Abstract
In recent years, there has been a growing interest in researching and developing new antimicrobial agents from various sources to combat microbial resistance. Therefore, a greater attention has been paid to antimicrobial activity screening and evaluating methods. Several bioassays such as disk-diffusion, well diffusion and broth or agar dilution are well known and commonly used, but others such as flow cytofluorometric and bioluminescent methods are not widely used because they require specified equipment and further evaluation for reproducibility and standardization, even if they can provide rapid results of the antimicrobial agent's effects and a better understanding of their impact on the viability and cell damage inflicted to the tested microorganism. In this review article, an exhaustive list of in vitro antimicrobial susceptibility testing methods and detailed information on their advantages and limitations are reported.
Keywords: Thin-layer chromatography (TLC)–bioautography, Time-kill test, Antimicrobial gradient method, Agar diffusion method
1. Introduction
Antimicrobial susceptibility testing can be used for drug discovery, epidemiology and prediction of therapeutic outcome. In this review, we focused on the use of antimicrobial testing methods for the in vitro investigation of extracts and pure drugs as potential antimicrobial agents.
After the revolution in the “golden era”, when almost all groups of important antibiotics (tetracyclines, cephalosporins, aminoglycosides and macrolides) were discovered and the main problems of chemotherapy were solved in the 1960s, the history repeats itself nowadays and these exciting compounds are in danger of losing their efficacy because of the increase in microbial resistance [1]. Currently, its impact is considerable with treatment failures associated with multidrug-resistant bacteria and it has become a global concern to public health [2], [3].
For this reason, discovery of new antibiotics is an exclusively important objective. Natural products are still one of the major sources of new drug molecules today. They are derived from prokaryotic bacteria, eukaryotic microorganisms, plants and various animal organisms. Microbial and plant products occupy the major part of the antimicrobial compounds discovered until now [4].
Plants and other natural sources can provide a huge range of complex and structurally diverse compounds. Recently, many researchers have focused on the investigation of plant and microbial extracts, essential oils, pure secondary metabolites and new synthetized molecules as potential antimicrobial agents [5], [6], [7]. However, when we reviewed the published articles on the antimicrobial effect of these natural products, the comparison between results is often difficult, because of the use of different non-standardized approaches inoculum preparation techniques, inoculum size, growth medium, incubation conditions and endpoints determination.
The fact that a plant extract exhibits antimicrobial activity is of interest, but this preliminary part of data should be trustworthy and allow researchers to compare results, avoiding work in which researchers use the antimicrobial activity investigation only as a complement to a phytochemical study.
A variety of laboratory methods can be used to evaluate or screen the in vitro antimicrobial activity of an extract or a pure compound. The most known and basic methods are the disk-diffusion and broth or agar dilution methods. Other methods are used especially for antifungal testing, such as poisoned food technique. To further study the antimicrobial effect of an agent in depth, time-kill test and flow cytofluorometric methods are recommended, which provide information on the nature of the inhibitory effect (bactericidal or bacteriostatic) (time-dependent or concentration-dependent) and the cell damage inflicted to the test microorganism.
Owing to the new attraction to the properties of new antimicrobial products like combating multidrug-resistant bacteria, it is important to develop a better understanding of the current methods available for screening and/or quantifying the antimicrobial effect of an extract or a pure compound for its applications in human health, agriculture and environment. Therefore, in this review, the techniques for evaluating the in vitro antimicrobial activity were discussed in detail.
2. Diffusion methods
2.1. Agar disk-diffusion method
Agar disk-diffusion testing developed in 1940 [8], is the official method used in many clinical microbiology laboratories for routine antimicrobial susceptibility testing. Nowadays, many accepted and approved standards are published by the Clinical and Laboratory Standards Institute (CLSI) for bacteria and yeasts testing [9], [10]. Although not all fastidious bacteria can be tested accurately by this method, the standardization has been made to test certain fastidious bacterial pathogens like streptococci, Haemophilus influenzae, Haemophilus parainfluenzae, Neisseria gonorrhoeae and Neisseria meningitidis, using specific culture media, various incubation conditions and interpretive criteria for inhibition zones [9].
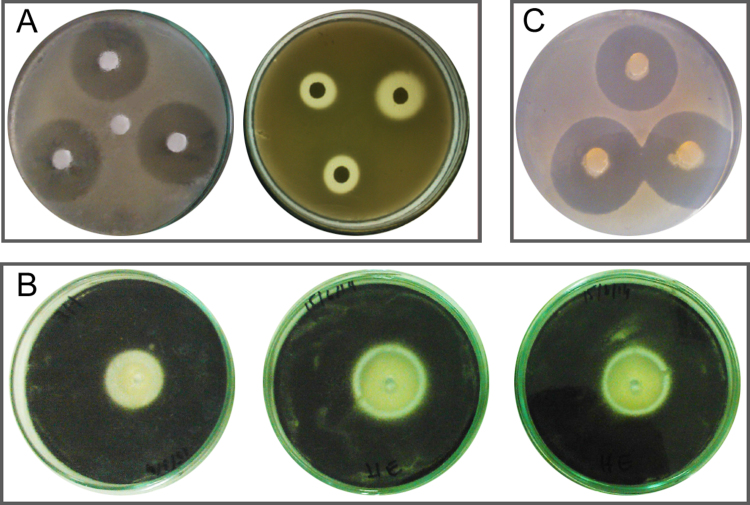
In this well-known procedure, agar plates are inoculated with a standardized inoculum of the test microorganism. Then, filter paper discs (about 6 mm in diameter), containing the test compound at a desired concentration, are placed on the agar surface. The Petri dishes are incubated under suitable conditions. Generally, antimicrobial agent diffuses into the agar and inhibits germination and growth of the test microorganism and then the diameters of inhibition growth zones are measured (Fig. 1A). Table 1 shows the growth media, temperature, period of incubation and inoculum size required by CLSI standards.
Fig. 1.
Agar diffusion methods: (A) disk-diffusion method of microbial extract using C. albicans as test microorganism, (B) agar well diffusion method of essential oil using Aspergillus niger as test microorganism, and (C) agar plug diffusion method of Bacillus sp. against C. albicans.
Table 1.
Culture media, microbial inoculum size and incubation conditions for antimicrobial susceptibility testing methods as recommended by CLSI.
| Methods | Microorganism | Growth medium | Final inoculum size | Incubation temperature (°C) | Incubation time (h) | Ref. |
|---|---|---|---|---|---|---|
| Disk-diffusion method | Bacteria | MHA | (0.5 McFarland) (1–2)×108 CFU/mL | 35±2 | 16–18 | M02-A [9] |
| Yeast | MHA+GMBa | (0.5 McFarland) (1–5)×106 CFU/mL | 35±2 | 20–24 | M44-A [10] | |
| Molds | Non-supplemented MHA | (0.4–5)×106 CFU/mL | – | – | M51-A [18] | |
| Broth microdilution | Bacteria | MHB | 5×105 ×CFU/mL | 35±2 | 20 | M07-A [56] |
| Yeast | RPMI 1640b | (0.5–2.5)×103 CFU/mL | 35 | 24–48 | M27-A [69] | |
| Molds | RPMI 1640b | (0.4–5)×104 CFU/mL | 35 | 48 for most fungi | M38-A [70] | |
| Broth macrodilution | Bacteria | MHB | 5×105 CFU/mL | 35±2 | 20 | M07-A [56] |
| Yeast | RPMI 1640b | (0.5–2.5)×103 CFU/mL | 35 | 46–50 | M27-A [69] | |
| Molds | RPMI 1640b | (0.4–5)×104 CFU/mL | 35 | 48 for most fungi | M38-A [70] | |
| Agar dilution | Bacteria | MHA | 104 CFU/spot | 35±2 | 16–20 | M07-A [56] |
| Time-kill test | Bacteria | MHB | 5×105 CFU/mL | 35±2 | 0, 4, 18, and 24 | M26-A [75] |
MHA: Mueller Hinton Agar. MHB: Mueller Hinton Broth.
GMB: the medium was supplemented with 2% glucose and 0.5 mg/mL methylene blue.
RPMI 1640: Roswell Park Memorial Institute medium (with glutamine, without bicarbonate, and with phenol red as a pH indicator) was 1640, buffered to pH 7.0 with MOPS (morpholine propane sulfonic acid) at 0.165 M.
Antibiogram provides qualitative results by categorizing bacteria as susceptible, intermediate or resistant [11]. Therefore, it is a typing tool based on the resistance phenotype of the microbial strain tested, its outcomes also guide clinicians in the appropriate selection of initial empiric treatments, and antibiotics used for individual patients in particular situations [12]. However, since the bacterial growth inhibition does not mean the bacterial death, this method cannot distinguish bactericidal and bacteriostatic effects.
Moreover, the agar disk-diffusion method is not appropriate to determine the minimum inhibitory concentration (MIC), as it is impossible to quantify the amount of the antimicrobial agent diffused into the agar medium. Nevertheless, an approximate MIC can be calculated for some microorganisms and antibiotics by comparing the inhibition zones with stored algorithms [13].
Nevertheless, disk-diffusion assay offers many advantages over other methods: simplicity, low cost, the ability to test enormous numbers of microorganisms and antimicrobial agents, and the ease to interpret results provided. Moreover, several studies have demonstrated the great interest in patients who suffer from bacterial infection of an antibiotherapy based on the antibiogram of the causative agent [14]. This fact is due to the good correlation between the in vitro data and the in vivo evolution [12].
Before its standardization, disk-diffusion method has been already used to test posaconazole against filamentous fungi [15], micafungin against Aspergillus [16], and caspofungin against Aspergillus and Fusarium [17]. Currently, a standardized antifungal disk-diffusion approach is used to test non-dermatophyte filamentous fungi [18]. The culture medium, inoculum size and incubation conditions are mentioned in Table 1 [19].
The above-mentioned advantages of this method, mainly simplicity and low cost, have contributed to its common use for the antimicrobial screening of plant extracts, essential oils and other drugs [20], [21], [22], [23].
2.2. Antimicrobial gradient method (Etest)
The antimicrobial gradient method combines the principle of dilution methods with that of diffusion methods in order to determine the MIC value. It is based on the possibility of creating a concentration gradient of the antimicrobial agent tested in the agar medium. The Etest® (BioMérieux) is a commercial version of this technique. In the procedure, a strip impregnated with an increasing concentration gradient of the antimicrobial agent from one end to the other is deposited on the agar surface, previously inoculated with the microorganism tested.
This method is used for the MIC determination of antibiotics, antifungals and antimycobacterials [24]. MIC value is determined at the intersection of the strip and the growth inhibition ellipse. It is simple to implement; thus, it is routinely used to meet the demands of clinicians. However, Etest® strips cost about $2–3 each. Therefore, this approach becomes costly if numerous drugs are tested [11].
Several previous studies have shown a good correlation between the MIC values determined by Etest and those obtained by broth dilution or agar dilution method [25], [26], [27]. This technique can also be performed to investigate the antimicrobial interaction between two drugs [28]. To study the combined effect of two antibiotics, an Etest strip, impregnated with a first antibiotic, is placed on a pre-inoculated agar plate surface. After one hour, the strip is removed and replaced by another one impregnated with a second antibiotic. The synergy is detected by a decrease of the MIC of the combination by at least two dilutions compared to that of the most active antibiotic tested alone [29]. Also for the same purpose, the Etest strips can be deposited on the agar medium in a cross formation with a 90° angle at the intersection between the scales at the respective MICs for the microorganism tested [30]. Then, after incubation, the fractional inhibitory concentration index (FICI) can be calculated using the following formula:
and
Synergy was defined by FICI ≤0.5 and antagonism by FICI >4. The FICI between 0.5 and 1 was interpreted as addition and between 1 and 4 as indifference [31].
2.3. Other diffusion methods
Further diffusion methods are used in the microbiology research laboratories to screen extracts, fractions or pure substances for their antimicrobial potency or to investigate the antagonism between microorganisms. Among these methods, the most common are listed below.
2.3.1. Agar well diffusion method
Agar well diffusion method is widely used to evaluate the antimicrobial activity of plants or microbial extracts [32], [33]. Similarly to the procedure used in disk-diffusion method, the agar plate surface is inoculated by spreading a volume of the microbial inoculum over the entire agar surface. Then, a hole with a diameter of 6 to 8 mm is punched aseptically with a sterile cork borer or a tip, and a volume (20–100 µL) of the antimicrobial agent or extract solution at desired concentration is introduced into the well. Then, agar plates are incubated under suitable conditions depending upon the test microorganism. The antimicrobial agent diffuses in the agar medium and inhibits the growth of the microbial strain tested (Fig. 1B).
2.3.2. Agar plug diffusion method
Agar plug diffusion method is often used to highlight the antagonism between microorganisms [34], [35], and the procedure is similar to that used in the disk-diffusion method. It involves making an agar culture of the strain of interest on its appropriate culture medium by tight streaks on the plate surface. During their growth, microbial cells secrete molecules which diffuse in the agar medium. After incubation, an agar-plot or cylinder is cut aseptically with a sterile cork borer and deposited on the agar surface of another plate previously inoculated by the test microorganism. The substances diffuse from the plug to the agar medium. Then, the antimicrobial activity of the microbial secreted molecules is detected by the appearance of the inhibition zone around the agar plug (Fig. 1C).
2.3.3. Cross streak method
Cross streak method is used to rapidly screen microorganisms for antagonism [36]. The microbial strain of interest is seeded by a single streak in the center of the agar plate. After an incubation period depending upon the microbial strain, the plate is seeded with the microorganisms tested by single streak perpendicular to the central streak. After further incubation, the antimicrobial interactions are analyzed by observing the inhibition zone size.
2.3.4. Poisoned food method
Poisoned food method is mostly used to evaluate the antifungal effect against molds [37], [38], [39]. The antifungal agent or the extract is incorporated into the molten agar at a desired final concentration and mixed well. Then, the medium is poured into Petri dishes. After overnight pre-incubation, the inoculation can be done by a mycelia disc ranging from 2 to 5 mm, which is deposited in the center of the plate. After further incubation under suitable conditions for the fungal strain tested, the diameters of fungal growth in control and sample plates are measured, and the antifungal effect is estimated by the following formula:
Where Dc is the diameter of growth in control plate and Ds is the diameter of growth in the plate containing tested antifungal agent. Sporulation can be also compared to the control.
Generally, when standardization of the method used fails, the researcher must carry a positive control with known antimicrobial molecule to compare the results found and assert the experimental approach right.
3. Thin-layer chromatography (TLC)–bioautography
In 1946, Goodall and Levi [40] combined paper chromatography method (PC) with contact bioautography to detect different penicillins for their determination. Thereafter, Fischer and Lautner [41] introduced TLC in the same field. This technique combines TLC with both biological and chemical detection methods. Several works have been done on the screening of organic extracts, mainly plant extracts, for antibacterial and antifungal activity by TLC–bioautography [42], [43]. As shown below, three bioautographic techniques, i.e., agar diffusion, direct bioautography and agar-overlay assay, have been described for the investigation of antimicrobial compounds by this approach.
3.1. Agar diffusion
Also known as agar contact method, it is the least-employed one of the techniques. It involves the transfer by diffusion of the antimicrobial agent from the chromatogram (PC or TLC) to an agar plate previously inoculated with the microorganism tested. After some minutes or hours to allow diffusion, the chromatogram is removed and the agar plate is incubated. The growth inhibition zones appear in the places, where the antimicrobial compounds contact with the agar layer [44].
3.2. Direct bioautography
Direct bioautography is the most applied method among these three methods. The developed TLC plate is dipped into or sprayed with a microbial suspension. Then, bioautogram is incubated at 25 °C for 48 h under humid condition [45]. For visualization of the microbial growth, tetrazolium salts are frequently used. These salts undergo a conversion to corresponding intensely colored formazan by the dehydrogenases of living cells [46], [47]. p-Iodonitrotetrazolium violet is the most suitable detection reagent [44], [48]. These salts are sprayed onto the bioautogram, which is reincubated at 25 °C for 24 h [49] or at 37 °C for 3–4 h [5]. The Mueller Hinton Broth supplemented with agar has been recommended to give a medium sufficient fluid to allow a best adherence to the TLC plate and maintain appropriate humidity for bacterial growth [50].
Direct bioautography may be utilized with either fungi or bacteria. It is the easiest technique for the detection of antifungal substances, and also gives consistent results for spore-producing fungi such as Aspergillus, Penicillium and Cladosporium [51], [52]. For bacteria, Bacillus subtilis, Staphylococcus aureus and Escherichia coli strains are frequently used to identify antibacterial compounds [42], [53].
3.3. Agar overlay bioassay
Also known as immersion bioautography, it is a hybrid of the both previous methods. TLC plate is covered with a molten seeded agar medium. In order to allow a good diffusion of the tested compounds into the agar medium, the plates can be placed at low temperature for few hours before incubation. After incubation under suitable conditions depending upon the test microorganism, staining can be made with tetrazolium dye. Like direct bioautography, this method can be applied to all microorganisms such as Candida albicans [54] and molds [43]. It provides well-defined growth inhibition zones and is not sensitive to contamination [44].
Overall, TLC–bioautography is a simple, effective and inexpensive technique for the separation of a complex mixture, and at the same time, it localizes the active constituents on the TLC plate. Therefore, it can be performed both in sophisticated laboratories and small laboratories which only have access to a minimum of equipment [44]. Although having sophisticated on-line high performance liquid chromatography coupled bioassay, which is becoming increasingly popular as the method of choice for a final clean-up of extractive fractions to obtain pure compounds, the TLC–bioautography offers a rapid technique for the screening of a large number of samples for bioactivity and in the bioactivity-guided fractionation [45]. It can be used for detection of antimicrobials in environmental and food samples as well as for searching for new antimicrobial drugs.
4. Dilution methods
Dilution methods are the most appropriate ones for the determination of MIC values, since they offer the possibility to estimate the concentration of the tested antimicrobial agent in the agar (agar dilution) or broth medium (macrodilution or microdilution). Either broth or agar dilution method may be used to quantitatively measure the in vitro antimicrobial activity against bacteria and fungi. MIC value recorded is defined as the lowest concentration of the assayed antimicrobial agent that inhibits the visible growth of the microorganism tested, and it is usually expressed in µg/mL or mg/L. There are many approved guidelines for dilution antimicrobial susceptibility testing of fastidious or non-fastidious bacteria, yeast and filamentous fungi. The most recognized standards are provided by the CLSI and the European Committee on Antimicrobial Susceptibility Testing (EUCAST). As advised, these guidelines provide a uniform procedure for testing that is practical to perform in most clinical microbiology laboratories. The development of such methodologic standards does not guarantee the clinical relevance of such testing. Nevertheless, it does allow the bioassay to be performed in a standardized approach in order to evaluate the clinical relevance of results [55].
4.1. Broth dilution method
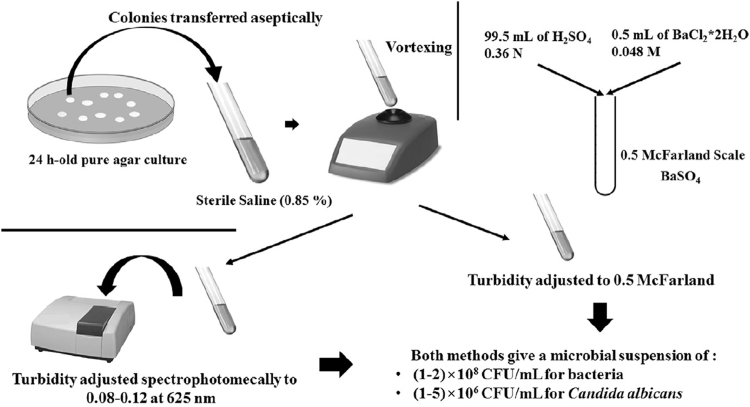
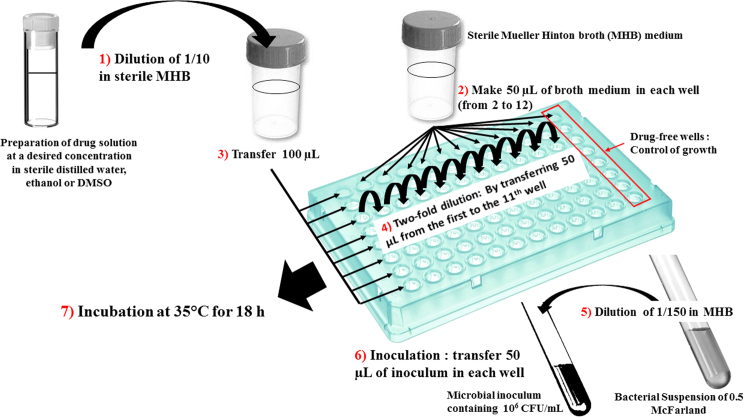
Broth micro- or macro-dilution is one of the most basic antimicrobial susceptibility testing methods. The procedure involves preparing two-fold dilutions of the antimicrobial agent (e.g. 1, 2, 4, 8, 16 and 32 µg/mL) in a liquid growth medium dispensed in tubes containing a minimum volume of 2 mL (macrodilution) or with smaller volumes using 96-well microtitration plate (microdilution) (Fig. 2). Then, each tube or well is inoculated with a microbial inoculum prepared in the same medium after dilution of standardized microbial suspension adjusted to 0.5 McFarland scale (Fig. 3). After well-mixing, the inoculated tubes or the 96-well microtitration plate are incubated (mostly without agitation) under suitable conditions depending upon the test microorganism (Table 1). The experimental methodology to perform accurately the microdilution is schematized in Fig. 4.
Fig. 2.
Broth microdilution method of plant extract against B. subtilis using resazurin as growth indicator.
Fig. 3.
0.5 McFarland microbial inoculum preparation by the direct colony suspension as recommended by CLSI guidelines.
Fig. 4.
Broth microdilution for antibacterial testing as recommended by CLSI protocol.
The MIC is the lowest concentration of antimicrobial agent that completely inhibits growth of the organism in tubes or microdilution wells as detected by the unaided eye [56]. Unlike microdilution method, the main disadvantages of the macrodilution method are the tedious, manual undertaking, risk of errors in the preparation of antimicrobial solutions for each test, and the comparatively large amount of reagents and space required [11]. Thus, the reproducibility and the economy of reagents and space that occurs due to the miniaturization of the test are the major advantages of the microdilution method. Nevertheless, the final result is significantly influenced by approach, which must be carefully controlled if reproducible results (intralaboratory and interlaboratory) are to be attained [56]. For the determination of MIC endpoint, viewing devices can facilitate reading microdilution tests and recording results with high ability to discern growth in the wells. Moreover, several colorimetric methods based on the use of dye reagents have been developed. Tetrazolium salts, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and 2,3-bis {2-methoxy-4-nitro-5-[(sulfenylamino) carbonyl]-2H-tetrazolium-hydroxide} (XTT), are often used in the MIC endpoint determination for both antifungal and antibacterial microdilution assays [57], [58], [59], [60]. The Alamar blue dye (resazurin), an effective growth indicator, can also be used for this purpose [61], [62], [63], [64].
It is well known that the inoculum size [65], the type of growth medium [66], the incubation time and the inoculum preparation method can influence MIC values [67], [68]. Therefore, broth dilution has been standardized by CLSI for testing bacteria that grow aerobically [56], yeast [69] and filamentous fungi [70]. The EUCAST broth dilution method is principally similar to that of CLSI with modifications usually concerning some of the test parameters such as inoculum preparation, inoculum size, and the MIC reading method which is visual in CLSI assay and spectrophotometric in EUCAST guidelines [71].
As regards to the conidium and spores forming fungi, the microdilution standardized by CLSI involves an inoculum of spores adjusted spectrophotometrically to 0.4×104–5×104 CFU/mL. However, in the EUCAST assay, the inoculum can be adjusted to (2–5)×105 CFU/mL by haemocytometer counting [72]. Numerous studies showed the importance of inoculum preparation by haemocytometer counting for reproducible and suitable preparation independent of the color and size of conidia [68], [73], [74].
The determination of minimum bactericidal concentration (MBC) or minimum fungicidal concentration (MFC), also known as the minimum lethal concentration (MLC), is the most common estimation of bactericidal or fungicidal activity. The MBC is defined as the lowest concentration of antimicrobial agent needed to kill 99.9% of the final inoculum after incubation for 24 h under a standardized set of conditions described in document M26-A [75], in which the MBC can be determined after broth macrodilution or microdilution by sub-culturing a sample from wells or tubes, yielding a negative microbial growth after incubation on the surface of non-selective agar plates to determine the number of surviving cells (CFU/mL) after 24 h of incubation. The bactericidal endpoint (MBC) has been subjectively defined as the lowest concentration, at which 99.9% of the final inoculum is killed [75]. MFC is also defined as the lowest concentration of the drug that yields 98%–99.9% killing effect as compared to the initial inoculum [71]. Several studies have been carried out for evaluation of different test parameters for determination of MFC of various drugs against Candida isolates [76], Aspergillus [77] and other molds [78].
4.2. Agar dilution method
The agar dilution method involves the incorporation of varying desired concentrations of the antimicrobial agent into an agar medium (molten agar medium), habitually using serial two-fold dilutions, followed by the inoculation of a defined microbial inoculum onto the agar plate surface. The MIC endpoint is recorded as the lowest concentration of antimicrobial agent that completely inhibits growth under suitable incubation conditions (Table 1).
This technique is suitable for both antibacterial and antifungal susceptibility testing. If multiple isolates are being tested against a single compound, or if the compound (or extract) tested masks the detection of microbial growth in the liquid medium with its coloring, agar dilution method is often preferred to broth dilution for the MIC determination. Nowadays, commercially produced inoculum replicators are available and can transfer between 32 and 60 different bacterial inocula to each agar plate. Agar dilution is often recommended as a standardized method for fastidious organisms [79] such as anaerobes and Helicobacter species. It has been also used for antifungal agent-drugs combinations against Candida sp., Aspergillus, Fusarium and dermatophytes [80], [81], [82], [83].
This method presents a good correlation with Etest mostly for antibacterial testing against both Gram-positive and Gram-negative bacteria. Moreover, category comparisons of agar dilution, disk-diffusion and broth microdilution methods give excellent results [25].
5. Time-kill test (time-kill curve)
Time-kill test is the most appropriate method for determining the bactericidal or fungicidal effect. It is a strong tool for obtaining information about the dynamic interaction between the antimicrobial agent and the microbial strain. The time-kill test reveals a time-dependent or a concentration-dependent antimicrobial effect [55].
For bacteria, this test has been well standardized and described in M26-A document of CLSI [75]. It is performed in broth culture medium using three tubes containing a bacterial suspension of 5×105 CFU/mL. The first and the second tubes contain the molecule or the extract tested usually at final concentrations of 0.25×MIC and 1×MIC, and the third one is considered as the growth control. The incubation is done under suitable conditions for varied time intervals (0, 4, 6, 8, 10, 12 and 24 h) [21], [55]. Then, the percentage of dead cells is calculated relatively to the growth control by determining the number of living cells (CFU/mL) of each tube using the agar plate count method. Generally, the bactericidal effect is obtained with a lethality percentage of 90% for 6 h, which is equivalent to 99.9% of lethality for 24 h [21]. In addition, this method can be used to determine synergism or antagonism between drugs (two or more) in combinations [28], [55]. Similarly, several antifungal substances were studied by this method [84], [85].
6. ATP bioluminescence assay
ATP bioluminescence assay is based on the capacity to measure adenosine triphosphate (ATP) produced by bacteria or fungi. As ATP is the chemical form of energy of all living cells, it is present in more or less a constant amount in a cell. Therefore, its quantification is used to estimate the microbial population in a sample. D-luciferin in the presence of the ATP undergoes conversion by luciferase to oxyluciferin that generates light. The quantity of the emitted light is measured by a luminometer and expressed as relative light unit (RLU) which can be converted into RLU/mole of ATP. Thus, there is a linear relationship between cell viability and luminescence measured.
Bioluminescence assay has a large range of applications, such as cytotoxicity test [86], in situ evaluation of the impact of biofilms in situ [87], and drug screening on Leishmania [88]. Moreover, It has been used by several authors for antibacterial testing [89], antimycobacterial testing [90], [91], antifungal against yeast [92] and molds [93]. The rapidity is the major advantage of this technique that provides quantitative results. Indeed it has been demonstrated that this technique can provide results in 3–5 days for antimycobacterial tests [90], [91] in comparison with the conventional dilution technique, which requires 3–4 weeks of incubation [90,91]. Bioluminescence assay also has the advantage of being used for antimicrobial testing in vivo or in situ [94].
7. Flow cytofluorometric method
Several years ago, the usefulness of flow cytometry for susceptibility testing of microorganisms was suggested. Thus, many authors investigated the antibacterial and antifungal activities of many drugs using this methodology [95], [96], [97], [98]. The rapid detection of damaged cells by this approach depends on the use of appropriate dyes staining [96], [99]. Therefore, propidium iodide (PI), a fluorescent and intercalating agent, is widely used as DNA stain [96]. Several studies were reported on the effectiveness of flow cytometer as a tool for antibacterial testing of essential oils against Listeria monocytogenes, using combined staining with PI for membrane damage evaluation and carboxyfluorescein diacetate (cFDA) for esterase activity detection [95]. Consequently, in addition to the lysed cells, three subpopulations (dead, viable and injured cells) can be clearly discriminated by this method. The injured cells are described as stressed cells exhibiting cellular components damages and subsequent impairment of reproductive growth [100]. Quantification of injured cells has an interesting outcome in food microbiology, as this subpopulation might be critical if cell recovery becomes possible, such as in temperature abuse conditions during food storage [95]. Indeed, flow cytofluorometric method allows the detection of antimicrobial resistance and estimates the impact of the molecule tested on the viability and cell damage of the tested microorganism [101]. Moreover, it gives reproducible results rapidly (2–6 h compared to 24–72 h for the microdilution method) [96]. However, the wide-spread use of this methodology for antimicrobial susceptibility testing currently appears unlikely due to the inaccessibility of the required flow cytometry equipment in various laboratories.
8. Conclusion
Currently, microbial infections have become an important clinical threat, with significant associated morbidity and mortality which is mainly due to the development of microbial resistance to the existing antimicrobial agents. Therefore, methods for antimicrobial susceptibility testing and discovering novel antimicrobial agents have been extensively used and continue to be developed. Some techniques were subjected to standardization by the CLSI and EUCAST, marking the major remarkable steps on this field. However, when testing natural products, some modifications of the standardized protocols are often requested. Thus, it is imperative to be careful not to change the basics of microbiology by diluting the culture media and using a highly concentrated inoculum. Moreover, if we consider the use of solvents that may affect the growth of the microorganism tested, we can say that making minor methodological adaptations to standardized protocols can be a solution to ensure accurate experimental approach and allow other researchers to compare results.
Footnotes
Peer review under responsibility of Xi’an Jiaotong University.
References
- 1.Mayers D.L., Lerner S.A., Ouelette M. vol. 2. Springer Dordrecht Heidelberg; London: 2009. (Antimicrobial Drug Resistance C: Clinical and Epidemiological Aspects). pp. 681–1347. [Google Scholar]
- 2.Guschin A., Ryzhikh P., Rumyantseva T. Treatment efficacy, treatment failures and selection of macrolide resistance in patients with high load of Mycoplasma genitalium during treatment of male urethritis with Josamycin. BMC Infect. Dis. 2015;15:1–7. doi: 10.1186/s12879-015-0781-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin I., Sawatzky P., Liu G. Antimicrobial resistance to Neisseria gonorrhoeae in Canada: 2009–2013. Can. Commun. Dis. Rep. 2015;41:40–41. doi: 10.14745/ccdr.v41i02a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berdy J. Bioactive microbial metabolites. J. Antibiot. 2005;58:1–26. doi: 10.1038/ja.2005.1. [DOI] [PubMed] [Google Scholar]
- 5.Runyoro D.K., Matee M.I., Ngassapa O.D. Screening of Tanzanian medicinal plants for anti-Candida activity. BMC Complement. Altern. Med. 2006;6:11. doi: 10.1186/1472-6882-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mabona U., Viljoen A., Shikanga E. Antimicrobial activity of Southern African medicinal plants with dermatological relevance: from an ethnopharmacological screening approach, to combination studies and the isolation of a bioactive compound. J. Ethnopharmacol. 2013;148:45–55. doi: 10.1016/j.jep.2013.03.056. [DOI] [PubMed] [Google Scholar]
- 7.Nazzaro F., Fratianni F., De Martino L. Effect of essential oils on pathogenic bacteria. Pharmaceuticals. 2013;6:1451–1474. doi: 10.3390/ph6121451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heatley N.G. A method for the assay of penicillin. Biochem. J. 1944;38:61–65. doi: 10.1042/bj0380061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CLSI, Performance Standards for Antimicrobial Disk Susceptibility Tests, Approved Standard, 7th ed., CLSI document M02-A11. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2012.
- 10.CLSI, Method for Antifungal Disk Diffusion Susceptibility Testing of Yeasts, Approved Guideline. CLSI document M44-A. CLSI, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898, USA, 2004.
- 11.Jorgensen J.H., Ferraro M.J. Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin. Infect. Dis. 2009;49:1749–1755. doi: 10.1086/647952. [DOI] [PubMed] [Google Scholar]
- 12.Caron F. Antimicrobial susceptibility testing : a four facets tool for the clinician. J. Des. Anti-Infect. 2012;14 186-174. [Google Scholar]
- 13.Nijs A., Cartuyvels R., Mewis A. Comparison and evaluation of Osiris and Sirscan 2000 antimicrobial susceptibility systems in the clinical microbiology laboratory. J. Clin. Microbiol. 2003;41:3627–3630. doi: 10.1128/JCM.41.8.3627-3630.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kreger B.E., Craven D.E., McCabe W.R. Gram-negative bacteremia. IV. Re-evaluation of clinical features and treatment in 612 patients. Am. J. Med. 1980;68:344–355. doi: 10.1016/0002-9343(80)90102-3. [DOI] [PubMed] [Google Scholar]
- 15.Lopez-Oviedo E., Aller A.I., Martín C. Evaluation of disk diffusion method for determining posaconazole susceptibility of filamentous fungi : comparison with CLSI broth microdilution method. Antimicrob. Agents Chemother. 2006;50:1108–1111. doi: 10.1128/AAC.50.3.1108-1111.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arikan S., Yurdakul P., Hascelik G. Comparison of two methods and three end points in determination of in vitro activity of Micafungin against Aspergillus spp. Antimicrob. Agents Chemother. 2003;47:2640–2643. doi: 10.1128/AAC.47.8.2640-2643.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arikan S., Paetznick V., Rex J.H. Comparative evaluation of disk diffusion with microdilution assay in susceptibility testing of caspofungin against Aspergillus and Fusarium isolates. Antimicrob. Agents Chemother. 2002;46:3084–3087. doi: 10.1128/AAC.46.9.3084-3087.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CLSI, Method for Antifungal Disk Diffusion Susceptibility Testing of Nondermatophyte Filamentous Fungi, Approved guideline, CLSI document M51-A. Clincal and Laboratory Standards Institute, 950 West Valley Roead, Suite 2500, Wayne, Pennsylvania 19087, USA, 2010.
- 19.Espinel-Ingroff A., Canton E., Fothergill A. Quality control guidelines for amphotericin B, itraconazole, posaconazole, and Voriconazole disk diffusion susceptibility tests with nonsupplemented Mueller–Hinton Agar (CLSI M51-A document) for nondermatophyte Filamentous Fungi. J. Clin. Microbiol. 2011;49:2568–2571. doi: 10.1128/JCM.00393-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fourati-Ben Fguira L., Fotso S., Ben Ameur-Mehdi R. Purification and structure elucidation of antifungal and antibacterial activities of newly isolated Streptomyces sp. strain US80. Res. Microbiol. 2005;156:341–347. doi: 10.1016/j.resmic.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Konaté K., Mavoungou J.F., Lepengué A.N. Antibacterial activity against β-lactamase producing Methicillin and Ampicillin-resistants Staphylococcus aureus: Fractional Inhibitory Concentration Index (FICI) determination. Ann. Clin. Microbiol. Antimicrob. 2012;11:18. doi: 10.1186/1476-0711-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Billerbeck V.G. Huiles Essentielles et Bactéries Résistantes aux Antibiotiques. Phytotherapie. 2007;5:249–253. [Google Scholar]
- 23.Das K., Tiwari R.K.S., Shrivastava D.K. Techniques for evaluation of medicinal plant products as antimicrobial agents: current methods and future trends. J. Med. Plants Res. 2010;4:104–111. [Google Scholar]
- 24.Hausdorfer J., Sompek E., Allerberger F. E-test for susceptibility testing of Mycobacterium tuberculosis. Int. J. Tuberc. Lung Dis. 1998;2:751–755. [PubMed] [Google Scholar]
- 25.Baker C.N., Stocker S.A., Culver D.H. Comparison of the E Test to agar dilution, broth microdilution, and agar diffusion susceptibility testing techniques by using a special challenge set of bacteria. J. Clin. Microbiol. 1991;29:533–538. doi: 10.1128/jcm.29.3.533-538.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berghaus L.J., Giguère S., Guldbech K. Comparison of Etest, disk diffusion, and broth macrodilution for in vitro susceptibility testing of Rhodococcus equi. J. Clin. Microbiol. 2015;53:314–318. doi: 10.1128/JCM.02673-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta P., Khare V., Kumar D. Comparative evaluation of disc diffusion and E-test with broth micro-dilution in susceptibility testing of amphotericin B, voriconazole and caspofungin against clinical Aspergillus isolates. J. Clin. Diagn. Res. 2015;9:2013–2016. doi: 10.7860/JCDR/2015/10467.5395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White R.L., Burgess D.S., Manduru M. Comparison of three different in vitro methods of detecting synergy : time-kill, checkerboard, and E test. Antimicrob. Agents Chemother. 1996;40:1914–1918. doi: 10.1128/aac.40.8.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Denes É., Hidri N. Synergie et Antagonisme en Antibiothérapie. Antibiotiques. 2009;11:106–115. [Google Scholar]
- 30.Gülmez D., Çakar A., Şener B. Comparison of different antimicrobial susceptibility testing methods for Stenotrophomonas maltophilia and results of synergy testing. J. Infect. Chemother. 2010;16:322–328. doi: 10.1007/s10156-010-0068-2. [DOI] [PubMed] [Google Scholar]
- 31.Bassolé I.H.N., Juliani H.R. Essential oils in combination and their antimicrobial properties. Molecules. 2012;17:3989–4006. doi: 10.3390/molecules17043989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Magaldi S., Mata-Essayag S., Hartung de Capriles C. Well diffusion for antifungal susceptibility testing. Int. J. Infect. Dis. 2004;8:39–45. doi: 10.1016/j.ijid.2003.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Valgas C., De Souza S.M., Smânia E.F.A. Screening methods to determine antibacterial activity of natural products. Braz. J. Microbiol. 2007;38:369–380. [Google Scholar]
- 34.Jiménez-Esquilín A.E., Roane T.M. Antifungal activities of actinomycete strains associated with high-altitude Sagebrush Rhizosphere. J. Ind. Microbiol. Biotechnol. 2005;32:378–381. doi: 10.1007/s10295-005-0007-x. [DOI] [PubMed] [Google Scholar]
- 35.Elleuch L., Shaaban M., Smaoui S. Bioactive secondary metabolites from a new terrestrial Streptomyces sp. TN262. Appl. Biochem. Biotechnol. 2010;162:579–593. doi: 10.1007/s12010-009-8808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lertcanawanichakul M., Sawangnop S. A comparison of two methods used for measuring the antagonistic activity of Bacillus species. Walailak J. Sci. Tech. 2008;5:161–171. [Google Scholar]
- 37.Ali-Shtayeh M.S., Ghdeib S.I. Abu. Antifungal activity of plant extracts against Dermatophytes. Mycoses. 1999;42:665–672. doi: 10.1046/j.1439-0507.1999.00499.x. [DOI] [PubMed] [Google Scholar]
- 38.Mukherjee P.K., Raghu K. Effect of temperature on antagonistic and biocontrol potential of Trichoderma sp. on Sclerotium rolfsii. Mycopathologia. 1997;139:151–155. doi: 10.1023/A:1006868009184. [DOI] [PubMed] [Google Scholar]
- 39.Kumar S.N., Nambisan B., Sundaresan A. Isolation and identification of antimicrobial secondary metabolites from Bacillus cereus associated with a Rhabditid Entomopathogenic Nematode. Ann. Microbiol. 2013;64:209–218. [Google Scholar]
- 40.Goodall R.R., Levi A.A. A microchromatographic method for the detection and approximate determination of the different penicillins in a mixture. Nature. 1946;158:675. doi: 10.1038/158675a0. [DOI] [PubMed] [Google Scholar]
- 41.Fischer R., Lautner H. On the paper chromatographic detection of penicillin preparations. Arch. Pharm. 1961;294:1–7. doi: 10.1002/ardp.19612940102. [DOI] [PubMed] [Google Scholar]
- 42.Horváth G., Jámbor N., Végh A. Antimicrobial activity of essential oils: the possibilities of TLC-bioautography. Flavour Fragr. J. 2010;25:178–182. [Google Scholar]
- 43.Mehrabani M., Kazemi A., Mousavi S.A. Ayatollahi. Evaluation of antifungal activities of Myrtus communis L. by bioautography method. Jundishapur J. Microbiol. 2013;6:1–7. [Google Scholar]
- 44.Marston A. Thin-layer chromatography with biological detection in phytochemistry. J. Chromatogr. A. 2011;1218:2676–2683. doi: 10.1016/j.chroma.2010.12.068. [DOI] [PubMed] [Google Scholar]
- 45.Dewanjee S., Gangopadhyay M., Bhattabharya N. Bioautography and its scope in the field of natural product chemistry. J. Pharm. Anal. 2015;5:75–84. doi: 10.1016/j.jpha.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choma I.M., Grzelak E.M. Bioautography detection in thin-layer chromatography. J. Chromatogr. A. 2011;1218:2684–2691. doi: 10.1016/j.chroma.2010.12.069. [DOI] [PubMed] [Google Scholar]
- 47.Grzelak E.M., Majer-Dziedzic B., Choma I.M. Development of a novel direct bioautography-thin-layer chromatography test: optimization of growth conditions for gram-negative bacteria, Escherichia coli. J. AOAC Int. 2011;94:1567–1572. doi: 10.5740/jaoac.10-385. [DOI] [PubMed] [Google Scholar]
- 48.Brantner A.H. Influence of various parameters on the evaluation of antibacterial compounds by the bioautographic TLC assay. Pharm. Pharmacol. Lett. 1997;7:152–154. [Google Scholar]
- 49.Silva M.T.G., Simas S.M., Batista T.G. Studies on antimicrobial activity, in vitro, of Physalis angulata L. (Solanaceae) fraction and Physalin B bringing out the importance of assay determination. Mem. Inst. Oswaldo Cruz. 2005;100:779–782. doi: 10.1590/s0074-02762005000700018. [DOI] [PubMed] [Google Scholar]
- 50.Shahat A.A., El-Barouty G., Hassan R.A. Chemical composition and antimicrobial activities of the essential oil from the seeds of Enterolobium contortisiliquum (leguminosae) J. Environ. Sci. Health. B. 2008;43:519–525. doi: 10.1080/03601230802174714. [DOI] [PubMed] [Google Scholar]
- 51.Suleiman M., McGaw L., Naidoo V. Detection of antimicrobial compounds by bioautography of different extracts of leaves of selected South African tree species. Afr. J. Tradit. Complement. Altern. Med. 2010;7:64–78. doi: 10.4314/ajtcam.v7i1.57269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Homans A., Fuchs A. Direct bioautography on thin-layer chromatograms as a method for detecting fungitoxic substances. J. Chromatogr. A. 1970;51:327–329. doi: 10.1016/s0021-9673(01)96877-3. [DOI] [PubMed] [Google Scholar]
- 53.Hamburger M.O., Cordell G.A. A direct bioautographic TLC assay for compounds possessing antibacterial activity. J. Nat. Prod. 1987;50:19–22. doi: 10.1021/np50049a003. [DOI] [PubMed] [Google Scholar]
- 54.Balouiri M., Bouhdid S., Harki E. Antifungal activity of Bacillus spp. isolated from Calotropis procera AIT. Rhizosphere against Candida albicans. Asian J. Pham. Clin. Res. 2015;8:213–217. [Google Scholar]
- 55.Pfaller M.A., Sheehan D.J., Rex J.H. Determination of fungicidal activities against yeasts and molds: lessons learned from bactericidal testing and the need for standardization. Clin. Microbiol. Rev. 2004;17:268–280. doi: 10.1128/CMR.17.2.268-280.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.CLSI, Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically, Approved Standard, 9th ed., CLSI document M07-A9. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2012
- 57.Al-Bakri A.G., Afifi F.U. Evaluation of antimicrobial activity of selected plant extracts by rapid XTT colorimetry and bacterial enumeration. J. Microbiol. Methods. 2007;68:19–25. doi: 10.1016/j.mimet.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 58.Liang H., Xing Y., Chen J. Antimicrobial activities of endophytic fungi isolated from Ophiopogon japonicus (Liliaceae) BMC Complement. Altern. Med. 2012;12:238. doi: 10.1186/1472-6882-12-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Monteiro M.C., de la Cruz M., Cantizani J. A new approach to drug discovery: high-throughput screening of microbial natural extracts against Aspergillus fumigatus using resazurin. J. Biomol. Screen. 2012;17:524–529. doi: 10.1177/1087057111433459. [DOI] [PubMed] [Google Scholar]
- 60.Kuhn D.M., Balkis M., Chandra J. Uses and limitations of the XTT assay in studies of Candida growth and metabolism. J. Clin. Microbiol. 2003;41:506–508. doi: 10.1128/JCM.41.1.506-508.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reis R.S., Neves I., Lourenço S.L.S. Comparison of flow cytometric and alamar blue tests with the proportional method for testing susceptibility of Mycobacterium tuberculosis to Rifampin and Isoniazid. J. Clin. Microbiol. 2004;42:2247–2248. doi: 10.1128/JCM.42.5.2247-2248.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ouedrhiri W., Bouhdid S., Balouiri M. Chemical composition of Citrus aurantium L. Leaves and zest essential oils, their antioxidant, antibacterial single and combined effects. J. Chem. Pharm. Res. 2015;7:78–84. [Google Scholar]
- 63.Bouhdid S., Abrini J., Zhiri A. Investigation of functional and morphological changes in Pseudomonas aeruginosa and Staphylococcus aureus cells induced by Origanum compactum essential oil. J. Appl. Microbiol. 2009;106:1558–1568. doi: 10.1111/j.1365-2672.2008.04124.x. [DOI] [PubMed] [Google Scholar]
- 64.Castilho A.L., Caleffi-Ferracioli K.R., Canezin P.H. Detection of drug susceptibility in rapidly growing mycobacteria by Resazurin broth microdilution assay. J. Microbiol. Methods. 2015;111:119–121. doi: 10.1016/j.mimet.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 65.Gehrt A., Peter J., Pizzo P.A. Effect of increasing inoculum sizes of pathogenic filamentous fungi on MICs of antifungal agents by Broth microdilution method. J. Clin. Microbiol. 1995;33:1302–1307. doi: 10.1128/jcm.33.5.1302-1307.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Meletiadis J., Meis J.F.G.M., Mouton J.W. Analysis of growth characteristics of filamentous fungi in different nutrient media. J. Clin. Microbiol. 2001;39:478–484. doi: 10.1128/JCM.39.2.478-484.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gomez-Lopez A., Aberkane A., Petrikkou E. Analysis of the influence of tween concentration, inoculum size, assay medium, and reading time on susceptibility testing of Aspergillus spp. J. Clin. Microbiol. 2005;43:1251–1255. doi: 10.1128/JCM.43.3.1251-1255.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rodriguez-Tudela J.L., Chryssanthou E., Petrikkou E. Interlaboratory evaluation of hematocytometer method of inoculum preparation for testing antifungal susceptibilities of filamentous fungi. J. Clin. Microbiol. 2003;41:5236–5237. doi: 10.1128/JCM.41.11.5236-5237.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.CLSI, Reference Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, Approved Standard, 2nd ed., NCCLS document M27-A2. CLSI, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898, USA, 2002.
- 70.CLSI, Reference Method for Broth Dilution Antifungal Susceptibility Testing Filamentous Fungi, Approved Standard, 2nd ed., CLSI document M38-A2, 950 West Valley Roadn Suite 2500,Wayne, Pennsylvania 19087, USA, 2008.
- 71.Arikan S. Current status of antifungal susceptibility testing methods. Med. Mycol. 2007;45:569–587. doi: 10.1080/13693780701436794. [DOI] [PubMed] [Google Scholar]
- 72.Lass-Flörl C., Cuenca-Estrella M., Denning D.W. Antifungal susceptibility testing in Aspergillus spp. according to EUCAST methodology. Med. Mycol. 2006;44:319–325. doi: 10.1080/13693780600779401. [DOI] [PubMed] [Google Scholar]
- 73.Petrikkou E., Rodri J.L., Gómez A. Inoculum standardization for antifungal susceptibility testing of filamentous fungi pathogenic for humans. J. Clin. Microbiol. 2001;39:1345–1347. doi: 10.1128/JCM.39.4.1345-1347.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aberkane A., Cuenca-Estrella M., Gomez-Lopez A. Comparative evaluation of two different methods of inoculum preparation for antifungal susceptibility testing of filamentous fungi. J. Antimicrob. Chemother. 2002;50:719–722. doi: 10.1093/jac/dkf187. [DOI] [PubMed] [Google Scholar]
- 75.CLSI, Methods for Determining Bactericidal Activity of Antimicrobial Agents. Approved Guideline, CLSI document M26-A. Clinical and Laboratory Standards Institute, 950 West Valley Roadn Suite 2500,Wayne, Pennsylvania 19087, USA, 1998.
- 76.Cantón E., Pemán J., Viudes A. Minimum fungicidal concentrations of amphotericin B for bloodstream Candida species. Diagn. Microbiol. Infect. Dis. 2003;45:203–206. doi: 10.1016/s0732-8893(02)00525-4. [DOI] [PubMed] [Google Scholar]
- 77.Espinel-Ingroff A., Fothergill A., Peter J. Testing conditions for determination of minimum fungicidal concentrations of new and established antifungal agents for Aspergillus spp.: NCCLS collaborative study. J. Clin. Microbiol. 2002;40:3204–3208. doi: 10.1128/JCM.40.9.3204-3208.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Espinel-Ingroff A., Chaturvedi V., Fothergill A. Optimal testing conditions for determining MICs and minimum fungicidal concentrations of new and established antifungal agents for uncommon molds: NCCLS collaborative study. J. Clin. Microbiol. 2002;40:3776–3781. doi: 10.1128/JCM.40.10.3776-3781.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.CLSI, Methods for Antimicrobial Dilution and Disk Susceptibility of Infrequently Isolated or Fastidious Bacteria, Approved Guideline, 2nd. ed., CLSI document M45-A2. Clinical and Laboratory Standards Institute, 950 West Valley Roadn Suite 2500,Wayne, Pennsylvania 19087, USA, 2010.
- 80.Menon T., Umamaheswari K., Kumarasamy N. Efficacy of fluconazole and itraconazole in the treatment of oral candidiasis in HIV patients. Acta Trop. 2001;80:151–154. doi: 10.1016/s0001-706x(01)00170-x. [DOI] [PubMed] [Google Scholar]
- 81.Imhof A., Balajee S.A., Mar K.A. New methods to assess susceptibilities of Aspergillus isolates to caspofungin. J. Clin. Microbiol. 2003;41:5683–5688. doi: 10.1128/JCM.41.12.5683-5688.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mock M., Monod M., Baudraz-Rosselet F. Tinea capitis dermatophytes: susceptibility to antifungal drugs tested in vitro and in vivo. Dermatology. 1998;197:361–367. doi: 10.1159/000018032. [DOI] [PubMed] [Google Scholar]
- 83.Speeleveld E., Gordts B., Van Landuyt H.W. Susceptibility of clinical isolates of Fusarium to antifungal drugs. Mycoses. 1996;39:37–40. doi: 10.1111/j.1439-0507.1996.tb00081.x. [DOI] [PubMed] [Google Scholar]
- 84.Clancy C.J., Huang H., Cheng S. Characterizing the effects of caspofungin on Candida albicans, Candida parapsilosis, and Candida glabrata isolates by simultaneous time-kill and postantifungal-effect experiments. Antimicrob. Agents Chemother. 2006;50:2569–2572. doi: 10.1128/AAC.00291-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Klepser M.E., Ernst E.J., Lewis R.E. Influence of test conditions on antifungal time-kill curve results: proposal for standardized methods. Antimicrob. Agents Chemother. 1998;42:1207–1212. doi: 10.1128/aac.42.5.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Crouch S.P., Kozlowski R., Slater K.J. The use of ATP Bioluminescence as a measure of cell proliferation and cytotoxicity. J. Immunol. Methods. 1993;160:81–88. doi: 10.1016/0022-1759(93)90011-u. [DOI] [PubMed] [Google Scholar]
- 87.Bozorg A., Gates I.D., Sen, Using A. Bacterial bioluminescence to evaluate the impact of biofilm on porous media hydraulic properties. J. Microbiol. Methods. 2015;109:84–92. doi: 10.1016/j.mimet.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 88.Paloque L., Vidal N., Casanova M. A new, rapid and sensitive bioluminescence assay for drug screening on Leishmania. J. Microbiol. Methods. 2013;95:320–323. doi: 10.1016/j.mimet.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 89.Finger S., Wiegand C., Buschmann H.J. Antibacterial properties of cyclodextrin–antiseptics–complexes determined by microplate laser nephelometry and ATP bioluminescence assay. Int. J. Pharm. 2013;452:188–193. doi: 10.1016/j.ijpharm.2013.04.080. [DOI] [PubMed] [Google Scholar]
- 90.Andreu N., Fletcher T., Krishnan N. Rapid measurement of antituberculosis drug activity in vitro and in macrophages using bioluminescence. J. Antimicrob. Chemother. 2012;67:404–414. doi: 10.1093/jac/dkr472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Beckers B., Lang H.R., Schimke D. Evaluation of a bioluminescence assay for rapid antimicrobial susceptibility testing of mycobacteria. Eur. J. Clin. Microbiol. 1985;4:556–561. doi: 10.1007/BF02013394. [DOI] [PubMed] [Google Scholar]
- 92.Finger S., Wiegand C., Buschmann H. Antimicrobial properties of cyclodextrin–antiseptics-complexes determined by microplate laser nephelometry and ATP bioluminescence assay. Int. J. Pharm. 2012;436:851–856. doi: 10.1016/j.ijpharm.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 93.Galiger C., Brock M., Jouvion G. Assessment of efficacy of antifungals against Aspergillus fumigatus : value of real-time bioluminescence imaging. Antimicrob. Agents Chemother. 2013;57:3046–3059. doi: 10.1128/AAC.01660-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vojtek L., Dobes P., Buyukguzel E. Bioluminescent assay for evaluating antimicrobial activity in insect haemolymph. Eur. J. Entomol. 2014;111:335–340. [Google Scholar]
- 95.Paparella A., Taccogna L., Aguzzi I. Flow cytometric assessment of the antimicrobial activity of essential oils against Listeria monocytogenes. Food Control. 2008;19:1174–1182. [Google Scholar]
- 96.Ramani R., Chaturvedi V. Flow cytometry antifungal susceptibility testing of pathogenic yeasts other than Candida albicans and comparison with the NCCLS broth microdilution test. Antimicrob. Agents Chemother. 2000;44:2752–2758. doi: 10.1128/aac.44.10.2752-2758.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Green L.J., Marder P., Mann L.L. LY303366 exhibits rapid and potent fungicidal activity in flow cytometric assays of yeast viability. Antimicrob. Agents Chemother. 1999;43:830–835. doi: 10.1128/aac.43.4.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Green L., Petersen B., Steimel L. Rapid determination of antifungal activity by flow cytometry. J. Clin. Microbiol. 1994;32:1088–1091. doi: 10.1128/jcm.32.4.1088-1091.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ramani R., Ramani A., Wong S.J. Rapid flow cytometric susceptibility testing of Candida albicans. J. Clin. Microbiol. 1997;35:2320–2324. doi: 10.1128/jcm.35.9.2320-2324.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yousef A.E., Courtney P.D. Basics of stress adaptation and implications in new-generation foods. In: Yousef A.E., Juneja V.K., editors. Microbial Stress Adaptation and Food Safety. CRC Press; Washington DC: 2003. pp. 2–8. [Google Scholar]
- 101.Tang Y.W., Stratton C.W. Springer; New York Heidelberg Dordrecht, London: 2013. Advanced Techniques in Diagnostic Microbiology, 2nd ed. pp. 937. [Google Scholar]