood for individuals with ASD, training in problem solving, and opportunities for social support, would have greater improvement in parental well-being and the parent-child relationship compared to families in the waitlist control condition. Given past work showing connections between family variables and behavioral outcomes for adolescents with ASD (e.g., Greenberg et al., 2006; Smith et al., 2008), we also hypothesized that families receiving the intervention would have adolescents who made more gains in social interactions than families who were in the waitlist condition. The secondary research questions related to the social validity of the intervention and included: how satisfied were participants with the intervention, what did participants report learning from the intervention, and what did participants report doing differently as a result of the intervention?
Methods
Participants
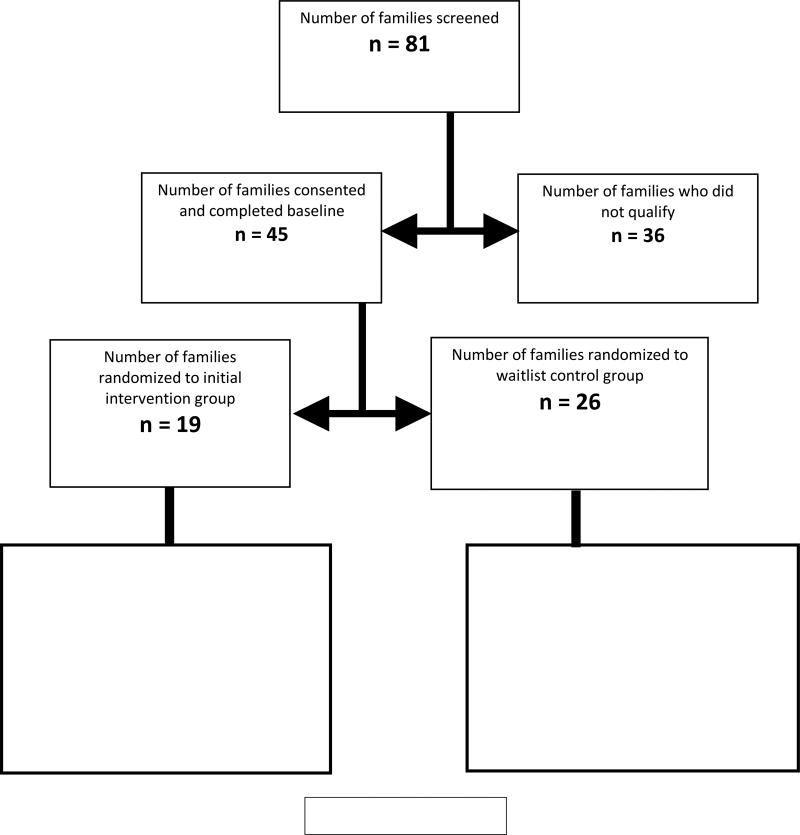
Families of adolescents with ASD (n=45 parent-adolescent dyads) were recruited through local autism groups, clinics, and university research registries. Inclusion criteria for the present study were: (1) the adolescent was 14 to 17 years of age; (2) the adolescent was currently participating in a general education setting for at least 50% of the school day; (3) the adolescent was verbally fluent (defined as able to speak in complex sentences); (4) the adolescent was currently residing with his or her parent or legal guardian; and (5) confirmation of the adolescent’s independent medical or educational diagnosis of autism spectrum disorder using the Social Communication Questionnaire (SCQ; Rutter, Bailey & Lord, 2003). As shown in Figure 1, following baseline data collection (Time 1), parent-adolescent dyads were randomly assigned to the intervention condition (n=19) or waitlist control condition (n=26). Three families (2 intervention, 1 control) exited the study after completing the Time 1 data collection (one due to family relocation out of state, one due to an unexpected change in family schedule, and one due to significant family illness). An additional family (intervention condition) became homeless over the course of the study and was lost to follow-up, resulting in final analytic sample of 41 families (n=16 intervention, n=25 controls).
Figure 1.
Consort Diagram
Although many families involved both mothers and fathers in the intervention, only one parent/guardian was designated as the family respondent for research purposes. During the screening process, the parent contacting the study was asked which parent, if there was more than one parent living in the home with the child, was most interested in participating in data collection as the parent respondent. Of the parent respondents in our final sample, 88% were mothers; the majority (95%) were White and over 75% had completed a bachelor’s degree. The families’ household incomes ranged from $20,000 to over $160,000 dollars per year (pre-tax income in 2011), with a median of $75,000.
The adolescents in our final sample ranged in age from 14 to 17 years (M=15.44; SD=1.03); 78% male and almost 90% were White. The adolescents were first diagnosed with an autism spectrum disorder at a wide range of ages, from before one year of age to 15 years of age (M=7.05, SD=4.40). As reported by their parents, the majority (76%) were taking at least one prescription medication, with 53% having a co-occurring diagnosis of anxiety and 21% having a co-occurring diagnosis of depression.
As presented in Table 1, there were no statically significant differences between the two groups at baseline in terms of parental education, ethnicity, income, or employment status. Also, there were no statistically significant differences between the intervention and control groups in adolescent variables of sex, age, age at diagnosis, number of behavior problems (as measured by the Scales of Independent Behaviors-Revised; Bruininks et al., 1996), or daily living skills (as measured by the Waisman Activities of Daily Living; Maenner et al., 2013). However, adolescent intelligence quotient (IQ), as measured by the Wechsler Abbreviated Scales of Intelligence (WASI; Wechsler, 1999), differed significantly between the groups, despite random assignment. The intervention group had higher IQ scores (M=109.38, SD=14.25) at baseline than the control group (M=94.20, SD=15.90), F=9.61, p=.004. IQ was subsequently controlled in all analyses.
Table 1.
Background Variables at Time 1 for Intervention (n=16) and Control (n=25) Groups
| Intervention | Control | F or Chi Square |
|
|---|---|---|---|
| Parent Variables | |||
| % Female | 94% | 84% | 0.87 |
| % College | 81% | 74% | 0.29 |
| % White | 96% | 94% | 0.10 |
| Average family income | $74,000 | $74,500 | 0.00 |
| % Employed | 75% | 88% | 1.17 |
| Adolescent Variables | |||
| % Male | 81% | 76% | 0.16 |
| Age | M=15.56 (SD=.73) | M=15.36 (SD=1.19) | 0.37 |
| Age at diagnosis | M=8.38 (SD=4.30) | M=6.20 (SD=4.34) | 2.47 |
| Number of behavior problems | M=5.00 (SD=2.66) | M=4.80 (SD=2.02) | 0.08 |
| Daily Living Skills | M=23.25 (SD=5.63) | M=22.43 (SD=5.38) | 0.28 |
| IQ | M=109.38 (SD=14.25) | M=94.20 (SD=15.90) | 9.61, p<.01 |
Procedures
The study was approved by BLINDED’s Institutional Review Board and all participants provided written informed consent before beginning with the study. Data were collected from parents and adolescents at two time points separated by approximately three months: Time 1 (pre-intervention) and Time 2 (post-intervention). For both waves of data collection, parents participated in a standardized interview and completed self-administered questionnaires regarding parental well-being and behaviors and activities of the son or daughter which we have successfully employed in our prior work with families of adolescents and adults with ASD. Adolescents also participated in a structured interview at each time point to answer questions related to friendships and social activities. The interviews and questionnaires were identical at each wave of data collection with three exceptions: (1) the Time 1 parent questionnaire included demographic questions, (2) the adolescent Time 1 assessment included cognitive testing, and (3) the Time 2 interview included exit interview questions related to satisfaction with the intervention for families in the intervention condition. Also, at the conclusion of each weekly session, adolescents and parents completed satisfaction surveys and intervention facilitators rated participant engagement.
Following the completion of the Time 1 data collection, families in the intervention condition participated in the Transitioning Together intervention program (BLINDED, 2012; 2014); families in the waitlist control condition were offered the opportunity to participate in the program after completion of the Time 2 data collection, with 100% participation.
The Transitioning Together intervention involved 2 individual family joining sessions, 8 weekly parent and teen group sessions, and ongoing resources and referrals. Joining sessions lasted approximately one hour; the purpose of the joining sessions was to build rapport and partnership and to clarify family goals for the program through the use of activities such as a family timeline and ecomap. Each family was allowed to include family members of their choosing to attend the joining sessions (e.g., some families invited a sibling or grandparent to attend), although most joining sessions were comprised of participating parents and adolescents. After families completed joining sessions, the weekly group sessions were held in the same time and place for both parents and teens, but in separate rooms. Group sessions lasted approximately 1.5 hours. Parent intervention group sessions involved education on a variety of topics relevant to ASD as well as guided practice in problem-solving (session topics and goals are presented in Table 2). The adolescent social group involved learning activities and games on topics such as sharing interests, goal setting, problem solving, and social planning (see Table 3 for session topics and goals). For both parents and teens, positivity and problem-solving were explicitly modeled and emphasized across all sessions.
Table 2.
Parent Session Topics and Goals
| Session | Goals |
|---|---|
|
| |
| Meet other families | |
| Session 1 Autism in Adulthood | *Learn about developmental course of ASD (Seltzer et al., 2003; Seltzer et al., 2004; Shattuck et al., 2007; Smith et al., 2012) |
|
| |
| Session 2 Employment Planning | *Learn about employment services and strategies (Taylor & Seltzer, 2011b; Taylor & Seltzer, 2013; Taylor, Henninger, & Mailick, 2015; Taylor, Smith, & Mailick, 2014) |
|
| |
| Session 3 College Planning and Problem Solving | *Learn about post-secondary services and planning strategies (Taylor & Seltzer, 2011b; Taylor & Seltzer, 2013; Taylor, Henninger, & Mailick, 2015; Taylor, Smith, & Mailick, 2014) |
| Practice problem-solving method | |
|
| |
| Session 4 Family Topics | *Learn about impact of autism on family and the environment on individuals with ASD (Baker et al., 2011; Baker, Smith, et al., 2011; Smith et al., 2008; Greenberg et al., 2006; Woodman et al., 2016) |
|
| |
| Session 5 Risks to Adult Independence | Learn strategies for behavior management during late adolescence and early adulthood |
| Discuss advocacy strategies when behaviors are misunderstood by community | |
|
| |
| Session 6 Community Involvement | *Finding community activities and social opportunities (Esbensen et al., 2010; Orsmond et al., 2004; Taylor & Seltzer, 2011b) |
| Discuss safety concerns for adults with ASD | |
|
| |
| Session 7 Legal Issues | *Receive information on long-term planning: guardianship, wills, trusts, etc. (Essex et al., 1997; Krauss et al., 2005) |
|
| |
| Session 8 Risks to Health and Wealth-Being | *Learn about risks to parental health and well-being (Abbeduto et al., 2004; Barker et al., 2010; Kring et al., 2008; Seltzer et al., 2010; Smith et al., 2012) |
Table 3.
Adolescent Session Topics and Goals
| Session | Goals |
|---|---|
| Session 1 Introductions | Practice asking questions of others/Establish structure and ground rules |
| Session 2 Goal Setting | Create a goal and outline steps to achieve goal |
| Session 3 Social Problem Solving | Discuss how to use problem solving strategies to address social issues |
| Session 4 Coping Strategies | Determine potential coping strategies for stressful situations |
| Session 5 Flex Week | Session activities determined by needs and interests of group |
| Session 6 Conversation | Practice different types of conversations |
| Session 7 Party Planning | Learns steps for planning a party and prepare to implement next week |
| Session 8 Party/Graduation | Execute party plan and receive graduation certificates |
We note that several steps were taken to ensure treatment fidelity. All intervention staff participated in training to learn about study goals and procedures, to review curriculum components (which were manualized and included fidelity checklists), and to role-play conducting joining sessions and multi-family group sessions. Parent groups were facilitated by one PhD-level psychologist and one graduate student; the adolescent groups were facilitated by a Masters-level psychologist or social worker and one or more graduate students. At the conclusion of each intervention sessions, the supervising psychologist led the other intervention staff in a short debriefing meeting so that staff could share feedback, ask questions, and problem-solve any issues that may have arisen during either the parent group or the adolescent group. Group facilitators also had supervision meetings twice a month to discuss field notes, troubleshoot problems, review resources and referrals for families, and receive constructive feedback. This type of continuous staff training and supervision is an important mechanism for treatment fidelity (Borkowski et al., 2006).
Measures
Parental depressive symptoms were measured using the Center for Epidemiological Studies Depression scale (CES-D; Radloff, 1977), a 20-item, well-validated self-report scale of depressive symptoms. Parents rated the frequency of depressive symptoms in the past week on a 4-point scale ranging from 0 (rarely) to 3 (most of the time). The coefficient alphas wer .91 at Time 1 and .91 at Time 2. General life stress was measured using the Perceived Stress Scale, a 10-item self-report questionnaire that measures a person’s evaluation of the stressfulness of the situations in the past month of their lives (Cohen & Williamson, 1988); higher scores reflect higher levels of stress. The coefficient alphas were .91 at Time 1 and .93 at Time 2. Parental problem solving was measured using problem-solving items from the Family Empowerment Scale (Koren et al., 1992); items were “I know the steps I need to take when I am concerned about my child’s services,” “I know what to do when problems arise with my child,” and “when faced with a problem involving my child, I decide what to do and do it.” The coefficeint alphas were .97 at Time 1 and .70 at Time 2.
Parent-child relationship
Parent-child relationship quality was measured using the Positive Affect Index (PAI; Bengtson and Schrader 1982). For the PAI, parents rated their feelings toward their son or daughter as well as their son or daughter’s feelings toward them in terms of understanding, trust, fairness, respect, and affection on a 6-point scale (1 = not at all to 6 = extremely). The coefficient alphas were .88 at Time 1 and .86 at Time 2. Parental subjective burden in interactions with the adolescent was measured with 7 items from the Zarit Burden Interview (Zarit et al., 1980) assessing interactional burden; example items include “I feel angry about my interactions with my son/daughter,” “I feel nervous or depressed about my interactions with my son/daughter,” and “I feel strained in my interactions with my son/daughter.” The coefficient alphas were .83 at Time 1 and .76 at Time 2. Parents also reported how often that felt happy or proud of their child on a 5 point scale (0 = never to 4 = all of the time); we have used this indicator our past work (Smith et al., 2012). The Five Minute Speech Sample (FMSS) was used to code expressed emotion based on the coding manual developed by Magaña et al. (1986). For the FMSS, parents were asked to speak about their adolescent with ASD for five minutes uninterrupted. The speech samples were tape recorded, transcribed, and coded for various components of expressed emotion, including criticism, warmth, and positive remarks. Criticism was rated on a three point scale of high (3), borderline (2), or low (1). Warmth was coded on a 5-point scale from 0 (no warmth) to 4 (high warmth) based on guidelines from the Camberwell Family Interview (Vaugh & Leff, 1976). Positive remarks was a count, with five or more top coded as 5. All FMSS transcripts were coded by an independent rater with 20 years of experience in expressed coding who was blind to treatment condition. Reliability checks were conducted on 20% of samples. We note that we have successfully utilized this methodology in past samples of adolescents and adults with ASD (see Greenberg et al., (2006) and Smith et al., (2008) for more thorough descriptions of the FMSS methodology).
Adolescent outcomes
Frequency of social interactions was measured using maternal report on items from the National Longitudinal Study of Adolescent Health (Add Health): hanging out with friends, sending texts, and receiving texts. Given that there were different response options for these questions, items were z scored and summed to create a composite, with higher scores reflecting more frequent social interaction. Autism symptoms were measured using parent report of the Social Responsiveness Scale (SRS; Constantino et al., 2003). The SRS is a 65 item rating scale that assesses autism symptom severity, with higher scores reflecting more significant social impairment. The total score was used in the current analysis. Social engagement was measured during weekly intervention sessions using observational ratings on a three point scale (not at all engaged to clearly engaged). Intervention facilitators used consensus coding to establish an engagement rating for each adolescent immediately following each intervention session.
Social Validity
Social validity measures were collected via a satisfaction survey and exit interview questions at Time 2 for intervention participants. Respondents indicated on a 4 point scale how valuable (1 = not at all valuable to 4 = very valuable) to them was (1) the information presented to the group and (2) the time spent interacting with other families. Overall satisfaction with the program was rated on a 7-point scale (1=very dissatisfied to 7=very satisfied). Participants answered open-ended questions about what was learned and what they will do differently as a result of the program. Open-end comments were coded for themes.
Data Analysis
We conducted a series of two (time) by two (group) repeated measures ANCOVAs to test for differences in change from Time 1 (pre-intervention) to Time 2 (post-intervention) between the intervention group and the control group, controlling for IQ. Dependent variables included measures of parent well-being (depressive symptoms, problem solving, and general life stress), parent child relationship (relationship quality, burden in interactions, being happy/proud, warmth, positive remarks, and criticism), and adolescent outcomes (autism symptoms, social interactions). Additionally, for the intervention group, within subjects change in social engagement was assessed using repeated measures ANOVA. Based on power calculations using G*Power3 software (Faul et al., 2007) we were adequately powered to detect medium effects with an alpha of .05. We examined social validity using descriptive statistics of satisfaction survey data and qualitative coding of open-ended interview questions. All responses to open-ended questions were verbatim transcribed. Combined transcripts were then utilized for line by line frequency coding for common themes by the first author and reviewed by all authors. The number of participants with comments related to each theme were then calculated, reflecting proportion of sample with similar thematic responses.
Results
Quantitative Change over Time
We first examined differences in change between the two groups from pre to post intervention on measures of parental well-being. As shown in Table 3, there was a significant group by time interaction for parental depressive symptoms, F=4.87, p < .05, such that parents in the intervention group had a decreased number of depressive symptoms following the intervention compared to baseline, whereas there were no differences from pre- to post- for the control group. We note that the clinical cut point for depressive symptoms on the CES-D is 16; the mean score for intervention group parents at baseline (M=19.90) was well above that cut point. However, the mean for the intervention group at post-intervention (M=14.46) was in the normal range, reflecting clinical as well as statistical significance. There also was a significant group by time interaction for parental problem solving, F=4.42, p < .05, such that scores on the Family Empowerment measure of problem-solving increased for parents in the intervention group from pre to post intervention but not for parents in the control group (p=.60). The interaction term for general life stress was not statistically significant, suggesting no significant differences between the groups in change from pre to post intervention.
Regarding parent-child relationships, as shown in Table 3, there were no statistically significant differences in change between the two groups in terms of parent-child relationship quality or expressed emotion variables (criticism, warmth, positive remarks). There was a significant group by time interaction for parents feeling happy/proud of their adolescent, F=6.55, p < .05. Parents in the intervention group reported a higher frequency of feeling happy/proud at post-intervention than at pre-intervention, but this was not observed in the control group. A similar pattern was observed for burden in interactions but this was at a trend level (p=.077).
We next examined differences in change between the two groups on measures of adolescent outcomes (see Table 3). The group by time interaction term was non-significant for autism symptoms. However, the group by time interaction term was statistically significant for frequency of social interactions, F=4.75, p < .05, such that social interactions increased from pre to post intervention for the intervention group, but not for controls (p = .82).
We note that IQ was included as a covariate in all analyses. IQ was significantly related to parent-child relationship quality, feeling happy/proud, and warmth, such that higher levels of IQ were associated with lower scores on these measures. However, IQ was not a significant covariate for any of the parental well-being outcomes. Similarly, IQ was not significantly associated with either autism symptoms or frequency of social interactions.
Next, we explored change over time in adolescent social engagement using repeated measures ANOVA. Ratings of social engagement were available for adolescents in the intervention group only, as these ratings were collected at the conclusion of each intervention group session. Mean social engagement was 2.43 (SD=.65) at Week 1 and 2.93 (SD=.27) at Week 8, reflecting a statistically significant increase across the weeks, F=2.66, p<.05.
Social Validity
We evaluated the social validity of the intervention through a satisfaction survey and exit interview questions during the Time 2 interview. Parents reported that the information presented (M=3.94, SD=0.25) and the interactions with other families (M=3.63; SD=0.62) were both valuable. Overall parental satisfaction with the program as reported at the Time 2 interview was high (M=6.63; SD=.62).
Next, parent responses to the question “Did you learn any new information during the course of the program” were coded for themes, resulting in seven commonly-reported areas of learning presented in Table 4: guardianship/powers of attorney, vocational rehabilitation services, planning and advocacy, resources related to services and community involvement, validation, specific strategies for addressing concerns with their adolescent, and college planning. We note that all parents responded that they had learned something new in the course of the program. The most common area of learning was legal information related to guardianship and powers of attorney. Interestingly, although the open-ended question asked about new information learned, a quarter of parents responded that by getting to know other families in the group, they learned that they were not alone in their experiences and struggles, which they found highly validating.
Table 4.
Results of 2 (Group) by 2 (Time) ANCOVAs Controlling for IQ
| Intervention Group | Control Group | ||||
|---|---|---|---|---|---|
|
| |||||
| Time 1 M(SD), n |
Time 2 M(SD), n |
Time 1 M(SD), n |
Time 2 M(SD), n |
Time by Group F | |
| Parental Well-being | |||||
|
| |||||
| Depressive Symptoms | 19.90 (3.04), 14 | 14.46 (2.97), 14 | 13.25 (2.40), 21 | 13.36 (2.35), 21 | 4.87; p=.035 |
| General Life Stress | 20.16 (2.20), 14 | 17.67 (2.30), 14 | 17.83 (1.74), 21 | 16.61 (1.80), 21 | .33; p=.572 |
| Problem Solving | 2.41 (0.24), 14 | 2.85 (0.20), 14 | 2.70 (0.19), 21 | 2.72 (0.16), 21 | 4.42; p=.04 |
|
| |||||
| Parent-Child Relationship | |||||
|
| |||||
| Relationship Quality | 45.08(2.12), 14 | 43.58(1.86), 14 | 43.90(1.68), 21 | 43.42(1.47), 21 | 0.20; p=.659 |
| Burden in Interactions | .68 (.13), 14 | .47 (.11), 14 | .49 (.10), 21 | .52 (.09), 21 | 3.35; p=.077 |
| Happy/Proud | 2.06(.24), 16 | 2.60(.17), 16 | 2.52(.18), 25 | 2.34(.13), 25 | 6.55; p=.015 |
| Warmth | 3.42(.30), 16 | 3.80(.31), 16 | 3.88(.25), 22 | 3.65(.26), 22 | 1.35; p=.254 |
| Positive Remarks | 3.08(.44), 16 | 2.5(.51), 16 | 1.85(.37), 22 | 2.01(.42), 22 | .53; p=.470 |
| Criticism | 1.76(.56), 16 | 2.01(.17), 16 | 2.54(.47), 22 | 1.72(.47), 22 | 1.69; p=.202 |
|
| |||||
| Adolescent Outcomes | |||||
|
| |||||
| Autism Symptoms | 97.94(7.17), 12 | 99.61(7.10), 12 | 88.98(6.31), 15 | 88.71(6.24), 15 | .164; p=.689 |
| Social Interactions | −.09 (.20), 16 | .33(.22), 16 | −.19(.16), 25 | −.21(.17), 25 | 4.75; p=.036 |
Parent responses to the question “Will you do anything differently based on your experiences in this group?” also were coded for themes as shown in Table 5. Being an advocate and specific action steps were the two most common themes, respectively. We note that for the advocacy theme, many parents reflected on how the program empowered them to be more persistent in their advocacy efforts, particularly as it related to school programming. Comments that fell into the specific action steps theme related to action steps already completed (e.g., enrolling in vocational rehabilitation, attending community events suggested during sessions, contacting a psychologist) as well as specific plans for future action (e.g., adding new detail to the transition plan in the IEP, organizing with other families). The final two themes related to changes in the parent’s relationship with the adolescent, specifically having new perspectives the adolescent, which included adjusted expectations, and allow the teen more responsibility, reflecting at times a need for the parent to “pull back” and encourage the teen to try for themselves.
Table 5.
Parent Self-Reported Learning from Program (from the Open-Ended Exit Interview)
| Area of New Learning |
% of Parents |
Example Quotes |
|---|---|---|
|
| ||
| Guardianship/ Powers of Attorney | 56.3% | “The legal pieces were very helpful to our family, like learning about guardianship.” |
| “Powers of attorney and when to do them and if they’re applicable for our child.” | ||
|
| ||
| Department of Vocational Rehabilitation (DVR) | 50.0% | “We learned it was appropriate for us to get hooked up with DVR and how to do that.” |
| “We didn’t know that DVR existed so we went from having no idea that he would quality for something like that to going through the whole process.” | ||
| “It gave me hope for DVR because when I talked to somebody [at school] it was almost like ‘don’t bother to apply.’” | ||
|
| ||
| Planning and Advocacy | 43.8% | “It gave me a wealth of information as far as what should have been going on in the school as far as transitioning.” |
| “How transition is supposed to be working when you’re in school. We had no idea and we still would have had no idea if we’d only had our school to rely on.” | ||
| “How to plan and how to figure out what to do for him … It was an excellent opportunity for me as a parent to figure out how to transverse all the transition stuff and to become a better advocate for my kid.” | ||
|
| ||
| Resources on Services and Community Involvement | 43.8% | “Learning about getting him involved in community stuff and keeping him involved and who to contact for what, like volunteer opportunity stuff.” |
| “All the information was geared towards kids like mine. It was so very helpful, the resources, the things that we knew nothing about or didn’t know.” | ||
| “The resources they gave, what I can do to broaden her horizons, especially community stuff.” | ||
|
| ||
| Validation | 25.0% | “It was very validating to hear other families talking about these same things.” |
| “We got that validation that his struggles are very much similar to other families who have high-functioning kids with autism. … That validation was really huge.” | ||
|
| ||
| Specific Strategies for Addressing Concerns with Teen | 18.8% | “Strategies for some of the things we have been struggling with, like organization.” |
| “Ideas for handling issues and also looking at issues in a different way.” | ||
|
| ||
| College Planning | 18.8% | “Knowing what questions to ask when considering postsecondary education was really useful.” |
| “The information about college and what to expect and ideas to try.” | ||
Discussion
The present study evaluated a multi-family group psychoeducation intervention, Transitioning Together, for families of adolescents with high-functioning ASD using a randomized waitlist control design. This study addressed a critical gap in research and practice for individuals with ASD by examining a program designed specifically to support the family system during the transition to adulthood (Smith & Anderson, 2014). Consistent with results of multi-family group psychoeducation interventions for families of individuals with mental health conditions (e.g., mood disorders; Sanford et al., 2006), our findings suggested benefits of the intervention on parent well-being, parent-child relations, and social outcomes for adolescents with ASD.
The goal of multifamily group psychoeducation is to provide (1) education about a clinical condition, (2) guided practice in problem-solving, and (3) opportunities for social support from others who have similar experiences in order to reduce the overall level of distress in the home and in turn improve outcomes for all family members (McFarlane et al., 2003). We found evidence of these effects in the current study. Specifically, compared to families in the waitlist control condition, parents in the intervention had increased problem-solving skills following the intervention, suggesting that parents learned new strategies and gained confidence as a result of training and practice in finding workable solutions for problems related to their children. Parental depressive symptoms also decreased from pre- to post-intervention for families in the intervention condition but not in the waitlist control condition. Given that depressive symptoms are often elevated in parents of adolescents and adults with ASD relative even to other disability groups (Abbeduto et al., 2004), this reduction in depressive symptoms for parents following the intervention is encouraging. Interestingly, there was not a statistically significant difference between the intervention and waitlist control group in change in perceived stress. As our measure of stress, the PSS, assessed general life stress, it may be that a measure of stress more directly related to parenting an adolescent with ASD such as the Parenting Stress Index (Abidin, 1997) or the Questionnaire on Resources and Stress (Konstantareas, Homatidis, & Plowright, 1992) would have been more proximal and sensitive to change.
Another key area in which we would expect to see significant changes following the intervention was in the domain of the parent-child relationship. Consistent with our pilot work (BLINDED 2012), we found that parents in the intervention had significant increases in being happy or proud of their adolescent with ASD from pre- to post-intervention compared to the waitlist control group. A similar pattern was observed for reductions in burden in interactions with the son or daughter, although this was not quite significant at the .05 level. Surprisingly, there were not statistically significant changes between groups in the expressed emotion variables (warmth, criticism, and positive remarks). In our pilot work we found significant improvement in ratings of warmth using the same coding system following the intervention (BLINDED, 2012). Also unexpected, child IQ was significantly related to warmth, parent-child relationship quality, and feeling happy/proud (but not other study measures such as parental depression or social interactions), such that higher levels of IQ were associated with lower scores on these measures. Although cases were randomly assigned, there was a significant difference in level of IQ between the two groups at baseline, with the intervention group having IQs over 10 points higher on average than the waitlist control group. It may be that even with statistical controls this difference in IQ obscured potential differences in change over time on these measures.
The final area in which benefits for families would be expected as a result of a multi-family group psychoeducation intervention is in the area of social functioning for the adolescent with ASD. Consistent with findings of family psychoeducation interventions with adolescents with other conditions (e.g., Sanford et al., 2006), in the present study there was a significant improvement in frequency of social interactions for adolescents in the intervention group following the intervention but not for adolescents in the control group. There was also significant improvement in ratings of social engagement across the 8 weeks of group sessions. These findings are particularly promising given that over half of the sample had a co-occurring diagnosis of anxiety and over a fifth had a diagnosis of depression. However, consistent with our pilot work (BLINDED, 2012), we did not observe significant change in level of autism symptoms as measured by the SRS. Given the relatively short timeframe of the study (3 months), the benefits of improved family functioning may not have had time to subsequently impact core autism symptoms. It also may be that this type of intervention approach may be better suited for addressing functional improvements for adolescents (e.g., spending more time with friends) rather than phenotypic characteristics. Core symptoms may be more effectively addressed with interventions specifically designed to remediate social and communication deficits. Additionally, it may be that the SRS is not the best measure for capturing change in autism symptoms, especially for individuals with less severe autism (Azad, Reisinger, Xie, & Mandell, 2016).
We also note that the Transitioning Together program had high social validity for families. Parents reported that the intervention content and interactions with other families were valuable and their overall satisfaction with the program was high. Qualitative data from open-ended interviews also aligned with the quantitative findings. Specifically, following completion of the intervention, parents reported that they became an advocate, took specific action steps, had new perspectives on their adolescent, and allowed their teen more responsibility as a result of the program. These themes are consistent with the quantitative findings of improved problem-solving (which includes action steps) and changes in attitudes (e.g., feeling happy or proud). All parents reported learning specific new information through the program, most notably information on legal issues such as guardianship, highlighting that families not only appreciated opportunities to practice problem-solving but also the education they received that was relevant to the transition to adulthood.
The present study had several limitations. Most notably, despite random assignment, there was a significant difference in IQ between the two conditions, with adolescents in the intervention group having higher IQs than adolescents in the control group. Although we controlled for IQ in all analyses, the uneven distribution of IQ may have influenced the results. Second, although our a power calculations indicated the study was adequately powered to detect medium effects, the sample size was still small and parents in the study were primarily White and highly educated, limiting the generalizability of the findings. It also may be that the program was not accessible to the full range of families impacted by having a child on the autism spectrum. Future work should extend this work and evaluate the multi-family group psychoeducation approach for families from culturally and linguistically diverse backgrounds and consider what possible adaptations may be needed to the curriculum. This gap is beginning to be addressed through the work of the Center on Secondary Education for Students with Autism study which includes a large, national sample with youth and families from diverse backgrounds (Kuhn, Borjas, & Smith, 2015; Odom, Duda, Kucharczyk, Cox, & Stabel, 2014). Third, we note that our study focused on adolescents with high functioning ASD (i.e., verbally fluently and primarily served in general education settings); additional research is needed to examine the effects of the program for adolescents with different support needs. Fourth, only one parent per family participated in data collection. It would be useful for future studies to collect data from both parents and to explore for potential differences in intervention effectiveness for mothers and fathers as well as the impact of completing the intervention together on the marital relationship. Finally, due to the basic pre-post design for this preliminary evaluation, the present study had only one time of data collection following the intervention; it would be very valuable to know if effects of the intervention were sustained for a longer duration than immediately following completion of the intervention.
In conclusion, results from this randomized waitlist control trail highlight potential benefits of the Transitioning Together program for adolescent social interactions, parental well-being, and parent-child relations. These findings are consistent with the gains demonstrated in studies of multi-family group psychoeducation interventions conducted with other populations (Dixon et al., 2000; McFarlane et al., 2003). Adding to the emerging literature on ways to support the well-being of the entire family system for children and youth with developmental disabilities (e.g., Dykens et al., 2014; Neece, 2014), the Transitioning Together is a promising multi-family group psychoeducation intervention to support adolescents with ASD and their parents during the transition to adulthood.
Table 6.
Parent Self-Reports of What They Will Do Differently (from the Open-Ended Exit Interview)
| Themes | % of Parents |
Example Quotes |
|---|---|---|
|
| ||
| Be an Advocate | 31.3% | “We’re going to push a lot harder for the school to do more with the IEP.” |
| “When the [program] talked about transition and quality of life it’s like I was finally validated because that’s what I’ve wanted. I just haven’t seen the school doing it. So now with the knowledge that I’ve been given about what’s out there and what can be done, I’m going to keep pushing … I’ve even considered if we can’t get help in the school then maybe I’ll get an attorney to start demanding some rights. I am prepared to take it up a notch.” | ||
| “We are in a better position to advocate for the services [child] should be receiving … it empowered us to do that.” | ||
|
| ||
| Specific Action Steps | 31.3% | “There was just an incident at the school. I was very proactive. Normally I would have gone in there like a mother bear, but this time I was thinking about my rights and his rights and I was on top of it. I used my knowledge.” |
| “I wrote a letter to the school and the district specialist asking to get him involved in some of work activities through school, like volunteering.” | ||
| “I’ve been working with him at home going through his likes and dislikes about careers, using what we got at the program.” | ||
| “We’re going to make sure there is more detail in his transition plan and that there are other people from outside groups involved [at the IEP].” | ||
|
| ||
| New Perspective on Teen | 25.0% | “It’s not that we forgot that he has Aspergers, but this group brought that back. You know, it’s hard for him too, and we don’t want to forget that. … We want to step back and think about how Aspergers affects him and respond with that in mind and plan with that in mind.” |
| “He wants to go to college now, to live on his own. I don’t think we realized that was attainable for him before.” | ||
|
| ||
| Allow Teen More Responsibility | 18.8% | “We let go and have given that responsibility to him. We have more things we need to think about letting go of.” |
| “We are now moving towards letting him take drivers ed and we are thinking about driving.” | ||
Acknowledgments
This research was supported by a grant from Autism Speaks (Grant #7523; Smith, PI) as well as a grant from the National Institute on Aging (R01AG08768, M.R. Mailick, PI). We also gratefully acknowledge support from the Waisman Center (U54 HD090256, Messing, PI) and UW-Madison’s Clinical and Translational Science Award Program for community intervention research (supported in part by grant U21 RR025011). We are extremely grateful to the families who participated in this study; without their generous support and commitment, our research would not be possible.
This research was supported by a grant from Autism Speaks (Grant #7523; Smith, PI) as well as a grant from the US Department of Education, Institute of Education Sciences, to support the work of the Center on Secondary Education for Students with Autism Spectrum Disorders (R324C12006; Odom, PI). We are extremely grateful to the families who participated in this study; without their generous support and commitment, our research would not be possible. We are also grateful for the support we received from the Waisman Center (P30 HD03352, M.Mailick, PI).
Footnotes
Conflict of Interest: Dr. Smith declares she has no conflict of interest. Dr. Greenberg declares he has no conflict of interest. Dr. Mailick declares she has no conflict of interest.
Compliance with Ethical Standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Contributor Information
Leann E. Smith, Waisman Center, University of Wisconsin-Madison, Madison, WI
Jan S. Greenberg, University of Wisconsin-Madison, Madison, WI
Marsha R. Mailick, Waisman Center, University of Wisconsin-Madison, Madison, WI
References
- Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond G, Murphy MM, Floyd F. Psycyhological well-being and coping in mothers of youths with autism, down syndrome, or fragile X syndrome. American Journal on Mental Retardation. 2004;109(3):237–254. doi: 10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Abidin RR. Parenting stress index: A measure of the parent-child system. In: Zalaquett CP, Wood RJ, editors. Evaluating stress: A book of resources. Lanham, MD: Scarecrow Education; 1997. pp. 277–291. [Google Scholar]
- Azad GF, Reisinger E, Xie M, Mandell DS. Parent and teacher concordance on the social responsiveness scale for children with autism. School Mental Health. 2016;8:368–376. doi: 10.1007/s12310-015-9168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Seltzer MM, Greenberg JS. Longitudinal effects of adaptability on behavior problems and maternal depression in families of adolescents with autism. Journal of Family Psychology. 2011;25(4):601–9. doi: 10.1037/a0024409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker J, Smith LE, Greenberg JS, Seltzer MM. Change in maternal criticism and behavior problems in adolescents and adults with autism across a seven-year period. Journal of Abnormal Psychology. 2011 doi: 10.1037/a0021900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker ET, Seltzer MM, Smith LE. Chronic parenting stress in mothers of adolescents and adults with autism: Vulnerability and resilience. In: Martin CR, Preedy VR, Patel VB, editors. The Comprehensive Guide to Autism. London: UK: Springer; 2013. [Google Scholar]
- Bengtson VL, Schrader SS. Parent–child relationship. In: Mangon DJ, Peterson WA, editors. Research instruments in social gerontology. Vol. 2. Minneapolis: University of Minnesota Press; 1982. pp. 115–185. [Google Scholar]
- Blacher J, McIntyre LL. Syndrome specificity and behavior disorders in young adults with intellectual disability: Cultural differences in family impact. Journal of Intellectual Disability Research. 2006;50:184–198. doi: 10.1111/j.1365-2788.2005.00768.x. [DOI] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, Minshew NJ, Eack SM. The relationshiop between stress and social funcitoning in adults with autism spectrum disorder and without intellectual disability. Autism Research. 2015;8:164–173. doi: 10.1002/aur.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruininks R, Woodcock R, Weatherman R, Hill B. Scales of Independent Behavior--Revised Comprehensive Manual. Itasca, IL: Riverside Publishing; 1996. [Google Scholar]
- Chiquelho R, Neves S, Mendes A, Relvas AP, Sousa L. ProFamilies: A psychoeducational multi-family group intervention for cancer patients and their families. European Journal of Cancer Care. 2011;20:337–344. doi: 10.1111/j.1365-2354.2009.01154.x. [DOI] [PubMed] [Google Scholar]
- Christensen DL, Baio J, Braun KV, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveillance Summary. 2016;65:1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park, CA: Sage; 1988. [Google Scholar]
- Constantino JN, Davis SA, Todd RD, Schindler MK, Gross MM, Brophy SL, et al. Validation of a brief quantitative measure of autistic traits: Comparison of the Social Responsiveness Scale with the Autism Diagnostic Interview-Revised. Journal of Autism and Developmental Disorders. 2003;33:427–433. doi: 10.1023/a:1025014929212. [DOI] [PubMed] [Google Scholar]
- Dixon L, Adams C, Lucksted A. Update on family psychoeducation for schizophrenia. Schizophrenia Bulletin. 2000;26:5–20. doi: 10.1093/oxfordjournals.schbul.a033446. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Fisher MH, Taylor JL, Lambert W, Miodrag N. Reducing distress in mothers of children with autism and other disabilities: A randomized trial. Pediatrics. 2014;134:e454–463. doi: 10.1542/peds.2013-3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenhower AS, Baker BL, Blacher J. Preschool children with intellectual disability: Syndrome specificity, behavior problems, and maternal well-being. Journal of Intellectual Disability Research. 2005;49:657–671. doi: 10.1111/j.1365-2788.2005.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esbensen AJ, Bishop SL, Seltzer MM, Greenberg JS, Taylor JL. Comparisons between individuals with autism spectrum disorders and individuals with Down syndrome in adulthood. American Journal of Intellectual and Developmental Disabilities. 2010;115(4):277–290. doi: 10.1352/1944-7558-115.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essex EL, Seltzer MM, Krauss MW. Residential transitions of adults with mental retardation: Predictors of waiting list use and placement. American Journal of Mental Retardation. 1997;101(6):613–629. [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Greenberg JS, Seltzer MM, Hong J, Orsmond GI. Bidirectional effects of expressed emotion and behavior problems and symptoms in adolescents and adults with autism. American Journal of Mental Retardation. 2006;111:229–249. doi: 10.1352/0895-8017(2006)111[229:BEOEEA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Gurney J, Fritz M, Ness K, Sievers P, Newschaffer C, Shapiro E. Analysis of prevalence trends of autism spectrum disorder in Minnesota. Archives of Pediatrics and Adolescent Medicine. 2003;157:622–627. doi: 10.1001/archpedi.157.7.622. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Lloyd T. Expressed emotion in families of children and adults with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:339–345. doi: 10.1002/mrdd.20173. [DOI] [PubMed] [Google Scholar]
- Hayes SA, Watson SL. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43:629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Henninger NA, Taylor JL. Outcomes in adults with autism spectrum disorders: a historical perspective. Autism. 2012;17:103–117. doi: 10.1177/1362361312441266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Good S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P. In review: Adults with autism spectrum disorders. Canadian Journal of Psychiatry. 2012;57(5) doi: 10.1177/070674371205700502. [DOI] [PubMed] [Google Scholar]
- Karst JS, Van Hecke AV, Carson AM, Stevens S, Schohl K, Dolan B. Parent and family outcomes of PEERS: A social skills intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45:752–765. doi: 10.1007/s10803-014-2231-6. [DOI] [PubMed] [Google Scholar]
- Klaus N, Fristad MA. Family psychoeducation as a valuable adjunctive intervention for children with bipolar disorder. Directions in Psychiatry. 2005;25:217–230. [Google Scholar]
- Konstantareas MM, Homatidis S, Plowright CM. Assessing resources and stress in parents of severely dysfunctional children through the Clarke modification of Holroyd’s Questionnaire on Resources and Stress. Journal of Autism and Develo9pmetnal Disorders. 1992;22:217–234. doi: 10.1007/BF01058152. [DOI] [PubMed] [Google Scholar]
- Koren PE, DeChillo N, Friesen BJ. Measuring empowerment in families whose children have emotional disabilities: A brief questionnaire. Rehabilitation Psychology. 1992;37:305–321. [Google Scholar]
- Krauss MW, Seltzer MM, Jacobson HT. Adults with autism living at home or in non-family settings: Positive and negative aspects of residential status. Journal of Intellectual Disability Research. 2005;49:111–124. doi: 10.1111/j.1365-2788.2004.00599.x. [DOI] [PubMed] [Google Scholar]
- Kring SR, Greenberg JS, Seltzer MM. Adolescents and adults with autism with and without co-morbid psychiatric disorders: Differences in maternal well-being. Journal of Mental Health Research in Intellectual Disabilities. 2008;1:53–74. doi: 10.1080/19315860801988228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn J, Borjas S, Smith L. Cultural and linguistic adaptation of an education and support program for families with adolescents with autism. Poster presented at the 2015 Association of University Centers on Disability Annual Conference; Washington, DC. 2015. Nov, [Google Scholar]
- Laugeson EA, Gantman A, Kapp SK, Orenski K, Ellingsen R. A randomized controlled trial to improve social skills in young adults with autism spectrum disorder: The UCLA PEERS program. Journal of Autism and Developmental Disorders. 2015;45:3978–3989. doi: 10.1007/s10803-015-2504-8. [DOI] [PubMed] [Google Scholar]
- Lounds J, Seltzer MM, Greenberg JS, Shattuck P. Transition and change in adolescents and young adults with autism: Longitudinal effects on maternal well-being. American Journal on Mental Retardation. 2007;112(6):401–417. doi: 10.1352/0895-8017. [DOI] [PubMed] [Google Scholar]
- Maenner M, Smith L, Hong J, Makuch R, Greenberg J, Mailick M. An evaluation of an activities of daily living scale for adolescents and adults with developmental disabilities. Disability and Health Journal. 2013;6:8–17. doi: 10.1016/j.dhjo.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña A, Goldstein M, Karno M, Miklowitz D, Jenkins J, Falloon I. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research. 1986;17:203–212. doi: 10.1016/0165-1781(86)90049-1. [DOI] [PubMed] [Google Scholar]
- McFarlane WR. Multifamily groups in the treatment of severe psychiatric disorders. New York, NY: Guilford Press; 2002. [Google Scholar]
- McFarlane WR, Dixon L, Lukens E, Lucksted A. Family psychoeducation and schizophrenia: A review of the literature. Journal of Marital and Family Therapy. 2003;29:223–245. doi: 10.1111/j.1752-0606.2003.tb01202.x. [DOI] [PubMed] [Google Scholar]
- Montes G, Halterman JS. Psychological functioning and coping among mothers of children with autism: A population-based study. Pediatrics. 2006;119:1040–1046. doi: 10.1542/peds.2006-2819. [DOI] [PubMed] [Google Scholar]
- Neece CL. Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. Journal of Applied Research in Intellectual Disabilities. 2014;27:174–186. doi: 10.1111/jar.12064. [DOI] [PubMed] [Google Scholar]
- Ng SM, Li AM, Lou VWW, Tso IF, Wan PYP, Chan DFY. Incorporating family therapy into asthma group intervention: A randomized waitlist-controlled trial. Family Process. 2008;47:115–130. doi: 10.1111/j.1545-5300.2008.00242.x. [DOI] [PubMed] [Google Scholar]
- Odom SL, Duda M, Kucharczyk S, Cox A, Stabel A. Applying an implementation science framework for adoption of a comprehensive program for high school students with autism spectrum disorder. Remedial and Special Education. 2014;2(35):123–132. [Google Scholar]
- Orsmond GI, Krauss MW, Seltzer MM. Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders. 2004;34(3):245–256. doi: 10.1023/b:jadd.0000029547.96610.df. [DOI] [PubMed] [Google Scholar]
- Orsmond GI, Seltzer MM. Adolescent siblings of individuals with an autism spectrum disorder: Testing a diathesis-stress model of sibling well-being. Journal of Autism and Developmental Disorders. 2009;39(7):1053–1065. doi: 10.1007/s10803-009-0722-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. Social Communication Questionnaire (SCQ) Los Angeles: Western Psychological Services; 2201. [Google Scholar]
- Sanford M, Boyle M, McClearly L, Miller J, Steele M, Duku E, et al. A pilot study of adjunctive family psychoeducation in adolescent major depression: Feasibility and treatment effect. Journal of American Academy of Child and Adolescent Psychiatry. 2006;45:386–395. doi: 10.1097/01.chi.0000198595.68820.10. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Krauss MW, Shattuck PT, Orsmond G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33:565–581. doi: 10.1023/b:jadd.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Shattuck P, Abbeduto L, Greenberg JS. The trajectory of development in adolescents and adults with autism. Mental Retardation Developmental Disabilities Research Reviews. 2004;10:234–247. doi: 10.1002/mrdd.20038. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Seltzer MM, Greenberg JS, Orsmond GI, Bolt D, Kring S, et al. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;13:129–135. doi: 10.1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Narendor SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. 2012;129(6):1042–1049. doi: 10.1542/peds.2011-2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Wagner M, Narendorf S, Sterzing P, Hensley M. Post-high school service use among young adults with an autism spectrum disorder. Archives of Pediatric and Adolescent Medicine. 2011;165:141–146. doi: 10.1001/archpediatrics.2010.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer GHS, Ethridge BL, Aldana SI. Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities:A meta-analysis. Mental Retardation and Developmental Disabilities Research Reviews. 2007 ;13:357–369. doi: 10.1002/mrdd.20175. [DOI] [PubMed] [Google Scholar]
- Smith LE, Anderson KA. The roles and needs of families of adolescents with ASD. Remedial and Special Education. 2014;35:114–122. doi: 10.1177/0741932513514616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, Seltzer MM, Hong J. Symptoms and behavior problems of adolescents and adults with autism: Effects of mother-child relationship quality, warmth, and praise. American Journal on Mental Retardation. 2008;113:378–393. doi: 10.1352/2008.113:387-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Hong J, Seltzer MM, Greenberg JS, Almeida DM, Bishop S. Daily experiences among mothers of adolescents and adults with ASD. Journal of Autism and Developmental Disorders. 2010;40:167–178. doi: 10.1007/s10803-009-0844-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Maenner MJ, Seltzer MM. Developmental trajectories in adolescents and adults with autism: The case of daily living skills. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:622–631. doi: 10.1016/j.jaac.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Henninger NA, Mailick MR. Longitudinal patterns of employment and postsecondary education for adults with autism and average-range IQ. Autism. 2015 doi: 10.1177/1362361315585643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Smith LE, Mailick MR. Engagement in vocational activities promotes behavioral development for adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2014;44:1447–1460. doi: 10.1007/s10803-013-2010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Mailick MR. A longitudinal examination of 10-year change in vocational and educational activities for adults with autism spectrum disorders. Developmental Psychology. 2013 doi: 10.1037/a0034297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Changes in the autism behavioral phenotype during the transition to adulthood. Journal of Autism and Developmental Disorders. 2010;40:1431–1446. doi: 10.1007/s10803-010-1005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Changes in the mother-child relationship during the transition to adulthood for youth with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2011a;41:1397–1410. doi: 10.1007/s10803-010-1166-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders. 2011b;41(5):566–74. doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaugh C, Leff J. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology. 1976;15:157–165. doi: 10.1111/j.2044-8260.1976.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale—Fourth Edition. San Antonio, TX: Pearson Assessment; 2008. [Google Scholar]
- Woodman AC, Smith LE, Greenberg JS, Mailick MR. Contextual factors predict patterns of change in functioning over 10 years among adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2016;46:176–189. doi: 10.1007/s10803-015-2561-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss MJ. Hardiness and social support as predictors of stress in mothers of typical children, children with autism, and children with mental retardation. Autism. 2002;6:115–130. doi: 10.1177/1362361302006001009. [DOI] [PubMed] [Google Scholar]
- Young ME, Fristad MA. Evidence based treatments for bipolar disorder in children and adolescents. Journal of Contemporary Psychotherapy. 2007;37:157–164. [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]