Abstract
Horizontal transfer of antibiotic resistance determinants contributes to dissemination of antibiotic resistance. Such transfer of resistance genes within the human gut has been documented in some in vivo studies. The present study investigated seven bla CTX-M-1-carrying Escherichia coli isolates from three consecutive faecal samples collected from one cystic fibrosis patient in a nine-months period, by analysing whole genome sequencing data. The analyses showed that the seven E. coli isolates represented three genetically diverse strains. All isolates contained bla CTX-M-1-carrying Incl1 plasmids that shared a common 101 kb backbone differing by only four SNPs. The plasmids harboured by the three different E. coli strains varied within limited regions suggestive of recombination events, according to the phylogenetic topology of the genomes of the isolates harbouring them. The findings strongly suggest that horizontal transfer of a bla CTX-M-1-carrying plasmid had occurred within the patient´s gut. The study illustrates the within-host diversity of faecally carried resistant E. coli isolates and highlights the value of collecting multiple bacterial colonies from longitudinally collected samples to assess faecal carriage of resistant enterobacteria. The clustering of the plasmids with the corresponding E. coli strains carrying them indicates that the plasmids appear to have adapted to their respective E. coli hosts.
Introduction
During the last 10 to 15 years a global epidemic of extended-spectrum beta-lactamase (ESBL)-producing enterobacteria has emerged1. The CTX-M enzymes constitute by far the most common group of ESBLs1–3. The bla CTX-M genes encoding the CTX-M enzymes are probably originally mobilized from the chromosomes of various species of the Kluyvera genus to plasmids well adapted particularly to Escherichia coli 4. Spread of CTX-M enzymes has to some extent occurred through dissemination of successful, virulent clones, e.g. E. coli ST131. According to Woerther et al. a huge diversity of bla CTX-M-carrying E. coli strains is present in the community with each carrier mostly harbouring his/her own strain that may disseminate in the immediate surroundings1. Previous studies of faecal carriage of ESBL-producing E. coli have demonstrated dissemination between household members5,6. Molecular characterization of the bacterial isolates revealed clonally related E. coli strains carrying the same ESBL genotype, but also genetically different strains carrying the same ESBL genotype5. Other recent studies have shown extensive within-host diversity in faecally carried ESBL-producing E. coli isolates with identical bla CTX-M variants detected in genetically different E. coli isolates from the same individual7,8. This is suggestive of transfer of resistance genes between different strains of E. coli. The gut of humans and animals is the main reservoir of E. coli and other enterobacteria and may constitute a suitable environment for horizontal gene transfer (HGT)9. The large number of microorganisms, more than 1013 bacterial cells residing in the gut10, and probably also biofilm formation contribute to high bacterial density and direct contact between bacterial cells, thus facilitating HGT within the gastrointestinal tract9,11. A common mechanism of HGT is by conjugation with plasmids acting as vectors. Numerous studies have documented conjugational transfer of resistance genes between bacteria in vitro and also in some animal models12–14. However, not many in vivo studies have actually proven HGT of resistance determinants within the human gut15–18.
Whole genome sequencing (WGS) of bacteria offers vast opportunities for detailed characterisation of bacterial isolates, including detection and classification of plasmids19,20. However, assembly of plasmids from WGS data generated by high-throughput sequencing technologies that produce short reads (≈100–300 bp) might be challenging20. Not many studies have so far used in silico plasmid extraction from bacterial WGS data to study in vivo HGT in the human gut21,22.
In a study of faecal carriage of resistant enterobacteria in children23 we identified the plasmid-carried bla CTX-M-1 in seven different E. coli isolates from three consecutive faecal samples from one patient. The seven E. coli isolates represented three different phenotypes according to their trimethoprim-sulfamethoxazole and tetracycline susceptibility patterns. The aim of this study was to assess the genetic relationship between these seven E. coli isolates and to further characterise their bla CTX-M-1-carrying plasmids by reconstructing them in silico from WGS data. Specifically, we wanted to explore whether bla CTX-M-1 was located on a common plasmid in all the isolates.
Methods
Ethics
The study was approved by the Regional Committee for Medical and Health Research Ethics – South East (“REK sør-øst”)(reference number 581–06–03092) and the study was conducted in accordance with the regulations from the committee and the principles of the Declaration of Helsinki. Written, informed consent was obtained from the participating child´s parents.
Collection and characteristics of the E. coli isolates and patient information
In a study of the prevalence of resistant intestinal Enterobacteriaceae in children23, one of the participants, a child with cystic fibrosis, submitted three faecal samples with time intervals of six months and three months, respectively. The faecal samples were analysed with a Direct MIC-gradient Strip Method to detect resistant Enterobacteriaceae 24. Two phenotypically different ESBL-producing E. coli isolates were detected both in sample one and sample two: one of the ESBL-producing E. coli isolates was resistant to trimethoprim-sulfamethoxazole, whereas the other was resistant to both trimethoprim-sulfamethoxazole and tetracycline. In sample three, a third ESBL-producing E. coli phenotype, susceptible to all non-beta-lactam antibiotics, was detected in addition to the two other phenotypes. For all of the three samples, one of each ESBL-producing E. coli phenotype was selected for WGS, in total seven isolates as shown in Table 1.
Table 1.
Seven extended-spectrum beta-lactamase (ESBL)-producing E. coli isolates from three faecal samples collected from one patient at three different time points. Additional phenotypic resistance detected in each isolate is shown in the parentheses.
| Faecal samples | |||
|---|---|---|---|
| Sample 1 (time 0) | Sample 2 (after 6 months) | Sample 3 (after 9 months) | |
| E. coli phenotypes isolated | 433-tz (SXT resistant) | 432-AT128 (SXT resistant) | 431-Ts-o (SXT resistant) |
| 433-at (SXT and TET resistant) | 432-CT-a-32 (SXT and TET resistant) | 431-Ts-lys (SXT and TET resistant) | |
| 431-Tz (No additional resistance) | |||
SXT, trimethoprim-sulfamethoxazole; TET, tetracycline.
The patient had been diagnosed with cystic fibrosis at Oslo University Hospital three years prior to the first faecal sample. Her airways were chronically colonized with Haemophilus influenzae and Staphylococcus aureus. In addition, Stenotrophomonas maltophilia and Achromobacter xylosoxidans, but not Pseudomonas aeruginosa, had been cultured sporadically. At CF diagnosis she was treated with ceftazidime, tobramycin and cloxacillin intravenously for 14 days. After this she had not been treated with any third-generation cephalosprins or carbapenems, but she had received repeated oral antibiotic courses, mainly trimethoprim-sulfamethoxazole, but also cephalexin, cloxacillin and amoxicillin. She also received several courses with these antibiotics during the study period.
Whole genome sequencing (WGS)
Genomic DNA was extracted using MagNa Pure 96 (Roche Diagnostics, Mannheim, Germany) according to the manufacturer’s instructions. DNA concentrations were measured using a Qubit fluorometer (Thermo Fisher Scientific, MA, USA) to determine DNA input. Isolates 431-Ts-o, 431-Ts-lys, 431-Tz, 433-tz, 433-at: Genomic libraries were prepared using KAPA HyperPlus Library Preparation Kit (Kapa Biosystems, MA, USA) and WGS was performed on an Illumina MiSeq platform using v2 reagent kits generating 2 × 250 bp paired-end reads (Illumina, San Diego, CA, USA) at the Norwegian Institute of Public Health, Oslo, Norway. Isolates 432-AT128 and 432-CT-a-32: Genomic libraries were prepared and WGS was performed on an Illumina HiSeq 2500 platform generating 2 × 125 bp paired-end reads at BGI Tech Solutions Co., Limited, Hong Kong.
Assembly of genomes and blaCTX-M-1-carrying plasmids
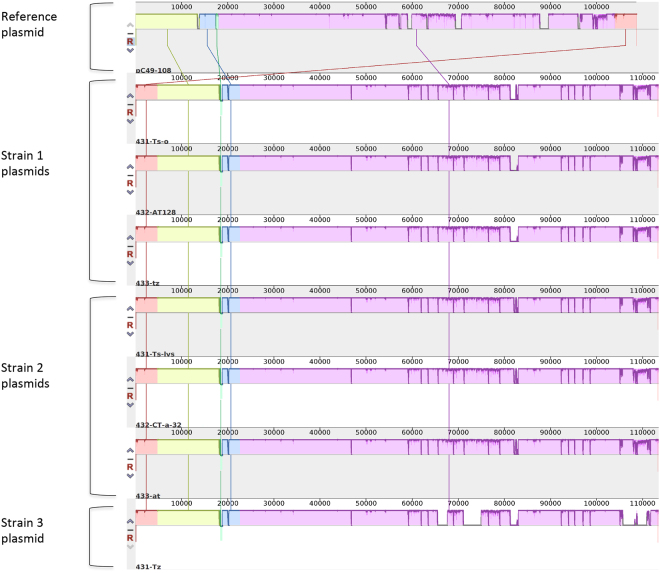
The sequenced reads were trimmed for adapter sequences using trimmomatic25 and subsequently quality corrected using BayesHammer26. Whole genome de novo assembly was carried out using SPAdes v 3.9.027, and PlasmidSPAdes28 was used to assemble and extract putative plasmid sequences from the sequenced reads (Fig. 1A). PlasmidSPAdes was run on all isolates, and the predicted plasmid contigs from the isolate having the largest contigs (isolate 431-Ts-lys), i.e. the largest contiguous predicted plasmid contigs also containing bla CTX-M-1, were BLASTed29 against the NCBI databases restricted to bacterial plasmids (Fig. 1B). The plasmid with the best hit (pC49–108, Accession number KJ484638) in terms of bit score and size was used as a reference for a subsequent plasmid assembly. This assembly was performed as follows: first, the plasmid-sequence of pC49–108 was used as a reference for the assembly of the putative plasmid sequences from each of the seven isolates. Second, each of the resulting assembled plasmid sequences were further used as templates of which contigs from the corresponding de novo assembled E. coli genomic sequences were sorted against, using CONTIGuator v 2.730 (Fig. 1C). Contigs were assessed using the Artemis Comparison Tools31 included in the CONTIGuator package. The contigs with a 99% nucleotide identity as well as they consisted of more than 10% of reference plasmid DNA were retained as putative plasmid contigs while those falling short of the criteria were excluded. This procedure was carried out to fill in genetic regions not found in the reference plasmid. The contig-assembled plasmid was in turn used as a reference to which reads from each E. coli isolate was mapped using both BowTie2 v 2.1.032 and SAMtools v 1.3.133 (Fig. 1D). Assembly details of the E. coli genomes can be found in Supplementary Table S1.
Figure 1.
The plasmid assembly method. Short reads from each isolate are de novo assembled using SPAdes, and putative plasmid contigs are assembled and extracted by plasmidSPAdes (A). The putative plasmid contigs are subsequently queried against the NCBI plasmid database and if suitable matches are detected, the best hit is used as a reference sequence (B). The assembled plasmid sequences obtained from mapping to the reference plasmid is then used as templates for which contigs from the corresponding de novo assembled E. coli genomic sequences are sorted against, using CONTIGuator2 (C). The contigs that have a 99% nucleotide identity as well as consisting of more than 10% of reference plasmid DNA are retained as putative plasmid contigs while those falling short of the criteria are excluded. Finally, the newly assembled plasmid contigs are used as a reference to which all the original short reads from each E. coli isolate are mapped using BowTie2 (D).
Detection of resistance genes and typing of the E. coli isolates
The assembled E. coli genomes were submitted to the web-based ResFinder service v 2.1 (Center for Genomic Epidemiology, DTU, Denmark) to identify acquired resistance genes34. Hits were accepted for matches with ≥99% nucleotide identity between the resistance gene in the database and the corresponding sequence in the genome, and the length of the query sequence covering ≥95% of the length of the gene in the database. Multilocus sequence typing (MLST) and serotyping of the E. coli isolates were performed in silico from the assembled genomes by MLST v 1.8 and SerotypeFinder v 1.1 (Center for Genomic Epidemiology, DTU, Denmark), respectively, using default settings35,36.
Phylogenetic analyses of the E. coli genomes
After de novo assembly, phylogenetic analyses were performed on the single nucleotide polymorphisms (SNPs) from the complete E. coli genome sequences with the putative plasmid sequences removed. The plasmid sequences were excluded by mapping all reads from each E. coli genome to the E. coli K-12 strain MG1655 chromosome (Accession number NC_000913.3) with BowTie 2 v 2.1.032. Further, SNP calling was carried out using parSNP v 1.2 from the Harvesttools suite37 by extracting the core genome, containing both coding and non-coding regions, and removal of putative recombinant regions with Gubbins v 2.238. The phylogenetic analysis was performed using the RAxML maximum likelihood estimation program v 8.2.439. The tree was bootstrapped 500 times and the nucleotide substitution matrix (GTR) was found with PhyML v 3.040 and the R-package ‘ape’41 (https://www.R-project.org/). The tree was obtained using FigTree v 1.4.2 (http://tree.bio.ed.ac.uk/software/figtree/).
Characterization and comparison of the plasmids
All putative plasmid sequences within the genome of each isolate were also identified with PlasmidFinder v 1.3 (Center for Genomic Epidemiology, DTU, Denmark)19 using the Enterobacteriaceae database with the detection threshold set to > 95% sequence identity. Characterization of the assembled bla CTX-M-1-containing plasmids by incompatibility (Inc) group and plasmid MLST (pMLST) was performed with PlasmidFinder v 1.3 and pMLST v 1.4 (Center for Genomic Epidemiology, DTU, Denmark), respectively19. SNP calling of the assembled bla CTX-M-1-containing plasmids was performed with BowTie2 v 2.1.032 and SAMtools33, but the low number of SNPs (four) did not allow for a reliable phylogenetic analysis and was therefore omitted. The core backbone of the plasmids was determined with both Roary v 3.8.042 (default settings) and ParSNP (fraction of coding/non-coding DNA shared amongst all plasmids). The gene presence-absence heat map of the plasmids was created with R v 3.3.3 from the Roary output and based on complete linkage hierarchical clustering with Euclidean distance. Comparison of all the assembled bla CTX-M-1-containing plasmids was performed and visualized using MAUVE43. All the plasmids were annotated using Prokka v 1.1144. Annotation of the plasmids was additionally improved by BLASTing of “hypothetical proteins” to NCBI databases.
Data availability
The E. coli genome short reads that were generated and analysed in this work are deposited to the European Nucleotide Archive (ENA), and the accession numbers of the seven genomes are shown in Supplementary Table S1. The fasta-files containing the seven assembled plasmid sequences are also available in the Supplementary Information.
Results
The E. coli isolates
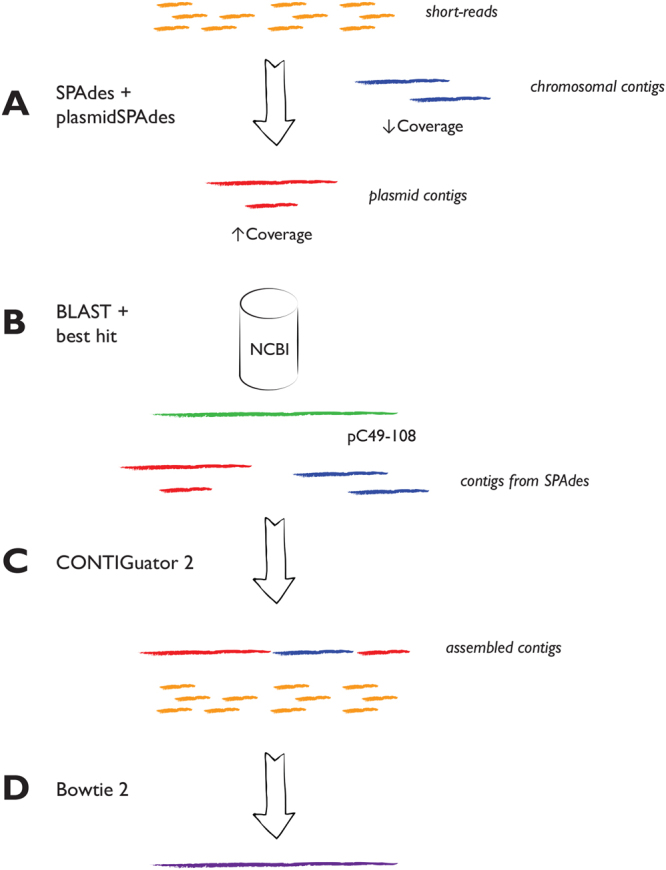
Analyses of the assembled E. coli genomes with respect to acquired resistance genes by ResFinder (Center for Genetic Epidemiology, DTU) detected bla CTX-M-1 in all seven E. coli isolates. The SNP-based phylogenetic tree presented in Fig. 2 shows that the seven isolates represent three different strains; strain 1: isolates 433-tz, 432-AT128, 431-Ts-o; strain 2: isolates 433-at, 432-CT-a-32, 431-Ts-lys; strain 3: isolate 431-Tz. The results of in silico typing (MLST and serotyping) of each isolate are shown in Table 2.
Figure 2.
Maximum Likelihood based phylogenetic analysis of core genome SNPs from seven bla CTX-M-1-containing E. coli isolates, with the reference E. coli K-12 strain MG1655 (Accession number NC_000913.3) included as out-group. Branch numbers designate bootstrap support.
Table 2.
Characteristics of seven E. coli isolates from faecal samples collected from one cystic fibrosis patient at three different time points.
| Isolate-ID | Sample time | Phenotypic resistance | Strain | Sequence type (MLST) | Serotype | Resistance genes* | Plasmid replicons |
|---|---|---|---|---|---|---|---|
| 433-tz | Study start | 3.generation cephalosporins, SXT | 1 | ST1640 | O124:H25 | bla CTX-M-1, dfrA14, dfrA17, sul2 | Incl1, IncFII (pRSB107), IncQ1, IncFIA, IncFIB (AP001918), Col8282, ColpVC, IncFII |
| 432-AT128 | 6 months | 3.generation cephalosporins, SXT | 1 | ST1640 | O124:H25 | bla CTX-M-1, dfrA14, dfrA17, sul2 | Incl1, IncFII (pRSB107), IncQ1, IncFIA, IncFIB (AP001918), Col8282, ColpVC |
| 431-Ts-o | 9 months | 3.generation cephalosporins, SXT | 1 | ST1640 | O124:H25 | bla CTX-M-1, dfrA14, dfrA17, sul2 | Incl1, IncFII (pRSB107), IncQ1, IncFIA, IncFIB (AP001918), Col8282, ColpVC |
| 433-at | Study start | 3.generation cephalosporins, SXT, TET | 2 | ST6331 | O82:H21 | bla CTX-M-1, dfrA17, sul1, sul2, tetA | Incl1, IncFIA, Col (MG828) |
| 432-CT-a-32 | 6 months | 3.generation cephalosporins, SXT, TET | 2 | ST6331 | O82:H21 | bla CTX-M-1, dfrA17, sul1, sul2, tetA | Incl1, IncFIA, Col (MG828) |
| 431-Ts-lys | 9 months | 3.generation cephalosporins, SXT, TET | 2 | ST6331 | O82:H21 | bla CTX-M-1, dfrA17, sul1, sul2, tetA | Incl1, IncFIA, Col (MG828) |
| 431-tz | 9 months | 3.generation cephalosporins | 3 | ST2144 | O166:H49 | bla CTX-M-1 | Incl1 |
SXT, trimethoprim-sulfamethoxazole; TET, tetracycline.
*Resistance genes detected by ResFinder (Centre for Genomic Epidemiology, DTU, Denmark) that explain the observed phenotypic resistance to 3. generation cephalosporins, trimethoprim-sulfamethoxazole and tetracycline.
The E. coli plasmids
In silico analyses of the genomes from the seven E. coli isolates by PlasmidFinder detected seven different plasmid replicons in the three isolates representing strain 1: Incl1, IncFII (pRSB107), IncQ1, IncFIA, IncFIB (AP001918), Col8282, ColpVC (Table 2). This indicates that these three isolates contain several (up to seven) different plasmids. In addition, another IncFII plasmid replicon was found in one of the strain 1 isolates (isolate 433-tz). The three isolates representing strain 2 contained three plasmid replicons: Incl1, IncFIA, Col (MG828), whereas isolate 431-Tz (strain 3) contained one Incl1 replicon only (Table 2).
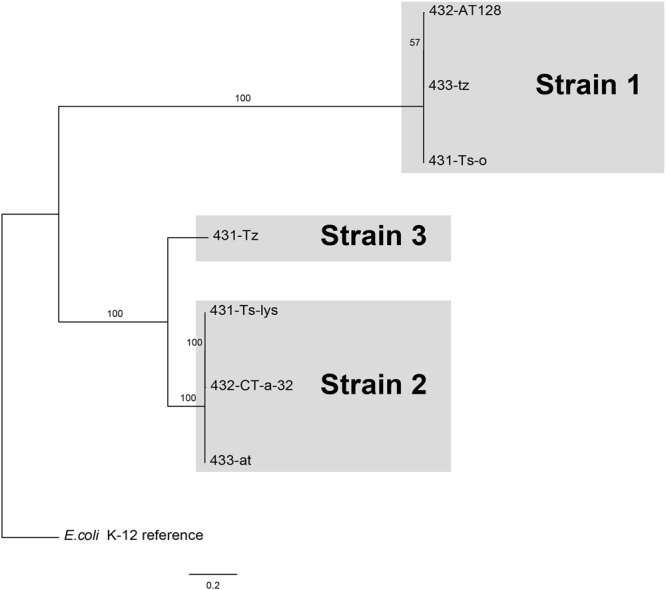
All the assembled bla CTX-M carrying plasmids from the seven E. coli isolates were Incl1 plasmids representing sequence type ST3. A Mauve comparison indicates that all the assembled plasmid sequences were almost identical, but with some differences among them located in delimited variable regions (Fig. 3).
Figure 3.
A Mauve comparison of seven bla CTX-M-1-containing Incl1/ST3 plasmids extracted in silico from seven E. coli isolates representing three different strains, and a reference plasmid (pC49–108, accession no. KJ484638). The height of the coloured segments indicates the degree of similarity between the plasmids where low height/missing region designates low similarity or absence of sequence. The label of each plasmid is located below the corresponding plasmid sequence.
All seven Incl1 plasmids shared a common 101 kb nucleotide sequence, which constitutes a core backbone of the complete 115 kb plasmid sequence (88% coverage). A corresponding SNP analysis based on the plasmid sequences (including the reference pC49–108) resulted in only four SNP differences within the backbone. Genes associated with conjugation (e.g. traC and pil genes) were detected within this common backbone. A list of annotated genes found in each plasmid is shown in Supplementary Table S2.
Comparison of the annotated plasmids with respect to the variable regions (nucleotide sequences not shared by all the plasmids) showed that these regions contained different genes, including genes encoding transposases and integrases. All three plasmids from the isolates belonging to strain 2 (the most complete plasmids) contained genes encoding TnpA transposase, transposase for Tn21 transposon, TnpR resolvase, and an integrase/recombinase (Supplementary Table S2). Corresponding genes were not found in the four plasmids from the other two E. coli strains (strain 1 and 3) that contained larger deletion blocks (Fig. 3).
Due to the close nucleotide similarity between the plasmids we created a gene presence- absence heat map of all plasmids in the present study, including the pC49–108 reference sequence, consisting of genes not included in the core backbone. From Fig. 4 it can be seen that the plasmids from E. coli strains 1 and 2 cluster according to their corresponding strain, while the plasmid from strain 3 clusters closely with the GenBank reference plasmid.
Figure 4.
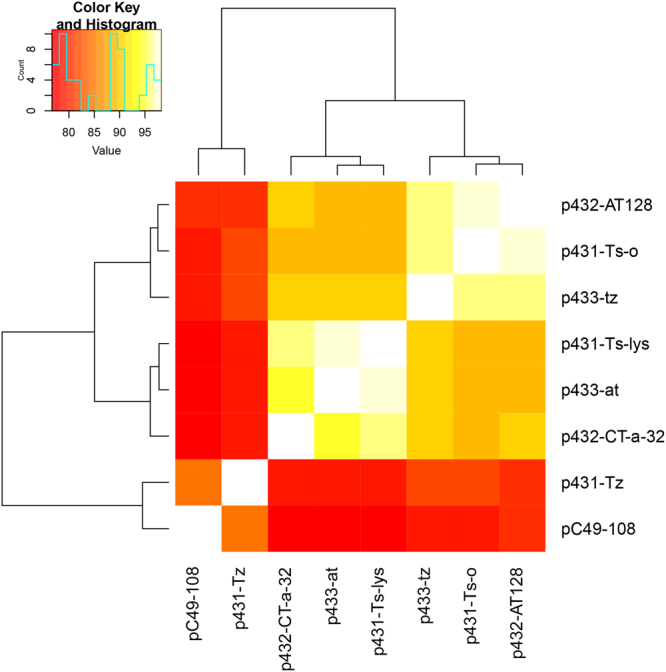
Gene presence-absence heat map of seven bla CTX-M-1-carrying Incl1/ST3 plasmids extracted from seven E. coli isolates and a reference plasmid (pC49–108, accession number KJ484638) obtained from the NCBI database. The key legend top left designates % of the genes common to the plasmids, exempting core backbone genes present in all.
A further interrogation of the plasmids available in public repositories that resemble those in the present study the most, indicates that pC49–108, and to a lesser degree pH2291–112 (Accession number KJ484629), pC59–112 (Accession number KJ484637), pC60–108 (Accession number KJ484635) are the closest. These are all Incl1/ST3 plasmids harbouring bla CTX-M-1 detected in E. coli isolates from humans and chicken45.
ResFinder detected no other resistance genes in any of the bla CTX-M-1 containing Incl1 plasmids from the seven isolates. This is in accordance with the phenotypic resistance profile of the E. coli isolate 431-Tz (susceptible to all the non-beta-lactam antibiotics tested), which harboured no other plasmid replicons than Incl1 (Table 2). dfrA genes in combination with sul genes were detected by ResFinder in all the six isolates representing strain 1 and strain 2 that were resistant to trimethoprim-sulfamethoxazole. tet genes were detected in the three tetracycline resistant strain 2 isolates (Table 2). These genes are probably located on some of the other plasmids detected in these strains (Table 2).
Discussion
In this study we explored seven ESBL-producing E. coli isolates and their corresponding bla CTX-M-1-carrying plasmids isolated from faecal samples from one cystic fibrosis patient at three different time points. The assessment of the isolates and the plasmids was exclusively based on WGS analyses. Assembly of plasmids from WGS short reads is challenging20, and complete reconstruction is often not possible due to the presence of repeat sequences, especially in large plasmids ( > 50 kbp)46. Here we aimed to reconstruct plasmid sequences by combining de novo assembly and reference-based read mapping relying on the successful detection of a reference plasmid (pC49–108) in the NCBI databases with a high degree of similarity with our plasmid sequences.
All seven ESBL-producing E. coli isolates carried bla CTX-M-1, but the isolates represented three different sequence types and serotypes. The phylogenetic analyses (Fig. 2) confirmed that this was in accordance with three genetically diverse groups of isolates that we designated strain 1, 2 and 3 (Table 2).
All seven bla CTX-M-1-carrying plasmids belonged to the same Inc group (Incl1) and represented the same pMLST (ST3). They shared a common 101 kb nucleotide core backbone containing only four SNP differences. This high degree of similarity between the plasmid backbones, also visualized by the Mauve comparison in Fig. 3, strongly suggests that they originate from a common plasmid that may have been transferred between the different E. coli strains. The environment within the human gut is favourable for horizontal gene transfer9,47, and the transfer of the bla CTX-M-1-containing plasmid is likely to have happened within the patient’s gut. It is well known that plasmids belonging to the Incl1 group often carry ESBL-coding genes and that they have the capacity of conjugational transfer48. Genes associated with conjugation (e.g. traC and pil genes, shown in Supplementary Table S2) were detected within the common backbone of all our plasmids and support the hypothesis that the plasmids probably have been transferred between different E. coli strains within the patient´s gut. The diversity of CTX-M-1 producing E. coli isolates found in our study is similar to findings in recent studies that have demonstrated great within-host diversity in faecally carried ESBL-producing E. coli isolates7,8. Stoesser et al. sequenced the genomes of 16 E. coli colonies from each of eight faecal samples from different individuals in Cambodia7. In two of the eight individuals, the same bla CTX-M variant occurred in different E. coli clones, and/or different bla CTX-M variants occurred in the same clone. Similar findings were demonstrated by Jørgensen et al. in a longitudinal study of faecal carriage of ESBL-producing E. coli and Klebsiella pneumoniae 8; ESBL production commonly occurred in diverse strains within the same host, and the same bla CTX-M variant was detected in genetically different E. coli isolates from the same faecal sample. These findings suggest horizontal transfer of bla CTX-M within the gut, but none of these studies assessed the mobile genetic elements (e.g. plasmids) that may have been involved in such transmission. Conlan et al. studied transmission of plasmids by analysing WGS data obtained from several sequencing platforms. They detected bla KPC-carrying pKpQIL plasmids with a common backbone in several K. pneumoniae isolates representing two different STs and in an E. coli isolate from faecal samples collected from the same patient at different time points21. Horizontal transfer of resistance genes may be facilitated by antibiotic exposure49, and the extensive antibiotic exposure in our patient may have promoted transfer of bla CTX-M between different E. coli strains. Such antibiotic treatment may also select resistant (e.g. ESBL-producing) strains of enterobacteria and concomitantly supress dominant populations of anaerobic species in the gut, thus promoting cell-to-cell contact between enterobacteria that enhances HGT. Stecher et al. showed that gut inflammation could boost HGT between pathogenic and commensal Enterobacteriaceae 50. This may also be of relevance in patients with CF since this disease is associated with intestinal inflammation51–53.
The bla CTX-M-1-carrying plasmids contained variable regions with genes encoding transposases and integrases (Supplementary Table S2). Notably, the most complete plasmids, harboured by the strain 2 isolates, contained several genes associated with recombination and transposable elements that were not detected in the plasmids from strains 1 and 3. The plasmids from E. coli strains 1 and 3 contained deletion blocks (Fig. 3) that may indicate that recombination events have happened in the plasmids within the different hosts. The phylogenetic SNP analysis of the E. coli genomes (Fig. 2), without the putative plasmid sequences, indicates that the plasmids differ according to the phylogenetic topology of the genomes of the isolates harbouring them. The gene presence-absence heat map of the plasmids (Fig. 4) also show that the plasmids cluster according to the three different E. coli strains, suggesting that the plasmids may have adapted within their respective hosts. The differences between the groups of clustered plasmids shown in Fig. 4 are most likely due to deleted and/or acquired accessory genes.
The closer clustering of the plasmids discussed above, as compared to the pC49–108 reference, and the large shared backbone of all plasmids considered, may suggest what best can be described as an adaptive ability. It has been demonstrated that plasmids co-evolve with their hosts54,55, which may result in the loss of genes conferring fitness cost. In this respect it is interesting to note that the strain represented by the single 431-Tz isolate, that contained the plasmid with largest deletion blocks, was isolated at a later time point than the isolates representing the other strains. It is therefore tempting to speculate that the plasmid was introduced to one of these strains and subsequently transferred to the other strains where co-evolution with the respective host in each strain has resulted in deletion events in the plasmids. The heavy antibiotic exposure to the patient may also have promoted the adaptive events in the plasmids within the E. coli hosts, as described by Porse et al.54. In an experimental study they demonstrated adaptive evolution by deletion of a costly region from a multidrug resistant plasmid in E. coli during antibiotic exposure, and that the increased plasmid stability was maintained also after the antibiotic selection pressure was removed.
One limitation of the present study is the use of short read sequencing data to reconstruct large plasmids (>100 kb). Several investigators have demonstrated that it may be challenging to obtain correct assemblies of large plasmids from short reads46,56,57. The occurrence of multiple repetitive nucleotide sequences (e.g. transposons and IS-sequences) and/or recombination events, both known to be common in plasmids, are demanding obstacles to overcome. For instance, if resistance genes are flanked by repetitive sequences (e.g. transposon elements) that are longer than the read lengths obtained by short-read based sequencing, it can be difficult to determine the correct genetic context of the resistance genes57. Therefore, long-read based sequencing methodology (e.g. Single Molecule Real-time Sequencing (SMRT), Pacific Biosciences or Nanopore sequencing, Oxford Nanopore) may hold great promise in obtaining properly assembled and closed plasmids20. Without these methods available, and only relying on the short read sequencing approach used in the present study, there may be inconsistencies regarding the plasmid’s variable regions as well as reverse complemented regions, and the extracted plasmids cannot be considered as fully closed. However, all the plasmids in our study cluster according to the E. coli strain to which they belong (Fig. 4), although the cluster analysis is based only on genes from the plasmid’s variable regions. There may be a possibility that the plasmids extracted by our method are divided between multiple plasmids, which may appear as one contig from the assembled short read data, or that the plasmid backbone has been integrated into different plasmid segments. However, such segments would most likely have been detected during the contig extraction step (Fig. 1C) by inconsistencies between the plasmids of the multiple isolates. We acknowledge that this could be difficult to verify in studies including only single isolates. The consistency of the finding of bla CTX-M-1-carrying Incl1 plasmids sharing a common backbone in two different E. coli strains (strain 1 and 2) isolated from three consecutive faecal samples during a nine-months period, strongly supports that a common plasmid is present in the different strains. As Incl1 plasmids are known to have conjugational capacity48, it is not unlikely that the plasmid has been horizontally transferred between the two strains and even to or from a third strain. However, this cannot be proven due to the methodological limitations described. While the availability of long read sequencing technology is increasing, short read sequencing platforms are still far more commonly available. Thus, extraction of plasmids from short-read data, and methods facilitating this, will probably still be used for some time to come.
In summary, we reconstructed bla CTX-M-1 containing Incl1 plasmids in silico from E. coli whole genome sequenced short reads by combining de novo assembly and reference-based read mapping relying of the successful detection of a reference plasmid in the NCBI databases with a high degree of similarity with our plasmid sequences. Seven bla CTX-M-1-carrying plasmids extracted from isolates that represented three genetically diverse E. coli strains isolated from faecal samples from one individual shared a common backbone. The findings strongly suggest horizontal transfer of the bla CTX-M-1-carrying plasmid between different E. coli strains within the patient´s gut, although our results need to be interpreted with some caution due to the limitations associated with plasmid assembly from short-read sequencing data. The differences between the plasmids, indicative of recombination events, corresponded to the E. coli strain carrying them, indicating that the plasmids appear to have adapted to their respective E. coli hosts.
The study illustrates the within-host diversity of faecally carried resistant E. coli isolates and highlights the value of collecting several bacterial colonies from longitudinally collected samples to assess faecal carriage of resistant enterobacteria.
Electronic supplementary material
Acknowledgements
This work was supported by grants from the Southern and Eastern Norway Regional Health Authority (Helse Sør-Øst) (grant 2014071), Barnestiftelsen, Oslo University Hospital and the Norwegian Surveillance System for Antimicrobial Drug Resistance (NORM).
Author Contributions
P.K.K. and J.B. designed the work and wrote the manuscript. P.K.K. performed the bacteriological work and WGS analyses. J.B. developed the method for plasmid assembly, performed WGS analyses and created the figures. K.W.G. designed the original study and collected the clinical samples. K.A. performed the whole genome sequencing of the E. coli isolates and contributed to the creation of the figures. All authors (P.K.K., K.W.G., K.A., M.S., T.G.A., F.M. and J.B.) contributed to the interpretation of the results and reviewed the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-18659-2.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Woerther PL, Burdet C, Chachaty E, Andremont A. Trends in human fecal carriage of extended-spectrum beta-lactamases in the community: toward the globalization of CTX-M. Clin. Microbiol. Rev. 2013;26:744–758. doi: 10.1128/CMR.00023-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geser N, Stephan R, Korczak BM, Beutin L, Hachler H. Molecular identification of extended-spectrum-beta-lactamase genes from Enterobacteriaceae isolated from healthy human carriers in Switzerland. Antimicrob. Agents Chemother. 2012;56:1609–1612. doi: 10.1128/AAC.05539-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruppe E, et al. Clinical predictive values of extended-spectrum beta-lactamase carriage in patients admitted to medical wards. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31:319–325. doi: 10.1007/s10096-011-1313-z. [DOI] [PubMed] [Google Scholar]
- 4.Canton R, Gonzalez-Alba JM, Galan JC. CTX-M Enzymes: Origin and Diffusion. Frontiers in microbiology. 2012;3:110. doi: 10.3389/fmicb.2012.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez-Bano J, Lopez-Cerero L, Navarro MD, Diaz de Alba P, Pascual A. Faecal carriage of extended-spectrum beta-lactamase-producing Escherichia coli: prevalence, risk factors and molecular epidemiology. The Journal of antimicrobial chemotherapy. 2008;62:1142–1149. doi: 10.1093/jac/dkn293. [DOI] [PubMed] [Google Scholar]
- 6.Valverde A, et al. High rate of intestinal colonization with extended-spectrum-beta-lactamase-producing organisms in household contacts of infected community patients. J. Clin. Microbiol. 2008;46:2796–2799. doi: 10.1128/JCM.01008-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stoesser N, et al. Extensive Within-Host Diversity in Fecally Carried Extended-Spectrum-Beta-Lactamase-Producing Escherichia coli Isolates: Implications for Transmission Analyses. J. Clin. Microbiol. 2015;53:2122–2131. doi: 10.1128/JCM.00378-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jorgensen SB, et al. Fecal carriage of extended spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae after urinary tract infection - A three year prospective cohort study. PLoS One. 2017;12:e0173510. doi: 10.1371/journal.pone.0173510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huddleston JR. Horizontal gene transfer in the human gastrointestinal tract: potential spread of antibiotic resistance genes. Infection and drug resistance. 2014;7:167–176. doi: 10.2147/IDR.S48820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sender R, Fuchs S, Milo R. Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol. 2016;14:e1002533. doi: 10.1371/journal.pbio.1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorensen SJ, Bailey M, Hansen LH, Kroer N, Wuertz S. Studying plasmid horizontal transfer in situ: a critical review. Nature reviews. Microbiology. 2005;3:700–710. doi: 10.1038/nrmicro1232. [DOI] [PubMed] [Google Scholar]
- 12.Duval-Iflah Y, Raibaud P, Tancrede C, Rousseau M. R-plasmic transfer from Serratia liquefaciens to Escherichia coli in vitro and in vivo in the digestive tract of gnotobiotic mice associated with human fecal flora. Infect. Immun. 1980;28:981–990. doi: 10.1128/iai.28.3.981-990.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schjorring S, Struve C, Krogfelt KA. Transfer of antimicrobial resistance plasmids from Klebsiella pneumoniae to Escherichia coli in the mouse intestine. The Journal of antimicrobial chemotherapy. 2008;62:1086–1093. doi: 10.1093/jac/dkn323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faure S, Perrin-Guyomard A, Delmas JM, Chatre P, Laurentie M. Transfer of plasmid-mediated CTX-M-9 from Salmonella enterica serotype Virchow to Enterobacteriaceae in human flora-associated rats treated with cefixime. Antimicrob. Agents Chemother. 2010;54:164–169. doi: 10.1128/AAC.00310-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gottig S, Gruber TM, Stecher B, Wichelhaus TA, Kempf VA. In vivo horizontal gene transfer of the carbapenemase OXA-48 during a nosocomial outbreak. Clin. Infect. Dis. 2015;60:1808–1815. doi: 10.1093/cid/civ191. [DOI] [PubMed] [Google Scholar]
- 16.Lester CH, Frimodt-Moller N, Sorensen TL, Monnet DL, Hammerum AM. In vivo transfer of the vanA resistance gene from an Enterococcus faecium isolate of animal origin to an E. faecium isolate of human origin in the intestines of human volunteers. Antimicrob. Agents Chemother. 2006;50:596–599. doi: 10.1128/AAC.50.2.596-599.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trobos M, Lester CH, Olsen JE, Frimodt-Moller N, Hammerum AM. Natural transfer of sulphonamide and ampicillin resistance between Escherichia coli residing in the human intestine. The Journal of antimicrobial chemotherapy. 2009;63:80–86. doi: 10.1093/jac/dkn437. [DOI] [PubMed] [Google Scholar]
- 18.Karami N, et al. Transfer of an ampicillin resistance gene between two Escherichia coli strains in the bowel microbiota of an infant treated with antibiotics. The Journal of antimicrobial chemotherapy. 2007;60:1142–1145. doi: 10.1093/jac/dkm327. [DOI] [PubMed] [Google Scholar]
- 19.Carattoli A, et al. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob. Agents Chemother. 2014;58:3895–3903. doi: 10.1128/AAC.02412-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orlek A, et al. Plasmid Classification in an Era of Whole-Genome Sequencing: Application in Studies of Antibiotic ResistanceEpidemiology. Frontiers in microbiology. 2017;8:182. doi: 10.3389/fmicb.2017.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conlan, S. et al. Plasmid Dynamics in KPC-Positive Klebsiella pneumoniae during Long-Term Patient Colonization. mBio7, 10.1128/mBio.00742-16 (2016). [DOI] [PMC free article] [PubMed]
- 22.Willemsen I, et al. Retrospective identification of a previously undetected clinical case of OXA-48-producing K. pneumoniae and E. coli: the importance of adequate detection guidelines. Infection. 2016;44:107–110. doi: 10.1007/s15010-015-0805-7. [DOI] [PubMed] [Google Scholar]
- 23.Knudsen PK, et al. Impact of extensive antibiotic treatment on faecal carriage of antibiotic-resistant enterobacteria in children in a low resistance prevalence setting. PLoS One. 2017;12:e0187618. doi: 10.1371/journal.pone.0187618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gammelsrud KW, Knudsen PK, Hoiby EA. A novel Direct MIC-gradient Strip Method to screen for antibiotic-resistant faecal Enterobacteriaceae. J. Microbiol. Methods. 2016;129:94–97. doi: 10.1016/j.mimet.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nikolenko SI, Korobeynikov AI, Alekseyev MA. BayesHammer: Bayesian clustering for error correction in single-cell sequencing. BMC Genomics. 2013;14(Suppl 1):S7. doi: 10.1186/1471-2164-14-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bankevich A, et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012;19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Antipov D, et al. plasmidSPAdes: assembling plasmids from whole genome sequencing data. Bioinformatics. 2016;32:3380–3387. doi: 10.1093/bioinformatics/btv688. [DOI] [PubMed] [Google Scholar]
- 29.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J. Mol. Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 30.Galardini M, Mengoni A, Bazzicalupo M. Mapping contigs using CONTIGuator. Methods Mol. Biol. 2015;1231:163–176. doi: 10.1007/978-1-4939-1720-4_11. [DOI] [PubMed] [Google Scholar]
- 31.Carver TJ, et al. ACT: the Artemis Comparison Tool. Bioinformatics. 2005;21:3422–3423. doi: 10.1093/bioinformatics/bti553. [DOI] [PubMed] [Google Scholar]
- 32.Langmead B, Salzberg SL. Fast gapped-read alignment with Bowtie 2. Nature methods. 2012;9:357–359. doi: 10.1038/nmeth.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li H, et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics. 2009;25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zankari E, et al. Identification of acquired antimicrobial resistance genes. The Journal of antimicrobial chemotherapy. 2012;67:2640–2644. doi: 10.1093/jac/dks261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larsen MV, et al. Multilocus sequence typing of total-genome-sequenced bacteria. J. Clin. Microbiol. 2012;50:1355–1361. doi: 10.1128/JCM.06094-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joensen KG, Tetzschner AM, Iguchi A, Aarestrup FM, Scheutz F. Rapid and Easy In Silico Serotyping of Escherichia coli Isolates by Use of Whole-Genome Sequencing Data. J. Clin. Microbiol. 2015;53:2410–2426. doi: 10.1128/JCM.00008-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Treangen TJ, Ondov BD, Koren S, Phillippy AM. The Harvest suite for rapid core-genome alignment and visualization of thousands of intraspecific microbial genomes. Genome Biol. 2014;15:524. doi: 10.1186/s13059-014-0524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Croucher NJ, et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 2015;43:e15. doi: 10.1093/nar/gku1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stamatakis A. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics. 2014;30:1312–1313. doi: 10.1093/bioinformatics/btu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guindon S, et al. New algorithms and methods to estimate maximum-likelihood phylogenies: assessing the performance of PhyML 3.0. Syst. Biol. 2010;59:307–321. doi: 10.1093/sysbio/syq010. [DOI] [PubMed] [Google Scholar]
- 41.Paradis E, Claude J, Strimmer K. APE: Analyses of Phylogenetics and Evolution in R language. Bioinformatics. 2004;20:289–290. doi: 10.1093/bioinformatics/btg412. [DOI] [PubMed] [Google Scholar]
- 42.Page AJ, et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics. 2015;31:3691–3693. doi: 10.1093/bioinformatics/btv421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Darling AC, Mau B, Blattner FR, Perna NT. Mauve: multiple alignment of conserved genomic sequence with rearrangements. Genome Res. 2004;14:1394–1403. doi: 10.1101/gr.2289704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30:2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 45.Wang J, et al. Nucleotide sequences of 16 transmissible plasmids identified in nine multidrug-resistant Escherichia coli isolates expressing an ESBL phenotype isolated from food-producing animals and healthy humans. The Journal of antimicrobial chemotherapy. 2014;69:2658–2668. doi: 10.1093/jac/dku206. [DOI] [PubMed] [Google Scholar]
- 46.Arredondo-Alonso, S., van Schaik, W., Willems, R. J. & Schürch, A. C. On the (Im)possibility to Reconstruct Plasmids from Whole Genome Short-Read SequencingData. bioRxiv, 1-18, 10.1101/086744 (2016).
- 47.van Schaik W. The human gut resistome. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015;370:20140087. doi: 10.1098/rstb.2014.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carattoli A. Resistance plasmid families in Enterobacteriaceae. Antimicrob. Agents Chemother. 2009;53:2227–2238. doi: 10.1128/AAC.01707-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beaber JW, Hochhut B, Waldor MK. SOS response promotes horizontal dissemination of antibiotic resistance genes. Nature. 2004;427:72–74. doi: 10.1038/nature02241. [DOI] [PubMed] [Google Scholar]
- 50.Stecher B, et al. Gut inflammation can boost horizontal gene transfer between pathogenic and commensal Enterobacteriaceae. Proc. Natl. Acad. Sci. USA. 2012;109:1269–1274. doi: 10.1073/pnas.1113246109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smyth RL, Croft NM, O’Hea U, Marshall TG, Ferguson A. Intestinal inflammation in cystic fibrosis. Arch. Dis. Child. 2000;82:394–399. doi: 10.1136/adc.82.5.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bruzzese E, et al. Intestinal inflammation is a frequent feature of cystic fibrosis and is reduced by probiotic administration. Aliment. Pharmacol. Ther. 2004;20:813–819. doi: 10.1111/j.1365-2036.2004.02174.x. [DOI] [PubMed] [Google Scholar]
- 53.Munck A. Cystic fibrosis: evidence for gut inflammation. Int. J. Biochem. Cell Biol. 2014;52:180–183. doi: 10.1016/j.biocel.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 54.Porse A, Schonning K, Munck C, Sommer MO. Survival and Evolution of a Large Multidrug Resistance Plasmid in New Clinical Bacterial Hosts. Mol. Biol. Evol. 2016;33:2860–2873. doi: 10.1093/molbev/msw163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Norberg P, Bergstrom M, Jethava V, Dubhashi D, Hermansson M. The IncP-1 plasmid backbone adapts to different host bacterial species and evolves through homologous recombination. Nature communications. 2011;2:268. doi: 10.1038/ncomms1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Conlan S, et al. Single-molecule sequencing to track plasmid diversity of hospital-associated carbapenemase-producing Enterobacteriaceae. Sci. Transl. Med. 2014;6:254ra126. doi: 10.1126/scitranslmed.3009845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sheppard AE, et al. Nested Russian Doll-Like Genetic Mobility Drives Rapid Dissemination of the Carbapenem Resistance Gene blaKPC. Antimicrob. Agents Chemother. 2016;60:3767–3778. doi: 10.1128/AAC.00464-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The E. coli genome short reads that were generated and analysed in this work are deposited to the European Nucleotide Archive (ENA), and the accession numbers of the seven genomes are shown in Supplementary Table S1. The fasta-files containing the seven assembled plasmid sequences are also available in the Supplementary Information.